SEARCH RESULTS FOR:
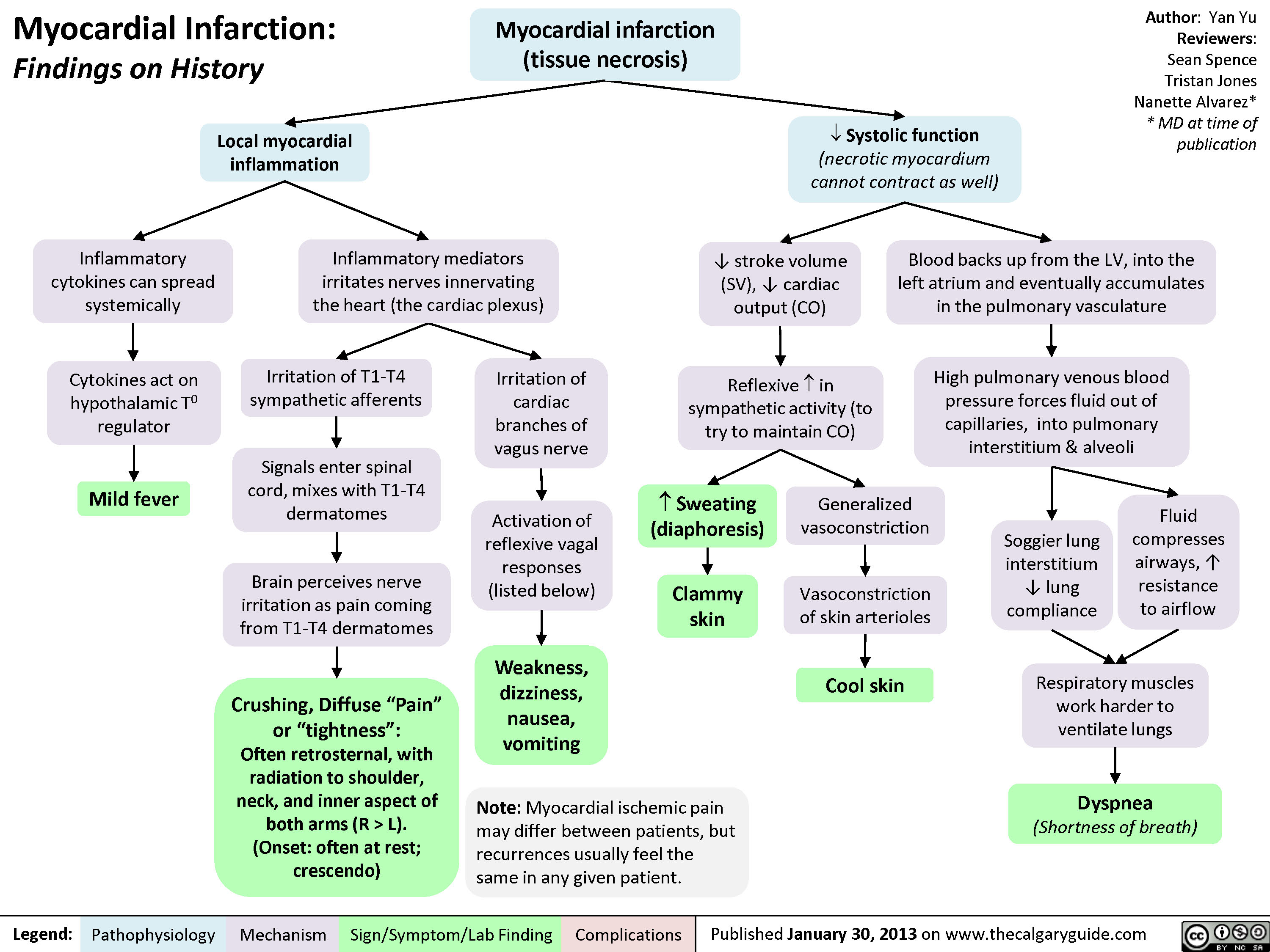
Myocardial Infarction: Findings on History
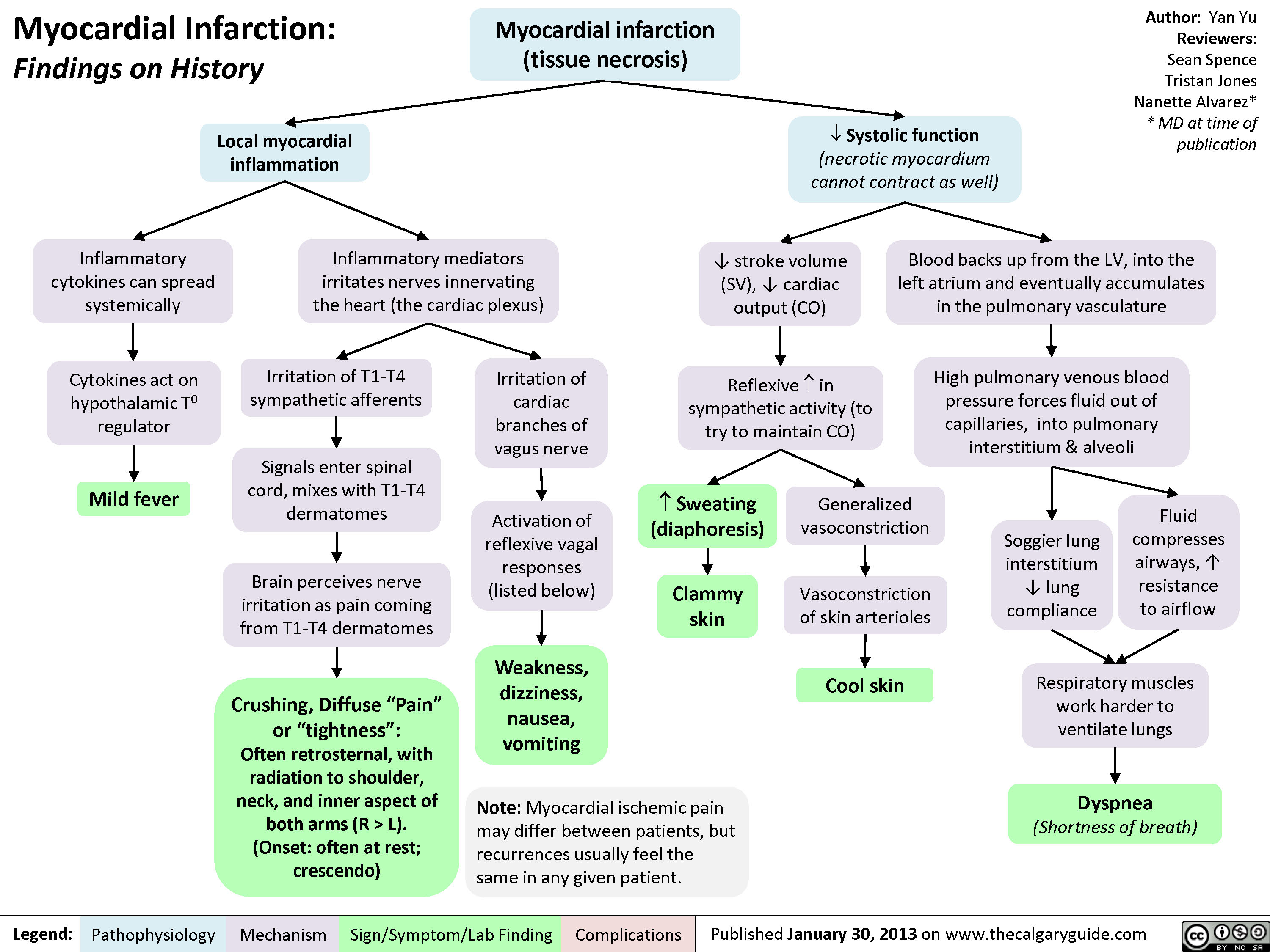 L).(Onset: often at rest; crescendo)Activation of reflexive vagal responses (listed below)Weakness, dizziness, nausea, vomitingInflammatory mediators irritates nerves innervating the heart (the cardiac plexus)Cytokines act on hypothalamic T0 regulatorMild fever? Sweating (diaphoresis)Inflammatory cytokines can spread systemicallyBrain perceives nerve irritation as pain coming from T1-T4 dermatomesBlood backs up from the LV, into the left atrium and eventually accumulates in the pulmonary vasculatureHigh pulmonary venous blood pressure forces fluid out of capillaries, into pulmonary interstitium & alveoliRespiratory muscles work harder to ventilate lungsSoggier lung interstitium ? lung complianceDyspnea(Shortness of breath)Fluid compresses airways, ? resistance to airflow
102 kB / 204 words" title="Yu Yan - MI Findings on History - FINAL.pptx -
Myocardial Infarction: Findings on HistoryLegend:Published January 30, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsAuthor: Yan YuReviewers:Sean SpenceTristan JonesNanette Alvarez** MD at time of publication Systolic function(necrotic myocardium cannot contract as well)Reflexive ? in sympathetic activity (to try to maintain CO)Clammy skin? stroke volume (SV), ? cardiac output (CO)Myocardial infarction (tissue necrosis)Note: Myocardial ischemic pain may differ between patients, but recurrences usually feel the same in any given patient.Generalized vasoconstrictionVasoconstriction of skin arteriolesCool skinLocal myocardial inflammationIrritation of T1-T4 sympathetic afferentsIrritation of cardiac branches of vagus nerveSignals enter spinal cord, mixes with T1-T4 dermatomesCrushing, Diffuse "Pain" or "tightness": Often retrosternal, with radiation to shoulder, neck, and inner aspect of both arms (R > L).(Onset: often at rest; crescendo)Activation of reflexive vagal responses (listed below)Weakness, dizziness, nausea, vomitingInflammatory mediators irritates nerves innervating the heart (the cardiac plexus)Cytokines act on hypothalamic T0 regulatorMild fever? Sweating (diaphoresis)Inflammatory cytokines can spread systemicallyBrain perceives nerve irritation as pain coming from T1-T4 dermatomesBlood backs up from the LV, into the left atrium and eventually accumulates in the pulmonary vasculatureHigh pulmonary venous blood pressure forces fluid out of capillaries, into pulmonary interstitium & alveoliRespiratory muscles work harder to ventilate lungsSoggier lung interstitium ? lung complianceDyspnea(Shortness of breath)Fluid compresses airways, ? resistance to airflow
102 kB / 204 words" />
L).(Onset: often at rest; crescendo)Activation of reflexive vagal responses (listed below)Weakness, dizziness, nausea, vomitingInflammatory mediators irritates nerves innervating the heart (the cardiac plexus)Cytokines act on hypothalamic T0 regulatorMild fever? Sweating (diaphoresis)Inflammatory cytokines can spread systemicallyBrain perceives nerve irritation as pain coming from T1-T4 dermatomesBlood backs up from the LV, into the left atrium and eventually accumulates in the pulmonary vasculatureHigh pulmonary venous blood pressure forces fluid out of capillaries, into pulmonary interstitium & alveoliRespiratory muscles work harder to ventilate lungsSoggier lung interstitium ? lung complianceDyspnea(Shortness of breath)Fluid compresses airways, ? resistance to airflow
102 kB / 204 words" title="Yu Yan - MI Findings on History - FINAL.pptx -
Myocardial Infarction: Findings on HistoryLegend:Published January 30, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsAuthor: Yan YuReviewers:Sean SpenceTristan JonesNanette Alvarez** MD at time of publication Systolic function(necrotic myocardium cannot contract as well)Reflexive ? in sympathetic activity (to try to maintain CO)Clammy skin? stroke volume (SV), ? cardiac output (CO)Myocardial infarction (tissue necrosis)Note: Myocardial ischemic pain may differ between patients, but recurrences usually feel the same in any given patient.Generalized vasoconstrictionVasoconstriction of skin arteriolesCool skinLocal myocardial inflammationIrritation of T1-T4 sympathetic afferentsIrritation of cardiac branches of vagus nerveSignals enter spinal cord, mixes with T1-T4 dermatomesCrushing, Diffuse "Pain" or "tightness": Often retrosternal, with radiation to shoulder, neck, and inner aspect of both arms (R > L).(Onset: often at rest; crescendo)Activation of reflexive vagal responses (listed below)Weakness, dizziness, nausea, vomitingInflammatory mediators irritates nerves innervating the heart (the cardiac plexus)Cytokines act on hypothalamic T0 regulatorMild fever? Sweating (diaphoresis)Inflammatory cytokines can spread systemicallyBrain perceives nerve irritation as pain coming from T1-T4 dermatomesBlood backs up from the LV, into the left atrium and eventually accumulates in the pulmonary vasculatureHigh pulmonary venous blood pressure forces fluid out of capillaries, into pulmonary interstitium & alveoliRespiratory muscles work harder to ventilate lungsSoggier lung interstitium ? lung complianceDyspnea(Shortness of breath)Fluid compresses airways, ? resistance to airflow
102 kB / 204 words" />
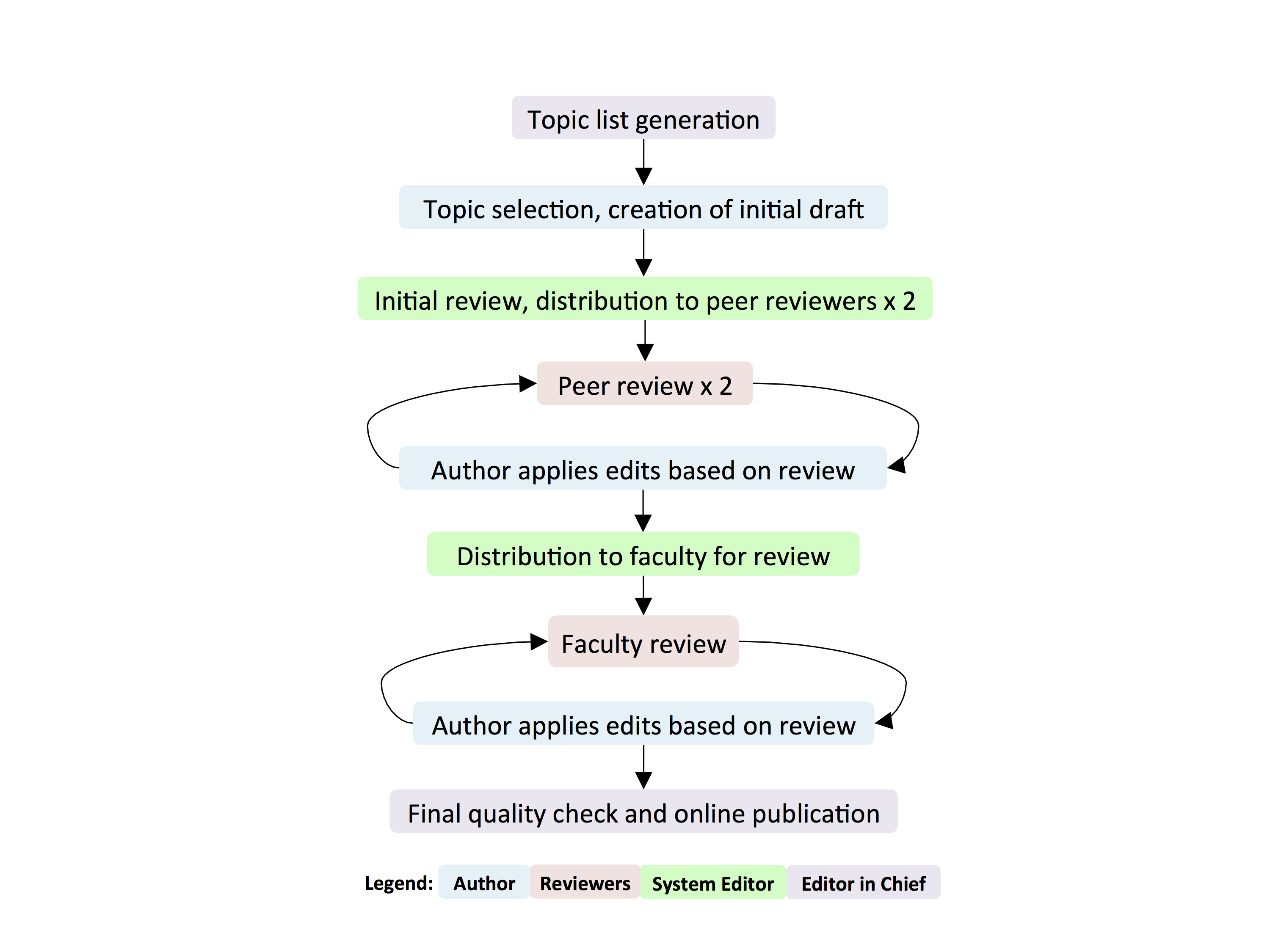
process
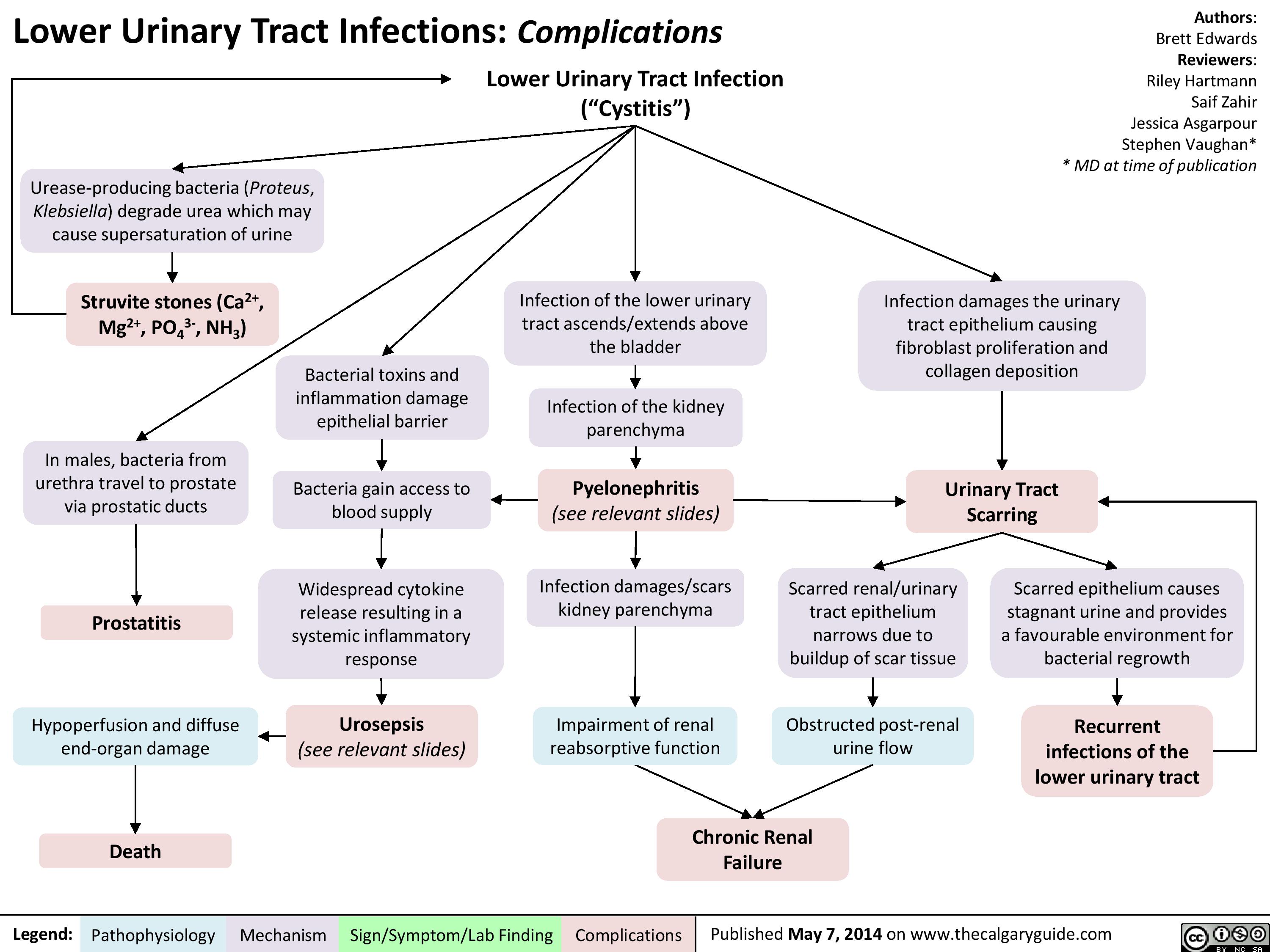
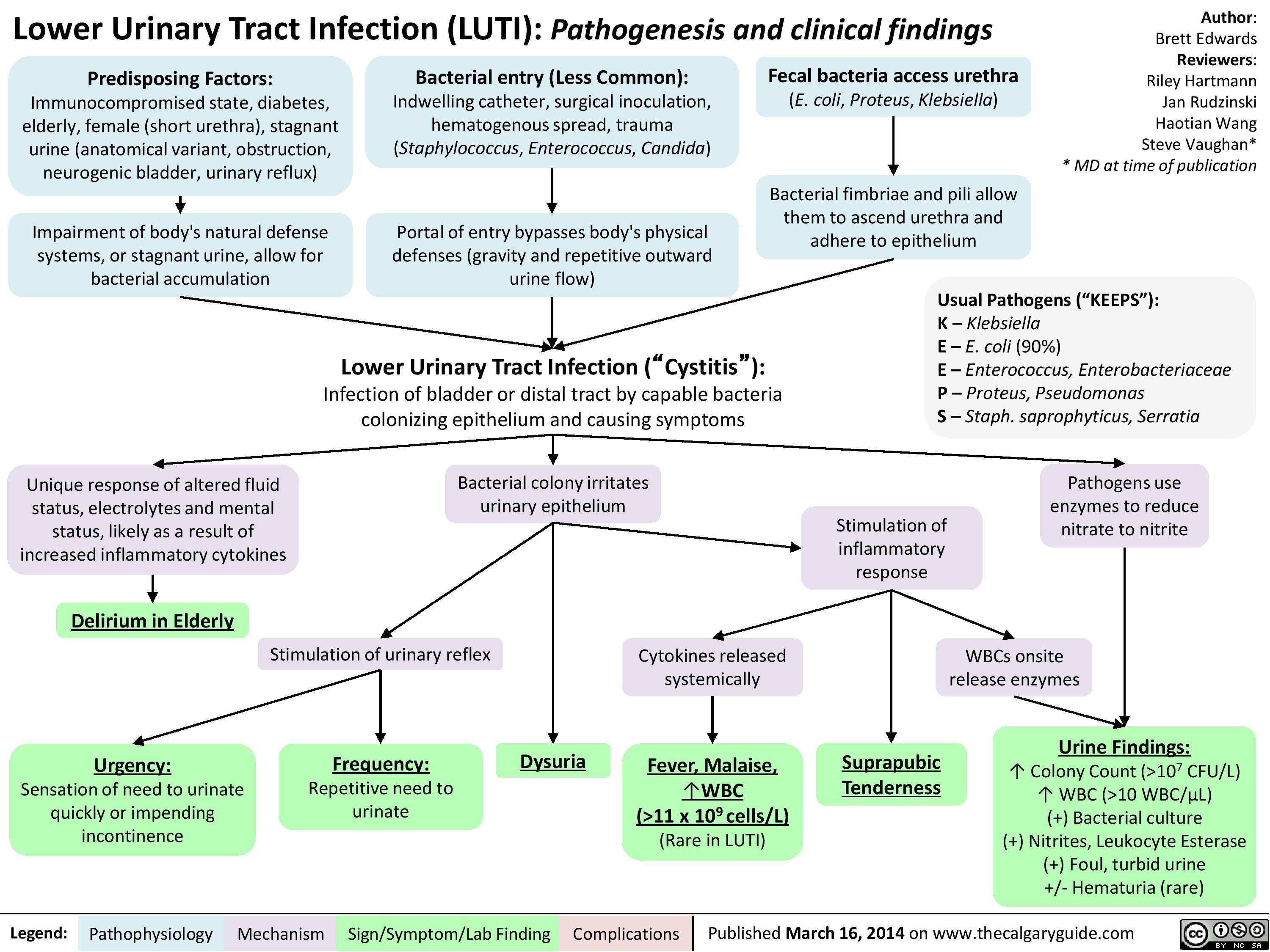
lower-urinary-tract-infections-complications
lower-urinary-tract-infection-pathogenesis-and-clinical-findings
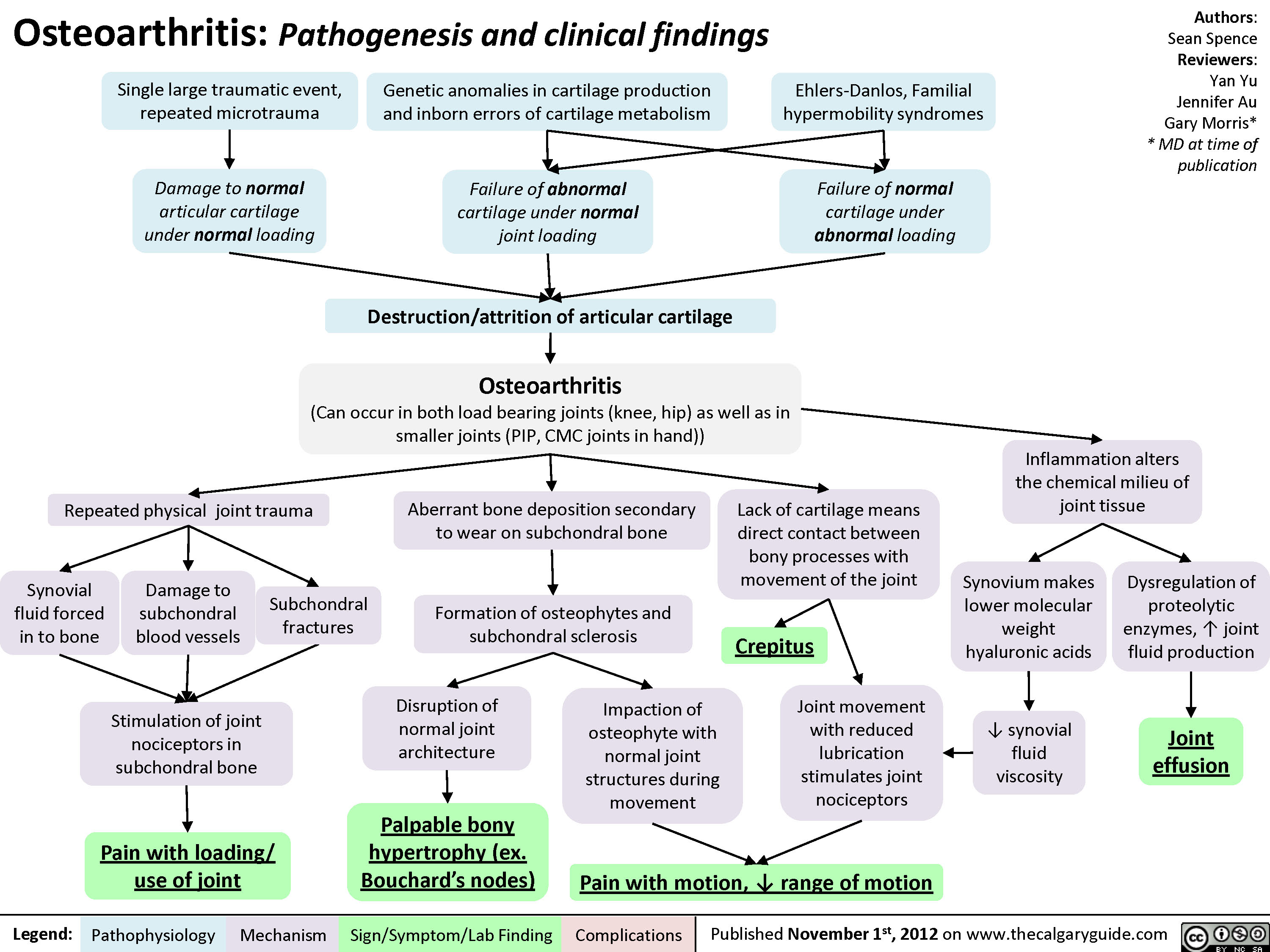
Osteoarthritis (OA): Clinical findings
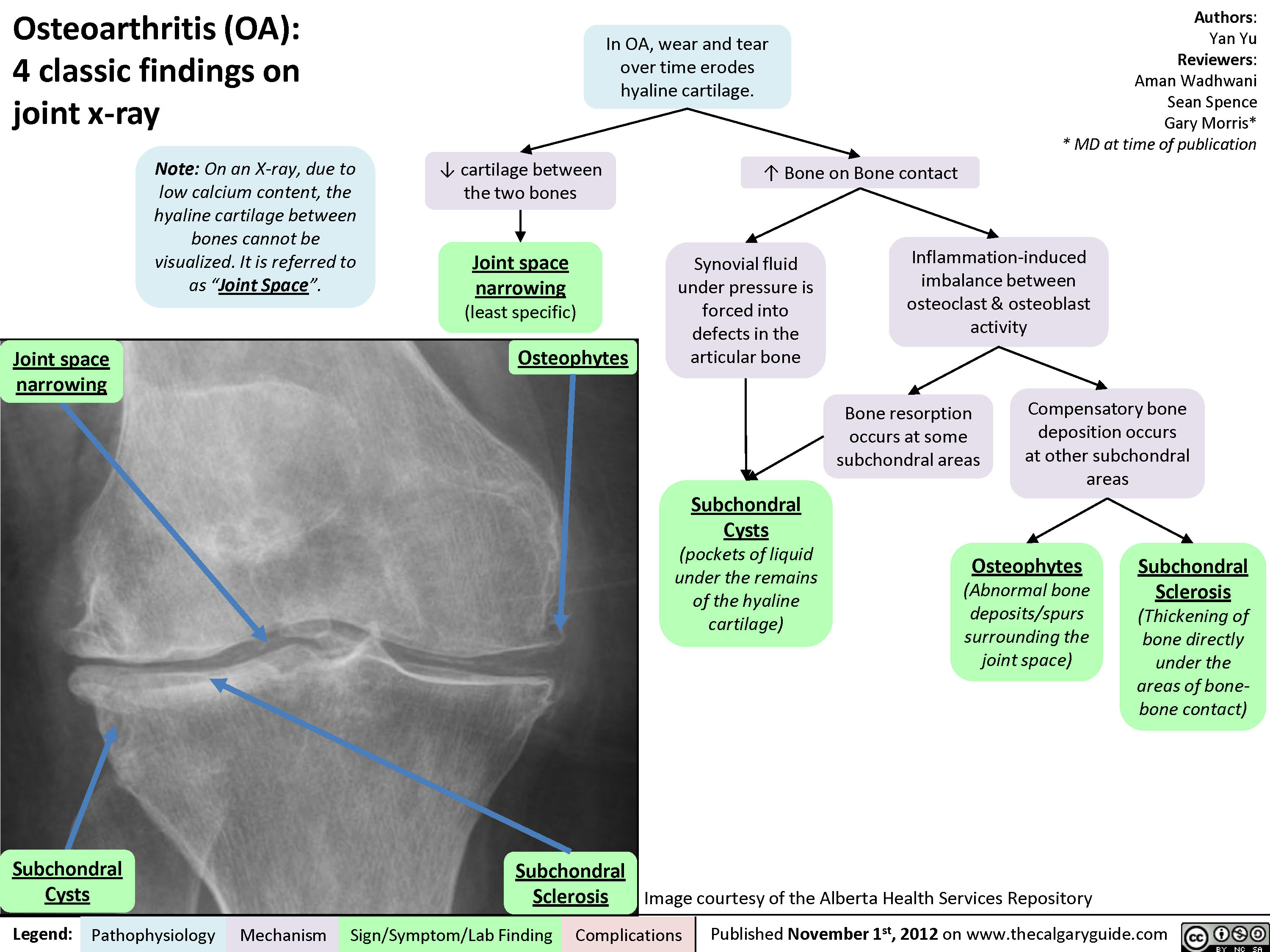
Osteoarthritis (OA): X-ray features
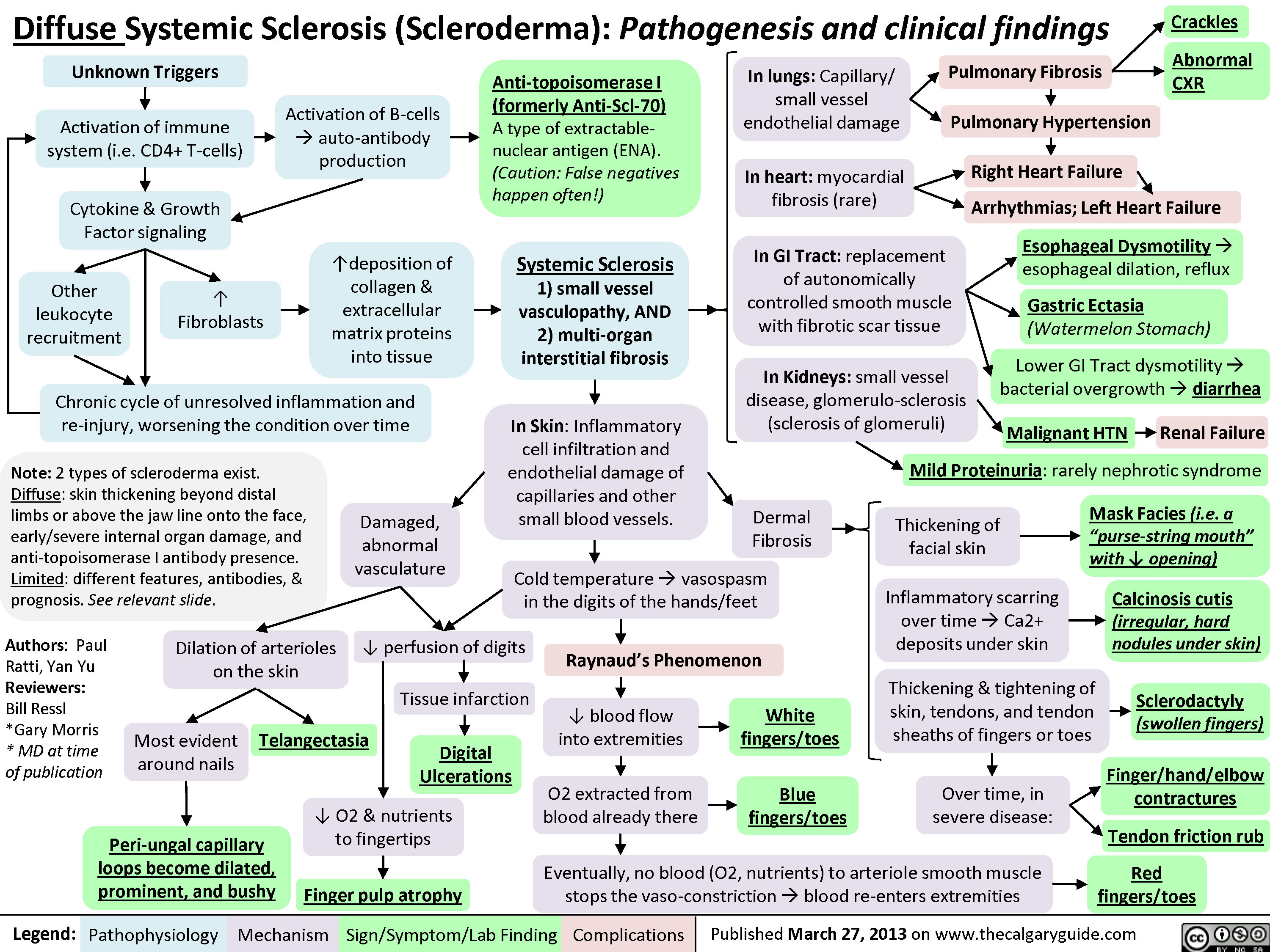
Diffuse Systemic Sclerosis (Scleroderma)
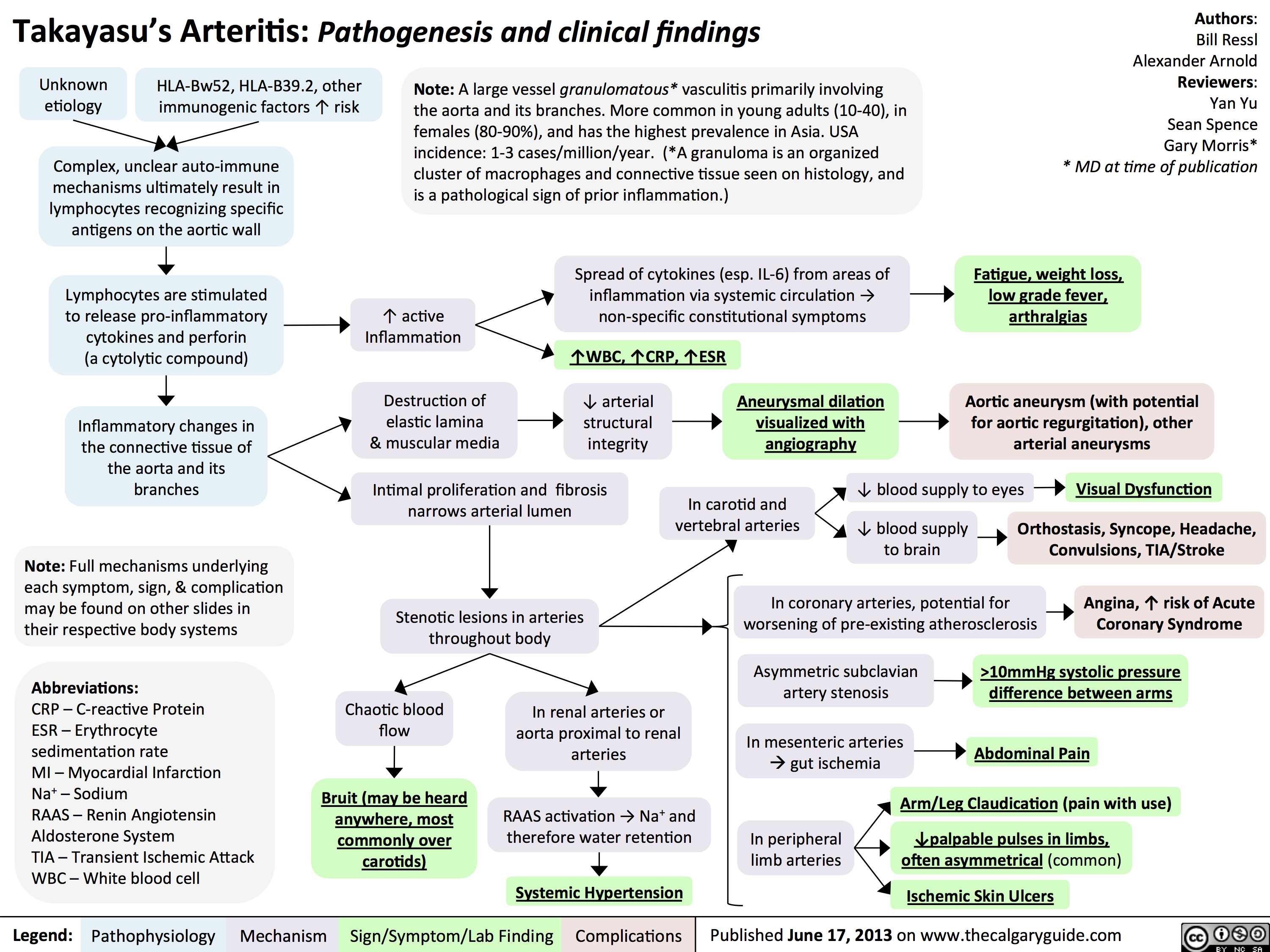
Takayasu's Arteritis: Pathogenesis and clinical findings
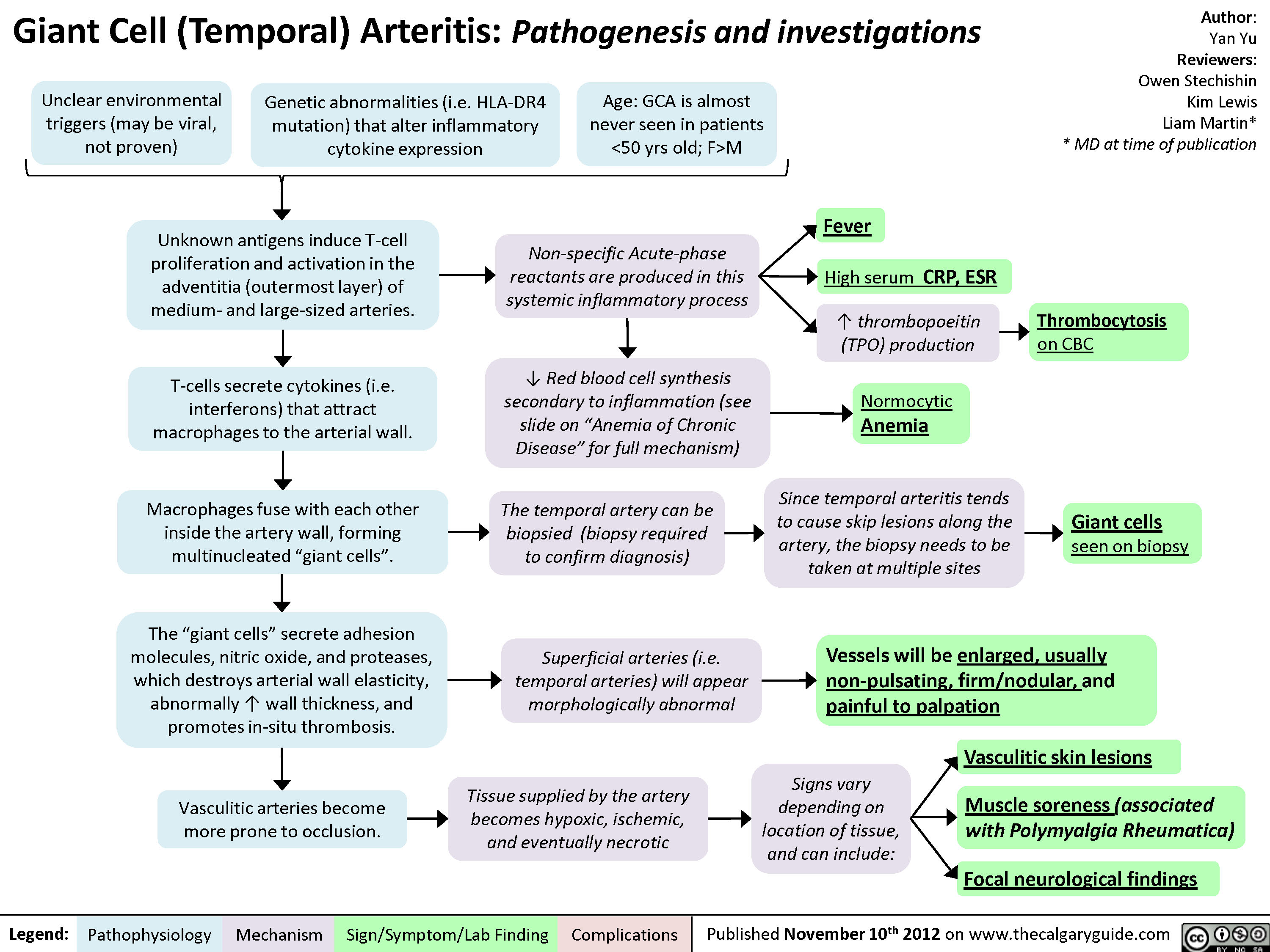
Giant Cell (Temporal) Arteritis: Pathogenesis and investigations

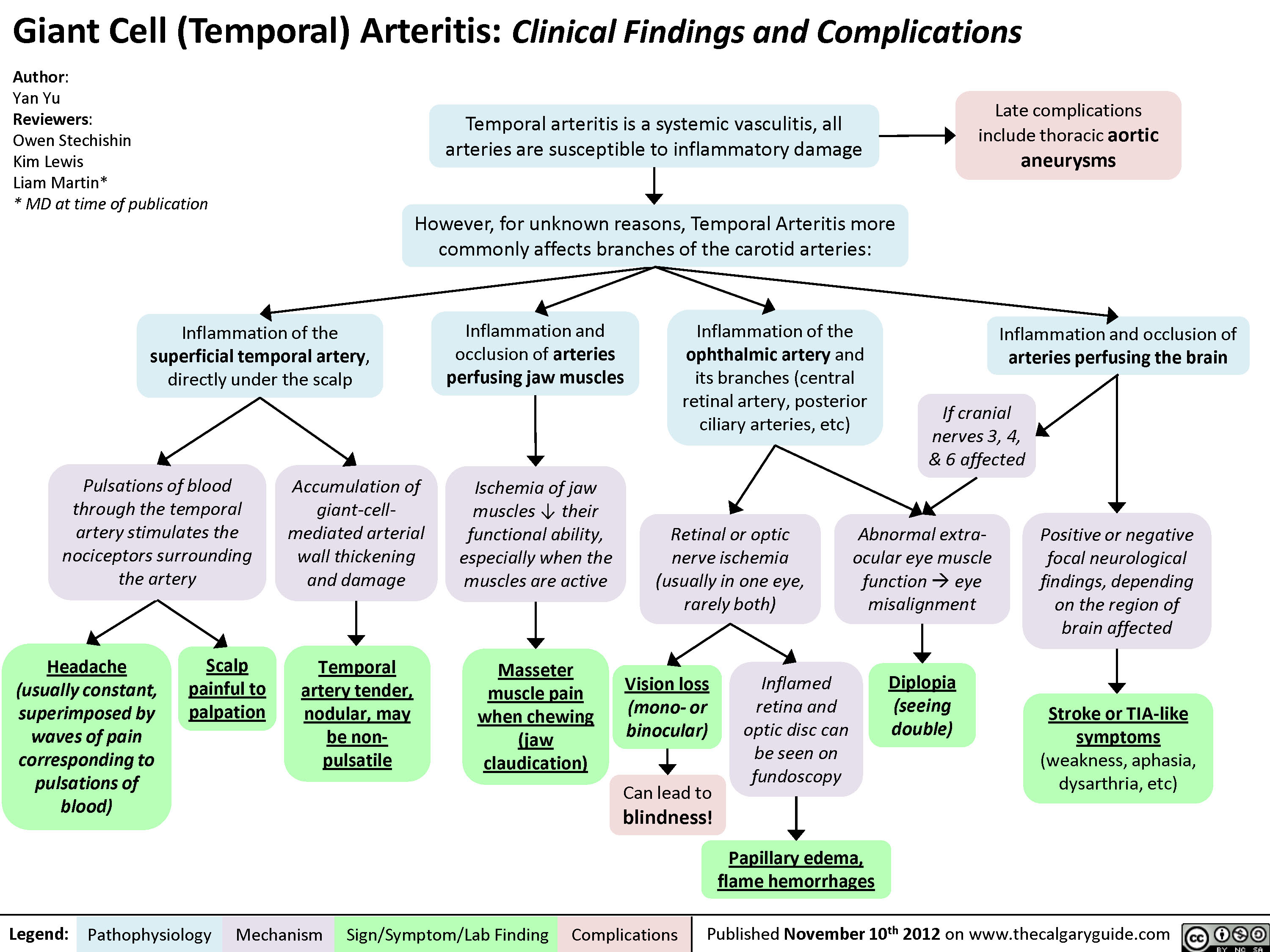
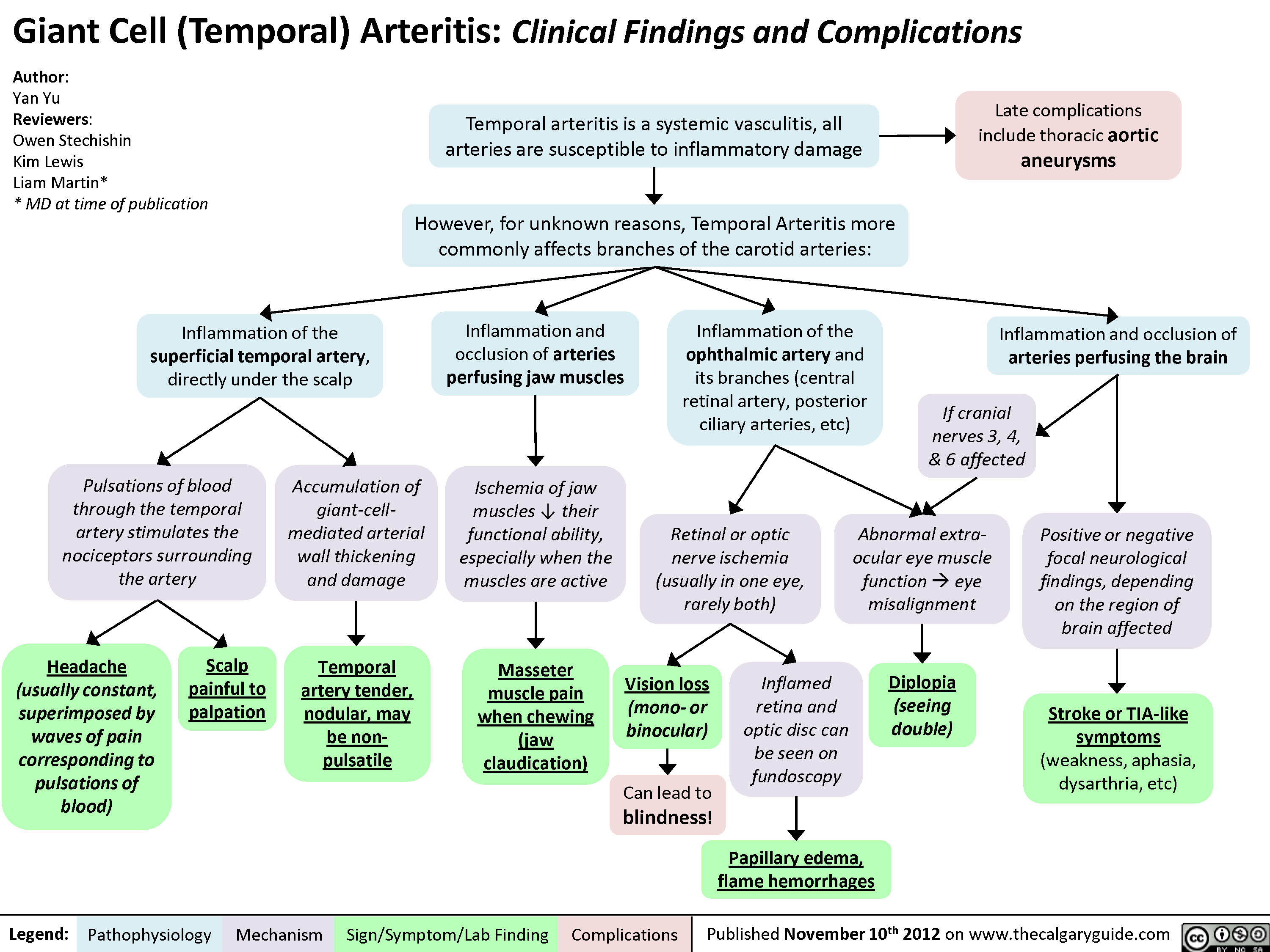
Giant Cell (Temporal) Arteritis: Clinical findings and Complications
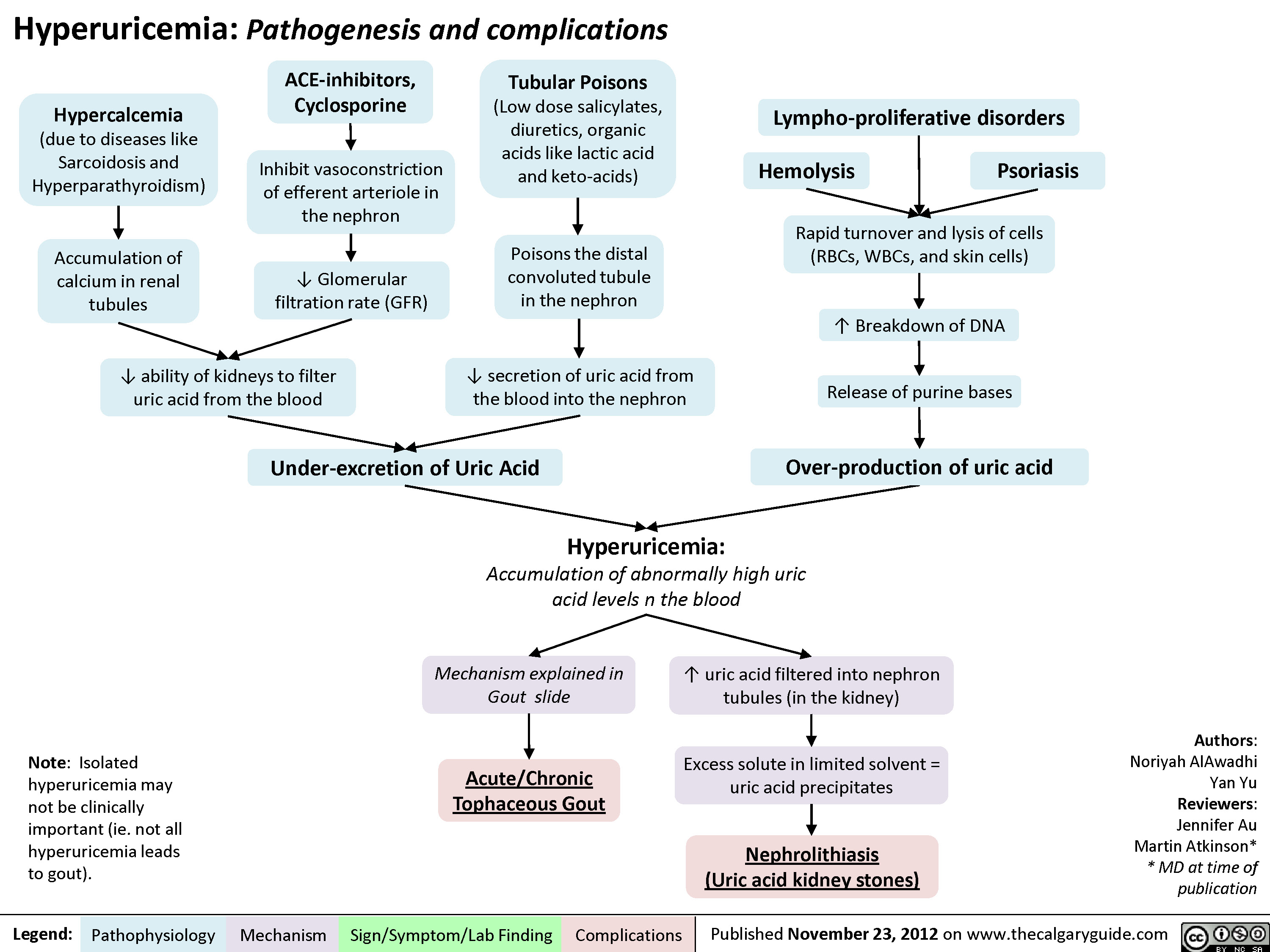
Hyperuricemia Pathogenesis and Complications
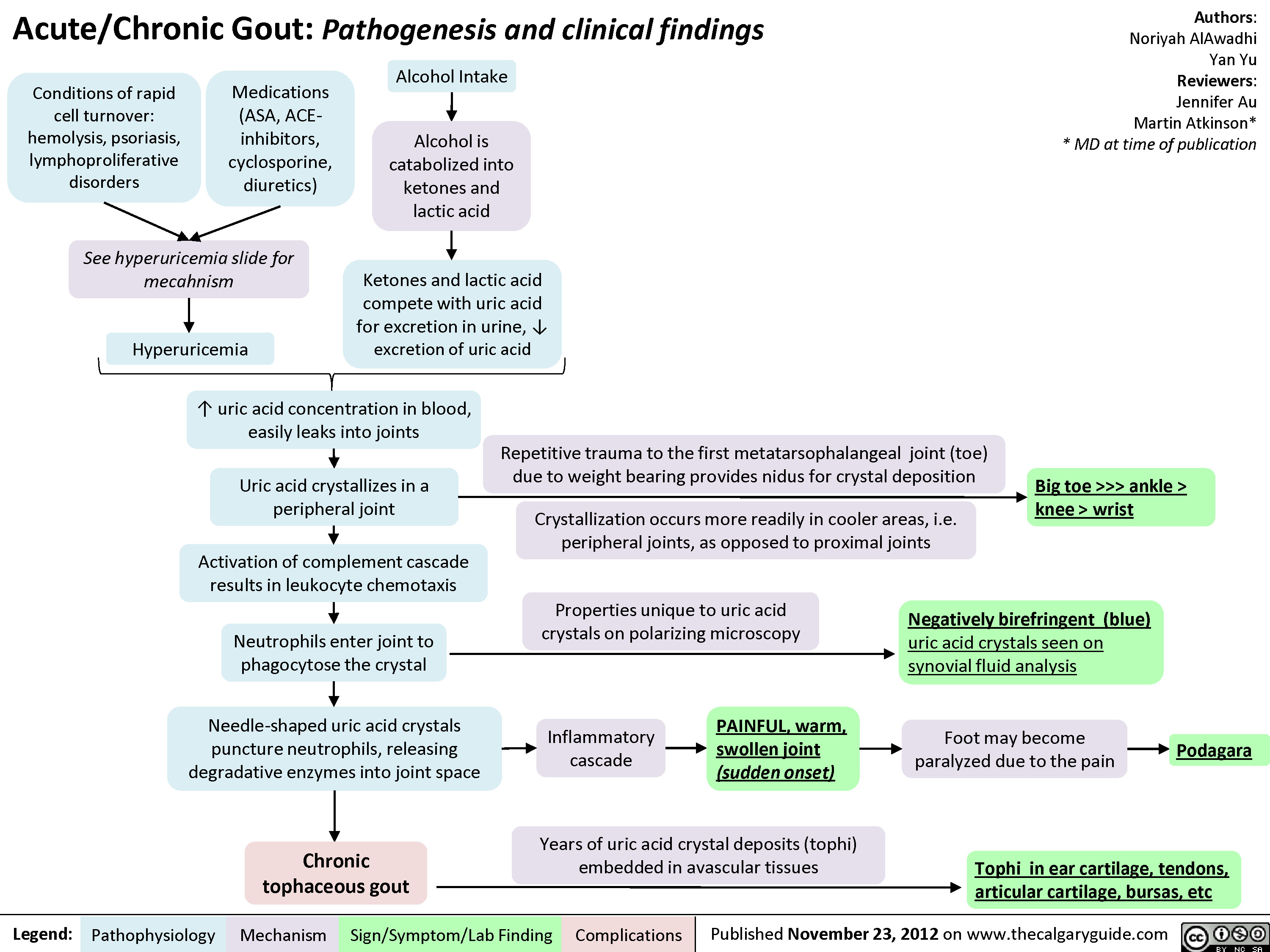
Gout Pathogenesis and Clinical Findings
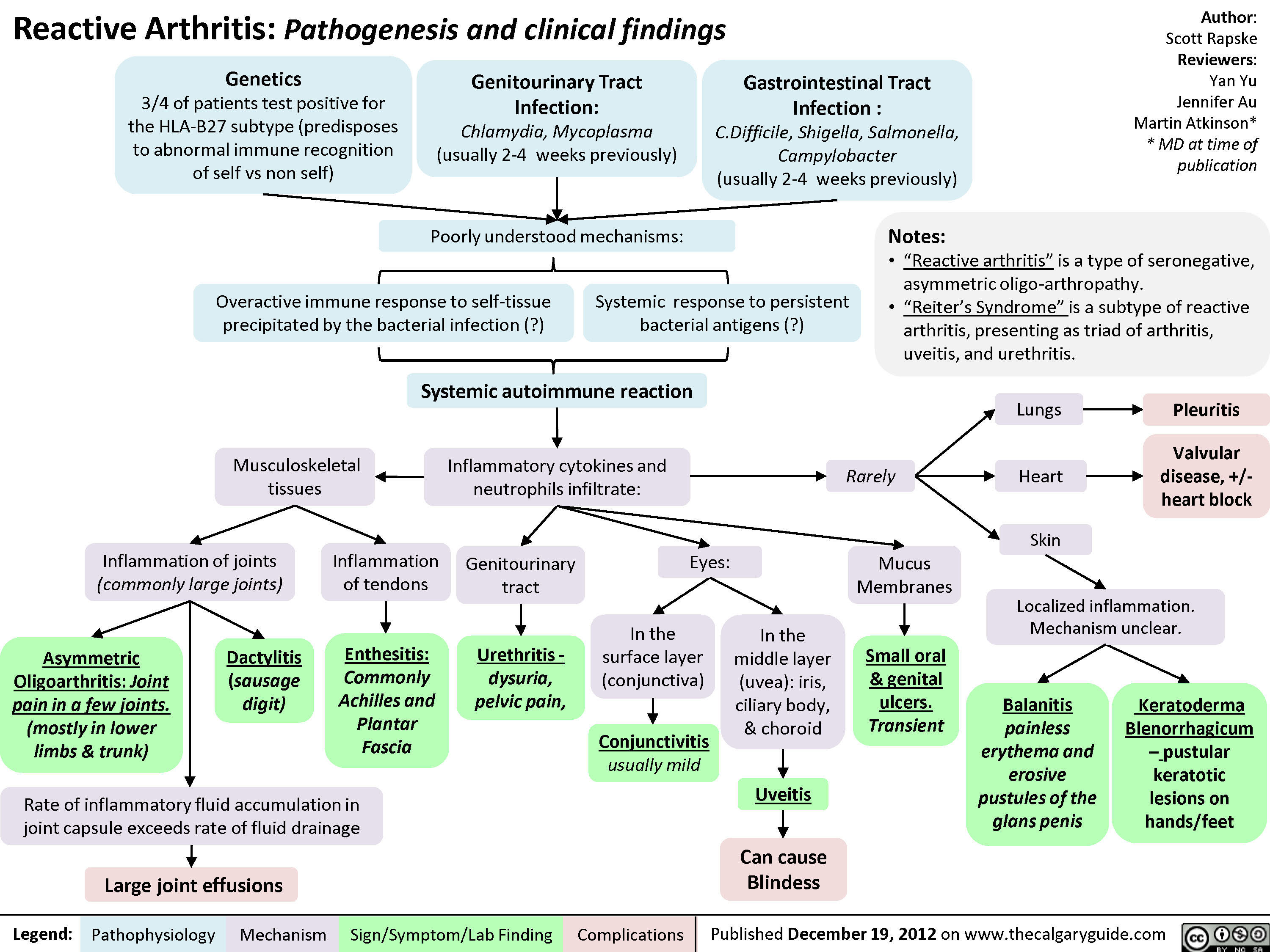
Reactive Arthritis
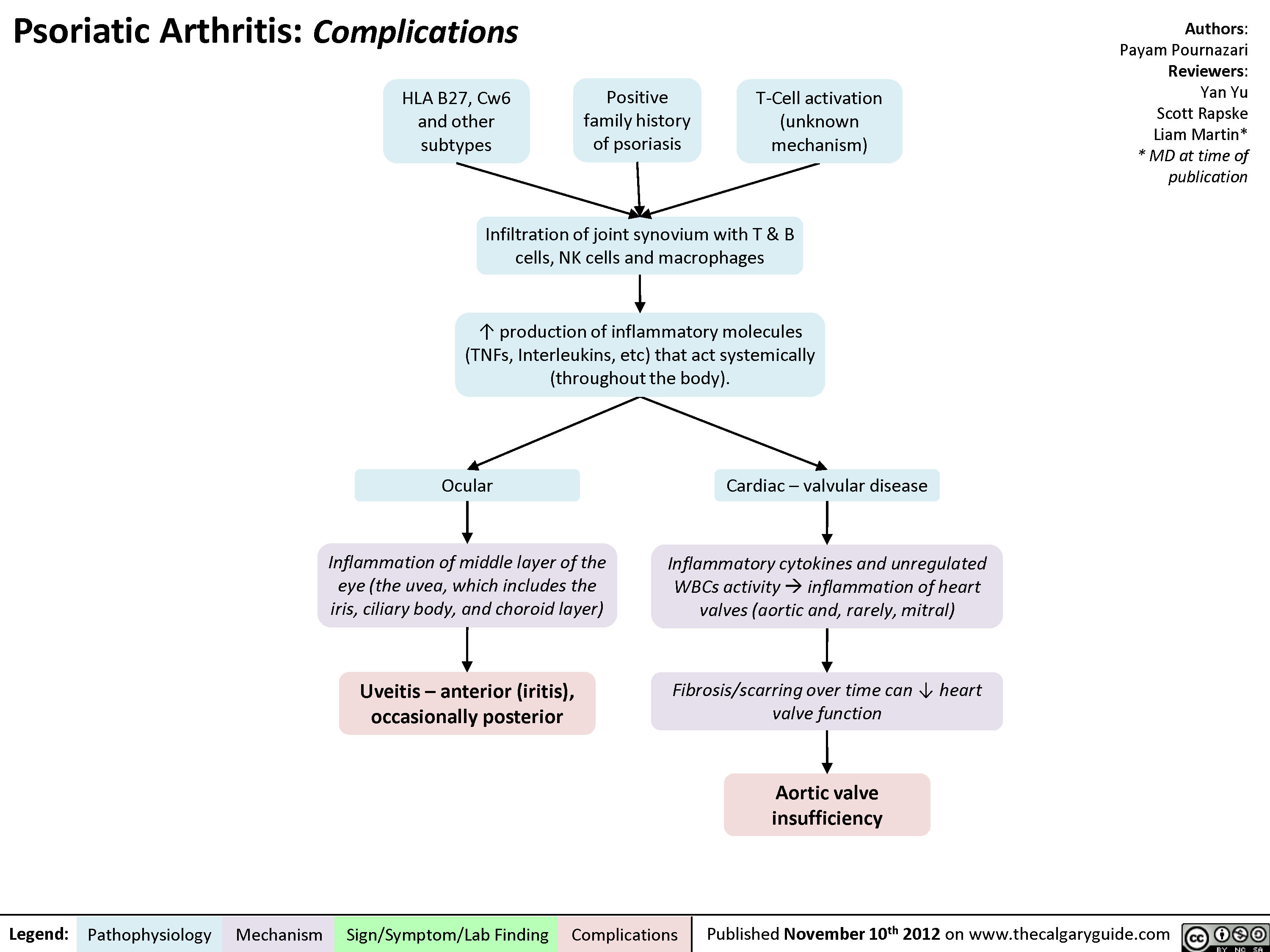
Psoriatic Arthritis: Complications
Psoriatic Arthritis - Pathogenesis and Clinical findings

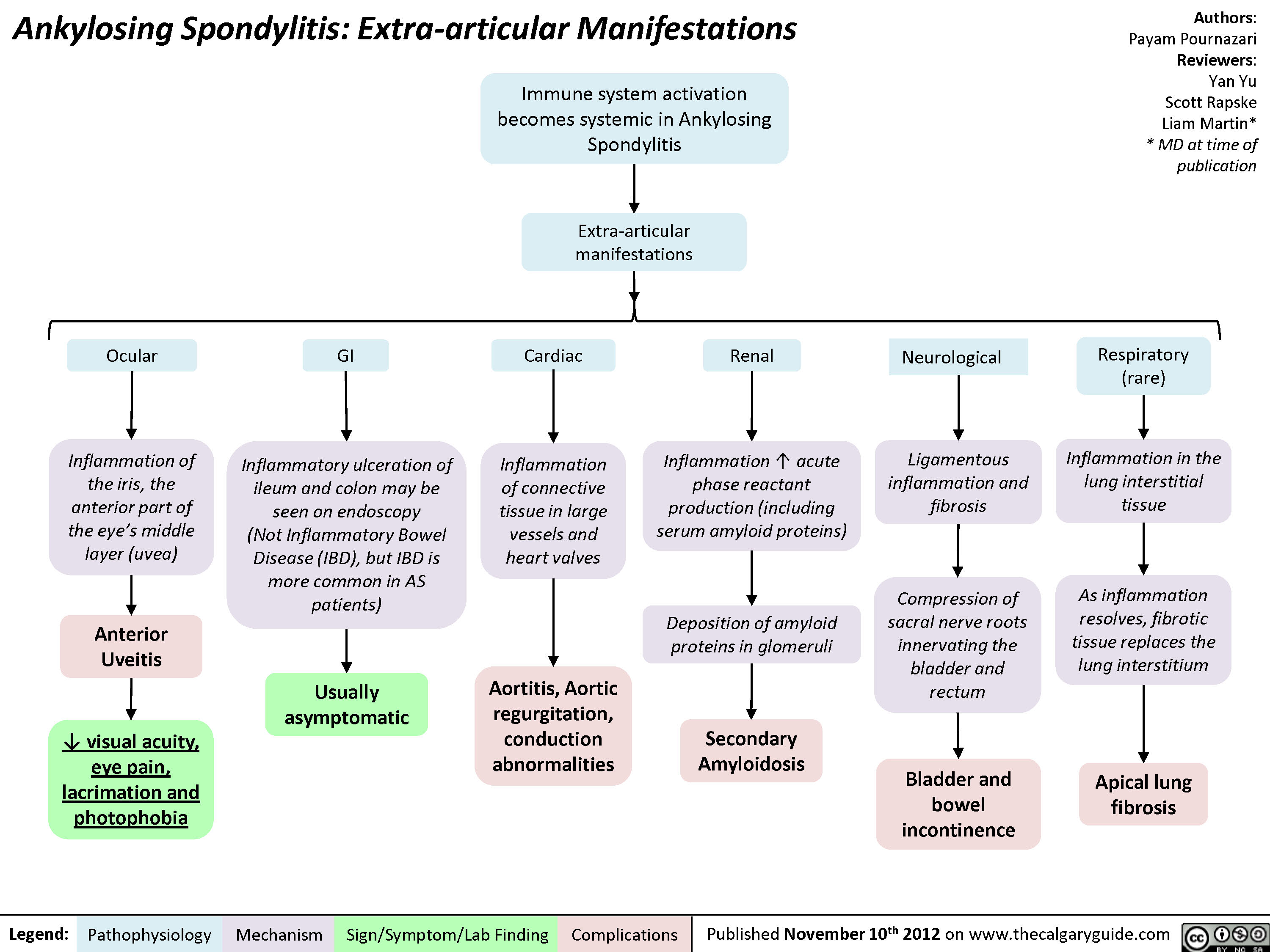
Ankylosing Spondylitis: Extra-articular Manifestations
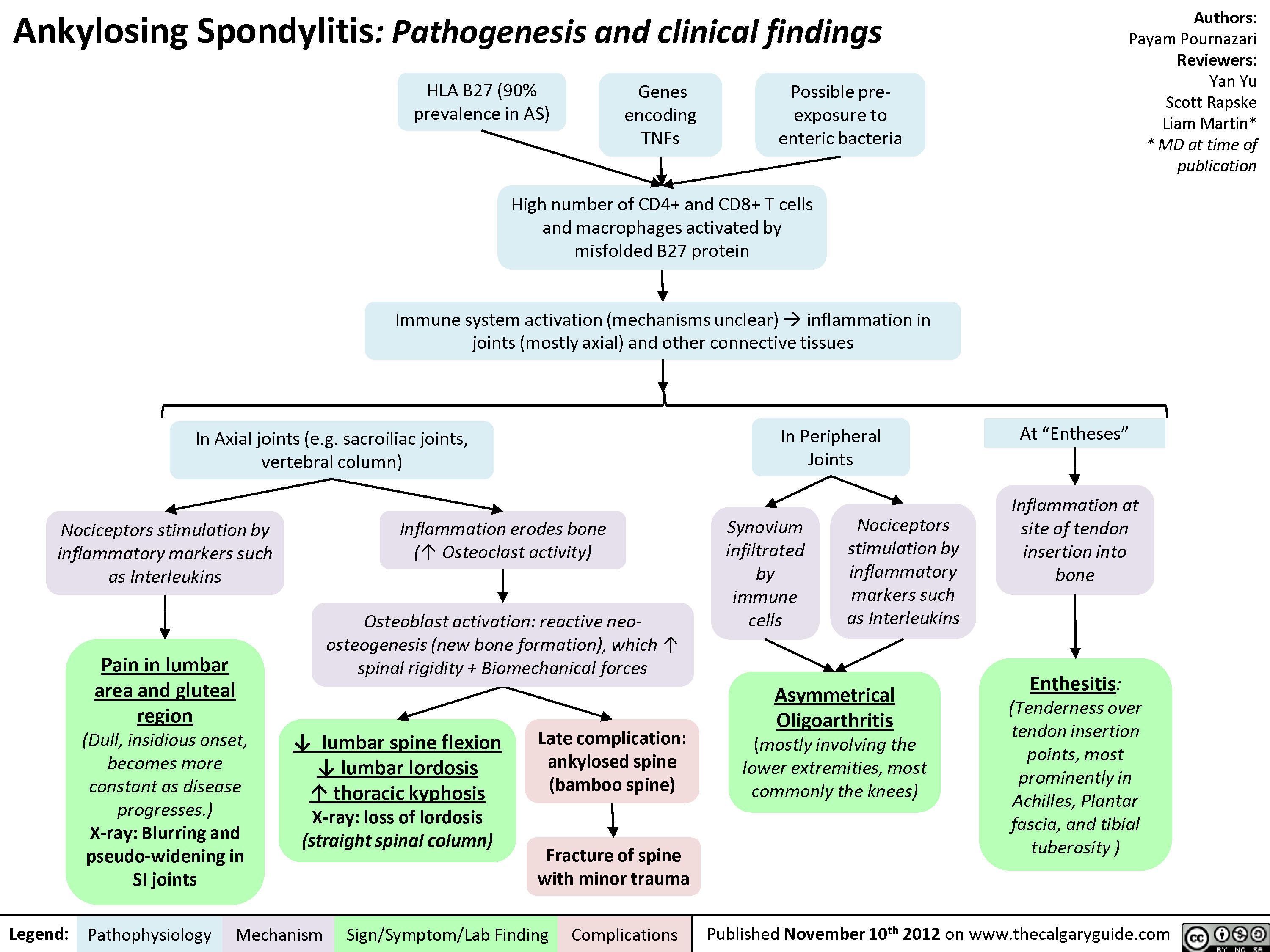
Ankylosing Spondylitis: Pathogenesis and Clinical findings
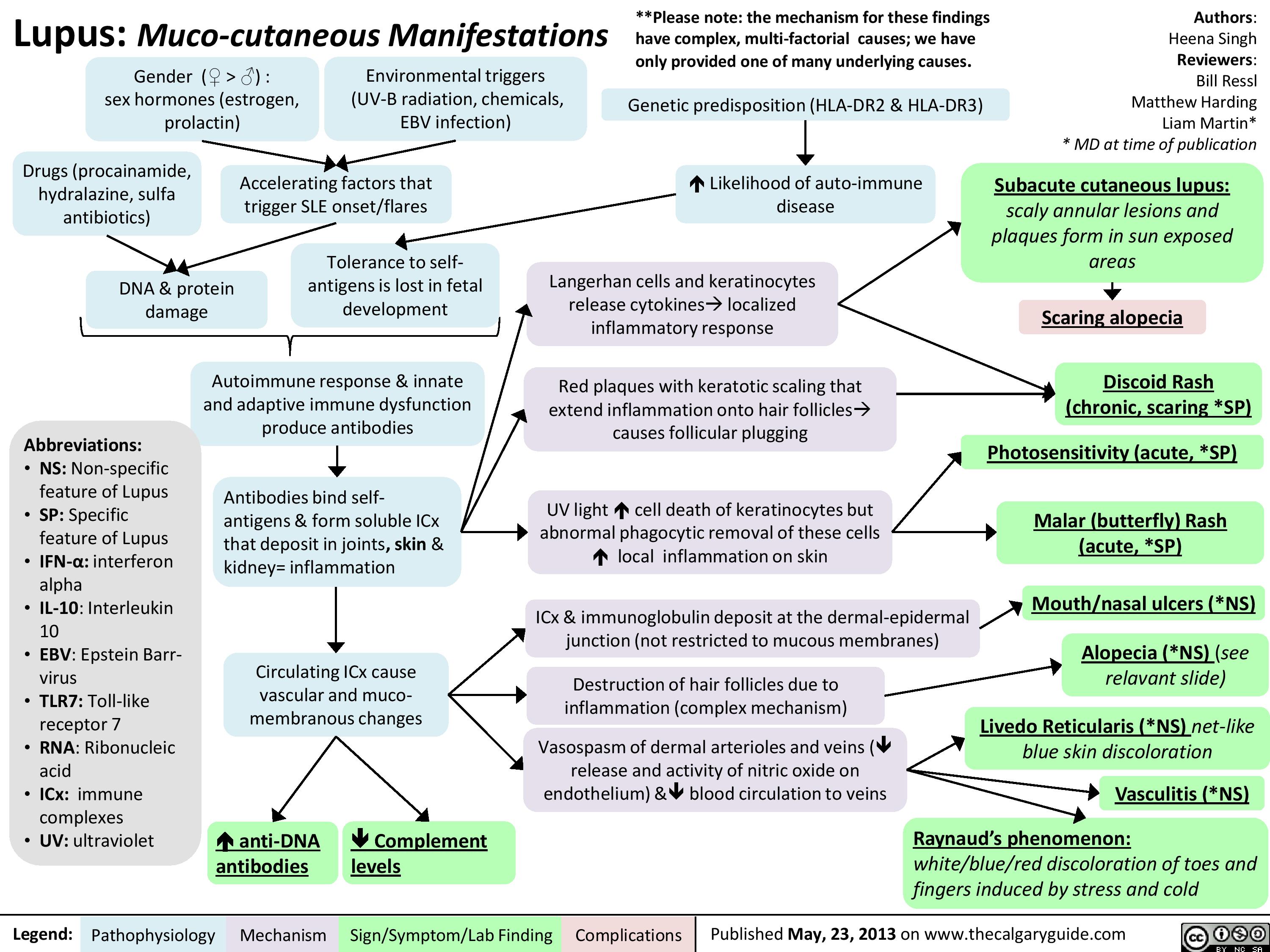
Lupus: Muco-cutaneous manifestations
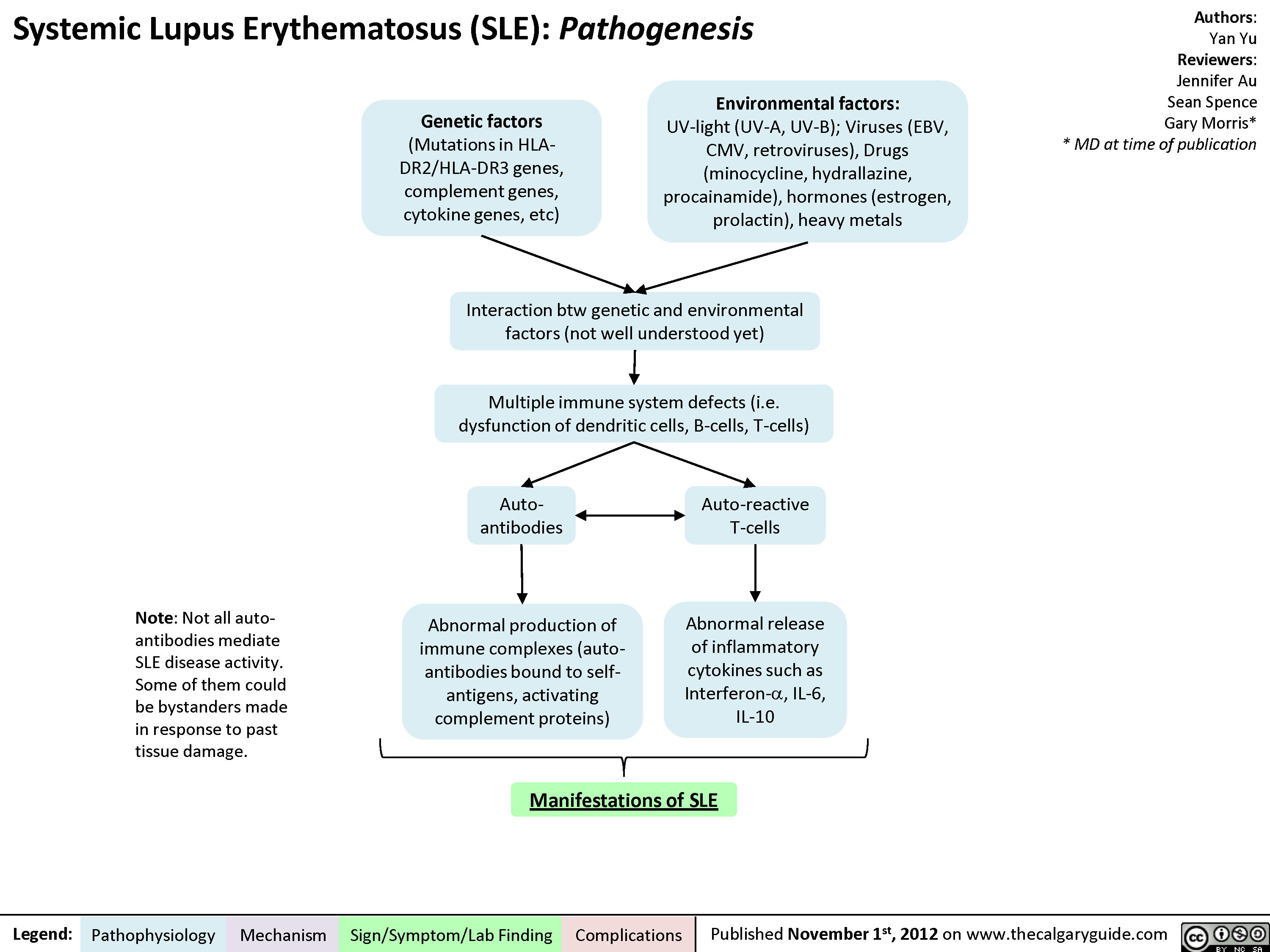
Pathogenesis of Lupus
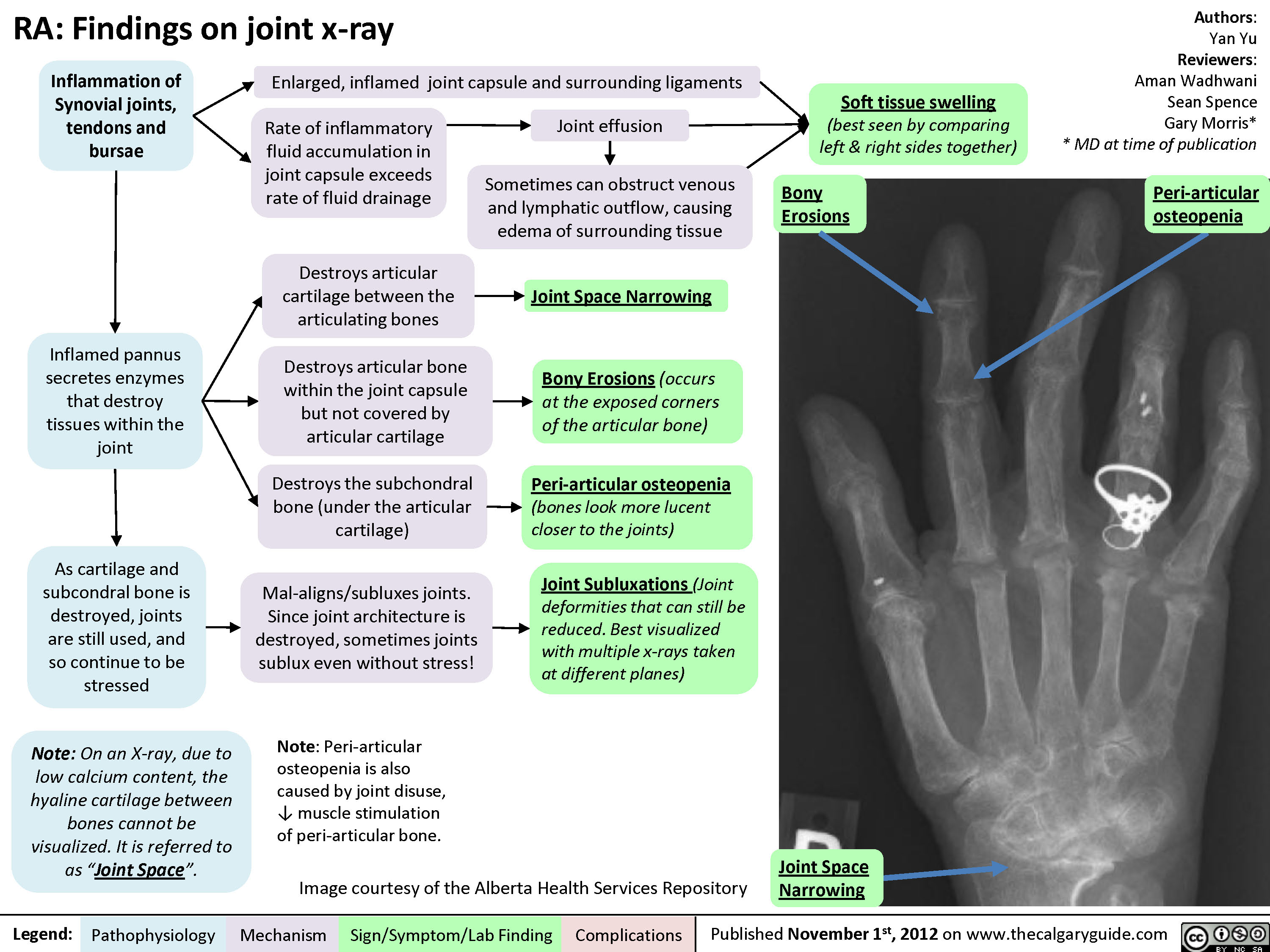
Rheumatoid arthritis (RA): X-ray features
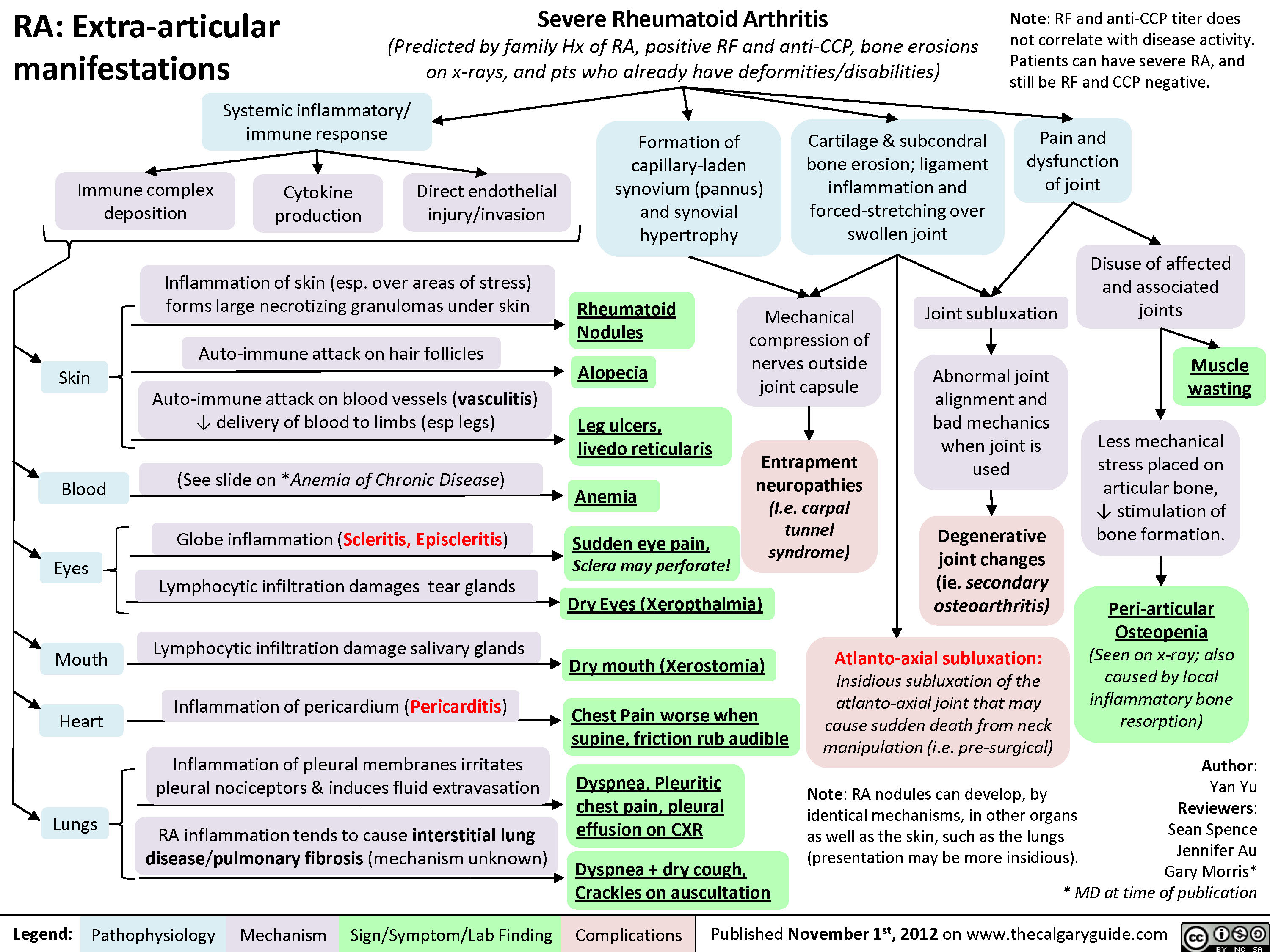
Rheumatoid arthritis (RA): Extra-articular manifestations
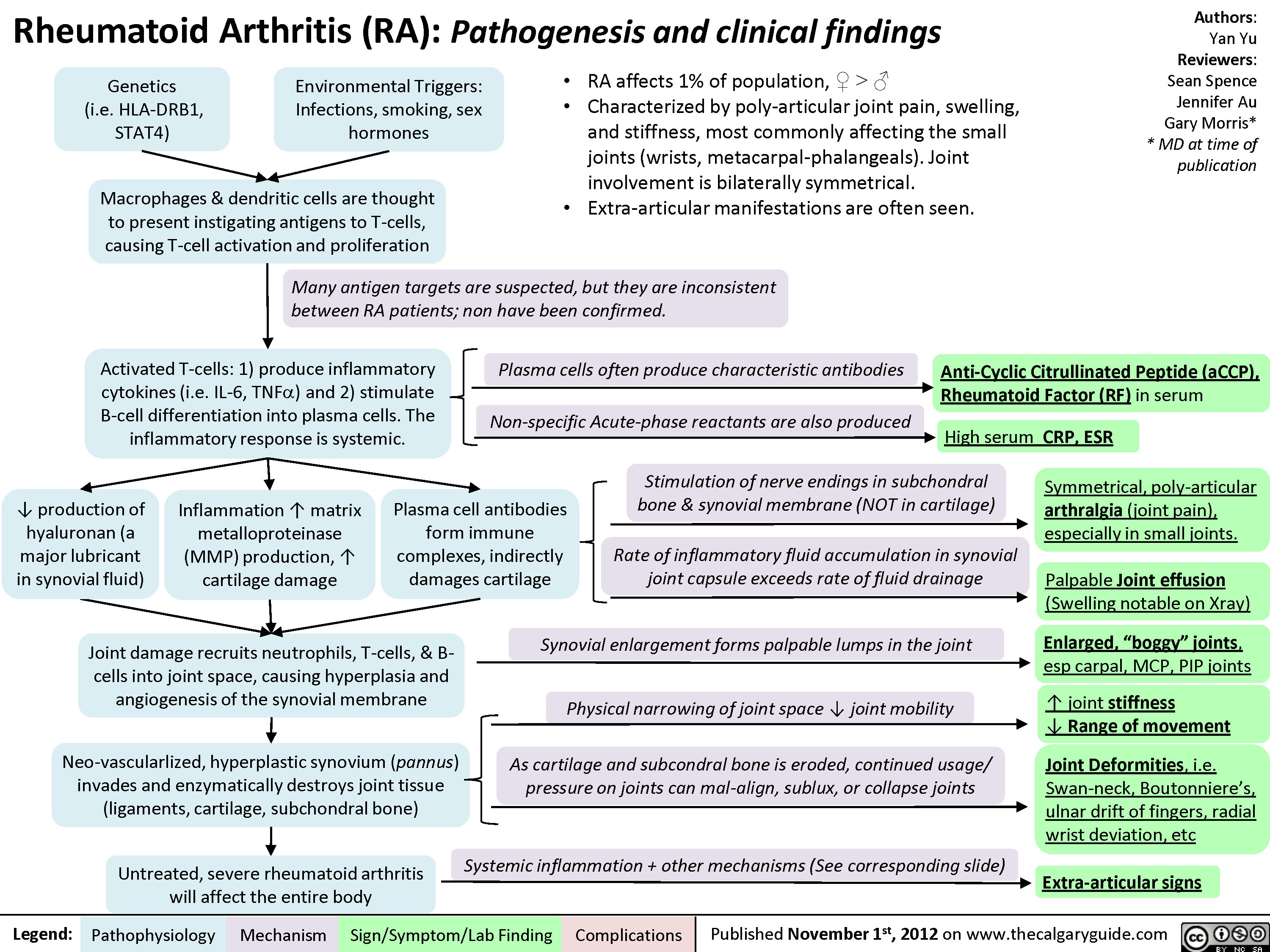
Rheumatoid arthritis (RA): Pathogenesis and Joint diseases features
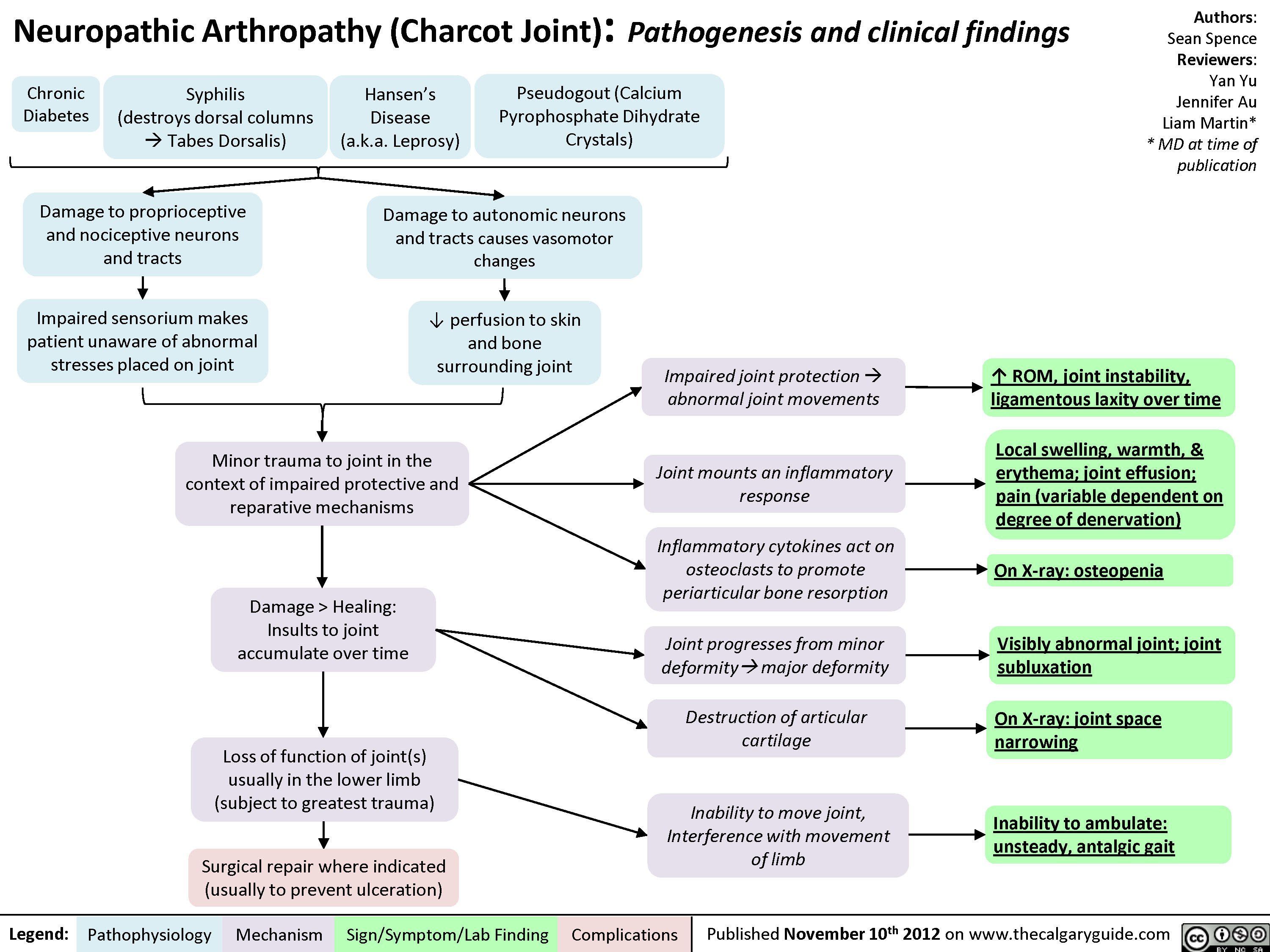
Charcot Joint: Pathogenesis and Clinical findings
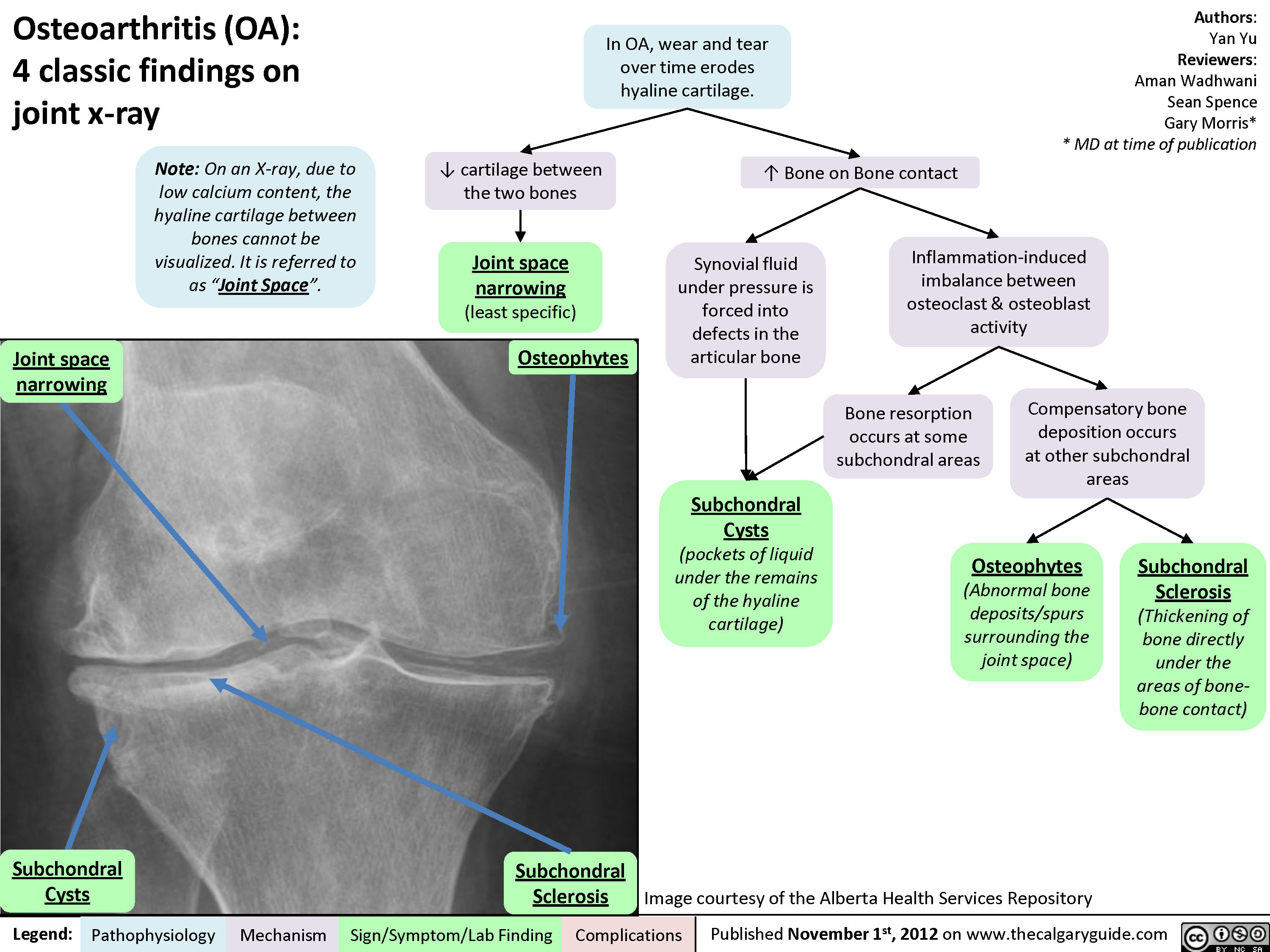
Osteoarthritis (OA): X-ray features
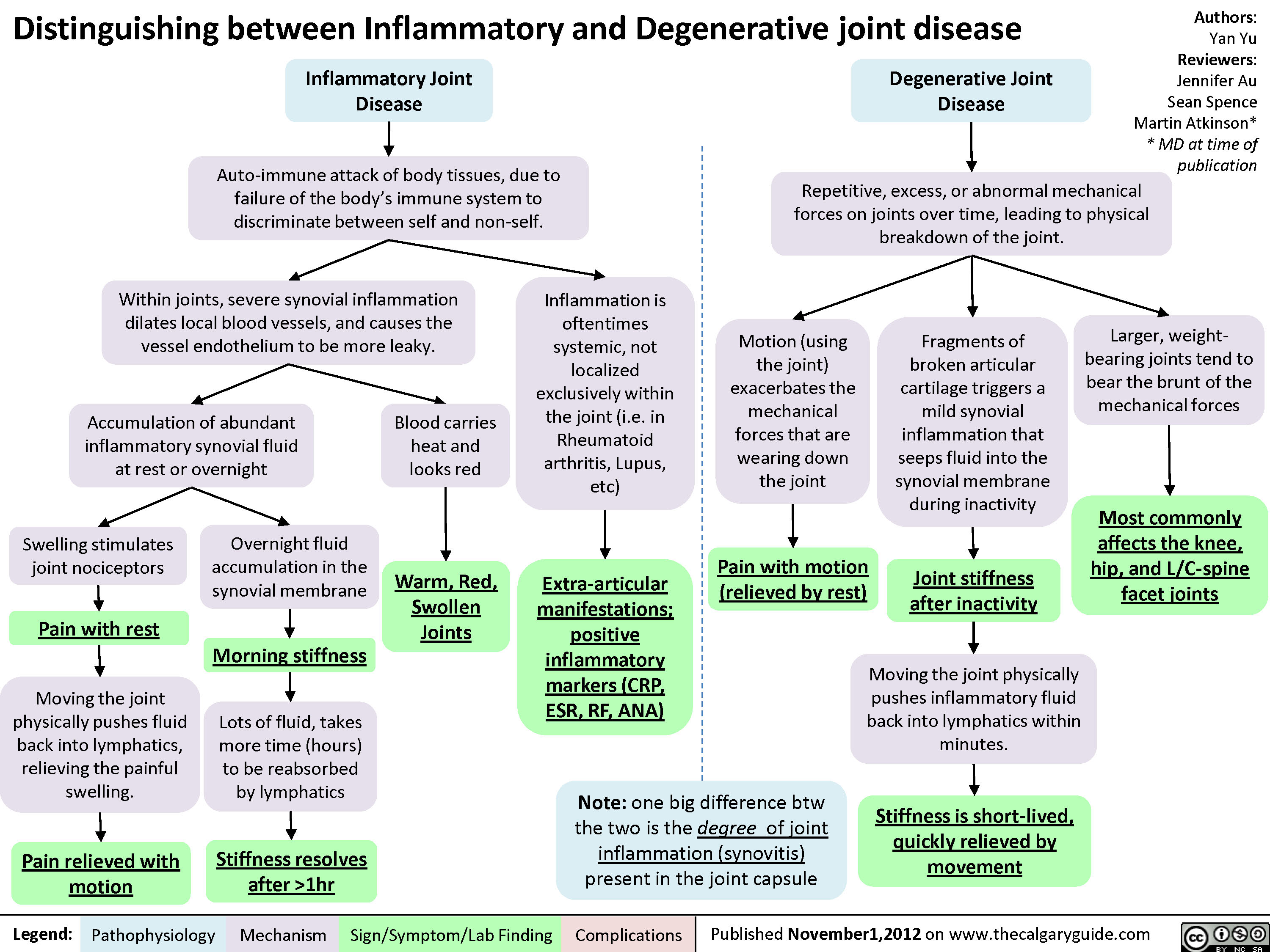
Degenerative Vs Inflammatory Joint Disease
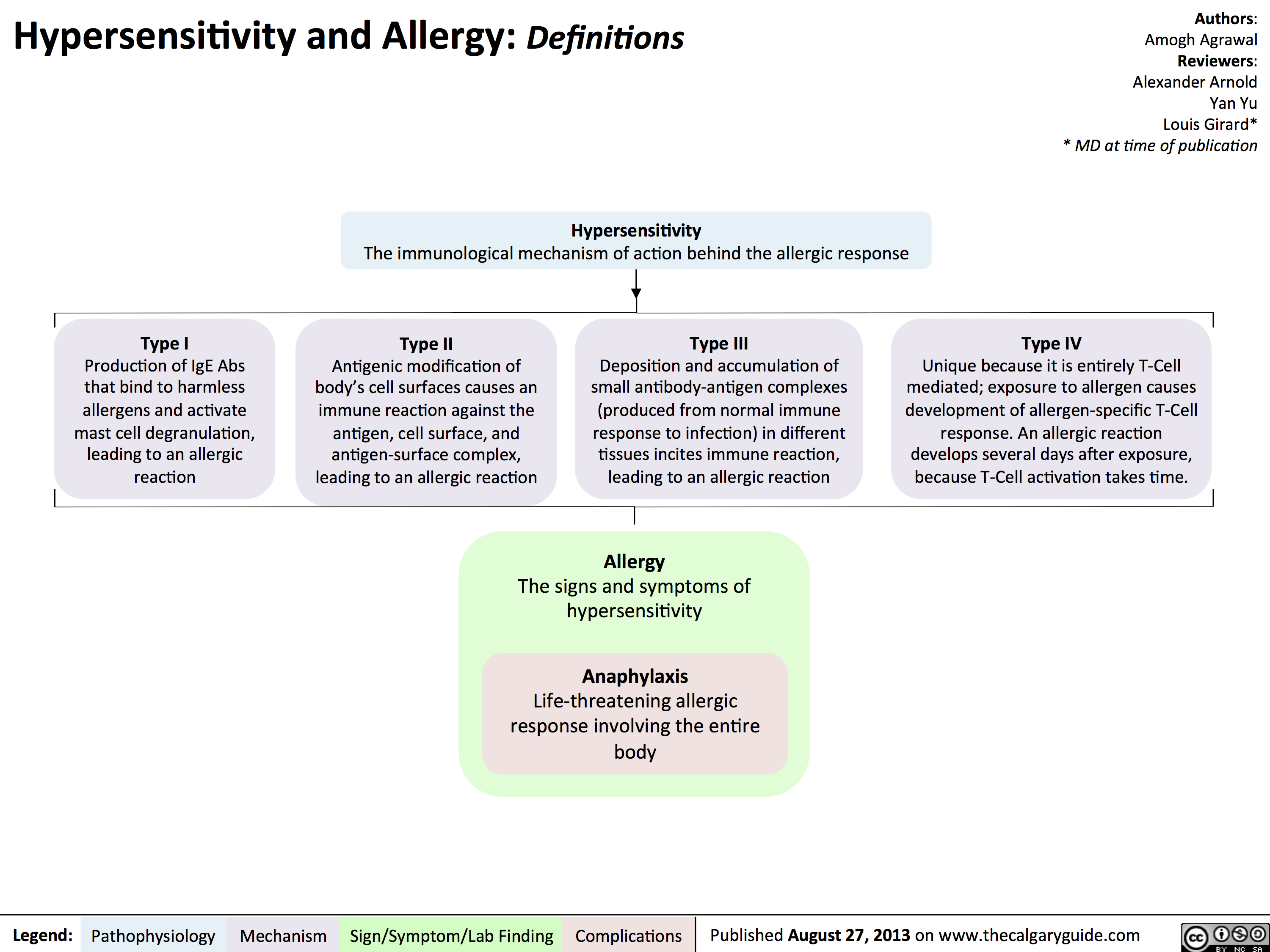
Hypersensitivity: Definitions
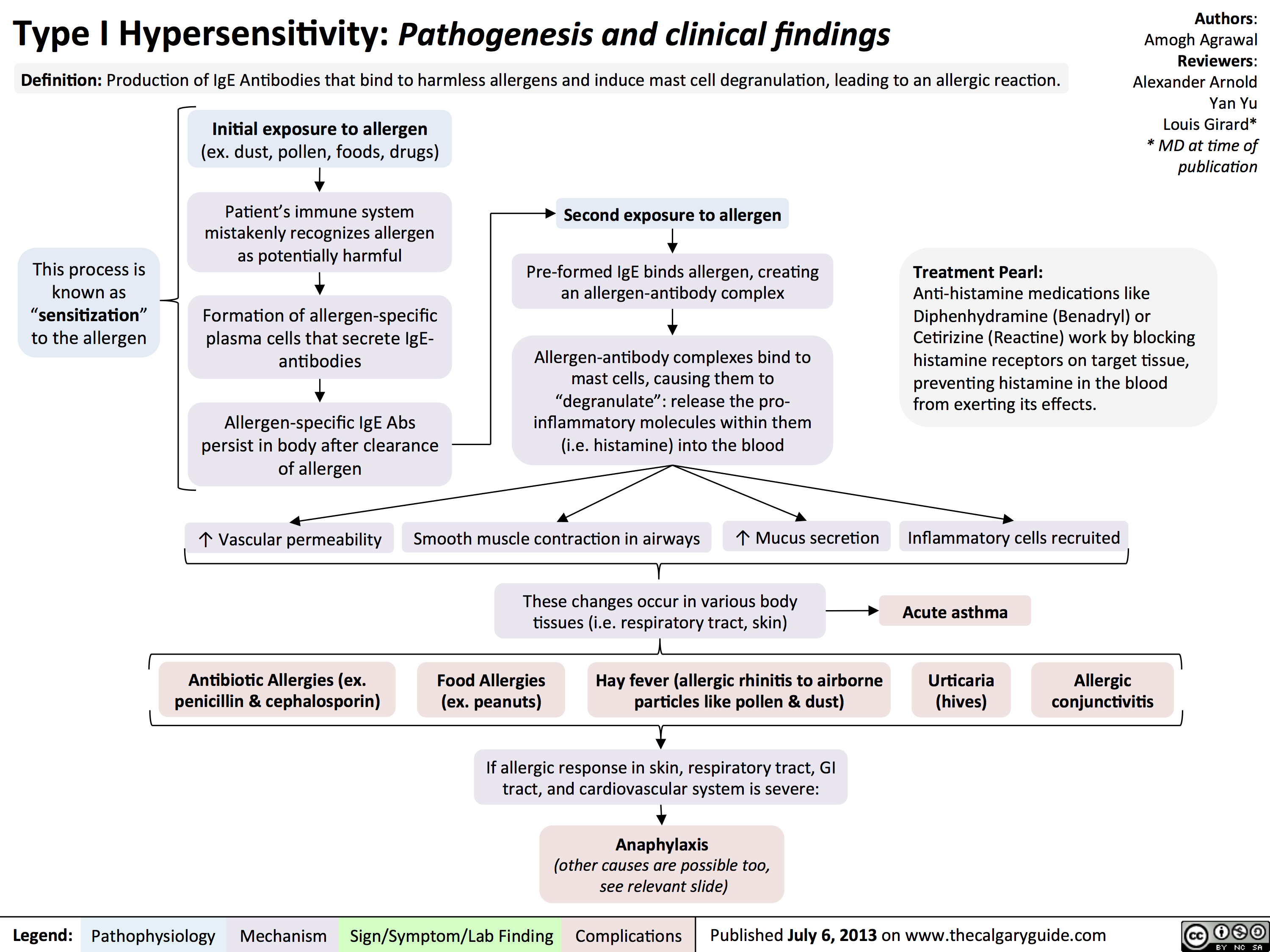
Type I Hypersensitivity: Pathogenesis and clinical findings
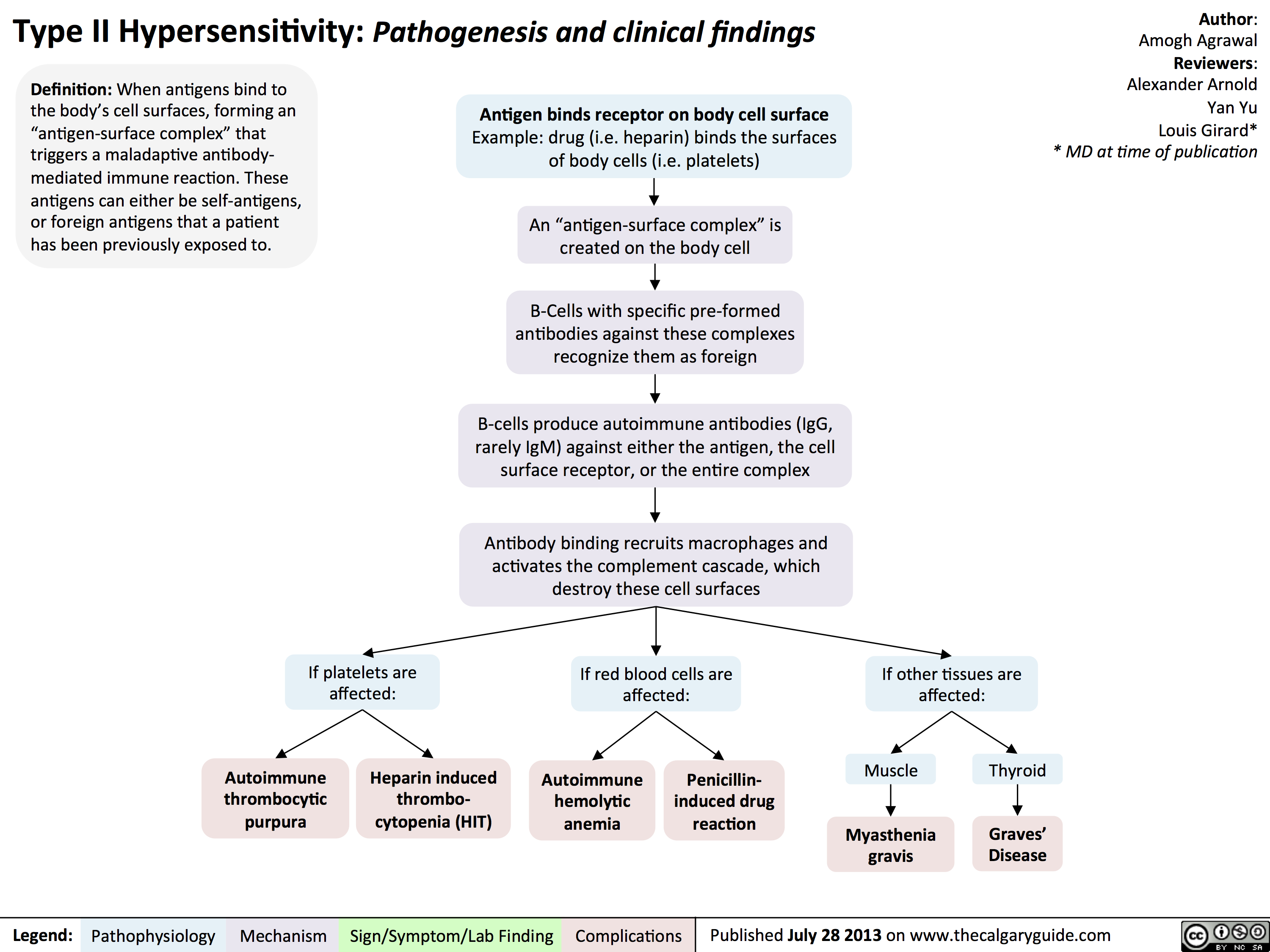
Type II Hypersensitivity: Pathogenesis and clinical findings
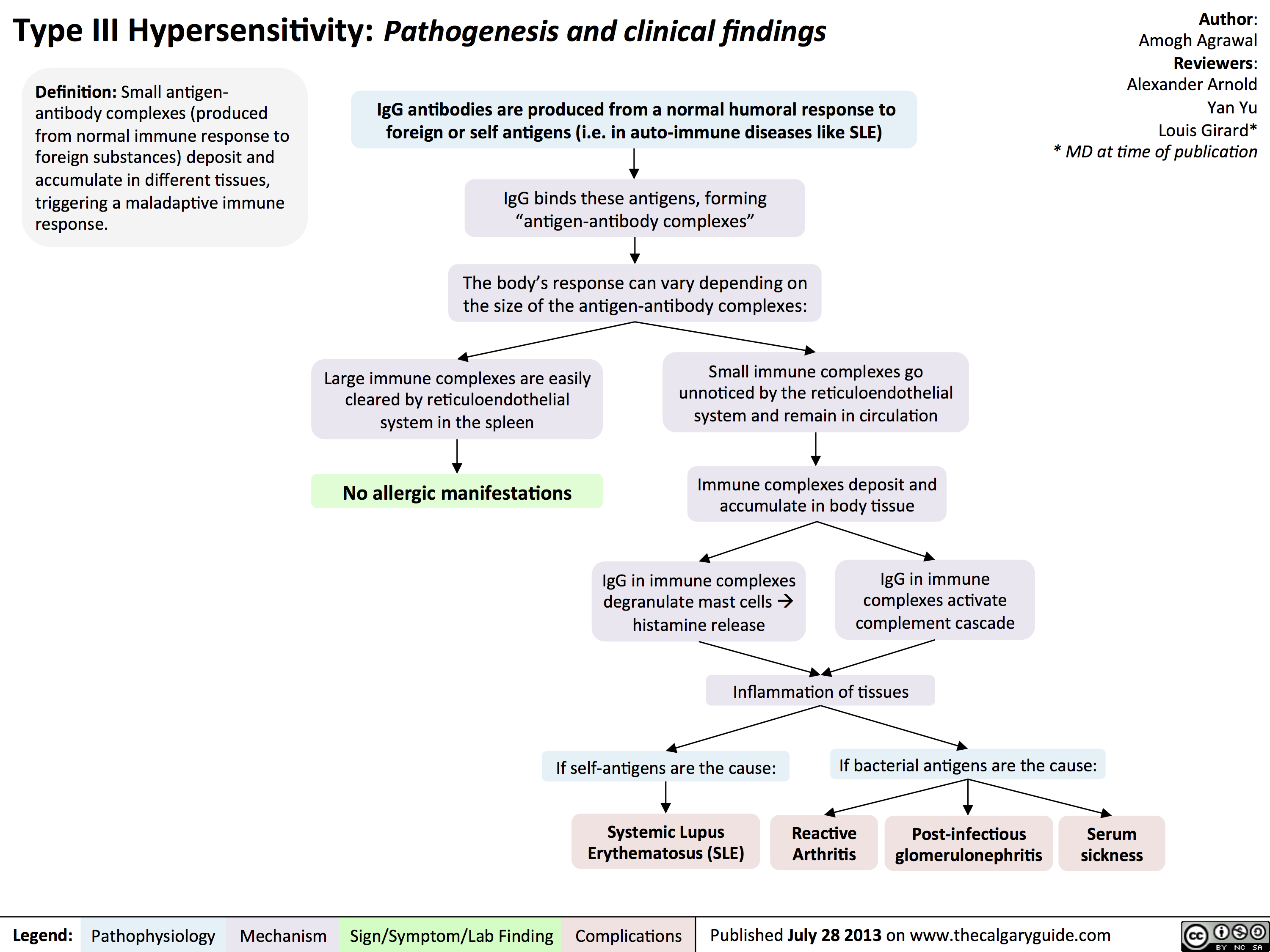
Type III Hypersensitivity: Pathogenesis and clinical findings
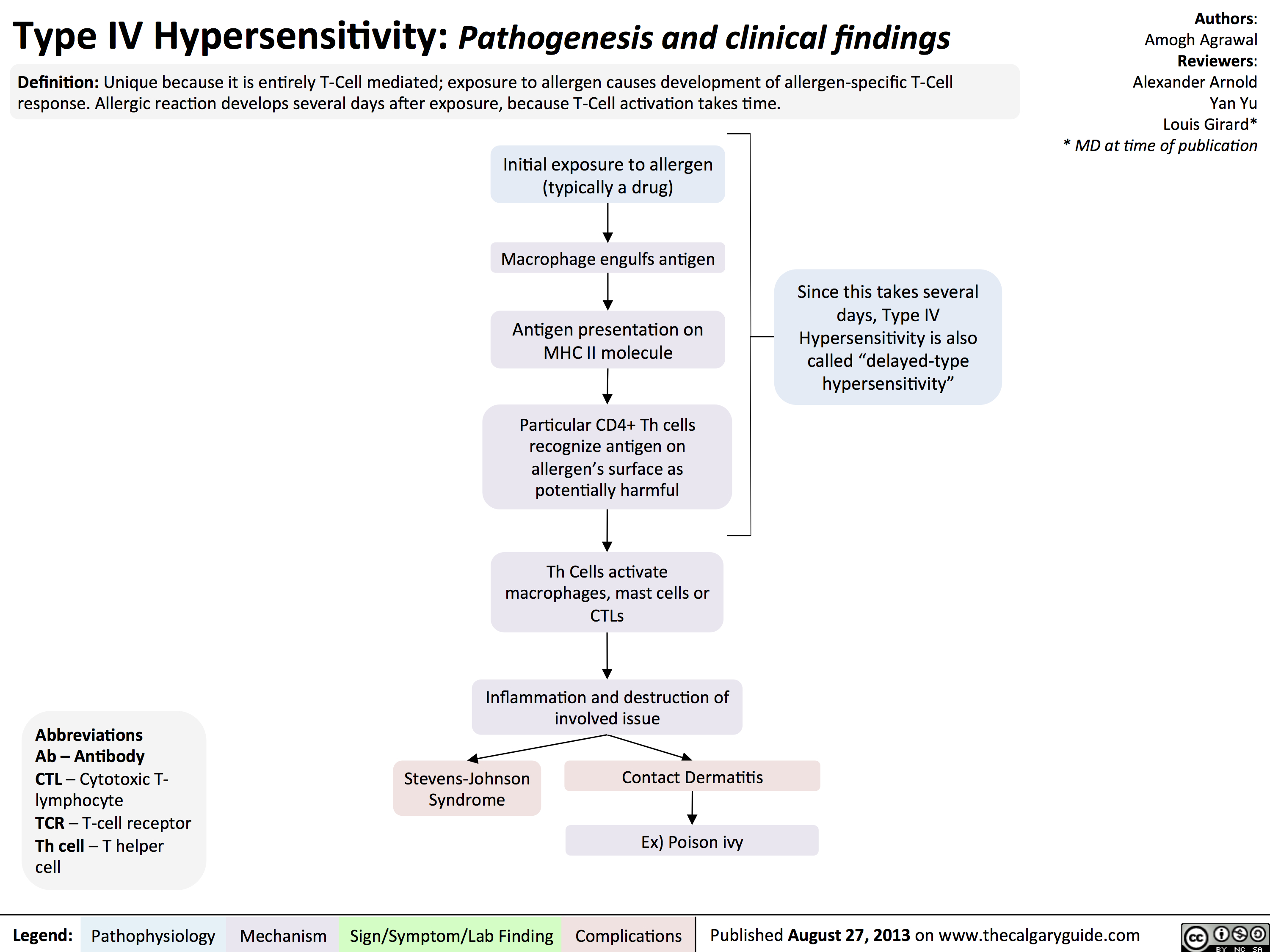
Type IV Hypersensitivity: Pathogenesis and clinical findings
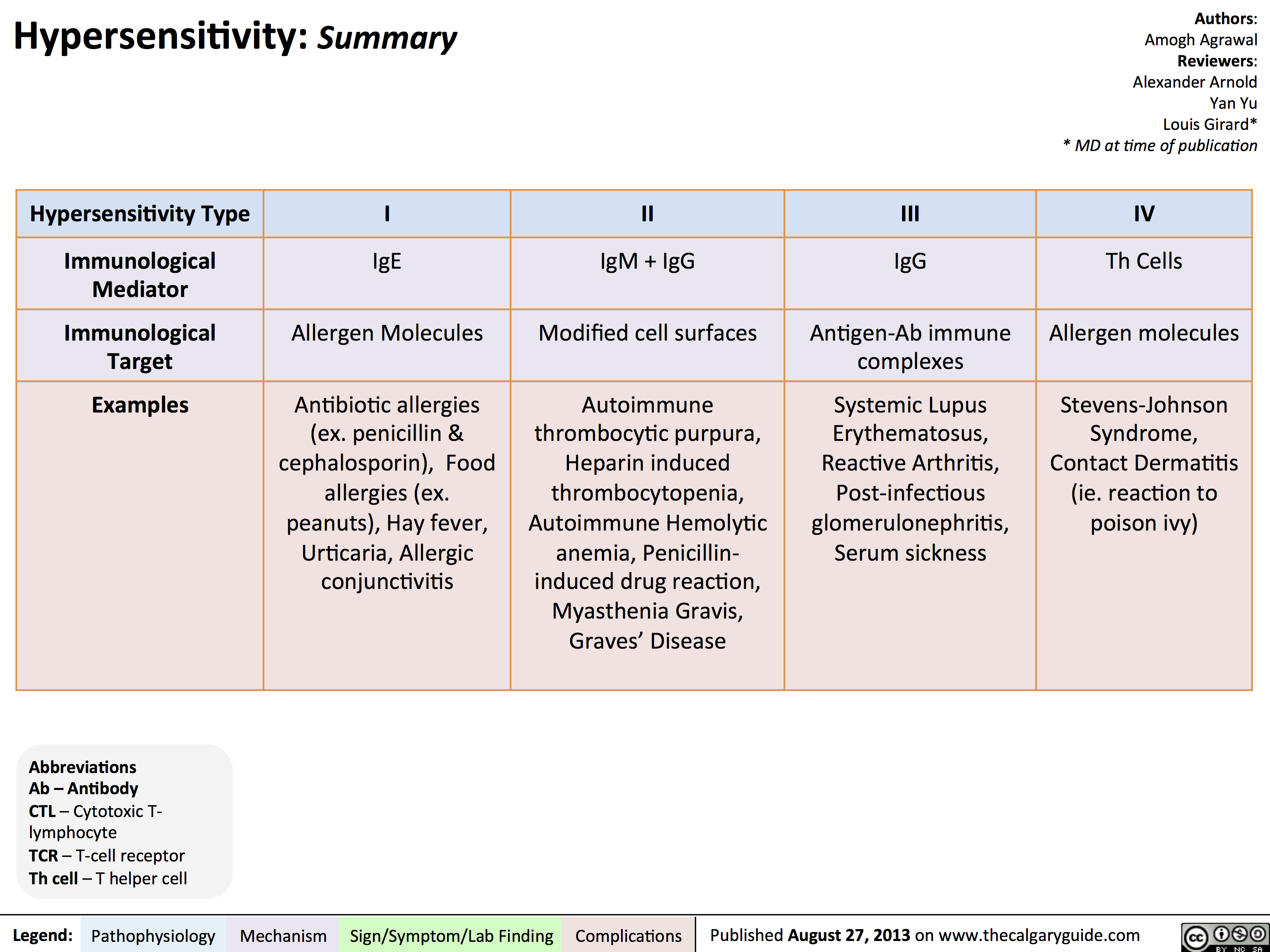
Hypersensitivity Summary
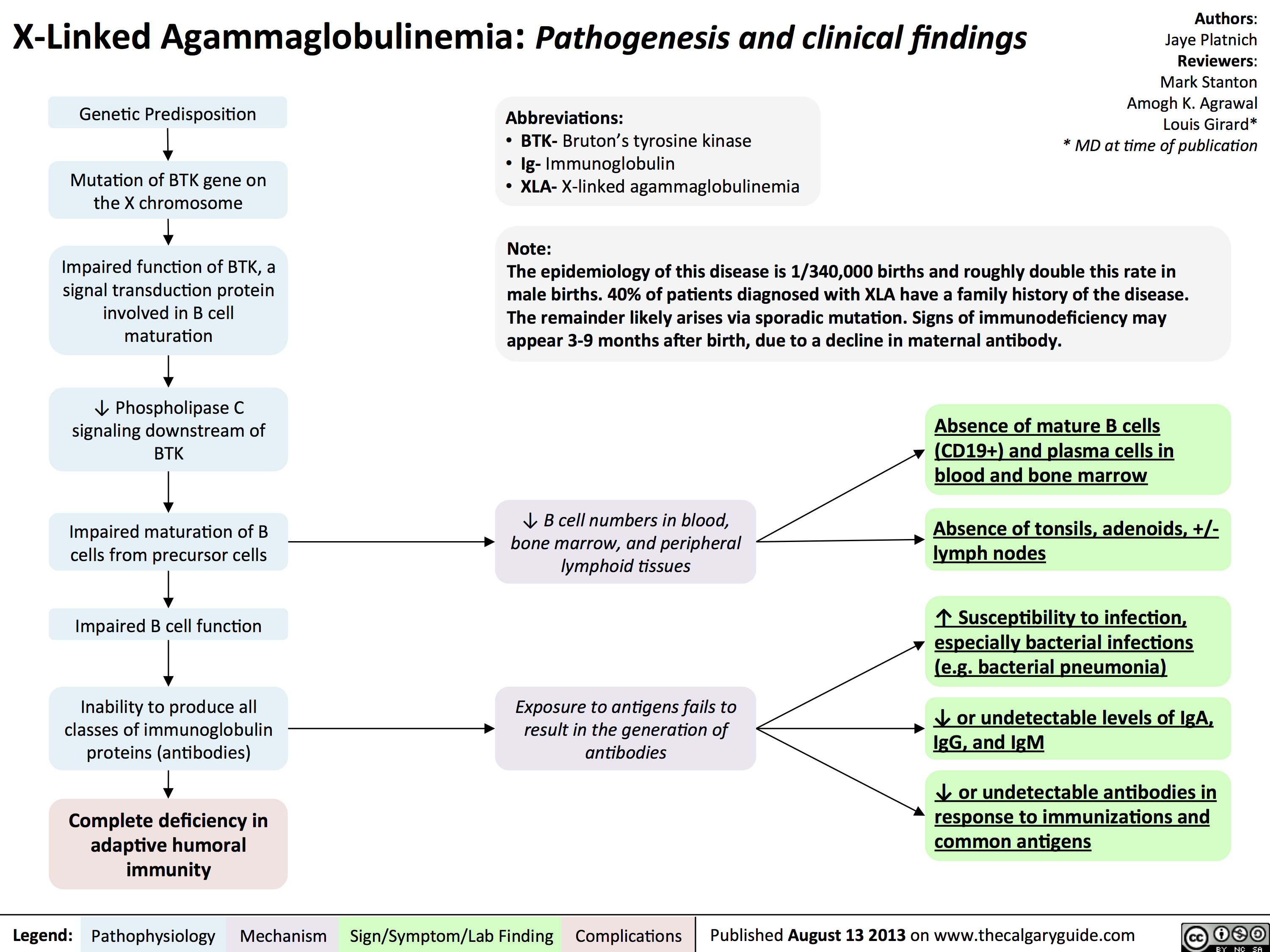
Agammaglobulinemia: Pathogenesis and clinical findings
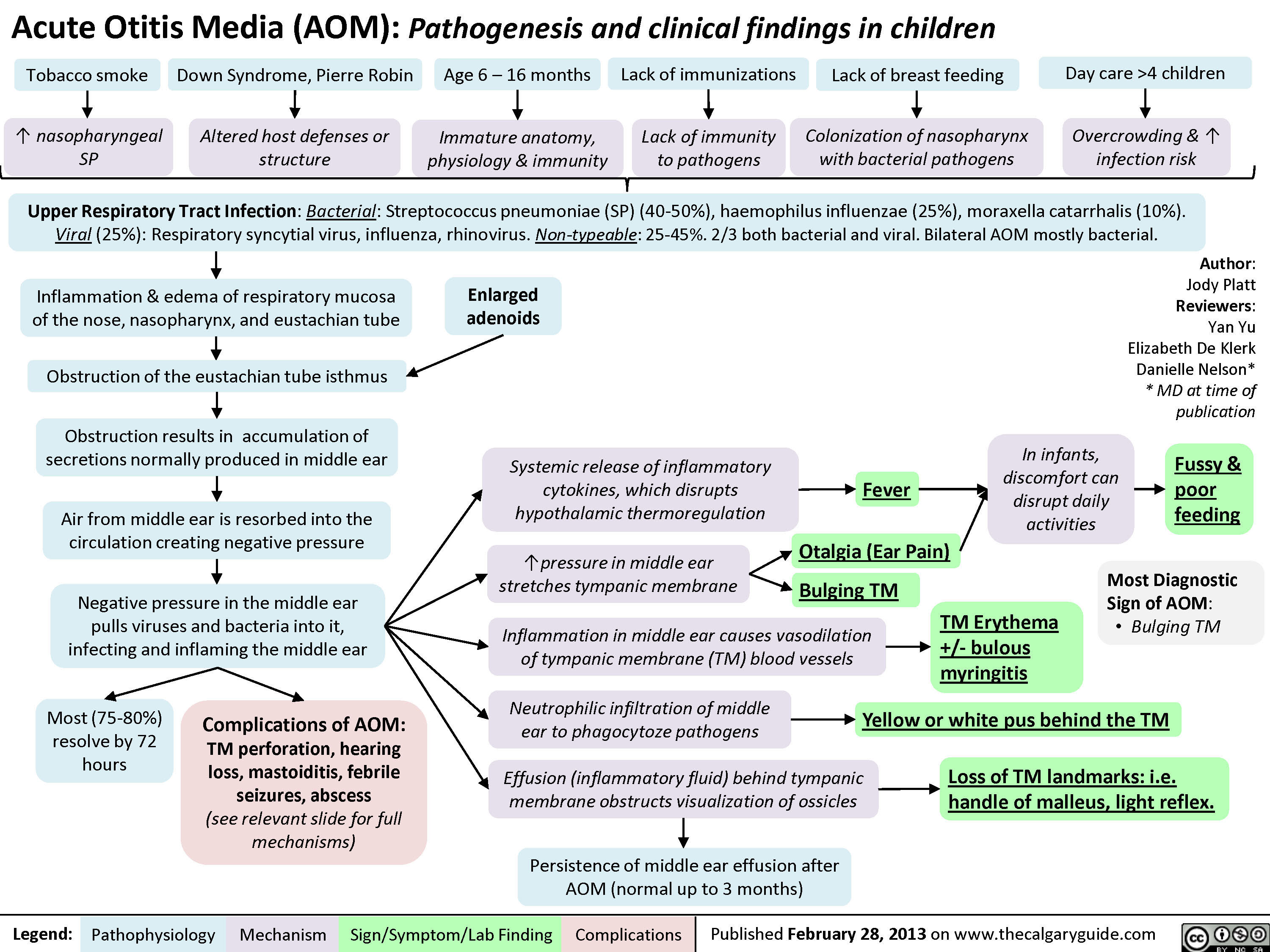
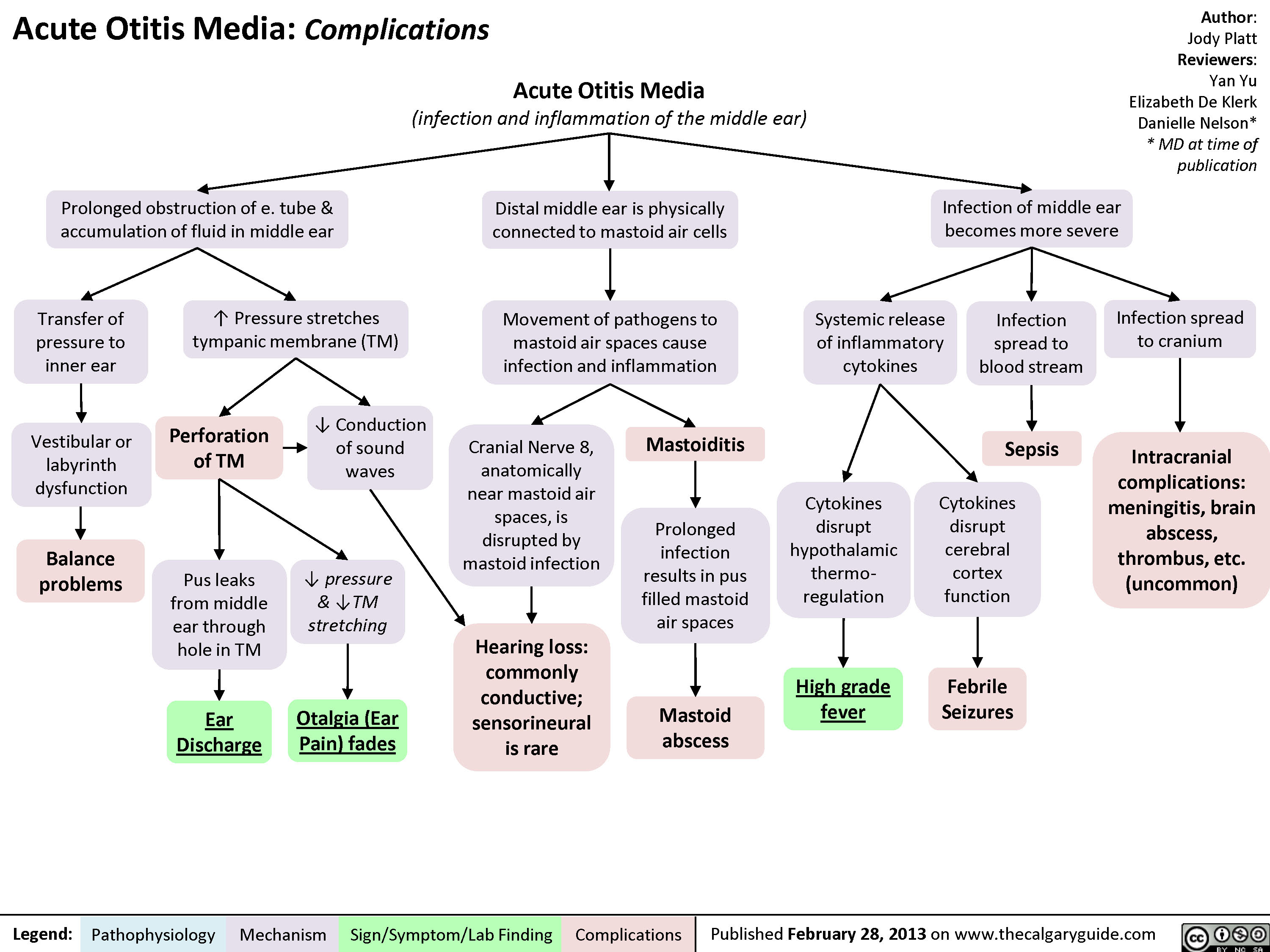
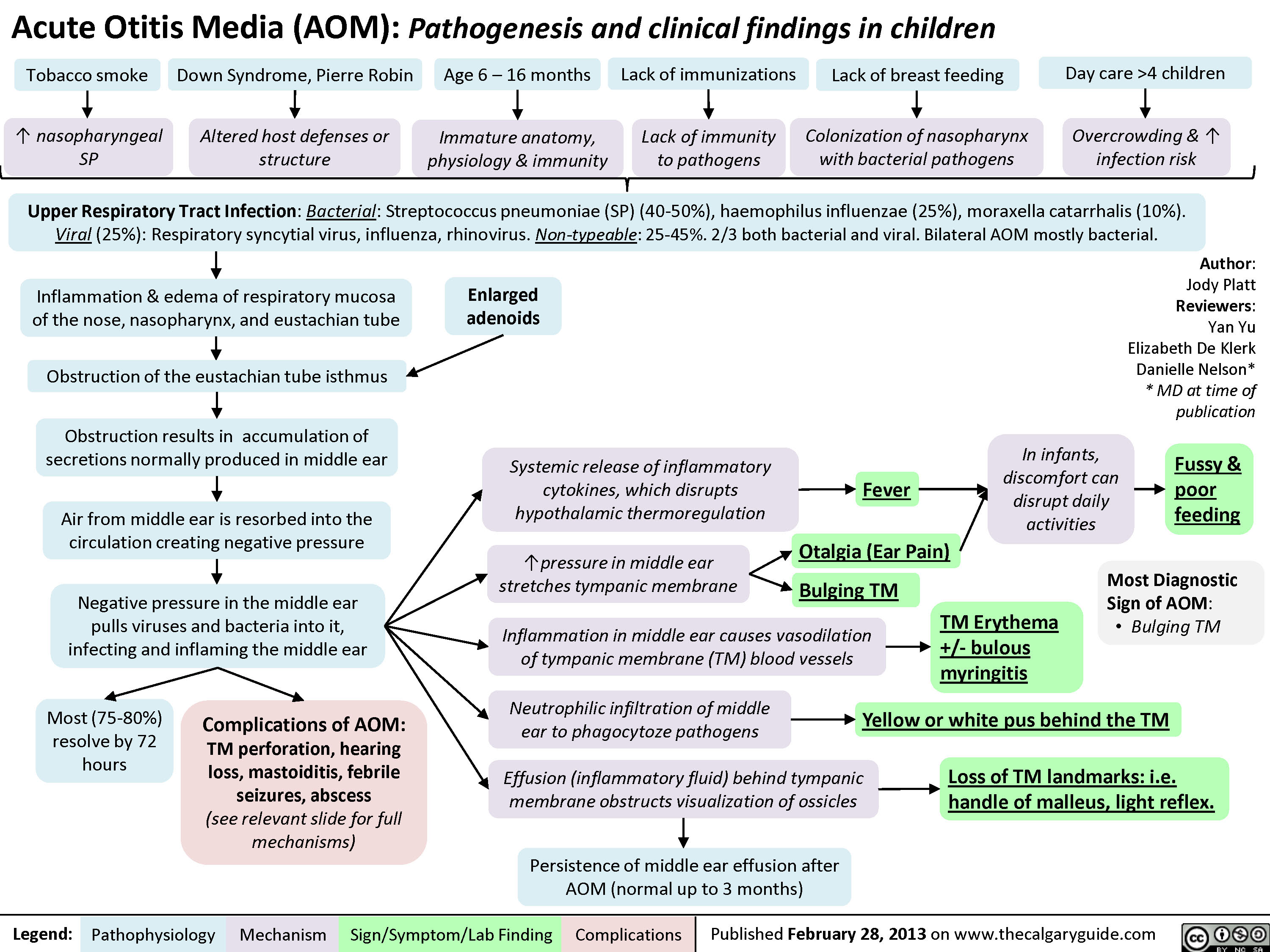
Acute Otitis Media: Pathogenesis and Clinical Findings (in Children)
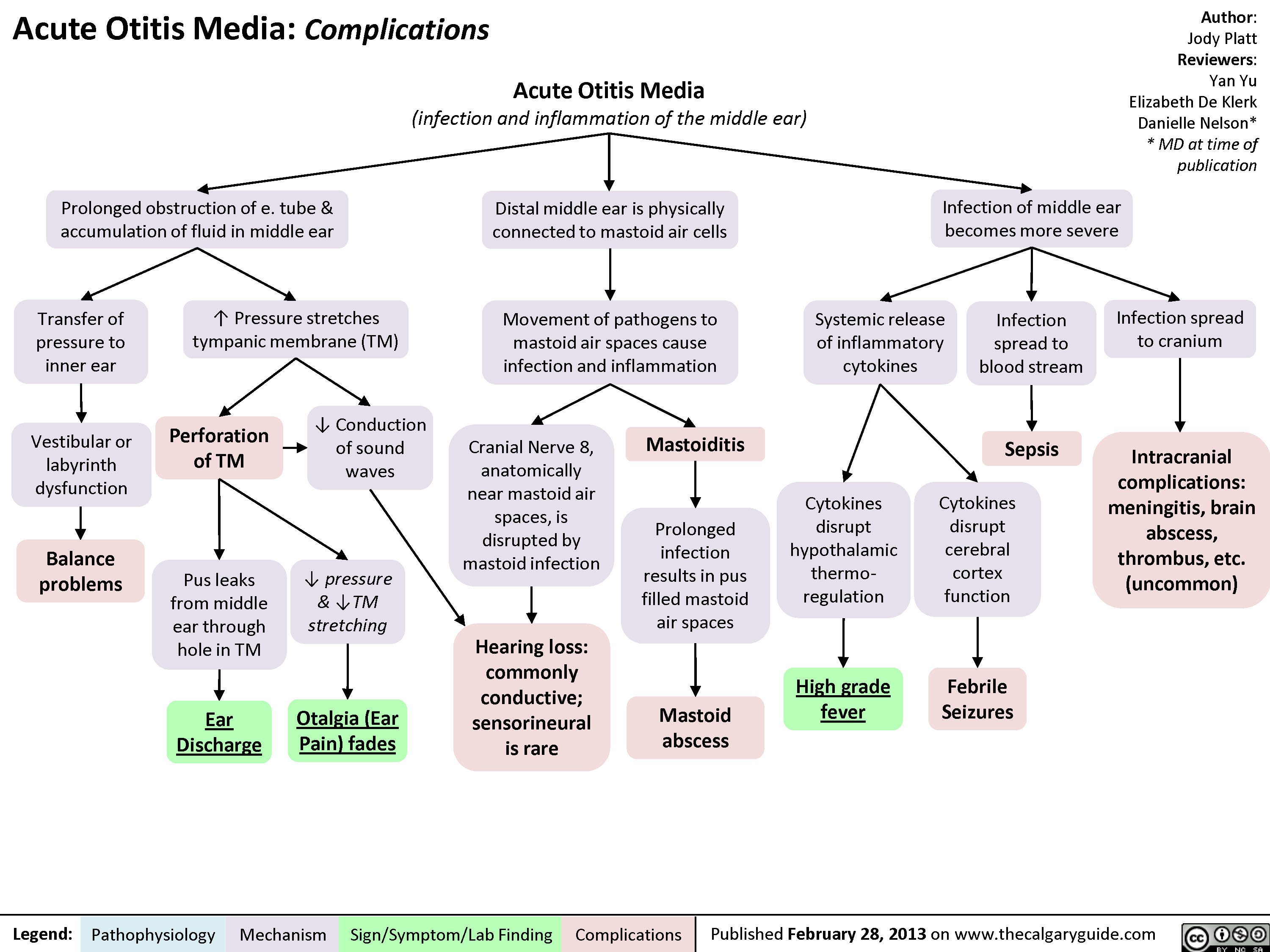
Acute Otitis Media: Complications
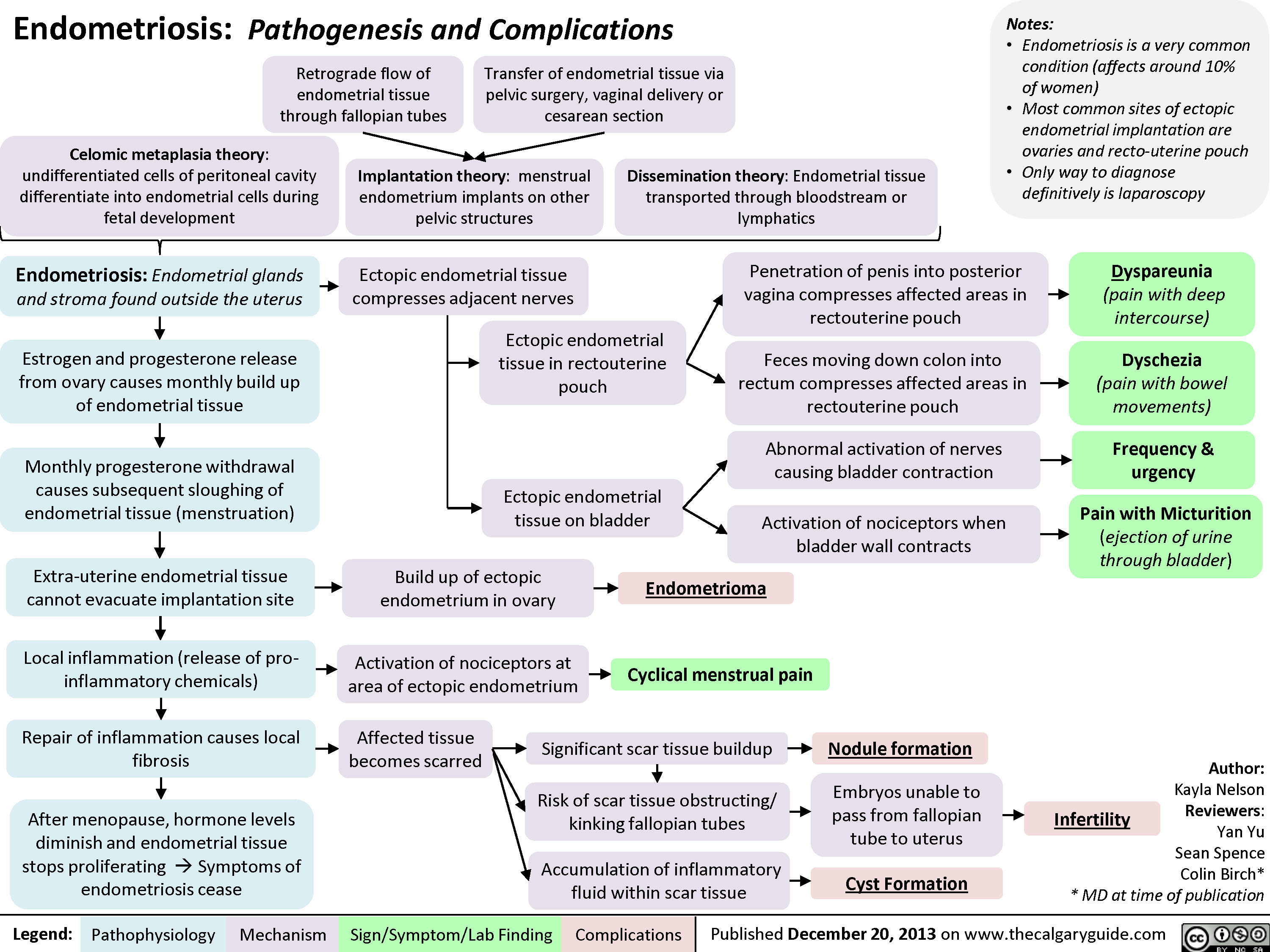
Endometriosis: Pathogenesis and Complications
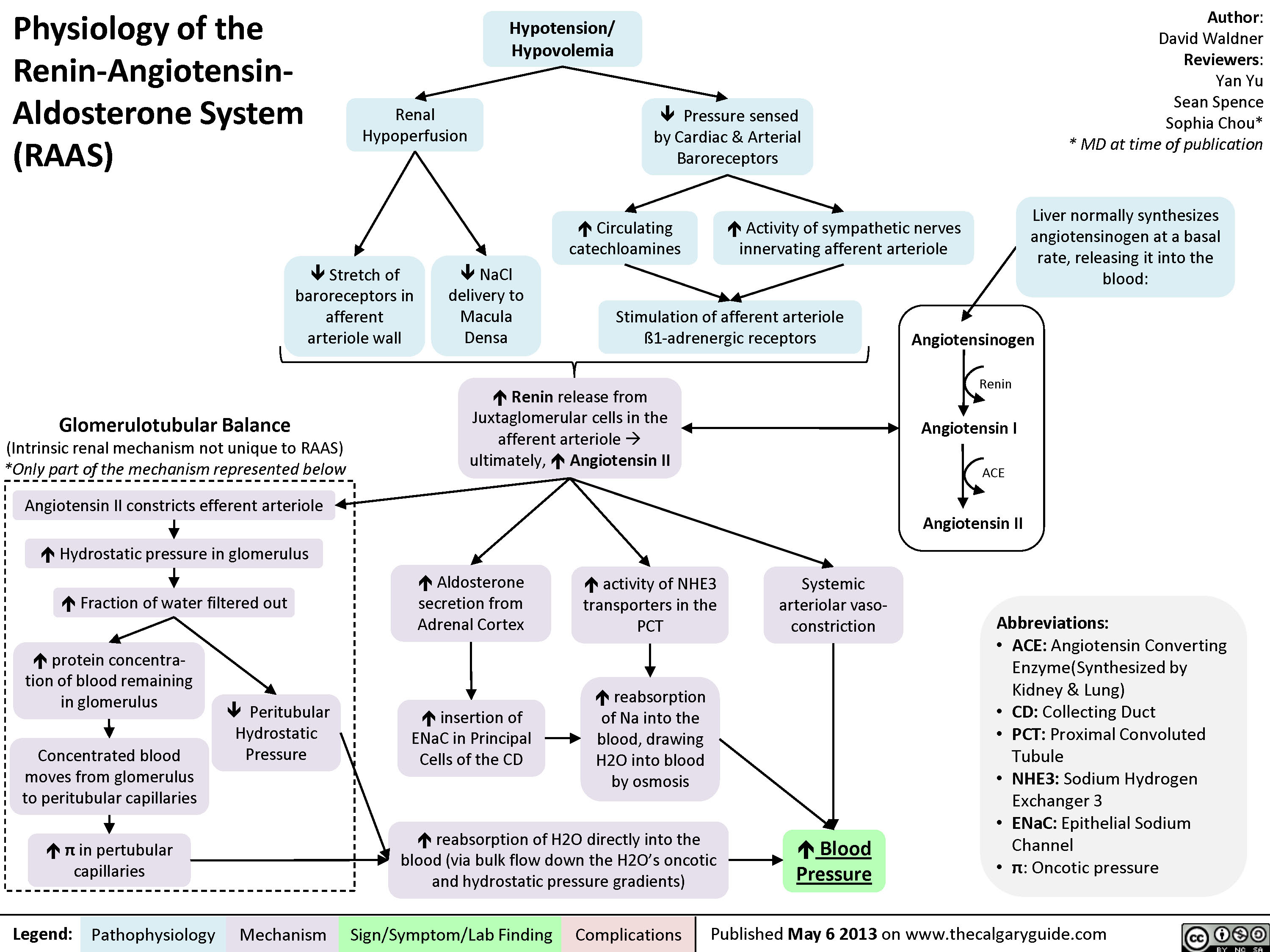
Physiology of the Renin-Angiotensin-Aldosterone System (RAAS)
Hypokalemia: Clinical Findings
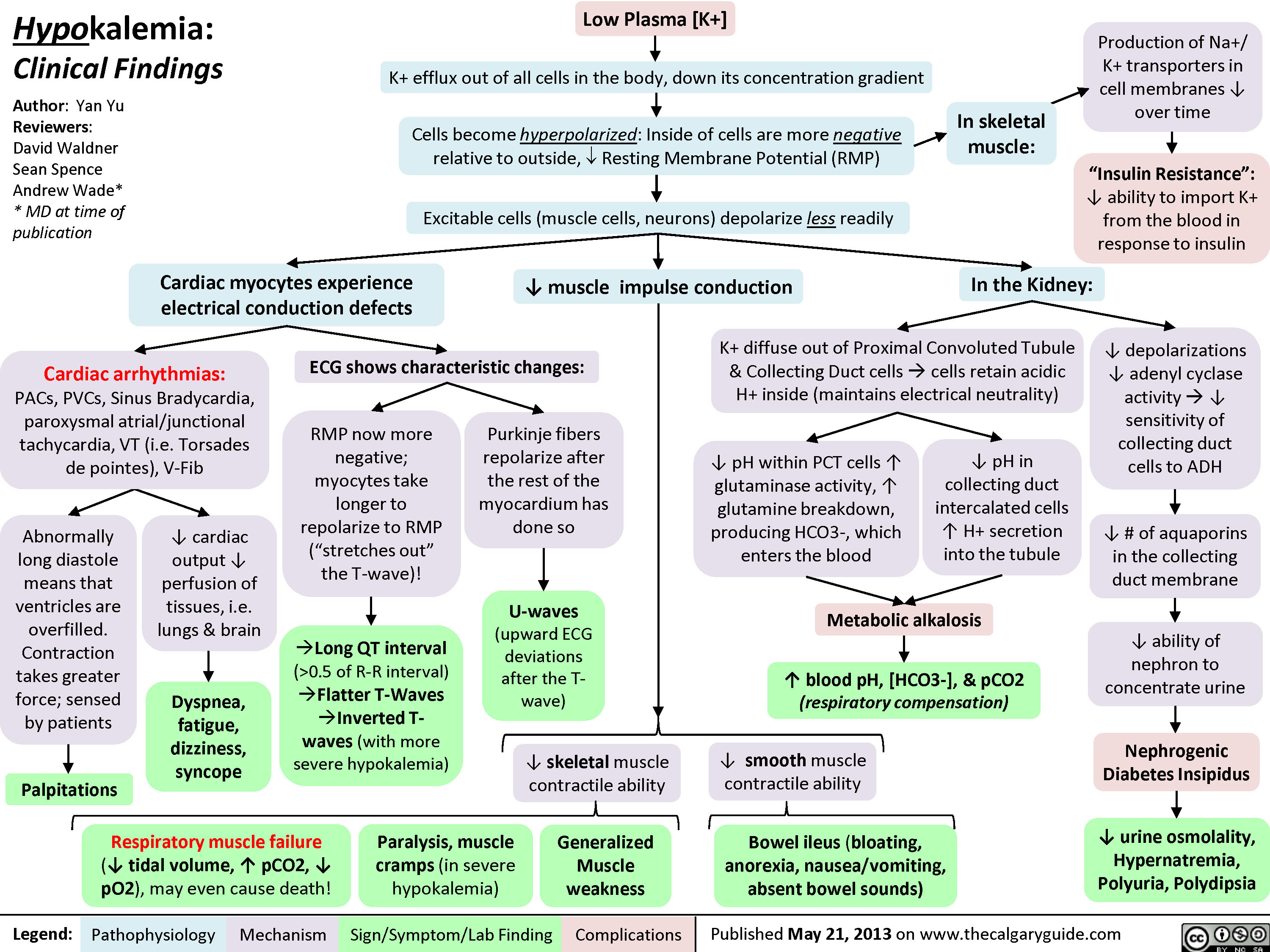 0.5 of R-R interval)?Flatter T-Waves ?Inverted T-waves (with more severe hypokalemia)Purkinje fibers repolarize after the rest of the myocardium has done soU-waves (upward ECG deviations after the T-wave)Cells become hyperpolarized: Inside of cells are more negative relative to outside, ? Resting Membrane Potential (RMP)In the Kidney:Generalized Muscle weaknessK+ diffuse out of Proximal Convoluted Tubule & Collecting Duct cells ? cells retain acidic H+ inside (maintains electrical neutrality)? pH within PCT cells ? glutaminase activity, ? glutamine breakdown, producing HCO3-, which enters the blood? blood pH, [HCO3-], & pCO2 (respiratory compensation)Low Plasma [K+]Abnormally long diastole means that ventricles are overfilled. Contraction takes greater force; sensed by patientsDyspnea, fatigue, dizziness, syncope? cardiac output ? perfusion of tissues, i.e. lungs & brainCardiac arrhythmias: PACs, PVCs, Sinus Bradycardia, paroxysmal atrial/junctional tachycardia, VT (i.e. Torsades de pointes), V-Fib? smooth muscle contractile abilityBowel ileus (bloating, anorexia, nausea/vomiting, absent bowel sounds)? pH in collecting duct intercalated cells ? H+ secretion into the tubuleMetabolic alkalosisParalysis, muscle cramps (in severe hypokalemia)Respiratory muscle failure (? tidal volume, ? pCO2, ? pO2), may even cause death!? depolarizations ? adenyl cyclase activity ? ? sensitivity of collecting duct cells to ADH? ability of nephron to concentrate urineNephrogenic Diabetes Insipidus? urine osmolality, Hypernatremia, Polyuria, Polydipsia? # of aquaporins in the collecting duct membrane"Insulin Resistance": ? ability to import K+ from the blood in response to insulinIn skeletal muscle:
117 kB / 307 word" title="Yu, Yan - Hypokalemia clinical findings - FINAL.pptx
Production of Na+/ K+ transporters in cell membranes ? over timeHypokalemia: Clinical FindingsAuthor: Yan YuReviewers:David WaldnerSean SpenceAndrew Wade** MD at time of publicationLegend:Published May 21, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsPalpitationsExcitable cells (muscle cells, neurons) depolarize less readilyK+ efflux out of all cells in the body, down its concentration gradientCardiac myocytes experience electrical conduction defects? muscle impulse conductionECG shows characteristic changes:? skeletal muscle contractile abilityRMP now more negative; myocytes take longer to repolarize to RMP("stretches out" the T-wave)! Long QT interval (>0.5 of R-R interval)?Flatter T-Waves ?Inverted T-waves (with more severe hypokalemia)Purkinje fibers repolarize after the rest of the myocardium has done soU-waves (upward ECG deviations after the T-wave)Cells become hyperpolarized: Inside of cells are more negative relative to outside, ? Resting Membrane Potential (RMP)In the Kidney:Generalized Muscle weaknessK+ diffuse out of Proximal Convoluted Tubule & Collecting Duct cells ? cells retain acidic H+ inside (maintains electrical neutrality)? pH within PCT cells ? glutaminase activity, ? glutamine breakdown, producing HCO3-, which enters the blood? blood pH, [HCO3-], & pCO2 (respiratory compensation)Low Plasma [K+]Abnormally long diastole means that ventricles are overfilled. Contraction takes greater force; sensed by patientsDyspnea, fatigue, dizziness, syncope? cardiac output ? perfusion of tissues, i.e. lungs & brainCardiac arrhythmias: PACs, PVCs, Sinus Bradycardia, paroxysmal atrial/junctional tachycardia, VT (i.e. Torsades de pointes), V-Fib? smooth muscle contractile abilityBowel ileus (bloating, anorexia, nausea/vomiting, absent bowel sounds)? pH in collecting duct intercalated cells ? H+ secretion into the tubuleMetabolic alkalosisParalysis, muscle cramps (in severe hypokalemia)Respiratory muscle failure (? tidal volume, ? pCO2, ? pO2), may even cause death!? depolarizations ? adenyl cyclase activity ? ? sensitivity of collecting duct cells to ADH? ability of nephron to concentrate urineNephrogenic Diabetes Insipidus? urine osmolality, Hypernatremia, Polyuria, Polydipsia? # of aquaporins in the collecting duct membrane"Insulin Resistance": ? ability to import K+ from the blood in response to insulinIn skeletal muscle:
117 kB / 307 word" />
0.5 of R-R interval)?Flatter T-Waves ?Inverted T-waves (with more severe hypokalemia)Purkinje fibers repolarize after the rest of the myocardium has done soU-waves (upward ECG deviations after the T-wave)Cells become hyperpolarized: Inside of cells are more negative relative to outside, ? Resting Membrane Potential (RMP)In the Kidney:Generalized Muscle weaknessK+ diffuse out of Proximal Convoluted Tubule & Collecting Duct cells ? cells retain acidic H+ inside (maintains electrical neutrality)? pH within PCT cells ? glutaminase activity, ? glutamine breakdown, producing HCO3-, which enters the blood? blood pH, [HCO3-], & pCO2 (respiratory compensation)Low Plasma [K+]Abnormally long diastole means that ventricles are overfilled. Contraction takes greater force; sensed by patientsDyspnea, fatigue, dizziness, syncope? cardiac output ? perfusion of tissues, i.e. lungs & brainCardiac arrhythmias: PACs, PVCs, Sinus Bradycardia, paroxysmal atrial/junctional tachycardia, VT (i.e. Torsades de pointes), V-Fib? smooth muscle contractile abilityBowel ileus (bloating, anorexia, nausea/vomiting, absent bowel sounds)? pH in collecting duct intercalated cells ? H+ secretion into the tubuleMetabolic alkalosisParalysis, muscle cramps (in severe hypokalemia)Respiratory muscle failure (? tidal volume, ? pCO2, ? pO2), may even cause death!? depolarizations ? adenyl cyclase activity ? ? sensitivity of collecting duct cells to ADH? ability of nephron to concentrate urineNephrogenic Diabetes Insipidus? urine osmolality, Hypernatremia, Polyuria, Polydipsia? # of aquaporins in the collecting duct membrane"Insulin Resistance": ? ability to import K+ from the blood in response to insulinIn skeletal muscle:
117 kB / 307 word" title="Yu, Yan - Hypokalemia clinical findings - FINAL.pptx
Production of Na+/ K+ transporters in cell membranes ? over timeHypokalemia: Clinical FindingsAuthor: Yan YuReviewers:David WaldnerSean SpenceAndrew Wade** MD at time of publicationLegend:Published May 21, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsPalpitationsExcitable cells (muscle cells, neurons) depolarize less readilyK+ efflux out of all cells in the body, down its concentration gradientCardiac myocytes experience electrical conduction defects? muscle impulse conductionECG shows characteristic changes:? skeletal muscle contractile abilityRMP now more negative; myocytes take longer to repolarize to RMP("stretches out" the T-wave)! Long QT interval (>0.5 of R-R interval)?Flatter T-Waves ?Inverted T-waves (with more severe hypokalemia)Purkinje fibers repolarize after the rest of the myocardium has done soU-waves (upward ECG deviations after the T-wave)Cells become hyperpolarized: Inside of cells are more negative relative to outside, ? Resting Membrane Potential (RMP)In the Kidney:Generalized Muscle weaknessK+ diffuse out of Proximal Convoluted Tubule & Collecting Duct cells ? cells retain acidic H+ inside (maintains electrical neutrality)? pH within PCT cells ? glutaminase activity, ? glutamine breakdown, producing HCO3-, which enters the blood? blood pH, [HCO3-], & pCO2 (respiratory compensation)Low Plasma [K+]Abnormally long diastole means that ventricles are overfilled. Contraction takes greater force; sensed by patientsDyspnea, fatigue, dizziness, syncope? cardiac output ? perfusion of tissues, i.e. lungs & brainCardiac arrhythmias: PACs, PVCs, Sinus Bradycardia, paroxysmal atrial/junctional tachycardia, VT (i.e. Torsades de pointes), V-Fib? smooth muscle contractile abilityBowel ileus (bloating, anorexia, nausea/vomiting, absent bowel sounds)? pH in collecting duct intercalated cells ? H+ secretion into the tubuleMetabolic alkalosisParalysis, muscle cramps (in severe hypokalemia)Respiratory muscle failure (? tidal volume, ? pCO2, ? pO2), may even cause death!? depolarizations ? adenyl cyclase activity ? ? sensitivity of collecting duct cells to ADH? ability of nephron to concentrate urineNephrogenic Diabetes Insipidus? urine osmolality, Hypernatremia, Polyuria, Polydipsia? # of aquaporins in the collecting duct membrane"Insulin Resistance": ? ability to import K+ from the blood in response to insulinIn skeletal muscle:
117 kB / 307 word" />
Hyperkalemia: Clinical Findings
![Yu, Yan - Hyperkalemia clinical findings - Published.pptx
Hyperkalemia: Clinical FindingsAuthor: Yan YuReviewers:Alexander ArnoldDavid WaldnerSean SpenceAndrew Wade** MD at time of publicationLegend:Published September 9, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsPalpitationsNotes: Symptoms usually manifest when plasma [K+] > 7.0 mmol/L, but can occur at lower [K+]s when hyperkalemia is acute.ECG changes can, but don't necessarily, correlate with a particular [K+].Initially: Excitable cells (muscle cells, neurons) undergo action potentials more readily? [K+ ] gradient between cells and the blood (K+ tends to stay inside cells, less K+ diffuses out)In the Heart:In Skeletal Muscle:[K+] >5.5 mmol/L :faster myocardial repolarization(](http://calgaryguide.ucalgary.ca/wp-content/uploads/2014/09/hyperkalemiaclinicalfindings.jpg) 6.5 mmol/L:? atrial conduction; slow signal transmission from SA to AV nodeCells become slightly depolarized: Resting Membrane Potential (RMP) is brought closer to thresholdIn the Kidney:Muscle weakness and even paralysis (respiratory muscle weakness is rare)? reabsorption of Na+ from Cortical Collecting Duct (CCD)CCD lumen remains more positively chargedMetabolic Acidosis(normal anion gap)Over time (when patients become symptomatic): Chronic membrane depolarization desensitizes voltage-gated Na+ channels (slows their opening) ? ? membrane excitability ? ? action potential generation[K+] > 7.0 mmol/L:? ventricular conductionBradycardiaProlonged, abnormal QRSAV blocks[K+] > 9.0 mmol/L:more conduction abnormalitiesPEA with bizarre wide-QRS rhythmV-fibAsystole? urinary H+ secretion by alpha-intercalated cellsHIGH Plasma [K+] (potassium ion concentration)Dyspnea, fatigue, dizziness, syncope? cardiac output ? ? perfusion of tissues, i.e. lungs & brainCardiac arrhythmias: Conduction blocks (AV block, Bundle branch blocks), VT , V-Fib, Bradycardia, Asystole.?? PR interval ?P-wave flattens, eventually disappearsIf severe, QRS & T-waves fuse:Sine-WavesThe higher the [K+], the slower the voltage-gated Na+ channels open, reflected by distinctive ECG changes:If the K+ is due to ? aldosterone effect ? principal cell dysfunctionHigh pH ? glutamate deamination, which normally produces NH4+? NH4+ reaches the thick ascending limb to be converted to NH3Less NH3 diffuses into the collecting duct to be converted to NH4+ through binding with H+ ? ? NH4+ and therefore ? H+ is excretedK+ moves into proximal tubule cells, causing H+ to diffuse out ? Intracellular alkalosis Irregular force and rhythm of cardiac muscle contraction is sensed by the patient? contraction impulse is conductedDefective electrical conduction through cardiac myocytesMore acid (H=) is retained in the body
118 kB / 357 words" title="Yu, Yan - Hyperkalemia clinical findings - Published.pptx
Hyperkalemia: Clinical FindingsAuthor: Yan YuReviewers:Alexander ArnoldDavid WaldnerSean SpenceAndrew Wade** MD at time of publicationLegend:Published September 9, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsPalpitationsNotes: Symptoms usually manifest when plasma [K+] > 7.0 mmol/L, but can occur at lower [K+]s when hyperkalemia is acute.ECG changes can, but don't necessarily, correlate with a particular [K+].Initially: Excitable cells (muscle cells, neurons) undergo action potentials more readily? [K+ ] gradient between cells and the blood (K+ tends to stay inside cells, less K+ diffuses out)In the Heart:In Skeletal Muscle:[K+] >5.5 mmol/L :faster myocardial repolarization("squeezes up" T-wave)Tall, peaked T-Waves Short QT interval (<0.5 of RR interval)[K+] > 6.5 mmol/L:? atrial conduction; slow signal transmission from SA to AV nodeCells become slightly depolarized: Resting Membrane Potential (RMP) is brought closer to thresholdIn the Kidney:Muscle weakness and even paralysis (respiratory muscle weakness is rare)? reabsorption of Na+ from Cortical Collecting Duct (CCD)CCD lumen remains more positively chargedMetabolic Acidosis(normal anion gap)Over time (when patients become symptomatic): Chronic membrane depolarization desensitizes voltage-gated Na+ channels (slows their opening) ? ? membrane excitability ? ? action potential generation[K+] > 7.0 mmol/L:? ventricular conductionBradycardiaProlonged, abnormal QRSAV blocks[K+] > 9.0 mmol/L:more conduction abnormalitiesPEA with bizarre wide-QRS rhythmV-fibAsystole? urinary H+ secretion by alpha-intercalated cellsHIGH Plasma [K+] (potassium ion concentration)Dyspnea, fatigue, dizziness, syncope? cardiac output ? ? perfusion of tissues, i.e. lungs & brainCardiac arrhythmias: Conduction blocks (AV block, Bundle branch blocks), VT , V-Fib, Bradycardia, Asystole.?? PR interval ?P-wave flattens, eventually disappearsIf severe, QRS & T-waves fuse:Sine-WavesThe higher the [K+], the slower the voltage-gated Na+ channels open, reflected by distinctive ECG changes:If the K+ is due to ? aldosterone effect ? principal cell dysfunctionHigh pH ? glutamate deamination, which normally produces NH4+? NH4+ reaches the thick ascending limb to be converted to NH3Less NH3 diffuses into the collecting duct to be converted to NH4+ through binding with H+ ? ? NH4+ and therefore ? H+ is excretedK+ moves into proximal tubule cells, causing H+ to diffuse out ? Intracellular alkalosis Irregular force and rhythm of cardiac muscle contraction is sensed by the patient? contraction impulse is conductedDefective electrical conduction through cardiac myocytesMore acid (H=) is retained in the body
118 kB / 357 words" />
6.5 mmol/L:? atrial conduction; slow signal transmission from SA to AV nodeCells become slightly depolarized: Resting Membrane Potential (RMP) is brought closer to thresholdIn the Kidney:Muscle weakness and even paralysis (respiratory muscle weakness is rare)? reabsorption of Na+ from Cortical Collecting Duct (CCD)CCD lumen remains more positively chargedMetabolic Acidosis(normal anion gap)Over time (when patients become symptomatic): Chronic membrane depolarization desensitizes voltage-gated Na+ channels (slows their opening) ? ? membrane excitability ? ? action potential generation[K+] > 7.0 mmol/L:? ventricular conductionBradycardiaProlonged, abnormal QRSAV blocks[K+] > 9.0 mmol/L:more conduction abnormalitiesPEA with bizarre wide-QRS rhythmV-fibAsystole? urinary H+ secretion by alpha-intercalated cellsHIGH Plasma [K+] (potassium ion concentration)Dyspnea, fatigue, dizziness, syncope? cardiac output ? ? perfusion of tissues, i.e. lungs & brainCardiac arrhythmias: Conduction blocks (AV block, Bundle branch blocks), VT , V-Fib, Bradycardia, Asystole.?? PR interval ?P-wave flattens, eventually disappearsIf severe, QRS & T-waves fuse:Sine-WavesThe higher the [K+], the slower the voltage-gated Na+ channels open, reflected by distinctive ECG changes:If the K+ is due to ? aldosterone effect ? principal cell dysfunctionHigh pH ? glutamate deamination, which normally produces NH4+? NH4+ reaches the thick ascending limb to be converted to NH3Less NH3 diffuses into the collecting duct to be converted to NH4+ through binding with H+ ? ? NH4+ and therefore ? H+ is excretedK+ moves into proximal tubule cells, causing H+ to diffuse out ? Intracellular alkalosis Irregular force and rhythm of cardiac muscle contraction is sensed by the patient? contraction impulse is conductedDefective electrical conduction through cardiac myocytesMore acid (H=) is retained in the body
118 kB / 357 words" title="Yu, Yan - Hyperkalemia clinical findings - Published.pptx
Hyperkalemia: Clinical FindingsAuthor: Yan YuReviewers:Alexander ArnoldDavid WaldnerSean SpenceAndrew Wade** MD at time of publicationLegend:Published September 9, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsPalpitationsNotes: Symptoms usually manifest when plasma [K+] > 7.0 mmol/L, but can occur at lower [K+]s when hyperkalemia is acute.ECG changes can, but don't necessarily, correlate with a particular [K+].Initially: Excitable cells (muscle cells, neurons) undergo action potentials more readily? [K+ ] gradient between cells and the blood (K+ tends to stay inside cells, less K+ diffuses out)In the Heart:In Skeletal Muscle:[K+] >5.5 mmol/L :faster myocardial repolarization("squeezes up" T-wave)Tall, peaked T-Waves Short QT interval (<0.5 of RR interval)[K+] > 6.5 mmol/L:? atrial conduction; slow signal transmission from SA to AV nodeCells become slightly depolarized: Resting Membrane Potential (RMP) is brought closer to thresholdIn the Kidney:Muscle weakness and even paralysis (respiratory muscle weakness is rare)? reabsorption of Na+ from Cortical Collecting Duct (CCD)CCD lumen remains more positively chargedMetabolic Acidosis(normal anion gap)Over time (when patients become symptomatic): Chronic membrane depolarization desensitizes voltage-gated Na+ channels (slows their opening) ? ? membrane excitability ? ? action potential generation[K+] > 7.0 mmol/L:? ventricular conductionBradycardiaProlonged, abnormal QRSAV blocks[K+] > 9.0 mmol/L:more conduction abnormalitiesPEA with bizarre wide-QRS rhythmV-fibAsystole? urinary H+ secretion by alpha-intercalated cellsHIGH Plasma [K+] (potassium ion concentration)Dyspnea, fatigue, dizziness, syncope? cardiac output ? ? perfusion of tissues, i.e. lungs & brainCardiac arrhythmias: Conduction blocks (AV block, Bundle branch blocks), VT , V-Fib, Bradycardia, Asystole.?? PR interval ?P-wave flattens, eventually disappearsIf severe, QRS & T-waves fuse:Sine-WavesThe higher the [K+], the slower the voltage-gated Na+ channels open, reflected by distinctive ECG changes:If the K+ is due to ? aldosterone effect ? principal cell dysfunctionHigh pH ? glutamate deamination, which normally produces NH4+? NH4+ reaches the thick ascending limb to be converted to NH3Less NH3 diffuses into the collecting duct to be converted to NH4+ through binding with H+ ? ? NH4+ and therefore ? H+ is excretedK+ moves into proximal tubule cells, causing H+ to diffuse out ? Intracellular alkalosis Irregular force and rhythm of cardiac muscle contraction is sensed by the patient? contraction impulse is conductedDefective electrical conduction through cardiac myocytesMore acid (H=) is retained in the body
118 kB / 357 words" />
Hypocalcemia: Clinical Findings
![Yu, Yan - Hypocalcemia - Clinical Findings - FINAL.pptx
Hypocalcemia: Clinical FindingsAuthor: Yan YuReviewers:David WaldnerSean SpenceGreg Kline** MD at time of publicationLegend:Published May 7, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsHypocalcemia(serum [Ca2+] <2.1mmol/L)Altered sensory ability of peripheral nervesLess Ca2+ outside cells, with no change in + charges inside cellsPeripheral paraesthesia? Neuronal
Yu, Yan - Hypocalcemia - Clinical Findings - FINAL.pptx
Hypocalcemia: Clinical FindingsAuthor: Yan YuReviewers:David WaldnerSean SpenceGreg Kline** MD at time of publicationLegend:Published May 7, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsHypocalcemia(serum [Ca2+] <2.1mmol/L)Altered sensory ability of peripheral nervesLess Ca2+ outside cells, with no change in + charges inside cellsPeripheral paraesthesia? Neuronal](http://calgaryguide.ucalgary.ca/wp-content/uploads/2014/09/Hypocalcemia-Clinical-Findings.jpg)
Hypercalcemia: Clinical Findings
Nephrotic Syndrome: Pathogenesis and Clinical Findings
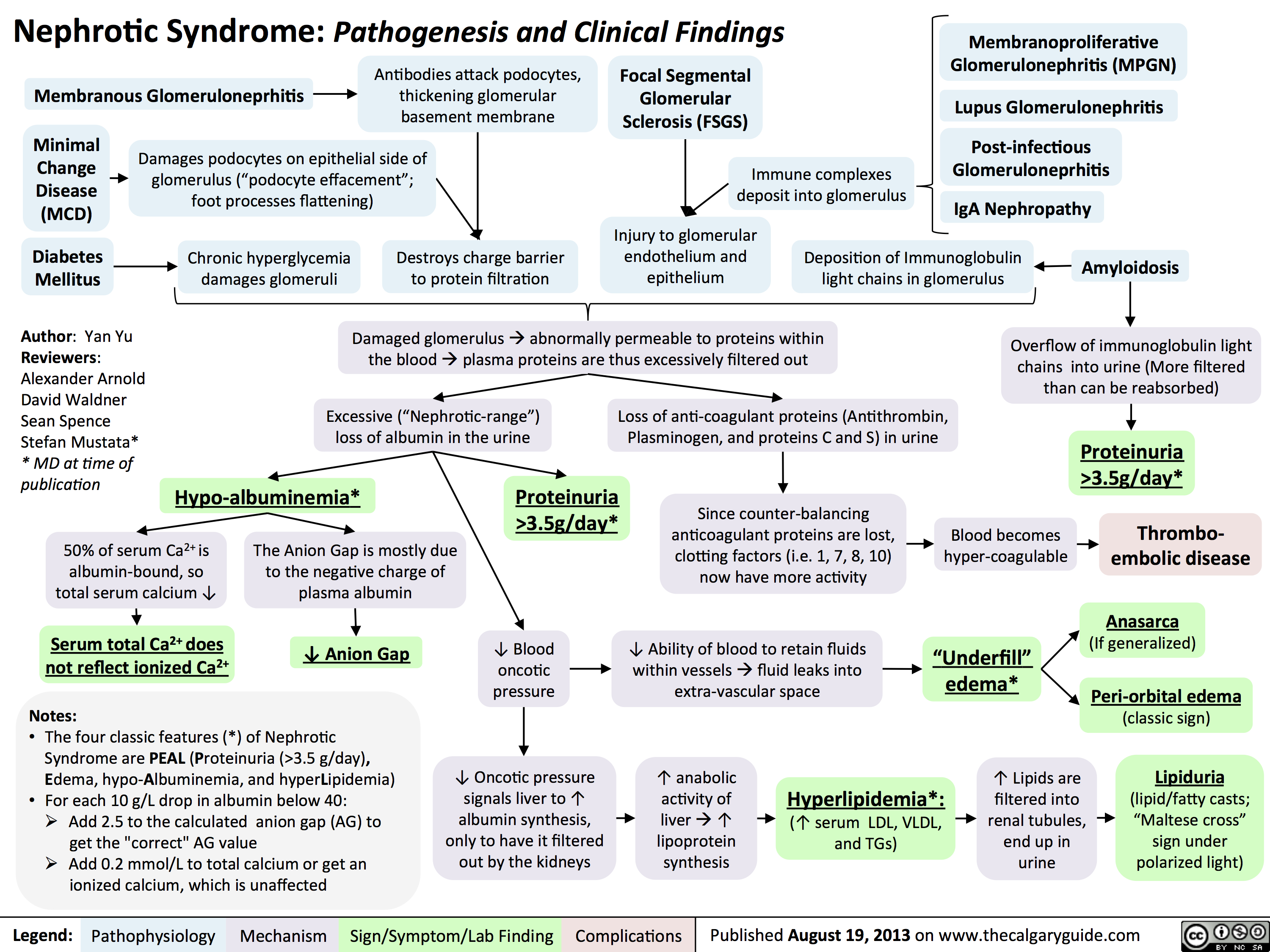 3.5g/day*? Ability of blood to retain fluids within vessels ? fluid leaks into extra-vascular spaceInjury to glomerular endothelium and epitheliumImmune complexes deposit into glomerulusDamaged glomerulus ? abnormally permeable to proteins within the blood ? plasma proteins are thus excessively filtered out? Oncotic pressure signals liver to ? albumin synthesis, only to have it filtered out by the kidneys? anabolic activity of liver ? ? lipoprotein synthesisHyperlipidemia*:(? serum LDL, VLDL, and TGs)Lipiduria(lipid/fatty casts; "Maltese cross" sign under polarized light)Since counter-balancing anticoagulant proteins are lost, clotting factors (i.e. 1, 7, 8, 10) now have more activityThrombo-embolic diseaseBlood becomes hyper-coagulable? Lipids are filtered into renal tubules, end up in urineMembranoproliferative Glomerulonephritis (MPGN)Lupus Glomerulonephritis Post-infectious GlomeruloneprhitisIgA NephropathyDamages podocytes on epithelial side of glomerulus ("podocyte effacement"; foot processes flattening)Diabetes MellitusChronic hyperglycemia damages glomeruliDeposition of Immunoglobulin light chains in glomerulusAmyloidosisAnasarca(If generalized)Peri-orbital edema (classic sign)Focal Segmental Glomerular Sclerosis (FSGS)Membranous GlomeruloneprhitisAntibodies attack podocytes, thickening glomerular basement membraneOverflow of immunoglobulin light chains into urine (More filtered than can be reabsorbed)Proteinuria >3.5g/day*The Anion Gap is mostly due to the negative charge of plasma albumin? Anion GapNotes: The four classic features (*) of Nephrotic Syndrome are PEAL (Proteinuria (>3.5 g/day), Edema, hypo-Albuminemia, and hyperLipidemia)For each 10 g/L drop in albumin below 40:Add 2.5 to the calculated anion gap (AG) to get the "correct" AG valueAdd 0.2 mmol/L to total calcium or get an ionized calcium, which is unaffected50% of serum Ca2+ is albumin-bound, so total serum calcium ? Serum total Ca2+ does not reflect ionized Ca2+ ? Blood oncotic pressure" title="Destroys charge barrier to protein filtrationNephrotic Syndrome: Pathogenesis and Clinical FindingsAuthor: Yan YuReviewers:Alexander ArnoldDavid WaldnerSean SpenceStefan Mustata** MD at time of publicationLegend:Published August 19, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsExcessive ("Nephrotic-range") loss of albumin in the urineHypo-albuminemia*Loss of anti-coagulant proteins (Antithrombin, Plasminogen, and proteins C and S) in urineMinimal Change Disease (MCD)"Underfill" edema*Proteinuria >3.5g/day*? Ability of blood to retain fluids within vessels ? fluid leaks into extra-vascular spaceInjury to glomerular endothelium and epitheliumImmune complexes deposit into glomerulusDamaged glomerulus ? abnormally permeable to proteins within the blood ? plasma proteins are thus excessively filtered out? Oncotic pressure signals liver to ? albumin synthesis, only to have it filtered out by the kidneys? anabolic activity of liver ? ? lipoprotein synthesisHyperlipidemia*:(? serum LDL, VLDL, and TGs)Lipiduria(lipid/fatty casts; "Maltese cross" sign under polarized light)Since counter-balancing anticoagulant proteins are lost, clotting factors (i.e. 1, 7, 8, 10) now have more activityThrombo-embolic diseaseBlood becomes hyper-coagulable? Lipids are filtered into renal tubules, end up in urineMembranoproliferative Glomerulonephritis (MPGN)Lupus Glomerulonephritis Post-infectious GlomeruloneprhitisIgA NephropathyDamages podocytes on epithelial side of glomerulus ("podocyte effacement"; foot processes flattening)Diabetes MellitusChronic hyperglycemia damages glomeruliDeposition of Immunoglobulin light chains in glomerulusAmyloidosisAnasarca(If generalized)Peri-orbital edema (classic sign)Focal Segmental Glomerular Sclerosis (FSGS)Membranous GlomeruloneprhitisAntibodies attack podocytes, thickening glomerular basement membraneOverflow of immunoglobulin light chains into urine (More filtered than can be reabsorbed)Proteinuria >3.5g/day*The Anion Gap is mostly due to the negative charge of plasma albumin? Anion GapNotes: The four classic features (*) of Nephrotic Syndrome are PEAL (Proteinuria (>3.5 g/day), Edema, hypo-Albuminemia, and hyperLipidemia)For each 10 g/L drop in albumin below 40:Add 2.5 to the calculated anion gap (AG) to get the "correct" AG valueAdd 0.2 mmol/L to total calcium or get an ionized calcium, which is unaffected50% of serum Ca2+ is albumin-bound, so total serum calcium ? Serum total Ca2+ does not reflect ionized Ca2+ ? Blood oncotic pressure" />
3.5g/day*? Ability of blood to retain fluids within vessels ? fluid leaks into extra-vascular spaceInjury to glomerular endothelium and epitheliumImmune complexes deposit into glomerulusDamaged glomerulus ? abnormally permeable to proteins within the blood ? plasma proteins are thus excessively filtered out? Oncotic pressure signals liver to ? albumin synthesis, only to have it filtered out by the kidneys? anabolic activity of liver ? ? lipoprotein synthesisHyperlipidemia*:(? serum LDL, VLDL, and TGs)Lipiduria(lipid/fatty casts; "Maltese cross" sign under polarized light)Since counter-balancing anticoagulant proteins are lost, clotting factors (i.e. 1, 7, 8, 10) now have more activityThrombo-embolic diseaseBlood becomes hyper-coagulable? Lipids are filtered into renal tubules, end up in urineMembranoproliferative Glomerulonephritis (MPGN)Lupus Glomerulonephritis Post-infectious GlomeruloneprhitisIgA NephropathyDamages podocytes on epithelial side of glomerulus ("podocyte effacement"; foot processes flattening)Diabetes MellitusChronic hyperglycemia damages glomeruliDeposition of Immunoglobulin light chains in glomerulusAmyloidosisAnasarca(If generalized)Peri-orbital edema (classic sign)Focal Segmental Glomerular Sclerosis (FSGS)Membranous GlomeruloneprhitisAntibodies attack podocytes, thickening glomerular basement membraneOverflow of immunoglobulin light chains into urine (More filtered than can be reabsorbed)Proteinuria >3.5g/day*The Anion Gap is mostly due to the negative charge of plasma albumin? Anion GapNotes: The four classic features (*) of Nephrotic Syndrome are PEAL (Proteinuria (>3.5 g/day), Edema, hypo-Albuminemia, and hyperLipidemia)For each 10 g/L drop in albumin below 40:Add 2.5 to the calculated anion gap (AG) to get the "correct" AG valueAdd 0.2 mmol/L to total calcium or get an ionized calcium, which is unaffected50% of serum Ca2+ is albumin-bound, so total serum calcium ? Serum total Ca2+ does not reflect ionized Ca2+ ? Blood oncotic pressure" title="Destroys charge barrier to protein filtrationNephrotic Syndrome: Pathogenesis and Clinical FindingsAuthor: Yan YuReviewers:Alexander ArnoldDavid WaldnerSean SpenceStefan Mustata** MD at time of publicationLegend:Published August 19, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsExcessive ("Nephrotic-range") loss of albumin in the urineHypo-albuminemia*Loss of anti-coagulant proteins (Antithrombin, Plasminogen, and proteins C and S) in urineMinimal Change Disease (MCD)"Underfill" edema*Proteinuria >3.5g/day*? Ability of blood to retain fluids within vessels ? fluid leaks into extra-vascular spaceInjury to glomerular endothelium and epitheliumImmune complexes deposit into glomerulusDamaged glomerulus ? abnormally permeable to proteins within the blood ? plasma proteins are thus excessively filtered out? Oncotic pressure signals liver to ? albumin synthesis, only to have it filtered out by the kidneys? anabolic activity of liver ? ? lipoprotein synthesisHyperlipidemia*:(? serum LDL, VLDL, and TGs)Lipiduria(lipid/fatty casts; "Maltese cross" sign under polarized light)Since counter-balancing anticoagulant proteins are lost, clotting factors (i.e. 1, 7, 8, 10) now have more activityThrombo-embolic diseaseBlood becomes hyper-coagulable? Lipids are filtered into renal tubules, end up in urineMembranoproliferative Glomerulonephritis (MPGN)Lupus Glomerulonephritis Post-infectious GlomeruloneprhitisIgA NephropathyDamages podocytes on epithelial side of glomerulus ("podocyte effacement"; foot processes flattening)Diabetes MellitusChronic hyperglycemia damages glomeruliDeposition of Immunoglobulin light chains in glomerulusAmyloidosisAnasarca(If generalized)Peri-orbital edema (classic sign)Focal Segmental Glomerular Sclerosis (FSGS)Membranous GlomeruloneprhitisAntibodies attack podocytes, thickening glomerular basement membraneOverflow of immunoglobulin light chains into urine (More filtered than can be reabsorbed)Proteinuria >3.5g/day*The Anion Gap is mostly due to the negative charge of plasma albumin? Anion GapNotes: The four classic features (*) of Nephrotic Syndrome are PEAL (Proteinuria (>3.5 g/day), Edema, hypo-Albuminemia, and hyperLipidemia)For each 10 g/L drop in albumin below 40:Add 2.5 to the calculated anion gap (AG) to get the "correct" AG valueAdd 0.2 mmol/L to total calcium or get an ionized calcium, which is unaffected50% of serum Ca2+ is albumin-bound, so total serum calcium ? Serum total Ca2+ does not reflect ionized Ca2+ ? Blood oncotic pressure" />
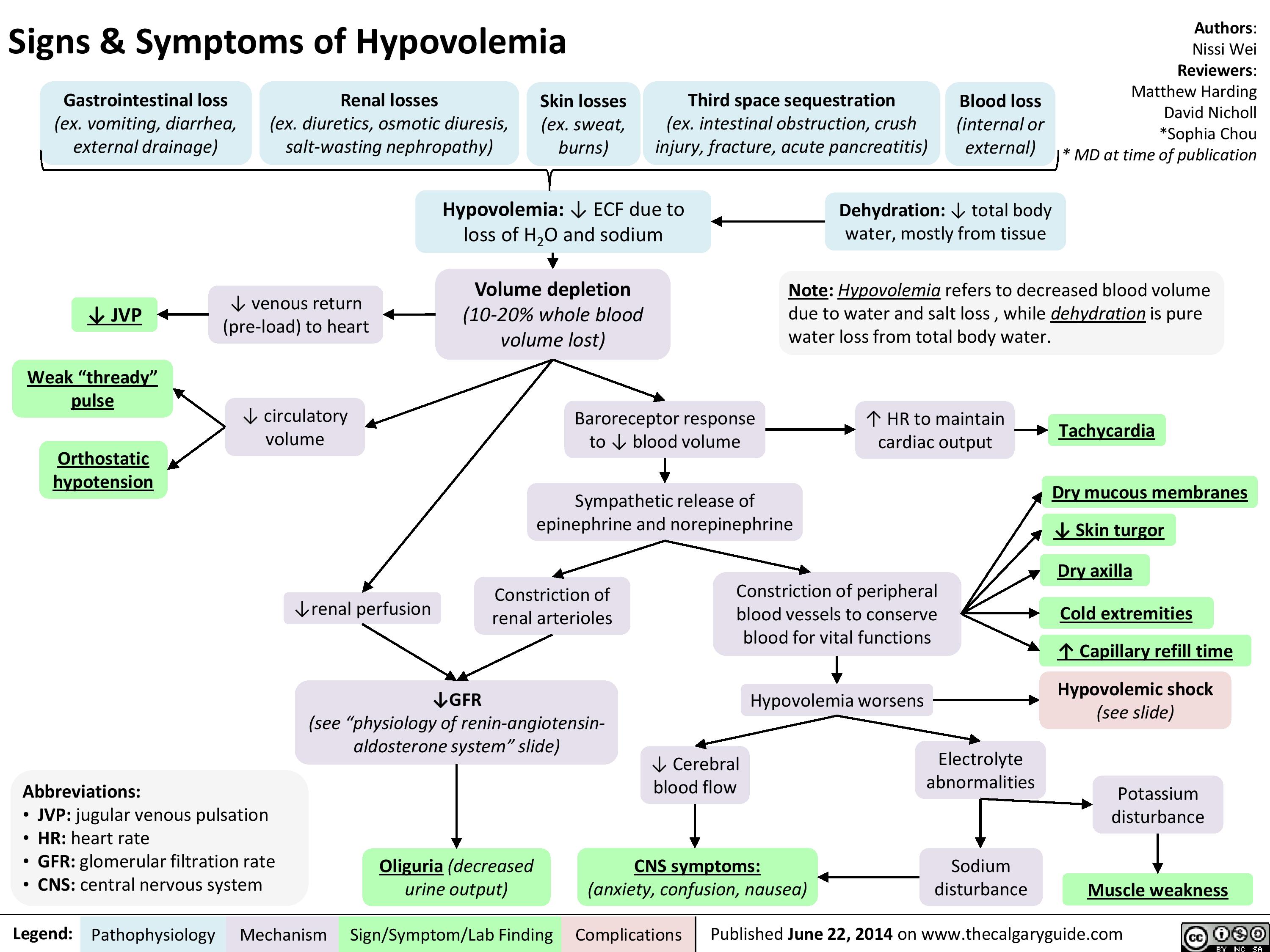
Signs and Symptoms of Hypovolemia
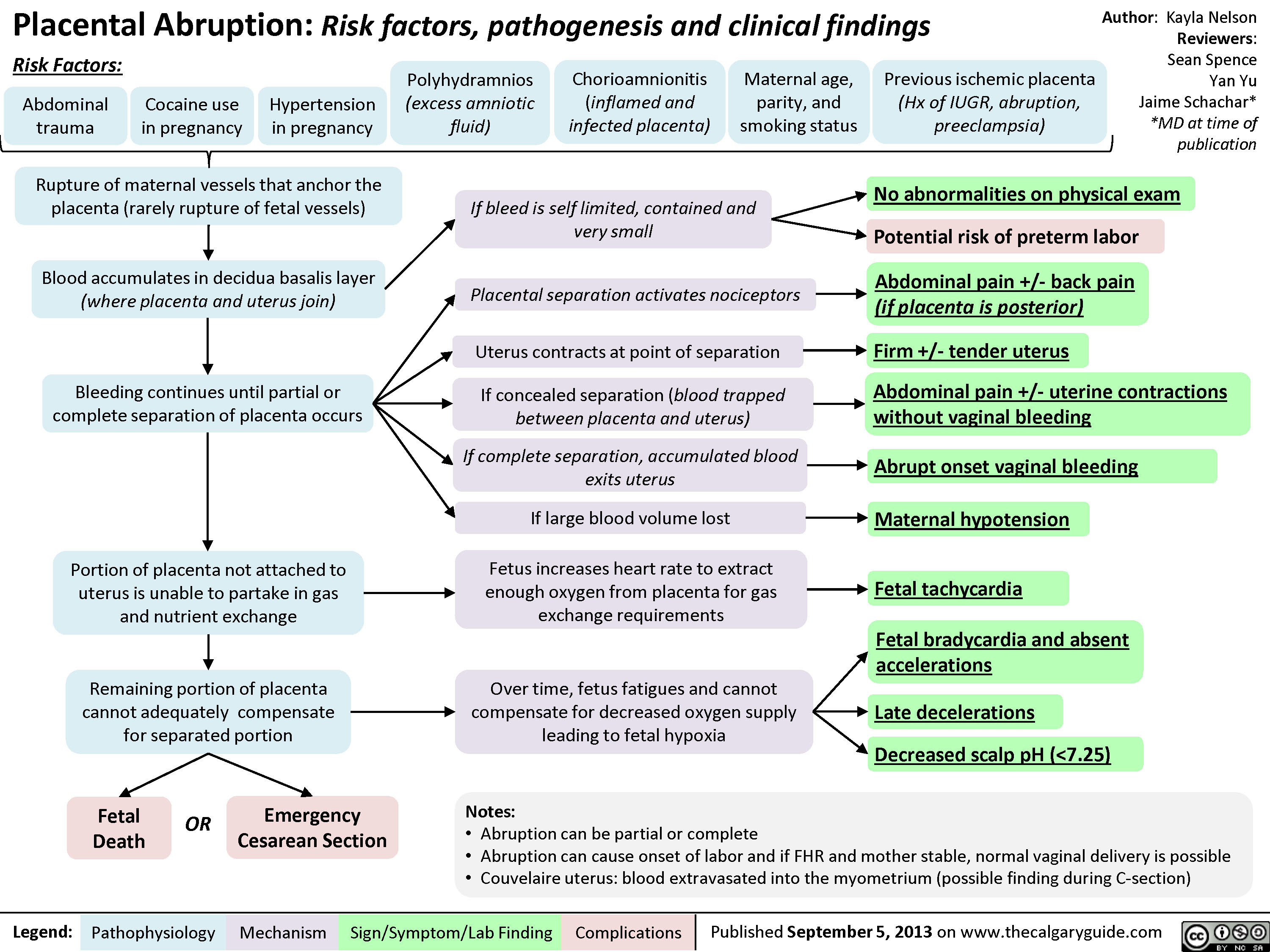
Placental Abruption
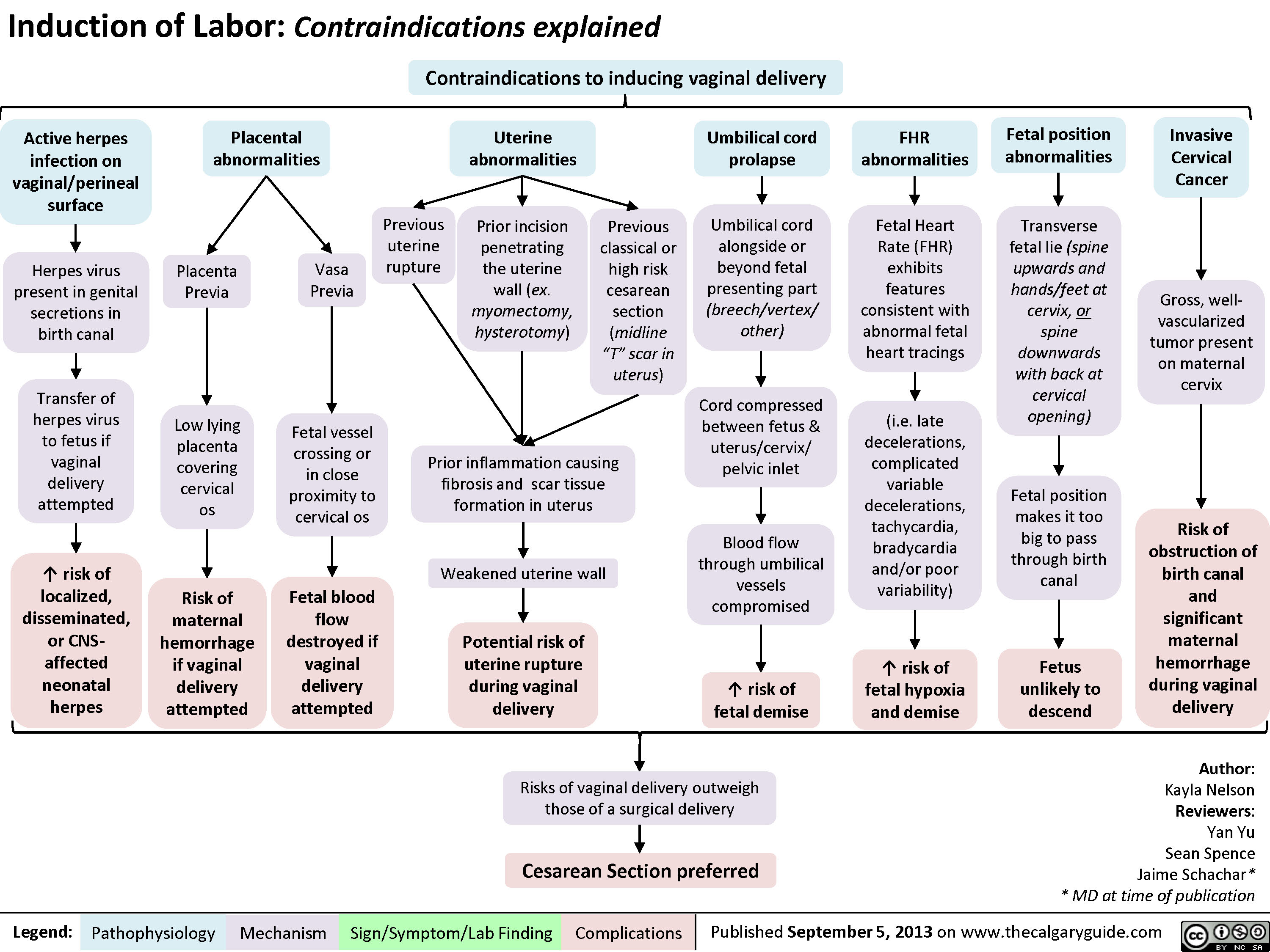
Contraindications to Inducing Vaginal Delivery
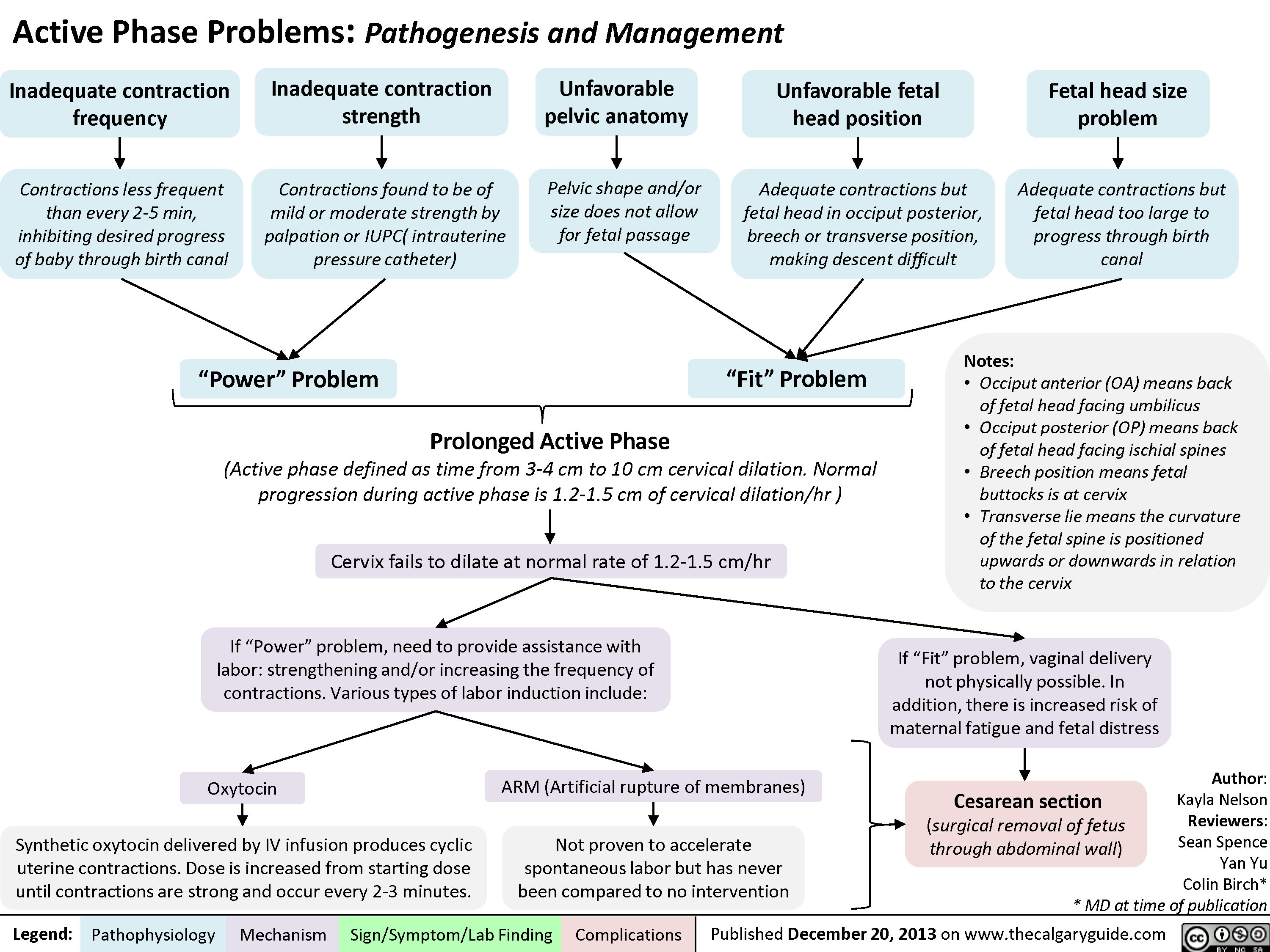
Active Phase Problems: Pathogenesis and Management
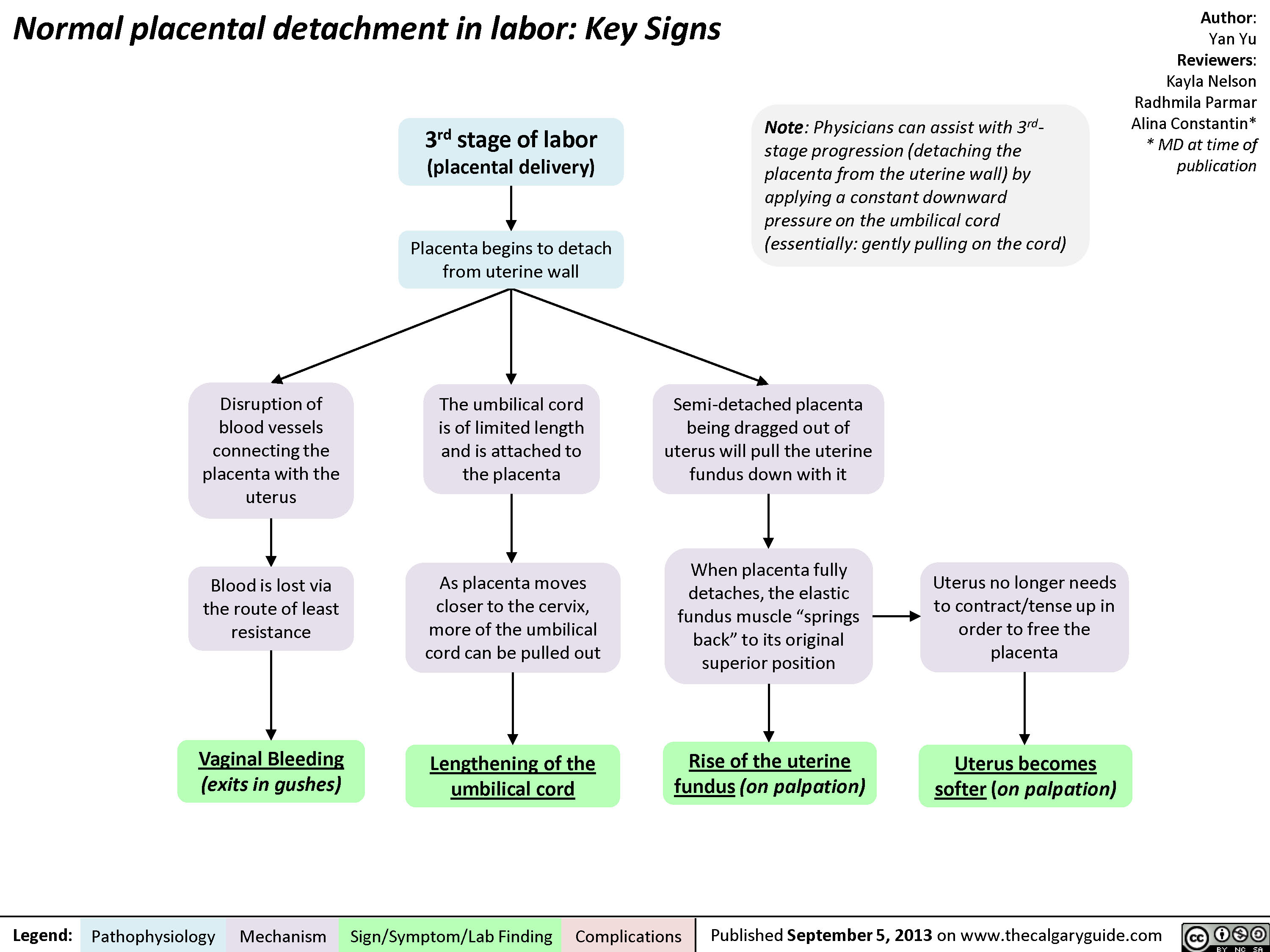
Normal Signs of Placental Detachment
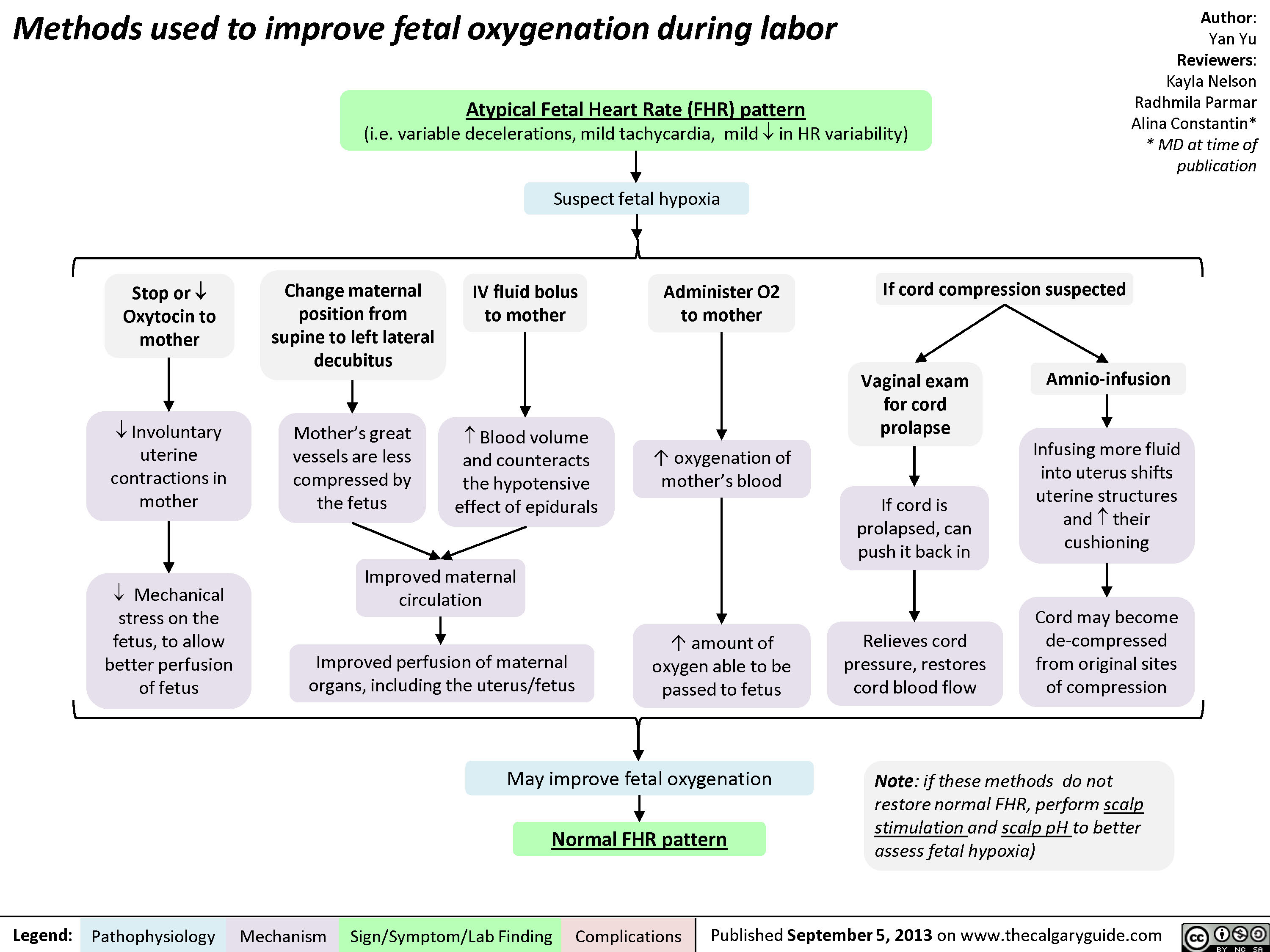
Methods to Improve Fetal Oxygenation
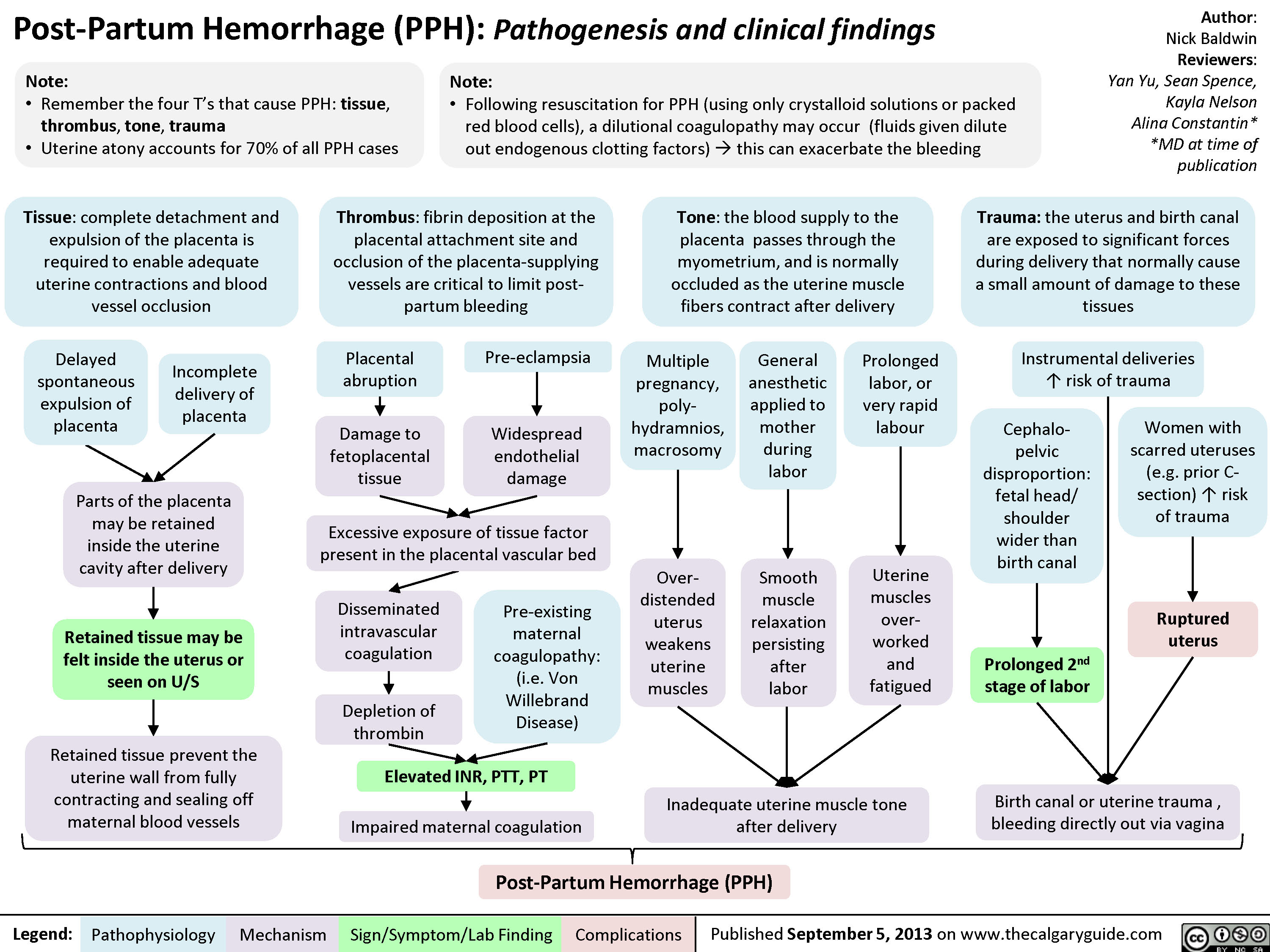
Post-Partum Hemorrhage
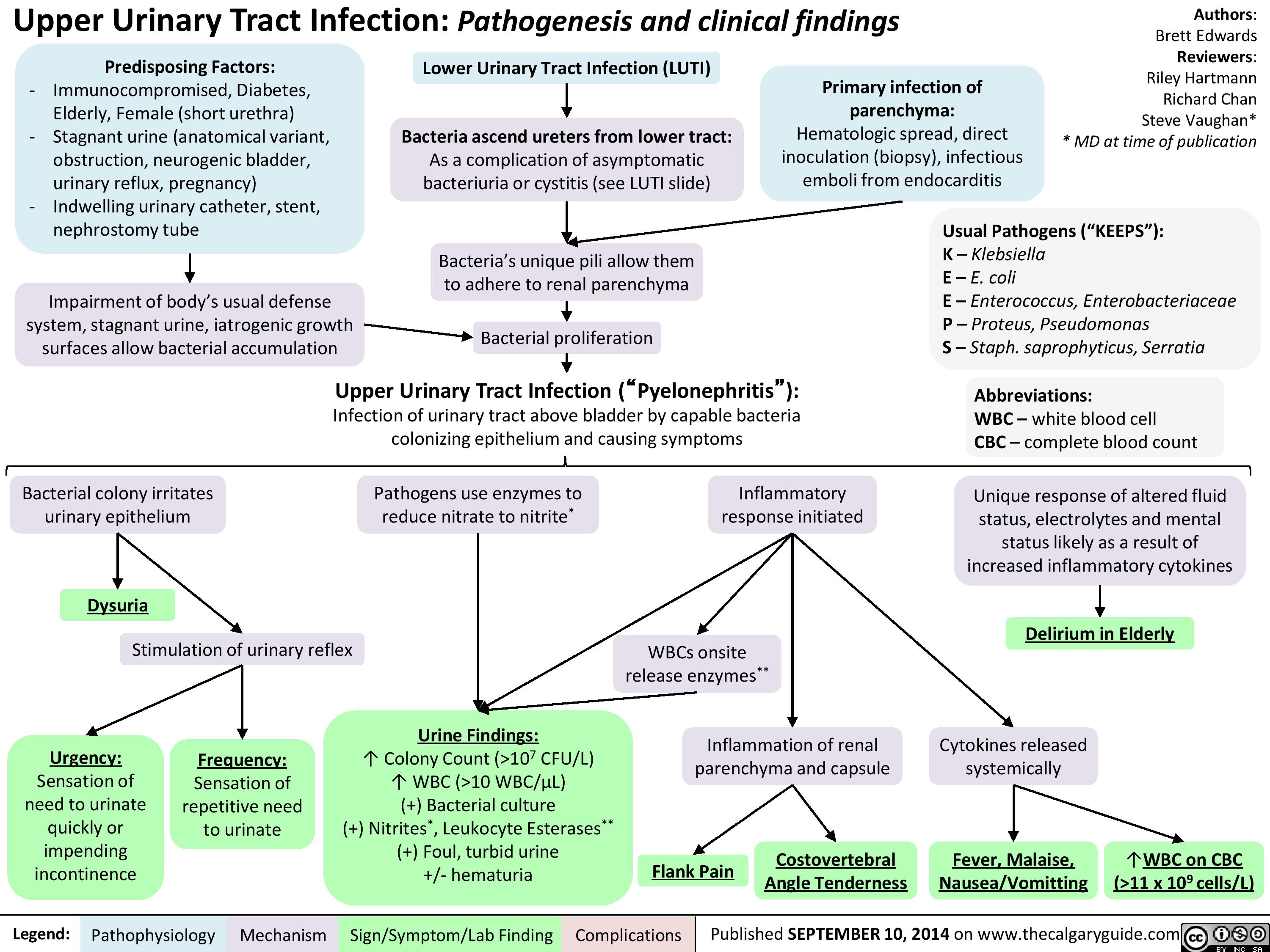
Upper Urinary Tract infection (UUTI): Pathogenesis and Clinical Findings
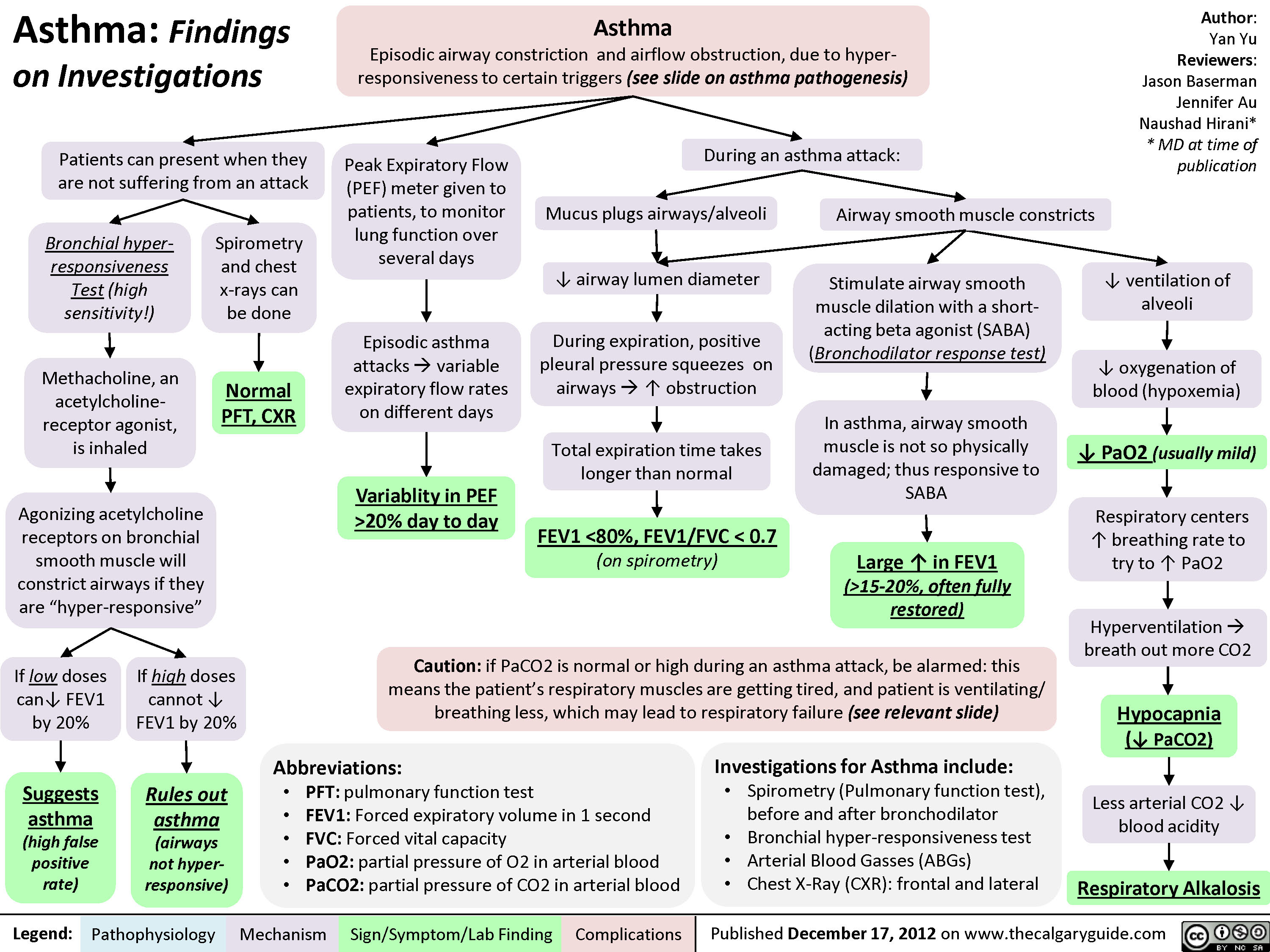
Asthma: Findings on Investigations
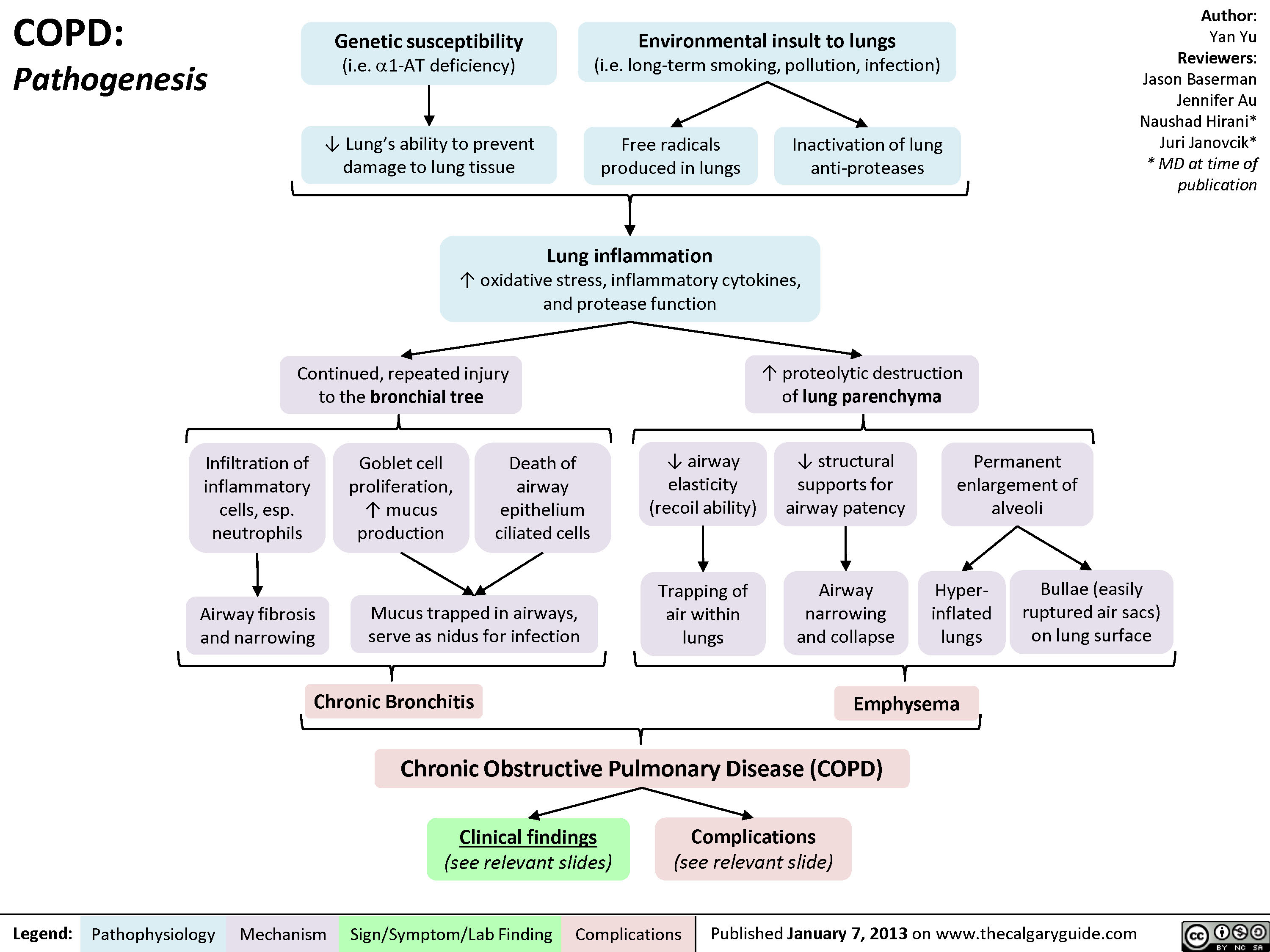
COPD: Pathogenesis
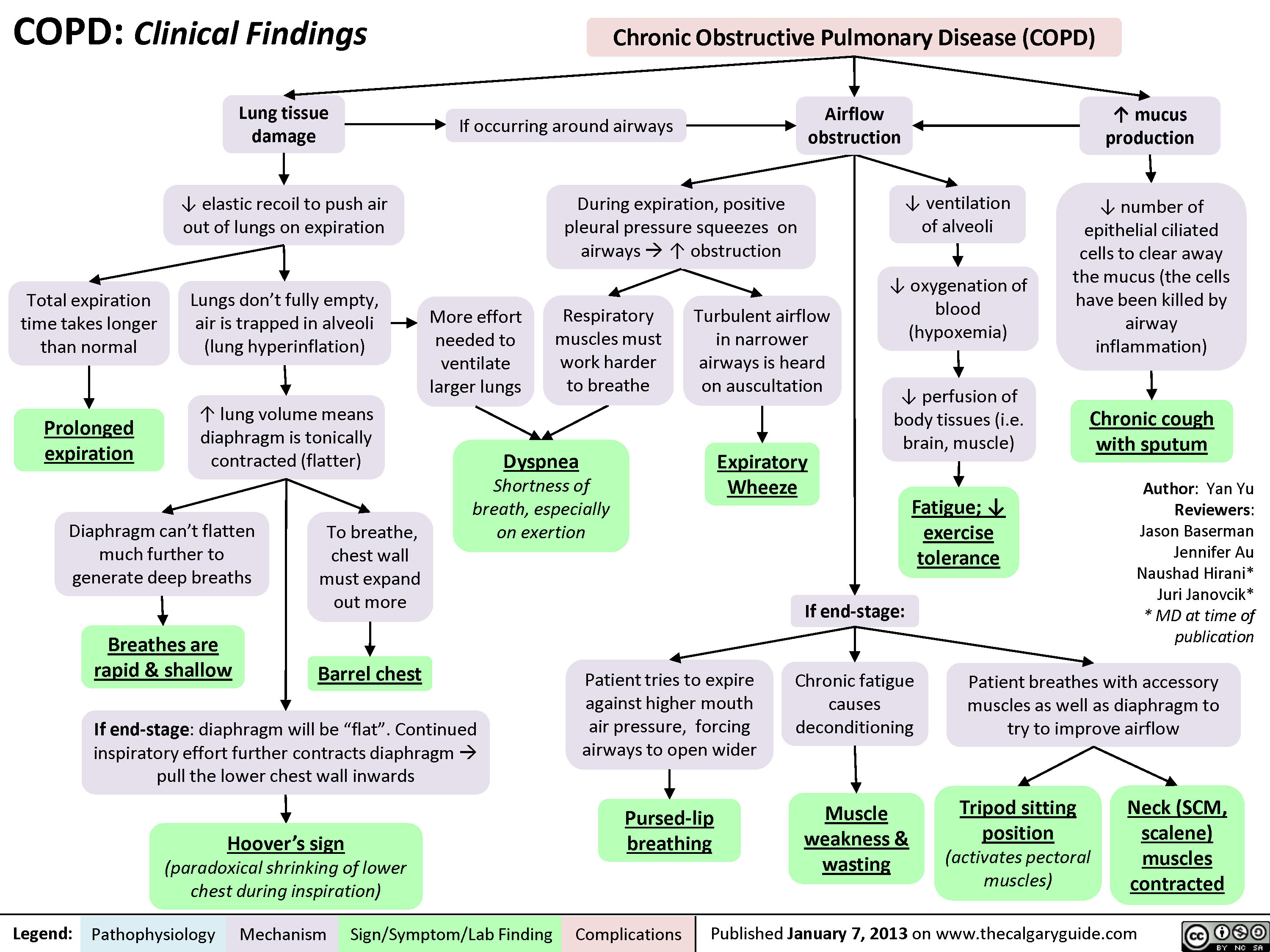
COPD: Clinical Findings
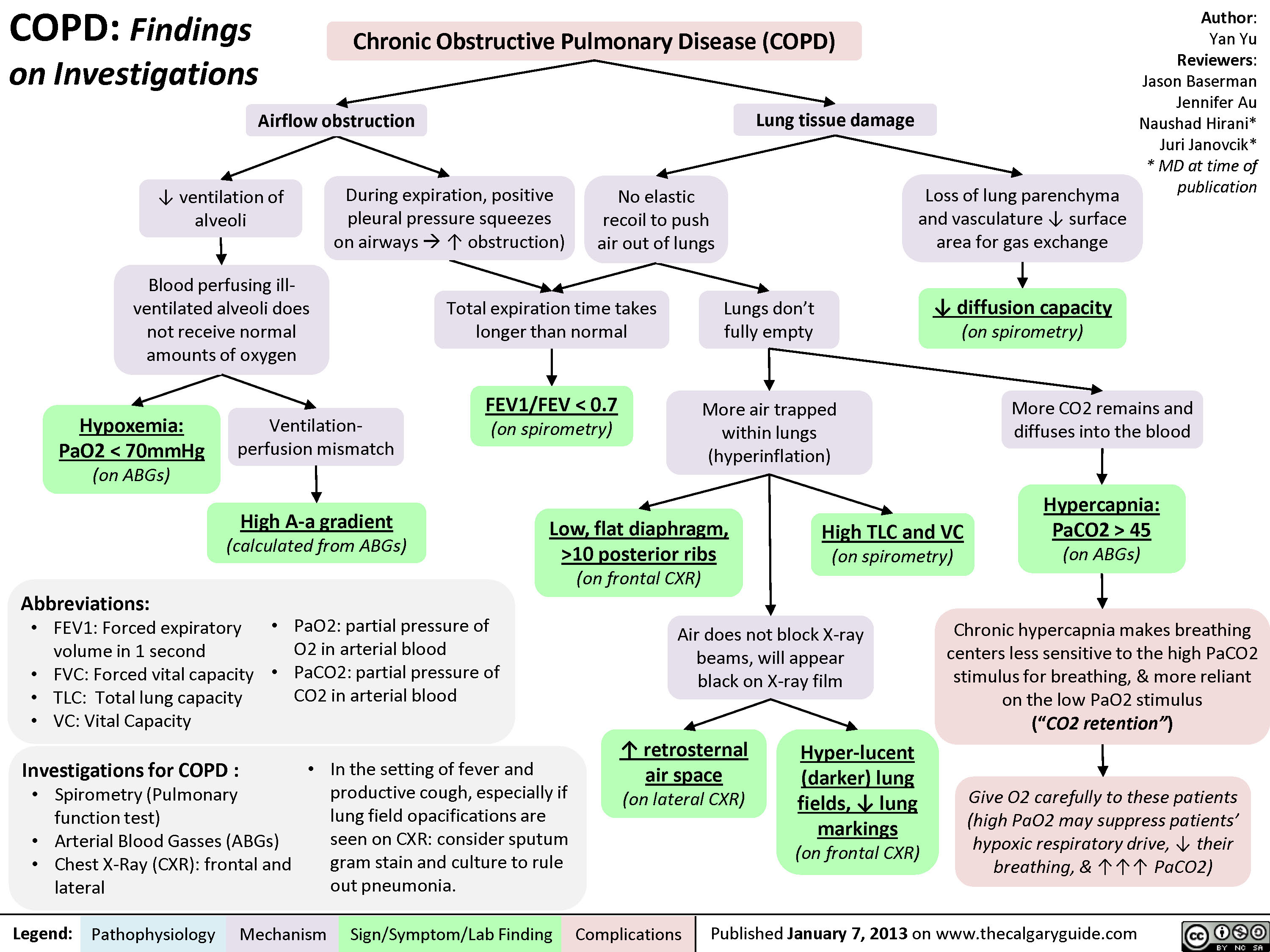
COPD: Findings on Investigations
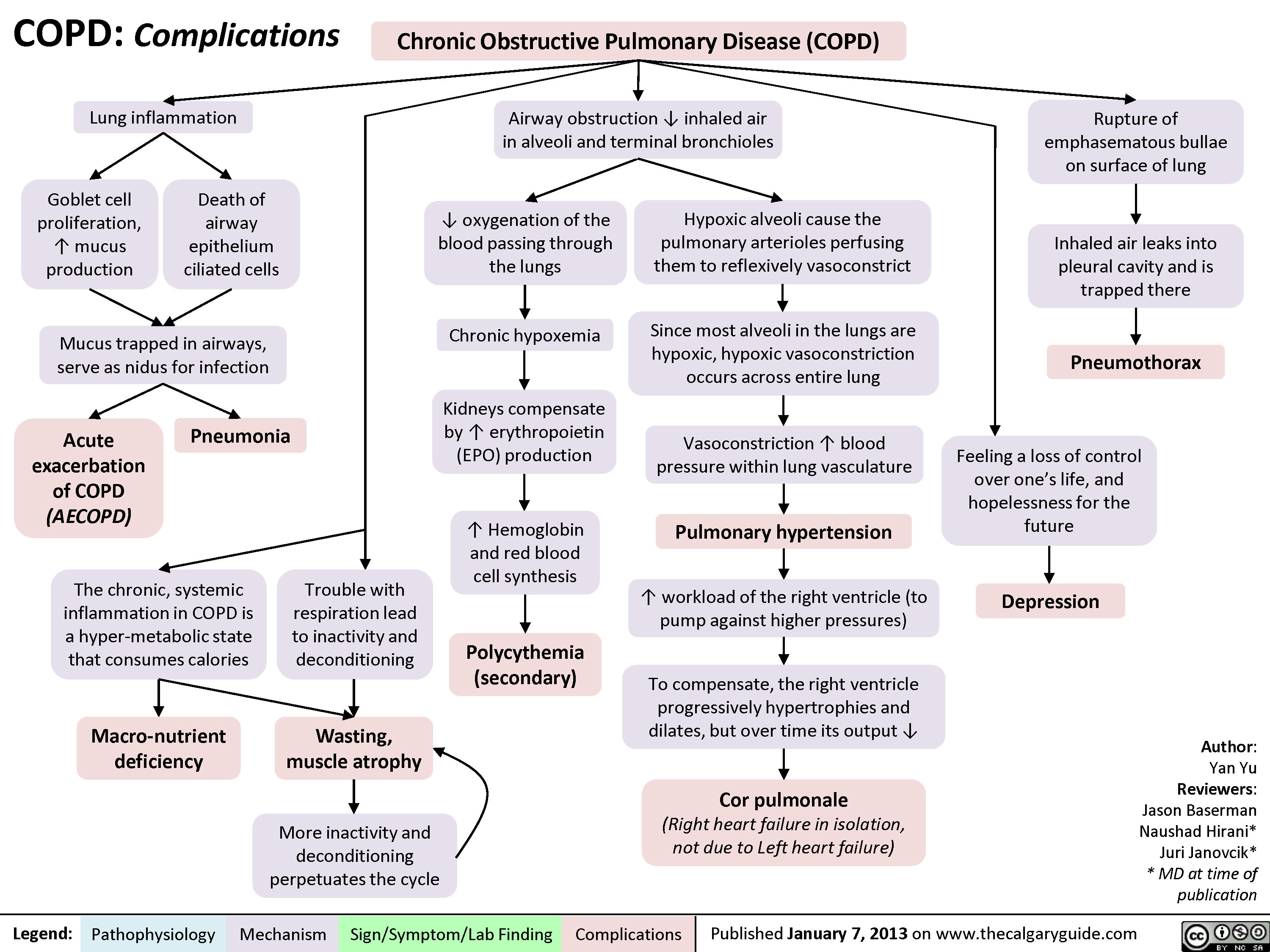
COPD: Complications
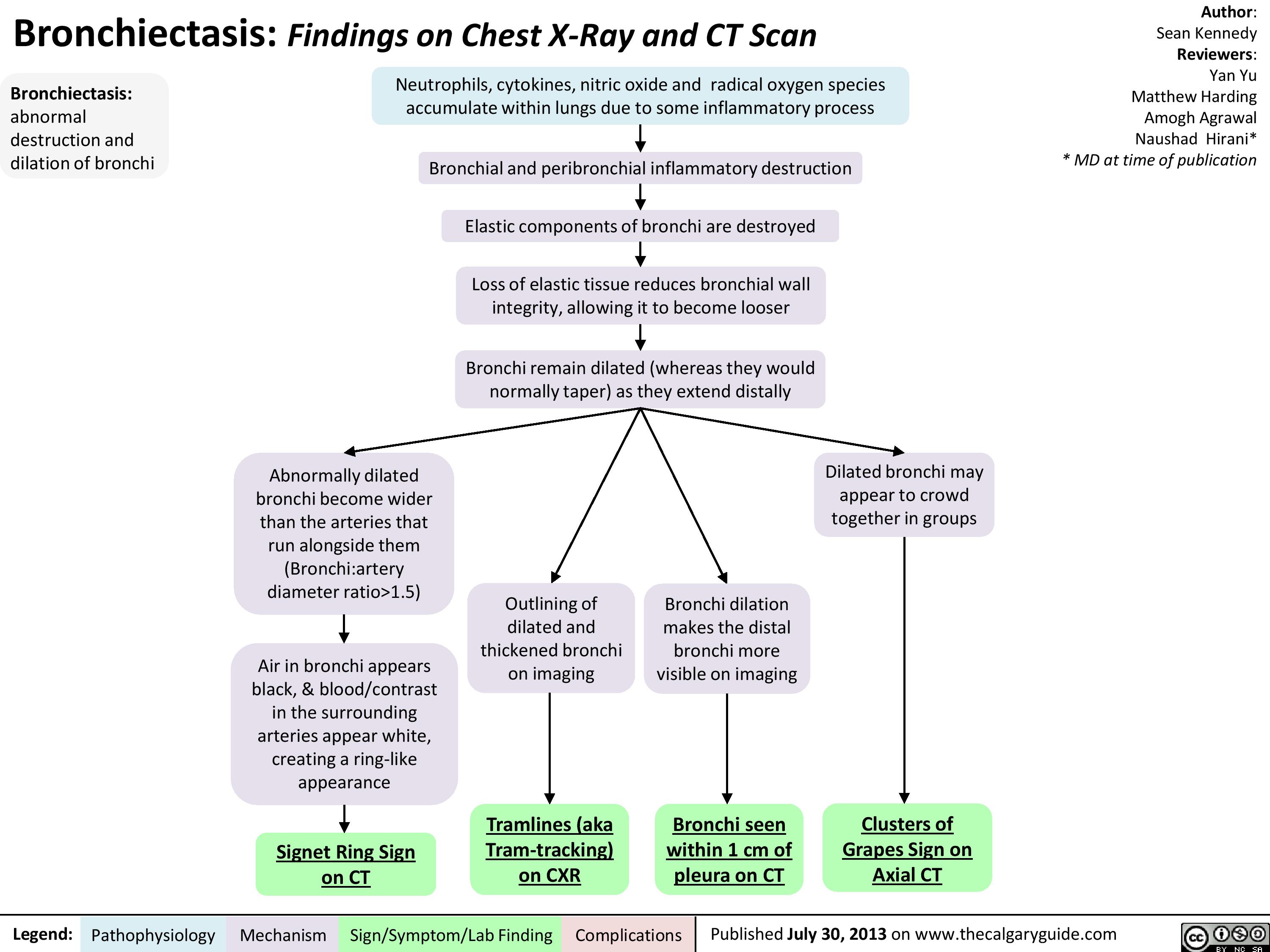
Bronchiectasis: Findings on Chest X-Ray and CT Scan
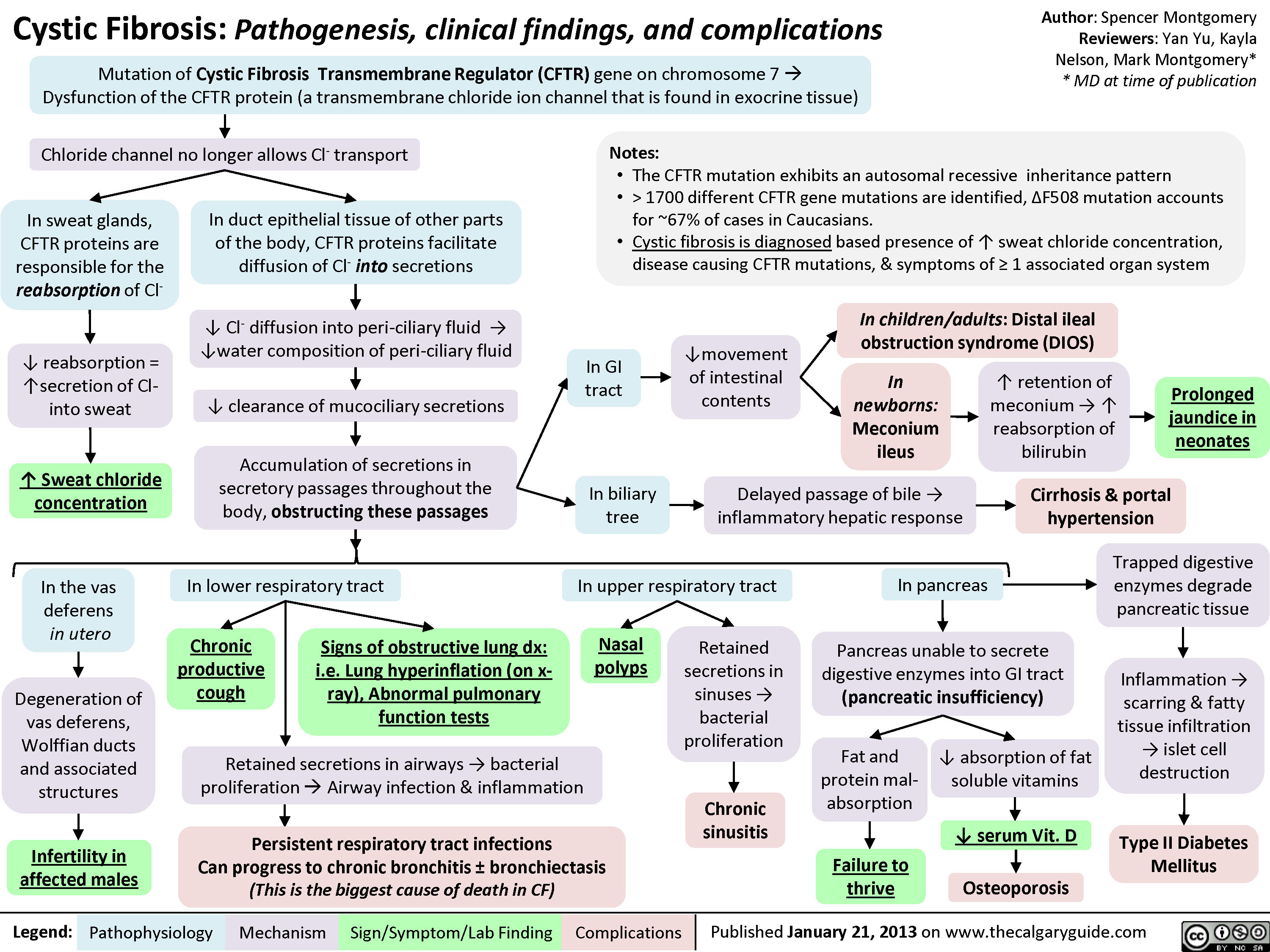
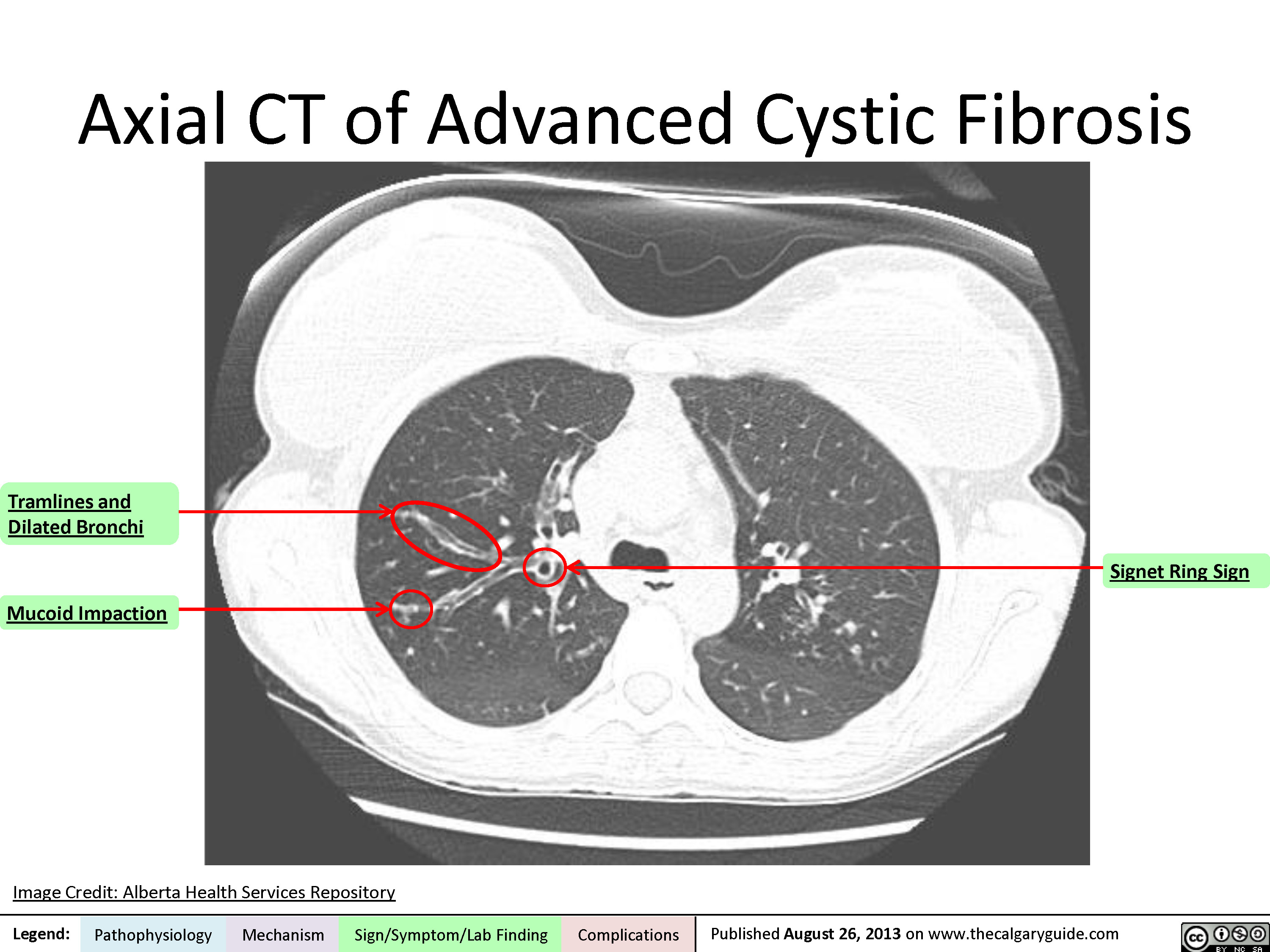
Cystic Fibrosis
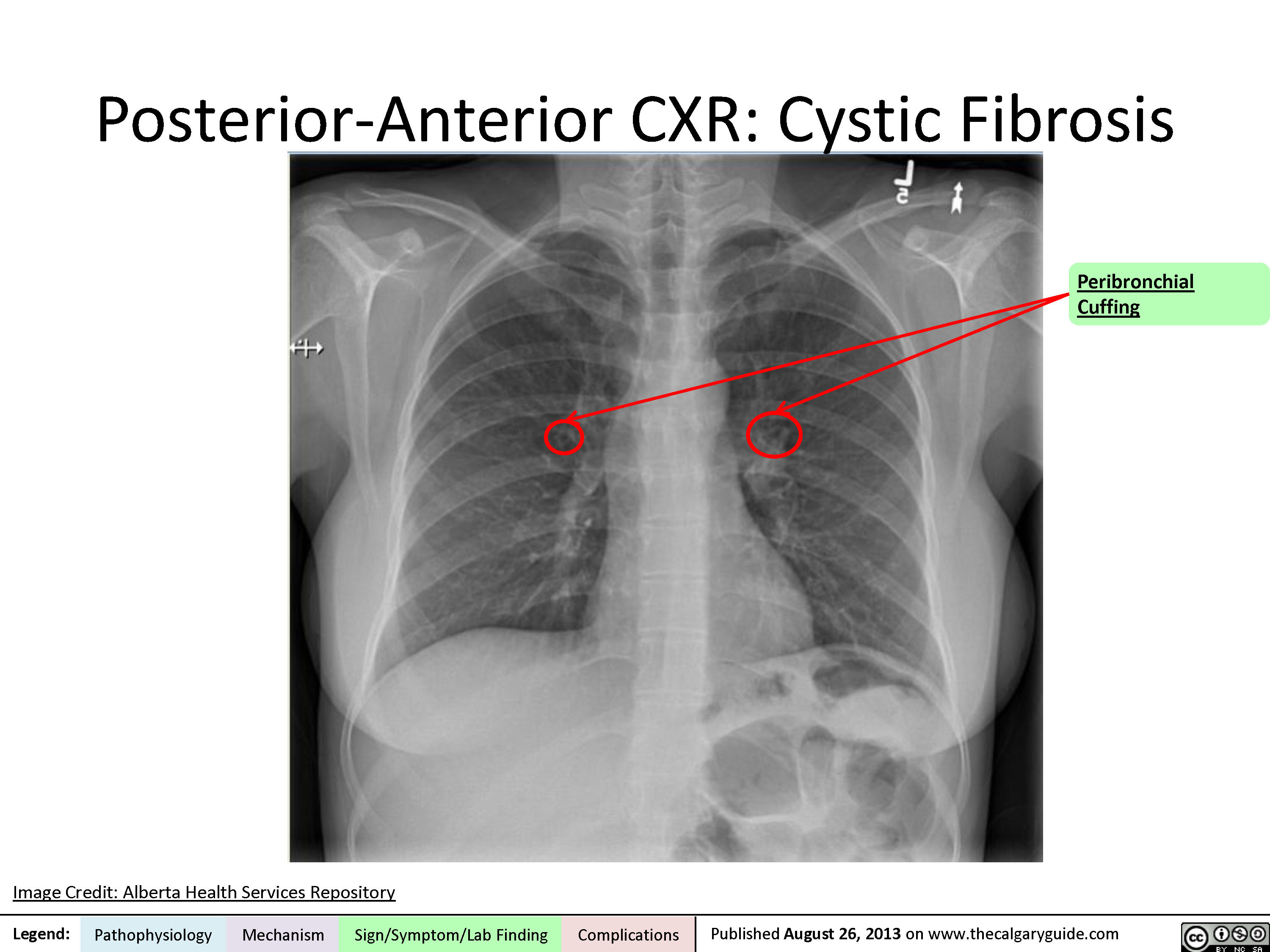
Posterior-Anterior Chest X-Ray
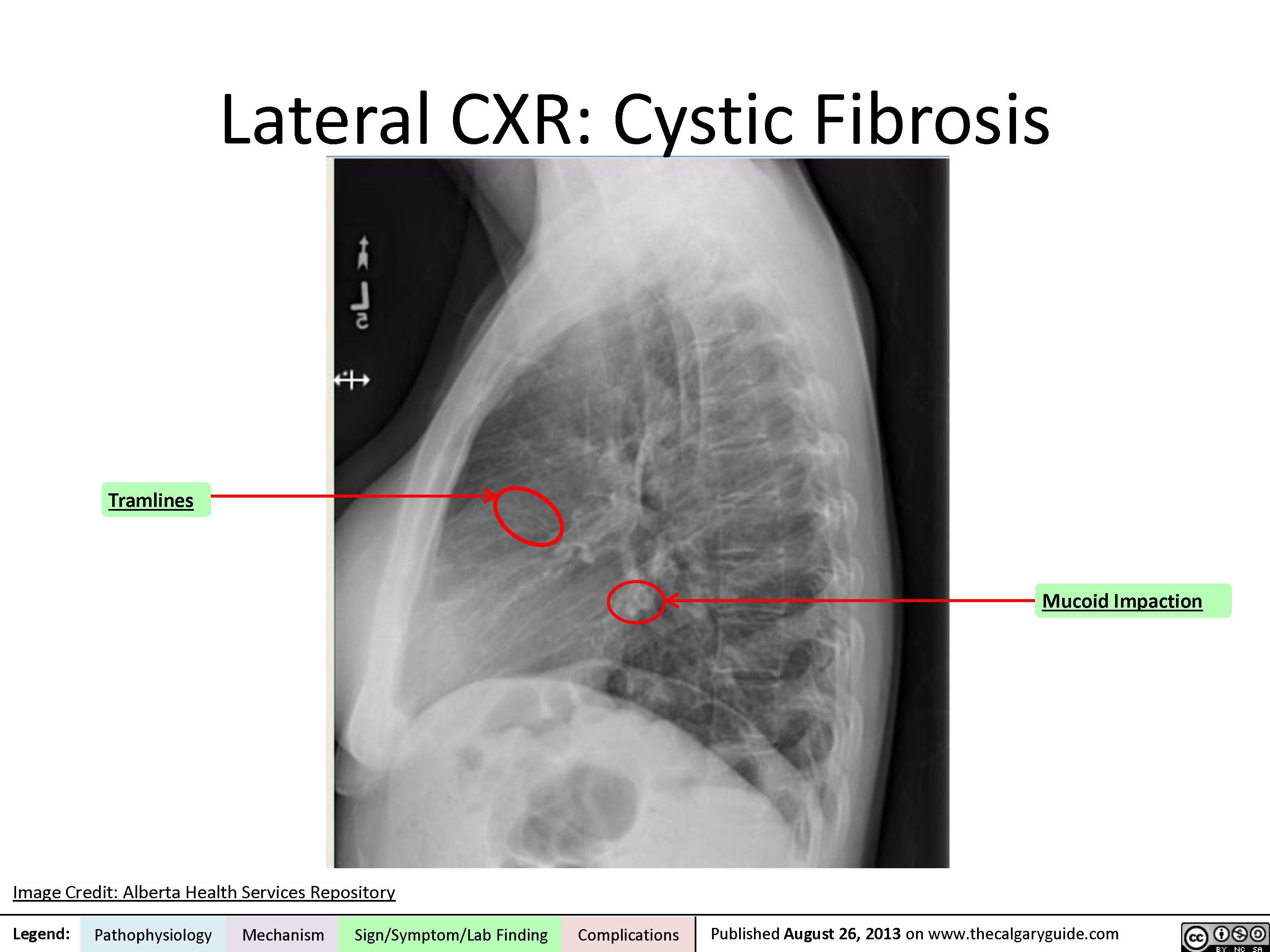
Lateral Chest X-Ray
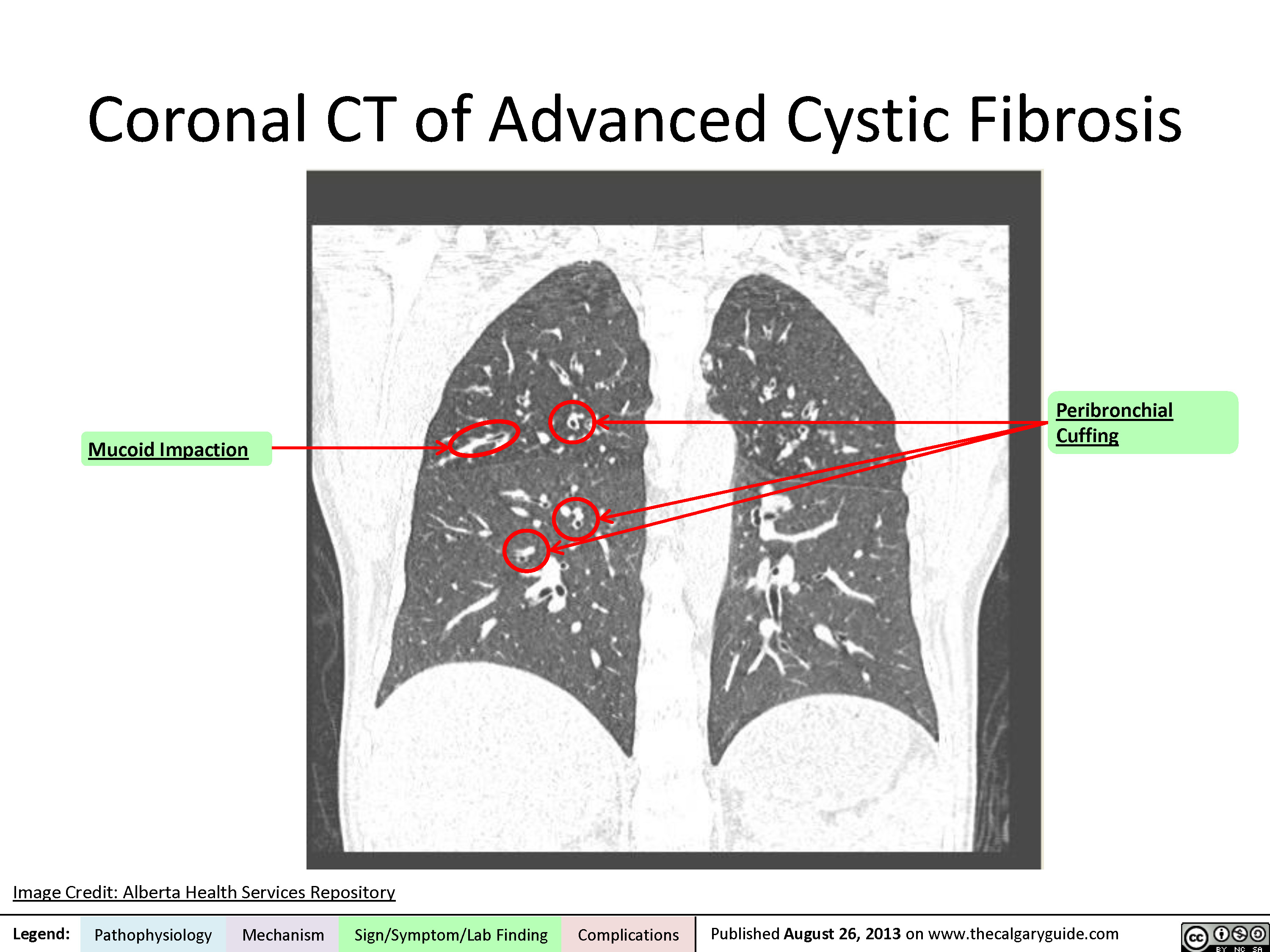
Coronal CT
Axial CT
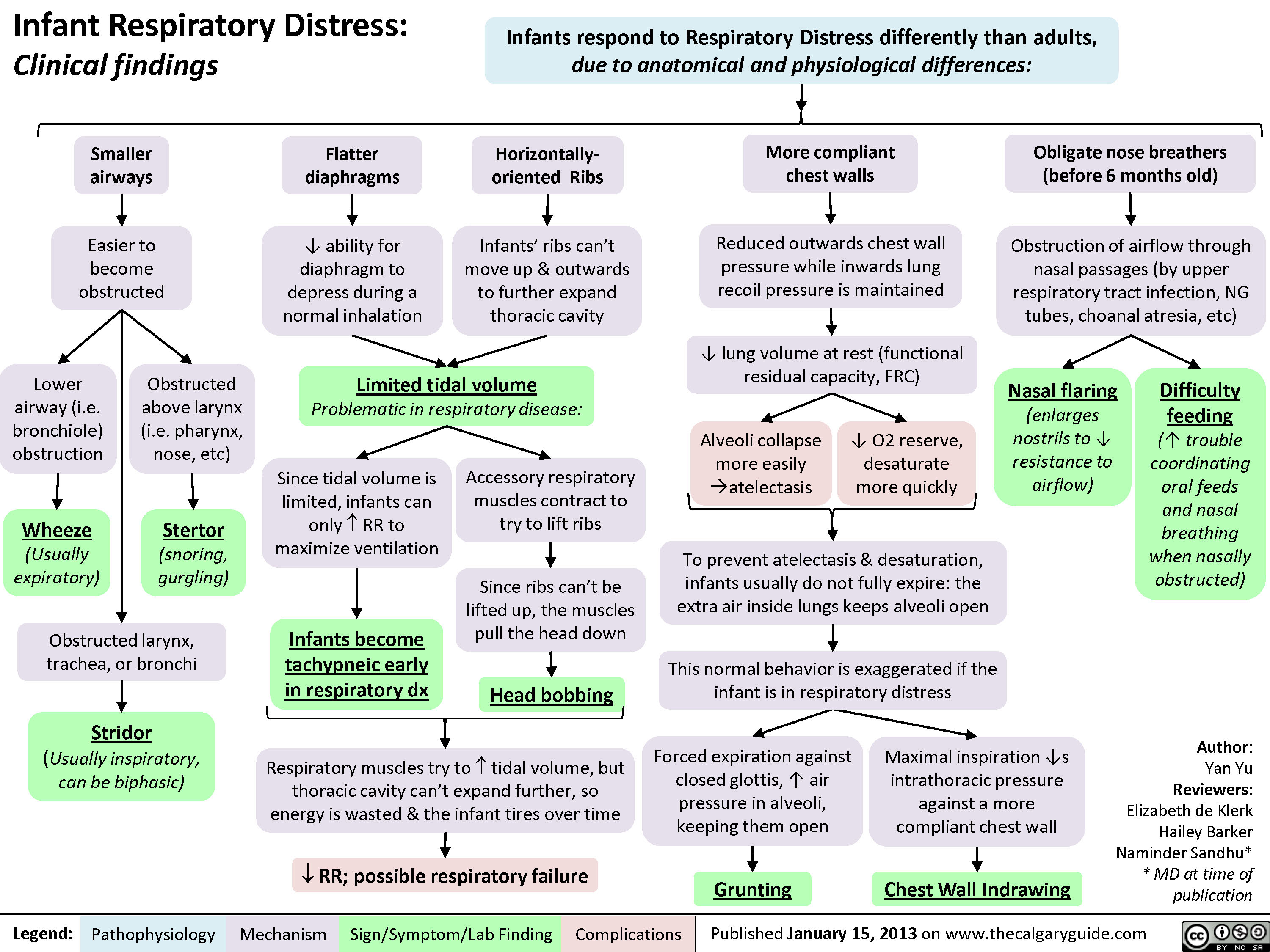
Infant Respiratory Distress: Clinical findings
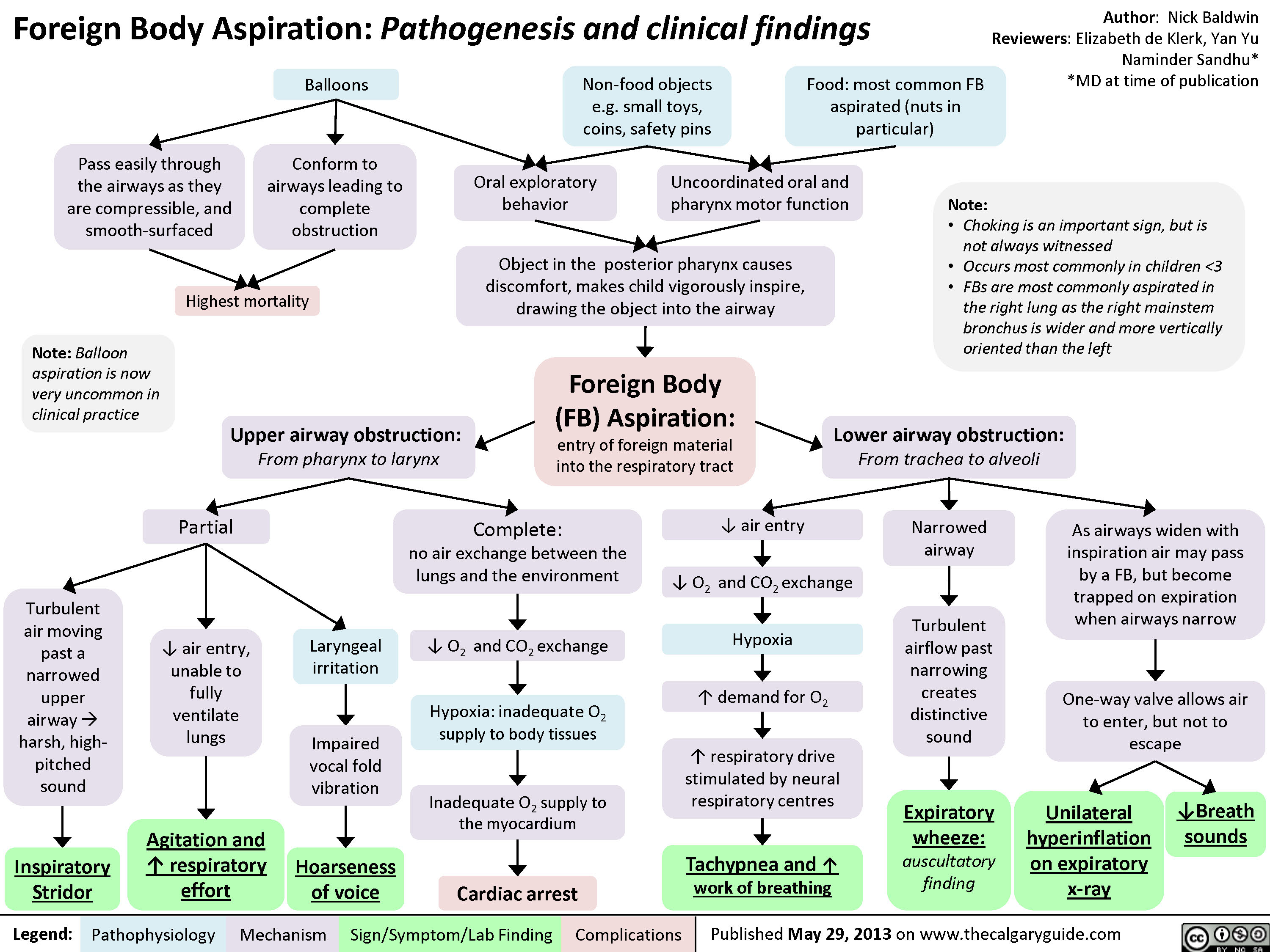
Foreign Body Aspiration
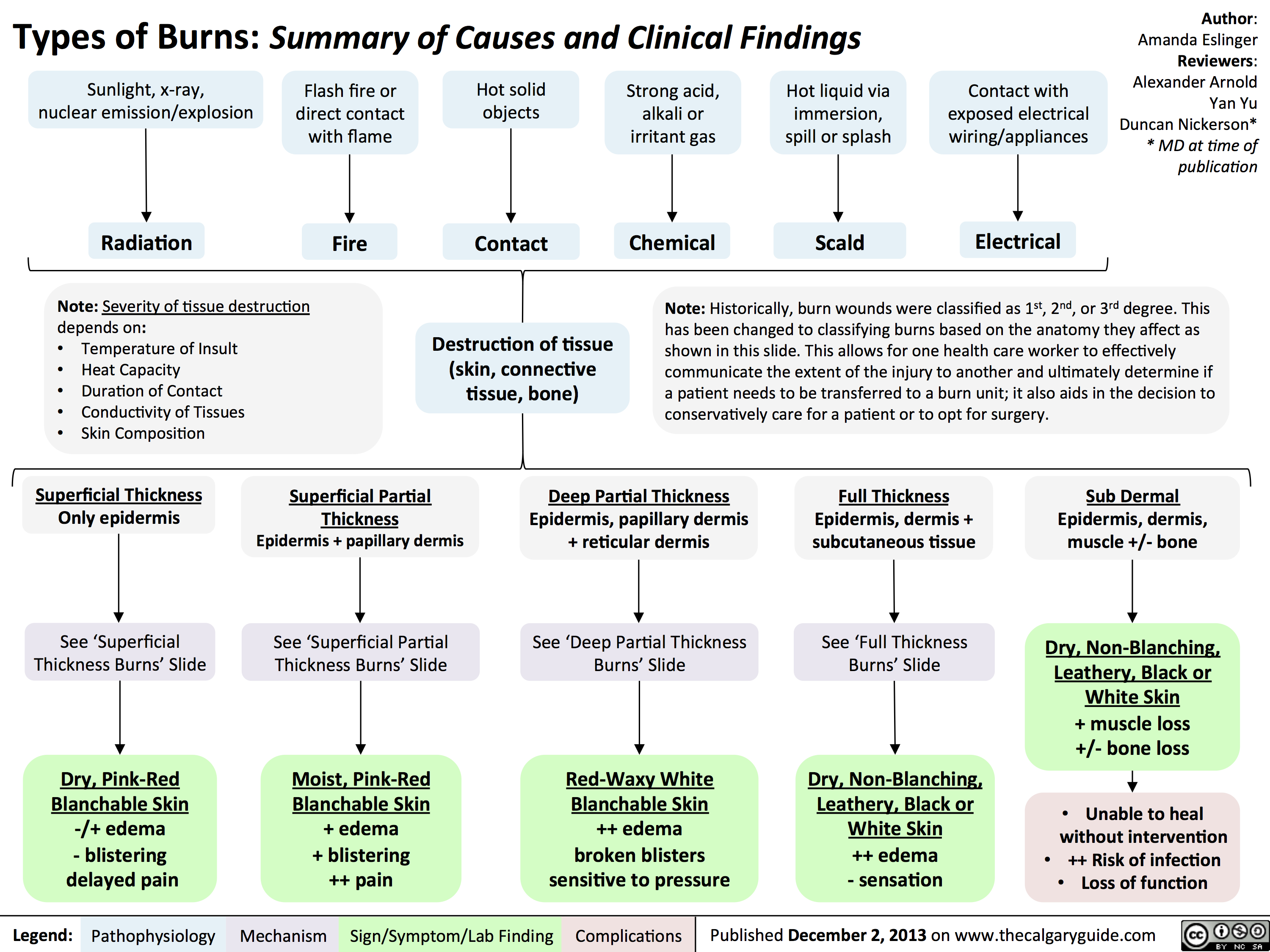
Types of Burns - Summary of Causes and Clinical Findings
Deep Partial Thickness Burns: Pathogenesis and Clinical Findings

