Rash
Medically reviewed by Drugs.com. Last updated on Jan 3, 2024.
What is a Rash?

A rash is a temporary eruption or discoloration of the skin and is often inflamed or swollen. Rashes come in many forms and levels of severity, and they last for different amounts of time. Some common causes of rashes include the following.
Infections
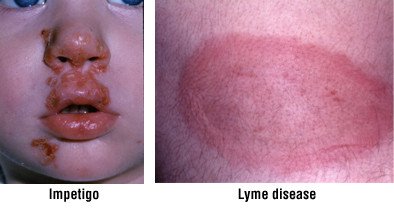
This broad category covers a wide range of illnesses, including:
- Viral infections, such as measles, rubella, roseola, fifth disease, varicella zoster, herpes or shingles

- Bacterial infections, such as impetigo, scarlet fever or Lyme disease
|
|
-
Fungal infections, such as jock itch (a fungal infection in the groin region)
-
Many others
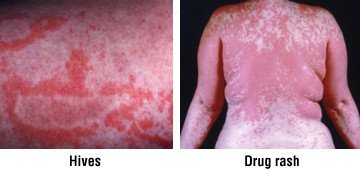
Allergic reactions
These can be triggered by:
- Medications, including antibiotics, seizure medications and diuretics
- Topical skin products, such as cosmetics, perfumes or skin creams
- Foods, especially peanuts, seafood and eggs
-
Insect stings (including bees, wasps and hornets)
Local irritants
This category includes diaper rash (caused by prolonged skin contact with urine and stool) and rashes caused by contact with harsh chemicals, such as laundry soaps and fabric softeners.