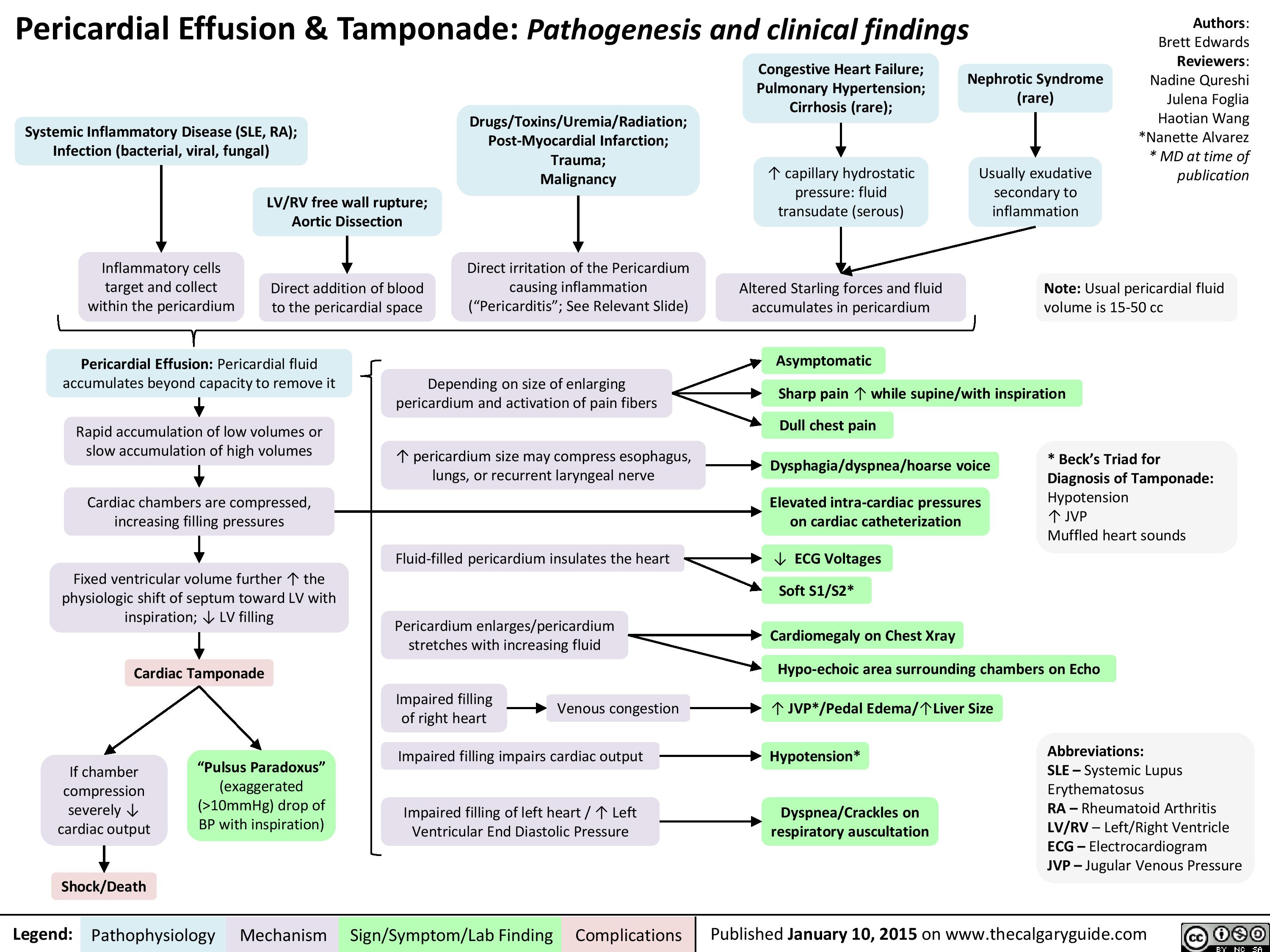
Pericardial Effusion and Tamponade: Pathogenesis and Clinical Findings
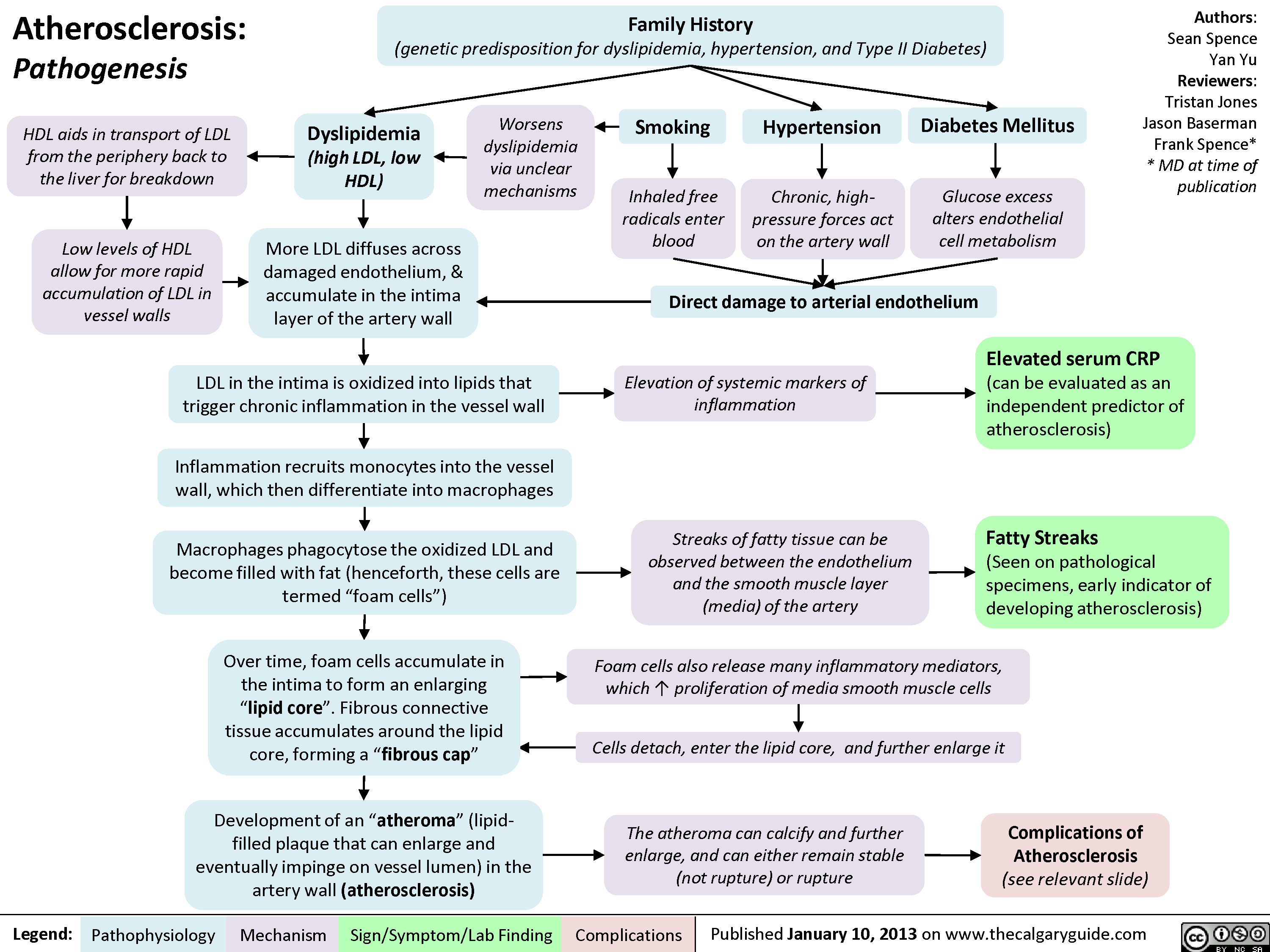
Atherosclerosis - Pathogenesis
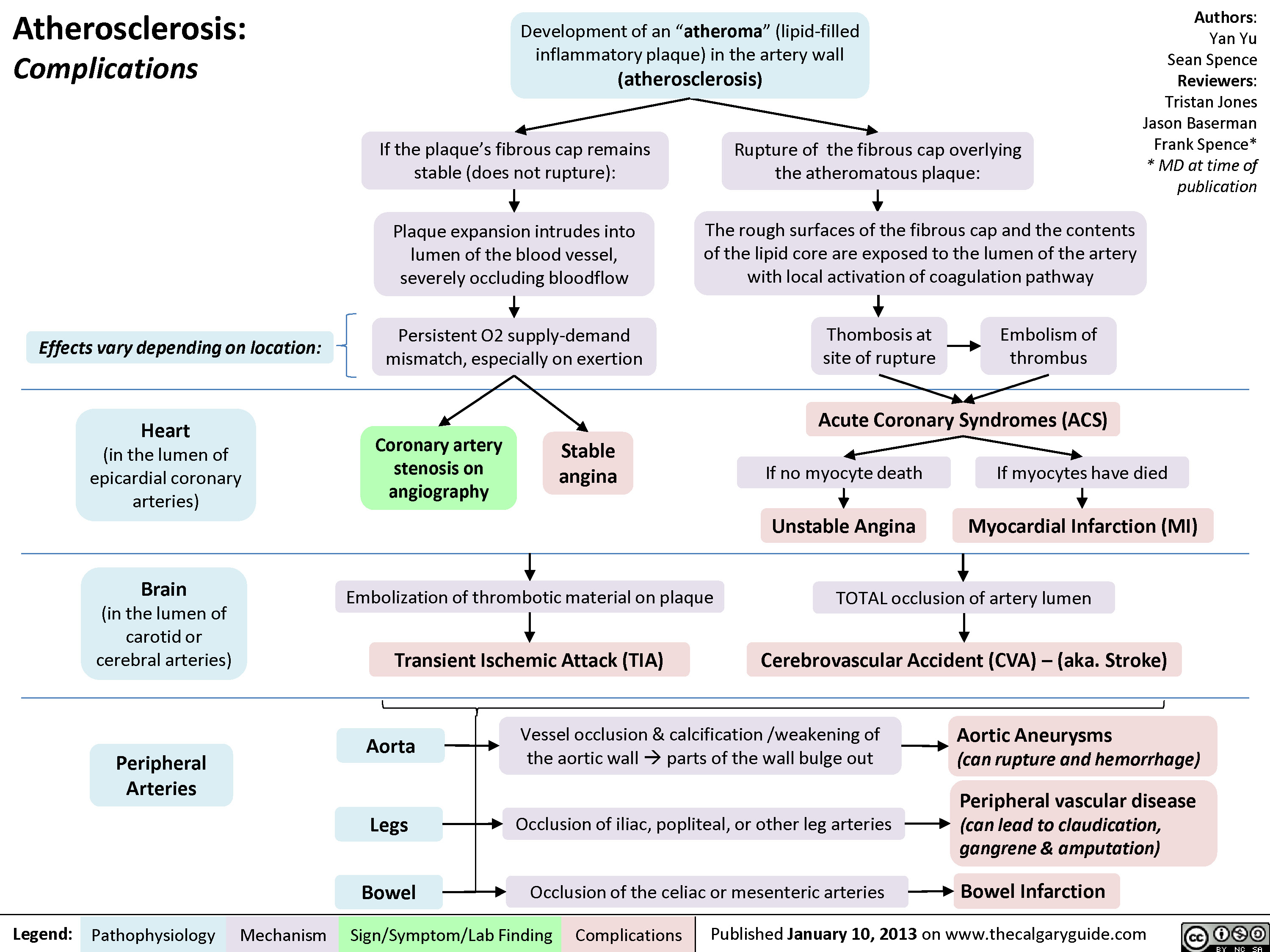
Atherosclerosis - Complications
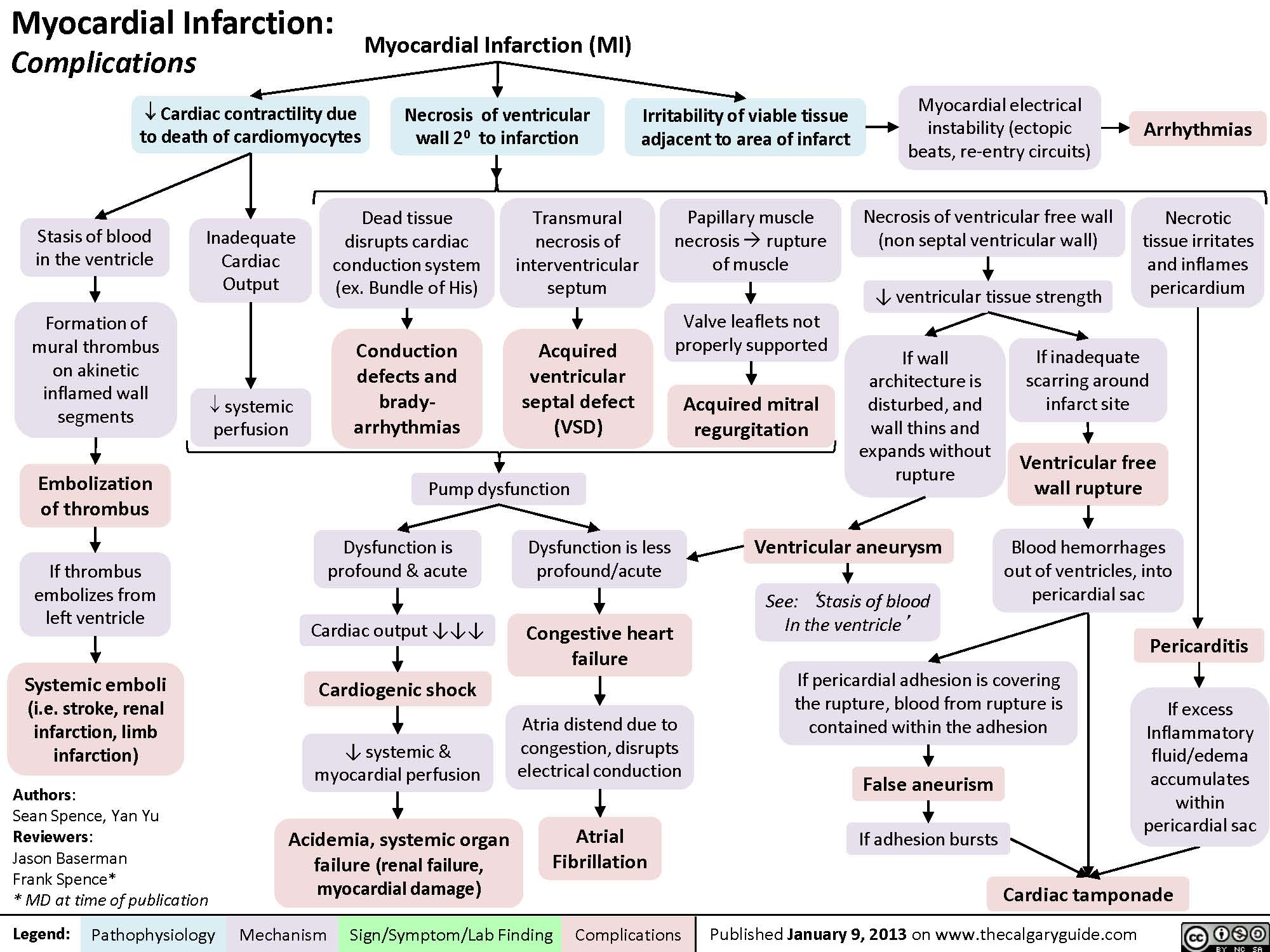
Complications of Myocardial Infarction
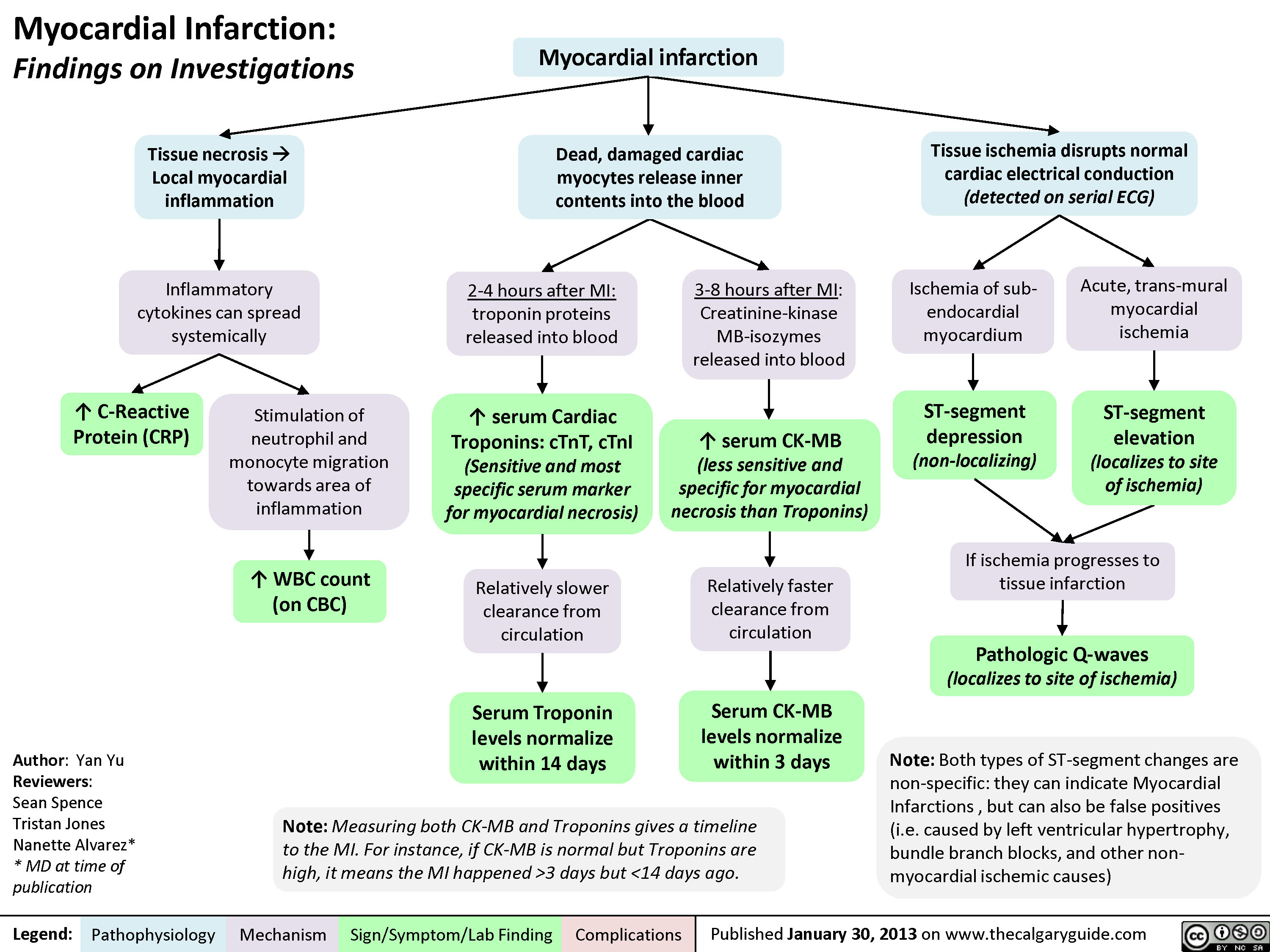
myocardial-infarction-findings-on-investigations
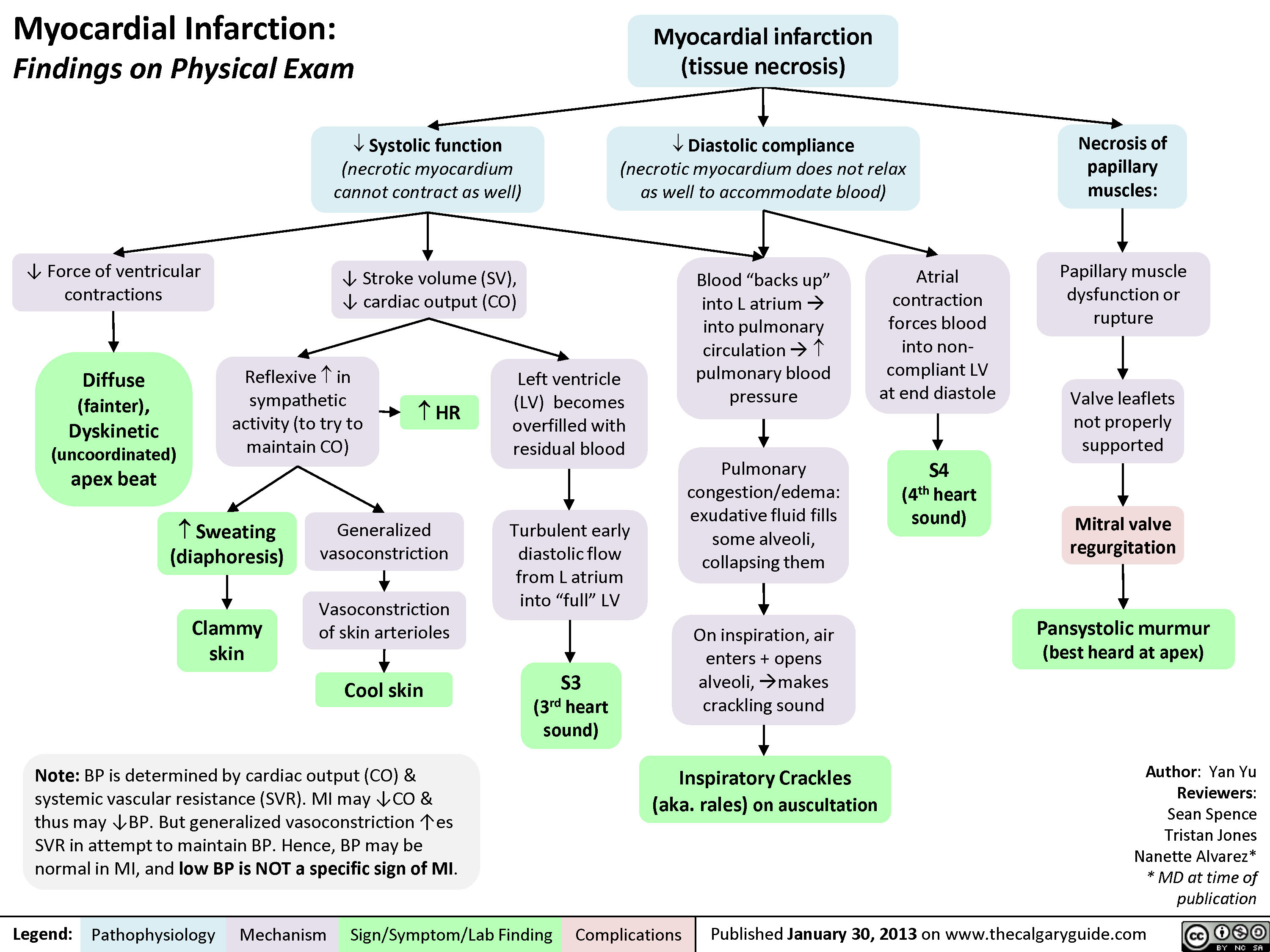
myocardial-infarction-findings-on-physical-exam
MI Findings on History
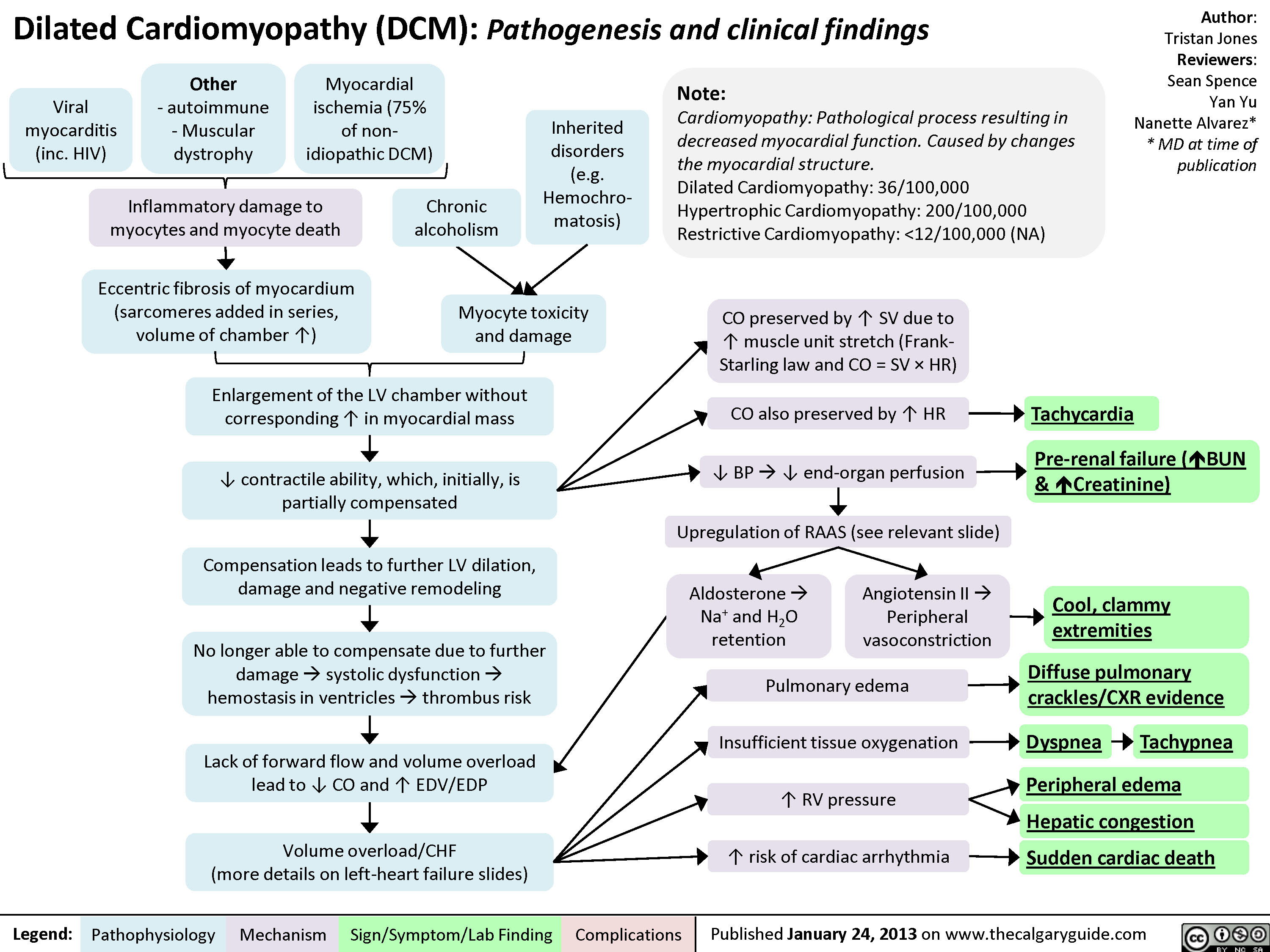
Dilated Cardiomyopathy
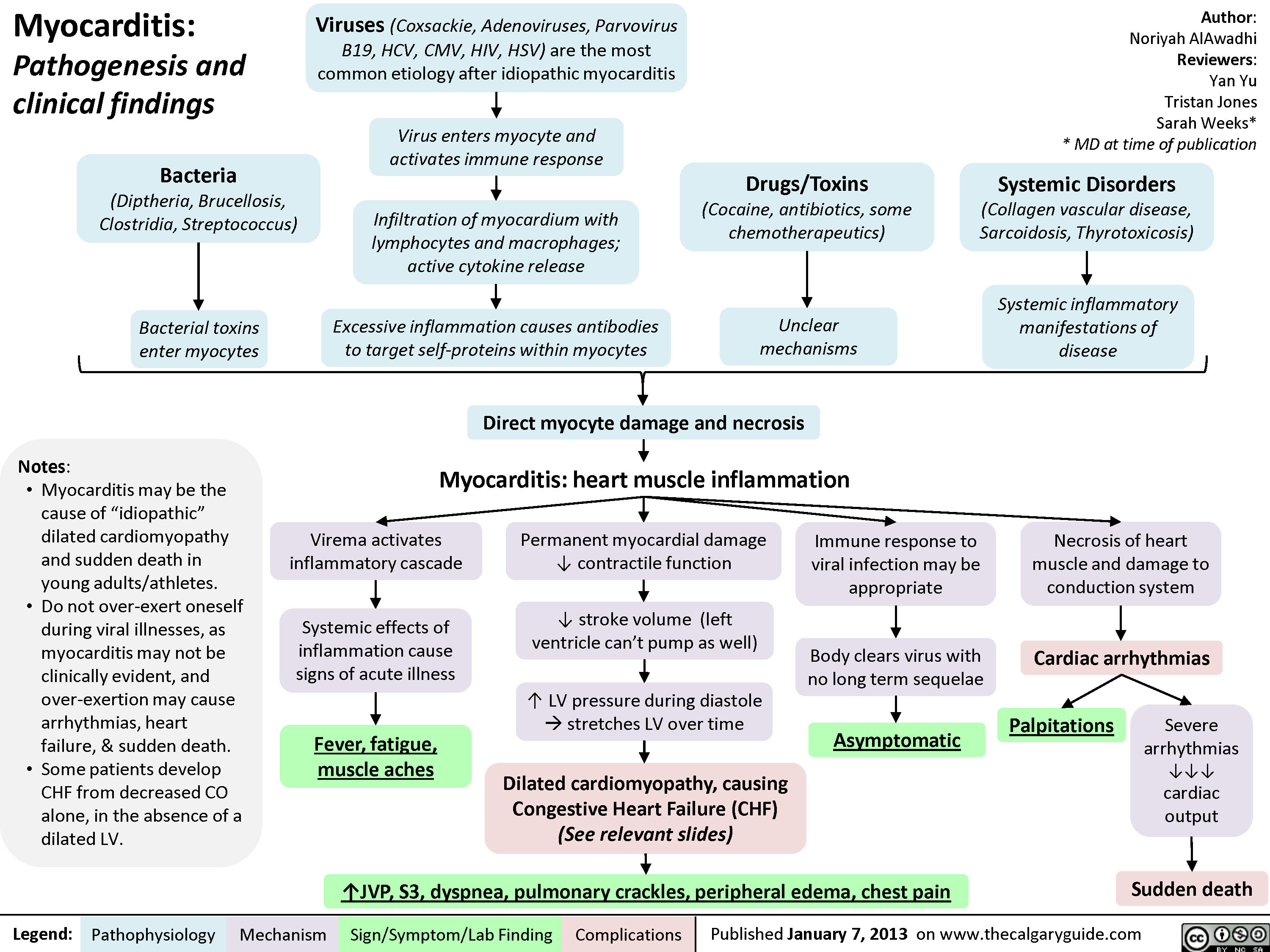
Myocarditis
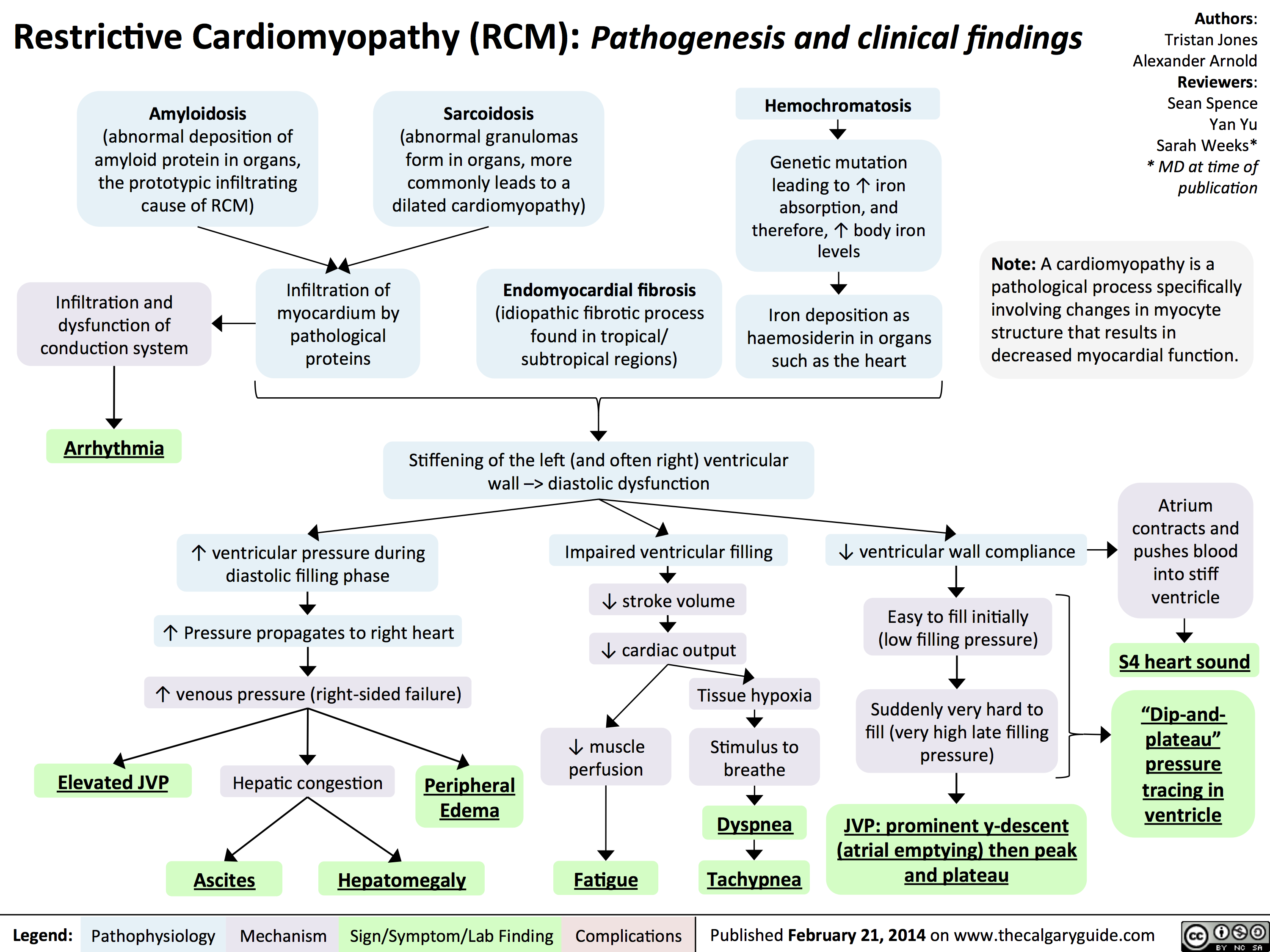
Restrictive Cardiomyopathy
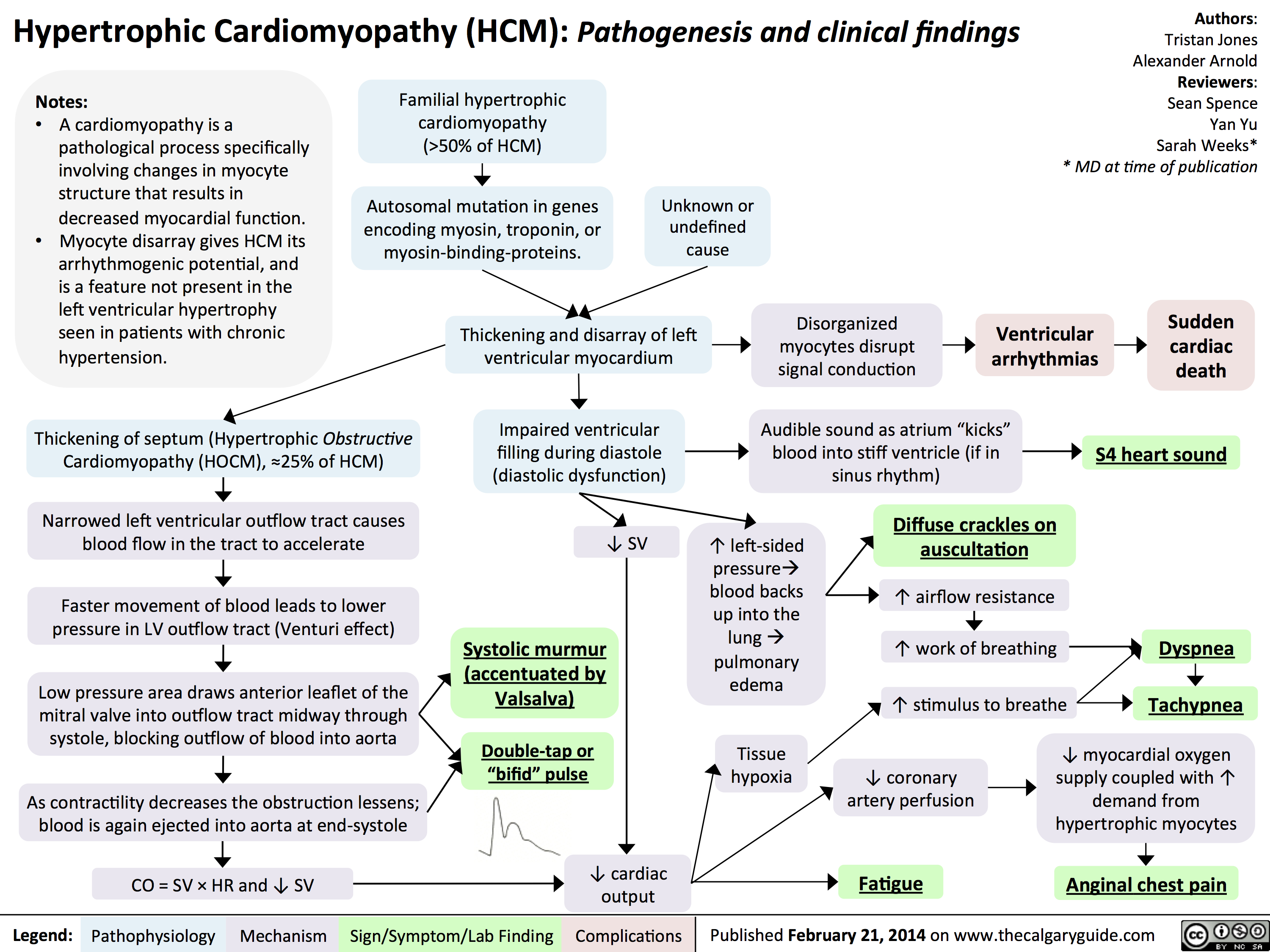
Hypertrophic Cardiomyopathy
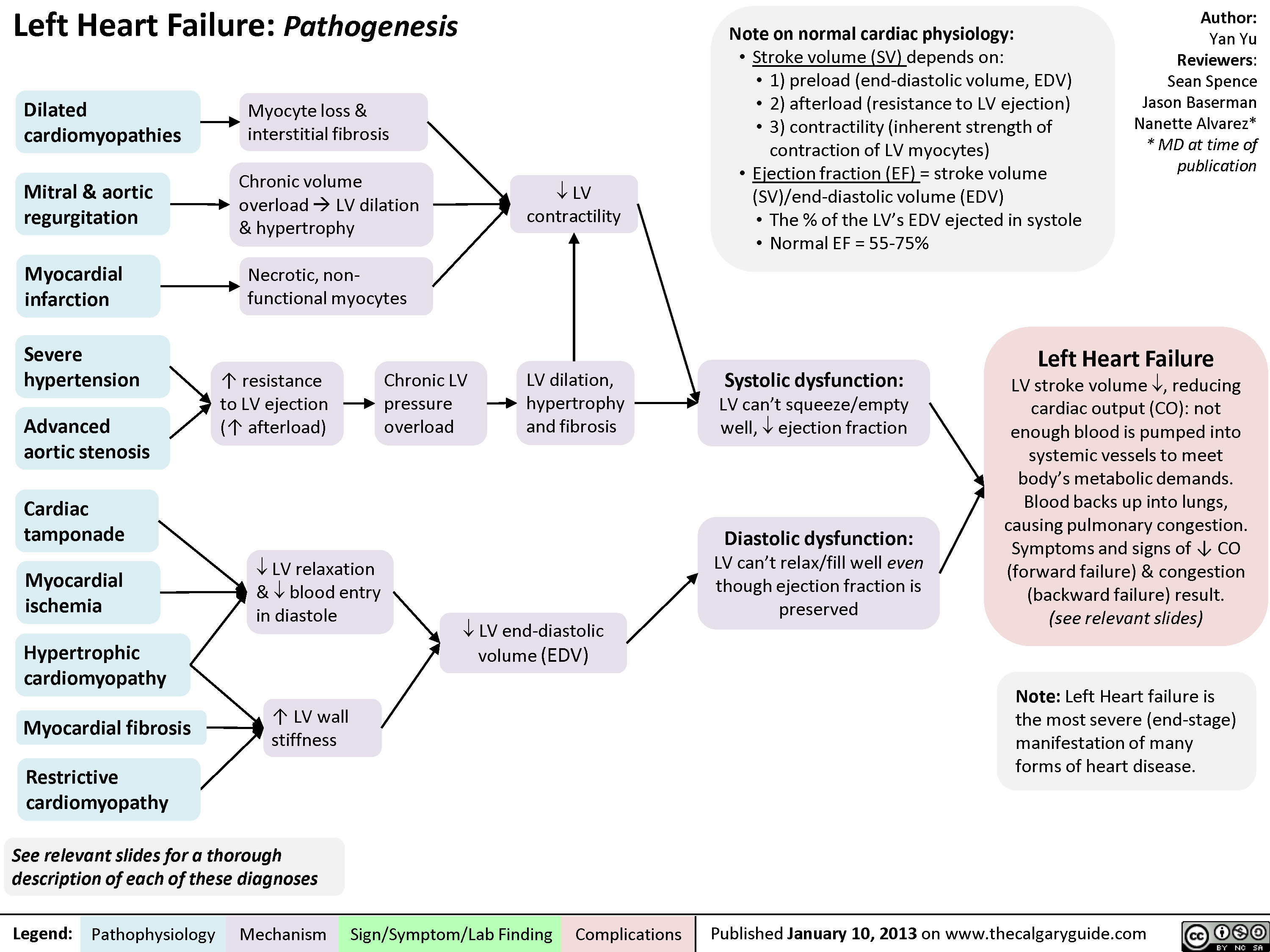
Left Heart Failure - Pathogenesis
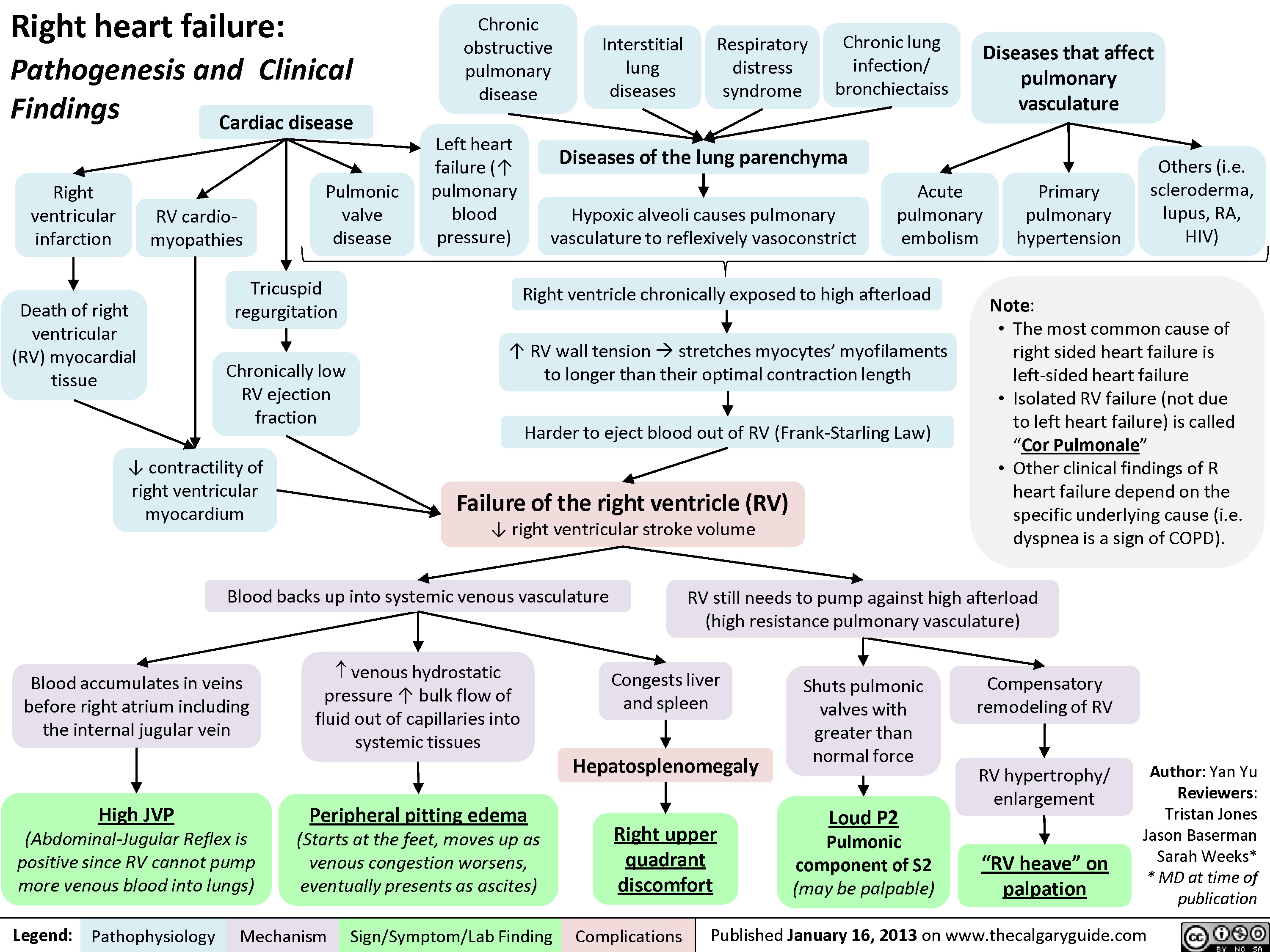
Right Heart Failure
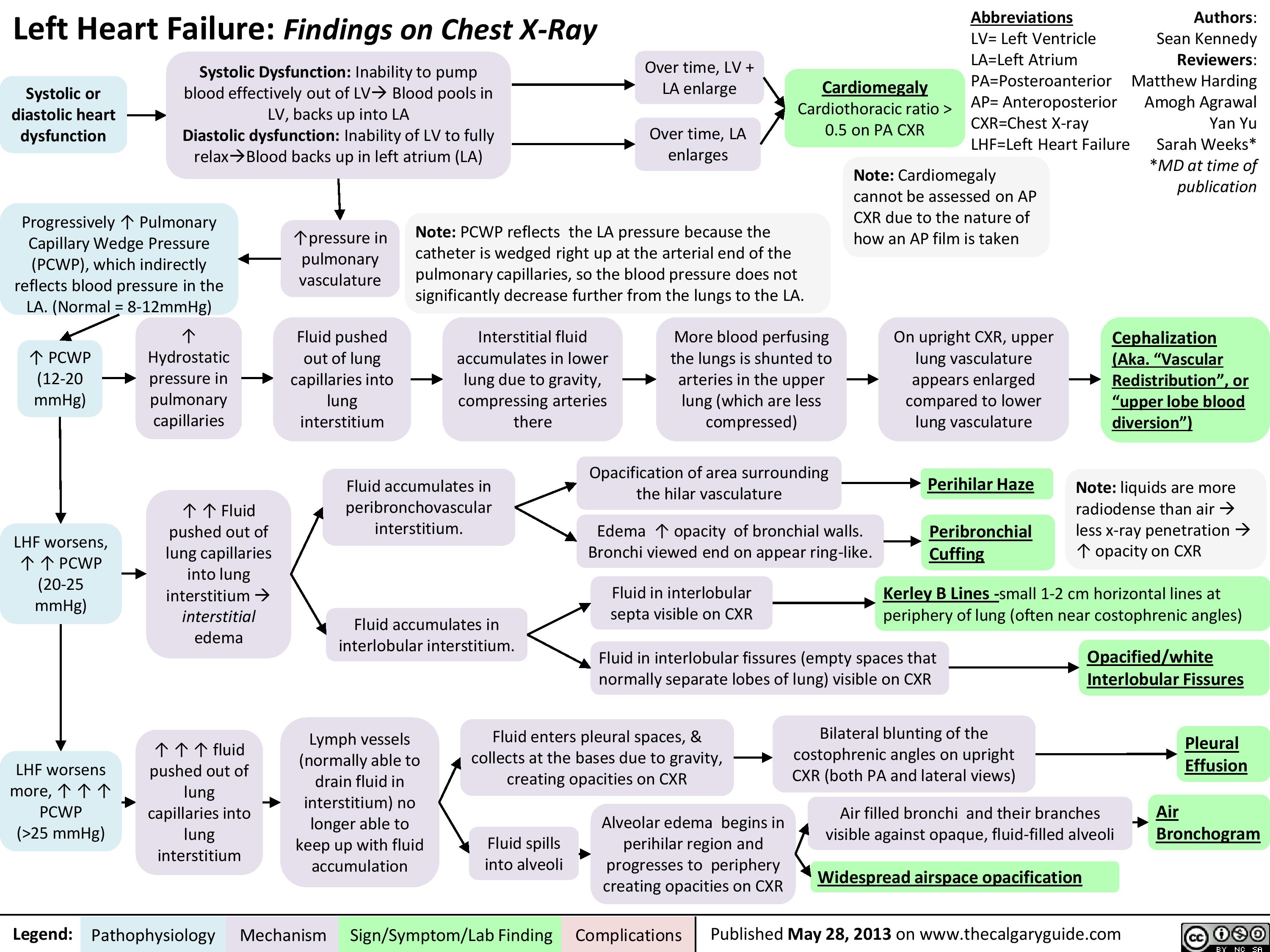
Left Heart Failure
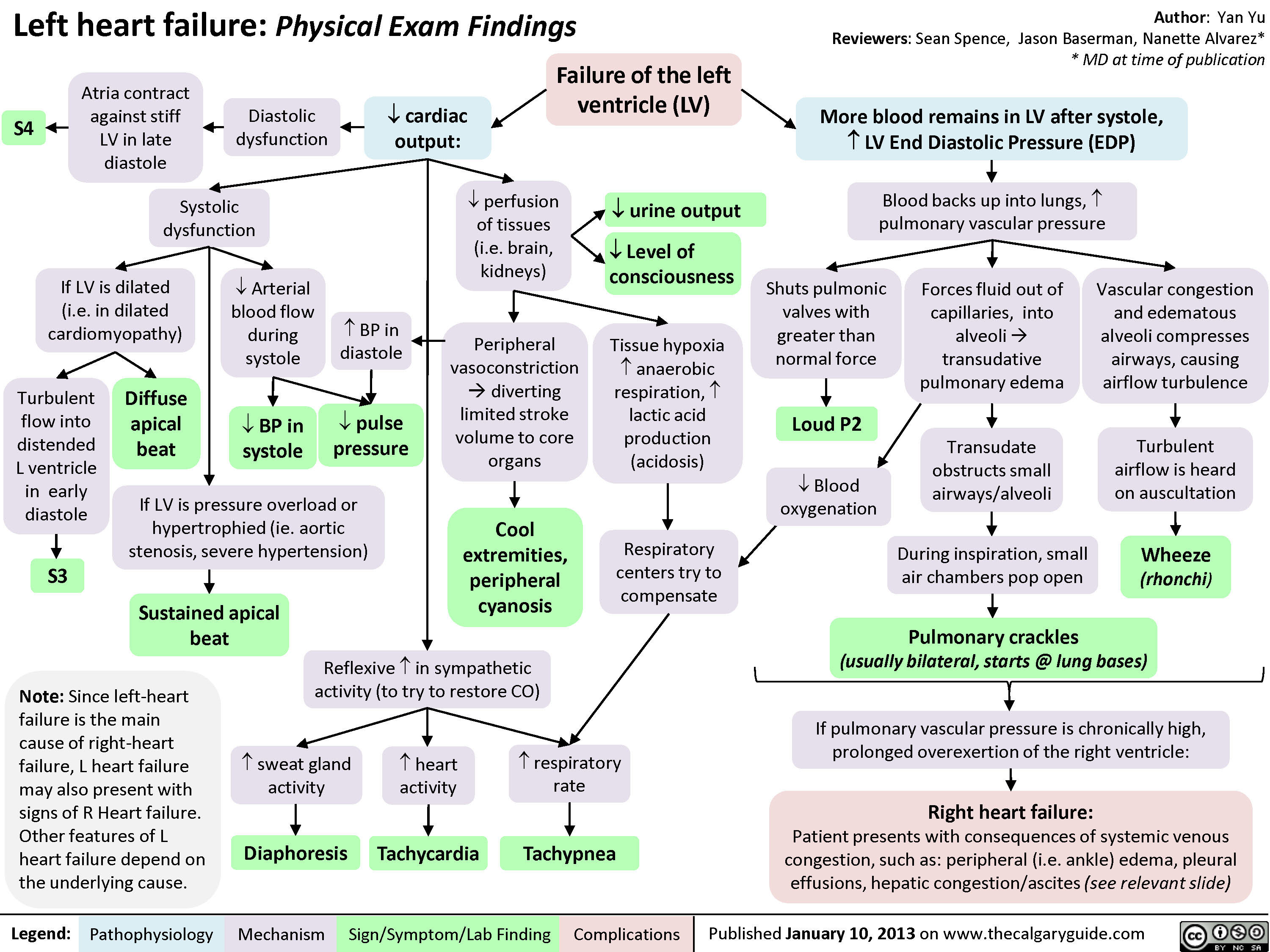
Left Heart Failure - Physical Exam Findings
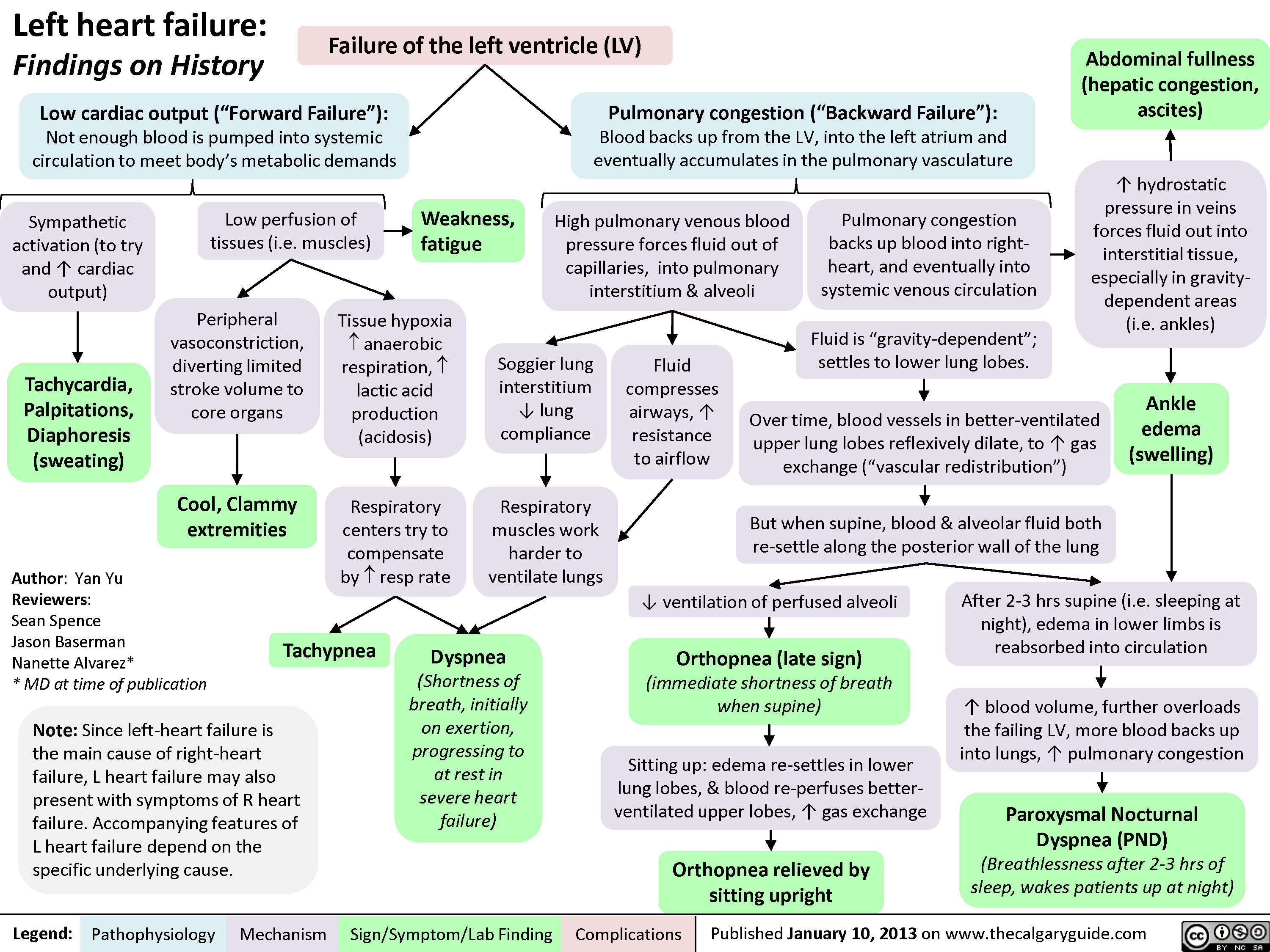
Left Heart Failure - Findings on History
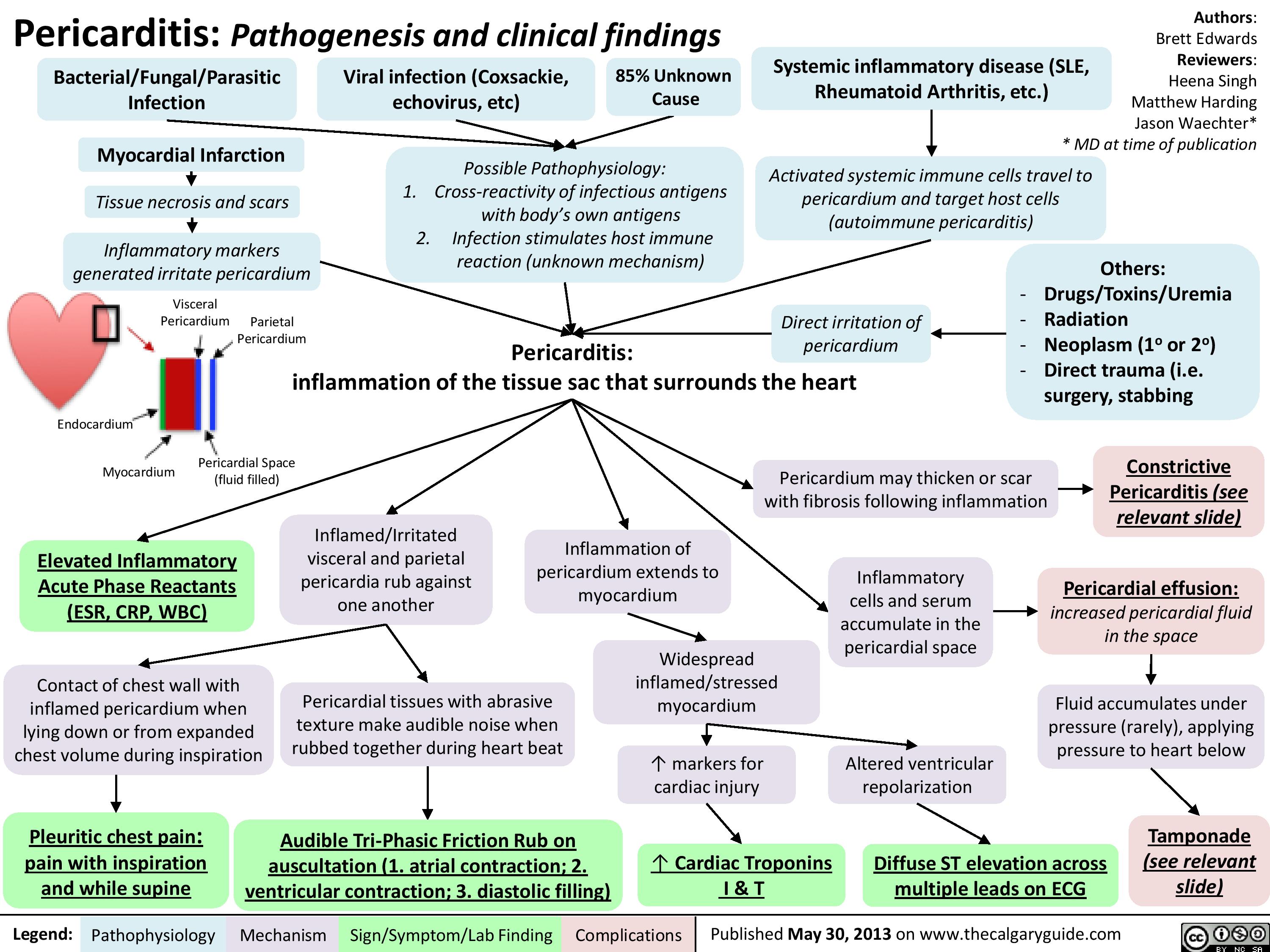
pericarditis
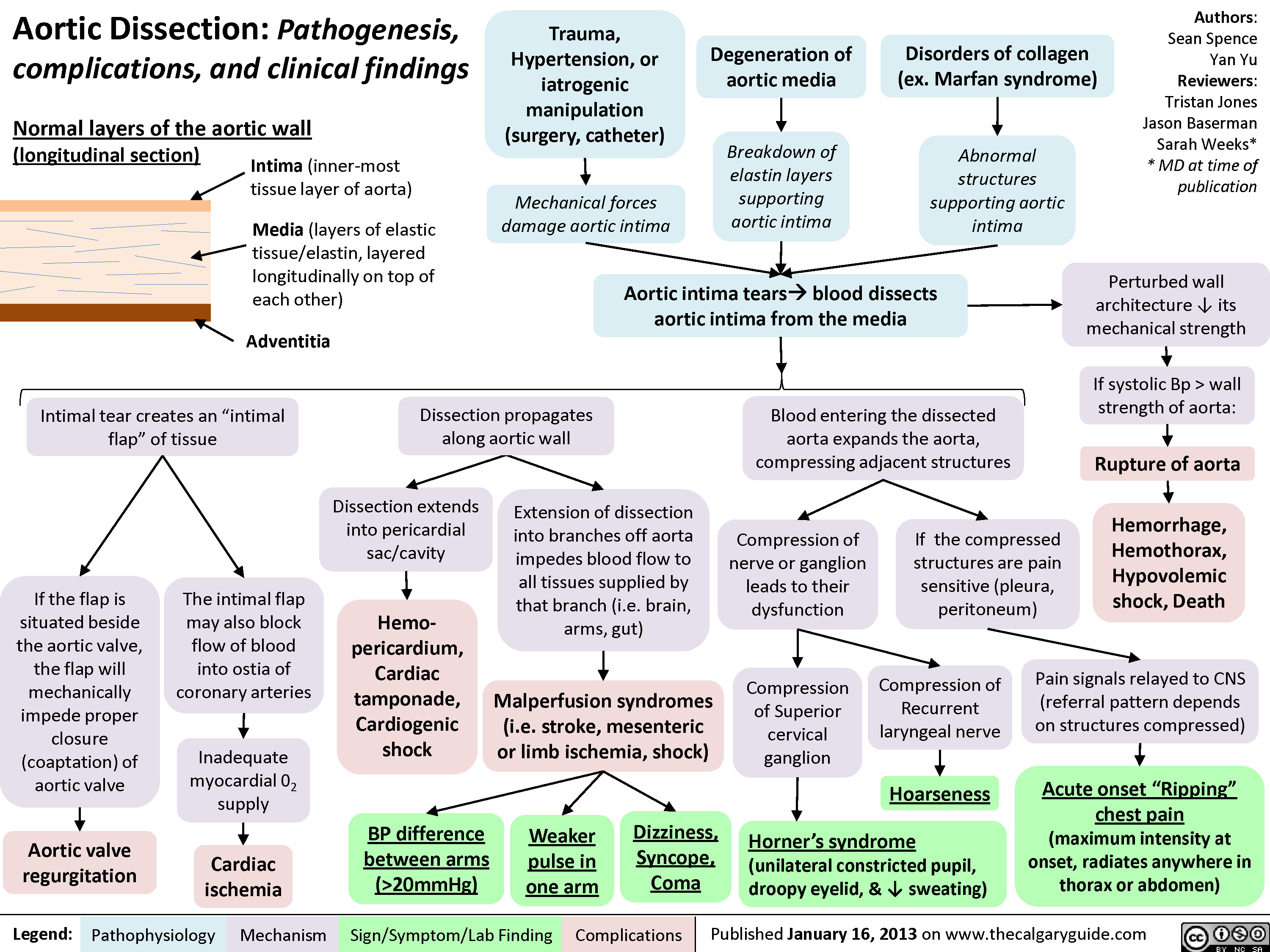
Aortic Dissection
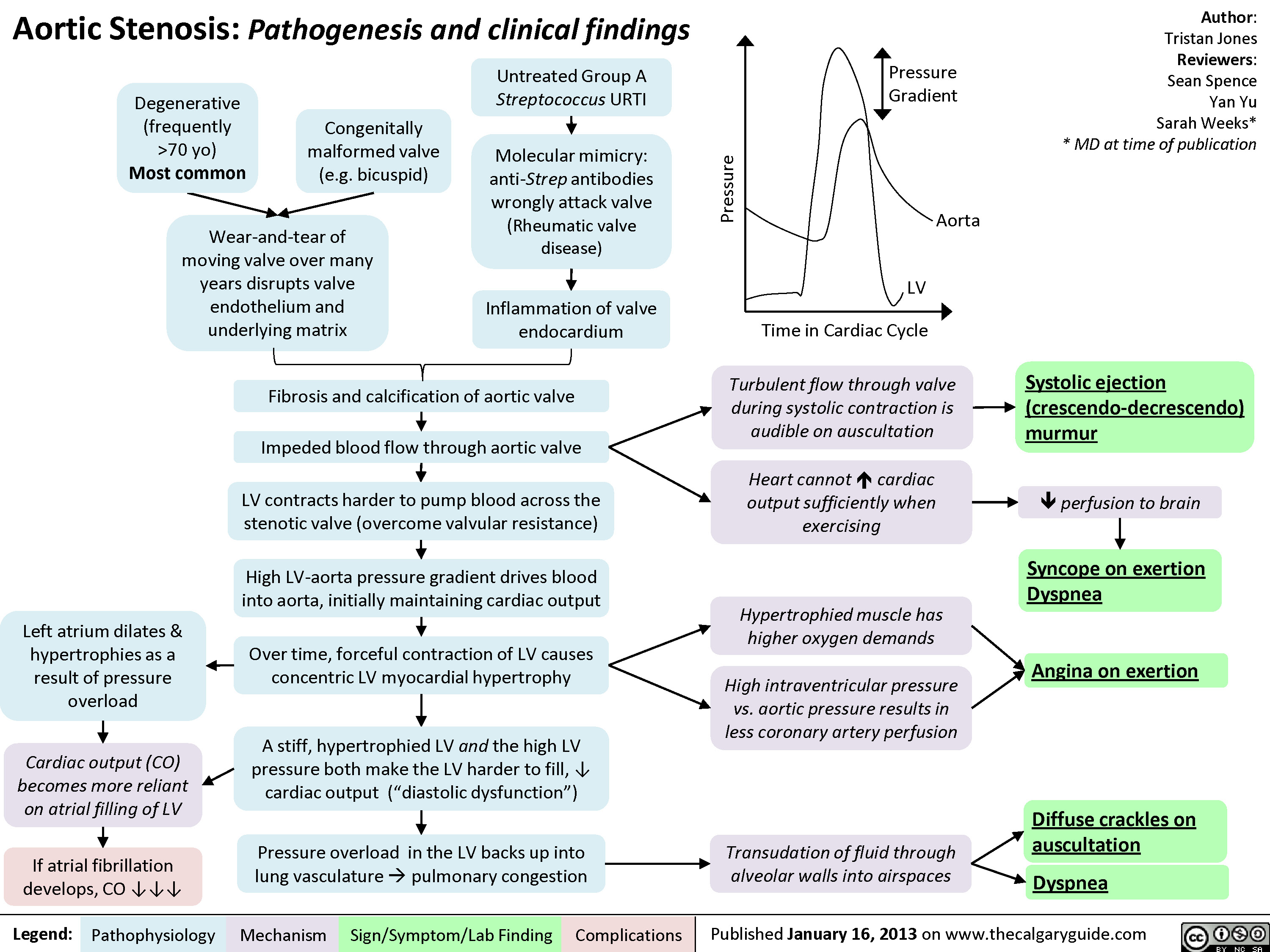
Aortic Stenosis - Pathogenesis and Clinical Findings
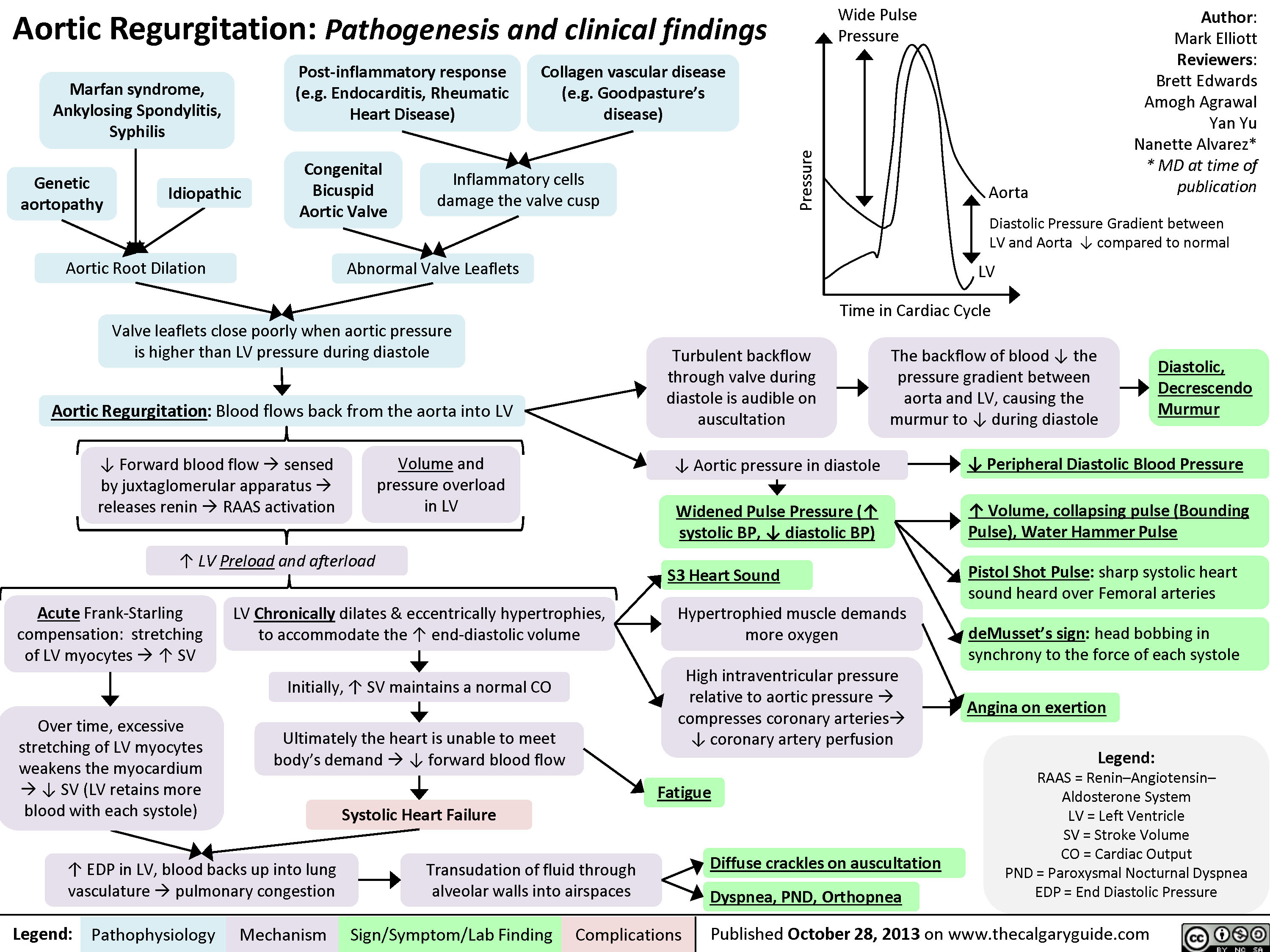
Aortic Regurgitation
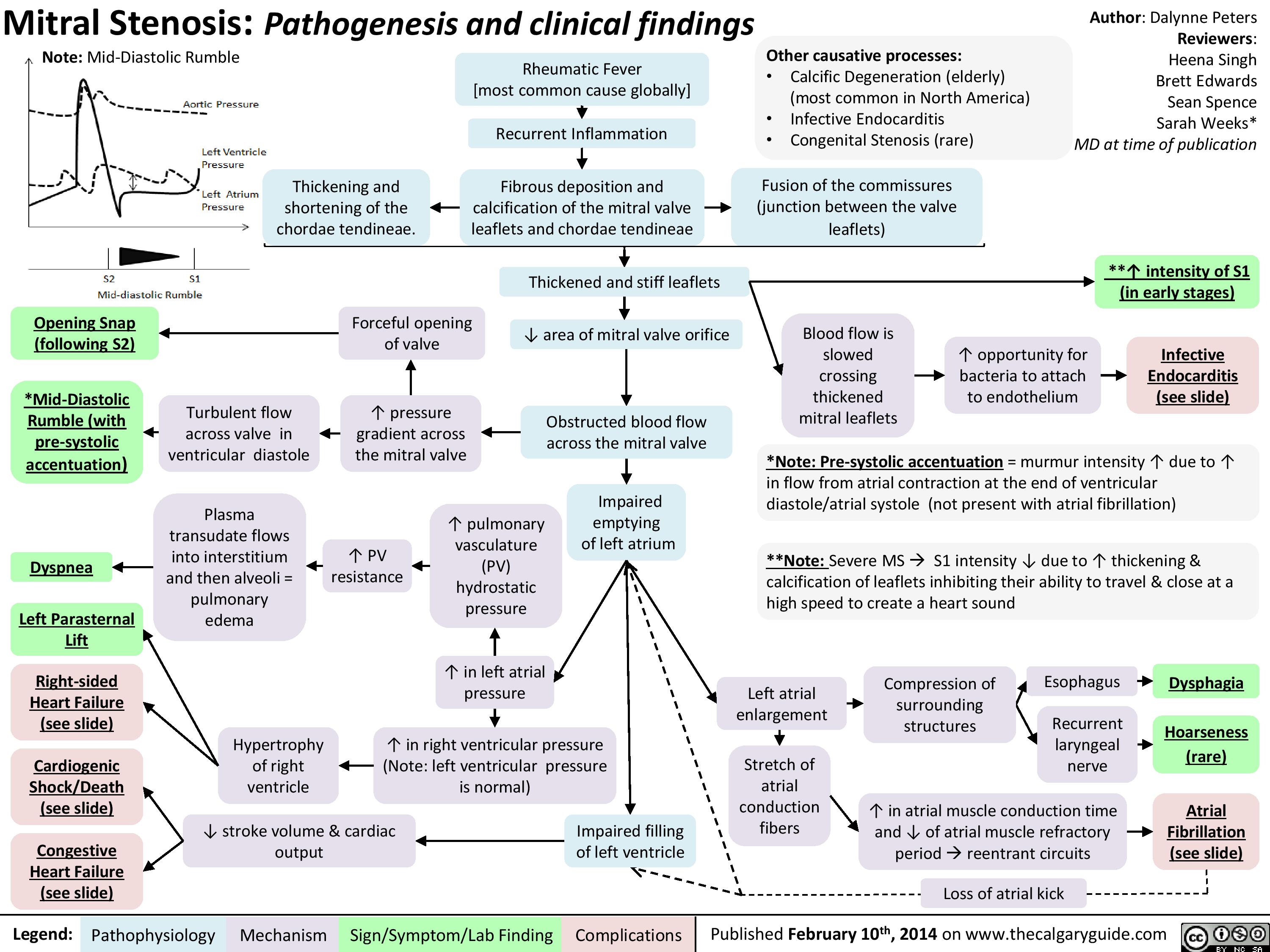
Mitral Stenosis
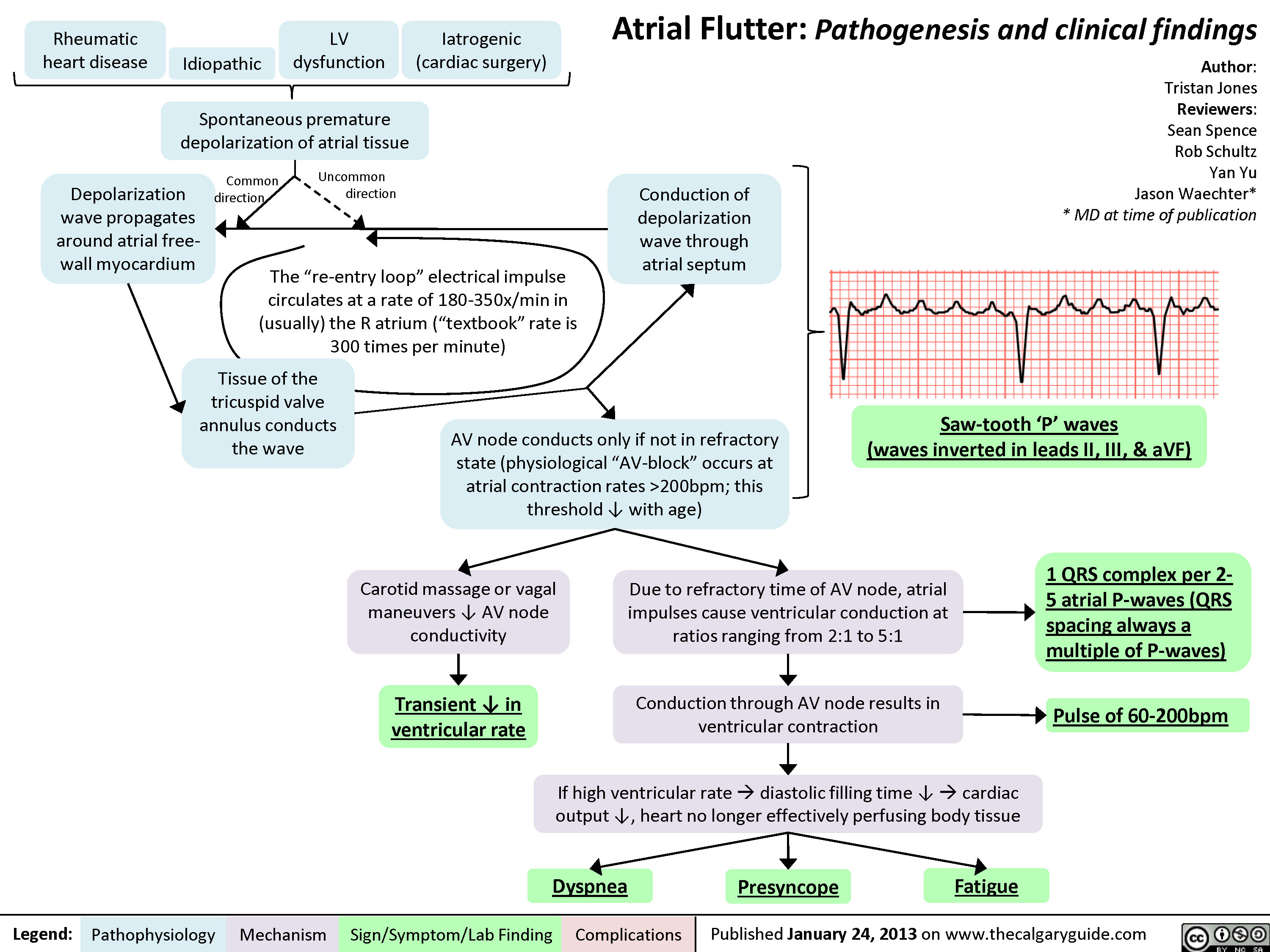
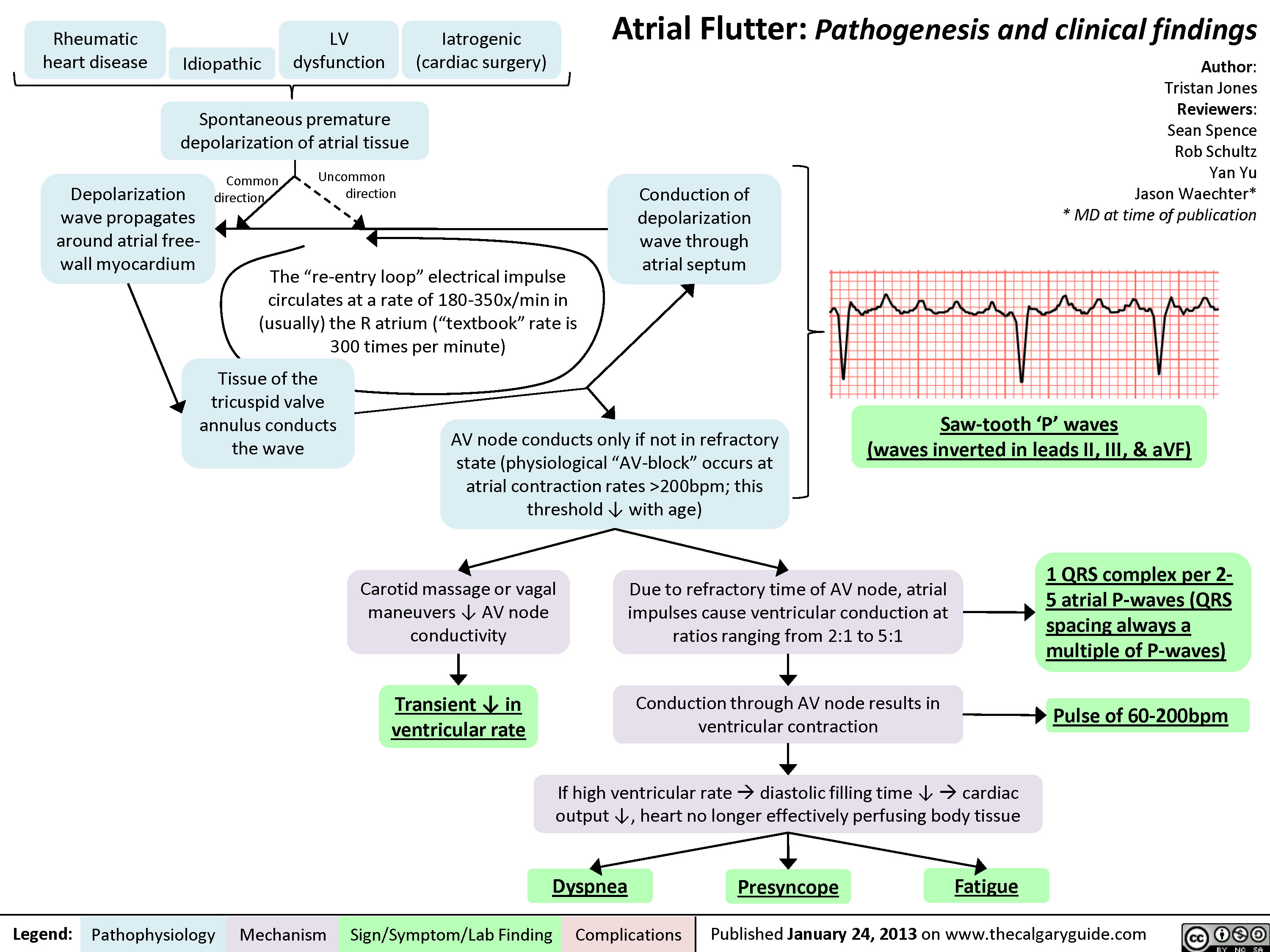
Atrial Flutter
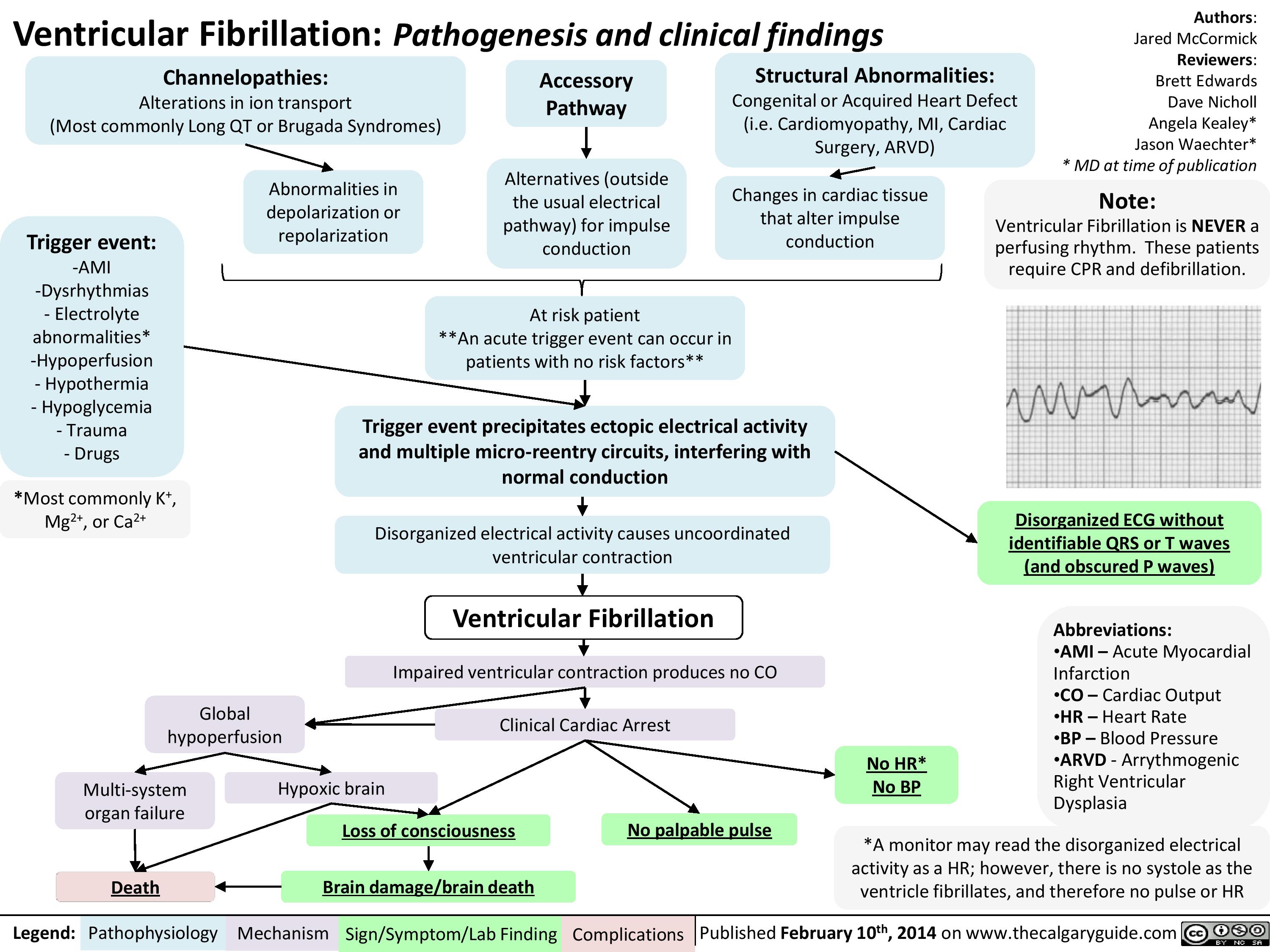
Ventricular fibrillation
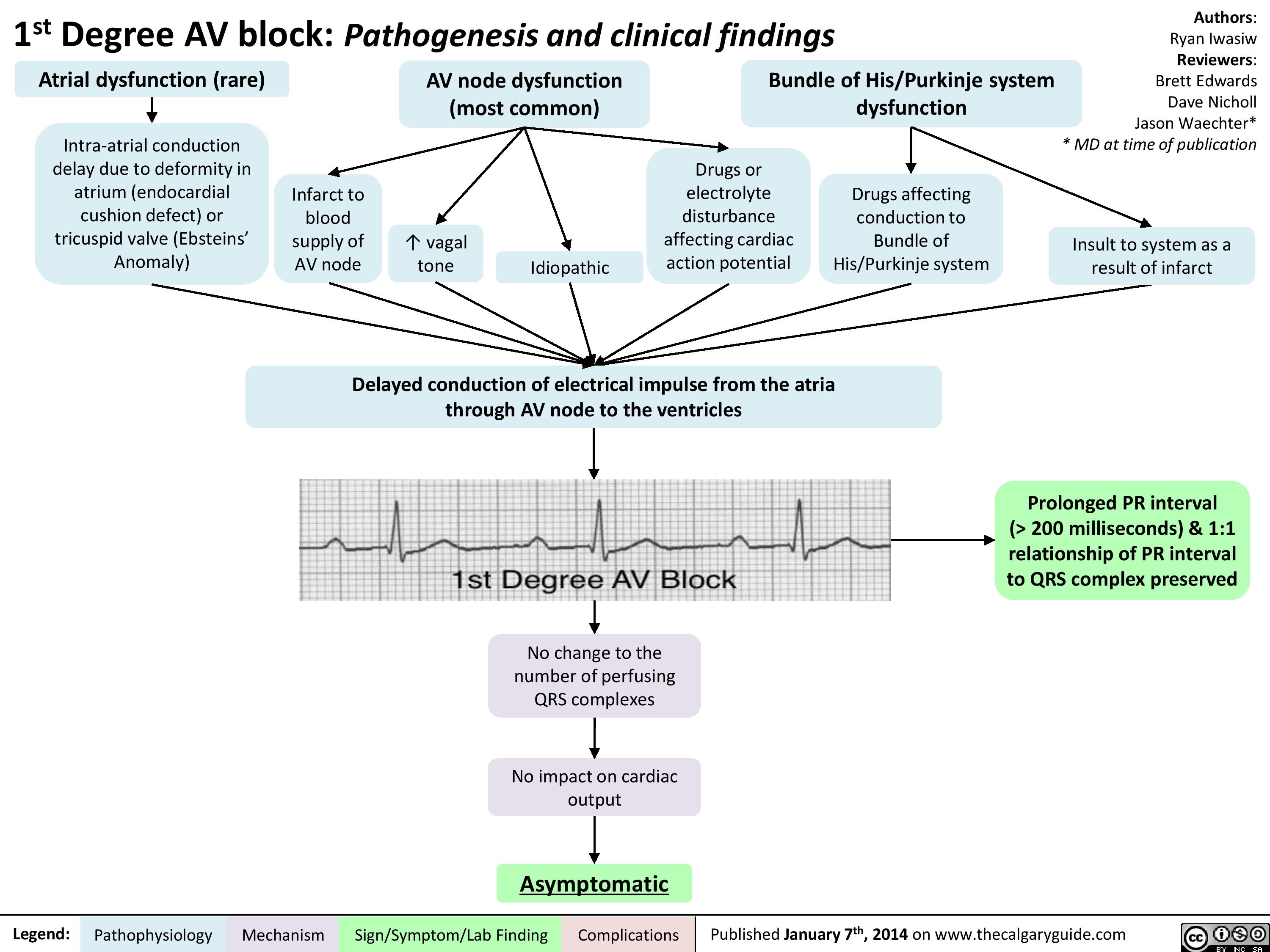
1st Degree AV block
Second Degree Heart Block - Mobitz Type II - Pathogenesis and clinical findings

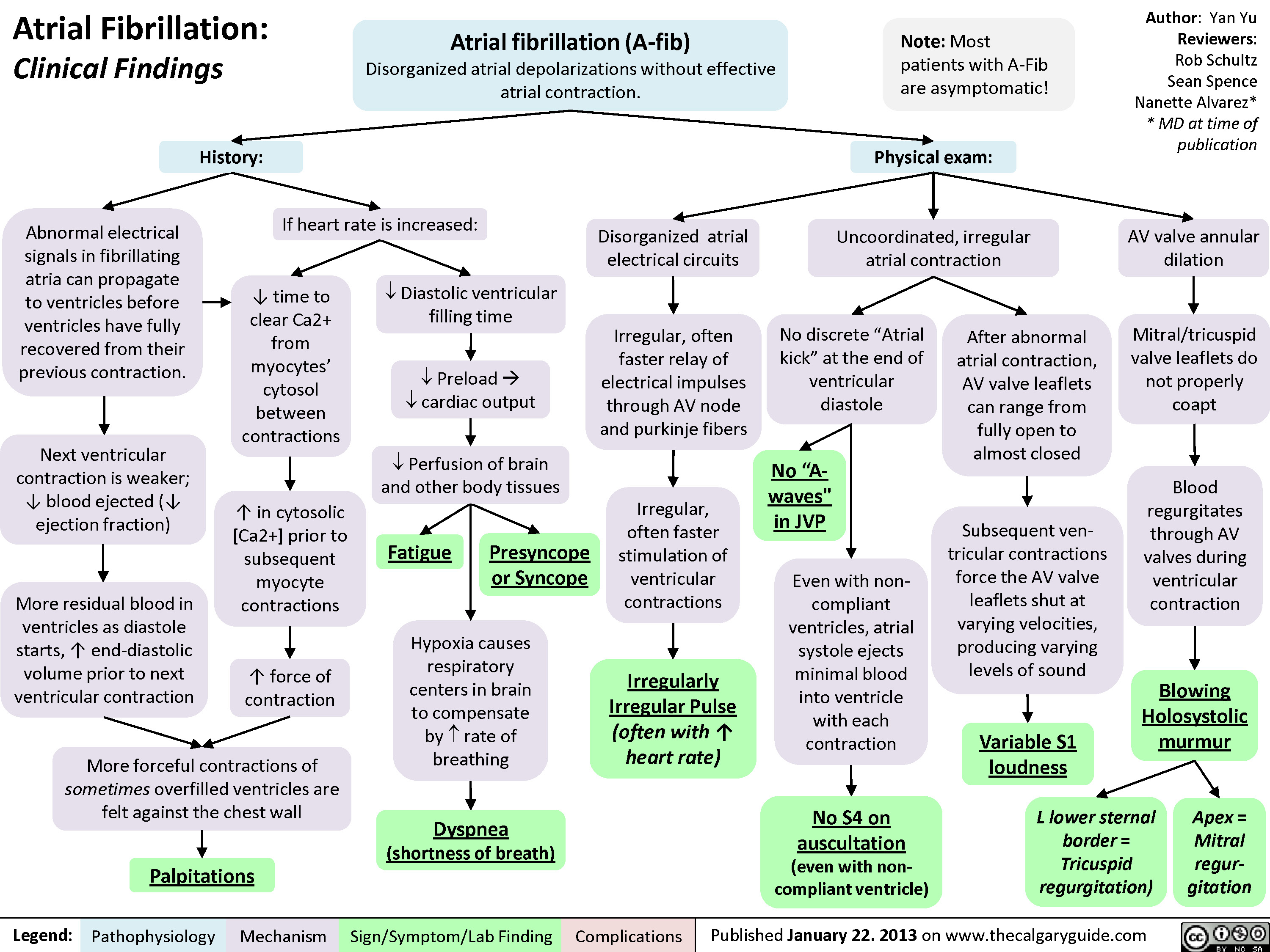
Atrial Fibrillation - Clinical Findings
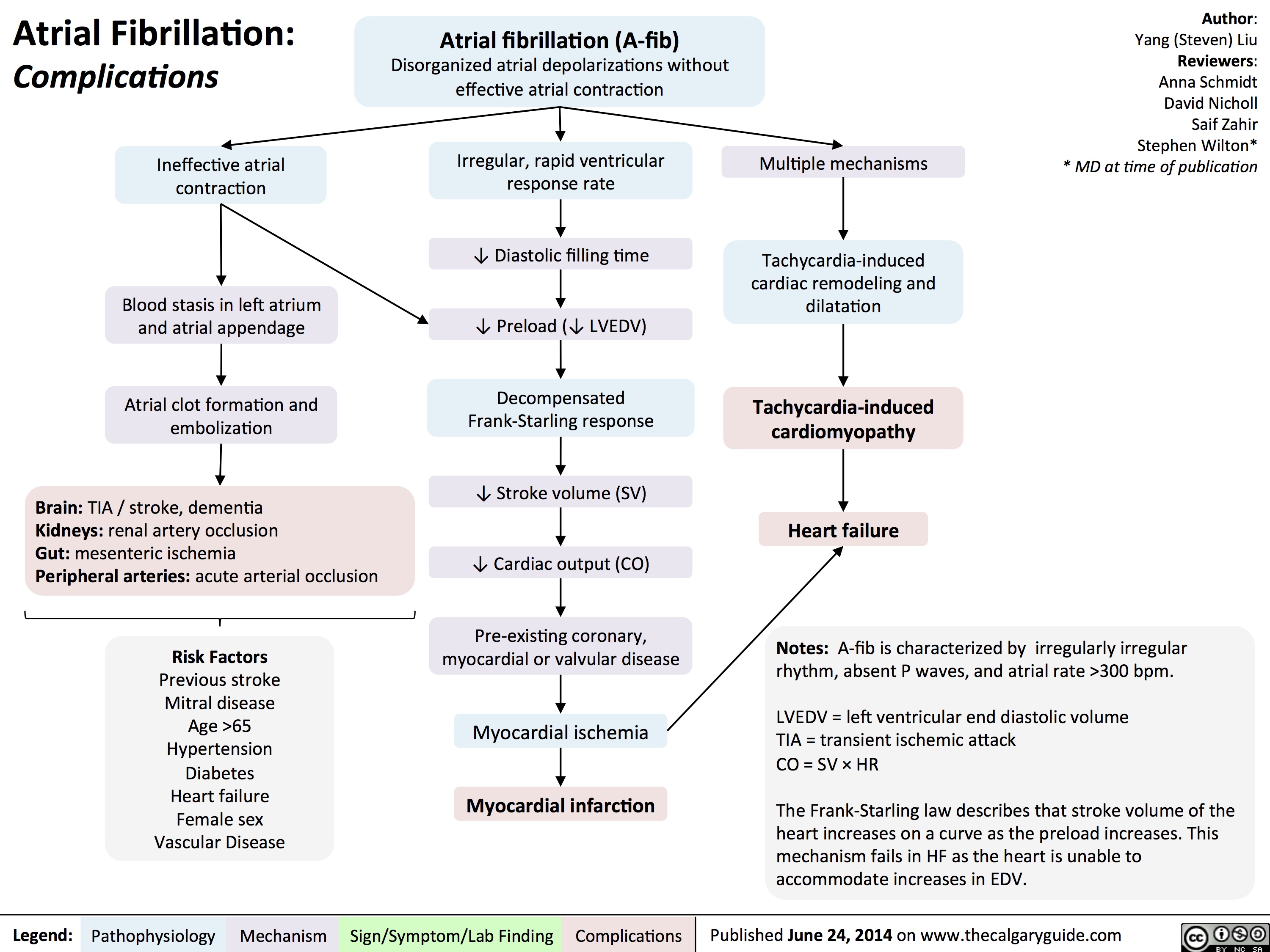
atrial-fibrillation-complications
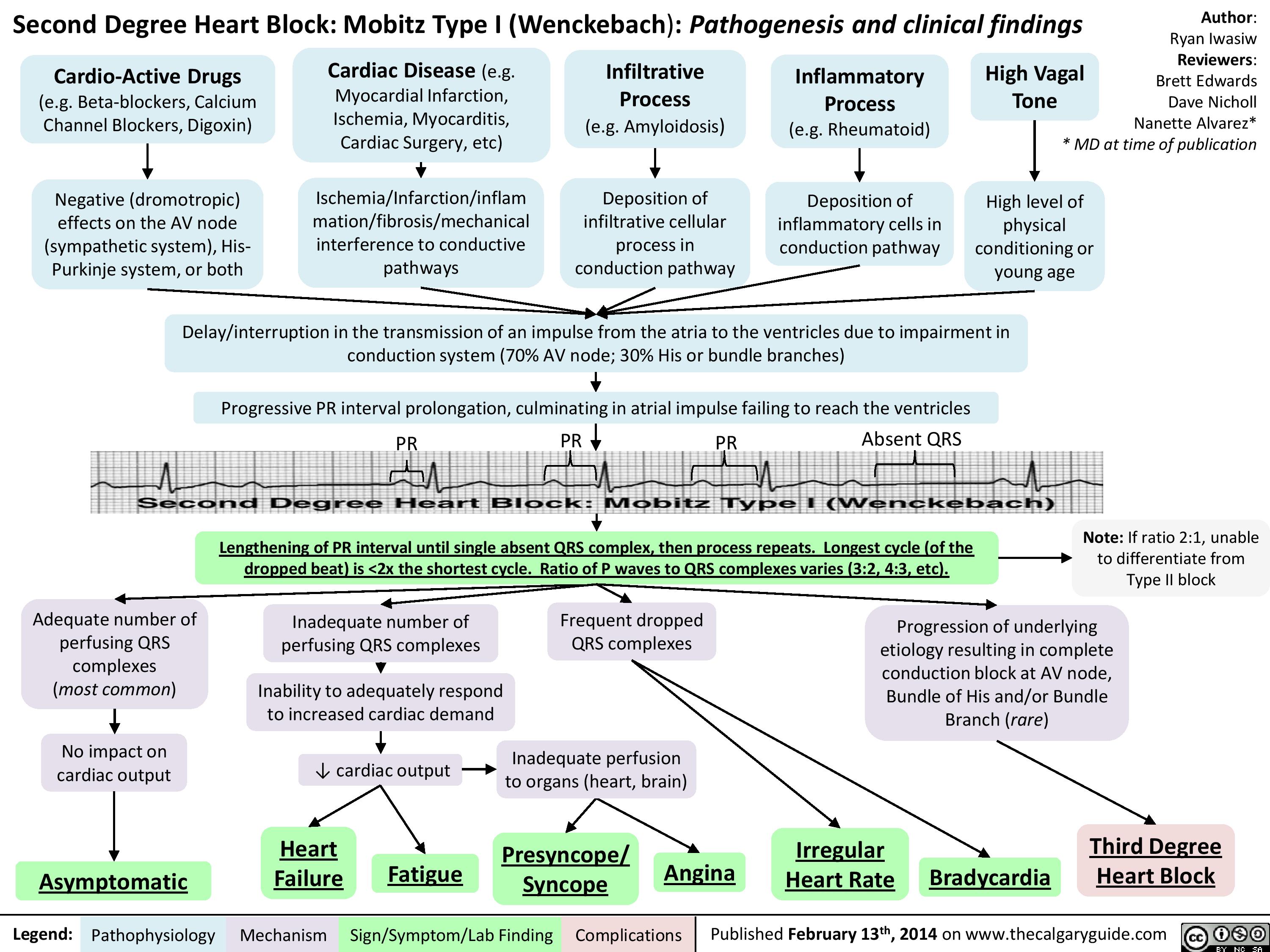
Second Degree Heart Block - Mobitz Type I (Wenckebach) - Pathogenesis and Clinical Findings
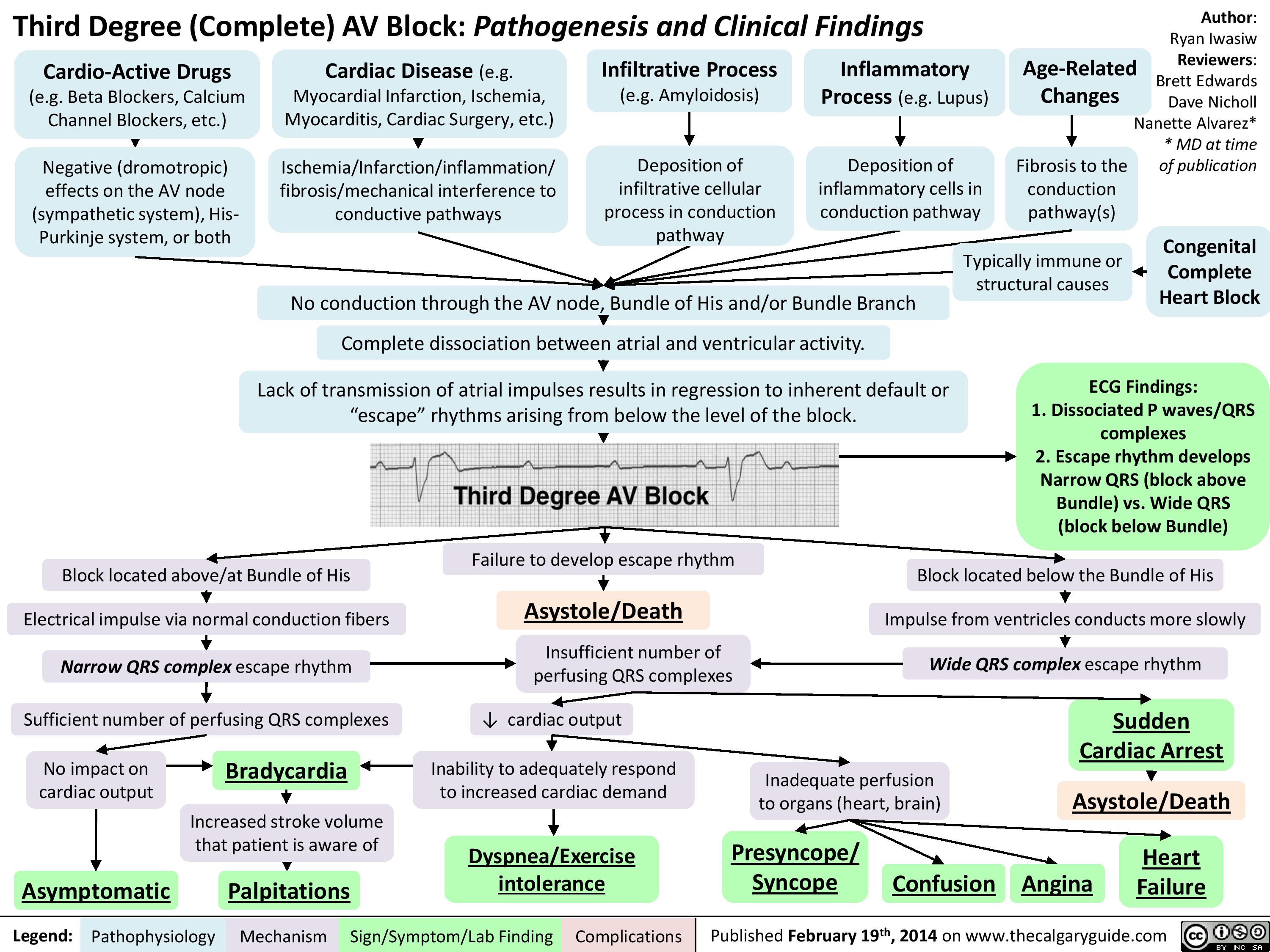
Third Degree (Complete) AV Block - Pathogenesis and Clinical Findings
Atrial Flutter (1)
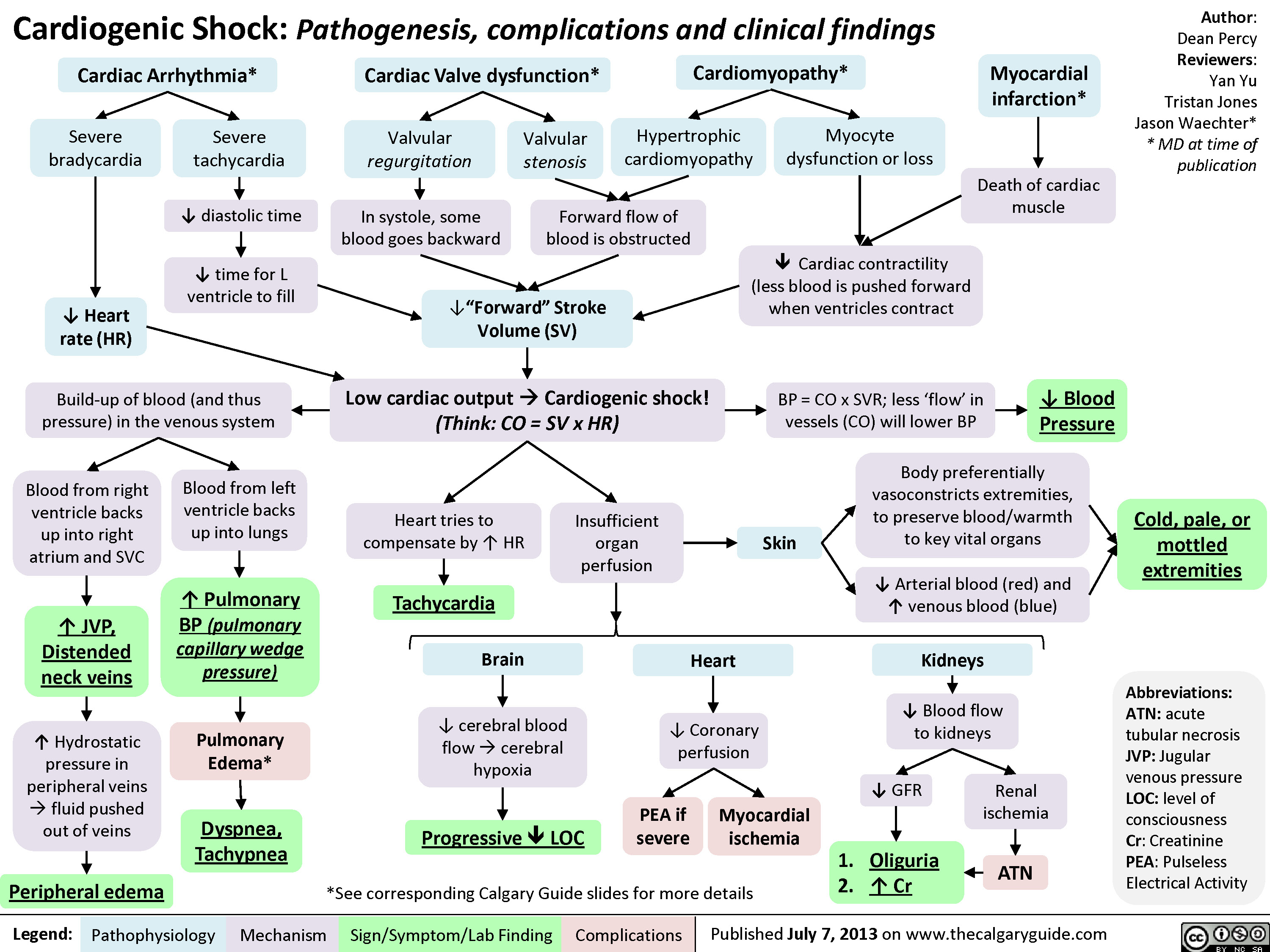
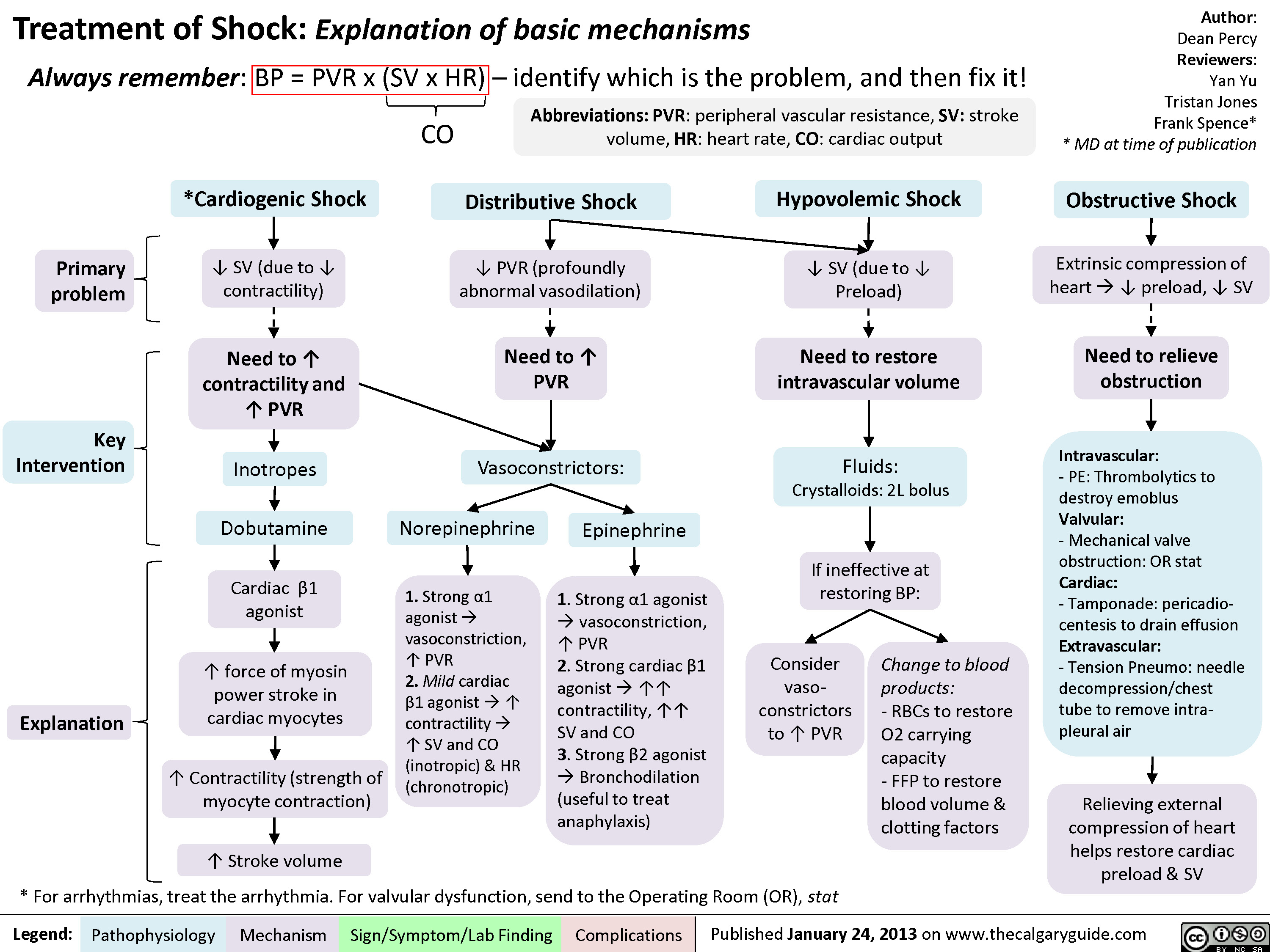
Cardiogenic Shock
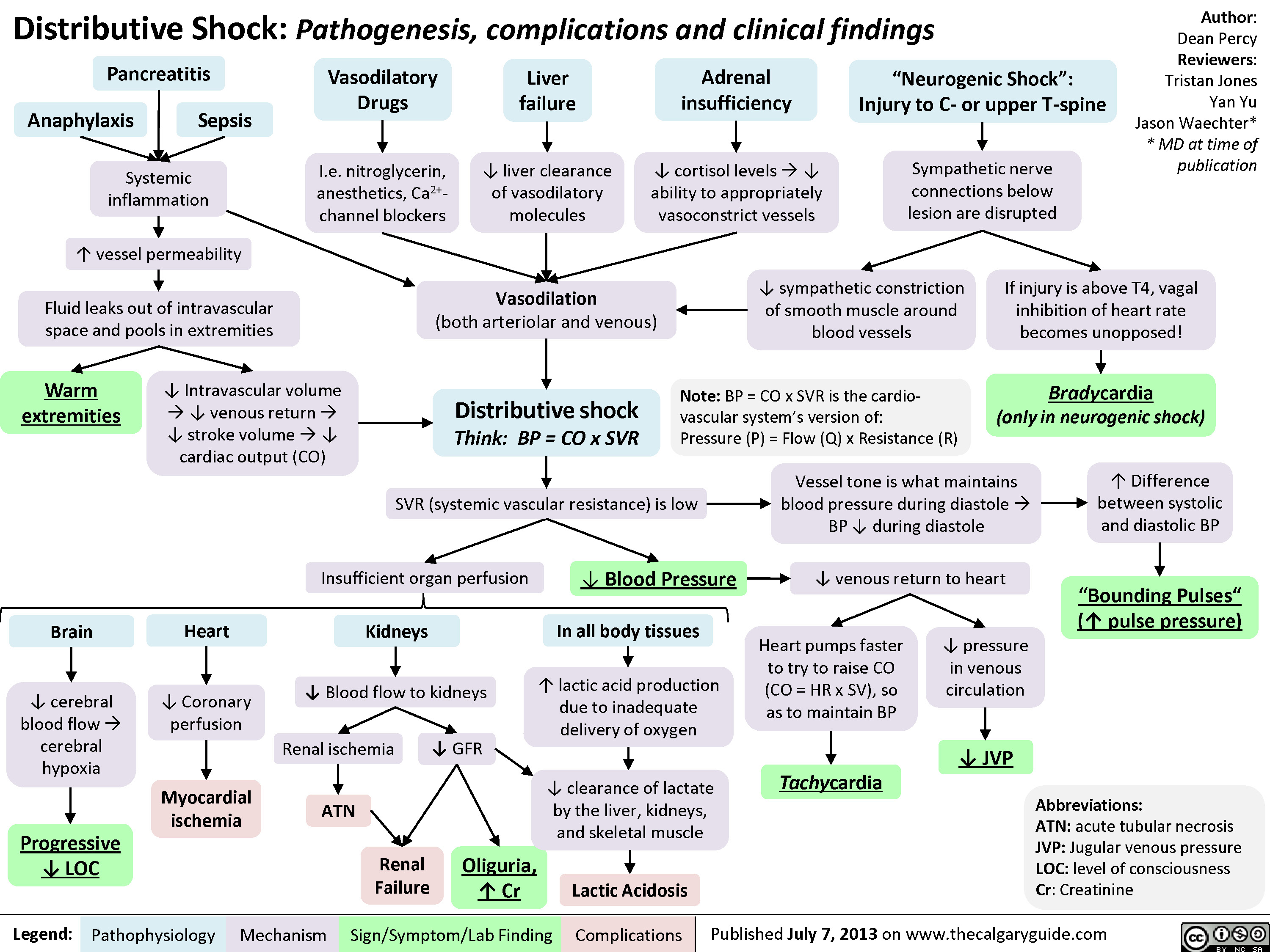
Distributive Shock
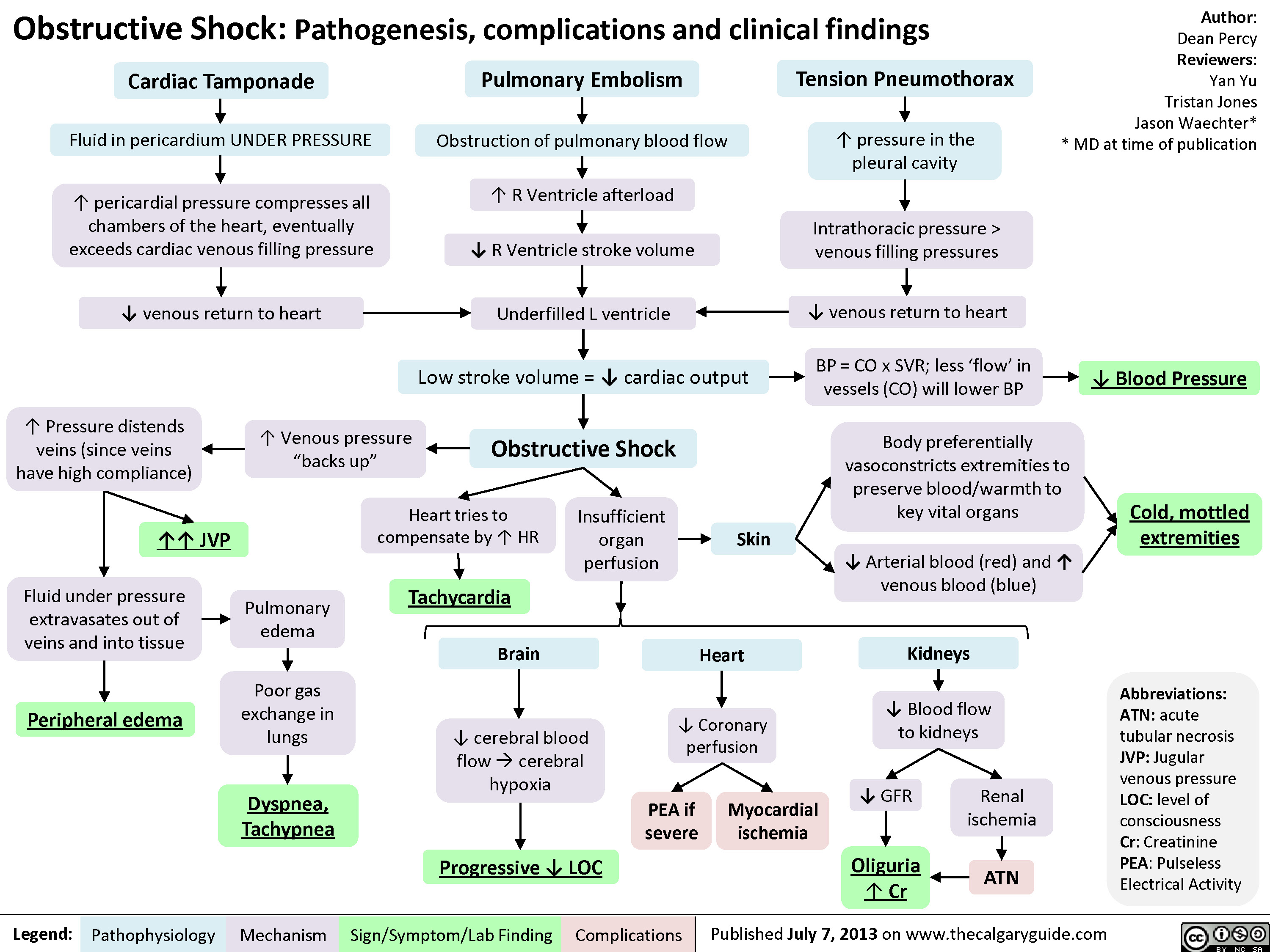
Obstructive Shock
Drugs used to treat shock
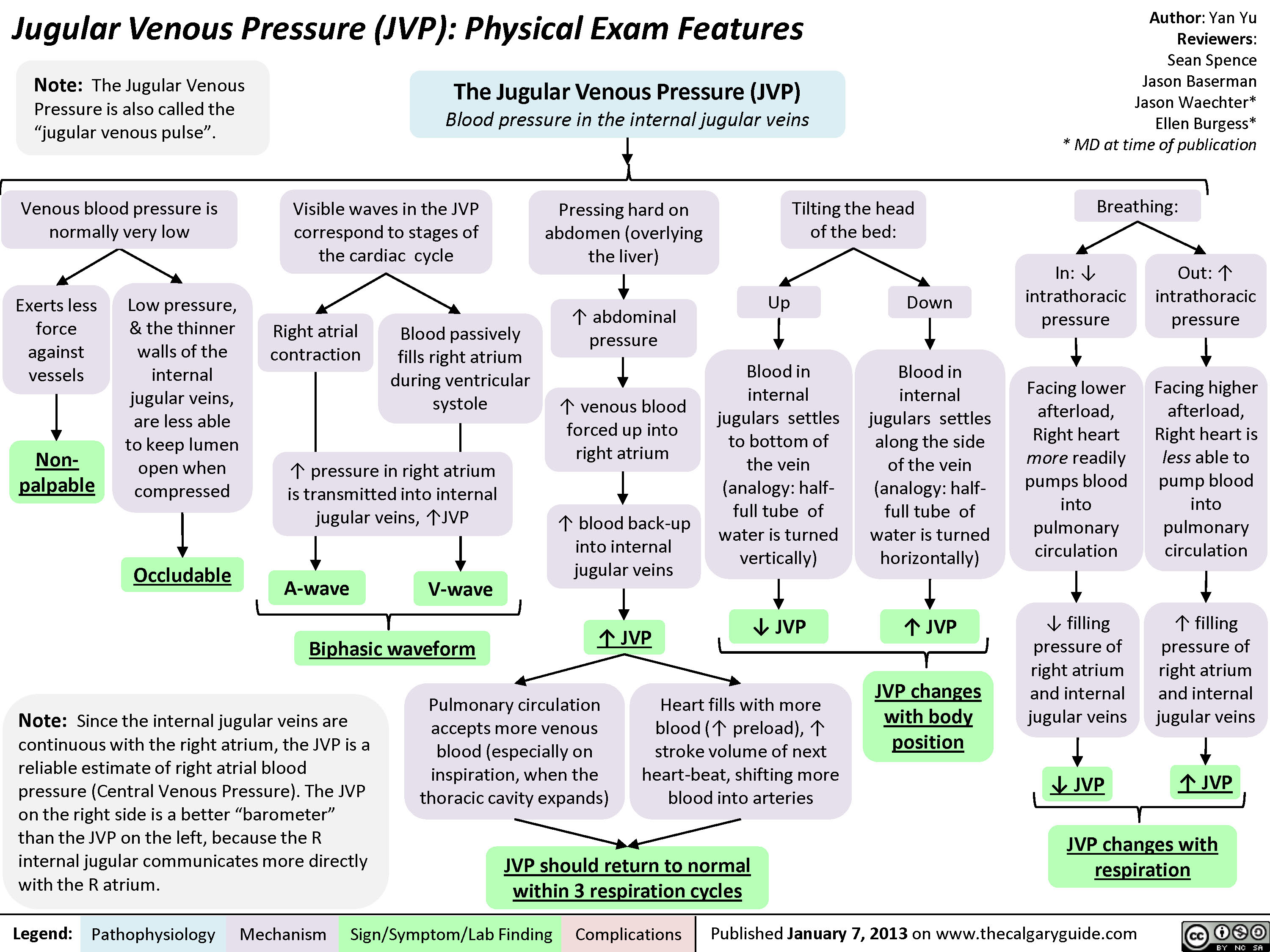
JVP-Physical Exam Features
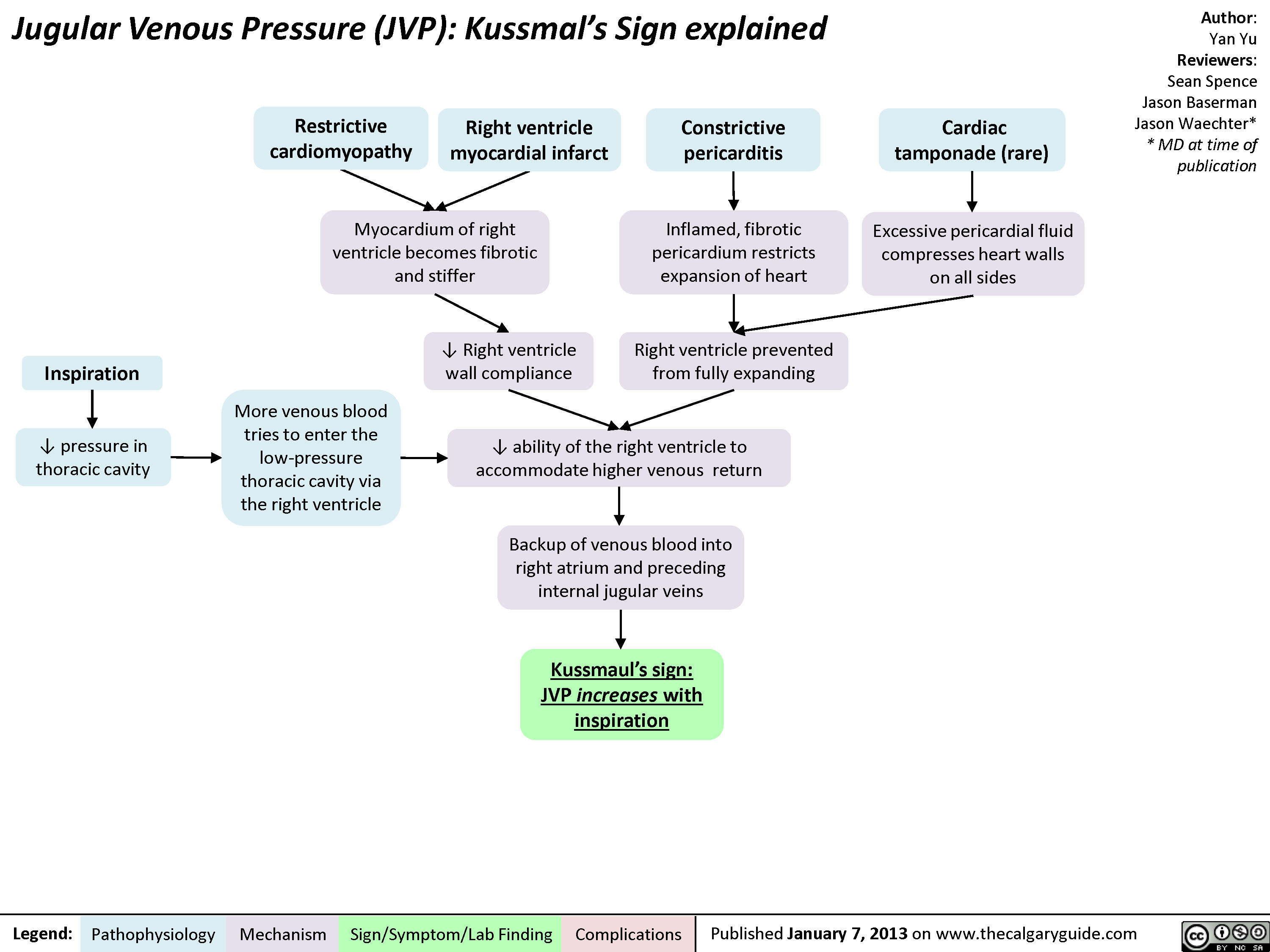
jvp-kussmals-sign-explained
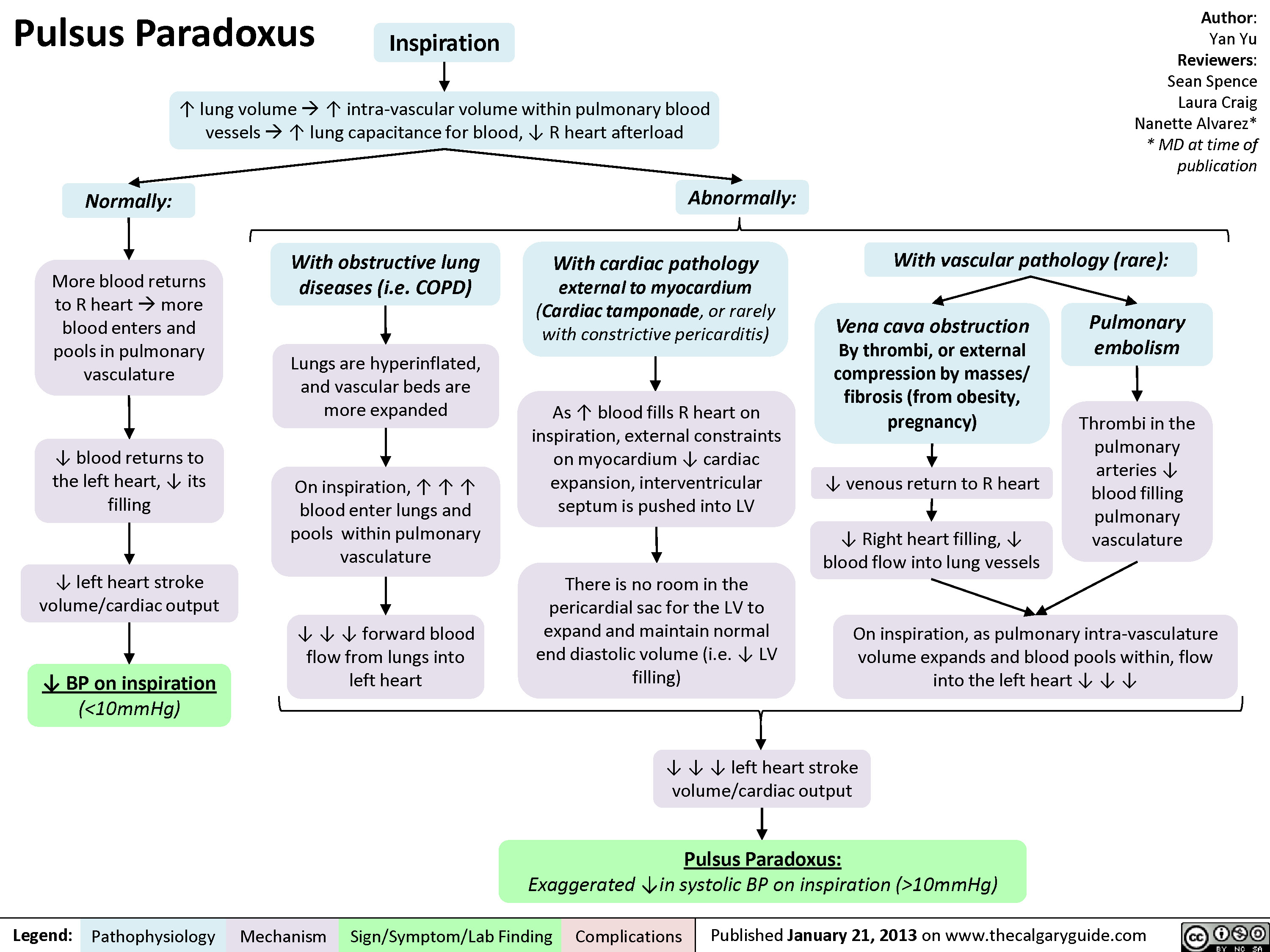
Pulsus Paradoxus
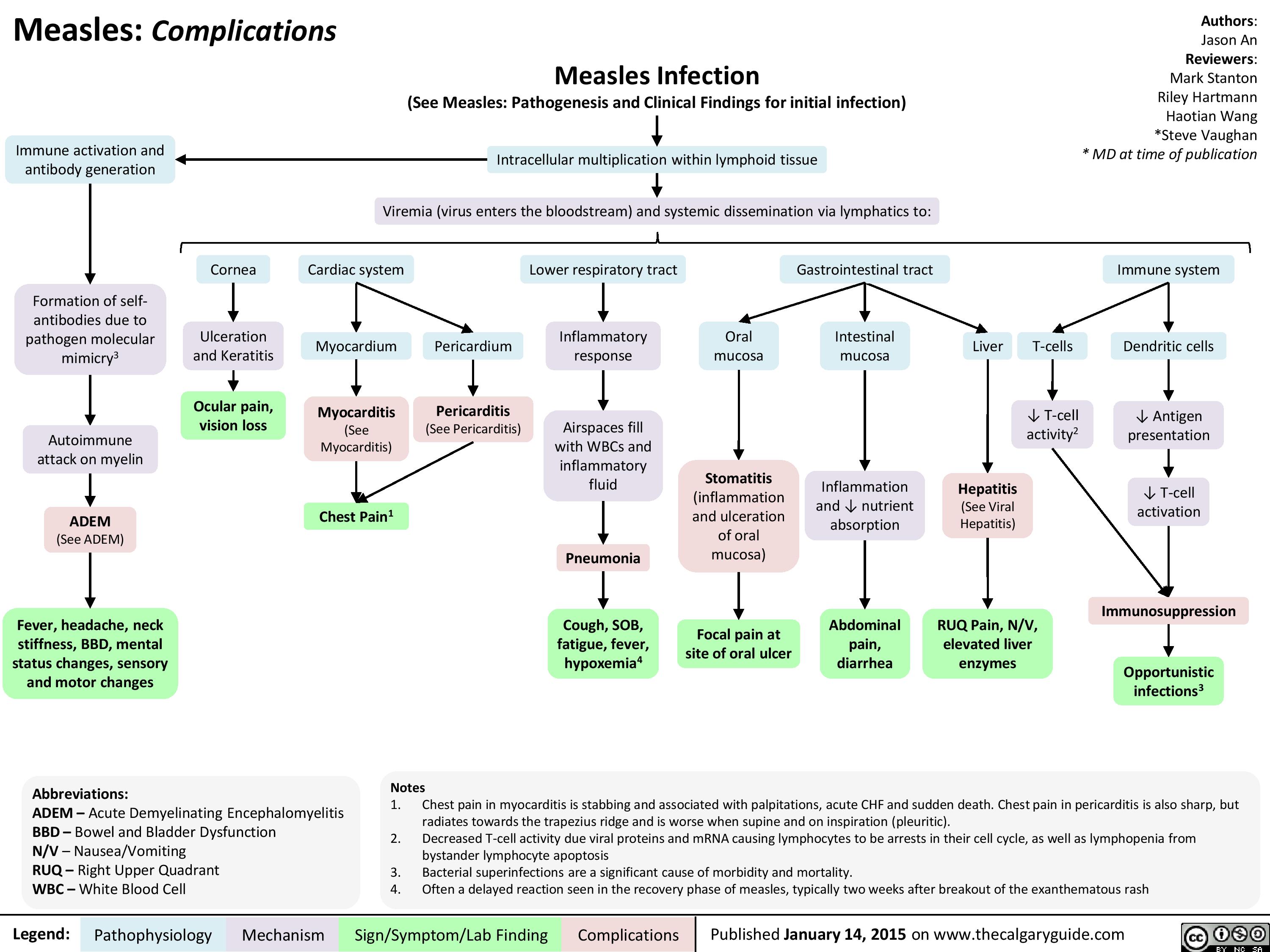
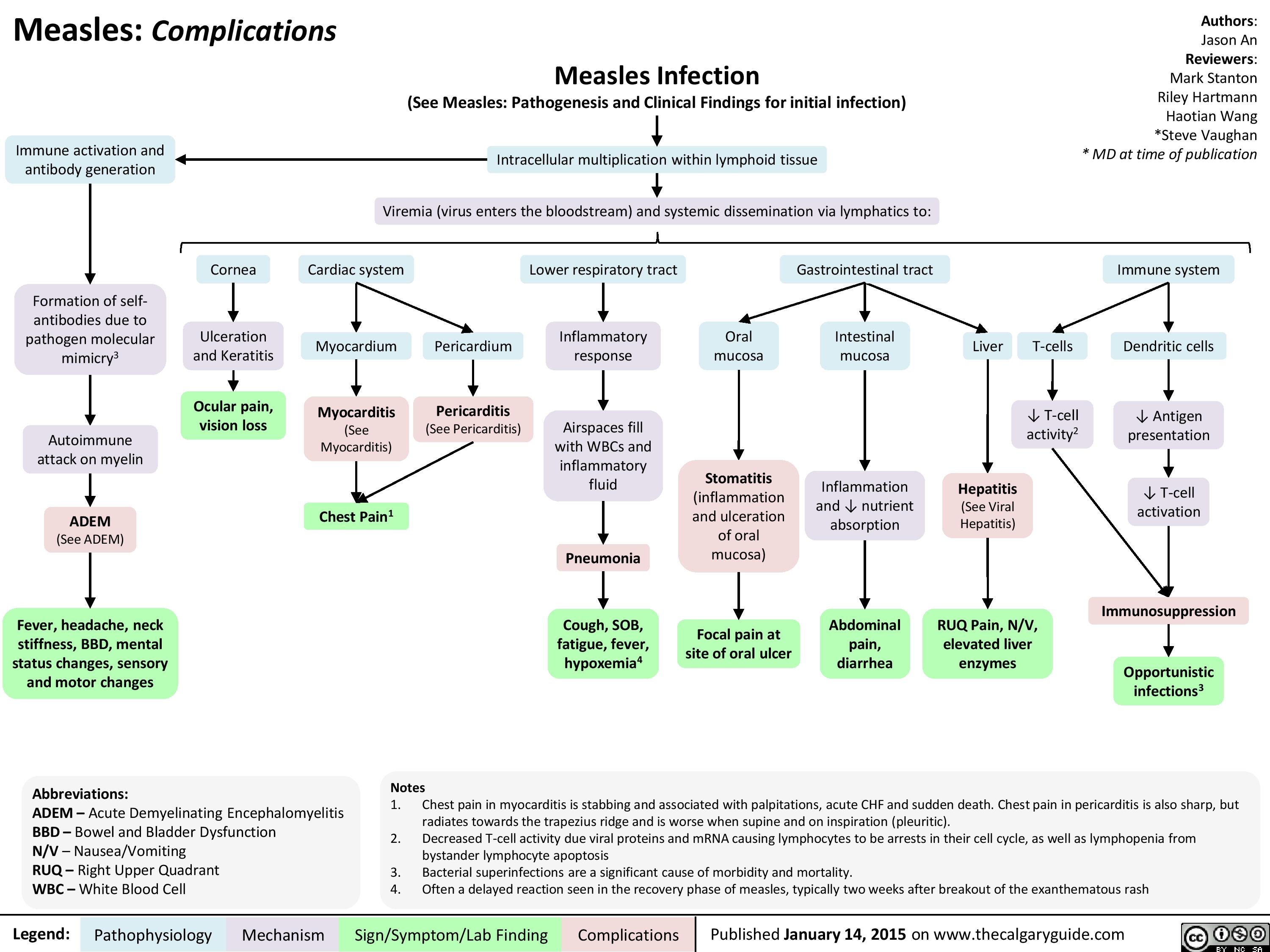
Complications of Measles Pathogenesis and Clinical Findings
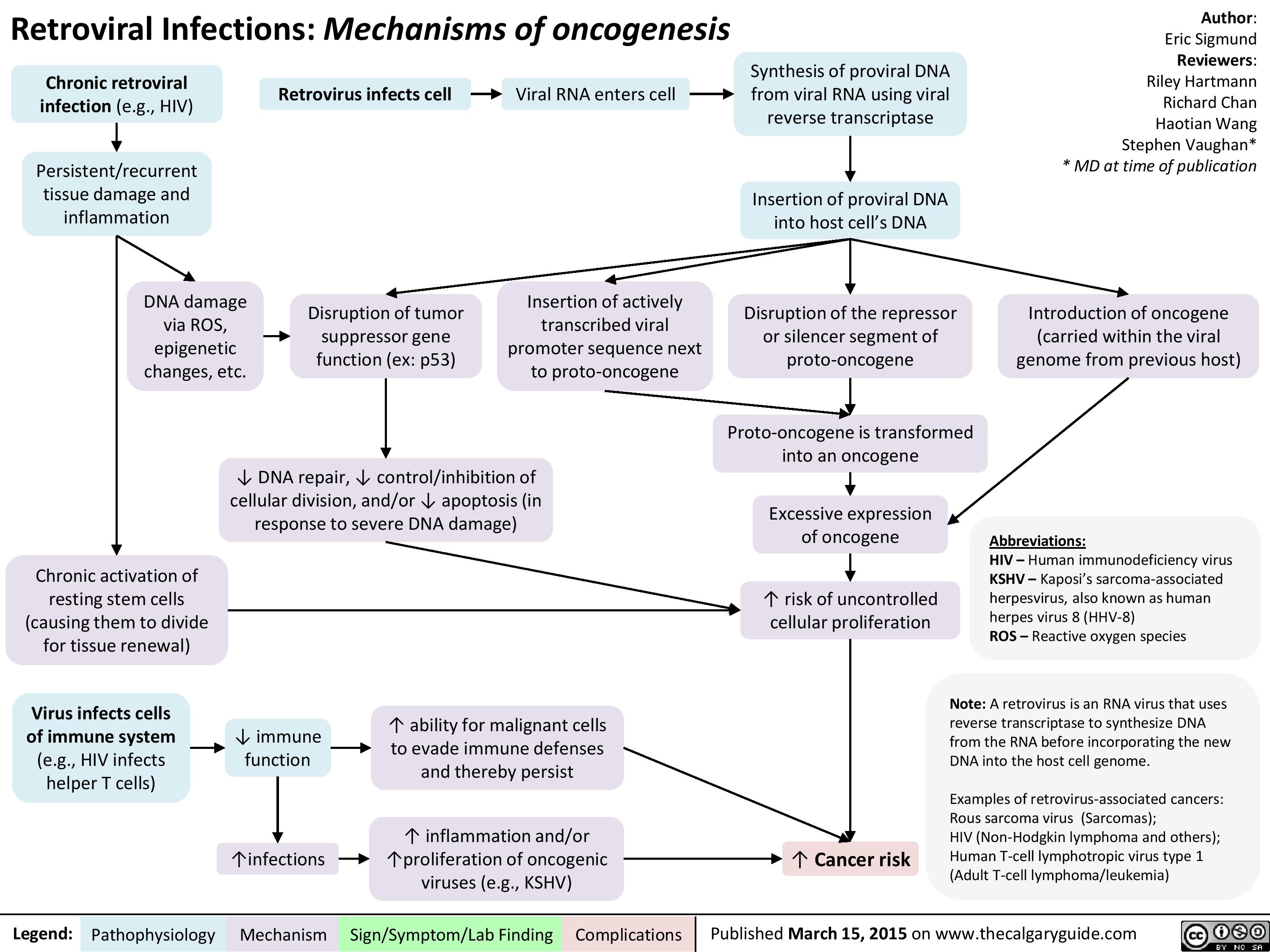
Retroviral Infections Mechanisms of oncogenesis
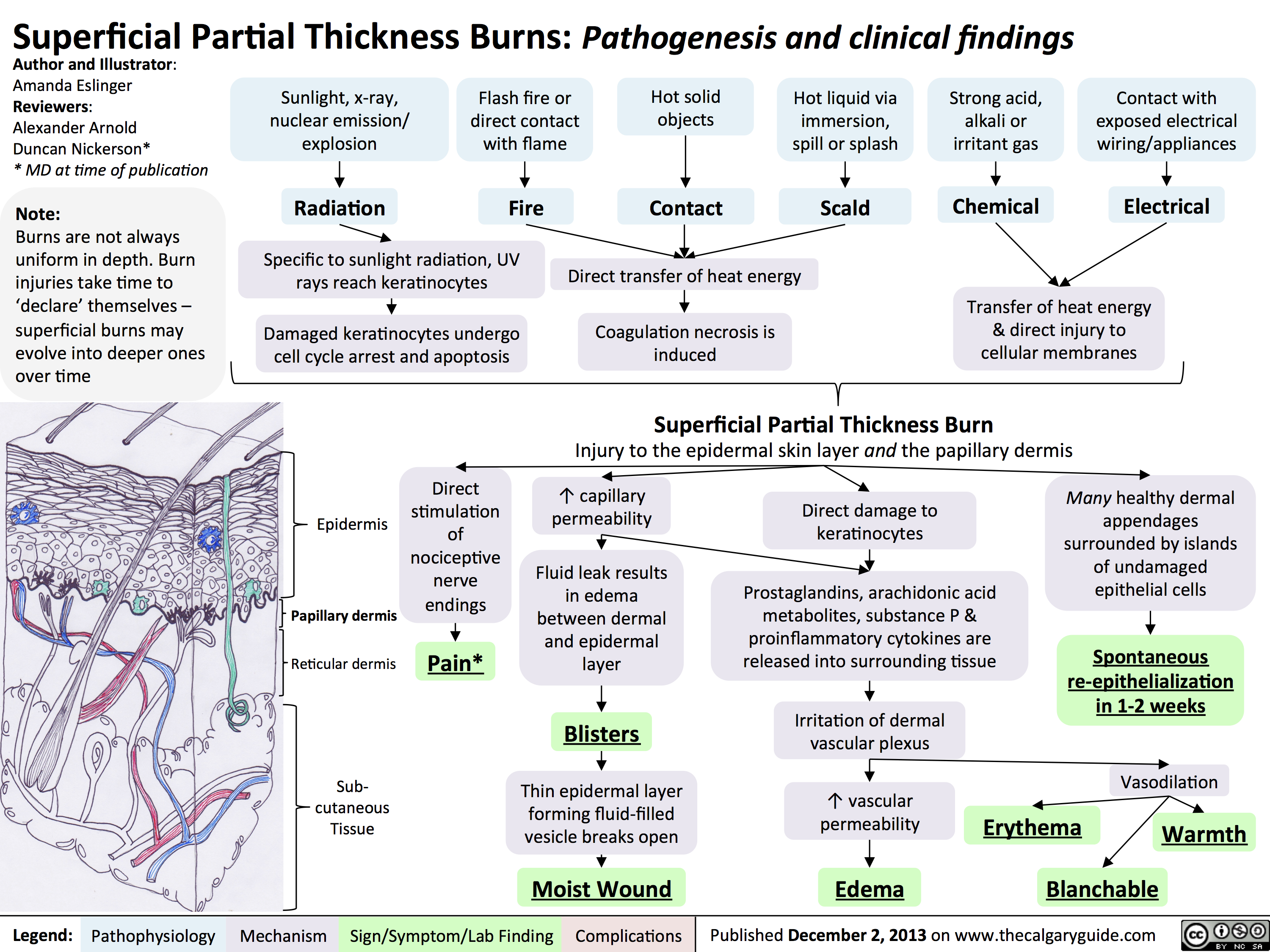
Superficial Partial Thickness Burns - Pathogenesis and Clinical Findings
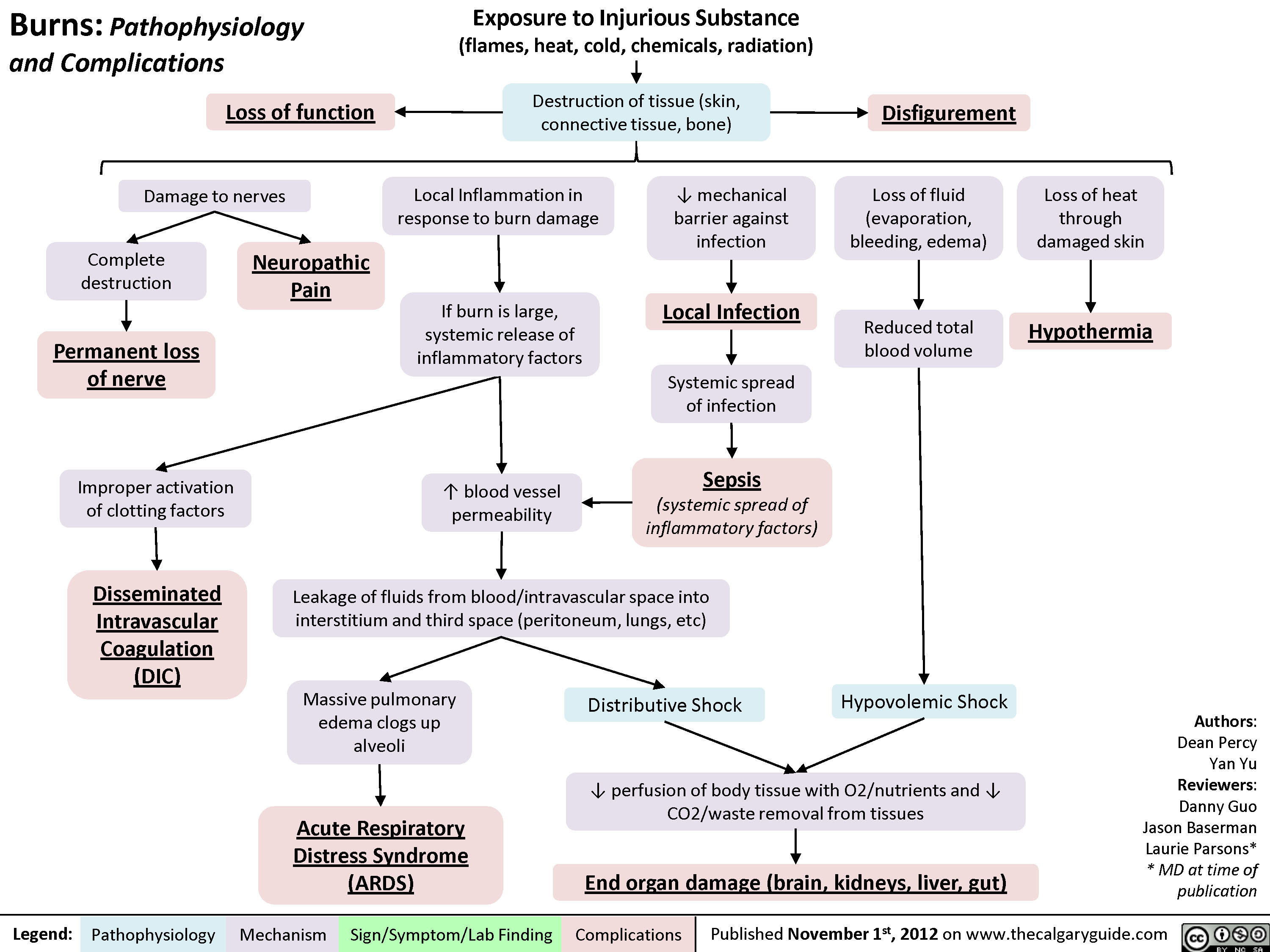
Complications of Burns
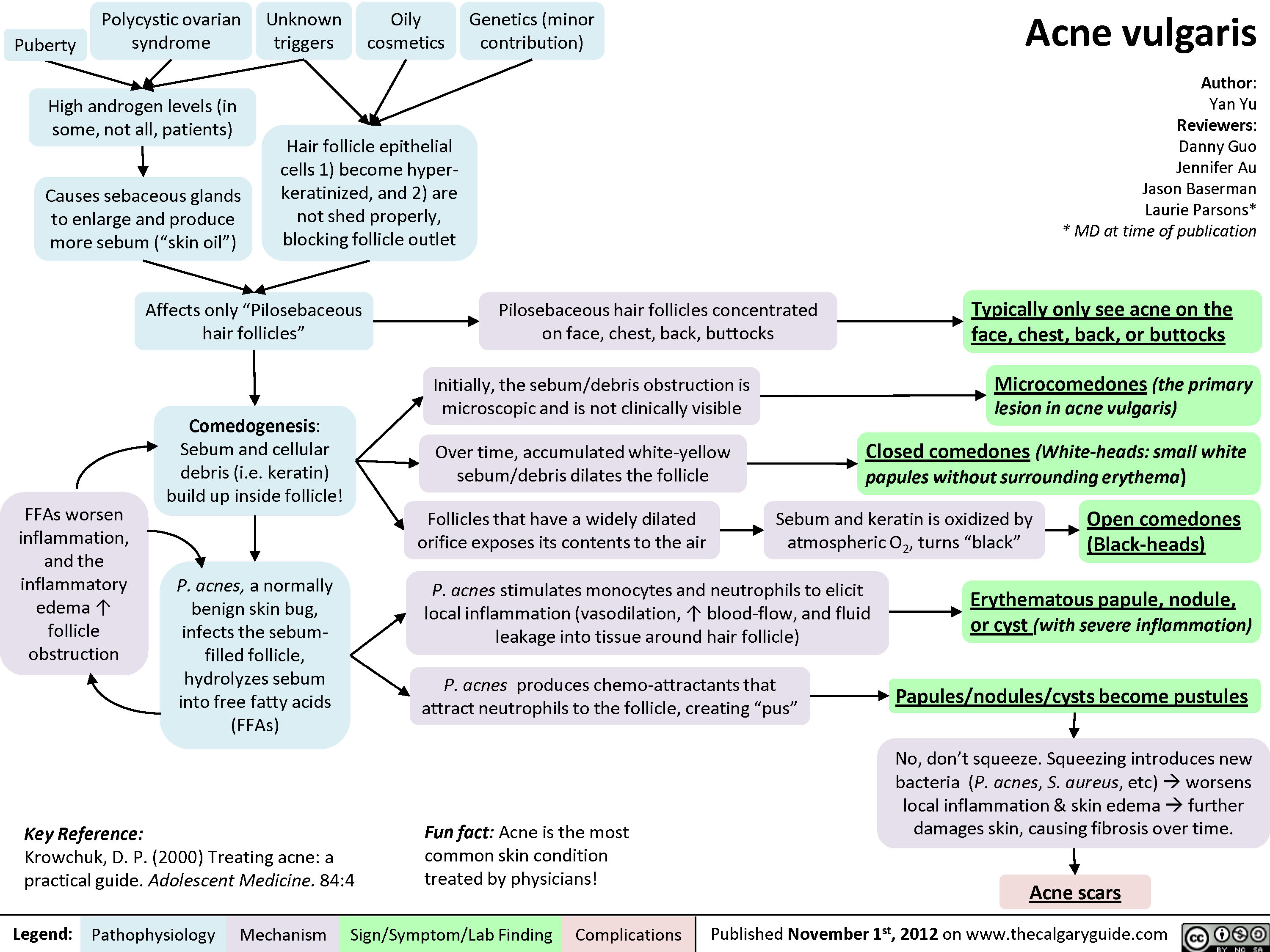
Acne Vulgaris
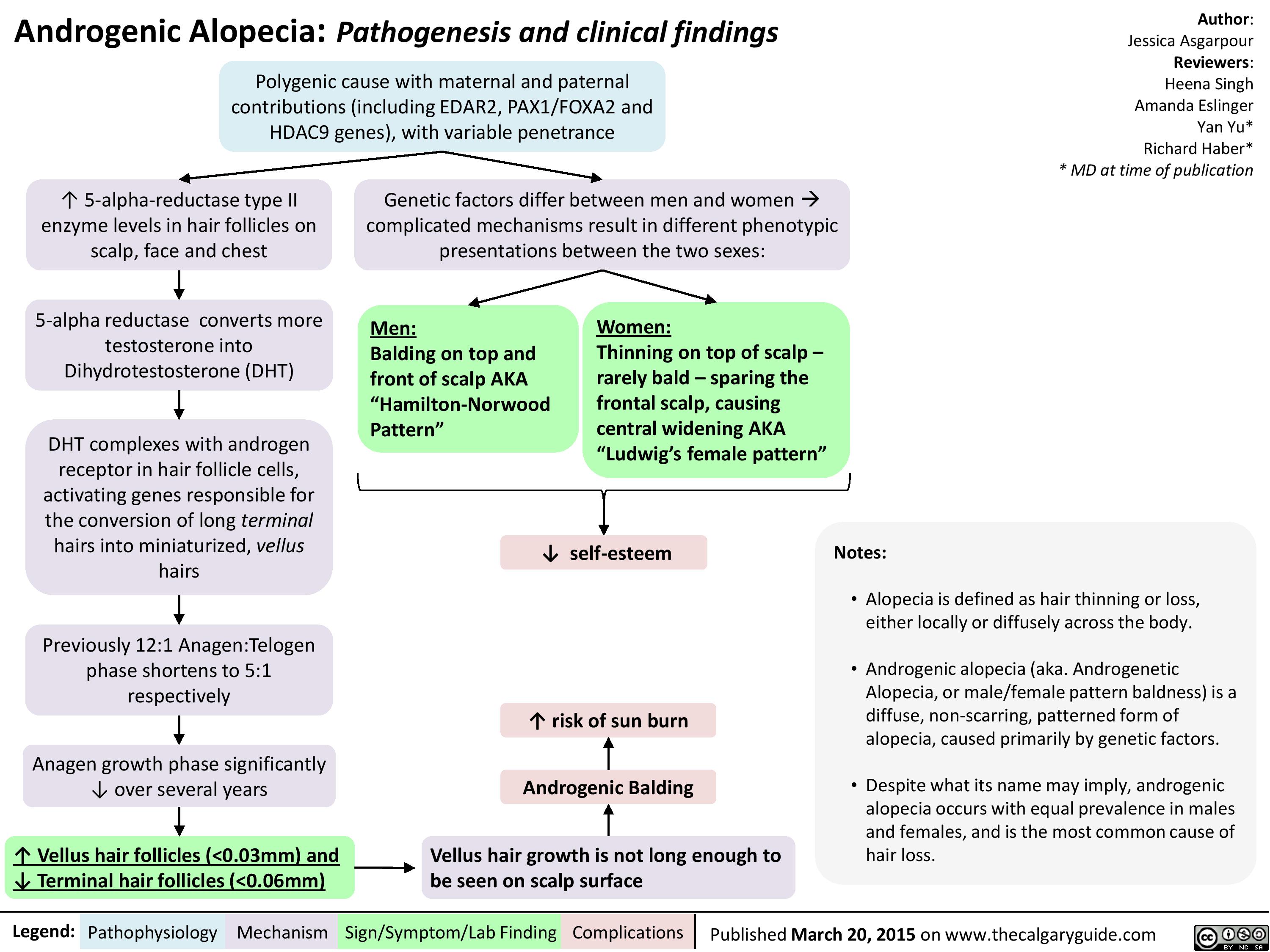
Androgenic Alopecia
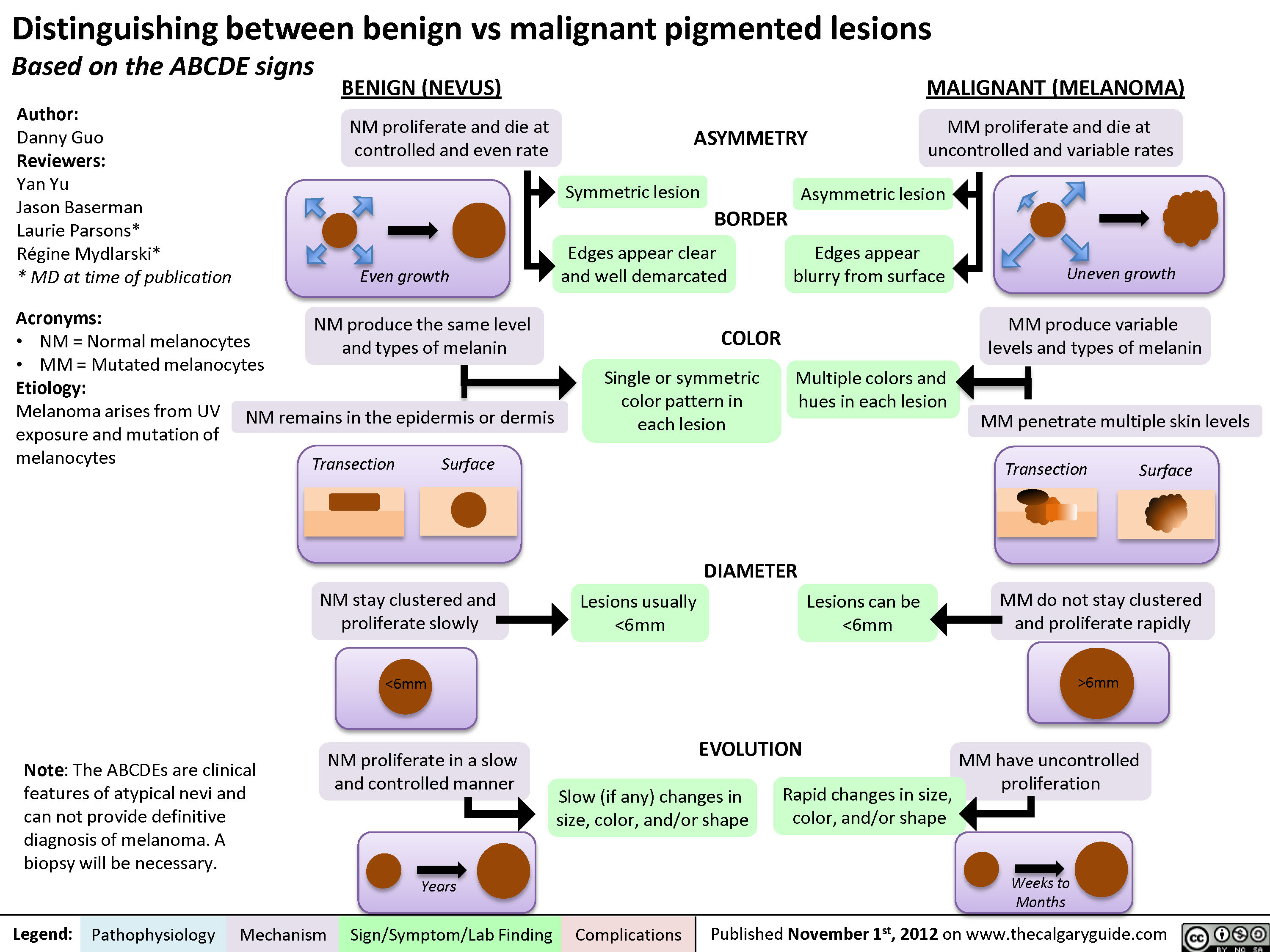
Distinguishing between Benign and Malignant Pigmented Lesions
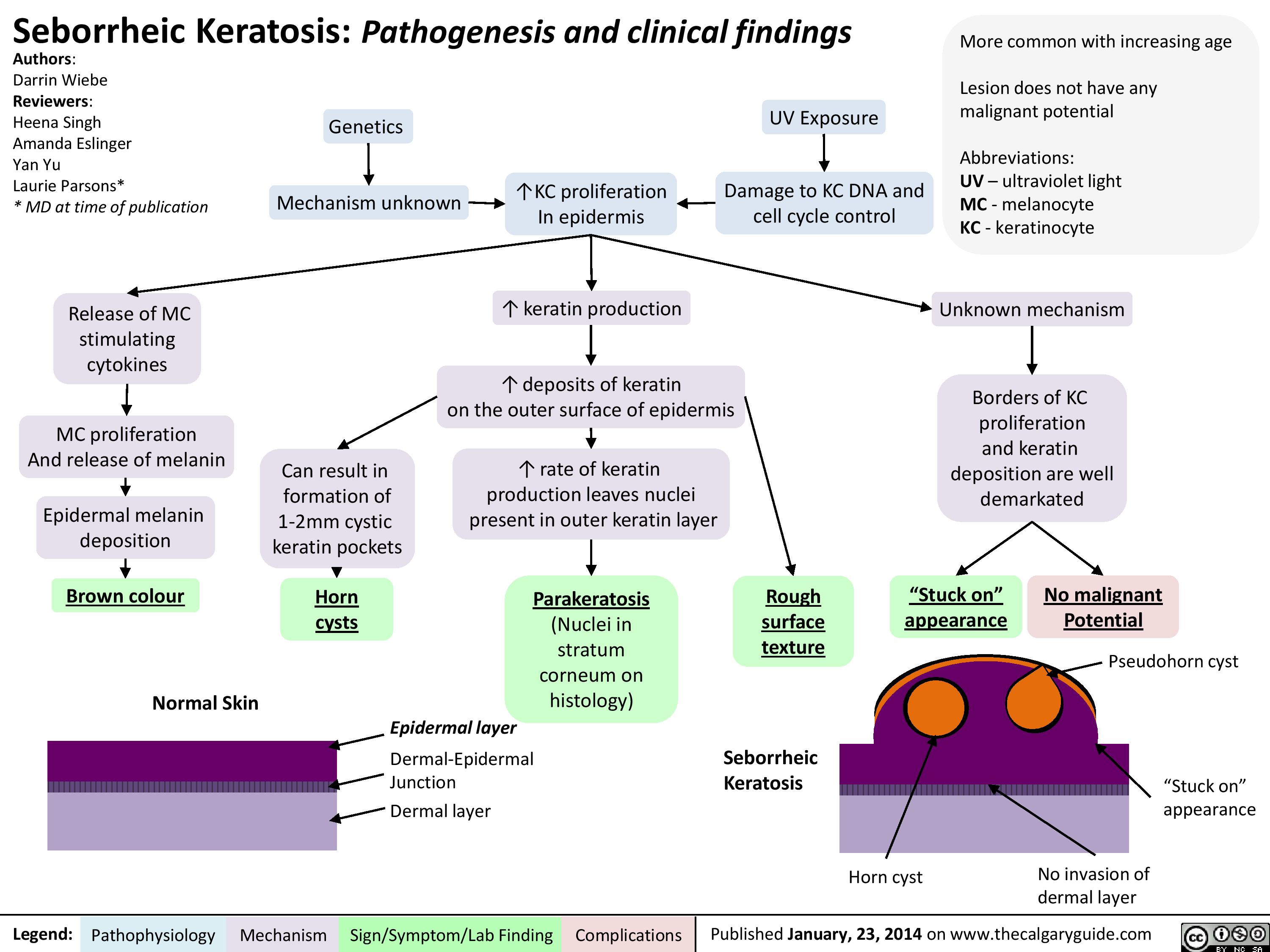
Seborrheic Keratosis
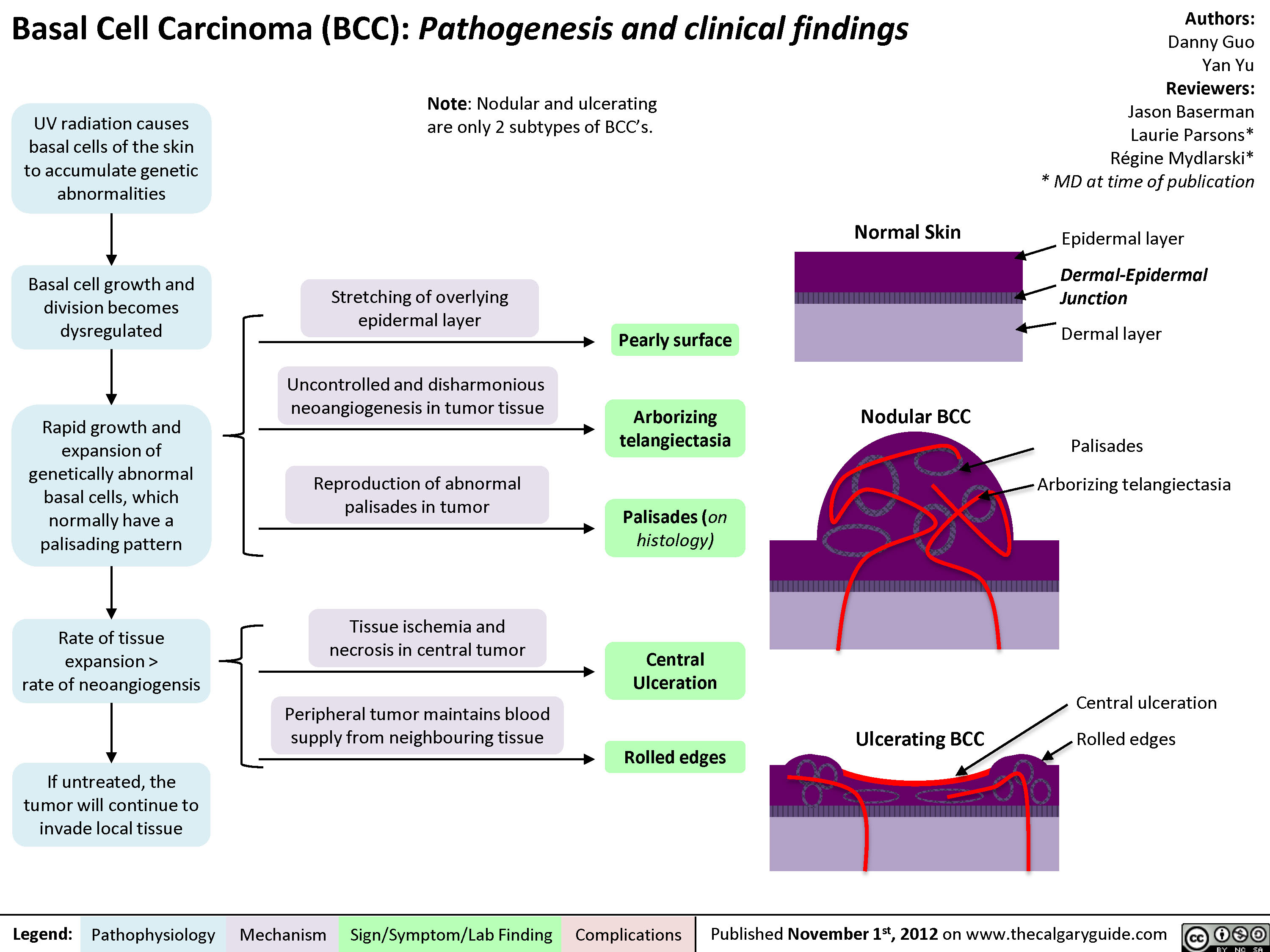
Basal Cell Carcinoma (BCC)
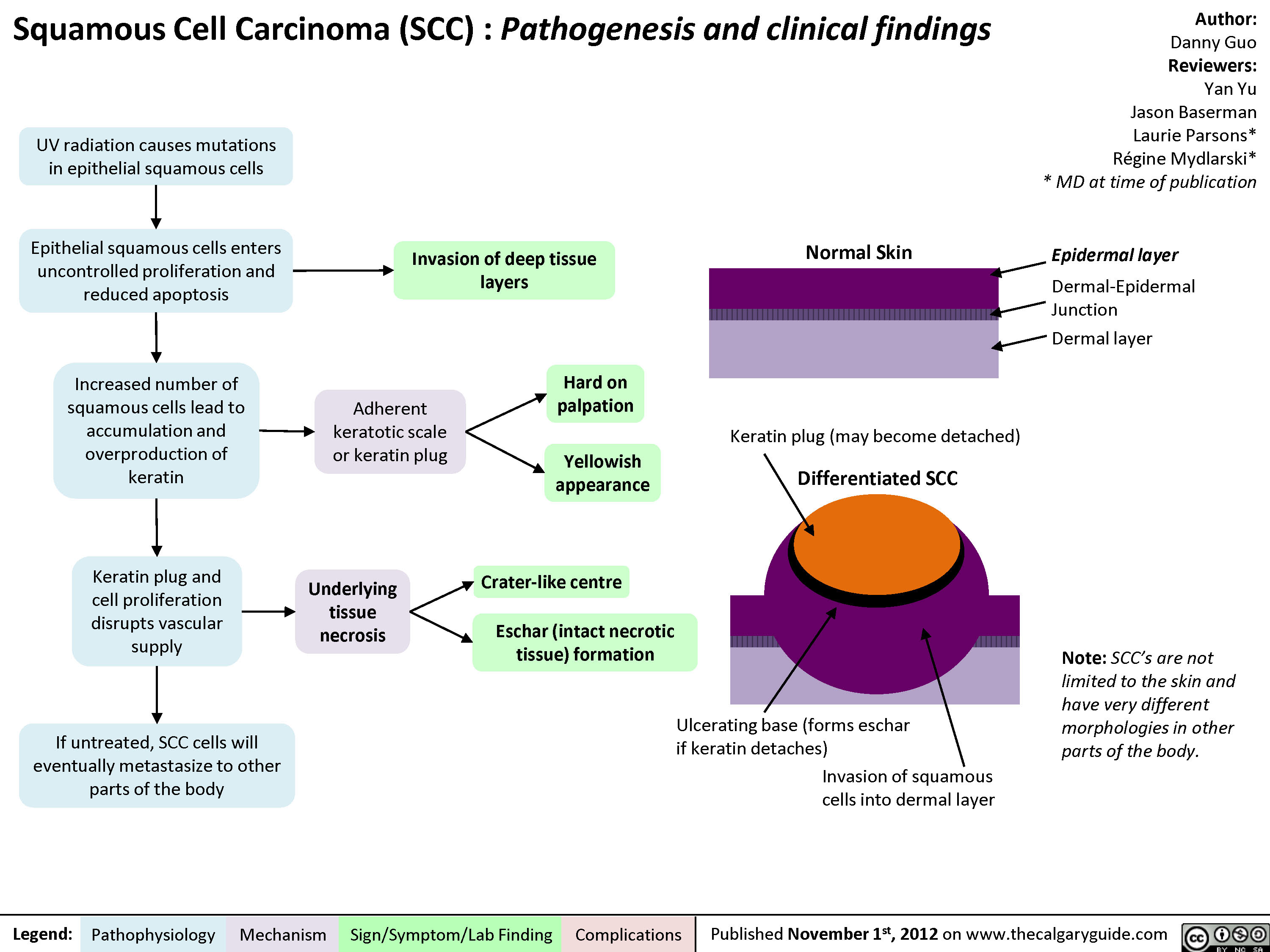
Squamous Cell Carcinoma (SCC)
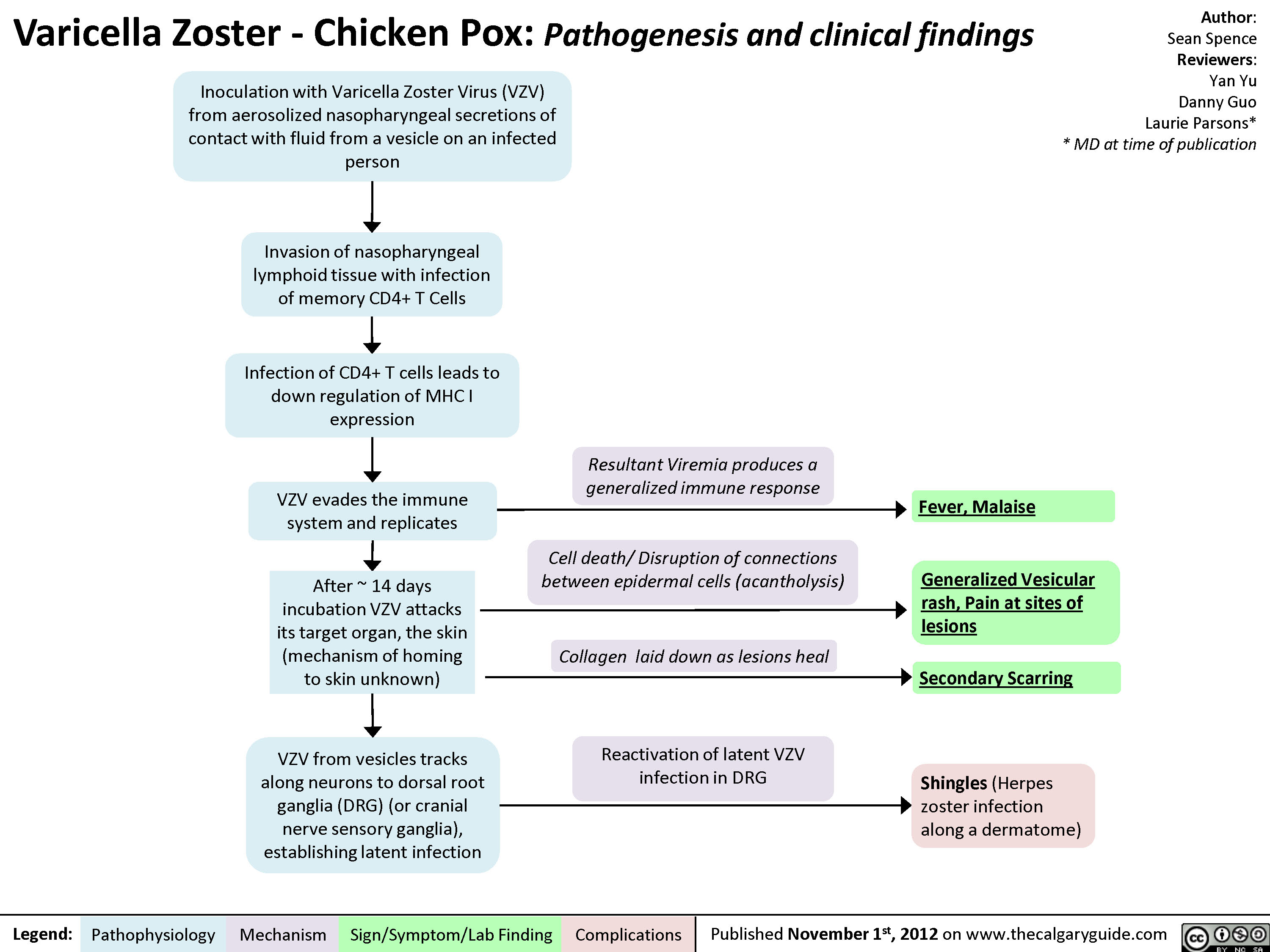
Varicella Zoster (Chicken Pox)
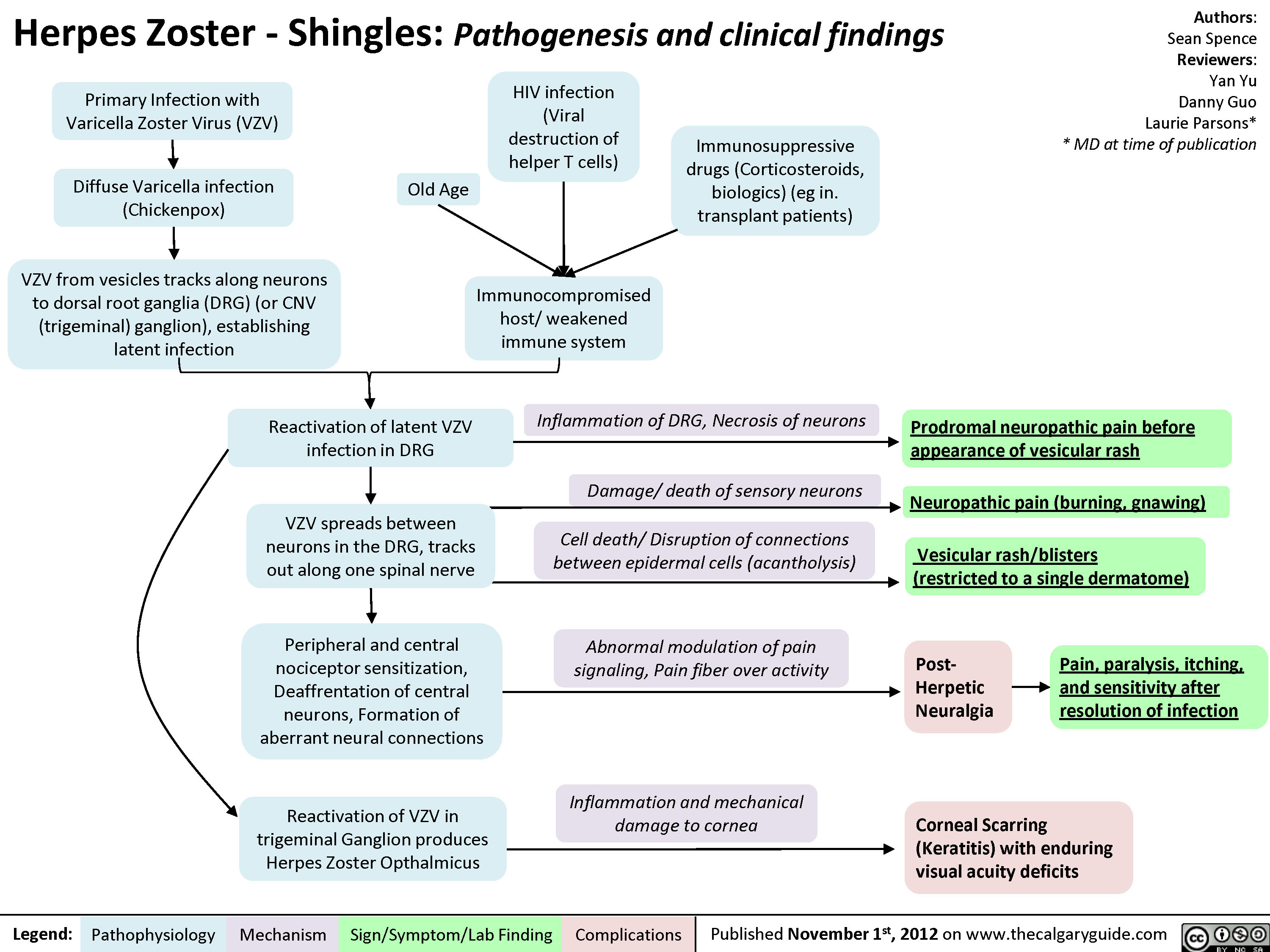
Herpes Zoster (Shingles)
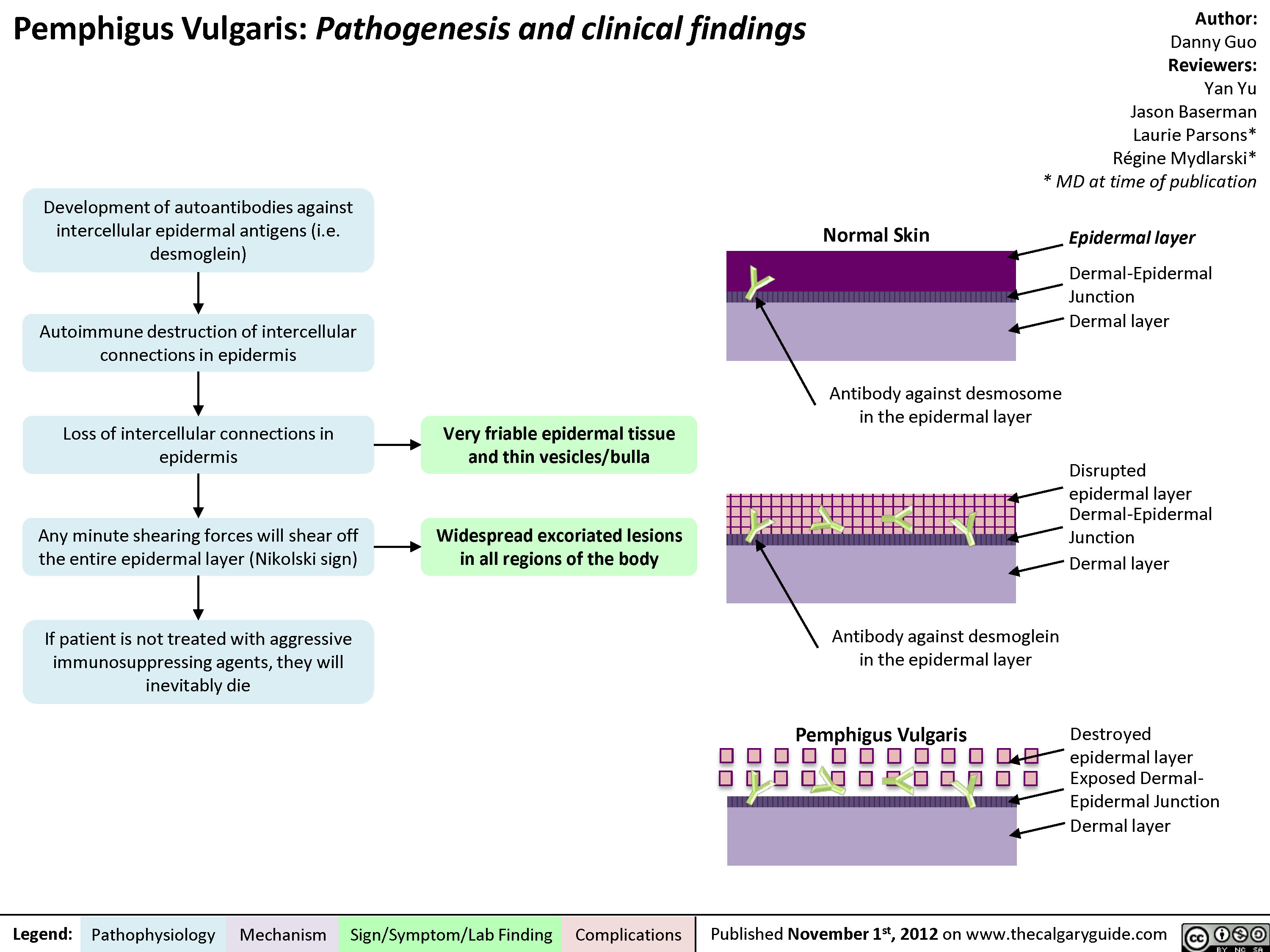
Pemphigus Vulgaris
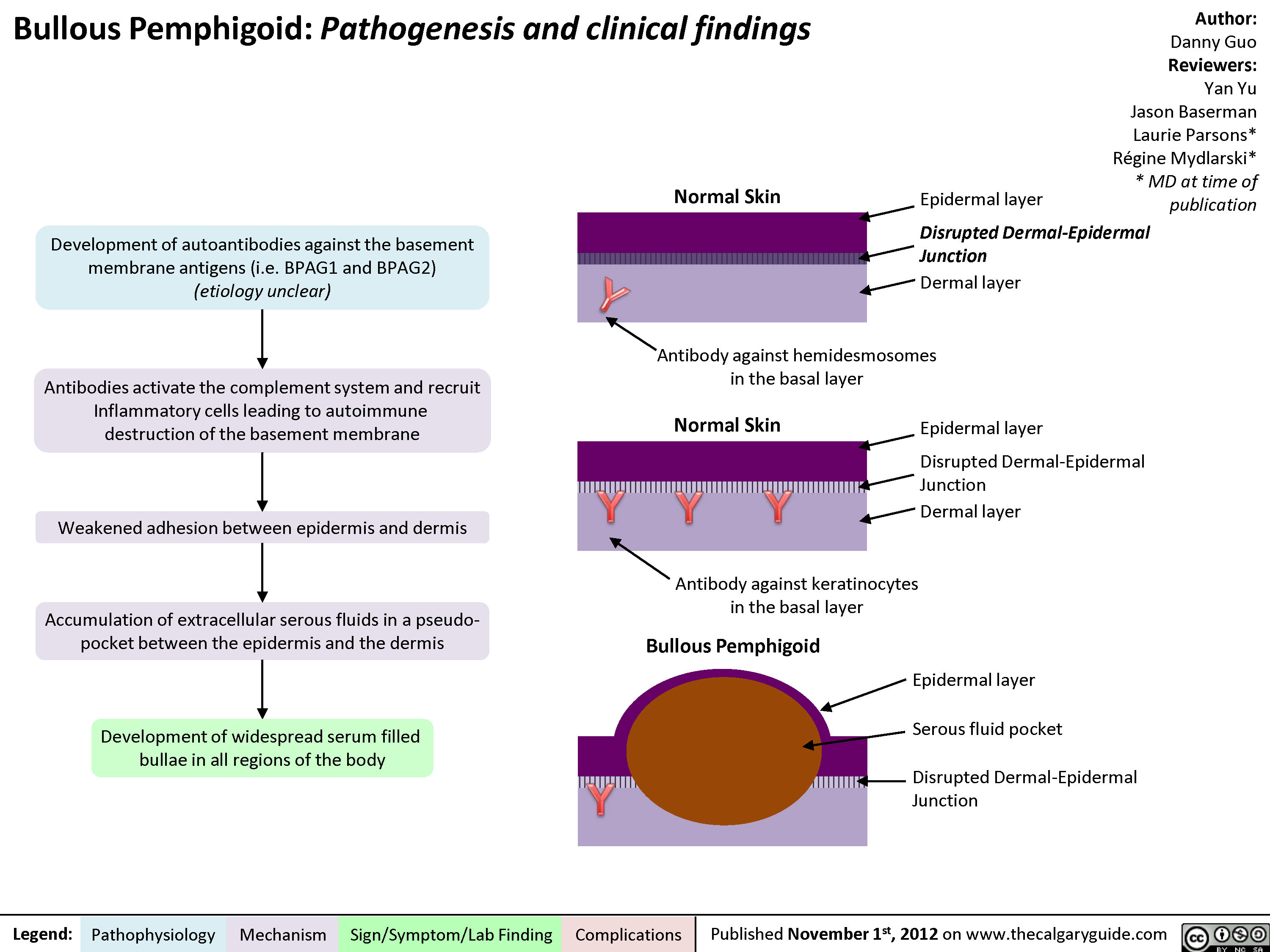
Bullous Pemphigoid
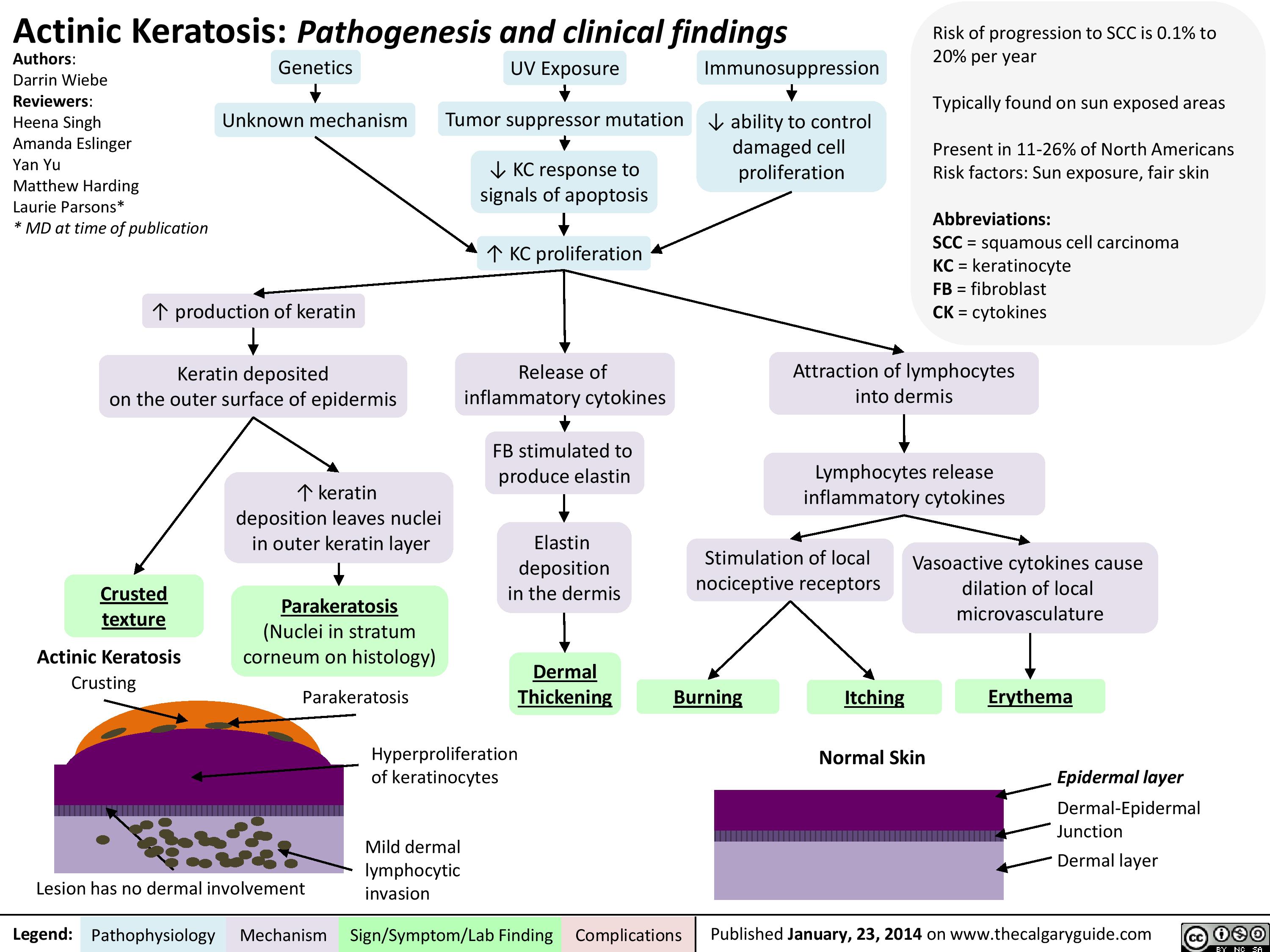
Actinic Keratosis
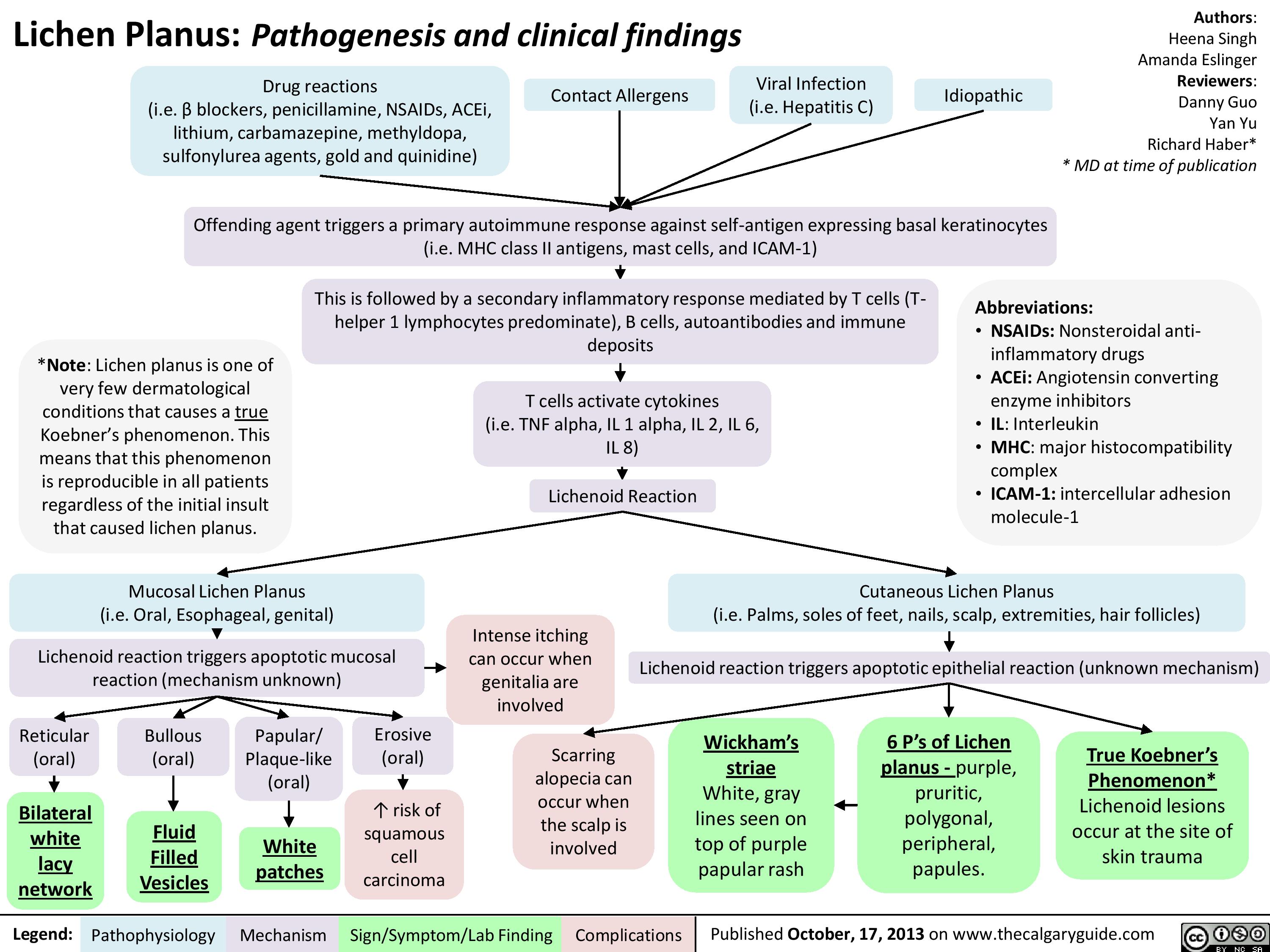
Lichen Planus
Herpes Simplex Virus (HSV)
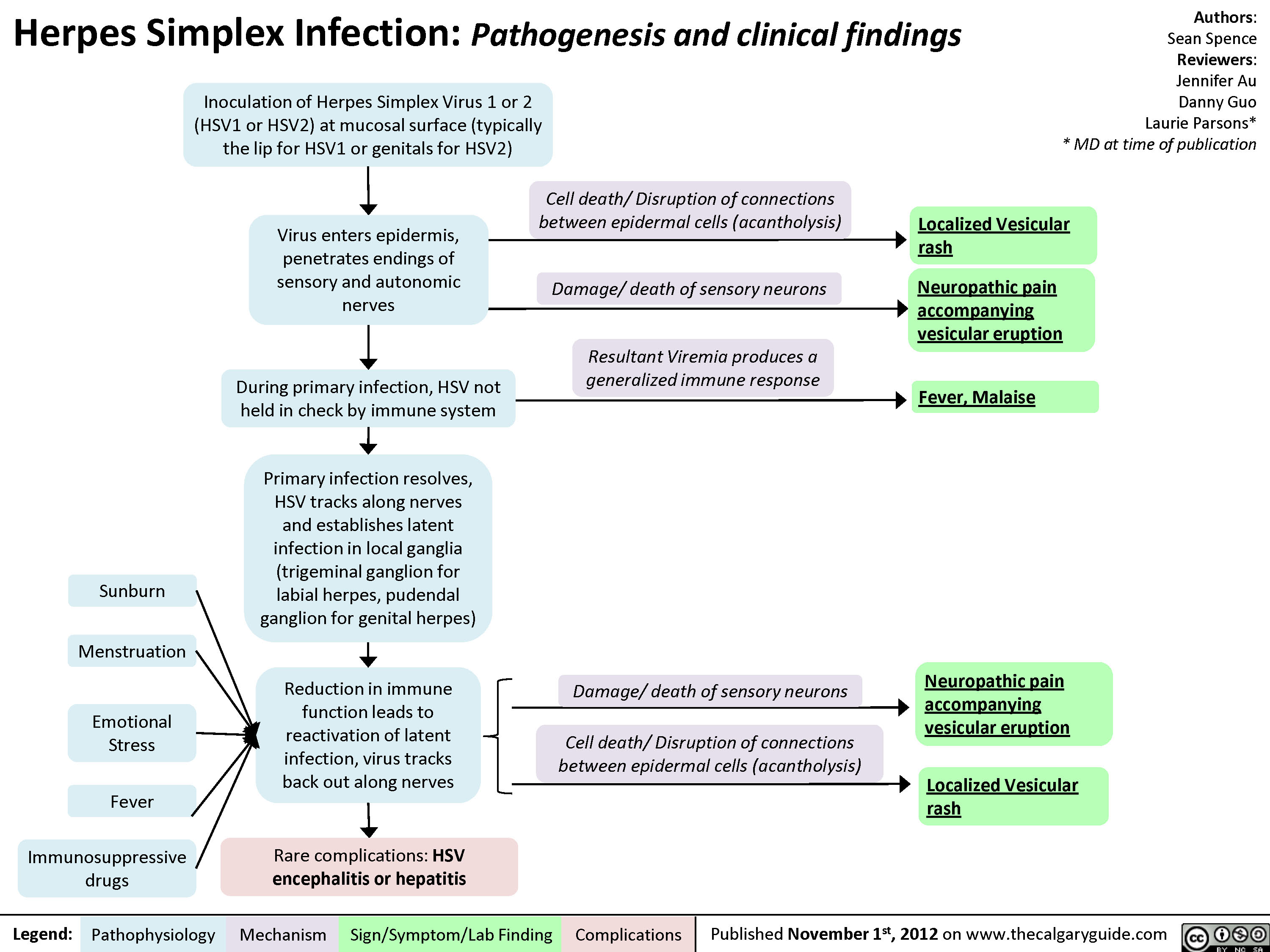
Herpes Simplex Virus (HSV)
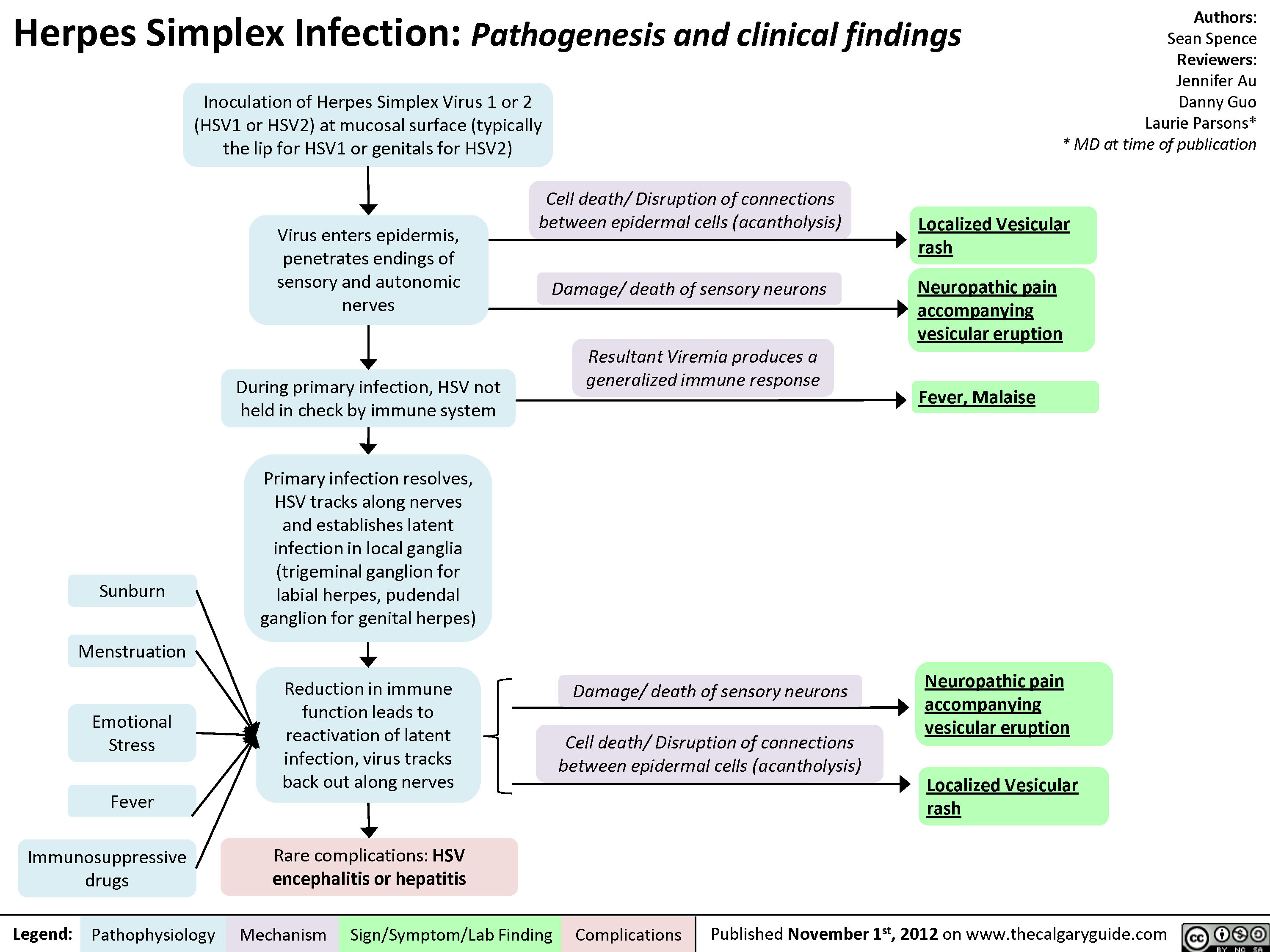
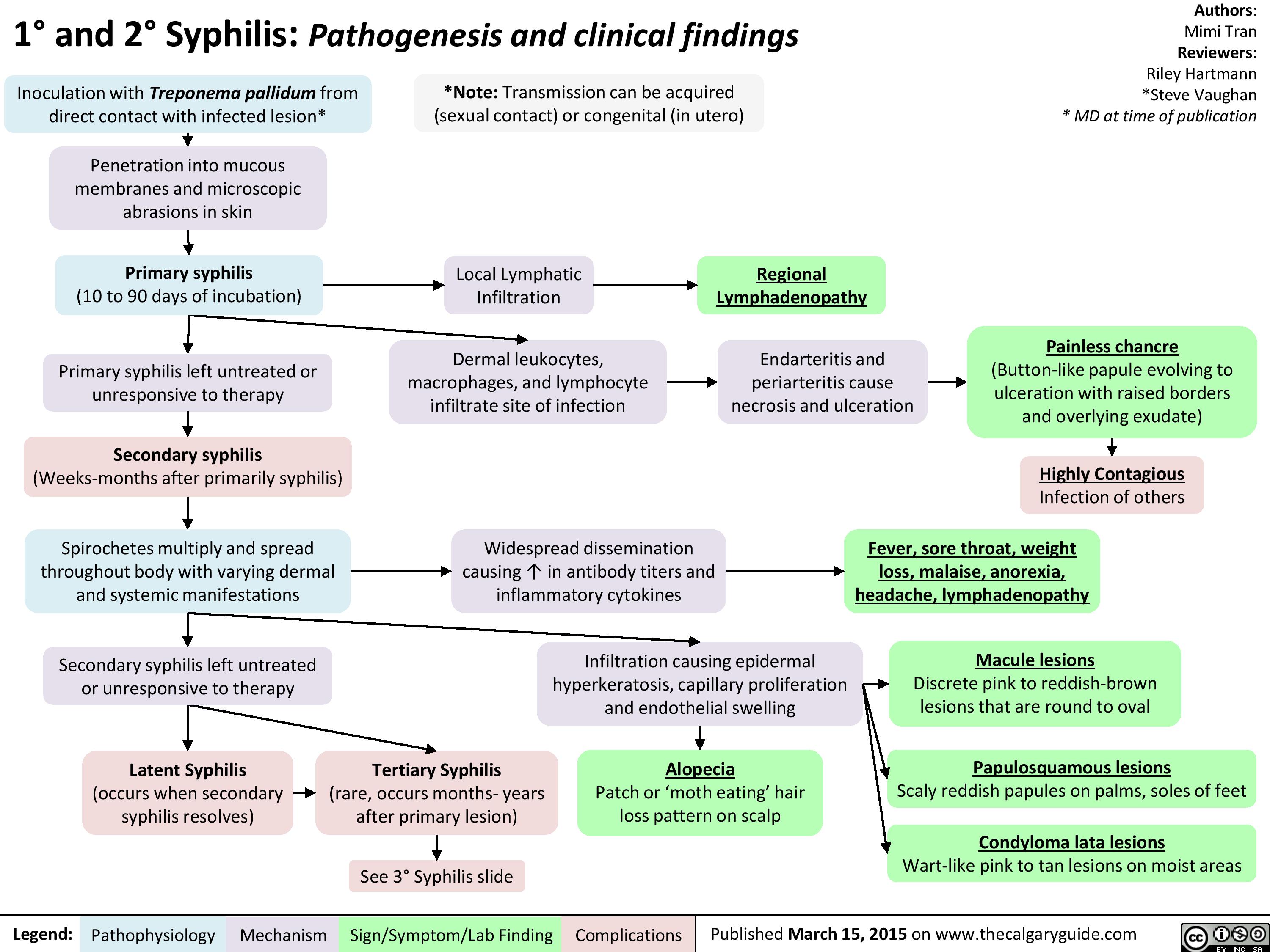
1-and-2-syphilis-pathogenesis-and-clinical-findings
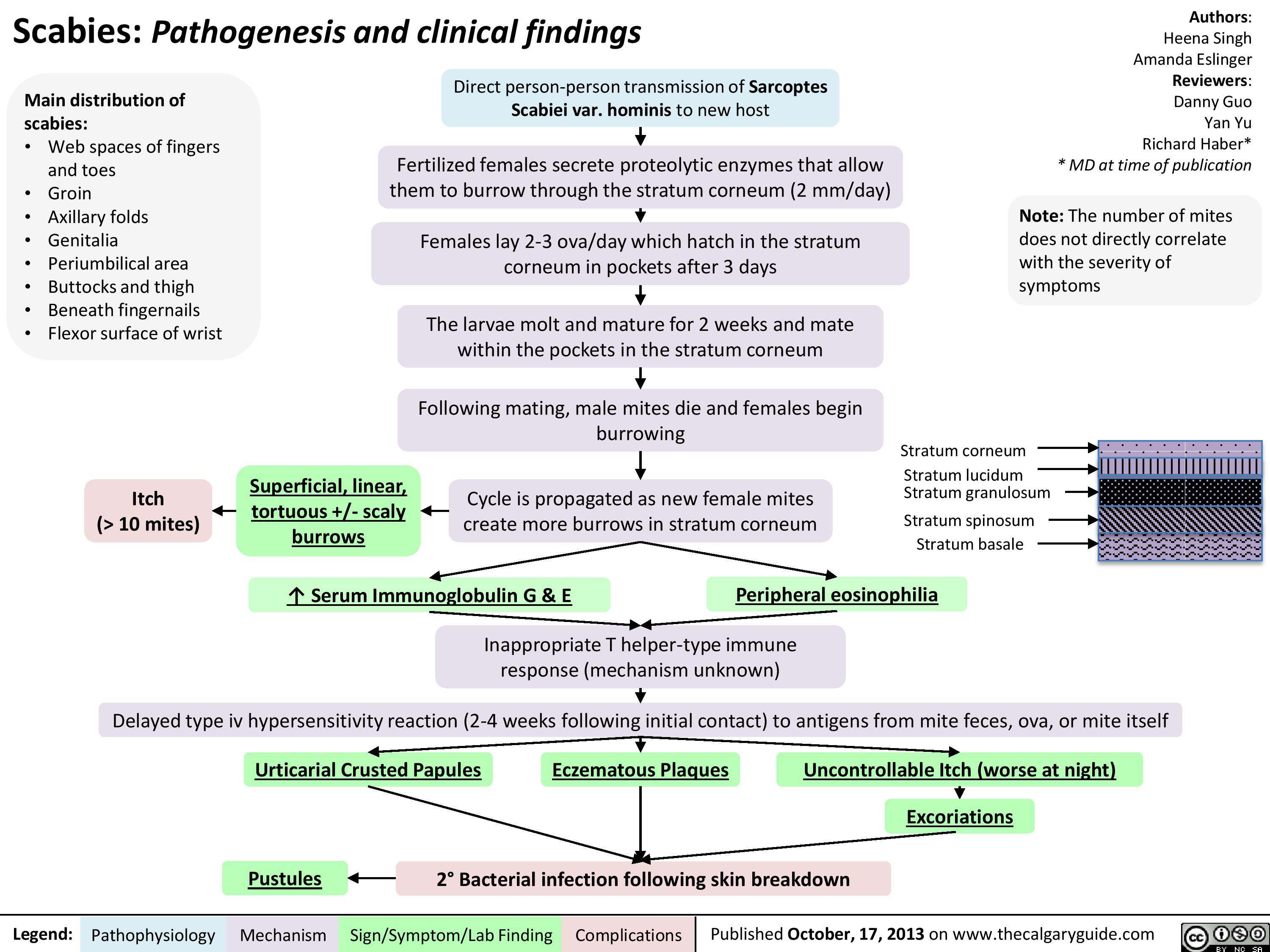
Scabies
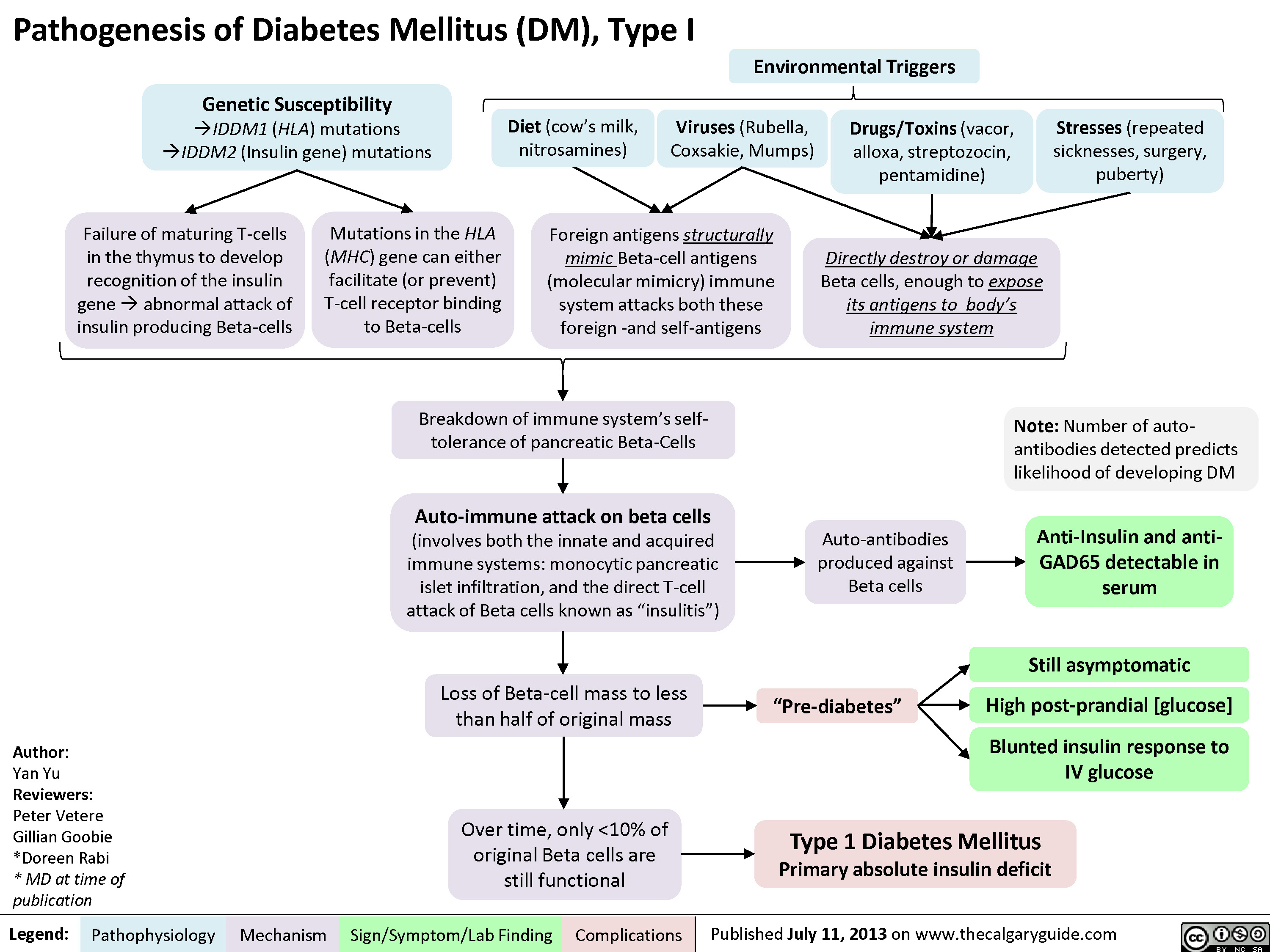
DM I pathogenesis
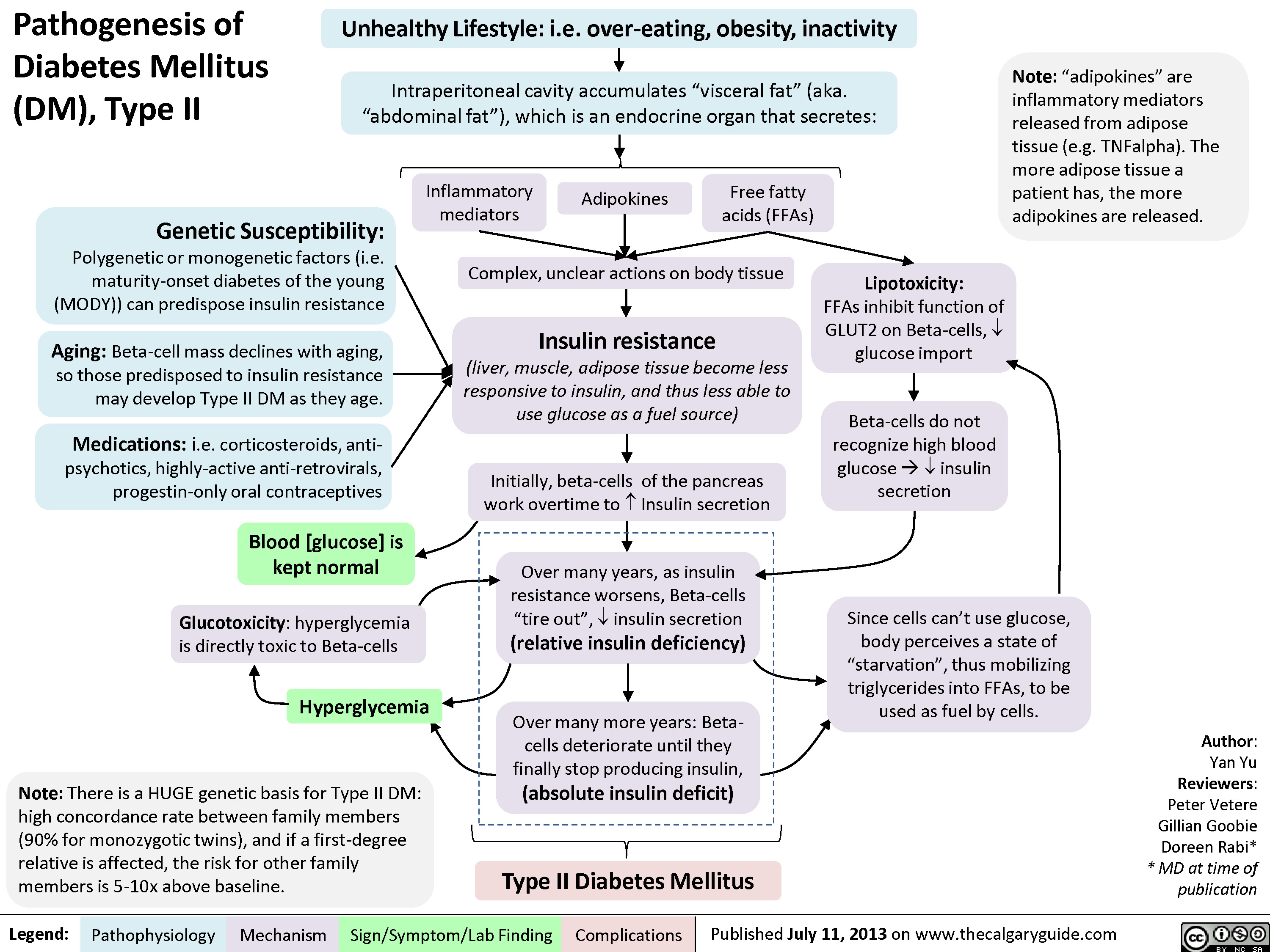
Pathogenesis of Diabetes mellitus DM), Type II
Diabetic Ketoacidosis

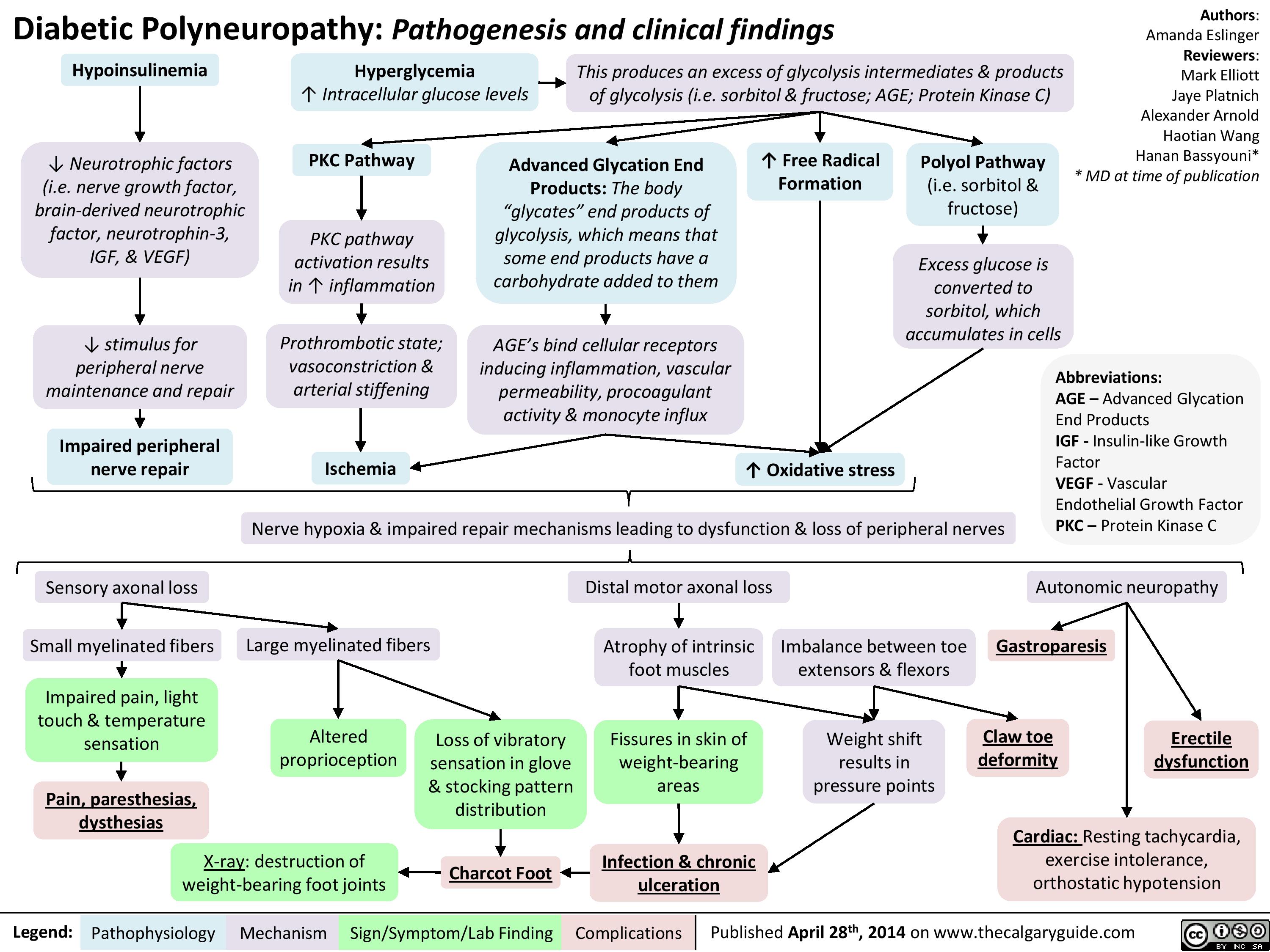
Diabetic Polyneuropathy
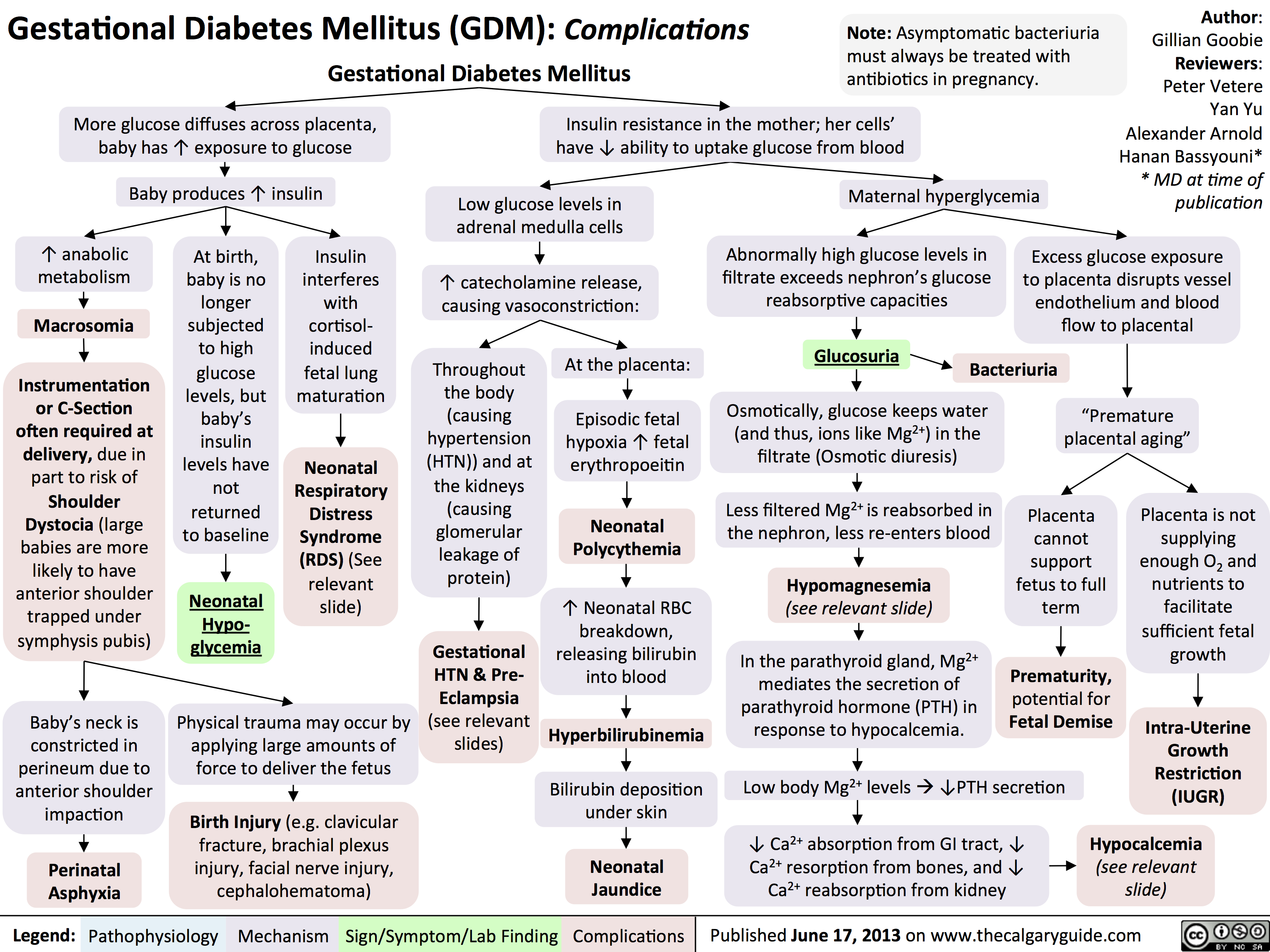
GDM Complications
Hypoglycemia - Pathogenesis