Poisonous plants
Poison ivy, poison oak and poison sumac share a highly allergenic sap resin that can cause allergic rashes in 70% of people exposed to it.
|
|
Autoimmune disorders
This category includes systemic lupus erythematosus (SLE or lupus), dermatomyositis and scleroderma, disorders in which the body's immune defenses mistakenly attack healthy areas of the body, including the skin.
Symptoms
Although rash is easily recognized, all rashes are not the same. Rashes vary in their appearance, timing, location or distribution, and duration. In general, rashes can be described as:
- Macular — Flat, red spots
- Papular — Small, raised, solid bumps
- Macular and papular — A combination
- Papulosquamous — A combination of papules and scaly areas
- Vesicular — Small, raised, fluid-filled blisters
Additional signs and symptoms that sometimes accompany rashes include:
- Fever
- Swollen lymph nodes (swollen glands)
- Signs of a severe allergic, potentially life-threatening reaction called anaphylaxis, which requires immediate emergency medical attention: difficulty breathing, hives, vomiting, abdominal cramps, rapid drop in blood pressure, confusion and unconsciousness
- Signs of an autoimmune disorder, such as lupus (may include fatigue, poor appetite, fever, joint swelling) or dermatomyositis (often includes weak muscles, swelling and violet discoloration of the eyelids and difficulty rising after sitting)
Diagnosis
Your doctor will ask you about your medical history, including your history of allergies and your work history, to check for possible exposure to chemical irritants or to people with infections. Your doctor also may ask specific questions about your rash, including:
- When it began — Did the rash appear after you ate a new food, tried a new skin care product or took a new medication?
- Location and pattern — Does the rash affect only sun-exposed areas or only areas in direct contact with gloves, shoes, goggles or face masks (as would be expected with allergic reactions to a chemical in the item)? Does it form a "butterfly" pattern over the cheeks and nose (a classic sign of lupus), or does it produce a bright red "slapped cheek" pattern (a sign of fifth disease)? If you are a hiker, does it form linear streaks along the lower legs (a sign of poison ivy)?
- Duration — Did the rash appear and disappear within a day or two (as in roseola), or has it lasted for a week (as in fifth disease) or longer (as in SLE)?
- Occupational exposures — Are you a day care worker who may be exposed to children with rash-producing illnesses (measles, rubella, roseola, fifth disease)? Do you work or play near wooded areas where there is an increased risk of tick bites?
Your doctor may suspect a specific cause based on your medical history and the history of your rash. Your doctor will try to confirm this suspicion by examining the rash's appearance, location, pattern and any associated symptoms. In many cases, the results of your physical examination will clarify the diagnosis, and no further tests will be needed.
When required, additional testing may include:
- Blood tests — Although most viral rashes do not require specific identification of the virus, blood tests are available to identify some viruses and bacteria that cause rash-producing infections. Blood tests also may be done to check for autoimmune disorders.
- Patch tests — If your doctor suspects a local allergic reaction, he or she may conduct skin tests called patch tests. In these tests, tiny amounts of various chemicals are placed on your skin for two days to see if an allergic rash develops.
- Wood's lamp — A Wood's lamp is a black light used to help evaluate rashes. Depending on the specific reason for the rash, the light may cause the affected area of skin to glow red, pale blue, yellow or white.
- Tzanck test — In this test, a blister is opened and scraped to obtain a sample that is checked in a laboratory for signs of herpes virus infection.
- KOH preparation — In this test, a skin area that is suspected of having a fungal infection is scraped gently. Scraped material is placed on a slide, treated with KOH (potassium hydroxide) and examined under the microscope for signs of fungi.
- Skin biopsy — In this procedure, the skin is numbed and a sample of affected skin is removed and examined in a laboratory. Stitches may be required.
Expected Duration
How long a rash lasts depends on its cause. However, most rashes usually disappear within a few days. For example, the rash of a roseola viral infection usually lasts 1 to 2 days, whereas the rash of measles disappears within 6 to 7 days. Rashes caused by an antibiotic allergy may last 3 to 14 days, whereas diaper rash almost always clears up within 1 week (if diapers are changed frequently).
Rashes resulting from lupus or dermatomyositis may last for an extended period of time.
Prevention
Prevention depends on the cause of the rash:
- Infections — Check that you and your children are up-to-date in your routine immunizations. Wash your hands frequently, bathe regularly and avoid sharing clothing or personal grooming items with other people. To prevent Lyme disease, wear light-colored clothing that contrasts with the dark tick and covers most of your skin when you go into the woods. Use approved tick repellents. Be aware that you are more likely to be exposed to ticks in areas of the country where Lyme disease is common.
- Allergic reactions — Avoid the specific food, medicine, skin care products or cosmetics that you had a reaction to. Never take a medicine prescribed for someone else. f you suspect that you are allergic to insect stings, talk to your doctor. You might see an allergist for testing and possible desensitization therapy. You also may need a bee-sting kit, which contains emergency medication to prevent potentially life-threatening reactions. Make sure you know where the kit is at home and consider getting an extra one if you participate often in an outdoor sport. Keep the second in your sports bag.
- Local irritants — For diaper rash, change diapers as soon as they become wet or soiled. Make sure that your baby's bottom is completely clean and dry before closing up the fresh diaper. For sensitivity to chemicals in cleaning products, switch to laundry soaps and fabric softeners that are free of dyes and perfumes. For irritation due to cosmetics, use hypoallergenic products that contain fewer skin-irritating preservatives and fragrances.
- Poisonous plants — Learn to recognize poison ivy, poison oak and poison sumac. When you hike in the woods or do yard work, cover exposed arms and legs with long-sleeved shirts and long pants.
Treatment
Treatment depends on the cause of the rash:
- Infections — Bacterial infections are treated with antibiotics. Fungal infections are treated with antifungal medications. Many viral infections that cause rash will go away within several days and require no medication. Less often, antiviral drugs are necessary.
- Allergic reactions — A severe allergic reaction is a life-threatening medical emergency. It must be treated immediately with epinephrine, a medication that opens narrowed airways and raises dangerously low blood pressure. High doses of corticosteroids and antihistamines also are used. Localized allergic reactions can be treated with topical or oral corticosteroids, antihistamines and ice to relieve the itching and swelling.
- Local irritants — Diaper rash is treated by changing diapers frequently and using nonprescription creams or ointments that contain zinc oxide and mineral oil.
- Poisonous plants — The skin should be flushed thoroughly with warm water to remove the allergenic substance. Only then should you lather with soap and water. If you use soap immediately before flushing the skin with water, you are apt to spread the allergenic plant oil over your skin. Once you have washed off the oil, it cannot spread. The rash is often treated with prescription topical steroids. However, oral steroids may be needed for extensive rashes or rashes on the face.
- Autoimmune disorders — These illnesses are treated with corticosteroid and immunosuppressive drugs, medications that suppress the patient's overactive immune system.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
When To Call a Professional
Seek immediate medical attention if you begin to have difficulty breathing or develop hives, a fever, a fast pulse, confusion or nausea. These could be signs of a life-threatening allergic reaction.
Always consult your doctor promptly if a rash:
- Worsens
- Lasts longer than one week
- Shows signs of local infection (oozing, redness or swelling of the skin)
- Occurs together with fever, chills, swollen glands or other symptoms of infection (sore throat, cough, headache, nasal congestion, etc.)
- Occurs together with symptoms that suggest an autoimmune disorder, such as recurring fever, malaise, fatigue, unexplained weight loss or joint swelling
Prognosis
The outlook for most rashes is excellent, especially after the cause has been identified accurately.
In severe allergic reactions, a patient can die within minutes without immediate medical treatment. With proper treatment, recovery usually is complete. However, the patient remains at risk of future severe reactions if he or she is exposed to the same allergy-producing agent. For this reason, a prescription for a self-injection pen containing epinephrine for emergencies usually is recommended for people with severe allergies.
For long-term autoimmune conditions, rash is only one of a wide variety of symptoms. The prognosis depends on the type and severity of the autoimmune disease.
Additional Info
National Institute of Arthritis and Musculoskeletal and Skin Diseases
National Insitutes of Health
https://www.niams.nih.gov/
American Academy of Dermatology
https://www.aad.org/
American Academy of Allergy, Asthma & Immunology (AAAAI)
https://www.aaaai.org/
The Food Allergy & Anaphylaxis Network
https://www.foodallergy.org/
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.