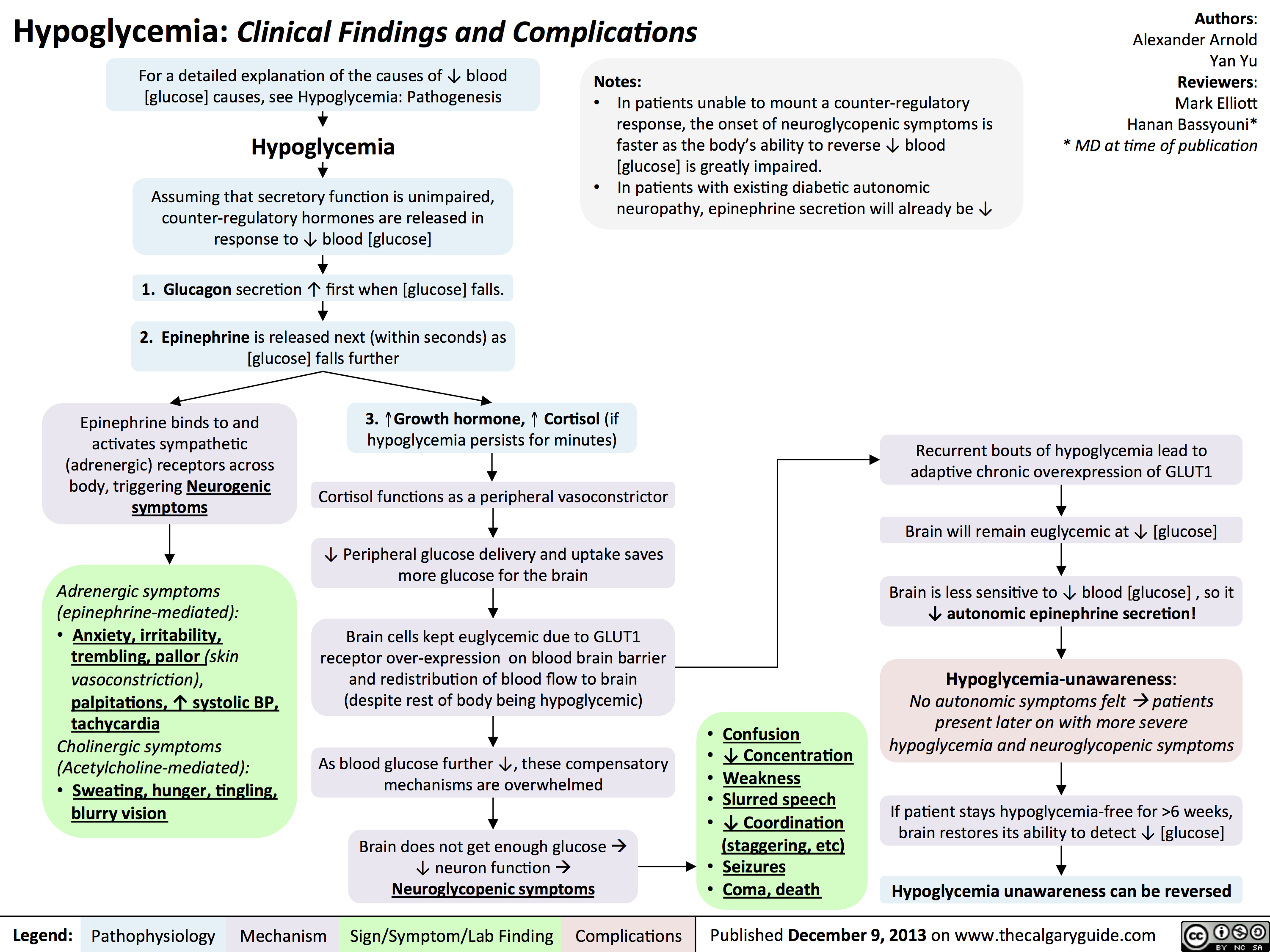
Hypoglycemia - Clinical Findings and Complications
Diabetic Hypoglycemia
![Yu, Yan - Diabetic Hypoglycemia - Clinical Findings - FINAL.pptx
? Epinephrine(Released within seconds as [glucose] falls further) Growth hormone, ? Cortisol (if hypoglycemia persists for minutes)Glucagon should ? when [glucose] falls. But here, glucagon release is inhibited by 1) diabetic auto-immune destruction of Alpha cells & 2) the high insulin.43210Plasma Glucose concentration (mmol/L)Liver should ? glycogenolysis & gluconeogenesisPeripheral vaso-constrictionPlasma [glucose] stays lowActivation of sympathetic (adrenergic) receptors across body, triggering Neurogenic symptomsPlasma [glucose] ?Excess subcutaneous insulin or insulin-secretagogue ?? [insulin] in the bloodOver time: [insulin] in the DM patient depends only on how much was injected or how much secretagogue was consumed; not on the body's physiological state.[Insulin] stays high in excessively-treated DM patientsPlasma [glucose] normally ?, but...High insulin transports plasma glucose into cells!In pts with existing diabetic autonomic neuropathy, epi-nephrine secretion will already be ?Brain does not get enough glucose, ? neuron function ? Neuroglycopenic symptomsTx: glucose intake![Glucose] returns to normalIf no glucose intake:Hypoglycemia-unawareness: No autonomic Sx felt so hypoglycemia not treated early ? pts present later on with more severe hypoglycemia and neuroglycopenic sxBrain cells kept chronically euglycemic due to GLUT1 receptor over-expression (despite rest of body being hypoglycemic)With many hypoglycemic events over time:Brain feels no need to ? glucose, so it ? autonomic epinephrine secretion!This is the normal sequence of hormone responses to ?ing plasma glucose levels.But this normal hormonal response will be blunted over time if there is 1) continued hypoglycemia dampening the sympathetic nervous system, and 2) long-standing diabetic neuropathy! (To be explained later in this flow chart)Abbreviations: [ ] = concentrationTx = TreatmentDM = Diabetes mellitusDiabetic Hypoglycemia: Pathogenesis and Clinical FindingsConfusionCan't concentrateWeaknessSlurred speech? coordination (staggering, etc)SeizuresComa, deathAdrenergic symptoms (epinephrine-mediated):Anxiety, irritability, trembling, pallor (skin vasoconstriction), palpitations, ? systolic BP, tachycardia Cholinergic symptoms(Acetylcholine-mediated):Sweating, hunger, tingling, blurry visionNote: In pts w/out DM, endogenous insulin secretion normally stops when blood [glucose] drops to <4mmol/LAuthor: Yan YuReviewers: Peter Vetere, Gillian Goobie, Hanan Bassyouni** MD at time of publicationLegend:Published June 14, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsMany hypoglycemic events over time blunt epinephrine secretion further.Hypoglycemia unawareness can be reversedIf pt stays hypoglycemia-free for >6 weeks, brain restores its ability to detect low glucose levels? peripheral glucose delivery and uptake (saving more glucose for the brain)Lack of glucagon effect reinforces hypoglycemia
124 kB / 361 words Yu, Yan - Diabetic Hypoglycemia - Clinical Findings - FINAL.pptx
? Epinephrine(Released within seconds as [glucose] falls further) Growth hormone, ? Cortisol (if hypoglycemia persists for minutes)Glucagon should ? when [glucose] falls. But here, glucagon release is inhibited by 1) diabetic auto-immune destruction of Alpha cells & 2) the high insulin.43210Plasma Glucose concentration (mmol/L)Liver should ? glycogenolysis & gluconeogenesisPeripheral vaso-constrictionPlasma [glucose] stays lowActivation of sympathetic (adrenergic) receptors across body, triggering Neurogenic symptomsPlasma [glucose] ?Excess subcutaneous insulin or insulin-secretagogue ?? [insulin] in the bloodOver time: [insulin] in the DM patient depends only on how much was injected or how much secretagogue was consumed; not on the body's physiological state.[Insulin] stays high in excessively-treated DM patientsPlasma [glucose] normally ?, but...High insulin transports plasma glucose into cells!In pts with existing diabetic autonomic neuropathy, epi-nephrine secretion will already be ?Brain does not get enough glucose, ? neuron function ? Neuroglycopenic symptomsTx: glucose intake![Glucose] returns to normalIf no glucose intake:Hypoglycemia-unawareness: No autonomic Sx felt so hypoglycemia not treated early ? pts present later on with more severe hypoglycemia and neuroglycopenic sxBrain cells kept chronically euglycemic due to GLUT1 receptor over-expression (despite rest of body being hypoglycemic)With many hypoglycemic events over time:Brain feels no need to ? glucose, so it ? autonomic epinephrine secretion!This is the normal sequence of hormone responses to ?ing plasma glucose levels.But this normal hormonal response will be blunted over time if there is 1) continued hypoglycemia dampening the sympathetic nervous system, and 2) long-standing diabetic neuropathy! (To be explained later in this flow chart)Abbreviations: [ ] = concentrationTx = TreatmentDM = Diabetes mellitusDiabetic Hypoglycemia: Pathogenesis and Clinical FindingsConfusionCan't concentrateWeaknessSlurred speech? coordination (staggering, etc)SeizuresComa, deathAdrenergic symptoms (epinephrine-mediated):Anxiety, irritability, trembling, pallor (skin vasoconstriction), palpitations, ? systolic BP, tachycardia Cholinergic symptoms(Acetylcholine-mediated):Sweating, hunger, tingling, blurry visionNote: In pts w/out DM, endogenous insulin secretion normally stops when blood [glucose] drops to <4mmol/LAuthor: Yan YuReviewers: Peter Vetere, Gillian Goobie, Hanan Bassyouni** MD at time of publicationLegend:Published June 14, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsMany hypoglycemic events over time blunt epinephrine secretion further.Hypoglycemia unawareness can be reversedIf pt stays hypoglycemia-free for >6 weeks, brain restores its ability to detect low glucose levels? peripheral glucose delivery and uptake (saving more glucose for the brain)Lack of glucagon effect reinforces hypoglycemia
124 kB / 361 words](http://calgaryguide.ucalgary.ca/wp-content/uploads/2015/05/Diabetic-Hypoglycemia-Clinical-Findings.jpg)
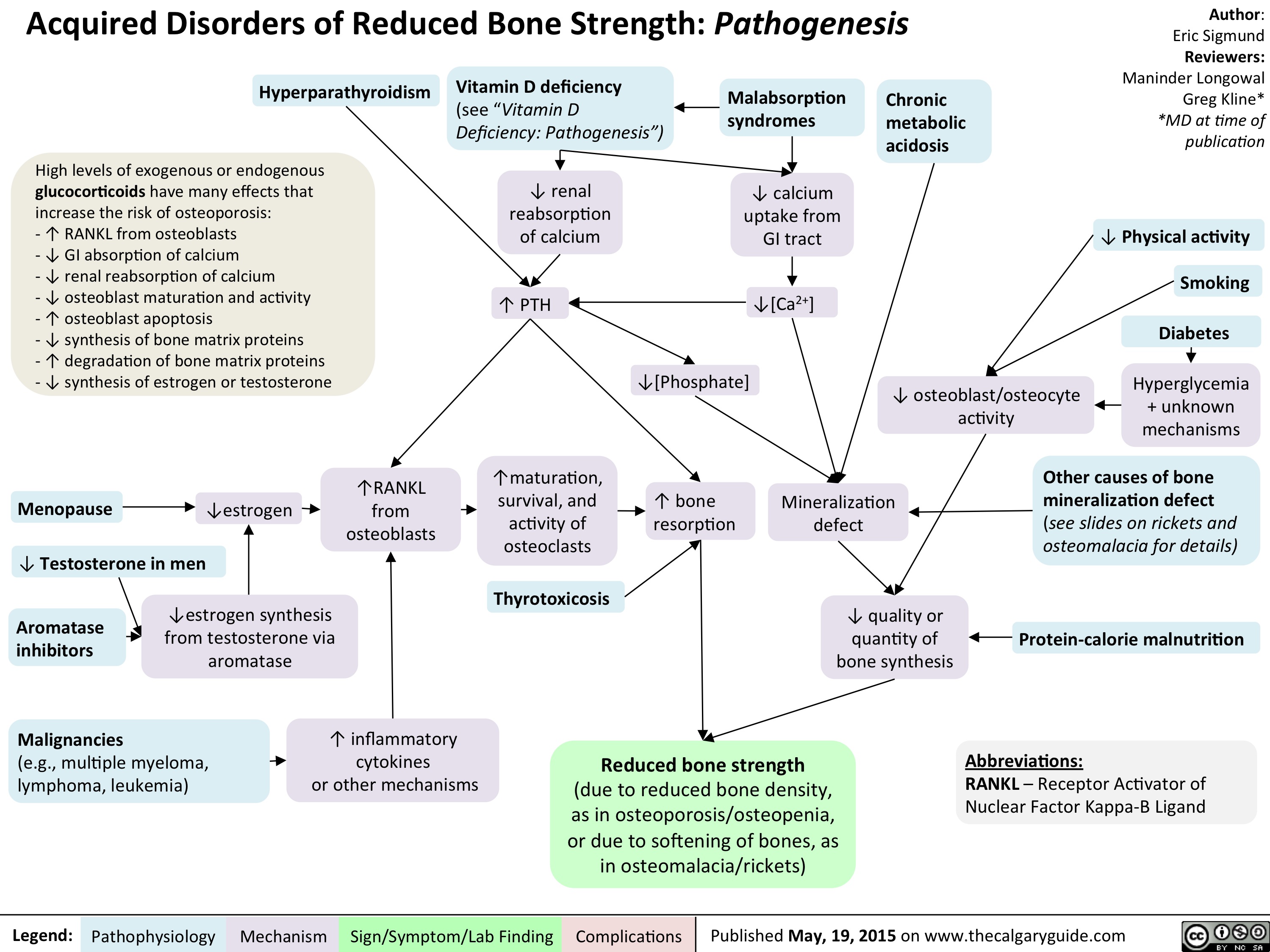
Acquired Disorders of Reduced Bone Strength - Pathogenesis
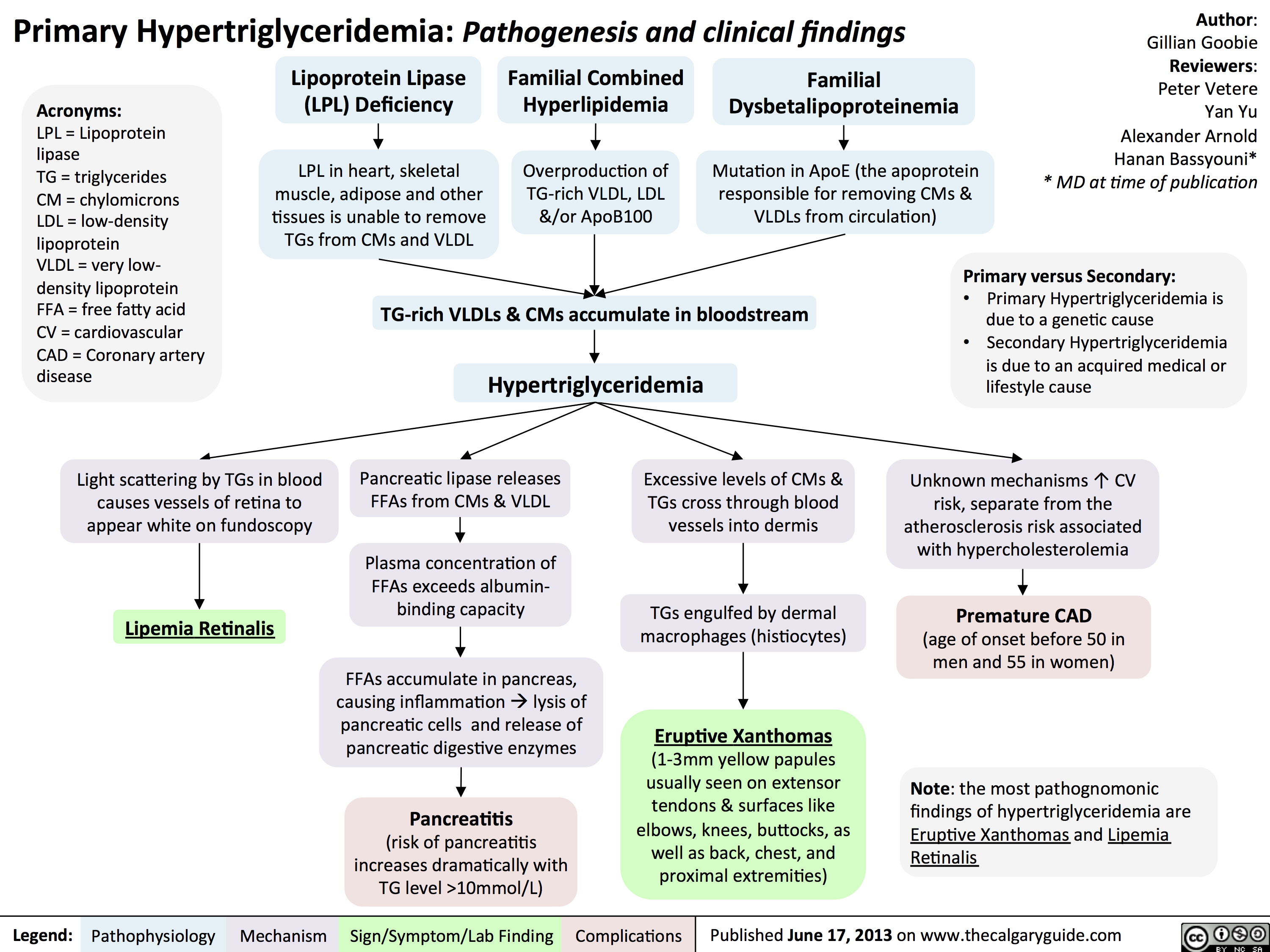
Primary Hypertriglyceridemia
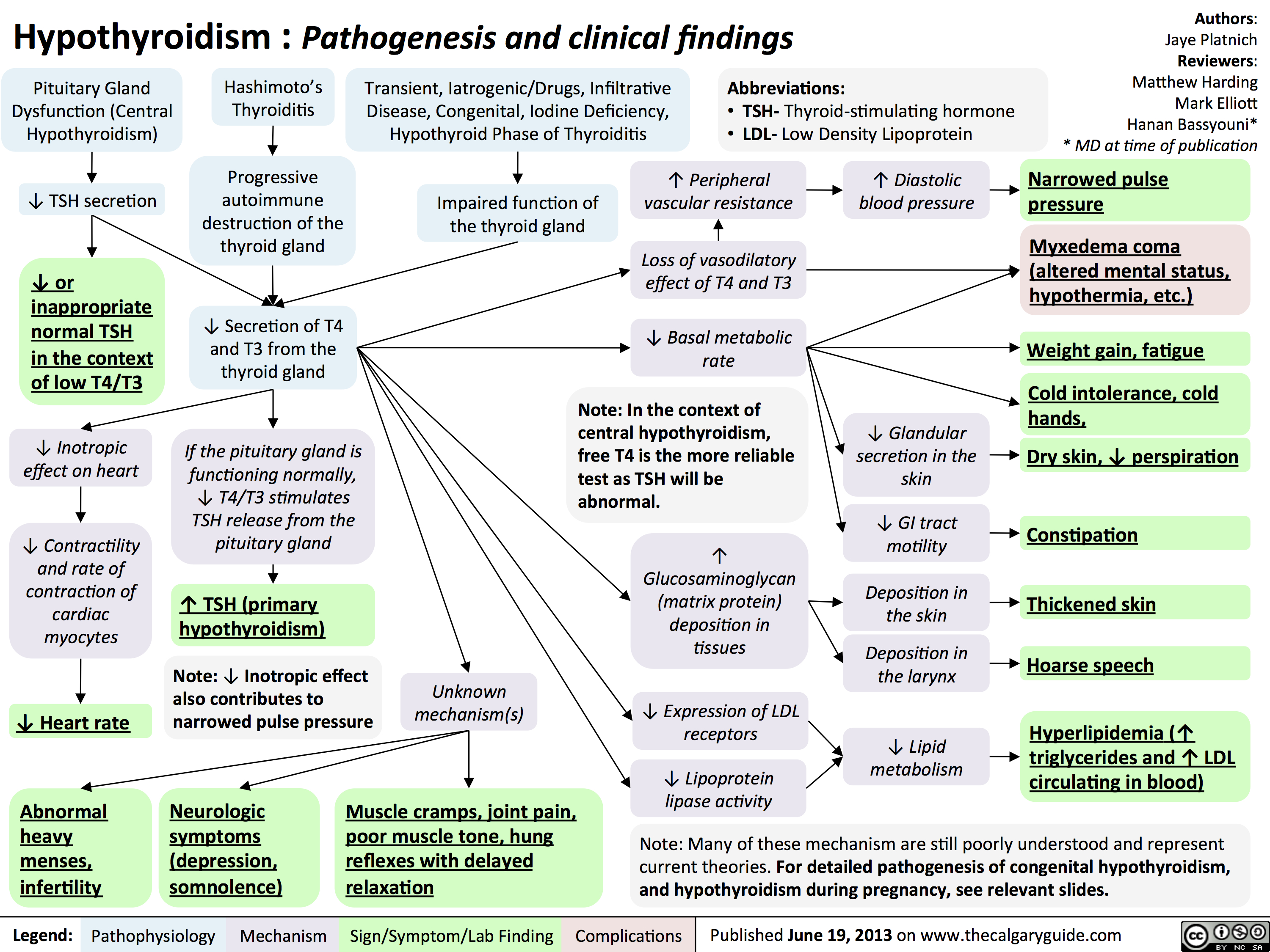
Hypothyroidism
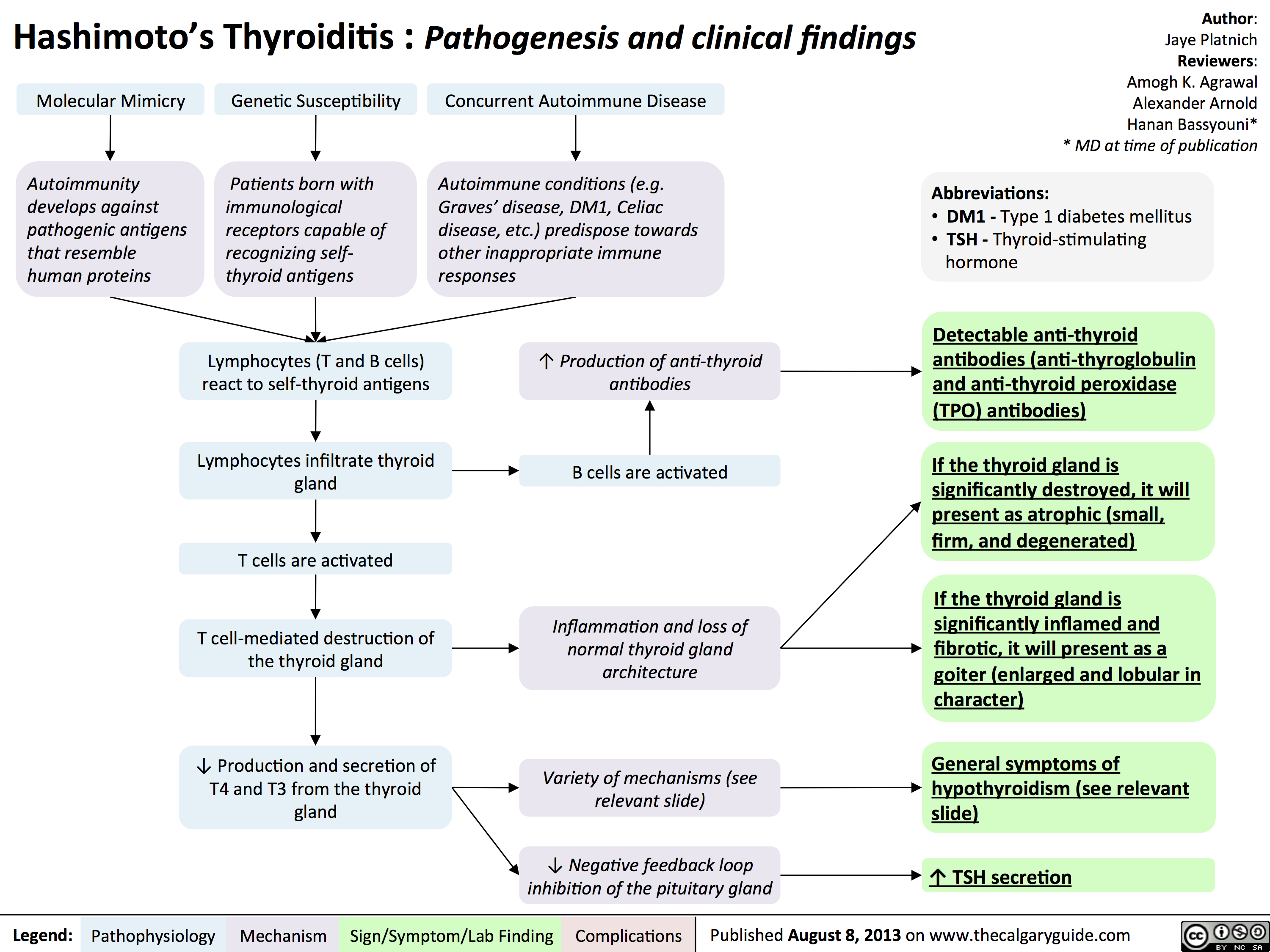
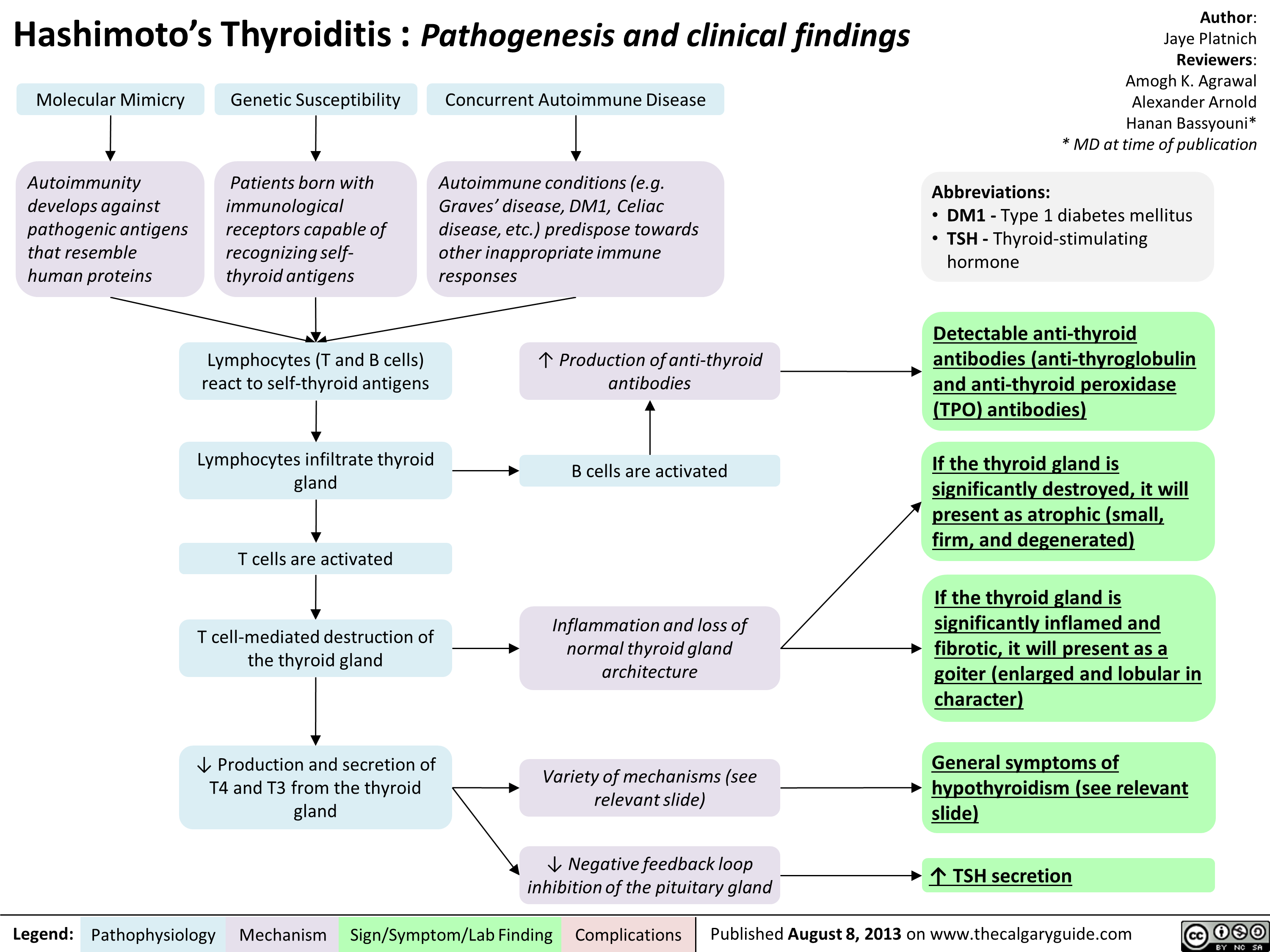
Hashimoto
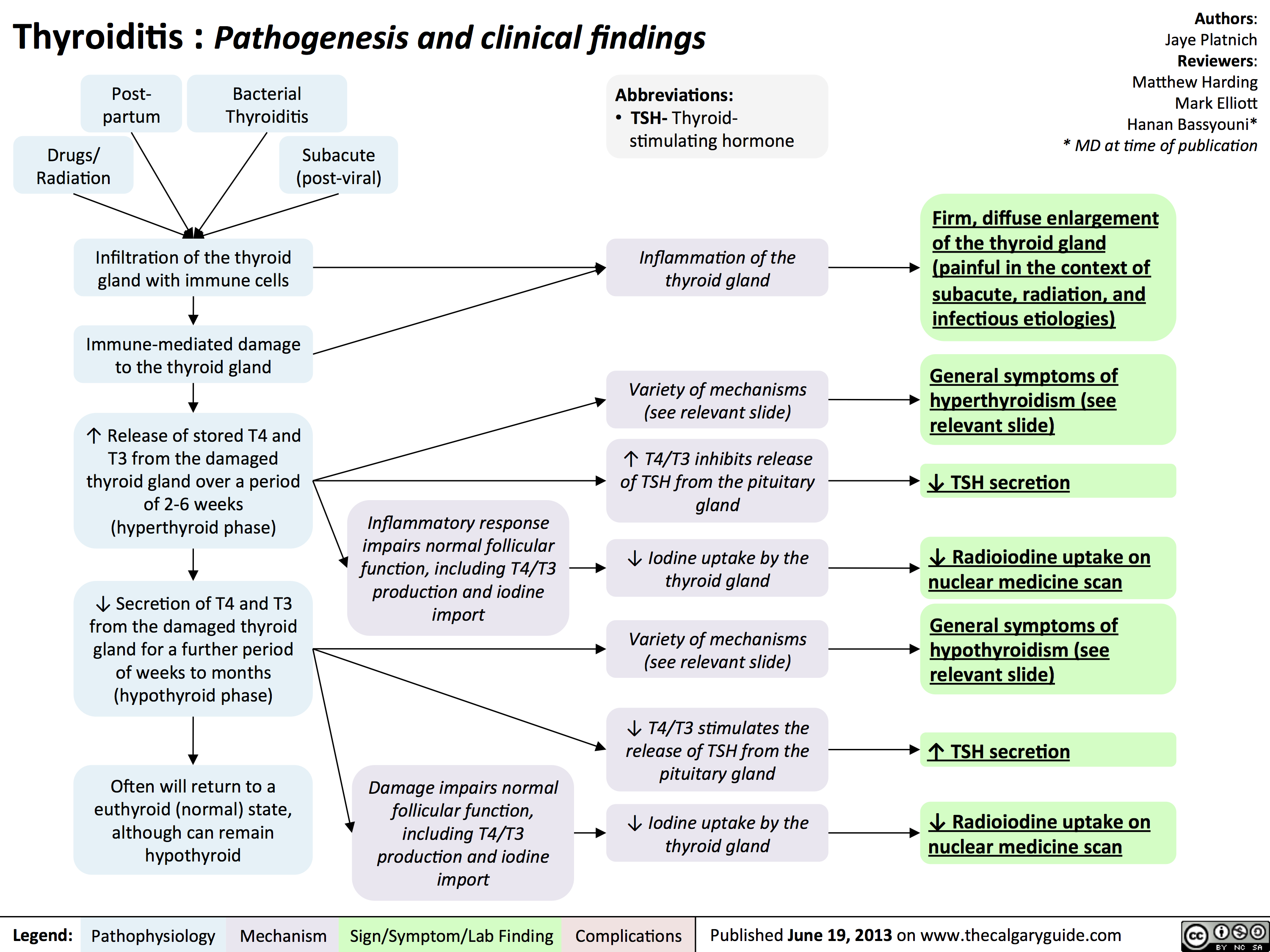
Thyroiditis
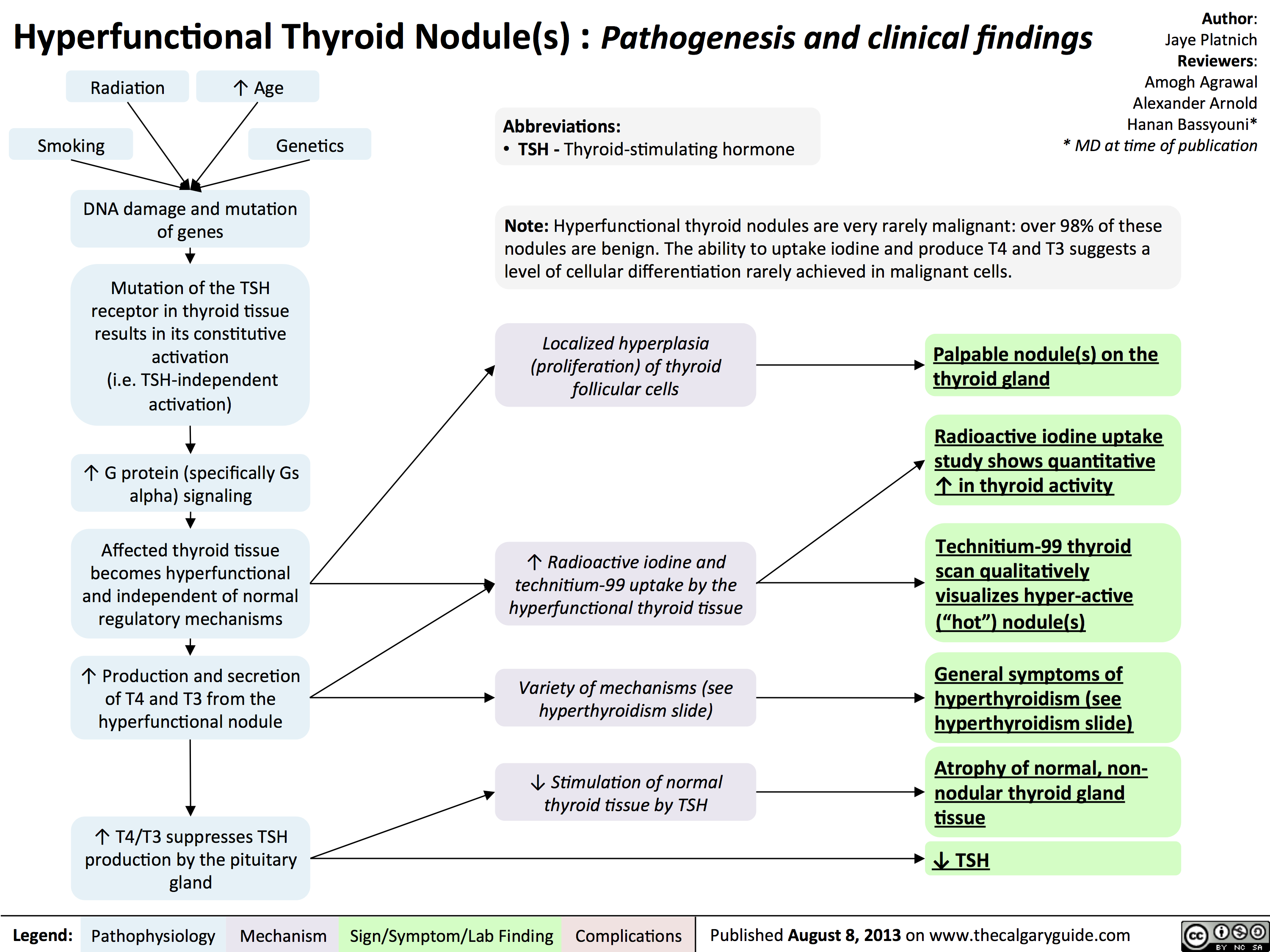
Hyperfunctional
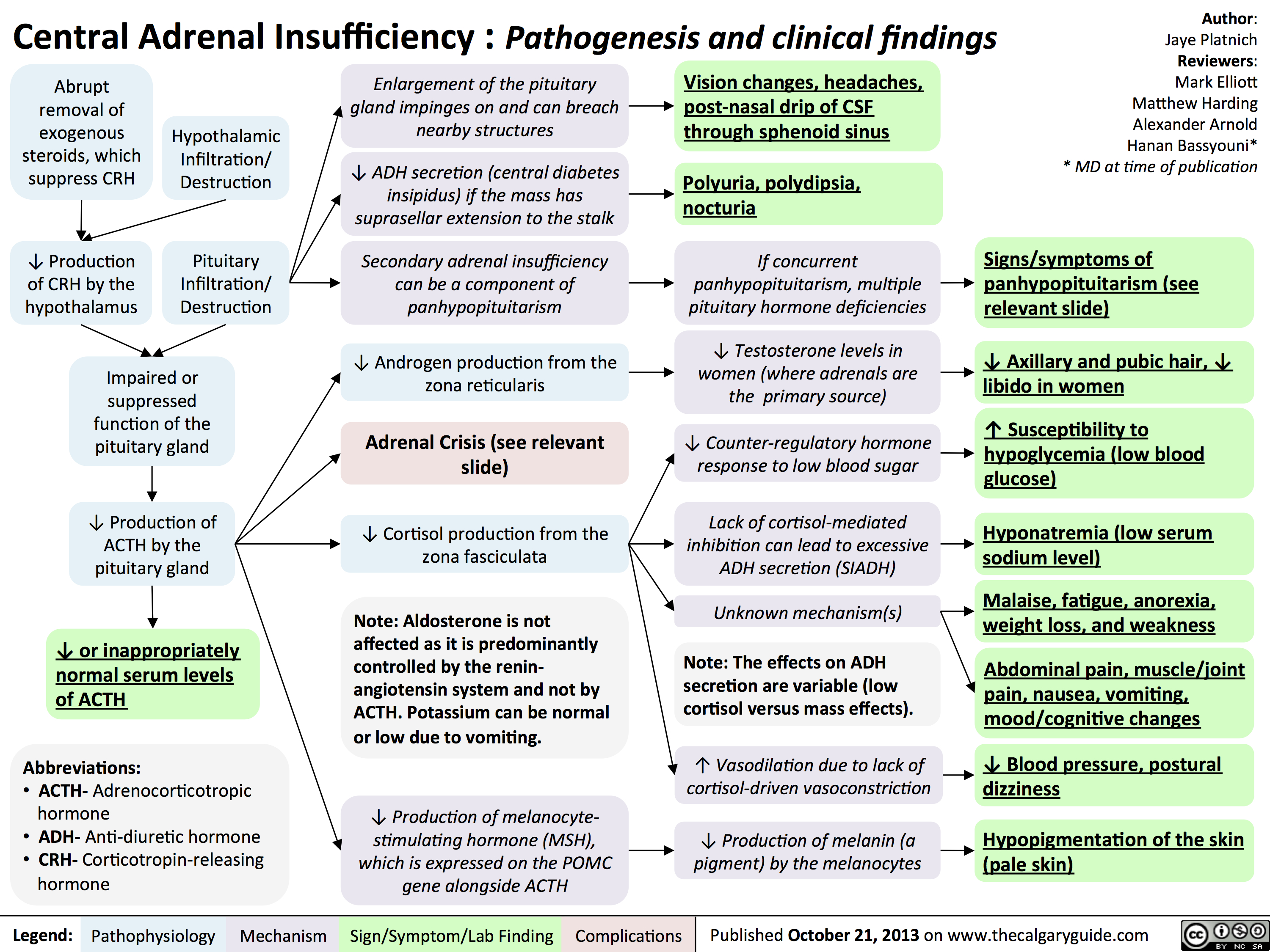
Central Adrenal Insufficiency - Pathogenesis and Clinical Findings
Clinical Findings of Androgen Deficiency
![Yu, Yan - Androgen Deficiency - FINAL.pptx
Hypogonadism in Males:Clinical Findings of Androgen Deficiency? secretion volume from seminal vesicle and prostateAuthor: Yan YuReviewers:Peter VetereGillian GoobieHanan Bassyouni** MD at time of publicationLegend:Published June 18, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplications? effect of testosterone on the brain? Libido(sensitive, but less specific)? [testosterone] : [estrogen] ratio at the male breast? ejaculate volume(a sensitive and specific sign)Gynecomastia (palpable breast tissue, not fat, directly under nipple)Fatigue,low mood, irrtabilityHot flashes, sweats(Can be nocturnal; occur only when hypogonadism is severe)Vasomotor neural response of unknown causeFewer spontaneous erections (i.e. in the morning)Lack of androgens (i.e. testosterone, DHT) in men past the age of pubertyIn advanced stages of the disease, after years of hypogonadism:(thus, less commonly seen)Low Bone Mass Density (BMD)Less testosterone to be converted into estrogen in bone? muscle bulk and strengthSmall, soft testicles(<4cm long on orchidometer)Lack of hormones to stimulate and maintain testicular hyperplasia/growthLoss of androgenic hair (on face, midline, and pubic area)Vertebral fracture (height loss), or other fragility fracturesIf sexual development is incomplete from puberty:Note: These clinical findings apply to many disorders, including:-Andropause-Hypopituitarism (suspect if other hormone abnormalities & Sx of mass lesion like visual field loss, diplopia, and headache exist)-Testicular Failure (if Hx of chemo, radiation, excess alcohol, and chronic liver disease)-Klinefelter's (if assoc. tall and eunuchoid stature, breast enlargement and cognitive deficiency - XXY)-Kallman's (if assoc. anosmia, and tall/eunuchoid stature)-Drugs (e.g. ketoconazole, anabolic steroids, spironolactone, digoxin, marijuana)Testosterone's inhibitory effect on estrogen is not enough to prevent breast growthDeficiency in testosterone during puberty delays fusion of epiphysesTall, eunuchoid statureNote: any disease involving an increase in aromatase activity (hyperthyroidism, cirrhosis, HCG-secreting tumors) will also cause relative estrogen excess & subsequent gynecomastia.
111 kB / 272 words Yu, Yan - Androgen Deficiency - FINAL.pptx
Hypogonadism in Males:Clinical Findings of Androgen Deficiency? secretion volume from seminal vesicle and prostateAuthor: Yan YuReviewers:Peter VetereGillian GoobieHanan Bassyouni** MD at time of publicationLegend:Published June 18, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplications? effect of testosterone on the brain? Libido(sensitive, but less specific)? [testosterone] : [estrogen] ratio at the male breast? ejaculate volume(a sensitive and specific sign)Gynecomastia (palpable breast tissue, not fat, directly under nipple)Fatigue,low mood, irrtabilityHot flashes, sweats(Can be nocturnal; occur only when hypogonadism is severe)Vasomotor neural response of unknown causeFewer spontaneous erections (i.e. in the morning)Lack of androgens (i.e. testosterone, DHT) in men past the age of pubertyIn advanced stages of the disease, after years of hypogonadism:(thus, less commonly seen)Low Bone Mass Density (BMD)Less testosterone to be converted into estrogen in bone? muscle bulk and strengthSmall, soft testicles(<4cm long on orchidometer)Lack of hormones to stimulate and maintain testicular hyperplasia/growthLoss of androgenic hair (on face, midline, and pubic area)Vertebral fracture (height loss), or other fragility fracturesIf sexual development is incomplete from puberty:Note: These clinical findings apply to many disorders, including:-Andropause-Hypopituitarism (suspect if other hormone abnormalities & Sx of mass lesion like visual field loss, diplopia, and headache exist)-Testicular Failure (if Hx of chemo, radiation, excess alcohol, and chronic liver disease)-Klinefelter's (if assoc. tall and eunuchoid stature, breast enlargement and cognitive deficiency - XXY)-Kallman's (if assoc. anosmia, and tall/eunuchoid stature)-Drugs (e.g. ketoconazole, anabolic steroids, spironolactone, digoxin, marijuana)Testosterone's inhibitory effect on estrogen is not enough to prevent breast growthDeficiency in testosterone during puberty delays fusion of epiphysesTall, eunuchoid statureNote: any disease involving an increase in aromatase activity (hyperthyroidism, cirrhosis, HCG-secreting tumors) will also cause relative estrogen excess & subsequent gynecomastia.
111 kB / 272 words](http://calgaryguide.ucalgary.ca/wp-content/uploads/2015/05/Clinical-Findings-of-Androgen-Deficiency.jpg)
Hypocalcemia - Clinical Findings
![Yu, Yan - Hypocalcemia - Clinical Findings - FINAL.pptx
Hypocalcemia: Clinical FindingsAuthor: Yan YuReviewers:David WaldnerSean SpenceGreg Kline** MD at time of publicationLegend:Published May 7, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsHypocalcemia(serum [Ca2+] <2.1mmol/L)Altered sensory ability of peripheral nervesLess Ca2+ outside cells, with no change in + charges inside cellsPeripheral paraesthesia? Neuronal Yu, Yan - Hypocalcemia - Clinical Findings - FINAL.pptx
Hypocalcemia: Clinical FindingsAuthor: Yan YuReviewers:David WaldnerSean SpenceGreg Kline** MD at time of publicationLegend:Published May 7, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsHypocalcemia(serum [Ca2+] <2.1mmol/L)Altered sensory ability of peripheral nervesLess Ca2+ outside cells, with no change in + charges inside cellsPeripheral paraesthesia? Neuronal](http://calgaryguide.ucalgary.ca/wp-content/uploads/2015/05/Hypocalcemia-Clinical-Findings.jpg)
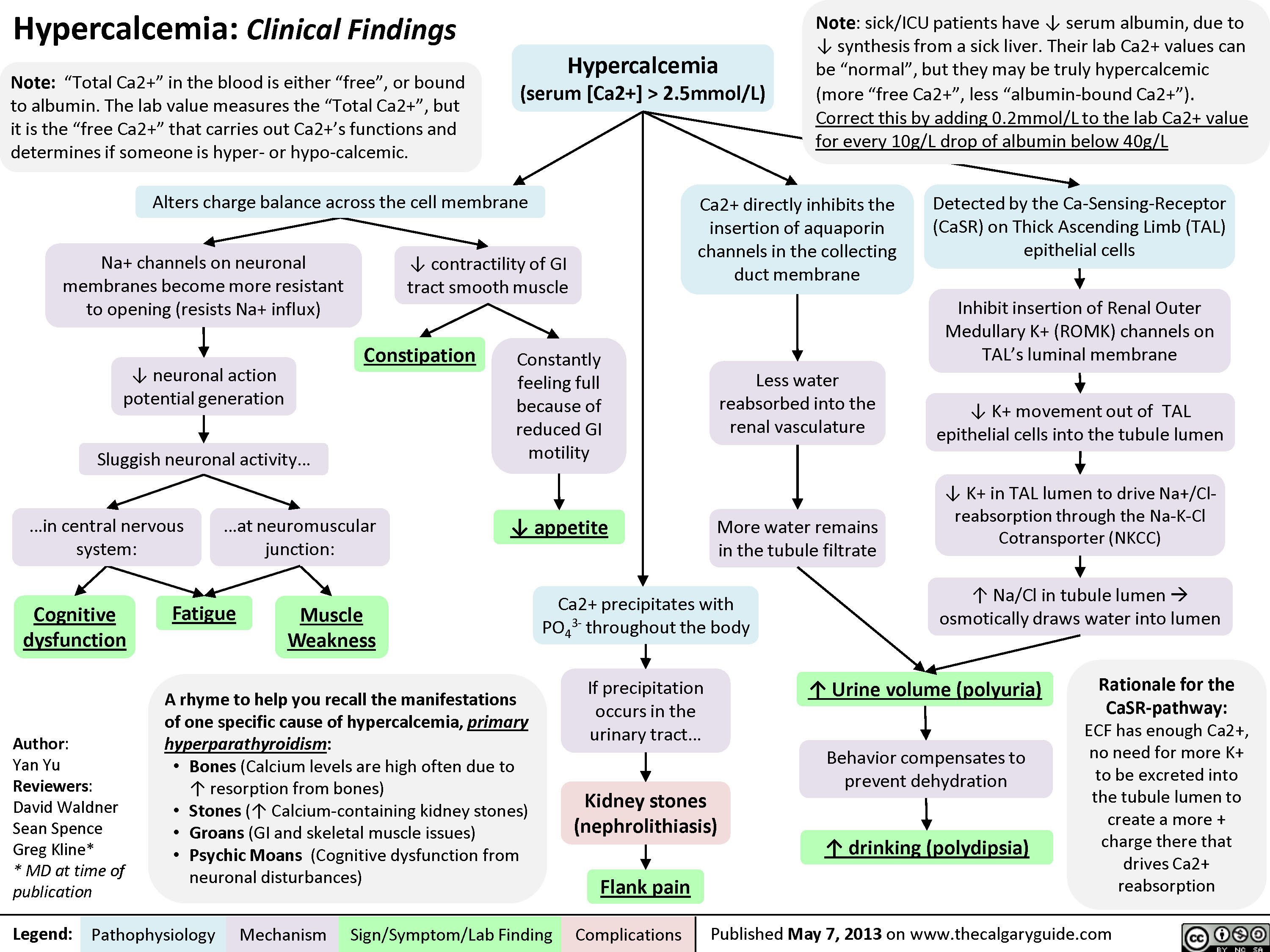
Hypercalcemia - Clinical Findings
![Yu, Yan - Hypercalcemia - Clinical Findings - FINAL.pptx
Hypercalcemia: Clinical FindingsAuthor: Yan YuReviewers:David WaldnerSean SpenceGreg Kline** MD at time of publicationLegend:Published May 7, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsHypercalcemia(serum [Ca2+] > 2.5mmol/L)Na+ channels on neuronal membranes become more resistant to opening (resists Na+ influx)Cognitive dysfunctionIf precipitation occurs in the urinary tract...Fatigue? contractility of GI tract smooth muscle? K+ movement out of TAL epithelial cells into the tubule lumen Alters charge balance across the cell membraneCa2+ precipitates with PO43- throughout the bodyDetected by the Ca-Sensing-Receptor (CaSR) on Thick Ascending Limb (TAL) epithelial cells? neuronal action potential generationSluggish neuronal activity...? appetiteConstipationFlank painInhibit insertion of Renal Outer Medullary K+ (ROMK) channels on TAL's luminal membrane? K+ in TAL lumen to drive Na+/Cl- reabsorption through the Na-K-Cl Cotransporter (NKCC)? Na/Cl in tubule lumen ? osmotically draws water into lumen? drinking (polydipsia)? Urine volume (polyuria)Rationale for the CaSR-pathway: ECF has enough Ca2+, no need for more K+ to be excreted into the tubule lumen to create a more + charge there that drives Ca2+ reabsorptionBehavior compensates to prevent dehydrationKidney stones (nephrolithiasis)Constantly feeling full because of reduced GI motilityCa2+ directly inhibits the insertion of aquaporin channels in the collecting duct membraneLess water reabsorbed into the renal vasculatureMore water remains in the tubule filtrateMuscle Weakness...in central nervous system:...at neuromuscular junction:A rhyme to help you recall the manifestations of one specific cause of hypercalcemia, primary hyperparathyroidism:Bones (Calcium levels are high often due to ? resorption from bones)Stones (? Calcium-containing kidney stones)Groans (GI and skeletal muscle issues) Psychic Moans (Cognitive dysfunction from neuronal disturbances)Note: sick/ICU patients have ? serum albumin, due to ? synthesis from a sick liver. Their lab Ca2+ values can be Yu, Yan - Hypercalcemia - Clinical Findings - FINAL.pptx
Hypercalcemia: Clinical FindingsAuthor: Yan YuReviewers:David WaldnerSean SpenceGreg Kline** MD at time of publicationLegend:Published May 7, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsHypercalcemia(serum [Ca2+] > 2.5mmol/L)Na+ channels on neuronal membranes become more resistant to opening (resists Na+ influx)Cognitive dysfunctionIf precipitation occurs in the urinary tract...Fatigue? contractility of GI tract smooth muscle? K+ movement out of TAL epithelial cells into the tubule lumen Alters charge balance across the cell membraneCa2+ precipitates with PO43- throughout the bodyDetected by the Ca-Sensing-Receptor (CaSR) on Thick Ascending Limb (TAL) epithelial cells? neuronal action potential generationSluggish neuronal activity...? appetiteConstipationFlank painInhibit insertion of Renal Outer Medullary K+ (ROMK) channels on TAL's luminal membrane? K+ in TAL lumen to drive Na+/Cl- reabsorption through the Na-K-Cl Cotransporter (NKCC)? Na/Cl in tubule lumen ? osmotically draws water into lumen? drinking (polydipsia)? Urine volume (polyuria)Rationale for the CaSR-pathway: ECF has enough Ca2+, no need for more K+ to be excreted into the tubule lumen to create a more + charge there that drives Ca2+ reabsorptionBehavior compensates to prevent dehydrationKidney stones (nephrolithiasis)Constantly feeling full because of reduced GI motilityCa2+ directly inhibits the insertion of aquaporin channels in the collecting duct membraneLess water reabsorbed into the renal vasculatureMore water remains in the tubule filtrateMuscle Weakness...in central nervous system:...at neuromuscular junction:A rhyme to help you recall the manifestations of one specific cause of hypercalcemia, primary hyperparathyroidism:Bones (Calcium levels are high often due to ? resorption from bones)Stones (? Calcium-containing kidney stones)Groans (GI and skeletal muscle issues) Psychic Moans (Cognitive dysfunction from neuronal disturbances)Note: sick/ICU patients have ? serum albumin, due to ? synthesis from a sick liver. Their lab Ca2+ values can be](http://calgaryguide.ucalgary.ca/wp-content/uploads/2015/05/Hypercalcemia-Clinical-Findings.jpg)
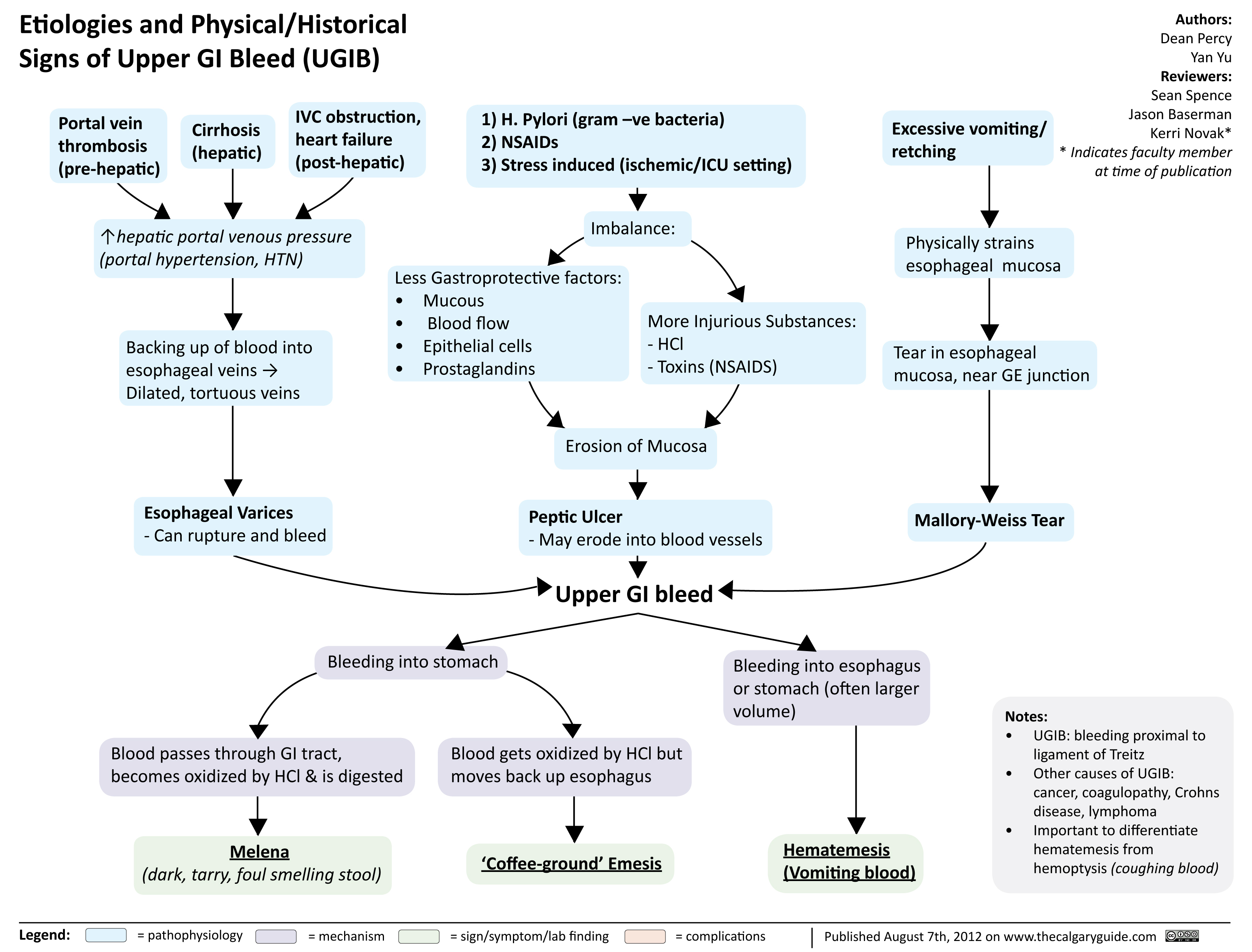
Etiologies and Physical Historical Signs of Upper GI Bleed
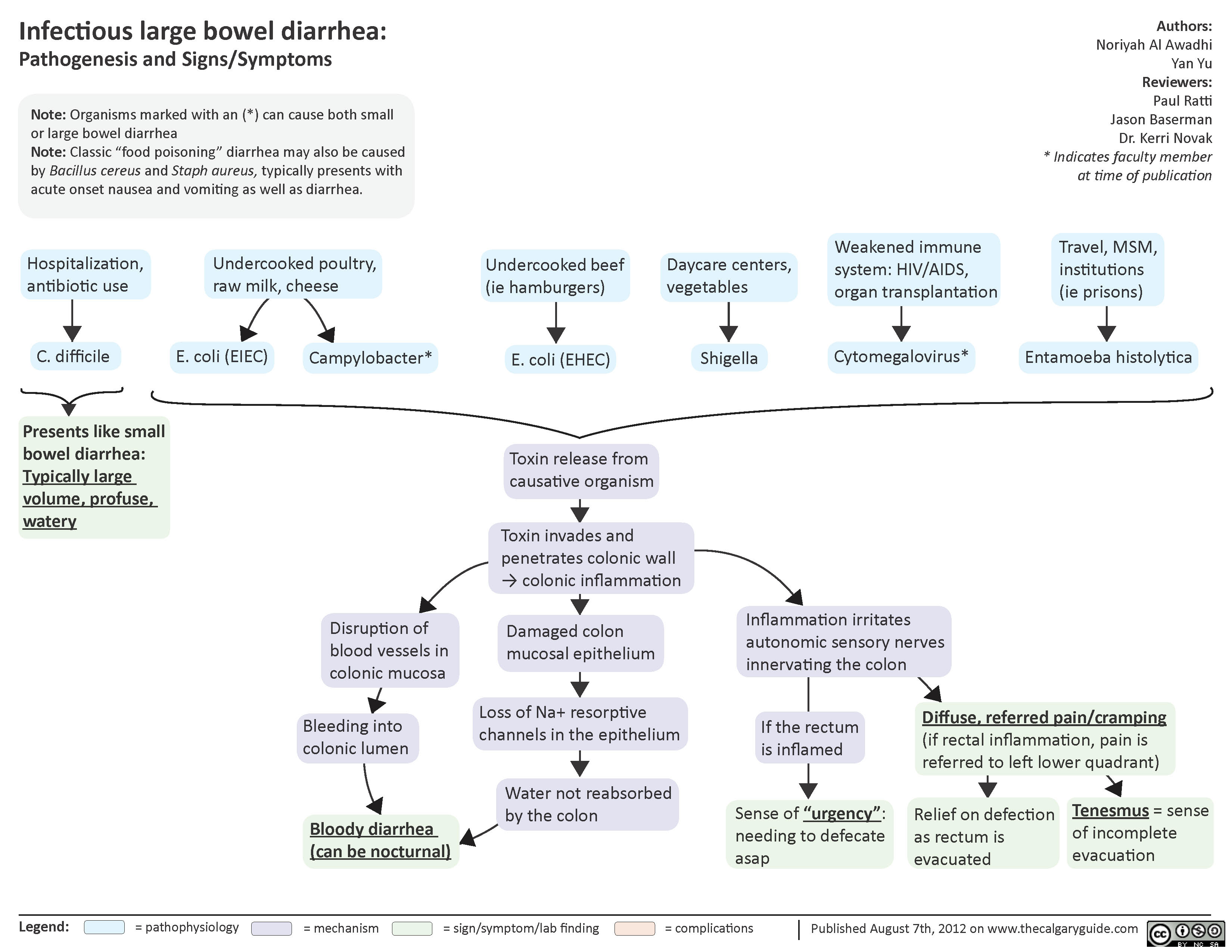
Infectious Large Bowel Diarrhea
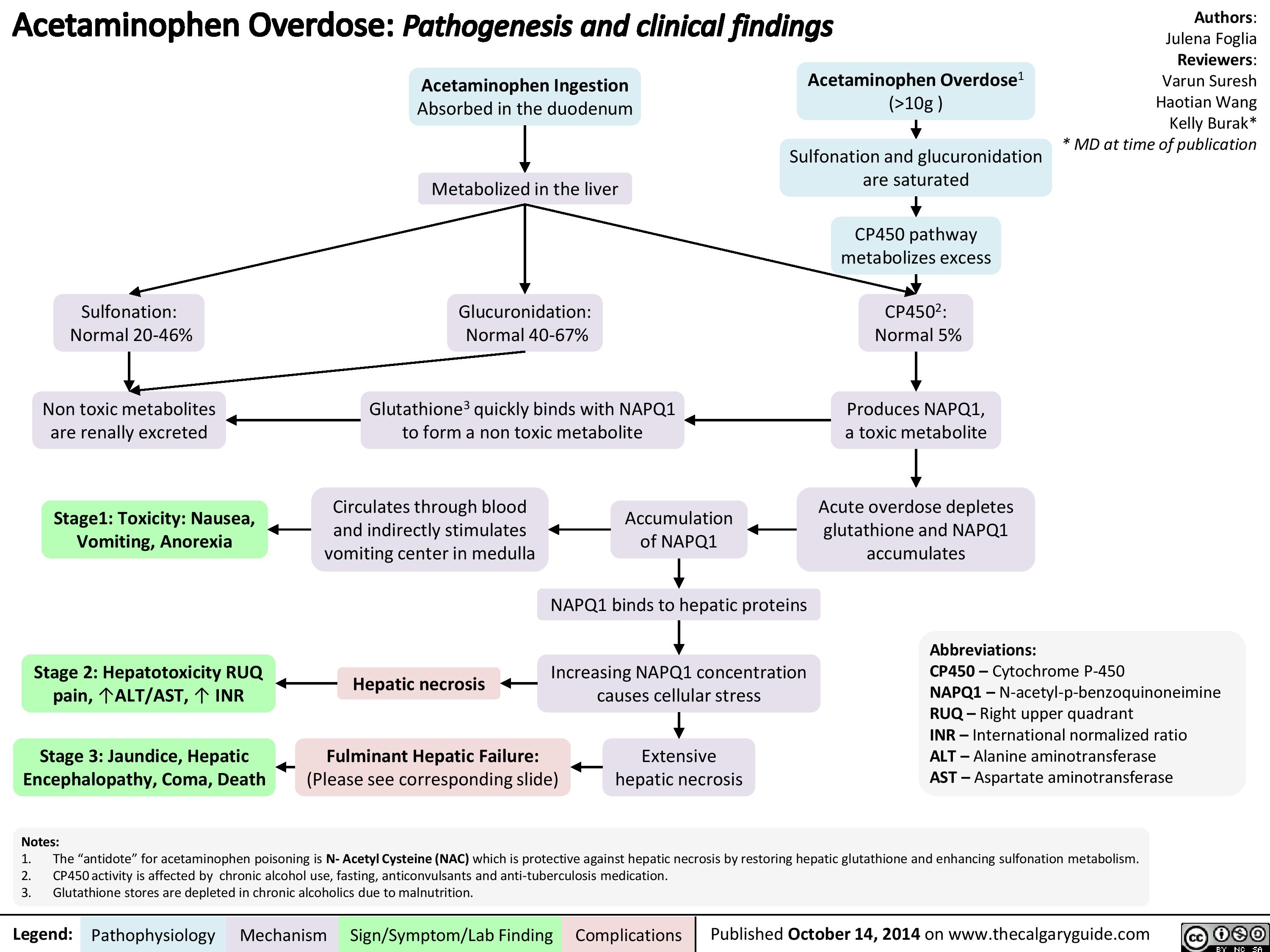
Acetaminophen Overdose
Gall Bladder Disorders
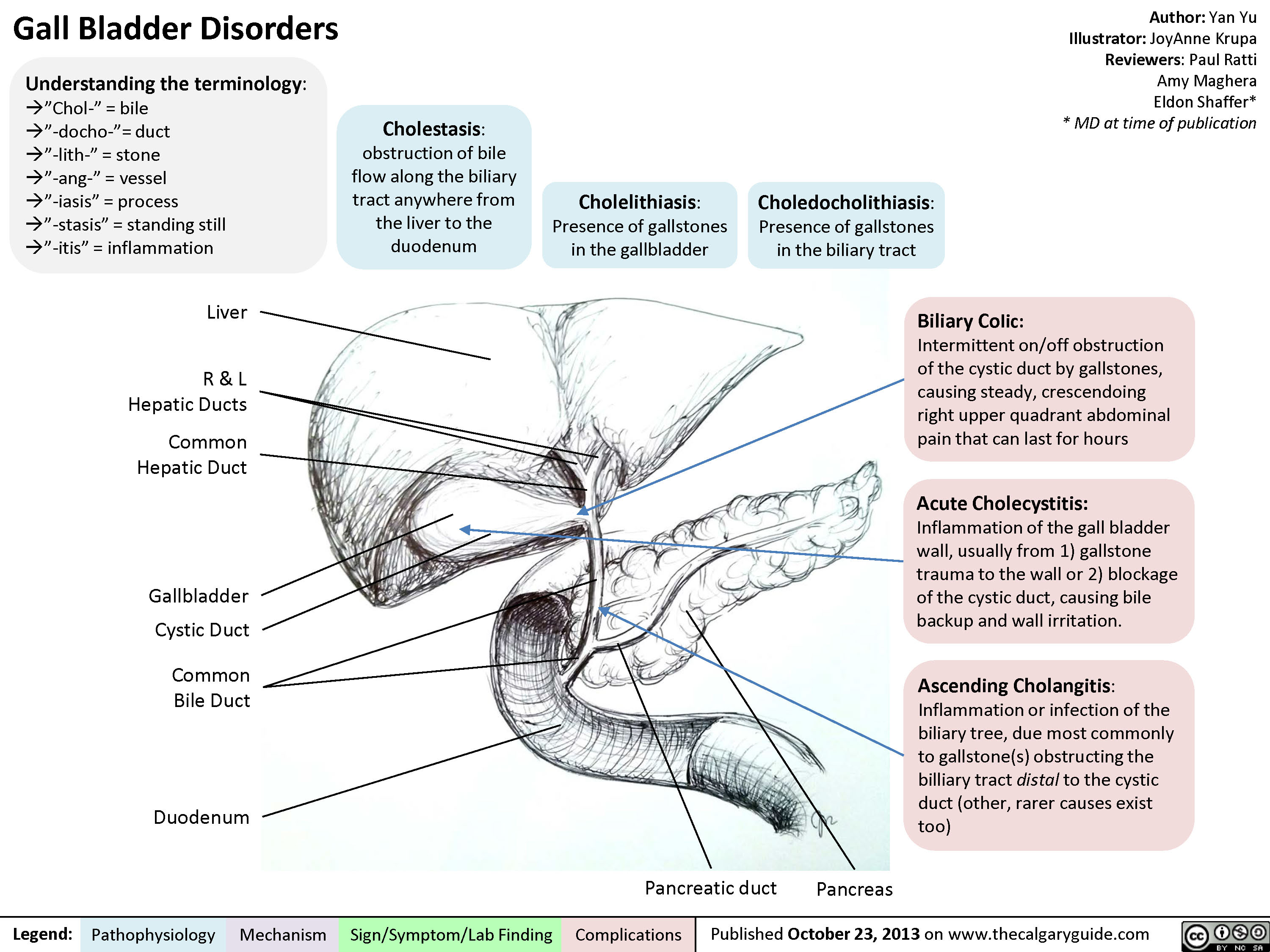
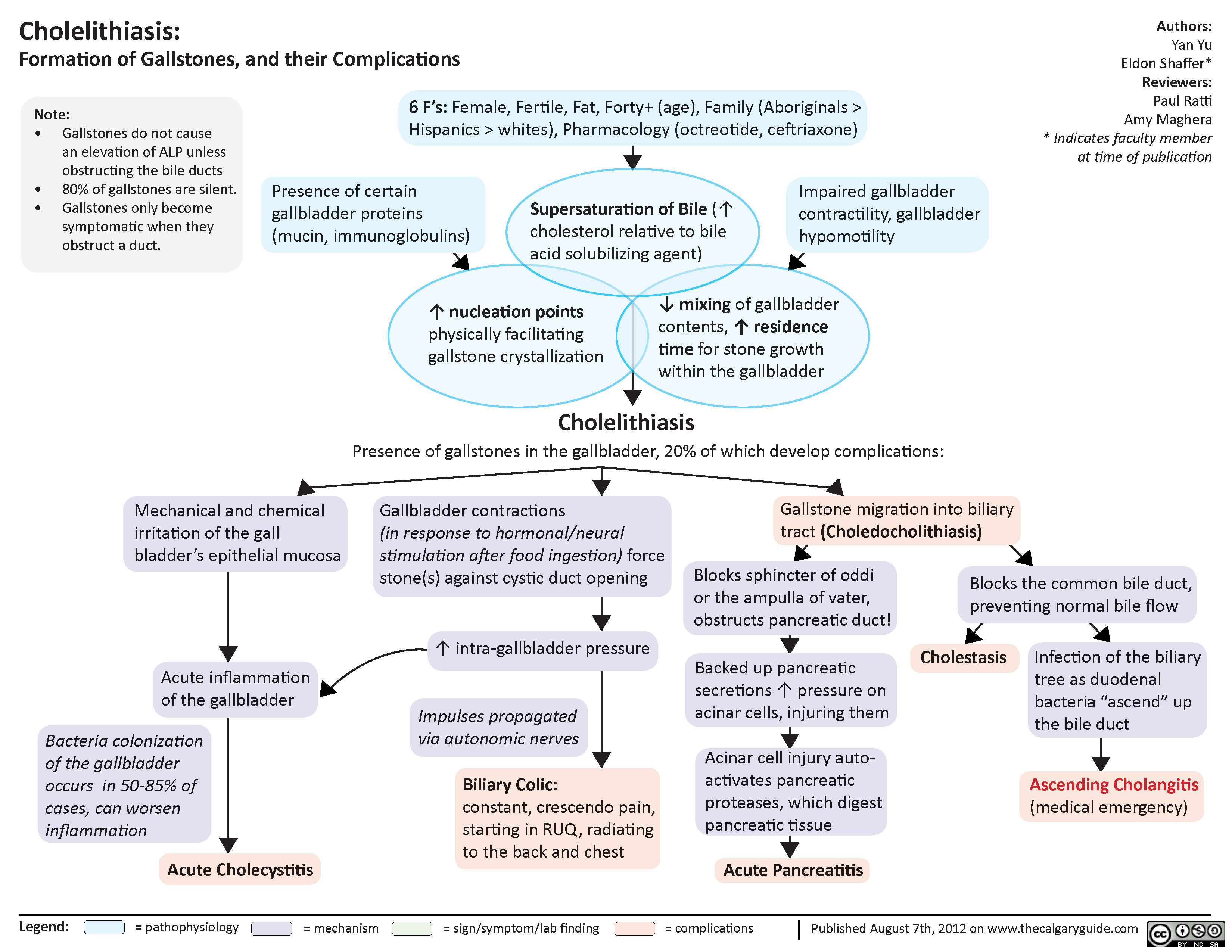
Cholelithiasis
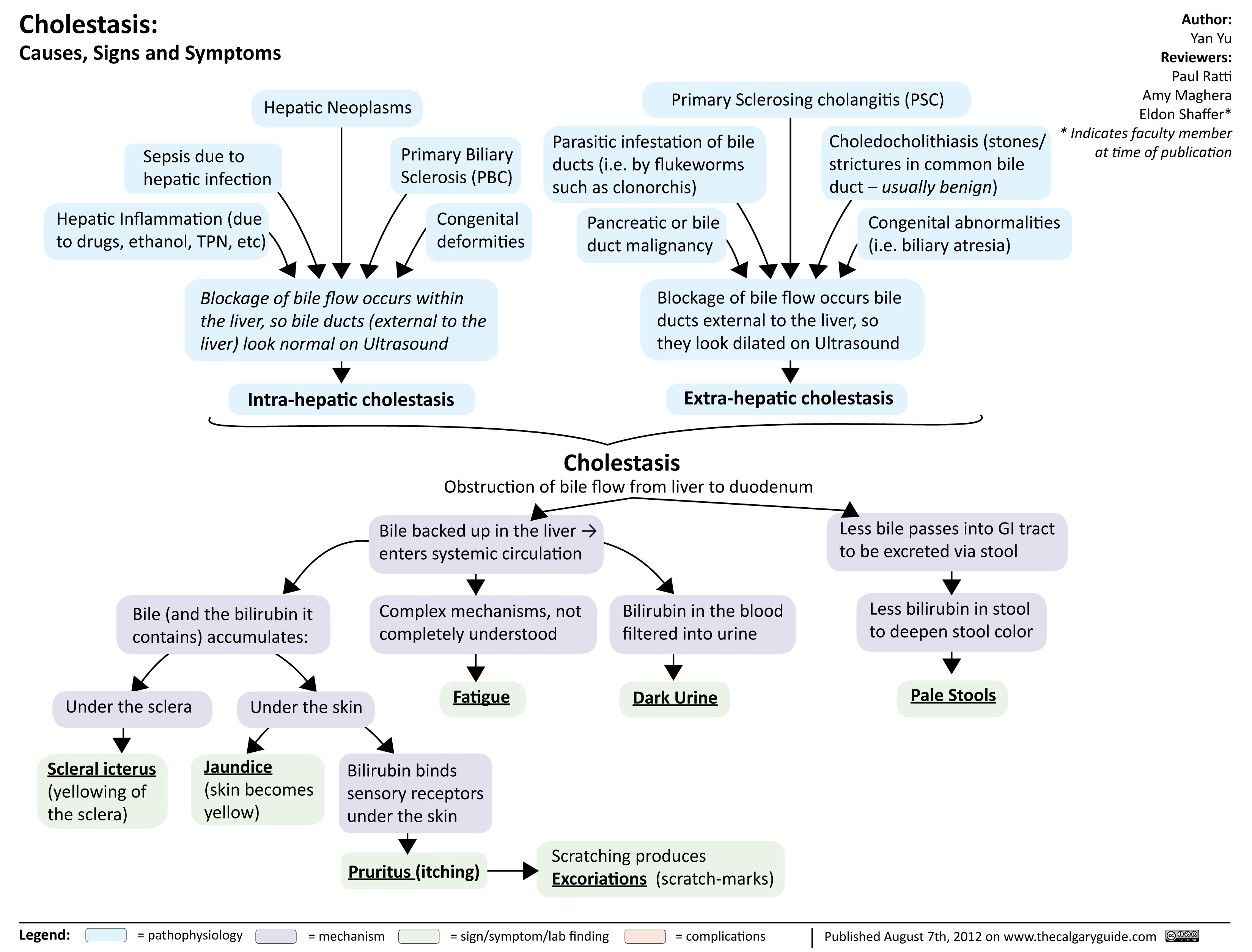
Cholestasis
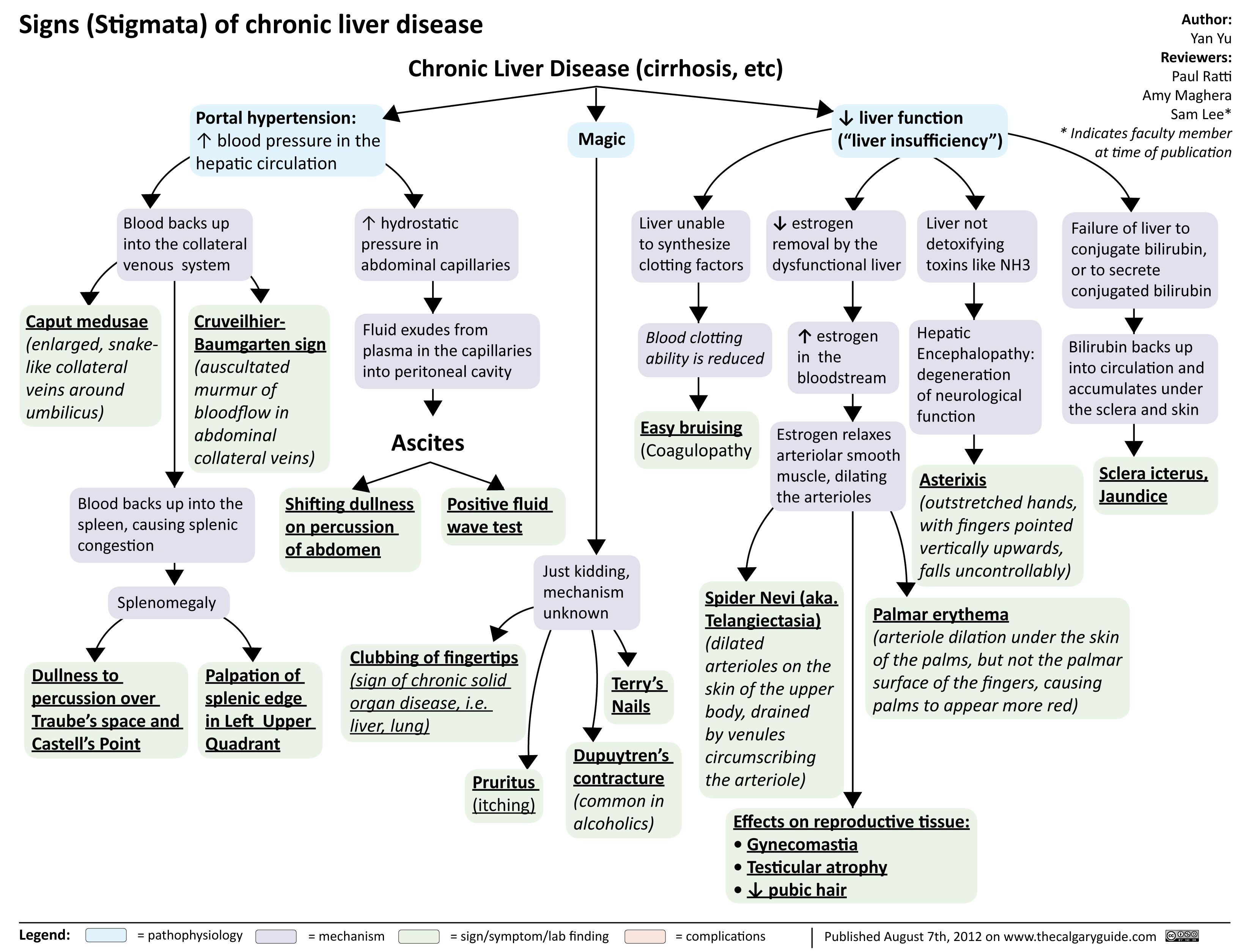
signs of chronic liver disease
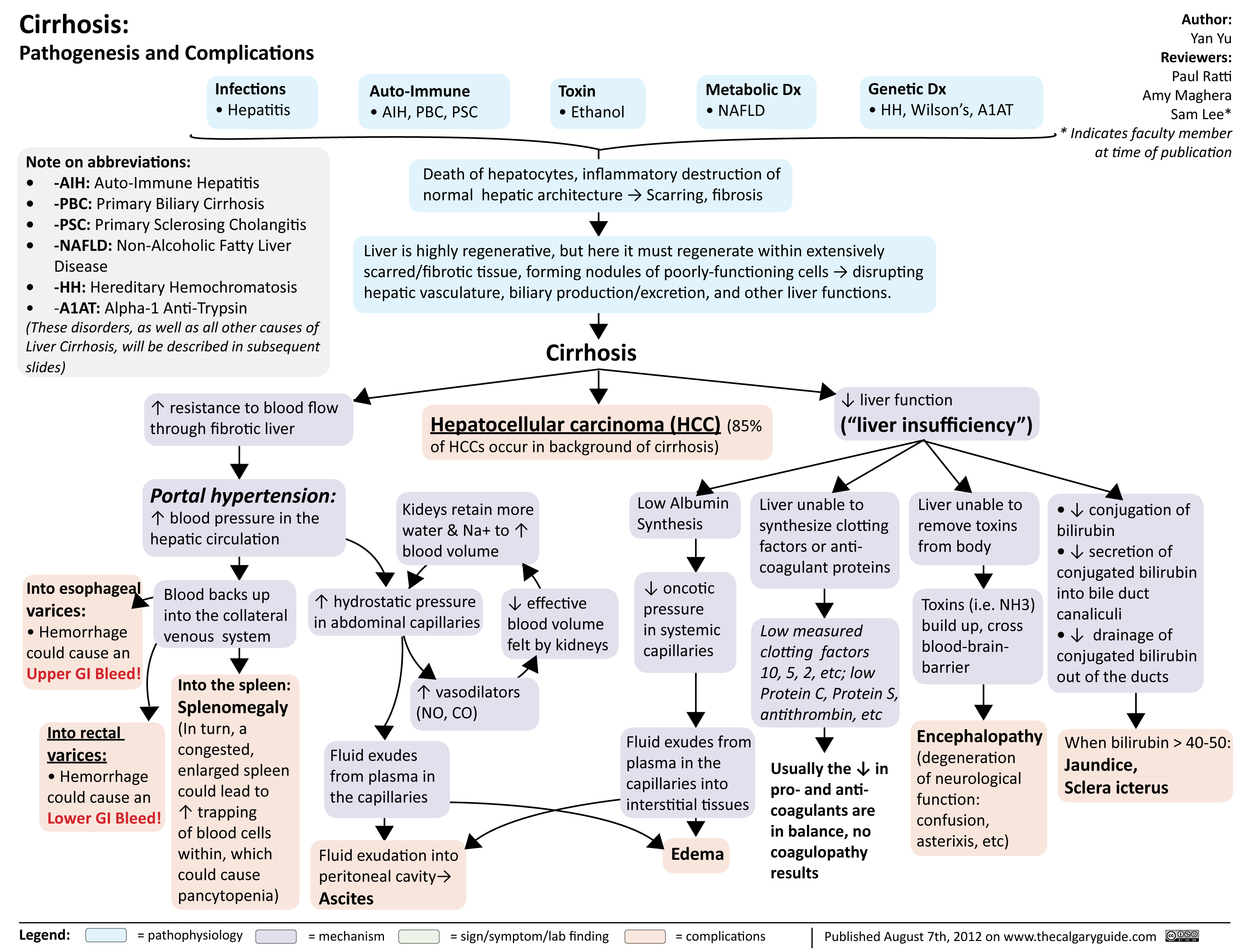
cirrhosis
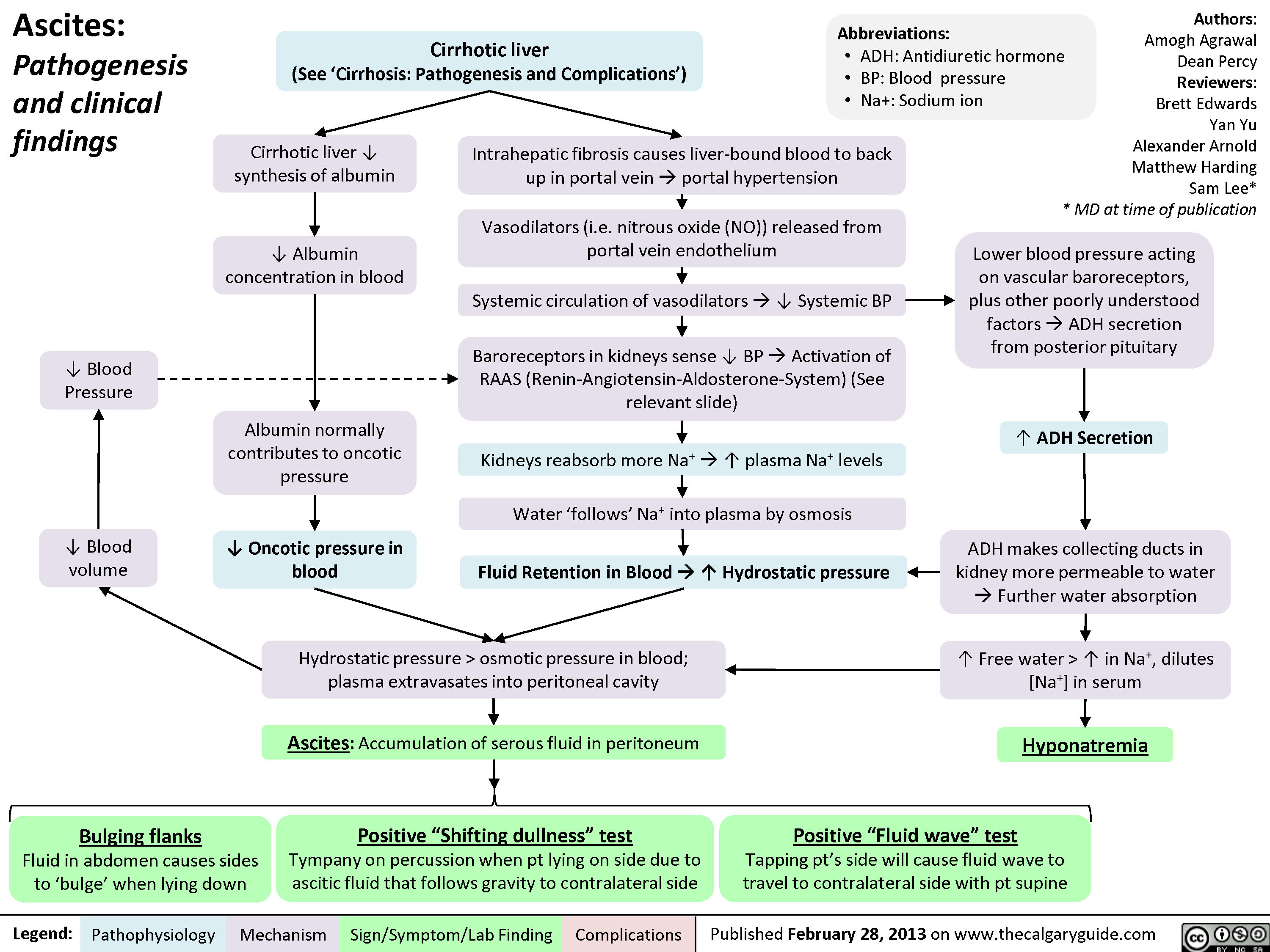
Ascites Clinical Findings
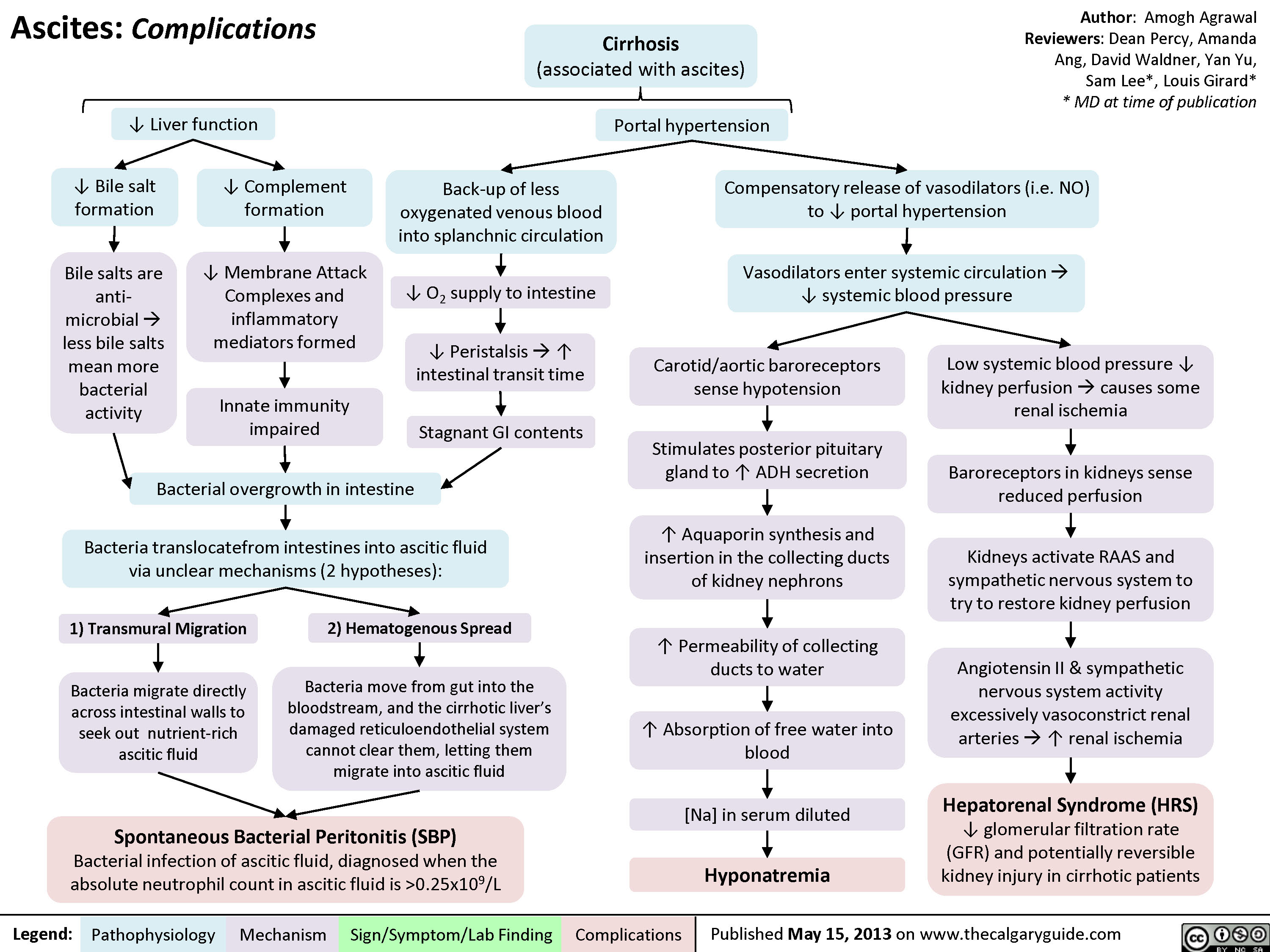
AscitesComplications
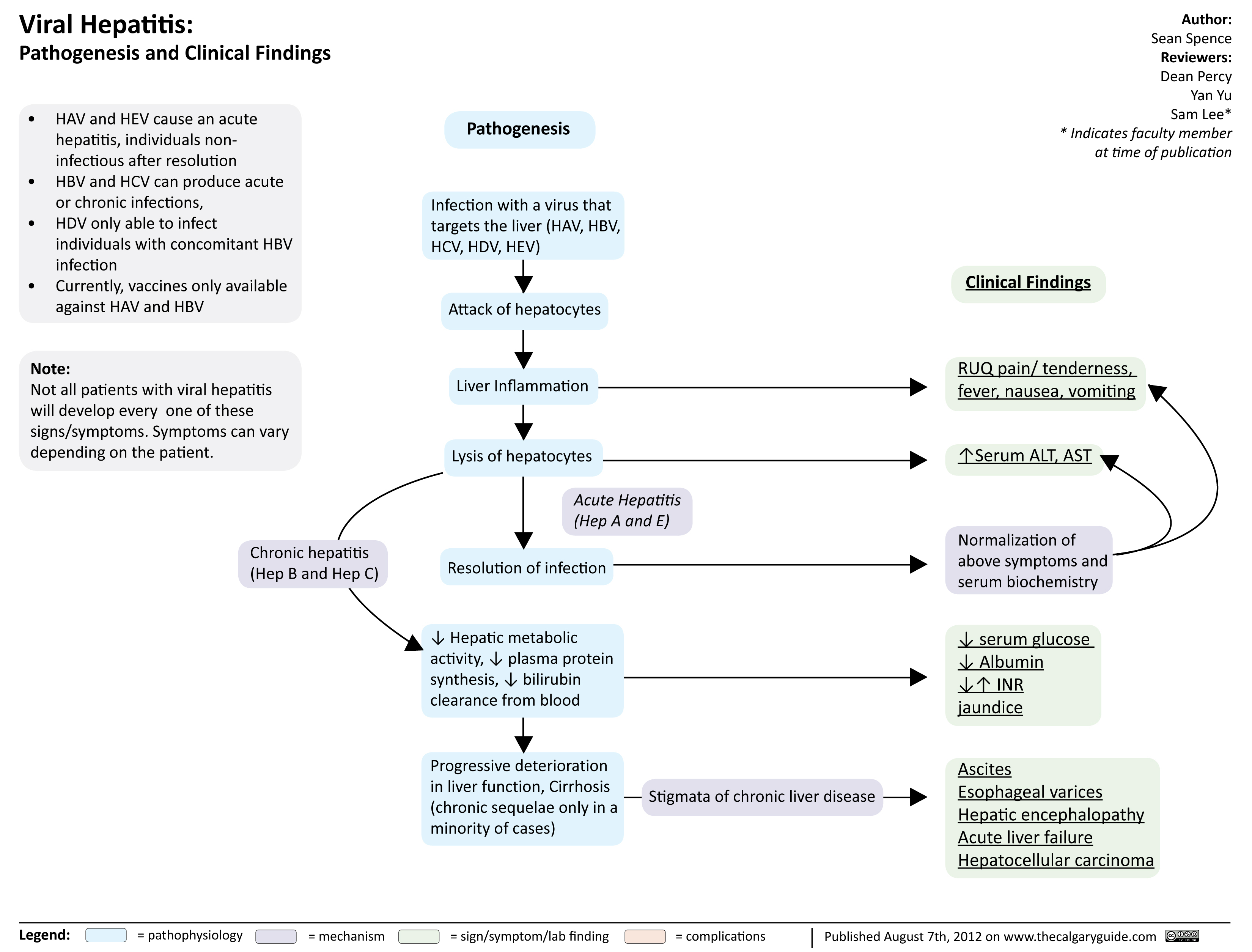
viral hepatits
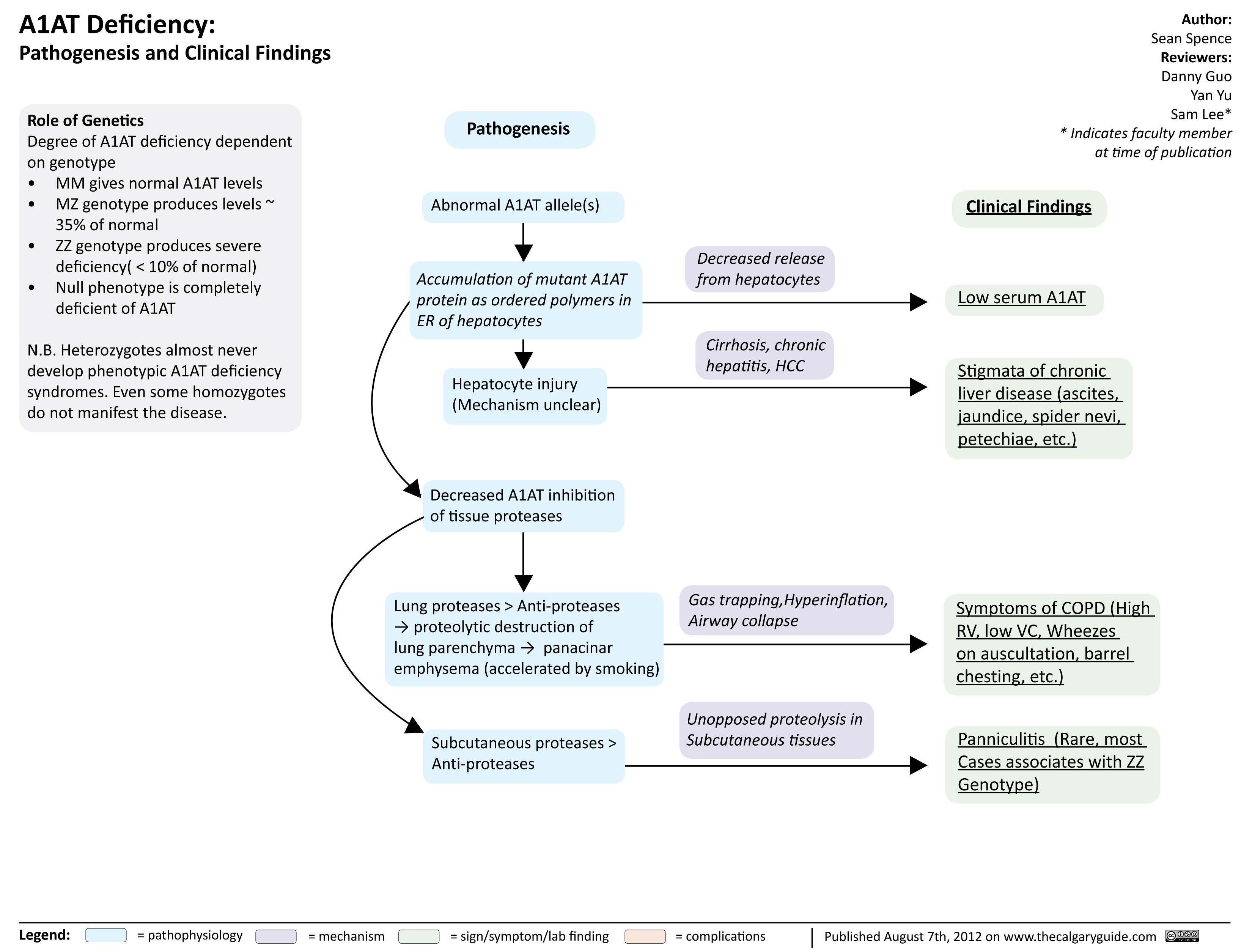
A1ATDeficiency
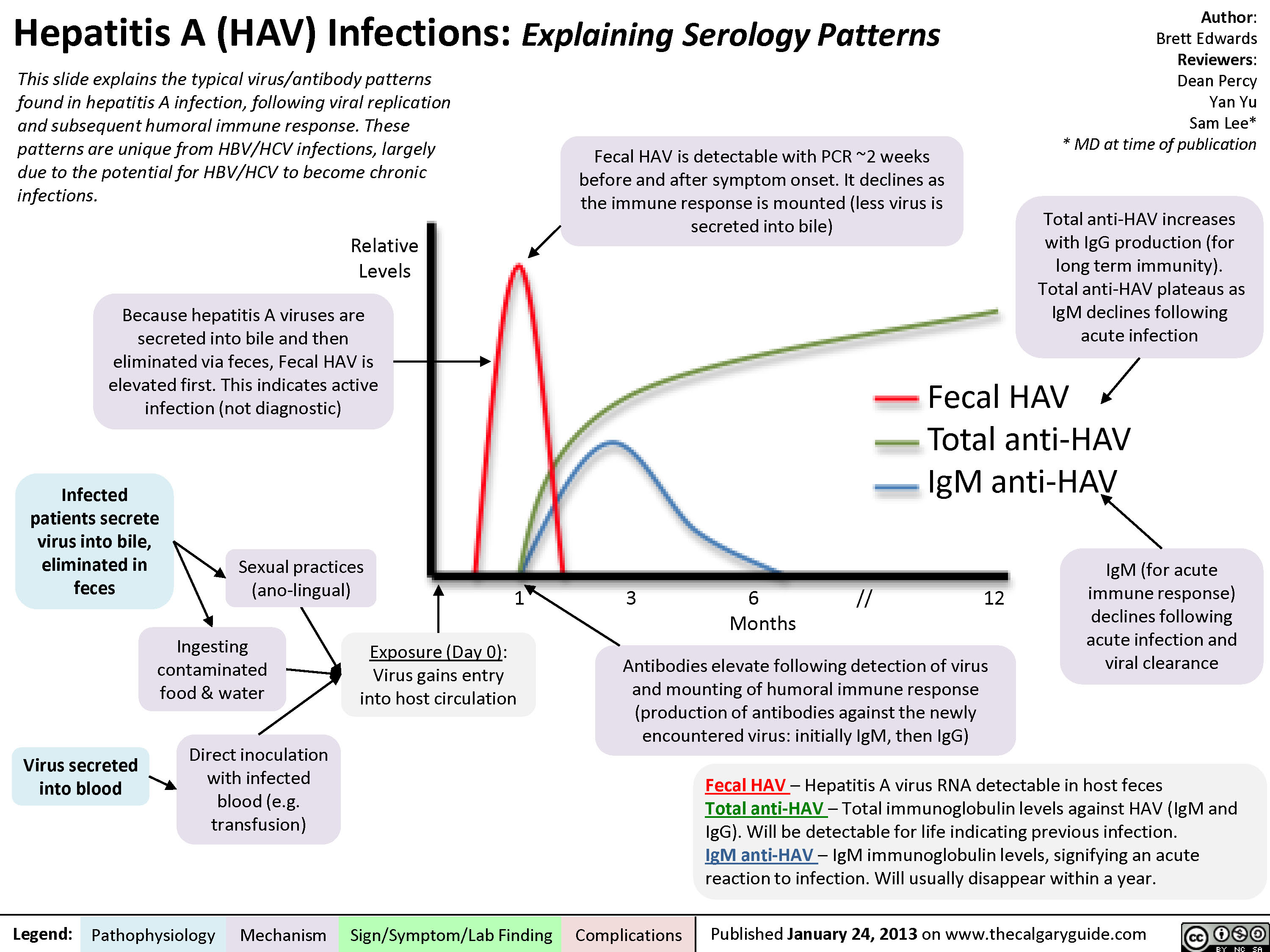
Hepatitis A (HAV) Infections
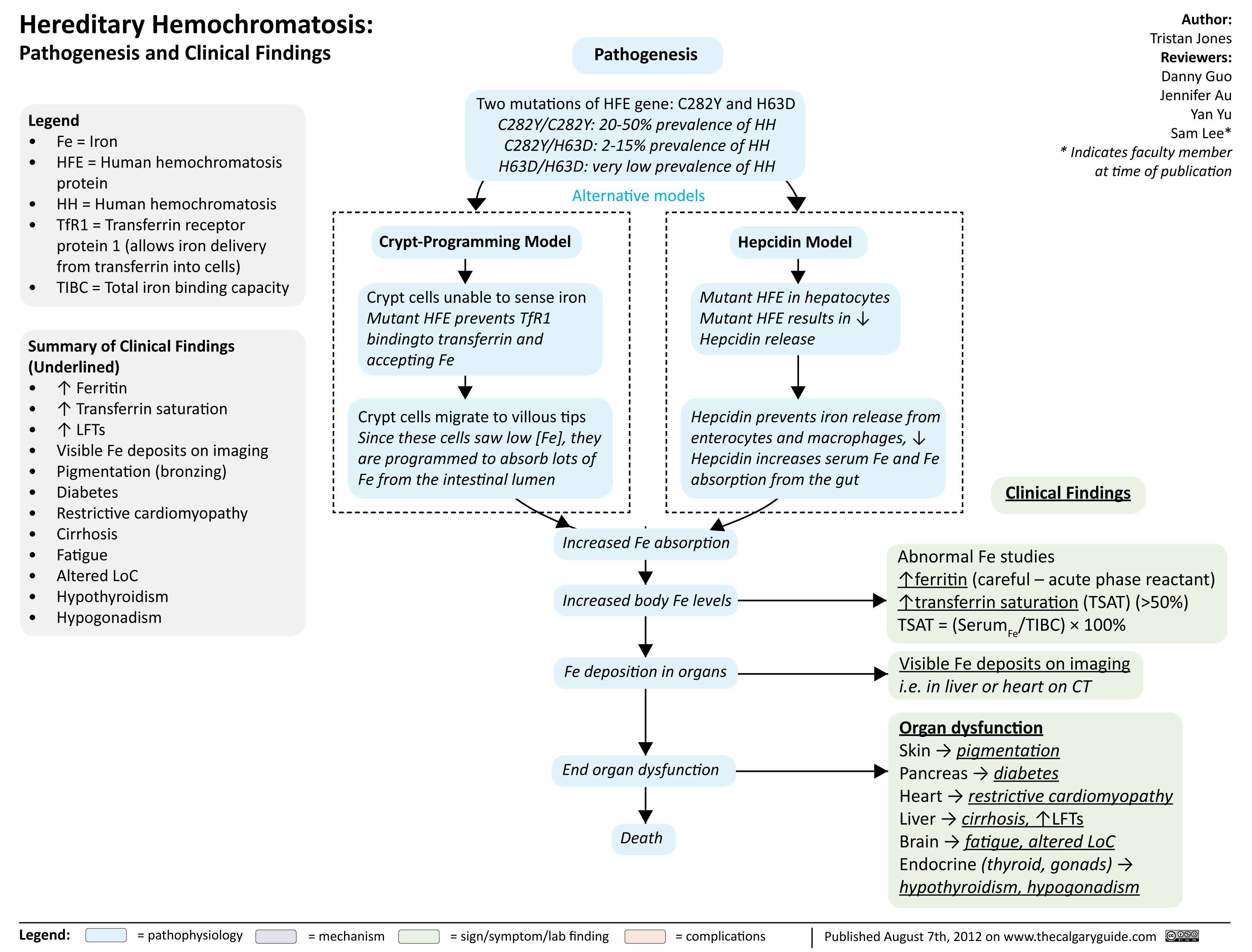
Hereditary hemochromatosis
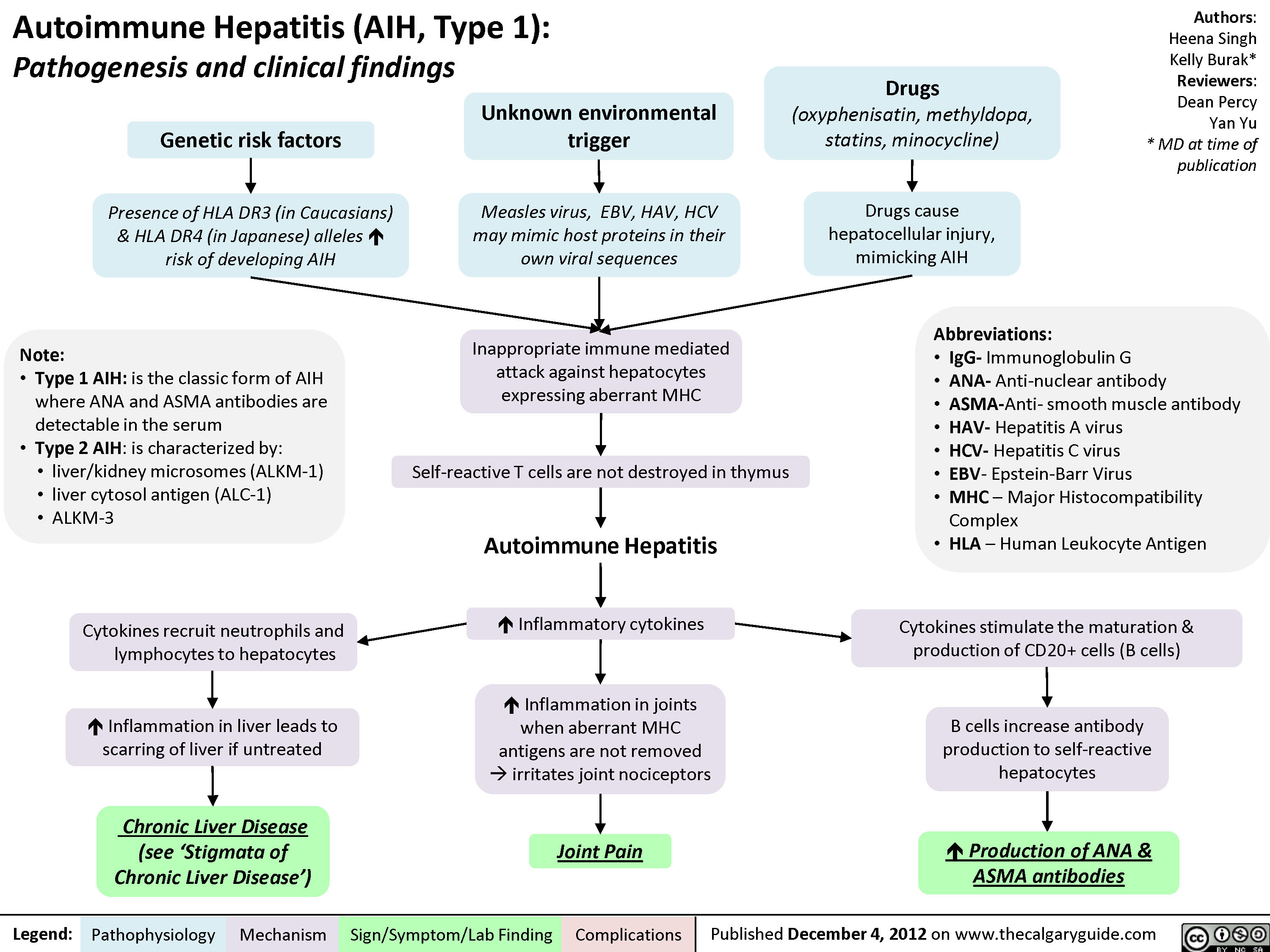
Auto-immune Hepatitis
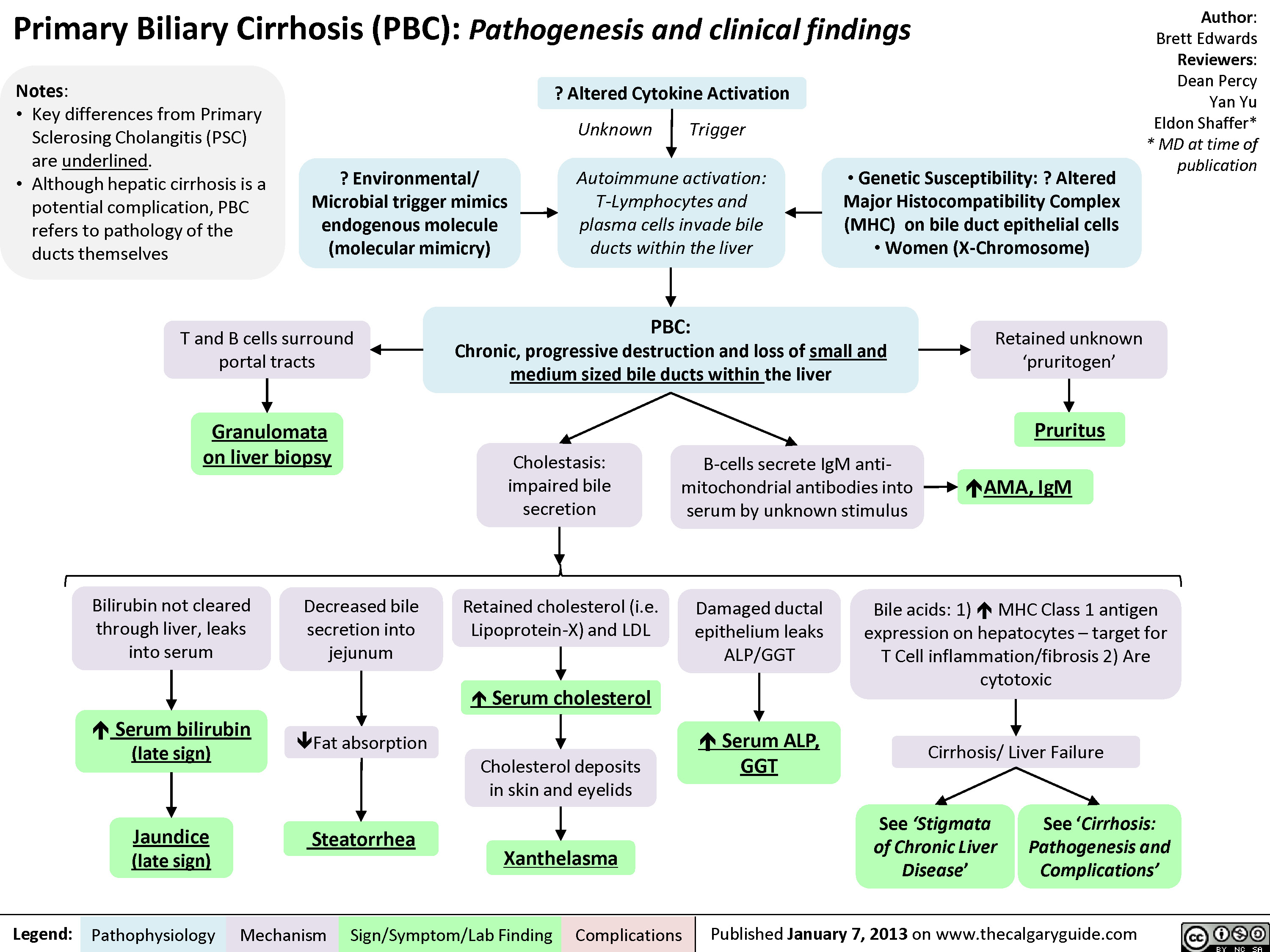
Primary Biliary Cirrhosis (PBC)
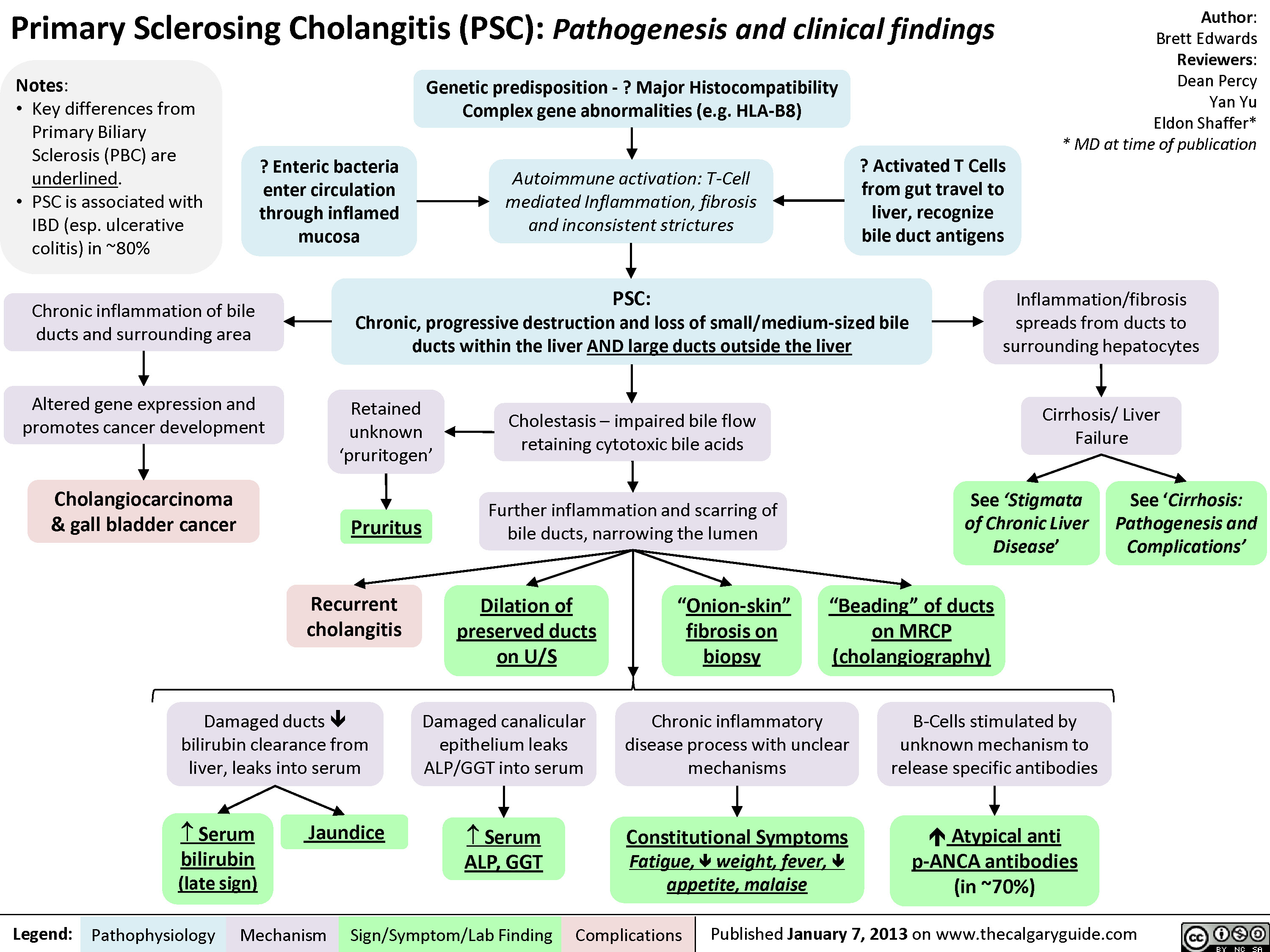
Primary Sclerosing Cholangitis (PSC)
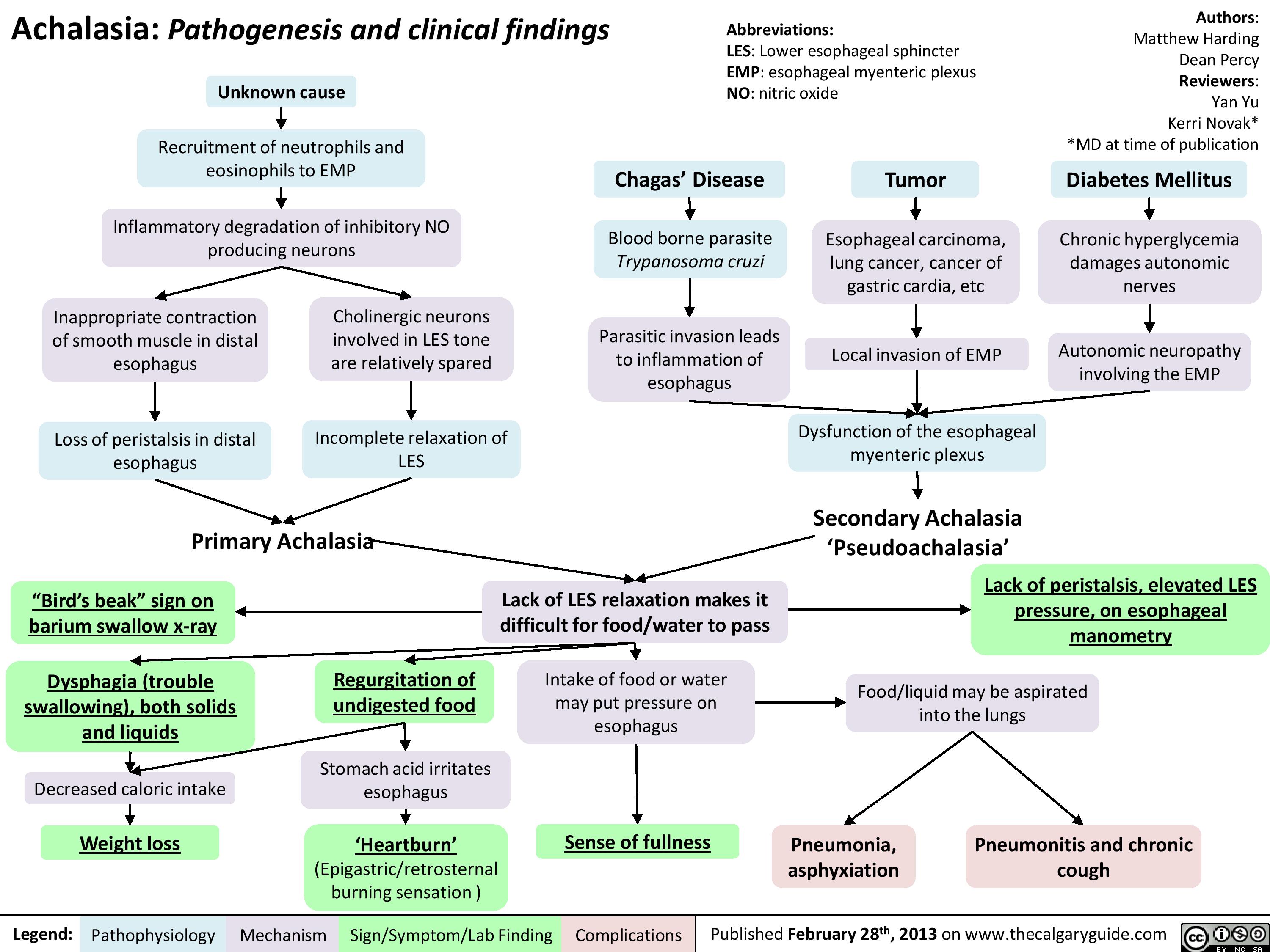
Achalasia Pathogenesis and clinical findings
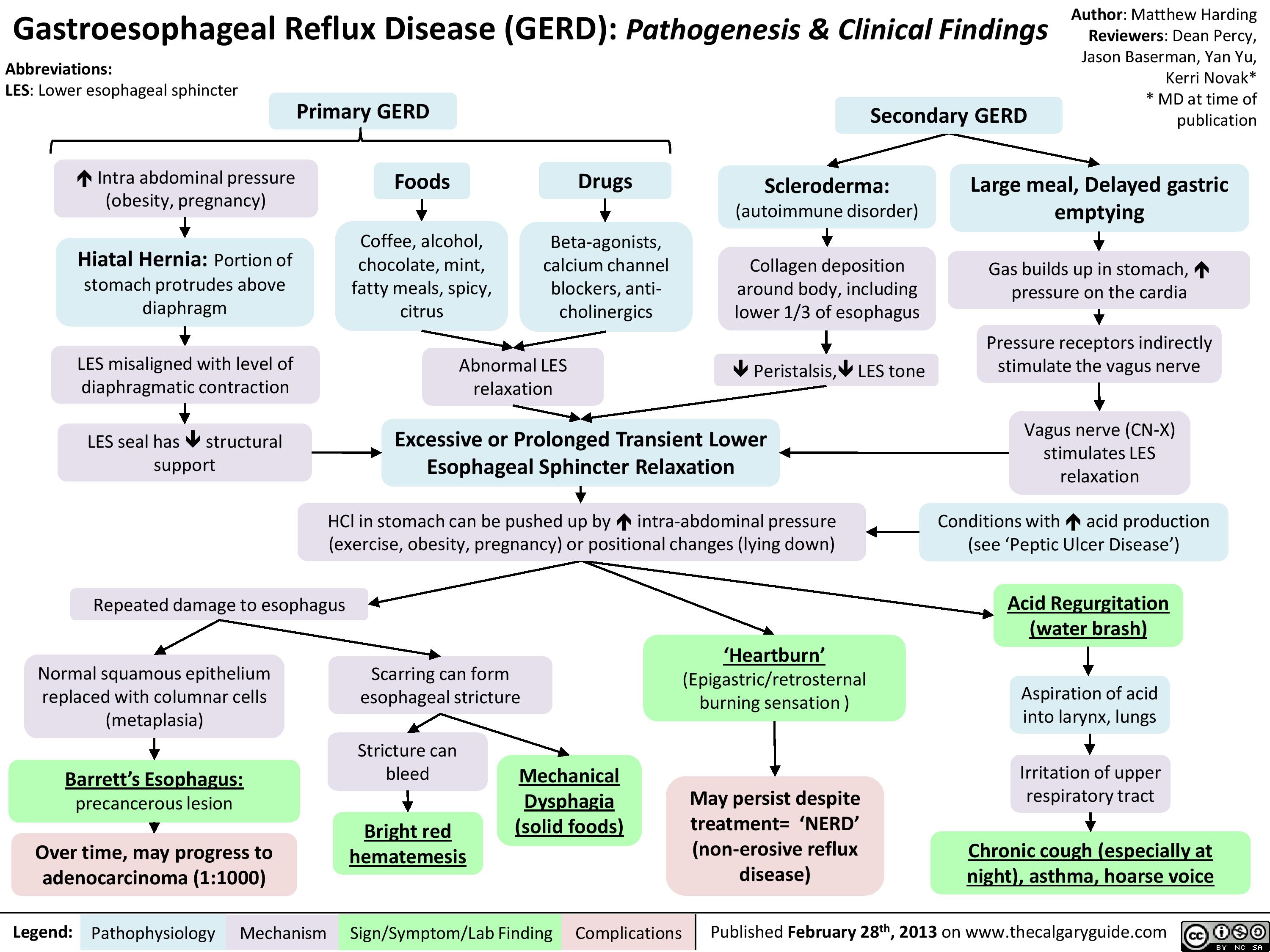
Gastroesophageal Reflux Disease (GERD) Pathogenesis and Clinical Findings
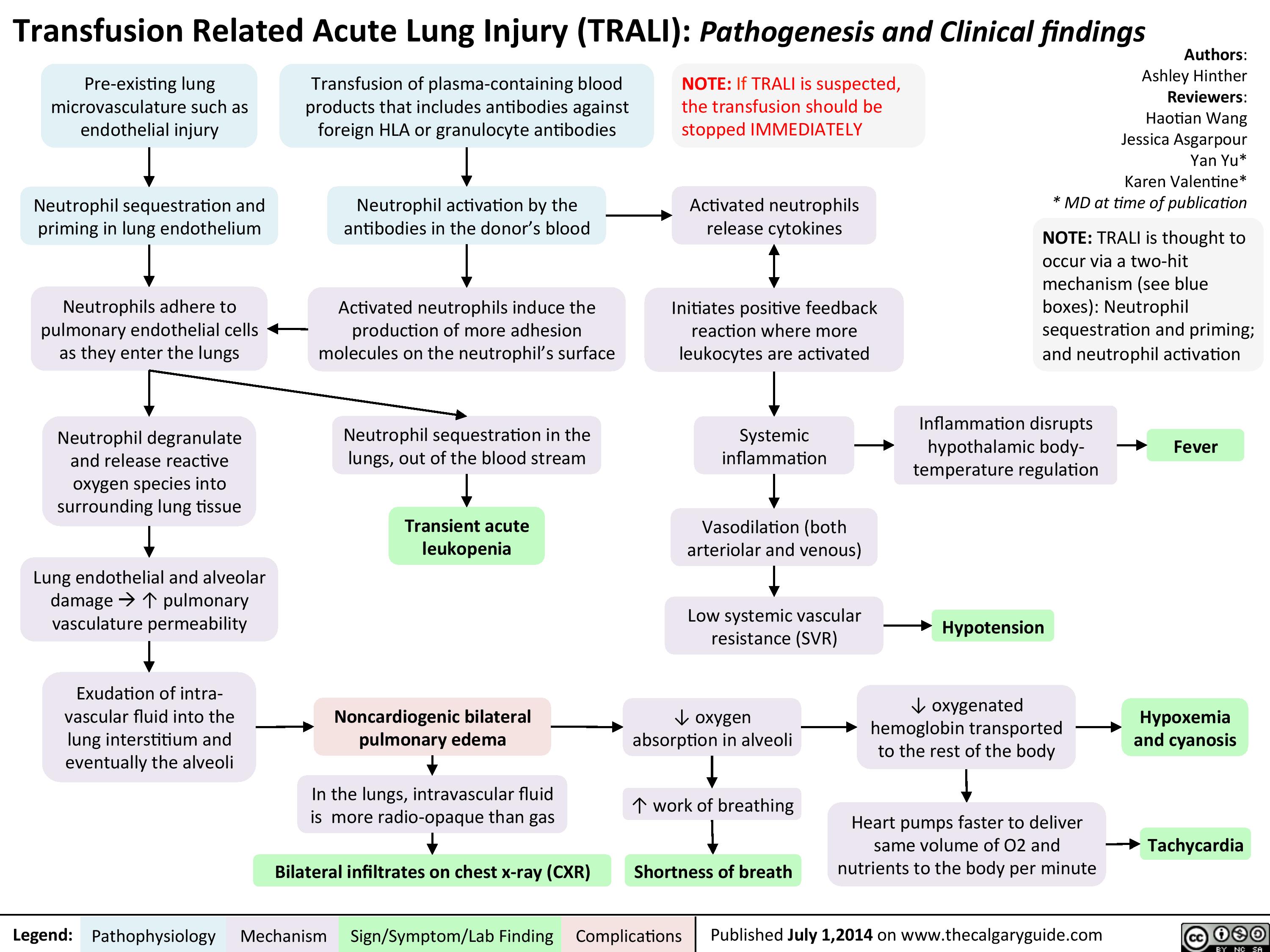
TRALI
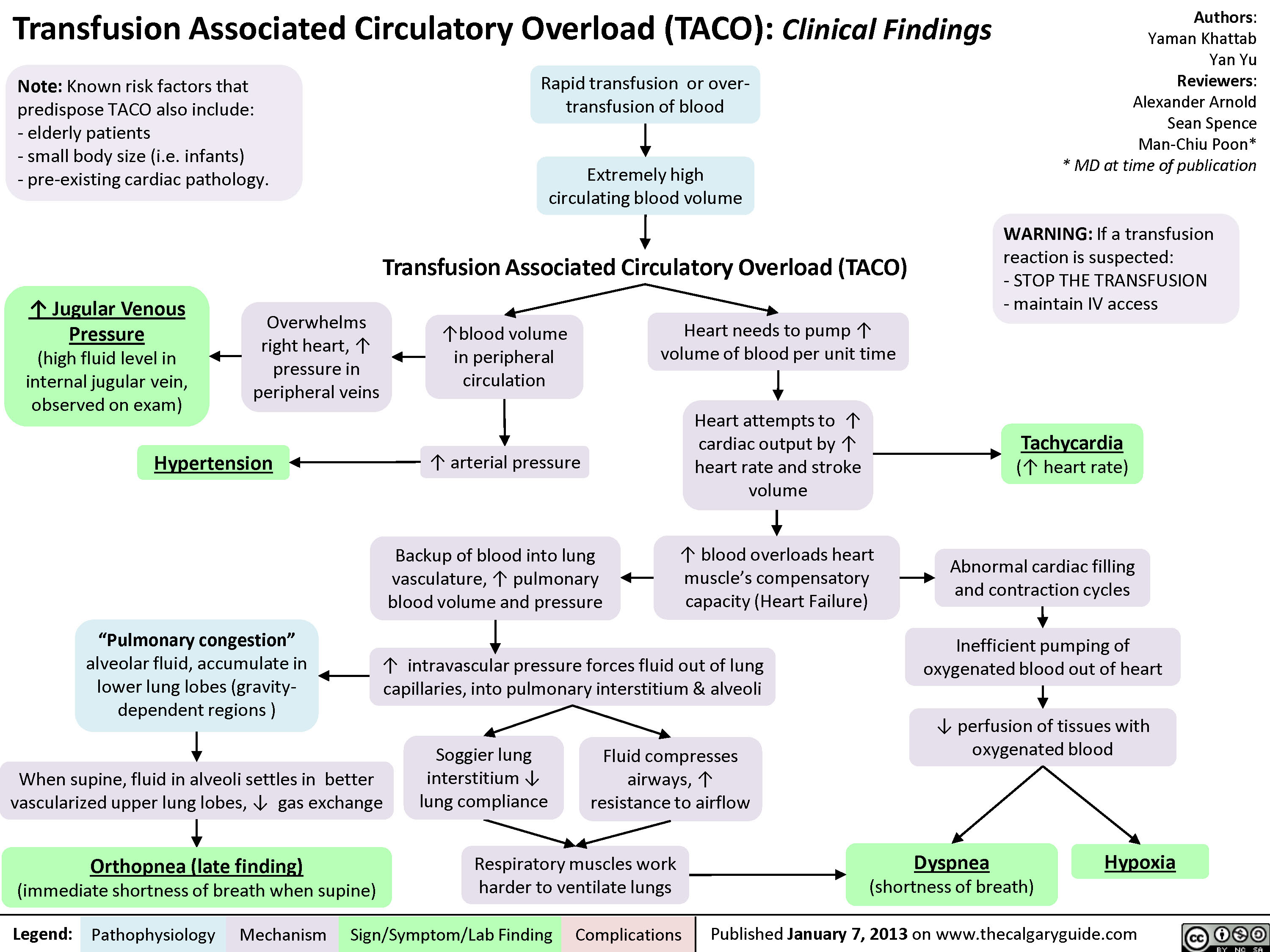
Transfusion Associated Circulatory Overload (TACO)
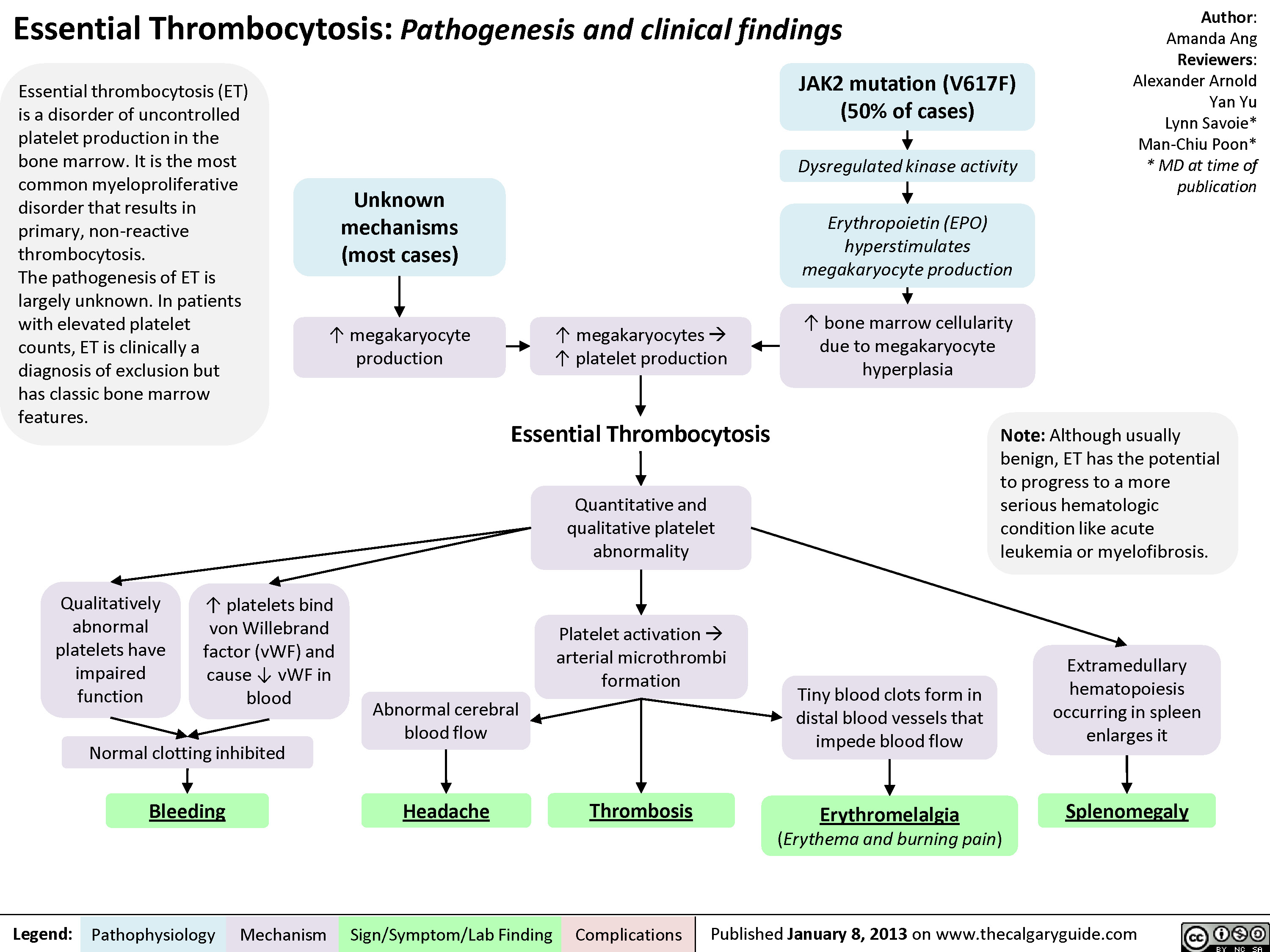
Essential Thrombocytosis (ET)
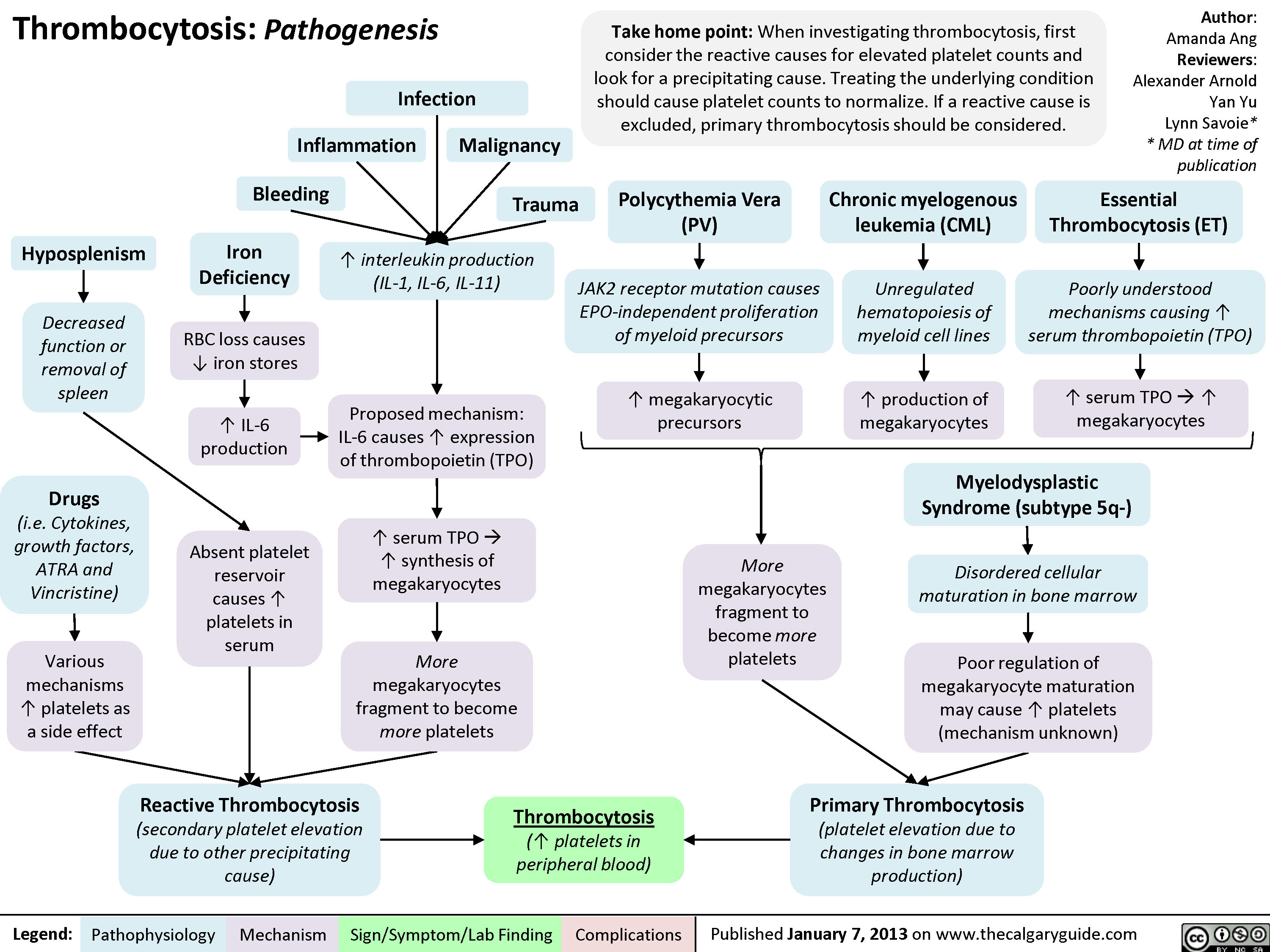
Pathogenesis of thrombocytosis
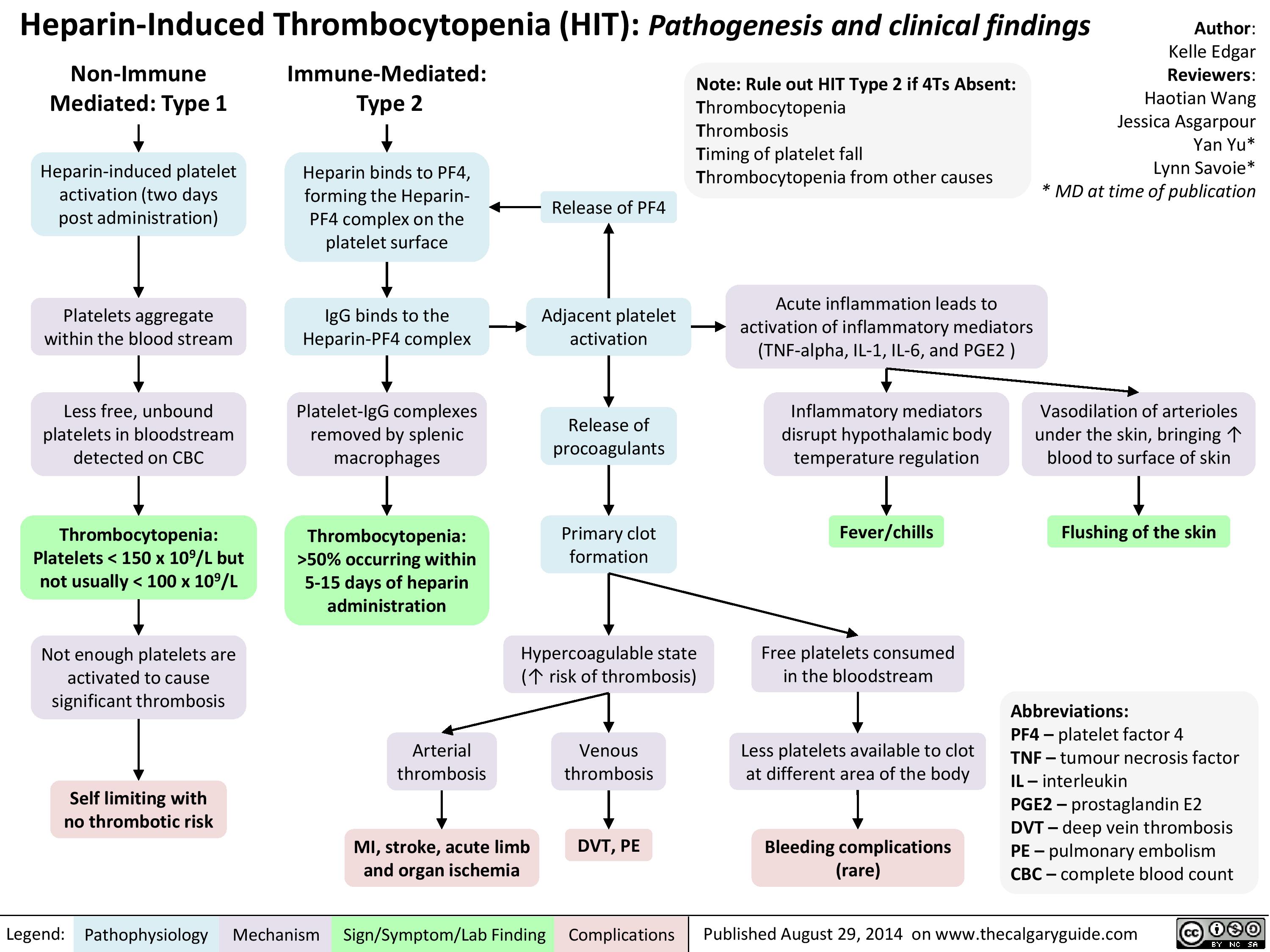
Heparin Induced Thrombocytopenia
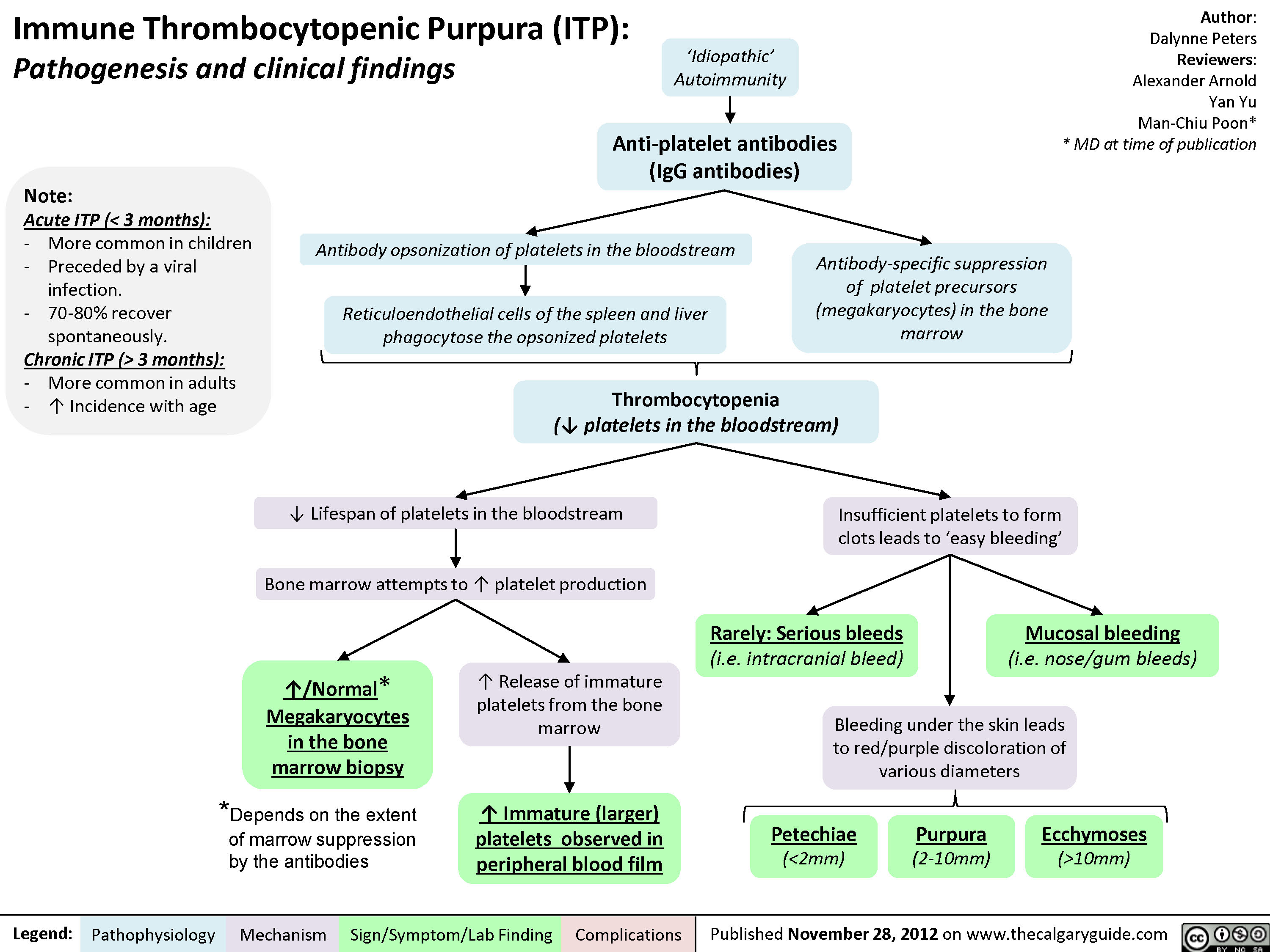
Immune thrombocytopenic purpura
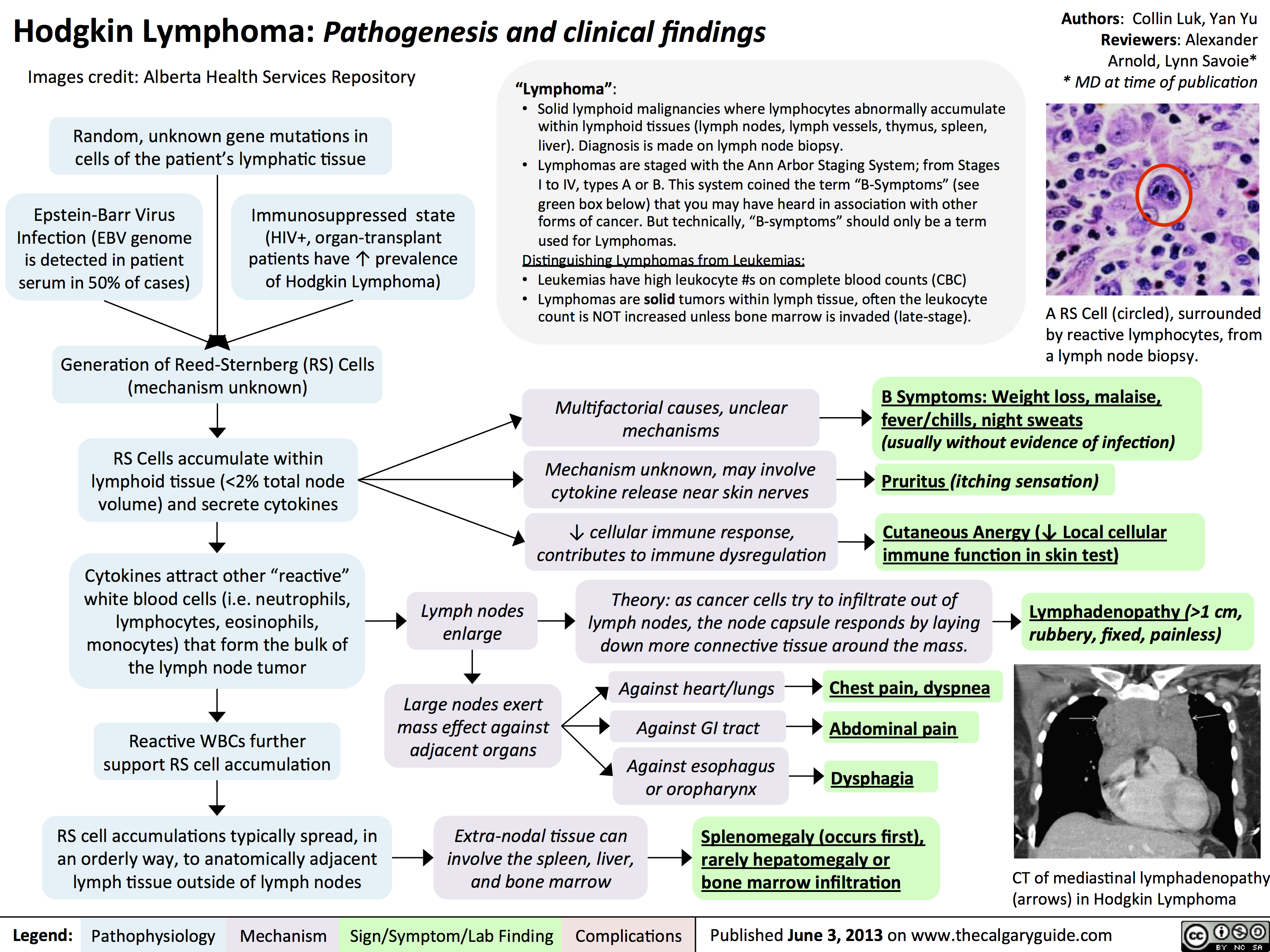
hodgkin lymphoma - pathogenesis and clinical findings
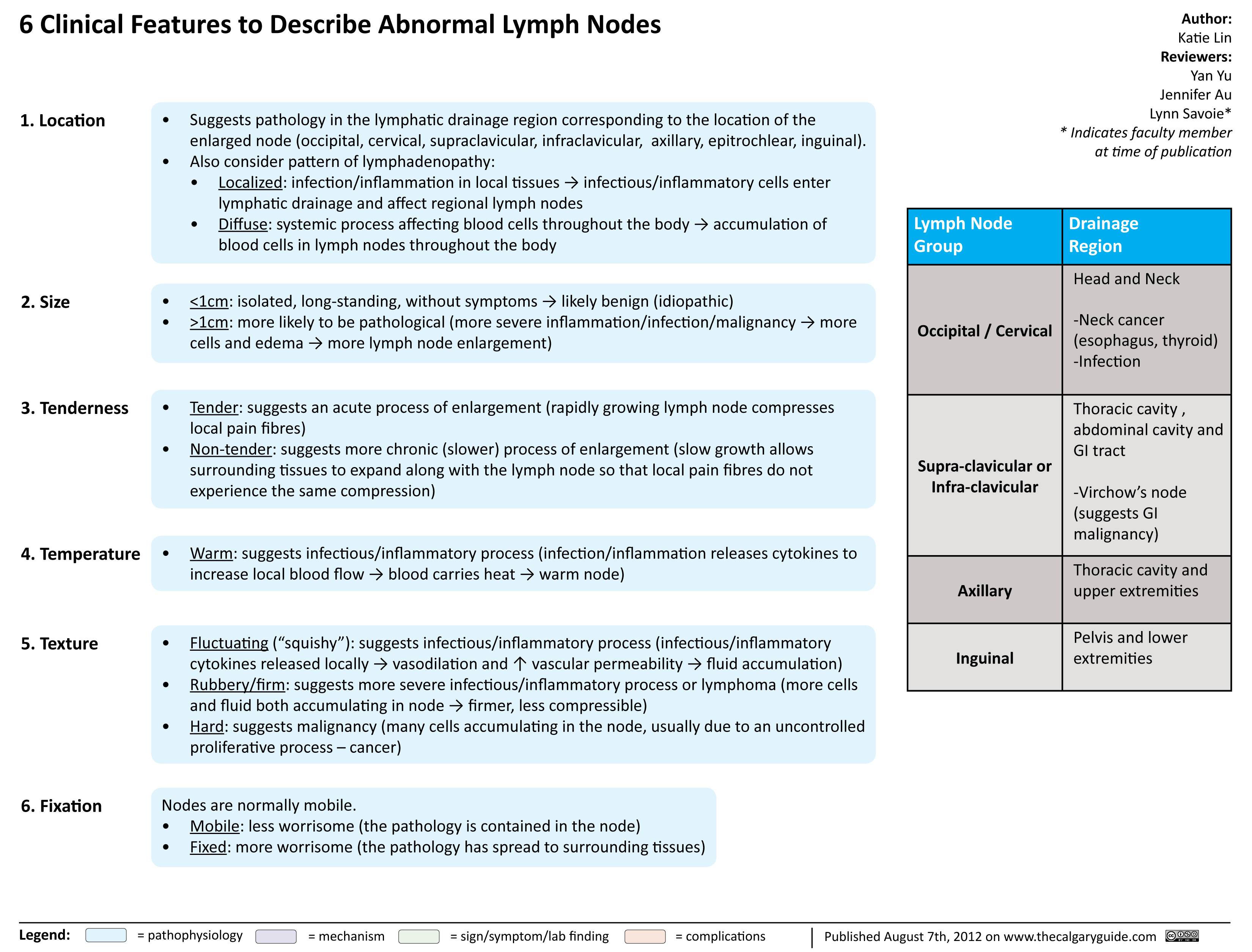
Clinical Features to Describe Abnormal Lymph Nodes
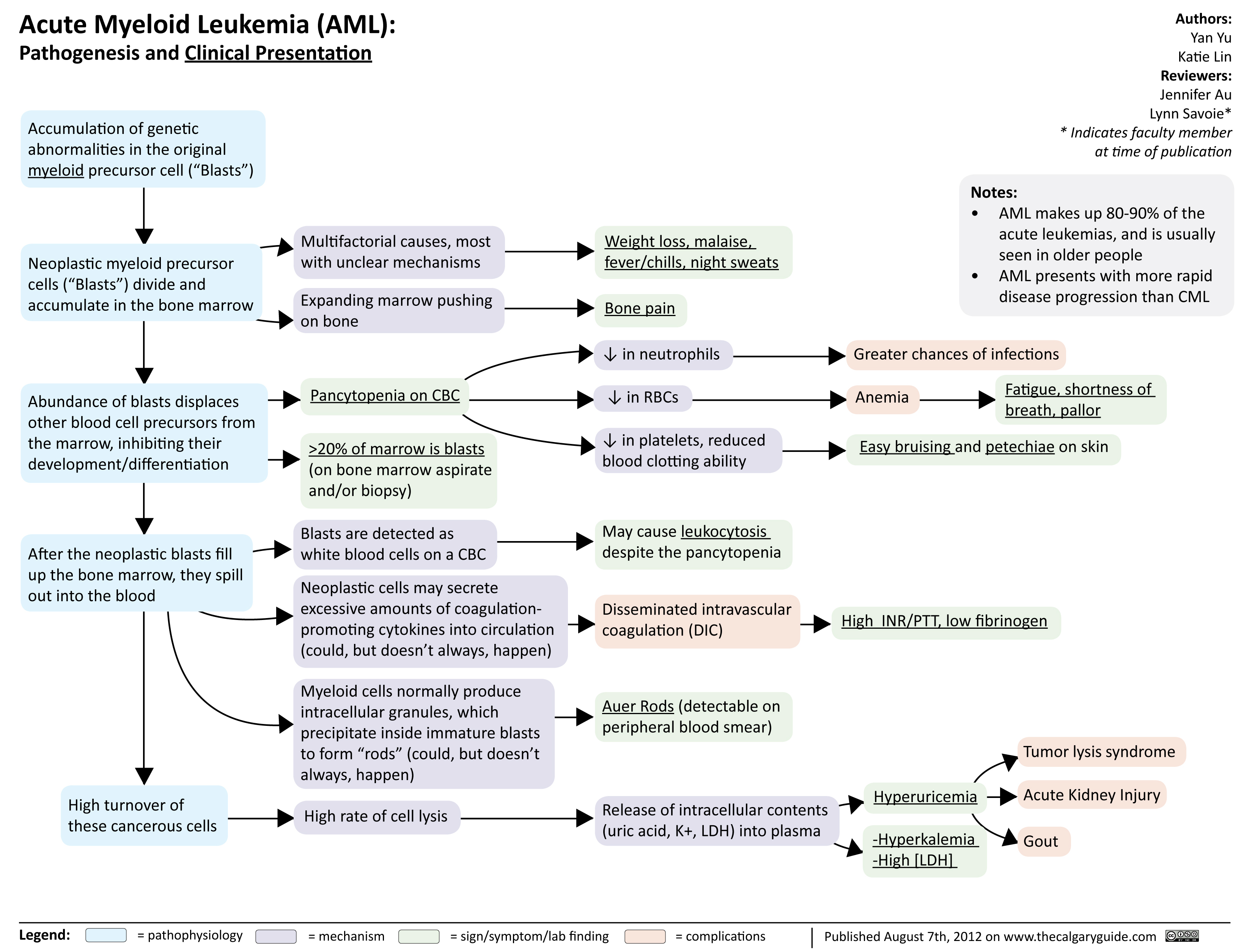
Acute Myeloid Leukemia
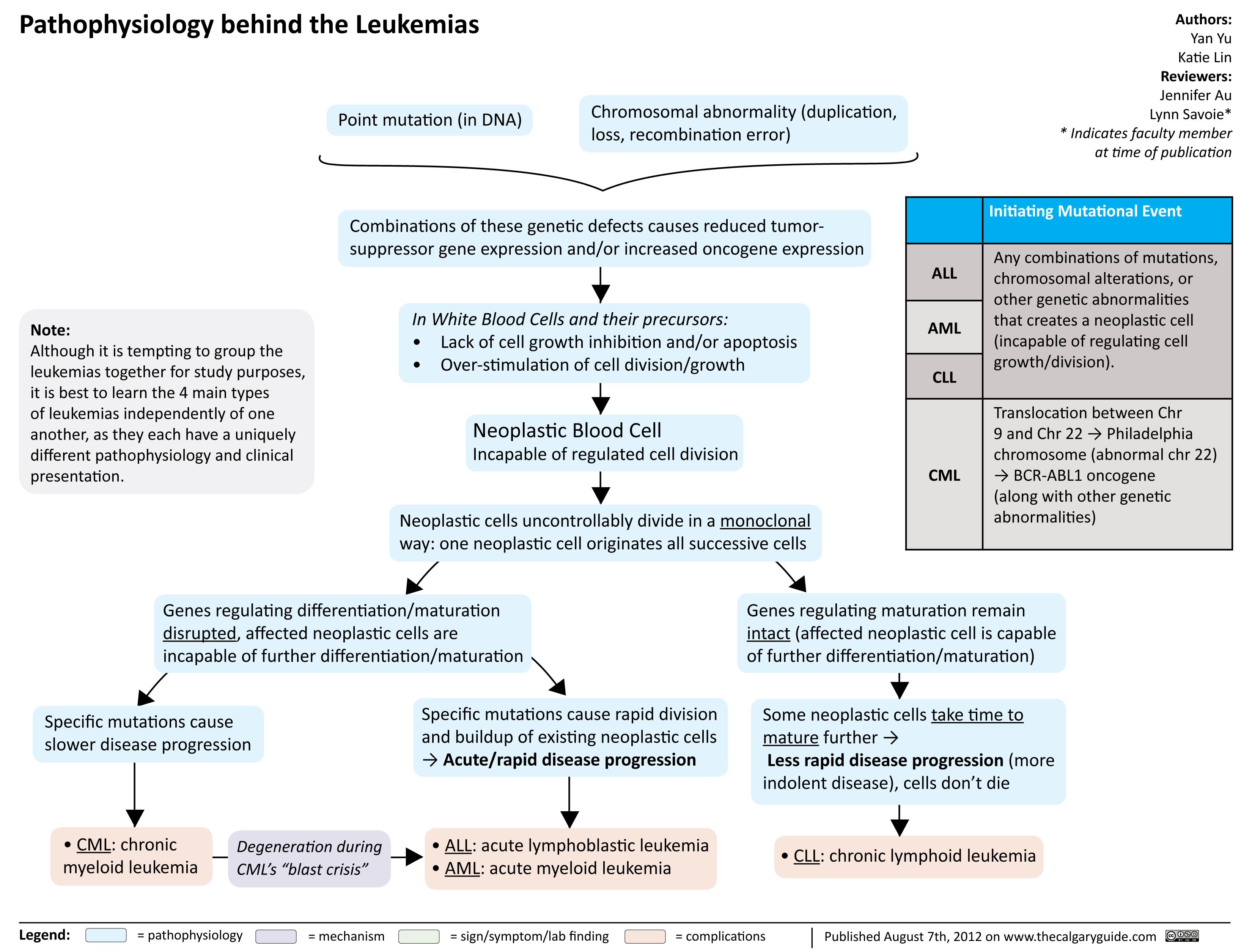
Pathophysiology behind the leukemias
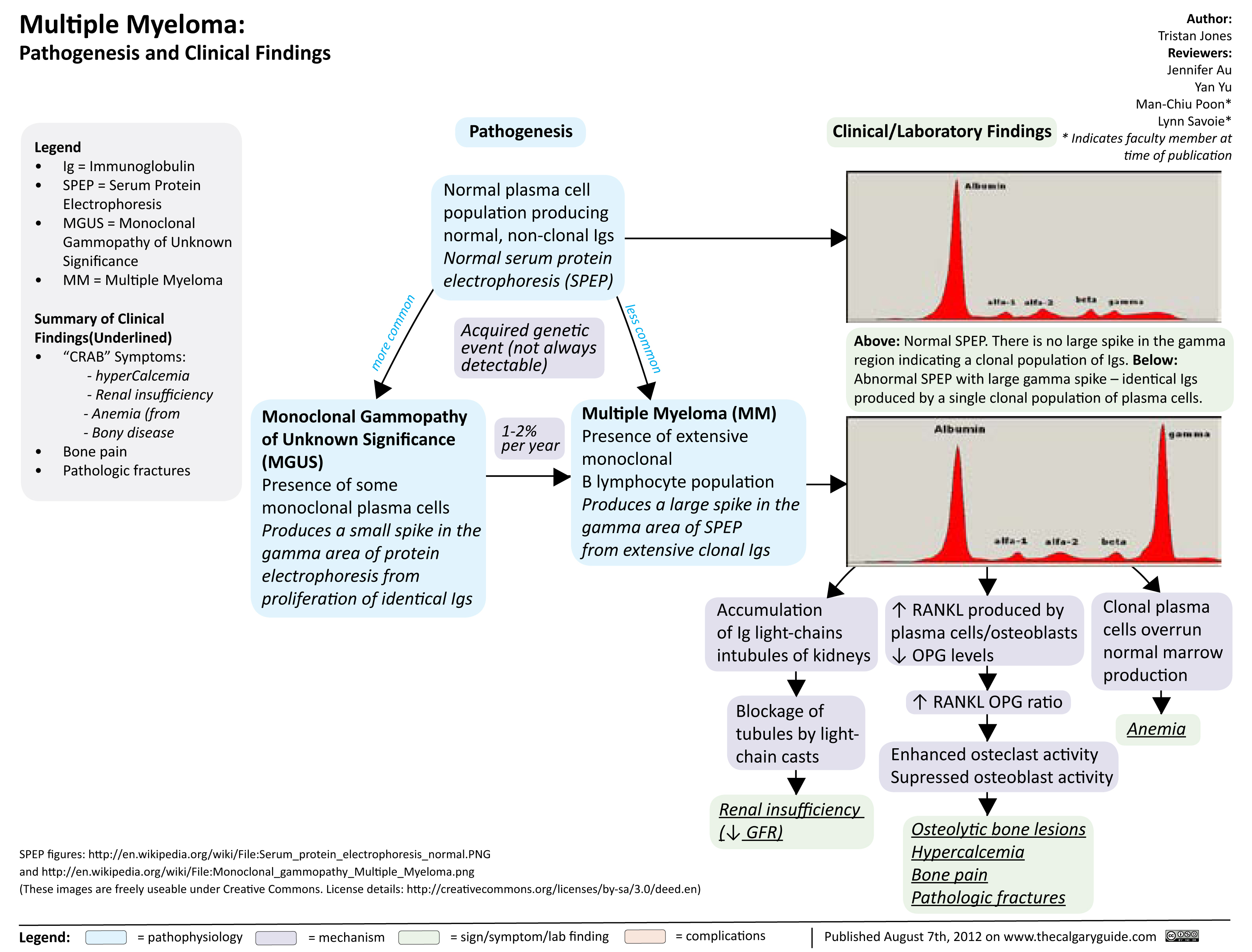
Multiple Myeloma
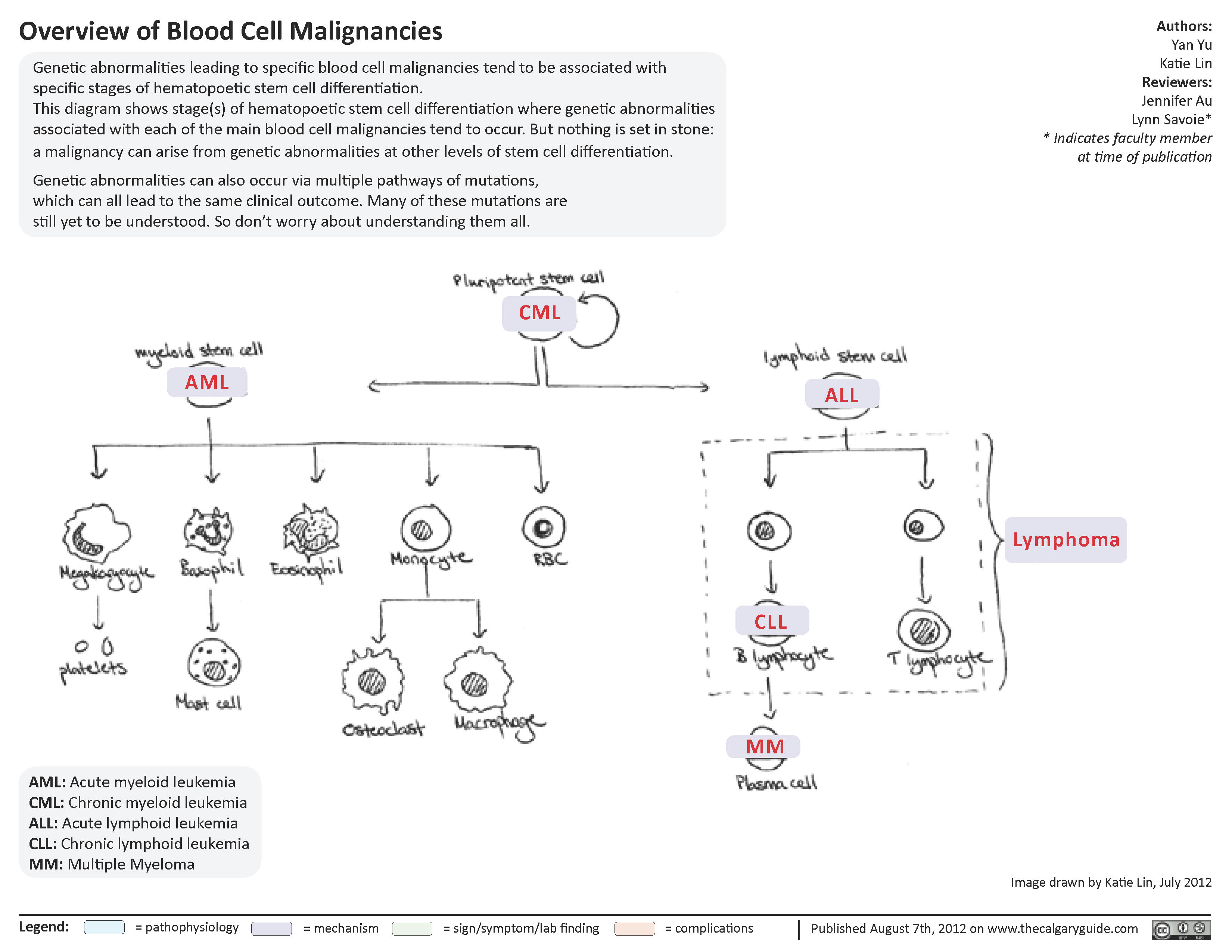
Overview of blood cell malignancies
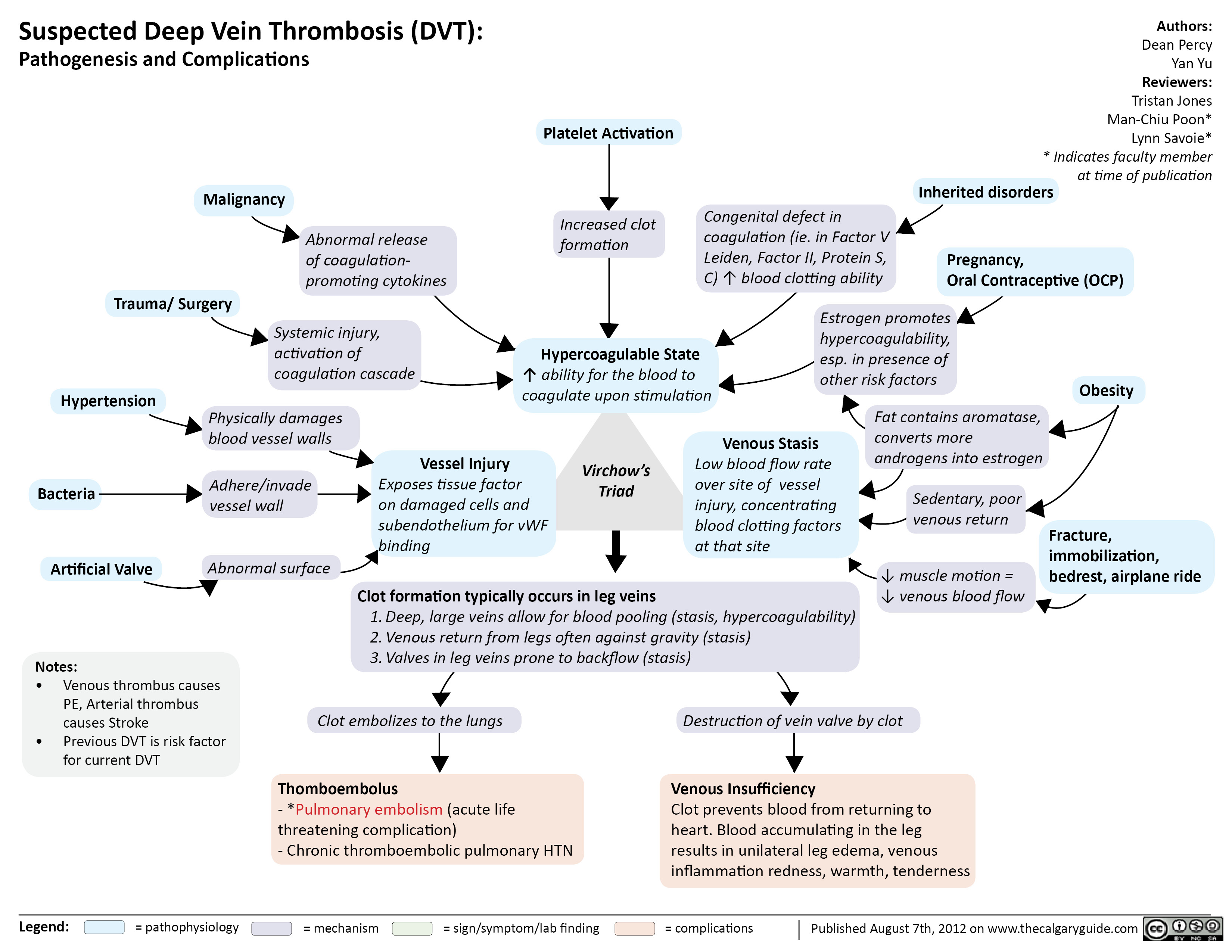
Suspected Deep Vein Thrombosis
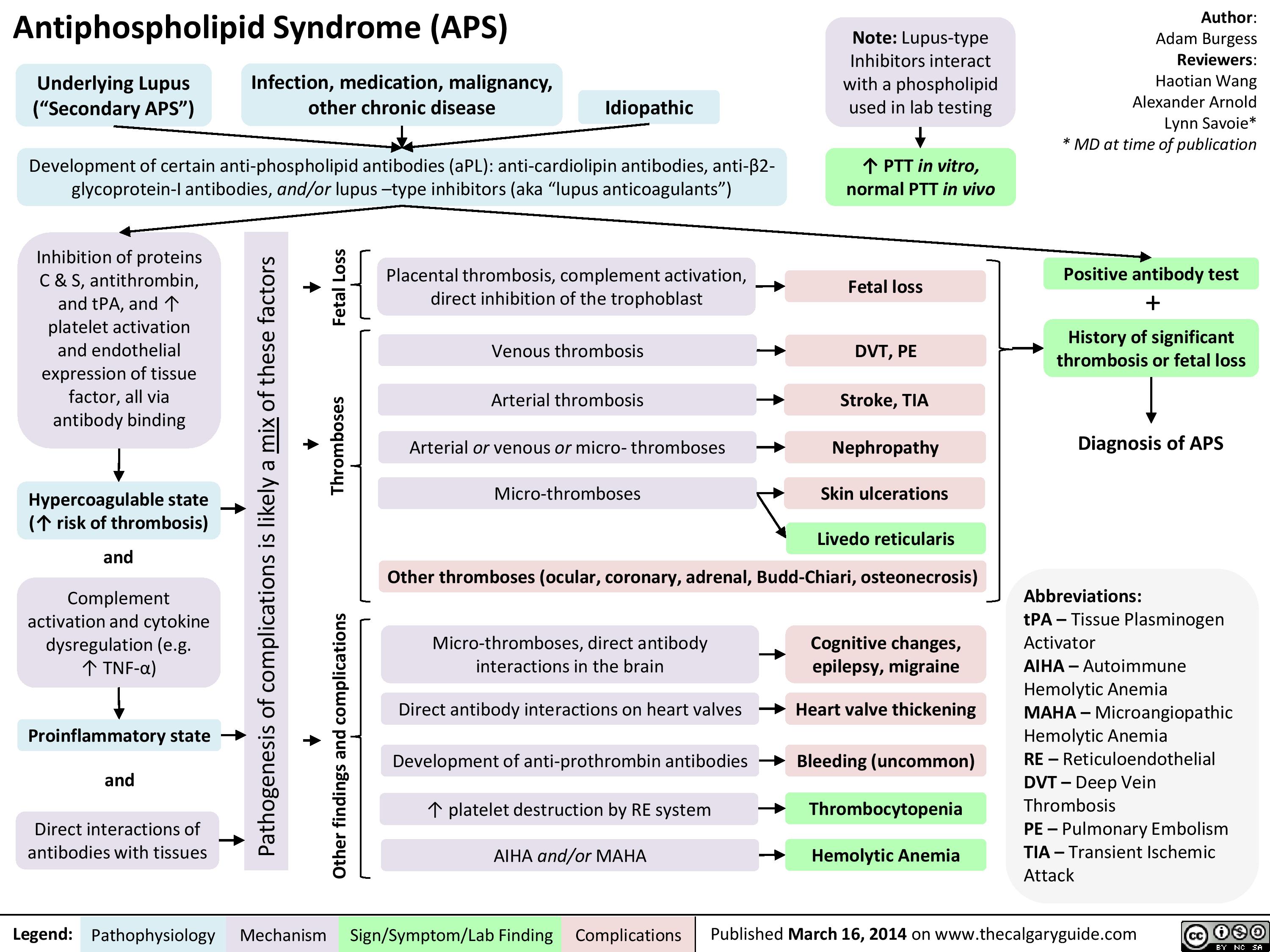
APS
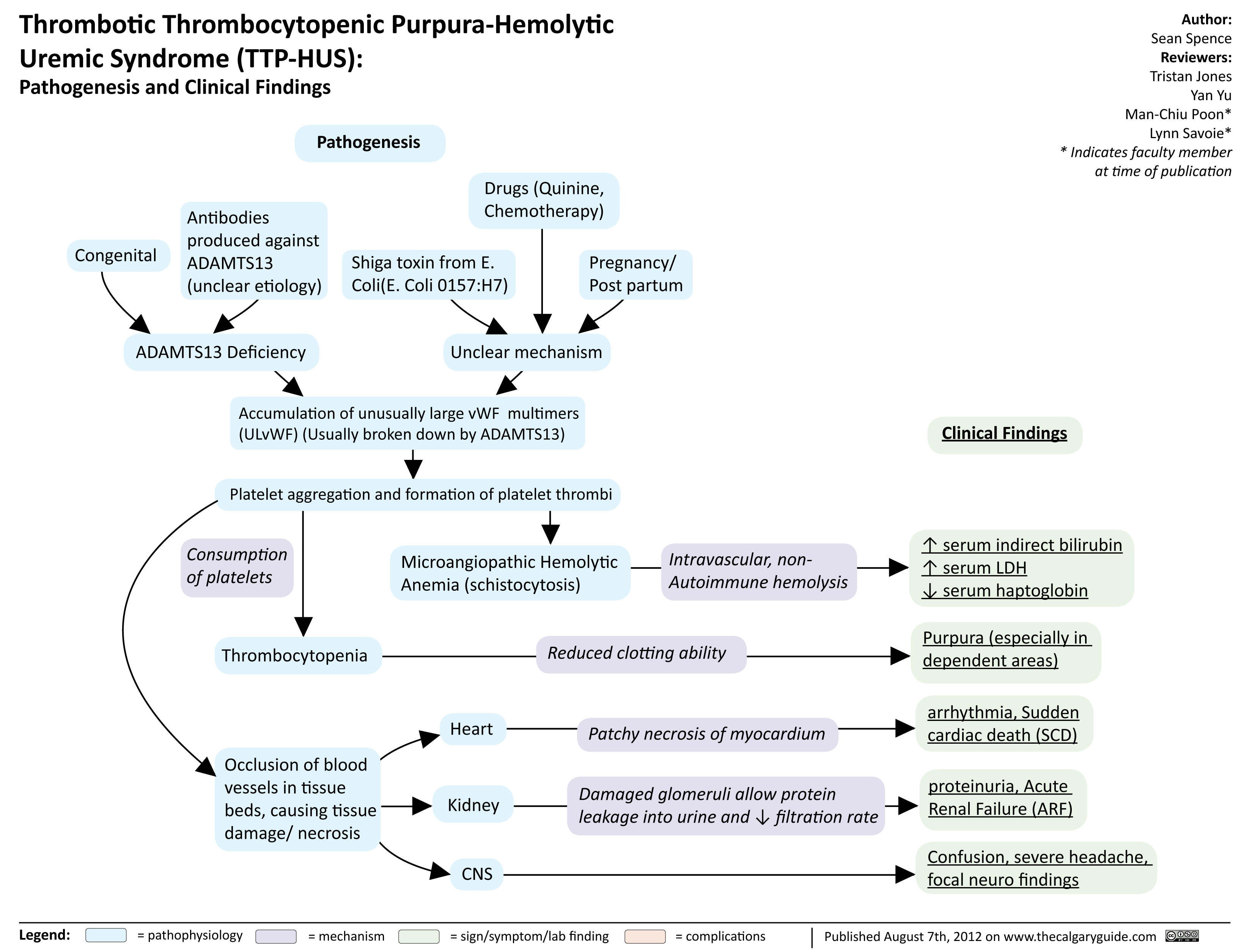
TTP HUS
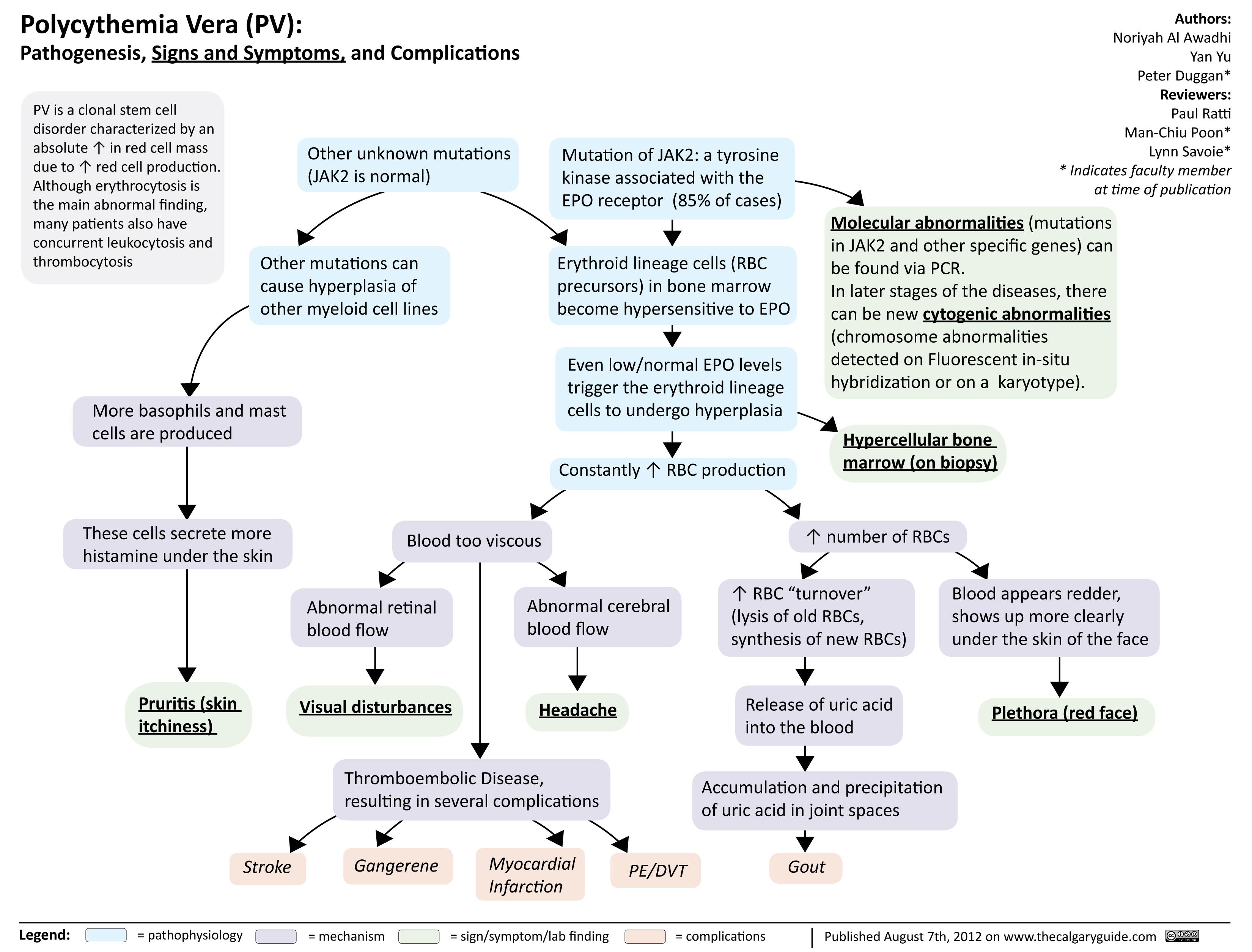
Polycythmia Vera
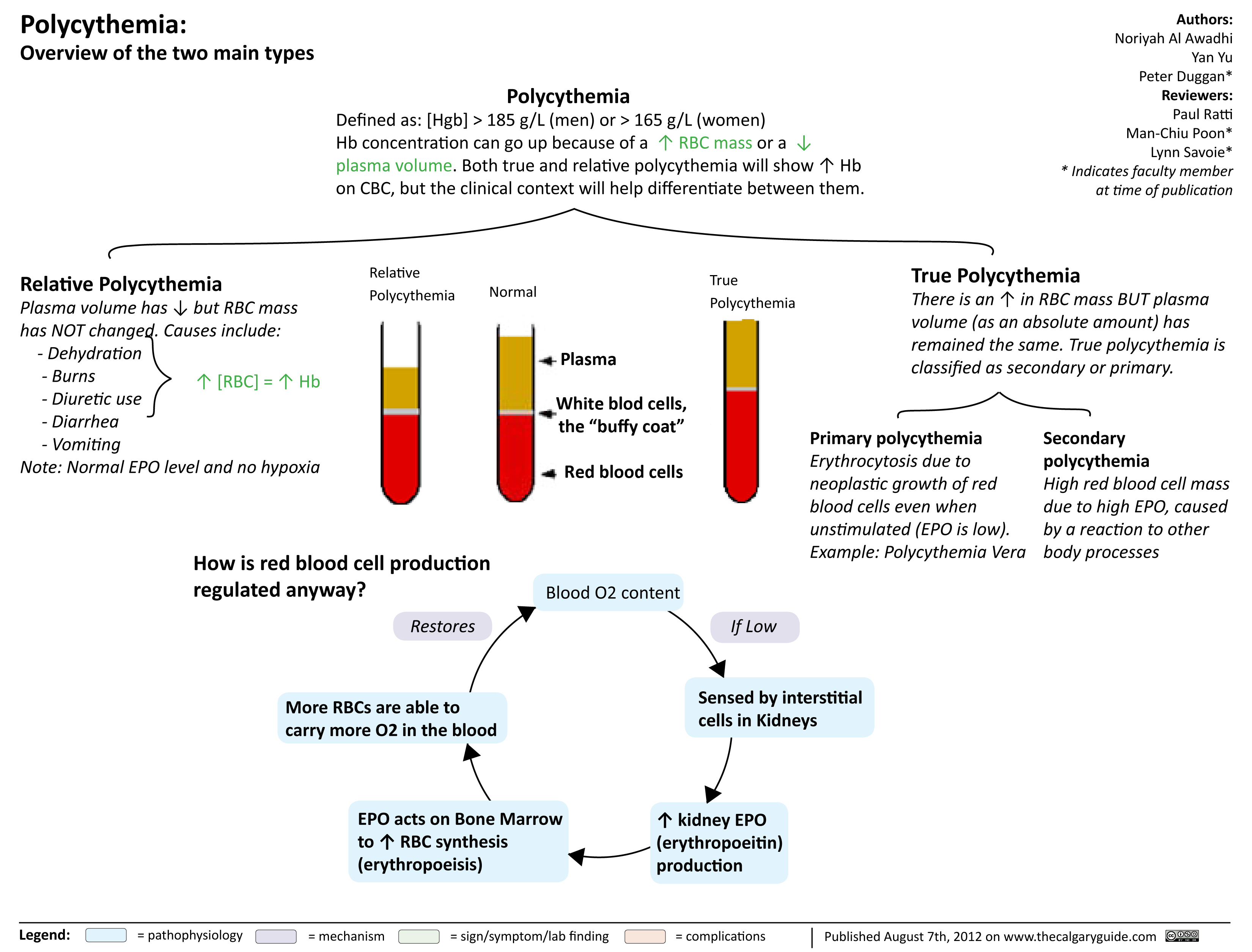
Polycythmia Overview
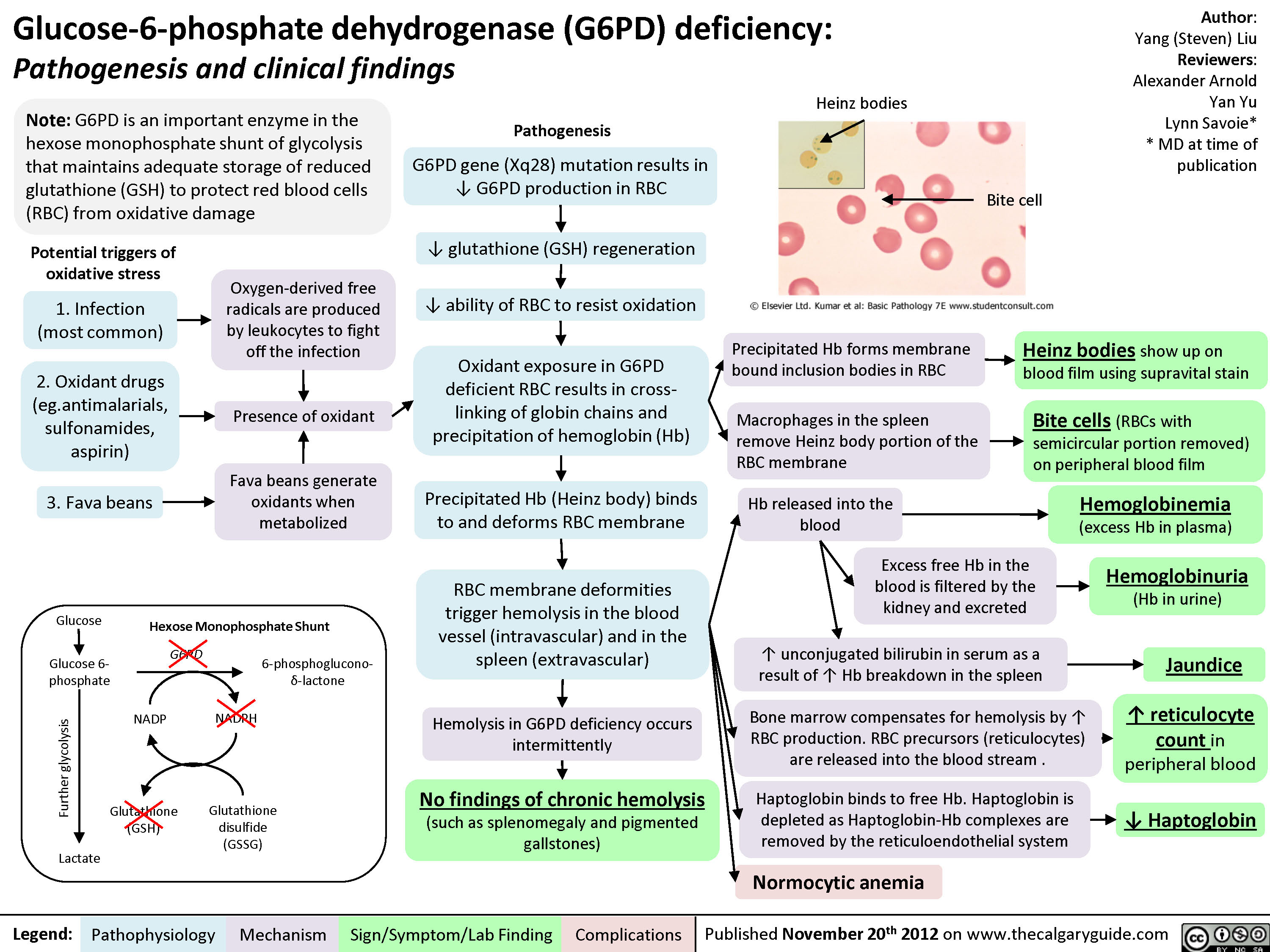
G6PD Deficiency
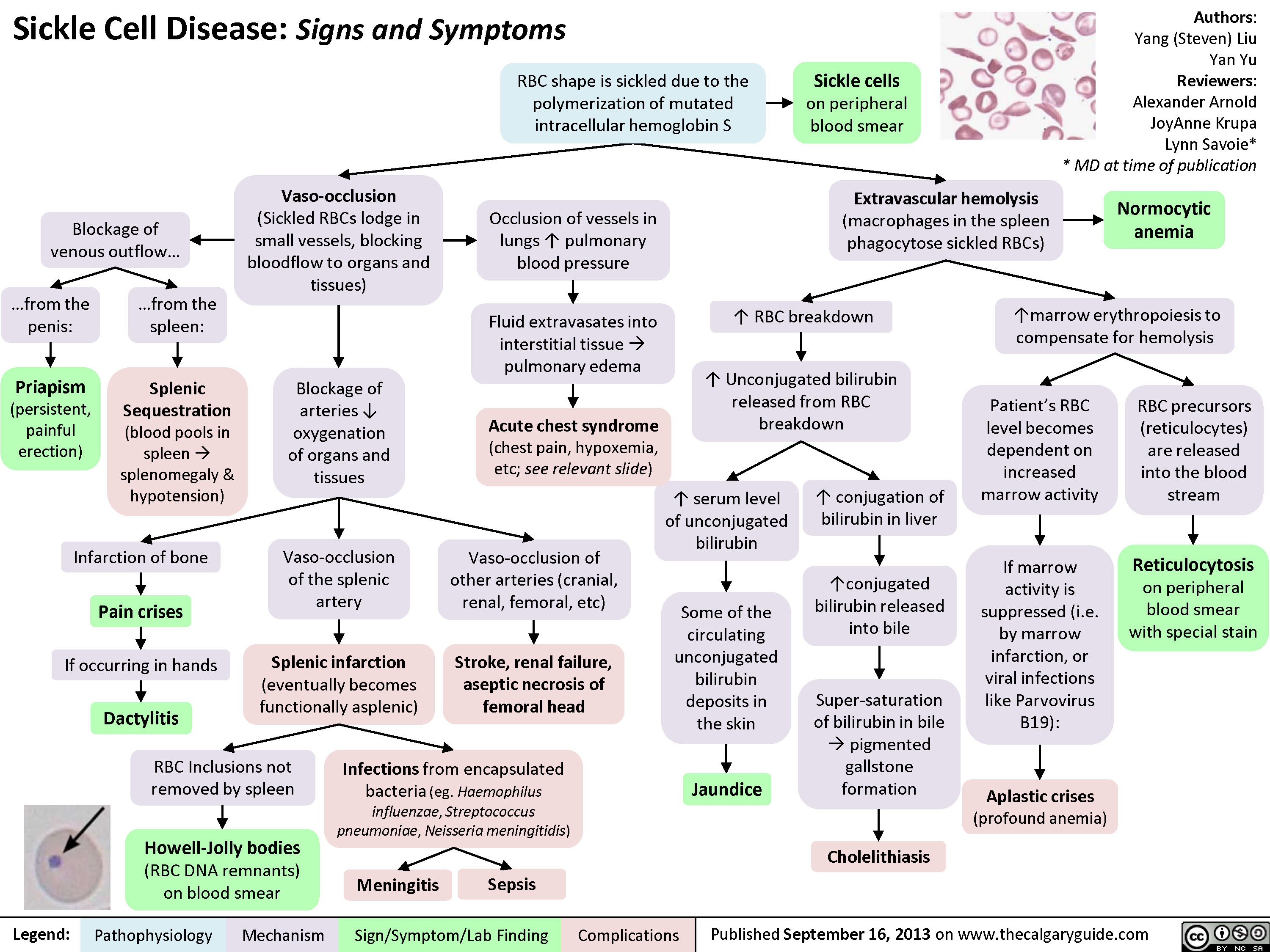
Sickle cell disease signs
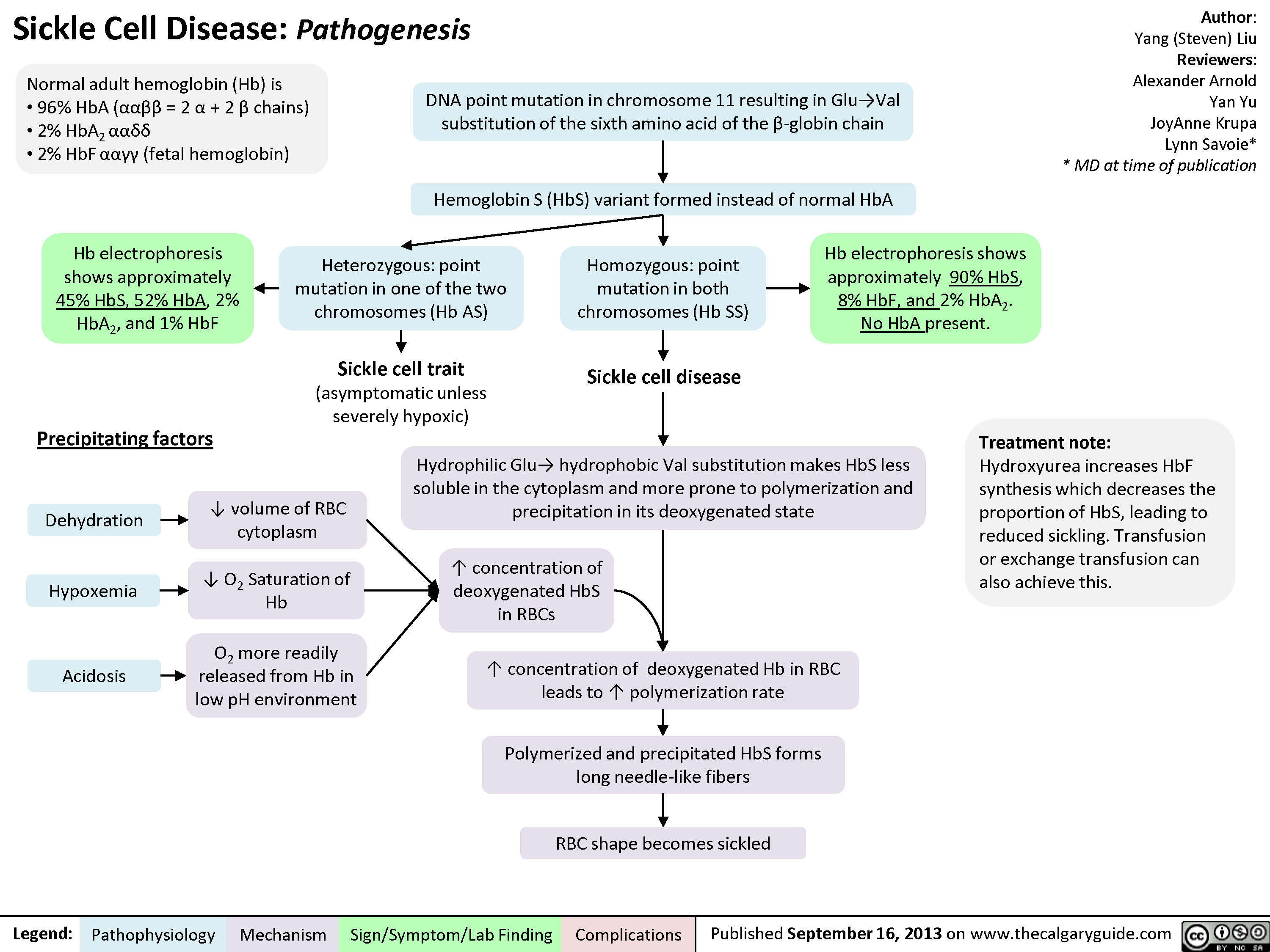
Sickle cell disease
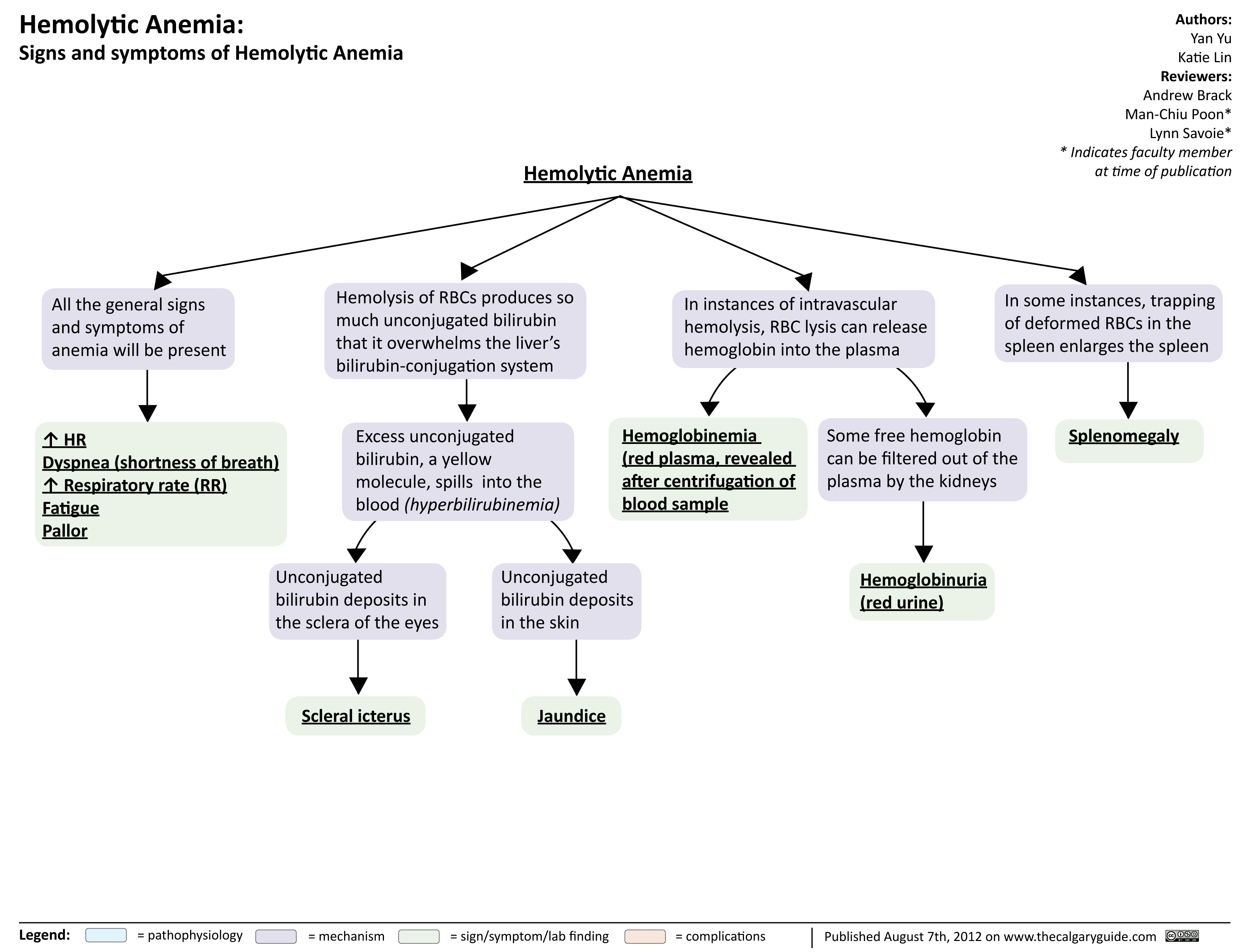
Hemolytic Anemia Signs and Symptoms
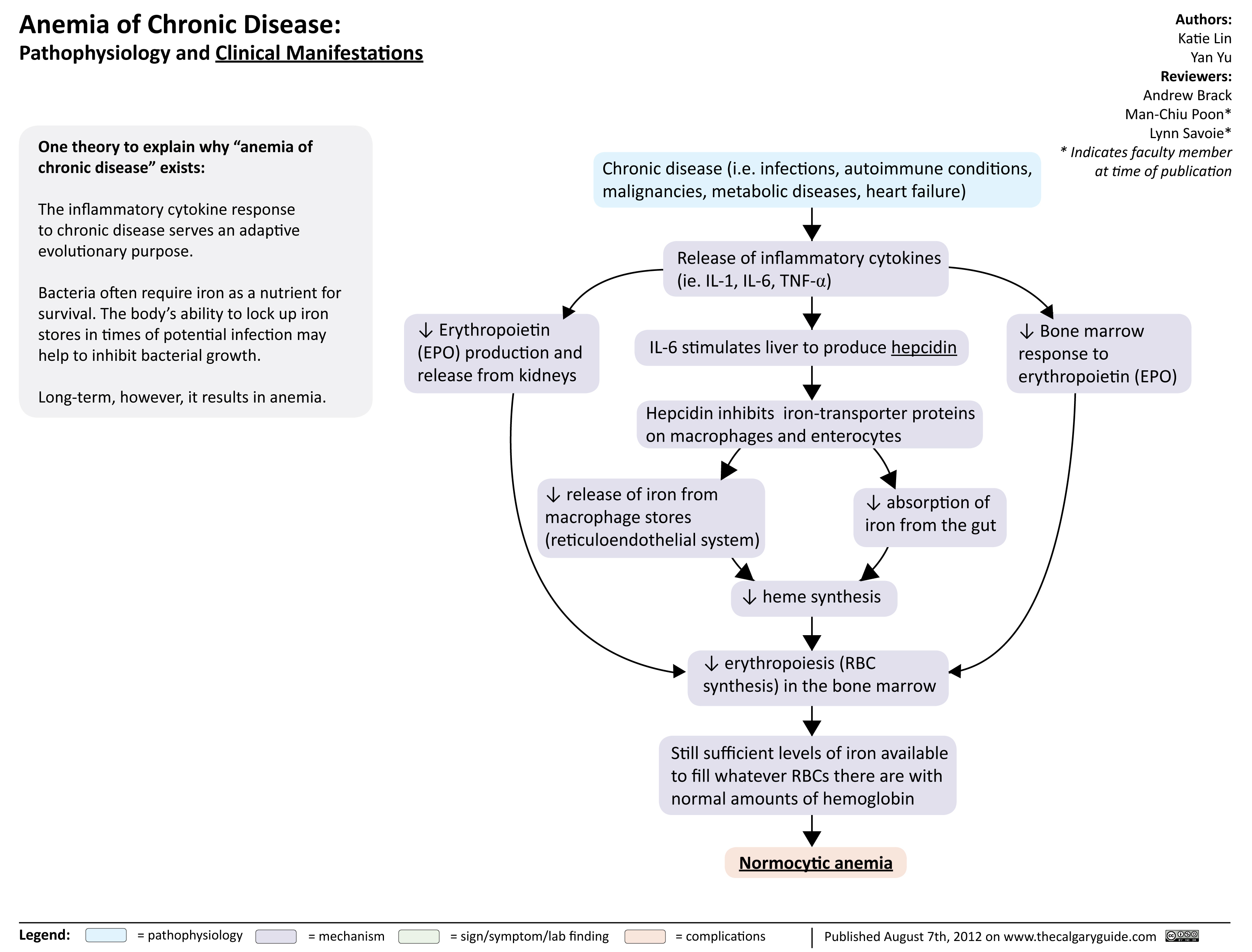
Anemia of Chronic Disease
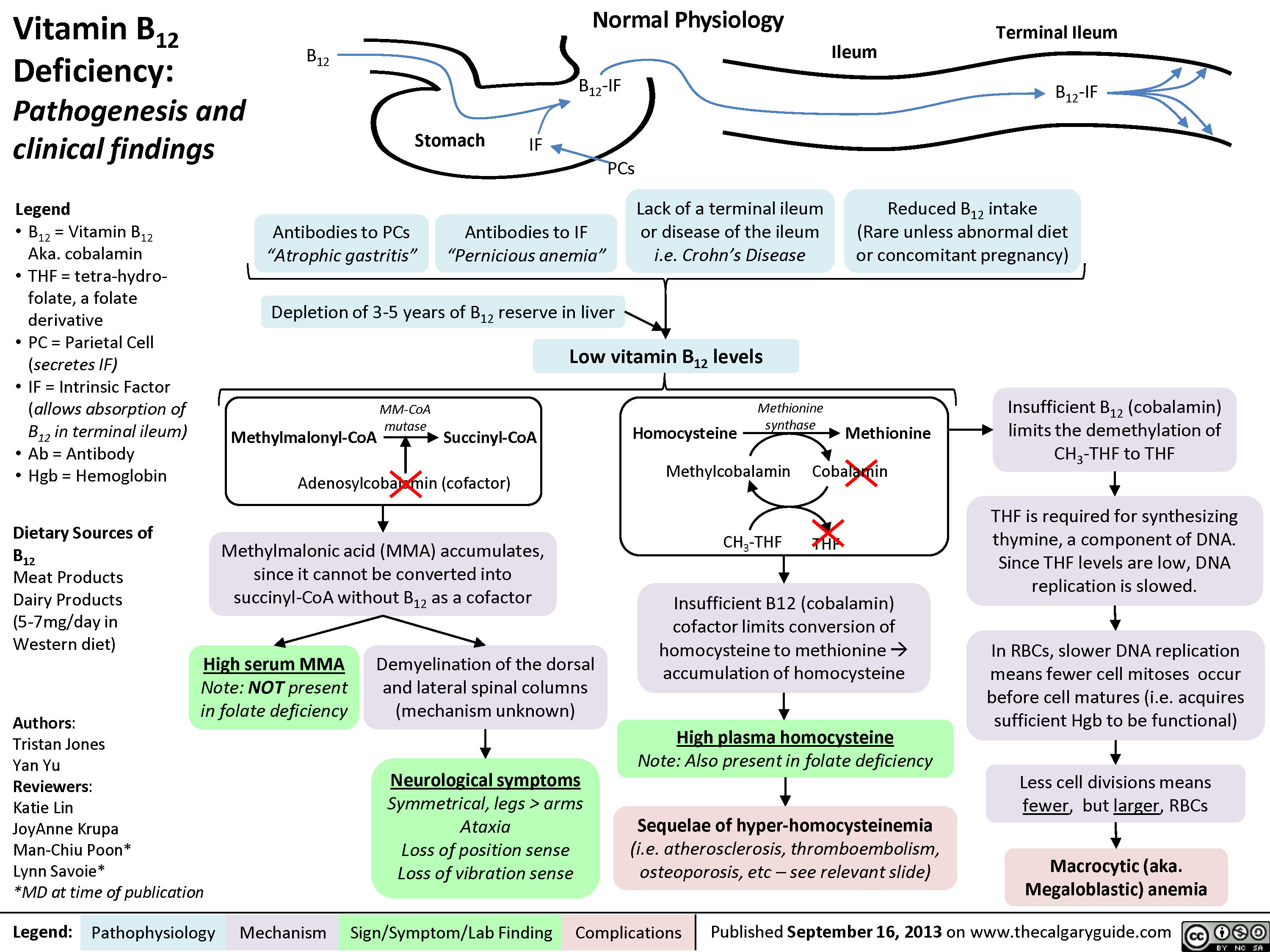
Vitamin B12 Deficiency
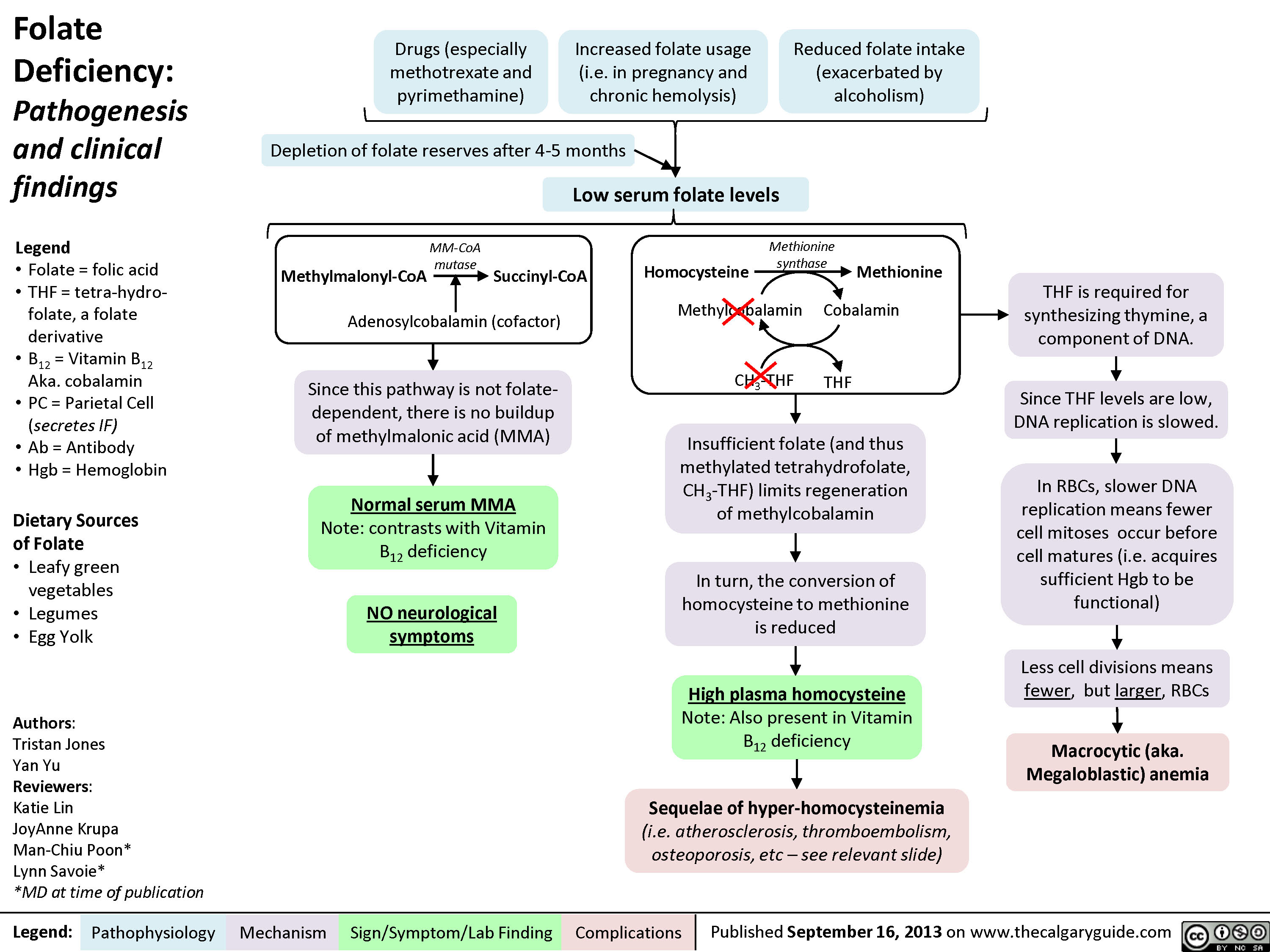
Folate Deficiency
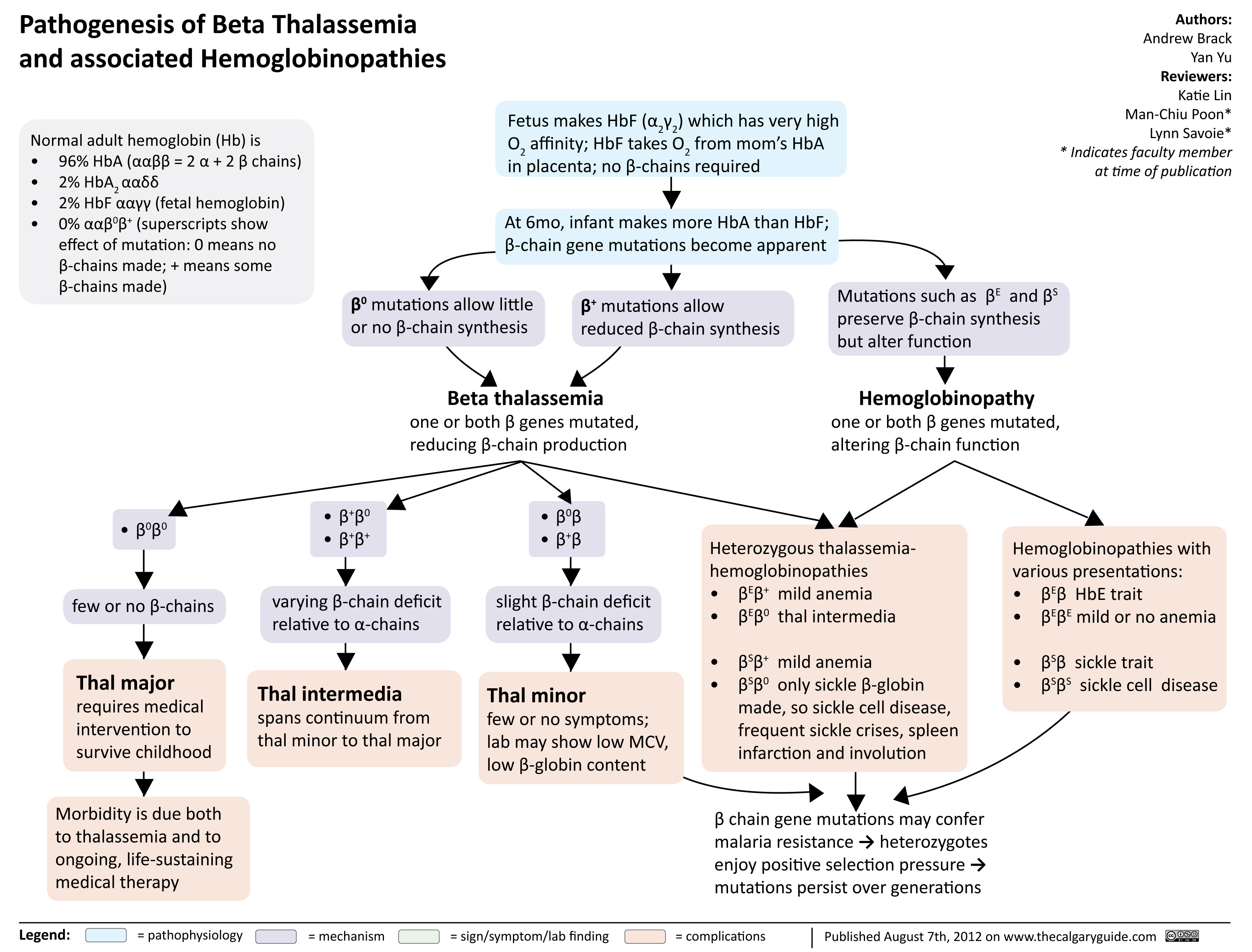
Pathogenesis of Beta Thalassemia
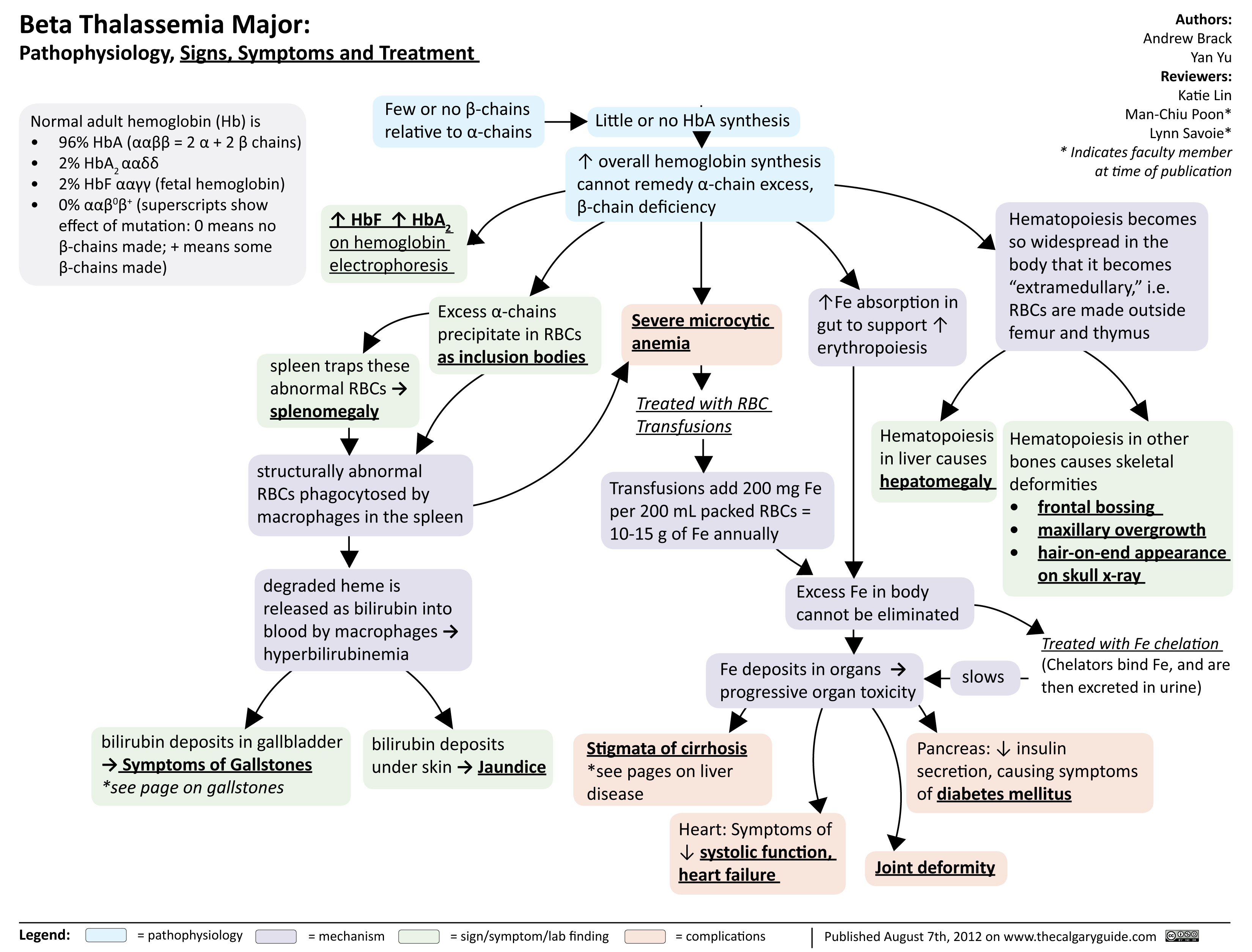
Beta Thalassemia Signs Symptoms Treatment
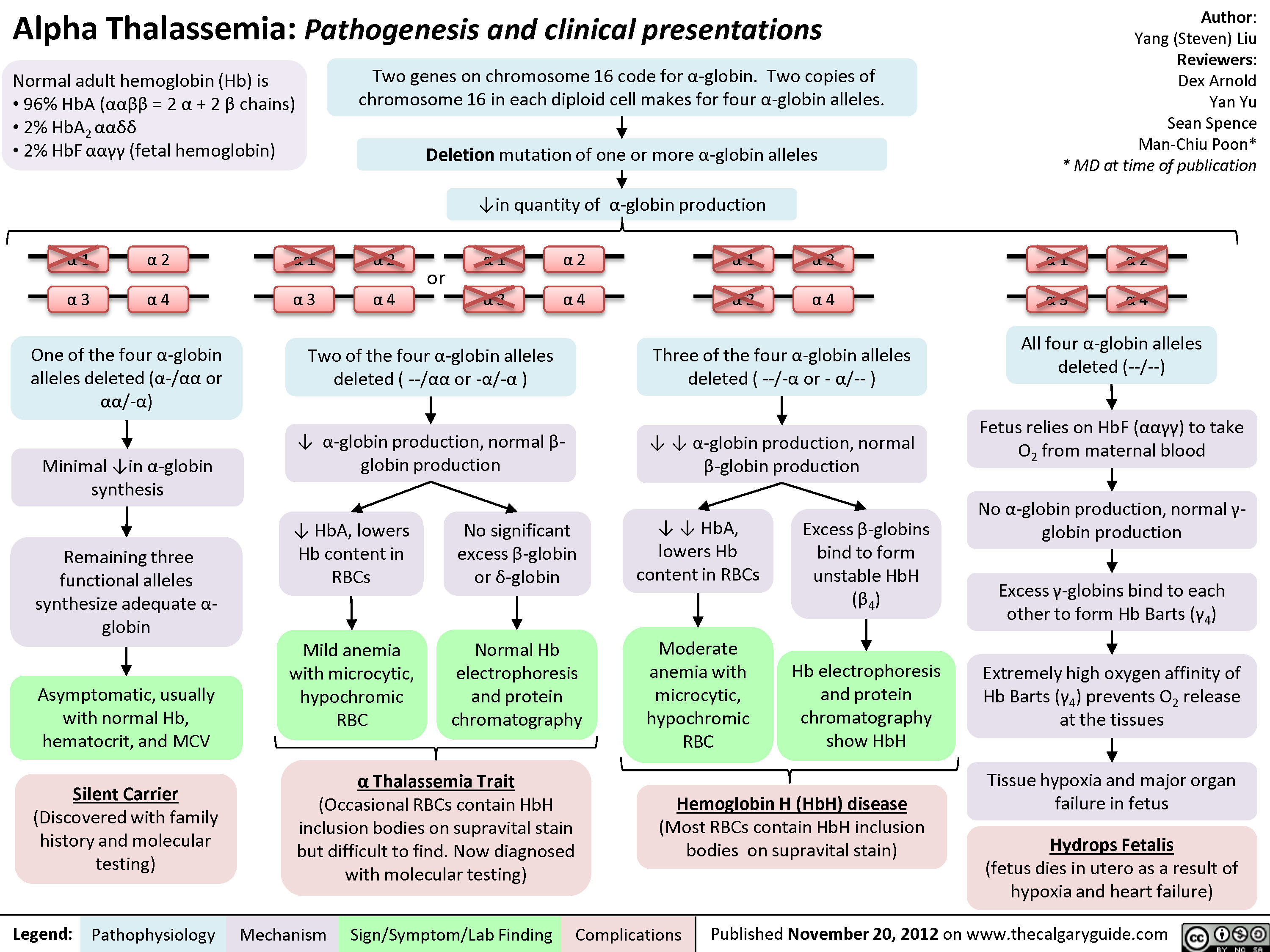
Alpha Thalassemia Pathogenesis
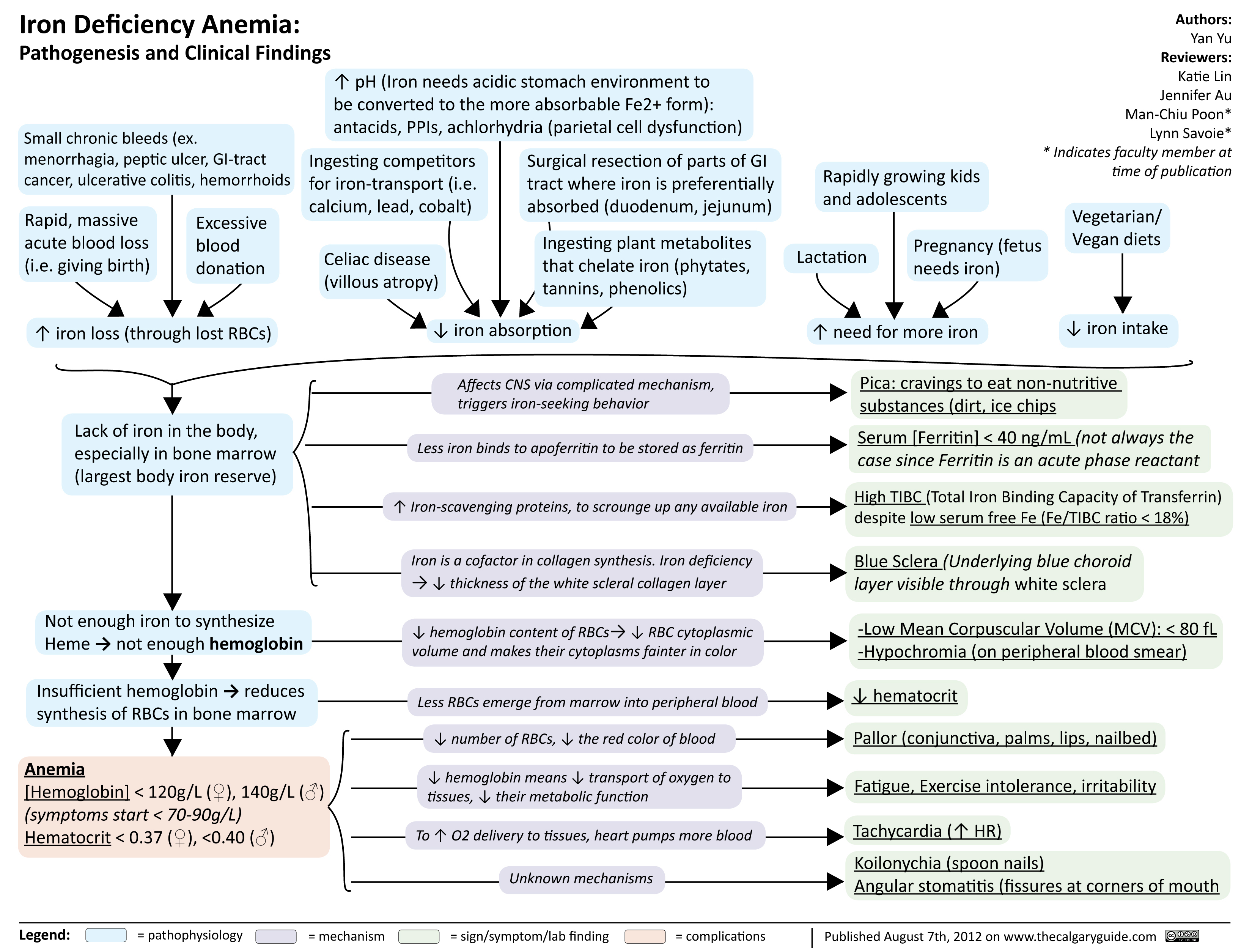
Iron Deficiency Anemia
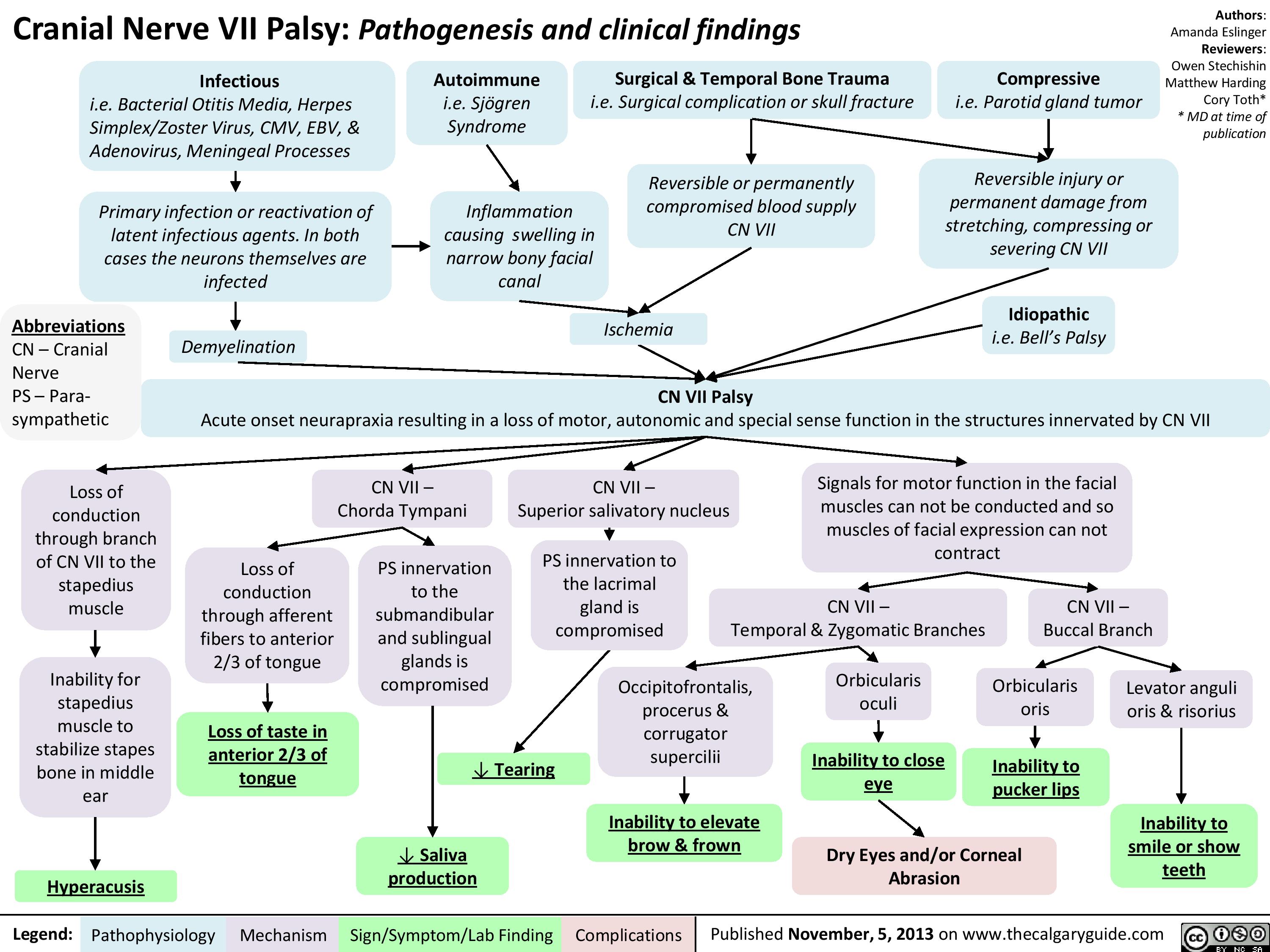
CNVII_Bells Palsy
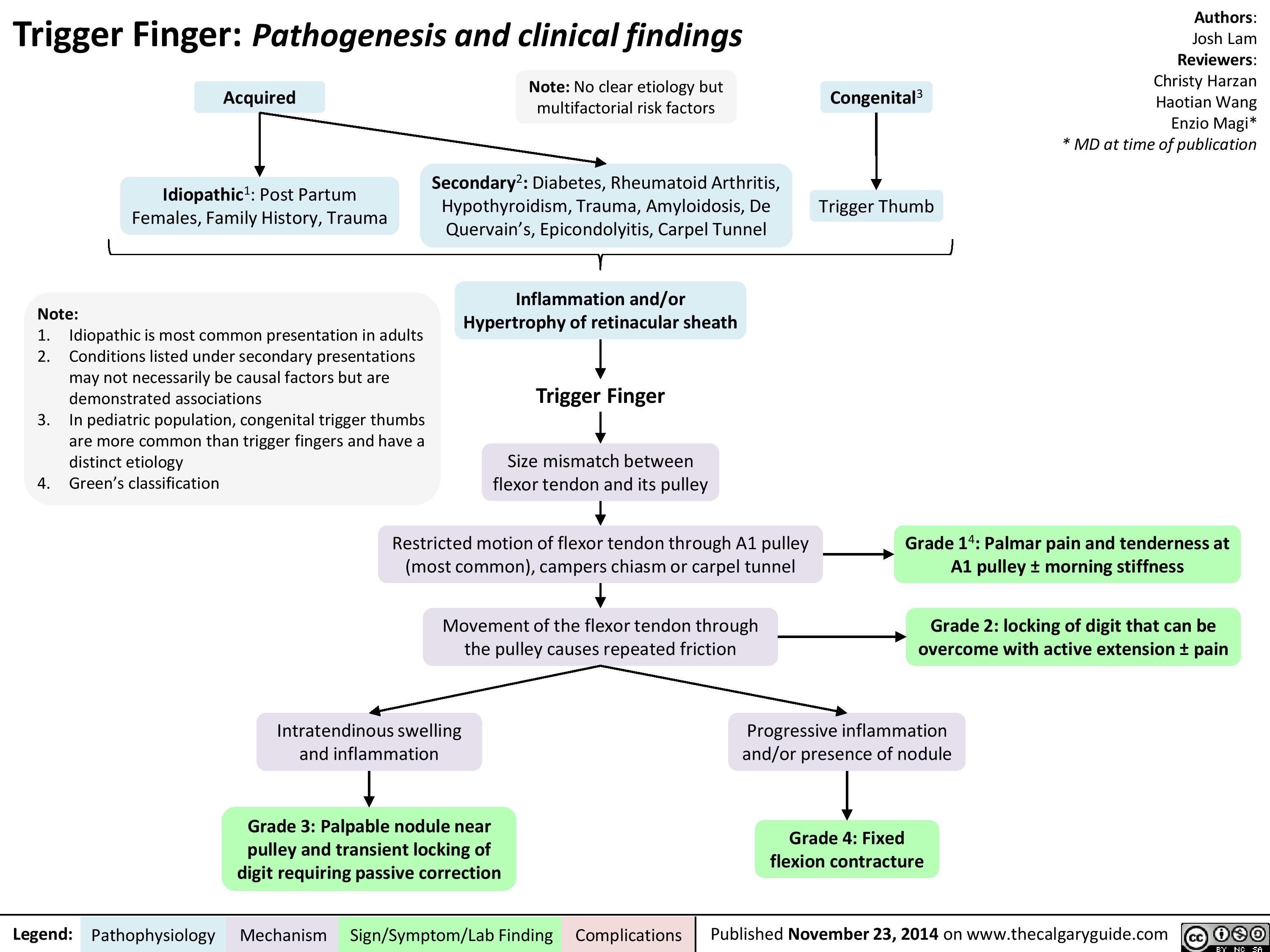
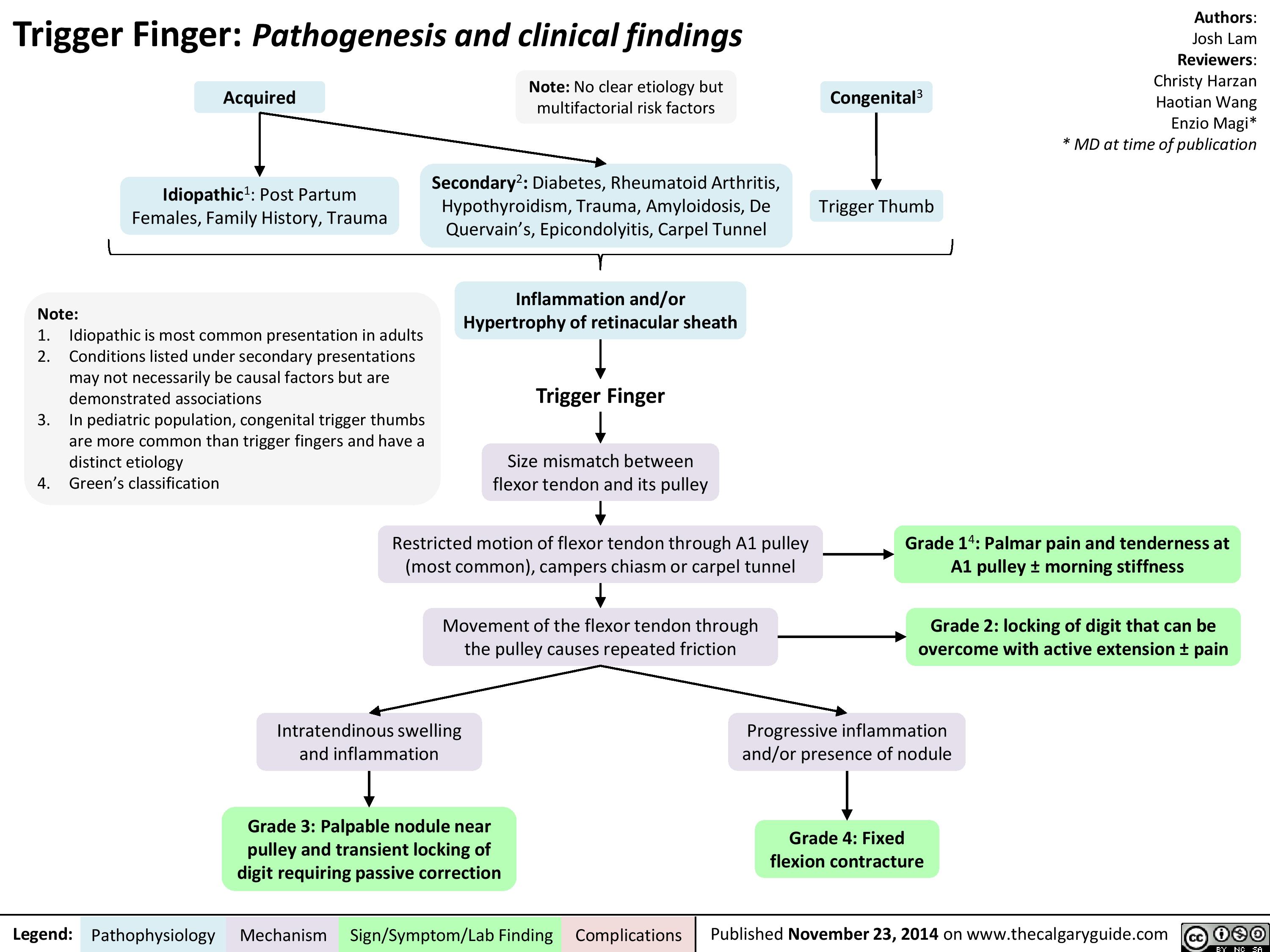
Trigger Finger
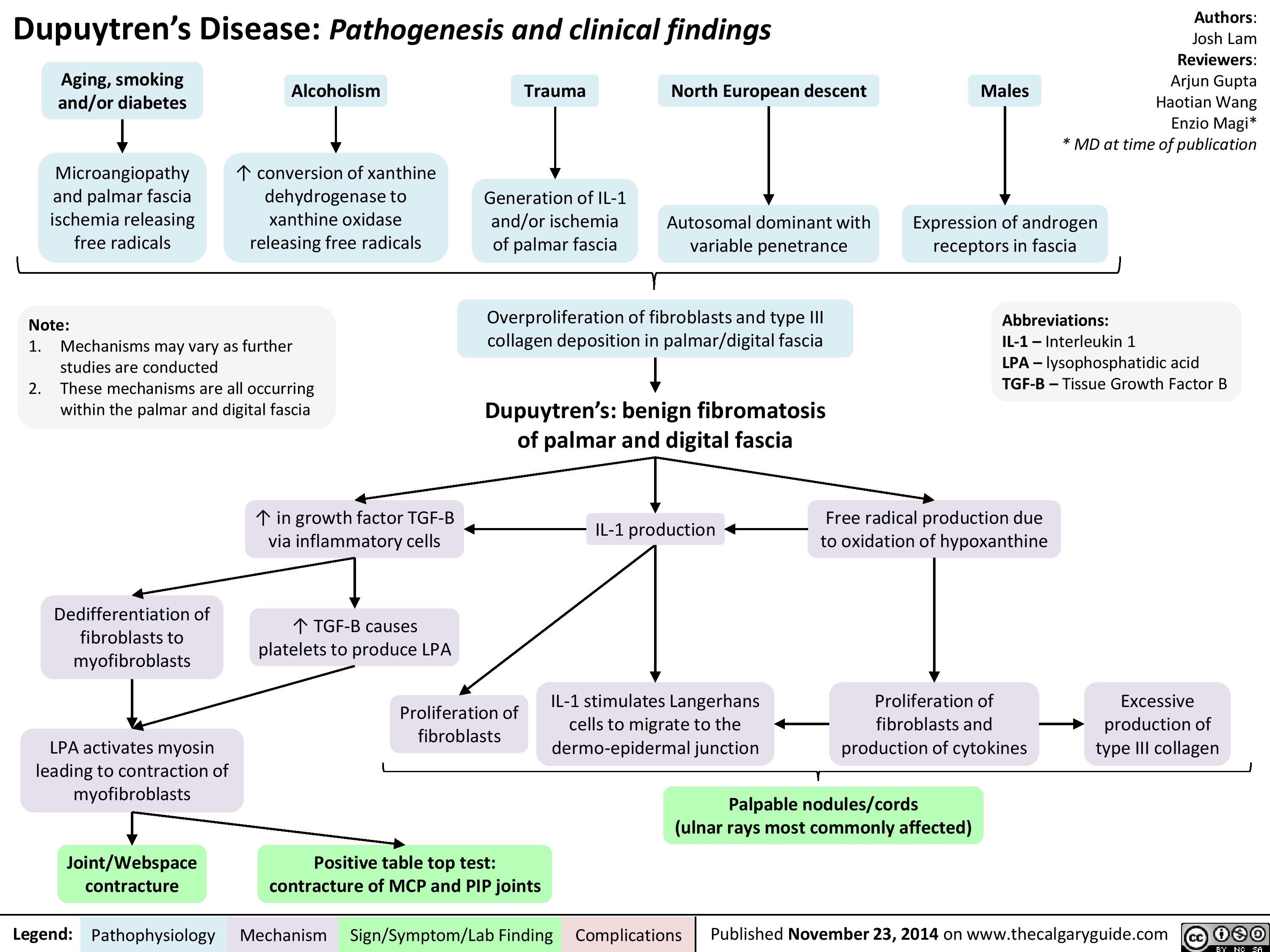
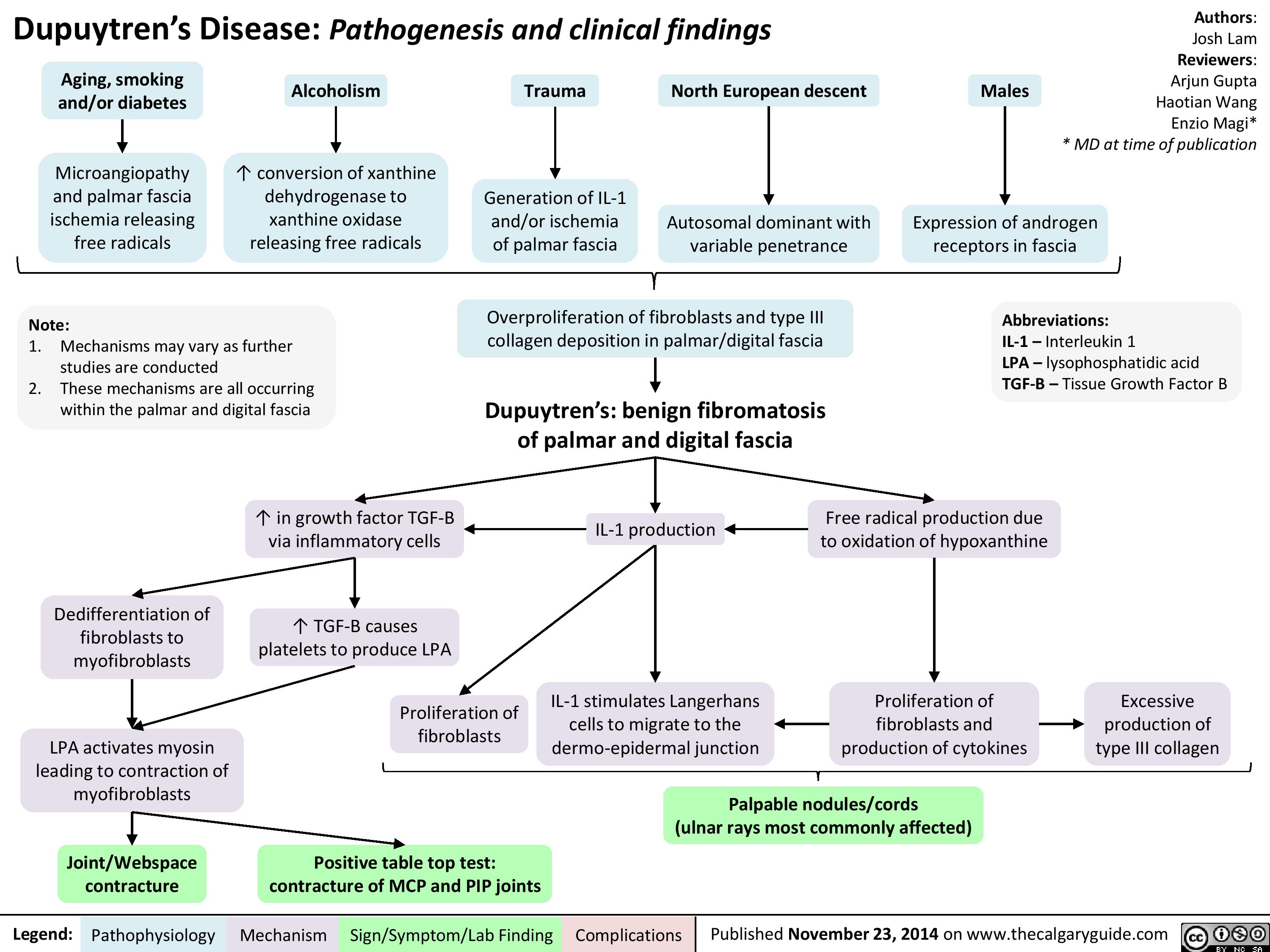
Dupuytren
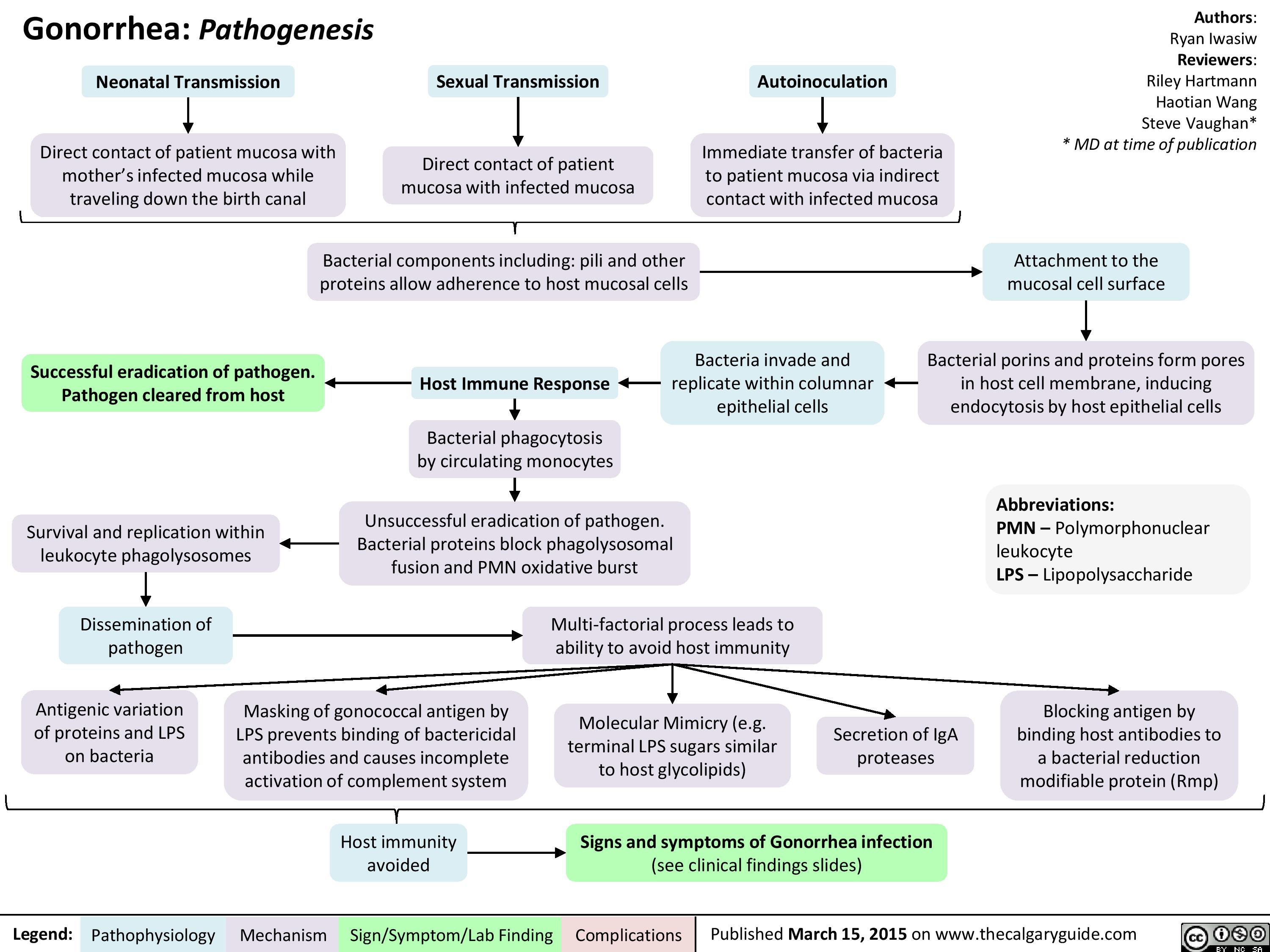
Gonorrhea Pathogenesis
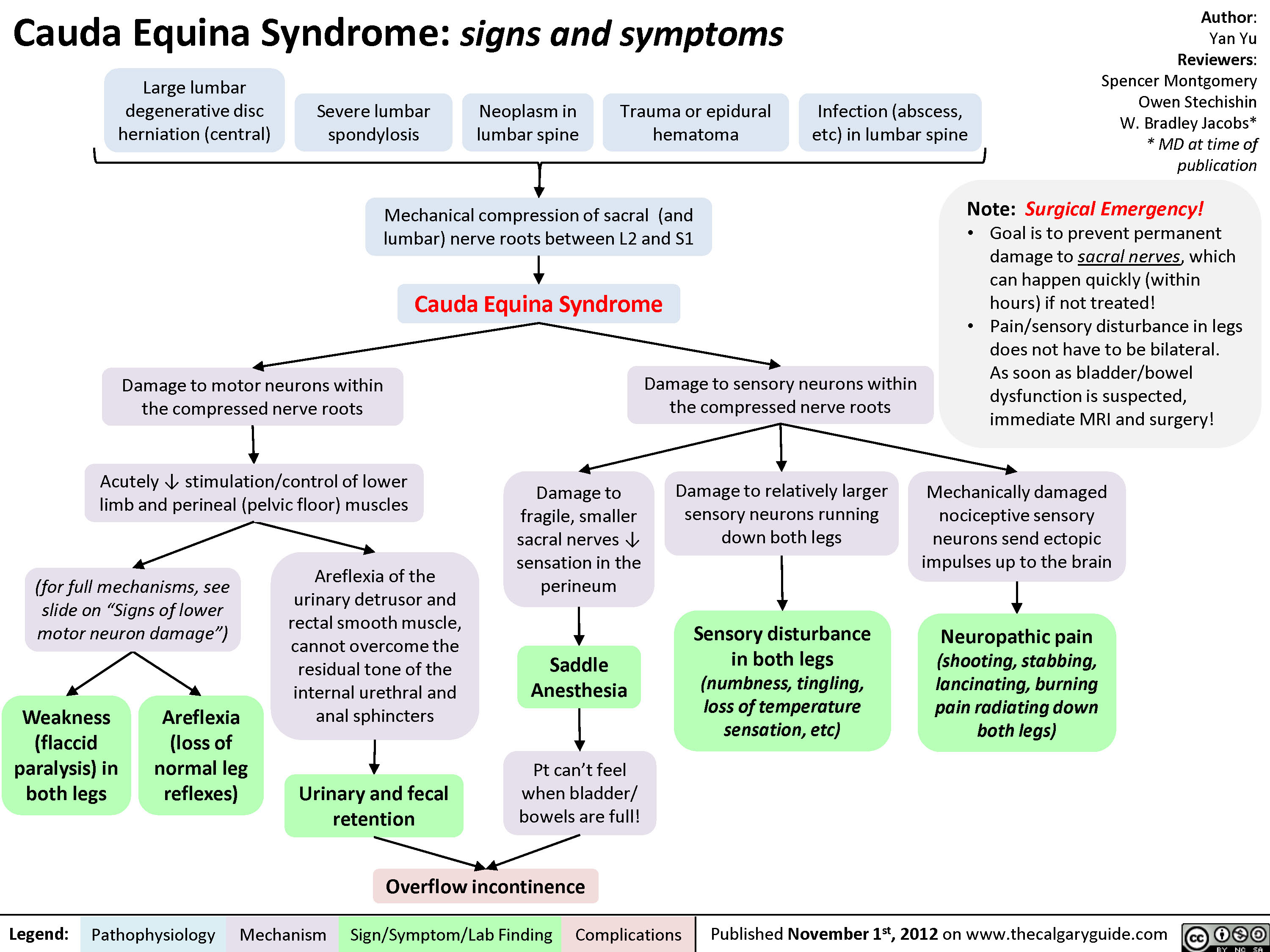
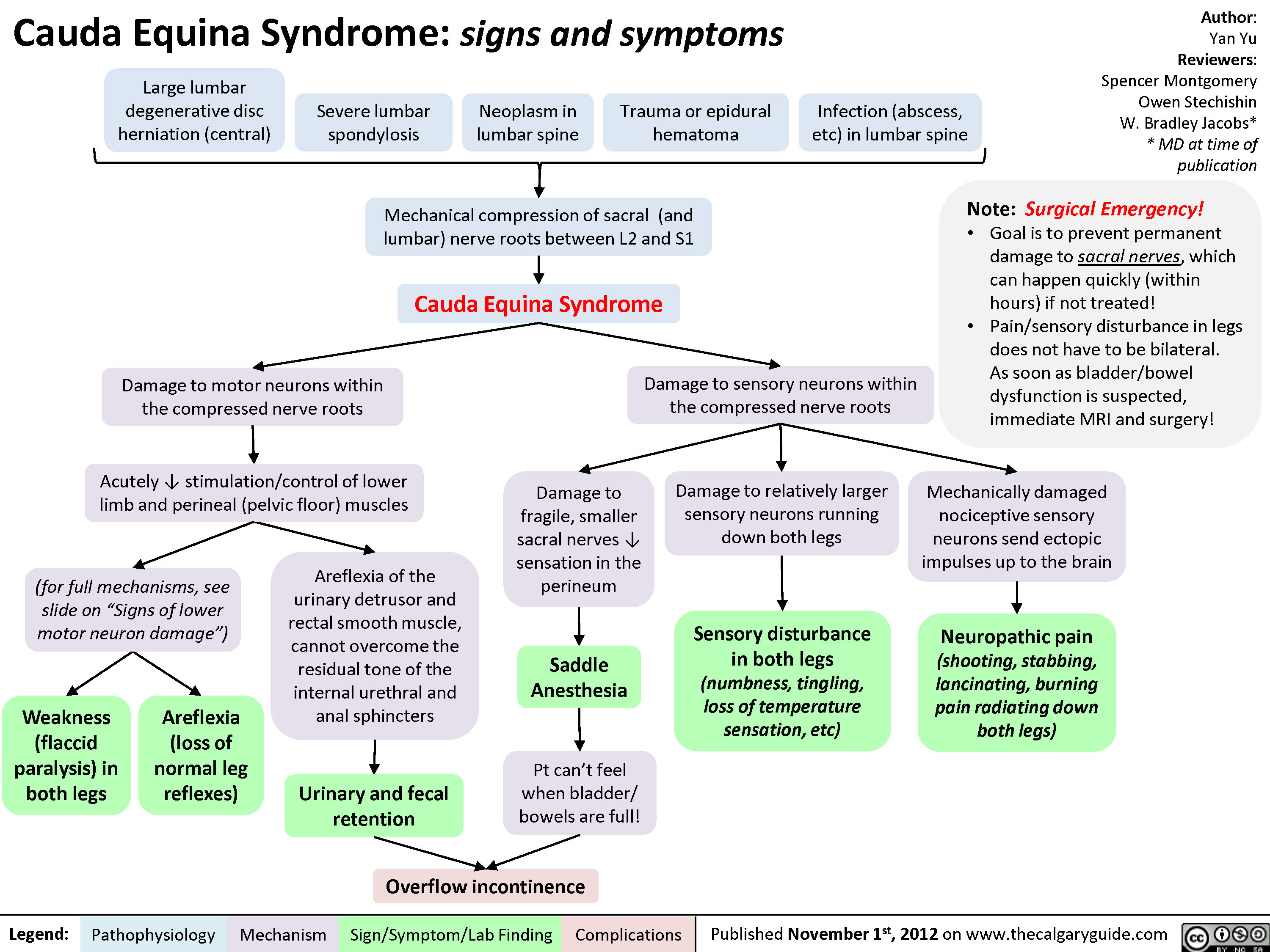
Cauda Equina Syndrome
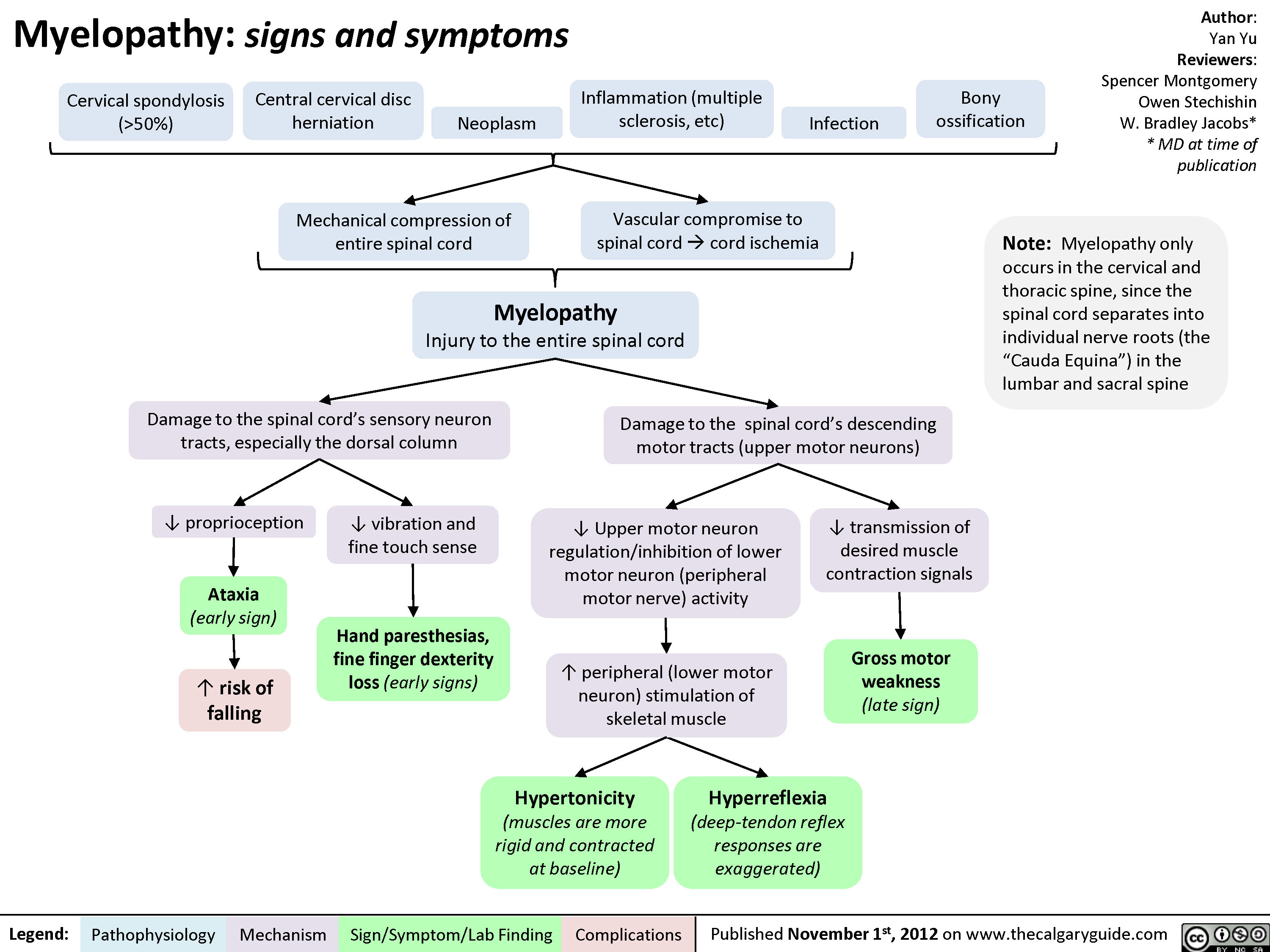
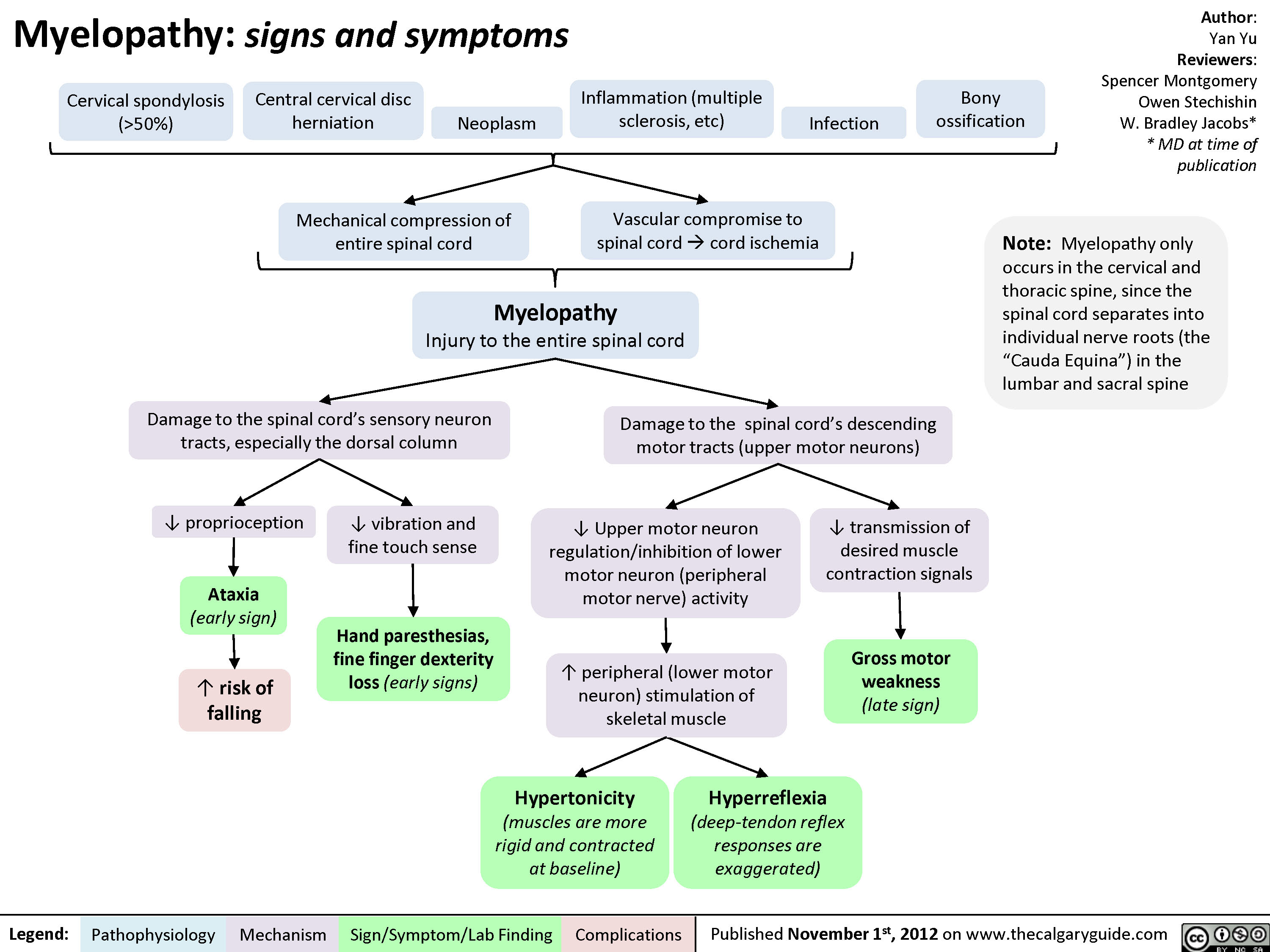
Myelopathy
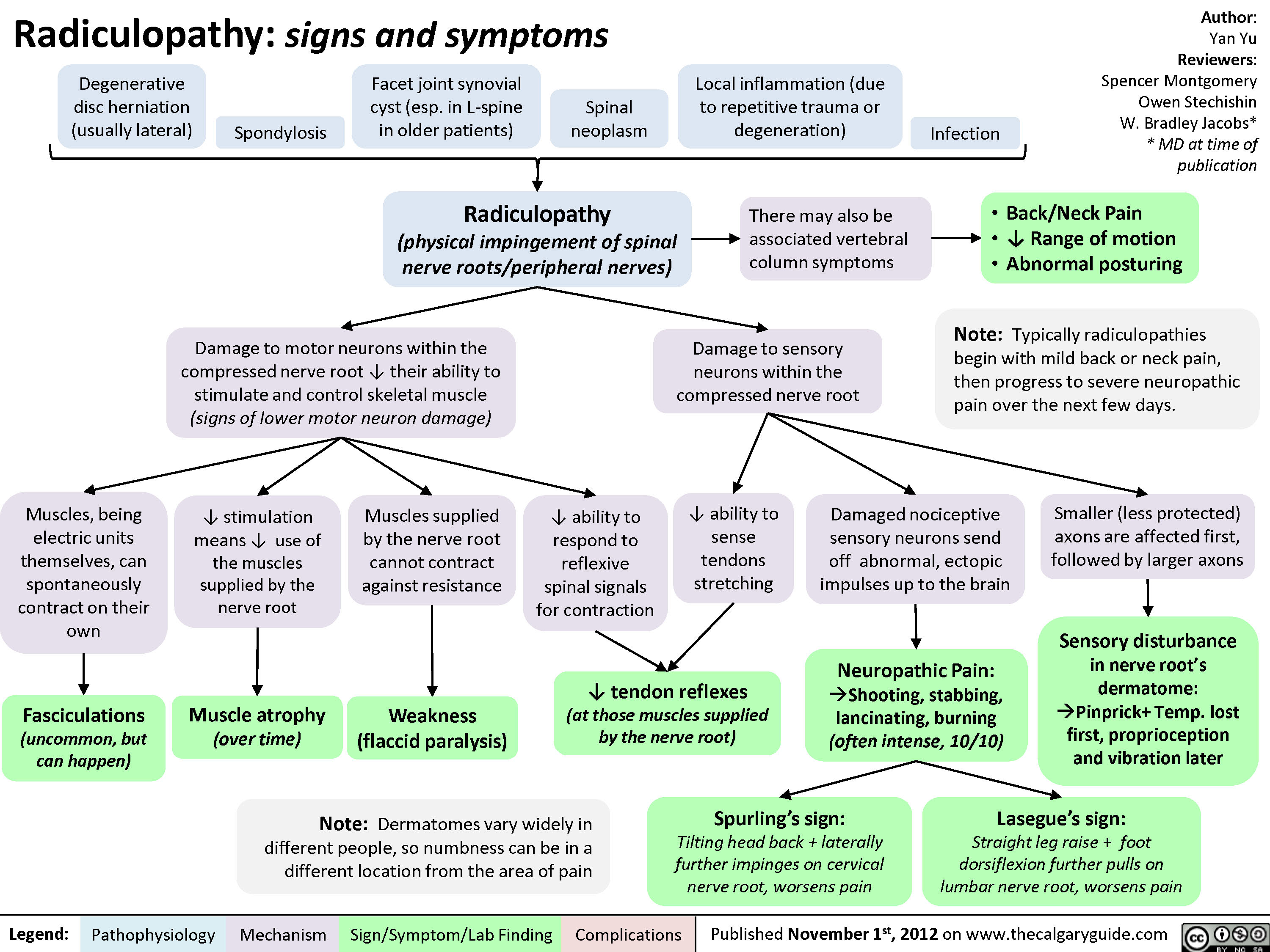
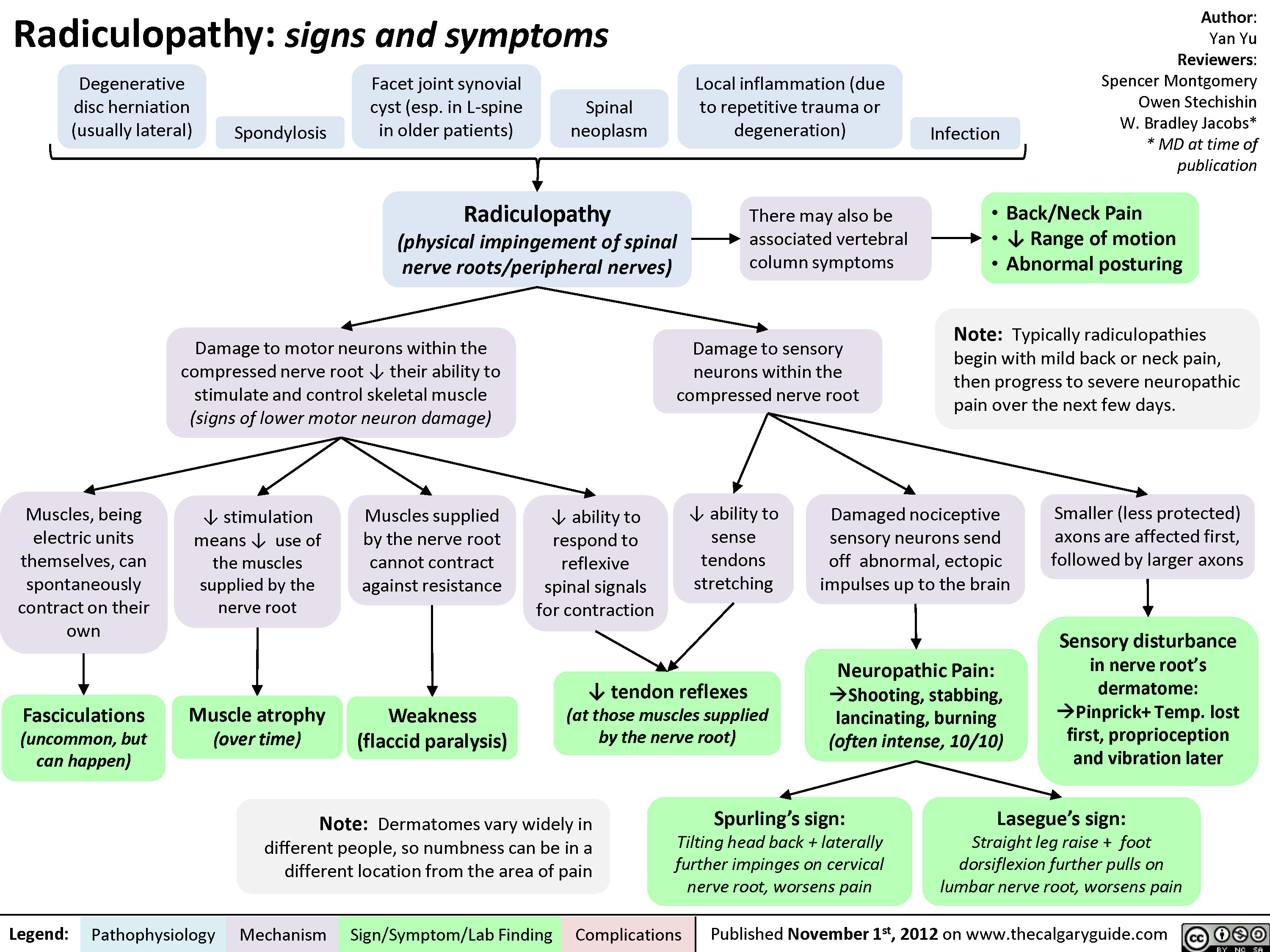
Radiculopathy
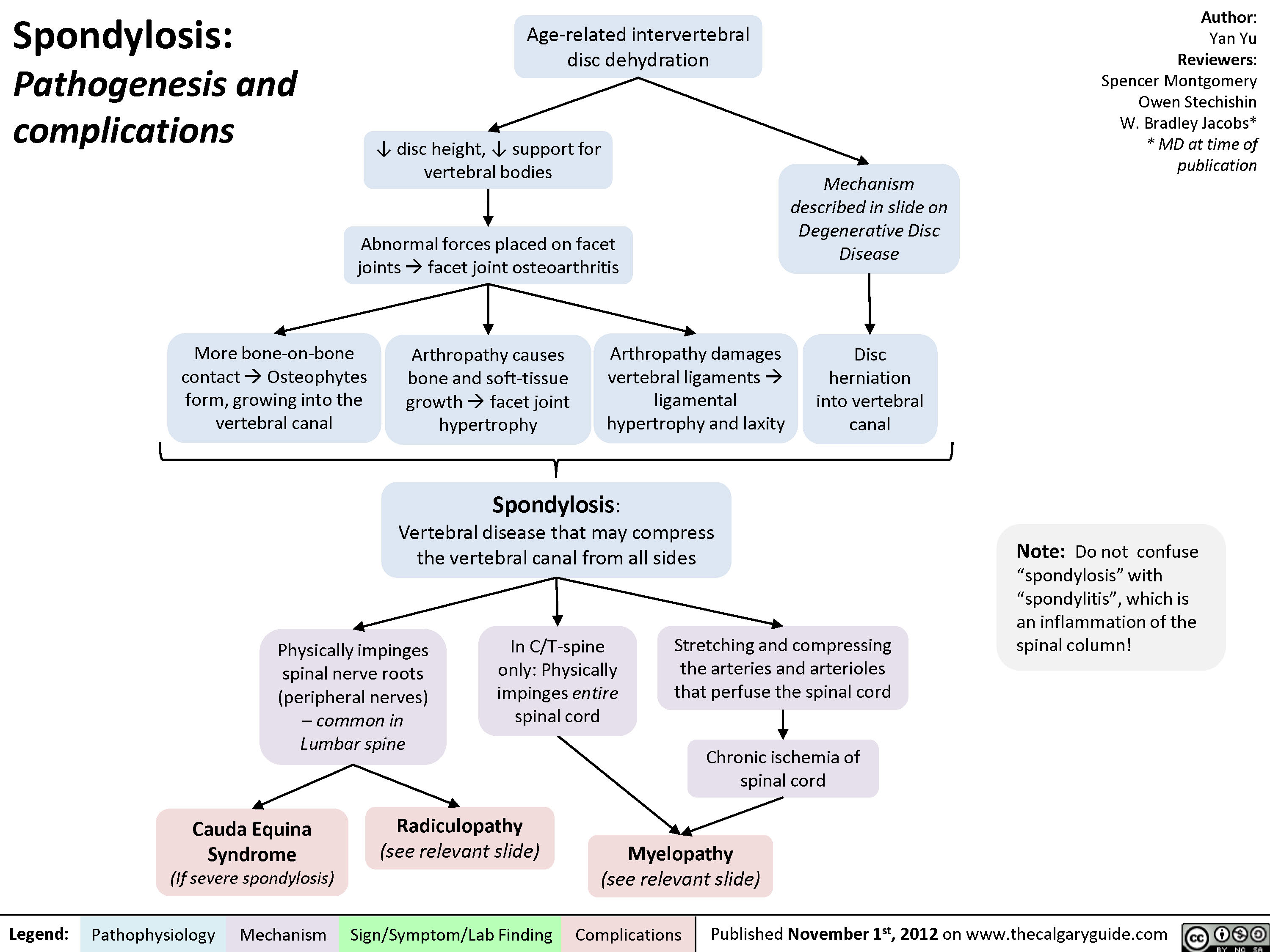
Spondylosis
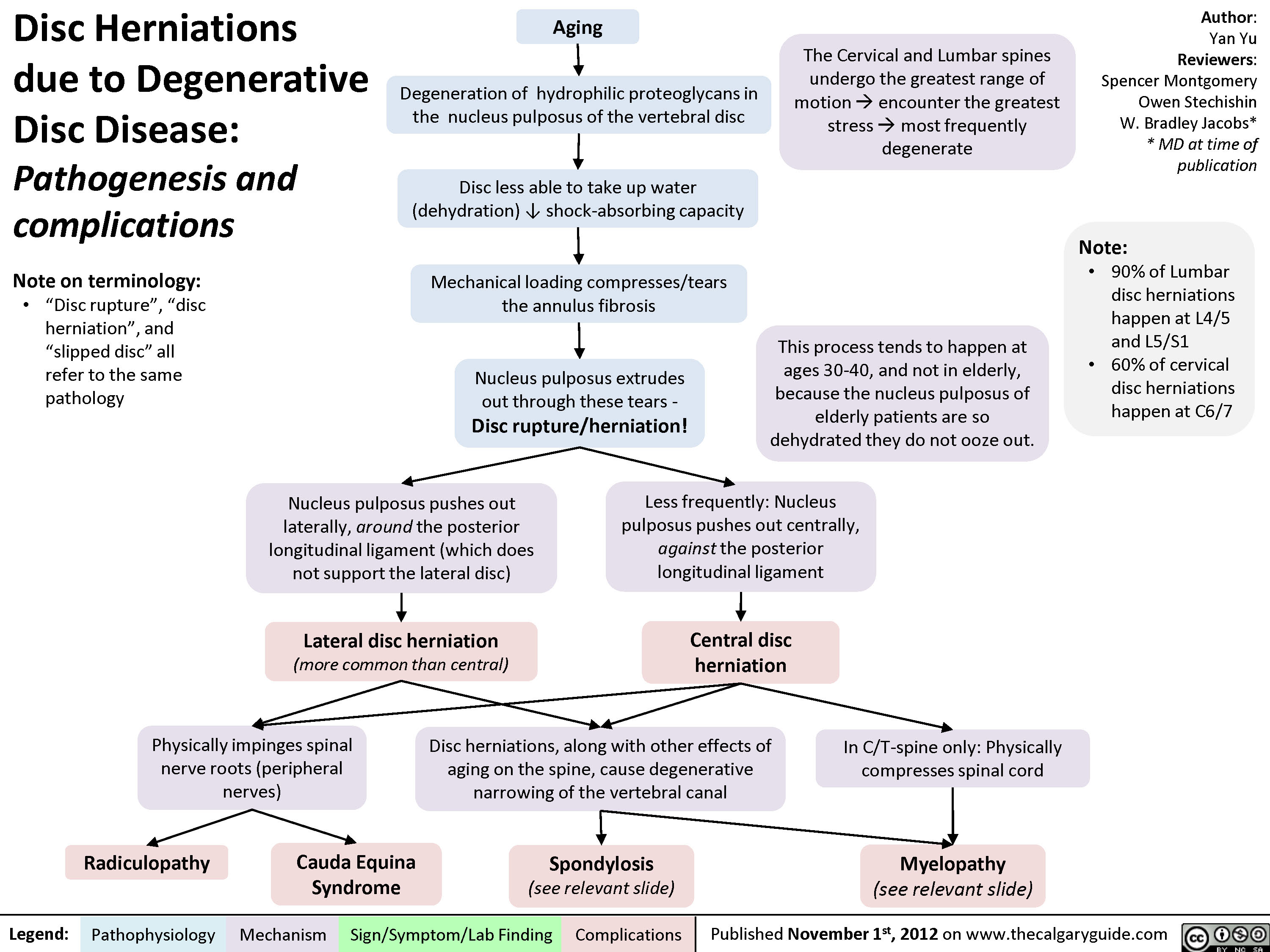
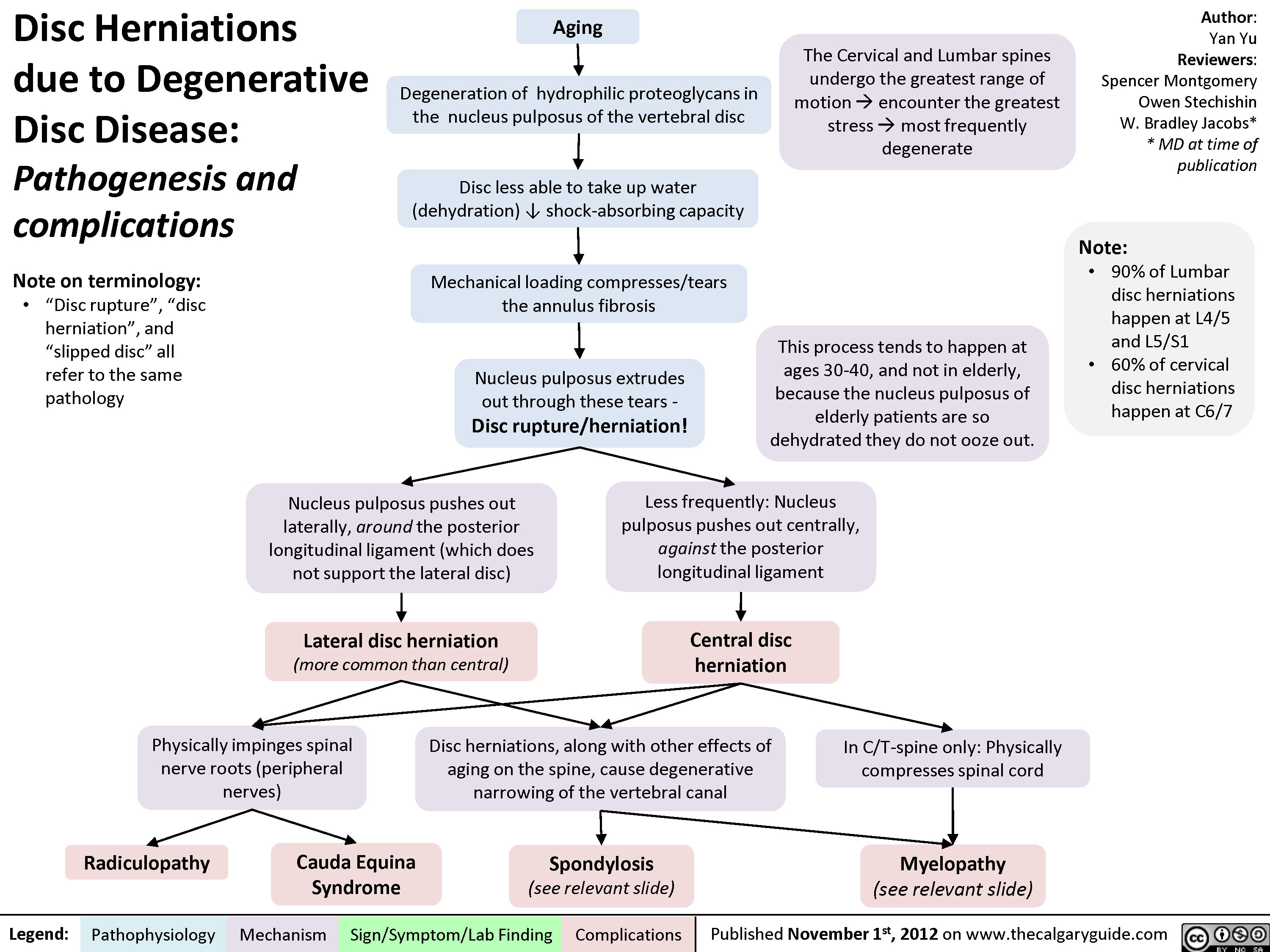
Disc Herniations
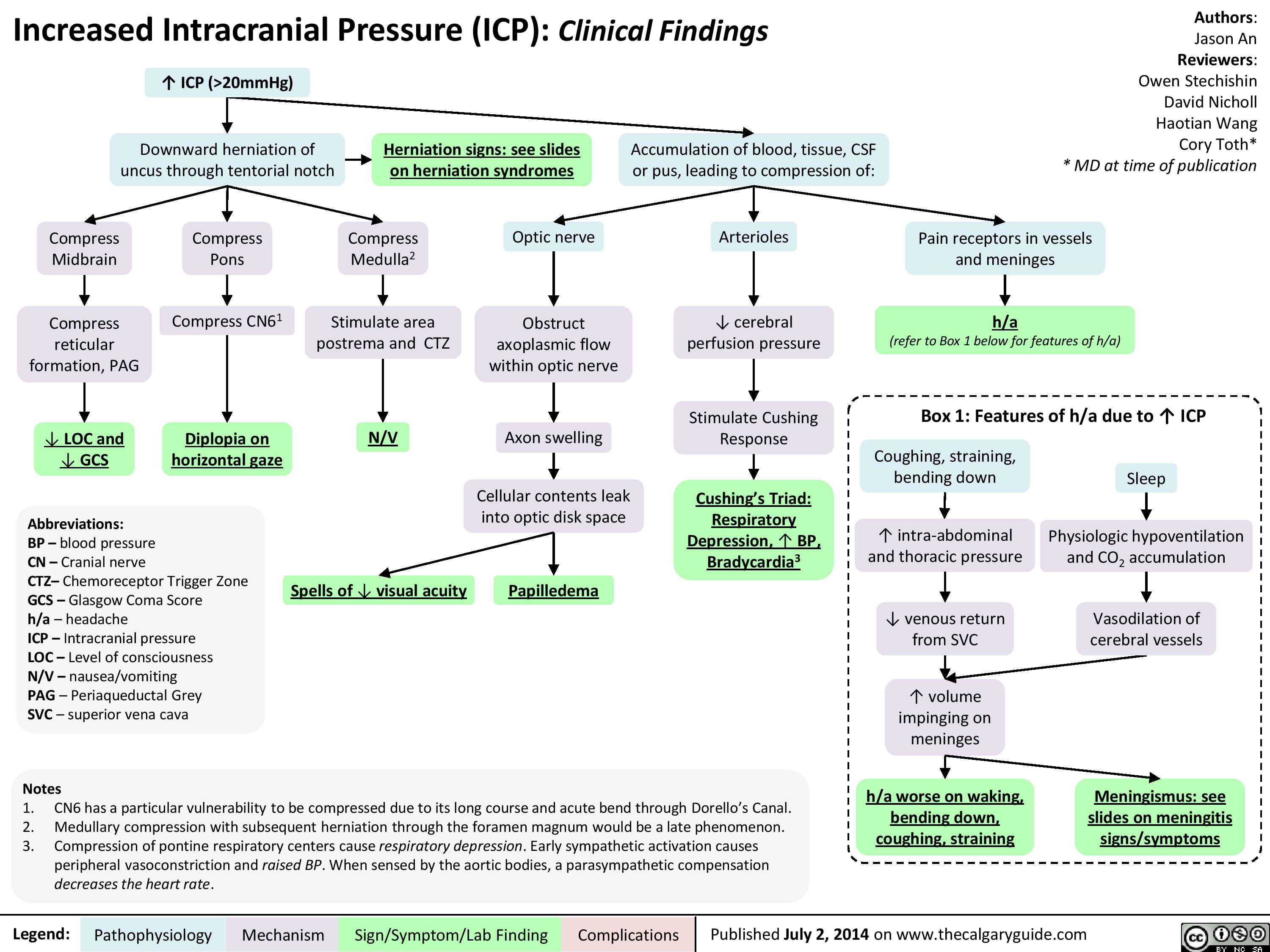
Presentation of increased ICP
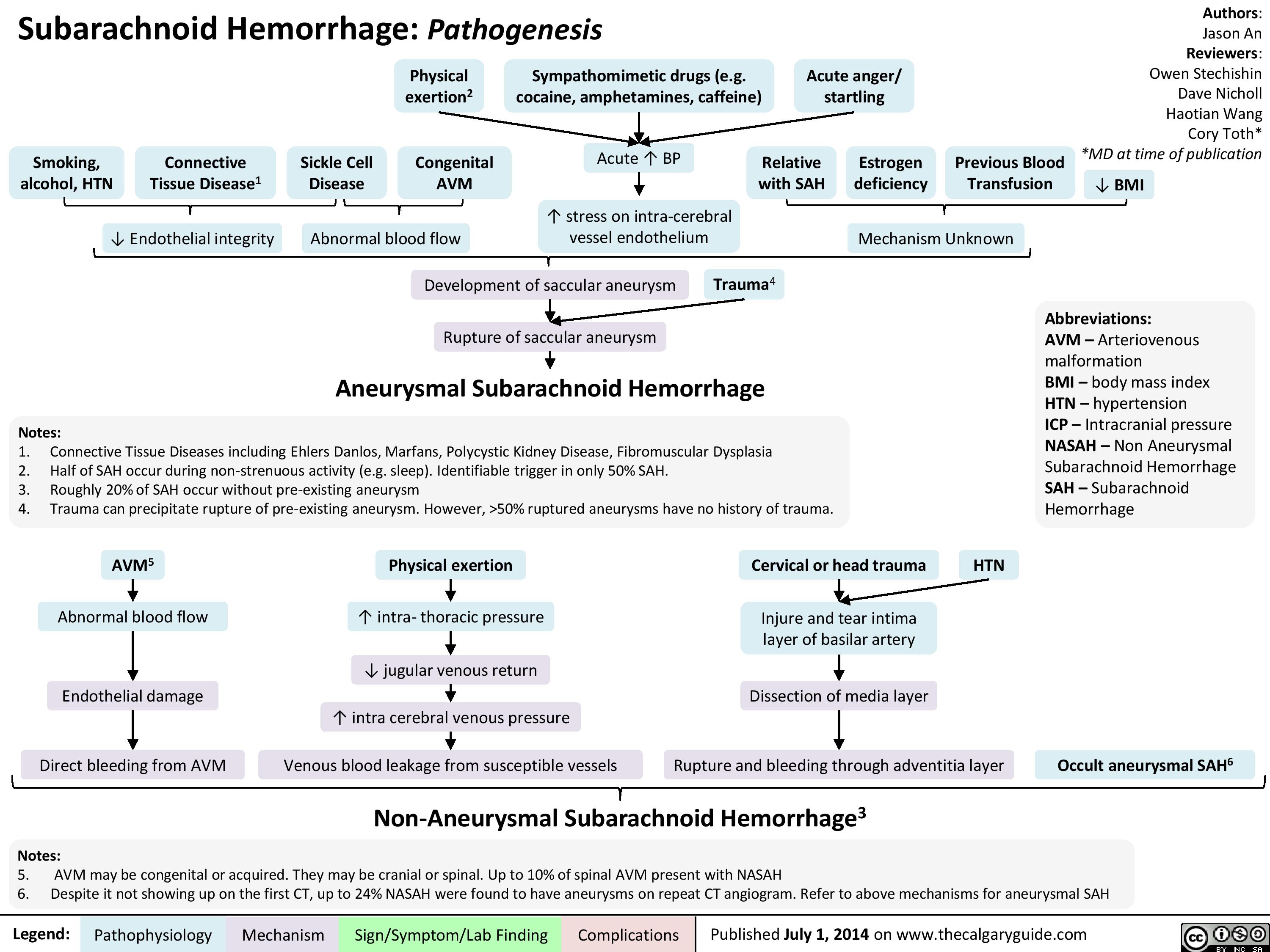
Pathogenesis of SAH
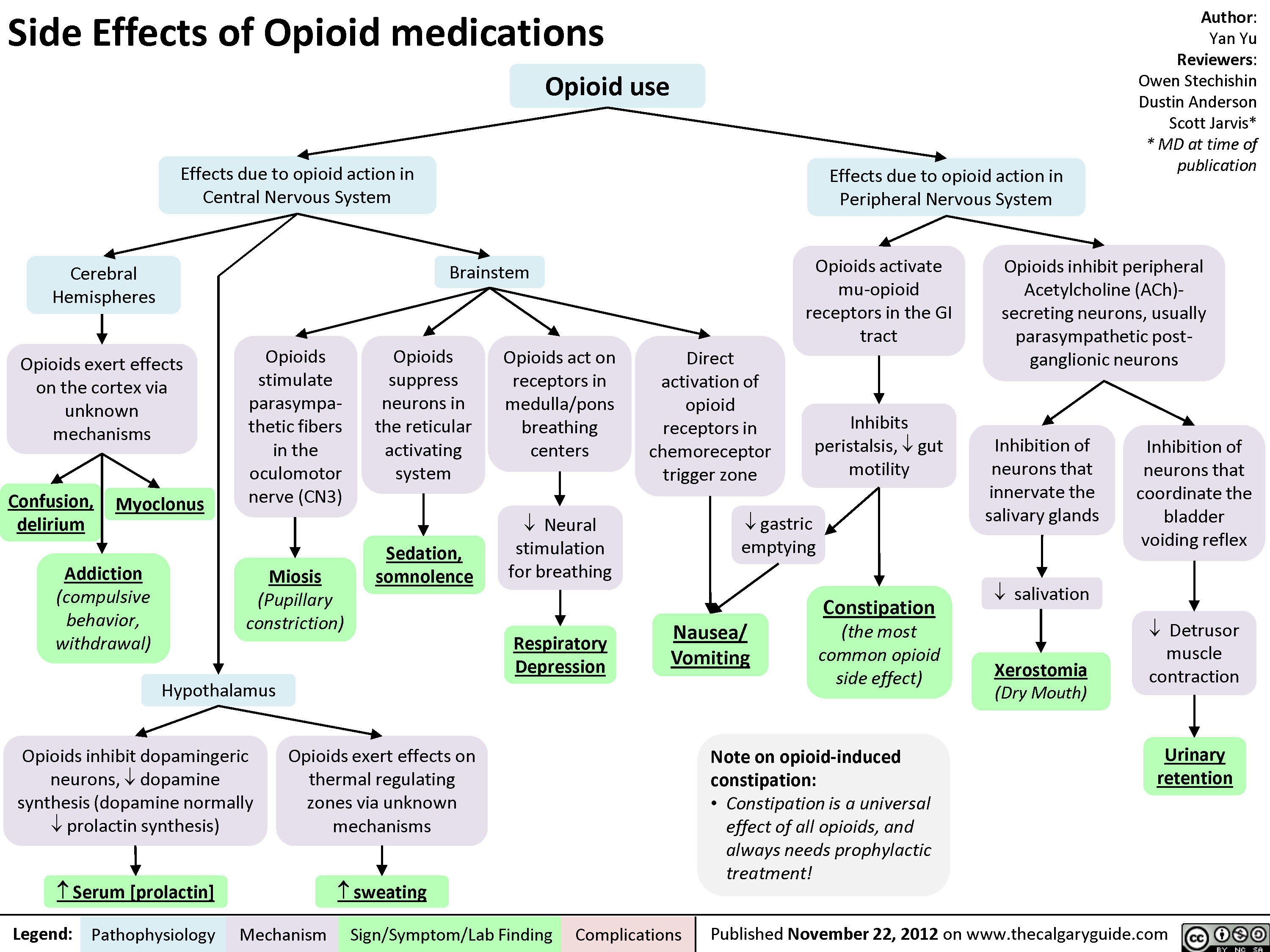
Side Effects of Opioid Medications
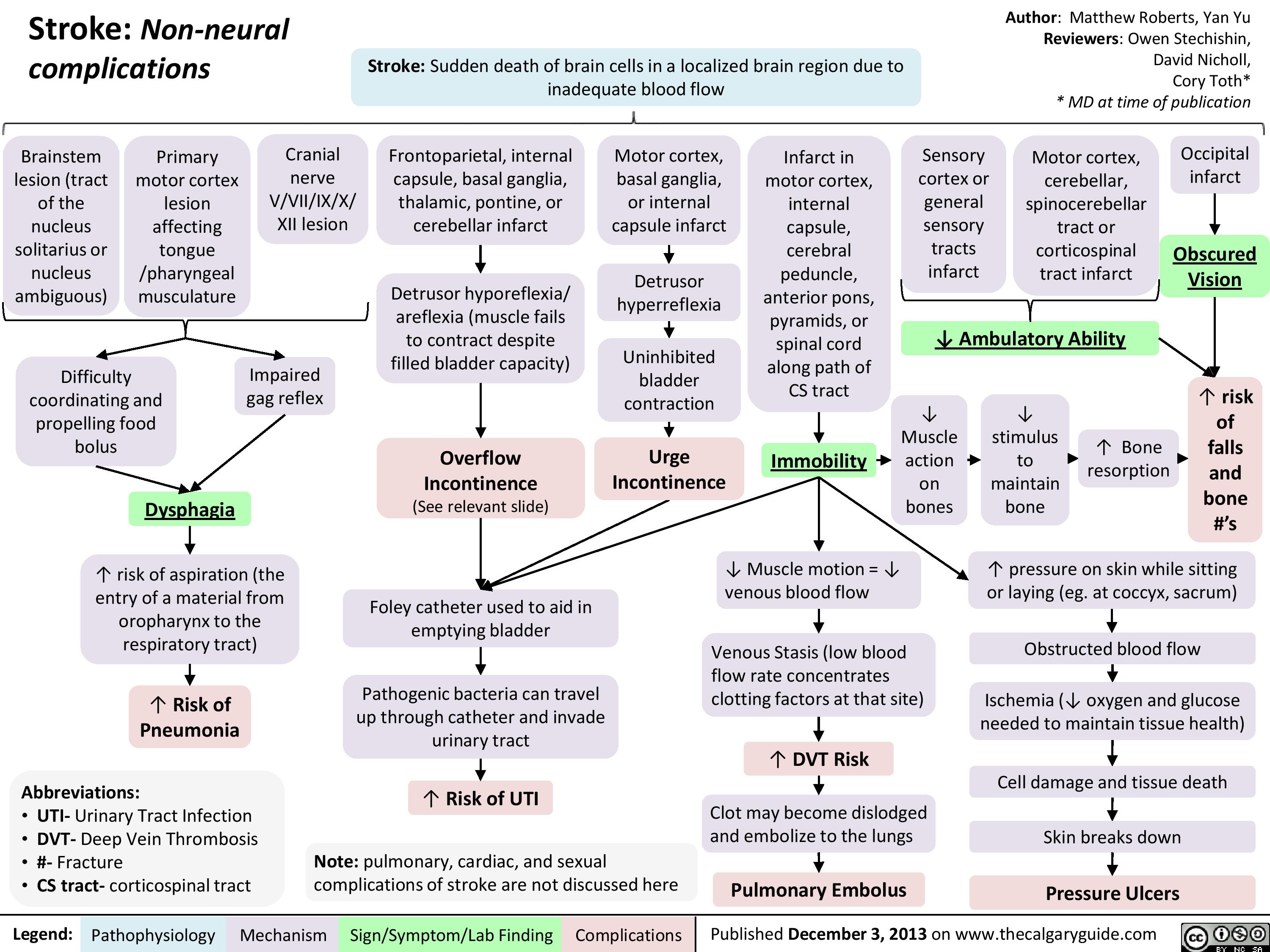
Non Neural Complications of Stroke
Giant Cell (Temporal) Arteritis - Pathogenesis and investigations
Giant Cell (Temporal) Arteritis - Clinical findings and Complications
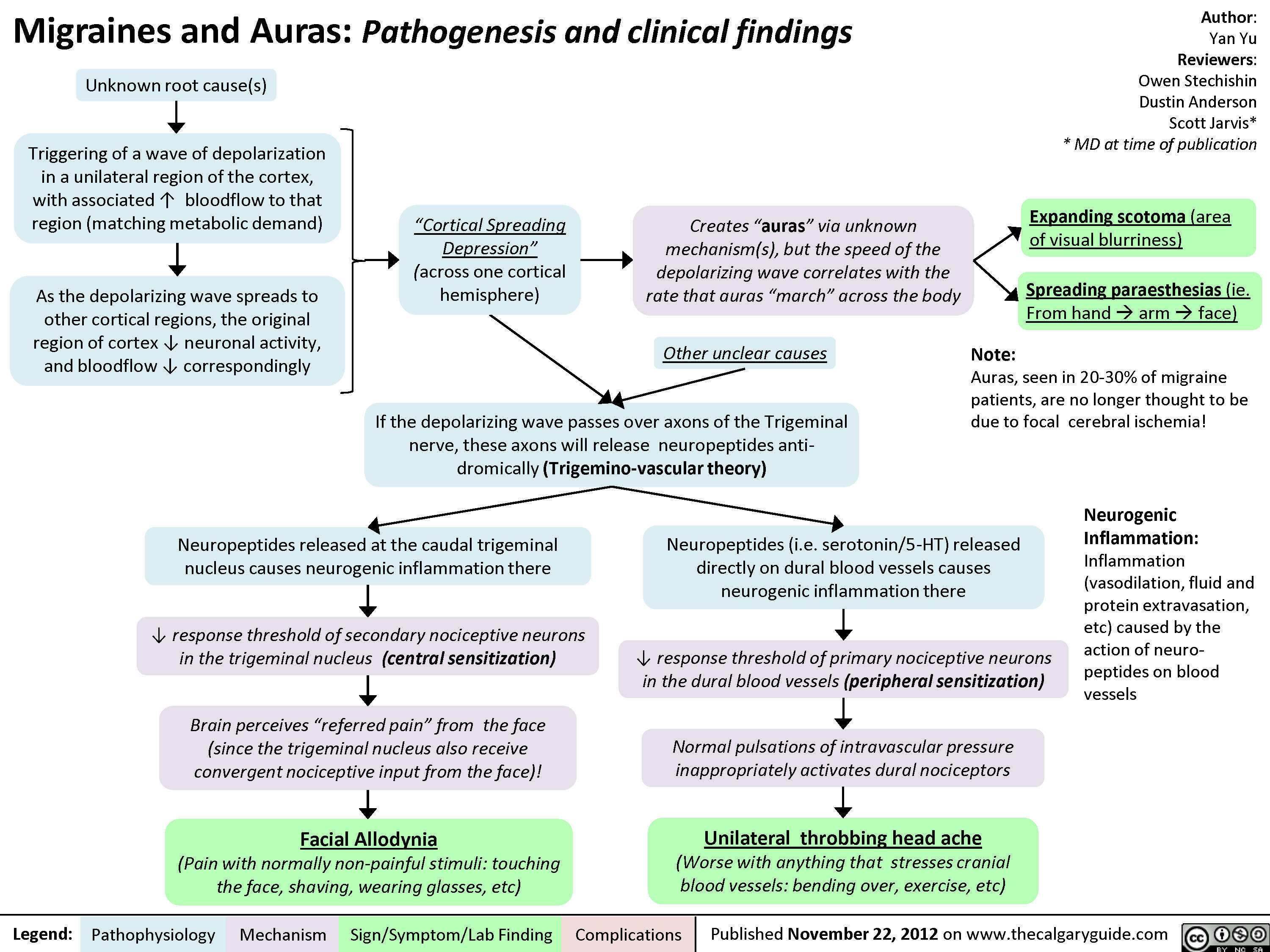
Migraines and Auras Pathogenesis and Clinical Findings
Pain Pathways in the Head

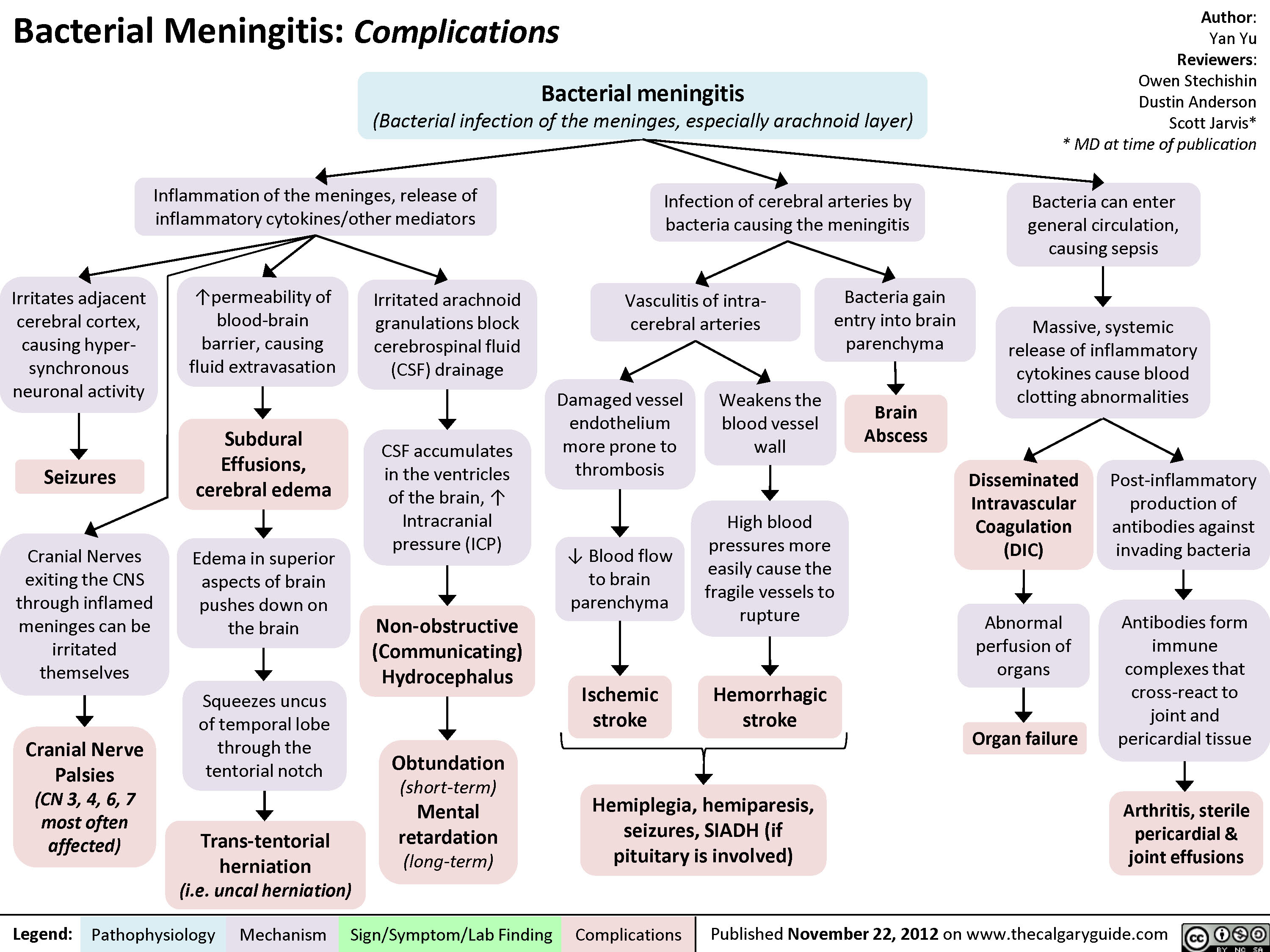
Bacterial Meningitis Complications
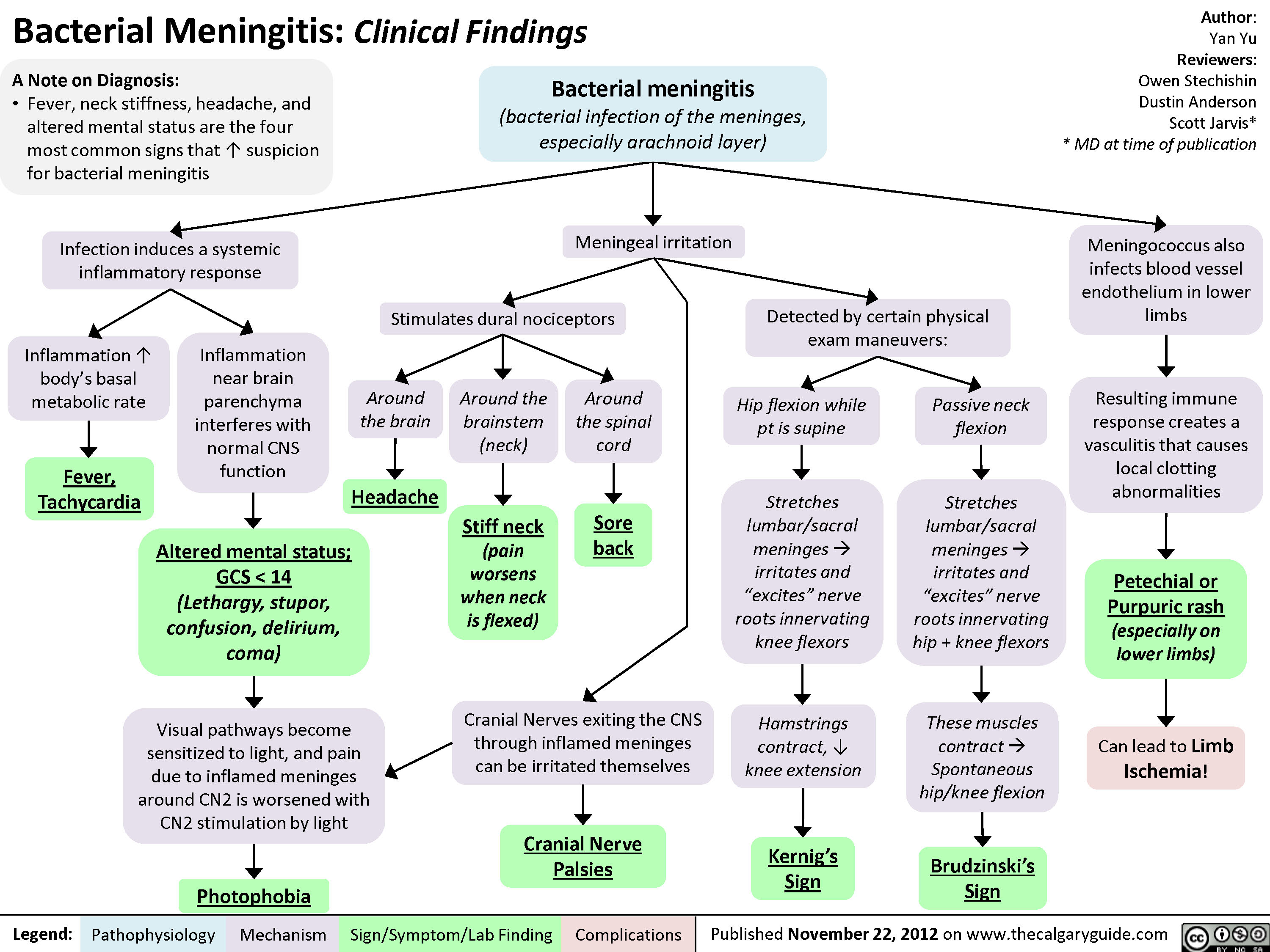
Bacterial Meningitis Clinical Findings
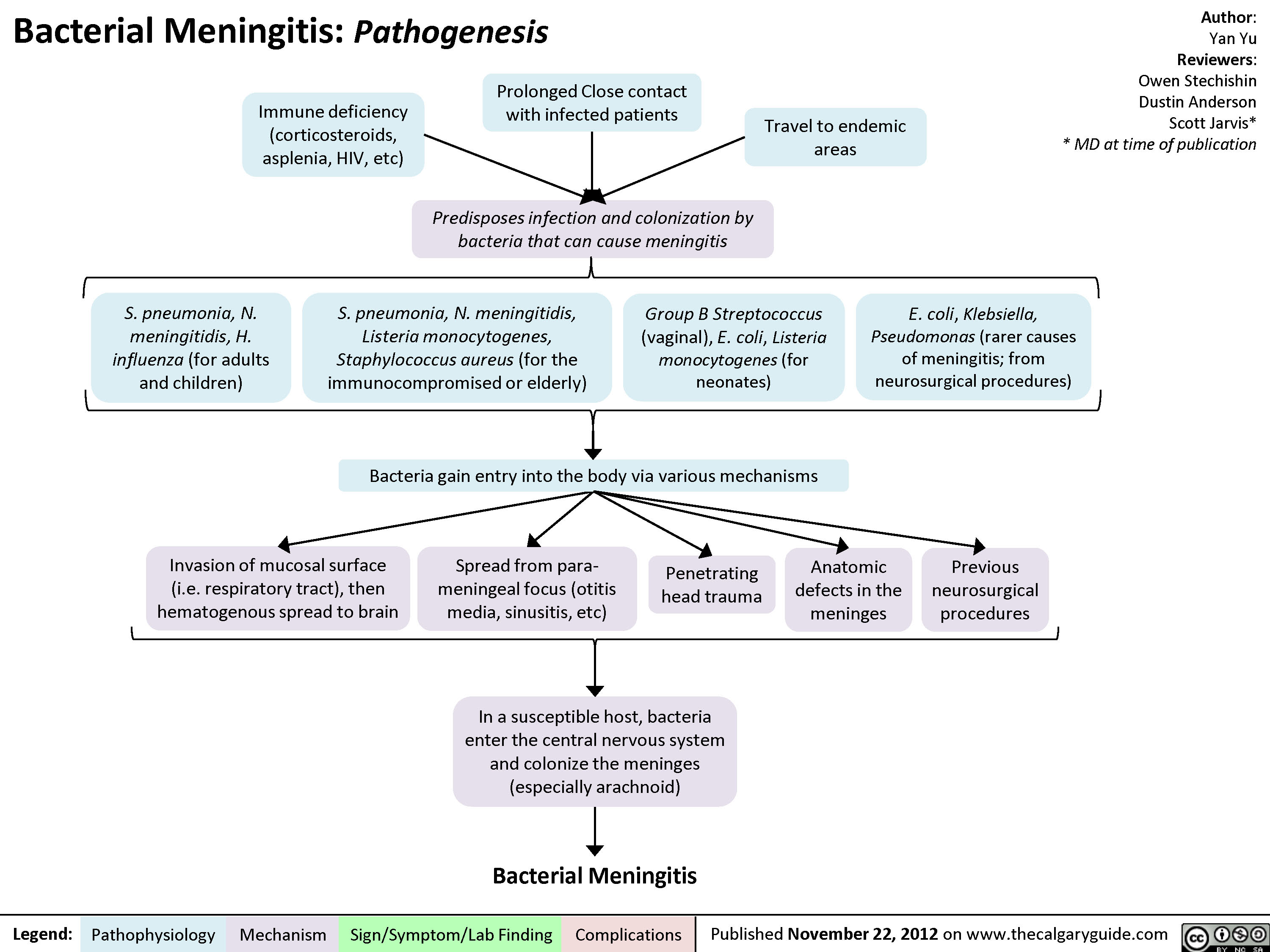
Bacterial Meningitis Pathogenesis
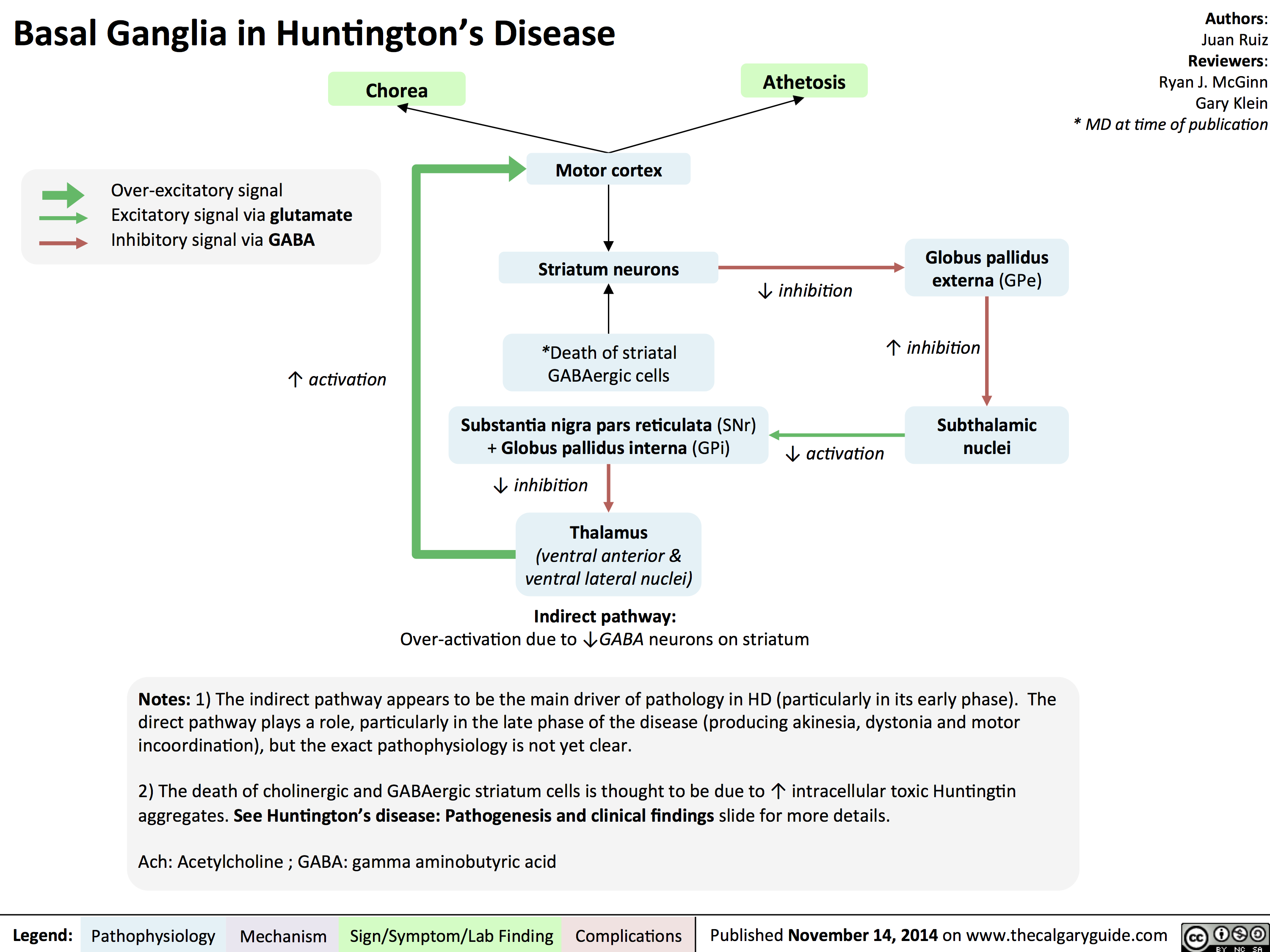
Basal Ganglia in Huntingtons Disease
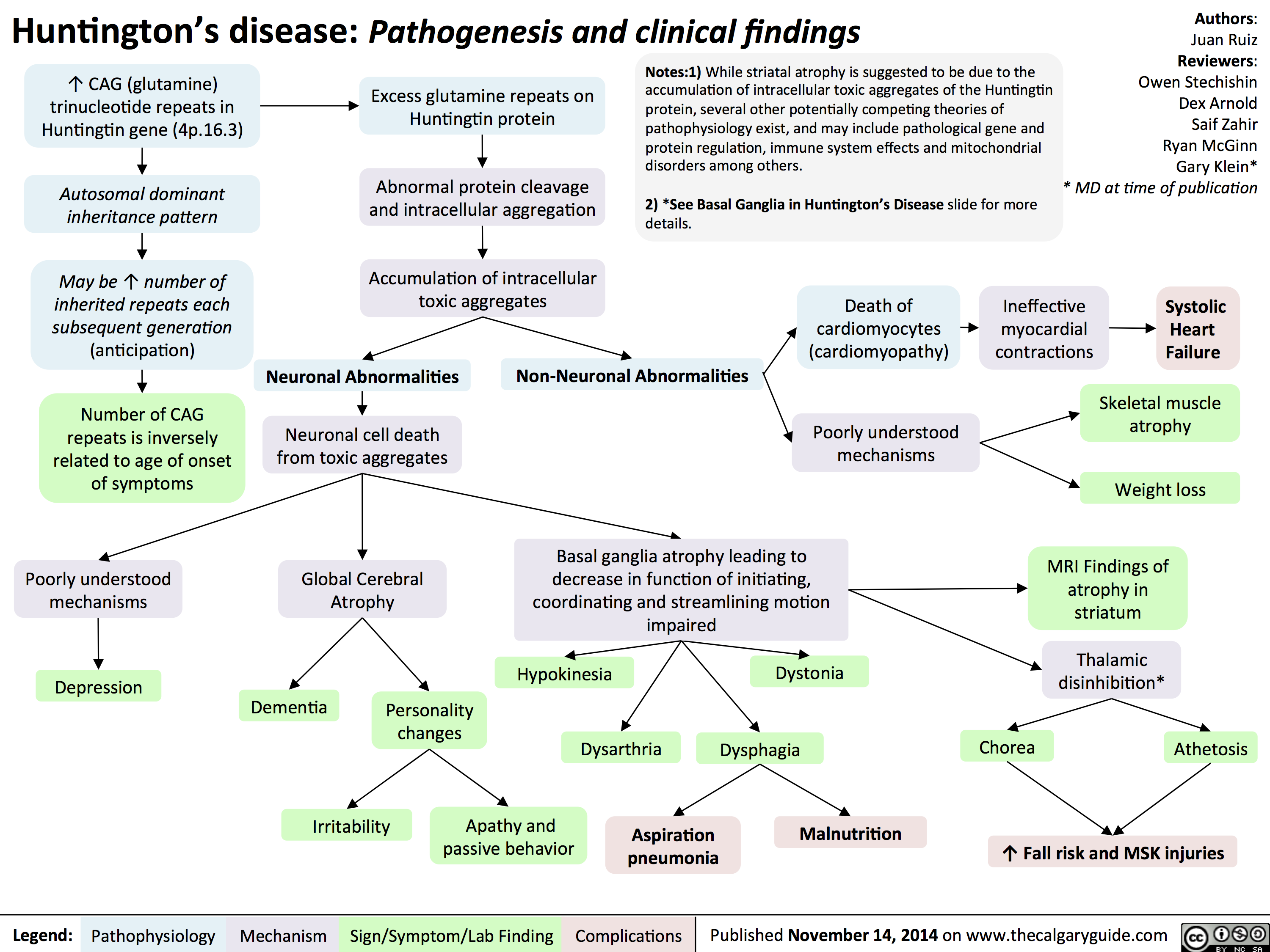
Huntingtons Disease Pathogenesis and Clinical Findings
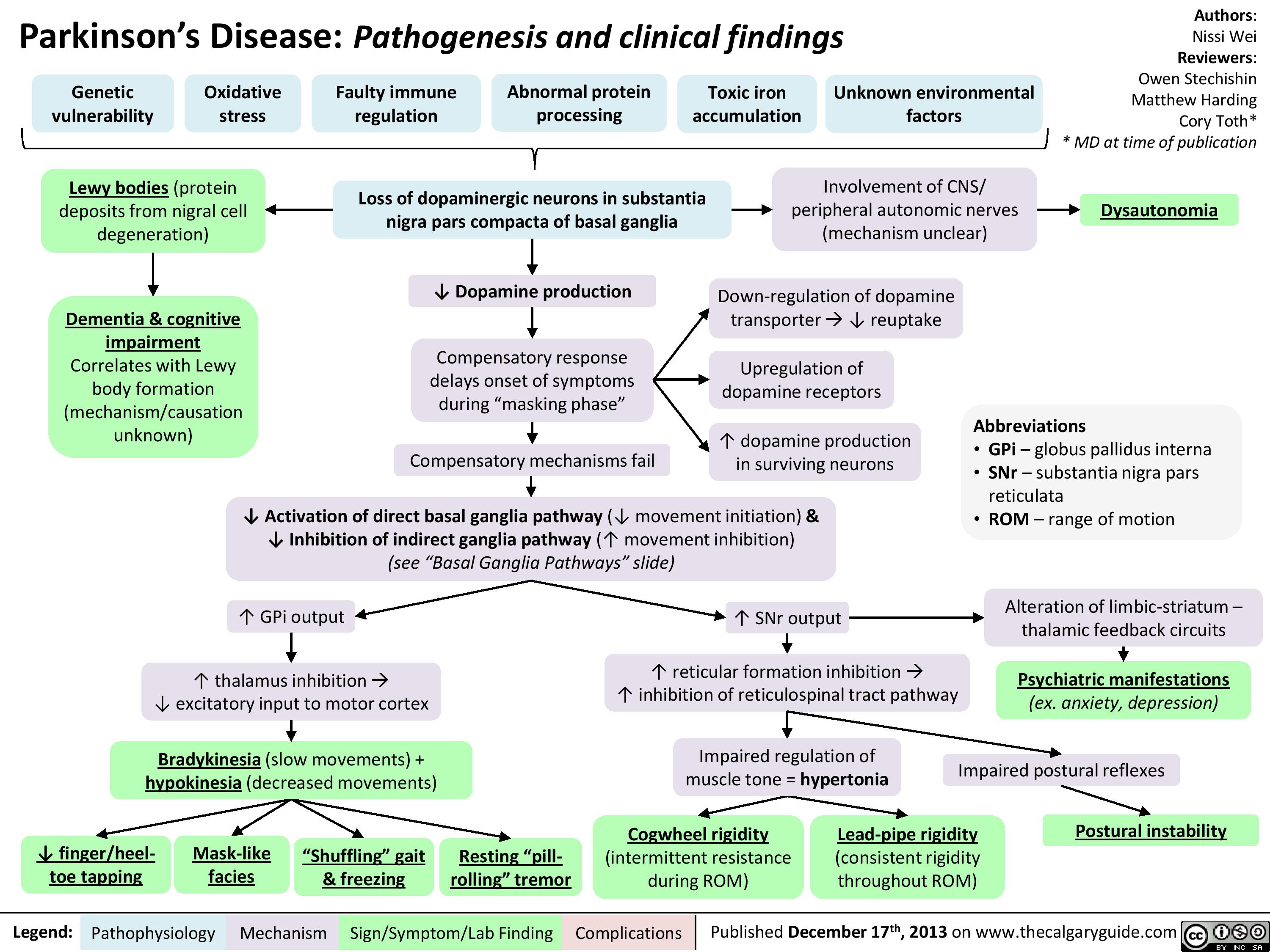
Parkinsons Disease
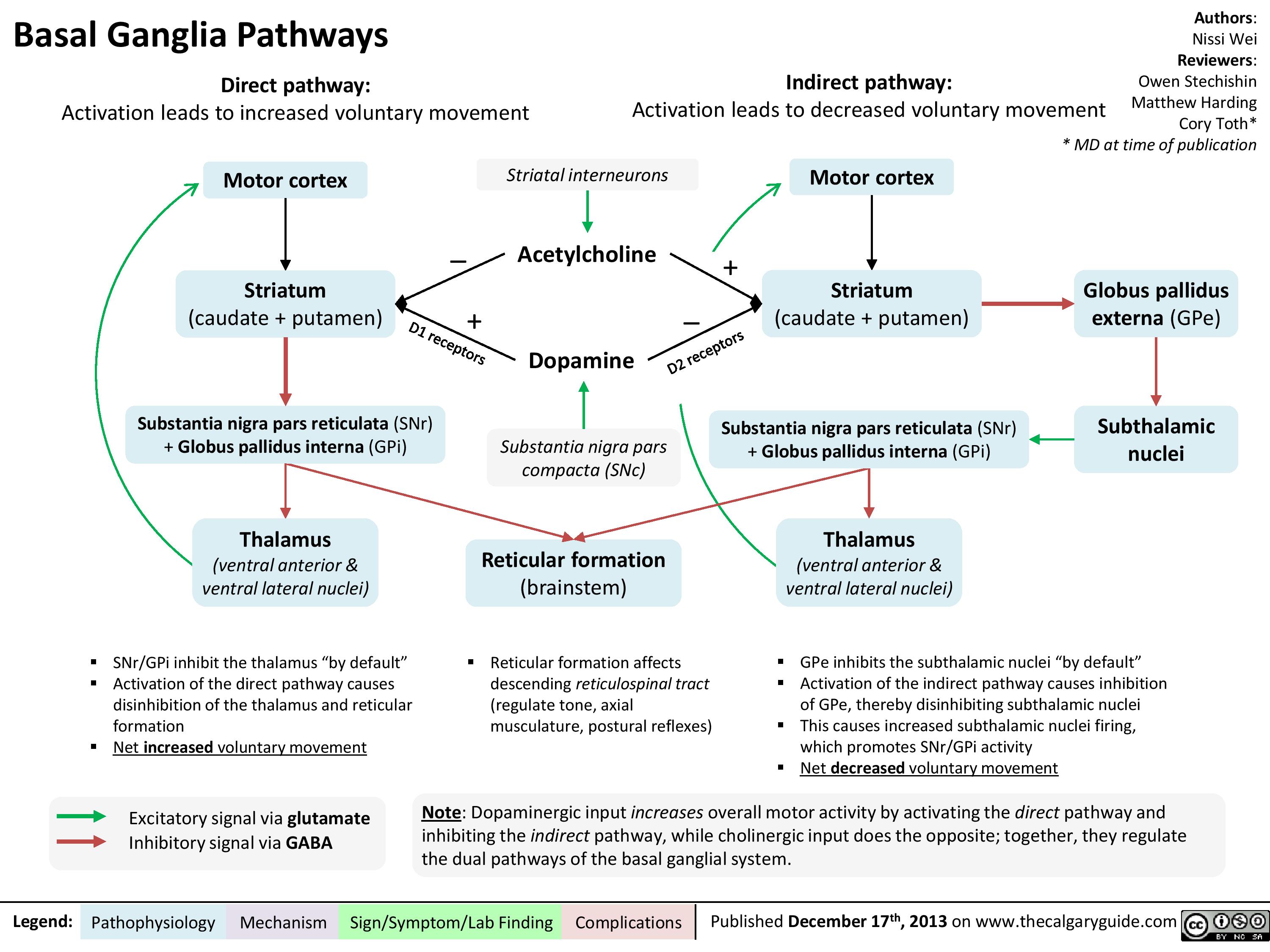
Basal ganglia pathways
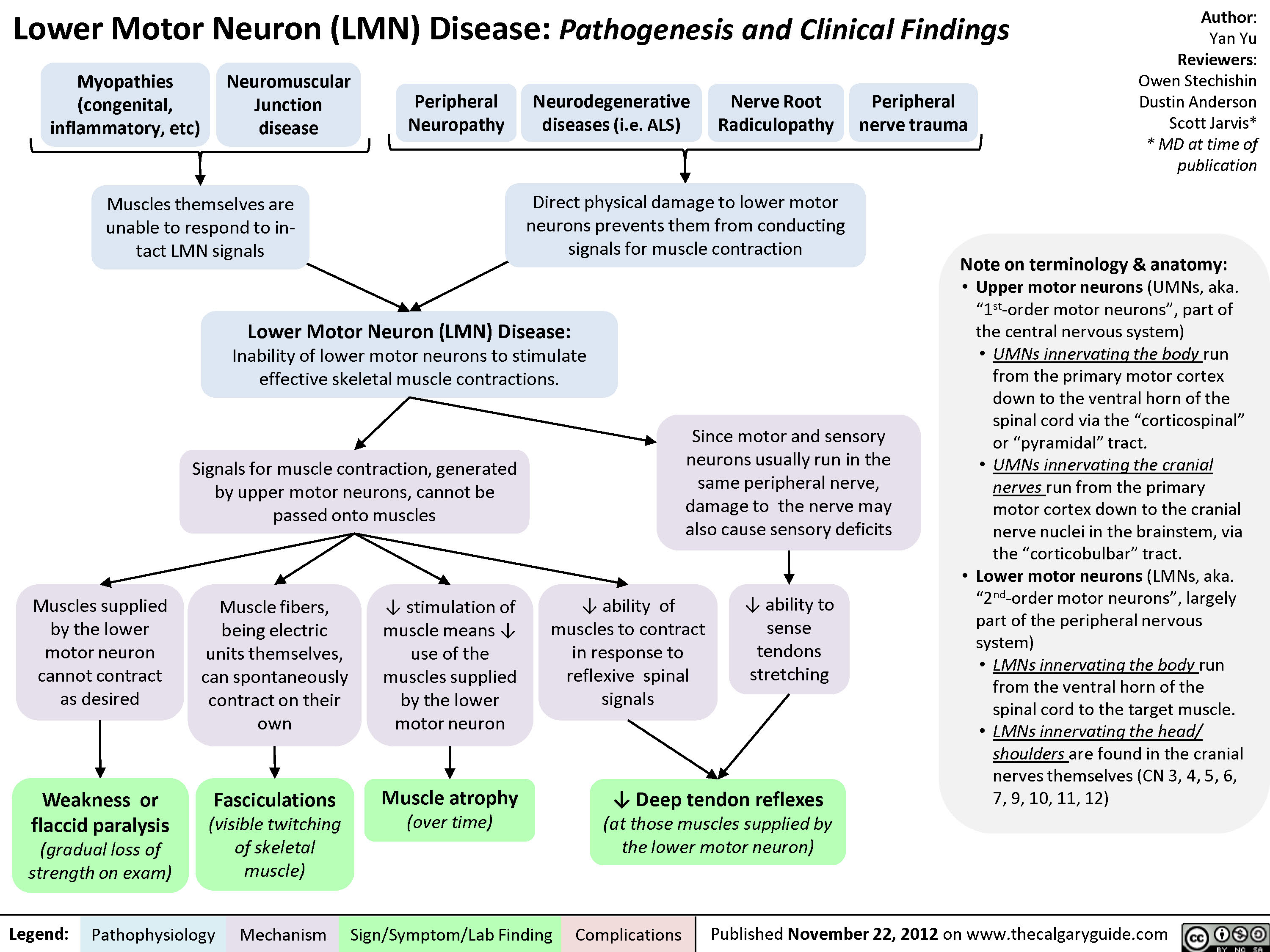
Lower Motor Neuron (UMN) Disease
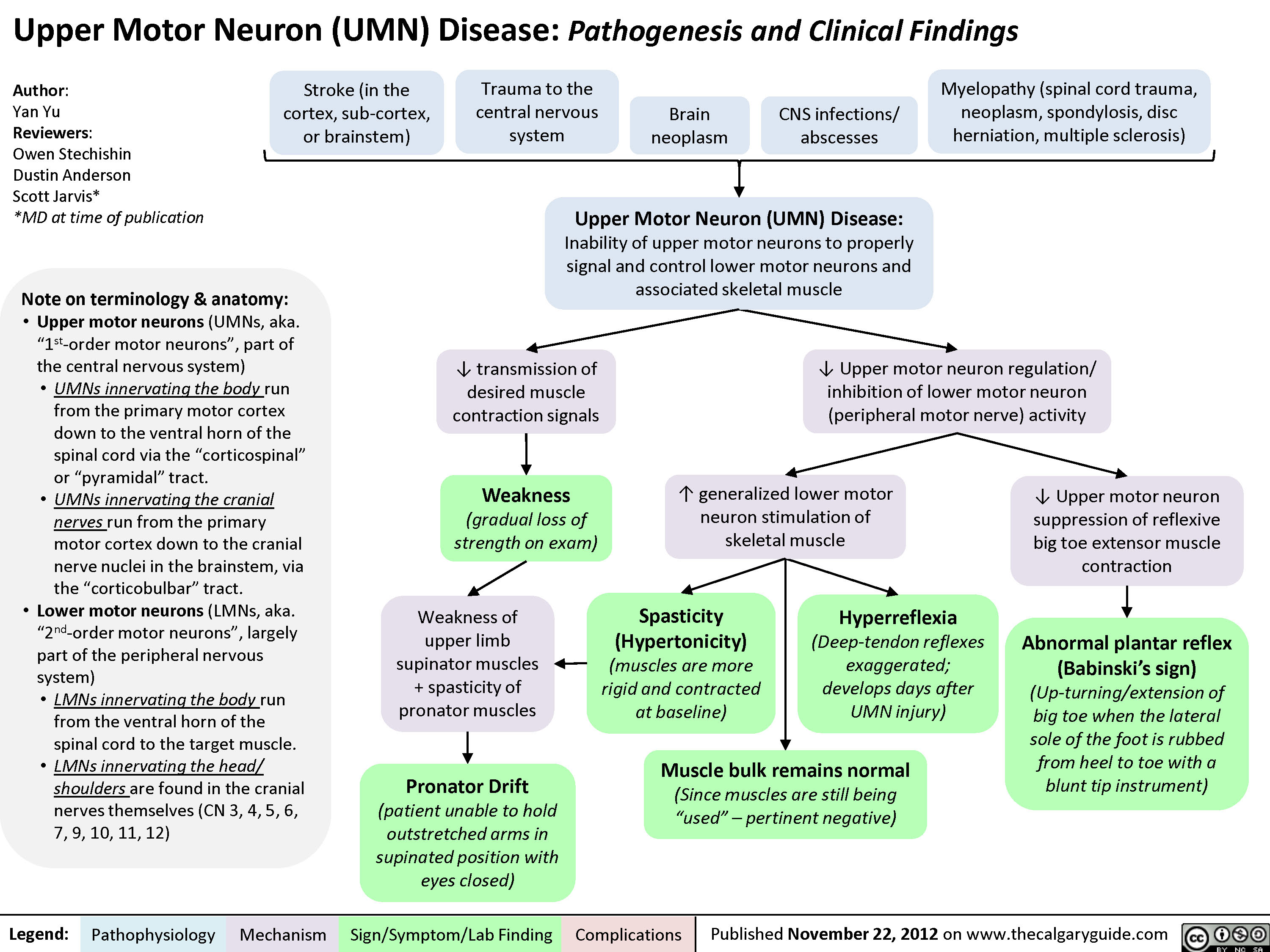
Upper Motor Neuron (UMN) Disease
Dupuytren
Trigger Finger
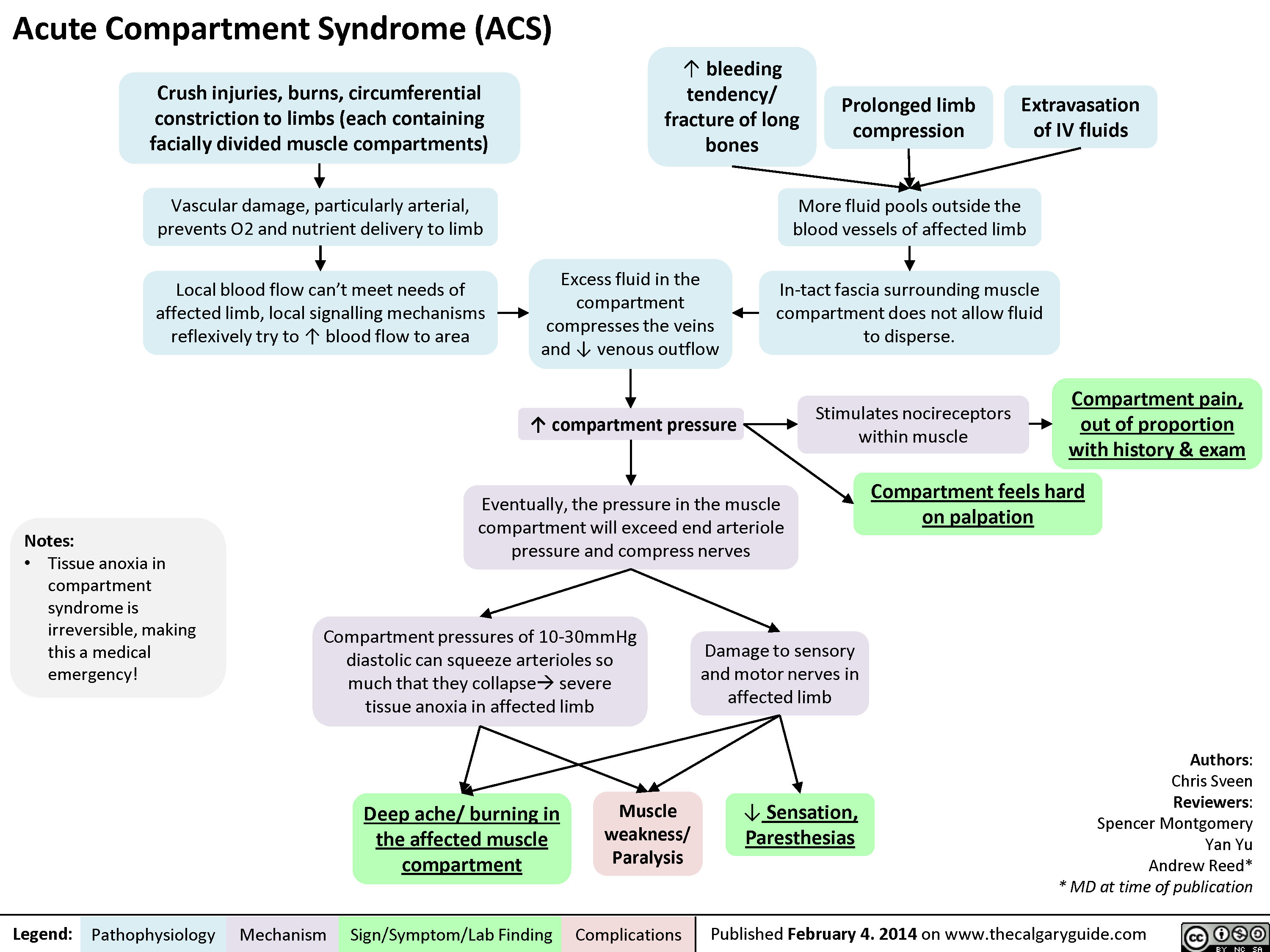
Acute Compartment Syndrome
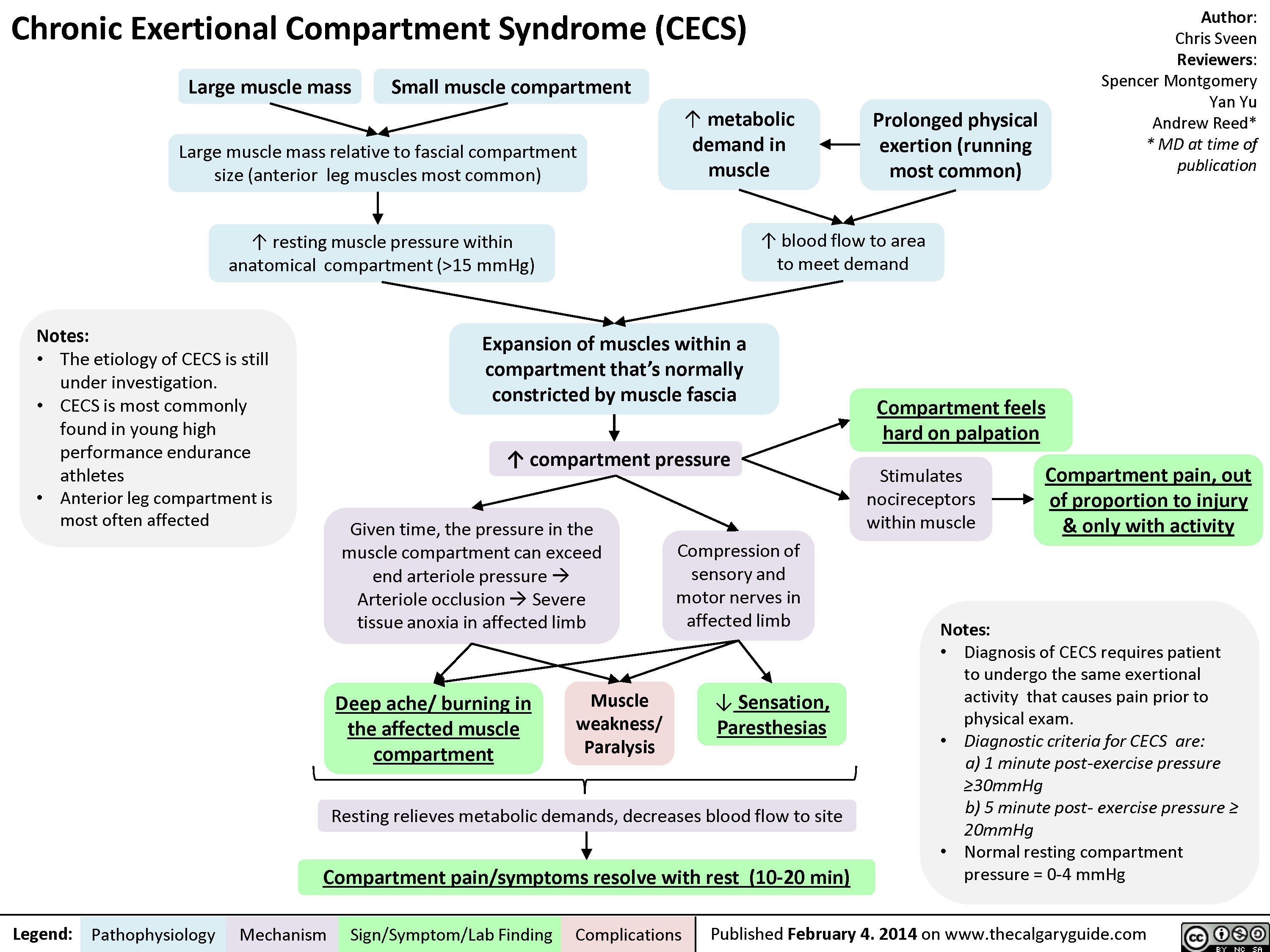
Chronic Exertional Compartment Syndrome
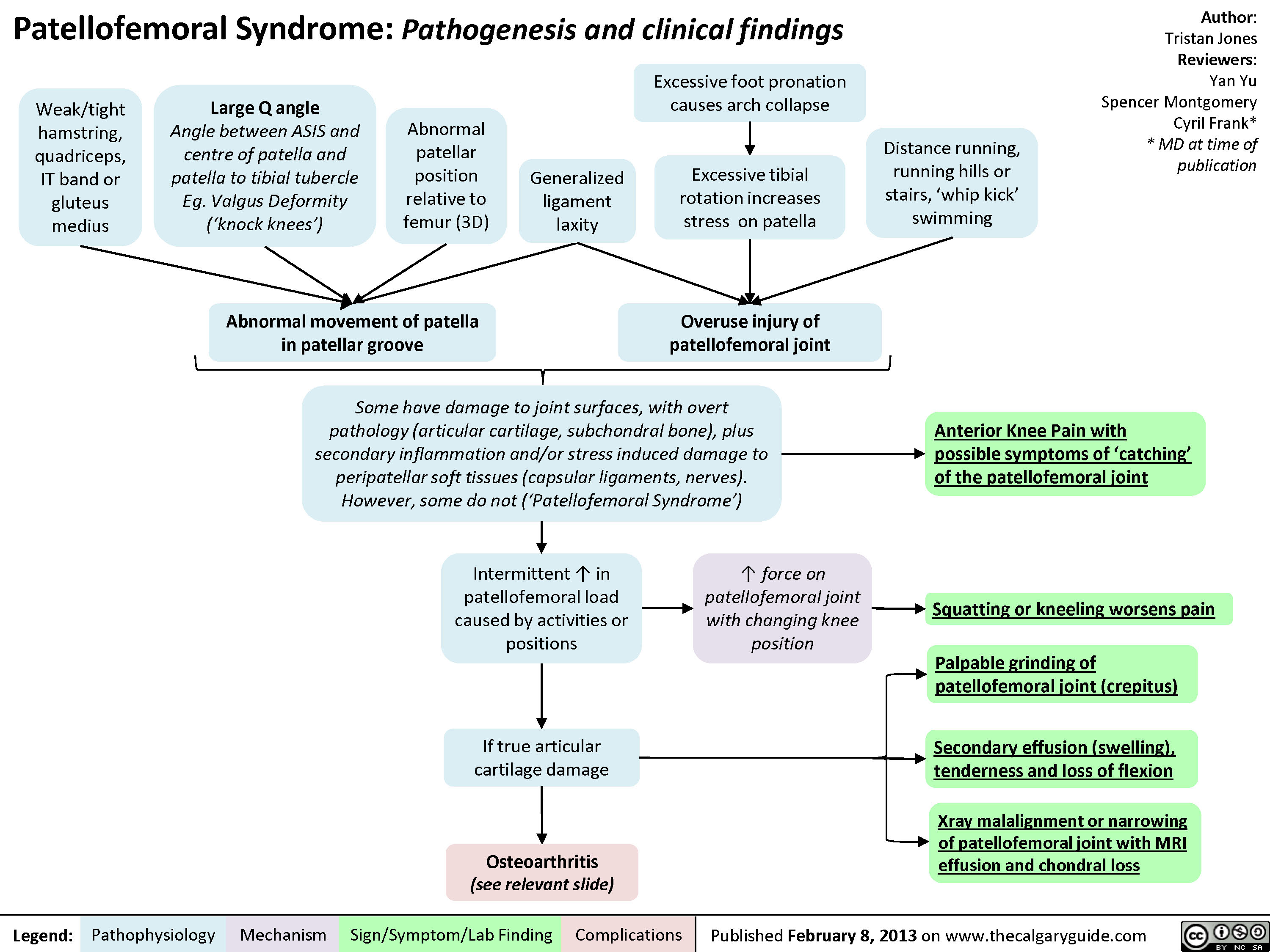
Patellofemoral Syndrome
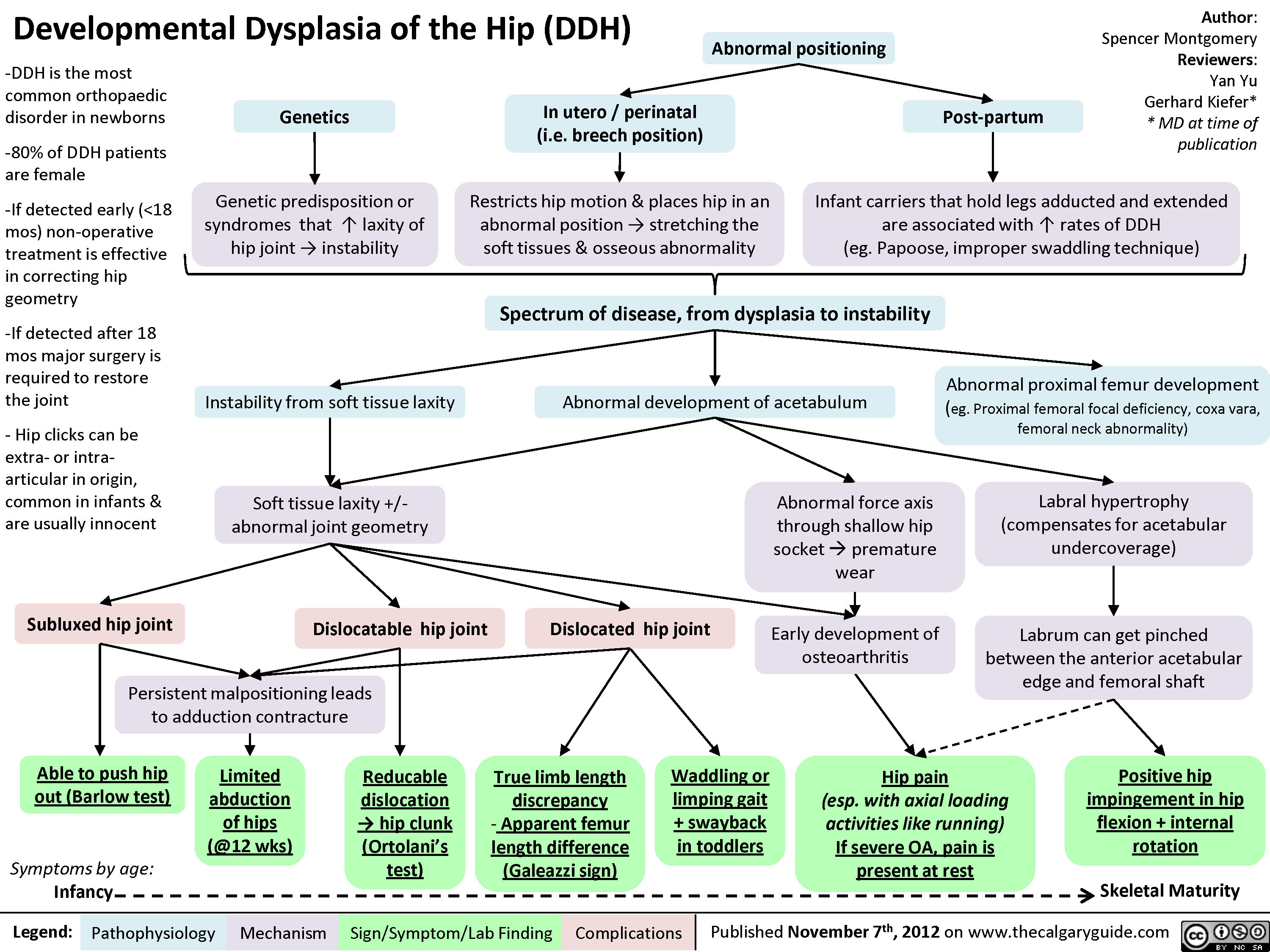
Developmental Dysplasia of the Hip (DDH)
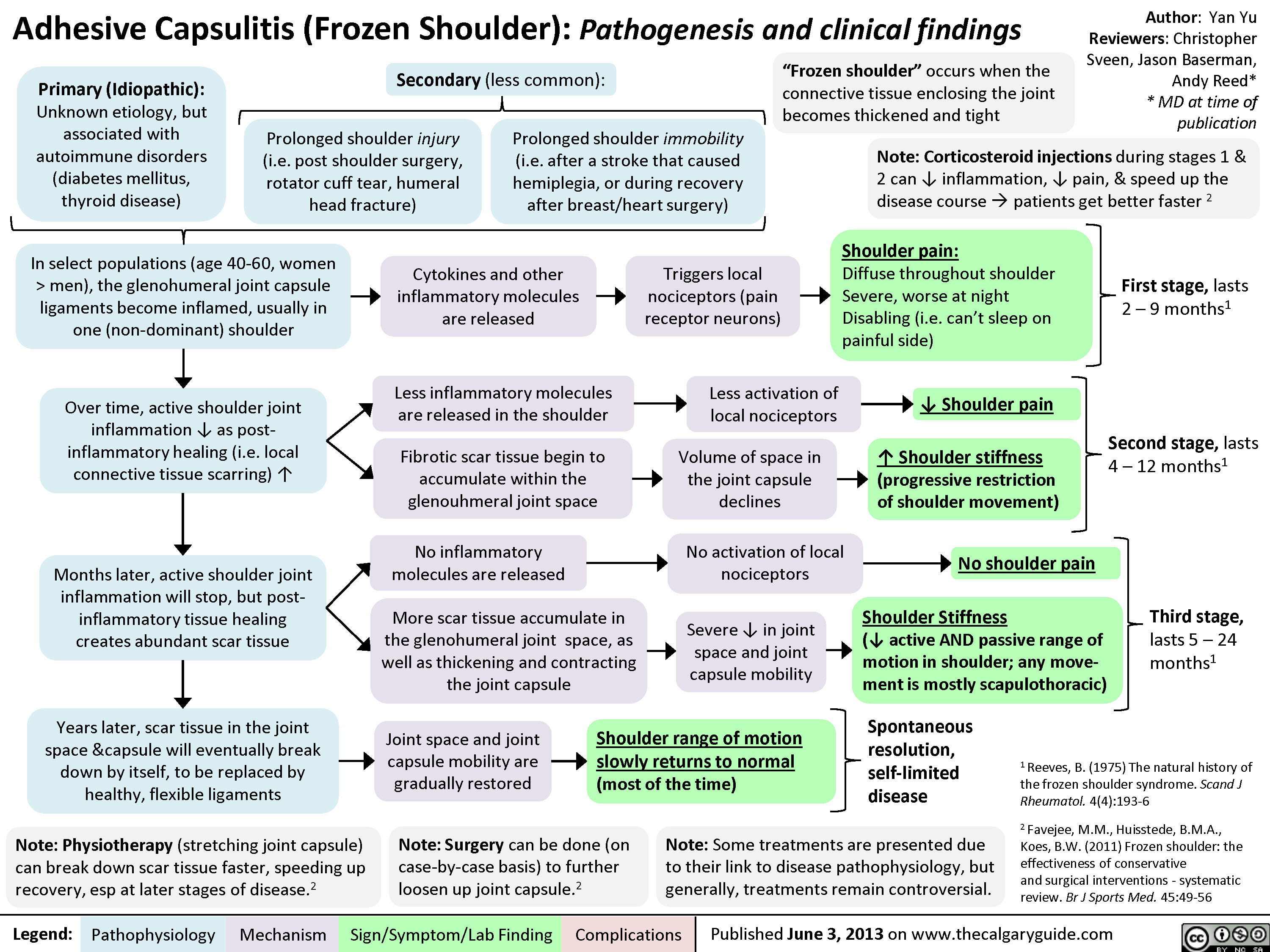
Adhesive Capsulitis
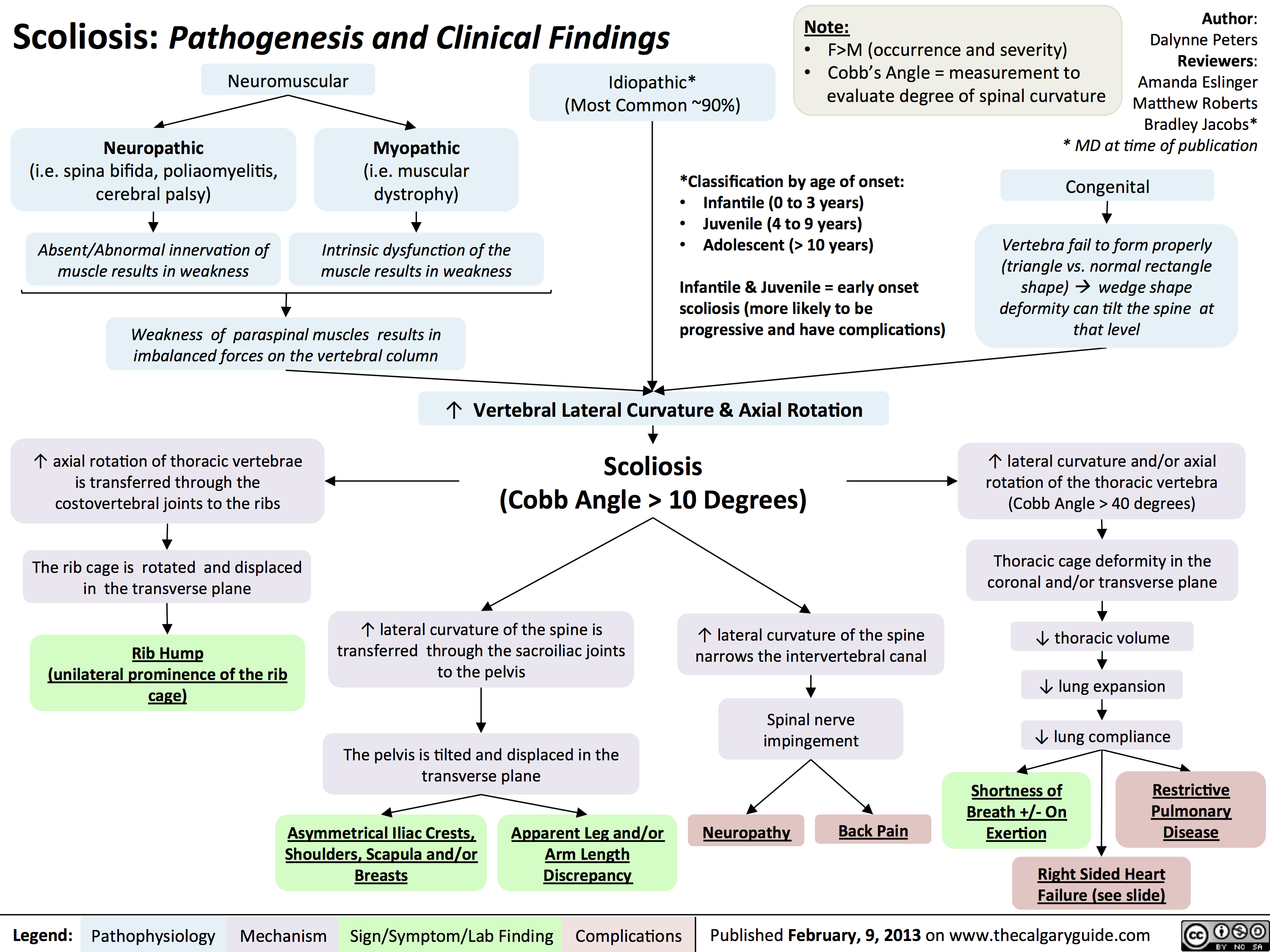
Scoliosis -Pathogenesis and Clinical Findings
Cauda Equina Syndrome
Myelopathy
Radiculopathy
Disc Herniations
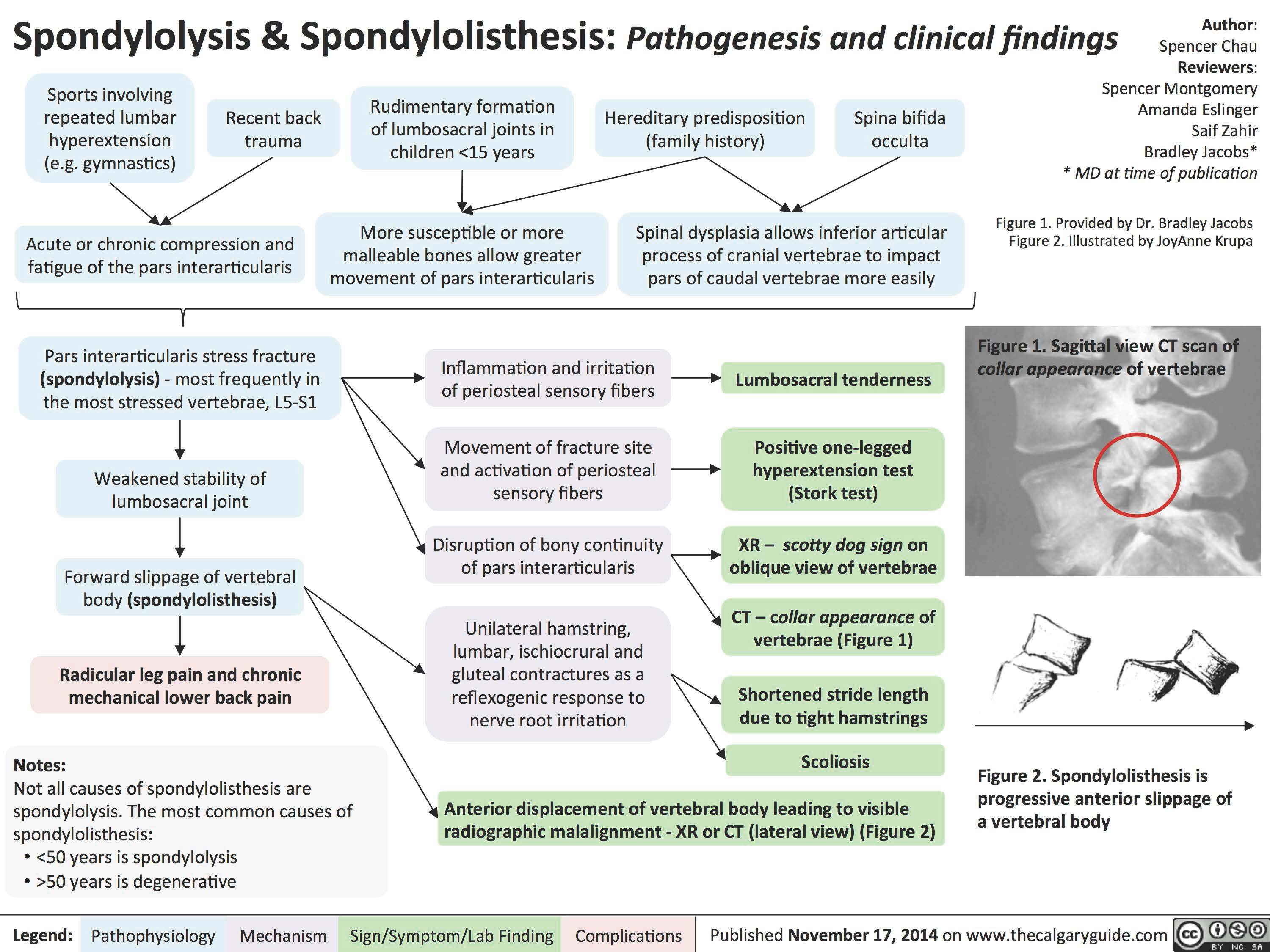
Spondylolysis _and_Spondylolisthesis Pathogenesis and Clinical Findings
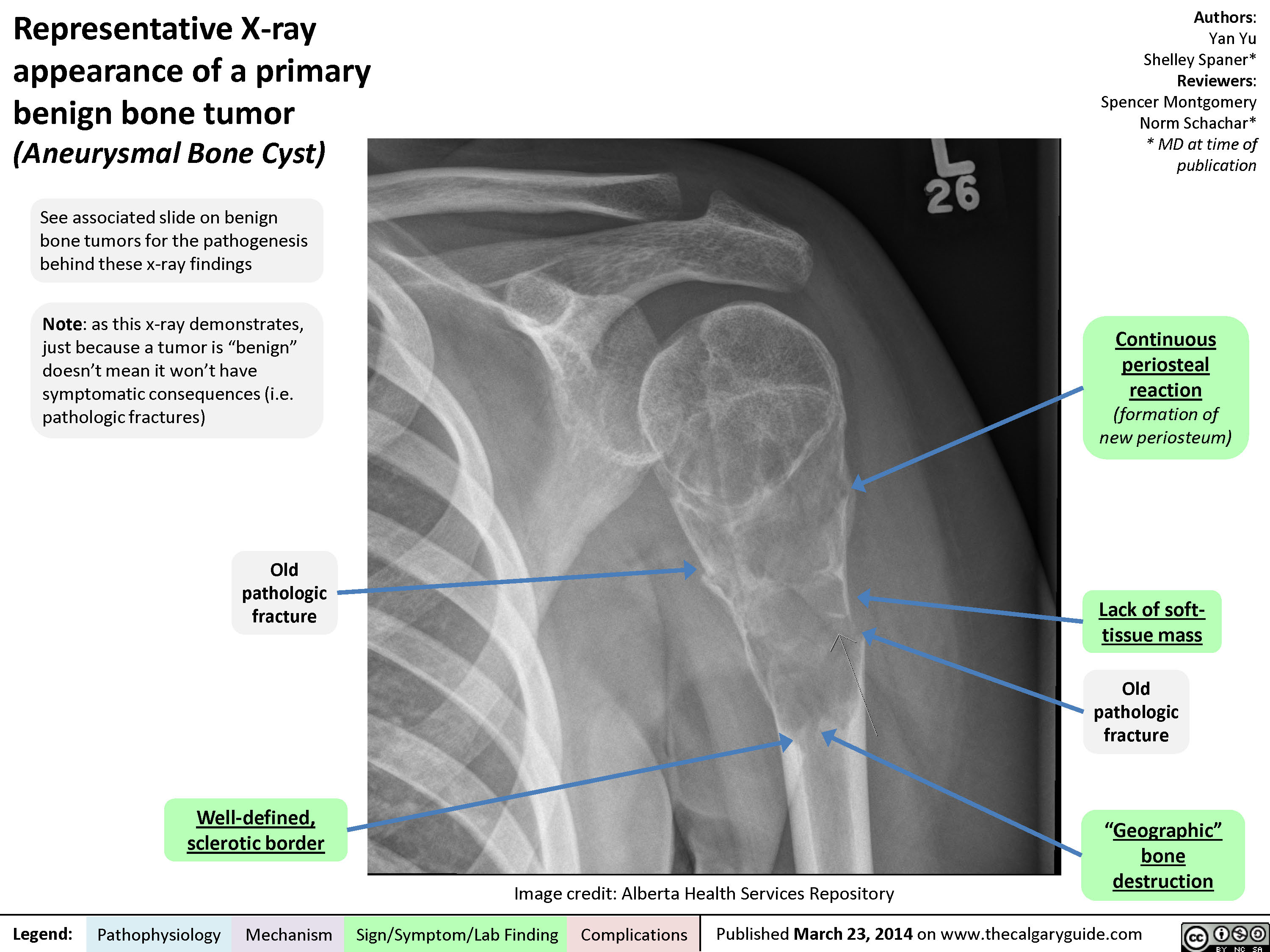
Representative X-ray appearance of a primary benign bone tumor
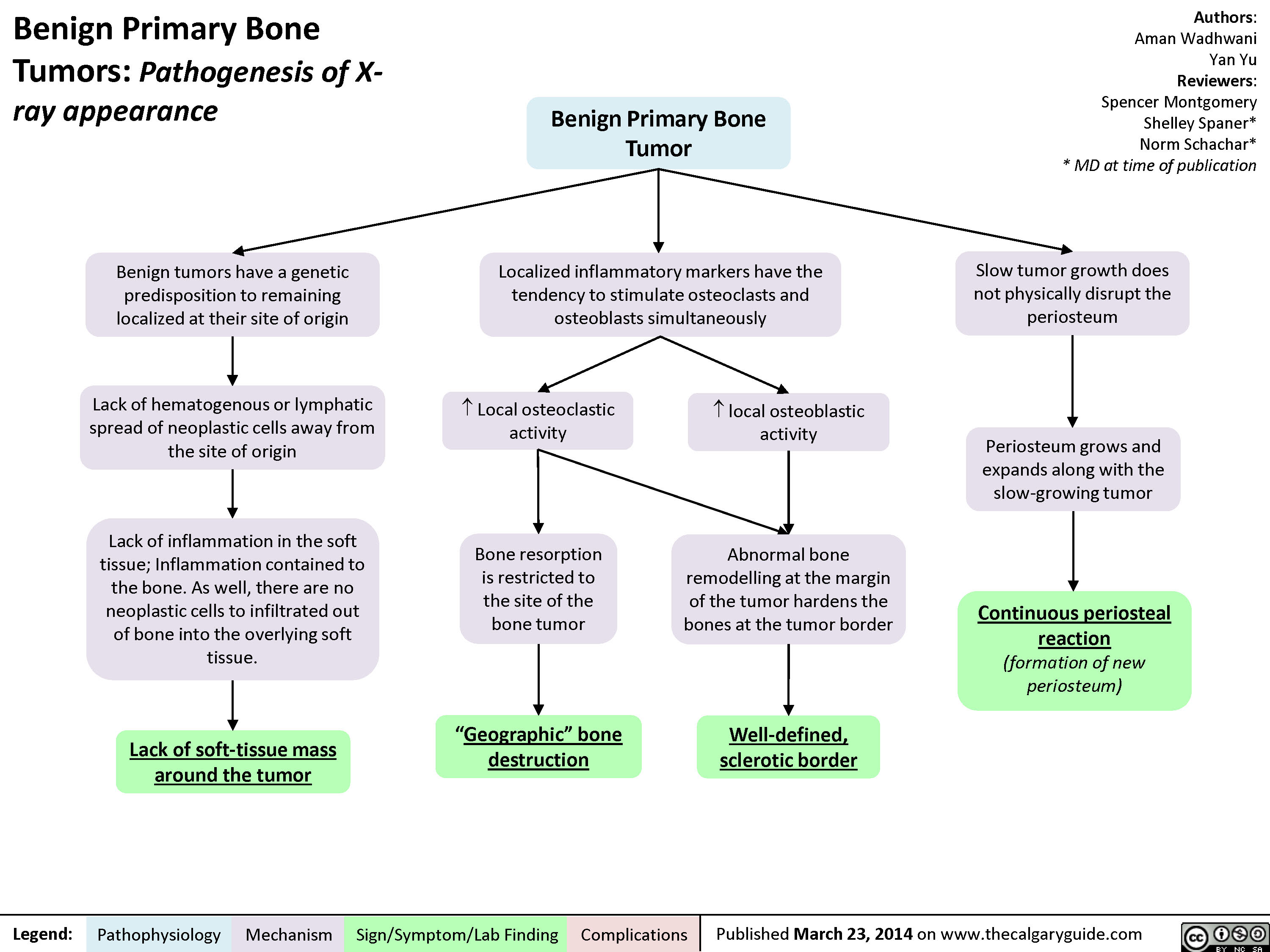
Benign Primary Bone Tumors - Pathogenesis of X-ray appearance
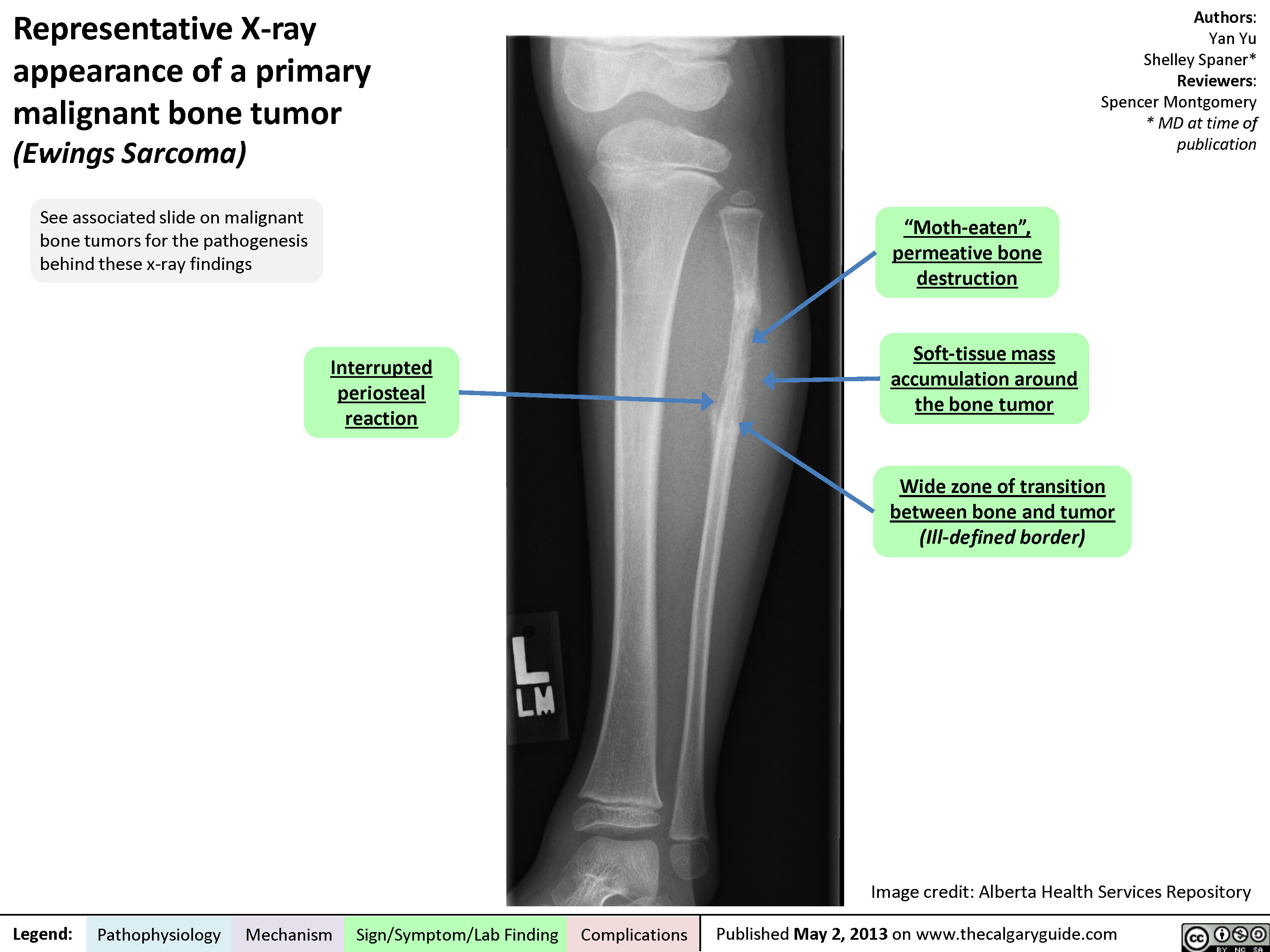
Representative X-ray appearance of a primary malignant bone tumor
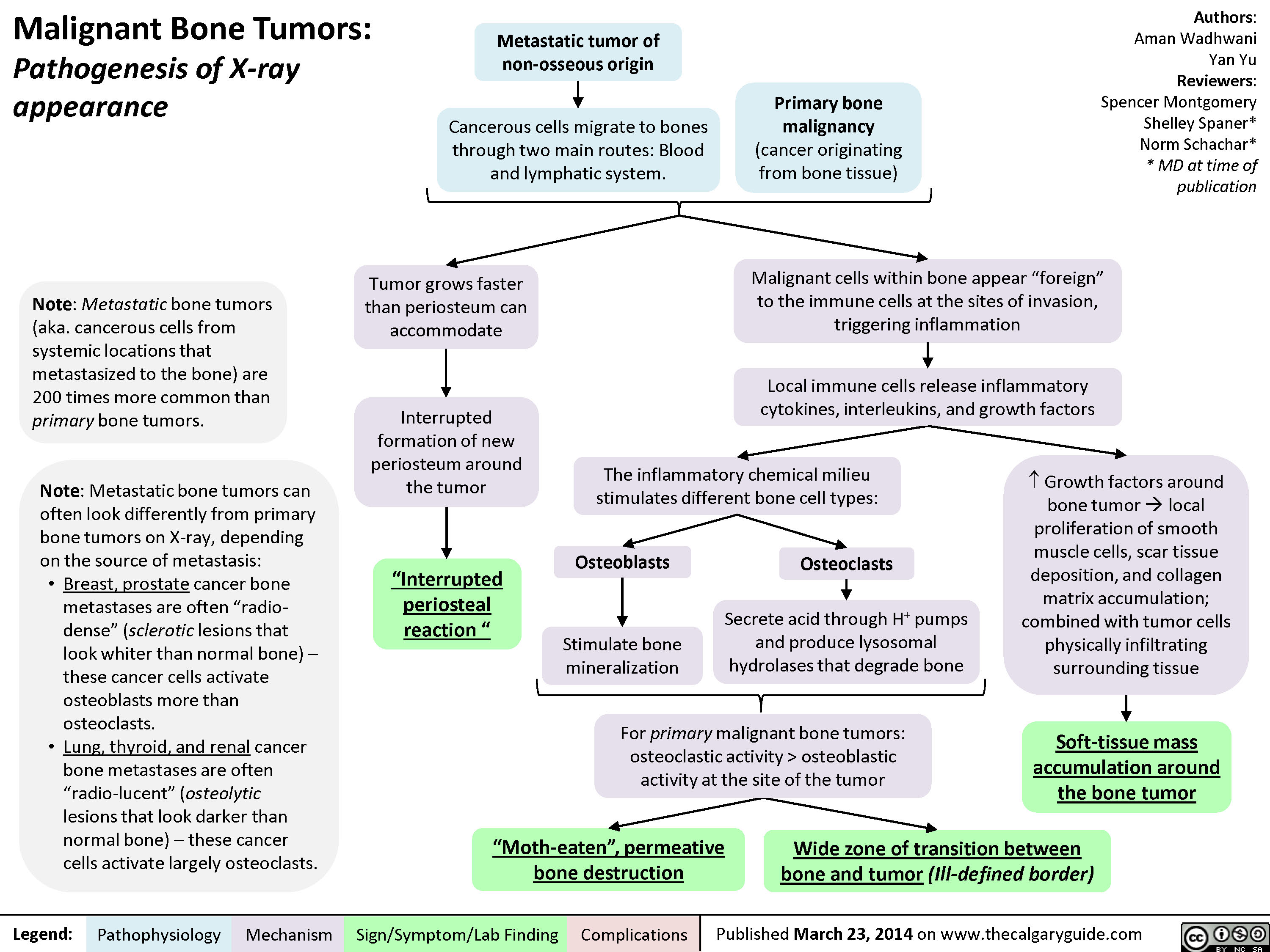
Malignant Bone Tumors - Pathogenesis of X-ray appearance
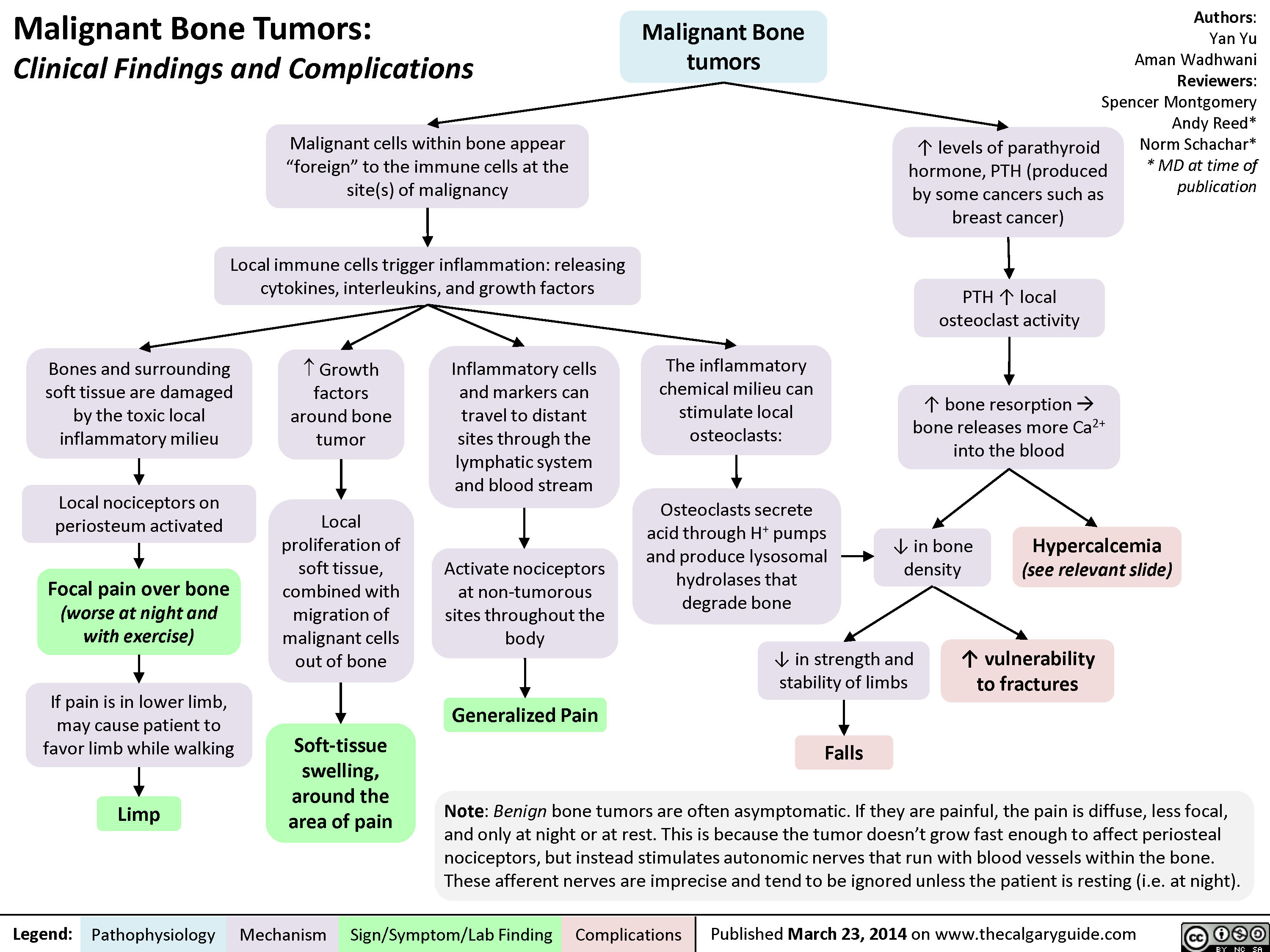
MSK tumors complications
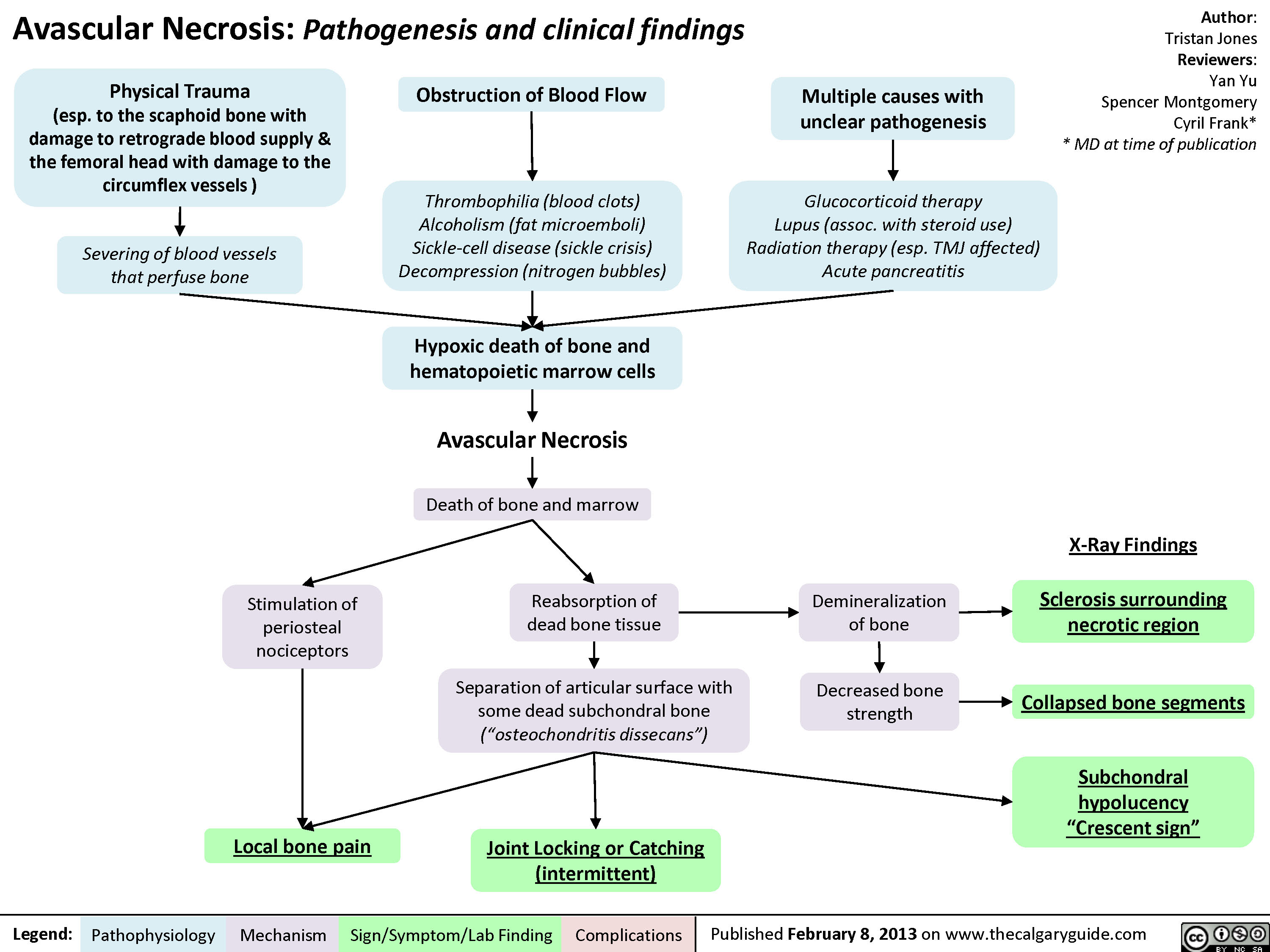
Avascular Necrosis - Pathogenesis and Clinical Findings
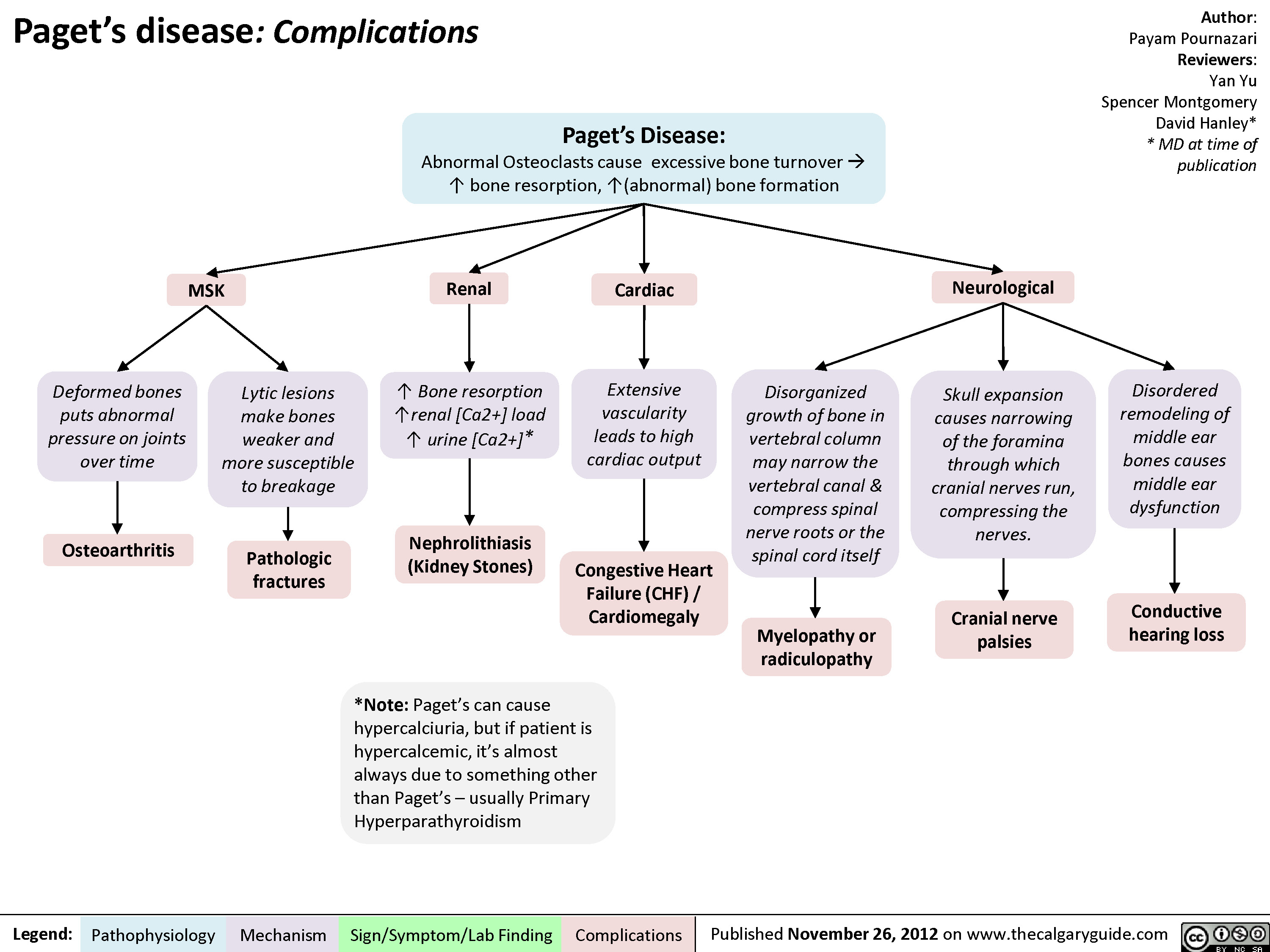
Pagets Disease Complications
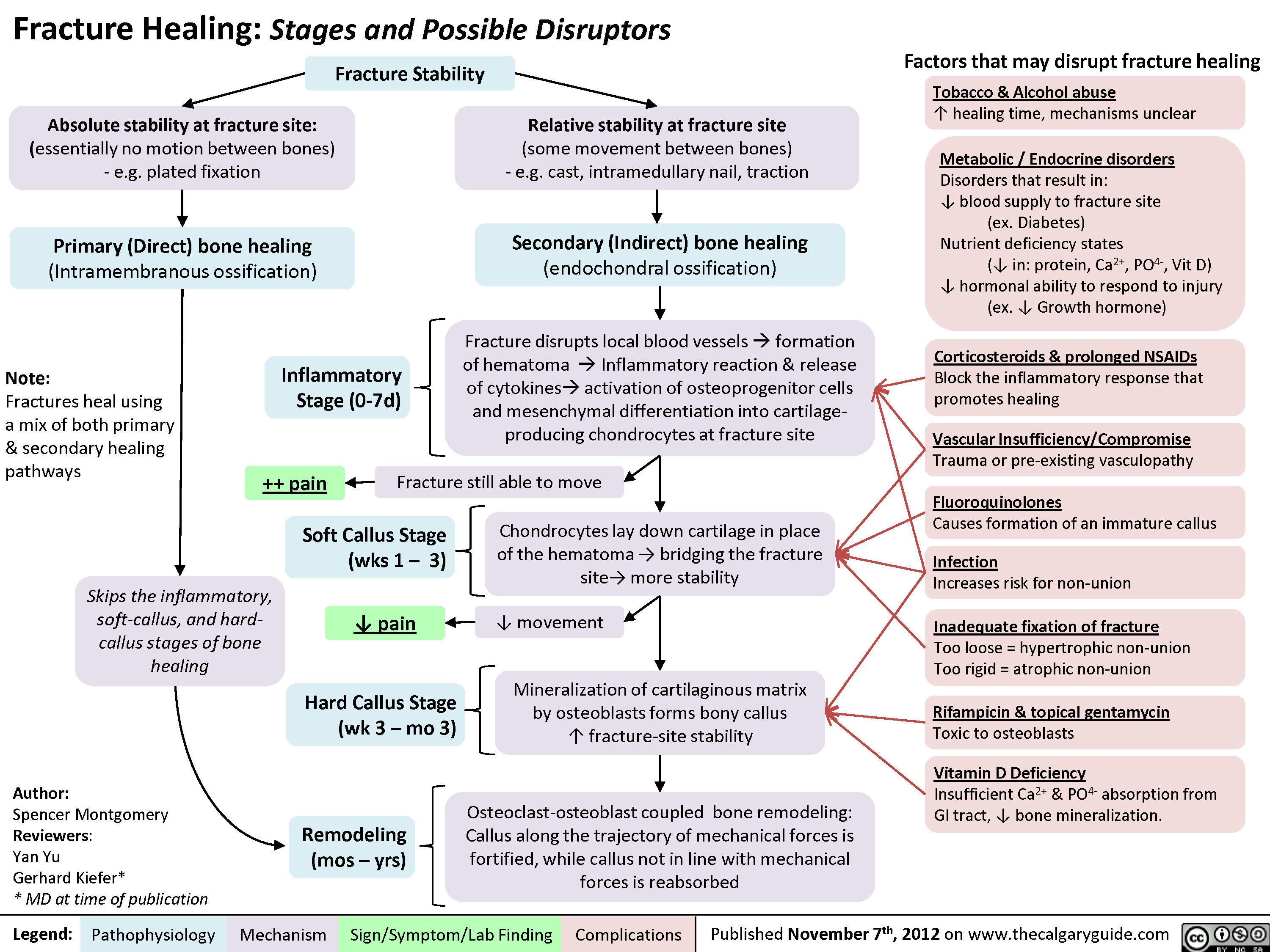
Fracture Healing (and disruptors of this process)
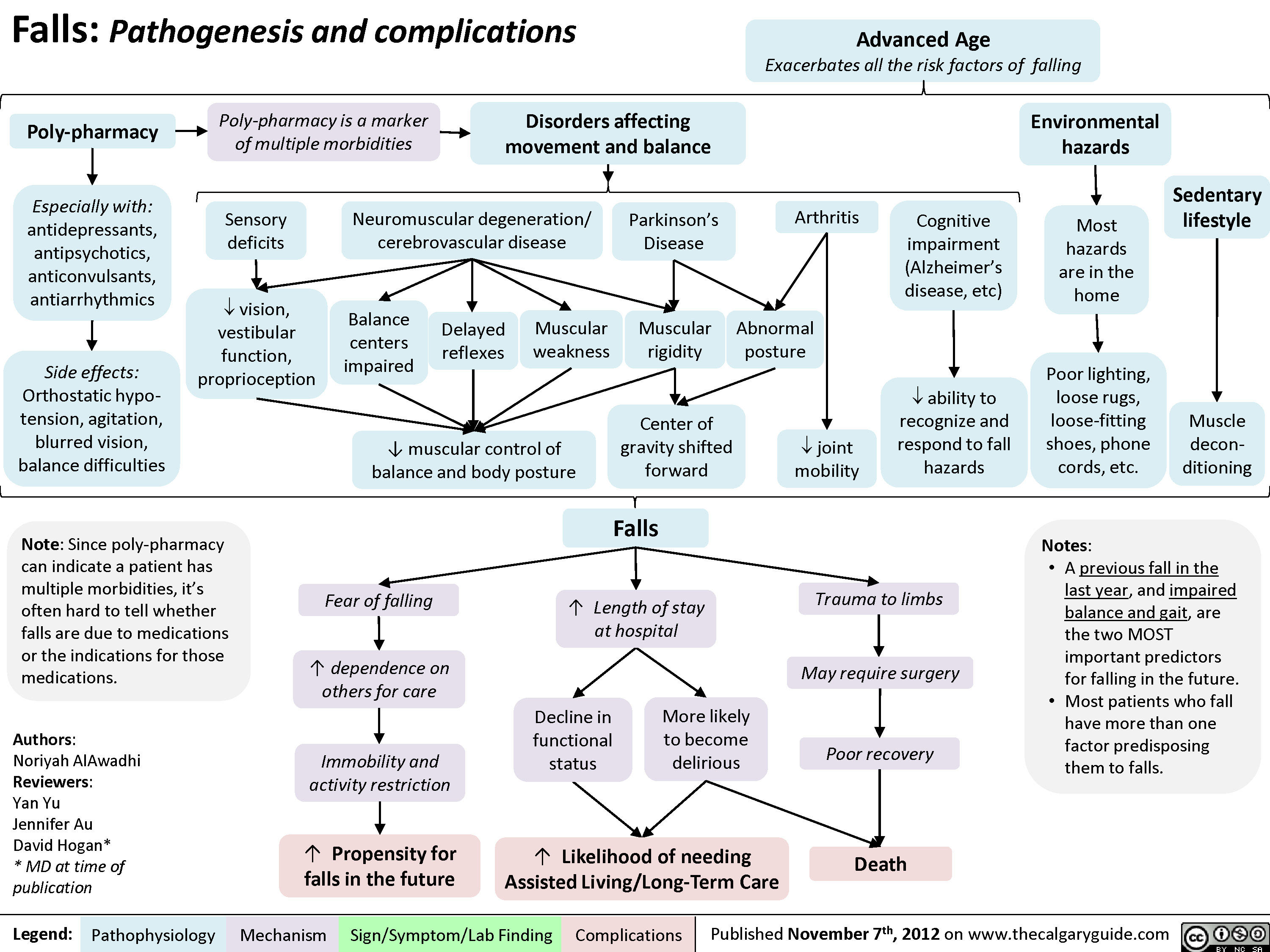
Falls
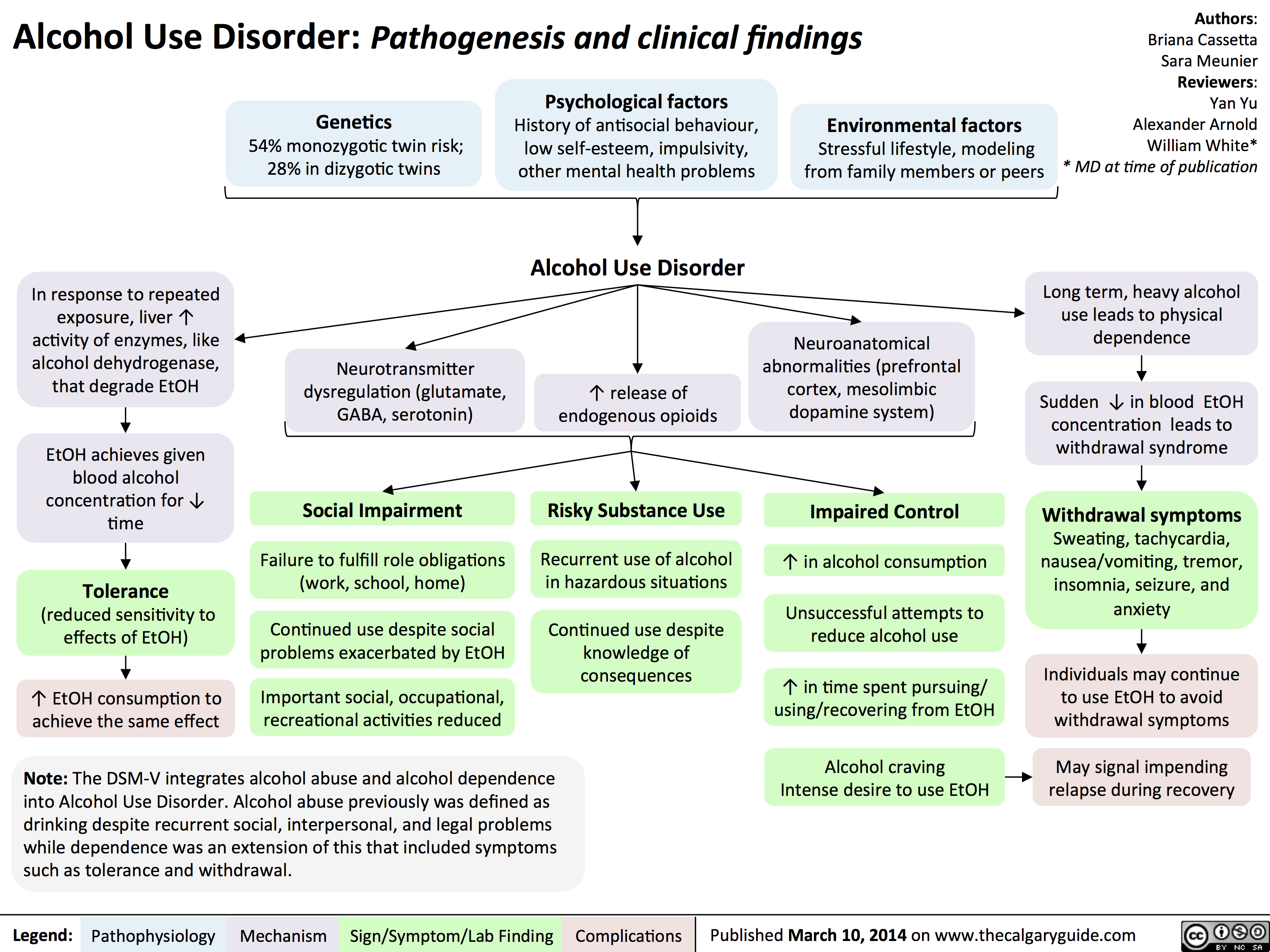
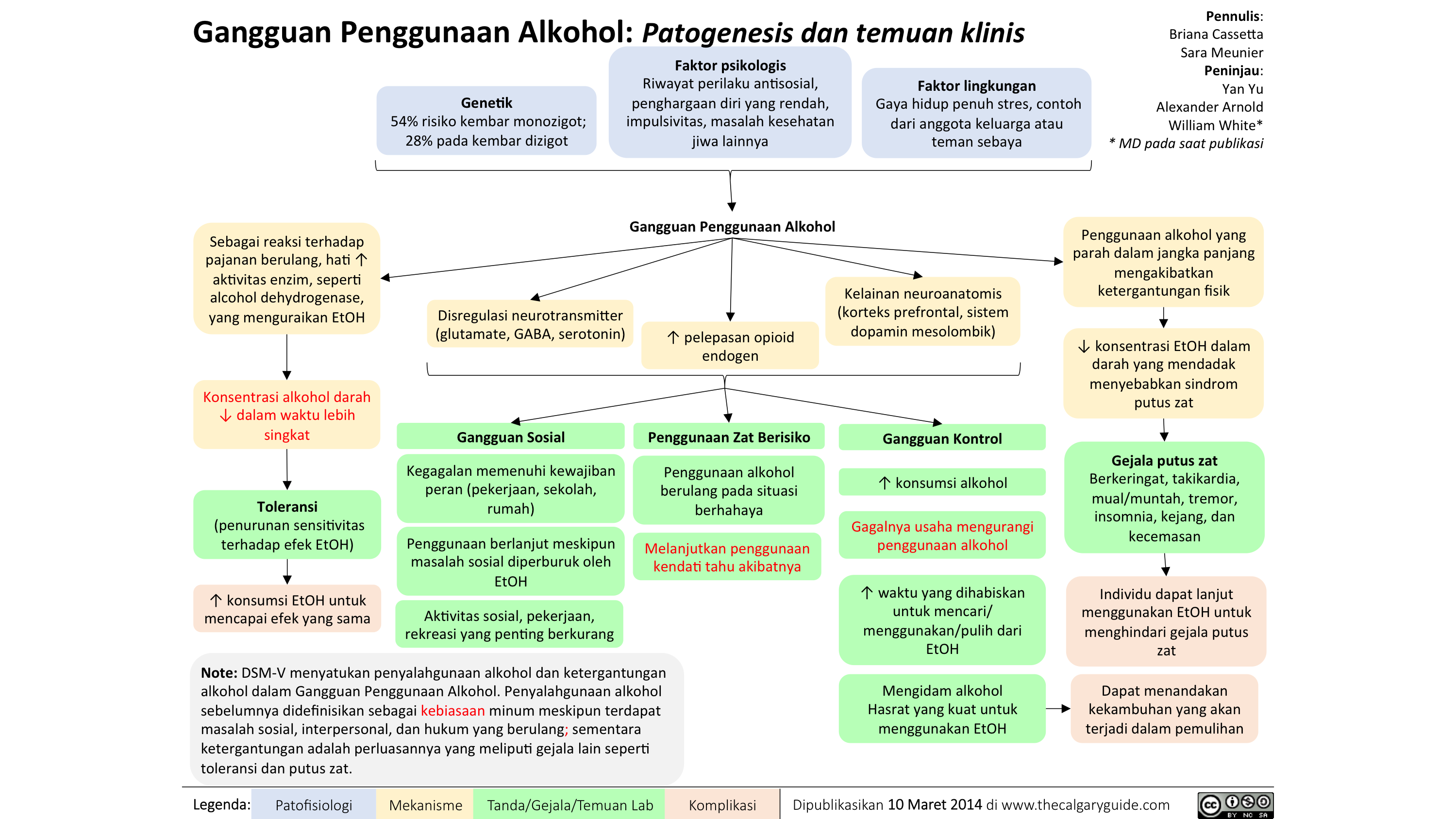
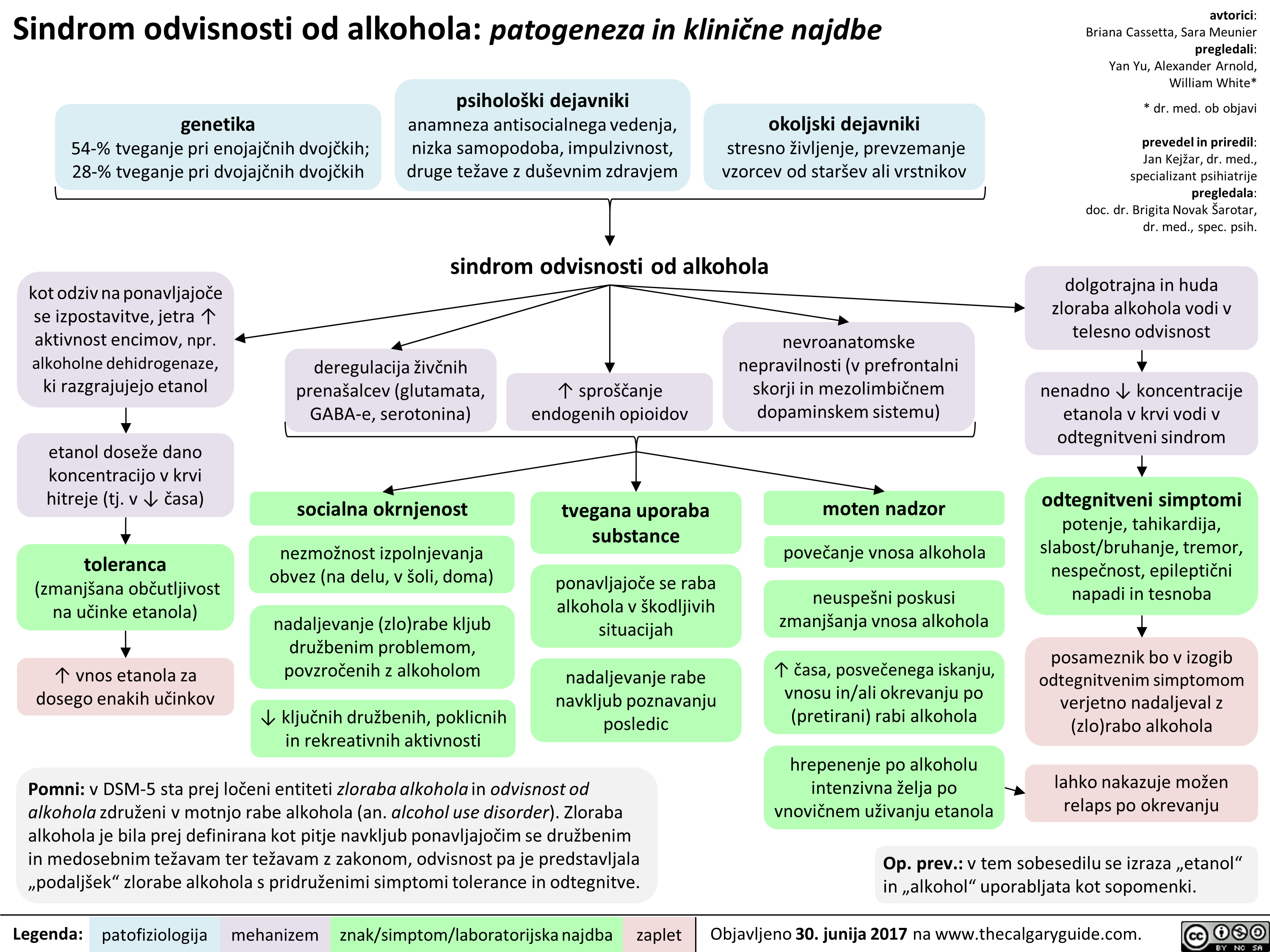
Alcohol Use Disorder
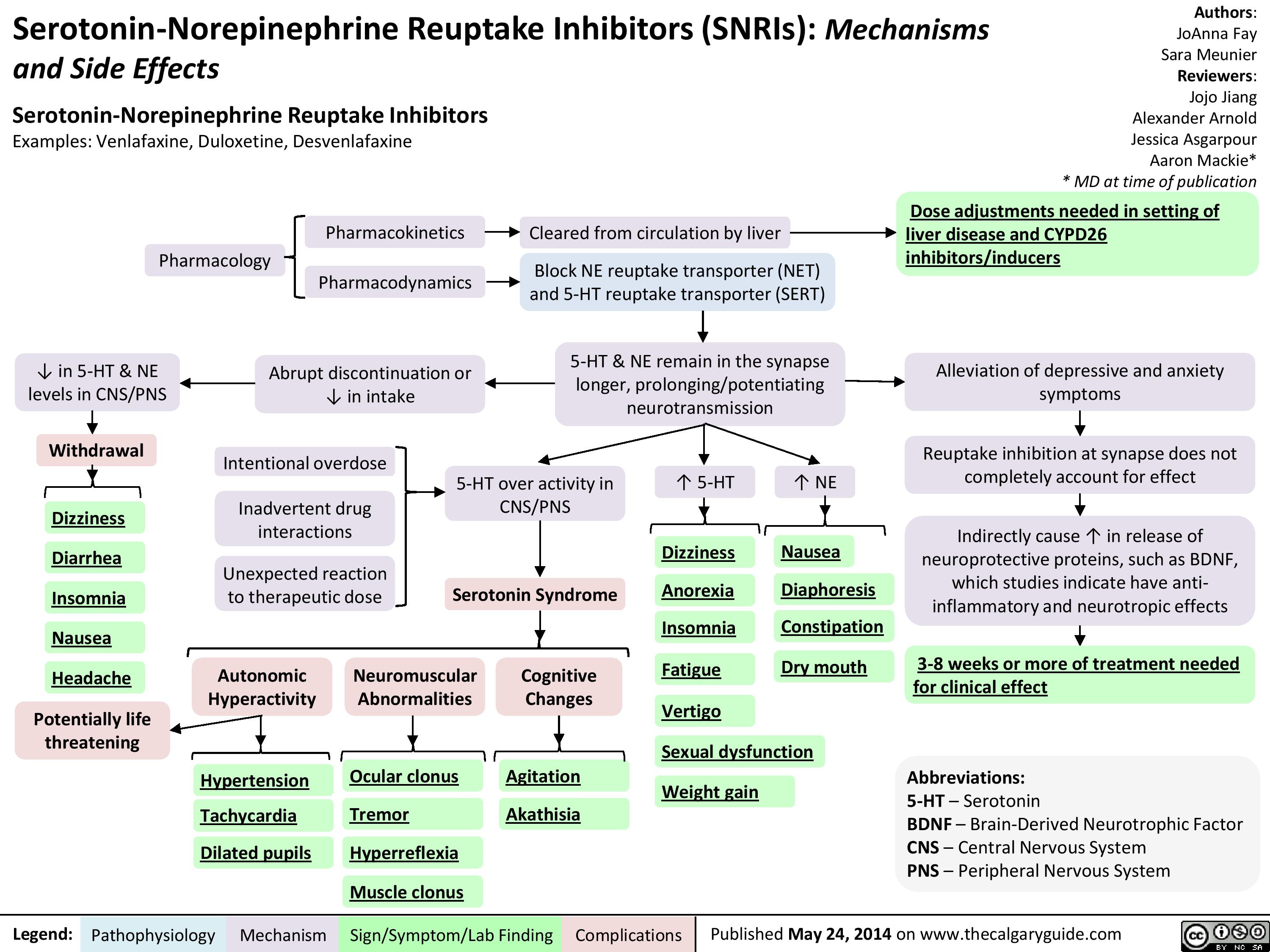
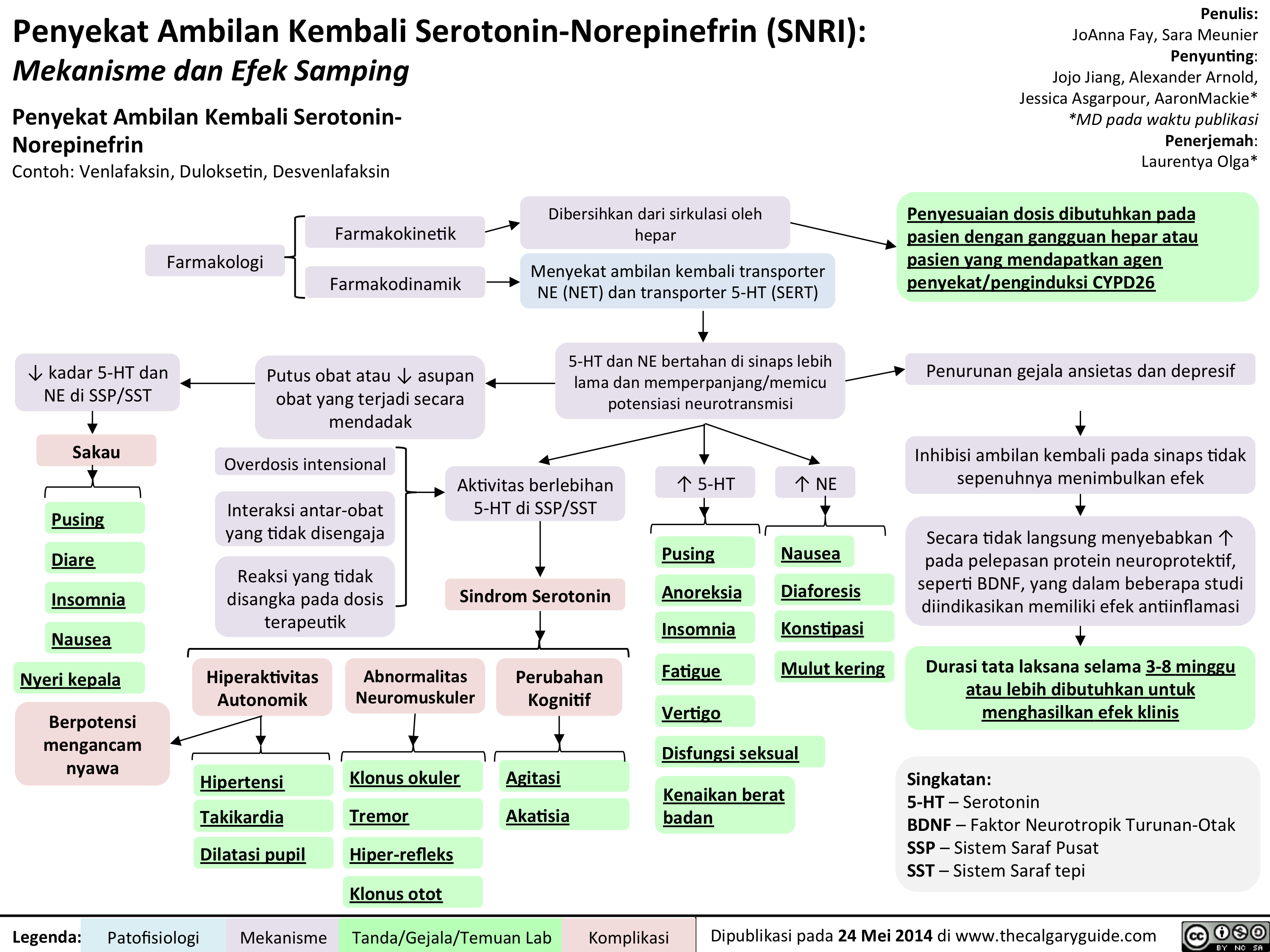
SNRIs
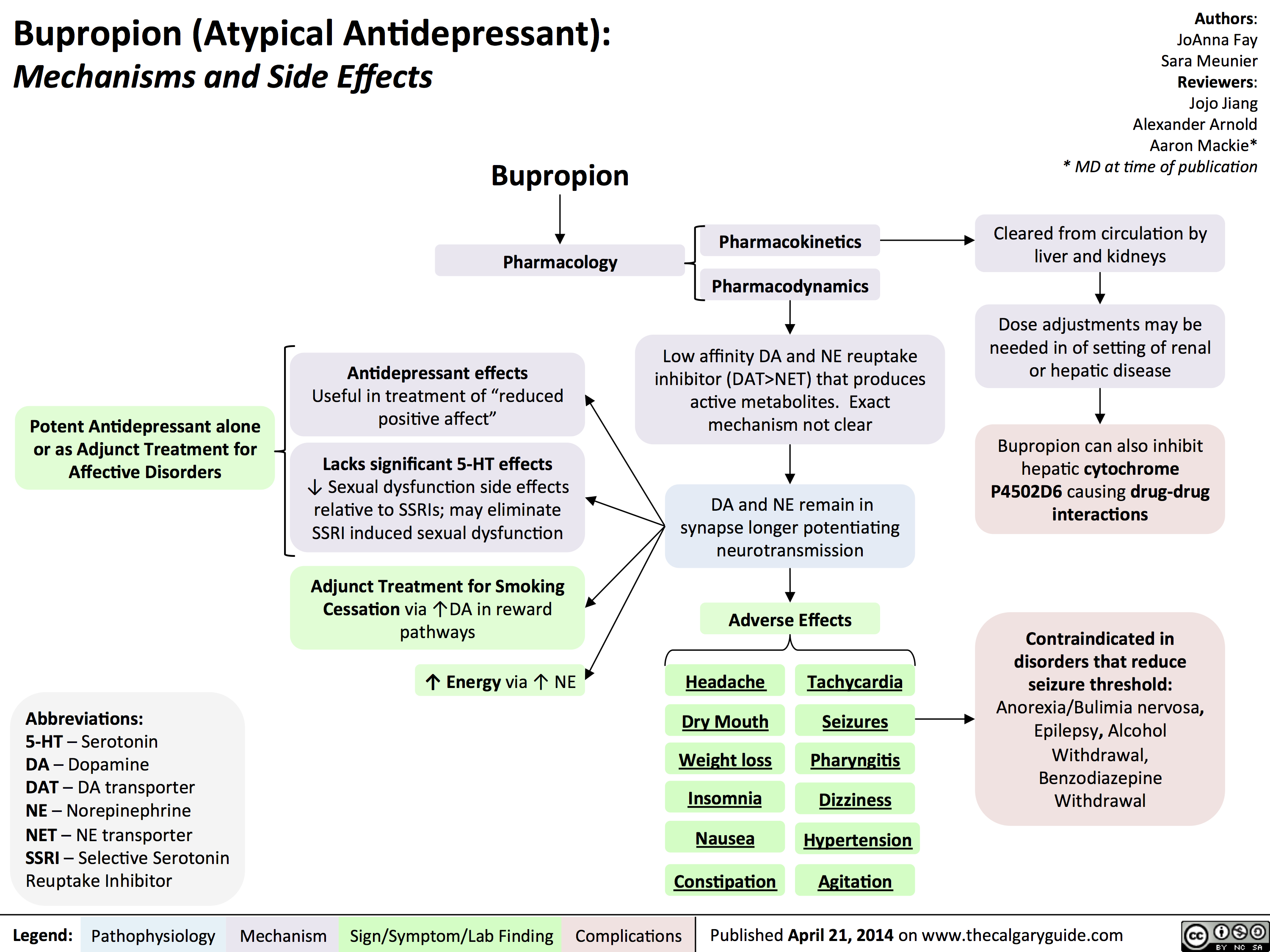
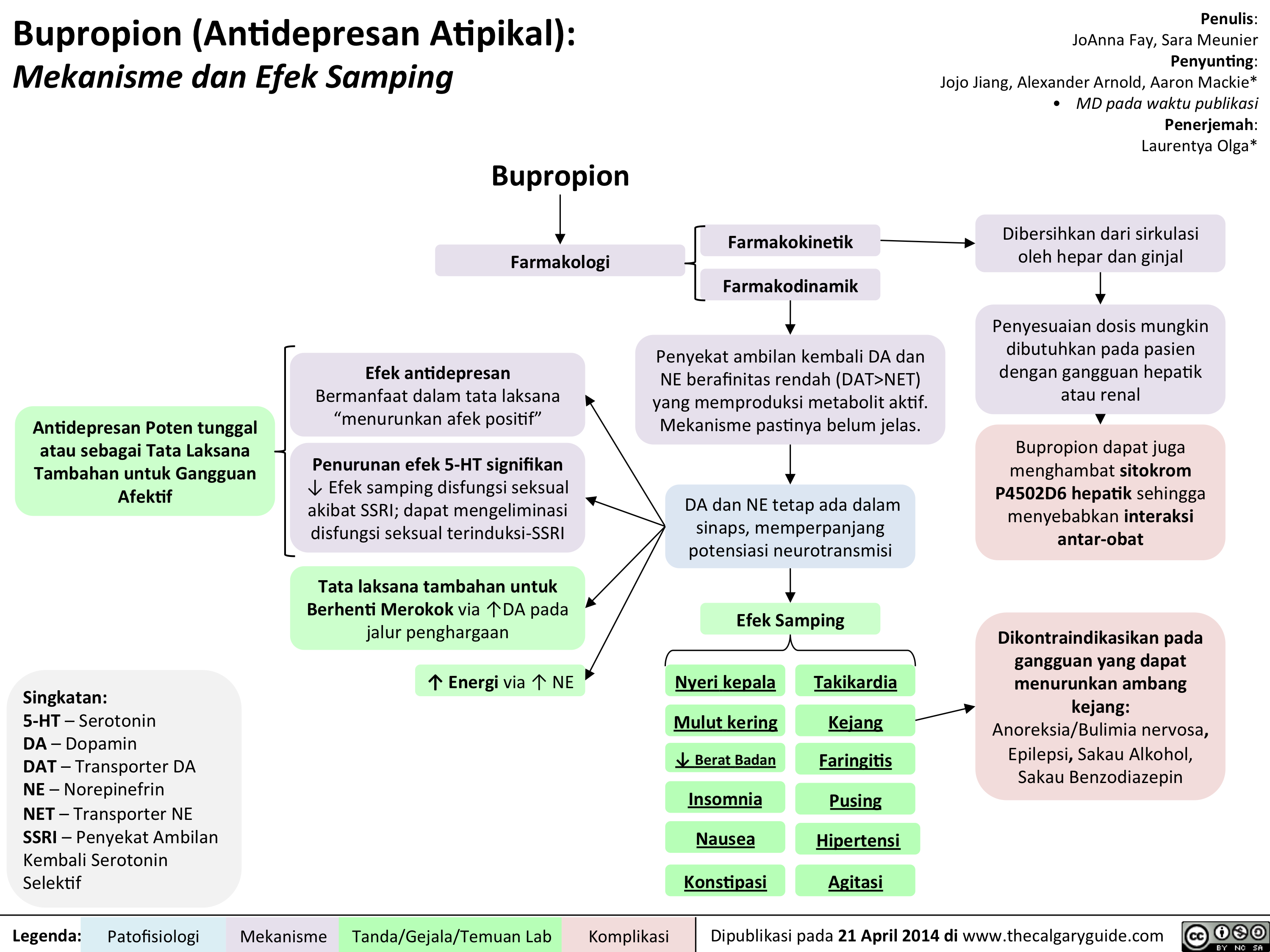
Bupropion
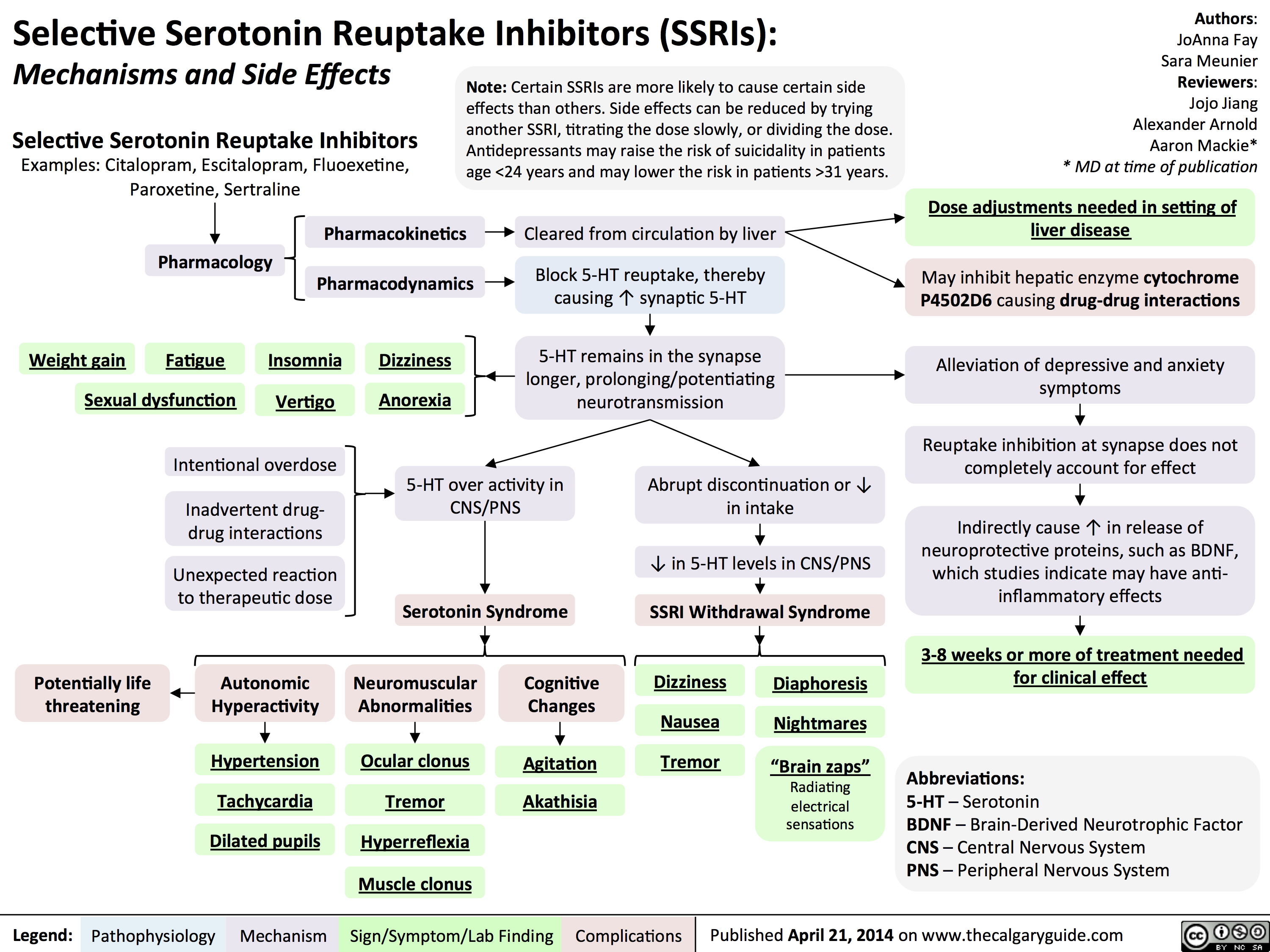
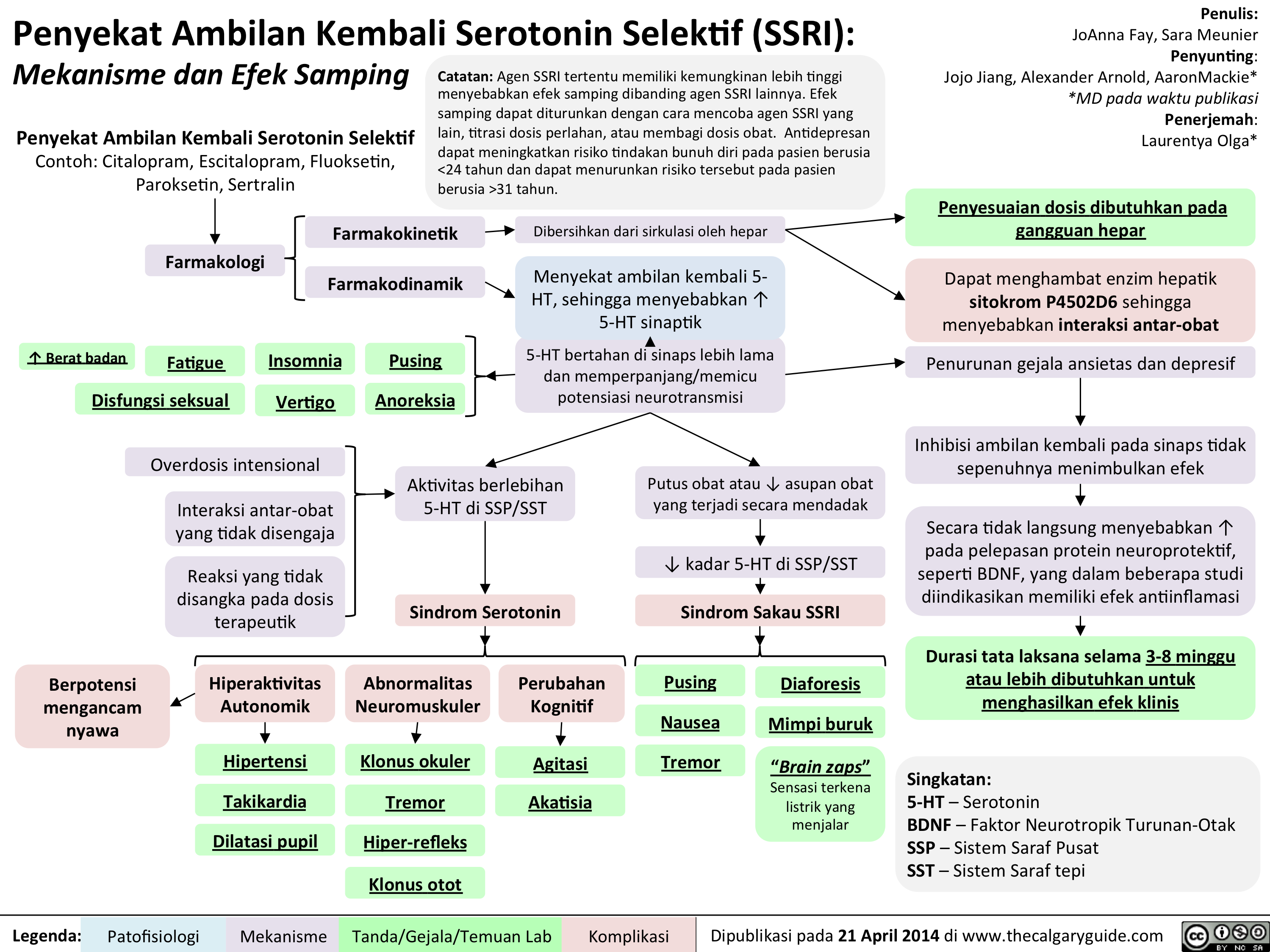
SSRIs
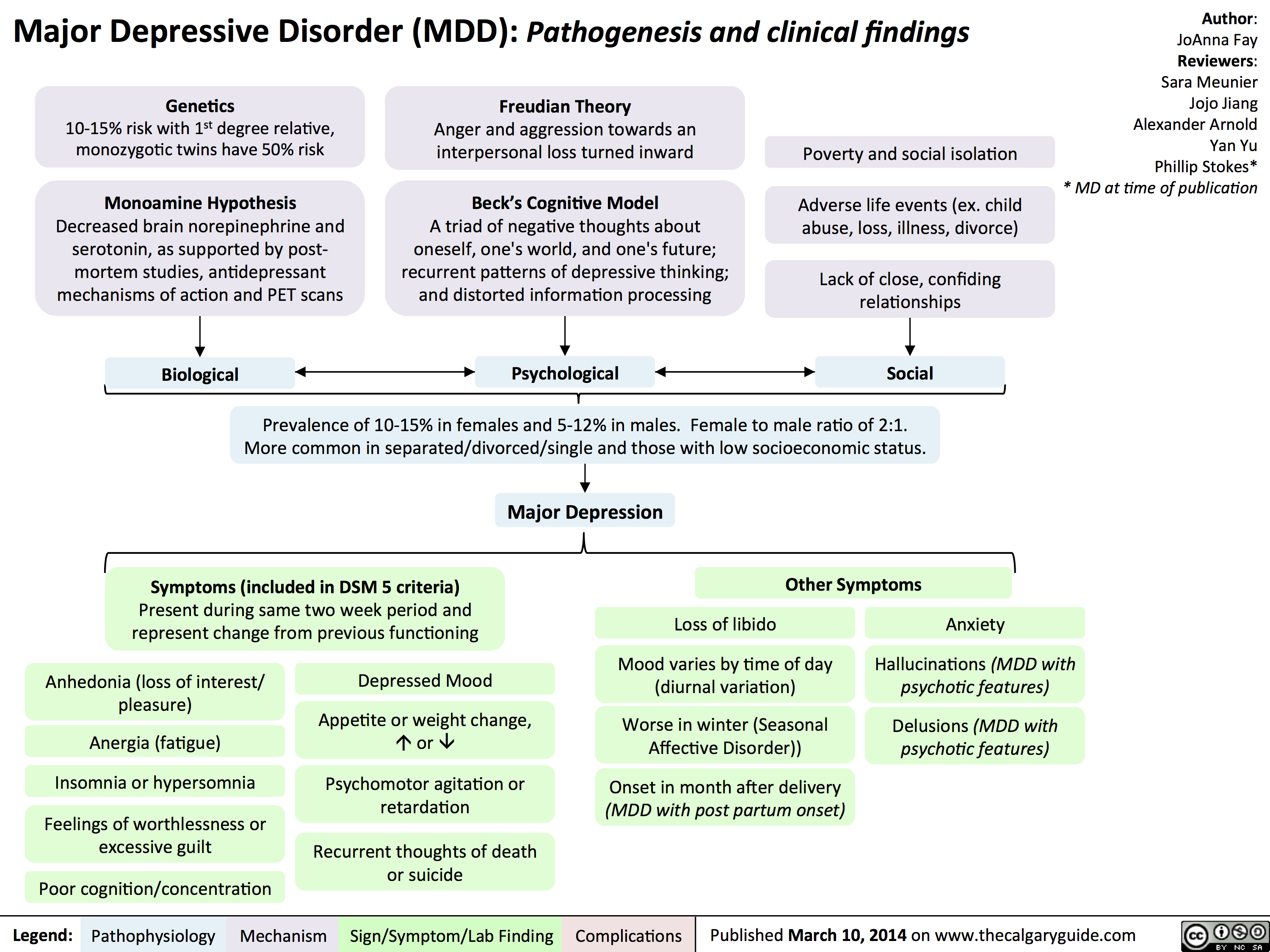
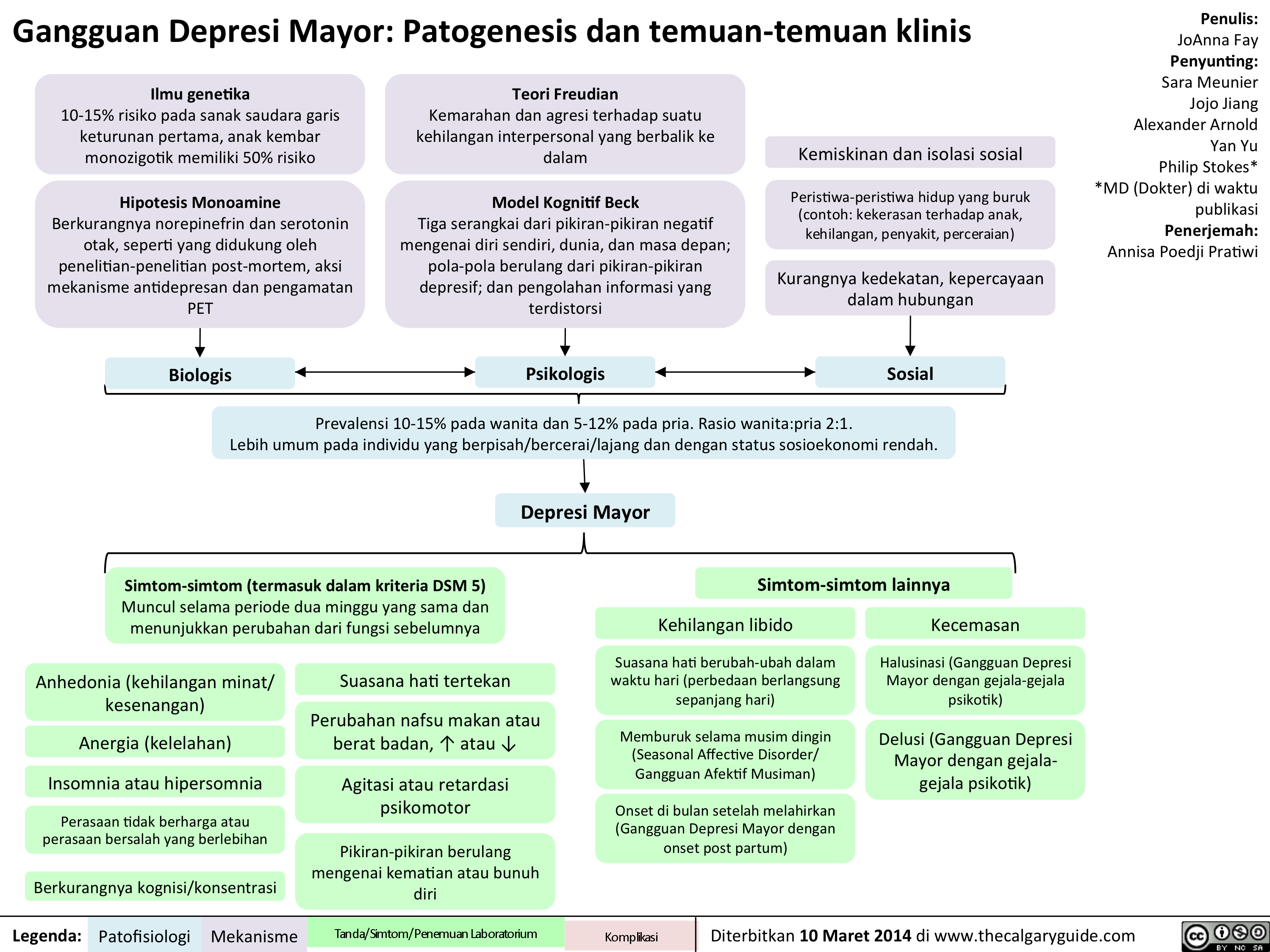
MDD
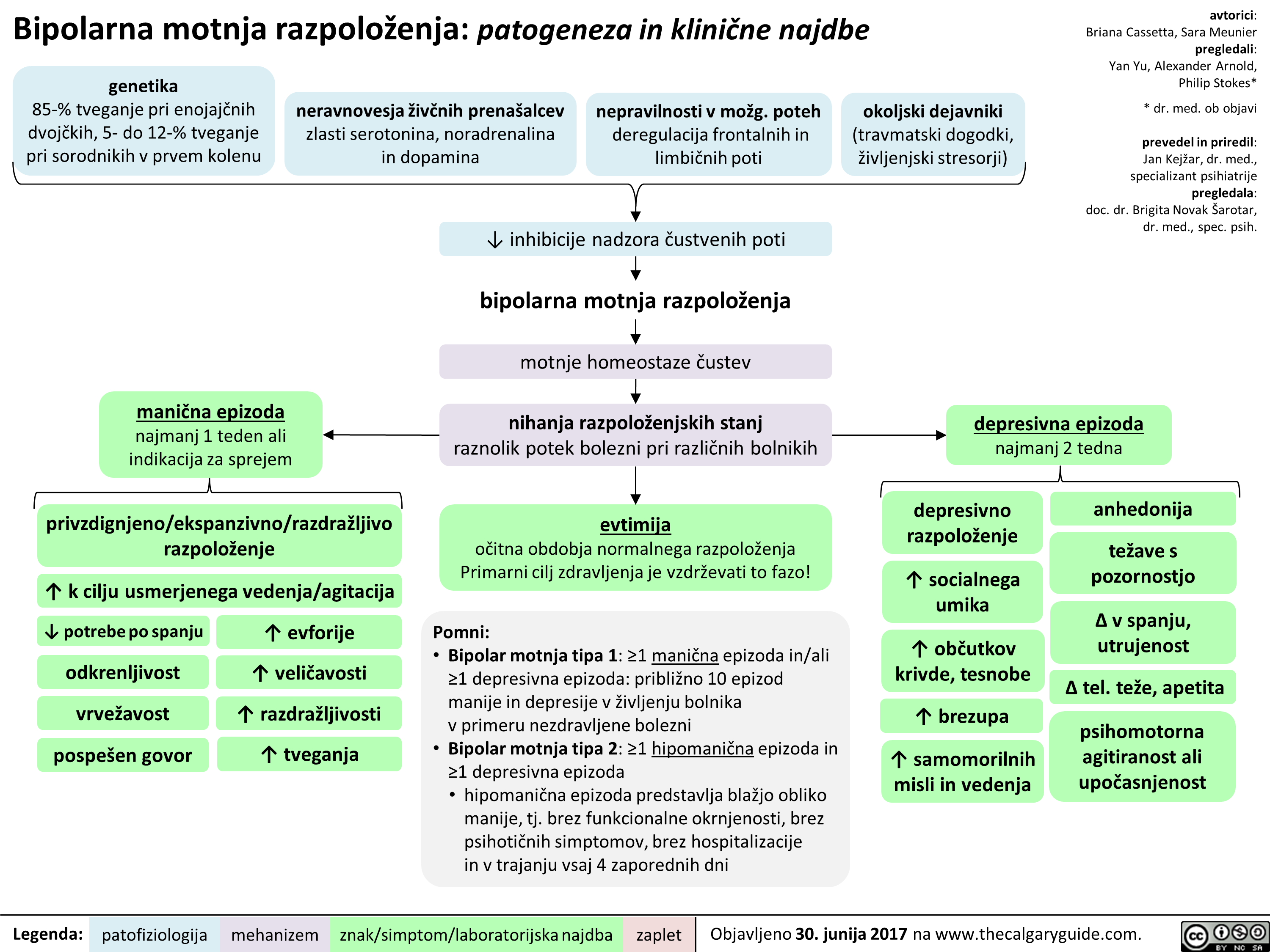
BipolarDisorder

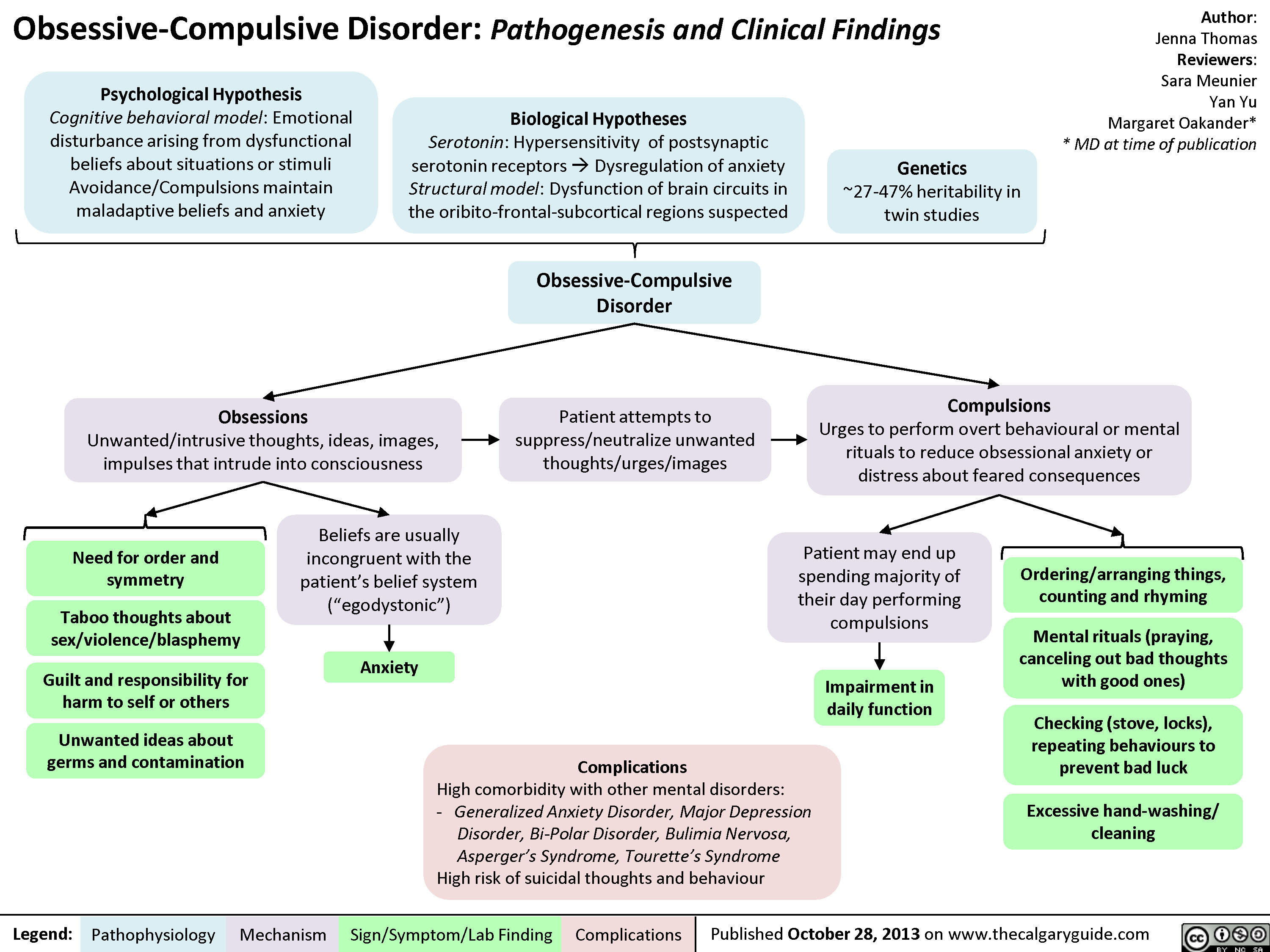
OCD
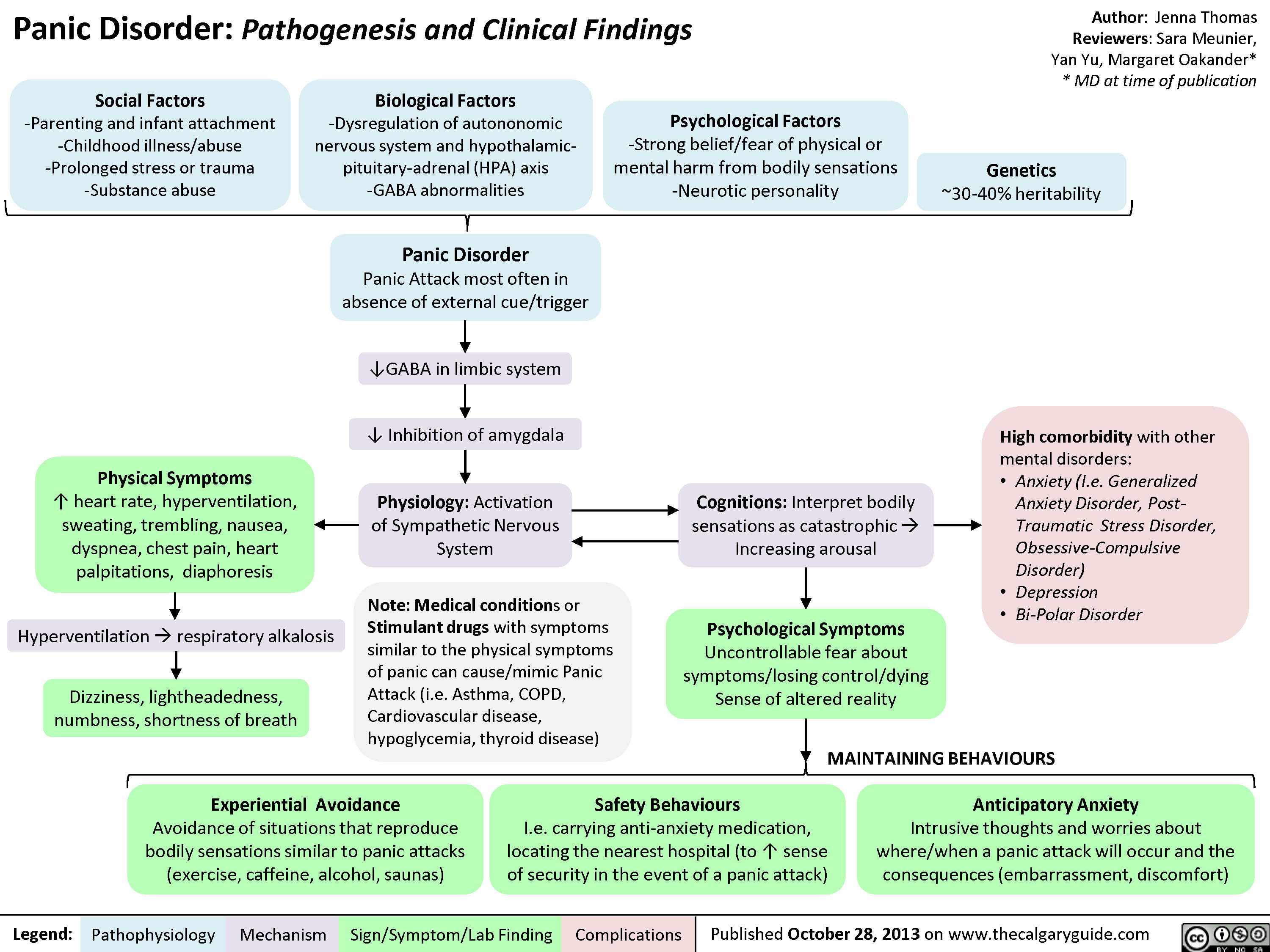
Panic Disorder
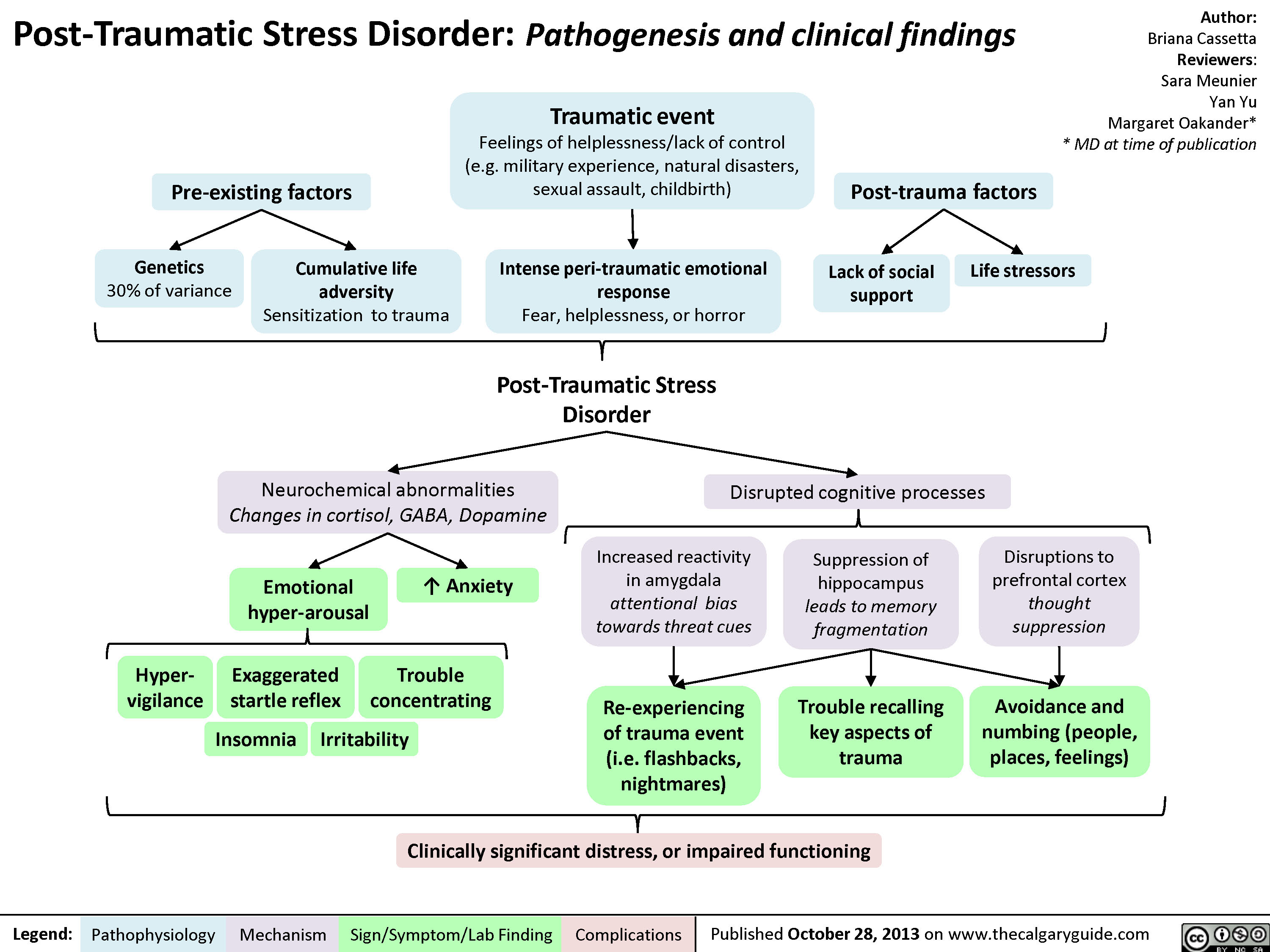
PTSD
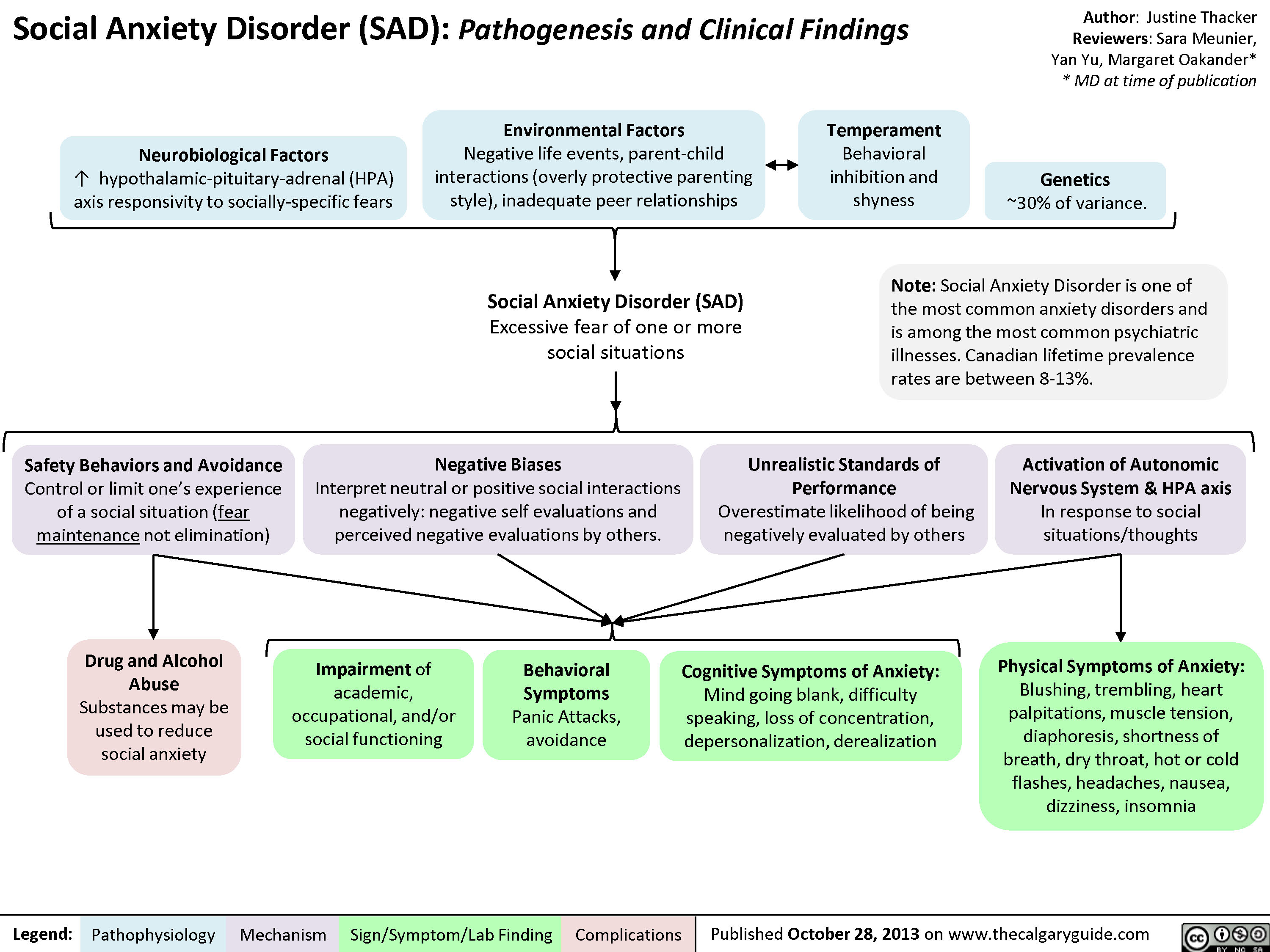
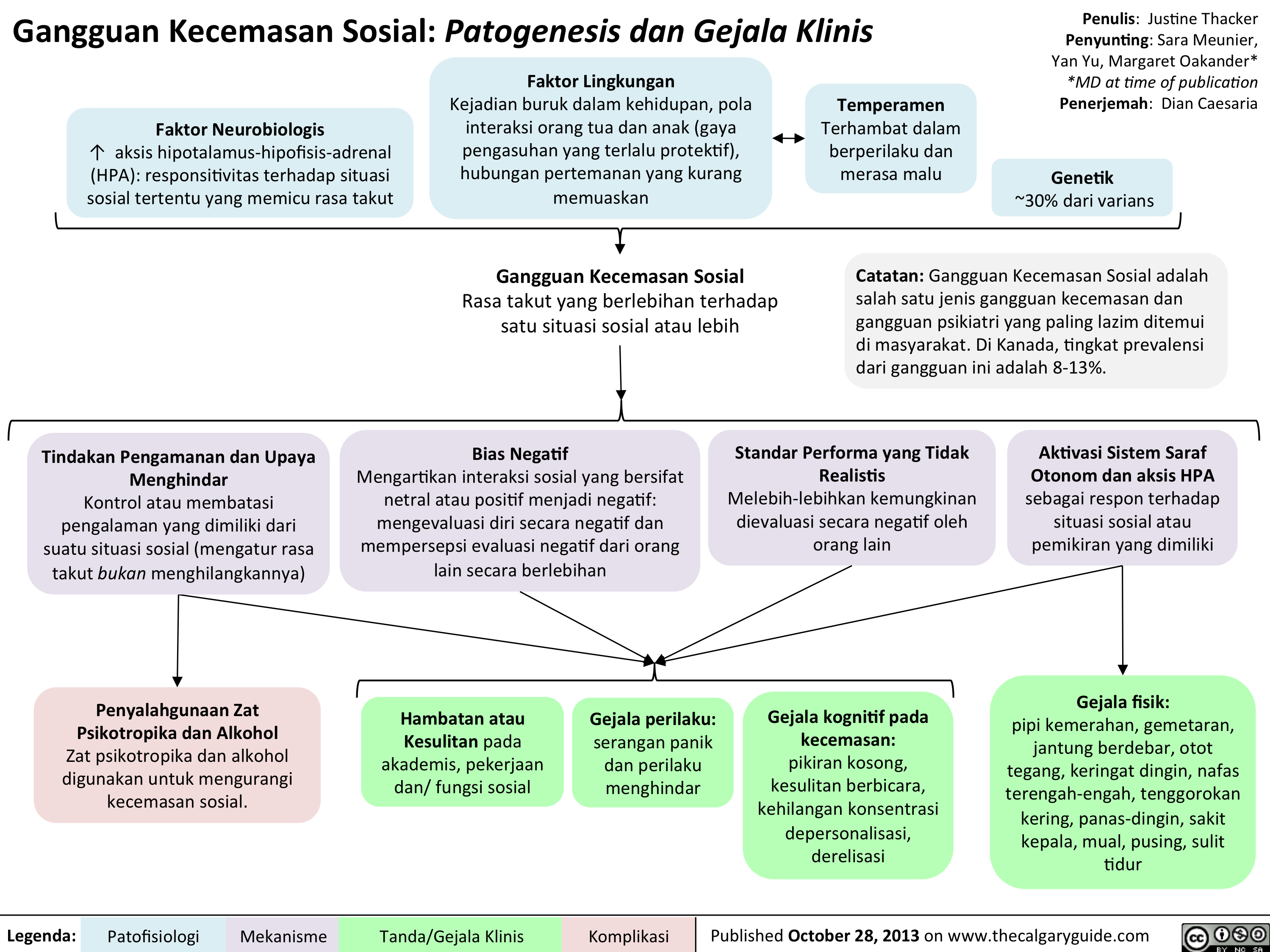
Social Anxiety
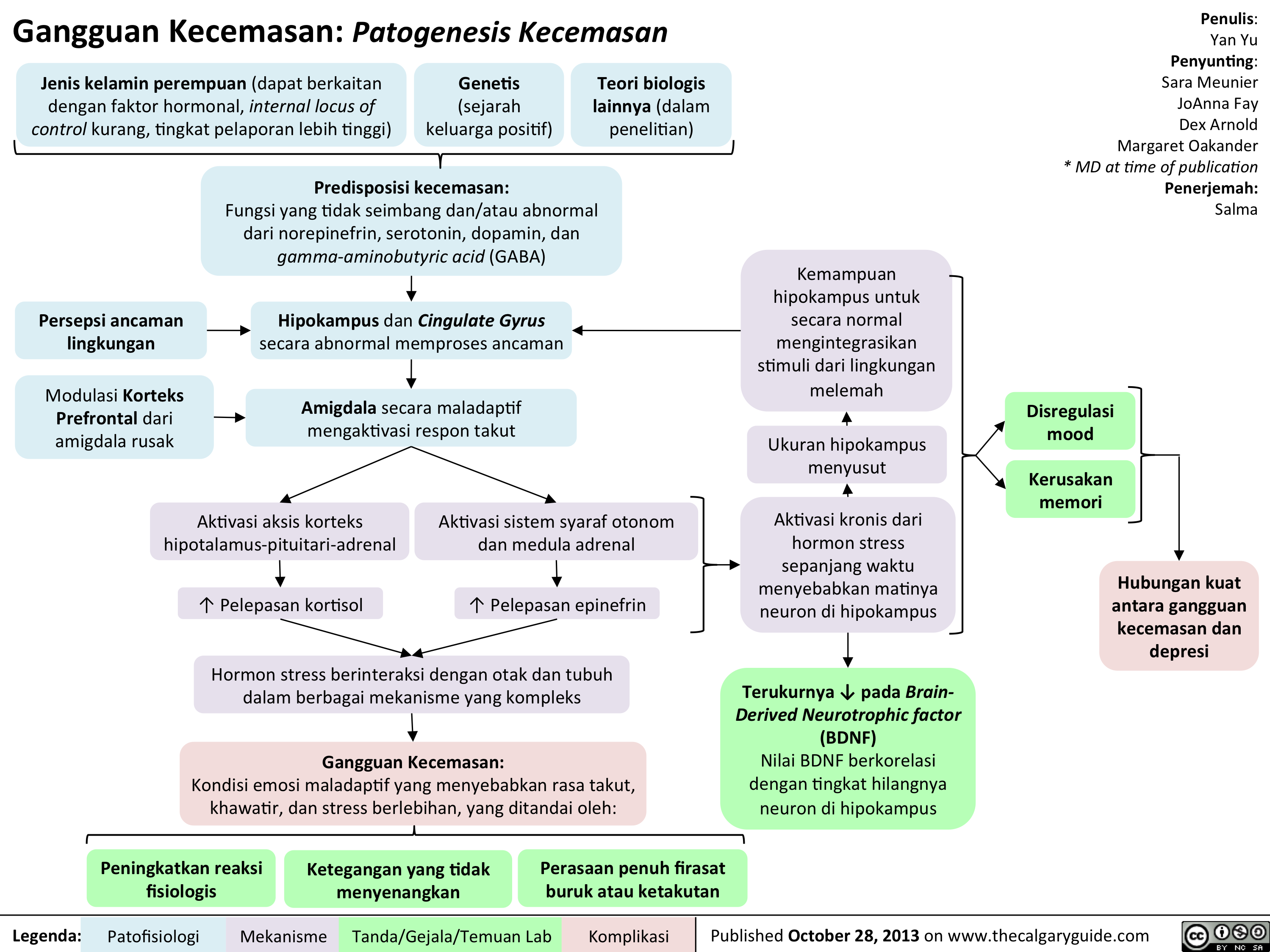
Pathogenesis of Anxiety Disorders

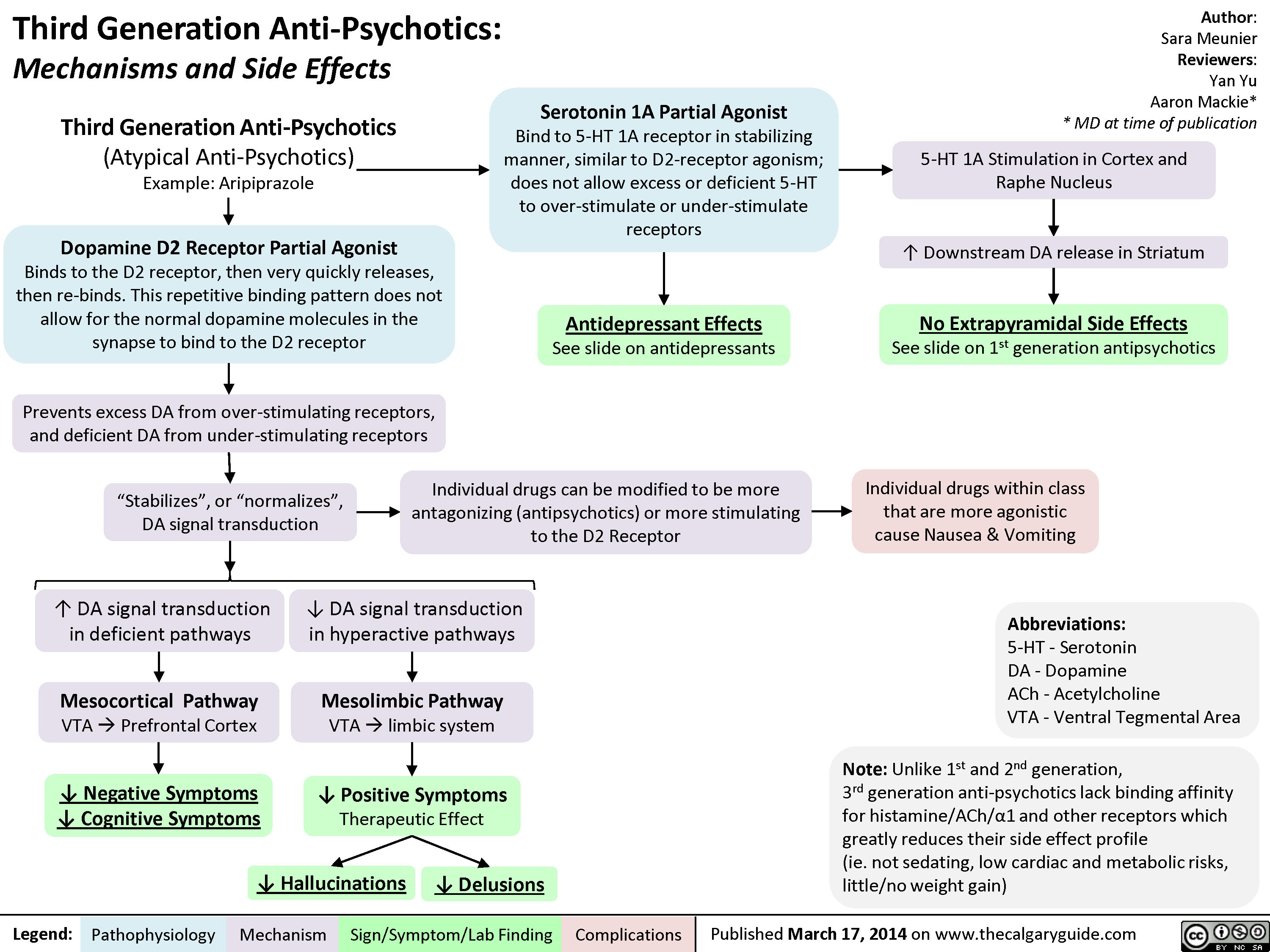
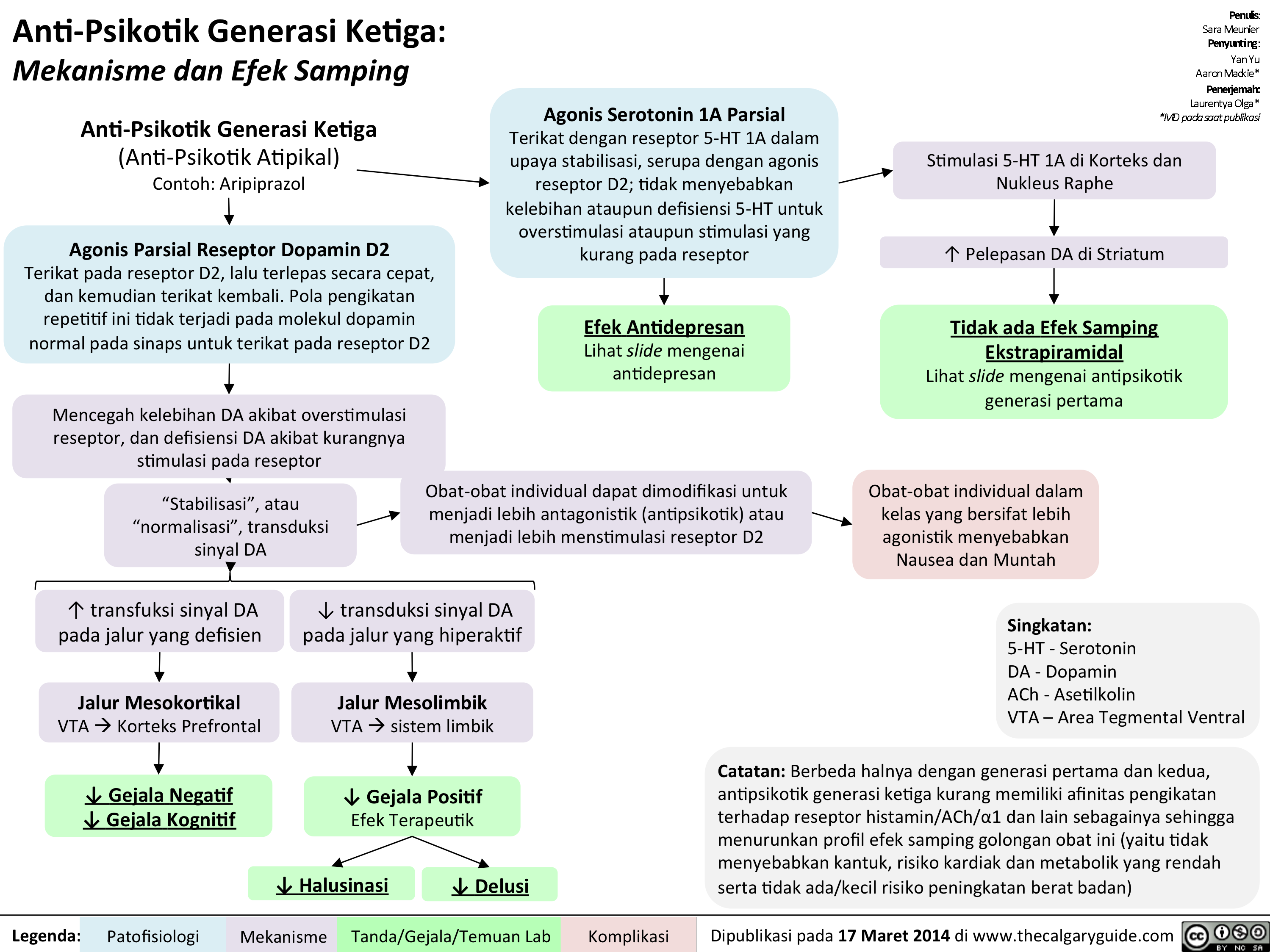
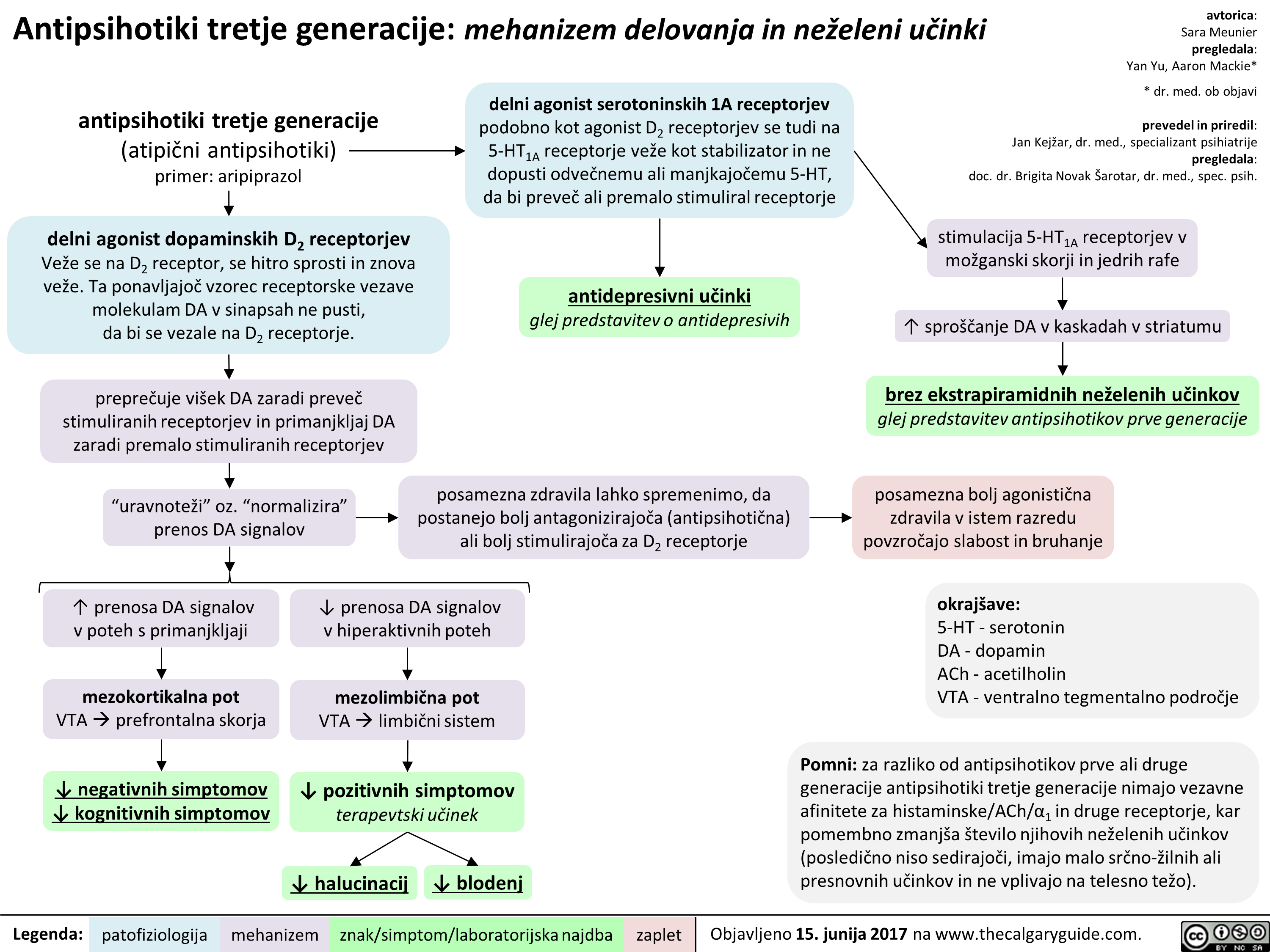
3rd gen anti-psychotics
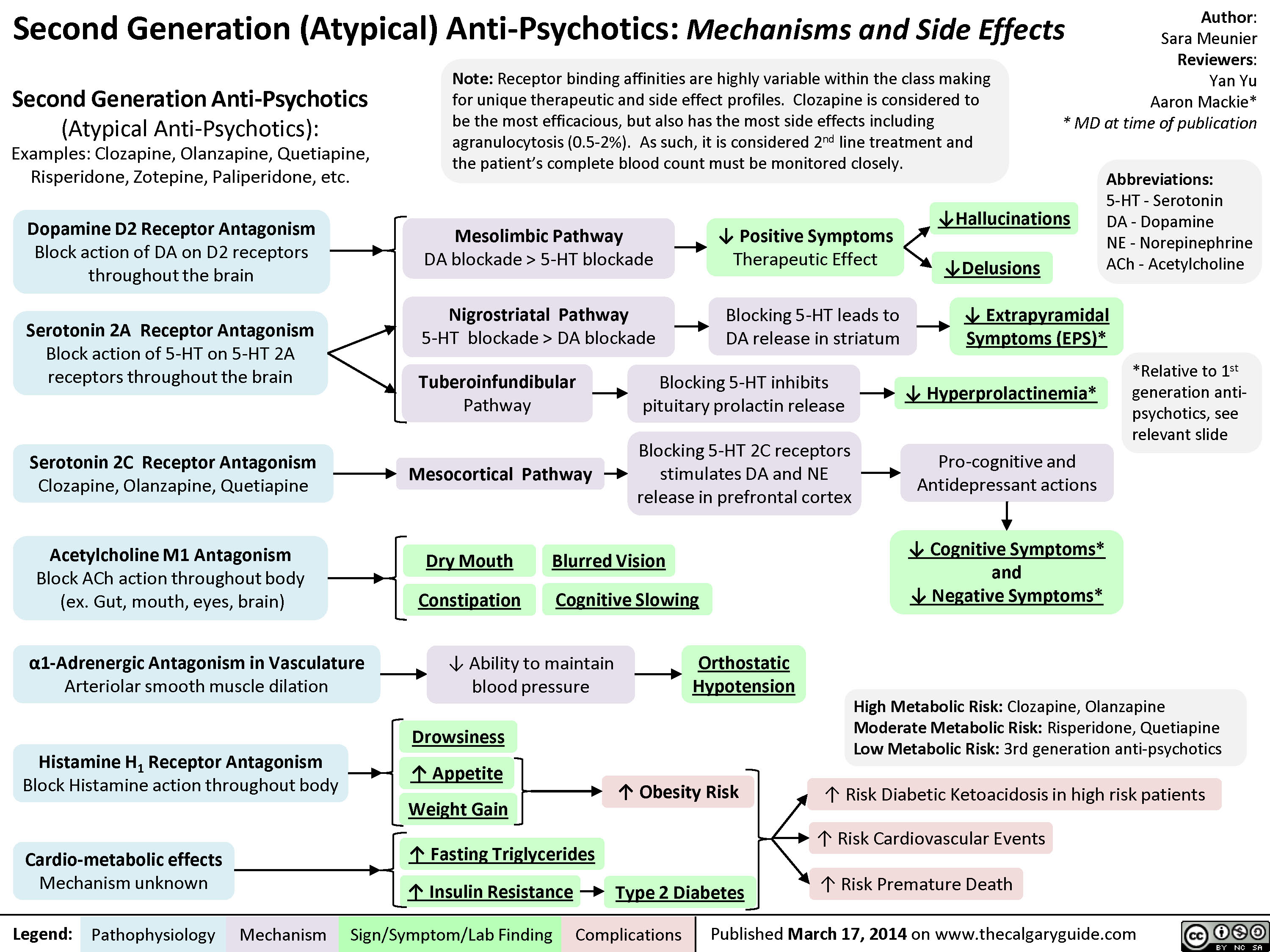
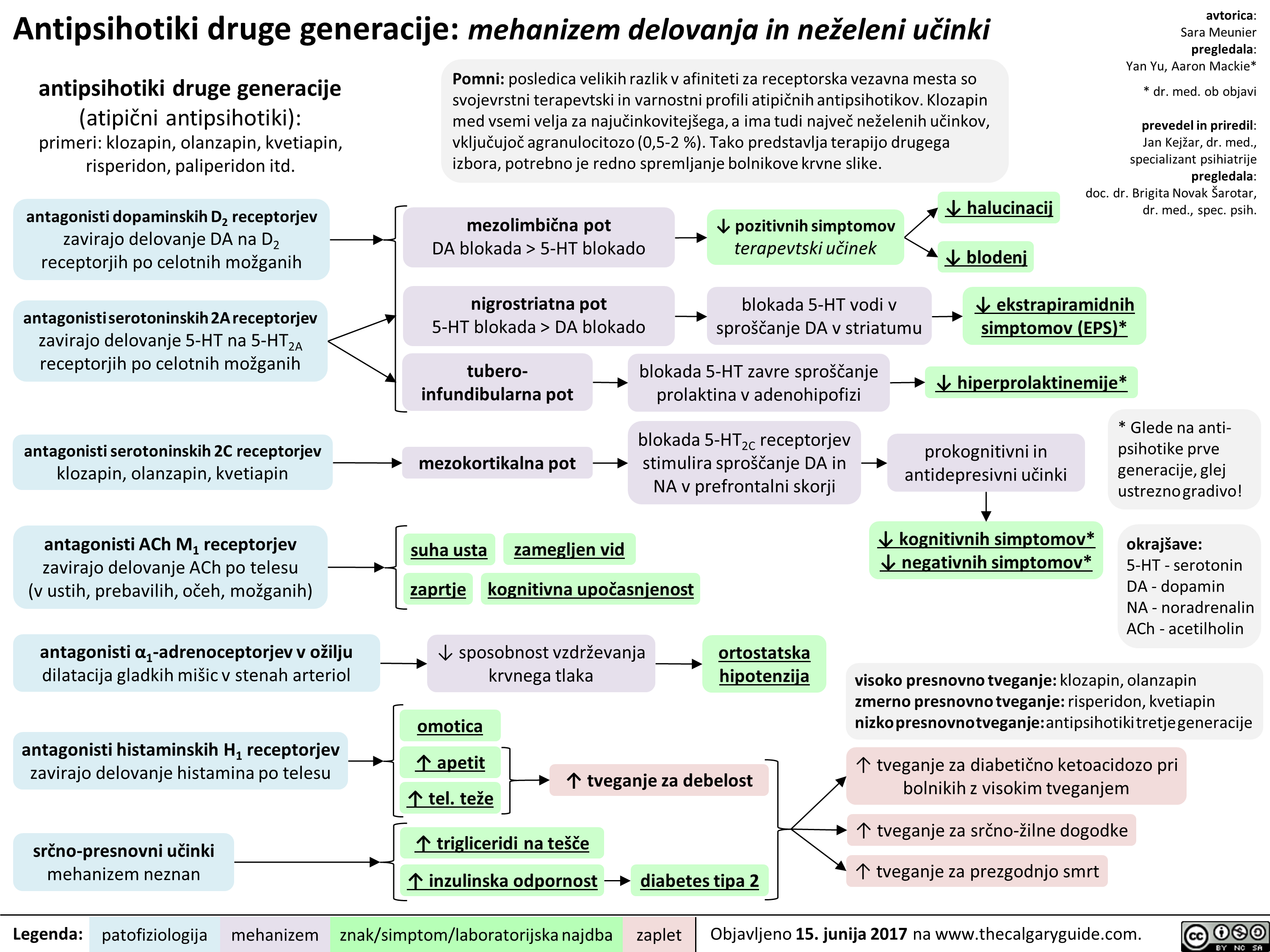
2nd generation antipsychotics
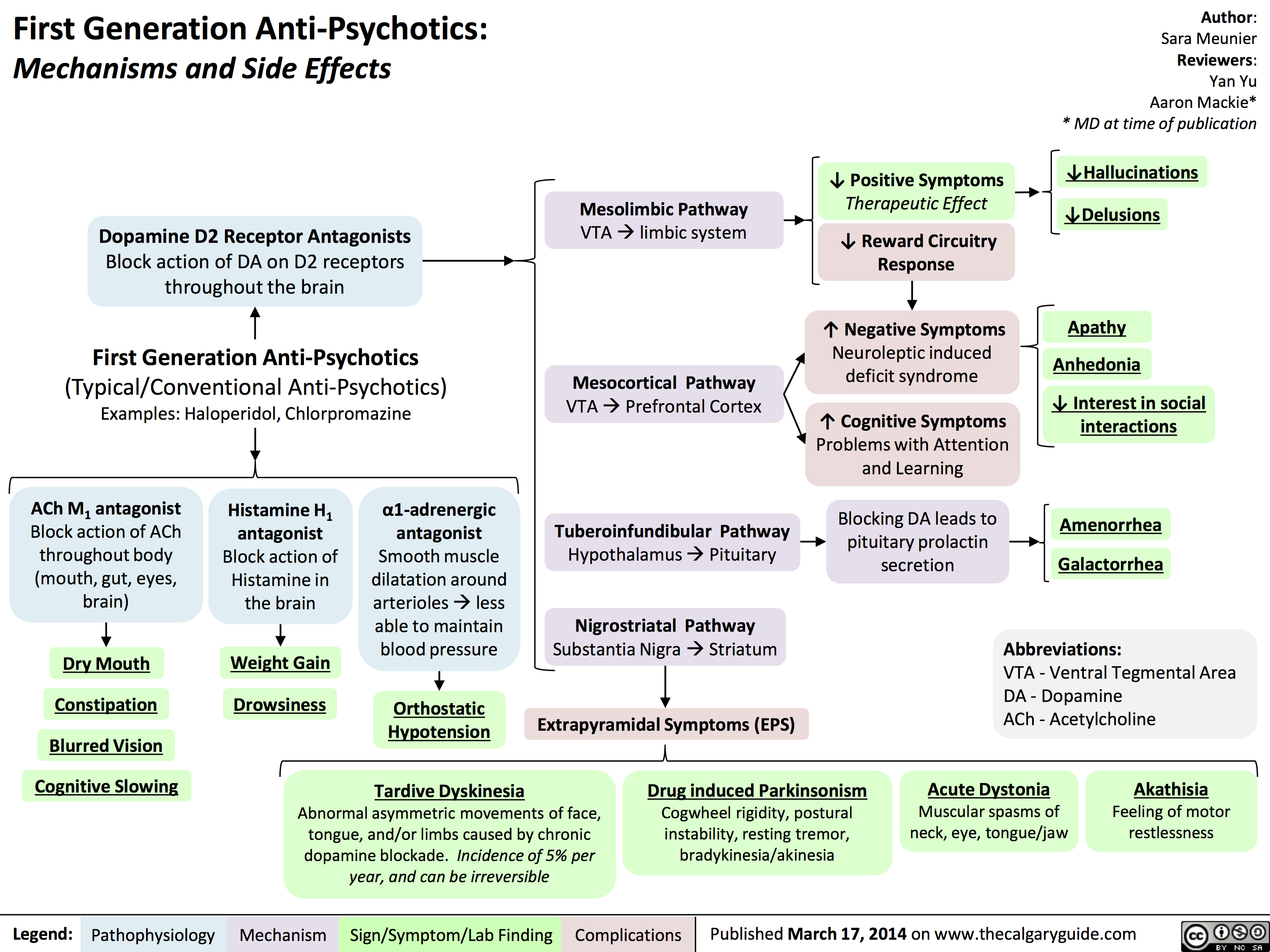
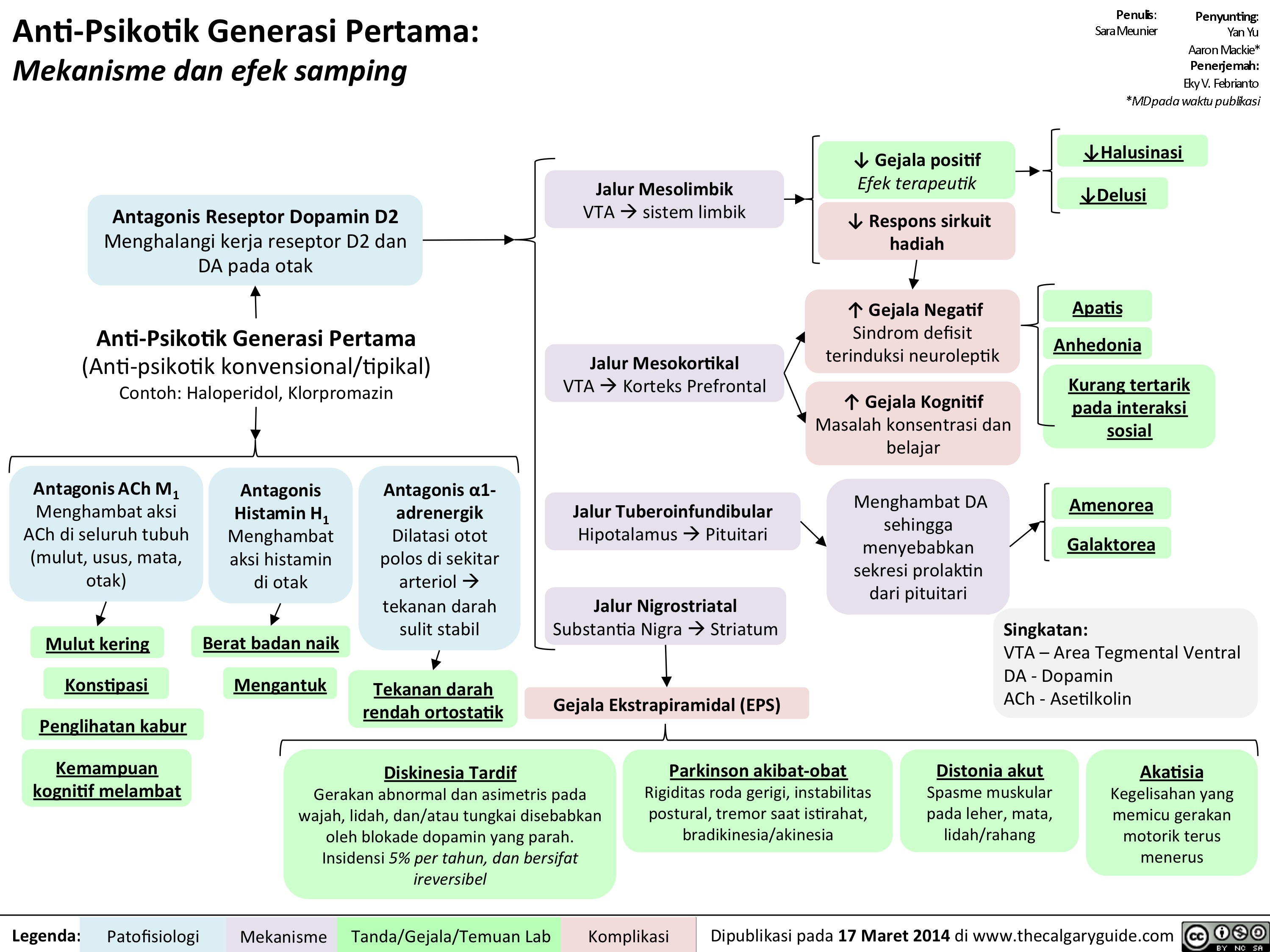
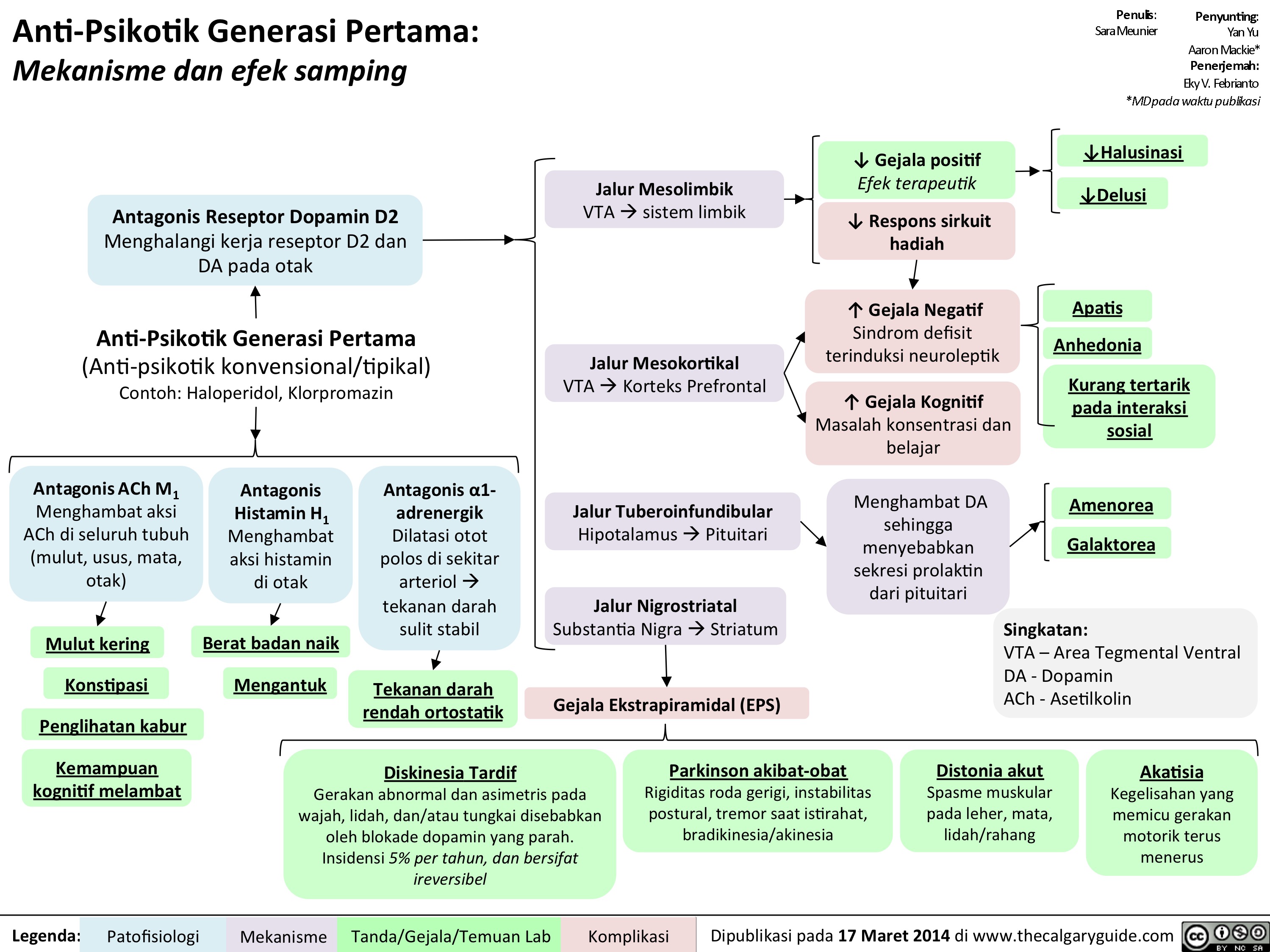
1st gen antipsychotics
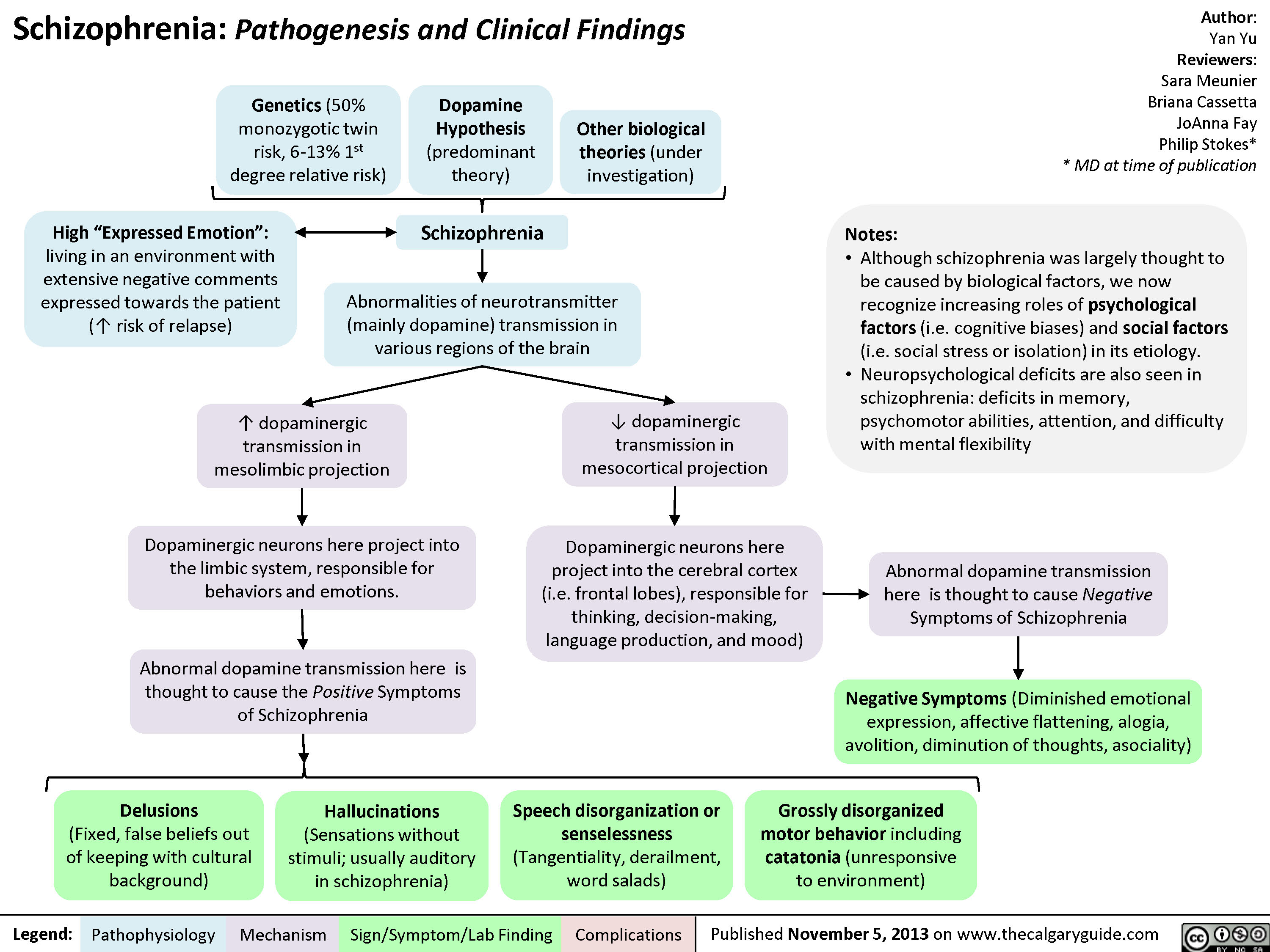
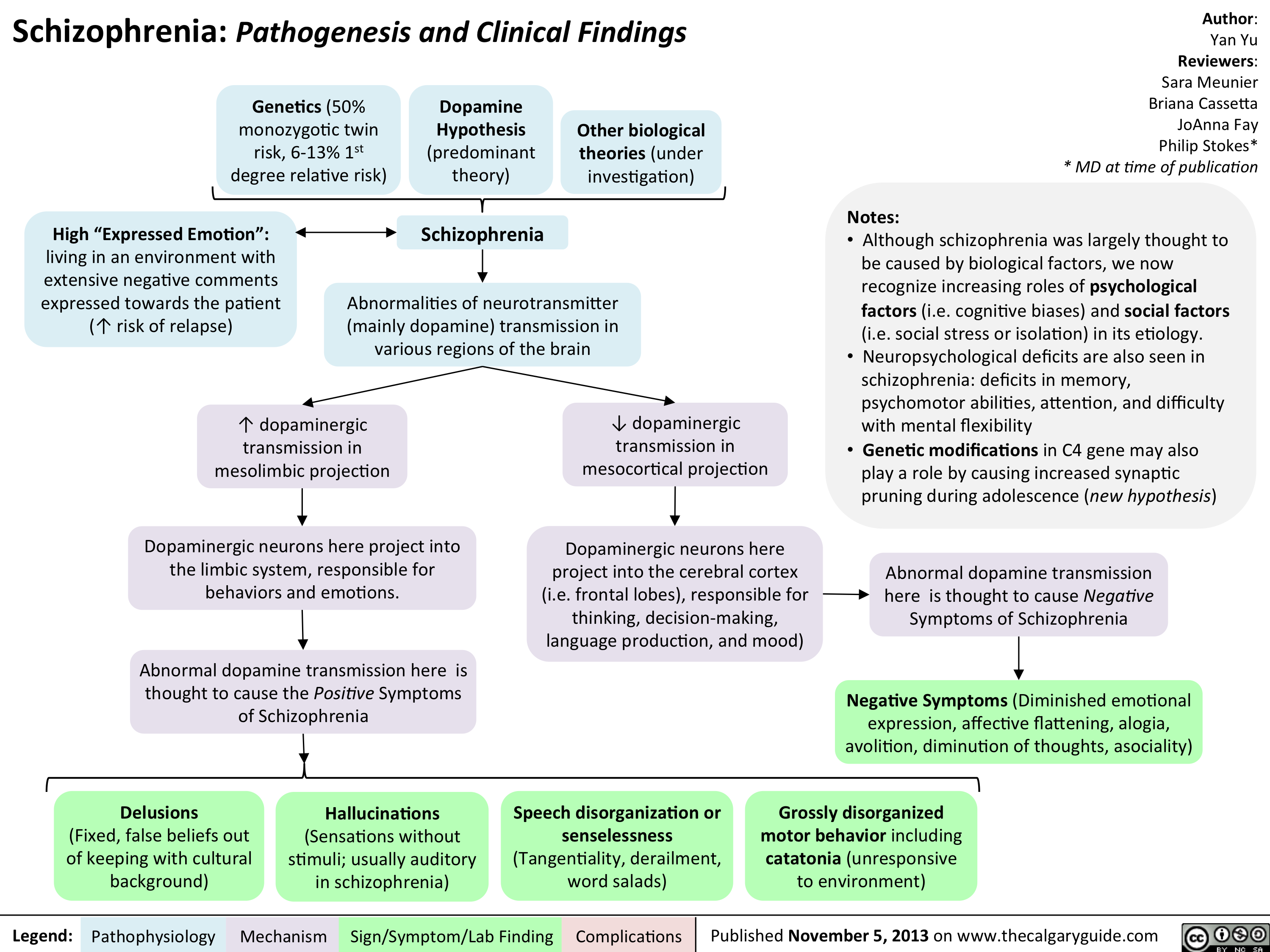
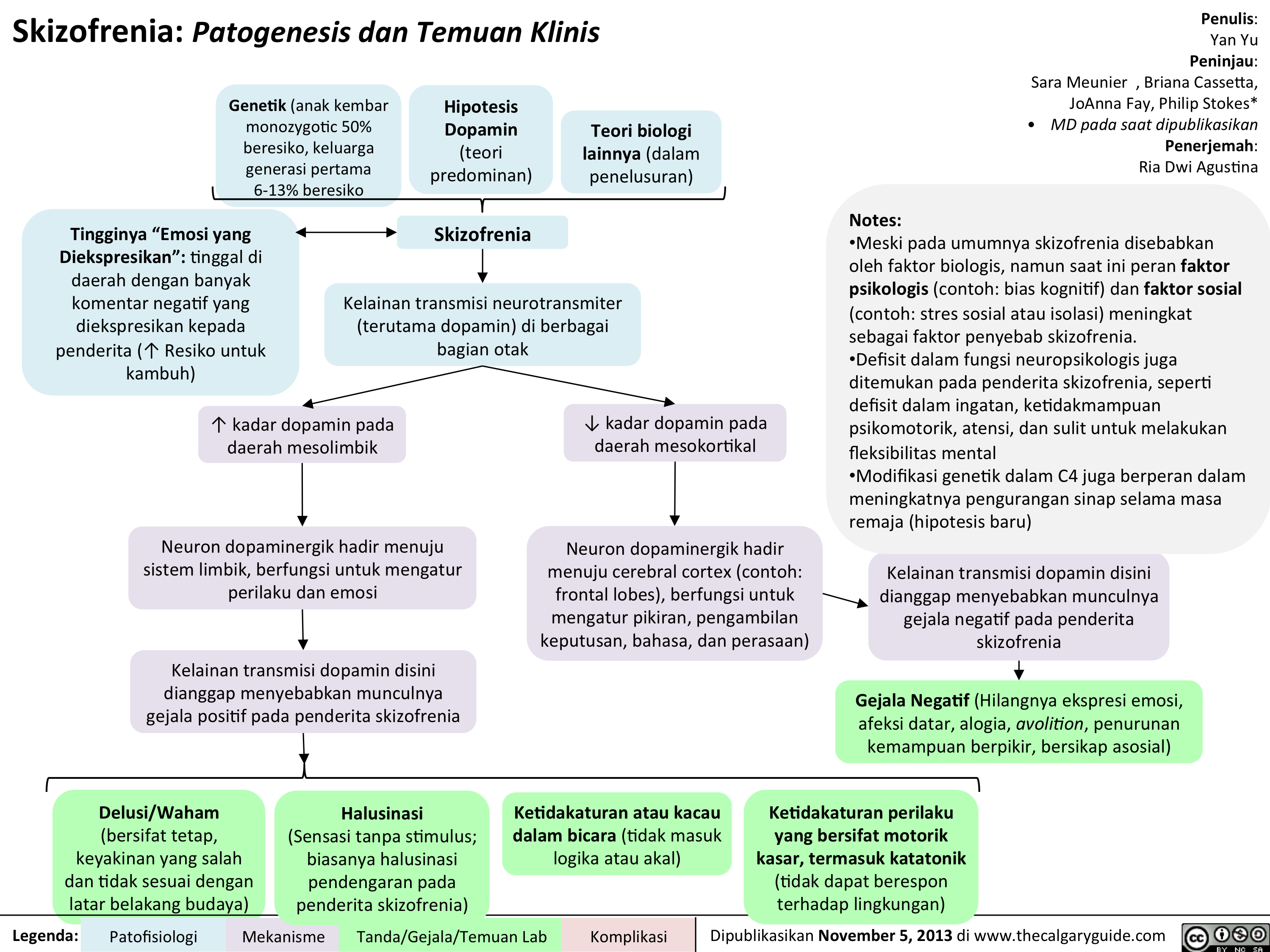
Schizophrenia Pathogenesis and Clinical Findings
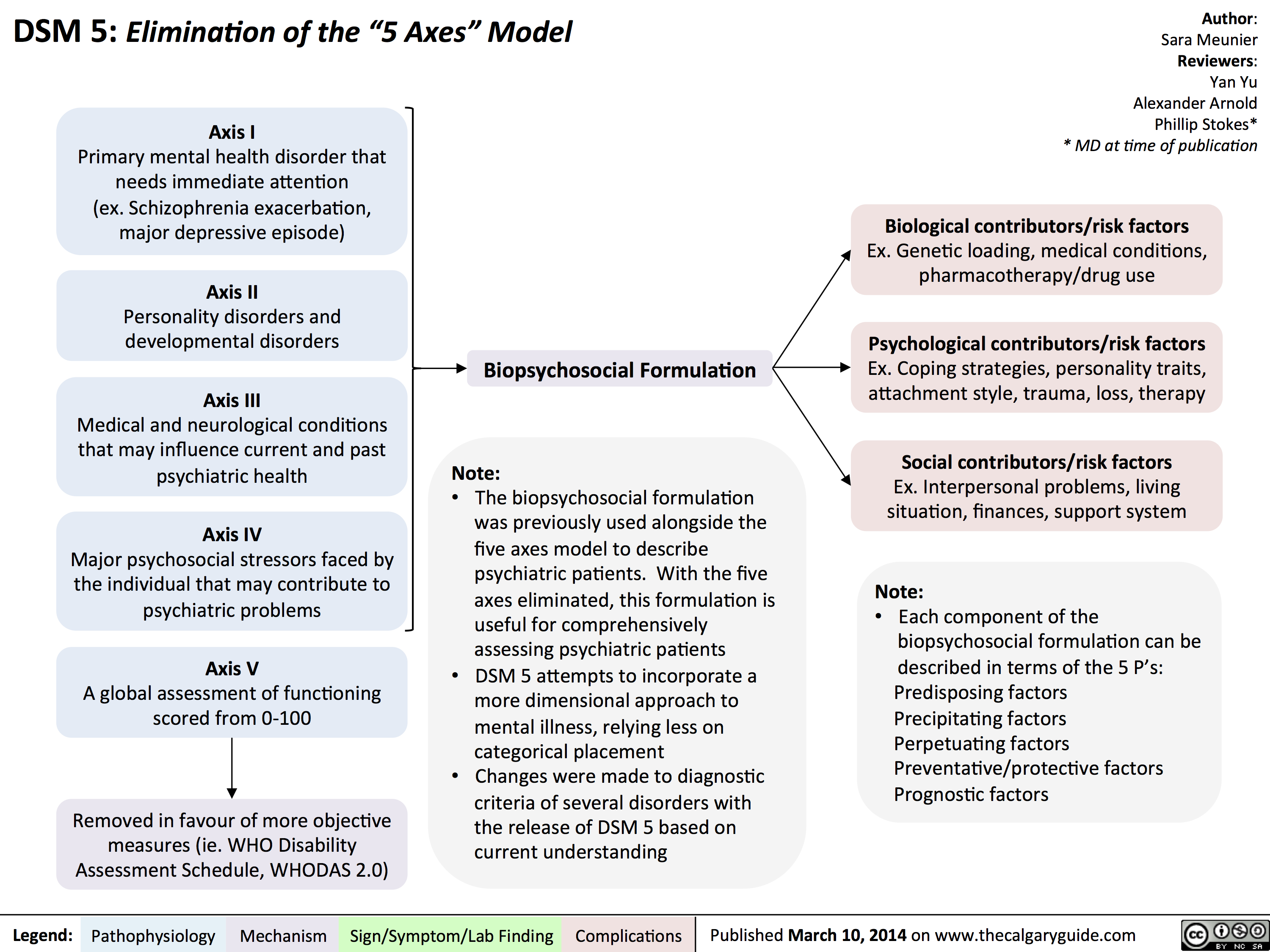
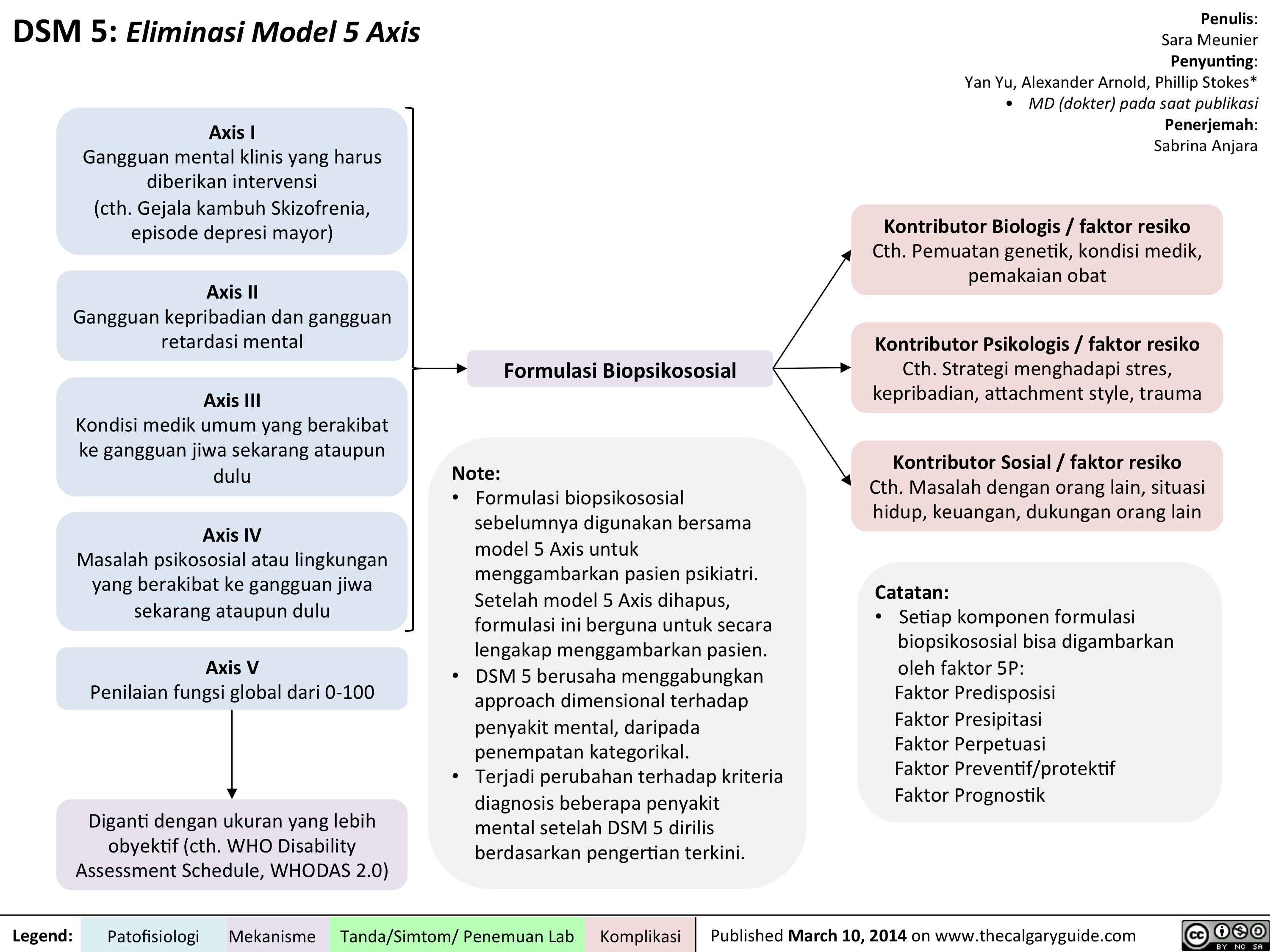
DSM - Axis to Formulation
Complications of Measles Pathogenesis and Clinical Findings
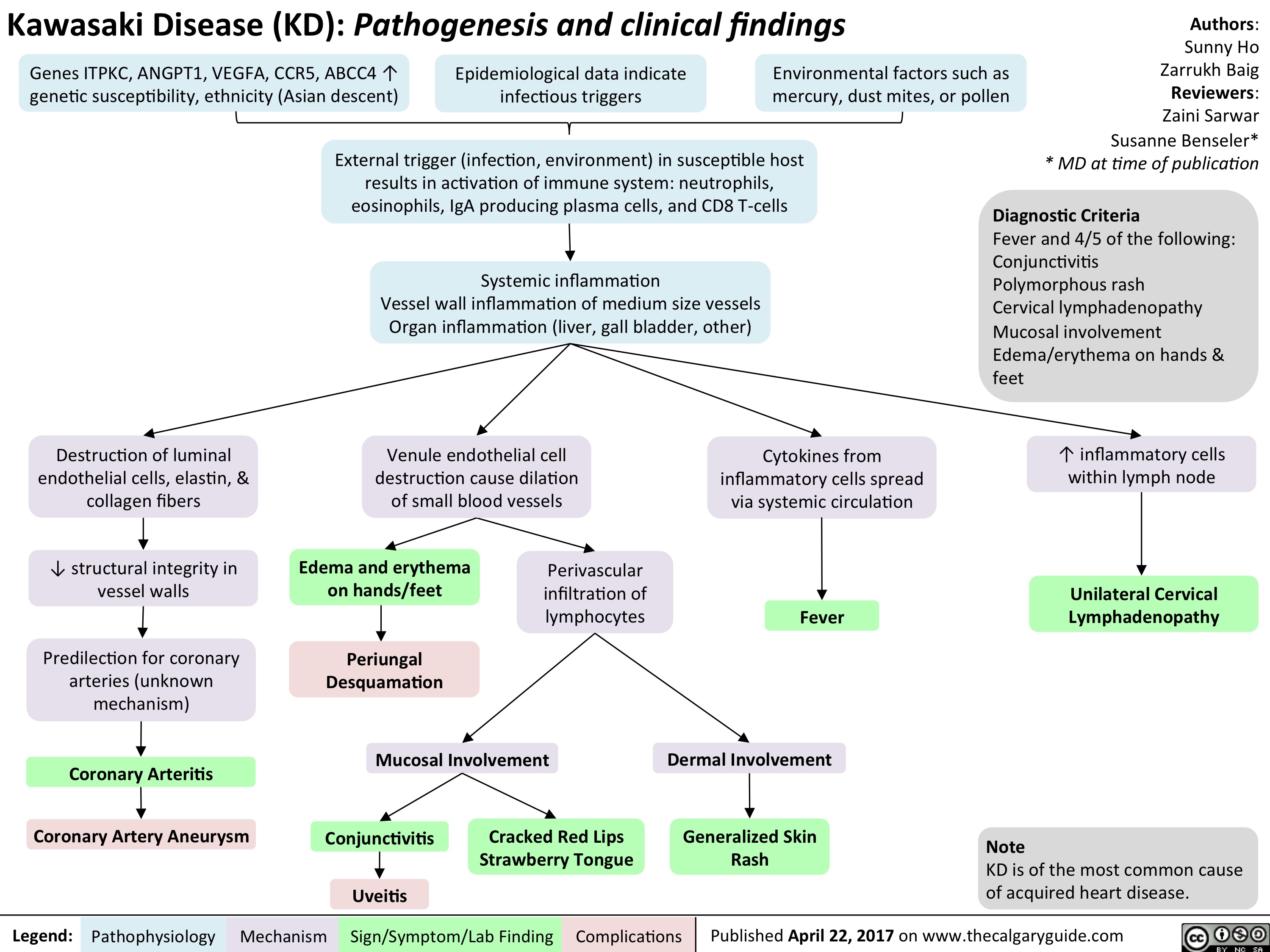
Kawasaki Disease

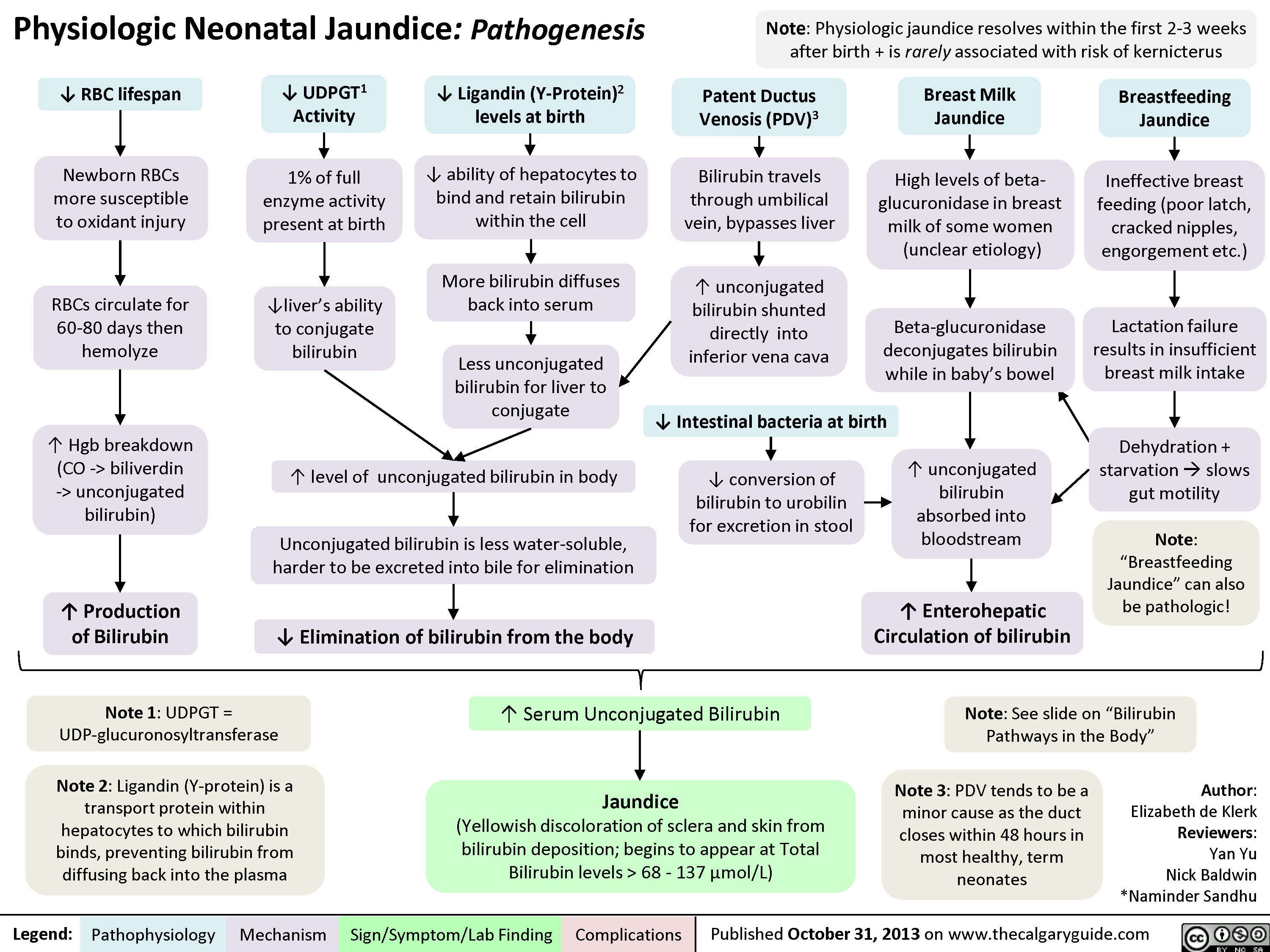
Physiologic Neonatal Jaundice
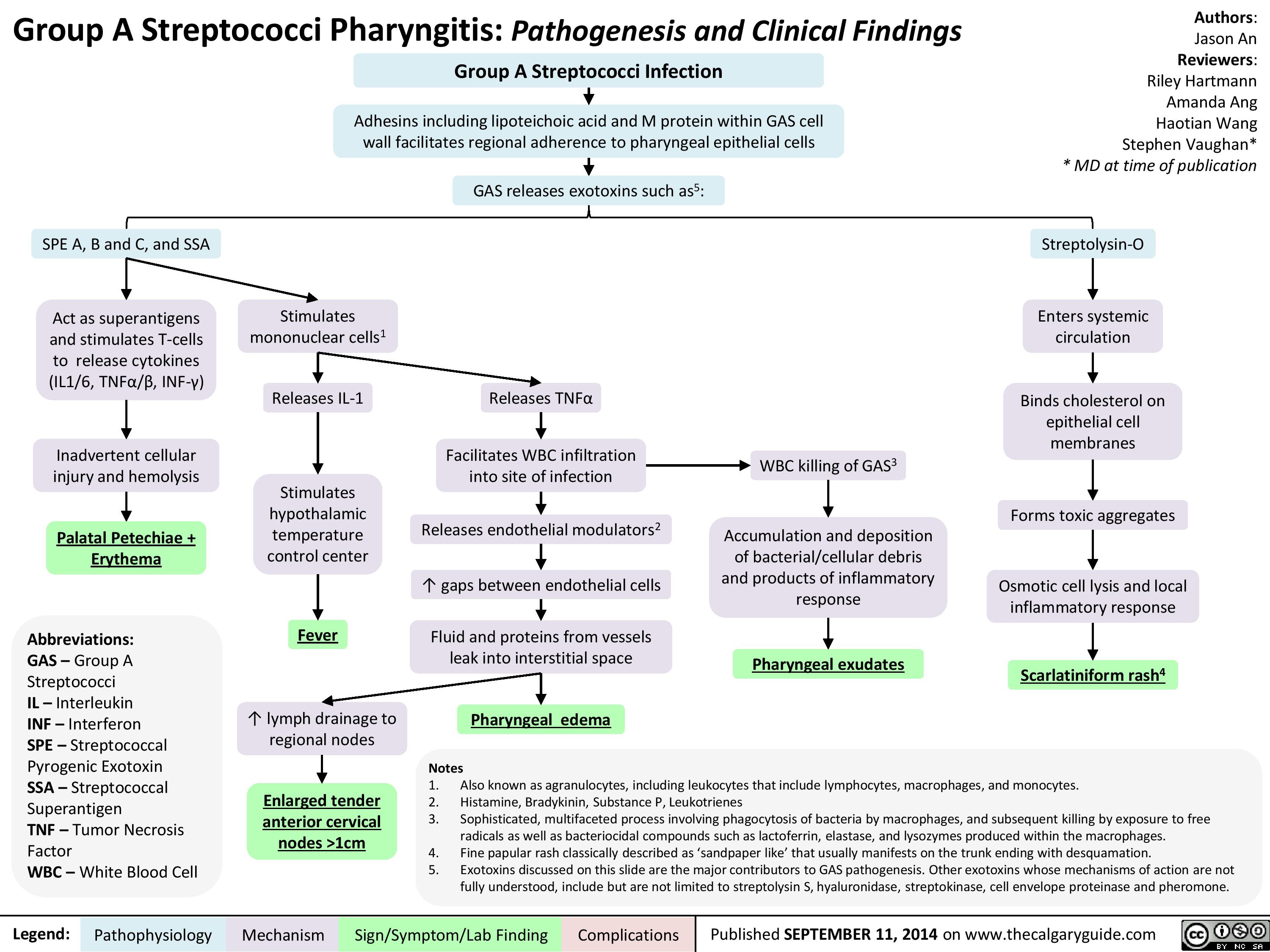
Group A Streptococci Pharyngitis Pathogenesis and Clinical Findings
AcuteOtitisComplications
Acute Otitis Media - Pathogenesis and Clinical Findings (in Children)
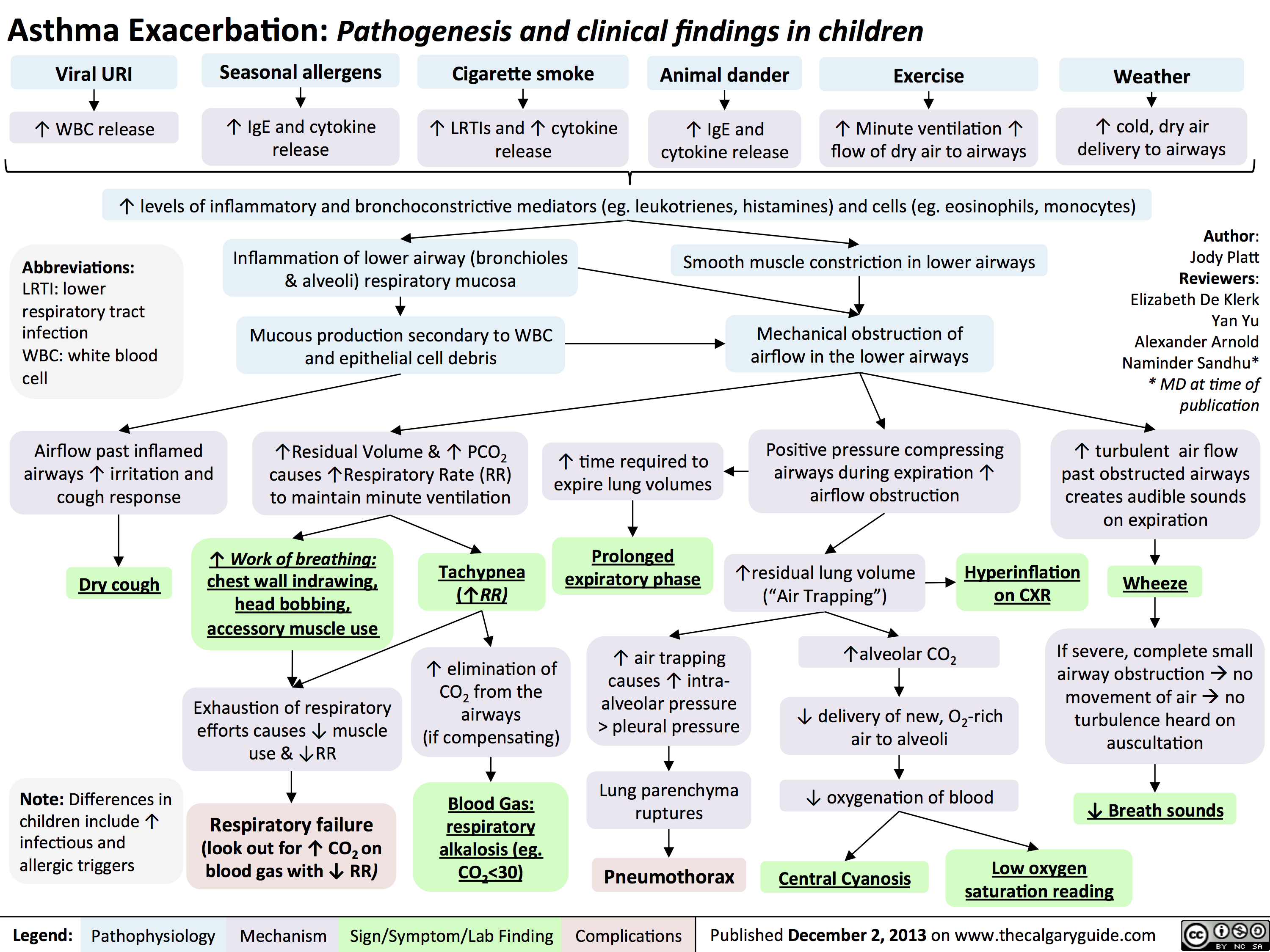
Asthma Exacerbation - Pathogenesis and Clinical Findings in Children
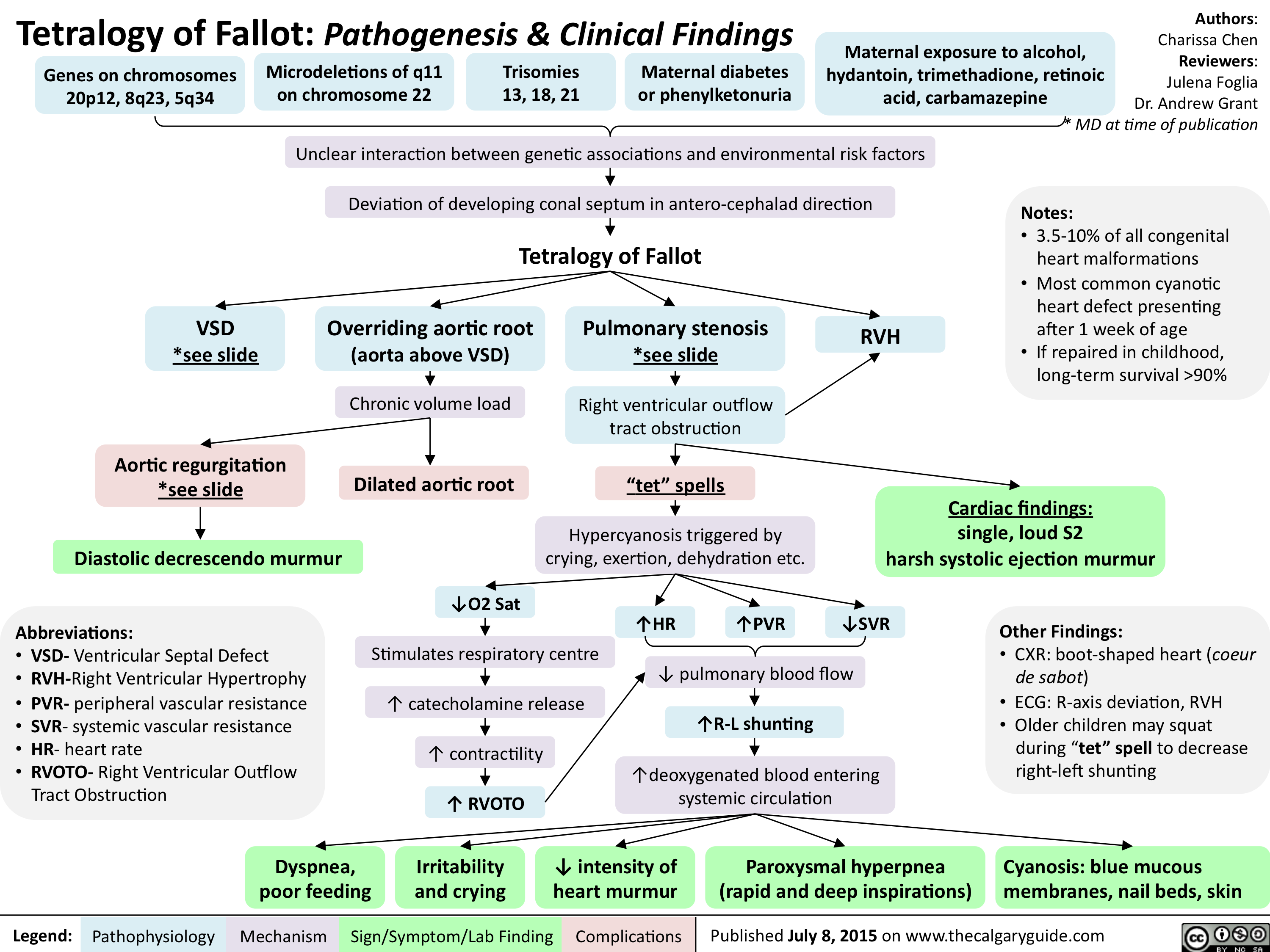
Tetralogy of Fallot-Pathogenesis & Clinical Findings
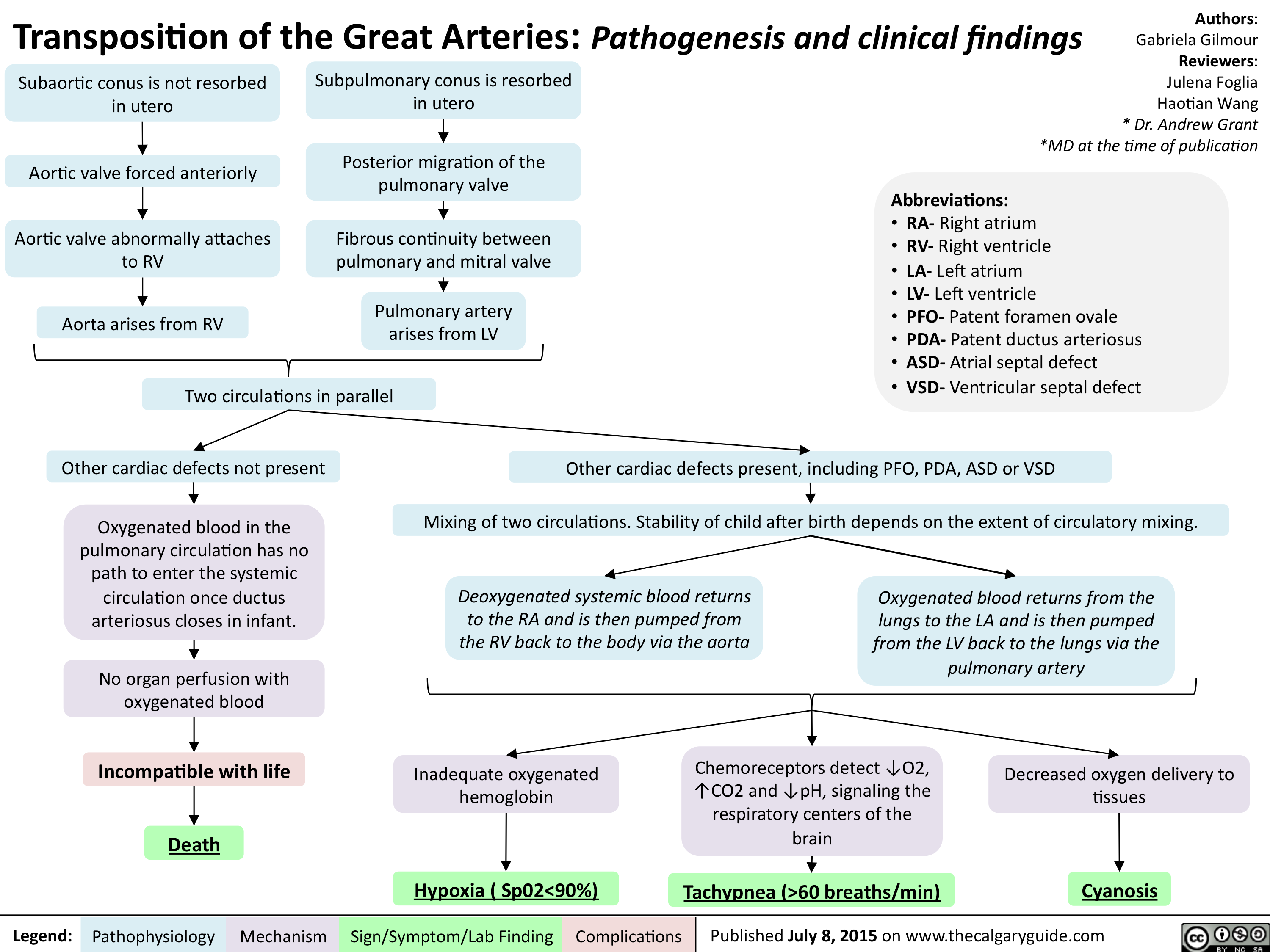
Transposition of the Great Arteries-Pathogenesis & clinical findings
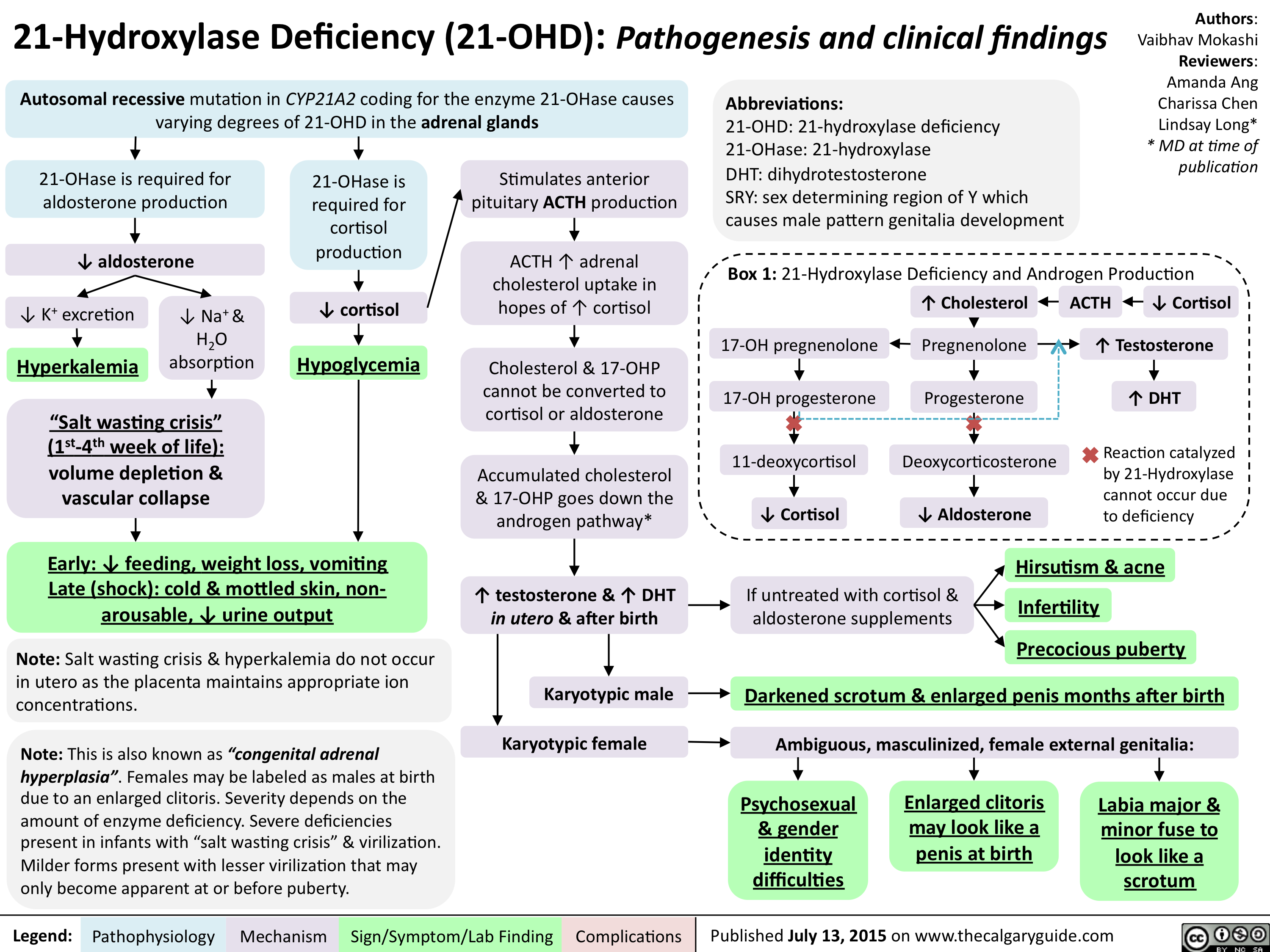
21-Hydroxylase Deficiency-Pathogenesis and clinical findings
Hallux Valgus pathogenesis and clinical findings - August 15 2015

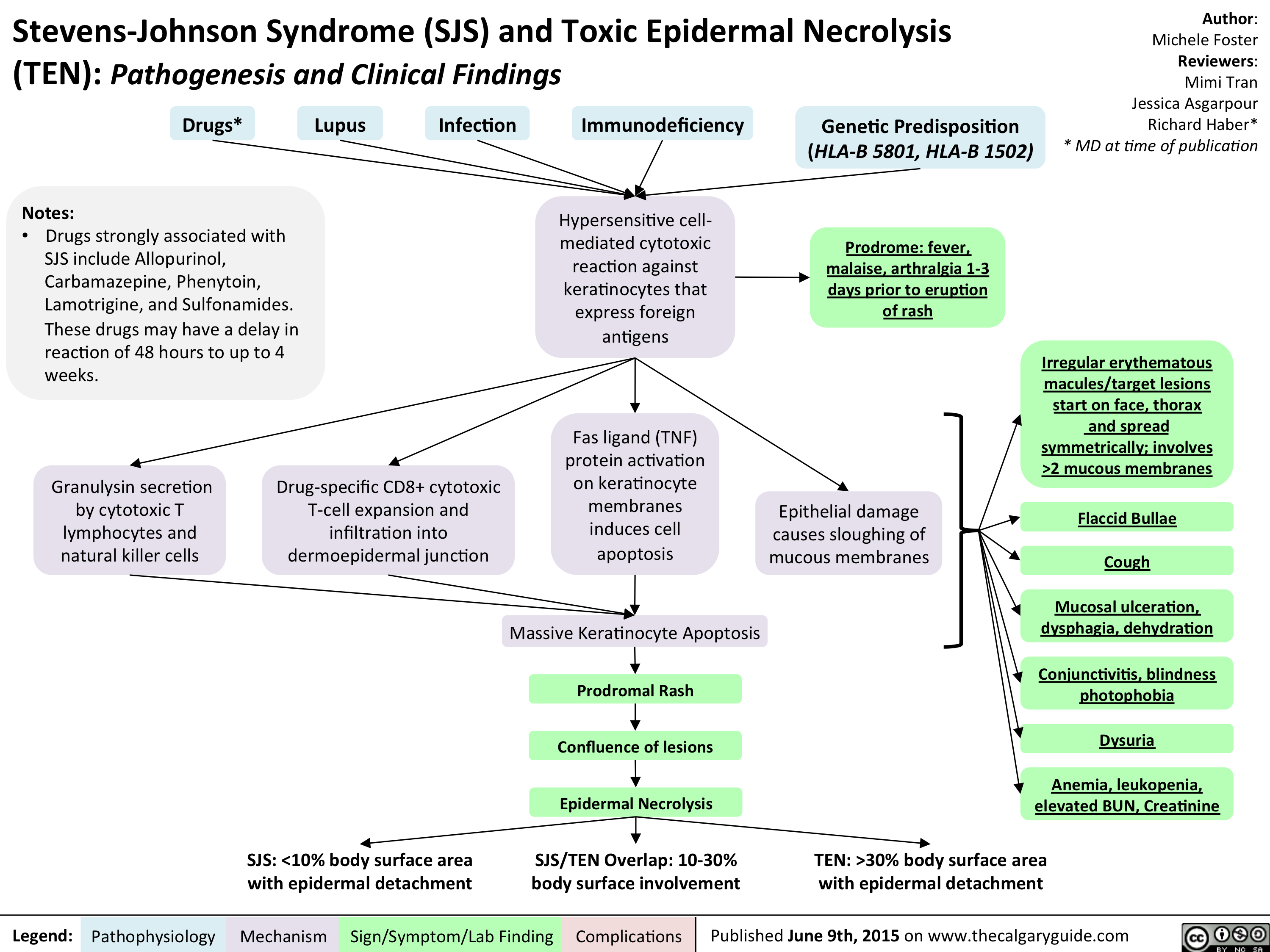
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) - Pathogenesis and Clinical Findings
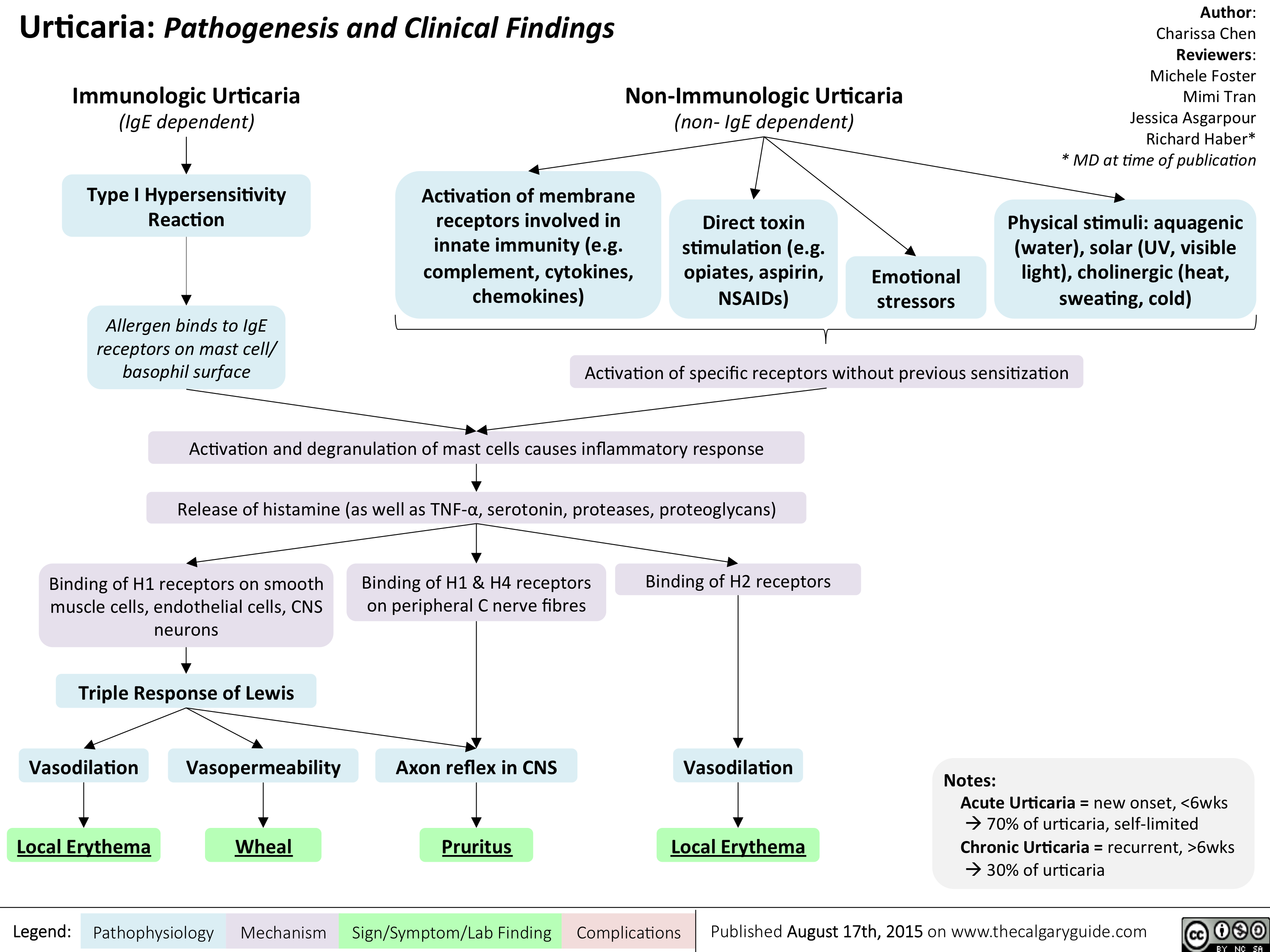
Urticaria- Pathogenesis and Clinical Findings
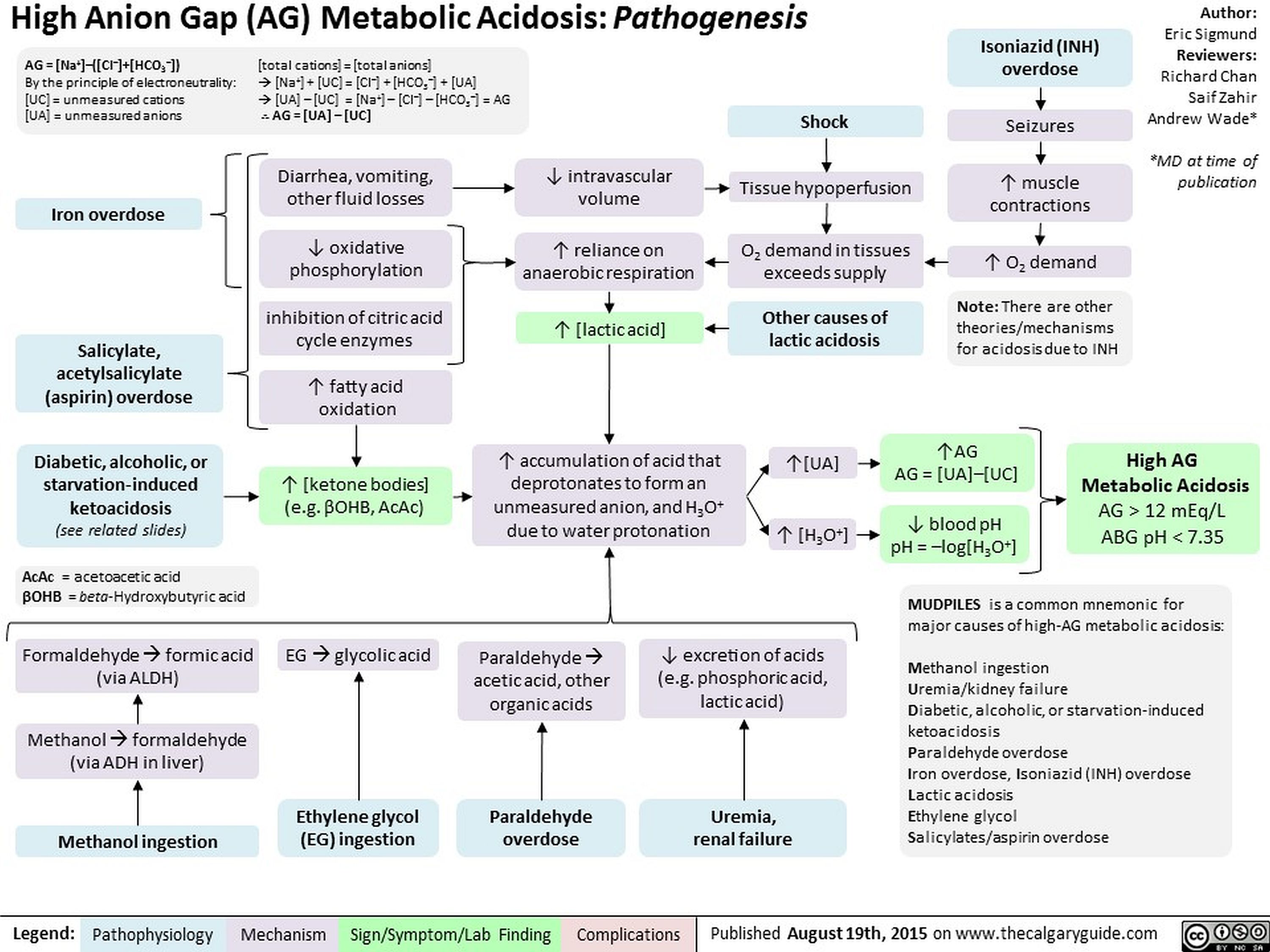
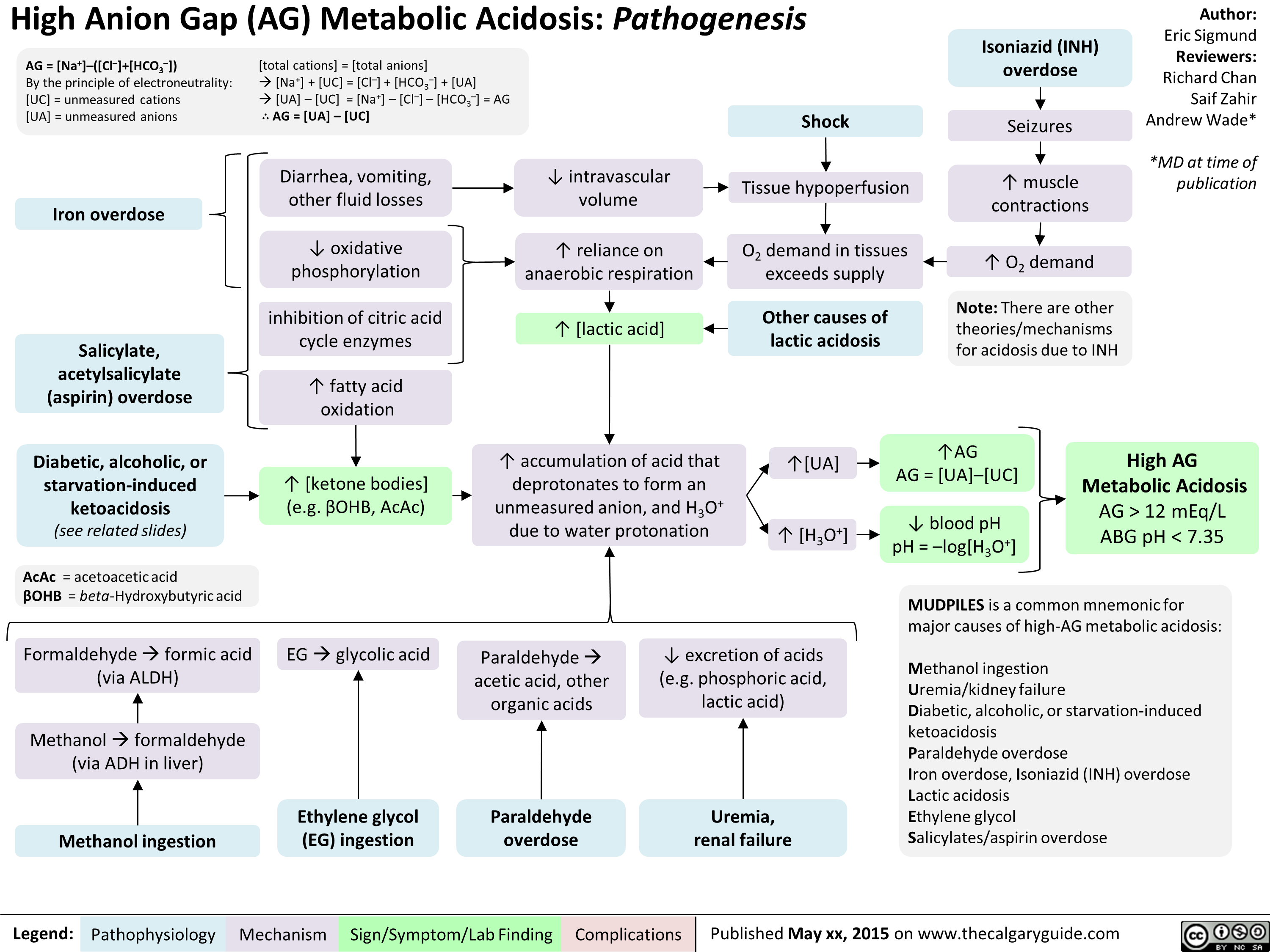
High Anion Gap Metabolic Acidosis Pathogenesis
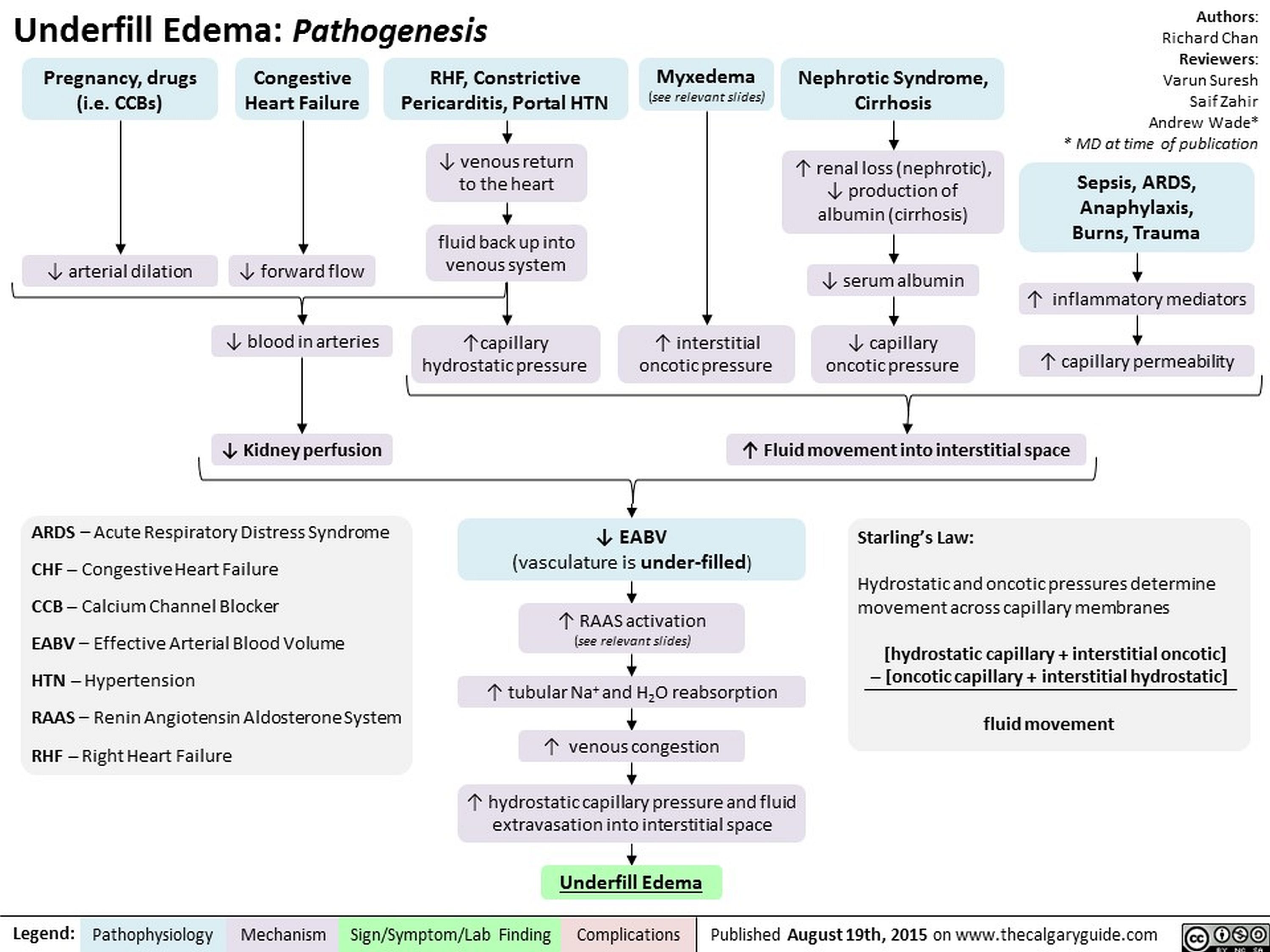
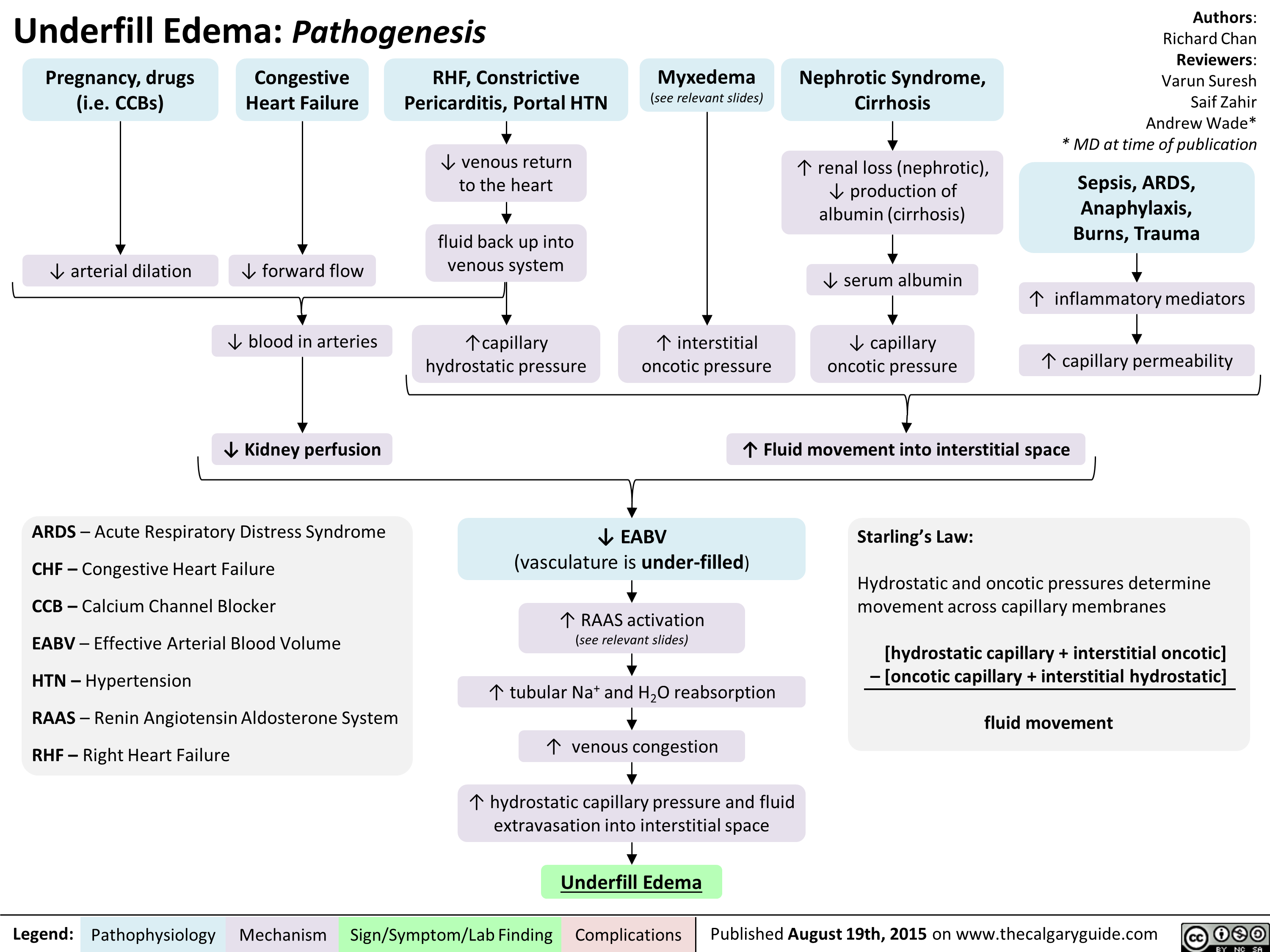
Underfill Edema Pathogenesis
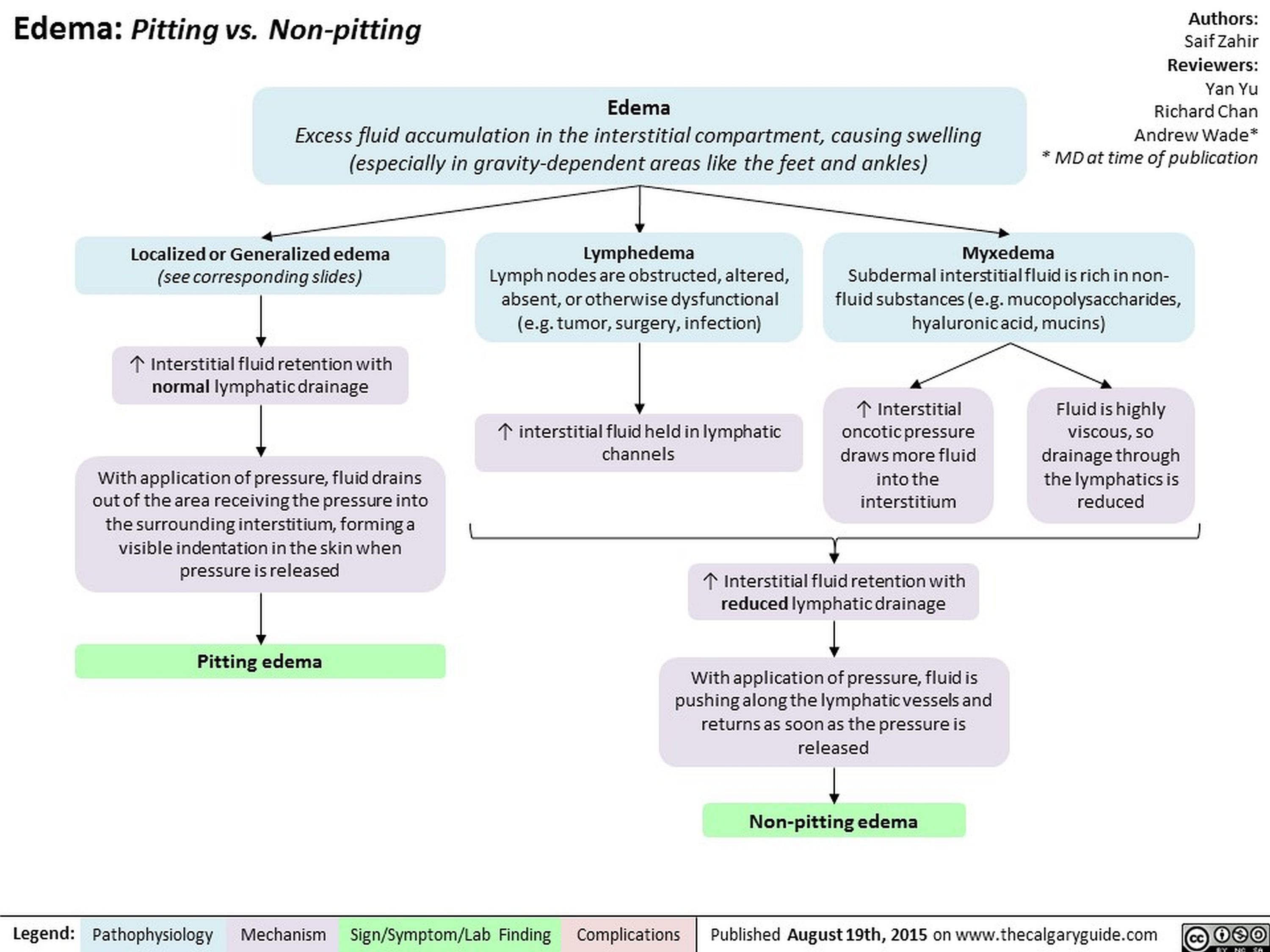
Edema Pitting vs Non-pitting
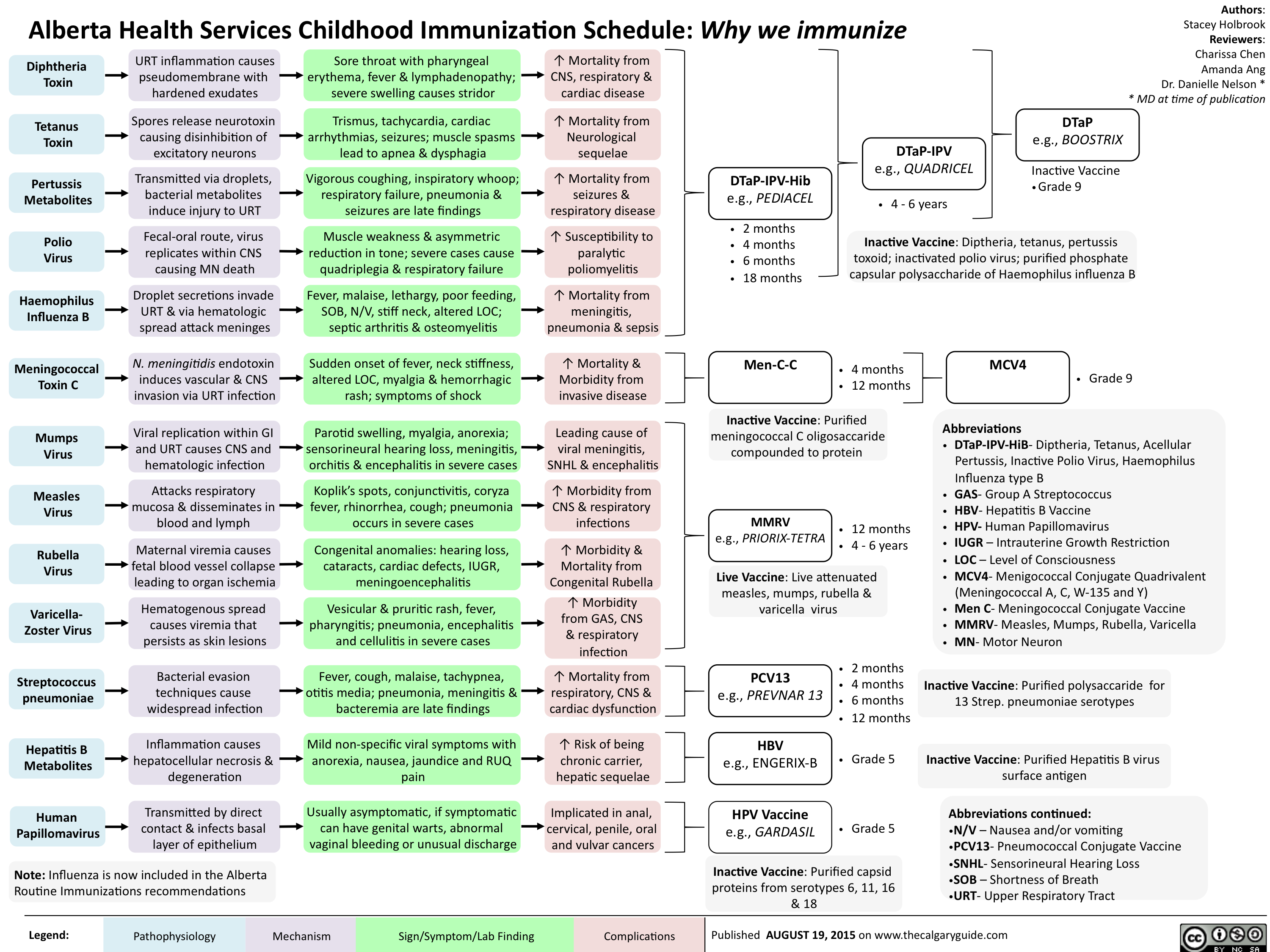
Childhood Immunization Schedule-Why we immunize
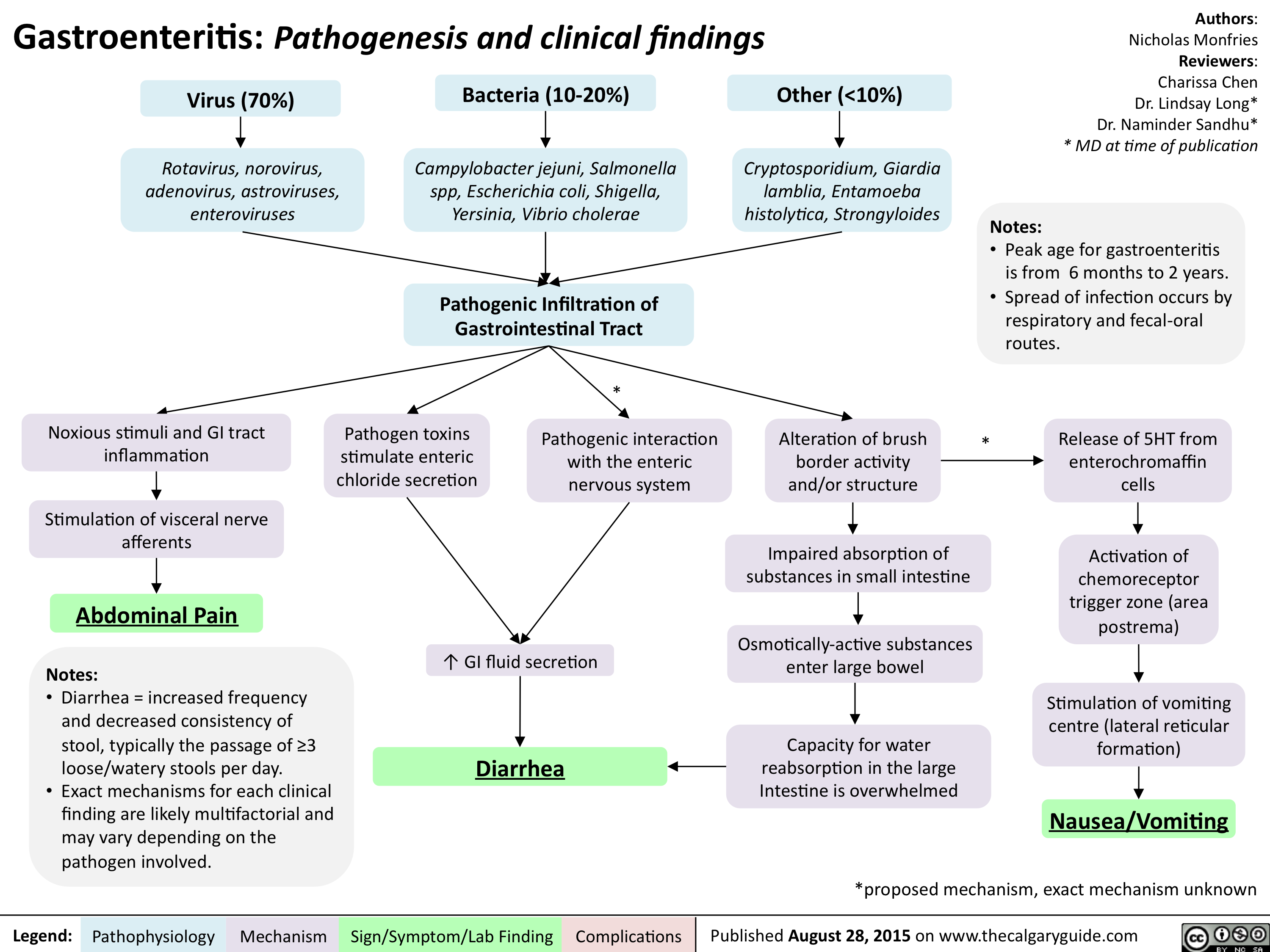
Gastroenteritis-Pathogenesis and clinical findings
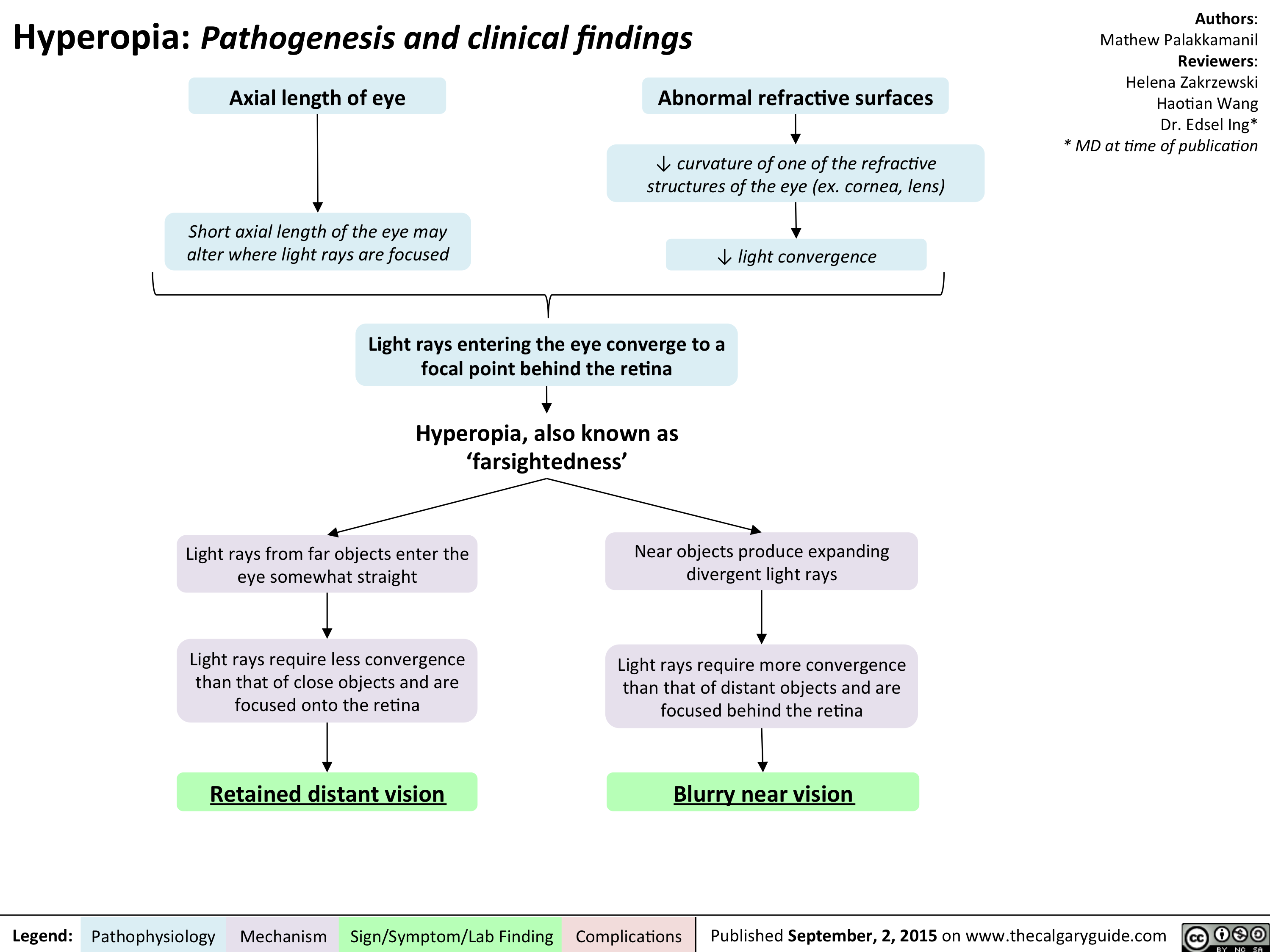
Hyperopia - Pathogenesis and Clinical Findings
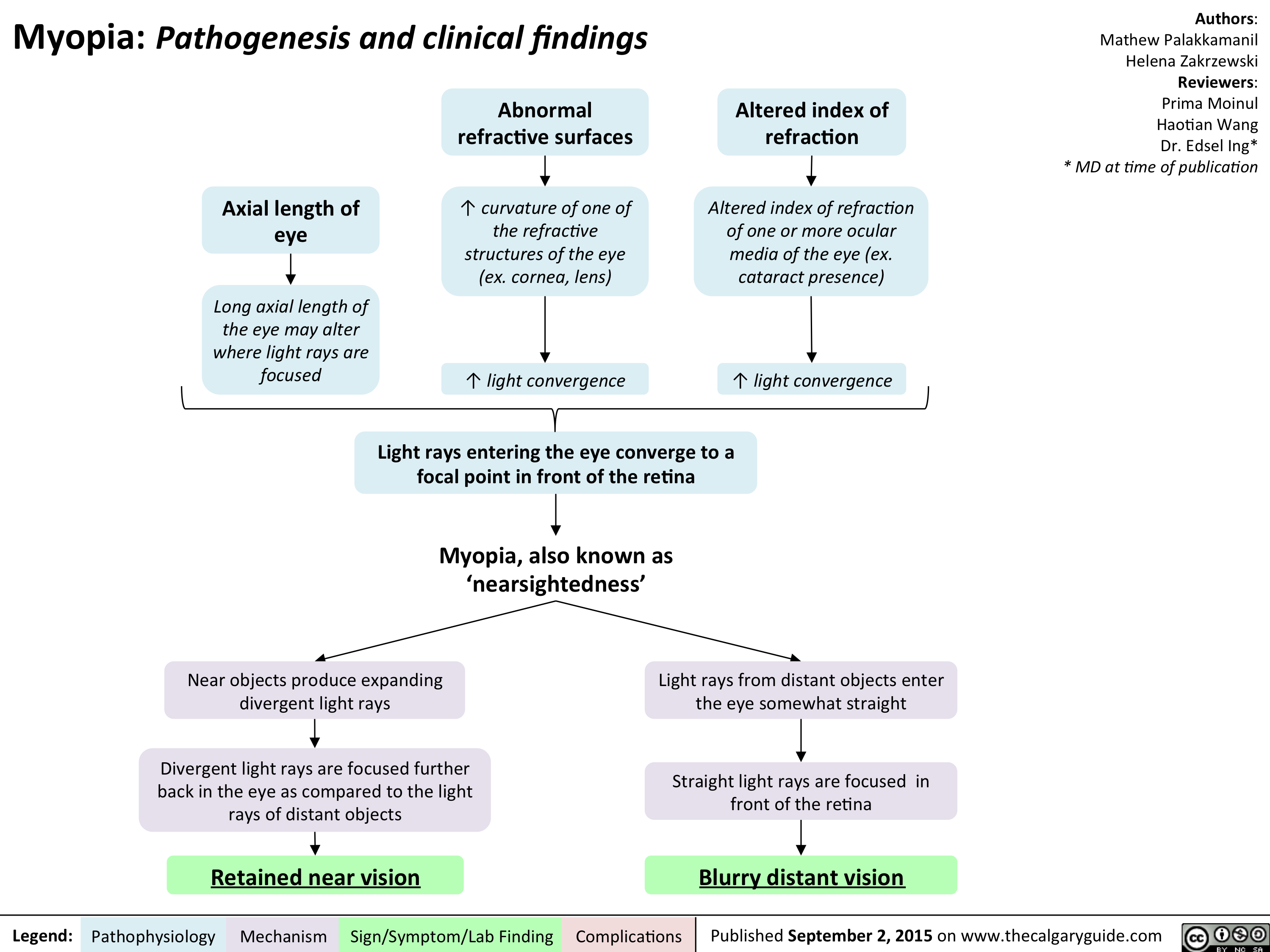
Myopia - Pathogenesis and clinical findings
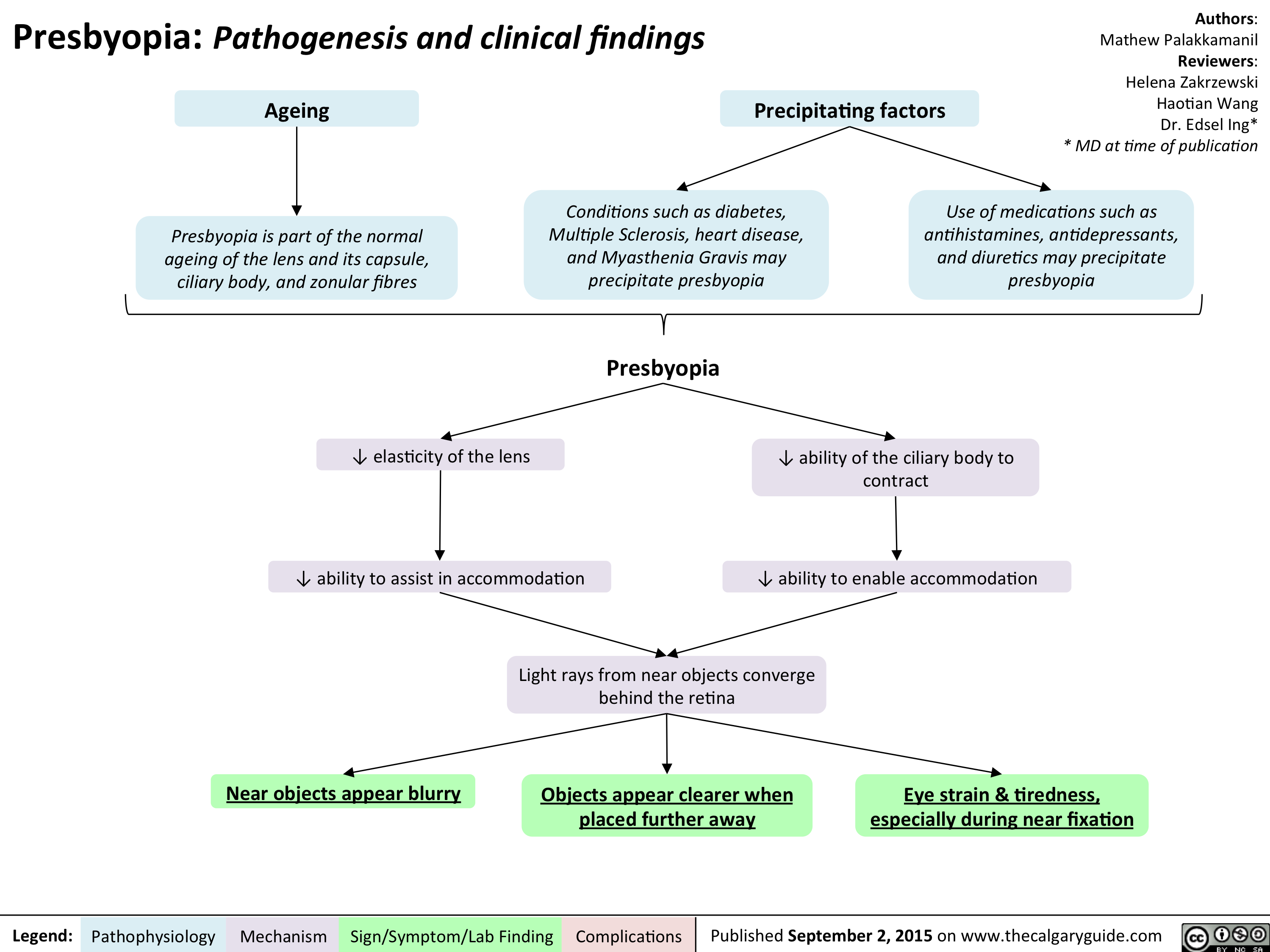
Presbyopia - Pathogenesis and clinical findings
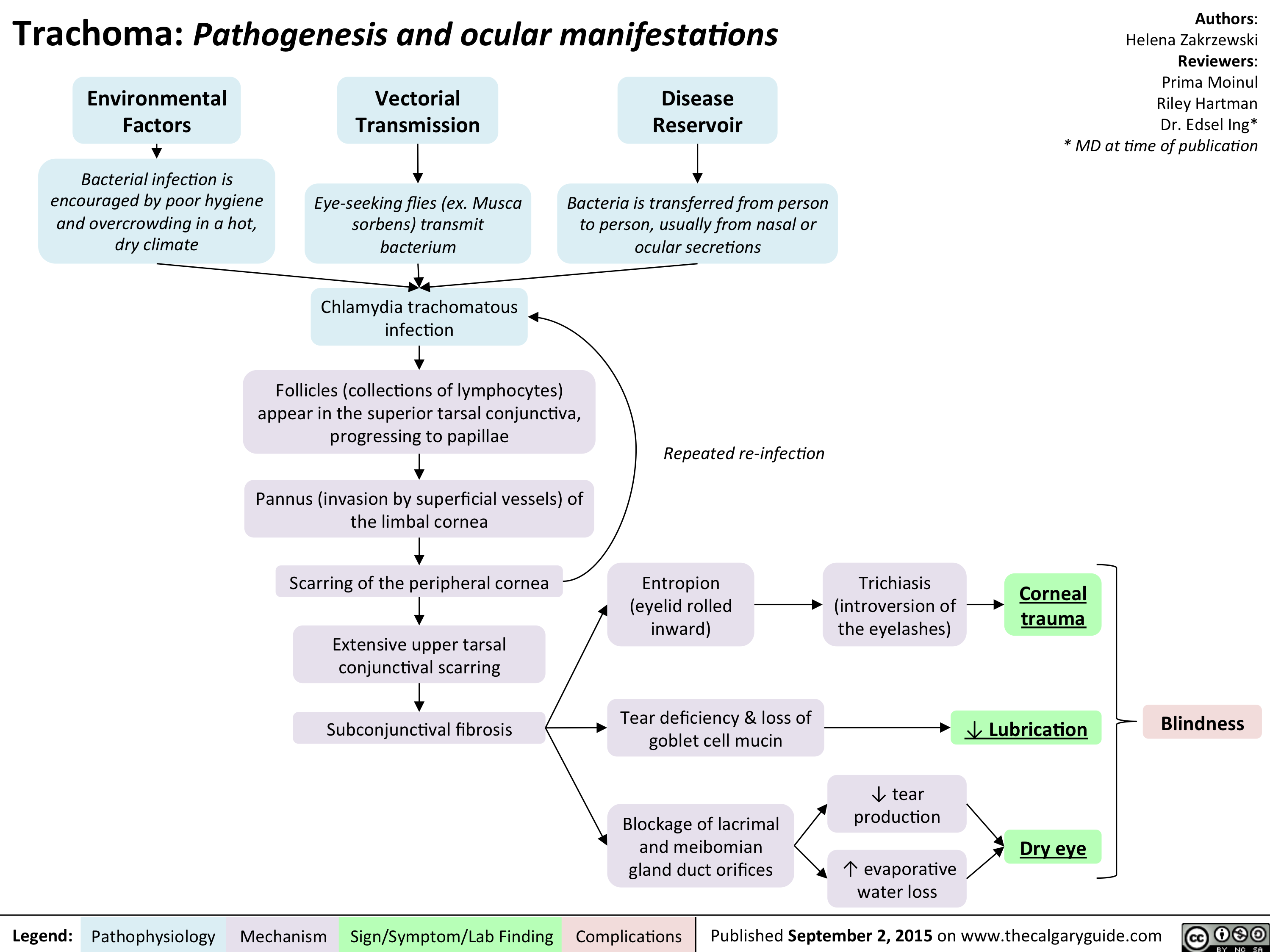
Trachoma - Pathogenesis and clinical findings
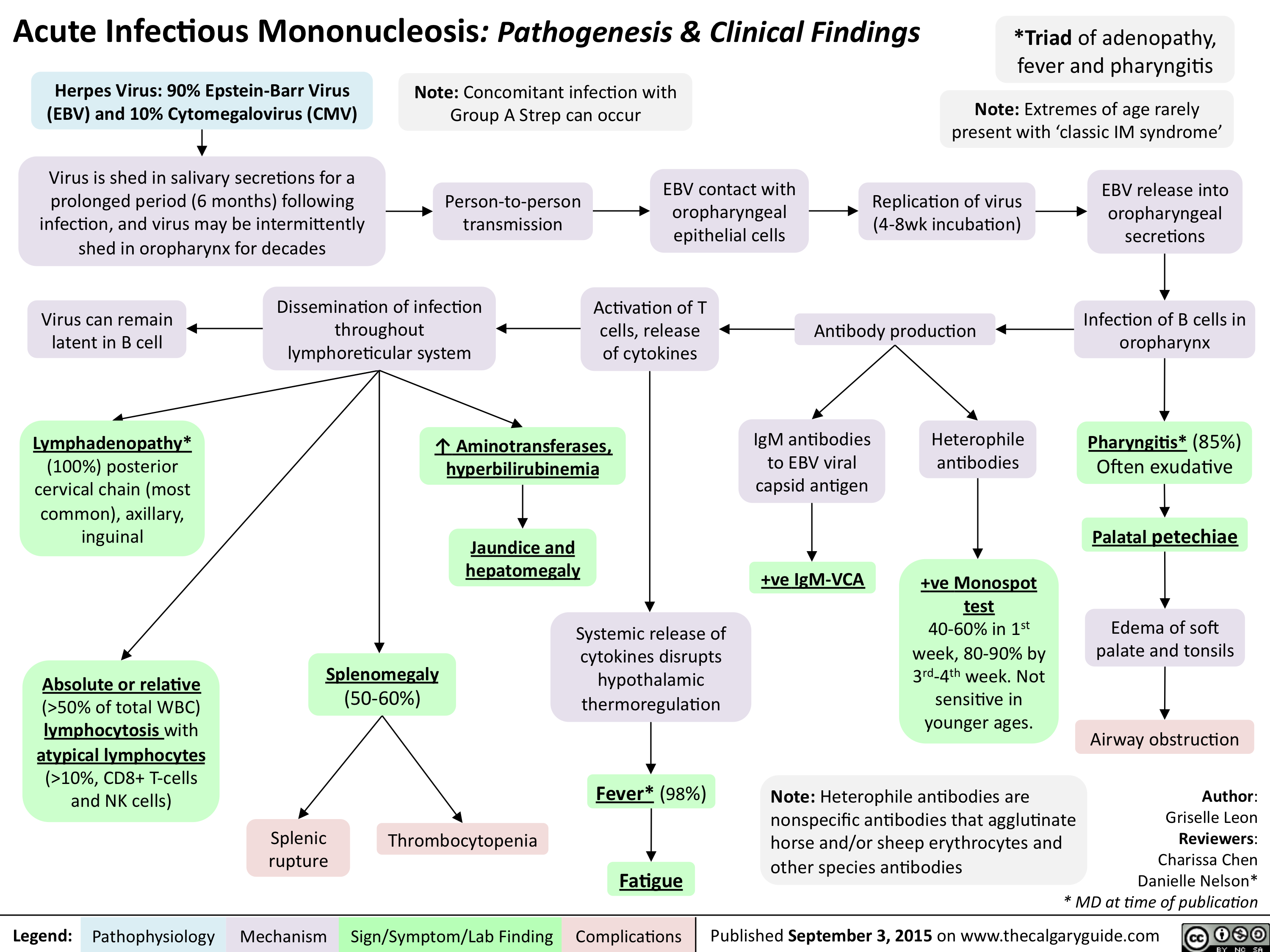
Acute Infectious Mononucleosis-Pathogenesis and clinical findings
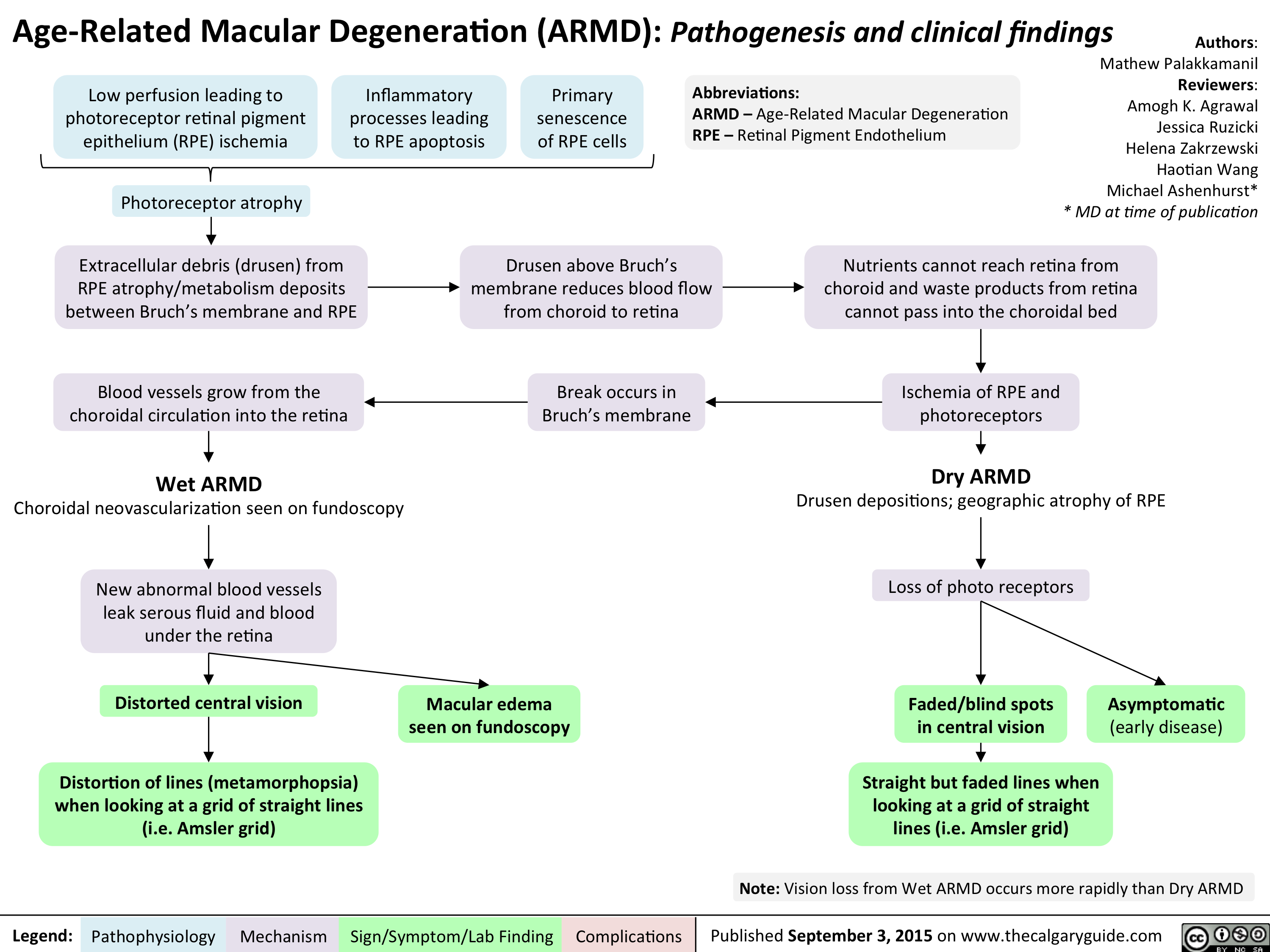
Age Related Macular Degeneration - Pathogenesis and clinical findings
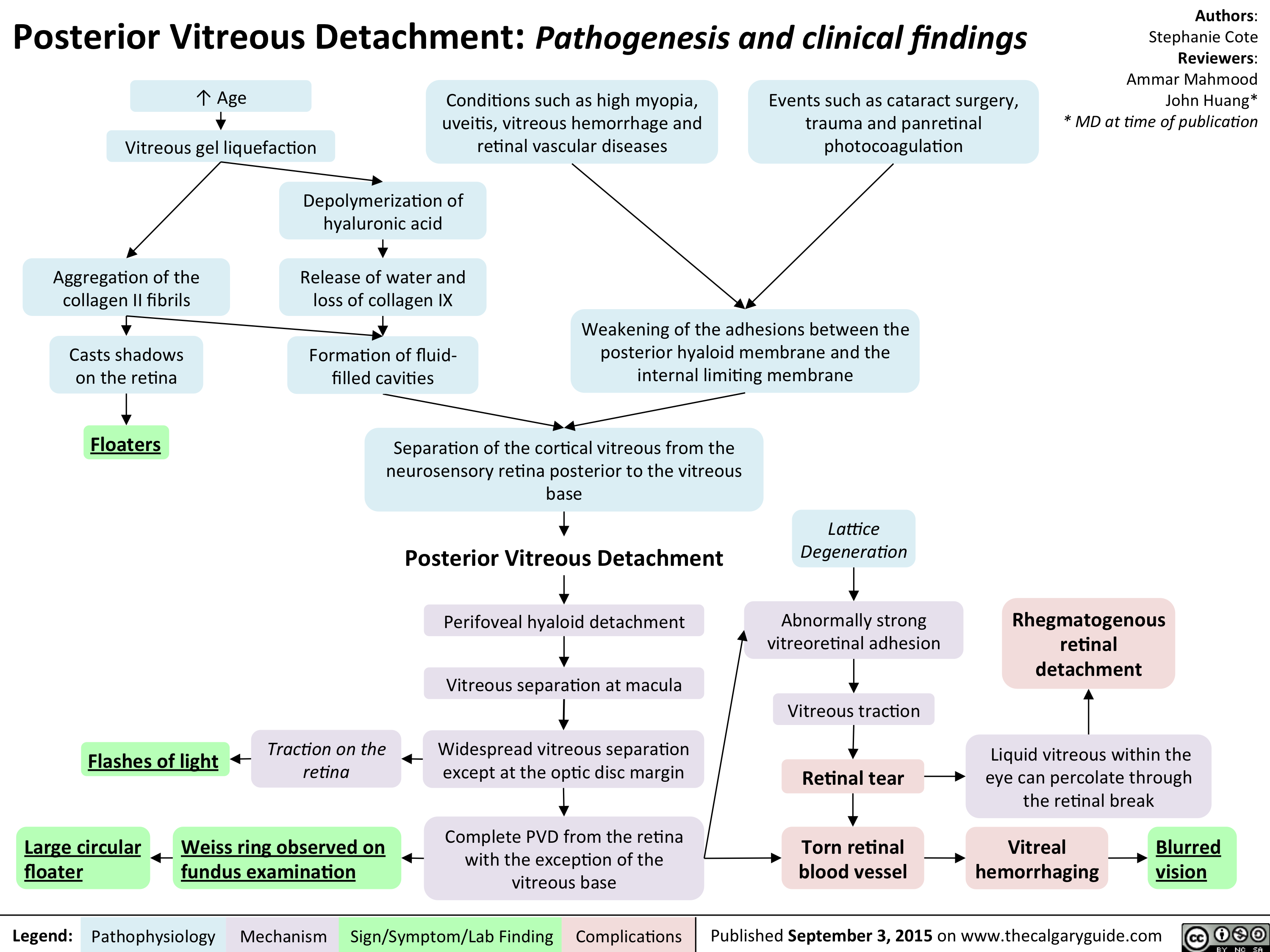
Posterior Vitreous Detachment - Pathogenesis and clinical findings
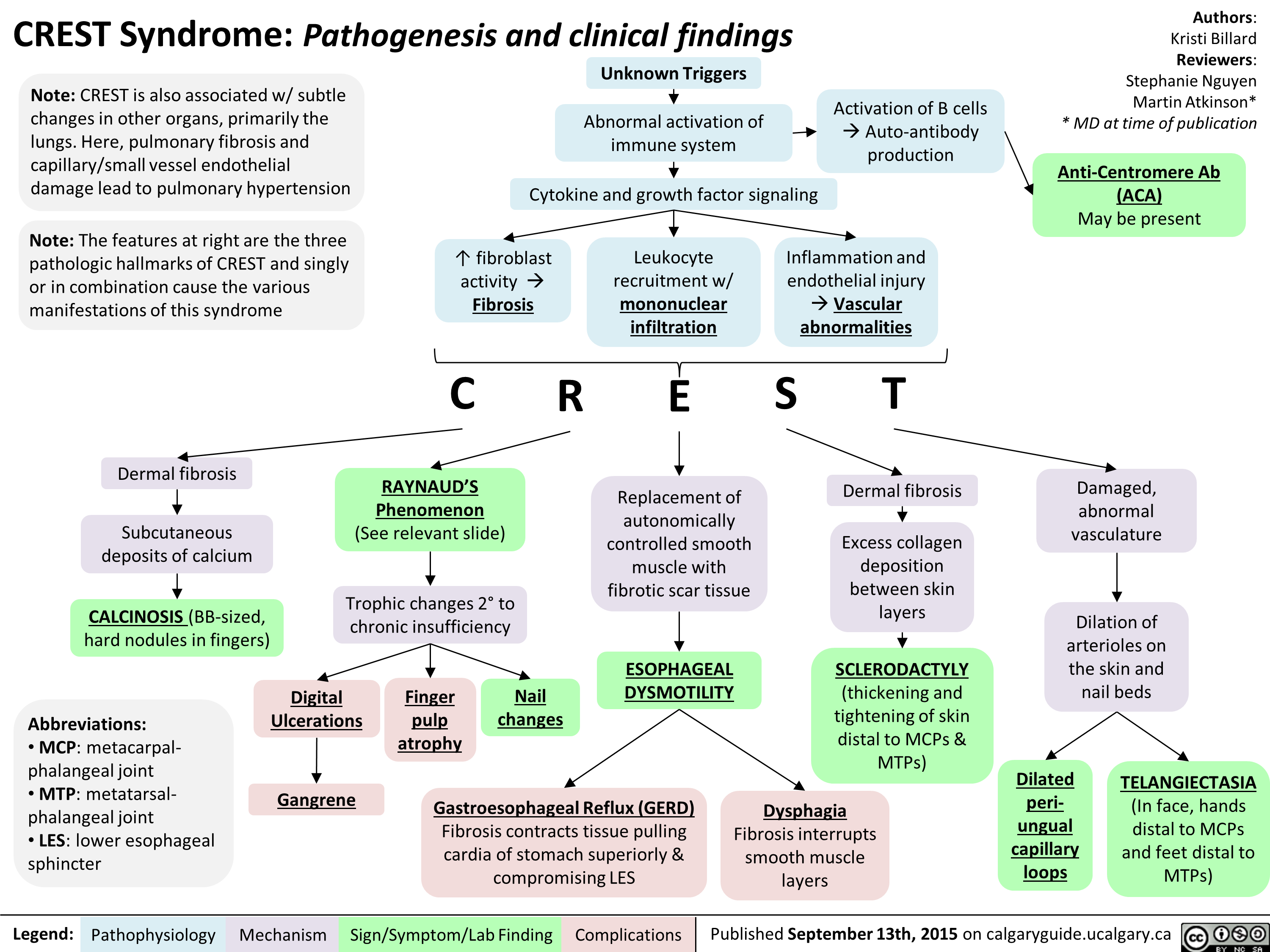
FINAL - CREST Syndrome Pathogenesis and clinical findings
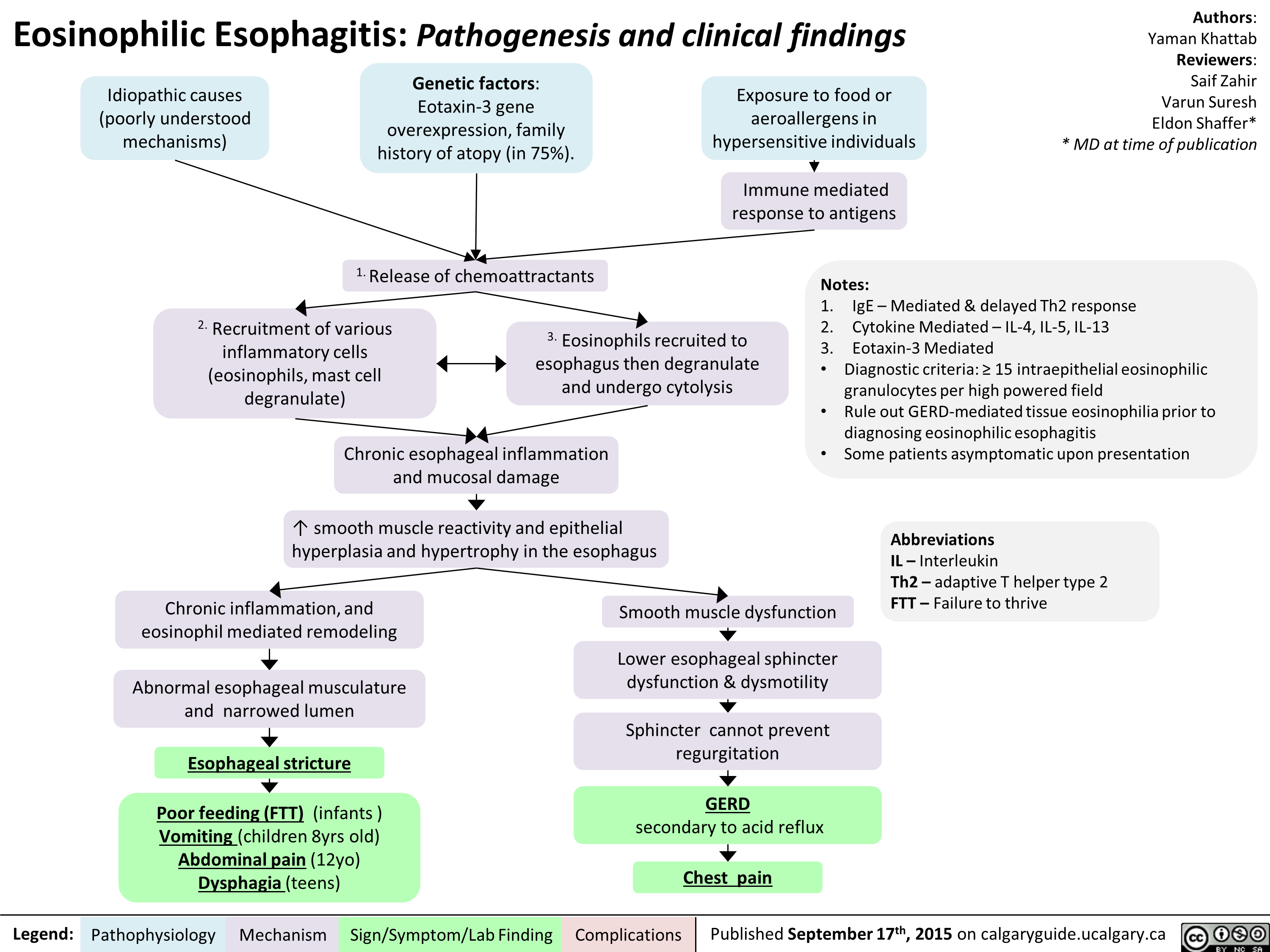
Eosinophillic Esophagitis -Kattab Yaman - Final For Publication
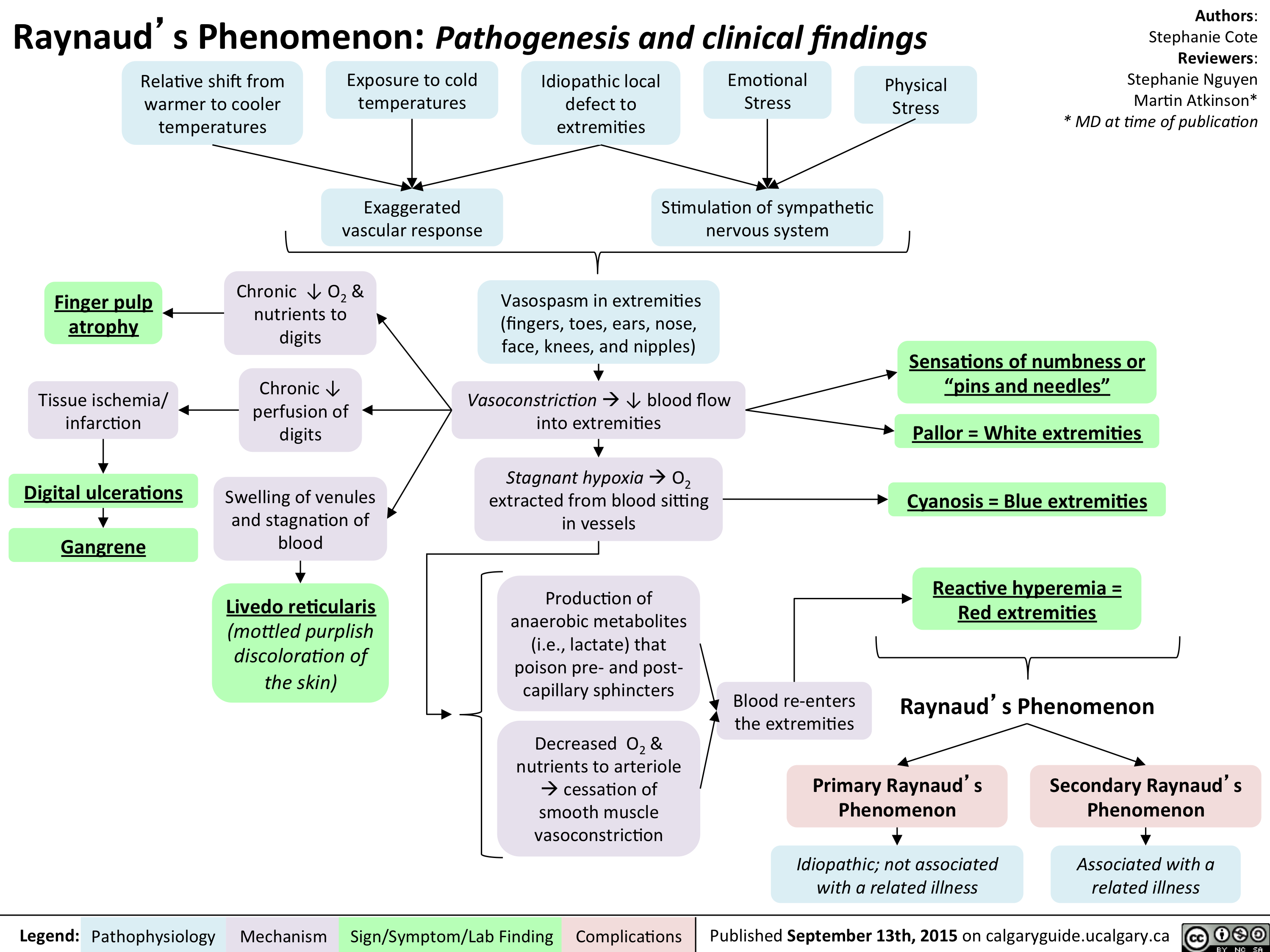
Raynaud Phenomenon Pathogenesis and Clinical Findings
Chan Richard - Underfill Edema - Final 210915
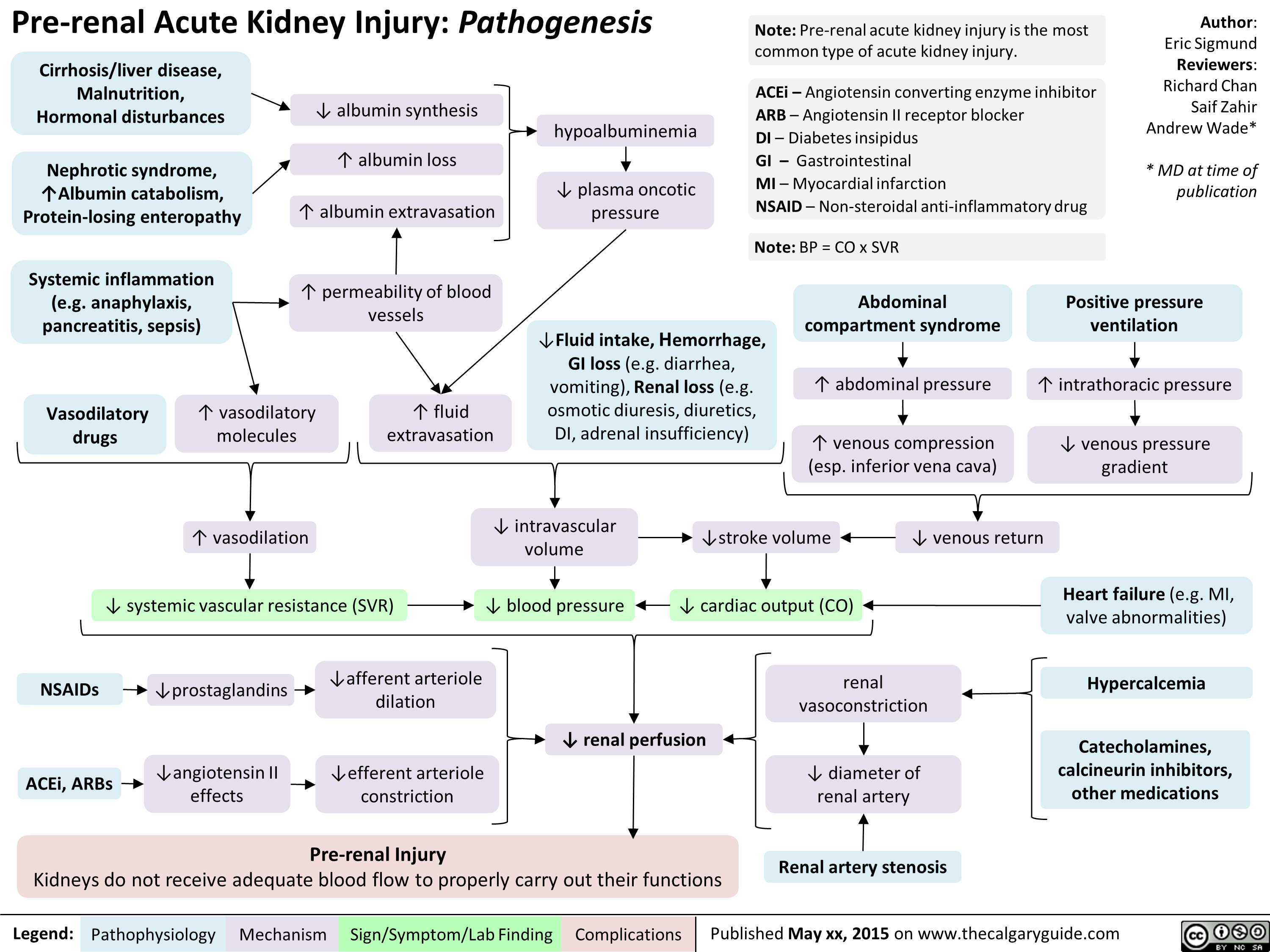
Pre-Renal Acute Kidney Injury Pathogenesis
High-AG Metabolic Acidosis Pathogenesis
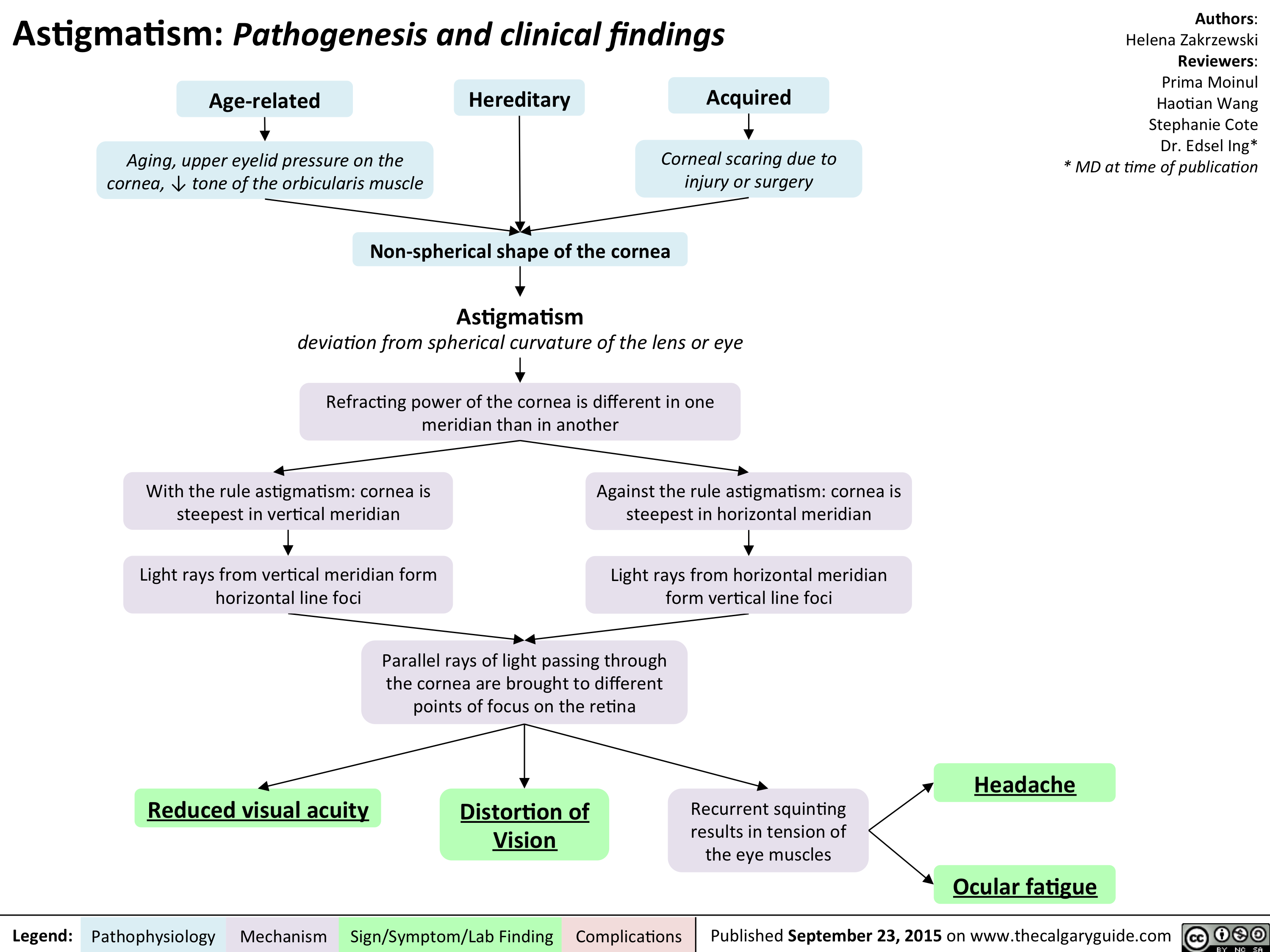
Astigmatism Pathogenesis and Clinical Findings
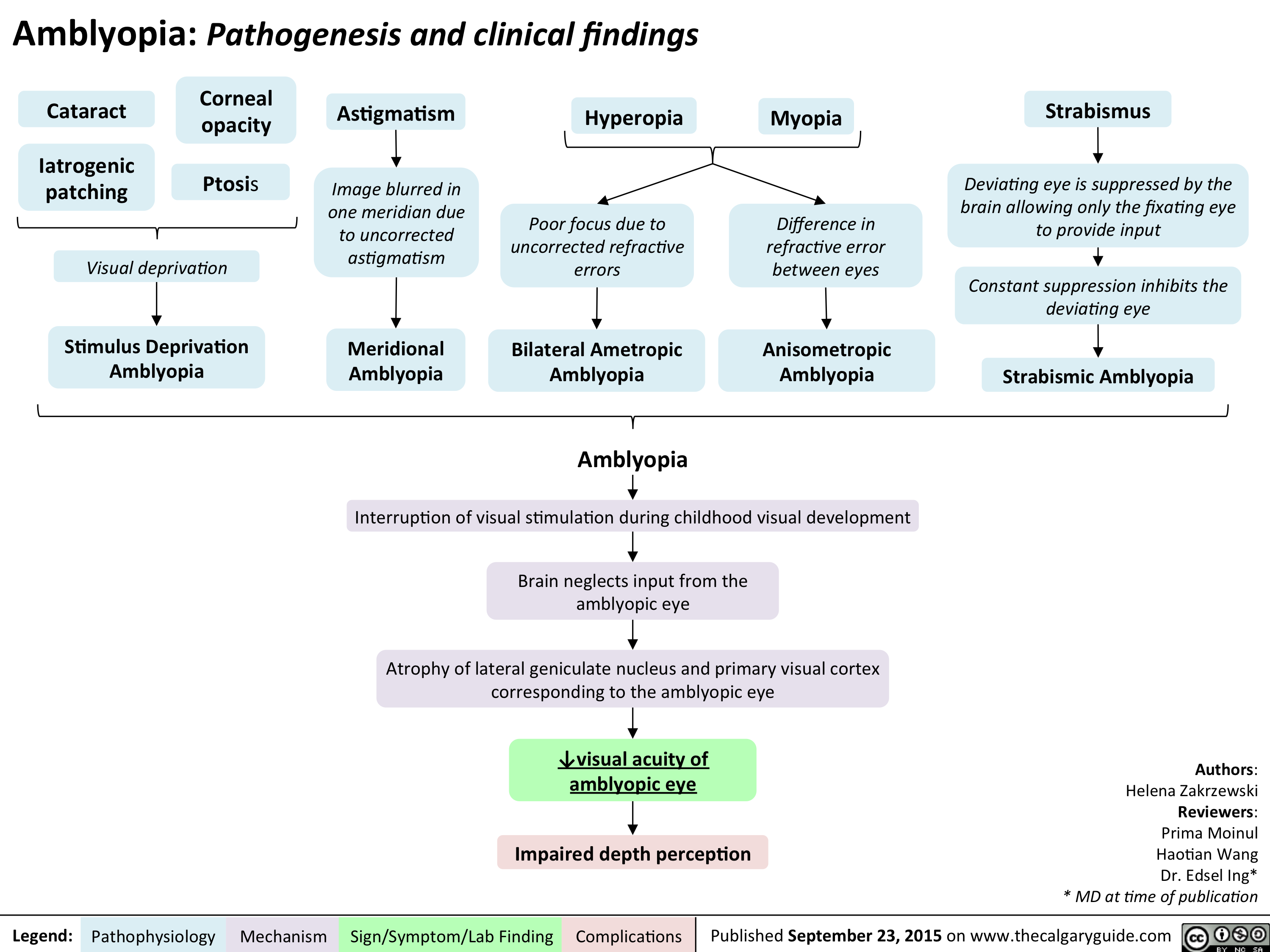
Amblyopia Pathogenesis and clinical findings
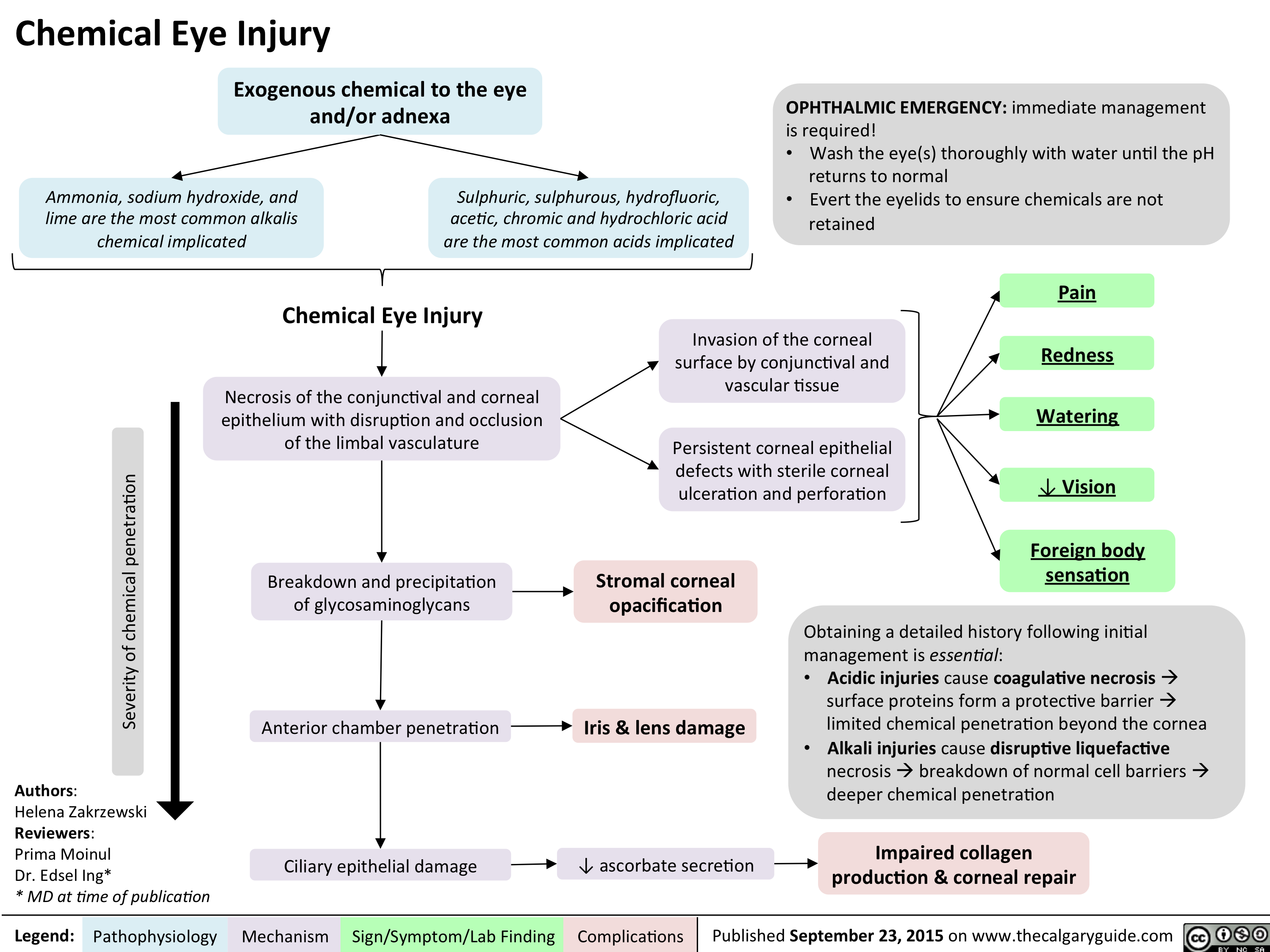
Chemical Eye Injury Pathogenesis and clinical findings
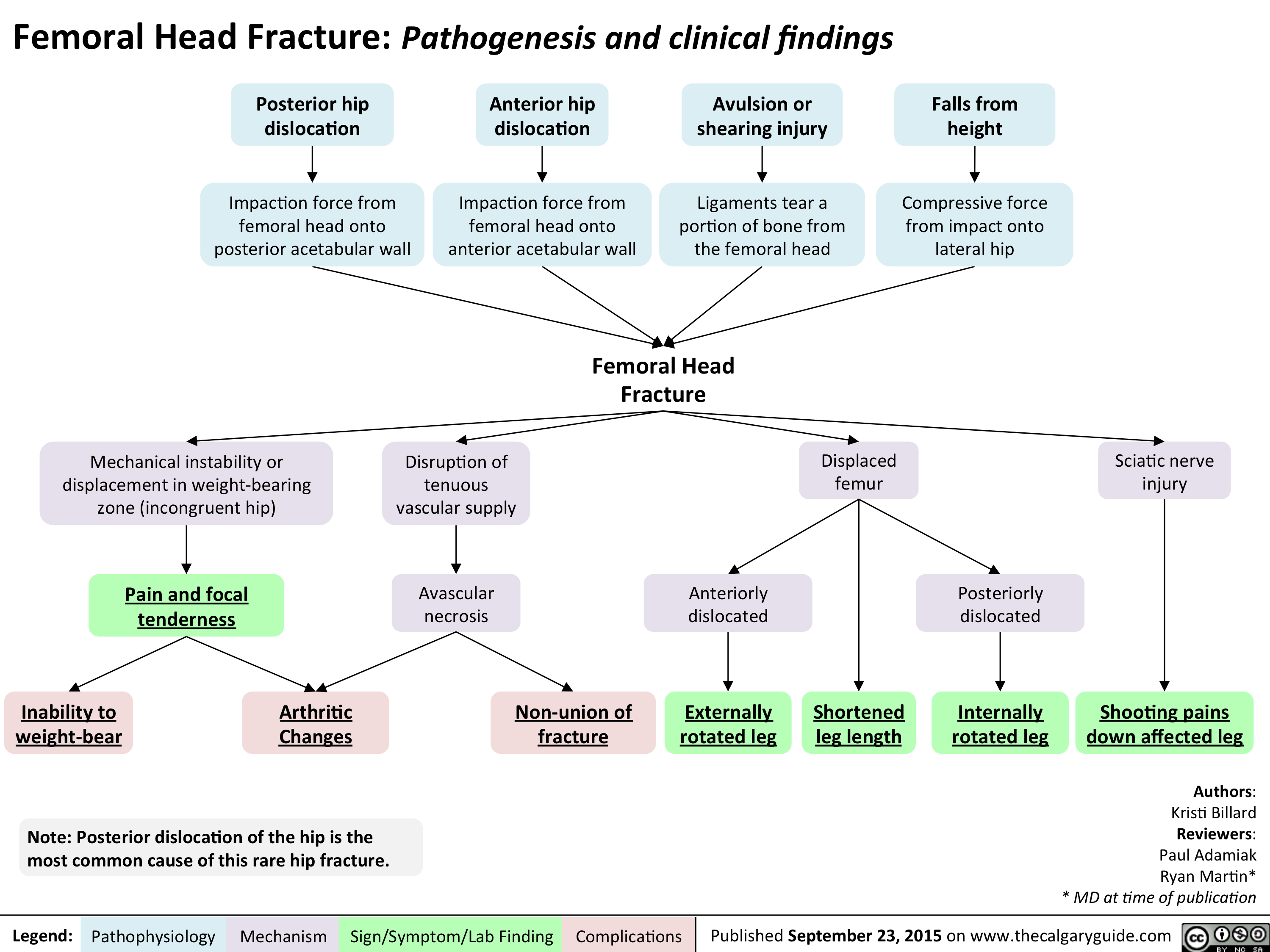
Femoral Head Fracture Pathogenesis and clinical findings
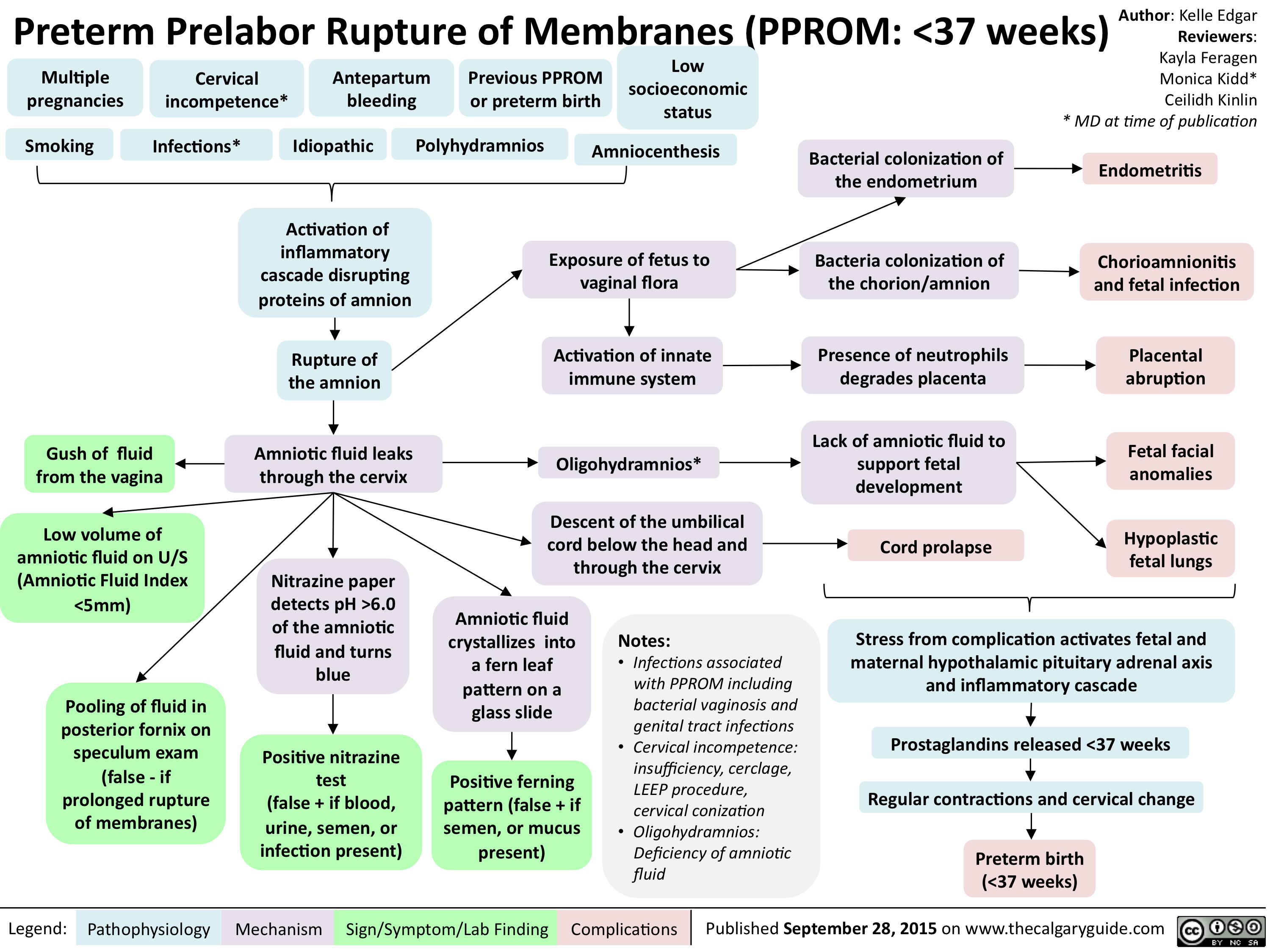
PPROM - Pathogenesis and clinical findings
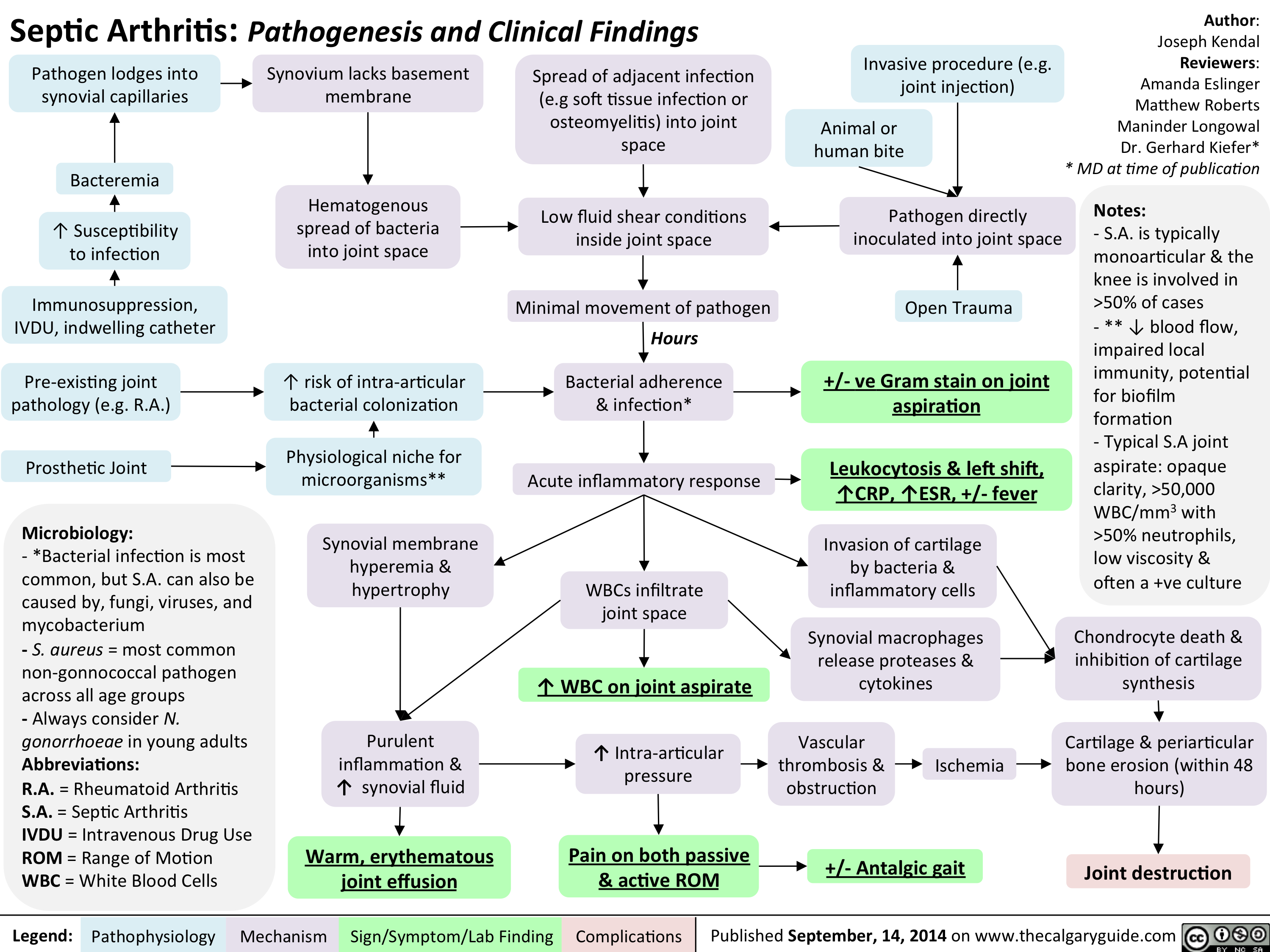
Septic arthitis pathogenesis and clinical findings
Family Med Slides Vitamin D Deficiency

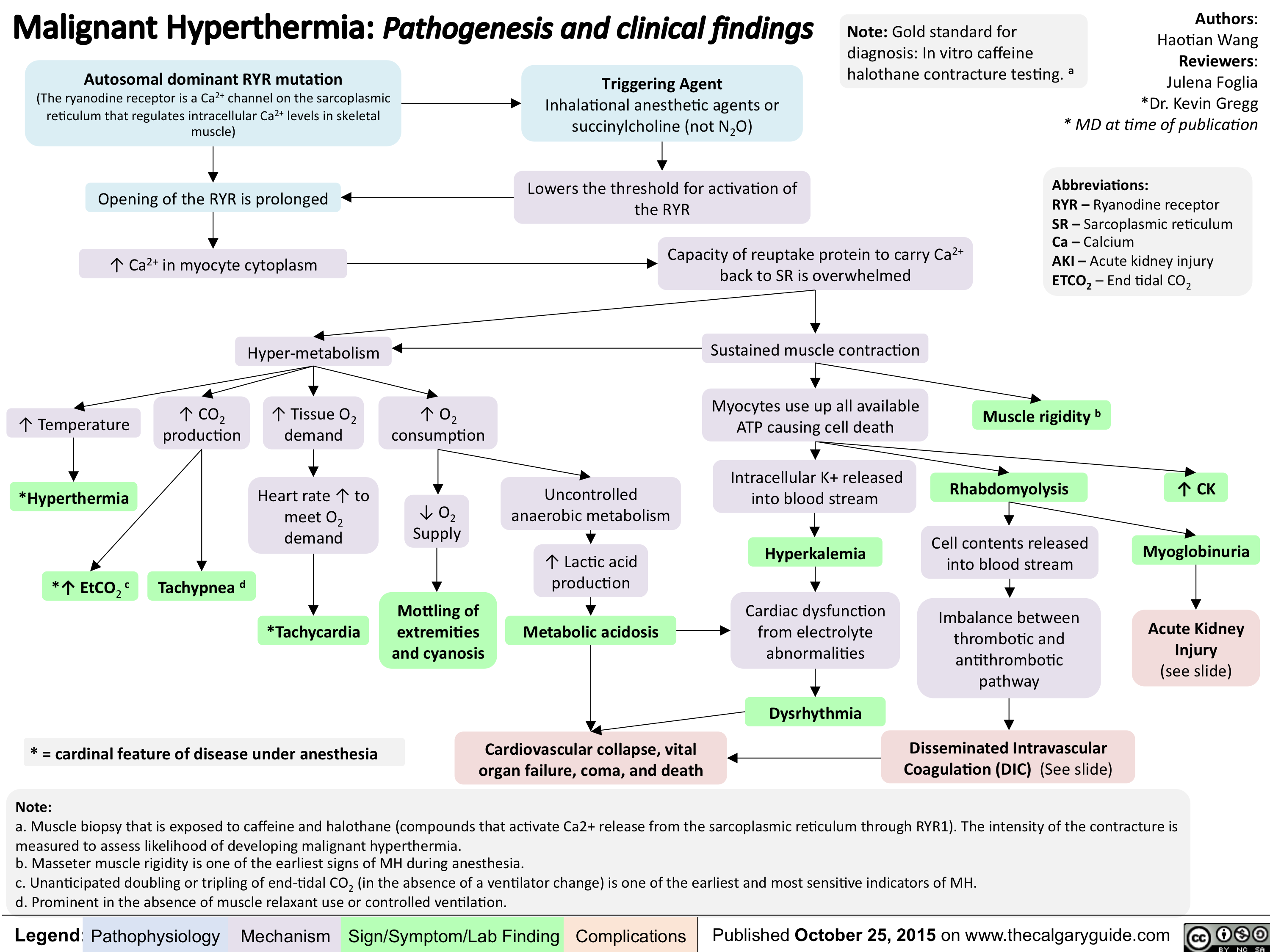
Malignant Hyperthermia-Pathogenesis and clinical findings
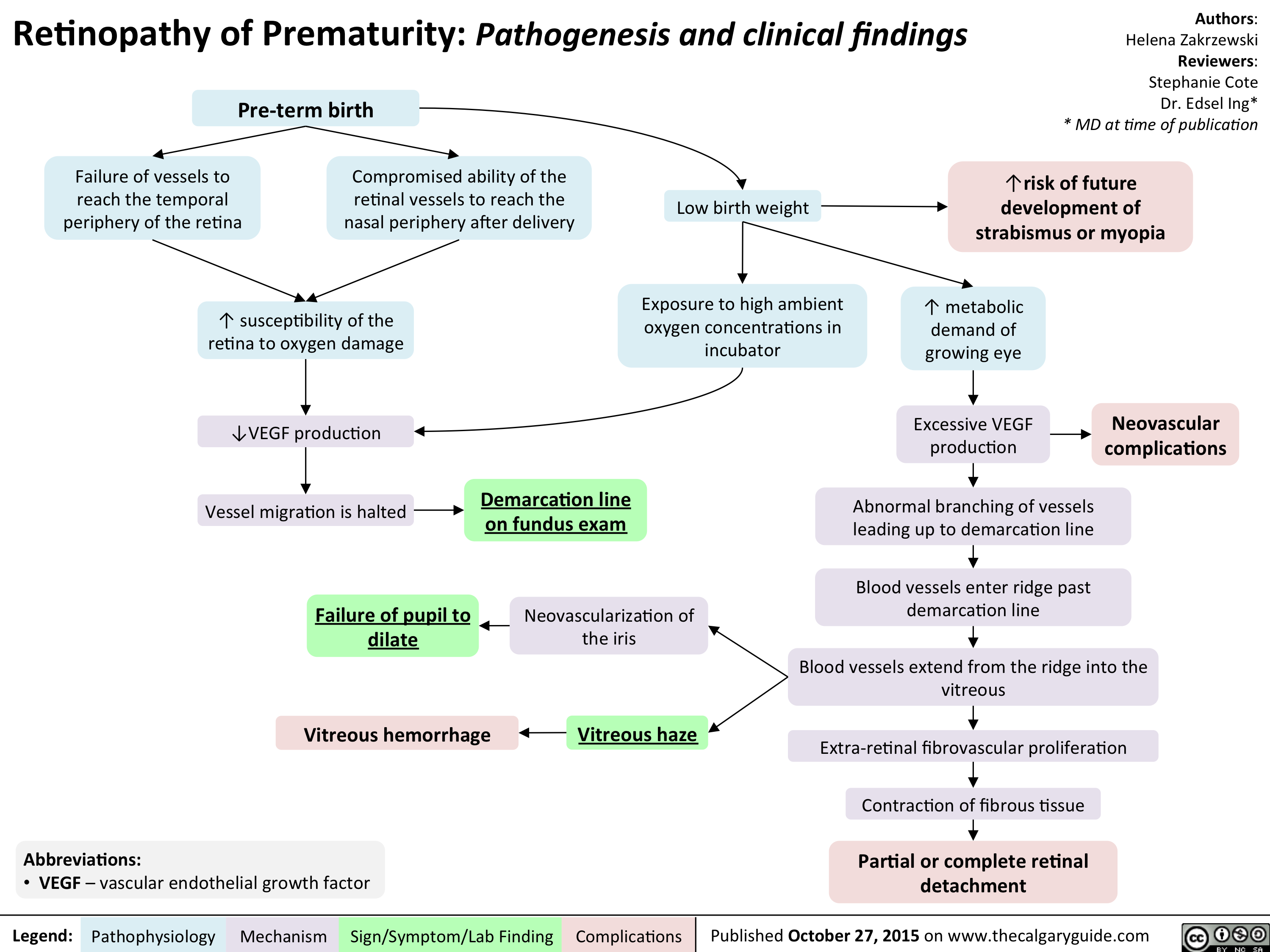
Retinopathy of Prematurity - Pathogenesis and clinical findings
Orthostatic Hypotension-Pathogenesis and clinical findings

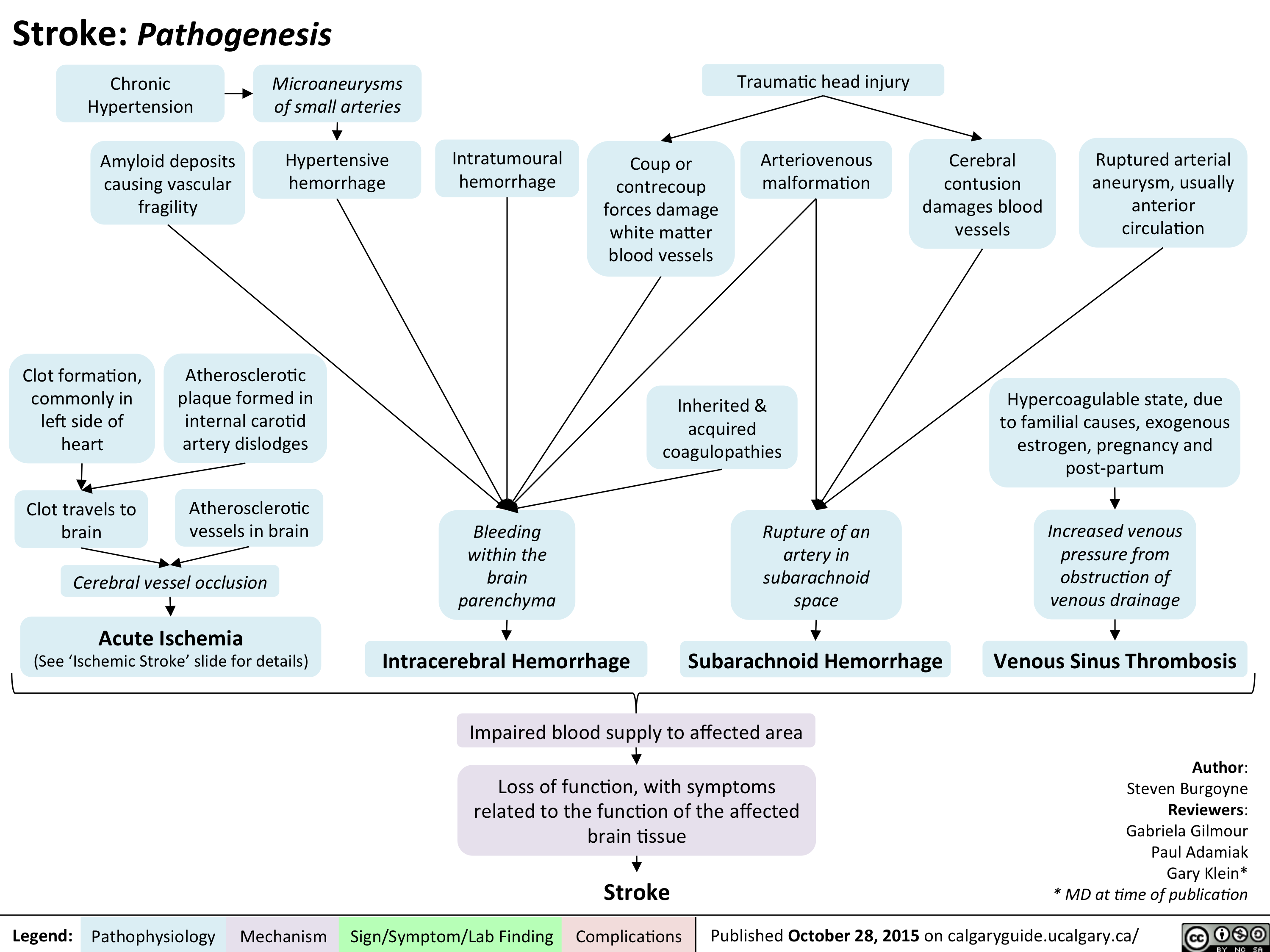
Stroke - Pathogenesis
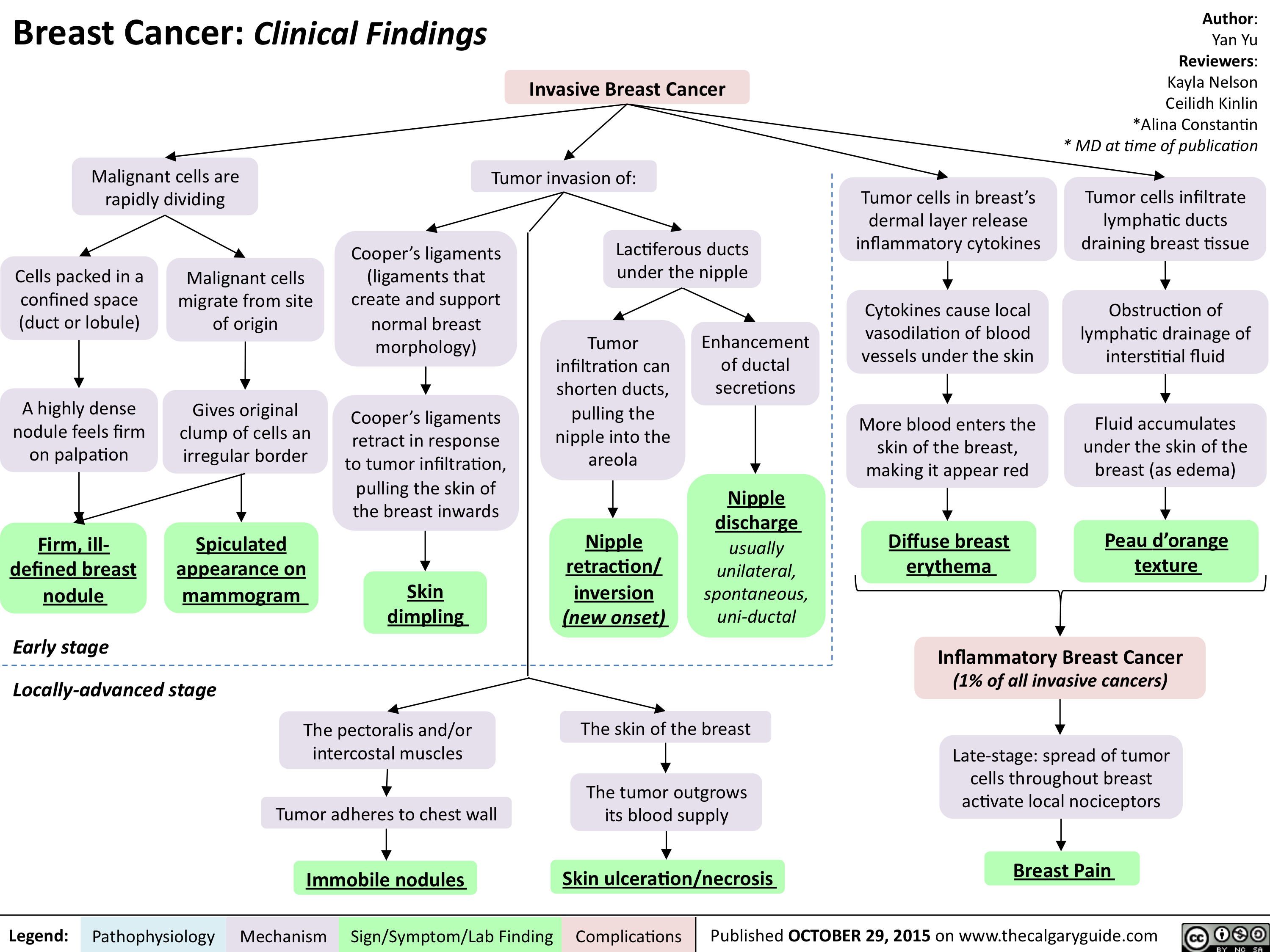
Breast Cancer - Clinical findings
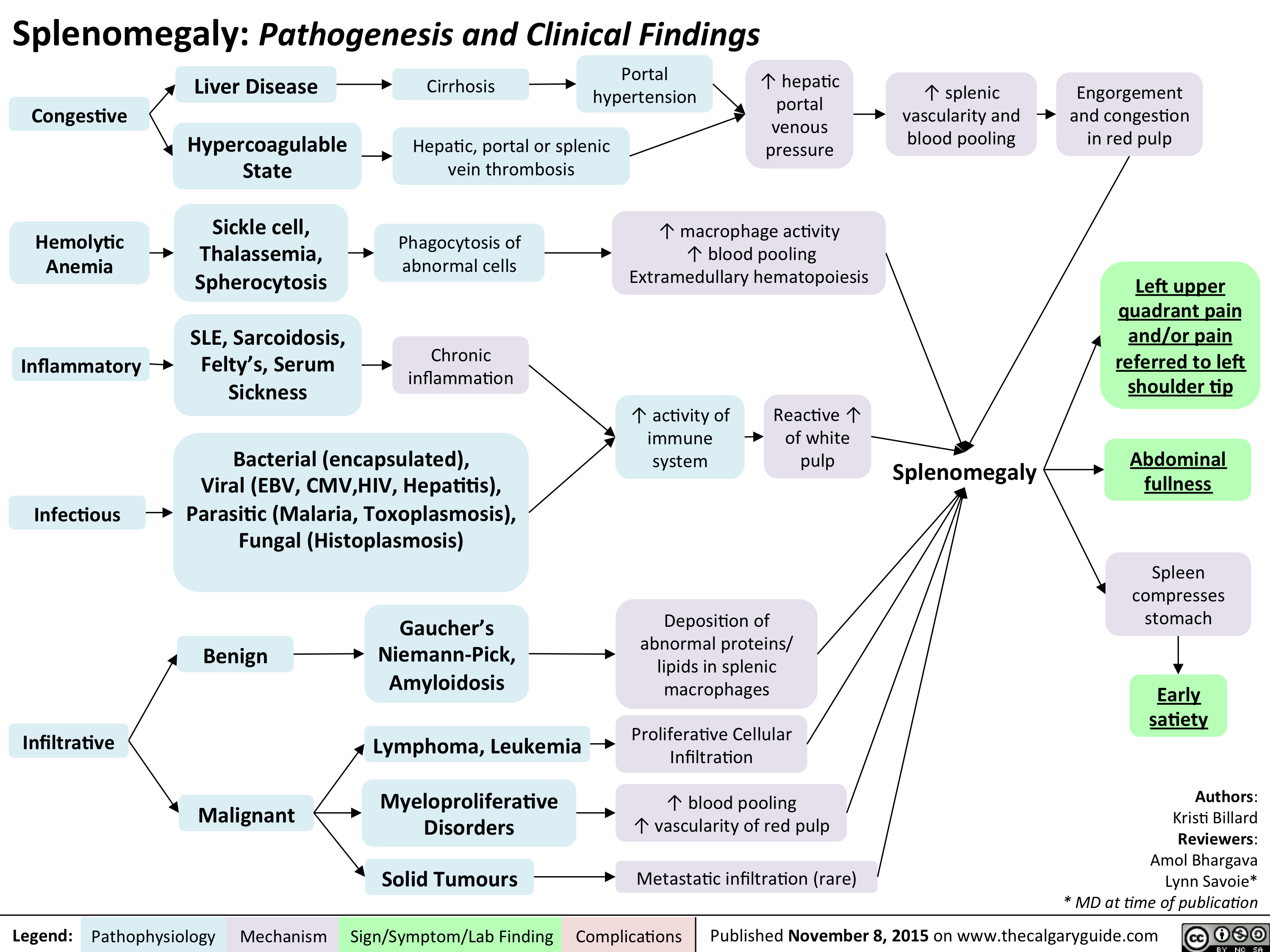
Splenomegaly - Pathogenesis and clinical findings
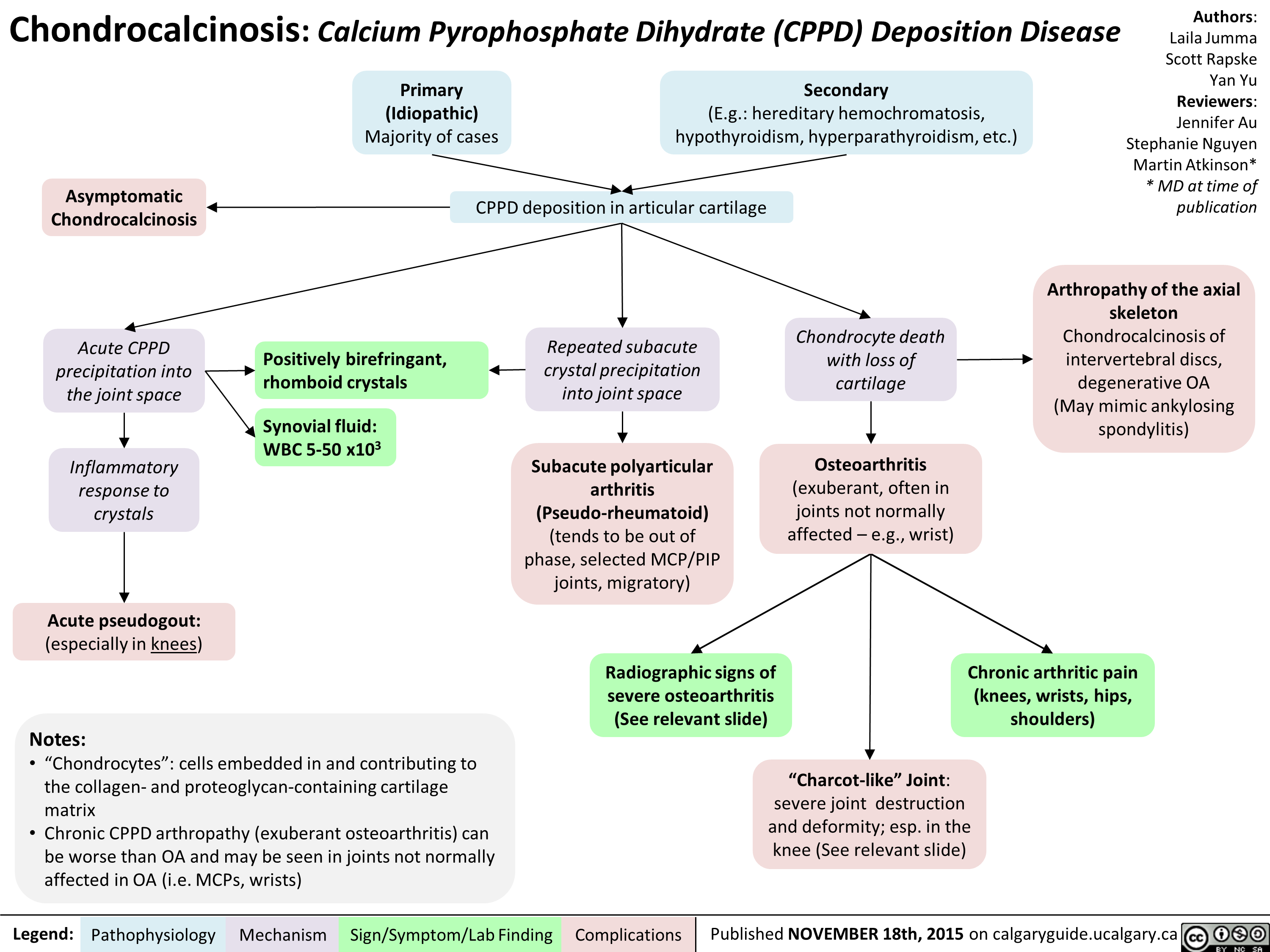
Chondrocalcinosis Calcium Pyrophosphate Dihydrate Deposition Disease
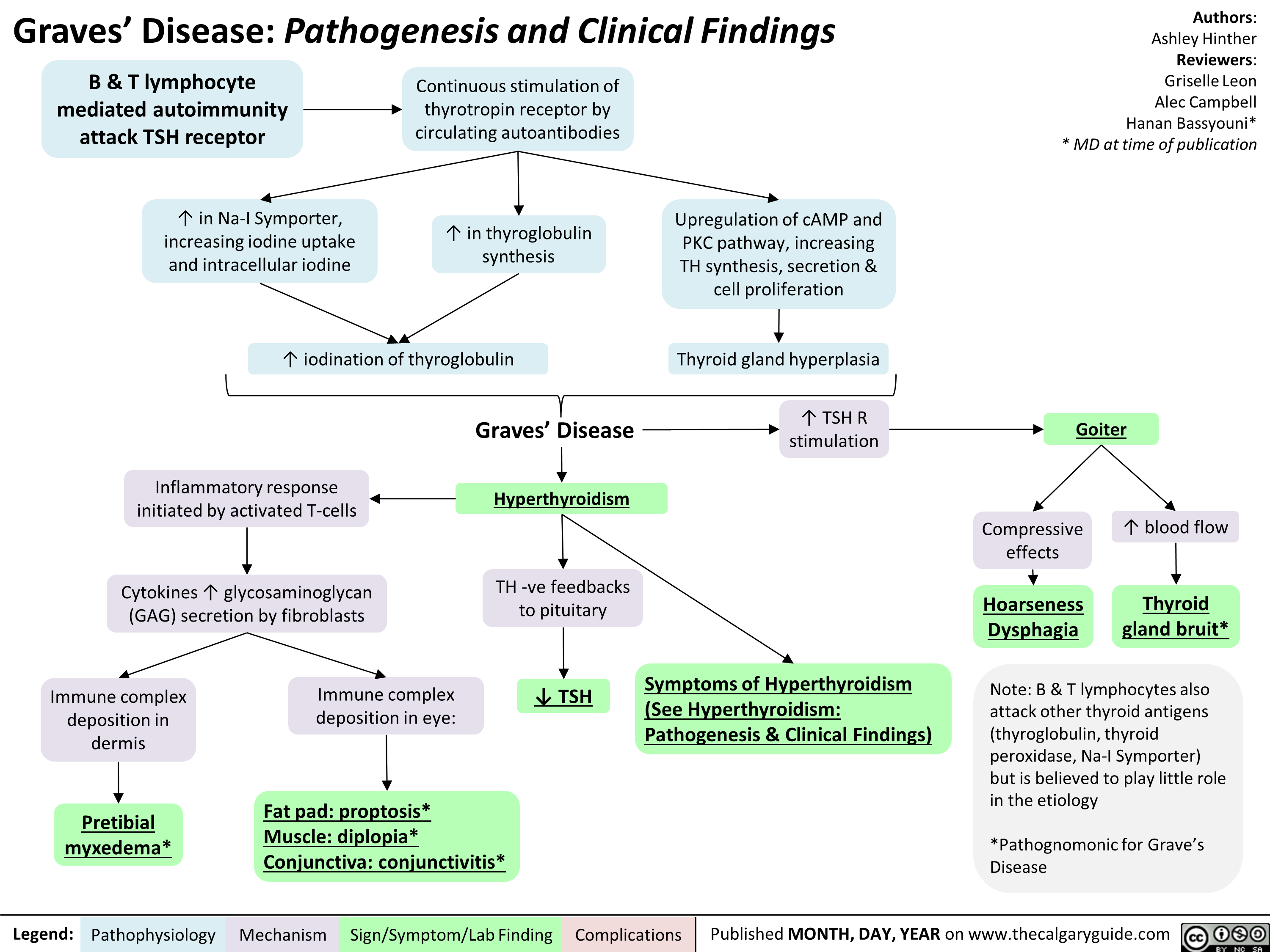
Graves' Disease Pathogenesis & Clinical Findings
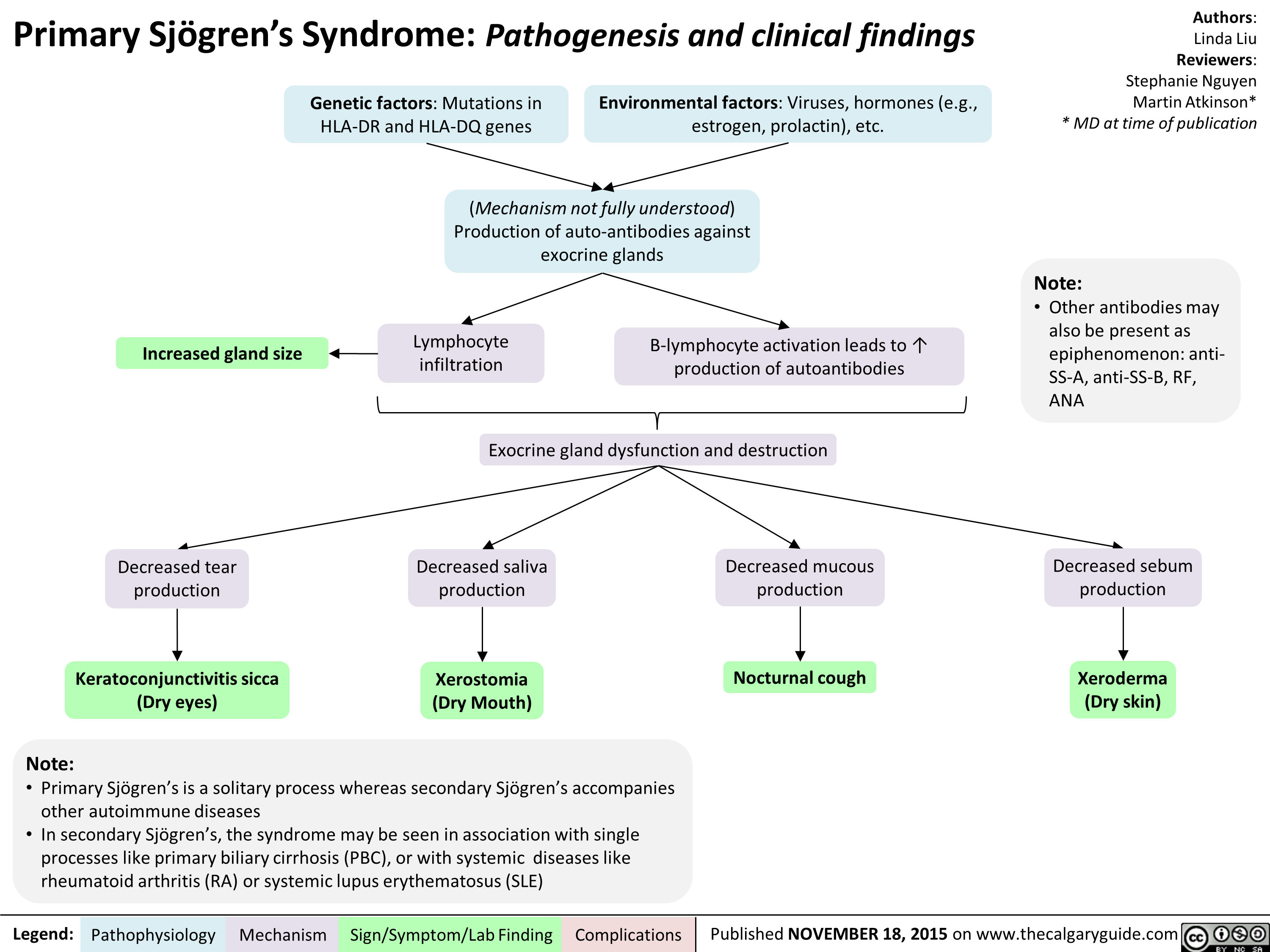
sjogrensyndrome
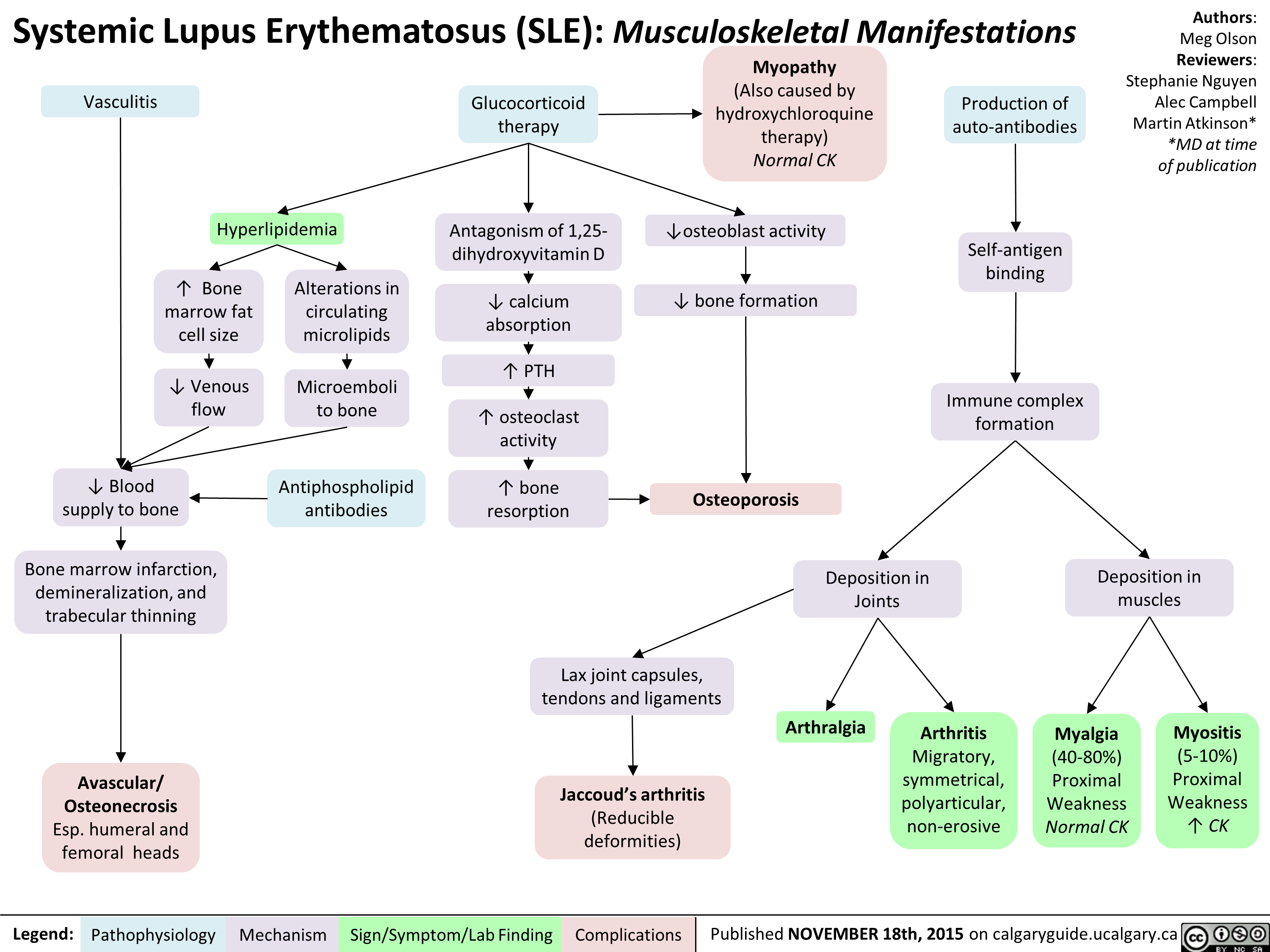
Systemic Lupus Erythematosis SLE Musculoskeletal Manifestations
Hashimoto's Thyroiditis Natural History and Clinical Findings

Hashimoto's Thyroiditis Pathogenesis and Clinical Findings
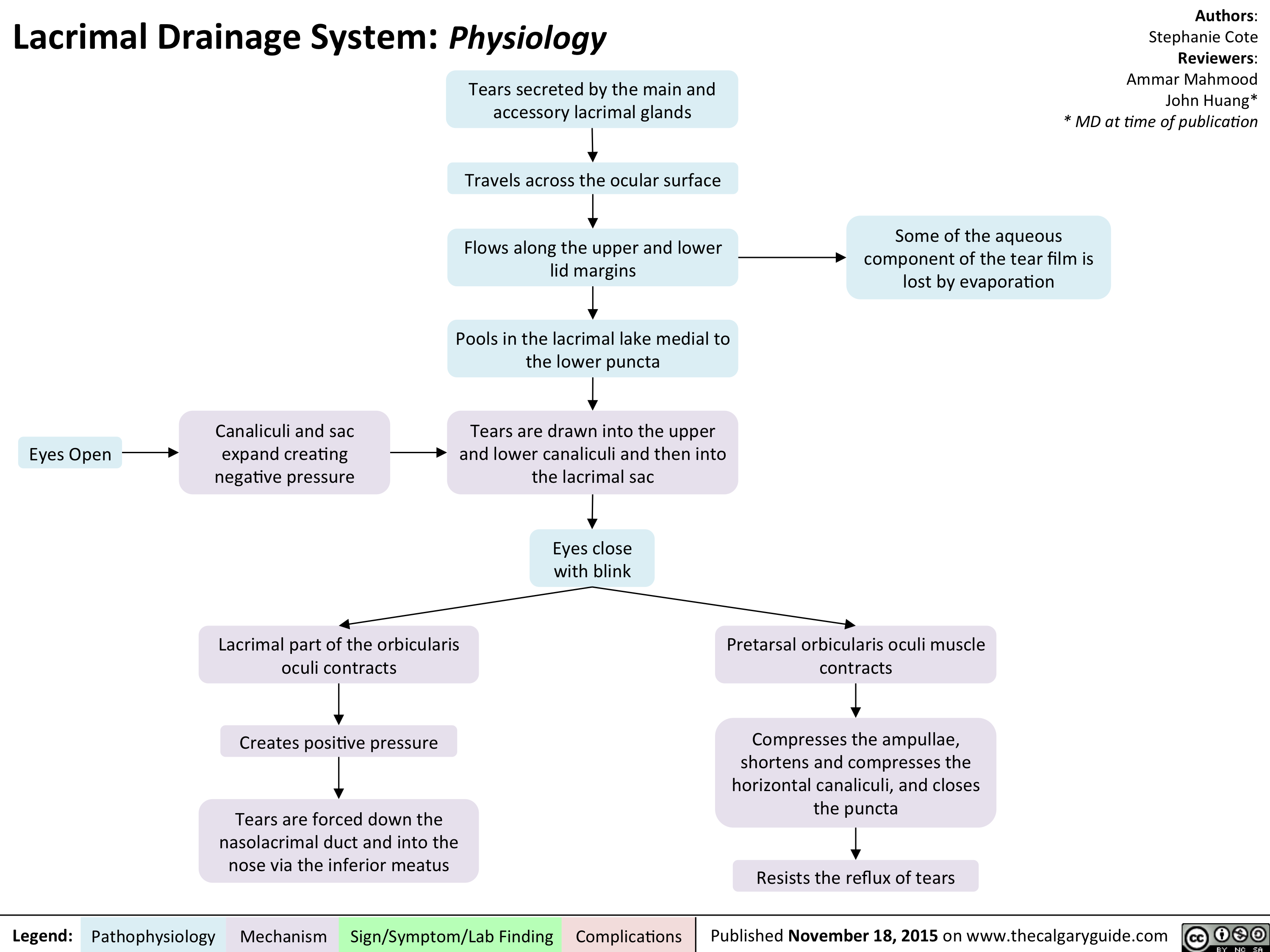
Lacrimal Drainage System - Physiology
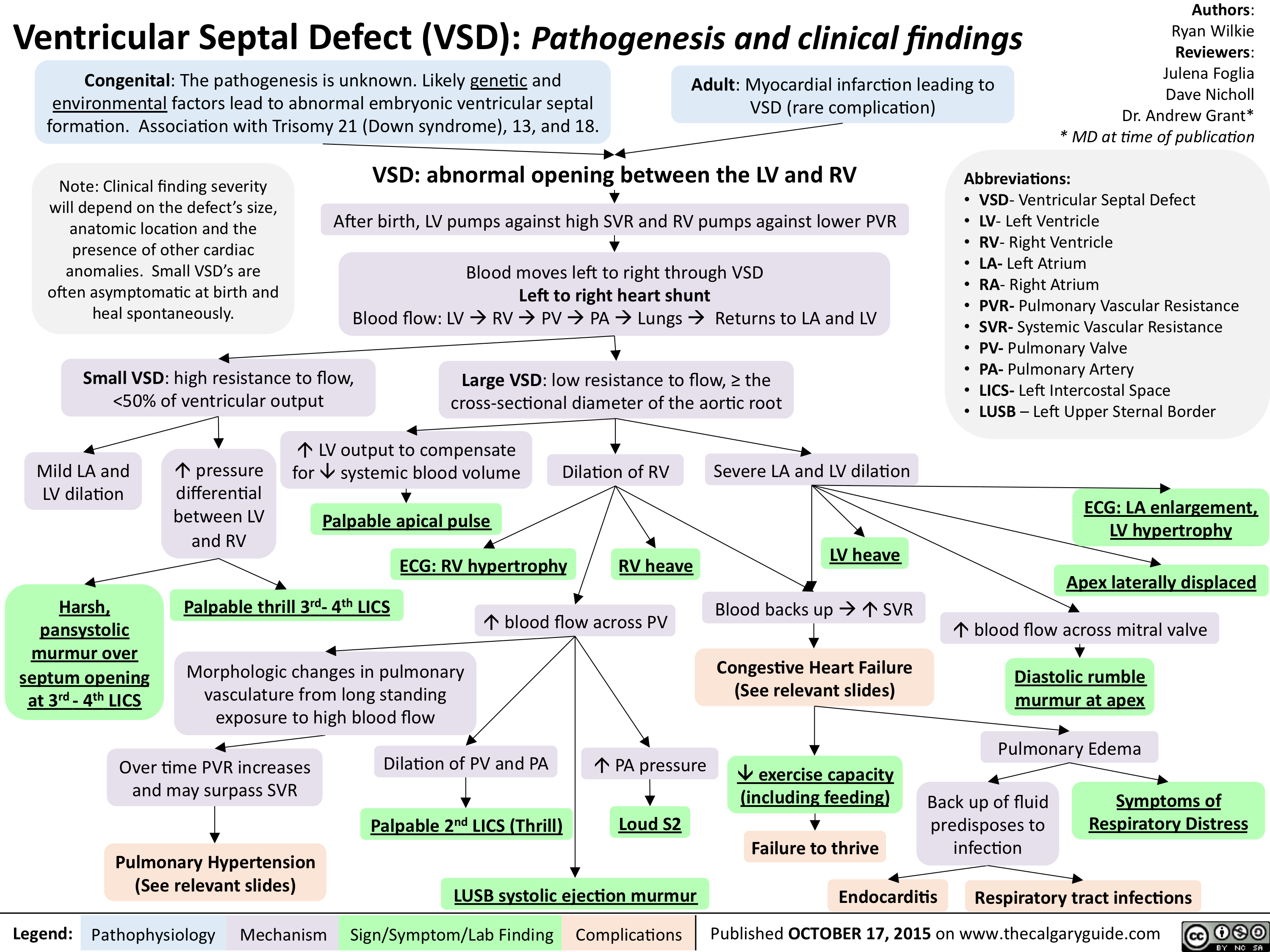
Ventricular Septal Defect (VSD)-Pathogenesis and clinical findings
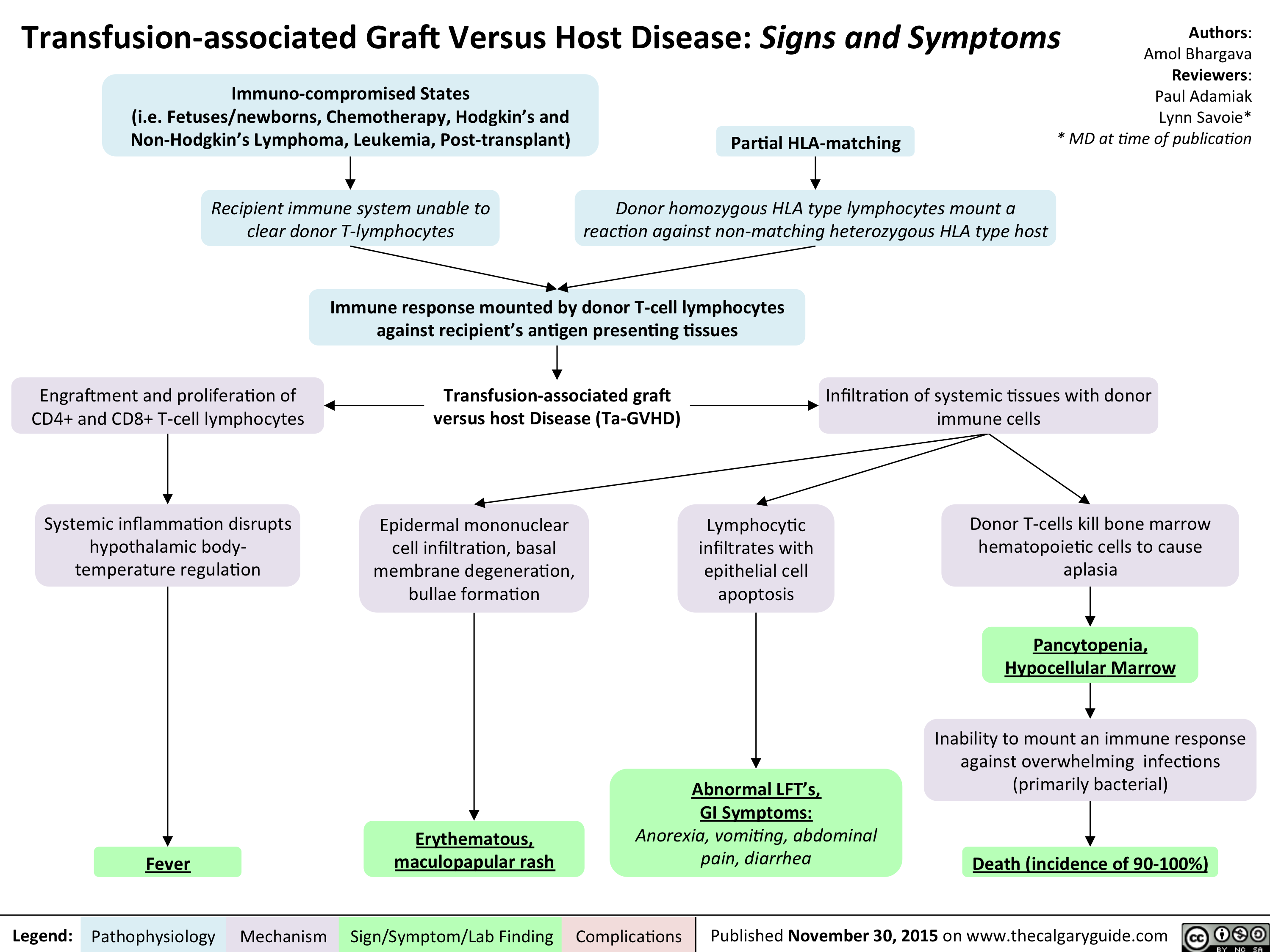
Transfusion-associated Graft Versus Host Disease - Signs and Symptoms
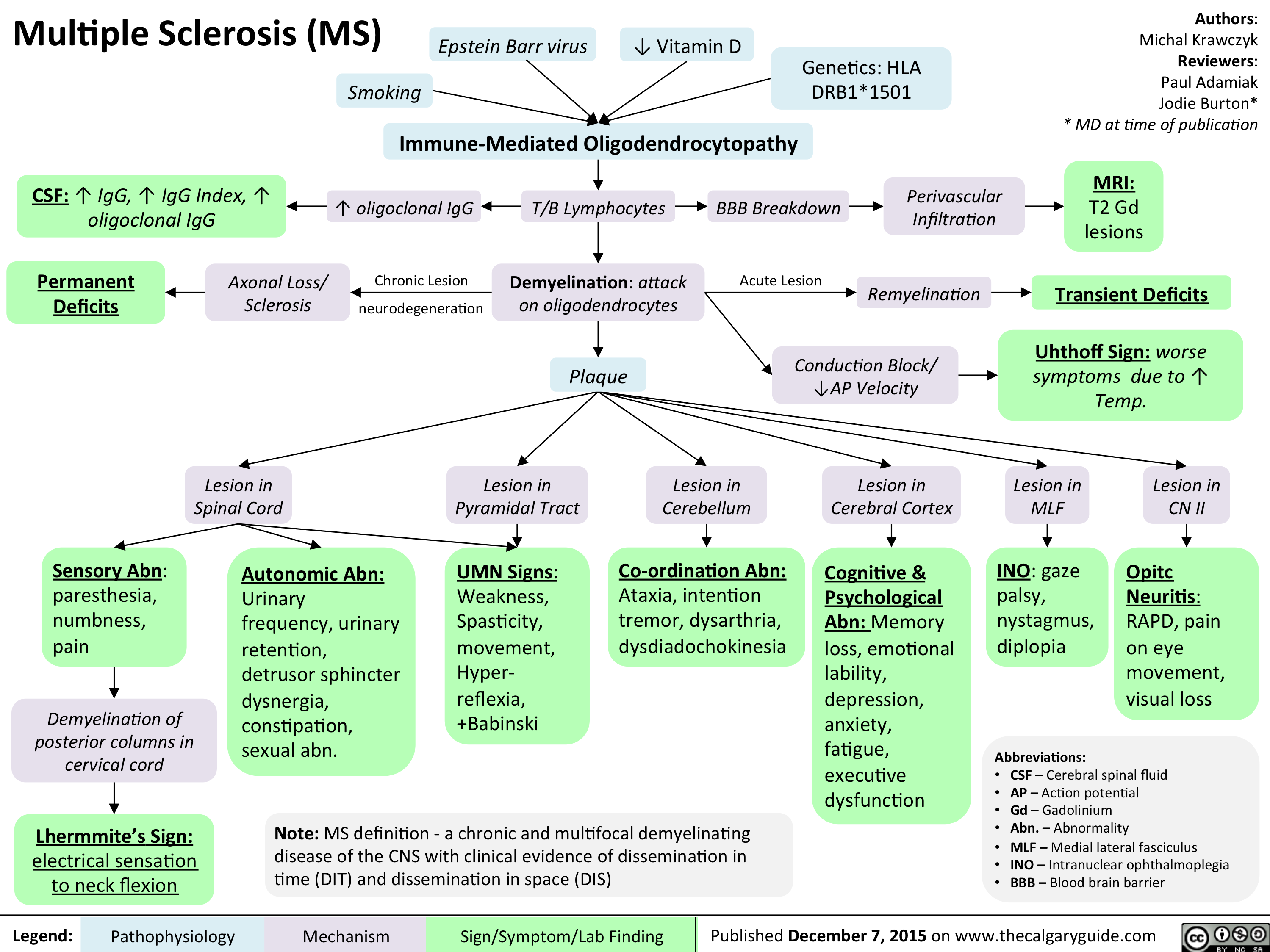
Multiple sclerosis (MS)
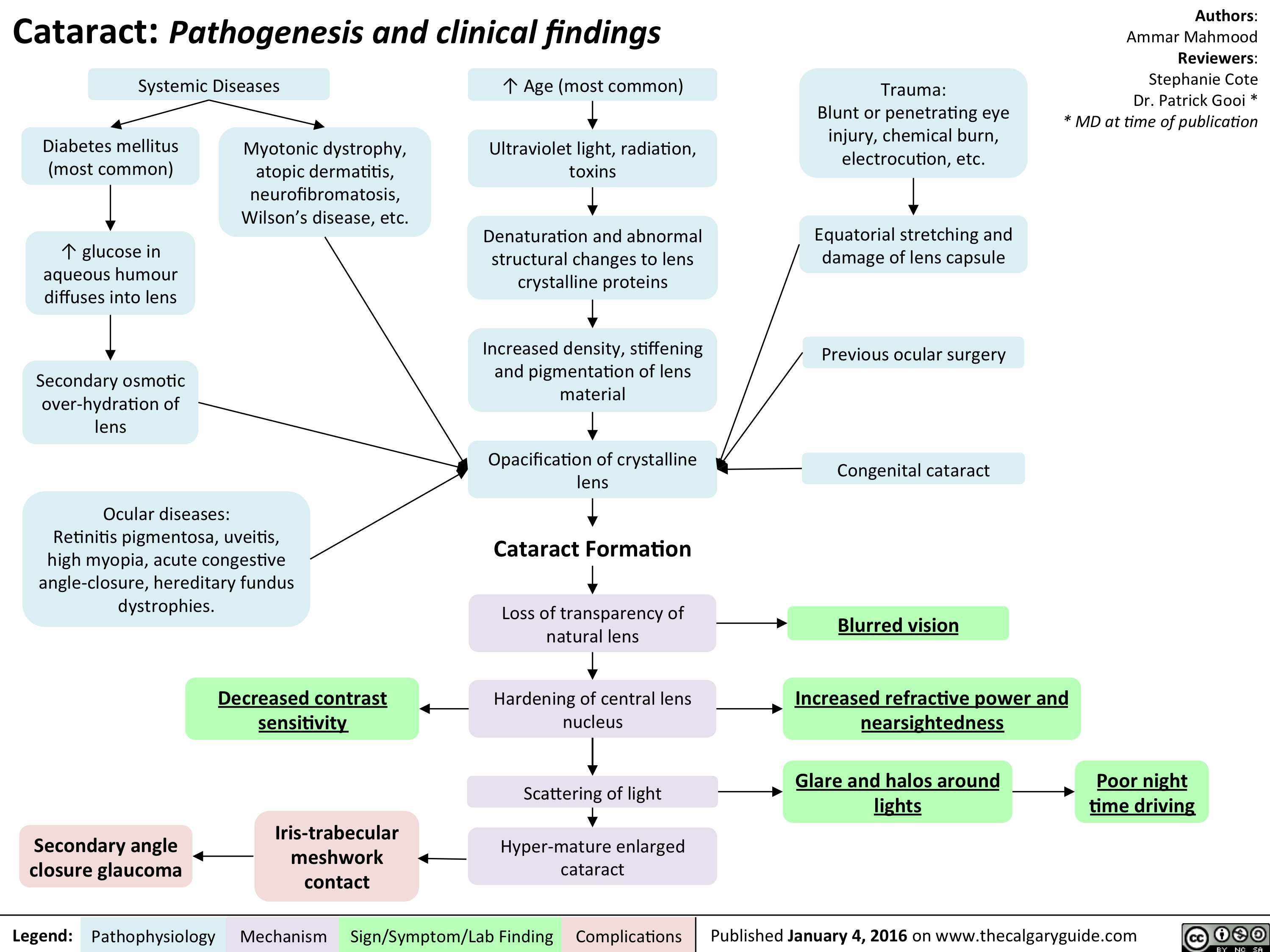
Cataracts - pathogenesis and clinical findings
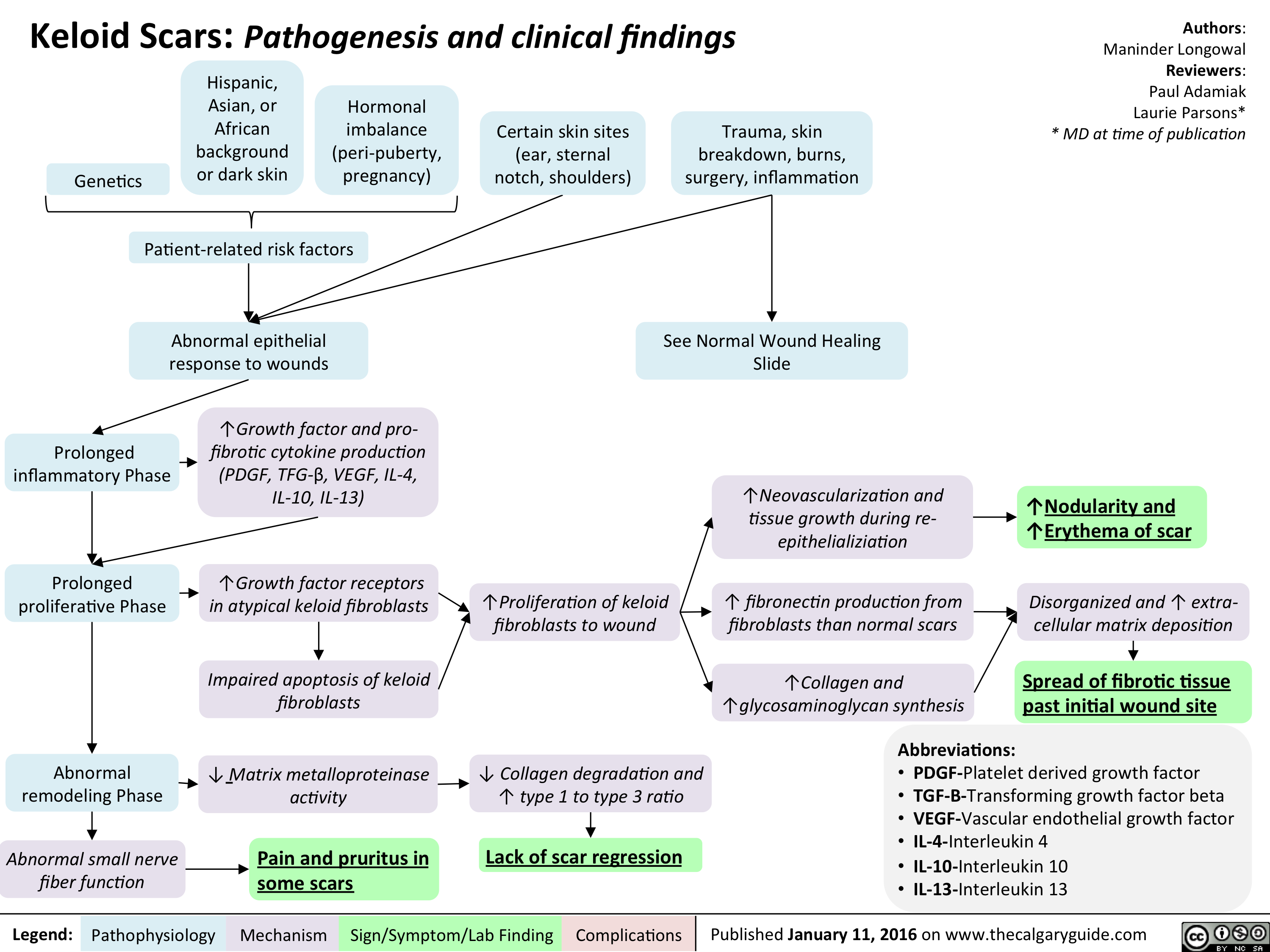
Keloid scar - pathogenesis and clinical findings
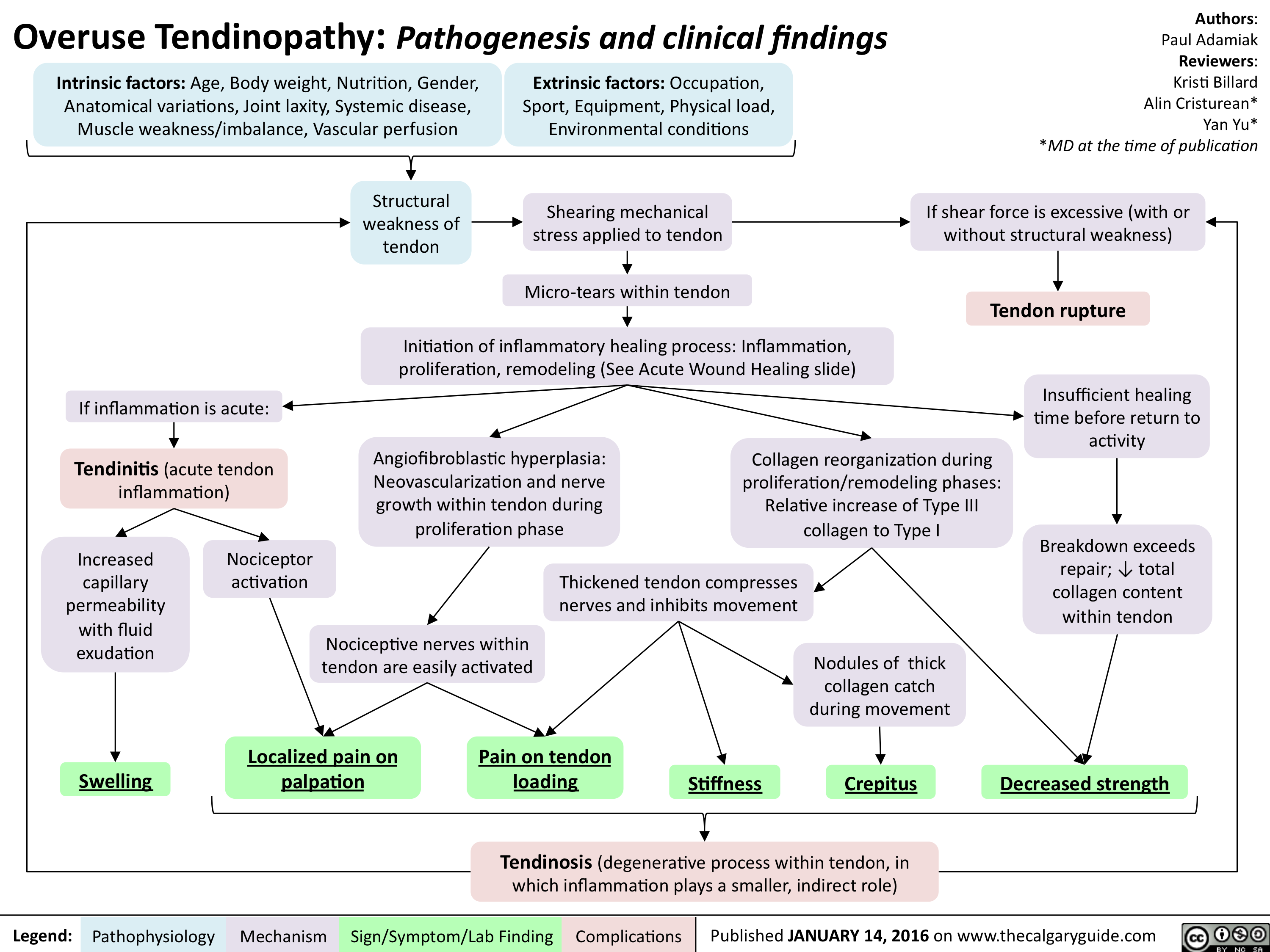
Overuse Tendinopathy -Pathogenesis and clinical findings
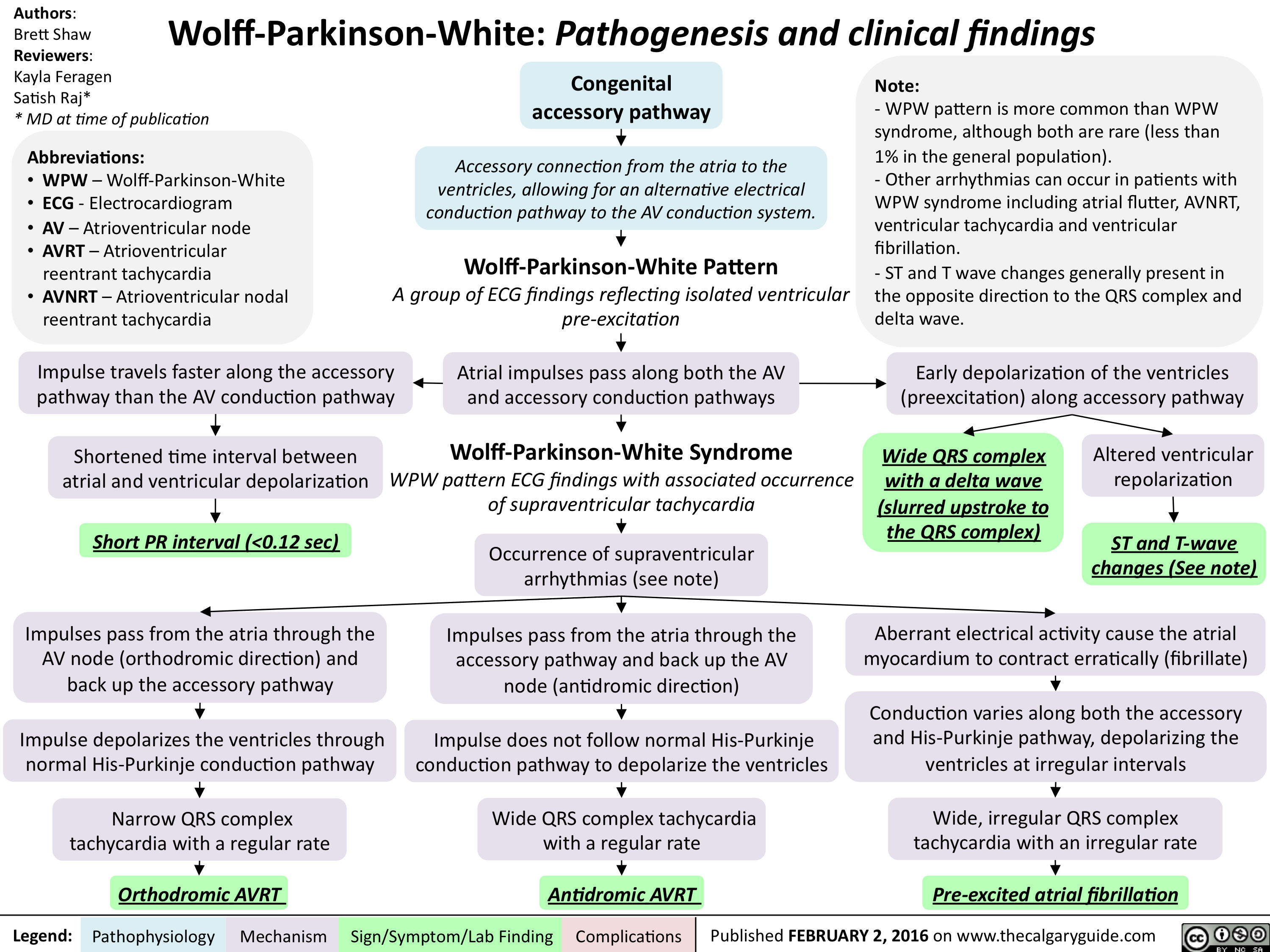
Wolff Parkinson White - Pathogenesis and clinical findings
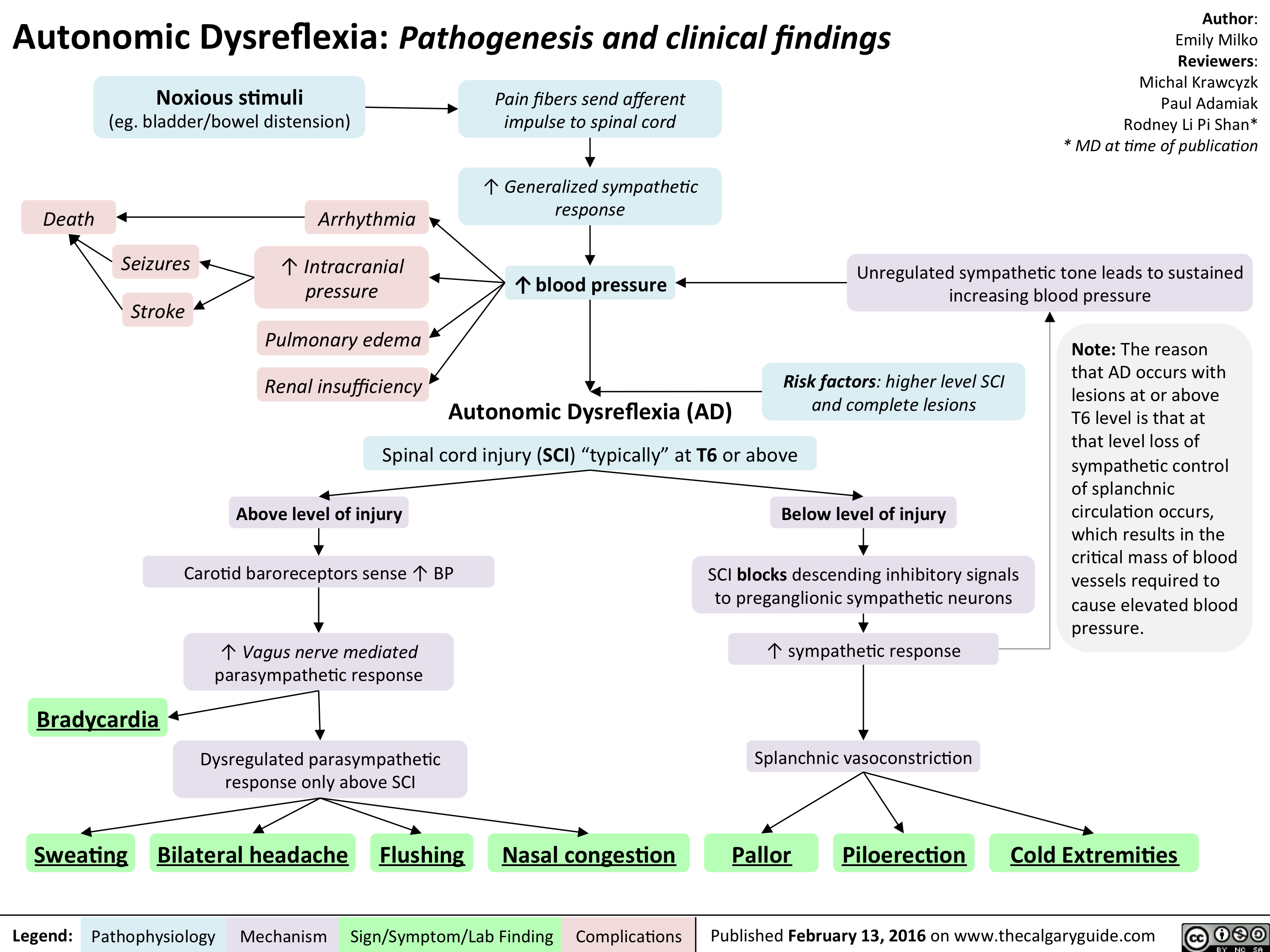
Autonomic Dysreflexia - Pathogenesis and clinical findings
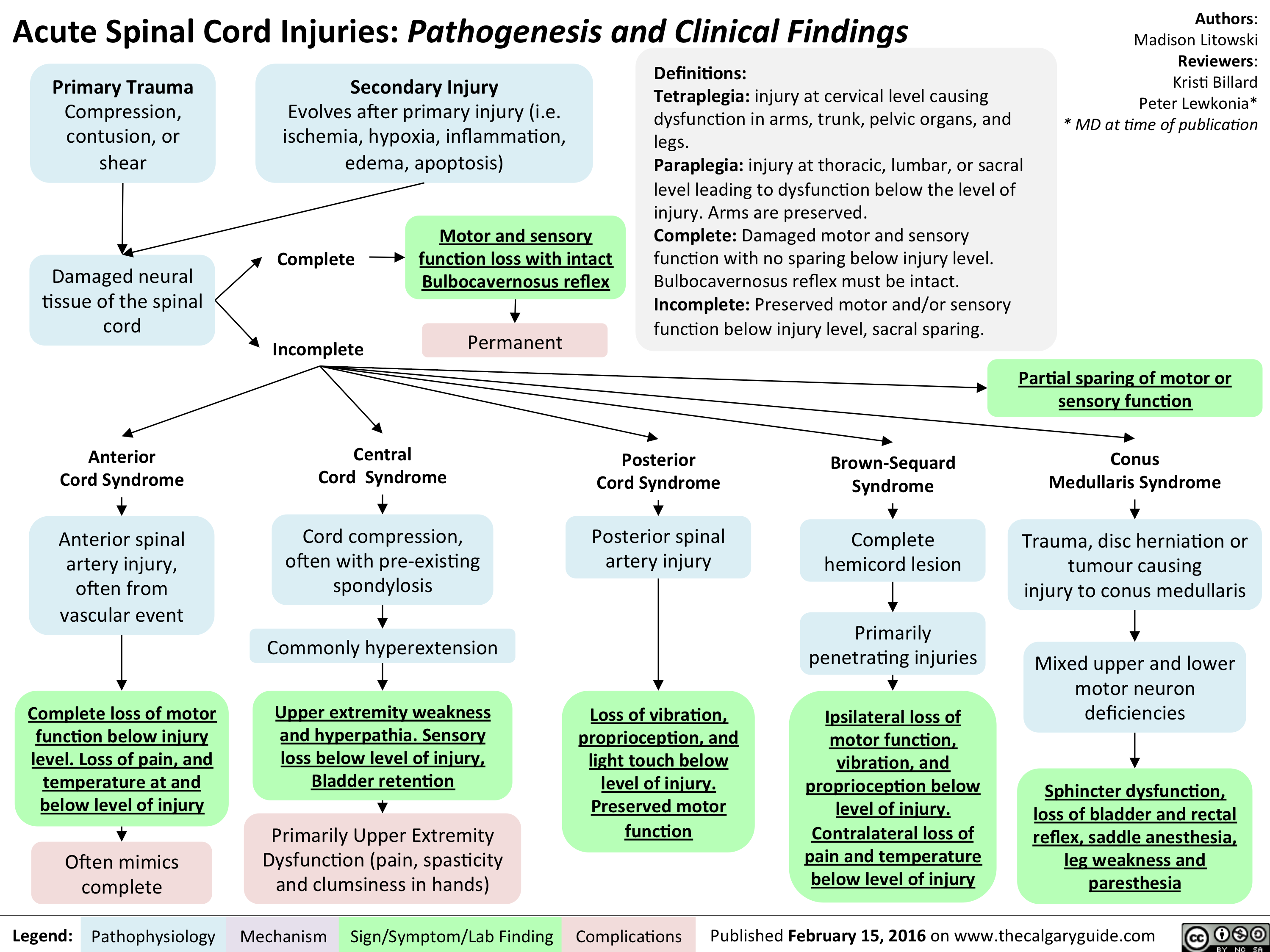
Acute Spinal Cord Injuries - Pathogenesis and clinical findings
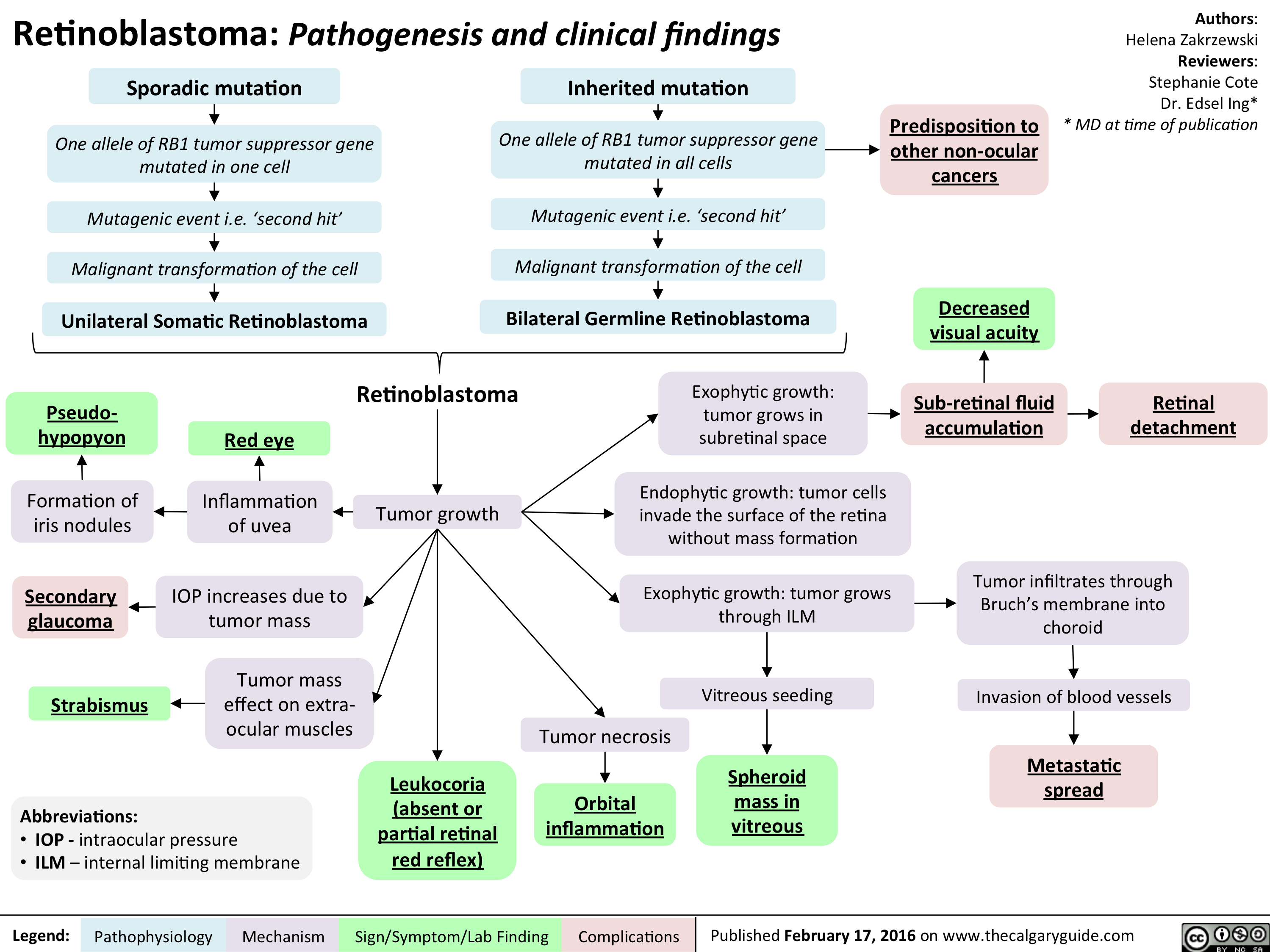
Retinoblastoma - Pathogenesis and clinical findings
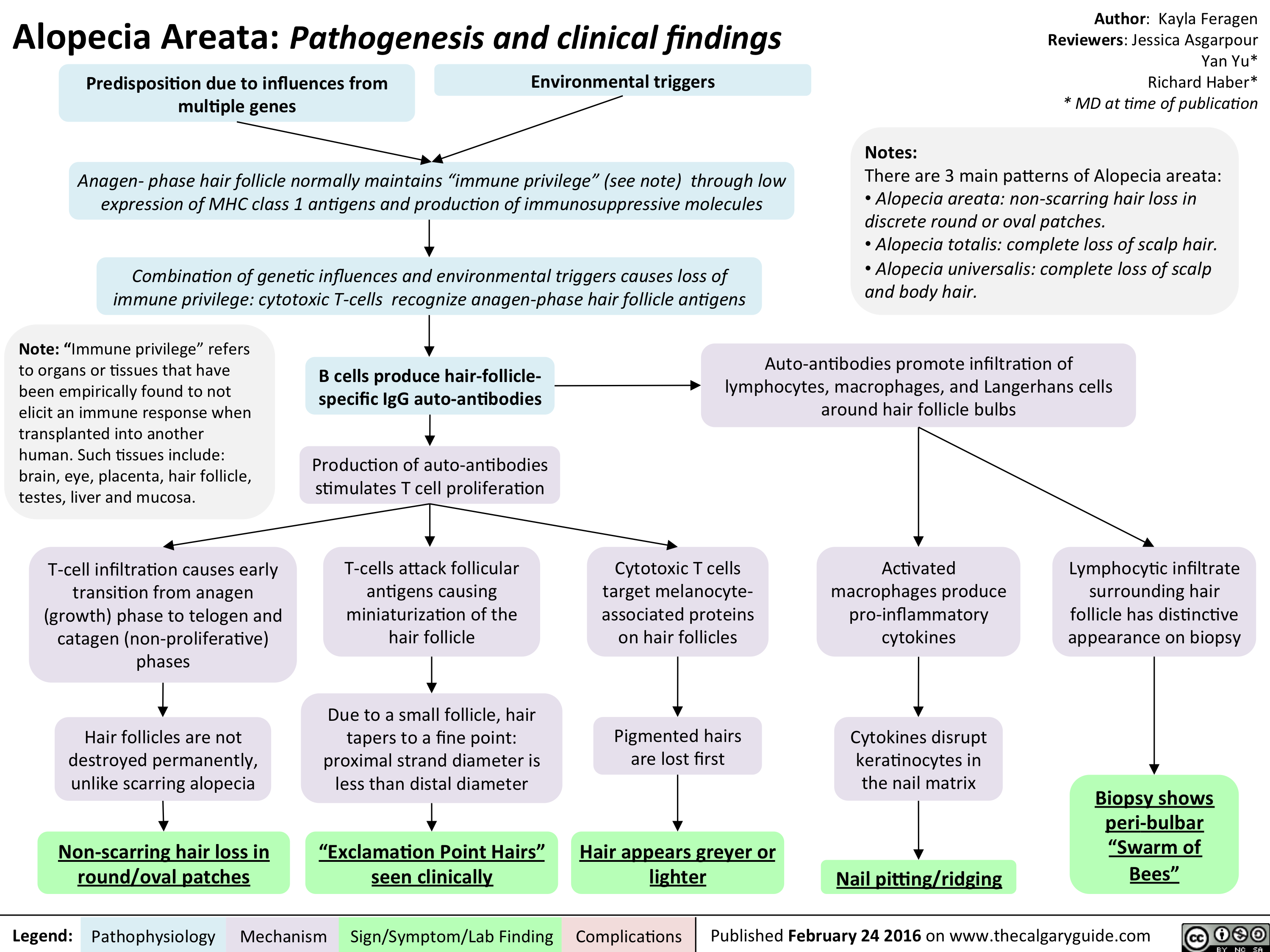
Alopecia Areata - Pathogenesis and clinical findings
Seasonal Affective Disorder - Pathogenesis and clinical findings v2

Yu, Y - Schizophrenia Pathogenesis and Clinical Findings - March 26 2016
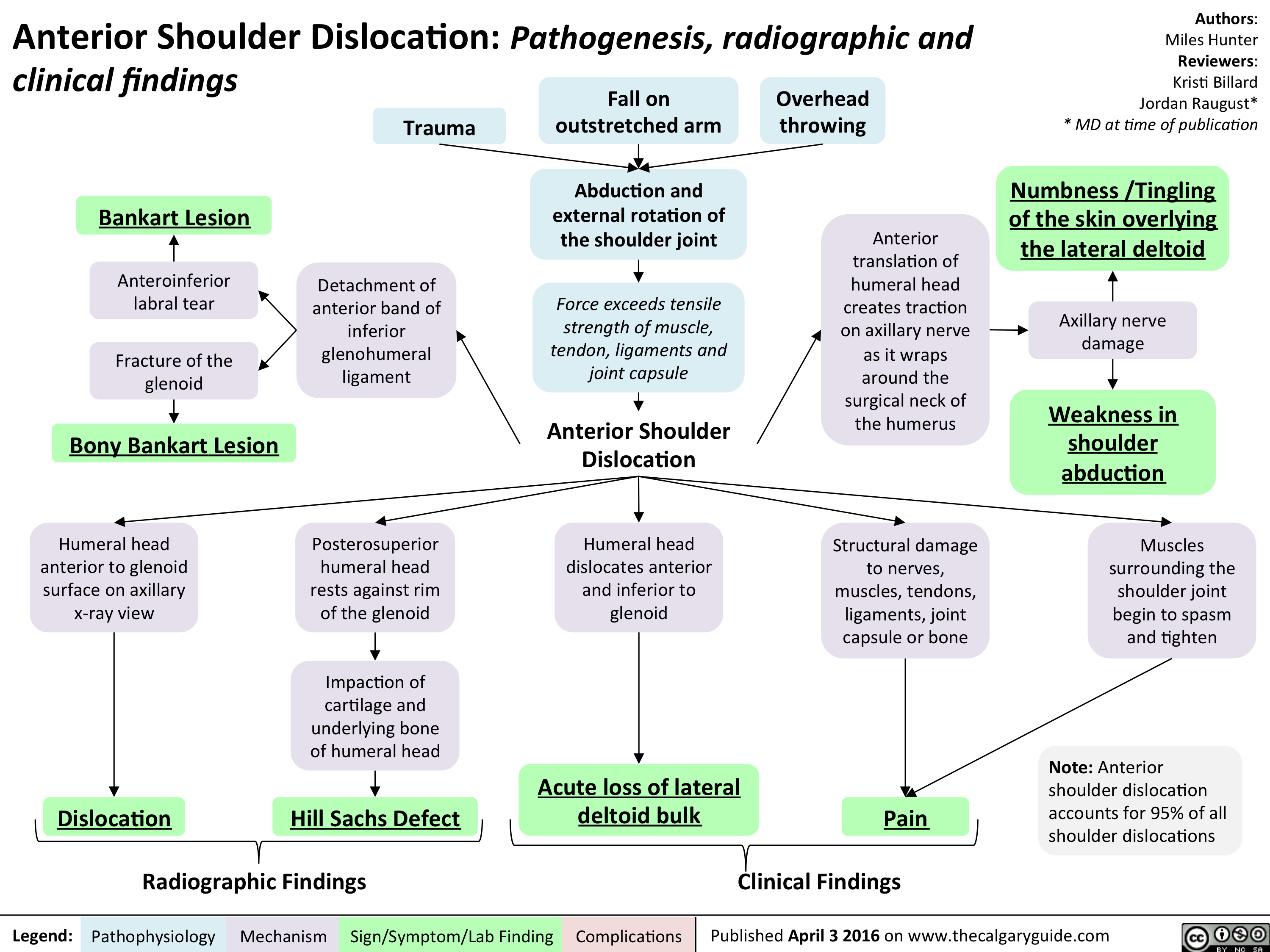
Anterior Shoulder Dislocation - Pathogensis clinical and radiographic findings
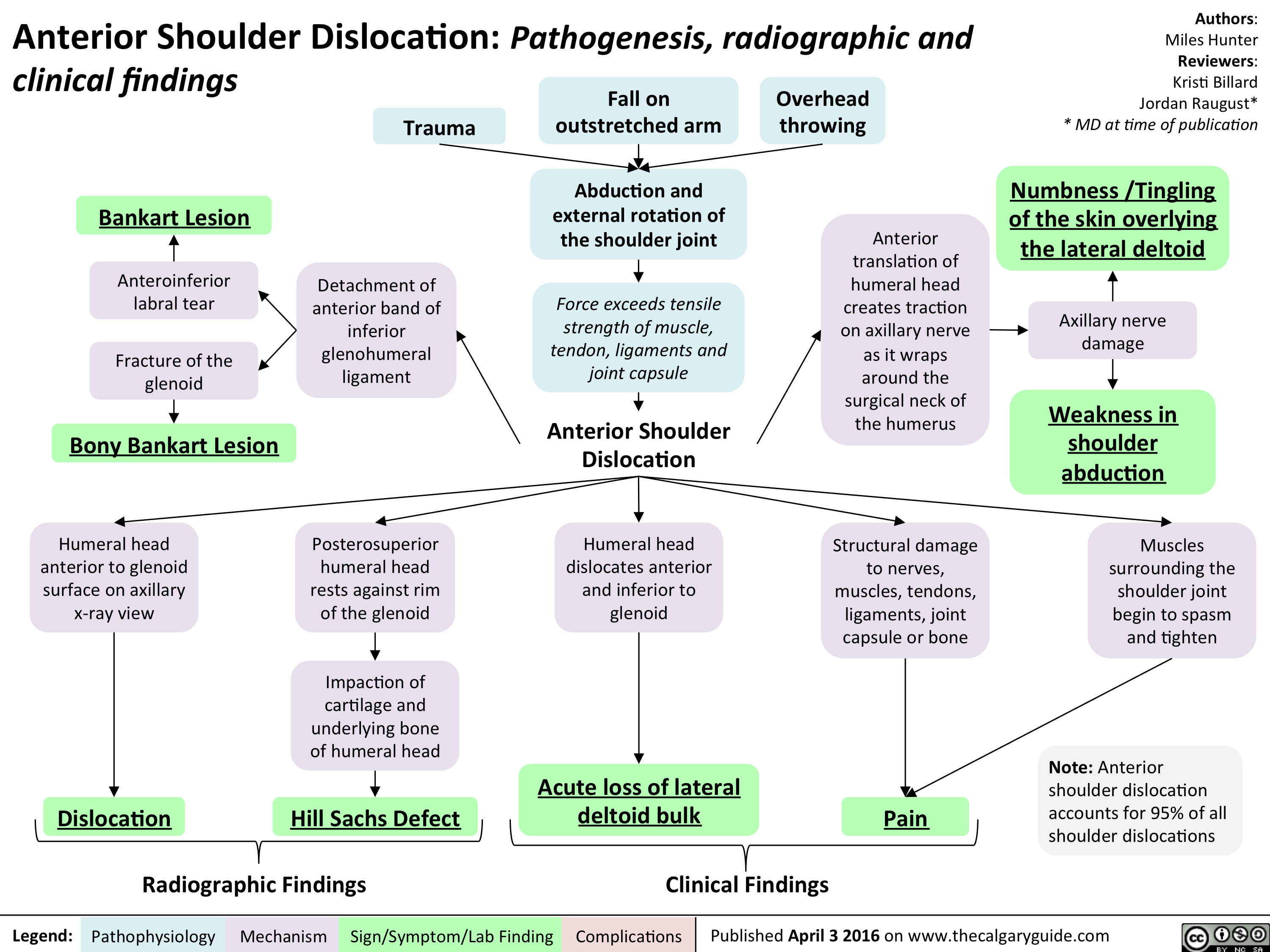
Anterior Shoulder Dislocation - Pathogensis clinical and radiographic findings
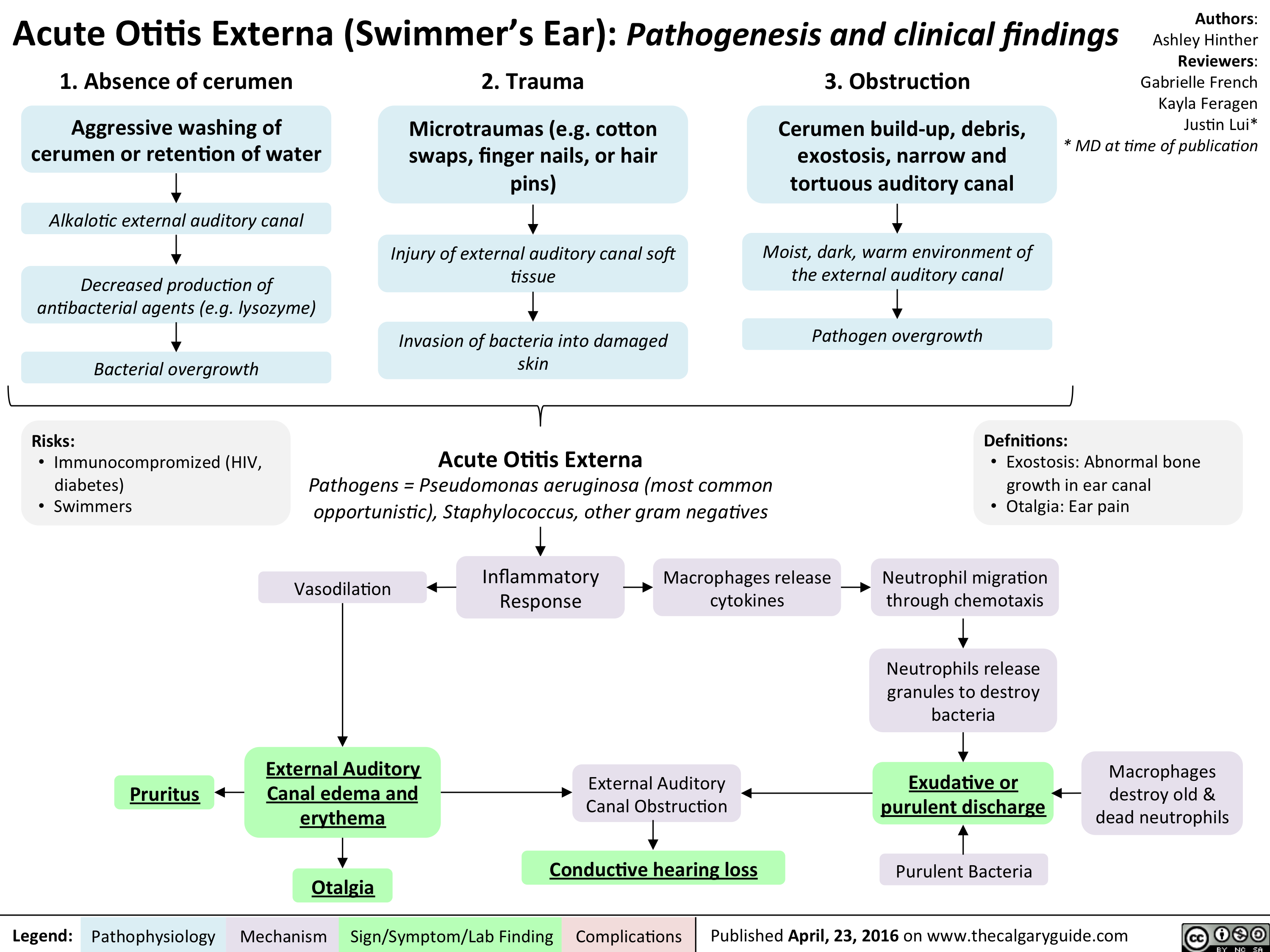
Allergic Rhinitis - Pathogenesis and clinical findings
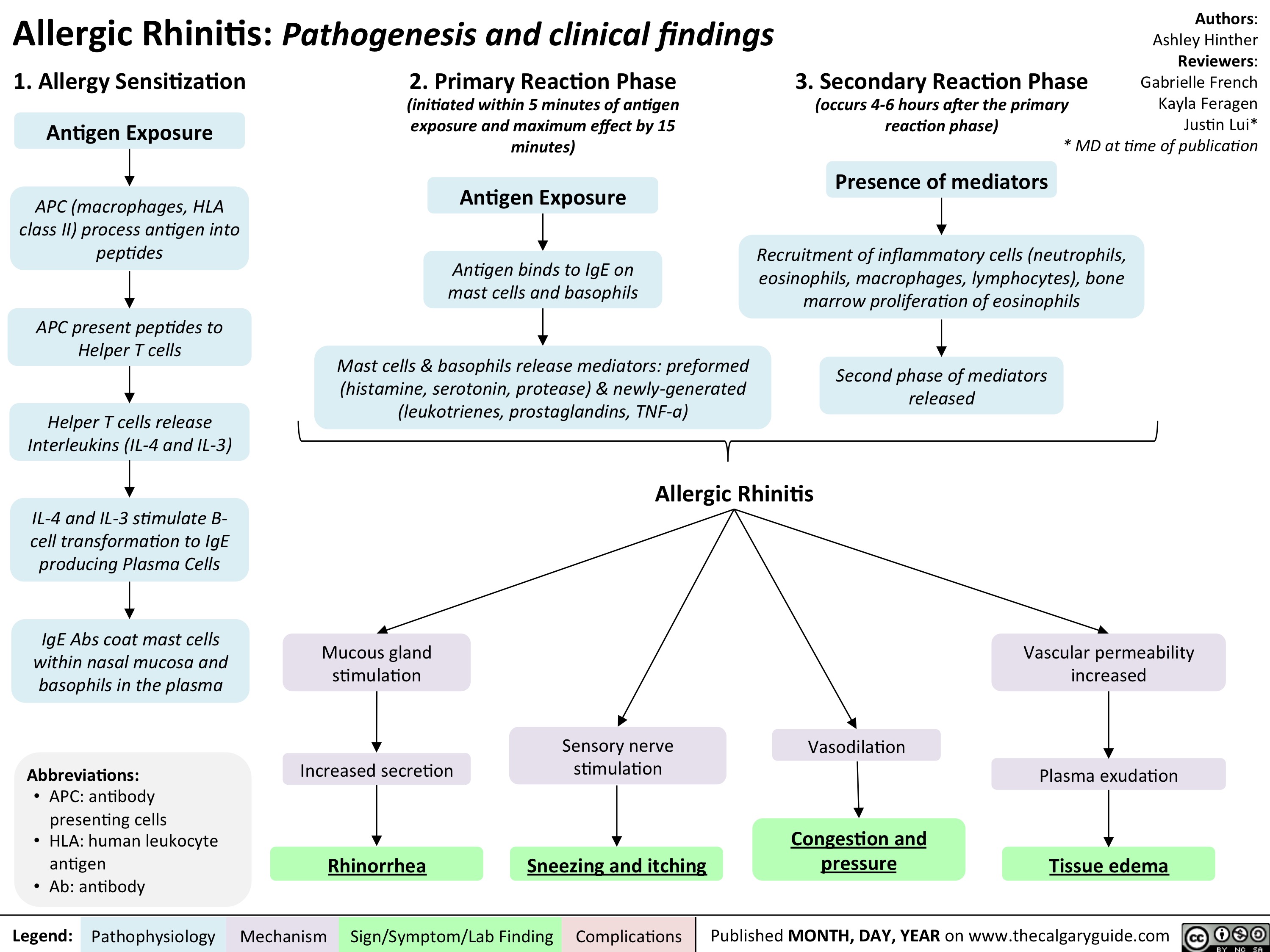
Allergic Rhinitis - Pathogenesis and clinical findings
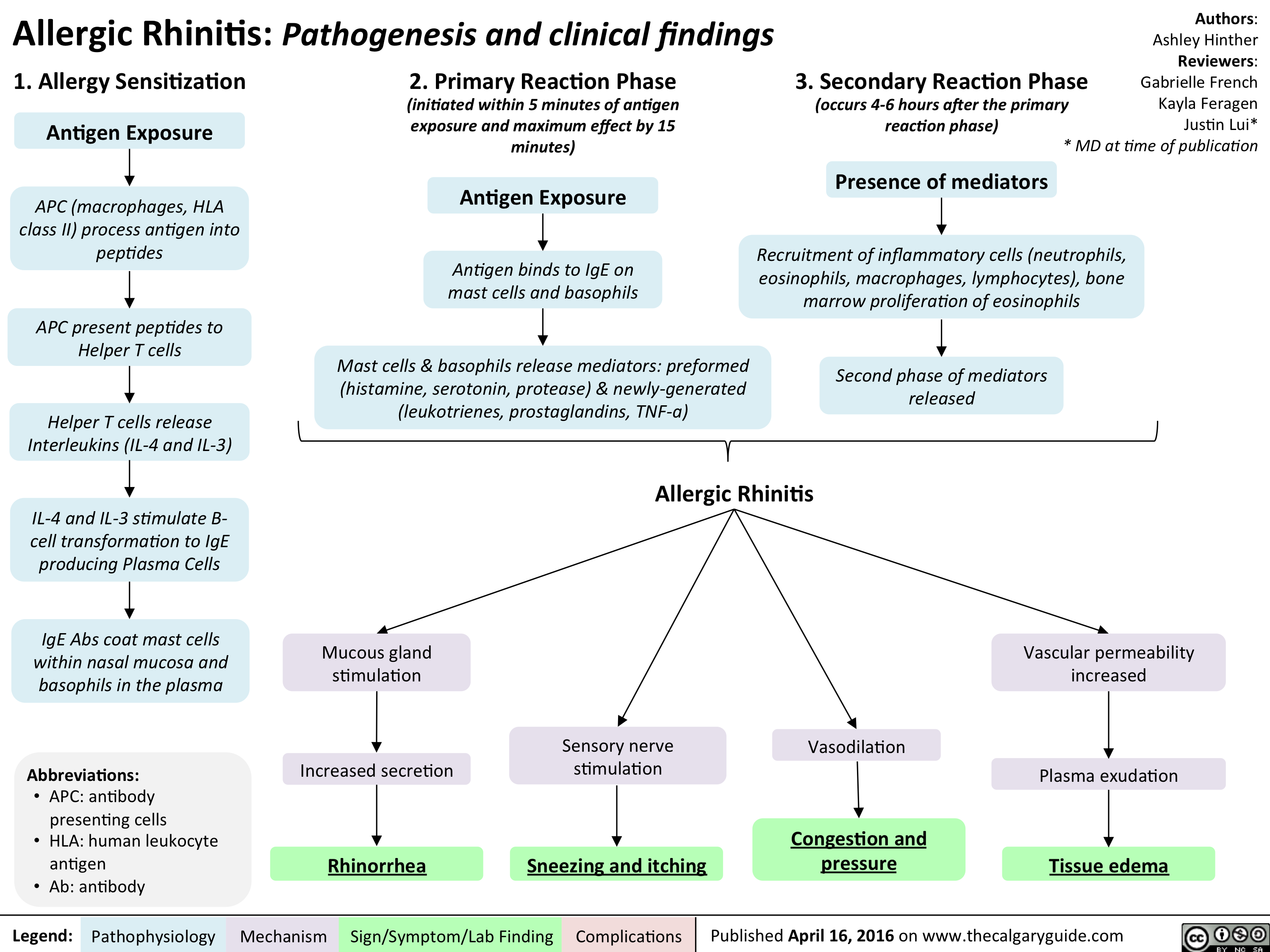
Olfactory Dysfunction - Pathogenesis and clinical findings
Tinnitus

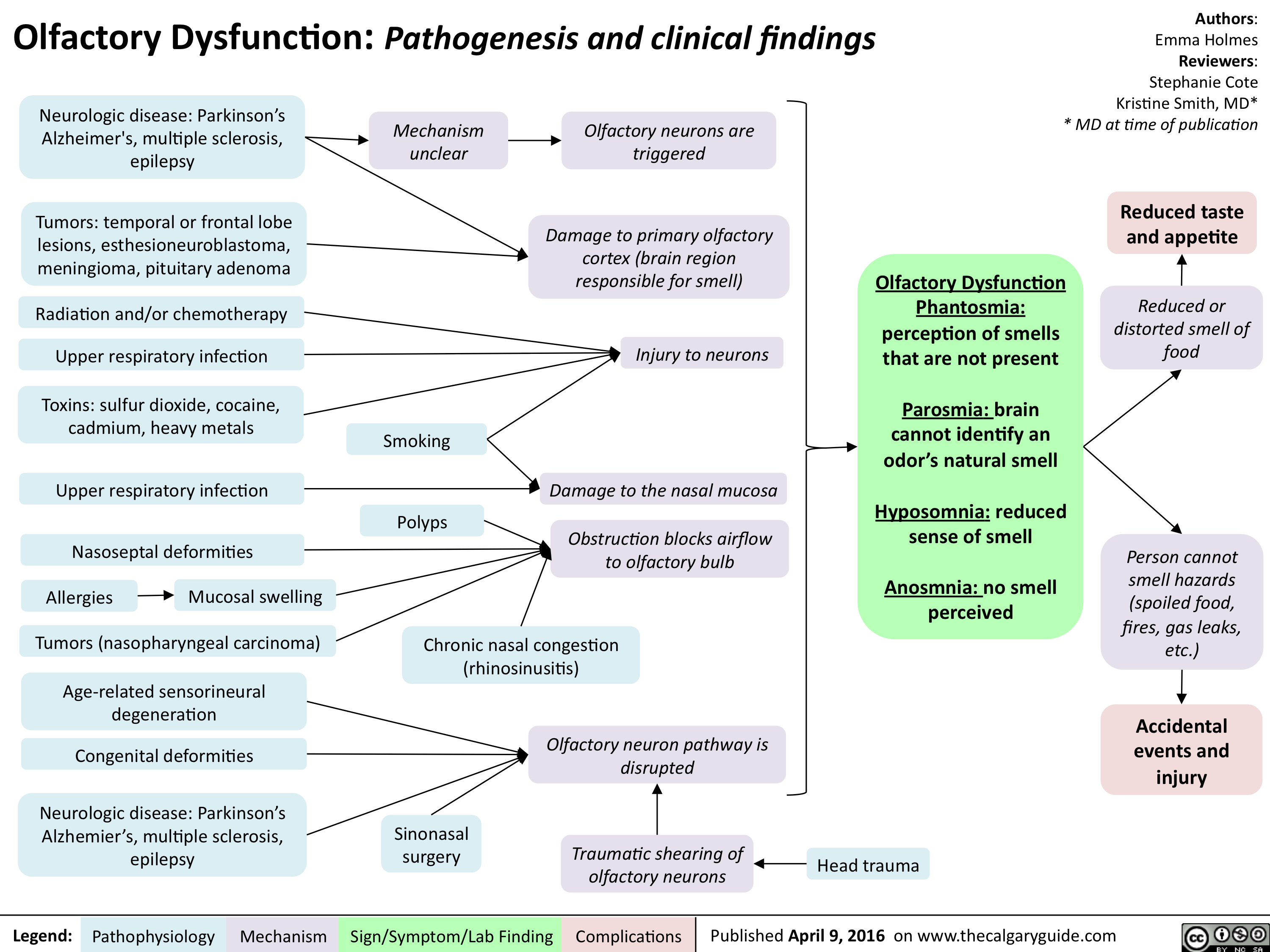
Acute Otitis Externa
Psoriasis: Pathogenesis and clinical findings

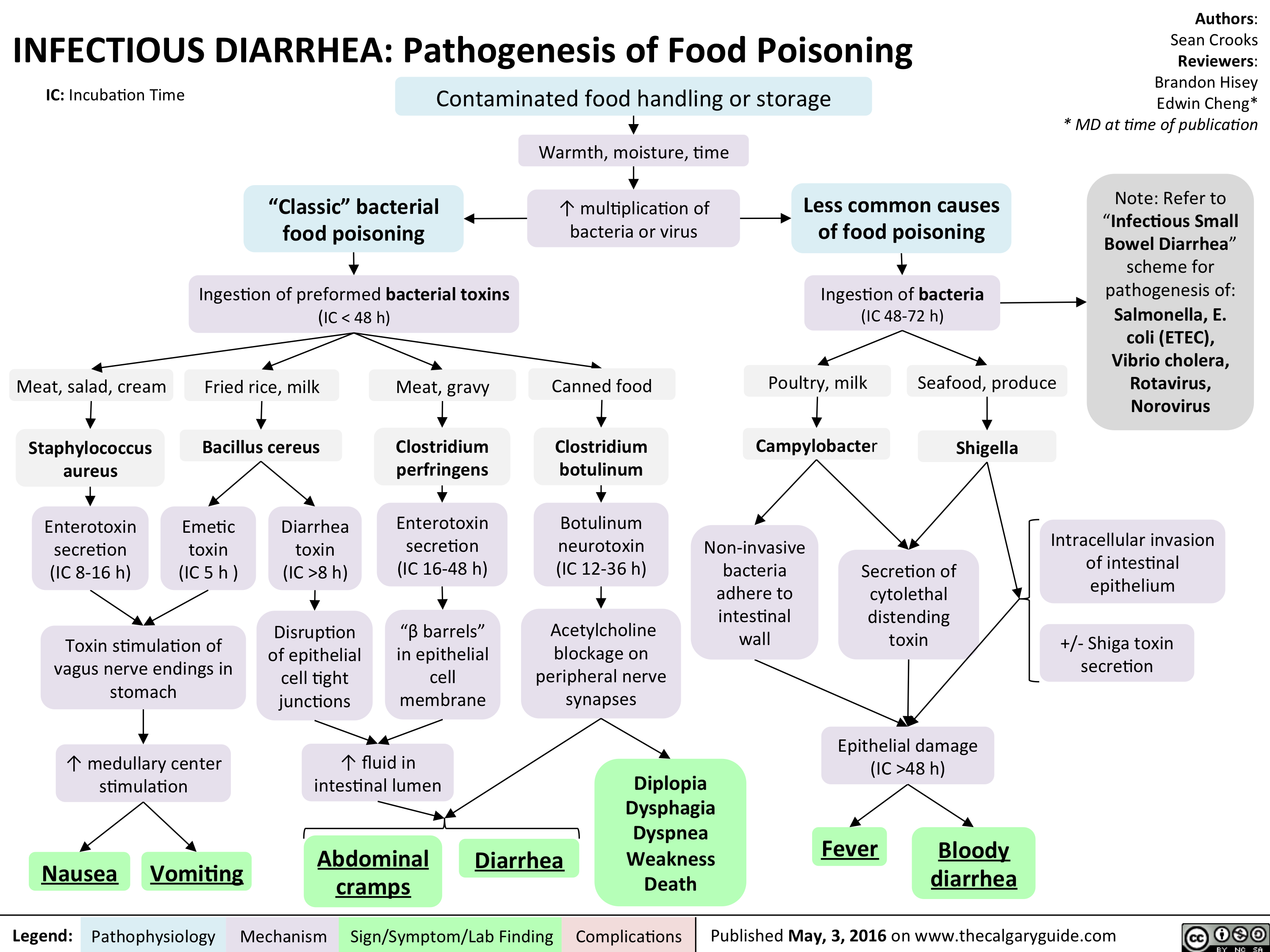
InfectiousFoodPoisoning
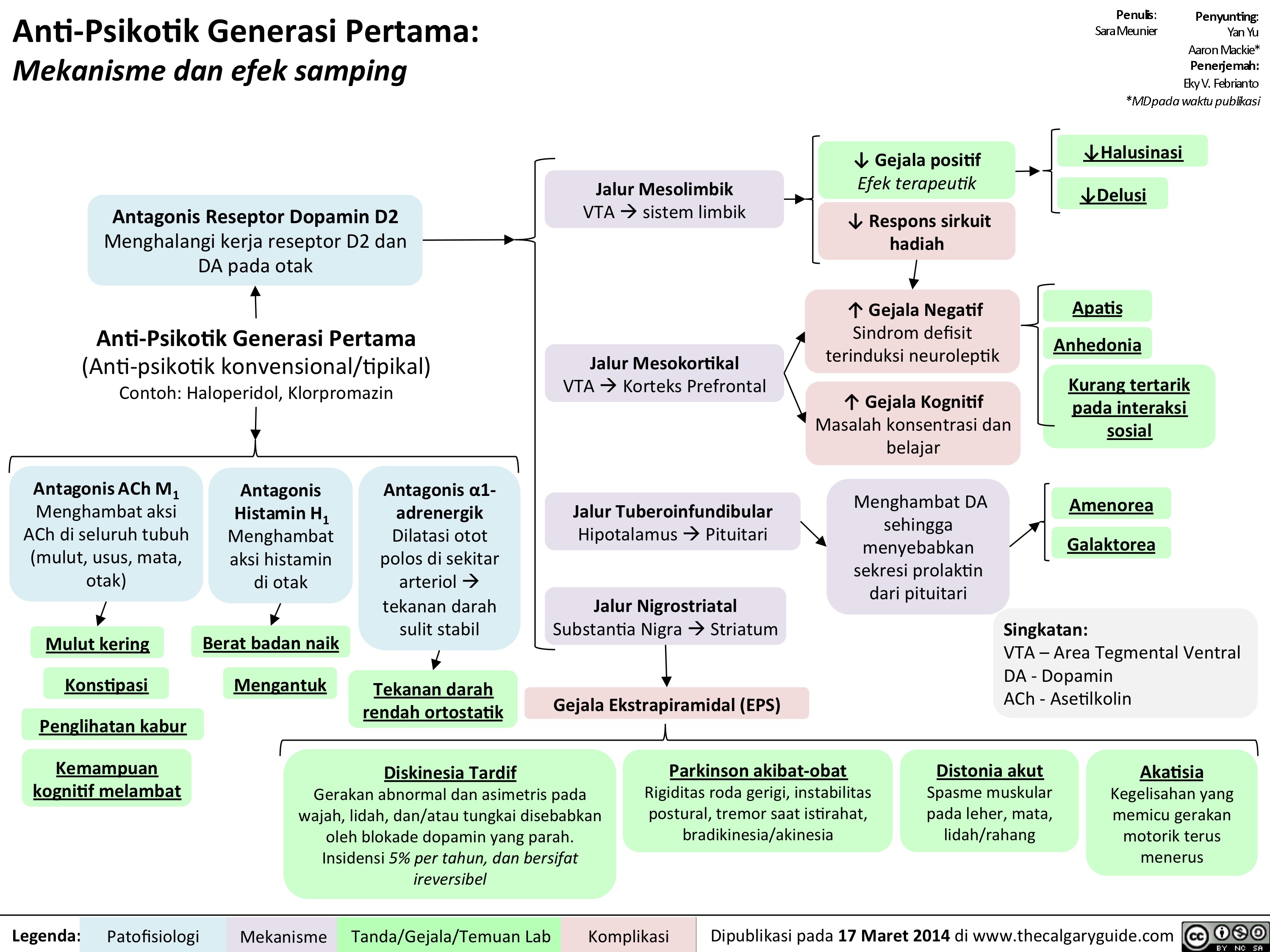
1st gen antipsychotics Translated
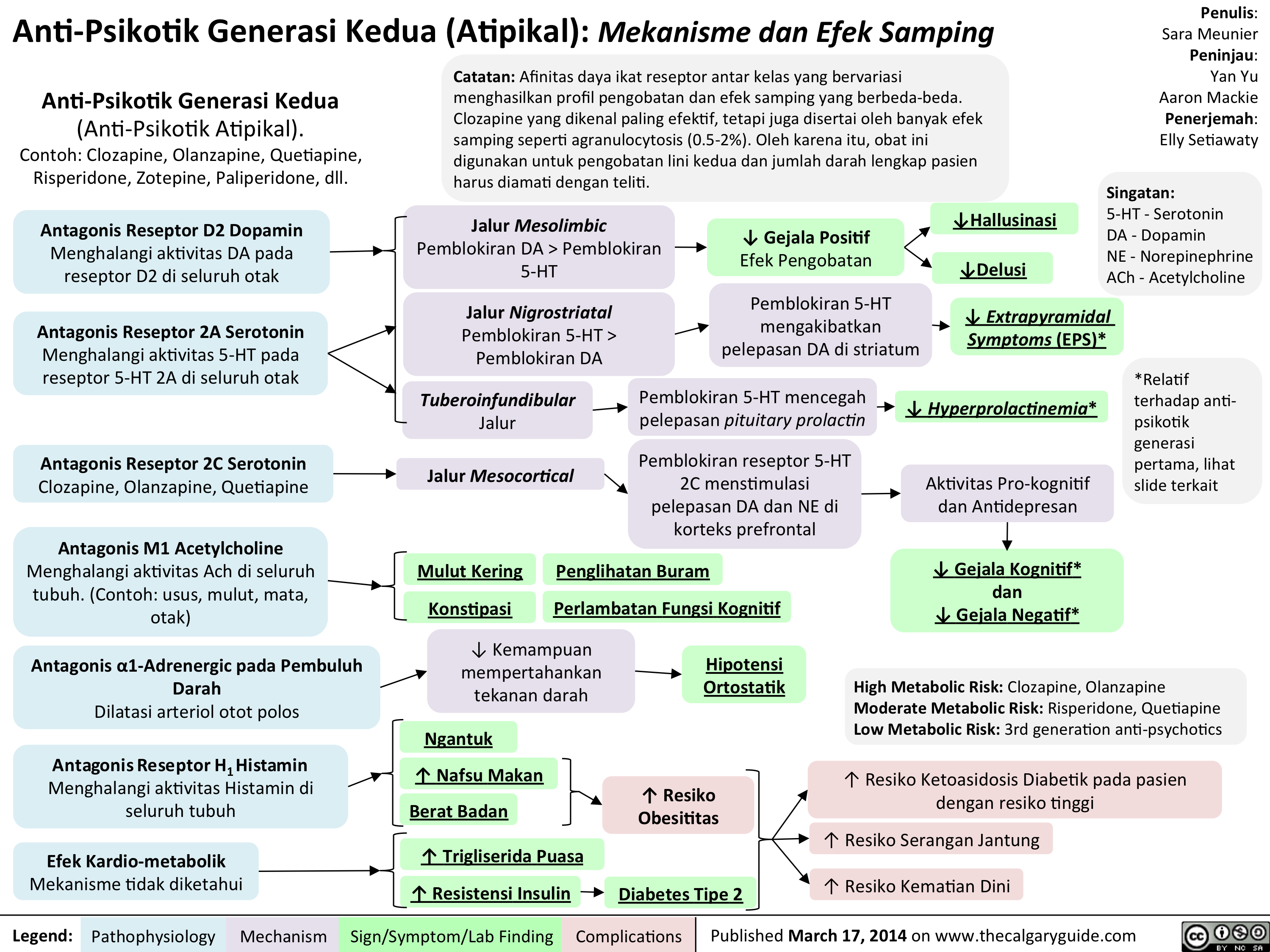
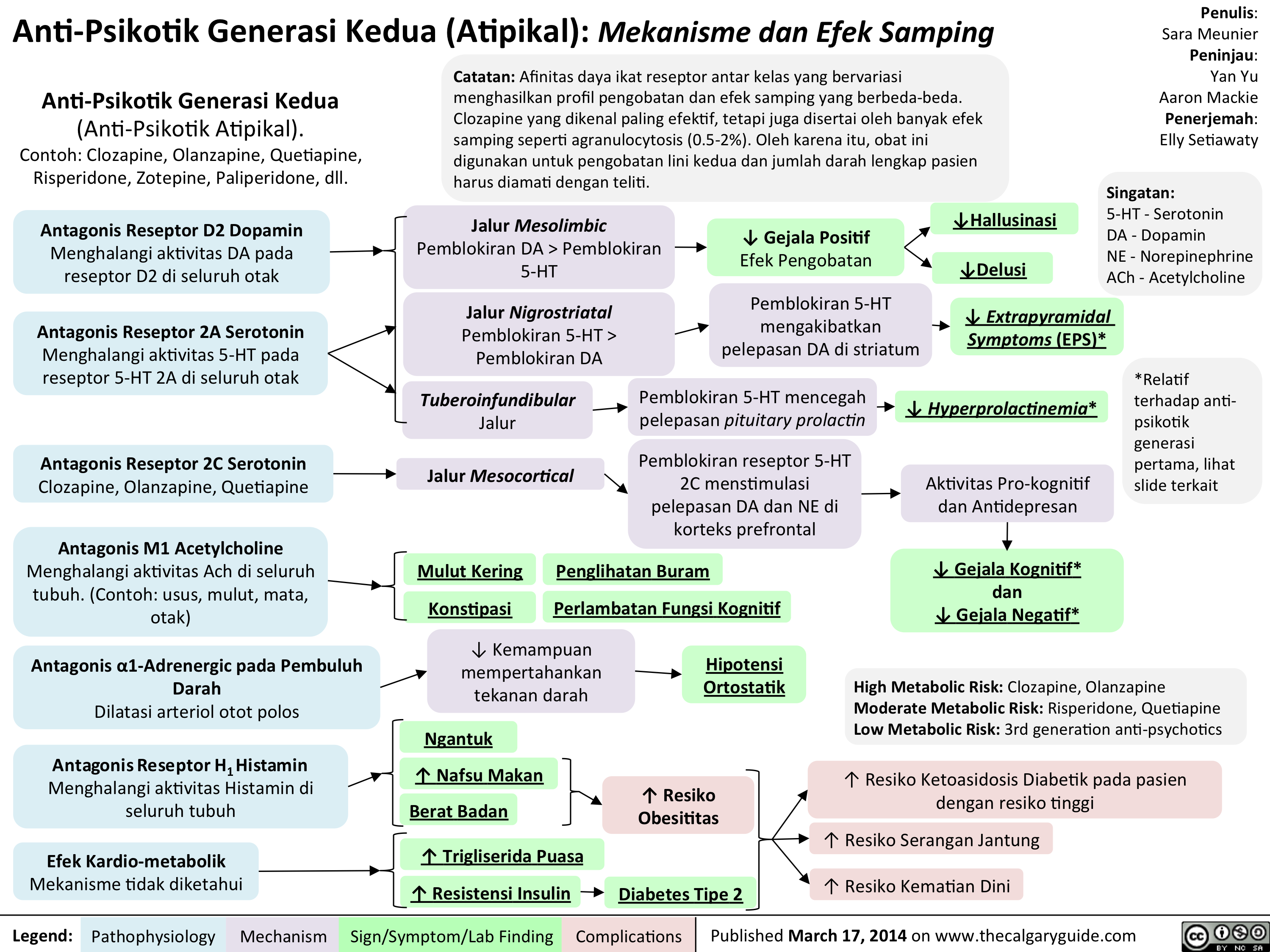
Anti-Psikotik Generasi Kedua: Mekanisme dan Efek Samping
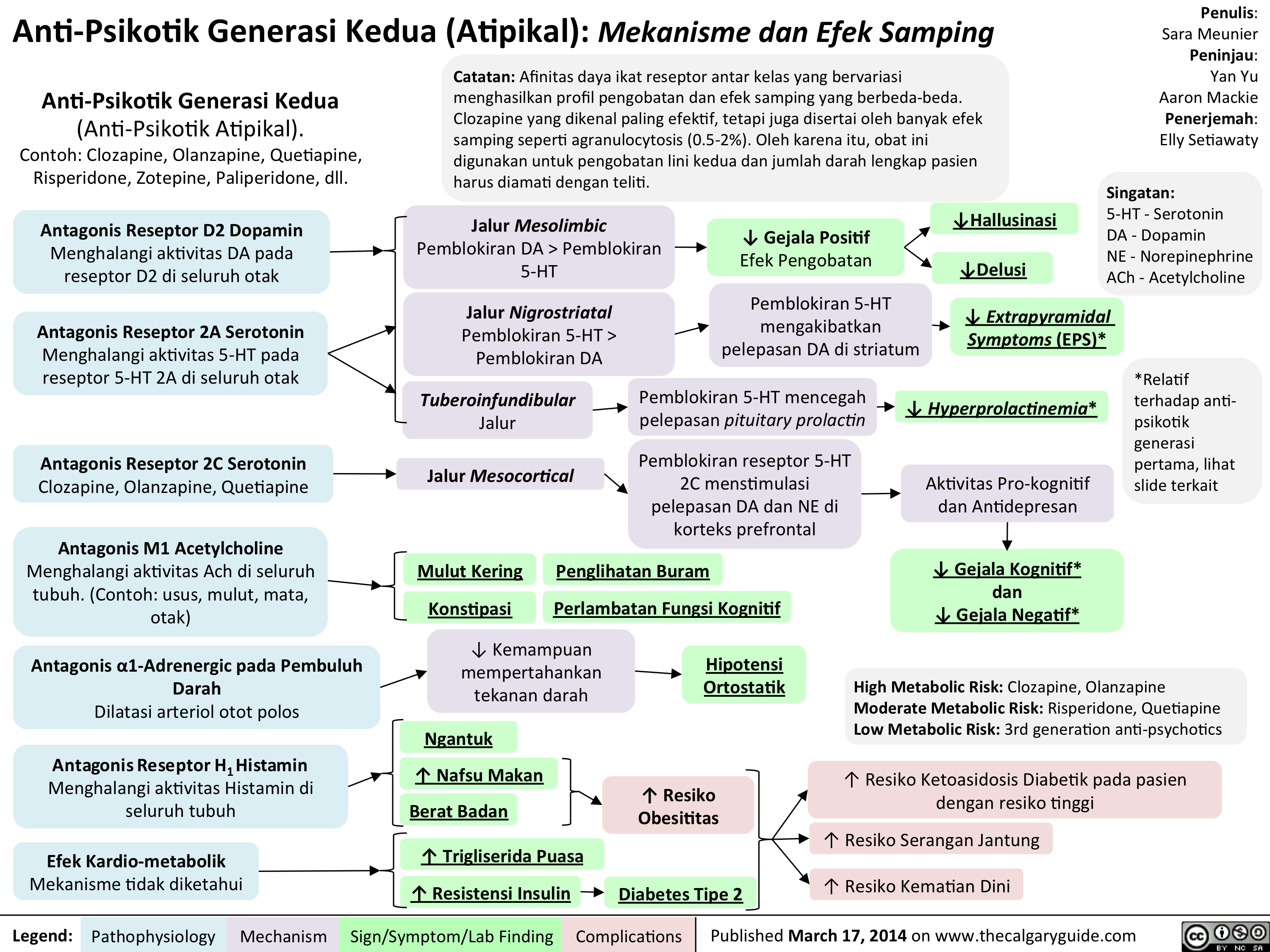
2nd generation antipsychotics Translated
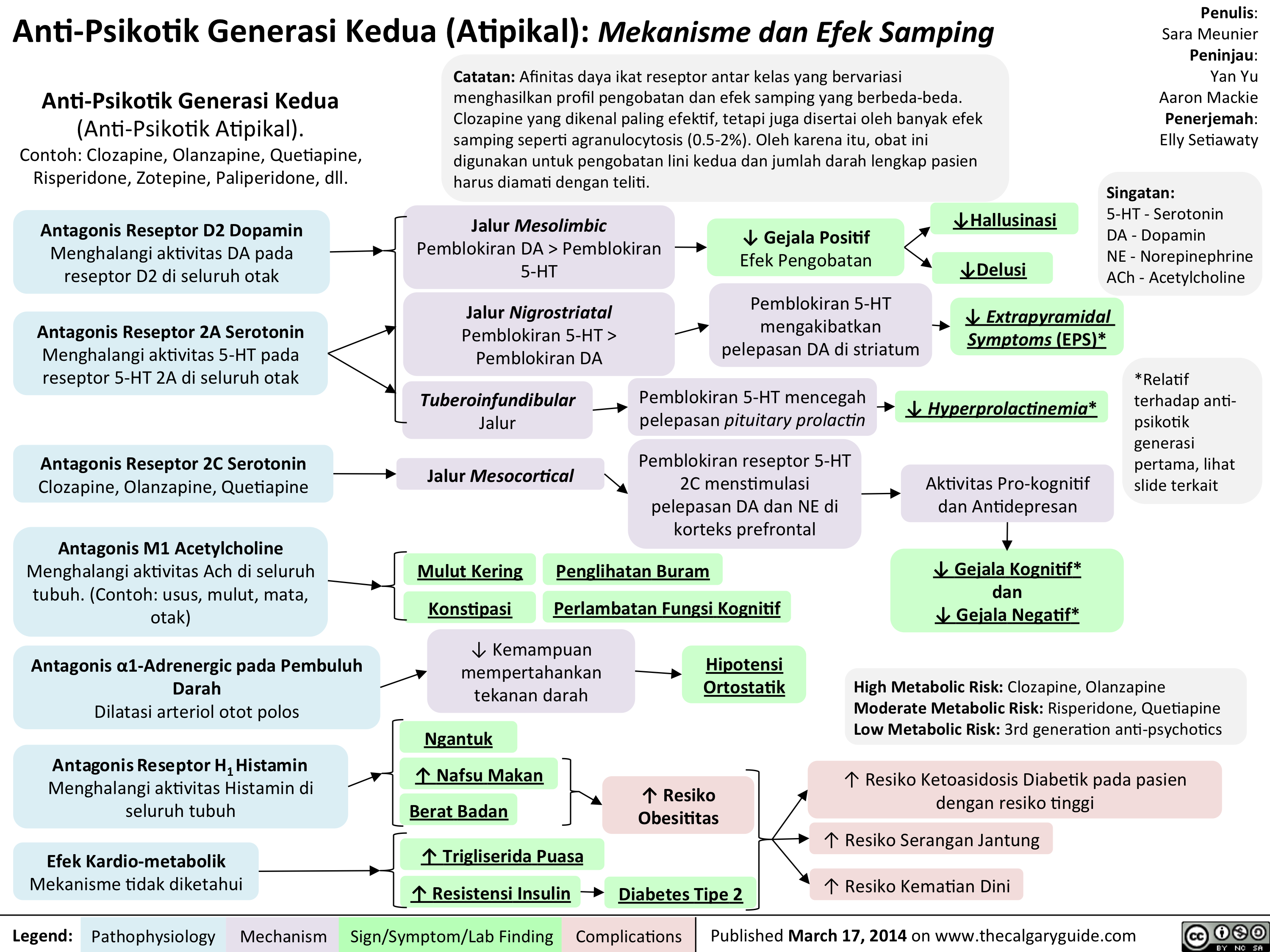
Anti-Psikotik Generasi Kedua (Atipikal): Mekanisme dan Efek Samping
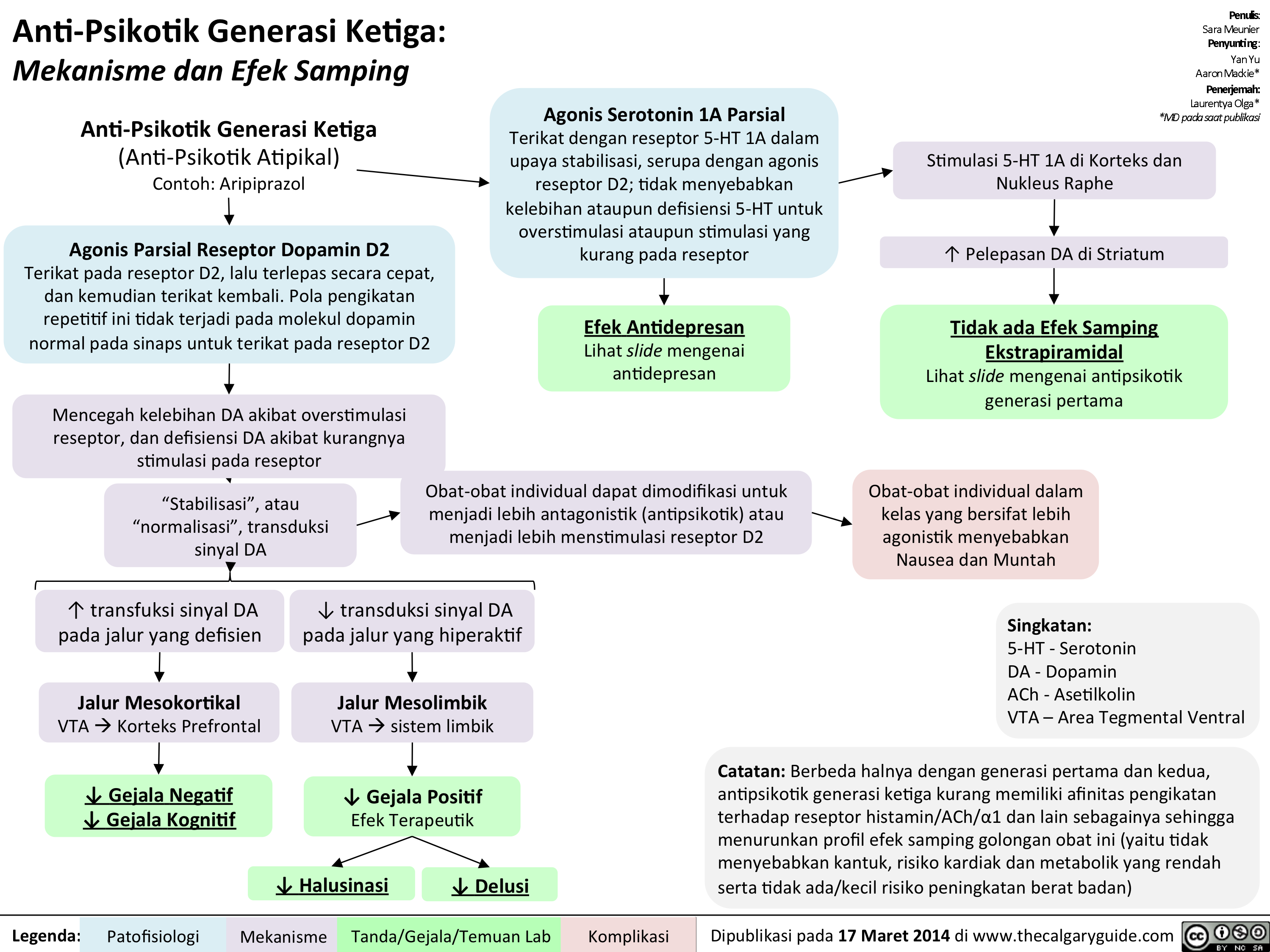
Anti-Psikotik Generasi Ketiga: Mekanisme dan Efek Samping
1st gen antipsychotics Translated
2nd generation antipsychotics Translated
1st gen antipsychotics Translated
3rd gen anti-psychotics Translated
Schizophrenia Pathogenesis Translated
Pathogenesis of Anxiety Disorders Translated
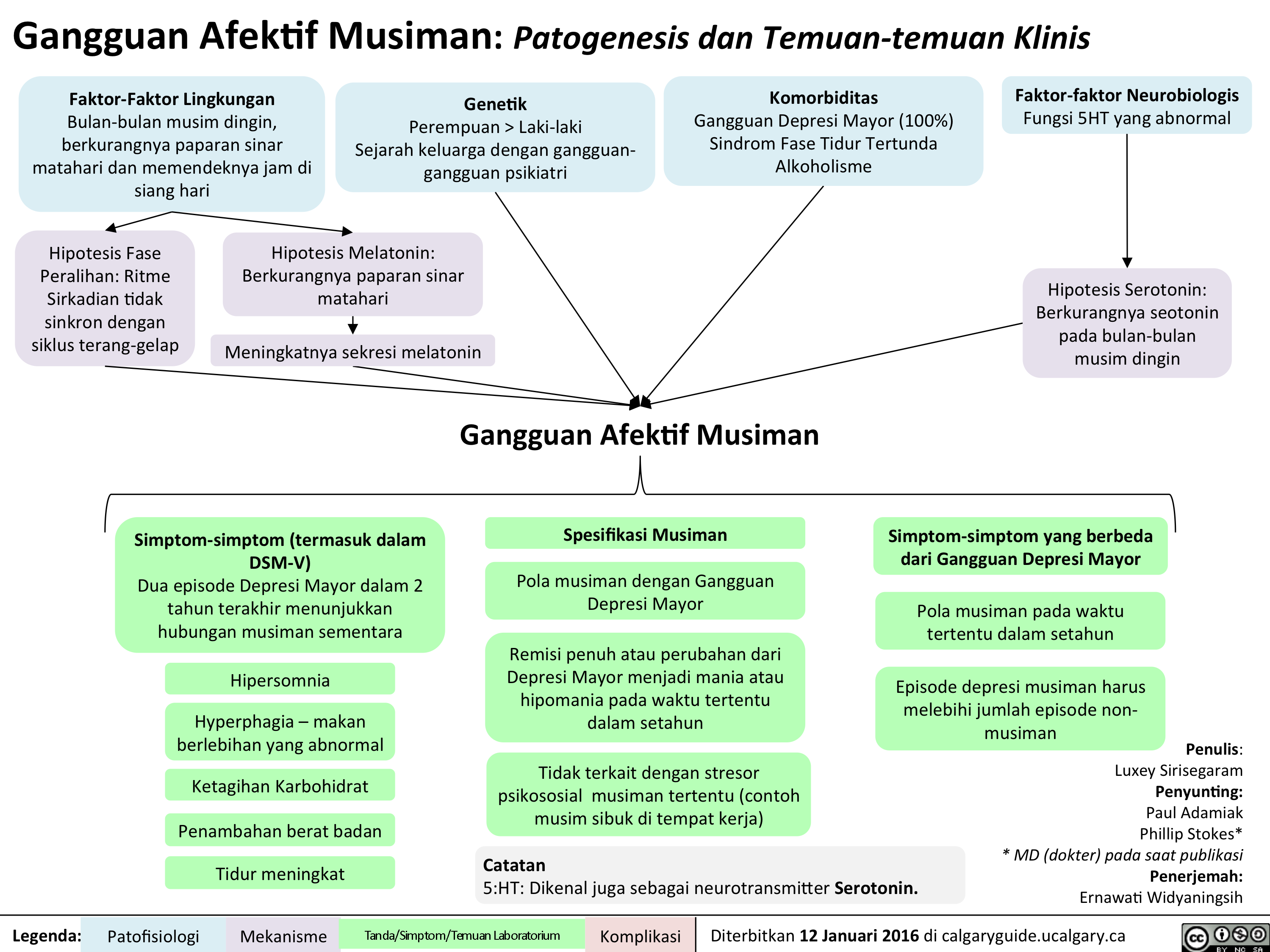
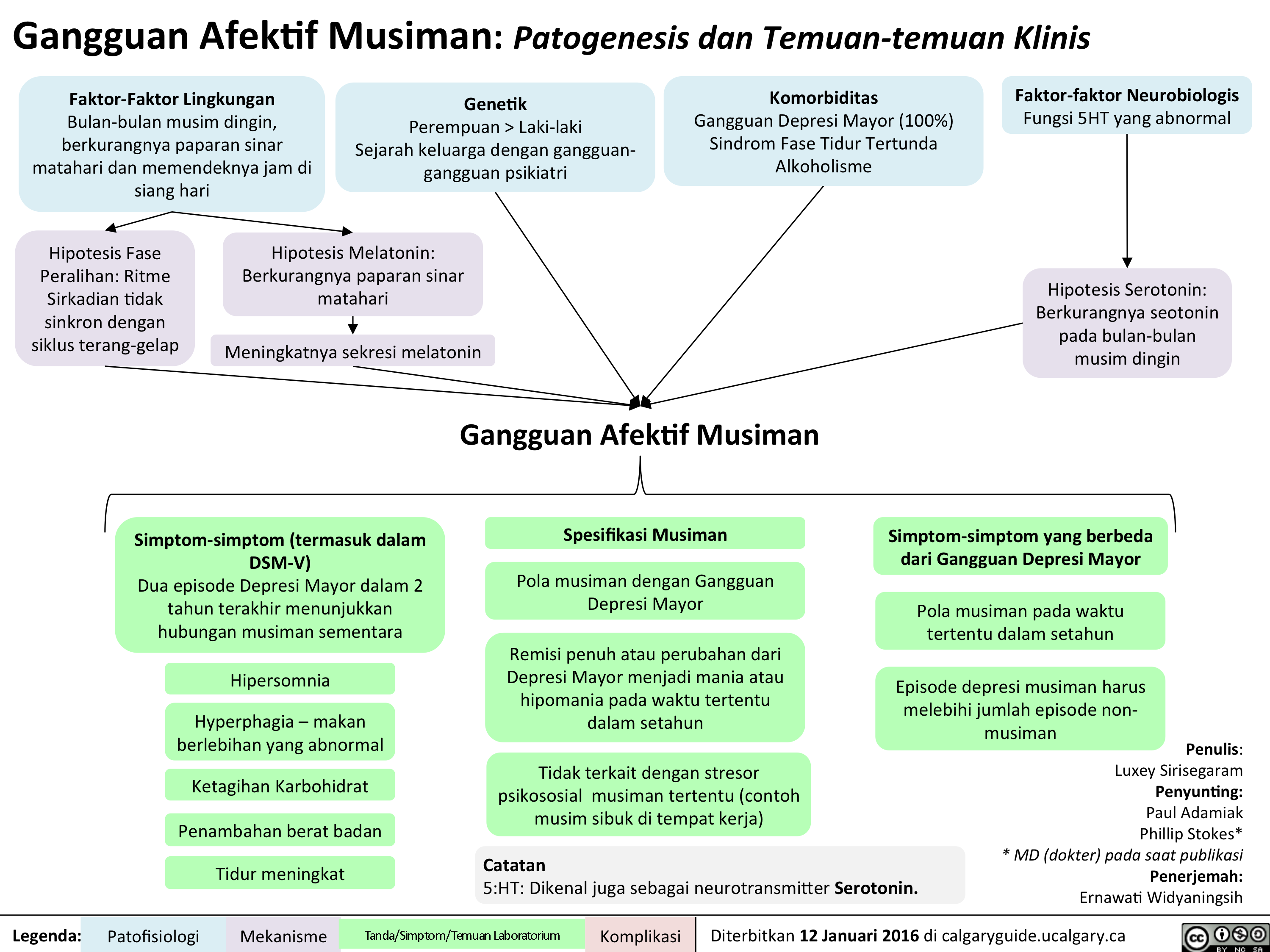
SAD Gangguan Afektif Musiman Translated
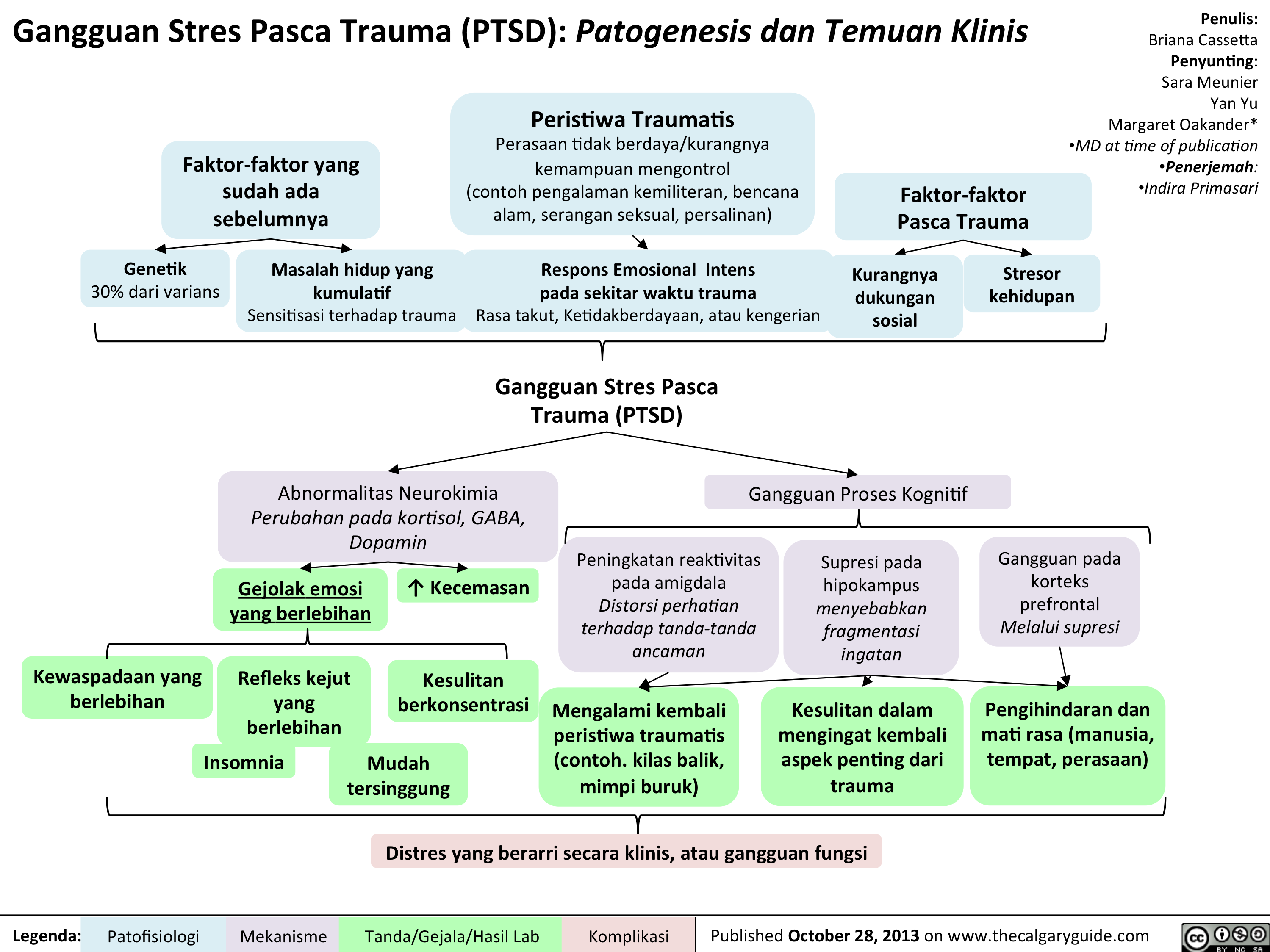
PTSD Translated
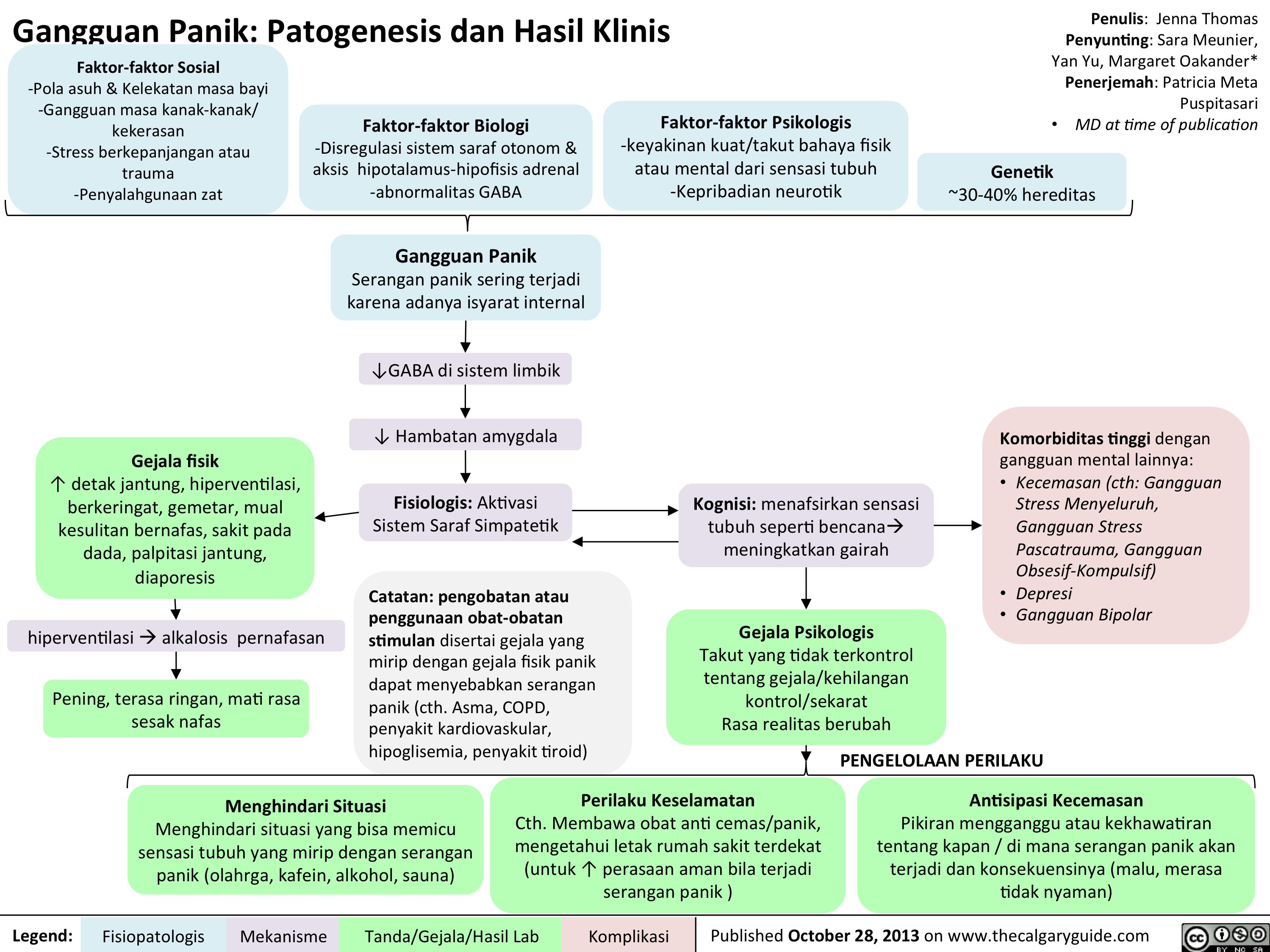
Panic Disorder Translated
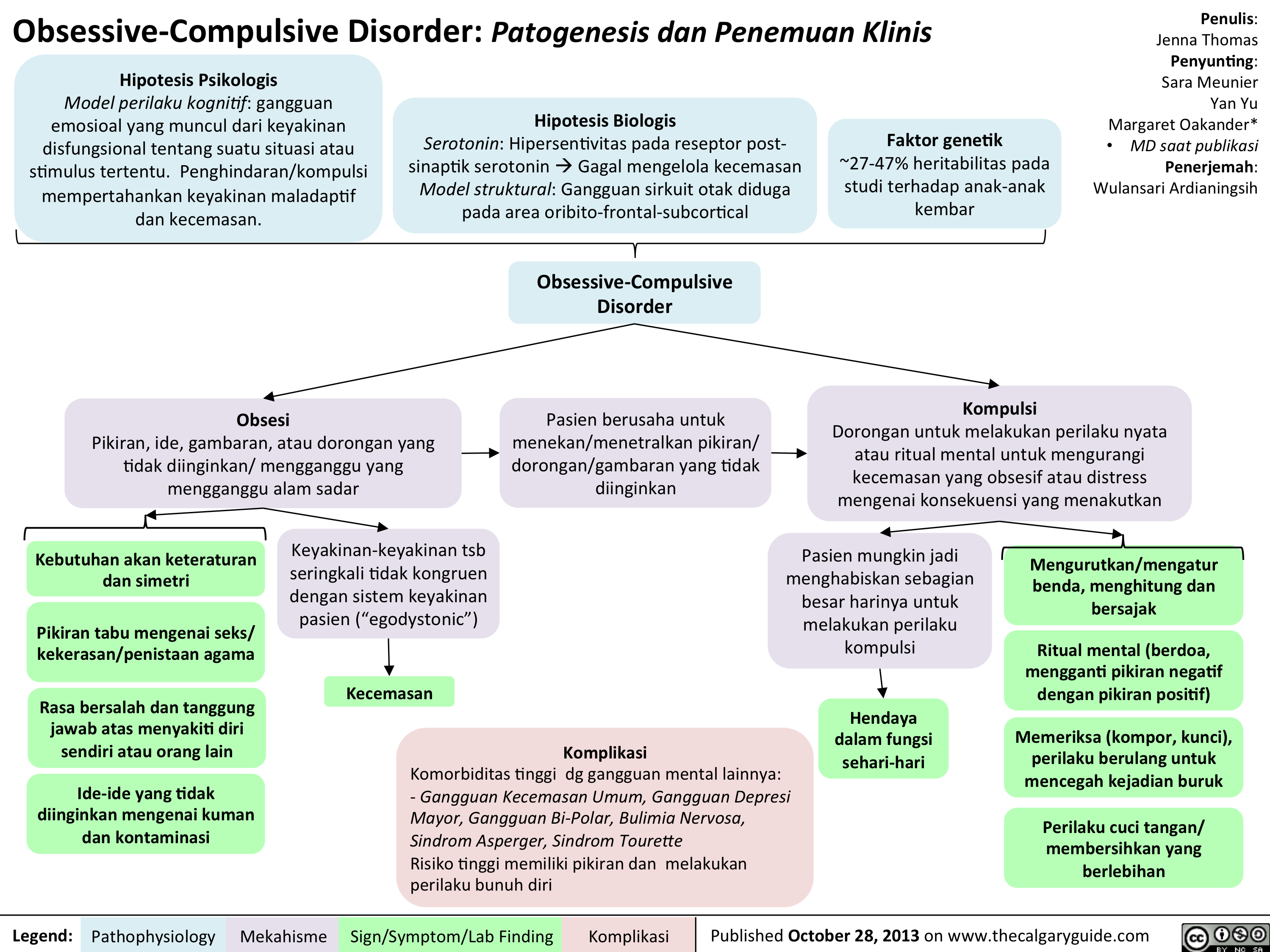
OCD Translated
Bipolar Disorder Translated

MDD Translated
SSRIs Translated
Bupropion Translated
SNRIs Translated
Thacker, J - Social Anxiety Translated
DSM - Axis to Formulation Translated
Alcohol Use Translated
Seasonal Affective Disorder: Pathogenesis and clinical findings
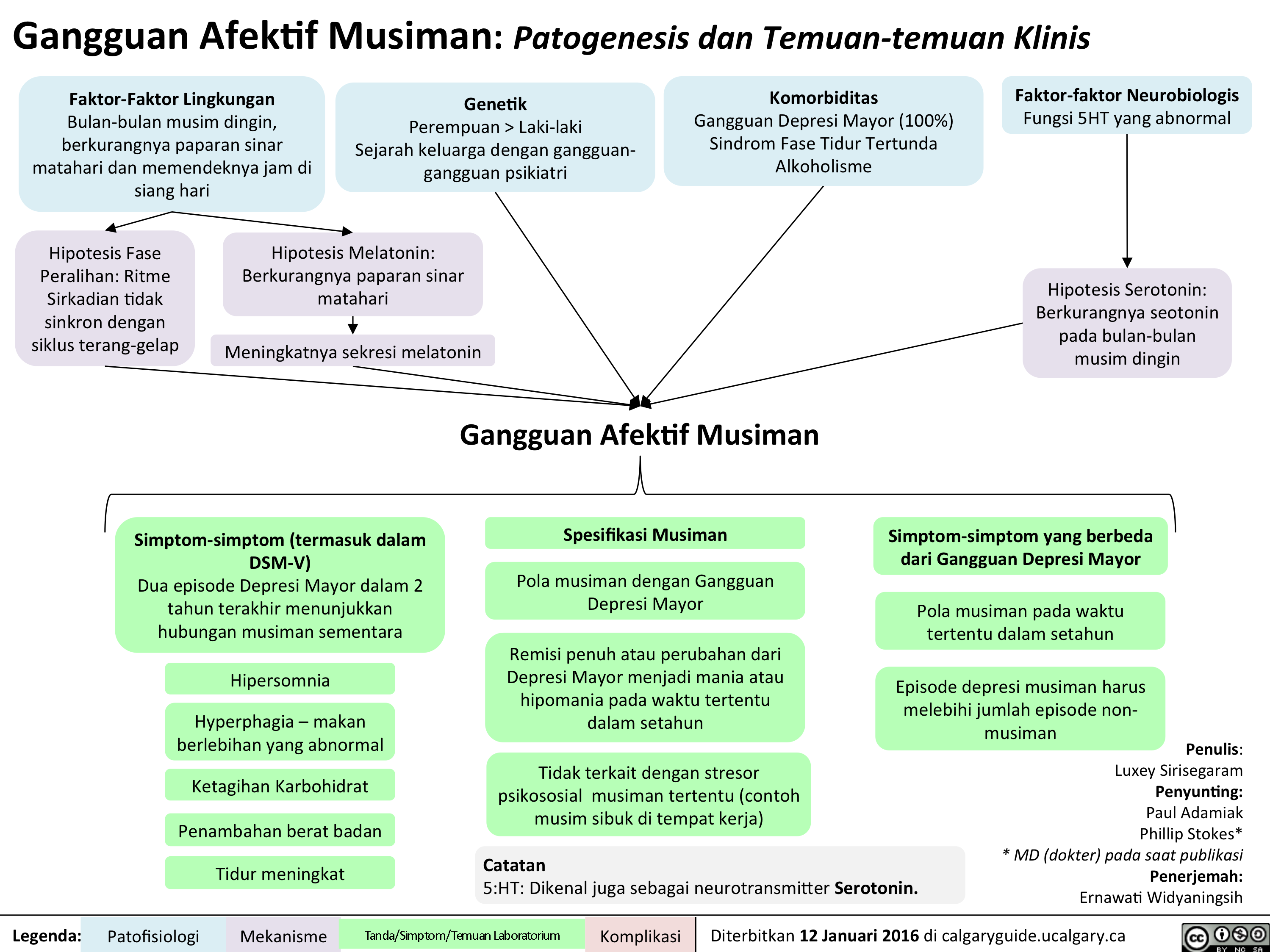
Seasonal Affective Disorder: Pathogenesis and clinical findings
Slide1
Slide1

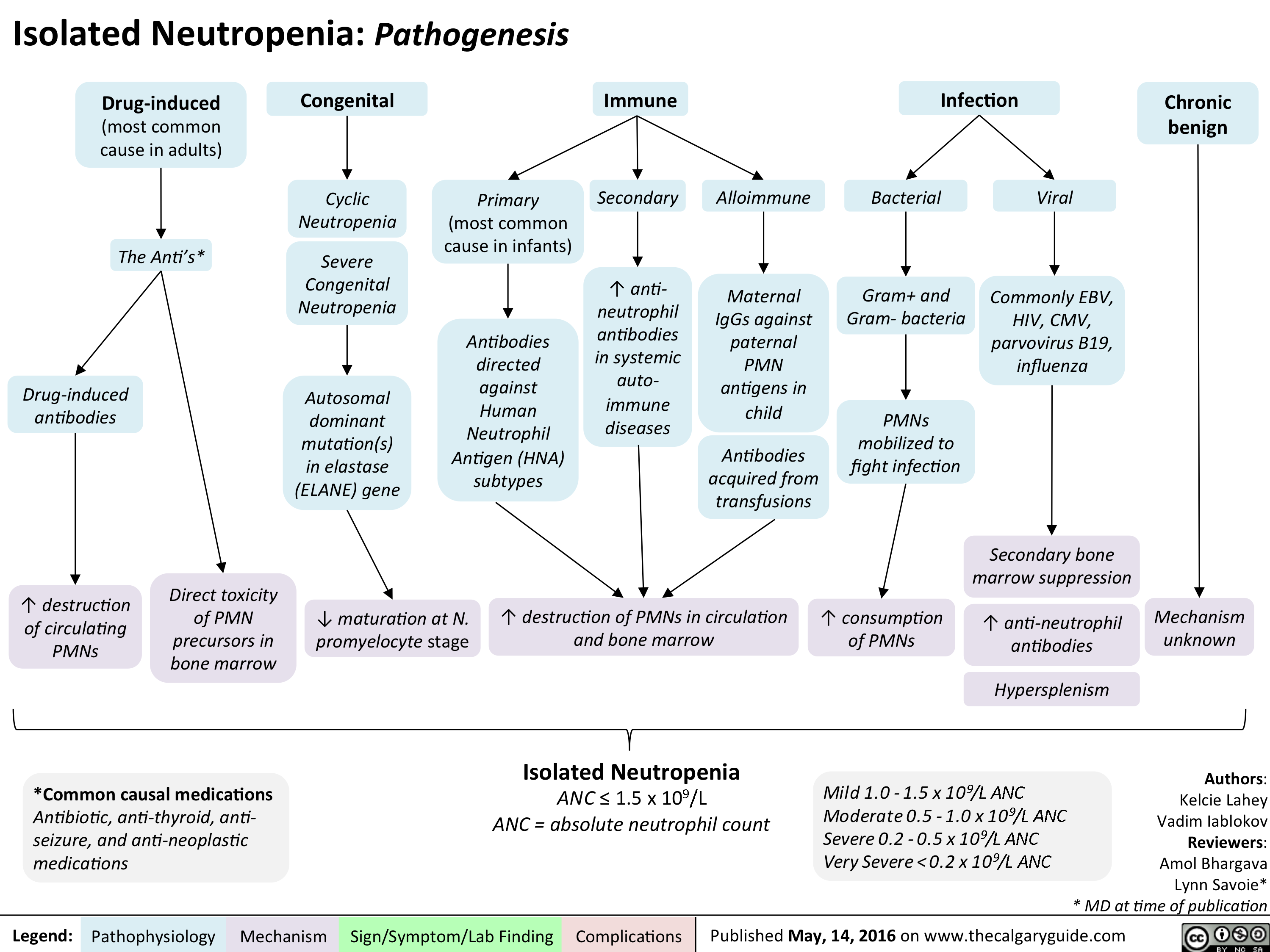
Isolated Neutropenia
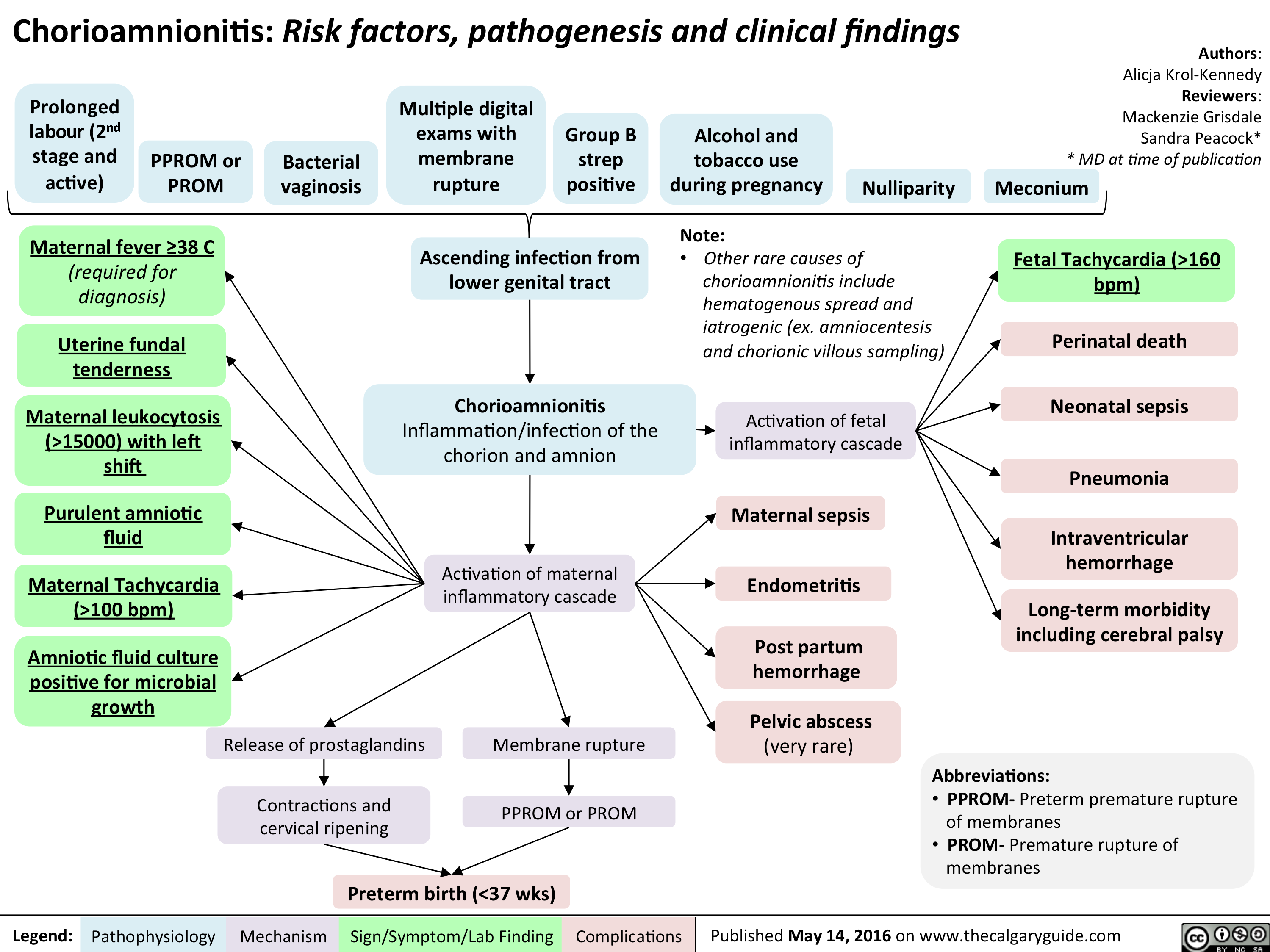
Chorioamnionitis: Risk factors, pathogenesis and clinical findings
Placental Complications During Labour
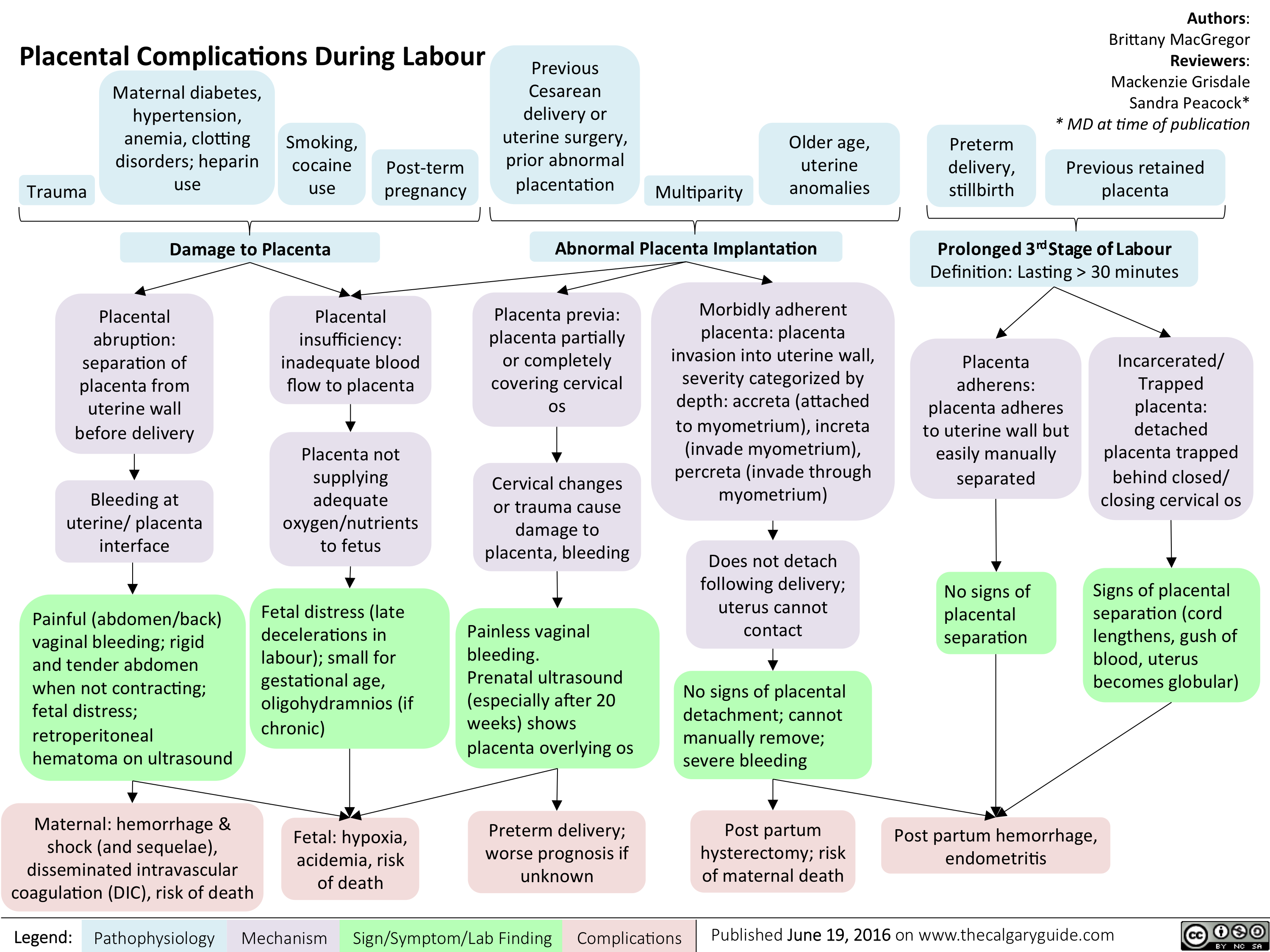
Placental Complications During Labour
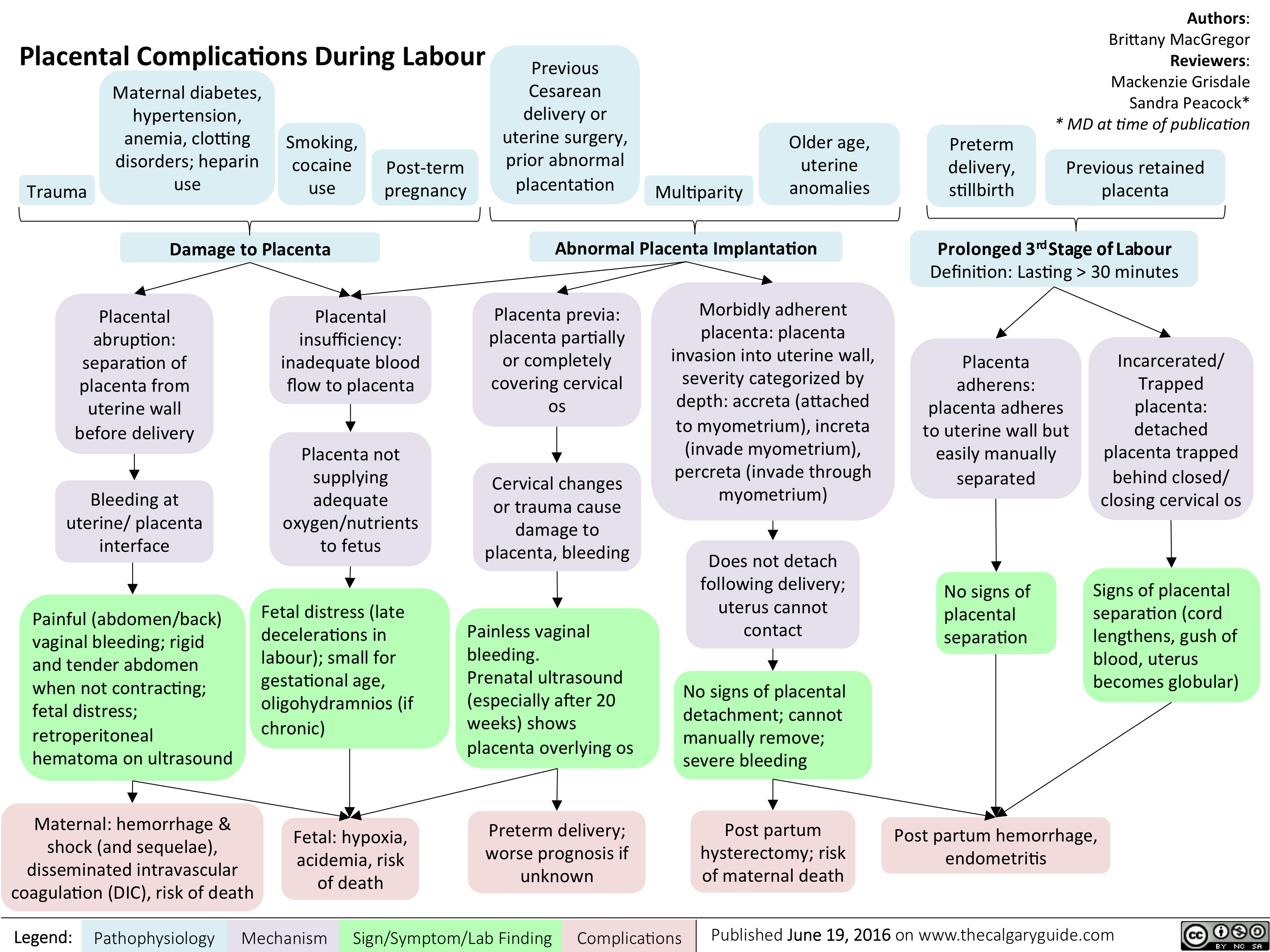
Acute Rheumatic Fever- Pathogenesis and Clinical Findings
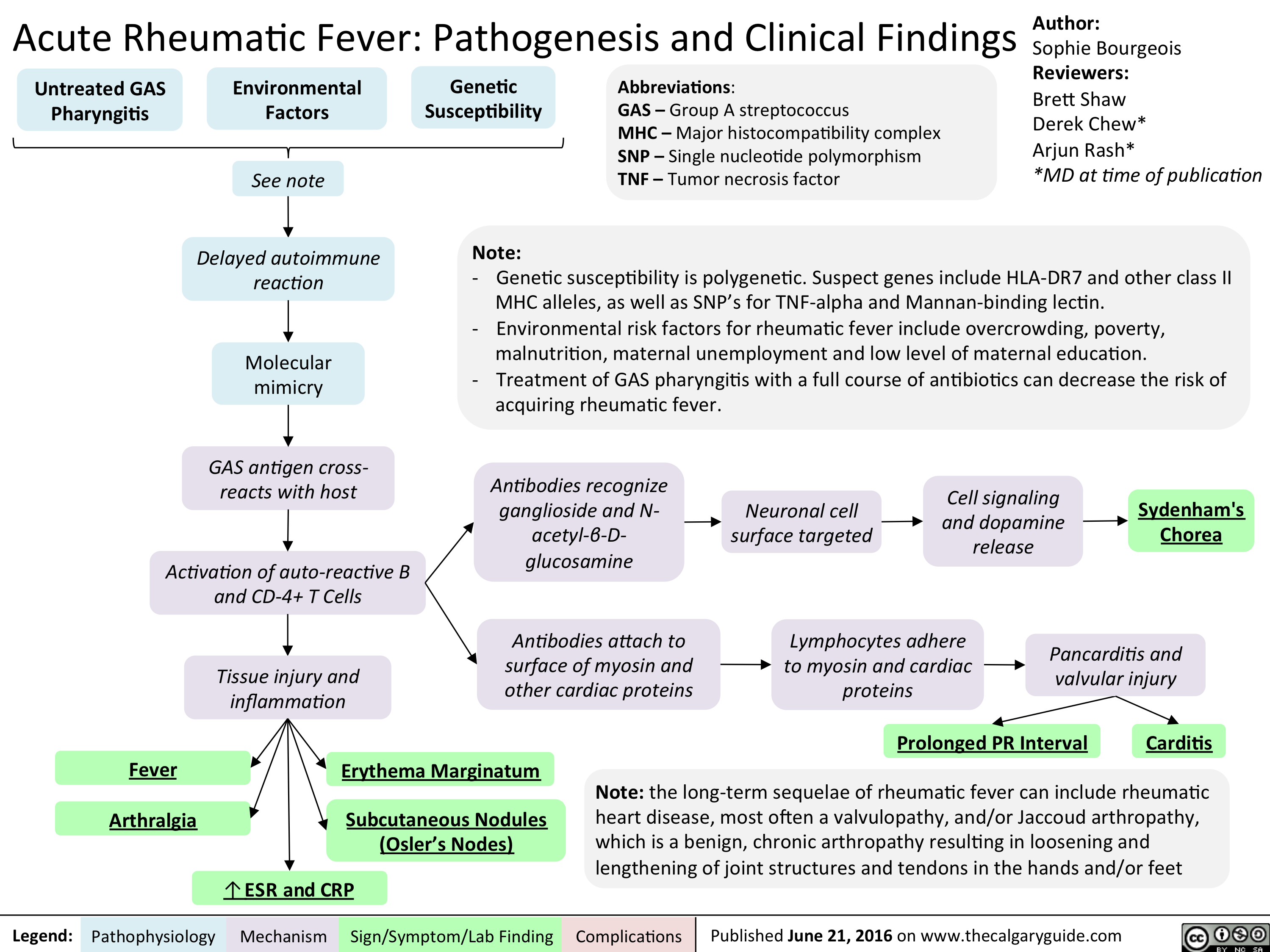
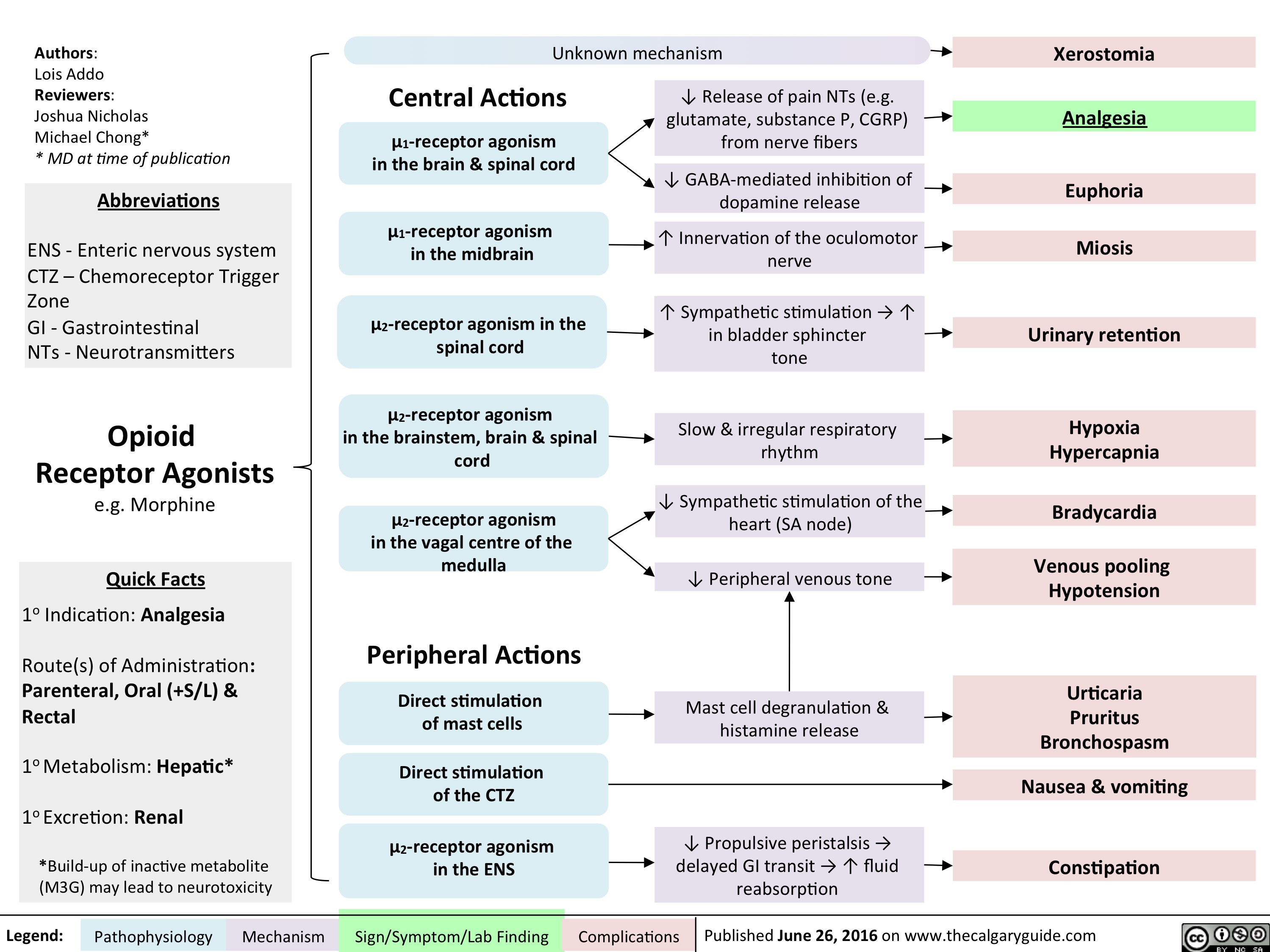
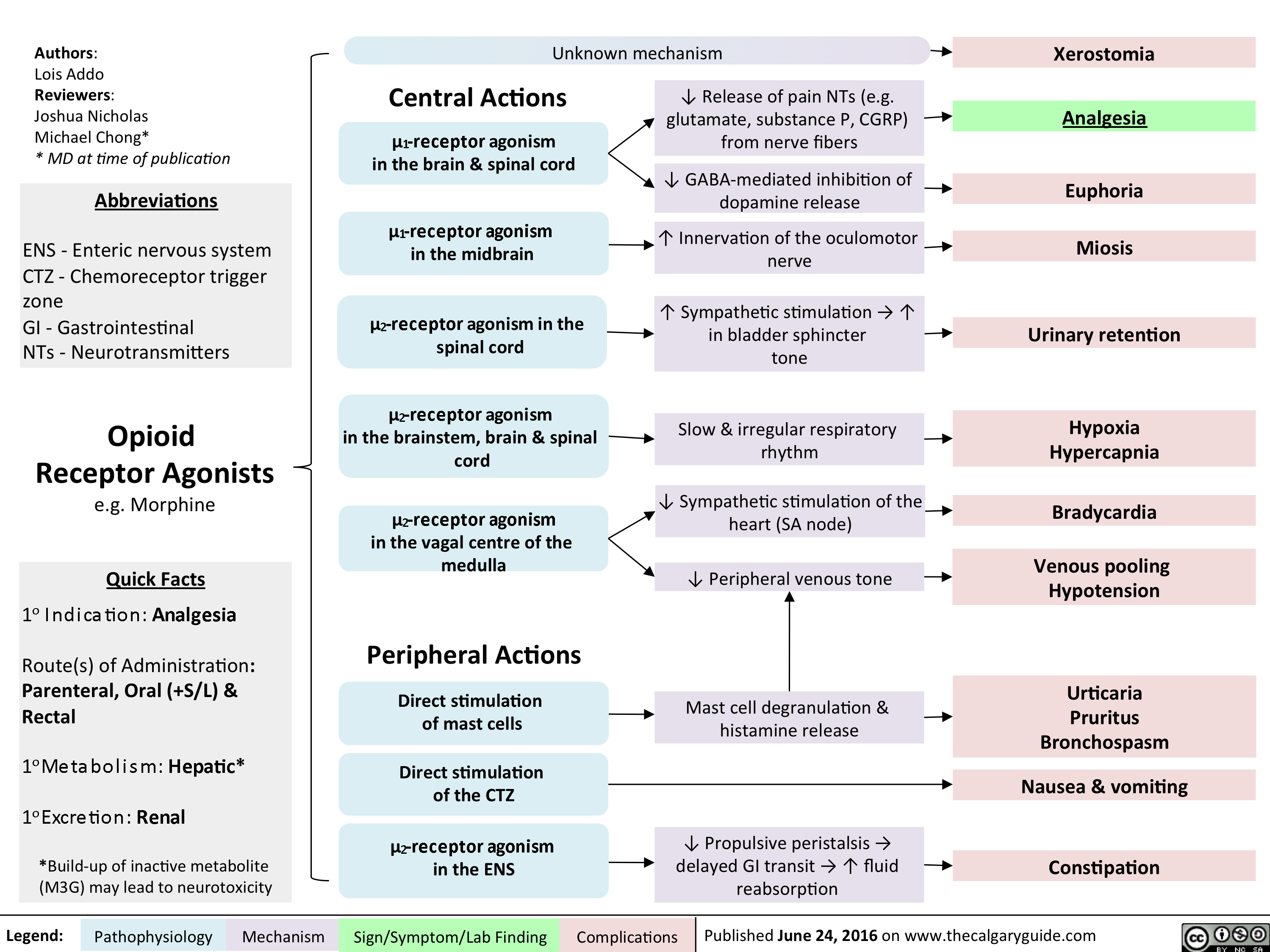
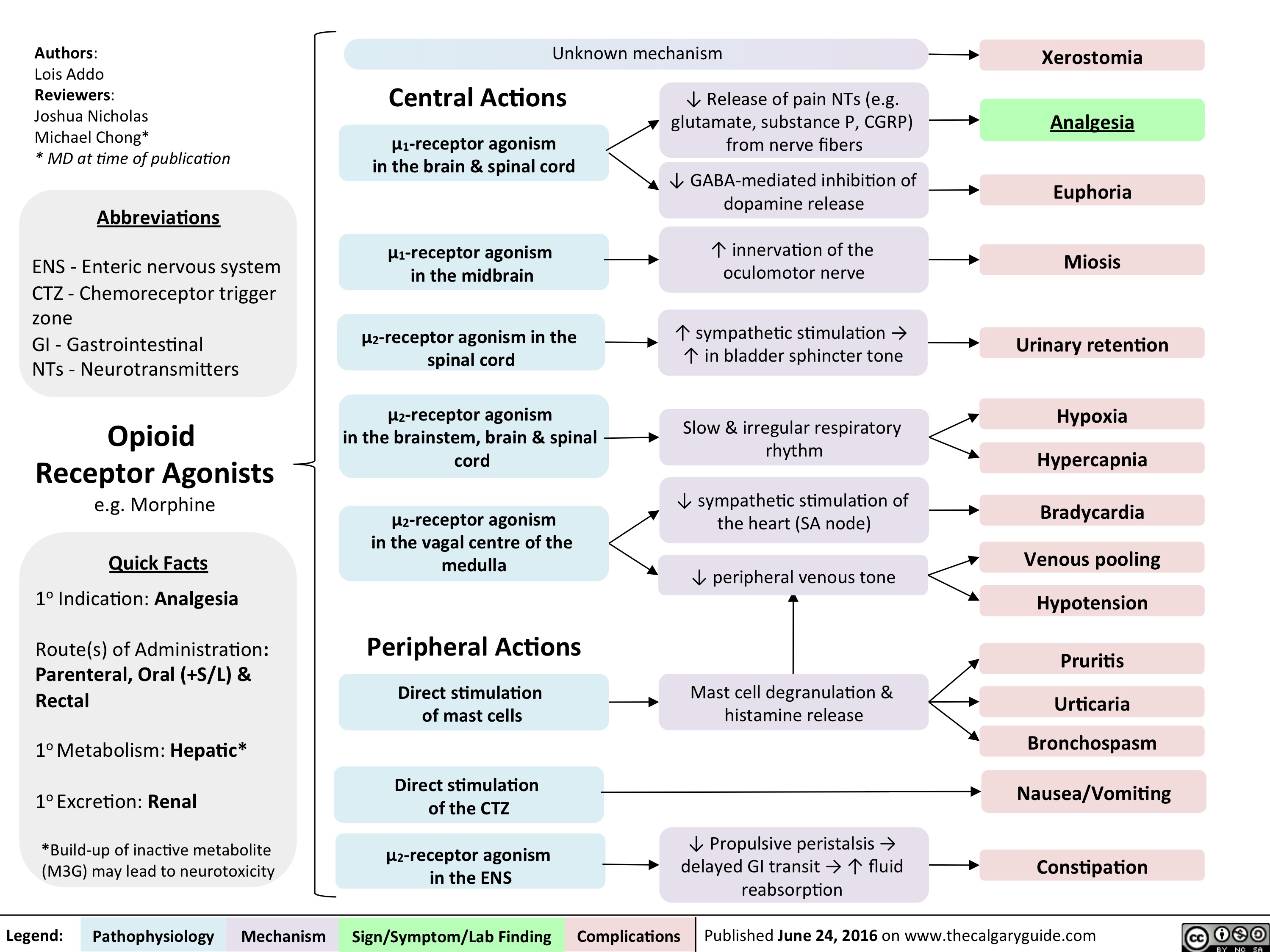
Opioid Receptor Agonists
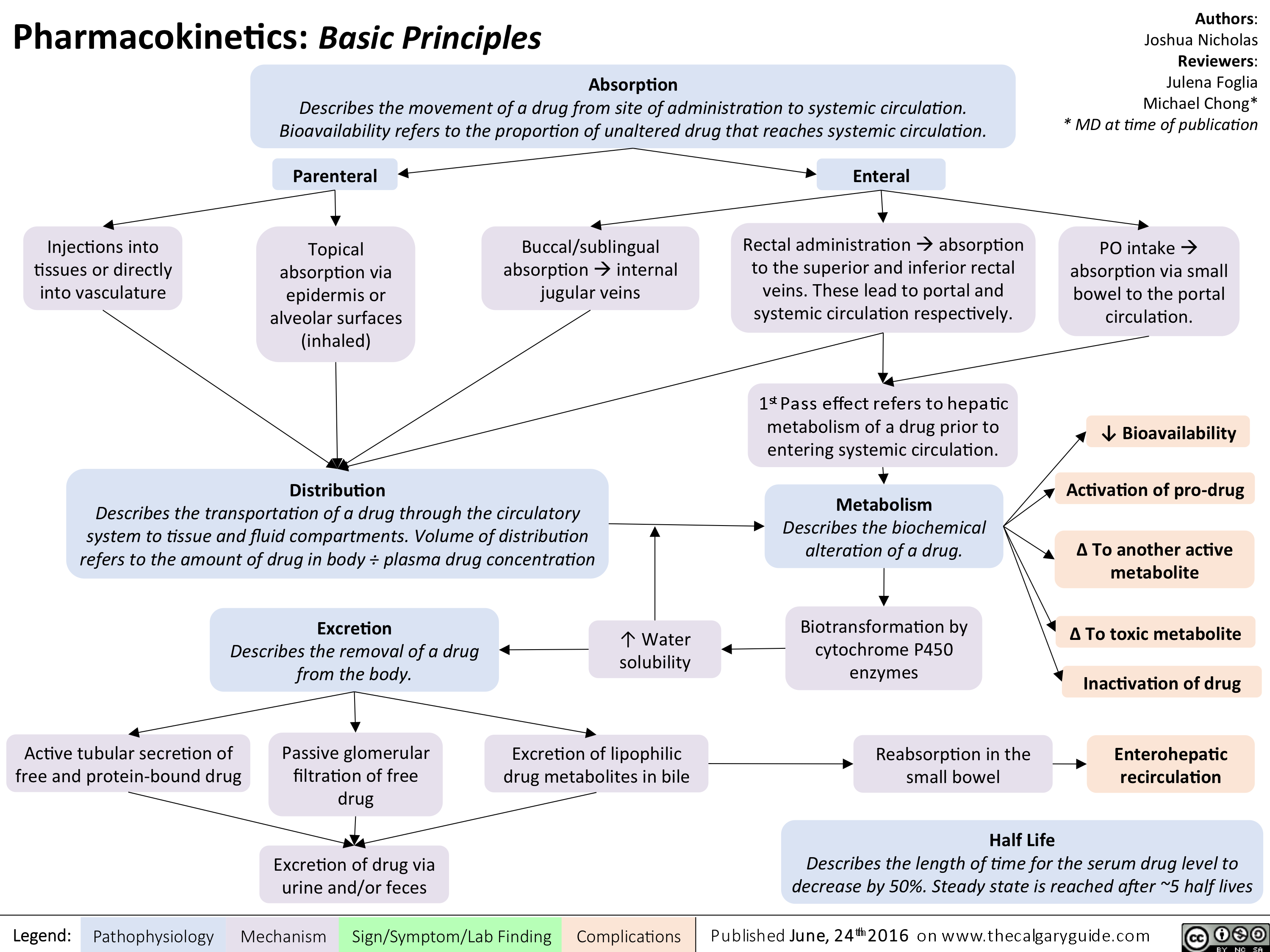
Pharmacokinetics Basic Principles
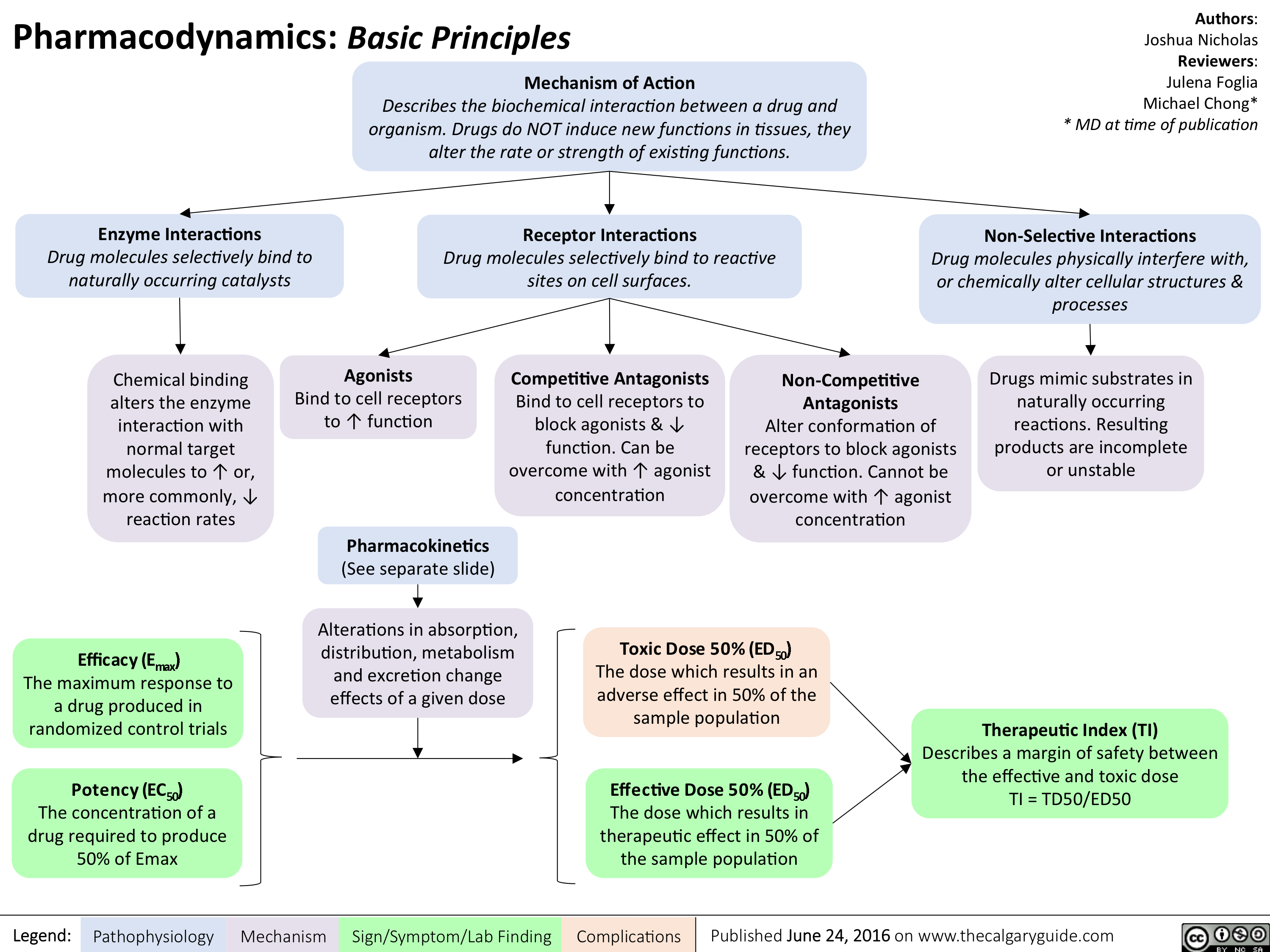
Pharmacodynamics Basic Principles
Opioid Receptor Agonists
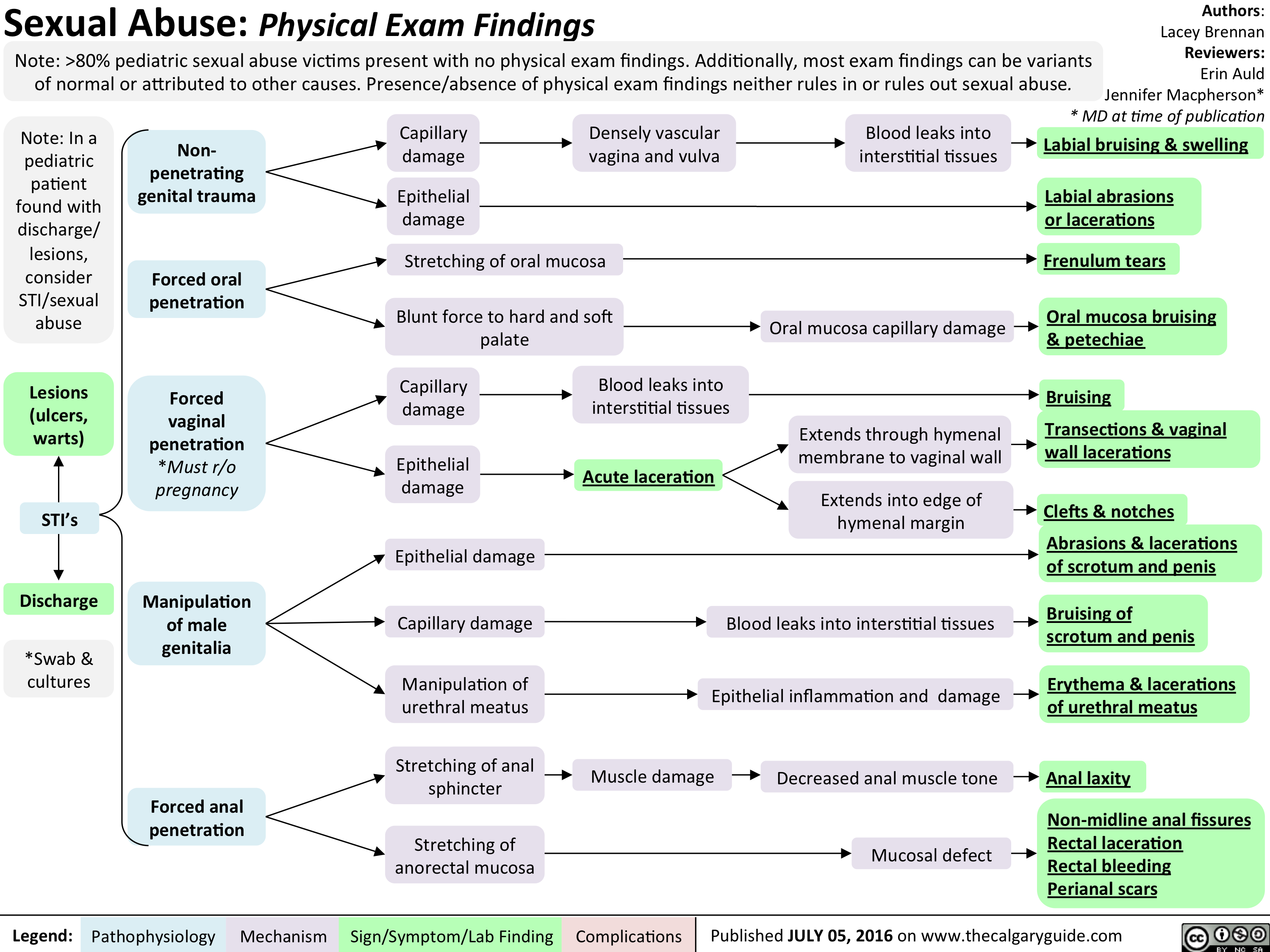
Peds Sexual Abuse
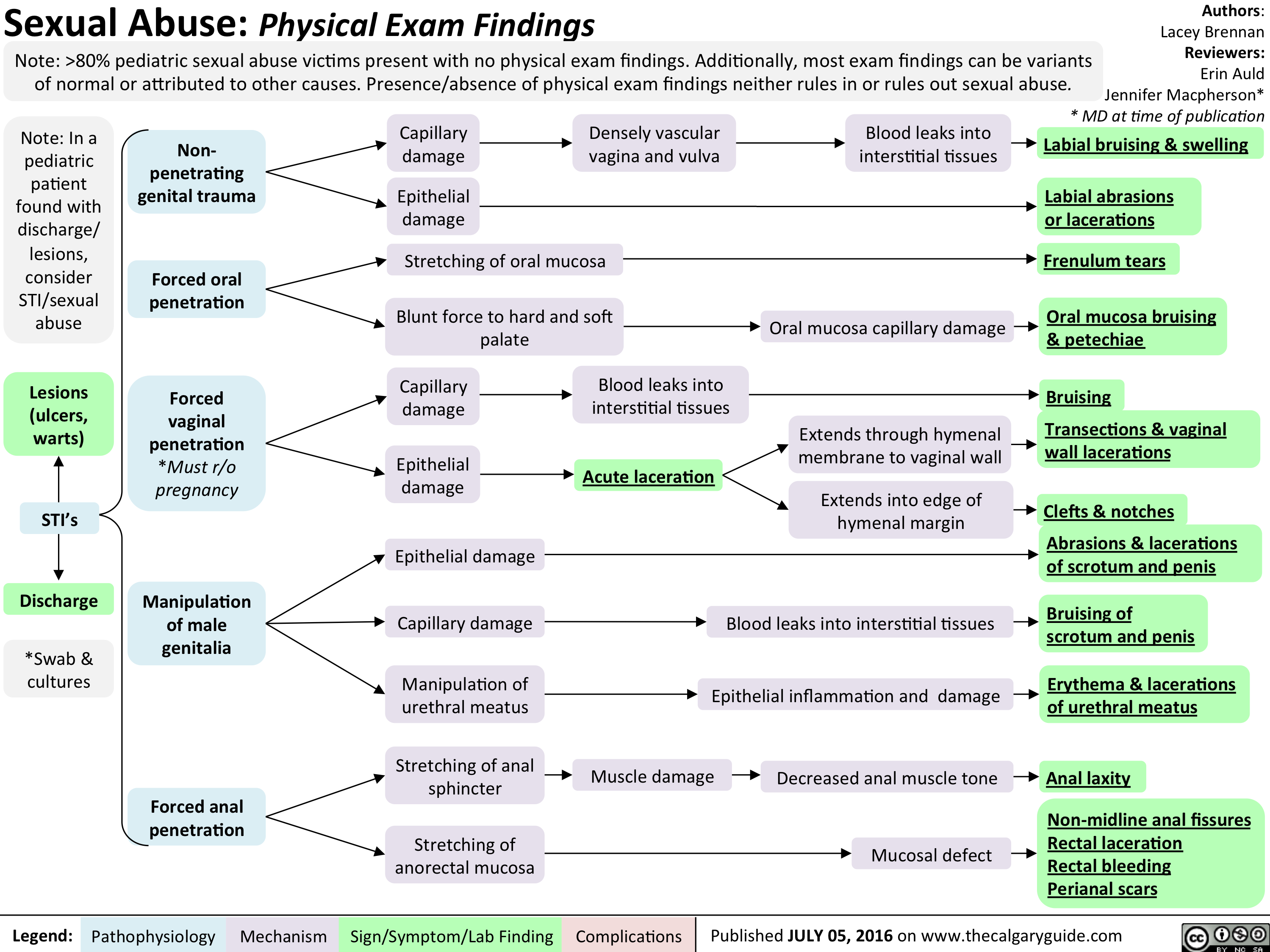
Peds Sexual Abuse
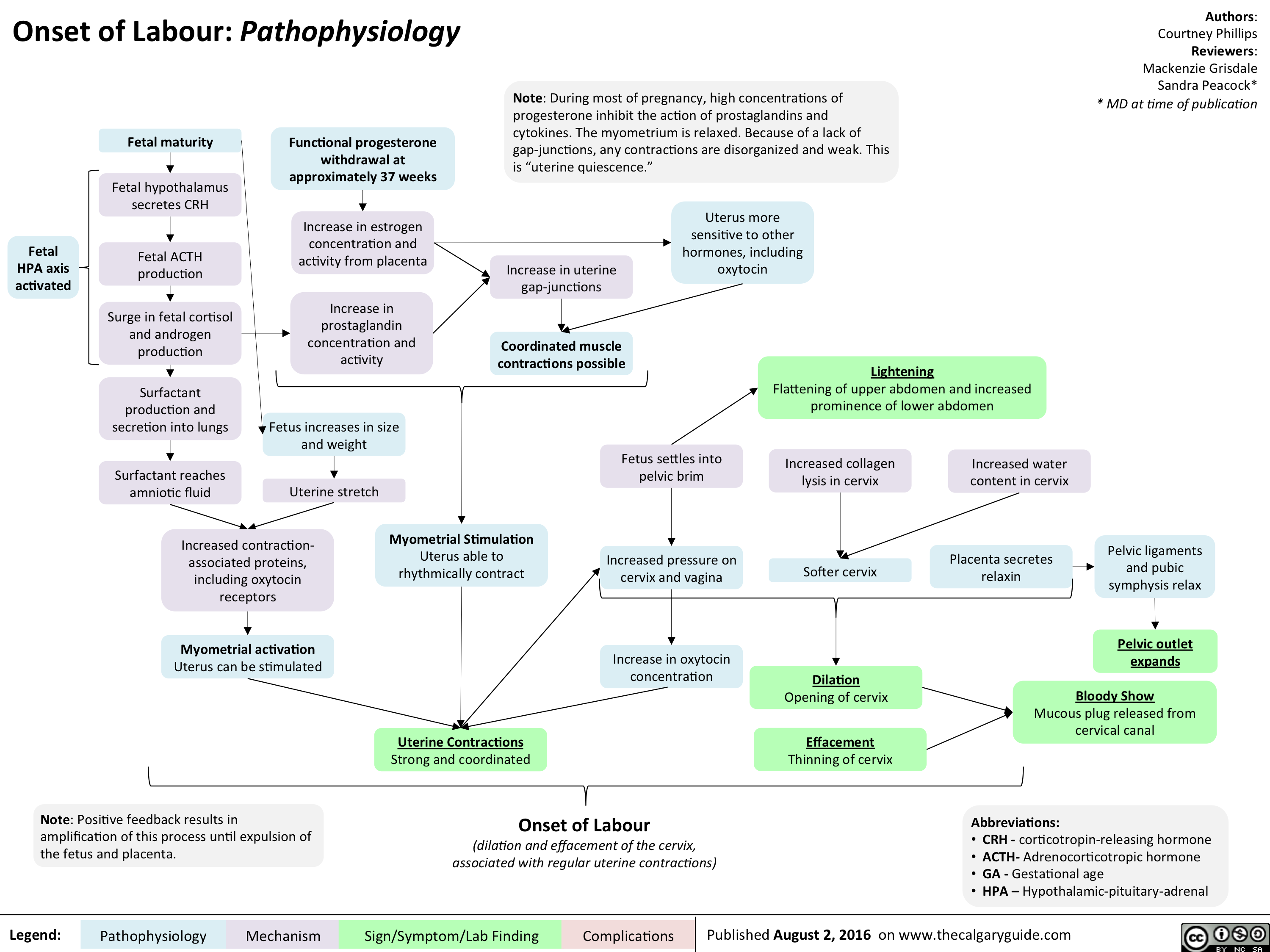
Onset of Labour- Pathophysiology
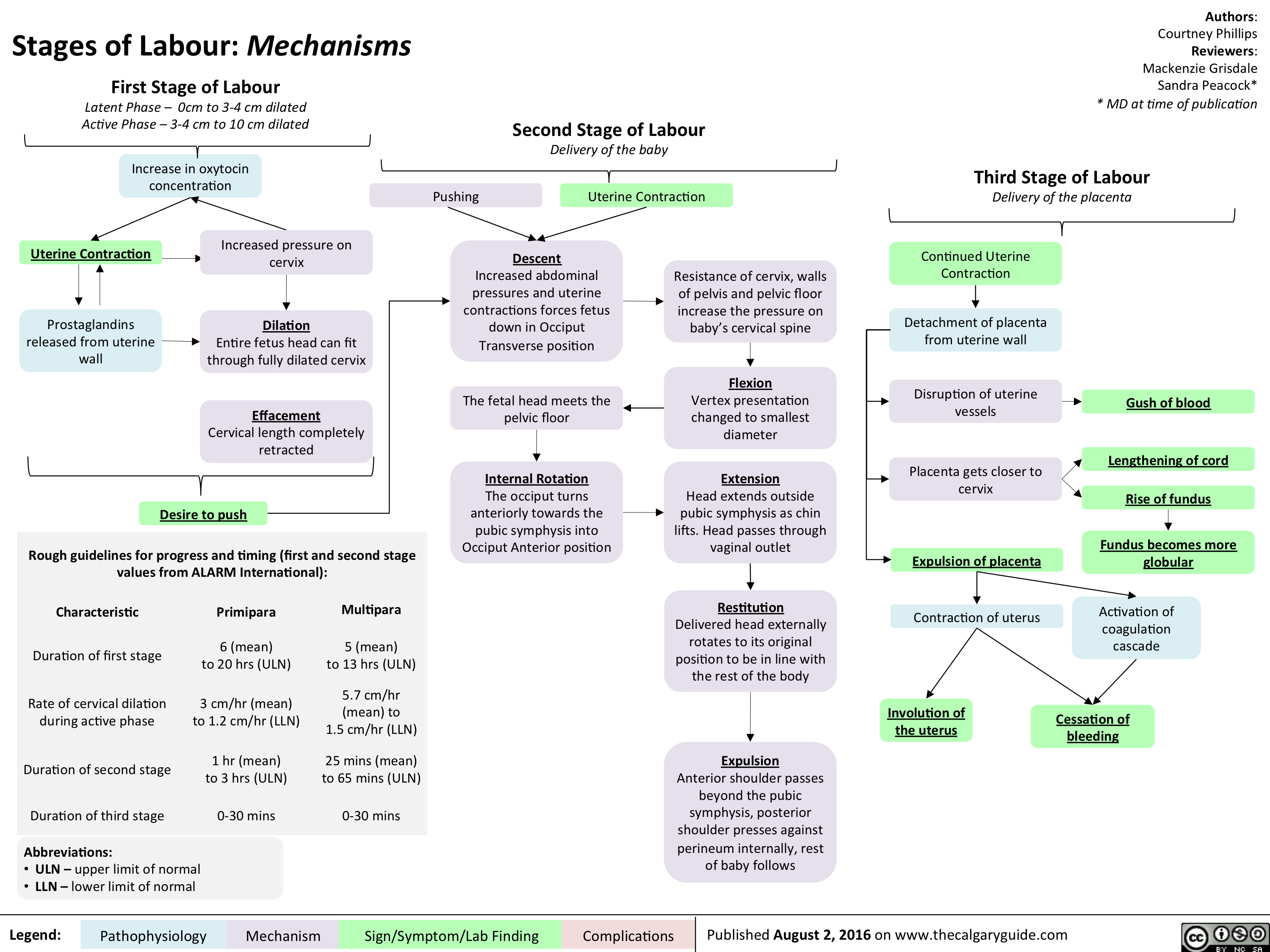
Stages of Labour- Mechanisms
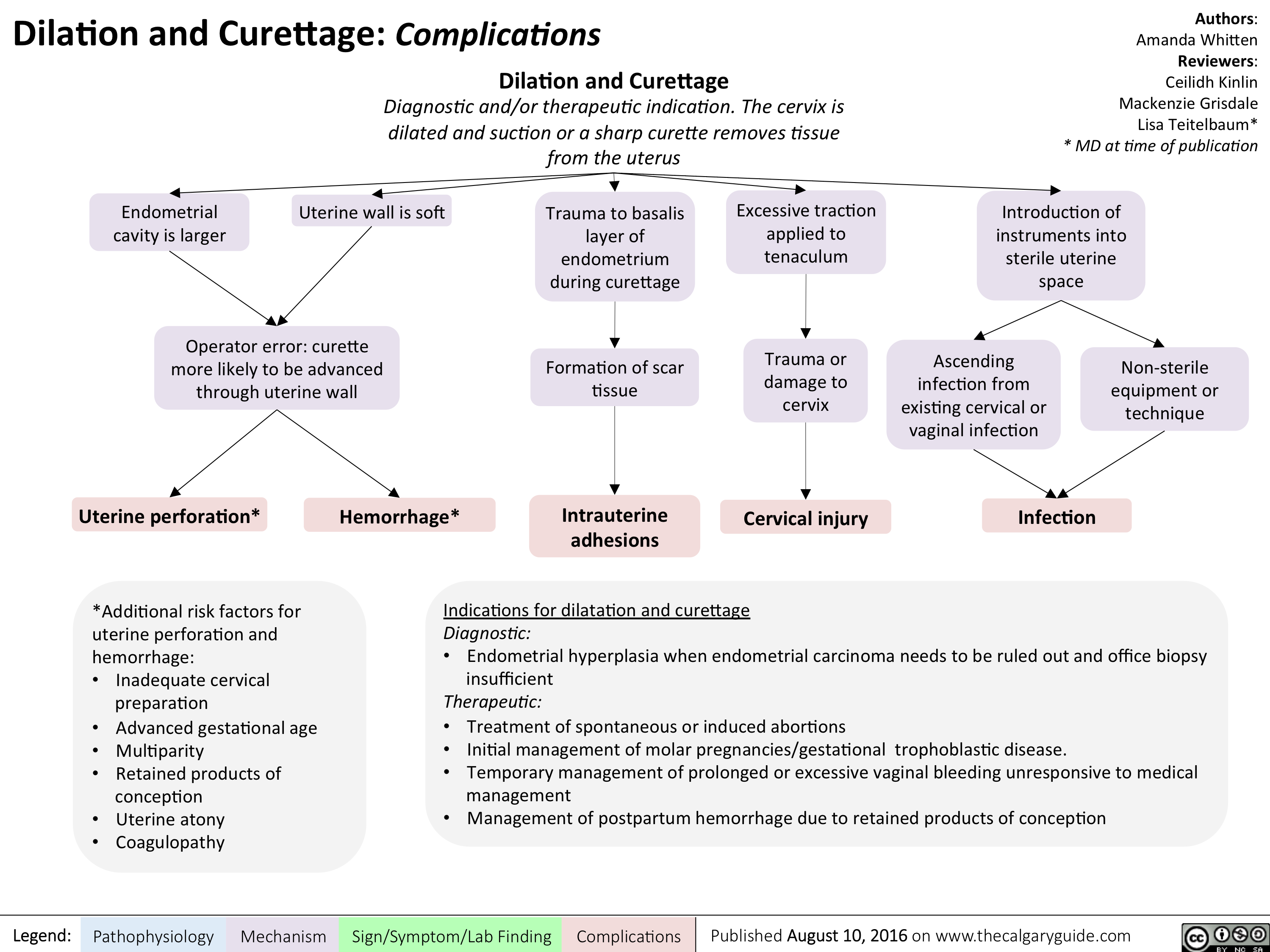
Dilatation and Curettage - Complications
myasthenia-gravis-final

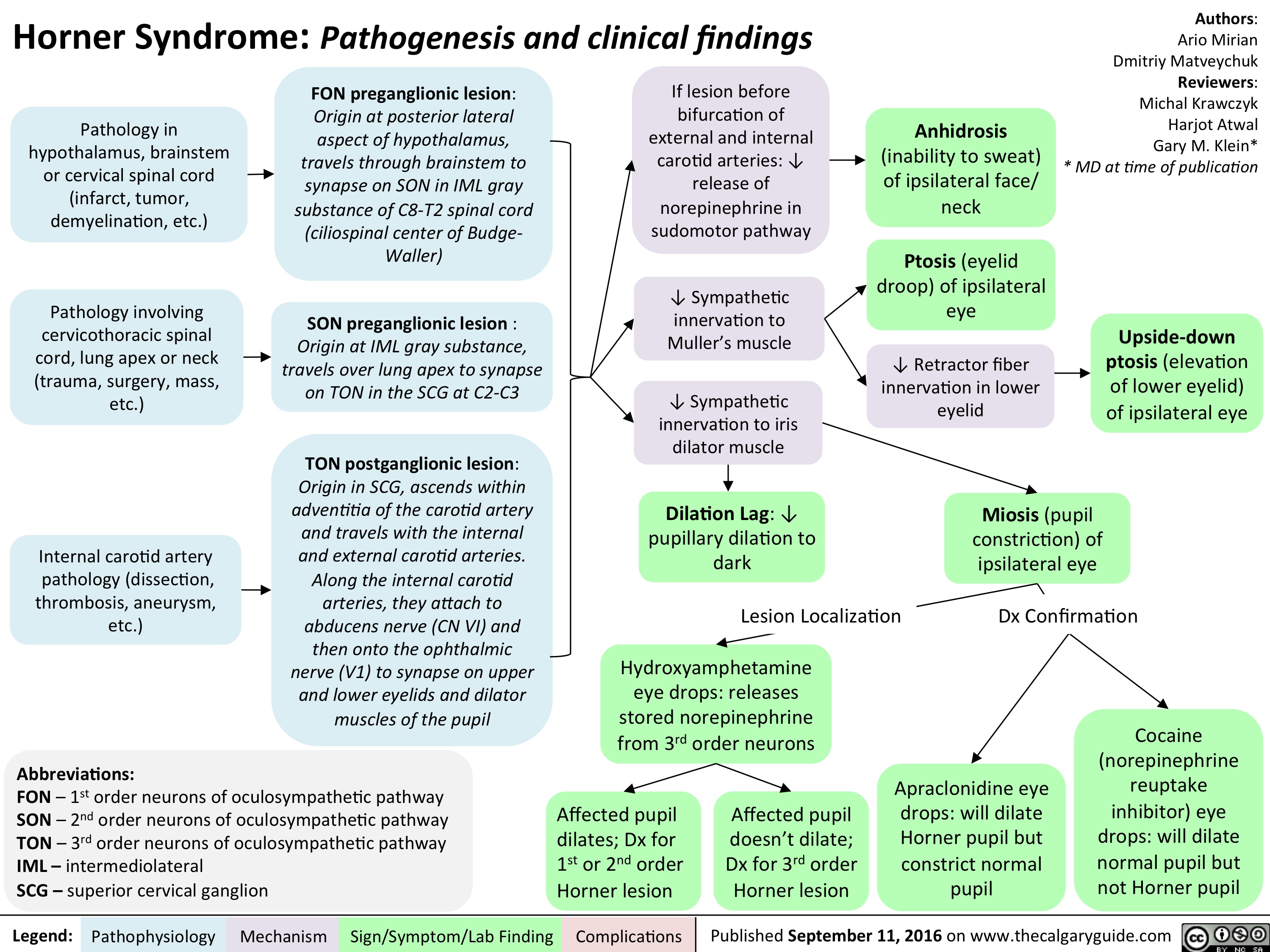
horner-syndrome
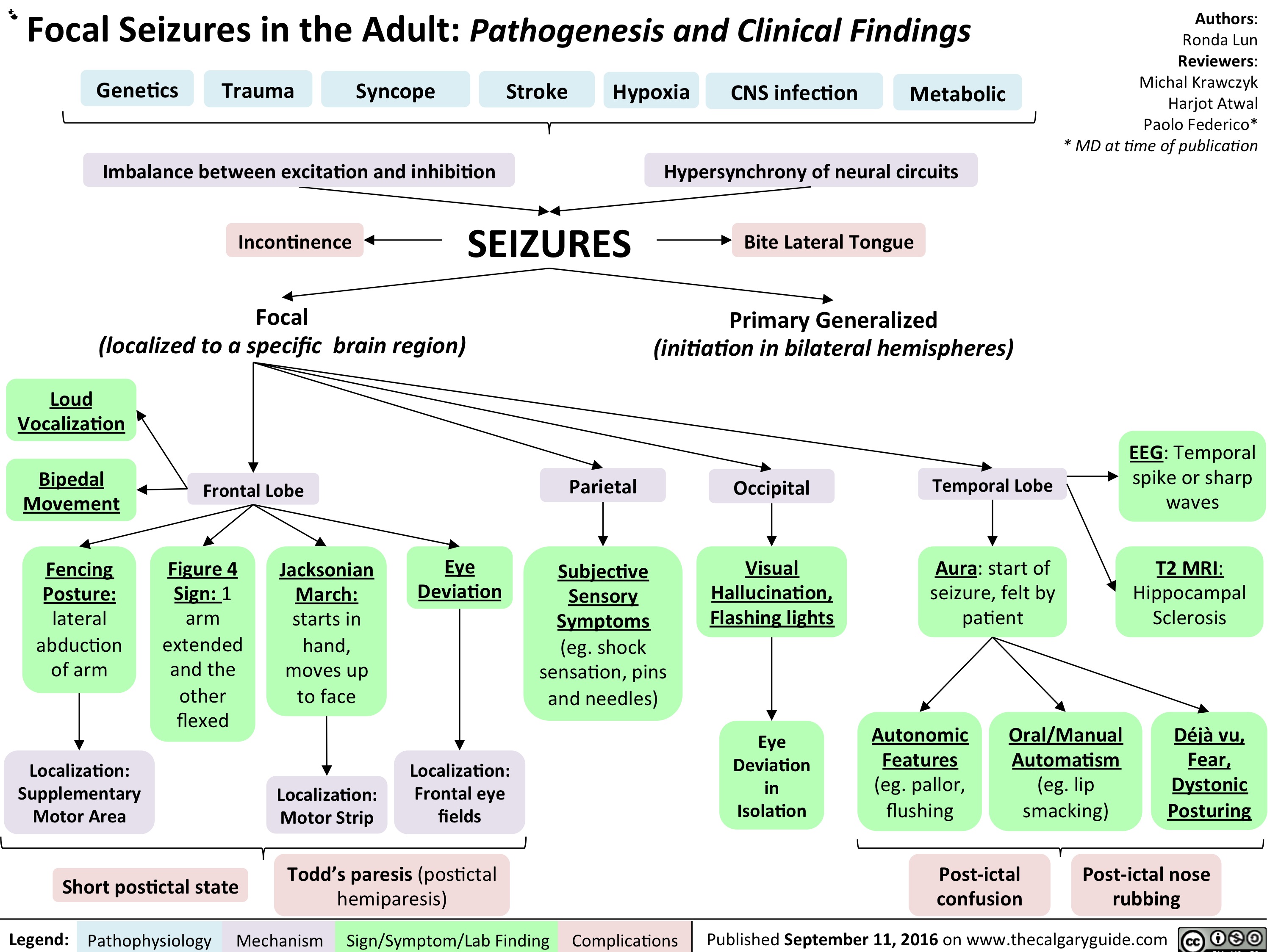
Focal Seizures in the adult: Pathogenesis and Clinical Findings
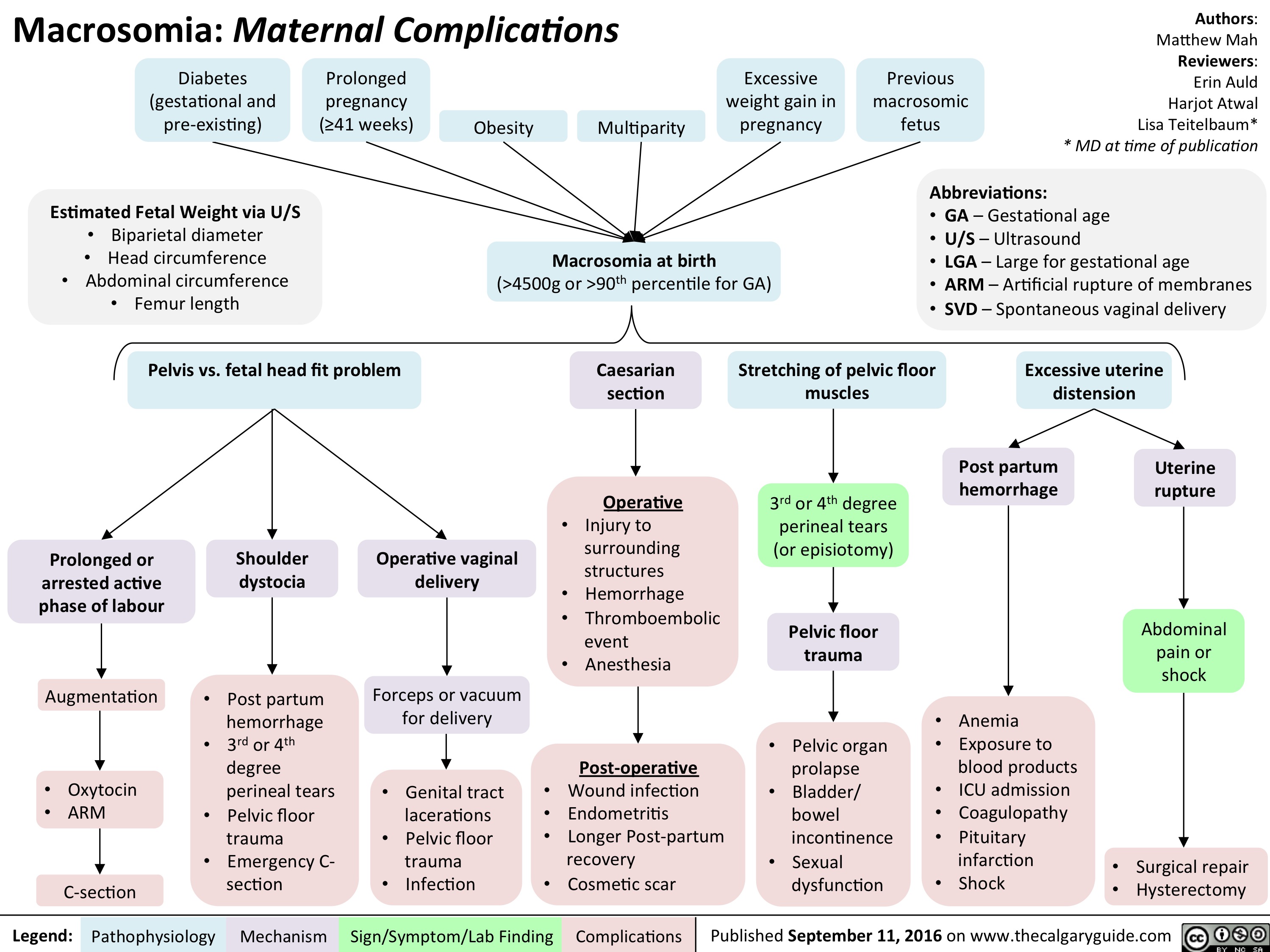
Macrosomia: Maternal Complications
Pediatric Uncompensated Shock: pathogenesis and clinical findings

Type 1 Respiratory Distress Syndrome

acute-closed-angle-glaucoma

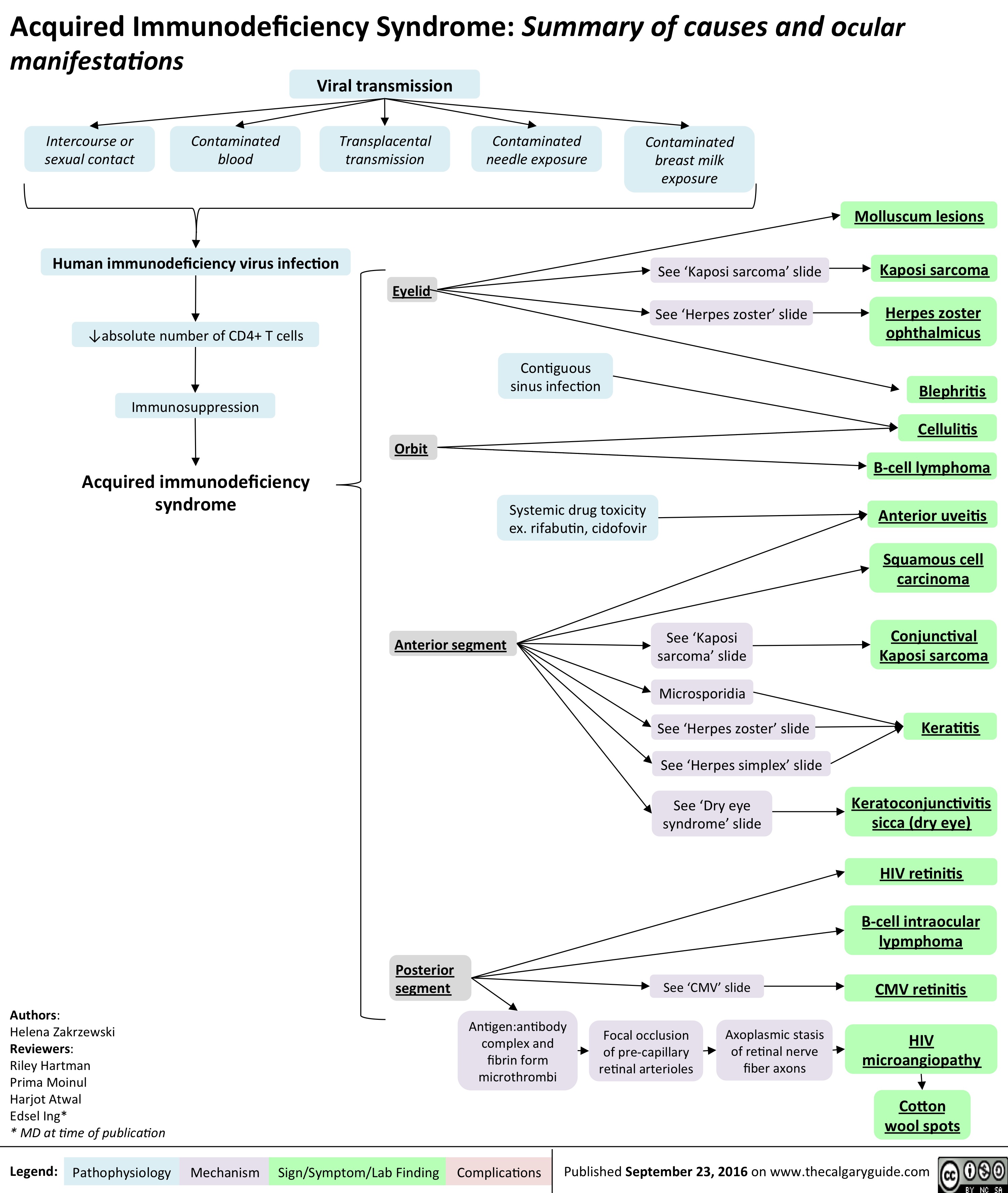
aids-and-cmv-retinitis
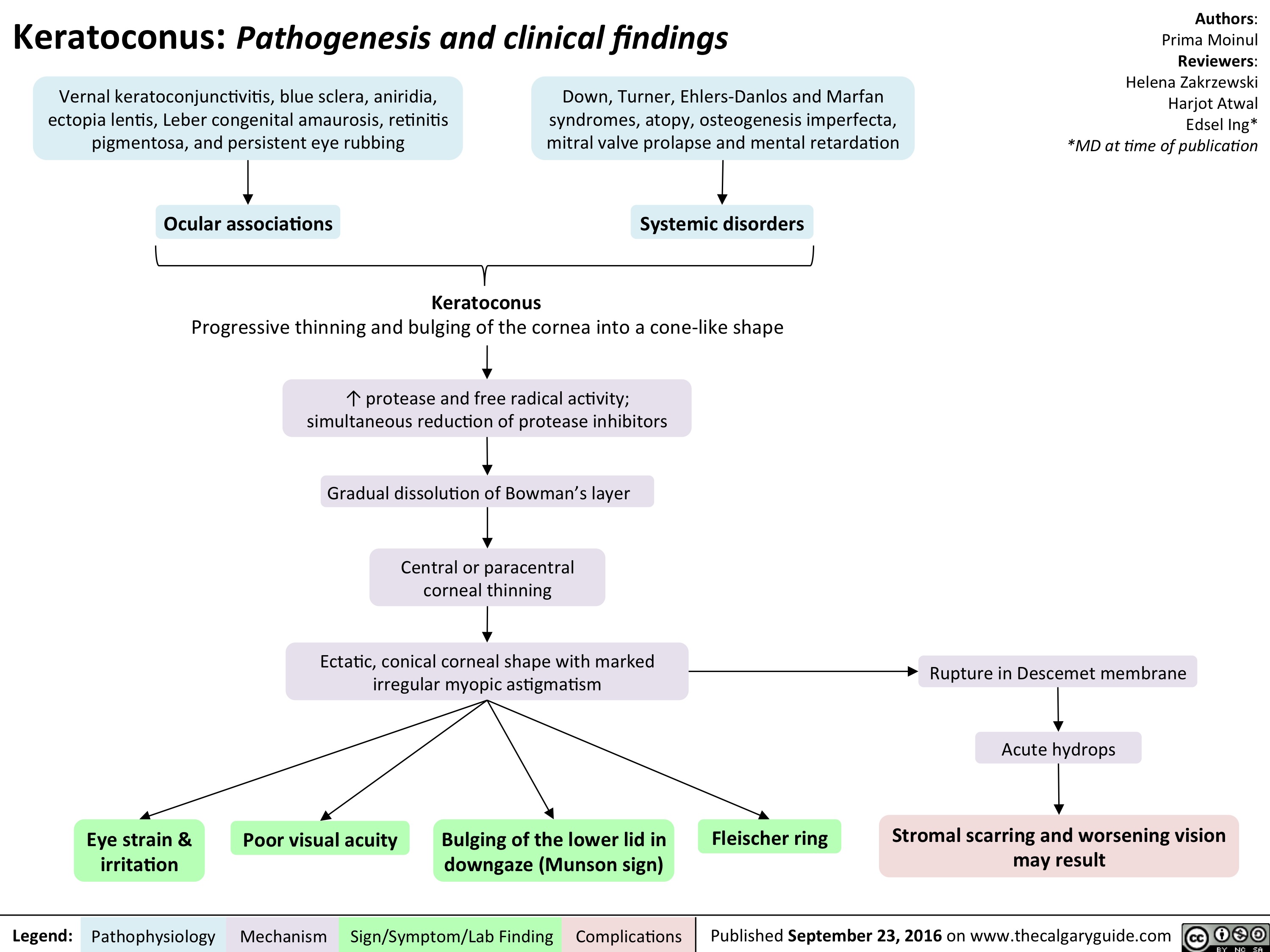
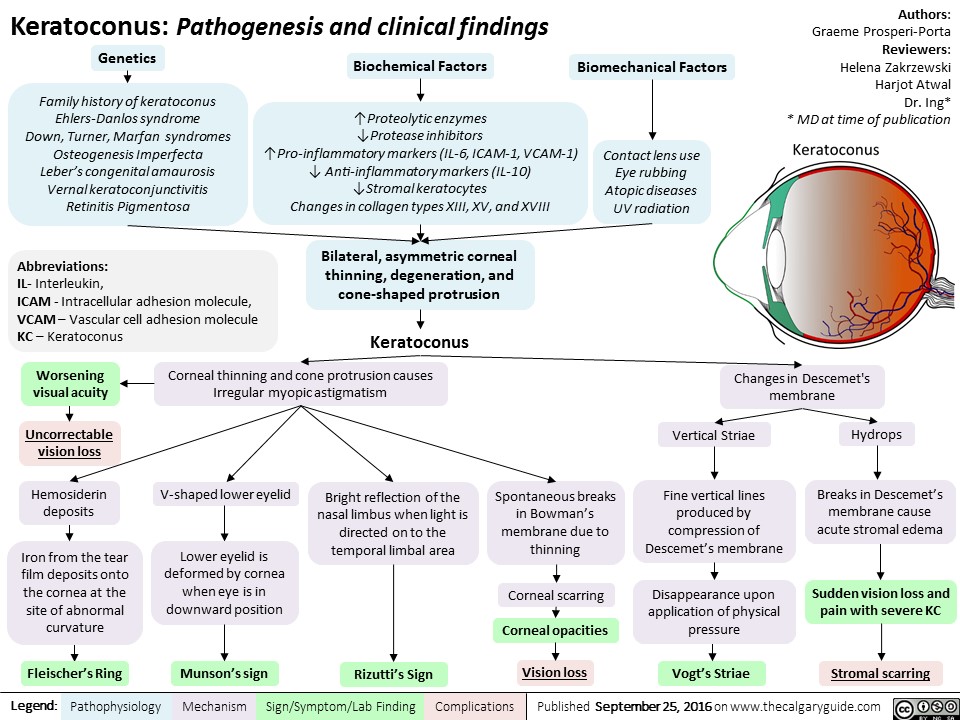
keratoconus
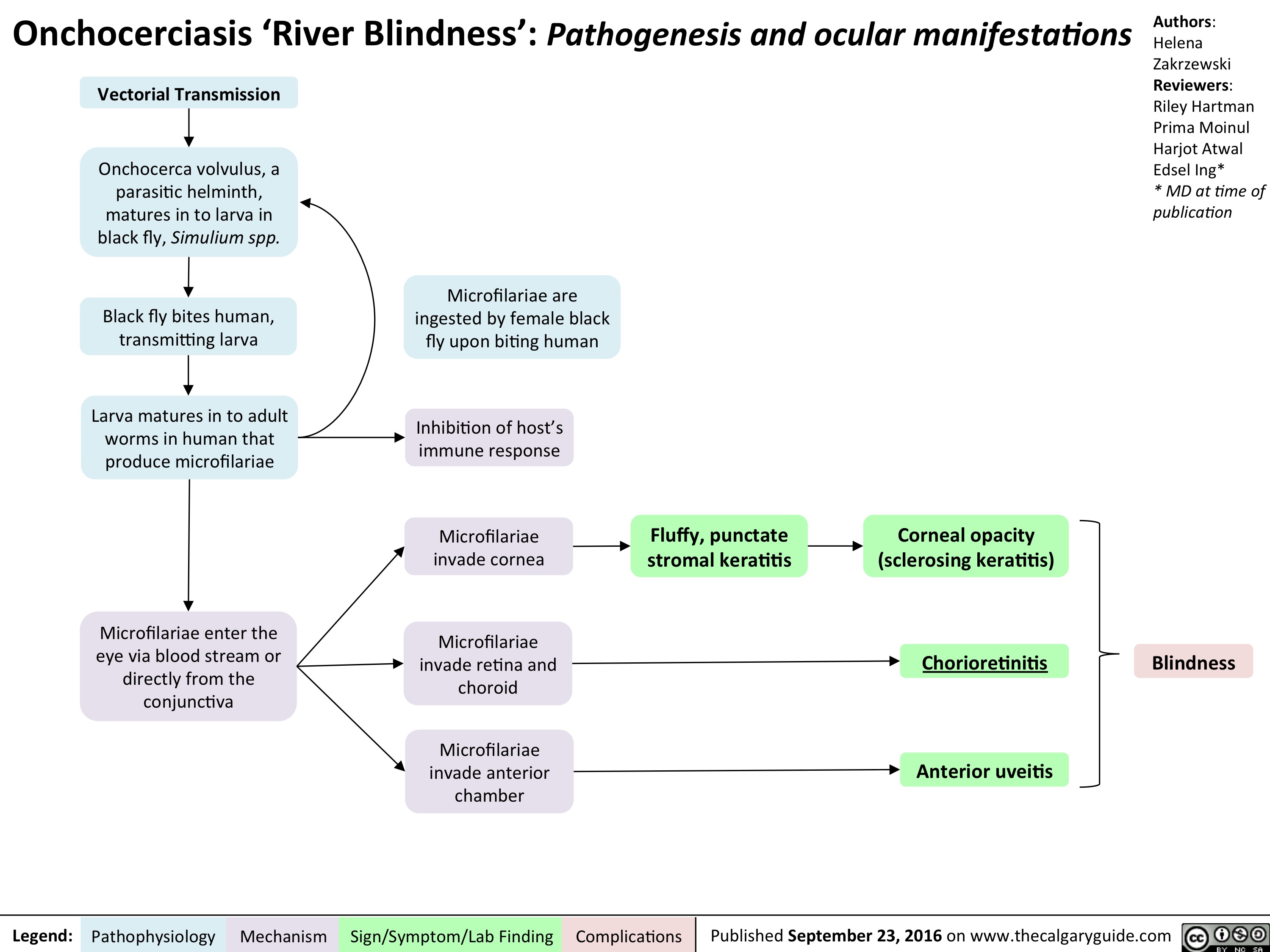
onchocerciasis
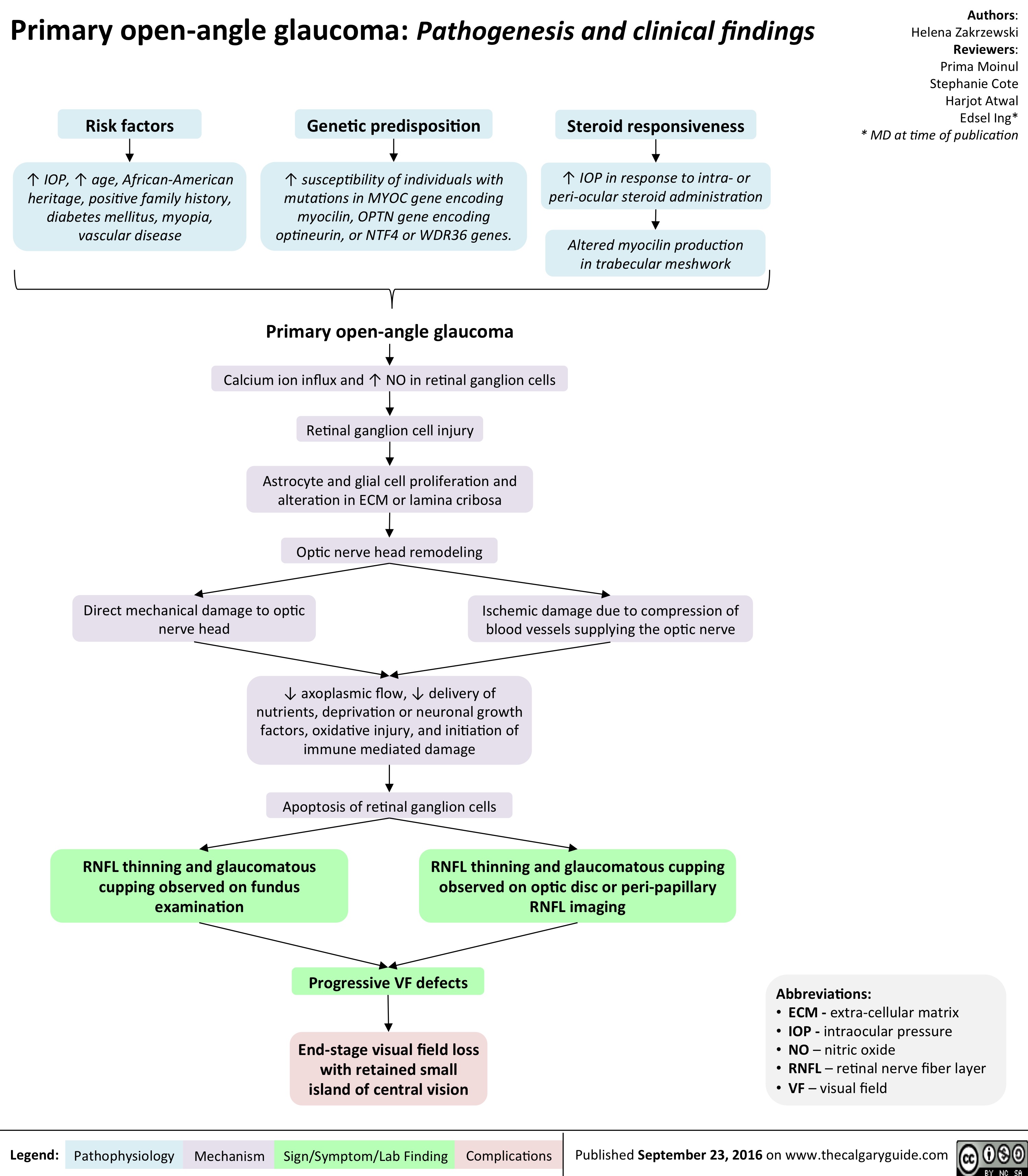
primary-open-angle-glaucoma
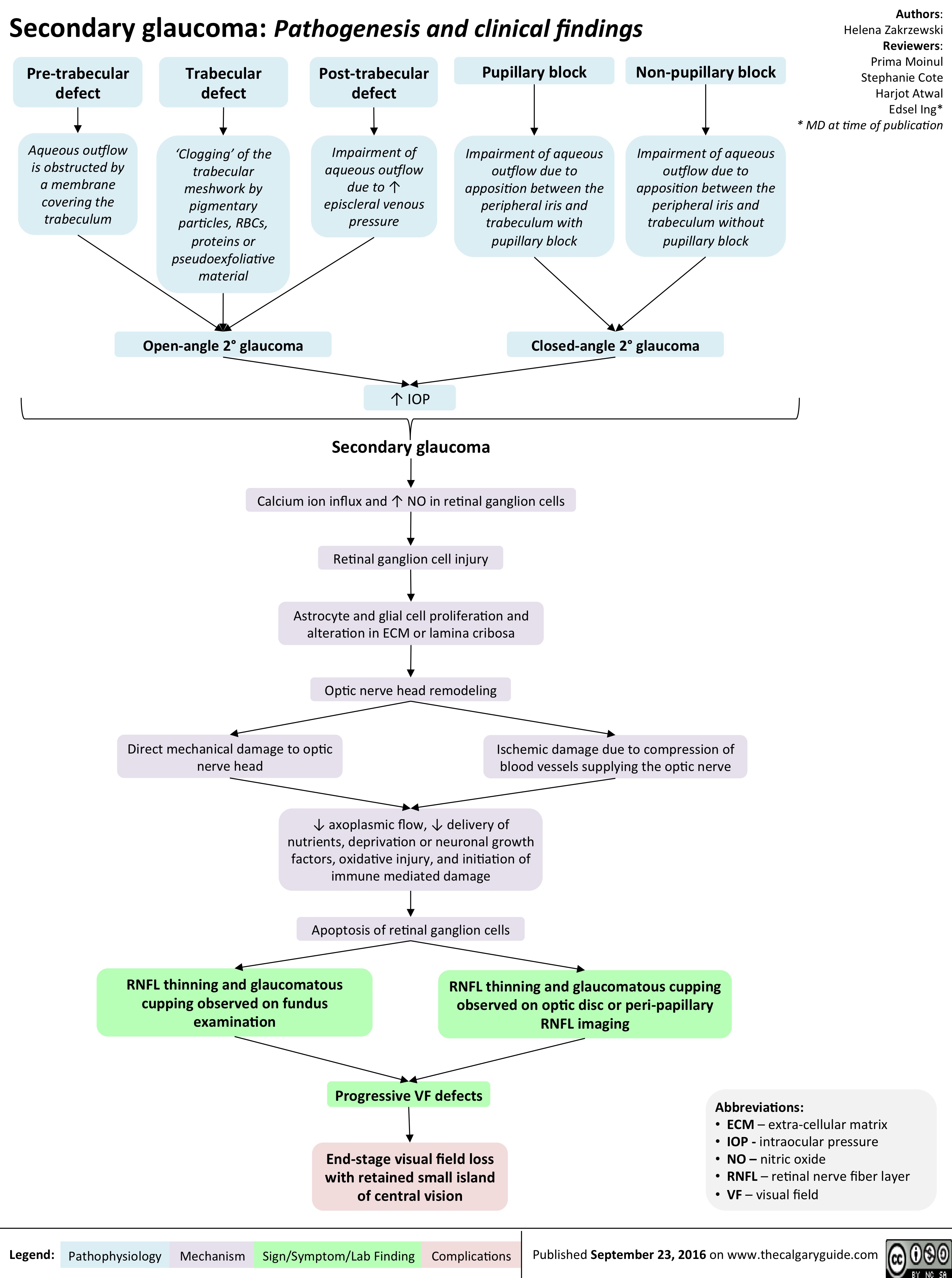
secondary-glaucoma
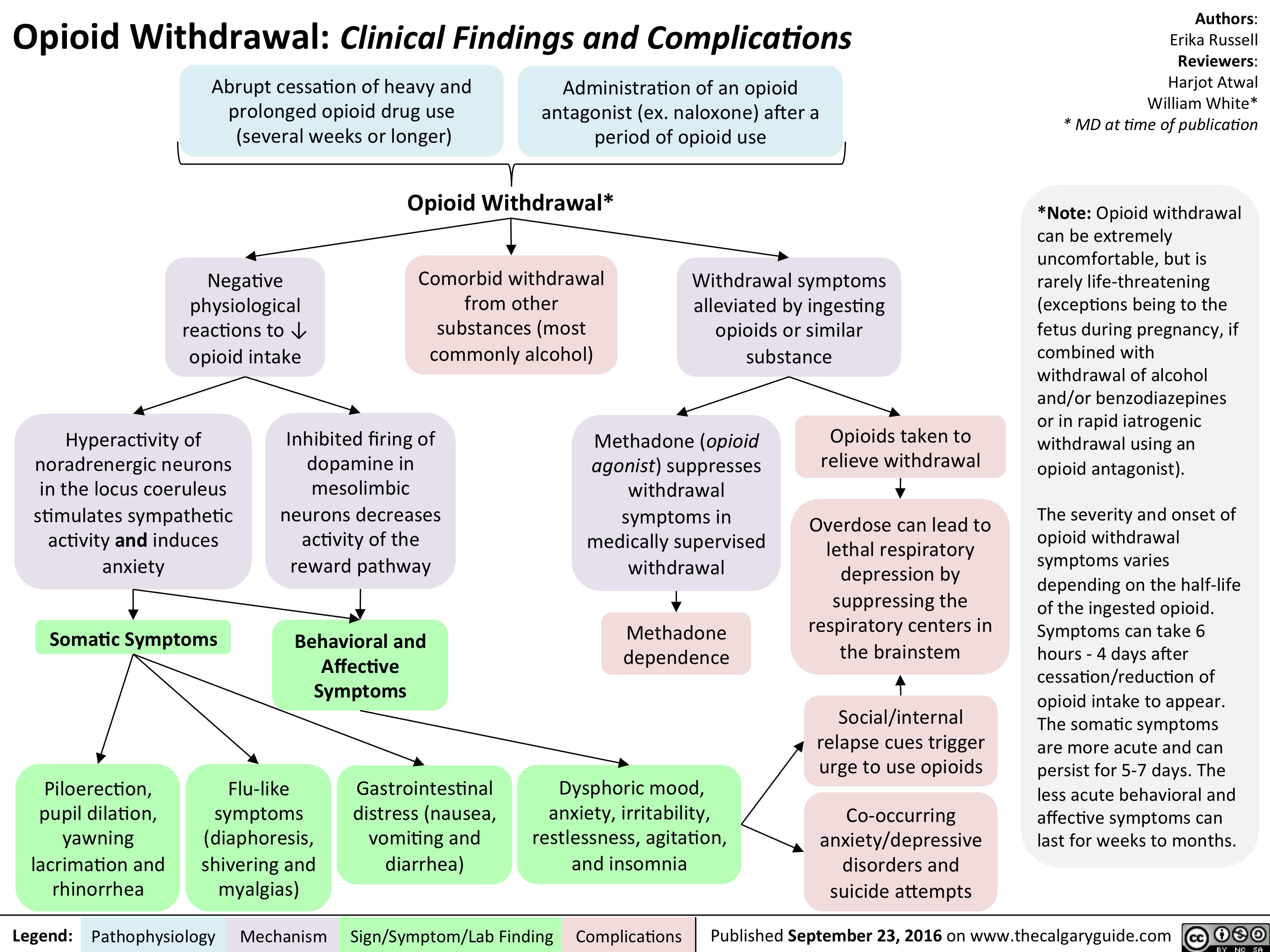
opioid-withdrawal
keratoconus
slide1
slide1
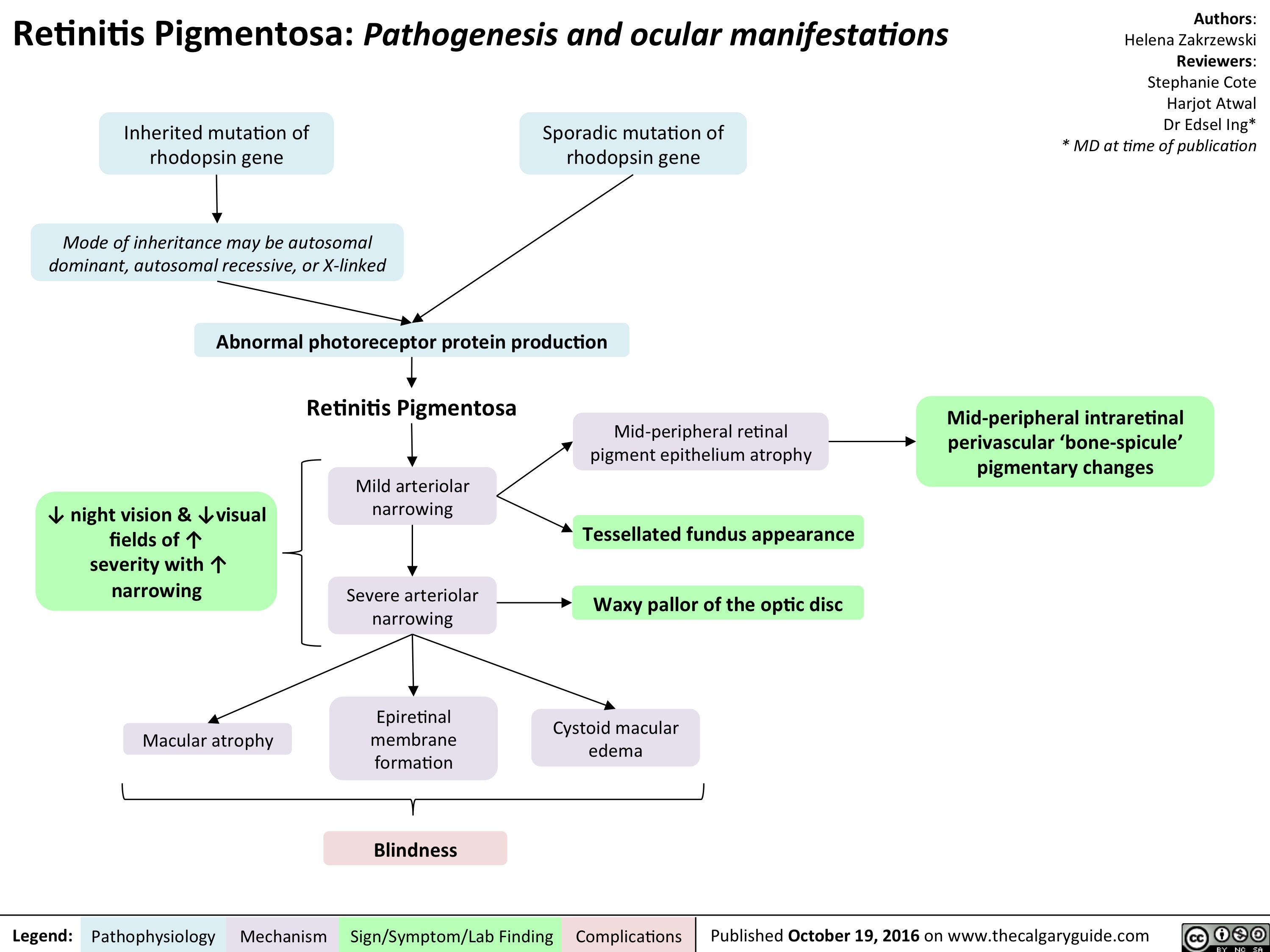
retinitis-pigmentosa-final
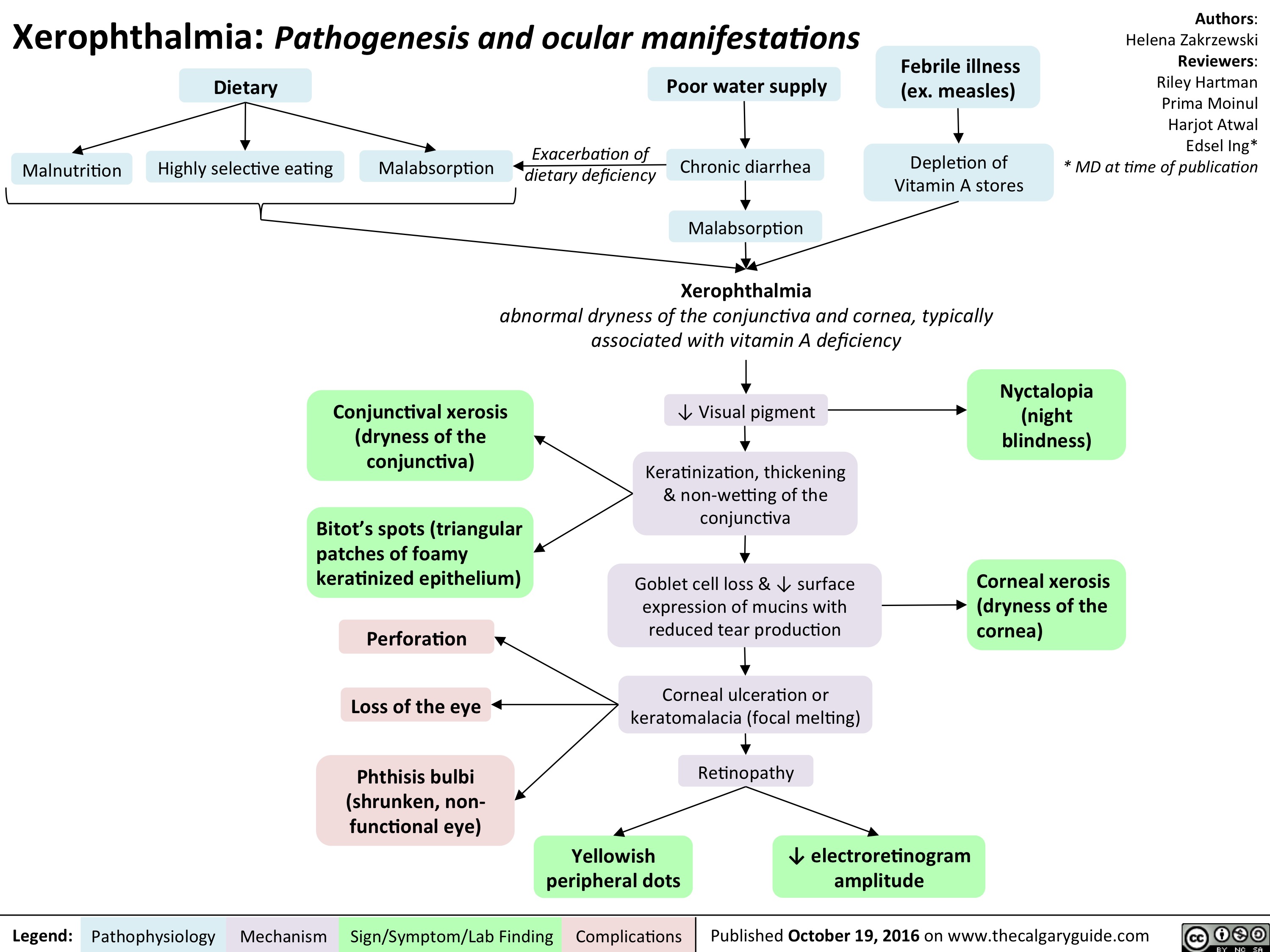
xerophthalmia-final
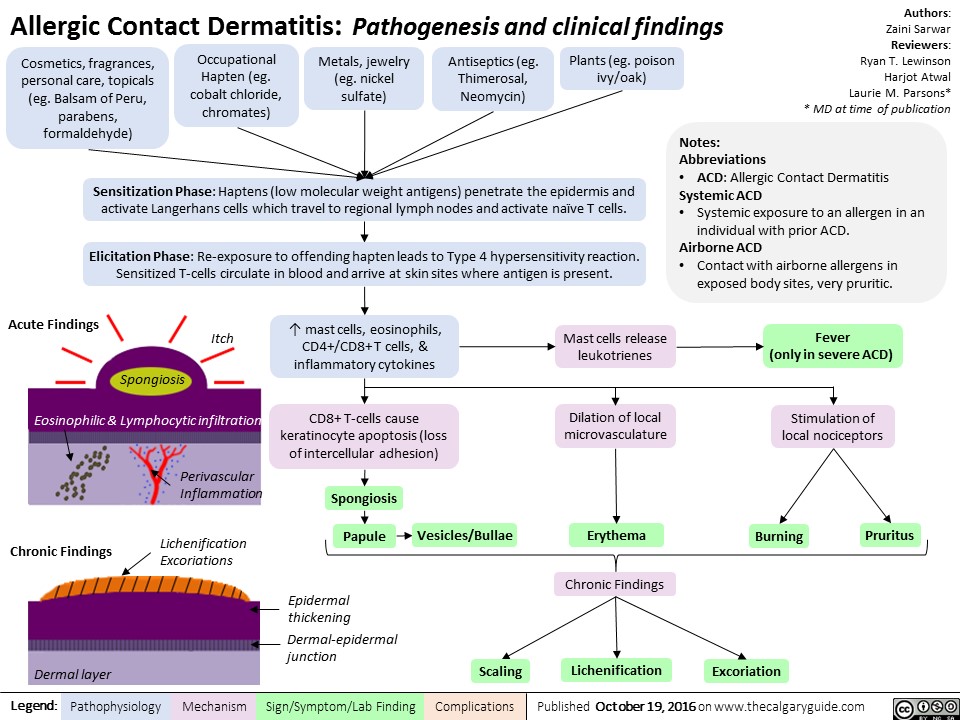
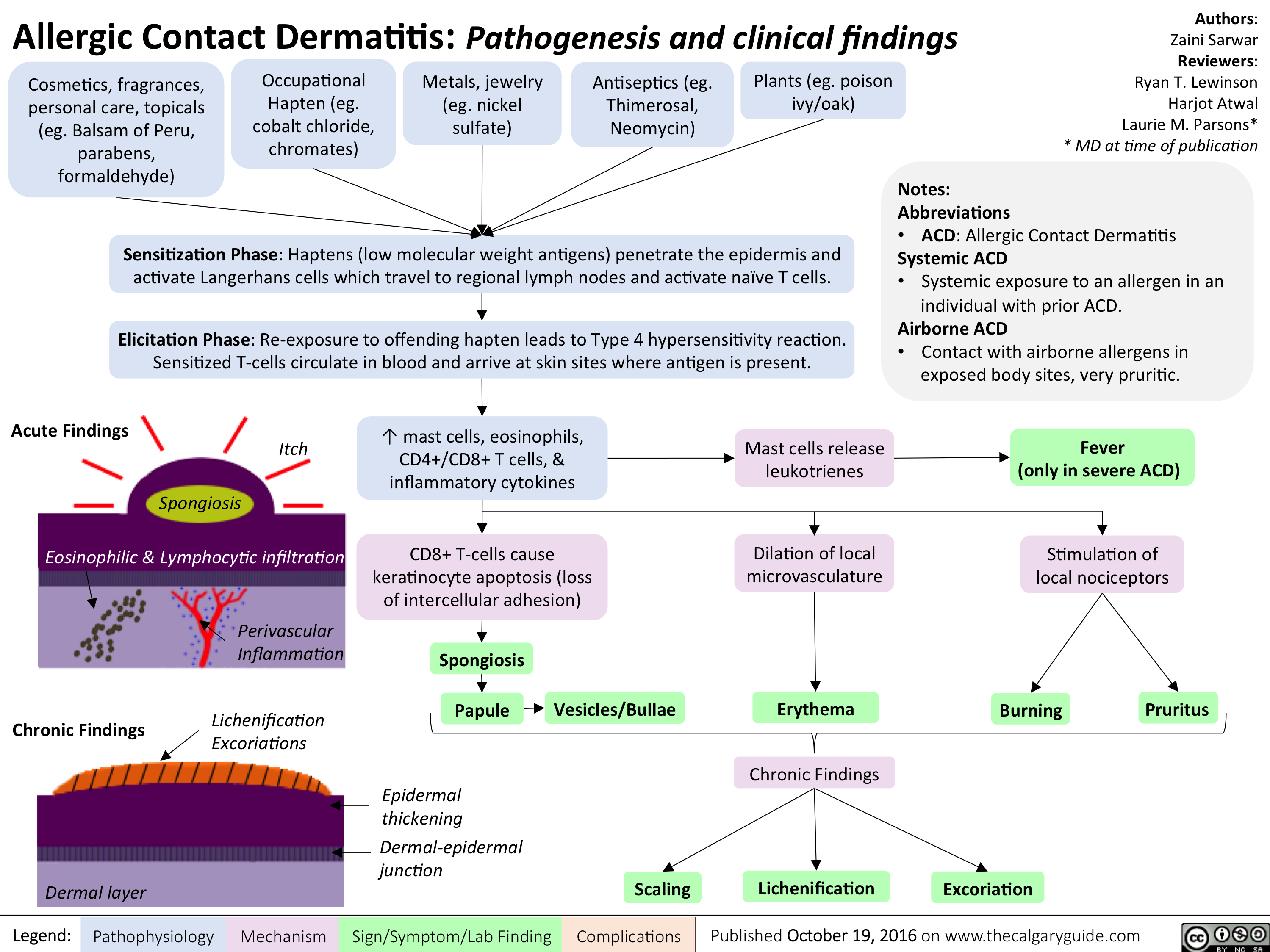
allergic-contact-dermatitis
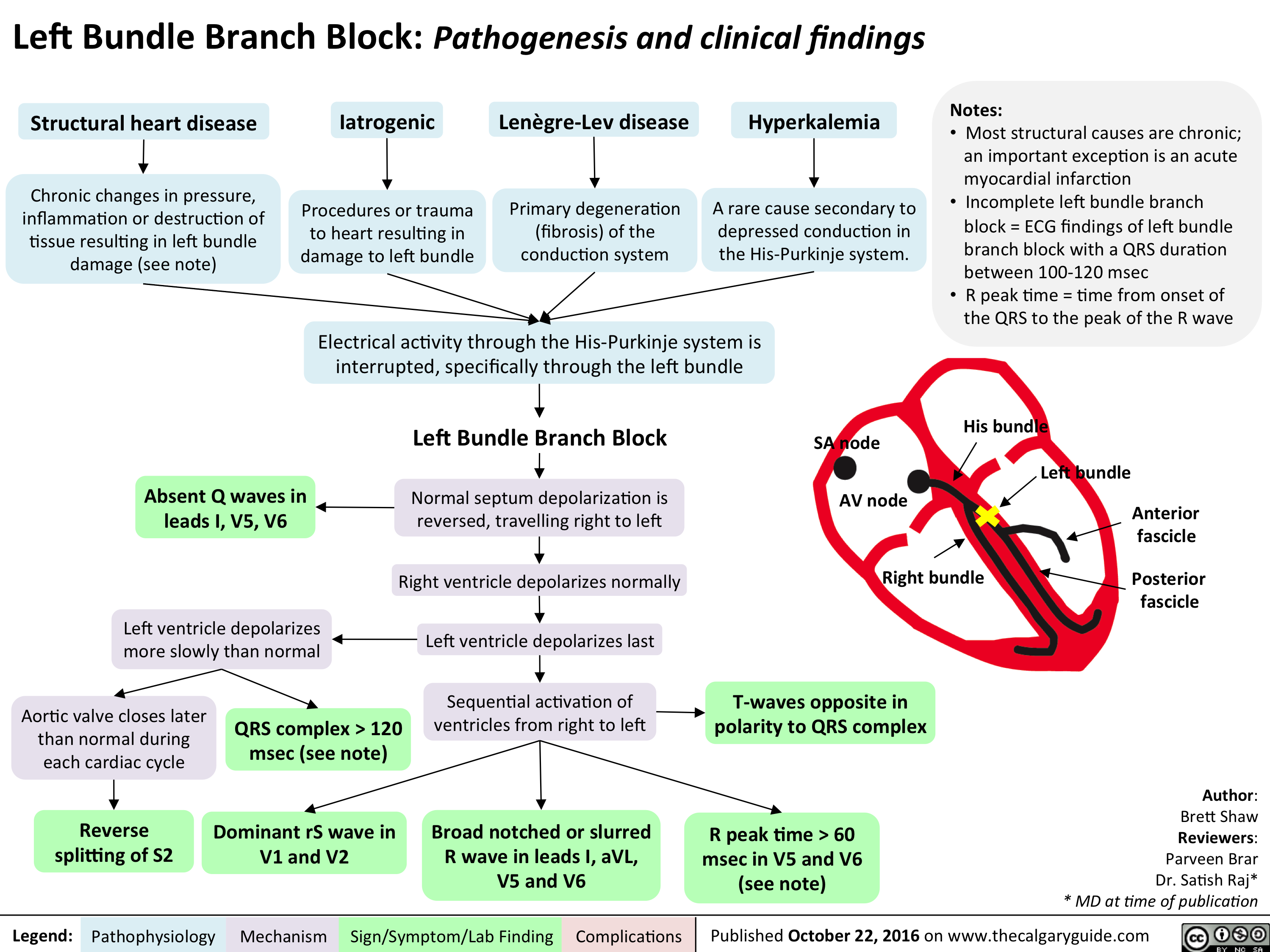
cardio_lbbb_oct-15
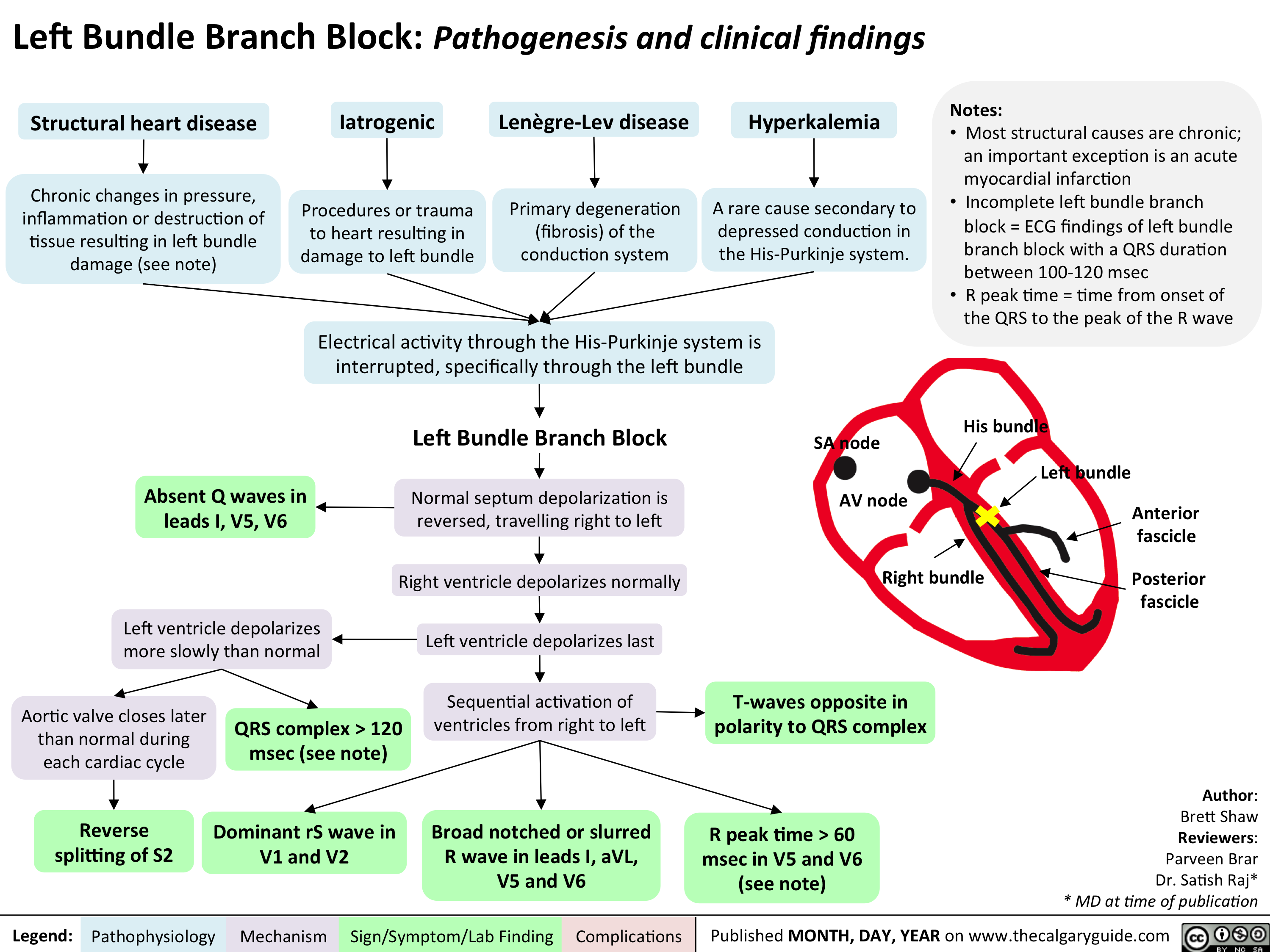
cardio_lbbb_oct-15
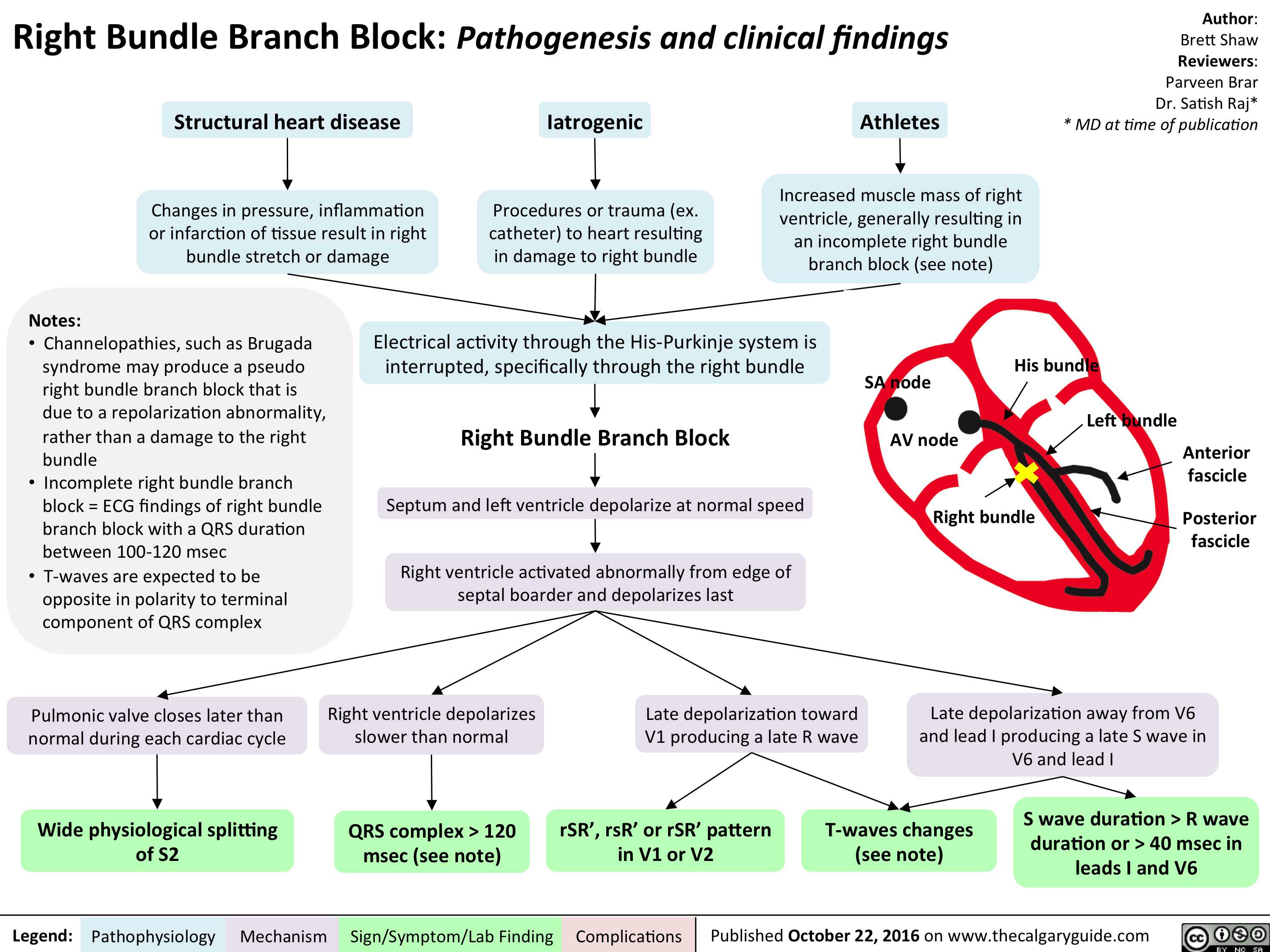
cardio_rbbb_oct-15
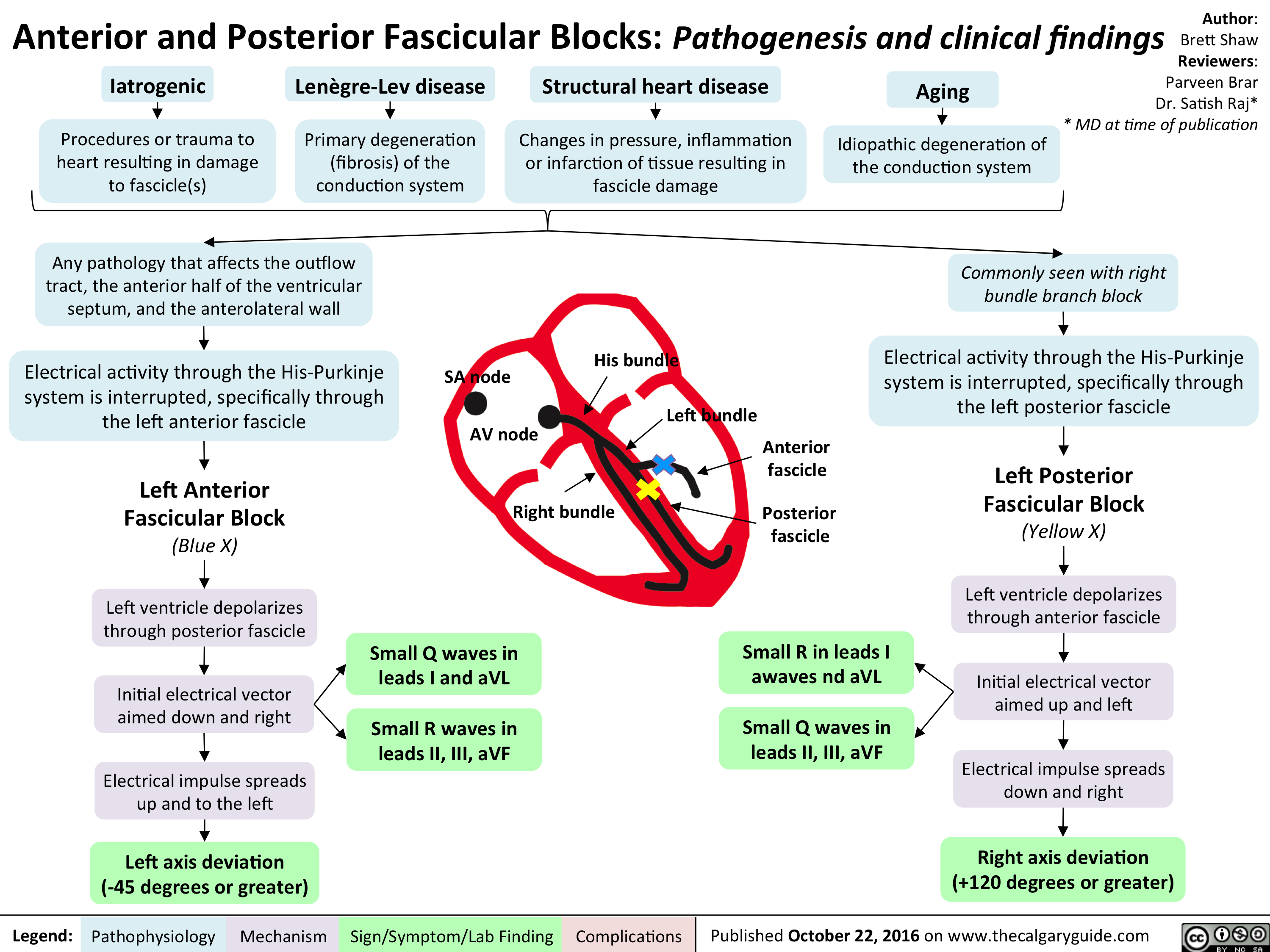
cardio_ant-and-post-fascicular-blocks_oct-15
allergic-contact-dermatitis
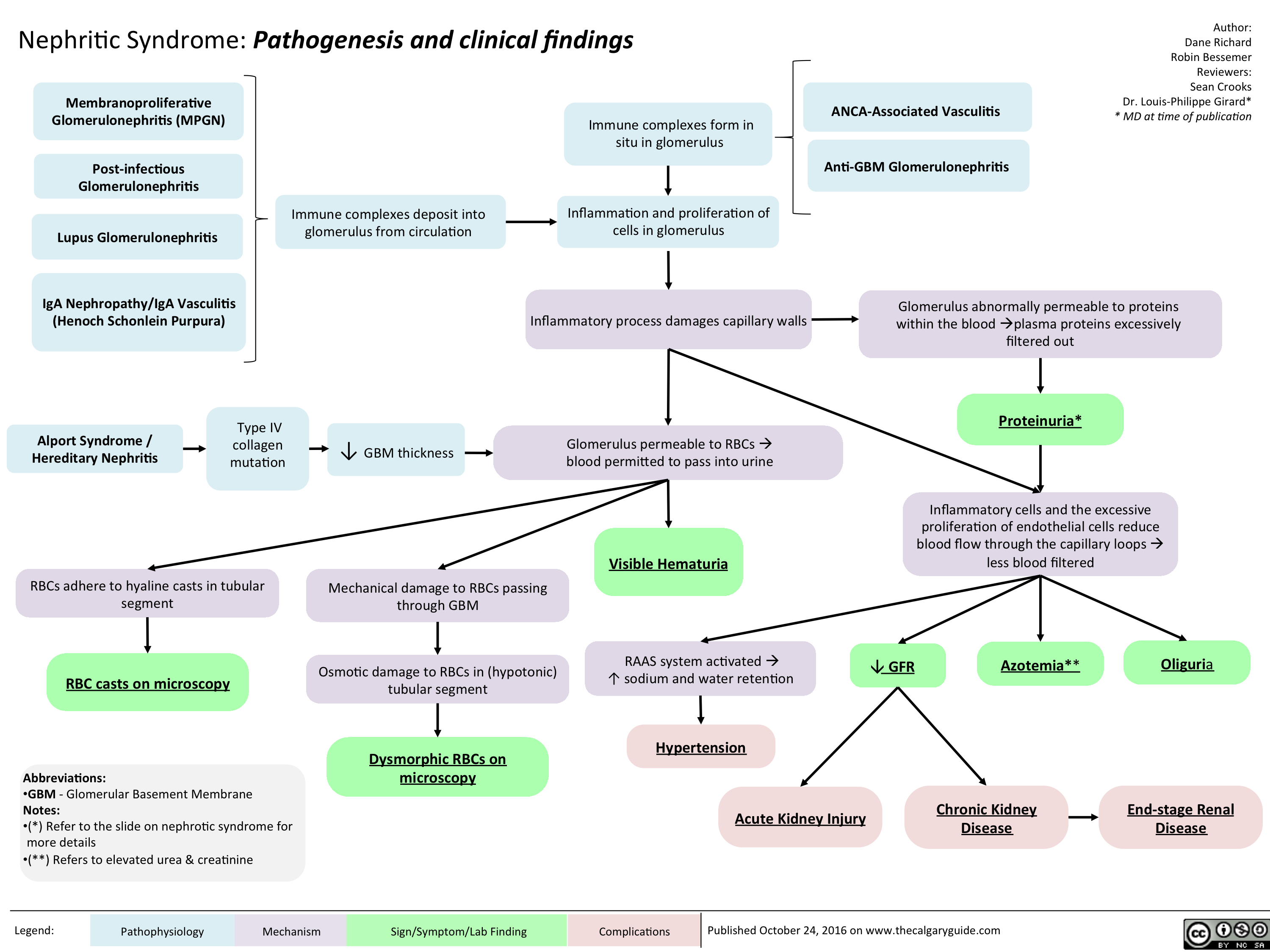
Nephritic Syndrome: Pathogenesis and clinical findings
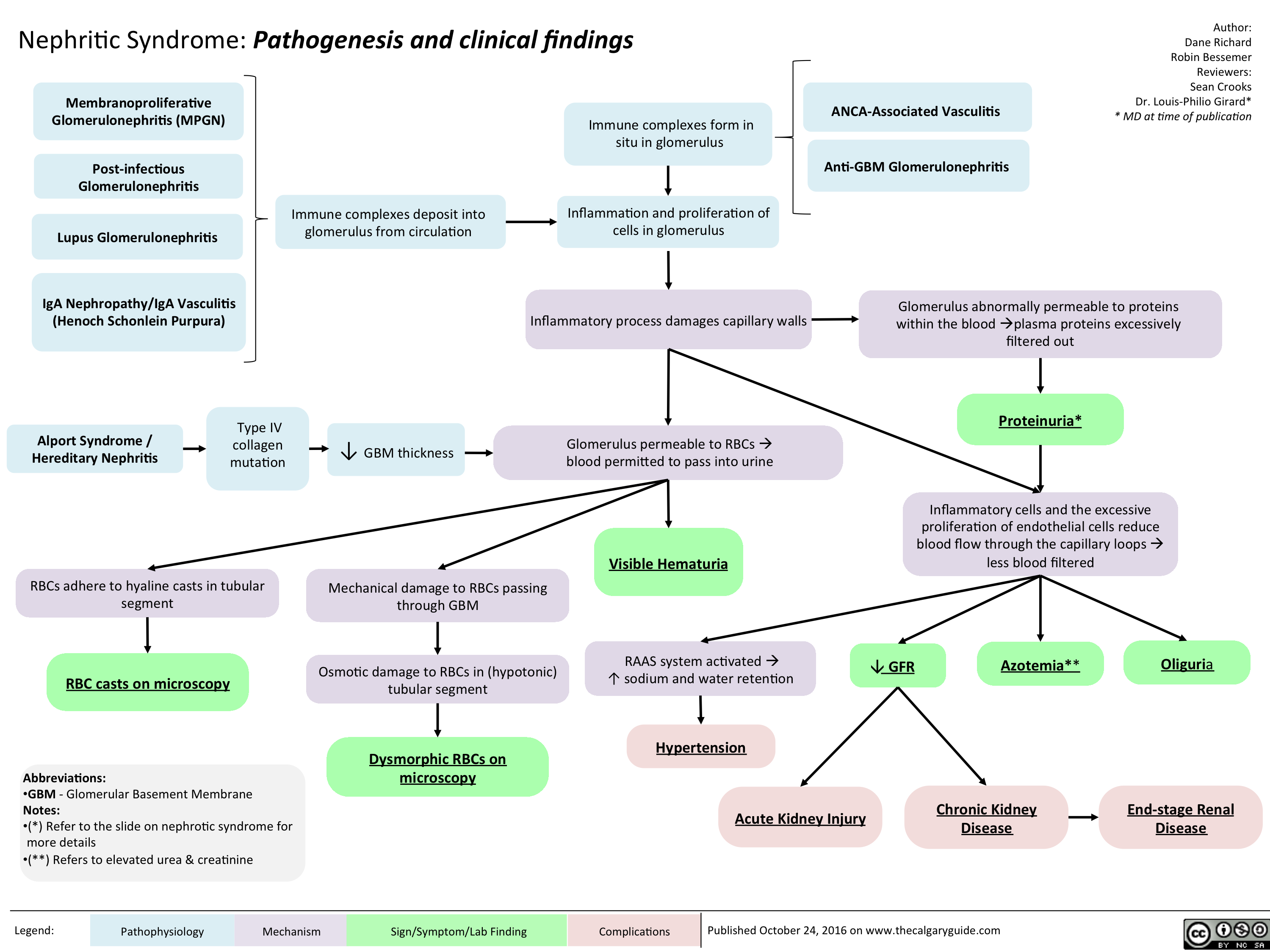
nephritic-syndrome
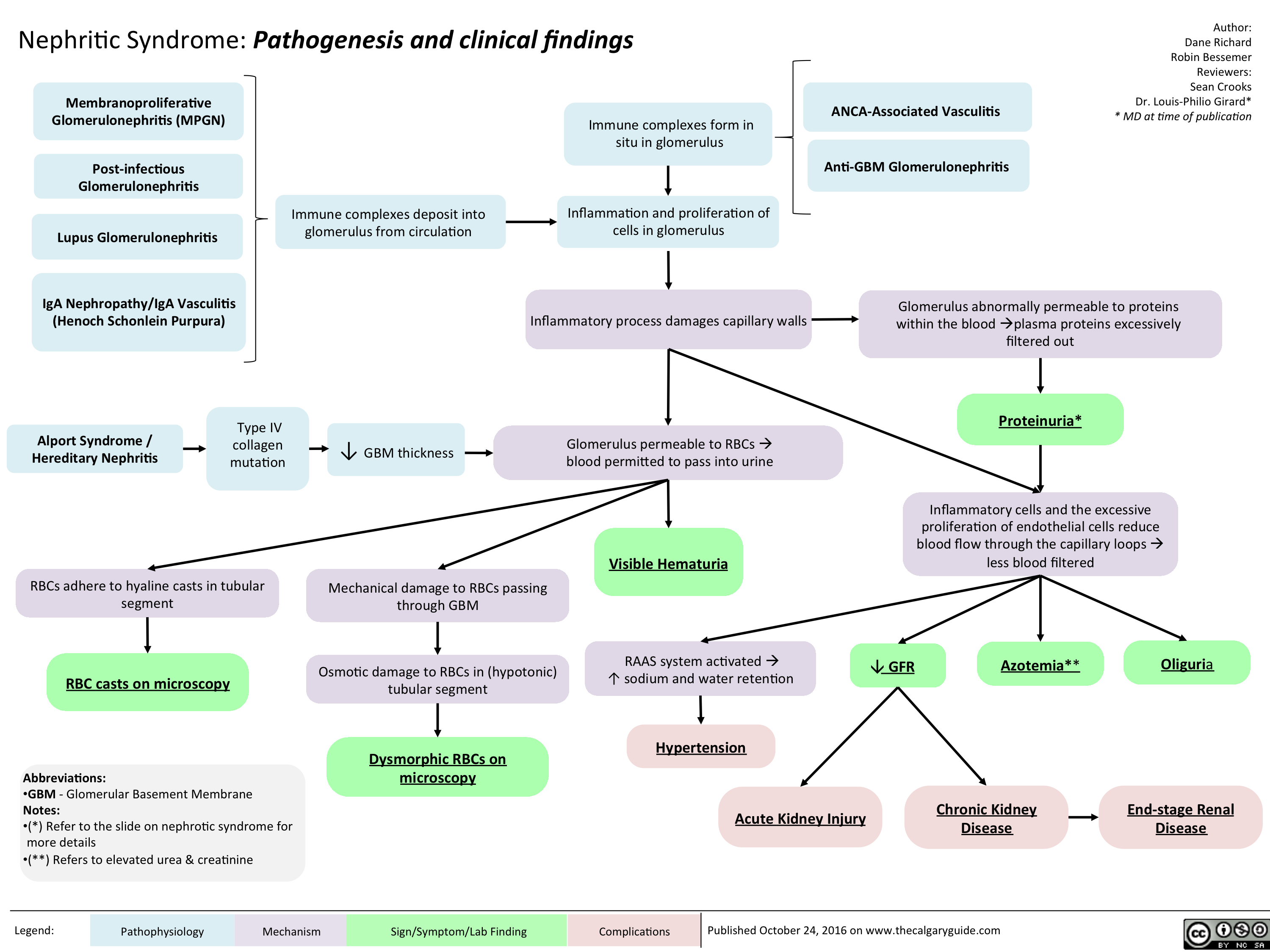
nephritic
Opioid Receptor Agonists
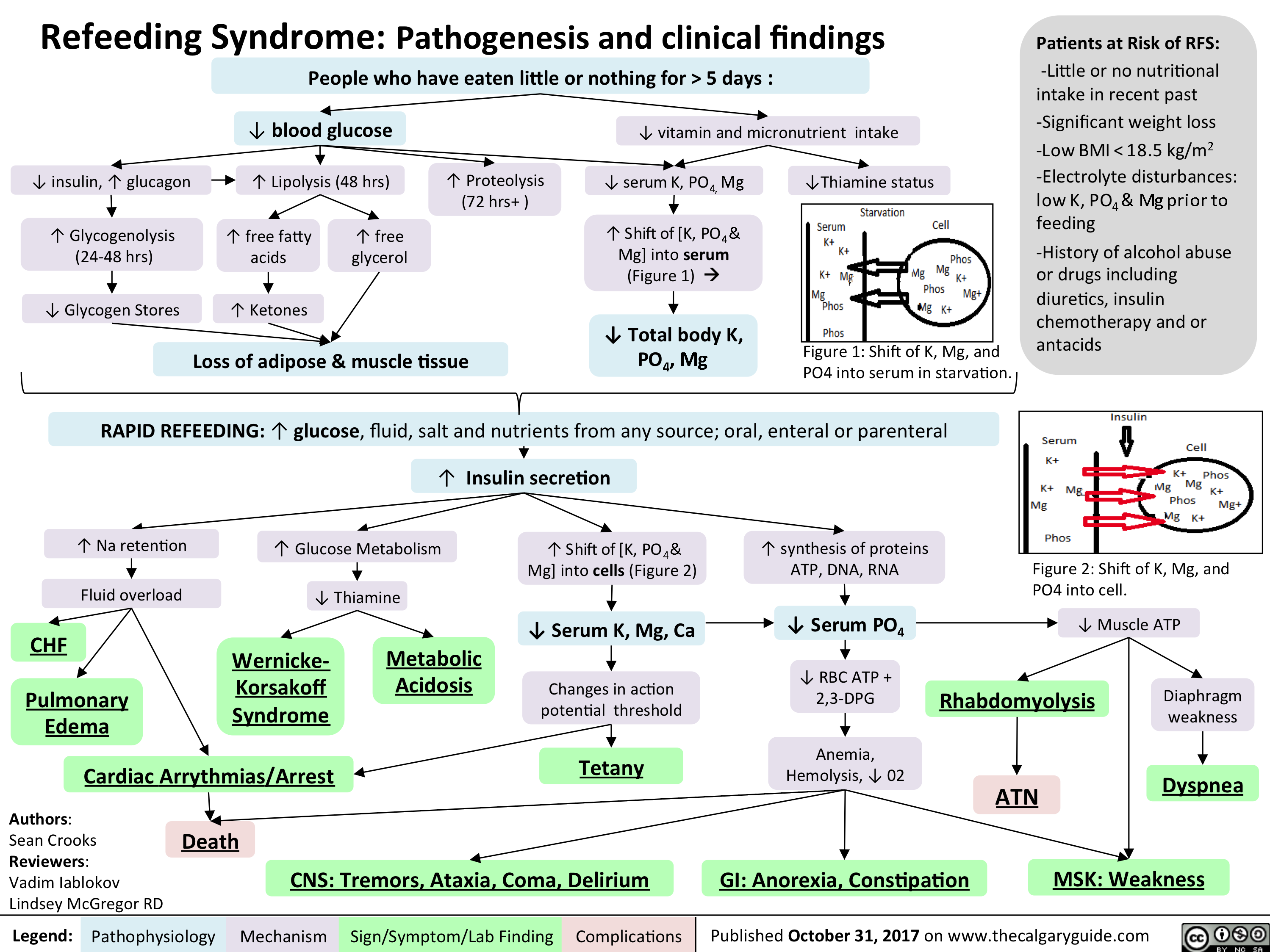
refeeding syndrome
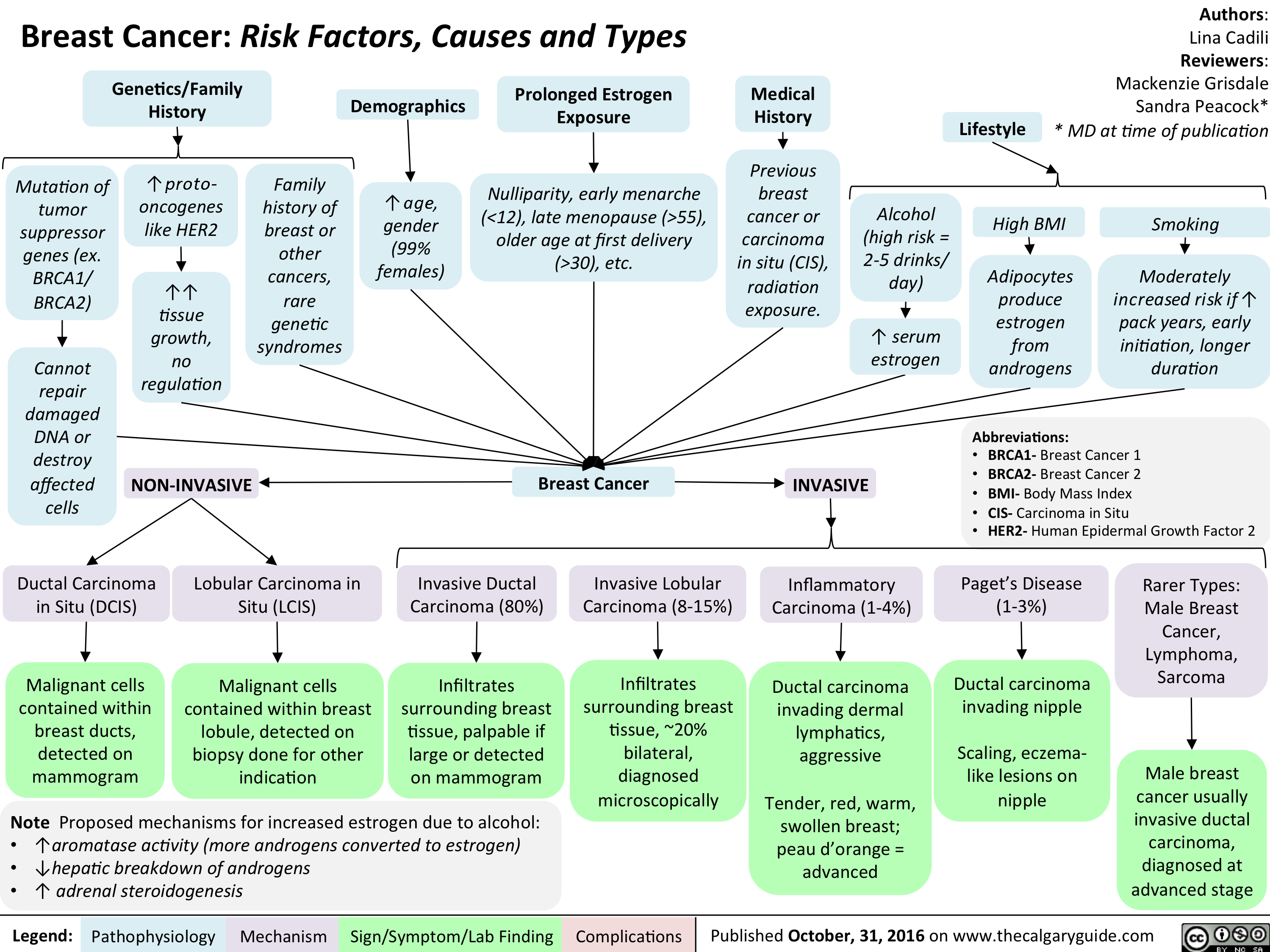
Breast Cancer Risk Factors Causes and Types
Hyperosmolar Hyperglycemic State
![Hyperosmolar Hyperglycemic State (HHS)
Note: HHS is only seen in Type II DM patients!
Note: In patients with either DKA or HHS, always look for an underlying cause (i.e. an infection)
Author: Yan Yu Reviewers:
Peter Vetere
Gill Goobie
Hanan Bassyouni* * MD at time of publication
Alters total body water & ion osmosis
Inadequate insulin production, insulin resistance, non- adherence to insulin Tx
Relative Insulin deficit
Stresses that ↑ Insulin demand: infections, pneumonia, MI, pancreatitis, etc)
Hyperglycemia
(Very high blood [glucose], higher than in DKA)
When blood [glucose] > 12mmol/L, glucose filtration > reabsorption, ↑ urine [glucose]
Glucosuria
Glucose in filtrate promotes osmotic diuresis: large- volume urine output
Polyuria
Dehydration
(↓ JVP, orthostasis: postural hypotension/ postural tachycardia, ↑ resting HR)
Some insulin still present, but not enoughsome glucose is utilized by muscle/fat cells, some remain in the blood
Cells not “starved”, but still need more energy
↑ release of Catabolic hormones: Glucagon, Epinephrine, Cortisol, GH
Body tries to ↑ blood [glucose], to hopefully ↑ cell glucose absorption
Hypothalamic cells sense low intra-cellular glucose, triggering feelings of hunger
Polyphagia
Note: the presence of some insulin directly inhibits lipolysis; thus, in HHS there is no ketone body production, and no subsequent metabolic acidosis and ketouria (unlike in DKA). If ketones are detected in an HHS patient it’s likely secondary to starvation or other mechanisms.
↓ ECF volume, ↑ ECF osmolarity (i.e. hypernatremia)
↑ Gluconeogenesis ↑ Glycogenolysis (in liver)
↓ Protein synthesis, ↑ proteolysis
(in muscle)
↑ Gluconeogenic substrates for liver If the patient doesn’t drink enough
water to replenish lost blood volume If pt is alert and
Electrolyte imbalance
water is accessible
Water osmotically leaves neurons, shrinking them
Neural damage: delirium, lethargy, seizure, stupor, coma
↓ renal perfusion, ↓ GFR
Renal Failure
(pre-renal cause; see relevant slides)
Polydipsia Note: in HHS, body K+ is lost via osmotic diuresis. But diffusion of K+ out of cells
may cause serum [K+] to be falsely normal/elevated. To prevent hypokalemia, give IV KCl along with IV insulin as soon as serum K+ <5.0mmol/L. But ensure patient has good renal function/urine output first, to avoid iatrogenic hyperkalemia!
Note: Electrolyte imbalances (i.e. hyperkalemia, hypernatremia) are worsened by the acute renal failure commonly coexisting with DKA/HHS
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 3, 2016 on www.thecalgaryguide.com
Hyperosmolar Hyperglycemic State (HHS)
Note: HHS is only seen in Type II DM patients!
Note: In patients with either DKA or HHS, always look for an underlying cause (i.e. an infection)
Author: Yan Yu Reviewers:
Peter Vetere
Gill Goobie
Hanan Bassyouni* * MD at time of publication
Alters total body water & ion osmosis
Inadequate insulin production, insulin resistance, non- adherence to insulin Tx
Relative Insulin deficit
Stresses that ↑ Insulin demand: infections, pneumonia, MI, pancreatitis, etc)
Hyperglycemia
(Very high blood [glucose], higher than in DKA)
When blood [glucose] > 12mmol/L, glucose filtration > reabsorption, ↑ urine [glucose]
Glucosuria
Glucose in filtrate promotes osmotic diuresis: large- volume urine output
Polyuria
Dehydration
(↓ JVP, orthostasis: postural hypotension/ postural tachycardia, ↑ resting HR)
Some insulin still present, but not enoughsome glucose is utilized by muscle/fat cells, some remain in the blood
Cells not “starved”, but still need more energy
↑ release of Catabolic hormones: Glucagon, Epinephrine, Cortisol, GH
Body tries to ↑ blood [glucose], to hopefully ↑ cell glucose absorption
Hypothalamic cells sense low intra-cellular glucose, triggering feelings of hunger
Polyphagia
Note: the presence of some insulin directly inhibits lipolysis; thus, in HHS there is no ketone body production, and no subsequent metabolic acidosis and ketouria (unlike in DKA). If ketones are detected in an HHS patient it’s likely secondary to starvation or other mechanisms.
↓ ECF volume, ↑ ECF osmolarity (i.e. hypernatremia)
↑ Gluconeogenesis ↑ Glycogenolysis (in liver)
↓ Protein synthesis, ↑ proteolysis
(in muscle)
↑ Gluconeogenic substrates for liver If the patient doesn’t drink enough
water to replenish lost blood volume If pt is alert and
Electrolyte imbalance
water is accessible
Water osmotically leaves neurons, shrinking them
Neural damage: delirium, lethargy, seizure, stupor, coma
↓ renal perfusion, ↓ GFR
Renal Failure
(pre-renal cause; see relevant slides)
Polydipsia Note: in HHS, body K+ is lost via osmotic diuresis. But diffusion of K+ out of cells
may cause serum [K+] to be falsely normal/elevated. To prevent hypokalemia, give IV KCl along with IV insulin as soon as serum K+ <5.0mmol/L. But ensure patient has good renal function/urine output first, to avoid iatrogenic hyperkalemia!
Note: Electrolyte imbalances (i.e. hyperkalemia, hypernatremia) are worsened by the acute renal failure commonly coexisting with DKA/HHS
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 3, 2016 on www.thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2015/05/Hyperosmolar-Hyperglycemic-State-HHS.jpg)
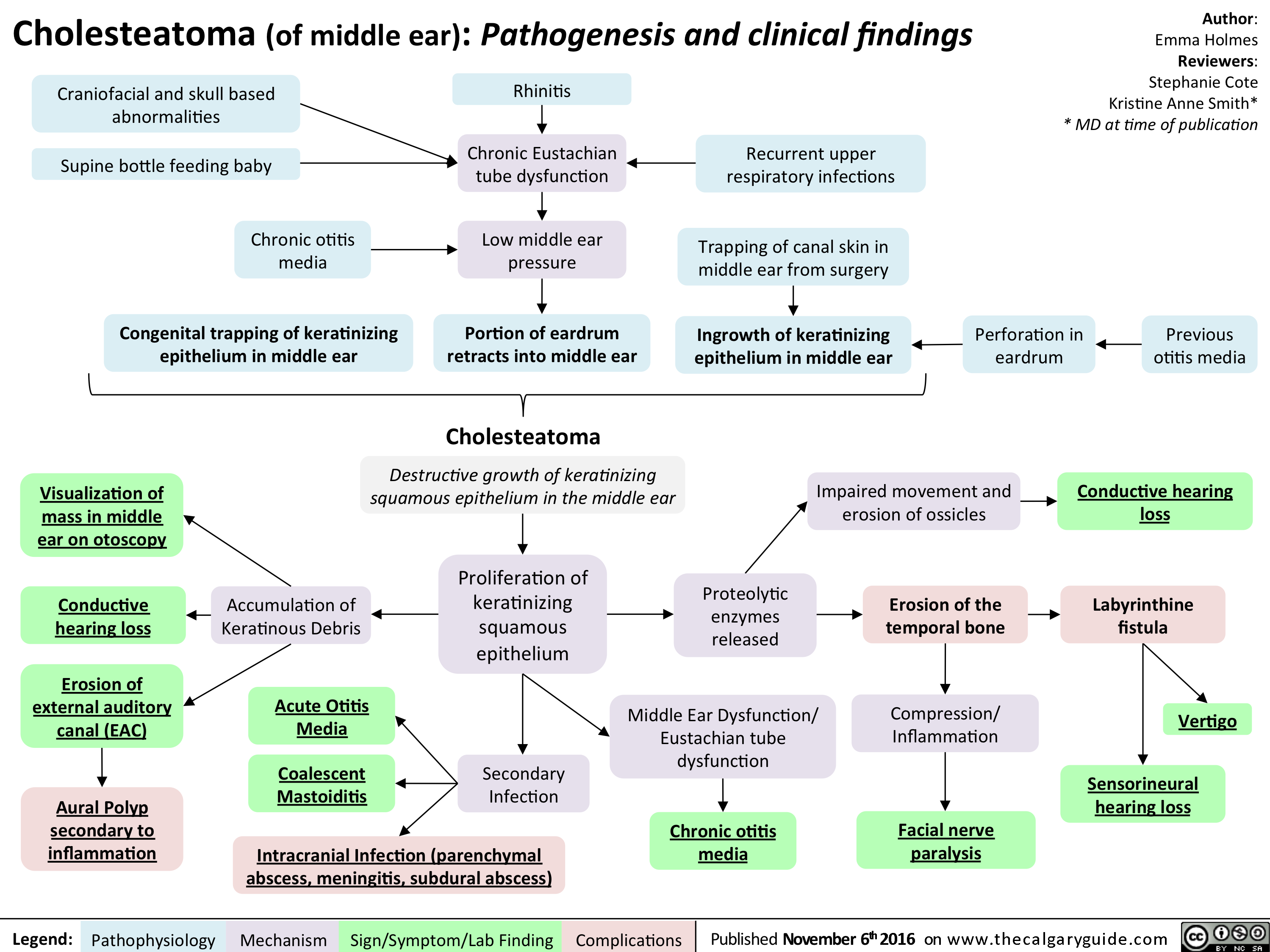
cholesteatoma-nov-4-2016_final-edits
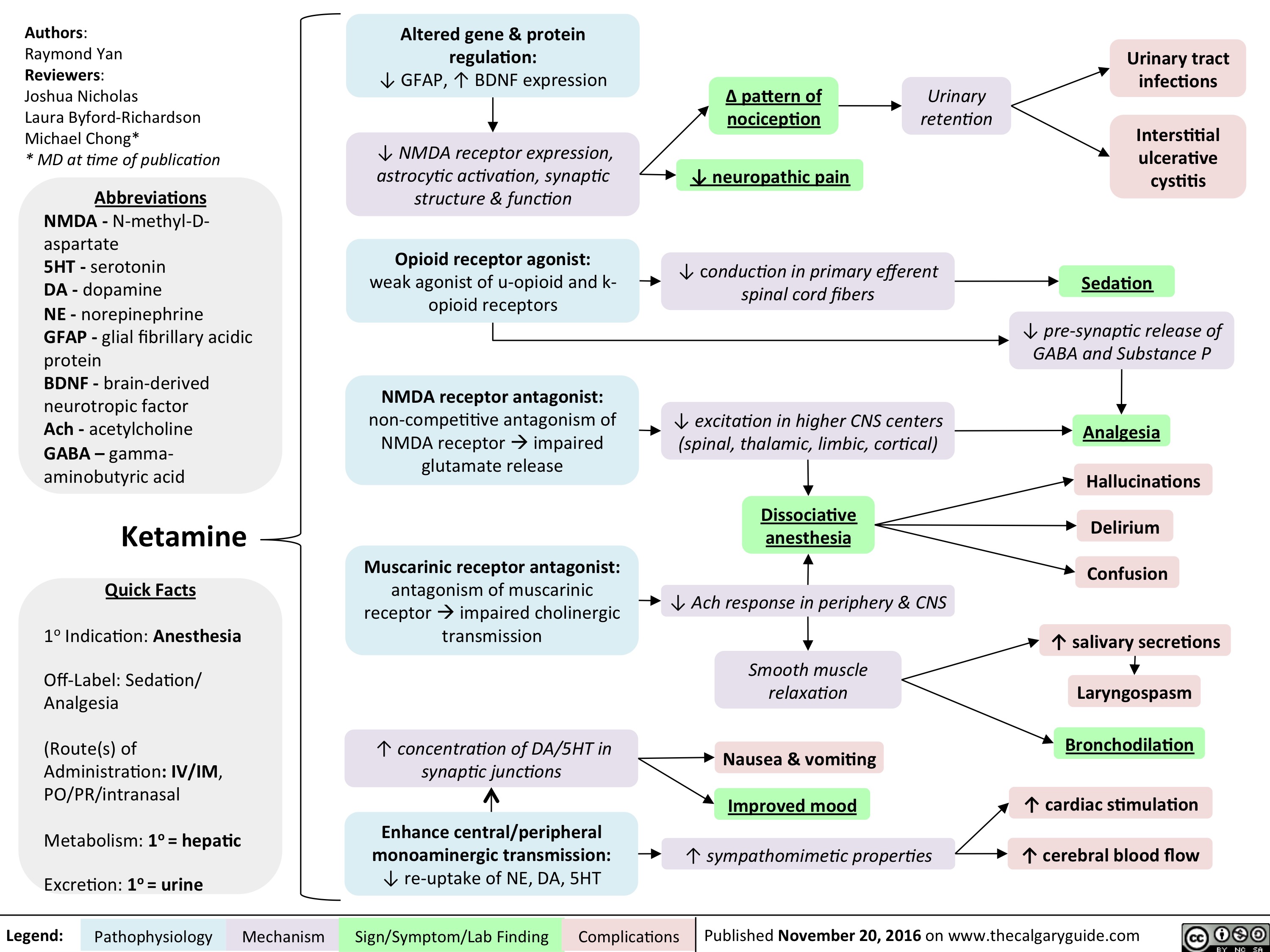
Ketamine
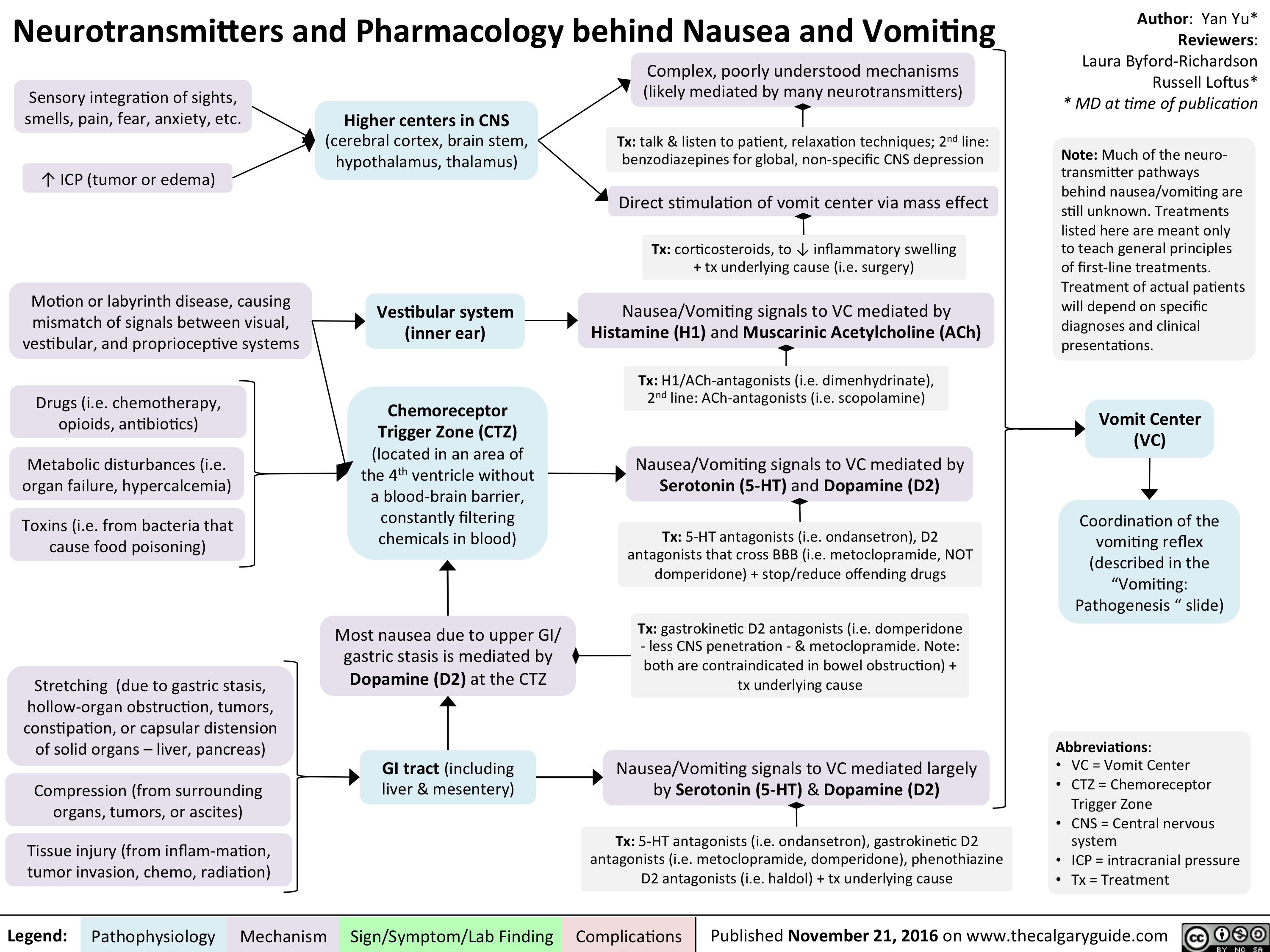
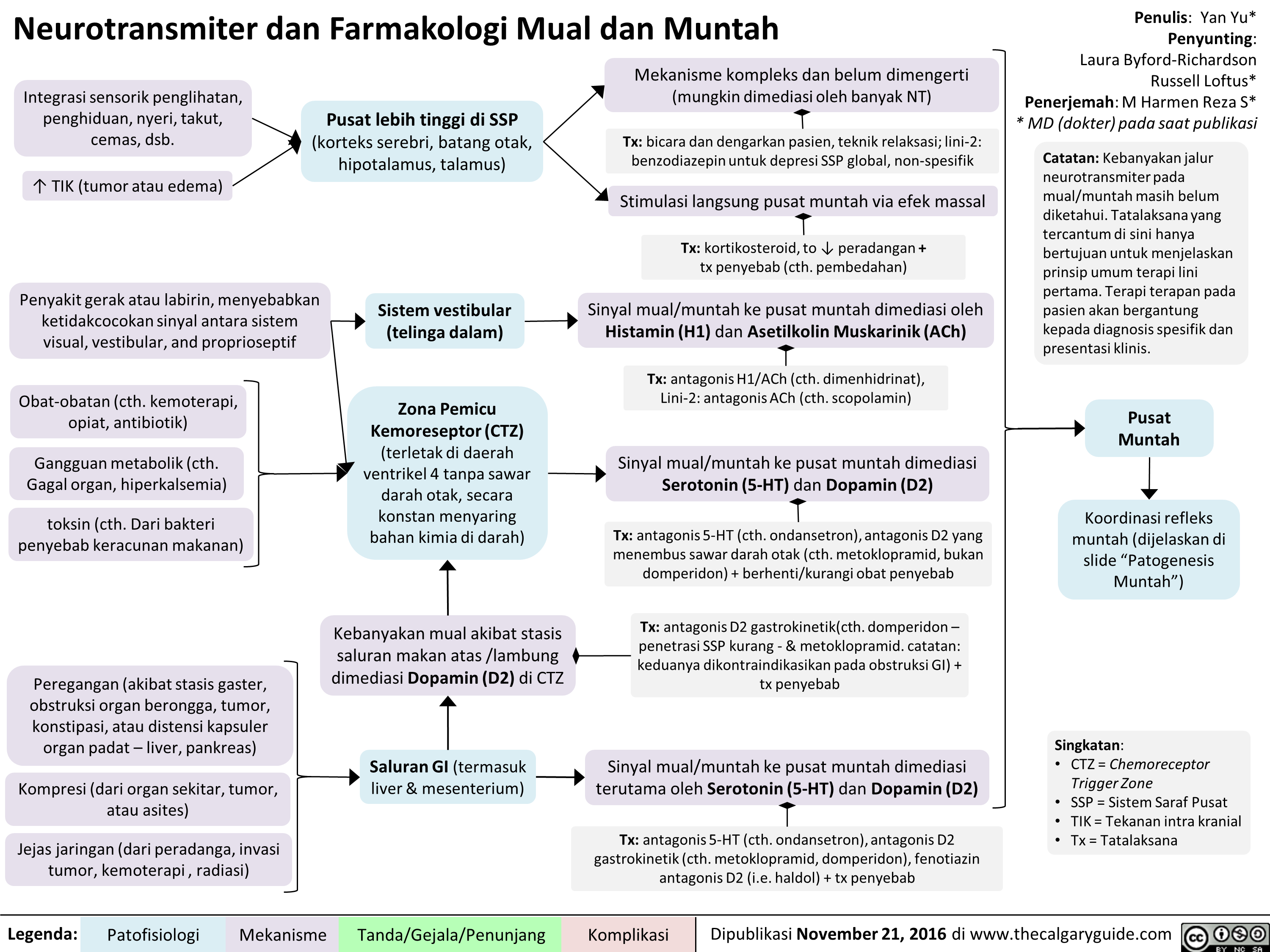
Neurotransmitters and Pharmacology behind Nausea and Vomiting
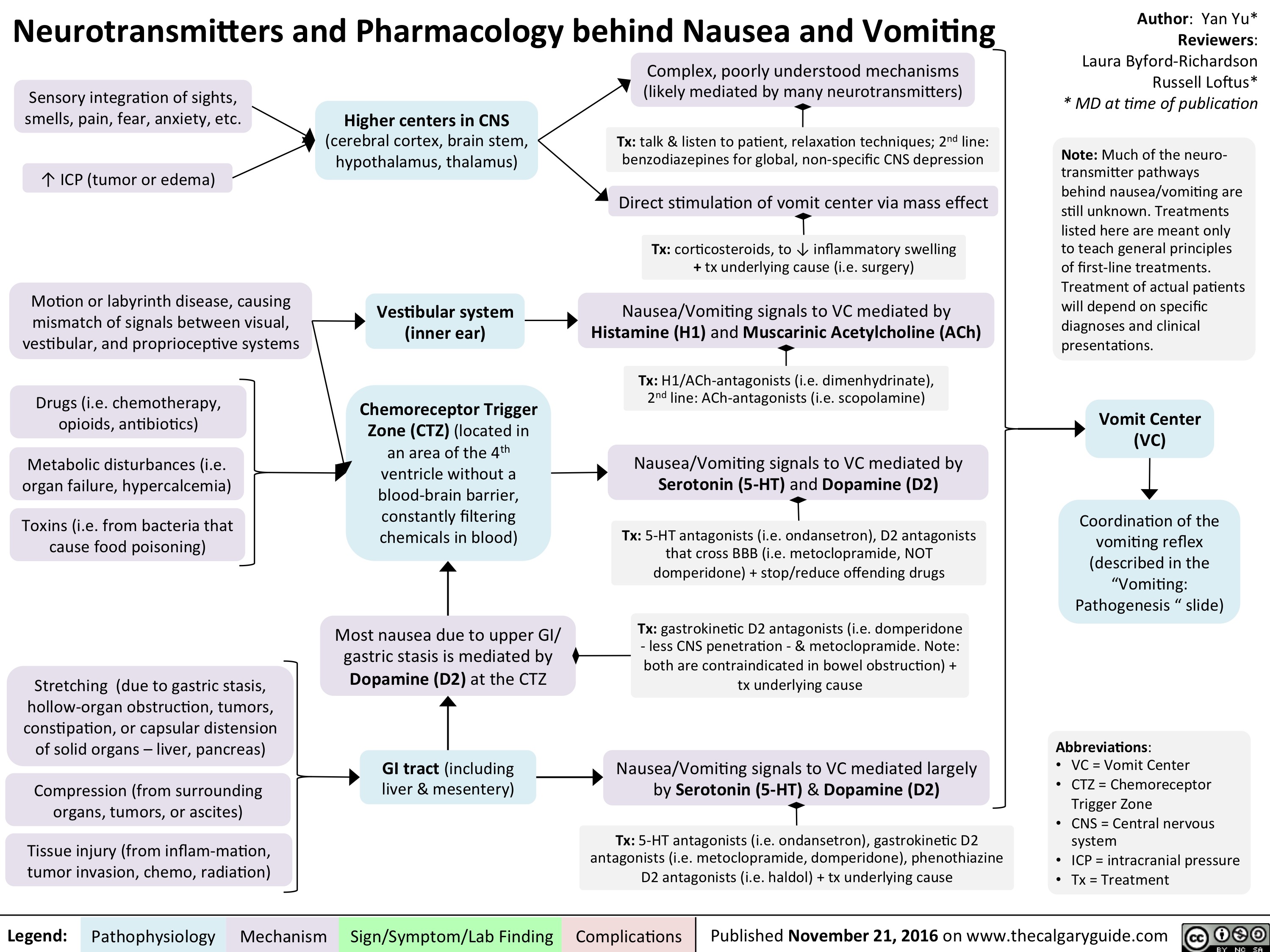
Neurotransmitters and Pharmacology behind Nausea and Vomiting
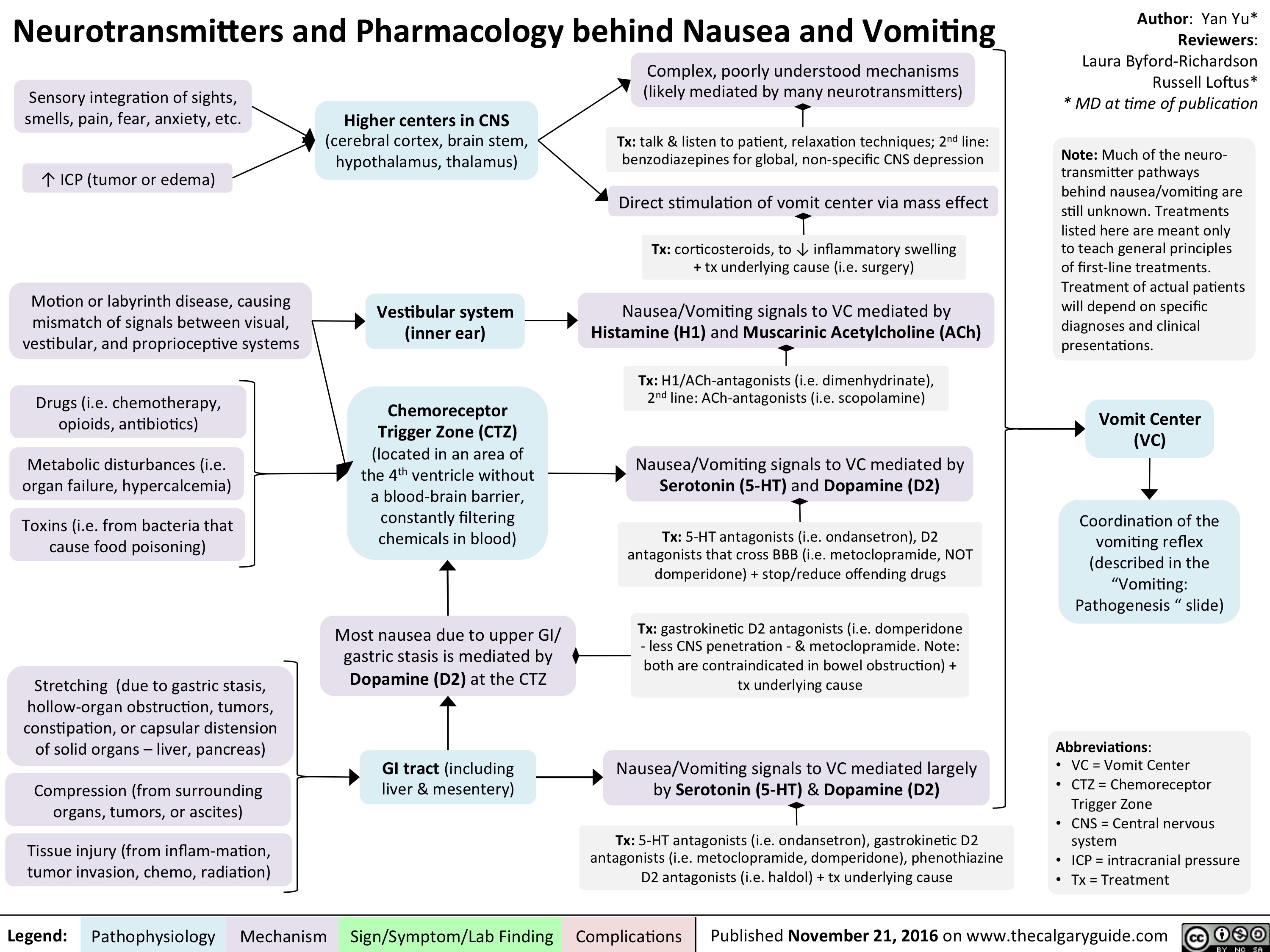
Neurotransmitters and Pharmacology behind Nausea and Vomiting
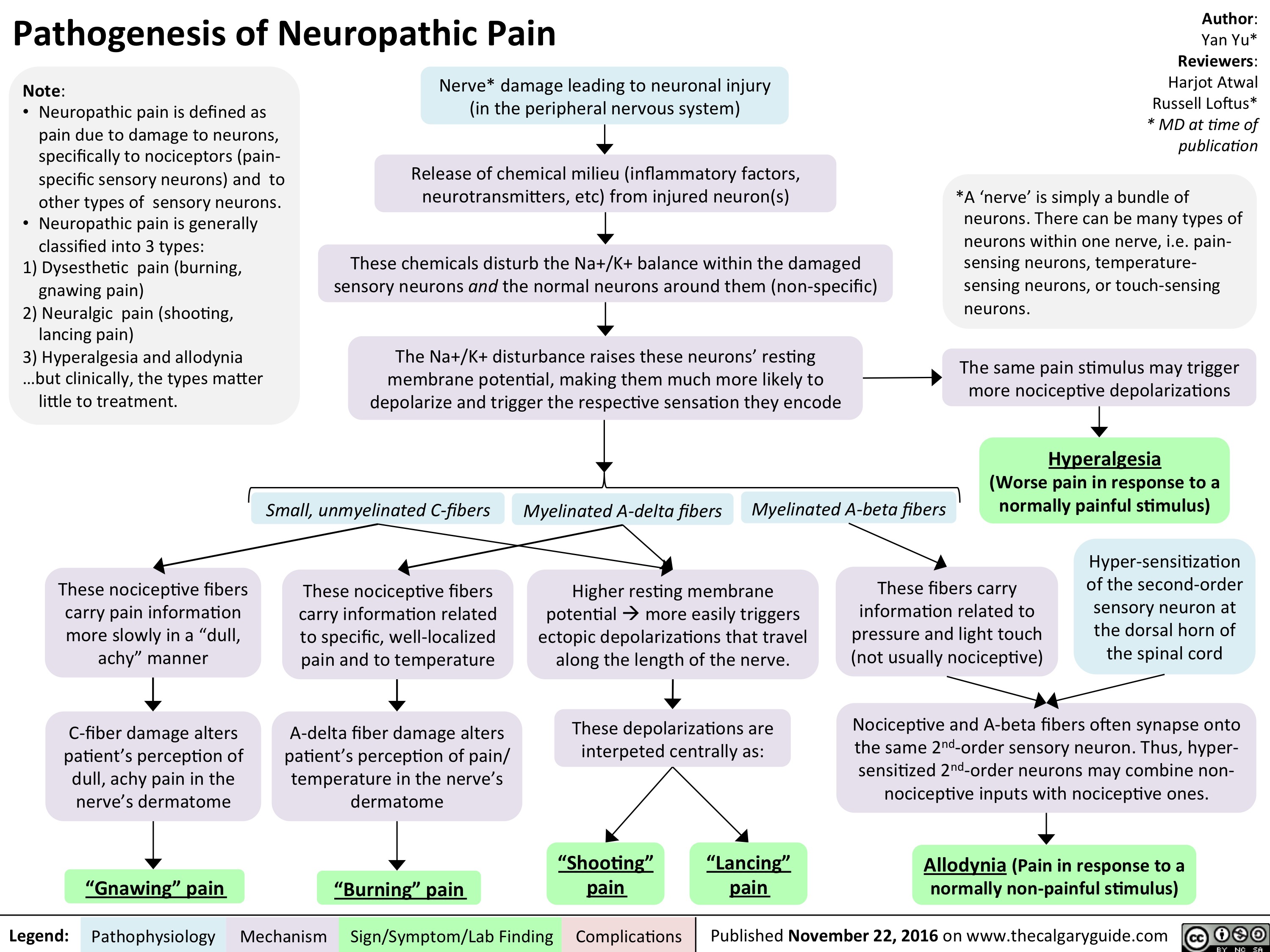
pathogenesis-of-neuropathic-pain
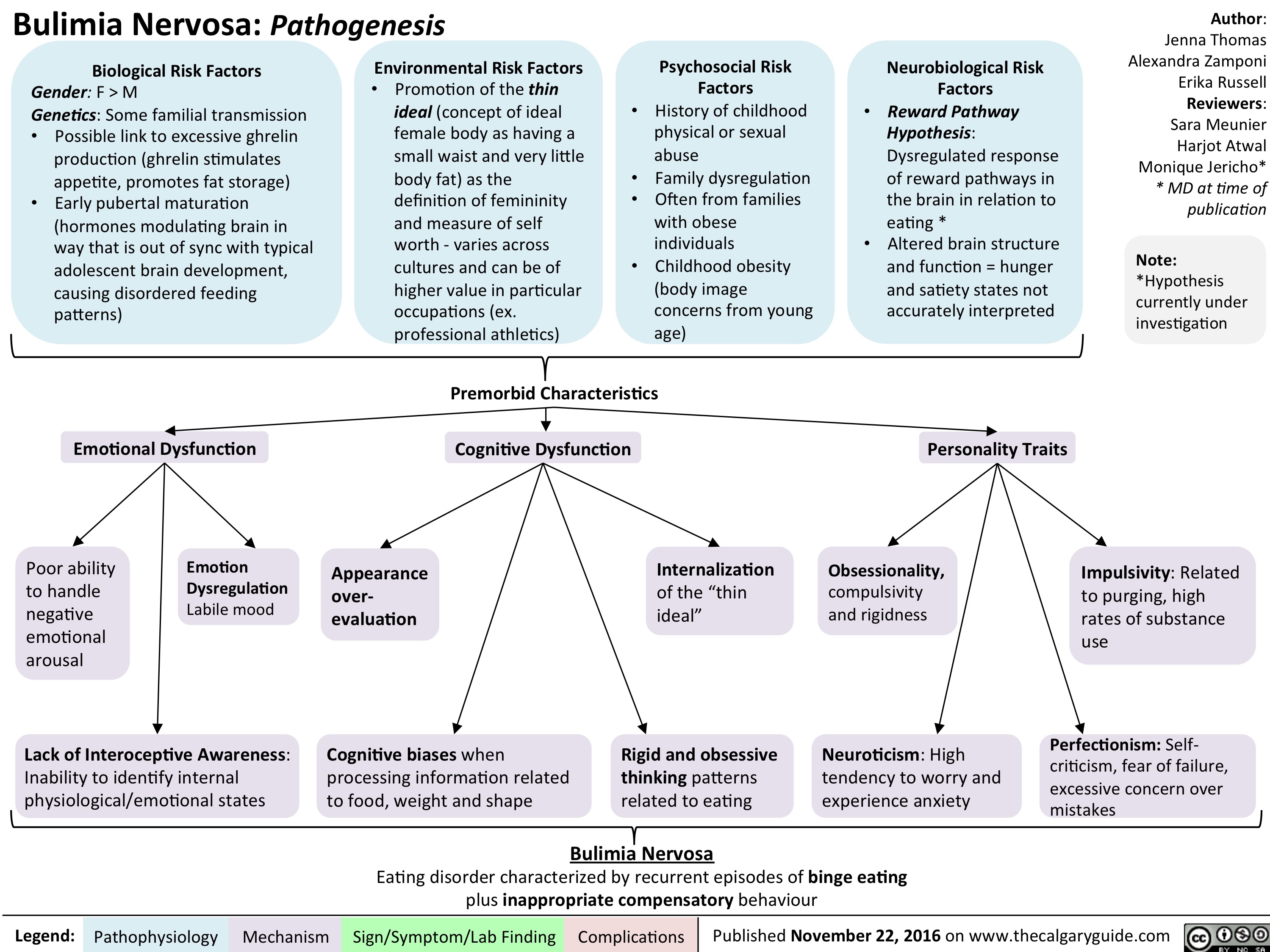
bn-pathogenesis
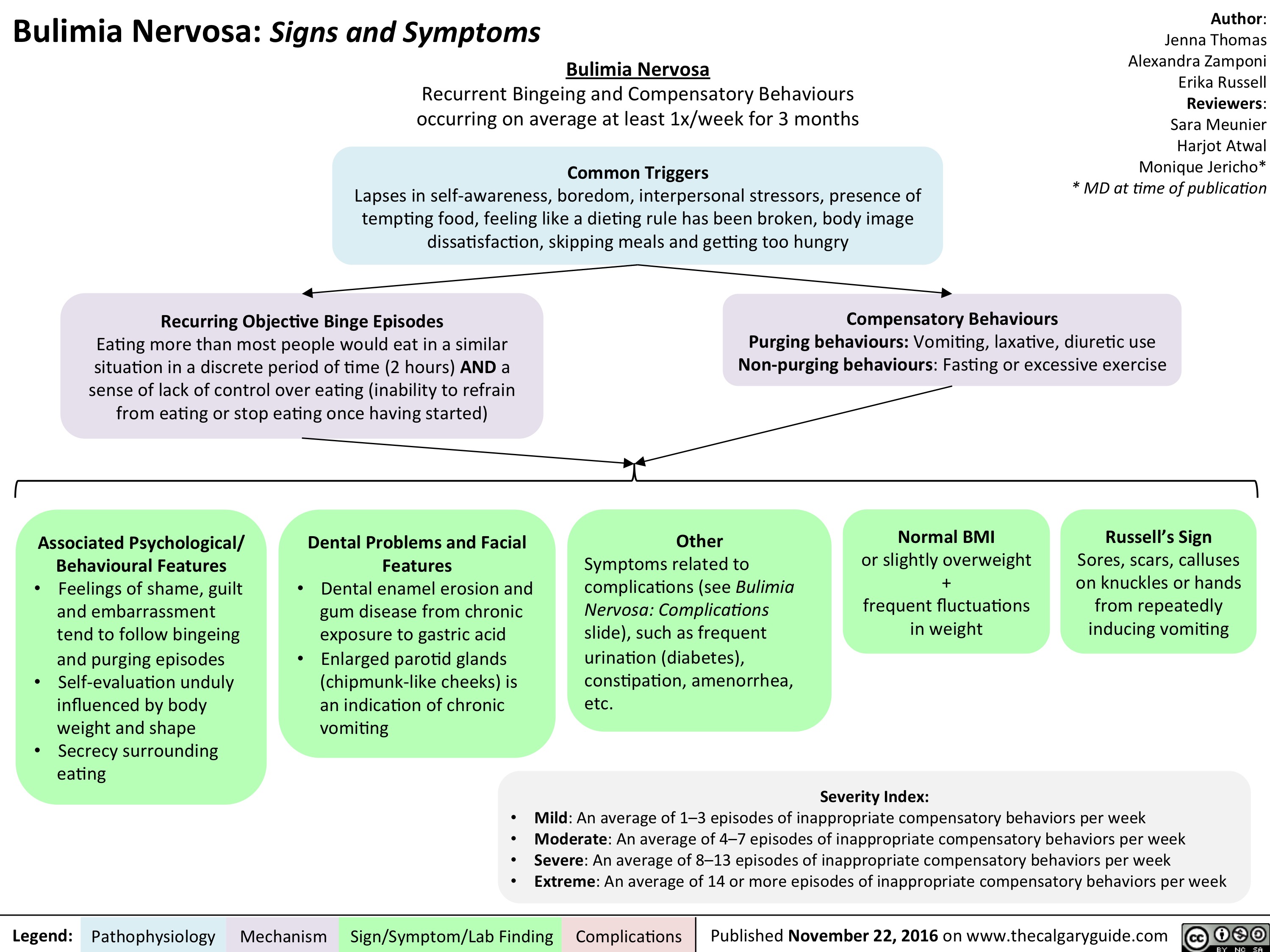
bn-signs-and-symptoms
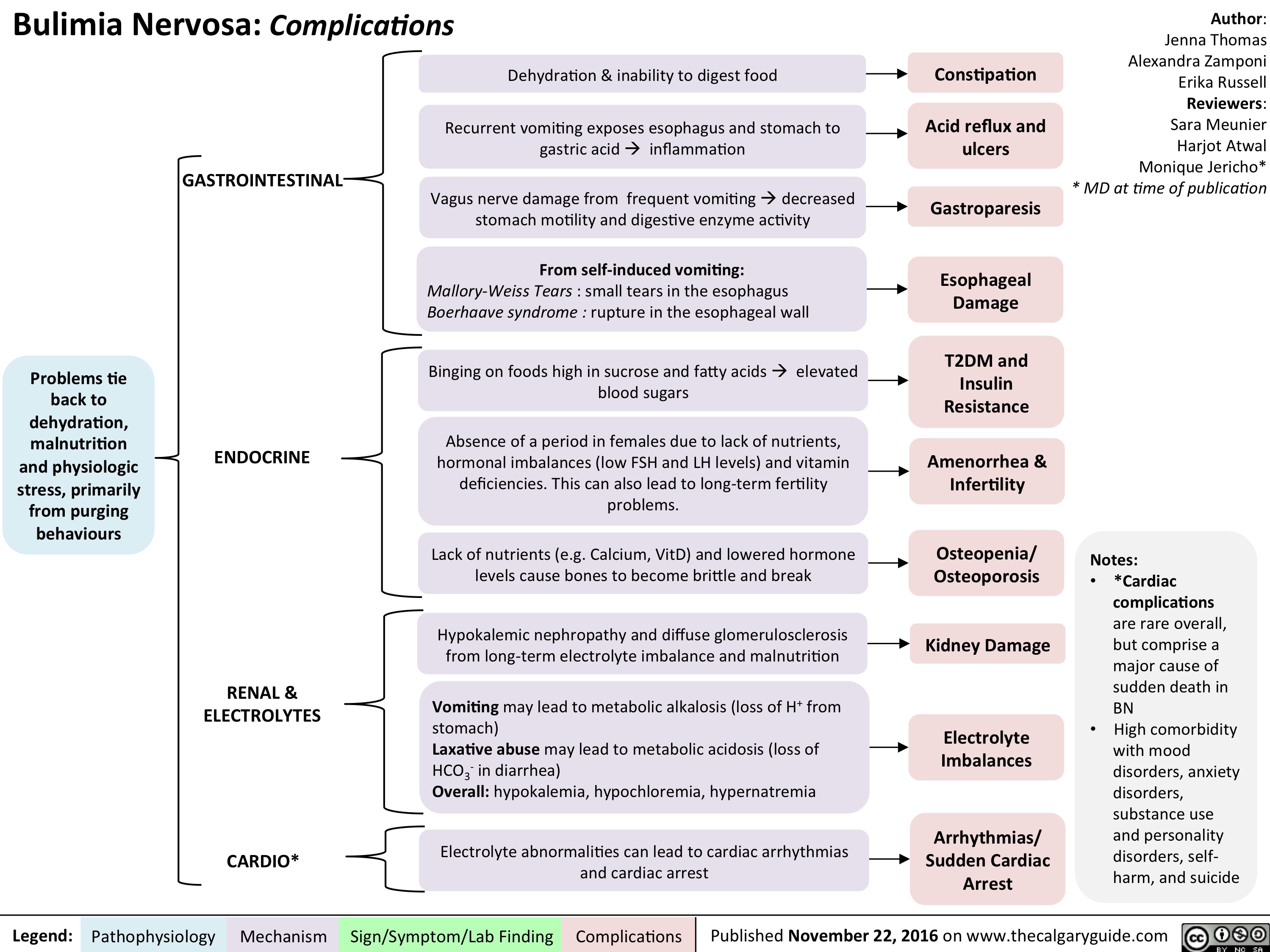
bn-complications
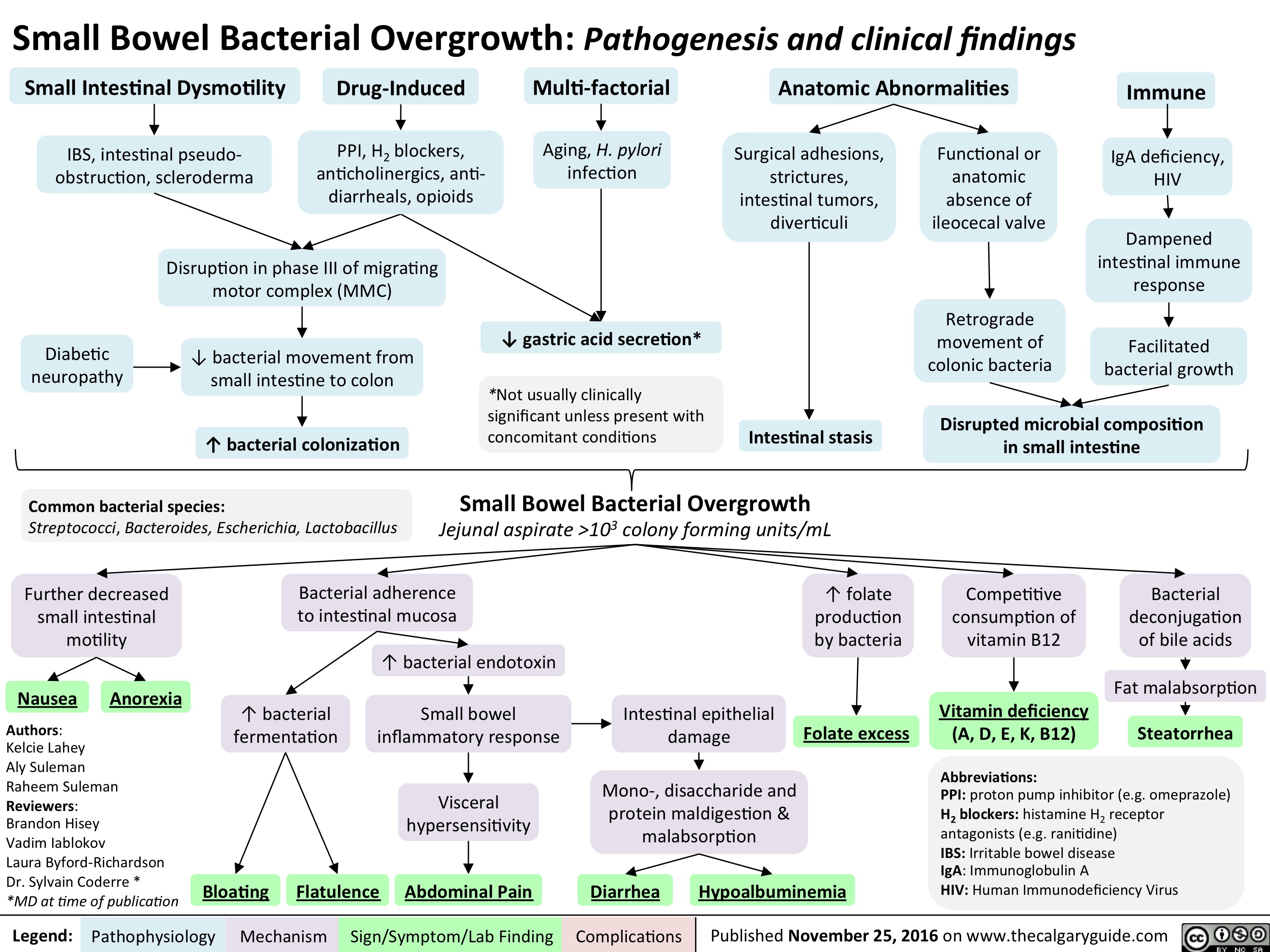
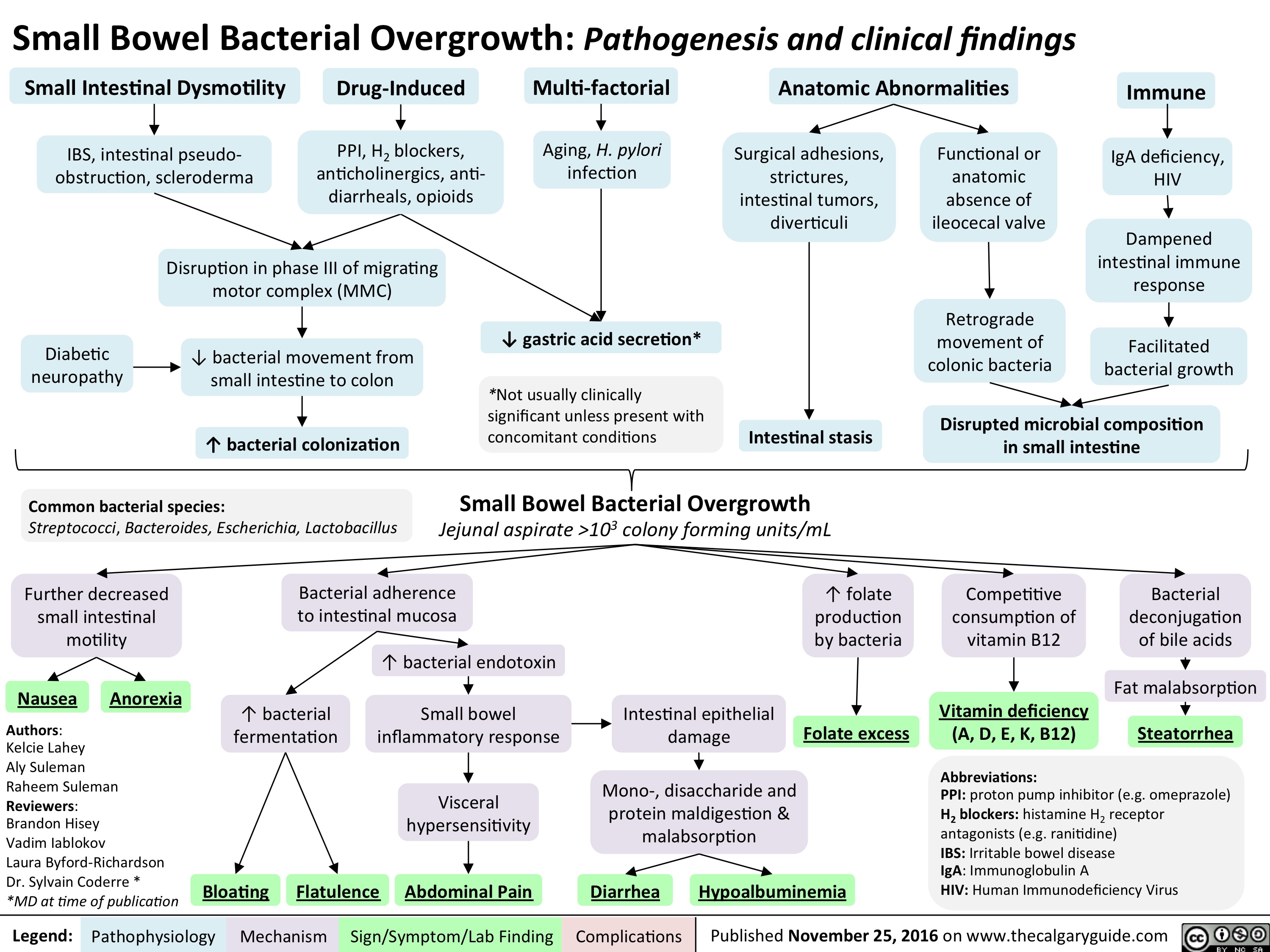
Small Bowel Bacterial Overgrowth: Pathogenesis and clinical findings
slide1
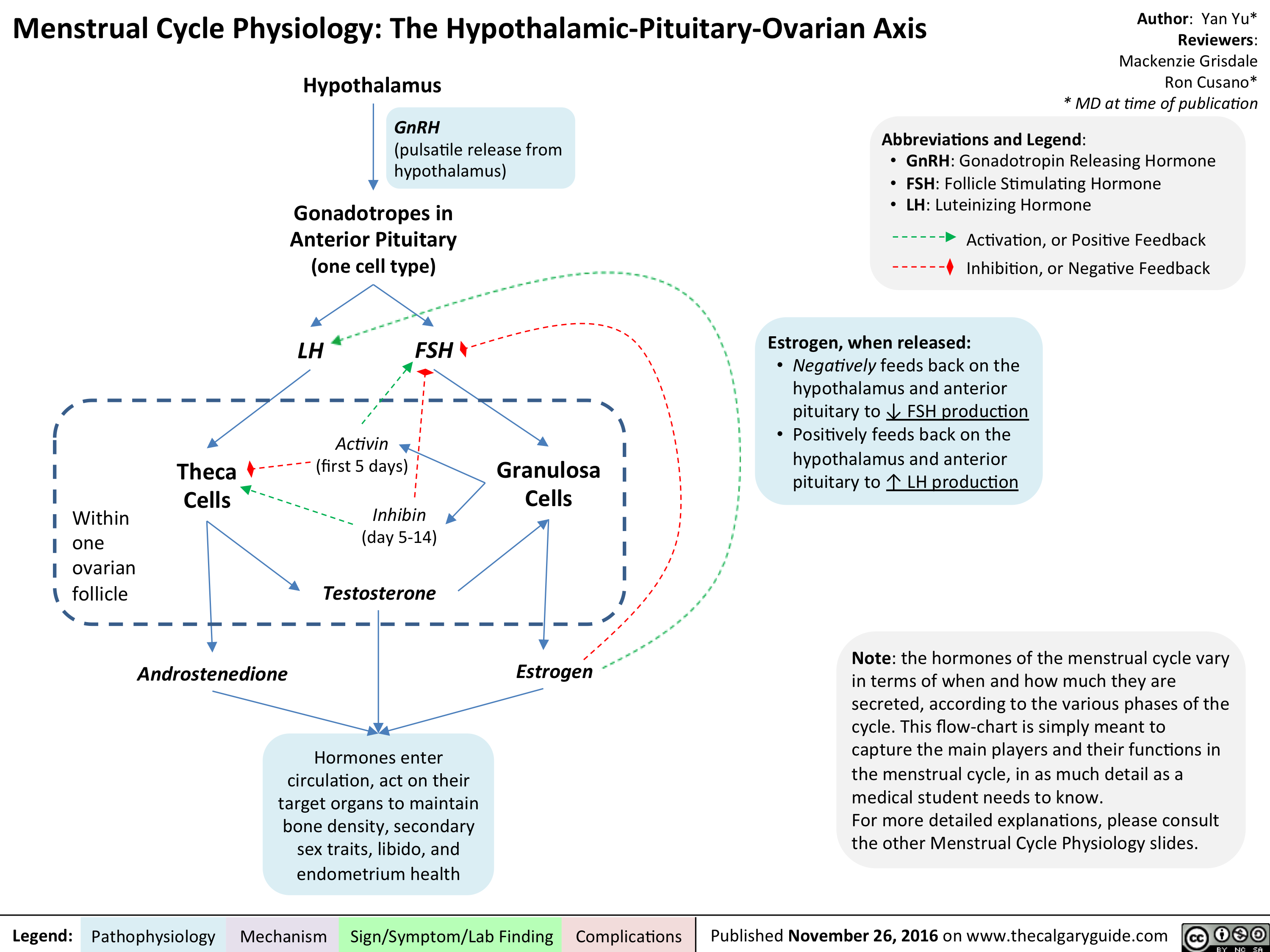
menstrual-cycle-physiology-the-hypothalamic-pituitary-ovarian-axis
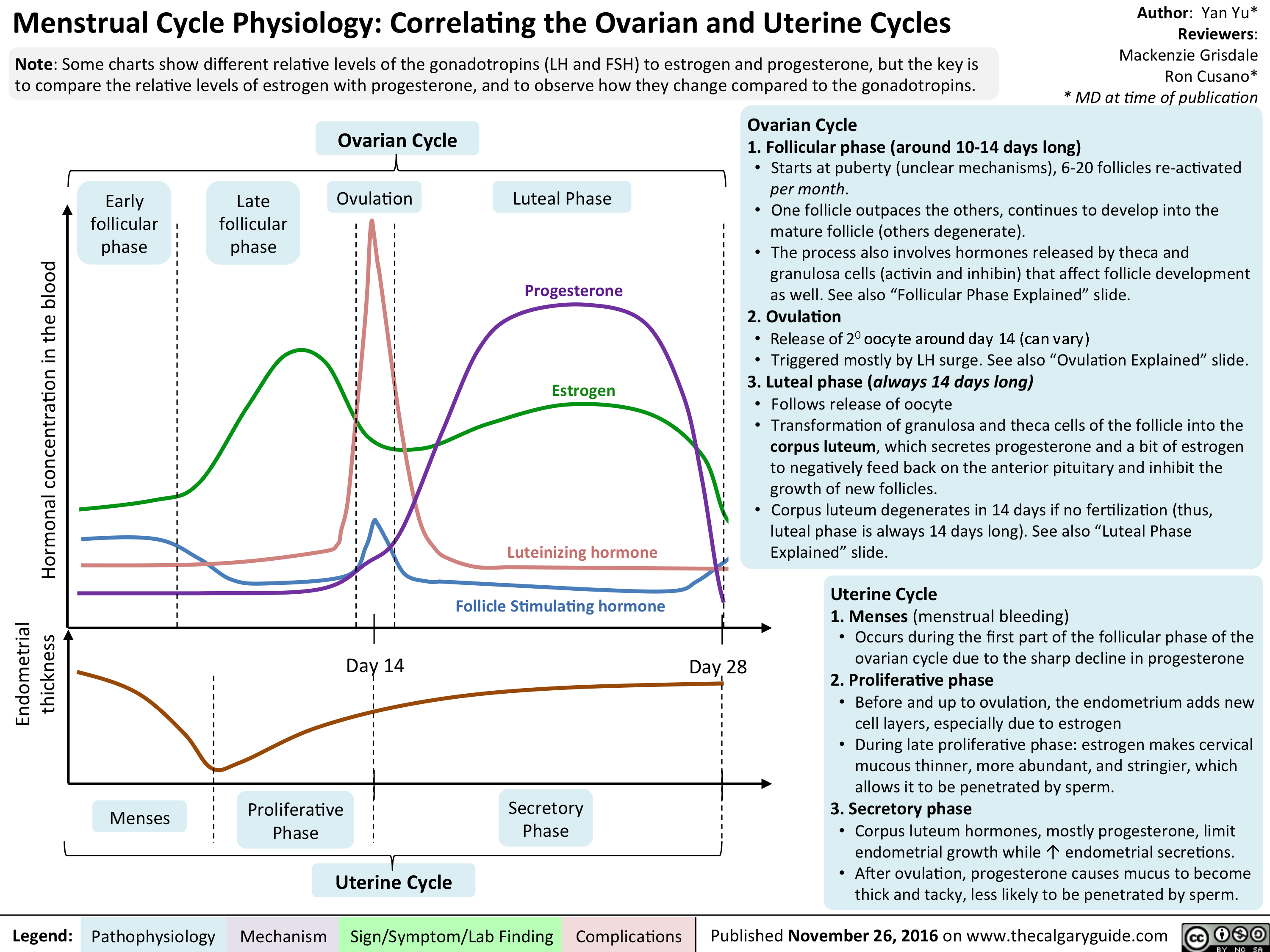
menstrual-cycle-physiology-correlating-the-ovarian-and-uterine-cycles
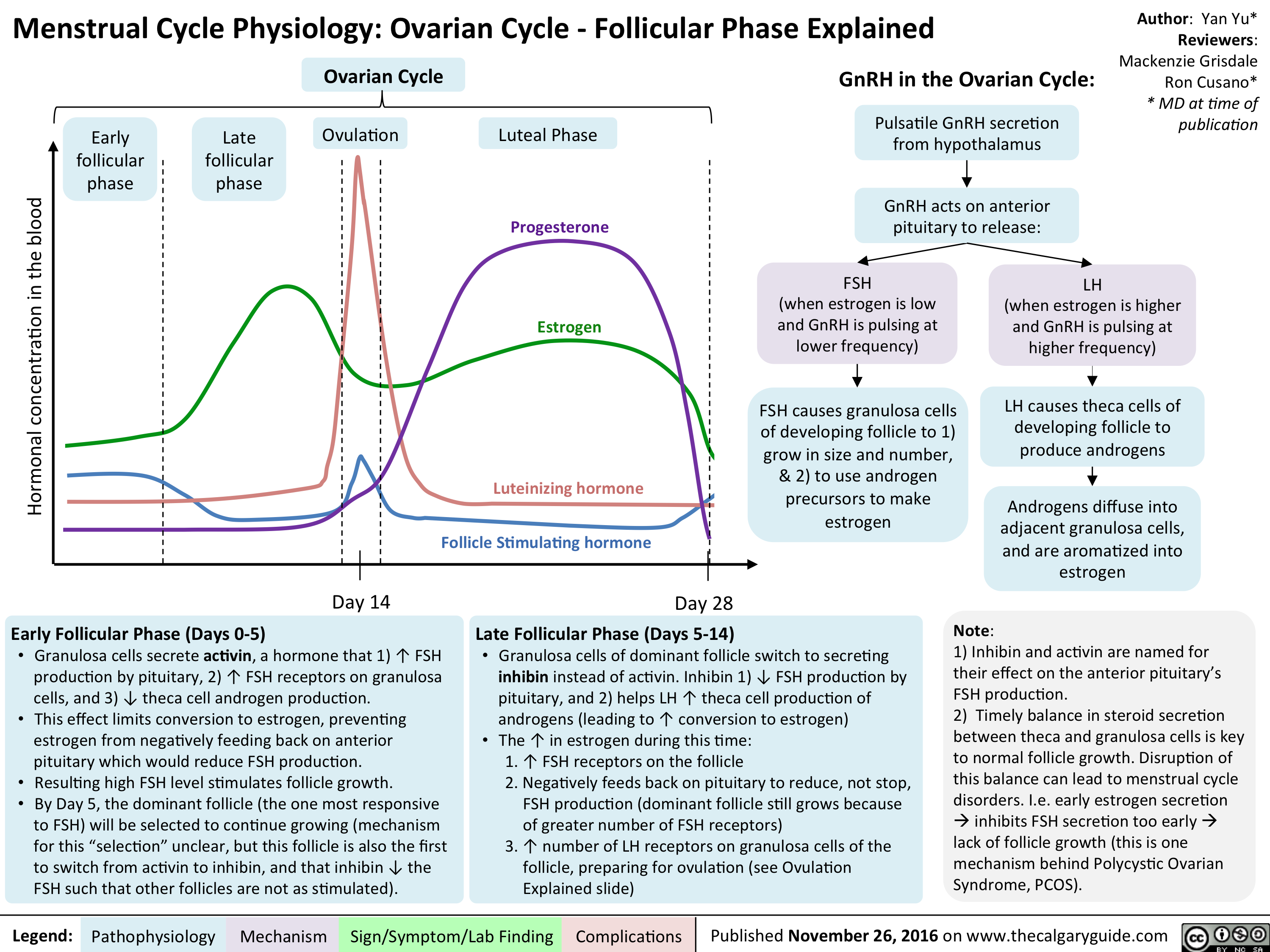
menstrual-cycle-physiology-ovarian-cycle-follicular-phase-explained
menstrual-cycle-physiology-ovarian-cycle-ovulation-explained

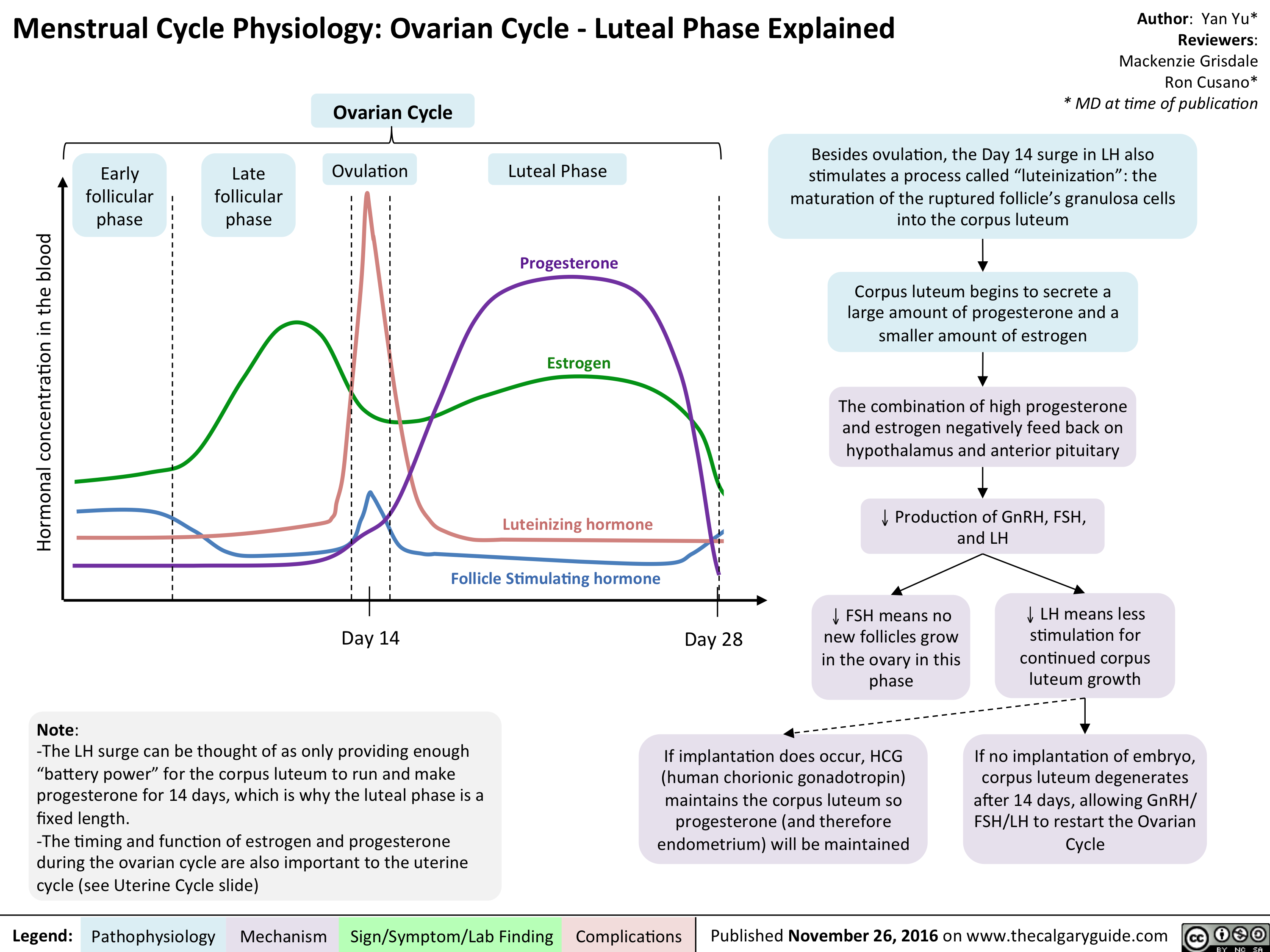
menstrual-cycle-physiology-ovarian-cycle-luteal-phase-explained
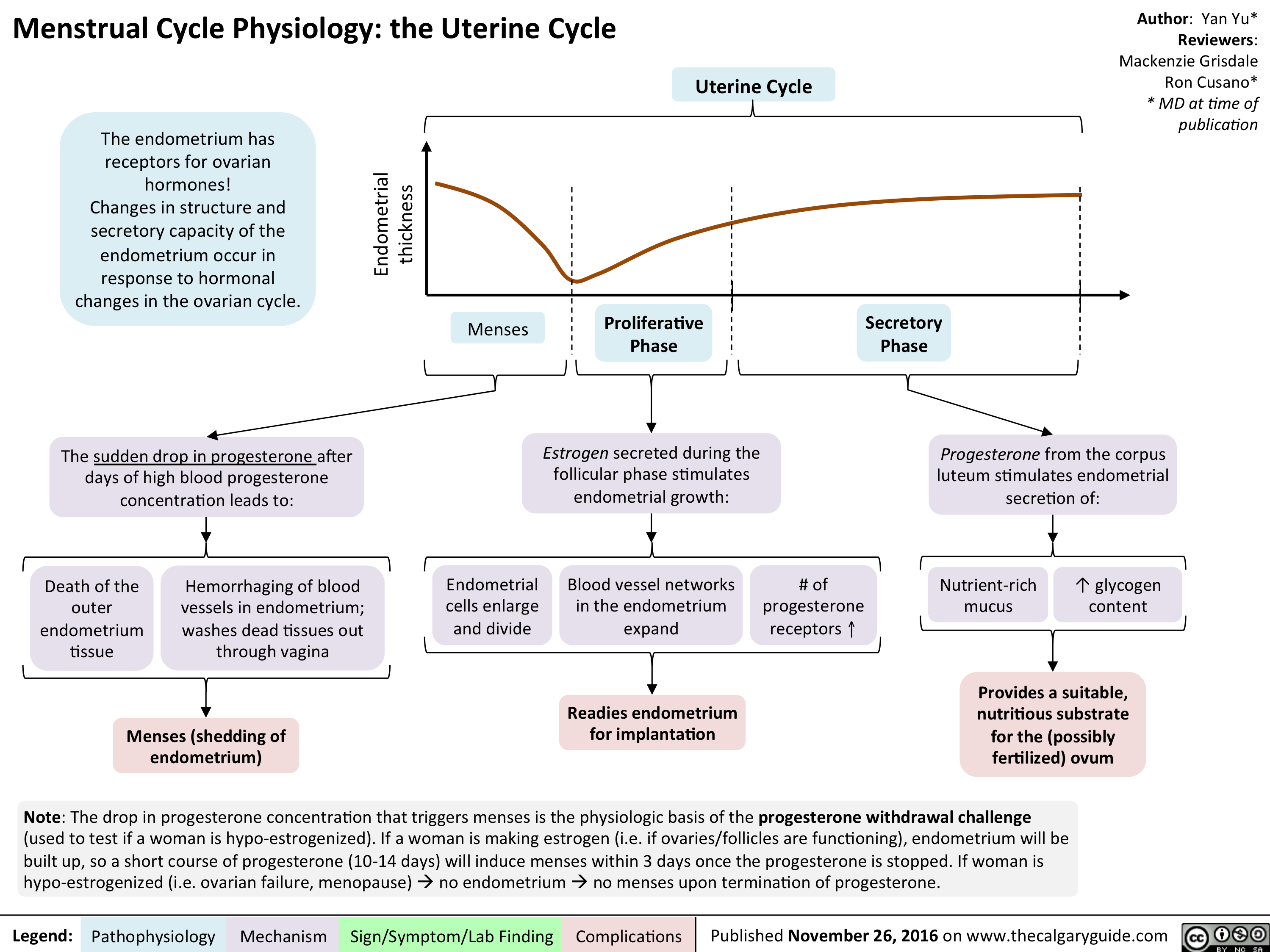
menstrual-cycle-physiology-the-uterine-cycle
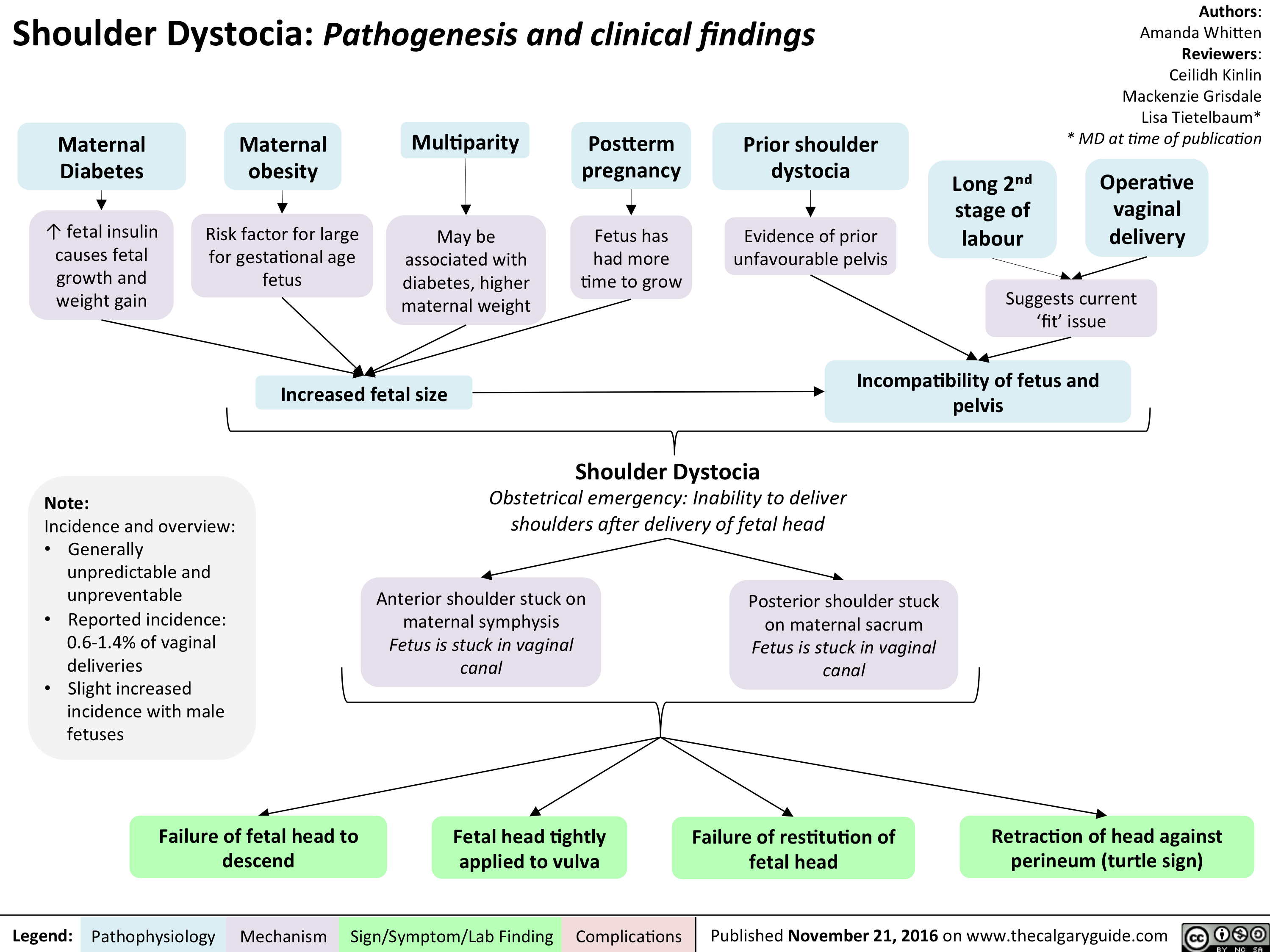
Shoulder Dystocia: Pathogenesis and Clinical Findings
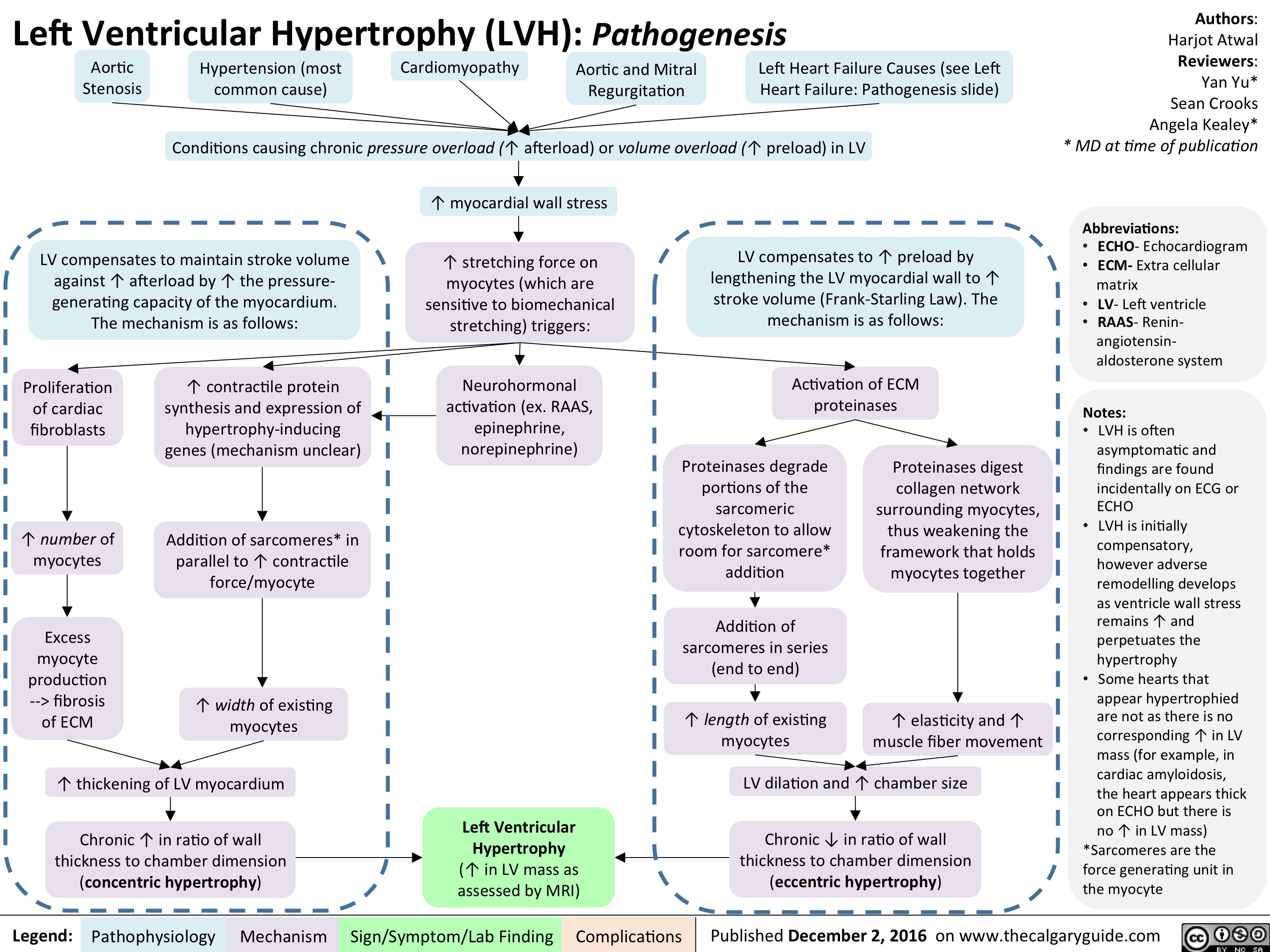
lvh-final
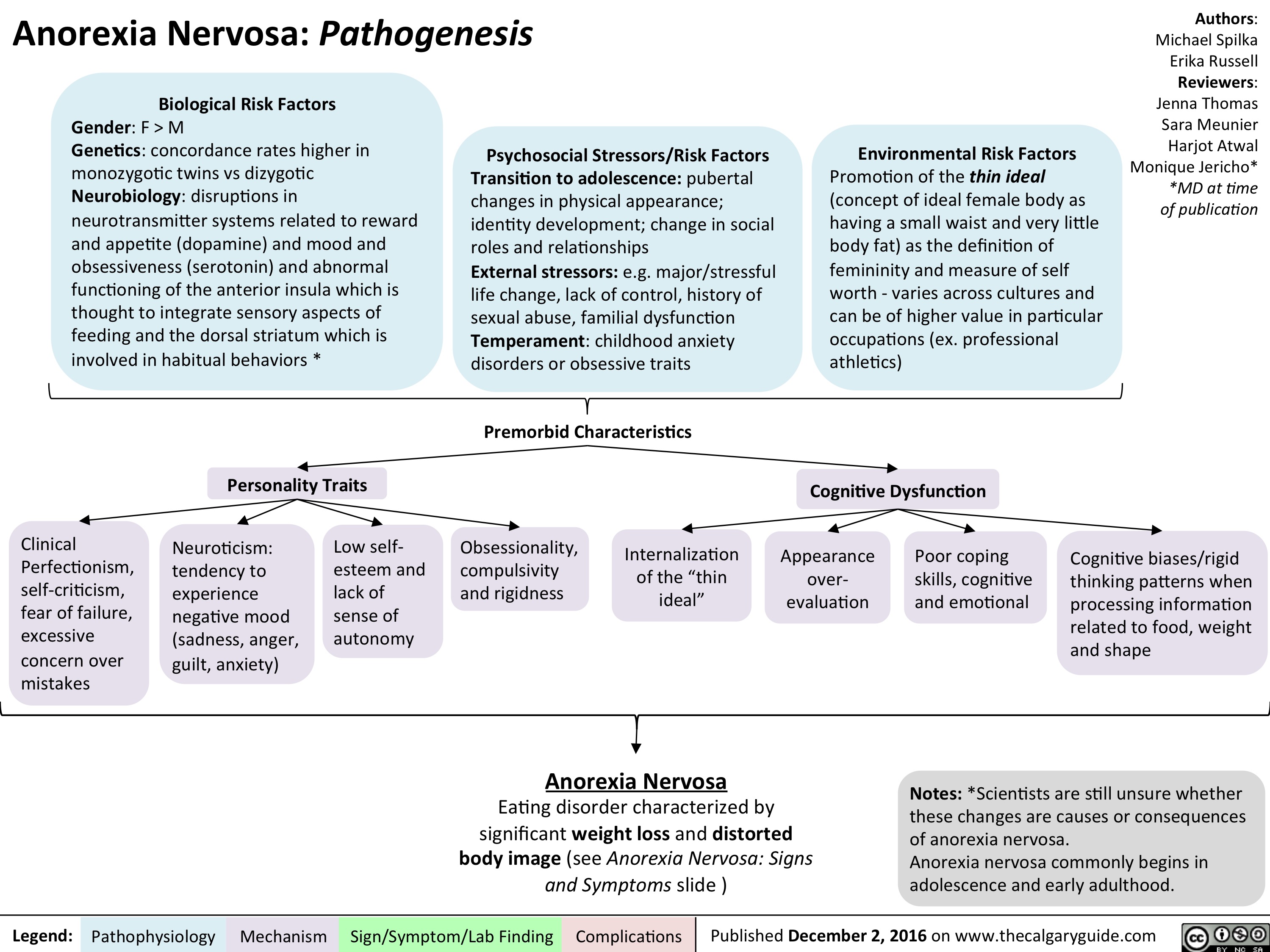
anorexia-nervosa
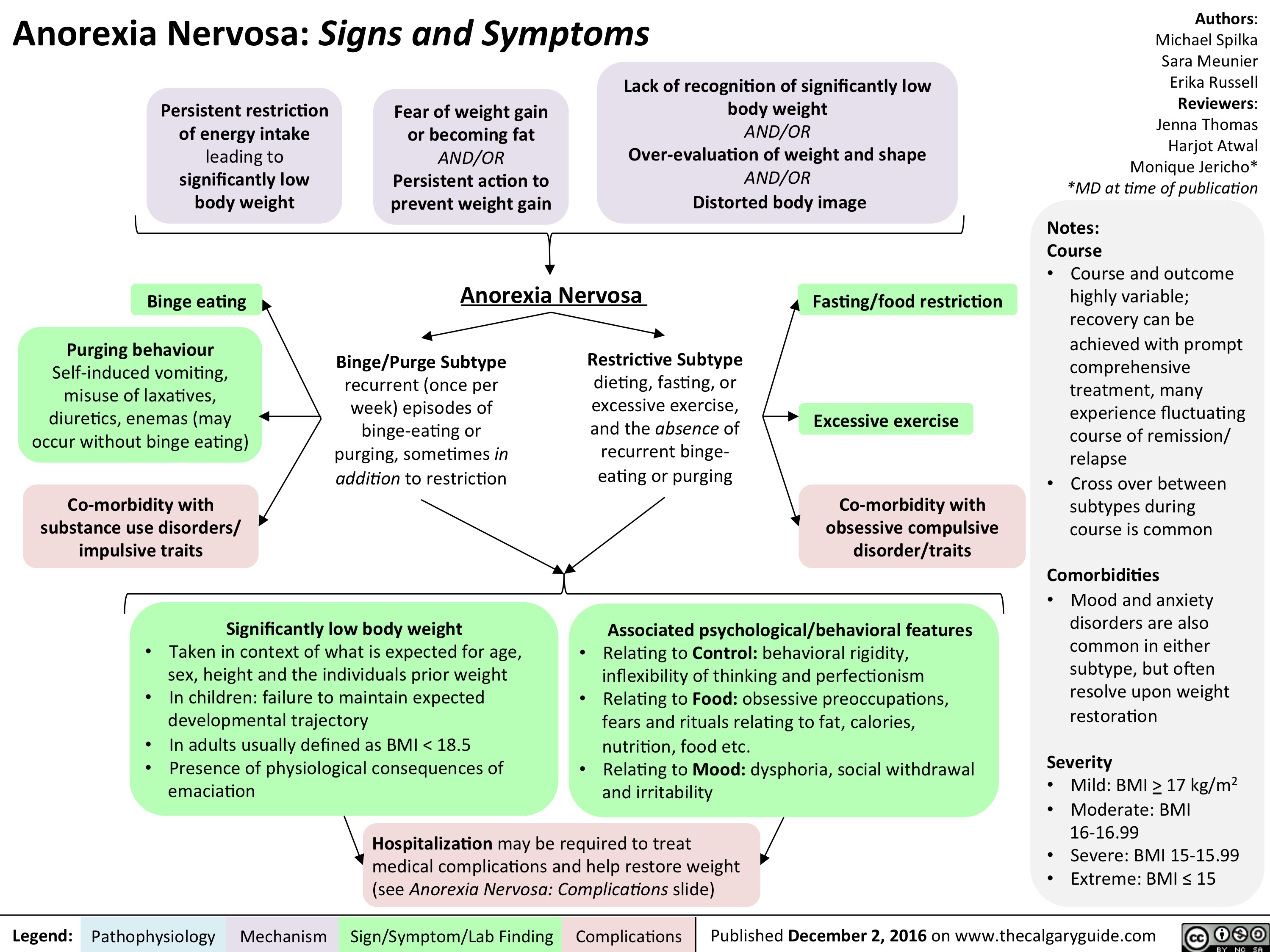
an-signs-and-symptoms
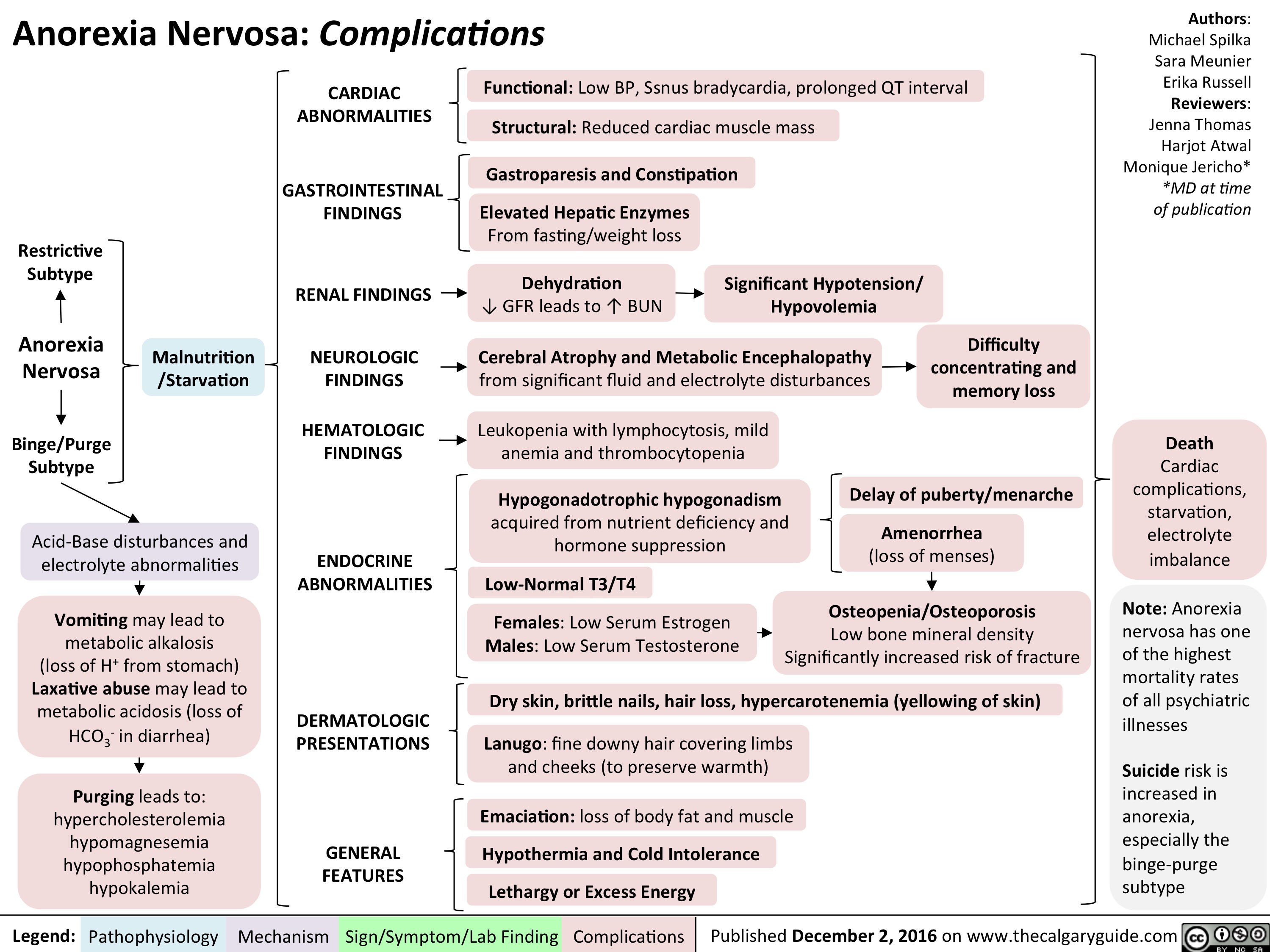
an-complications-final
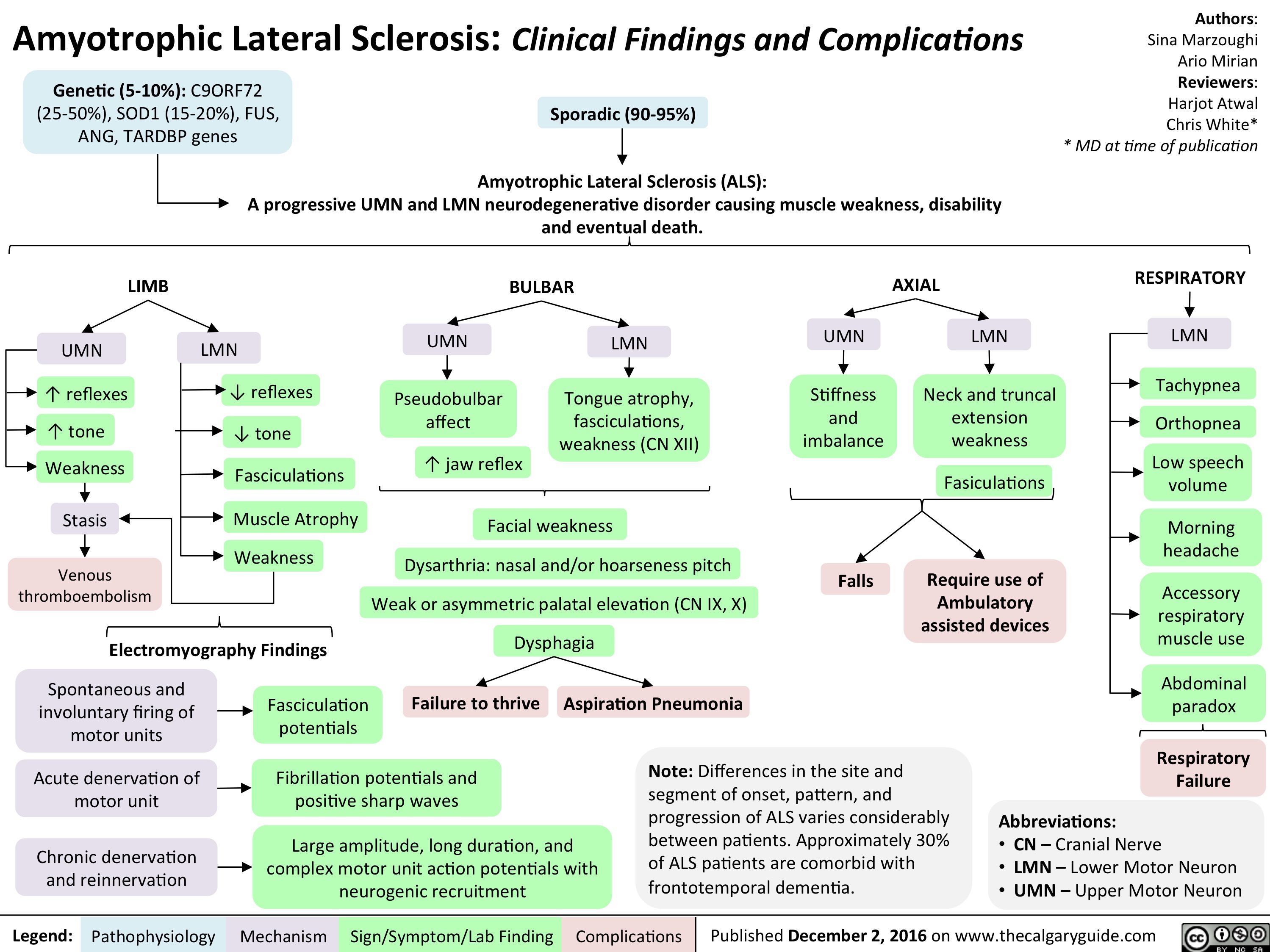
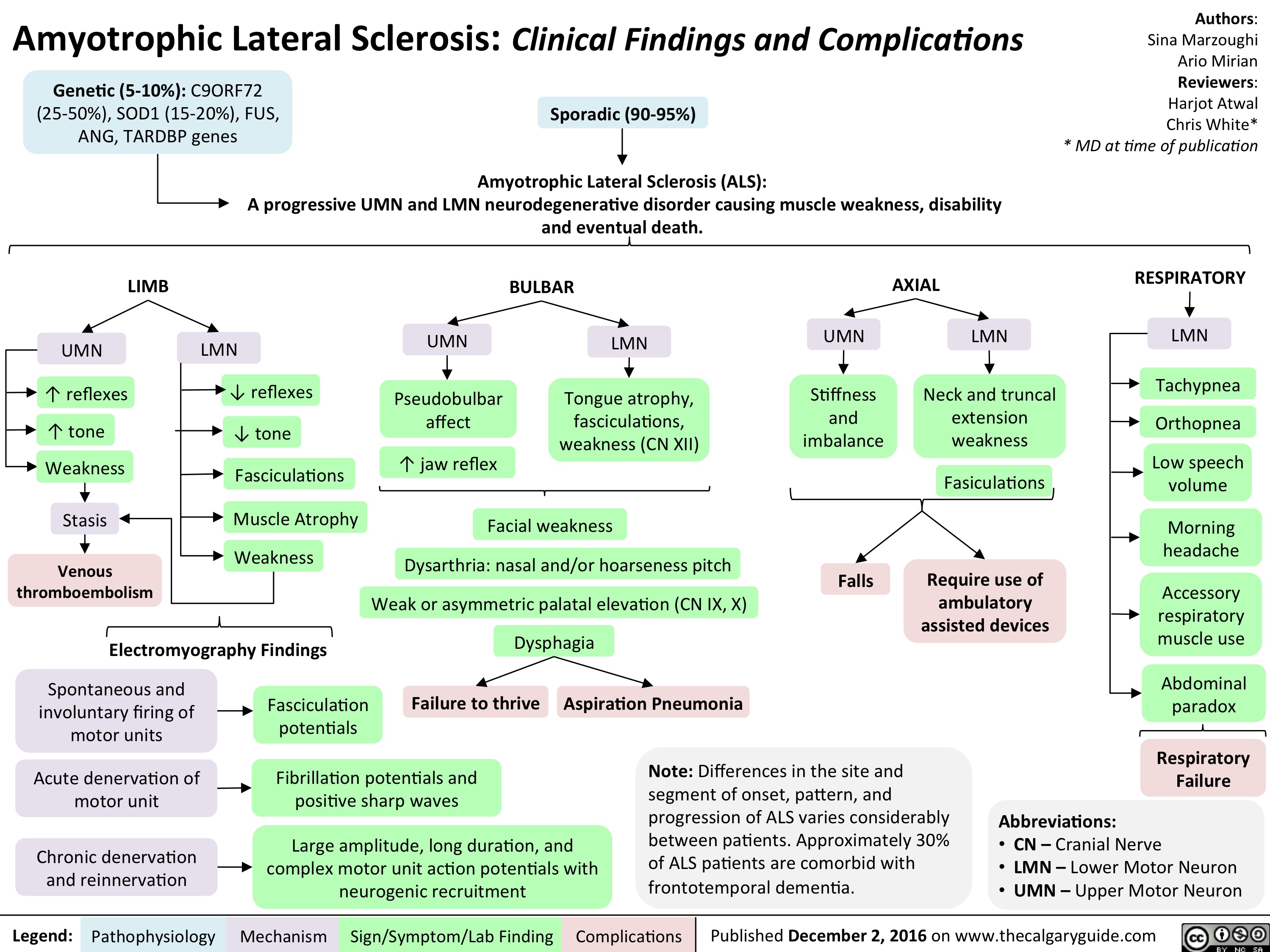
als-final
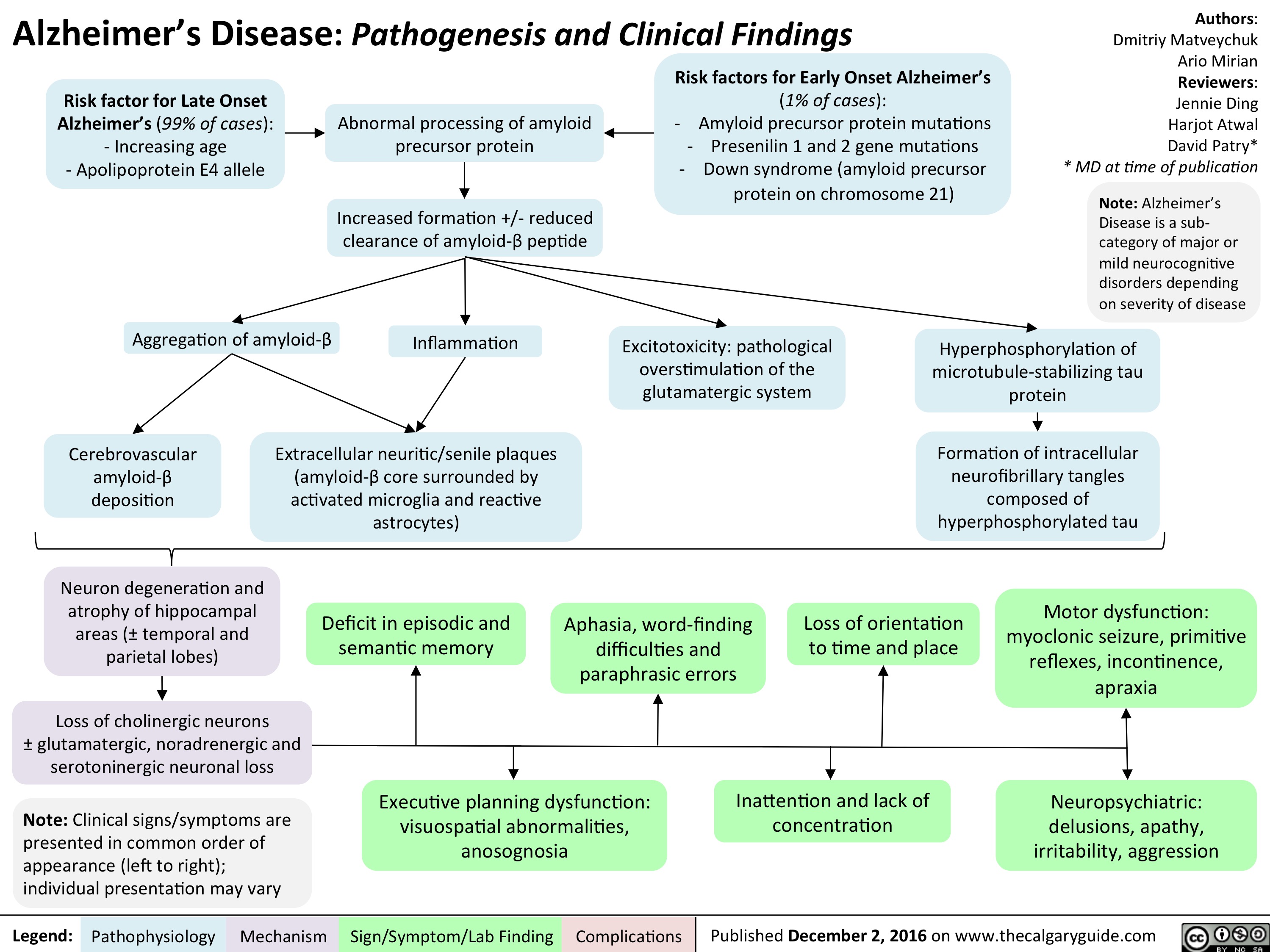
alzheimers-disease-final
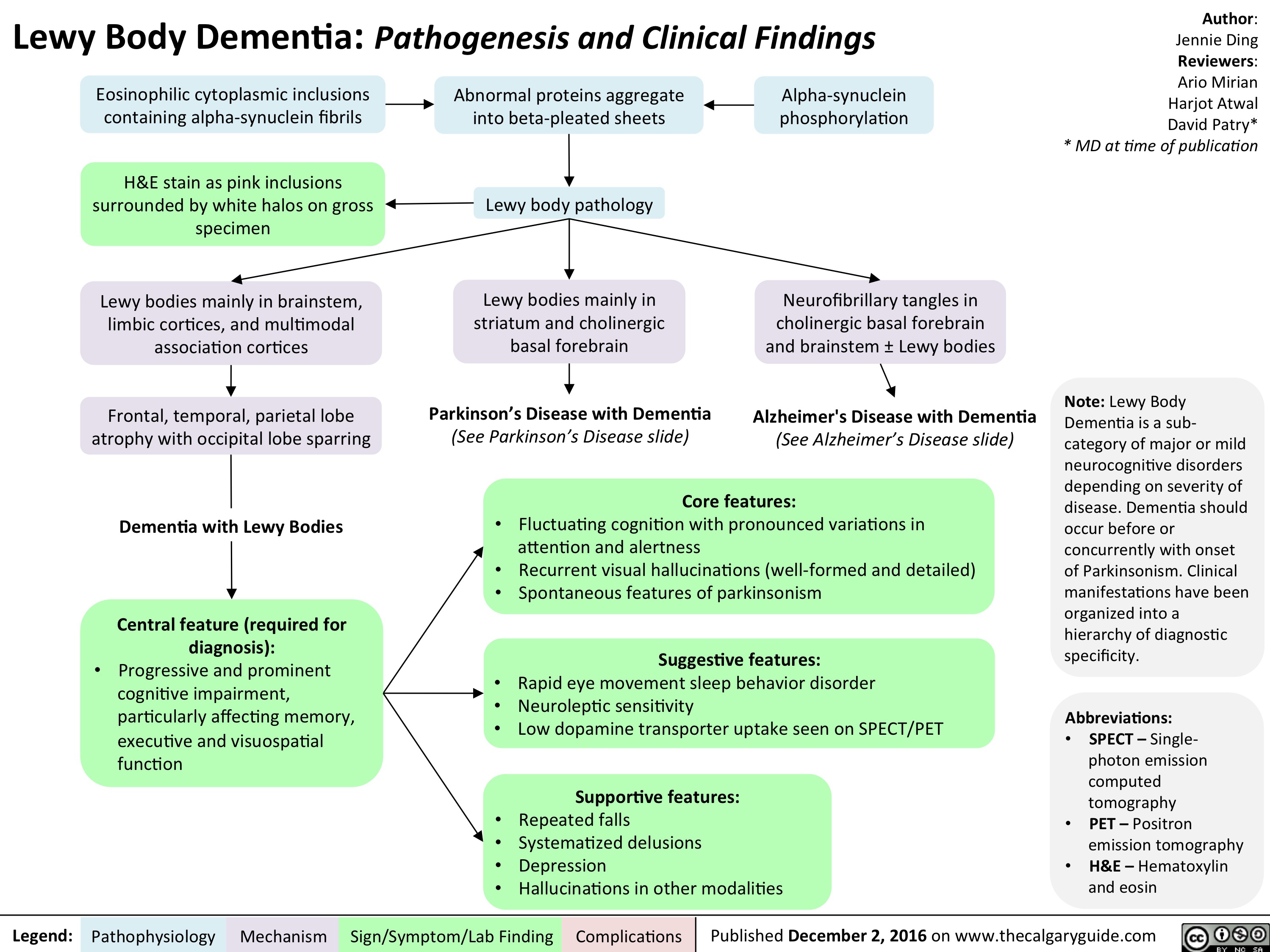
lewy-body-dementia-final
als-final
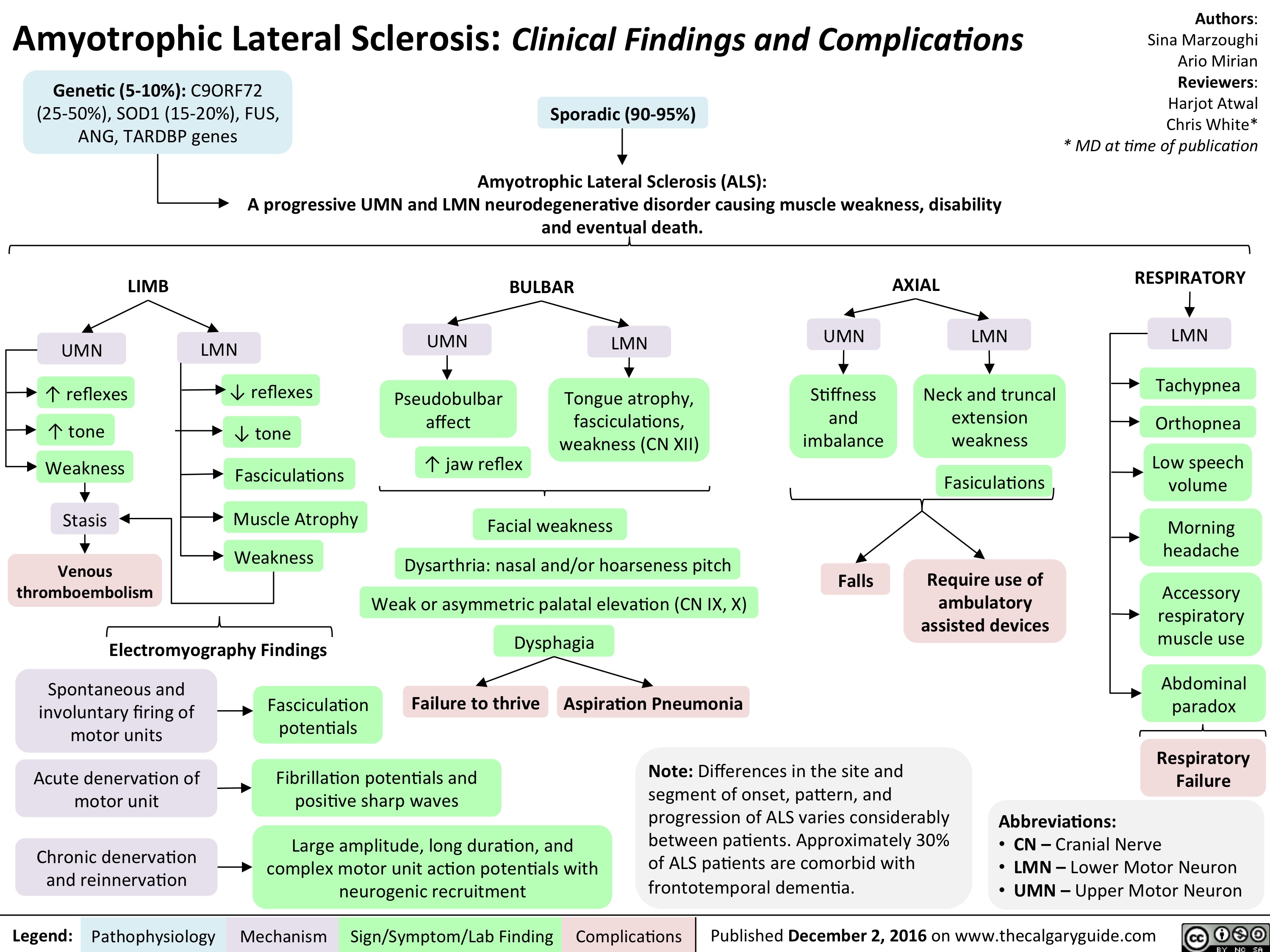
als-final
NSAIDs Final
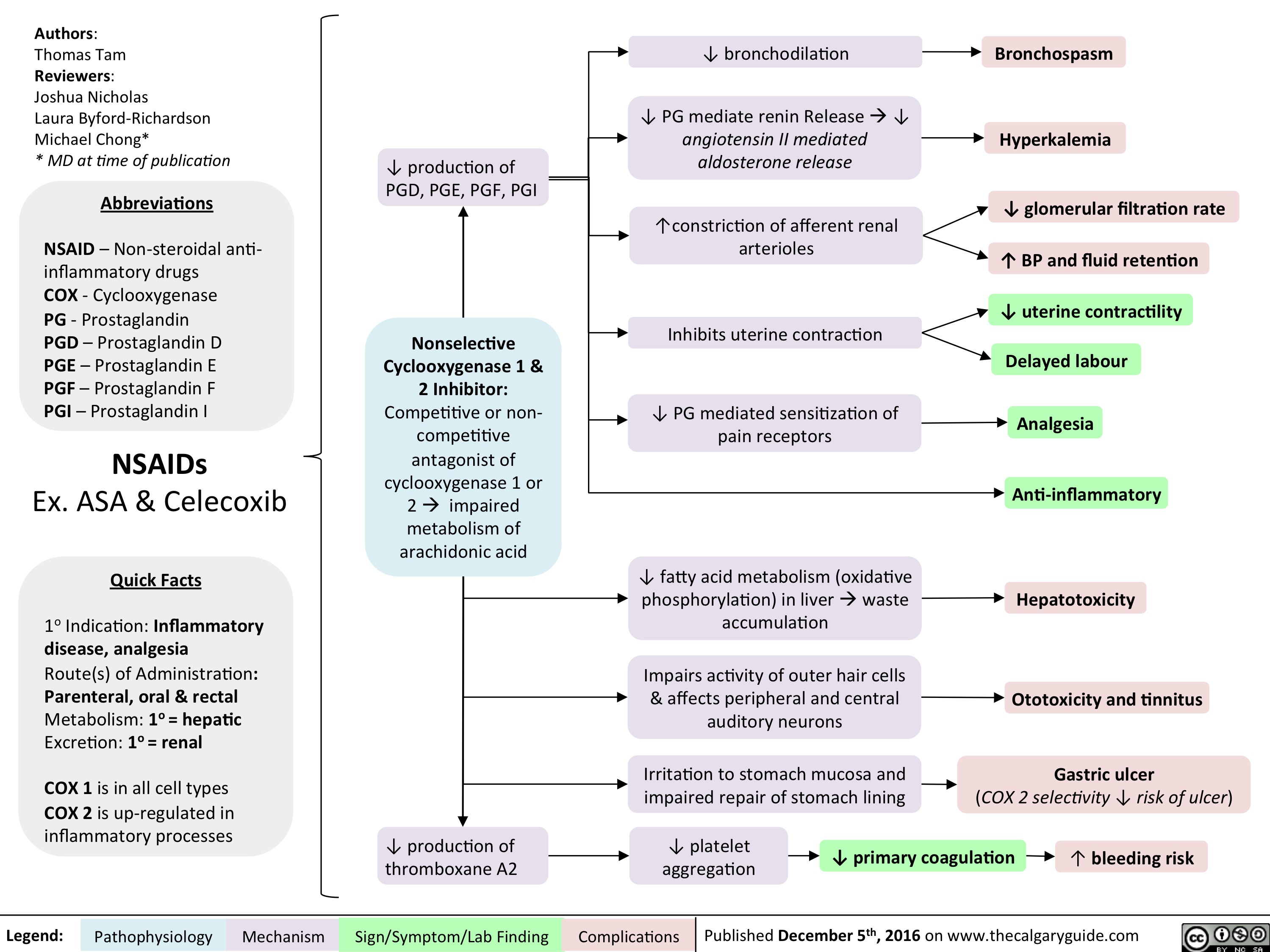
NSAIDs Final
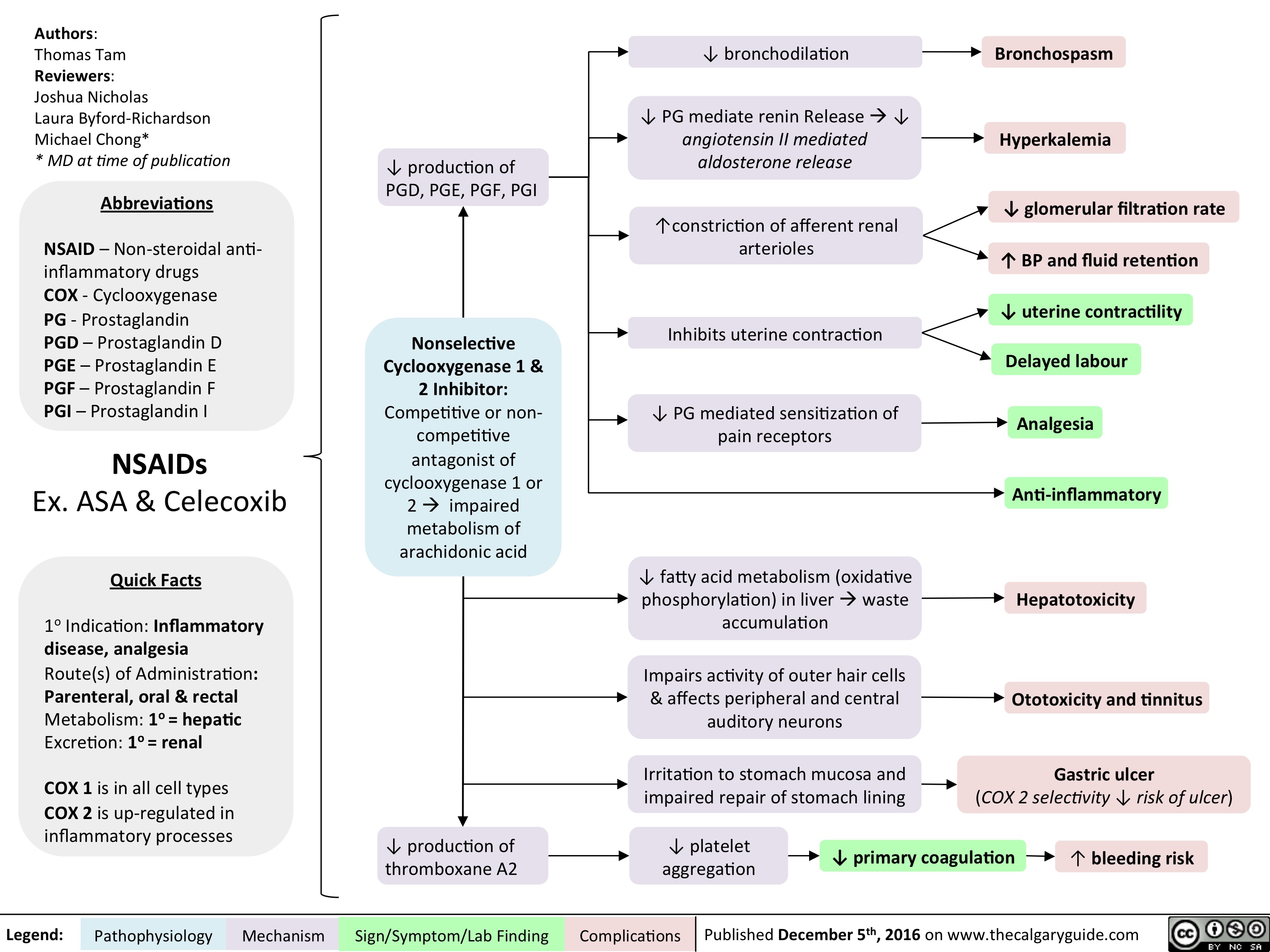
induction-of-labour-indications-and-contraindications
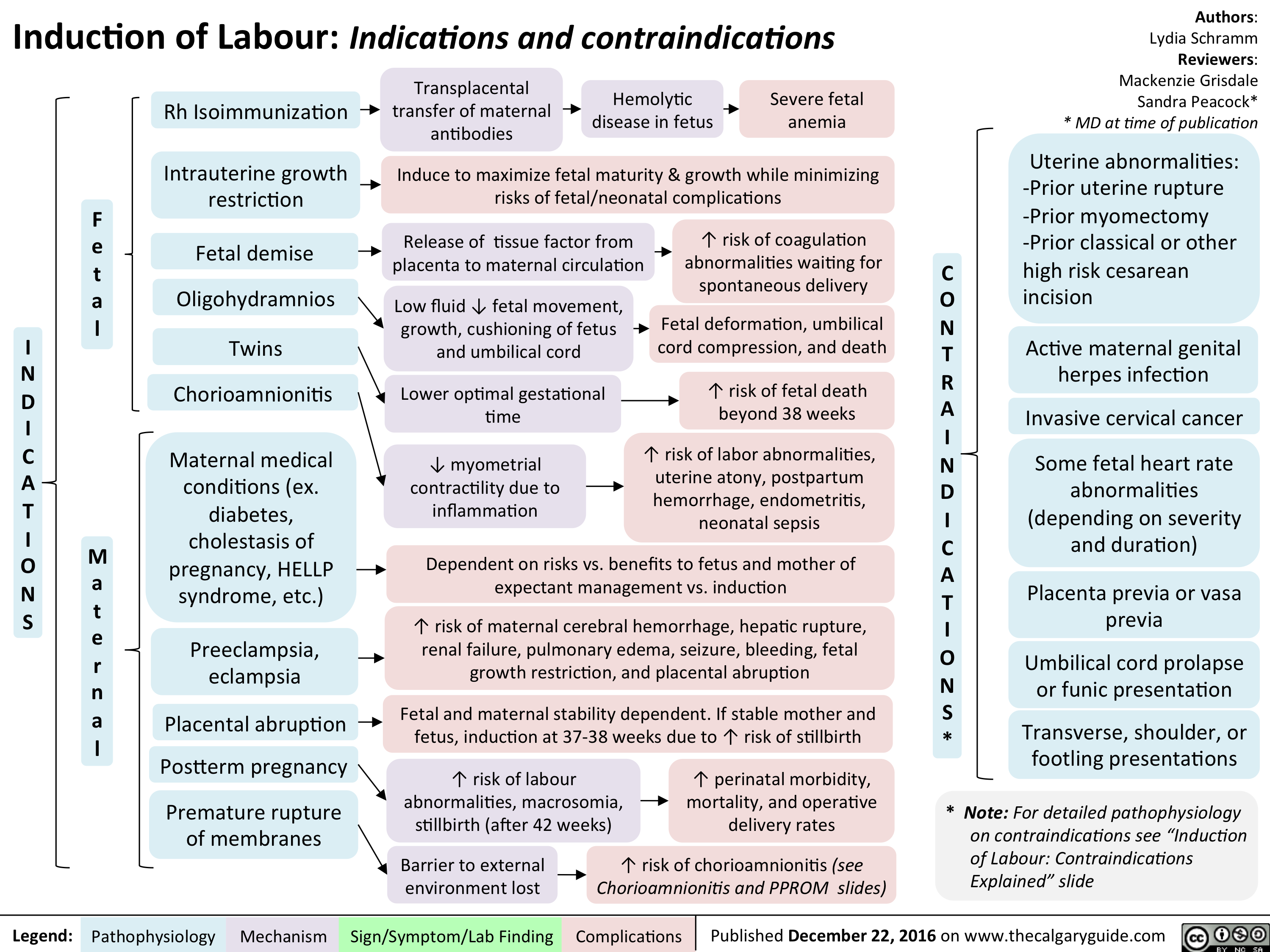
Stress Fracture v.5
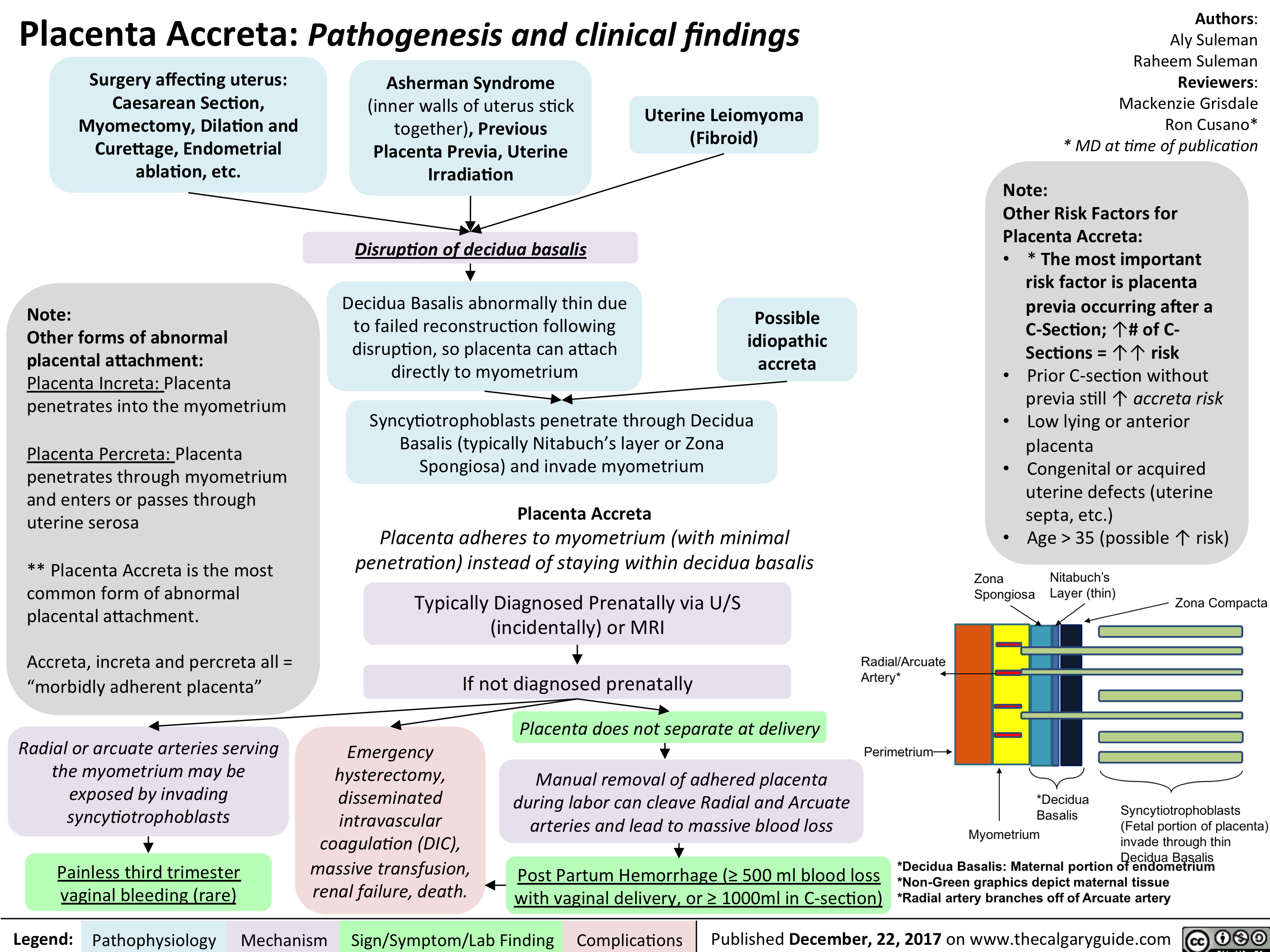
Placenta Accreta
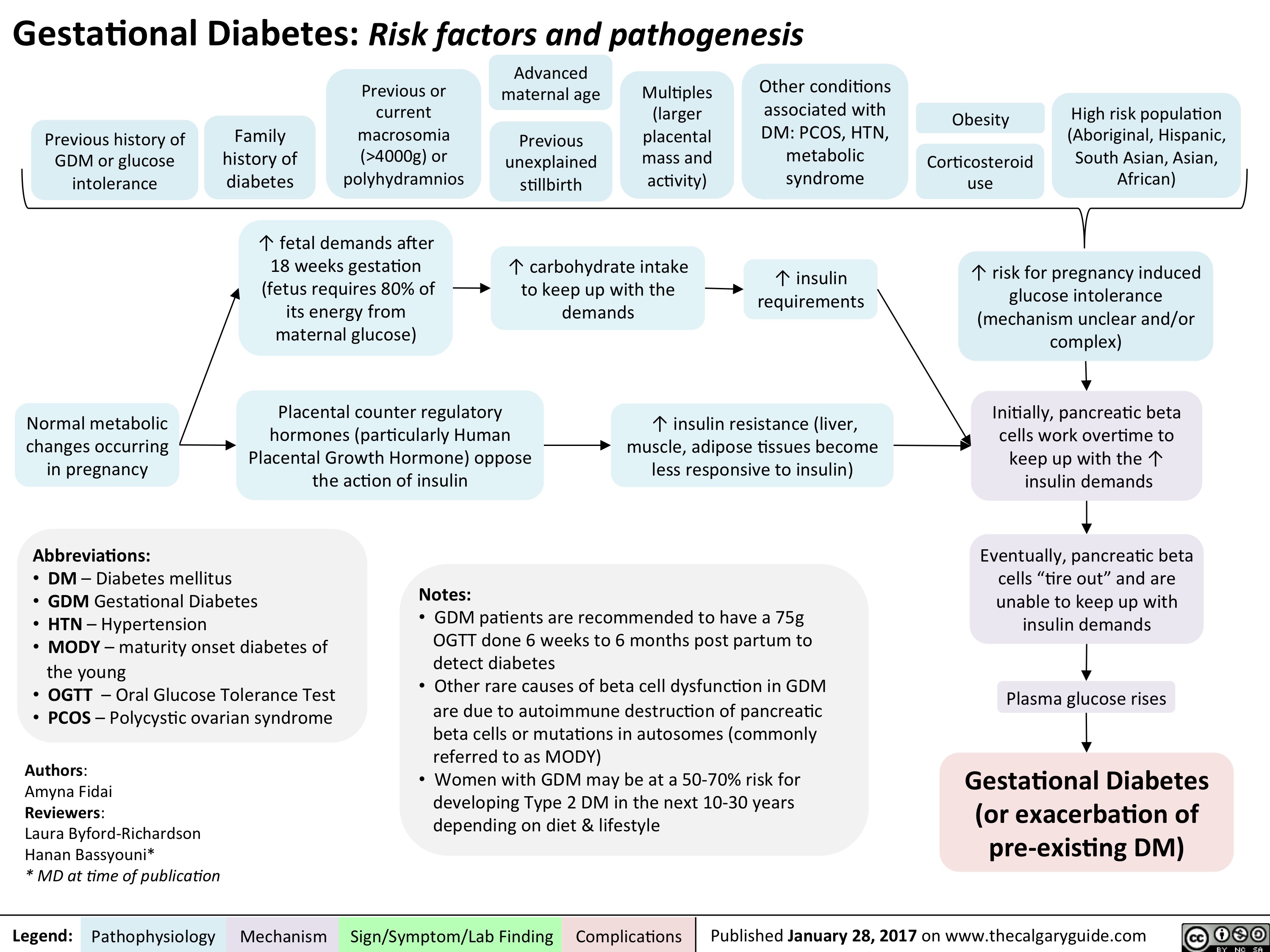
GDM: Risk factors and pathogenesis
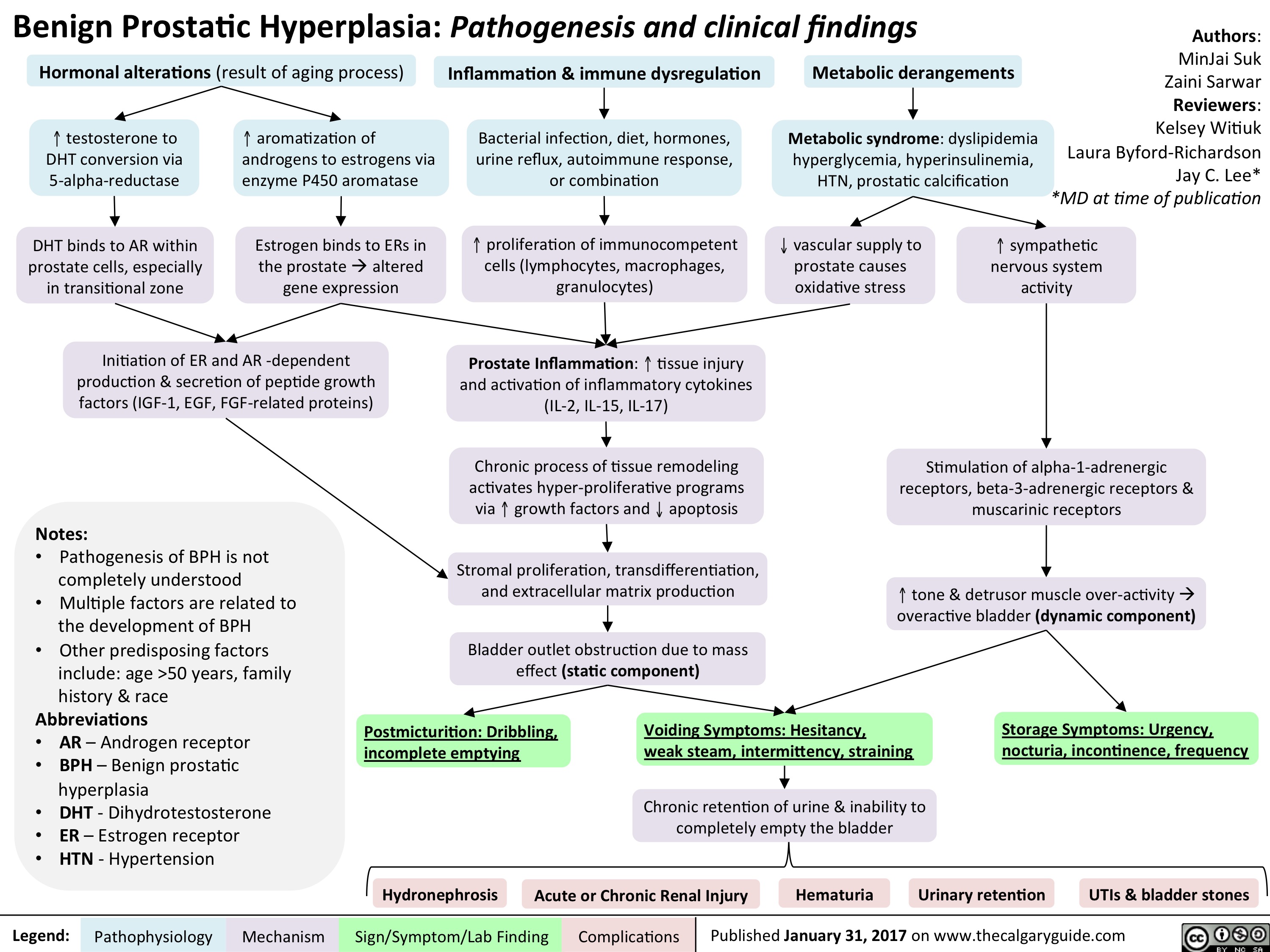
BPH Final
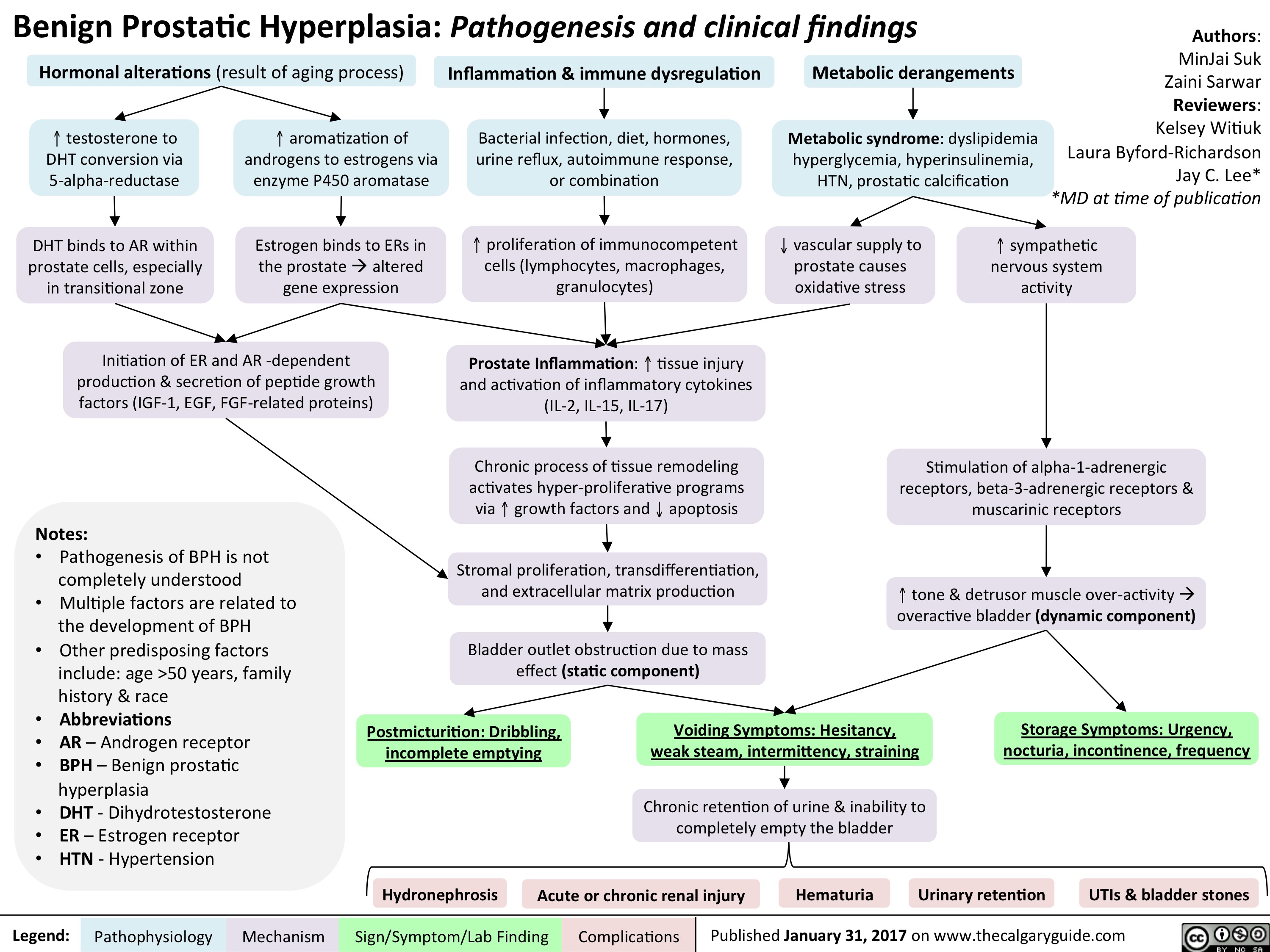
BPH Final
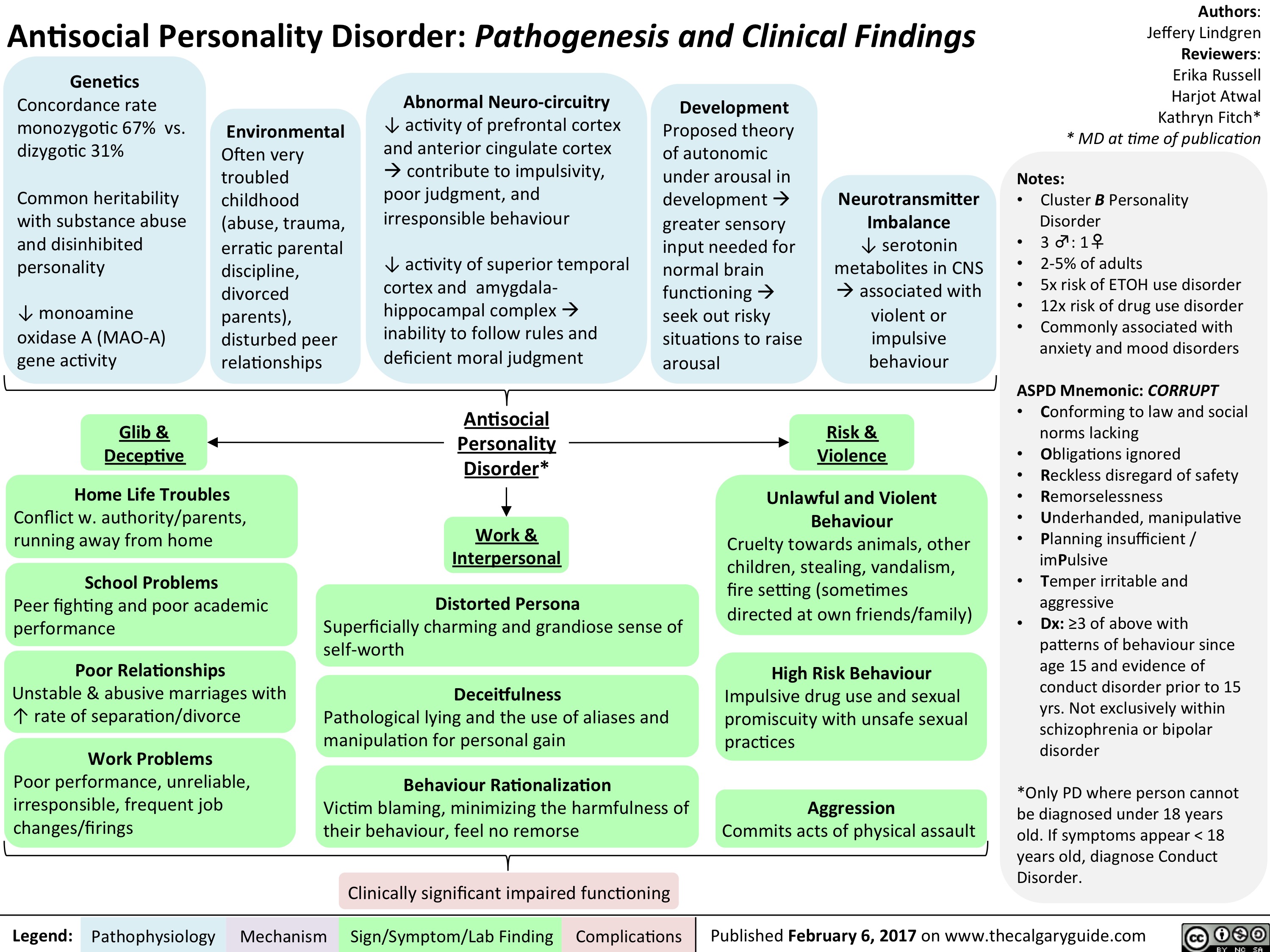
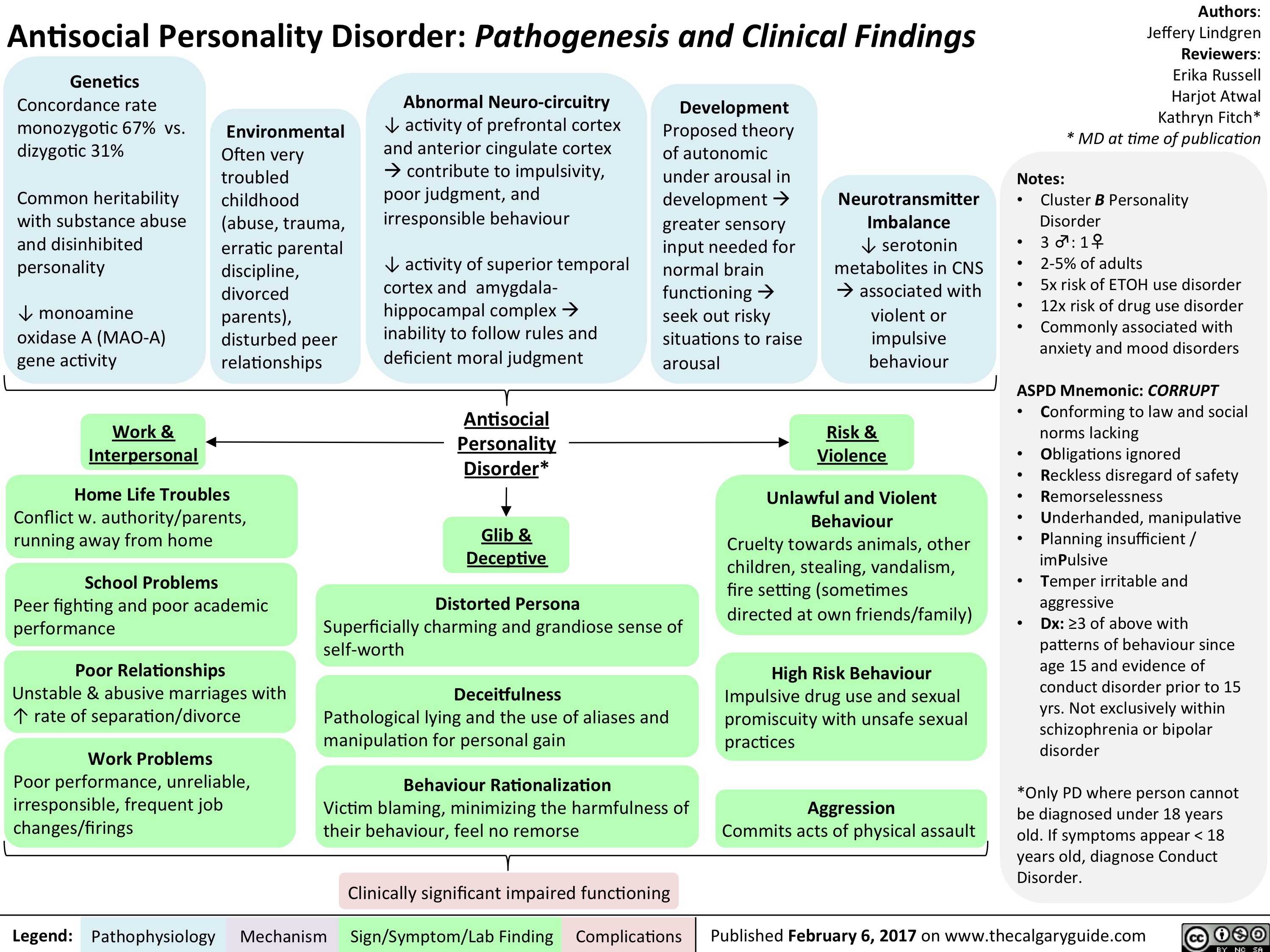
ASPD FINAL
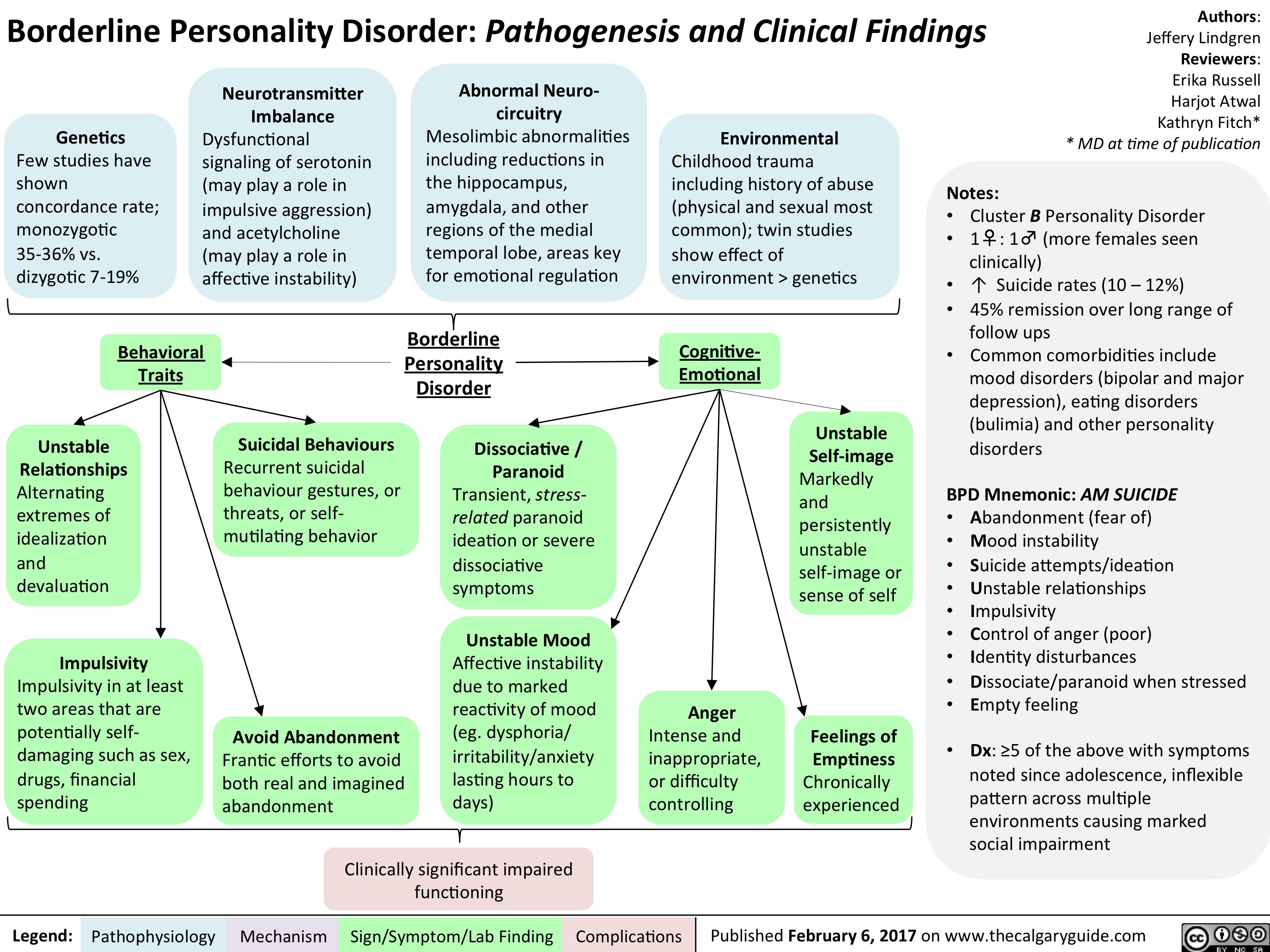
BPD FINAL
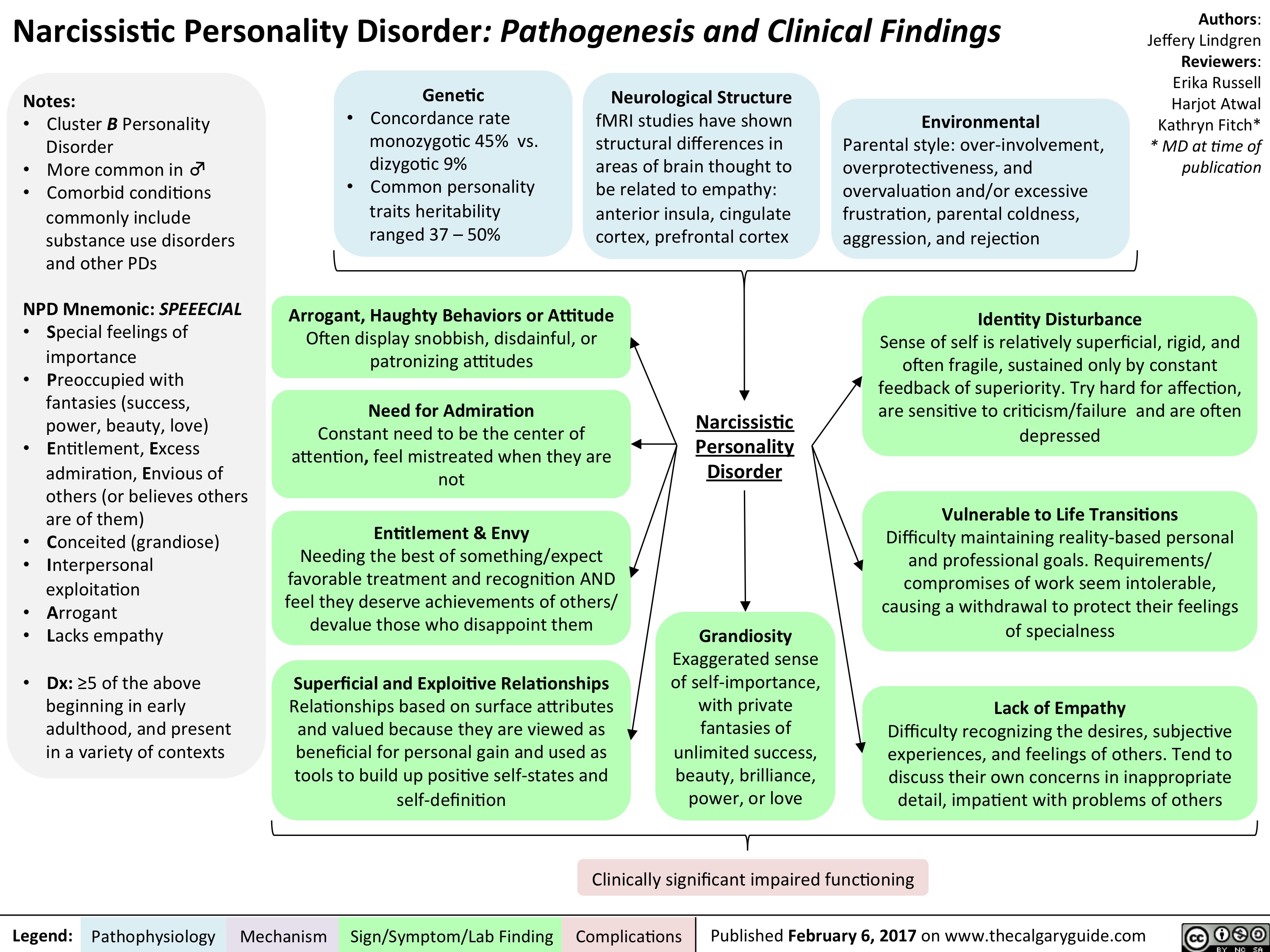
NPD FINAL
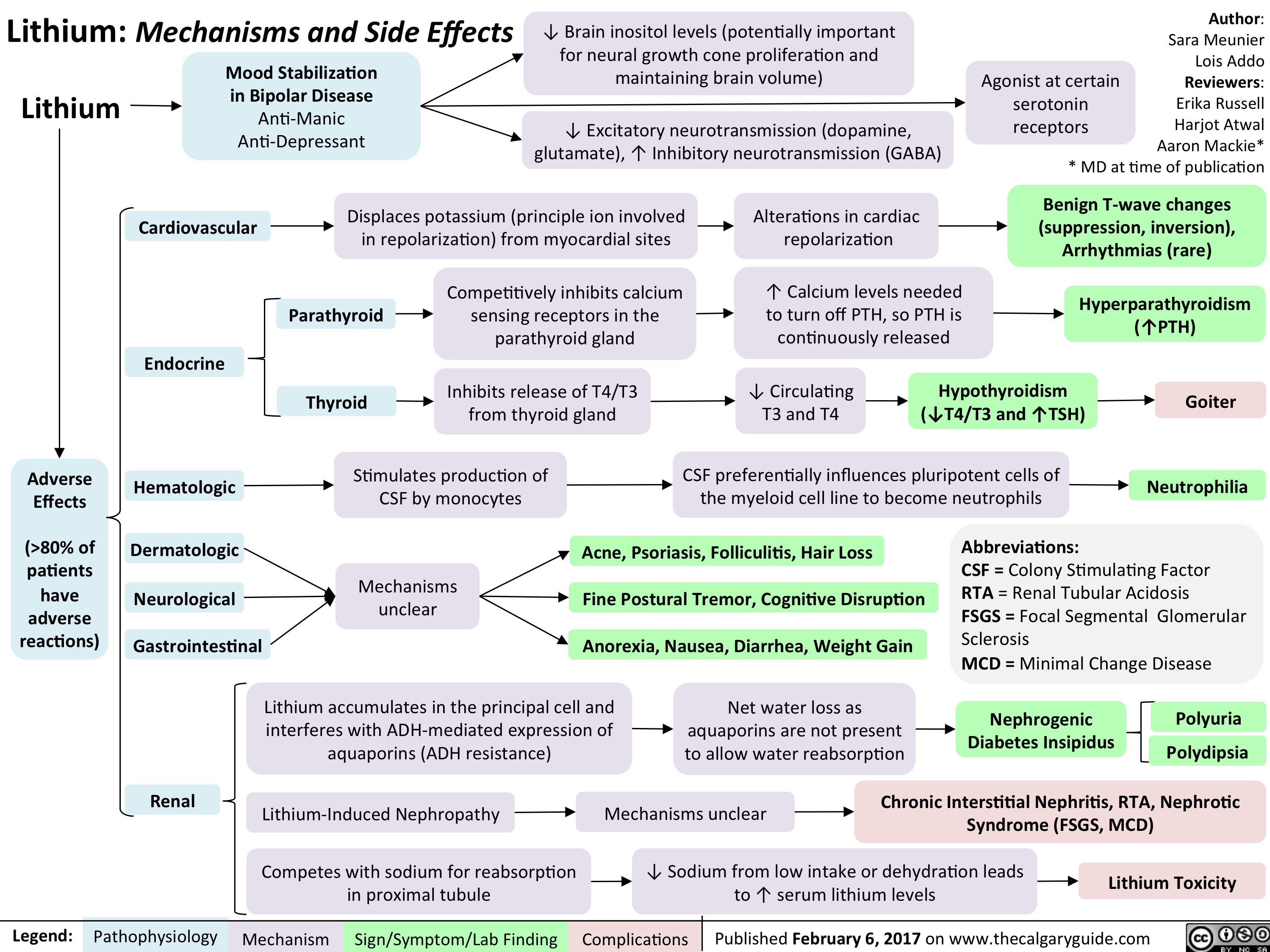
Lithium FINAL
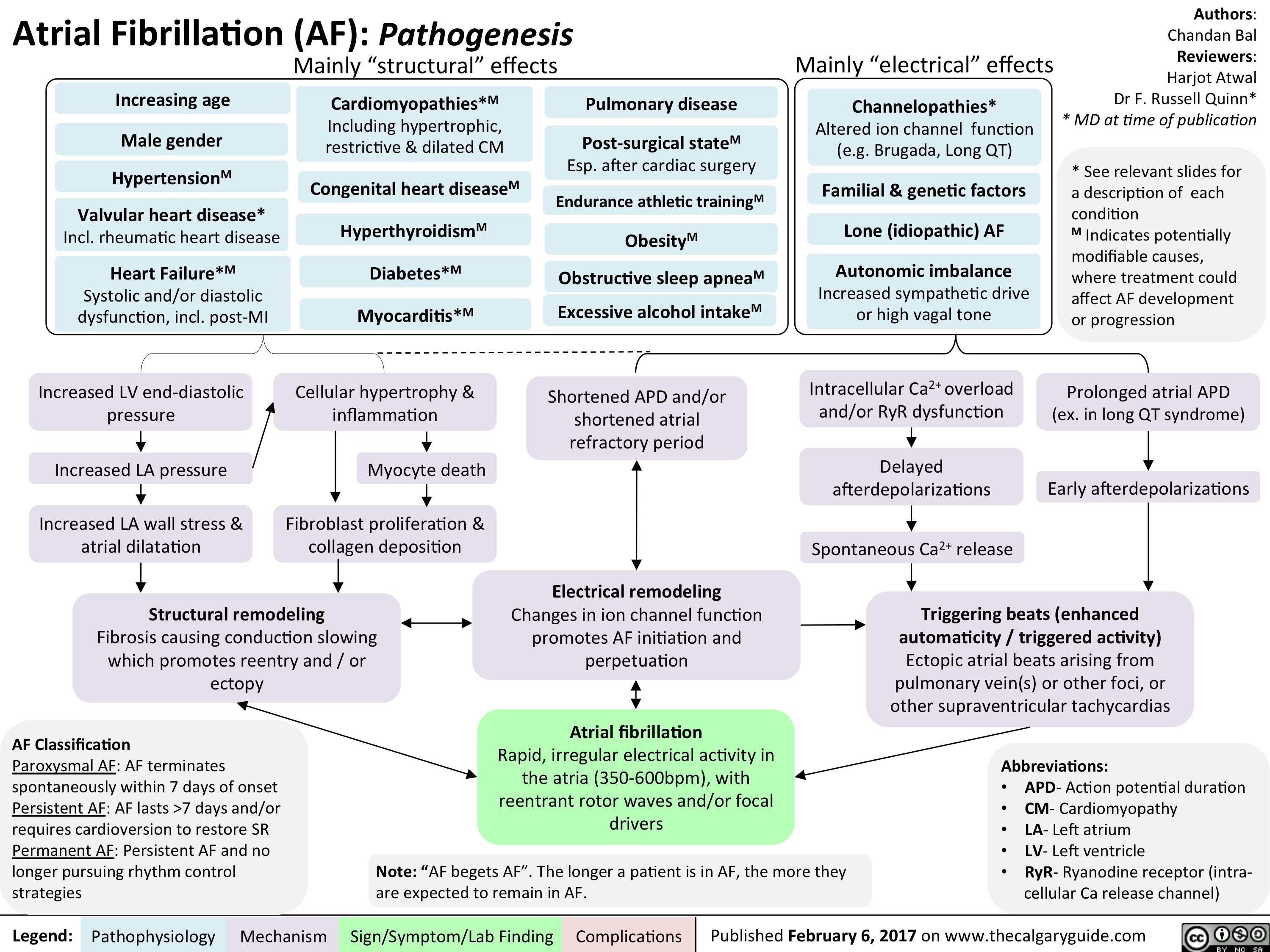
AF FINAL
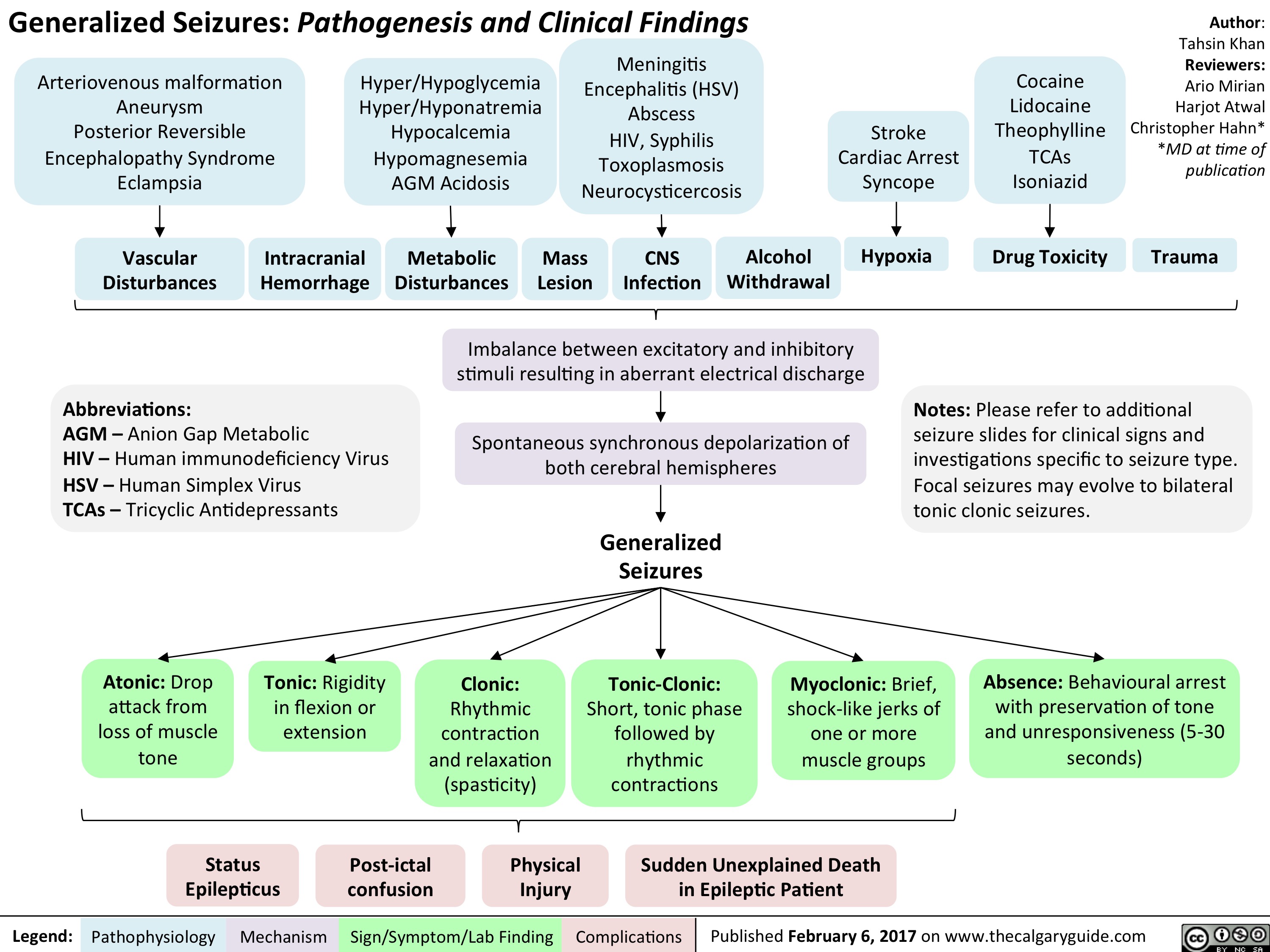
generalized-seizures-definitions
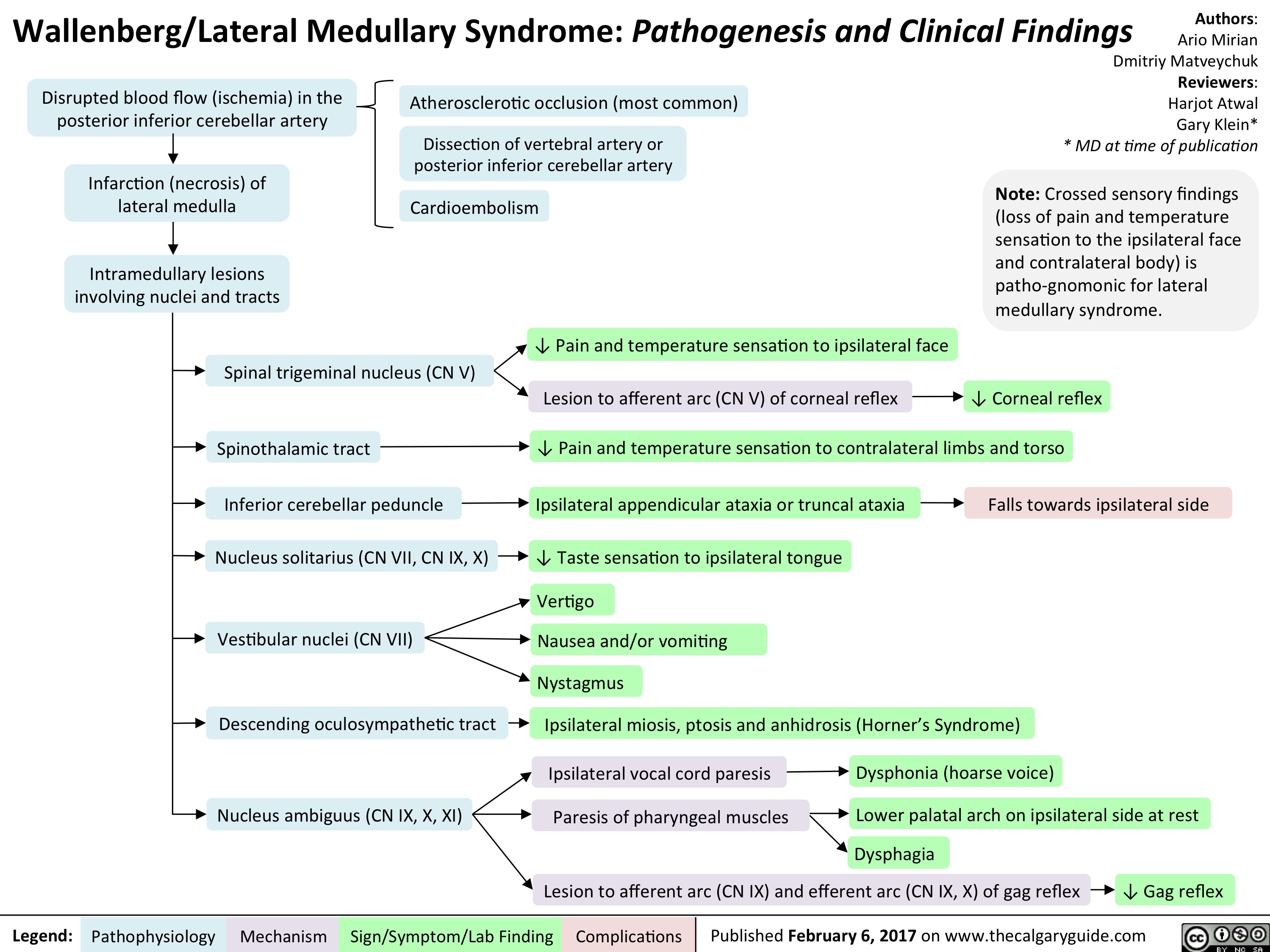
Lateral Medullary Syndrome FINAL
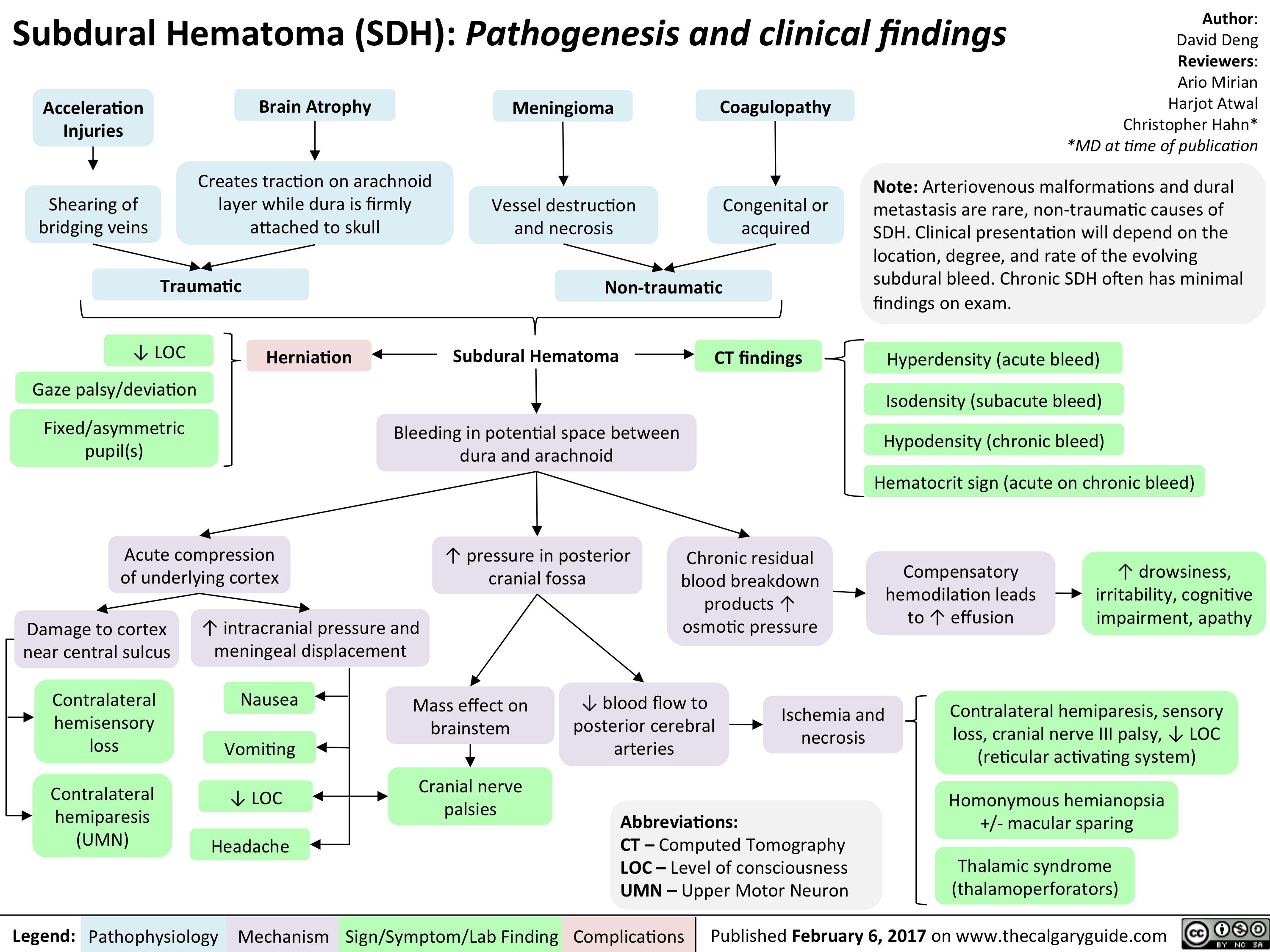
Subdural hematoma FINAL
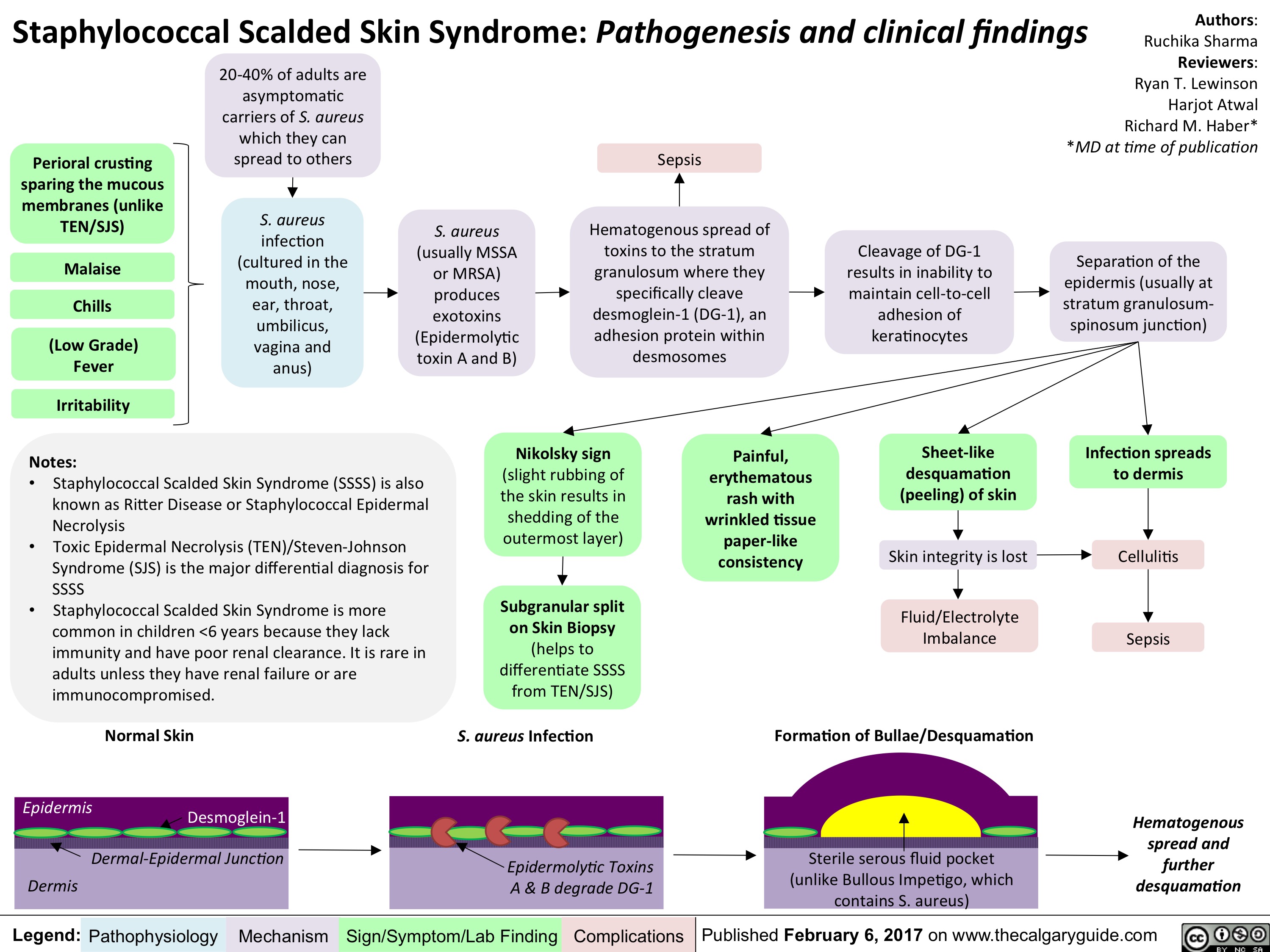
Staphylococcus Scalded Skin Syndrome FINAL
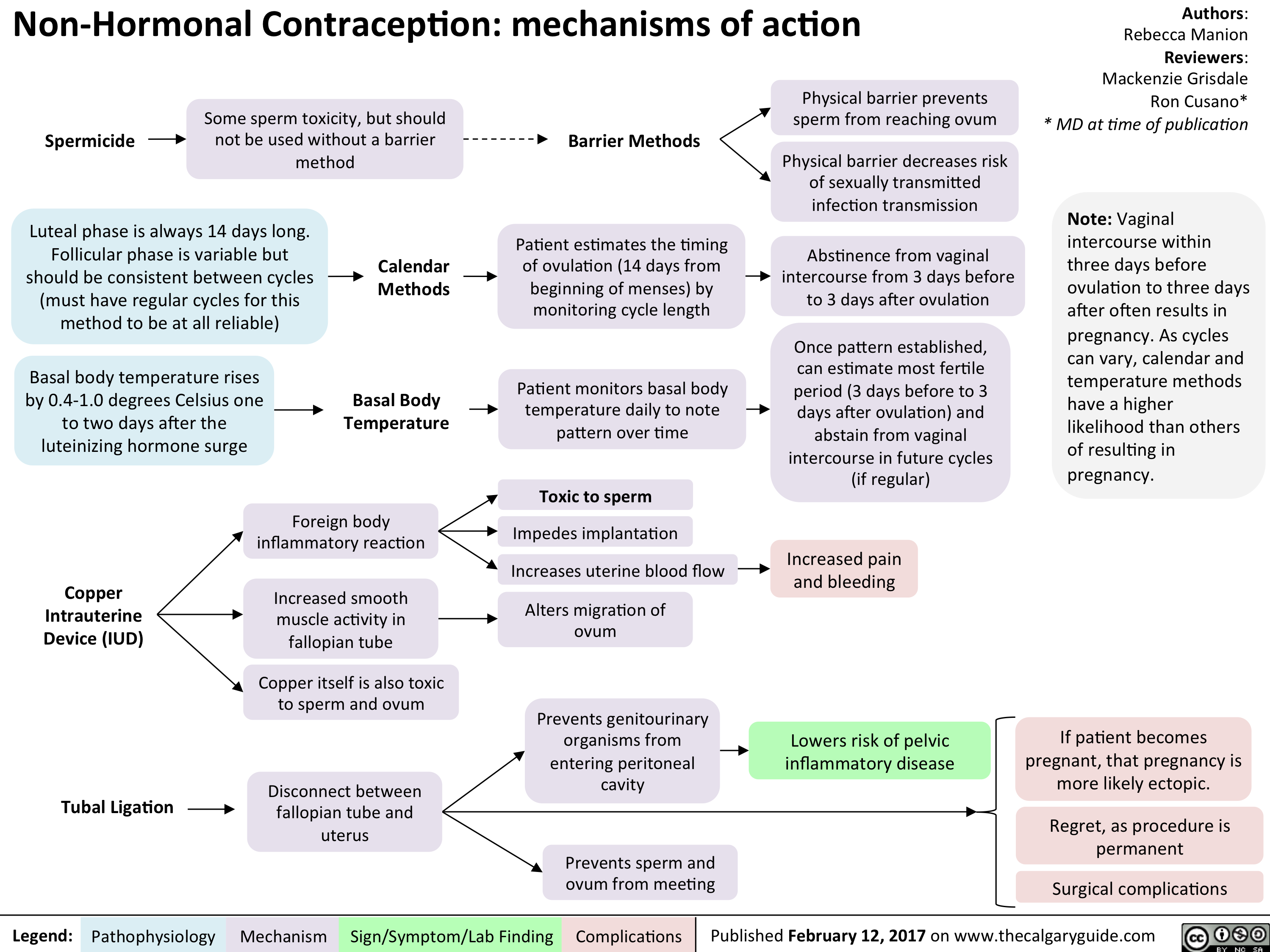
Manion contraception MOAs
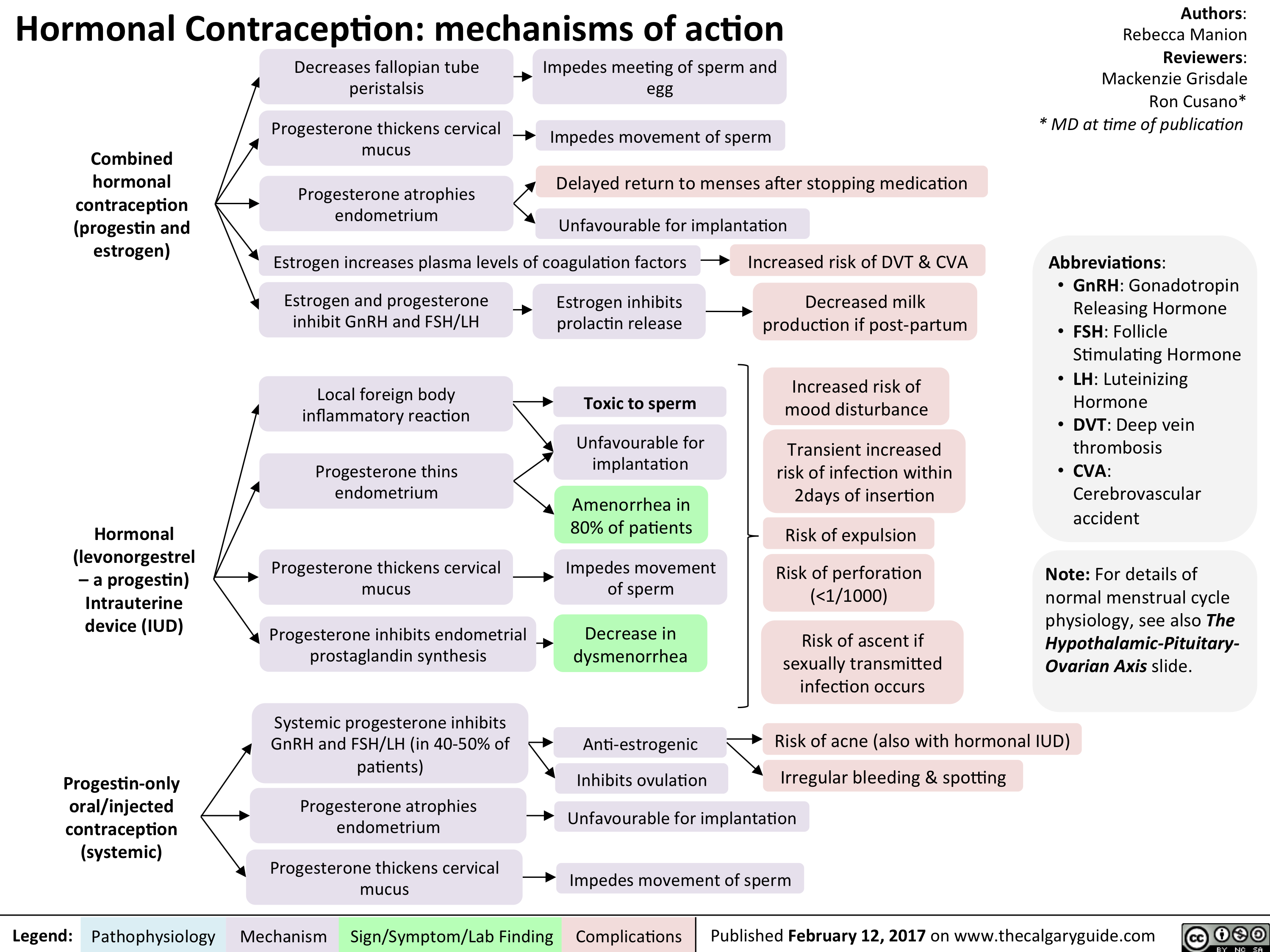
Manion contraception MOAs2
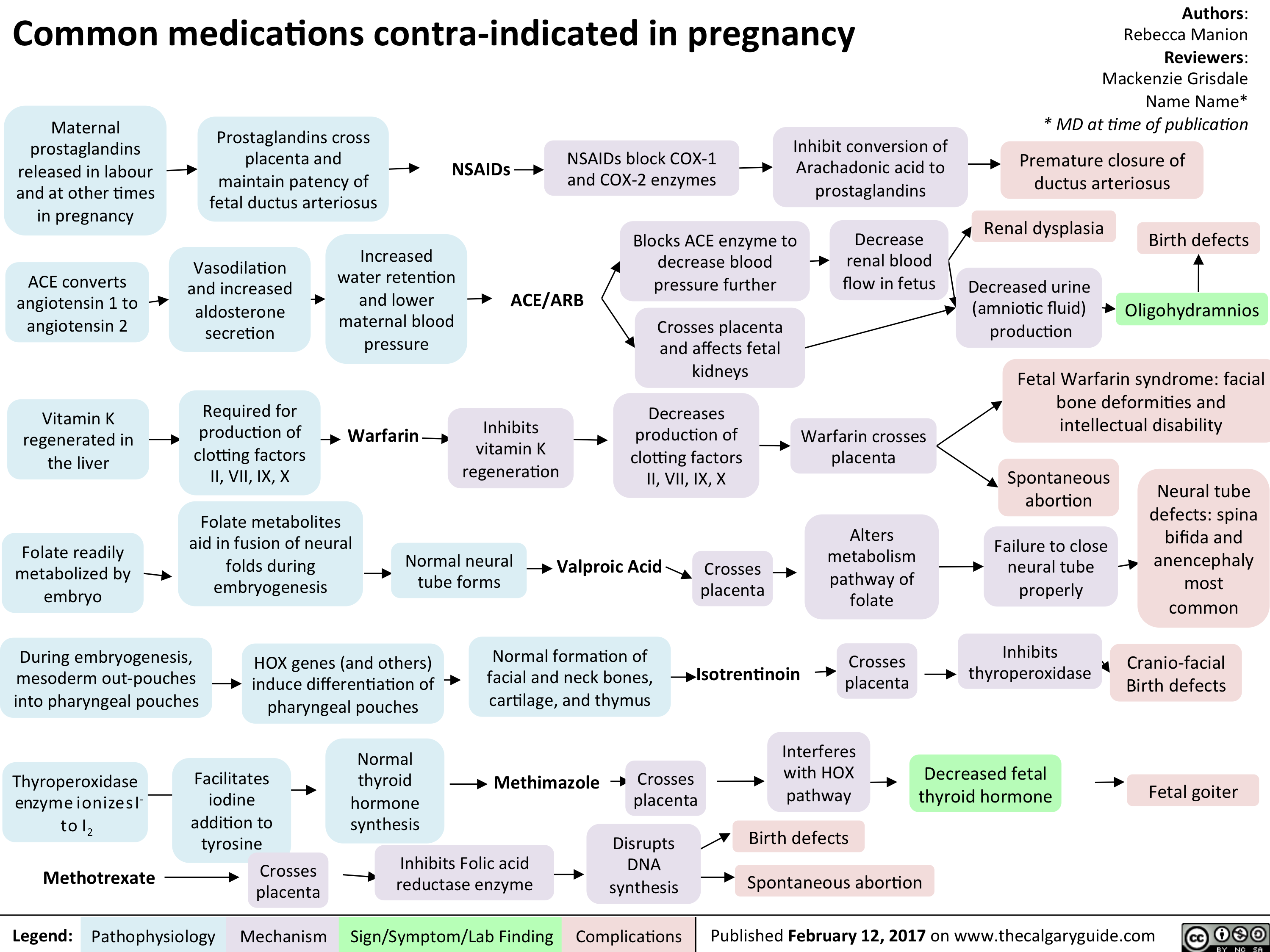
Common meds contra in Preg
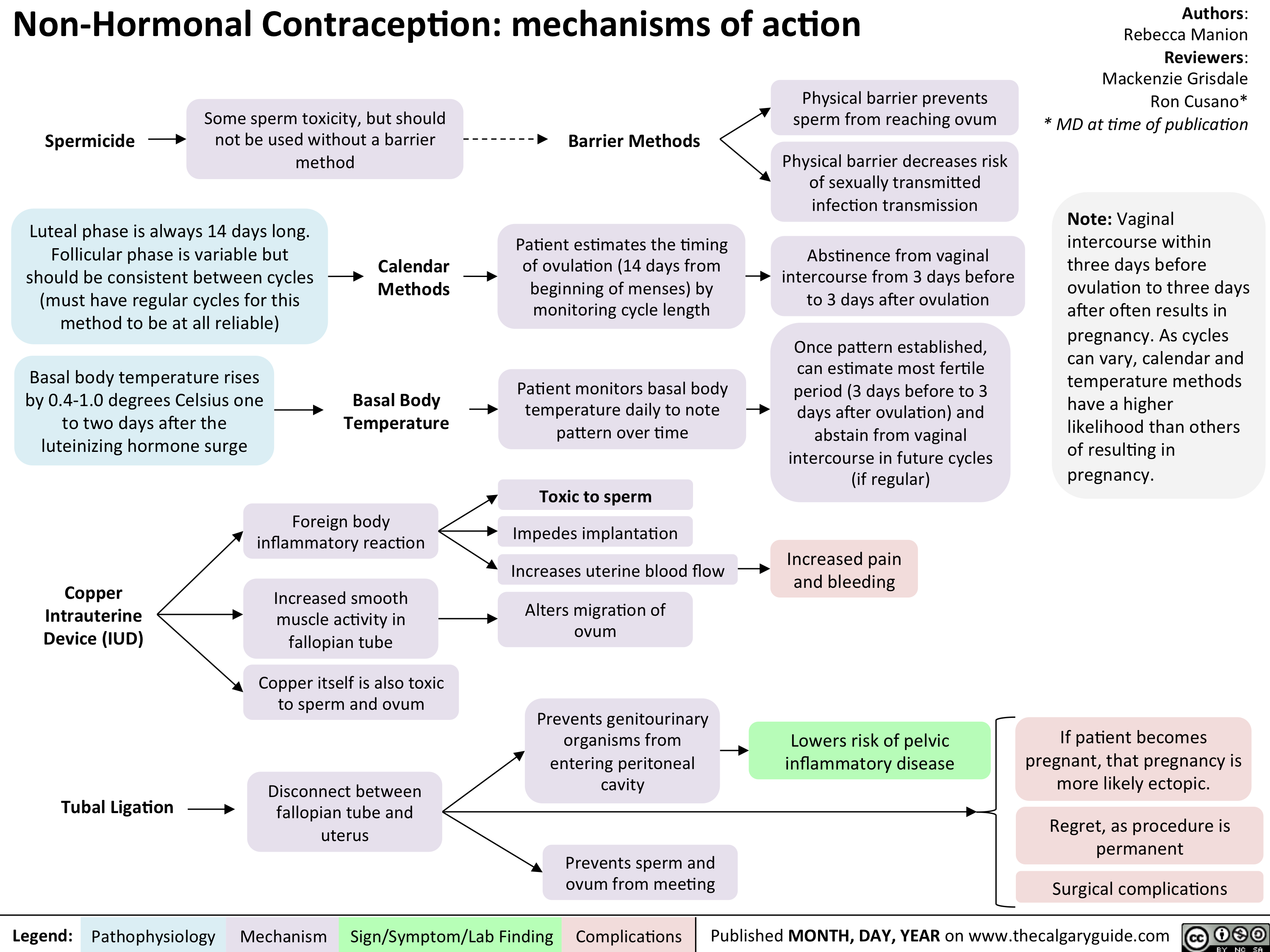
Non hormonal
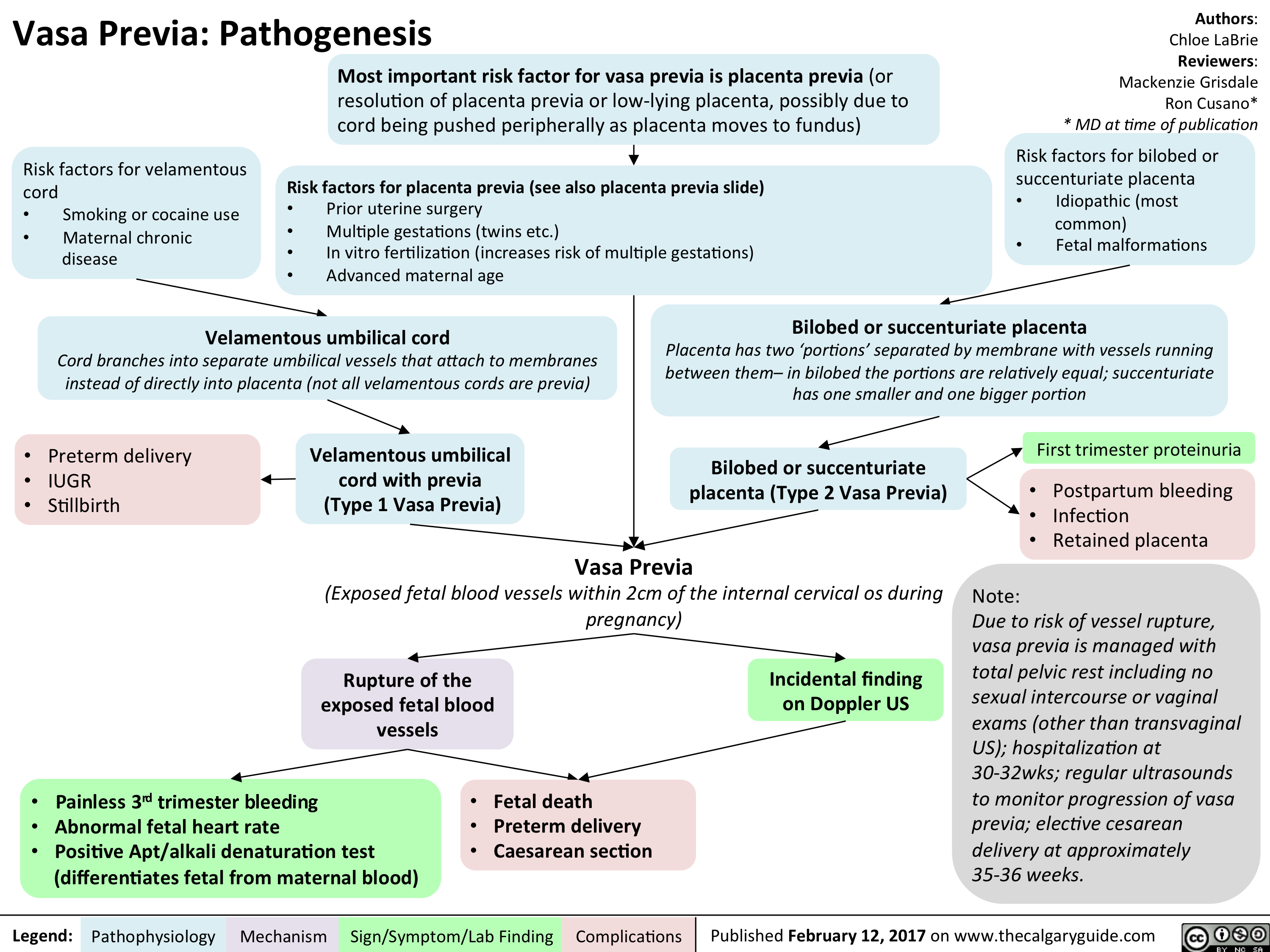
Vasa Previa
ASPD FINAL
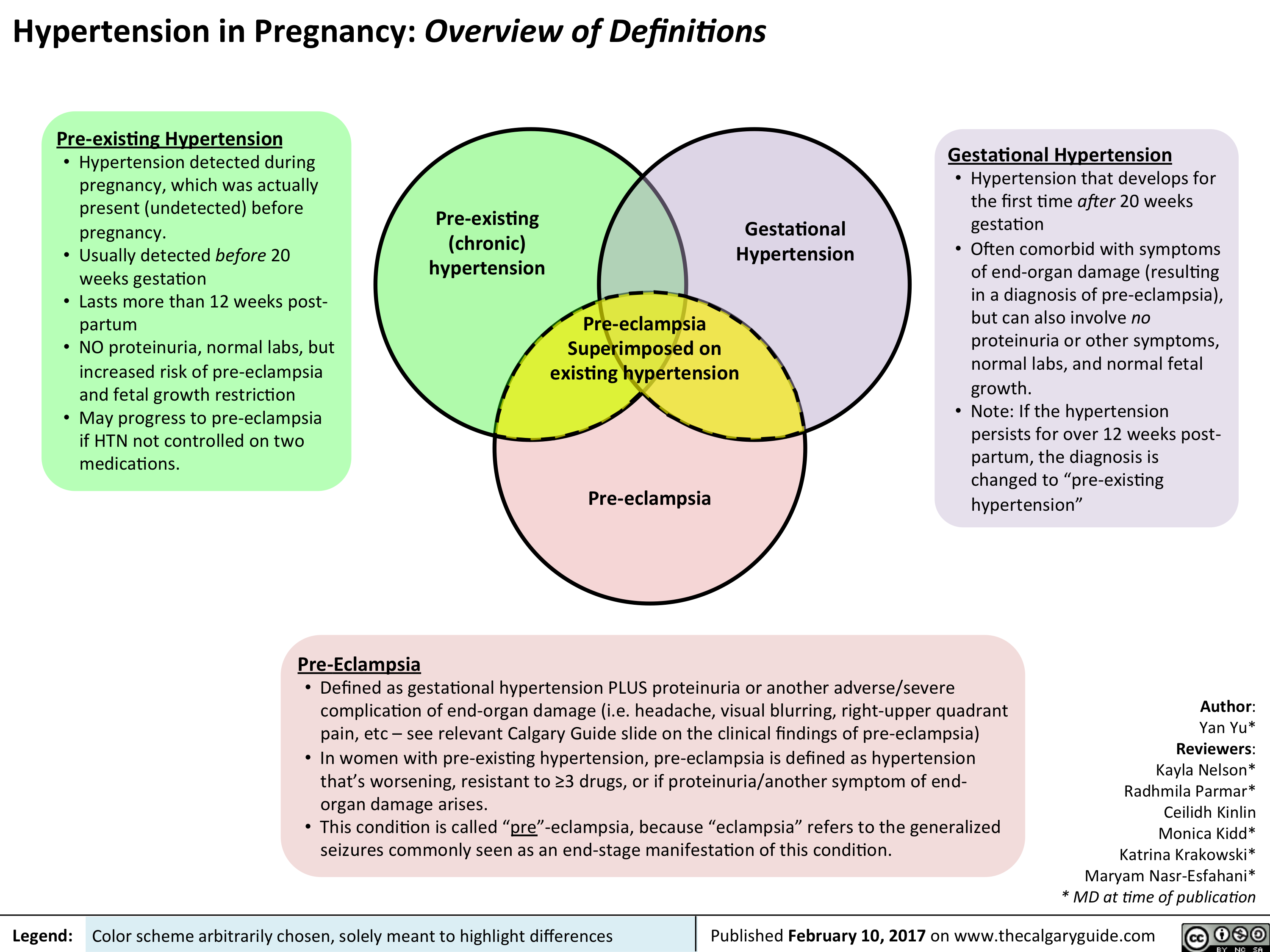
hypertension-in-pregnancy-overview-of-definitions
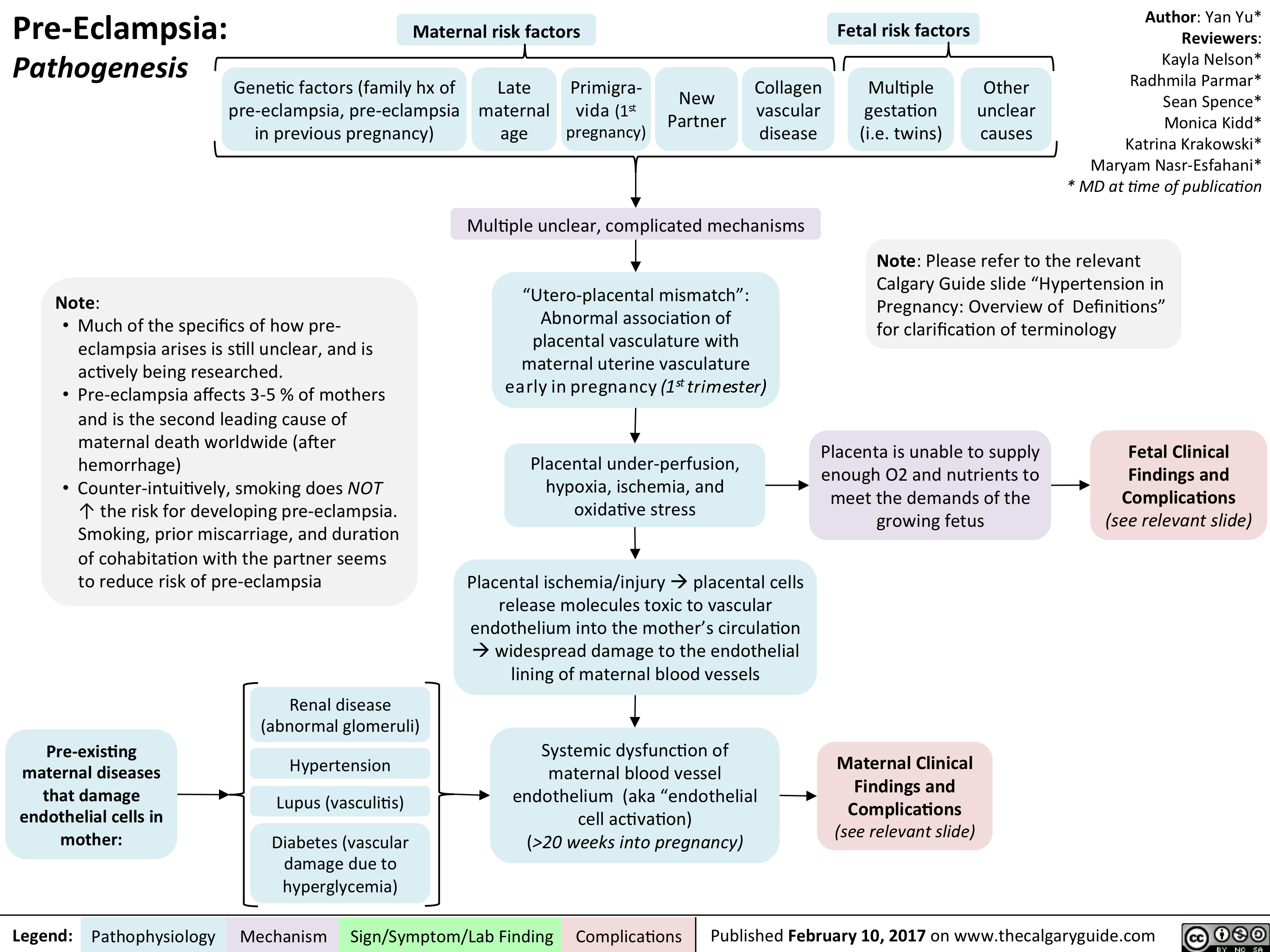
Yu Yan - Pre-eclampsia pathogenesis - publish
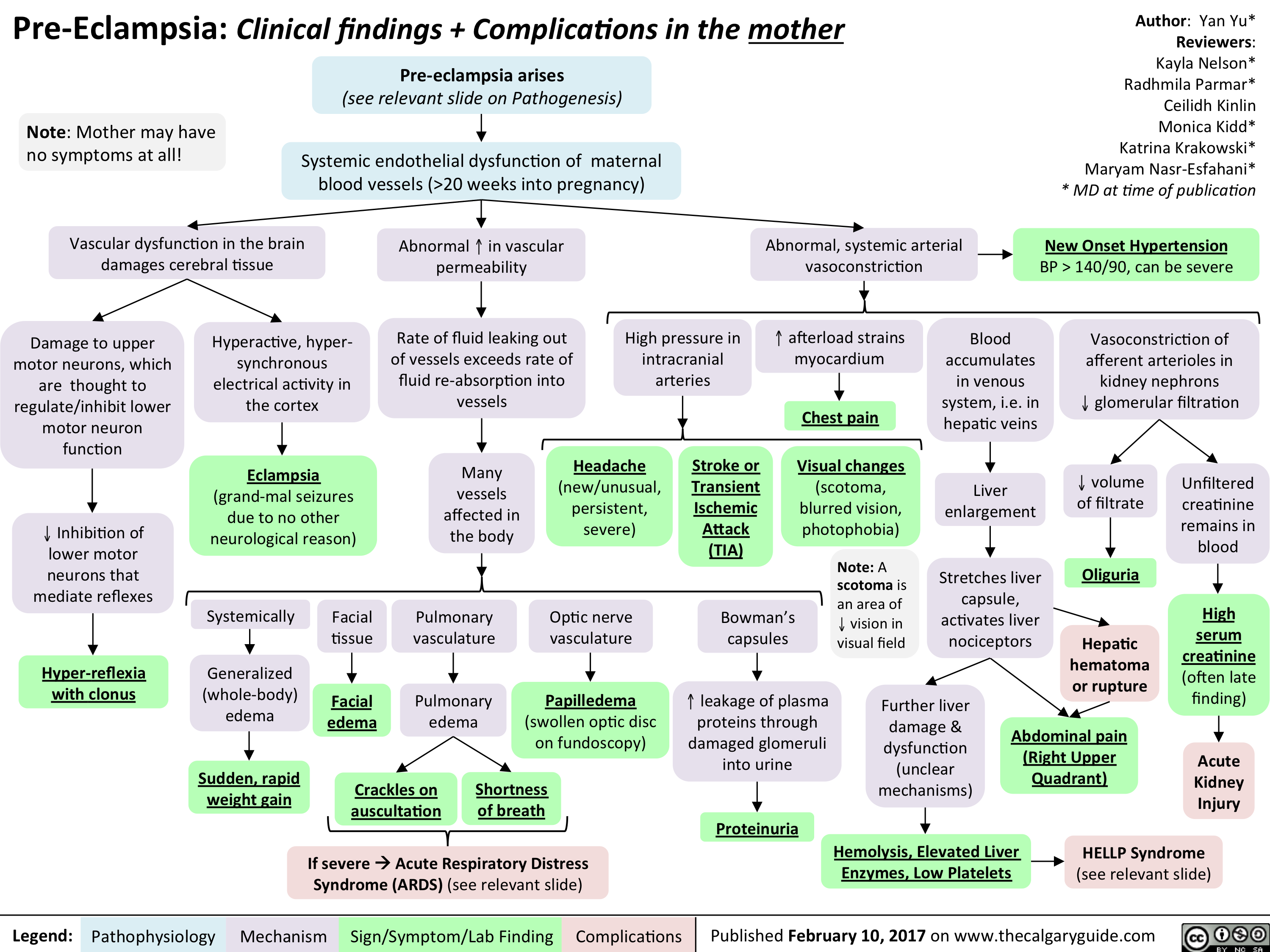
Yu Yan - Pre-eclampsia Maternal Complications - publish
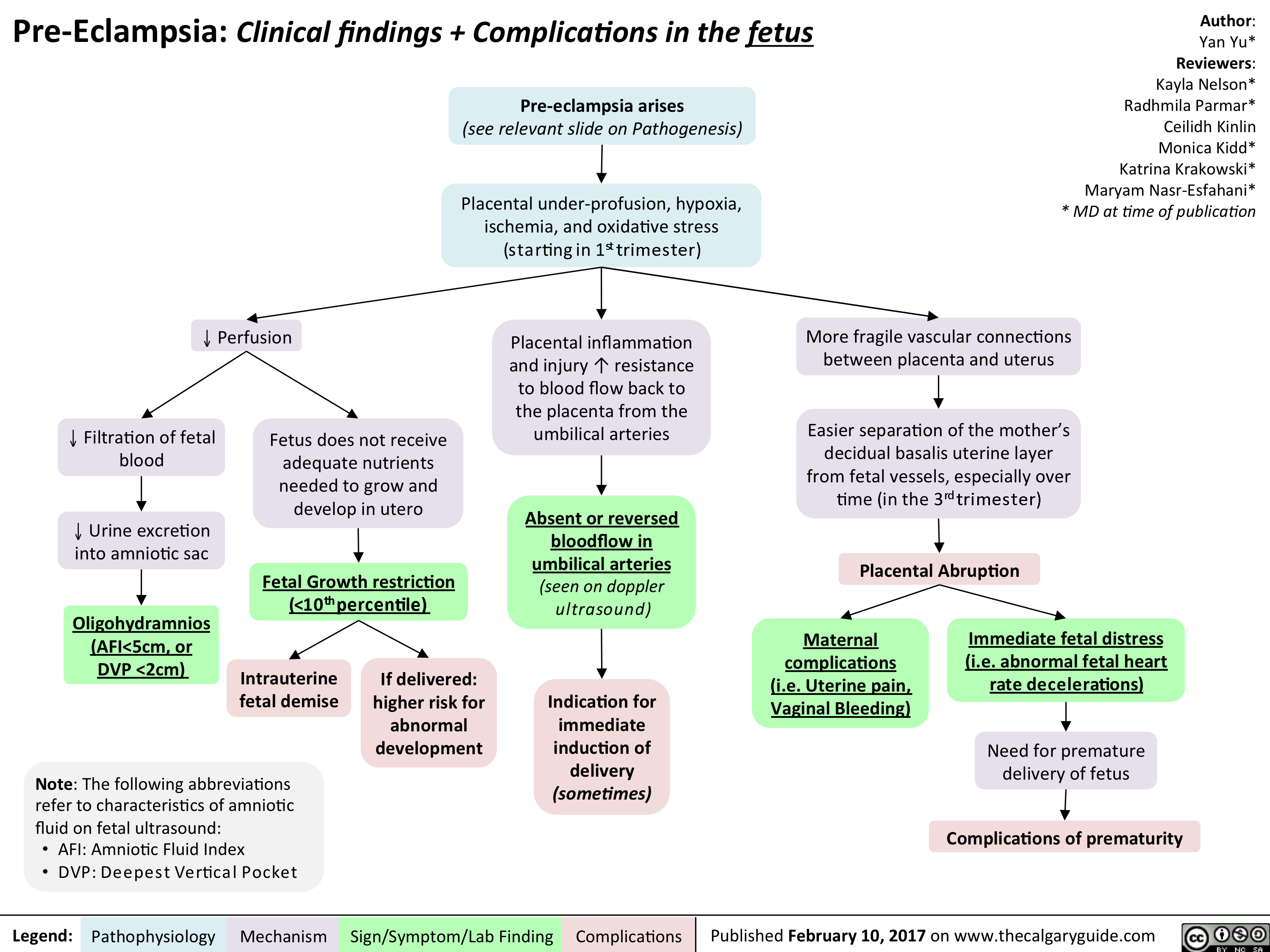
Yu Yan - Pre-eclampsia Fetal Complications - publish
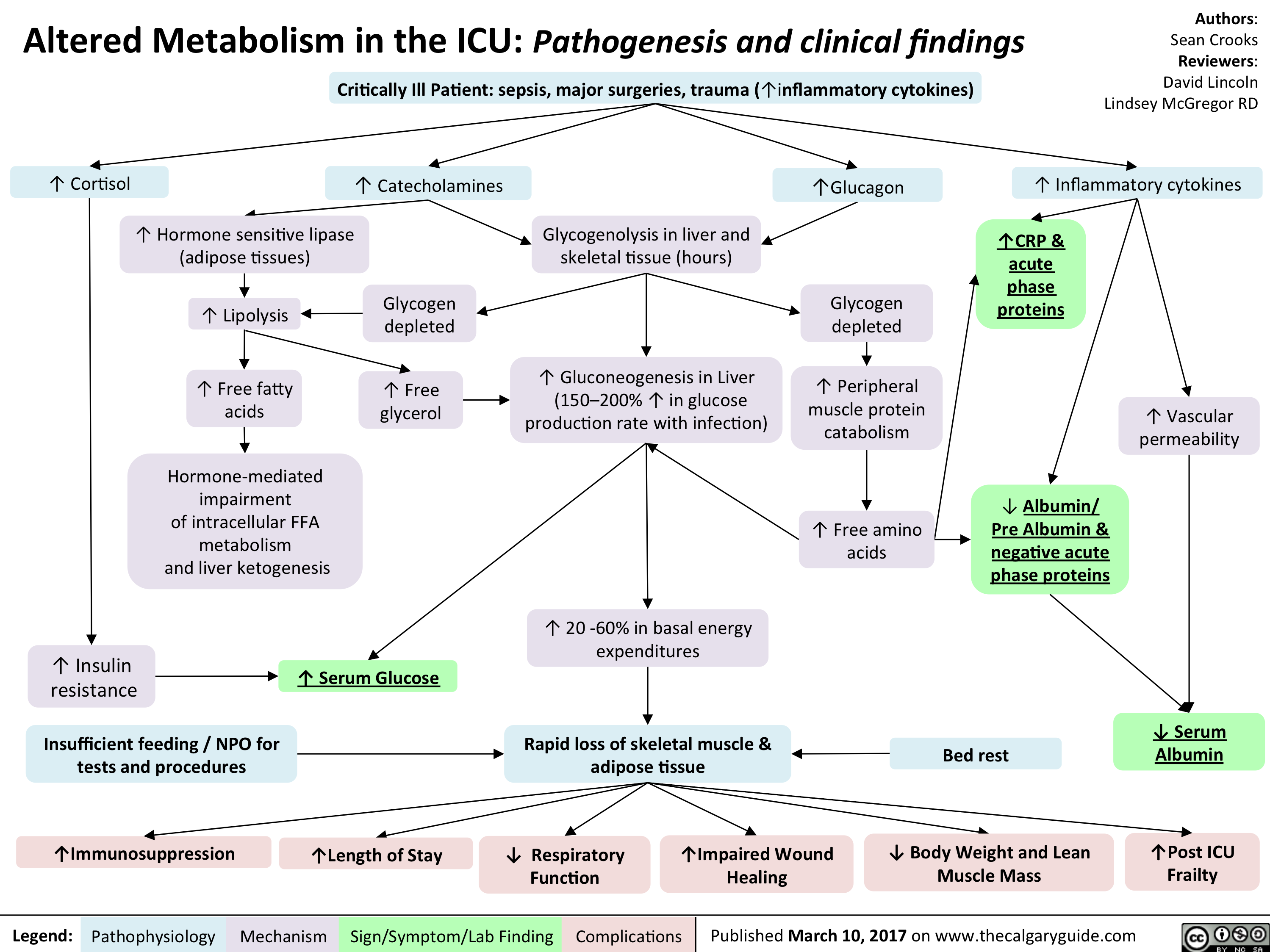
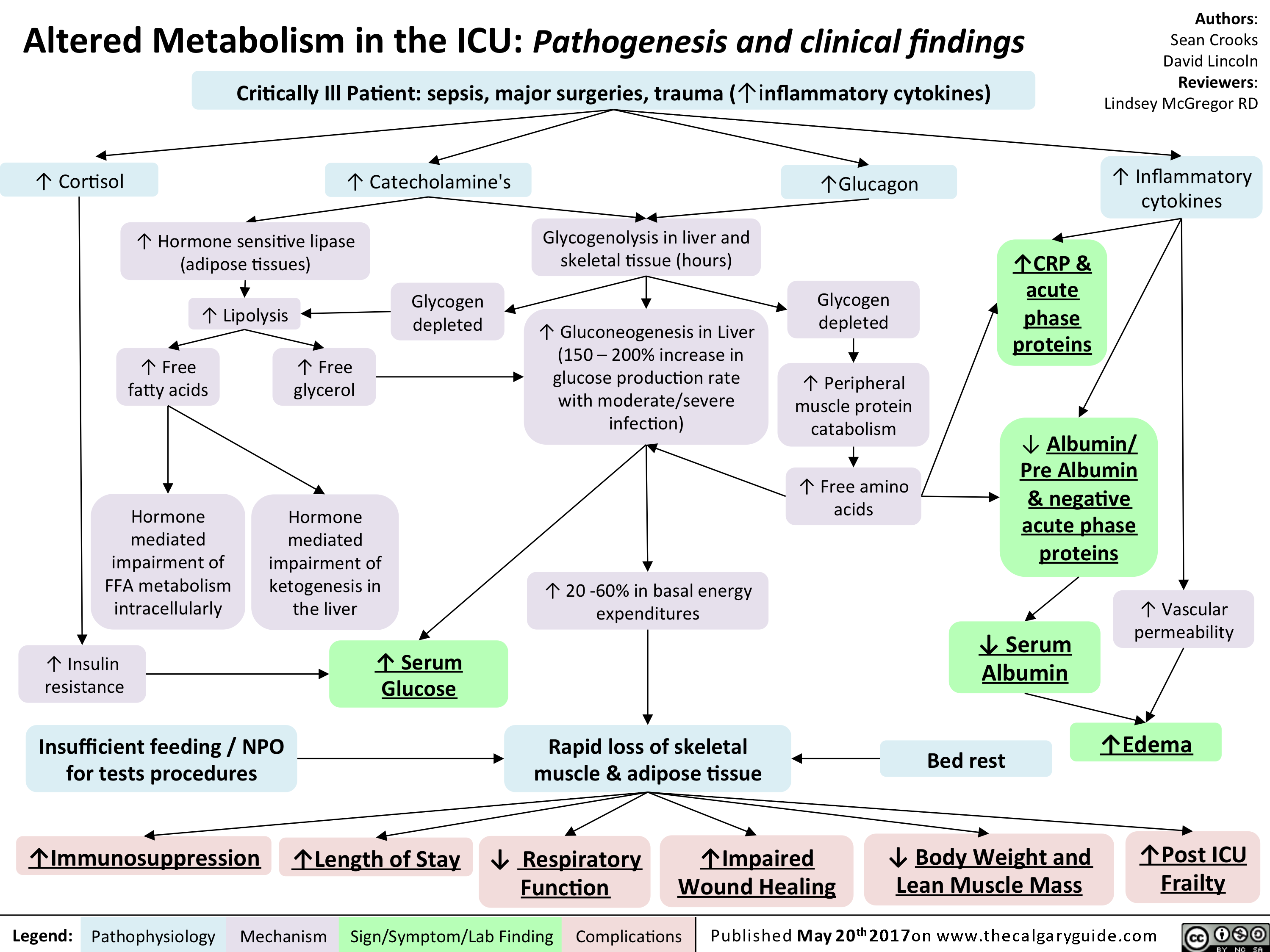
Altered Metabolism in the ICU
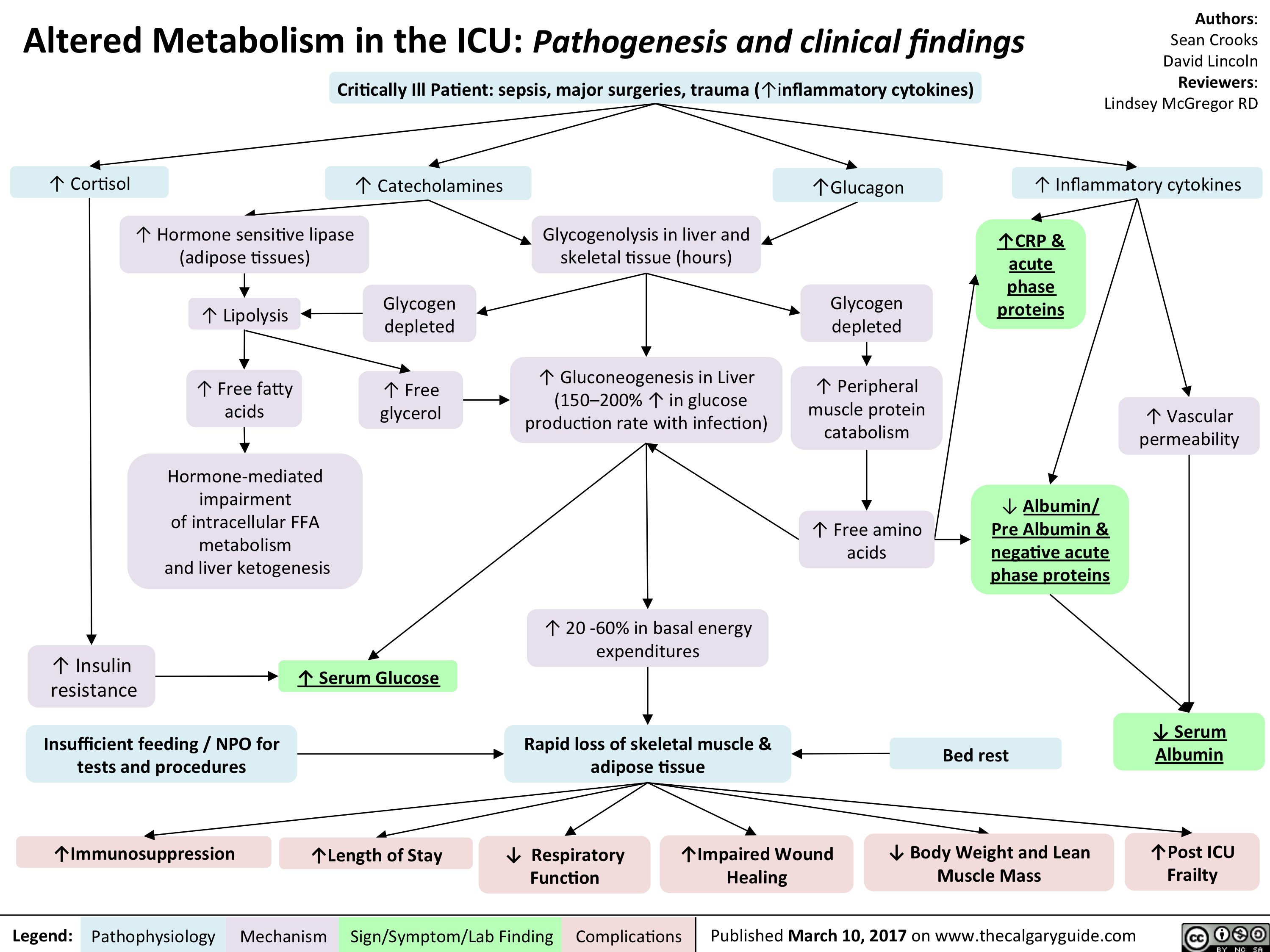
Altered Metabolism in the ICU- Pathogenesis and clinical findings
Mental Status Exam

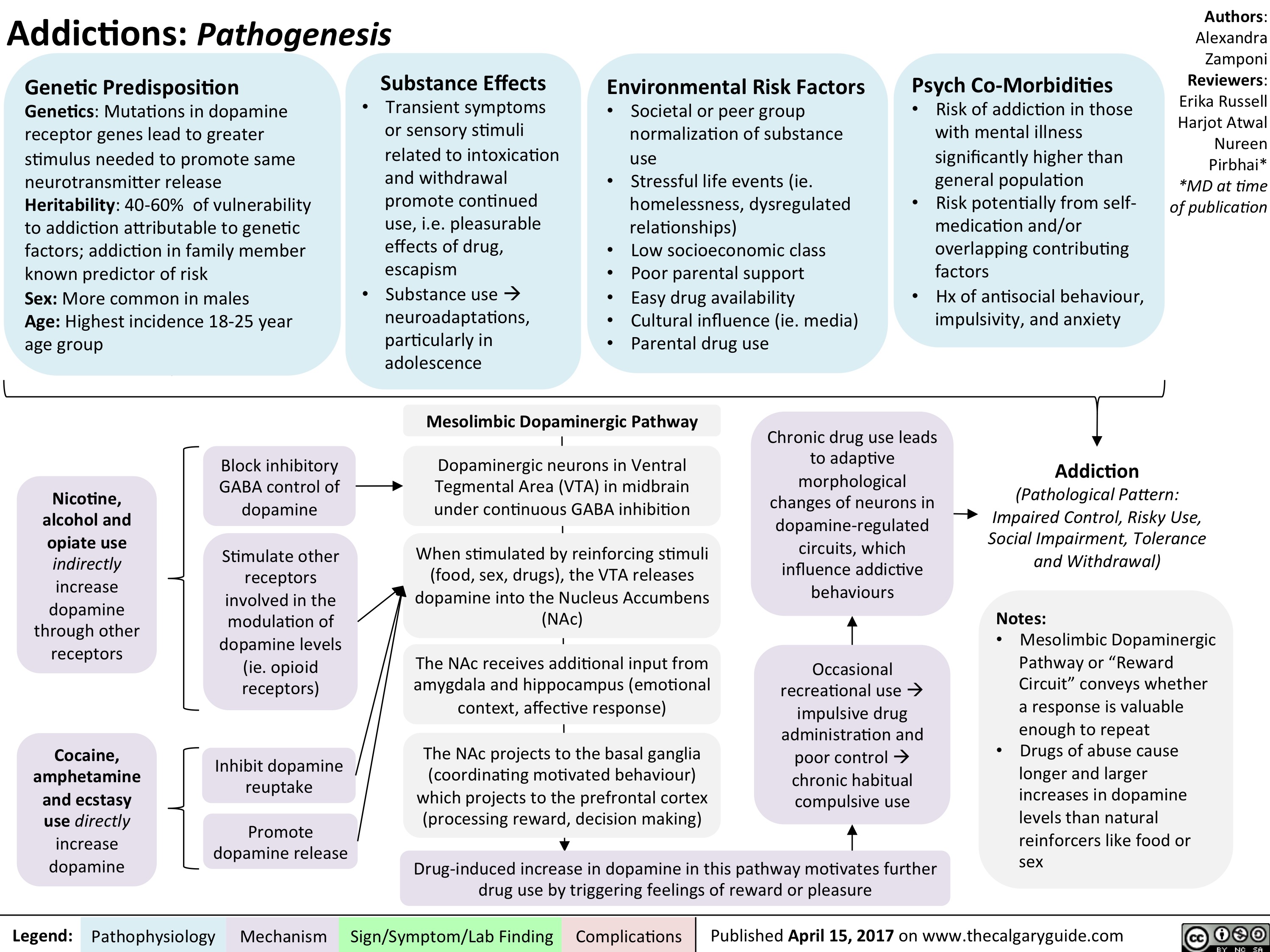
Addiction Long-term Consequences

Addiction Pathogenesis
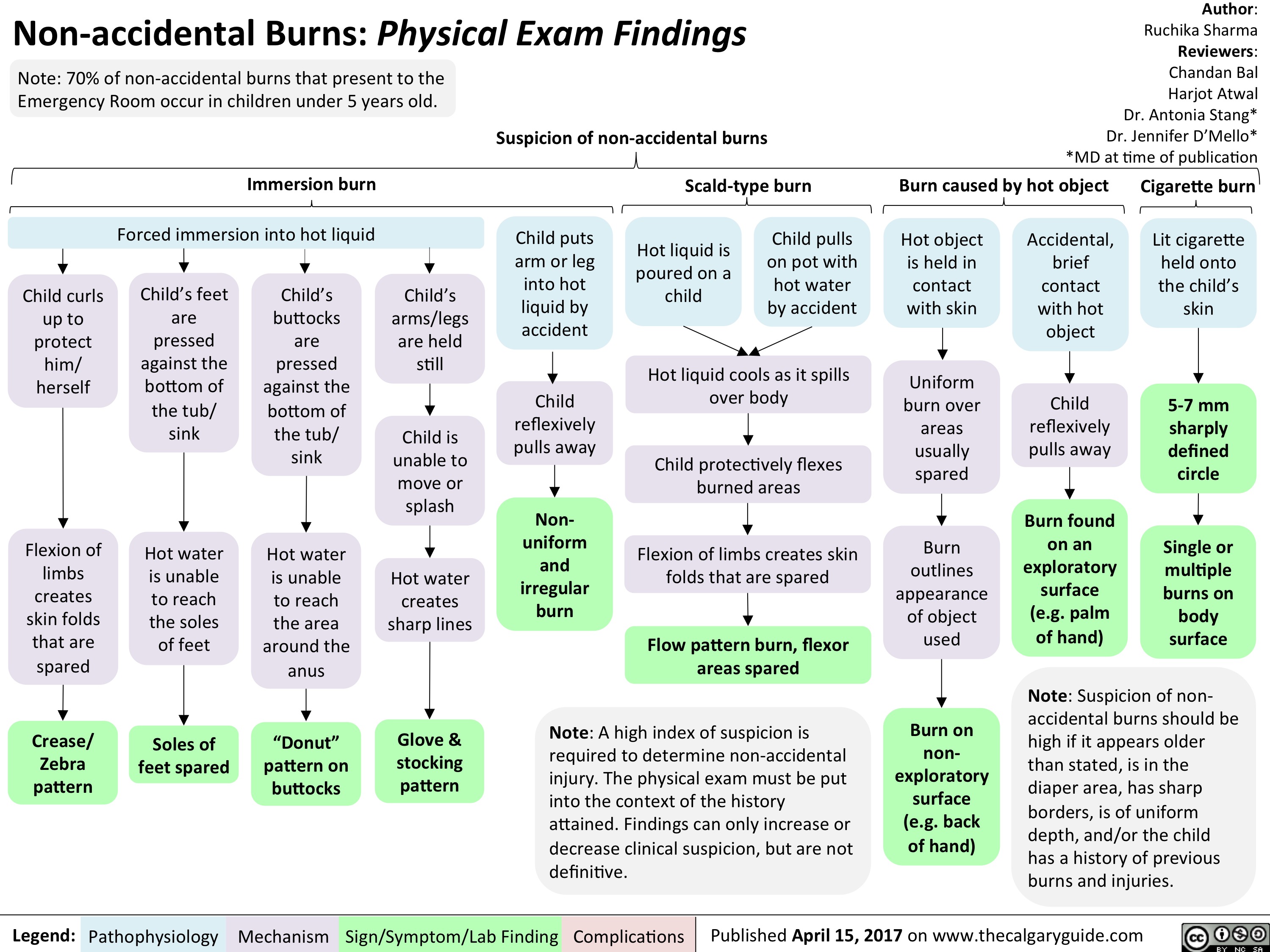
Non-accidental Burns
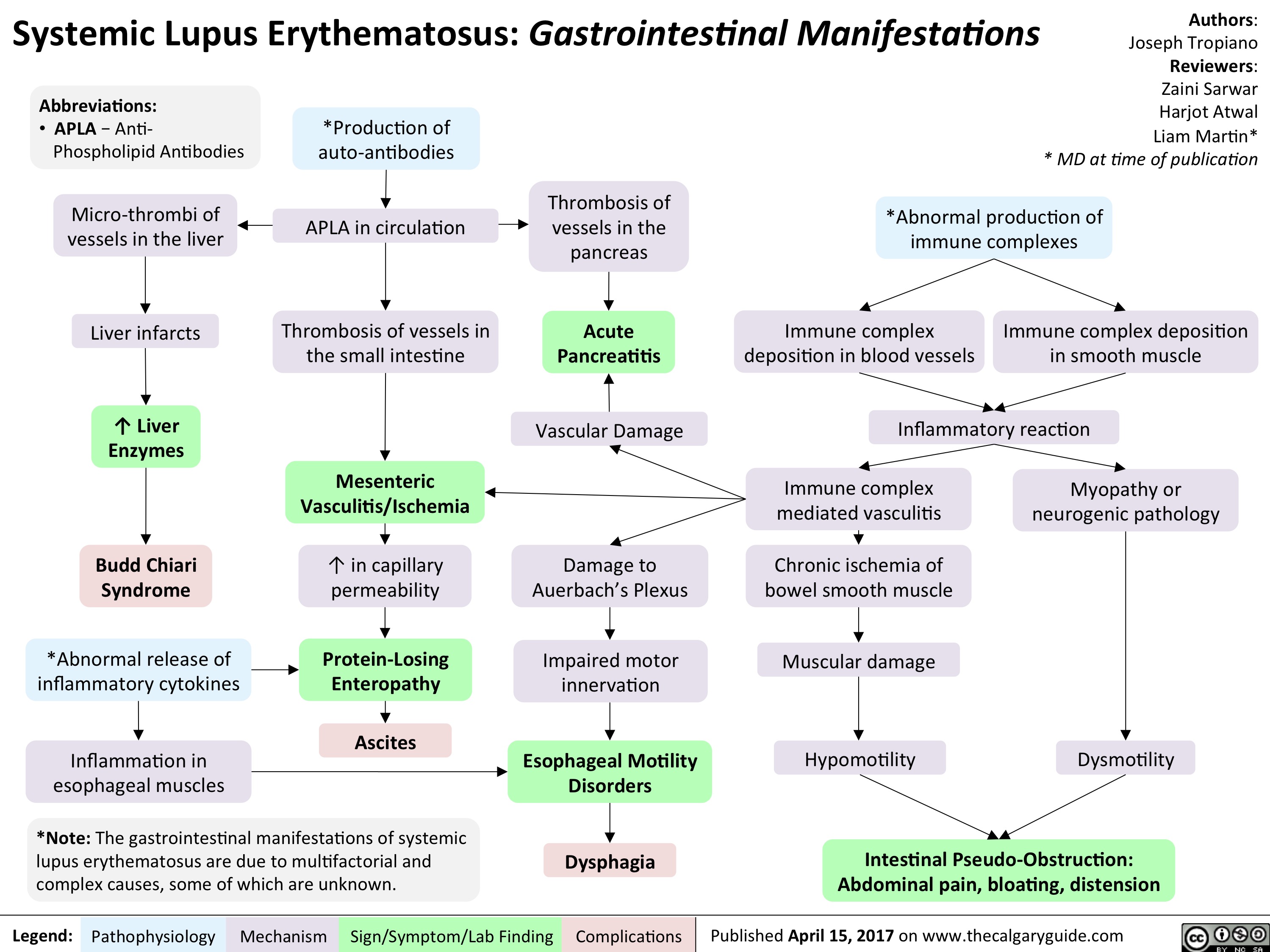
SLE-GI Manifestations
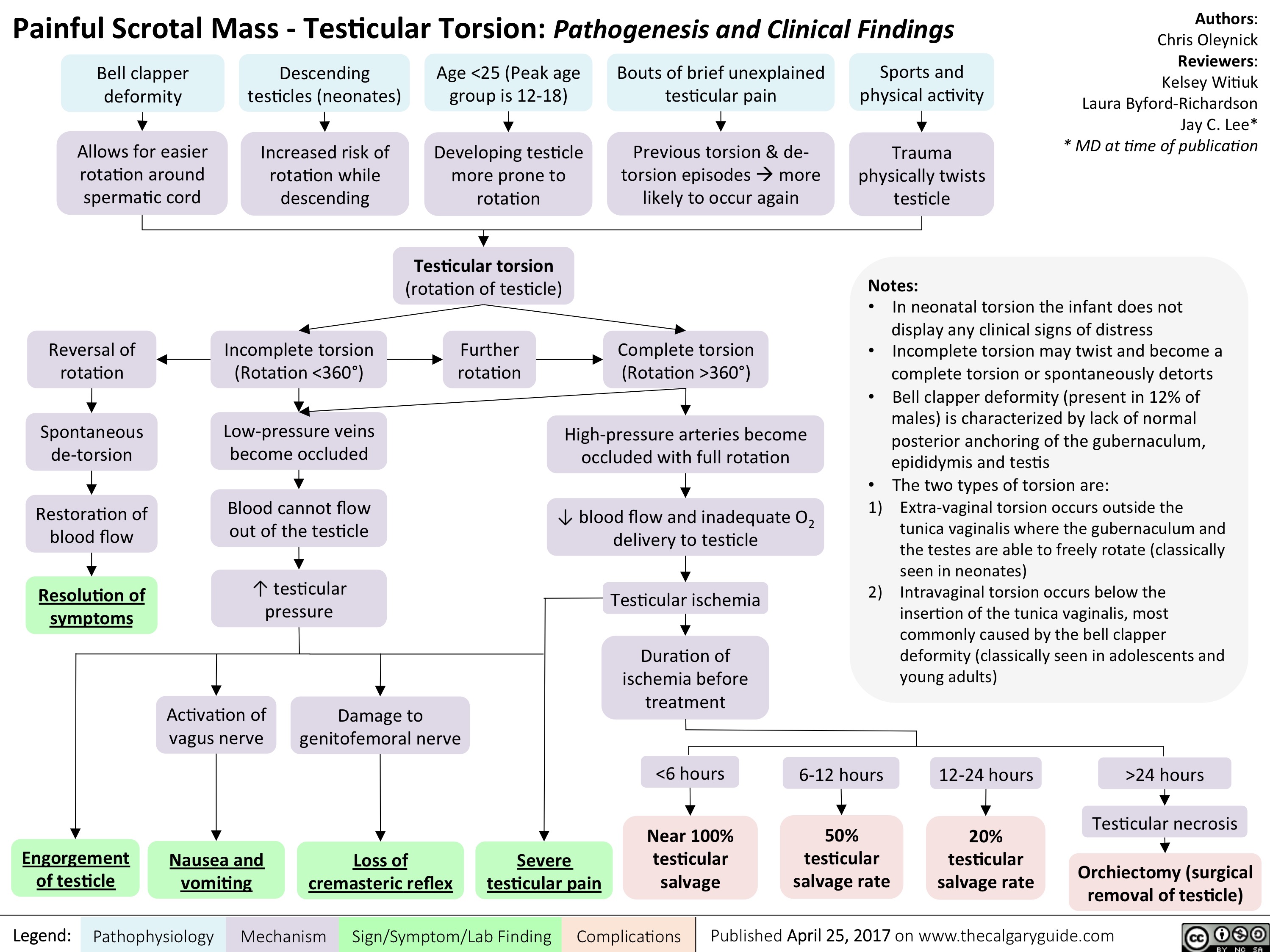
Testicular Torsion
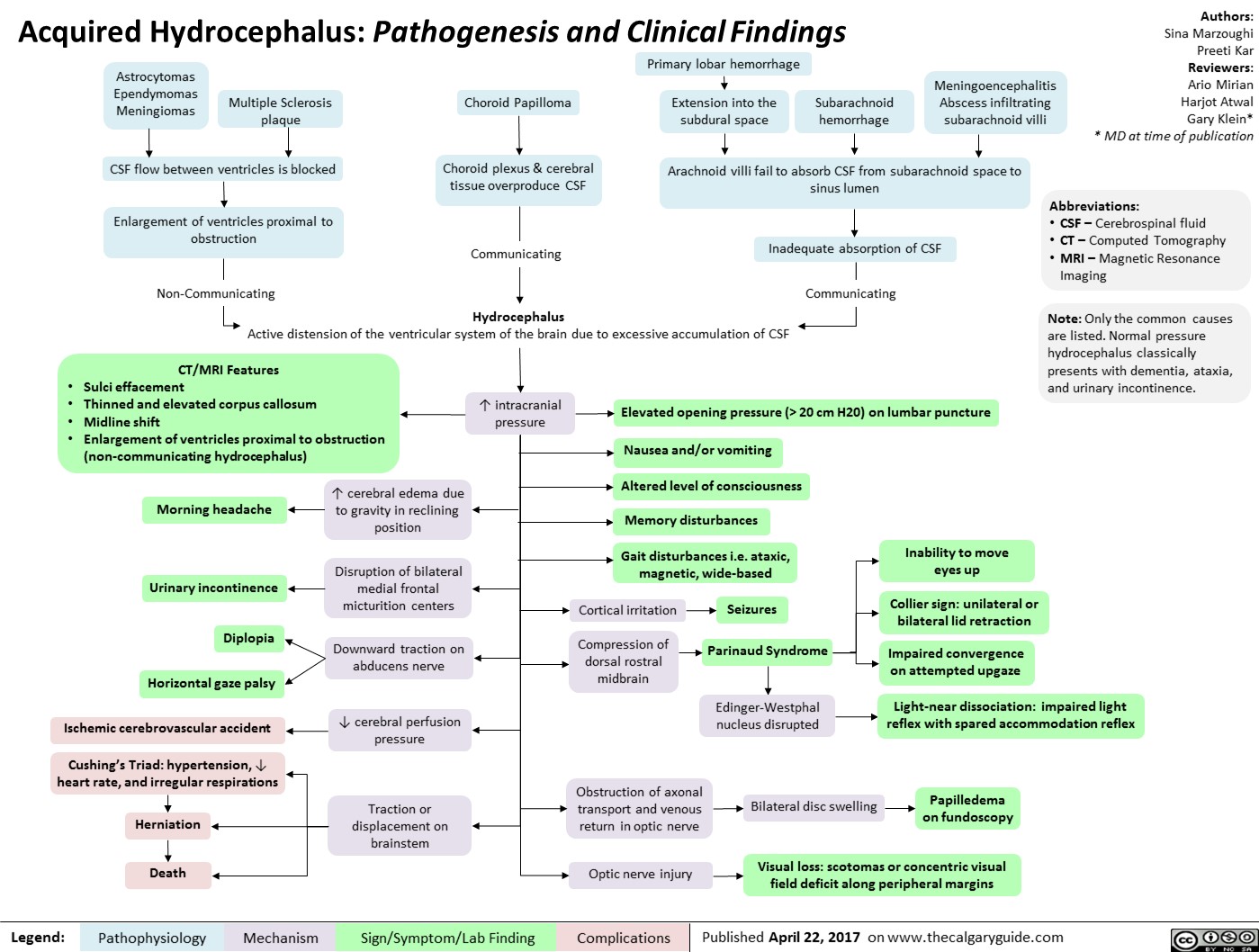
Acquired Hydrocephalus
Kawasaki Disease
Secondary Hemostasis: Coagulation Cascade

systemic-lupus-erythematosus-gastrointestinal-manifestations

Critical Care Malnutrition
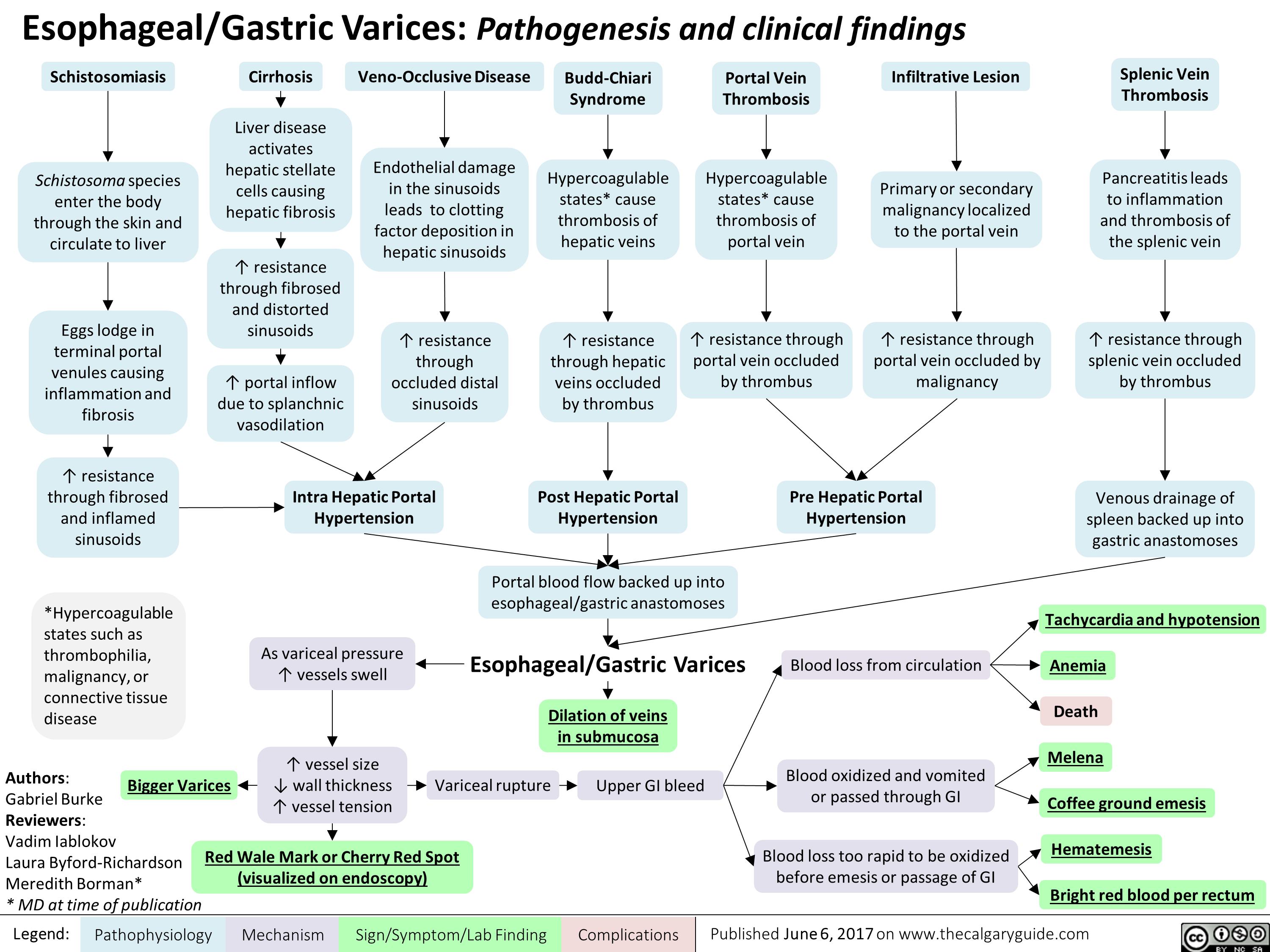
esophageal-gastric-varices
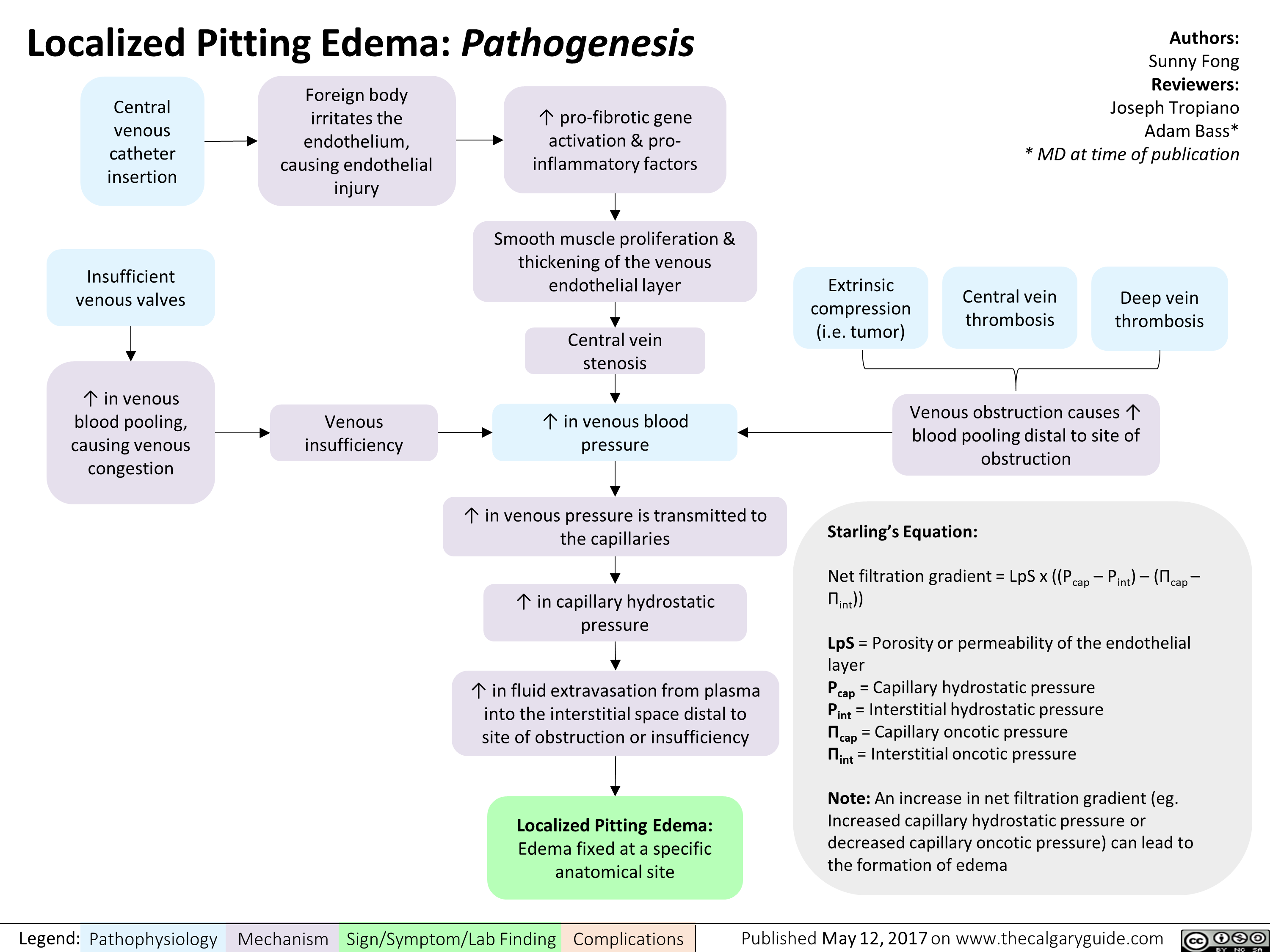
localized-pitting-edema
Neurotransmitters-and-Pharmacology-behind-Nausea-and-Vomiting - IN
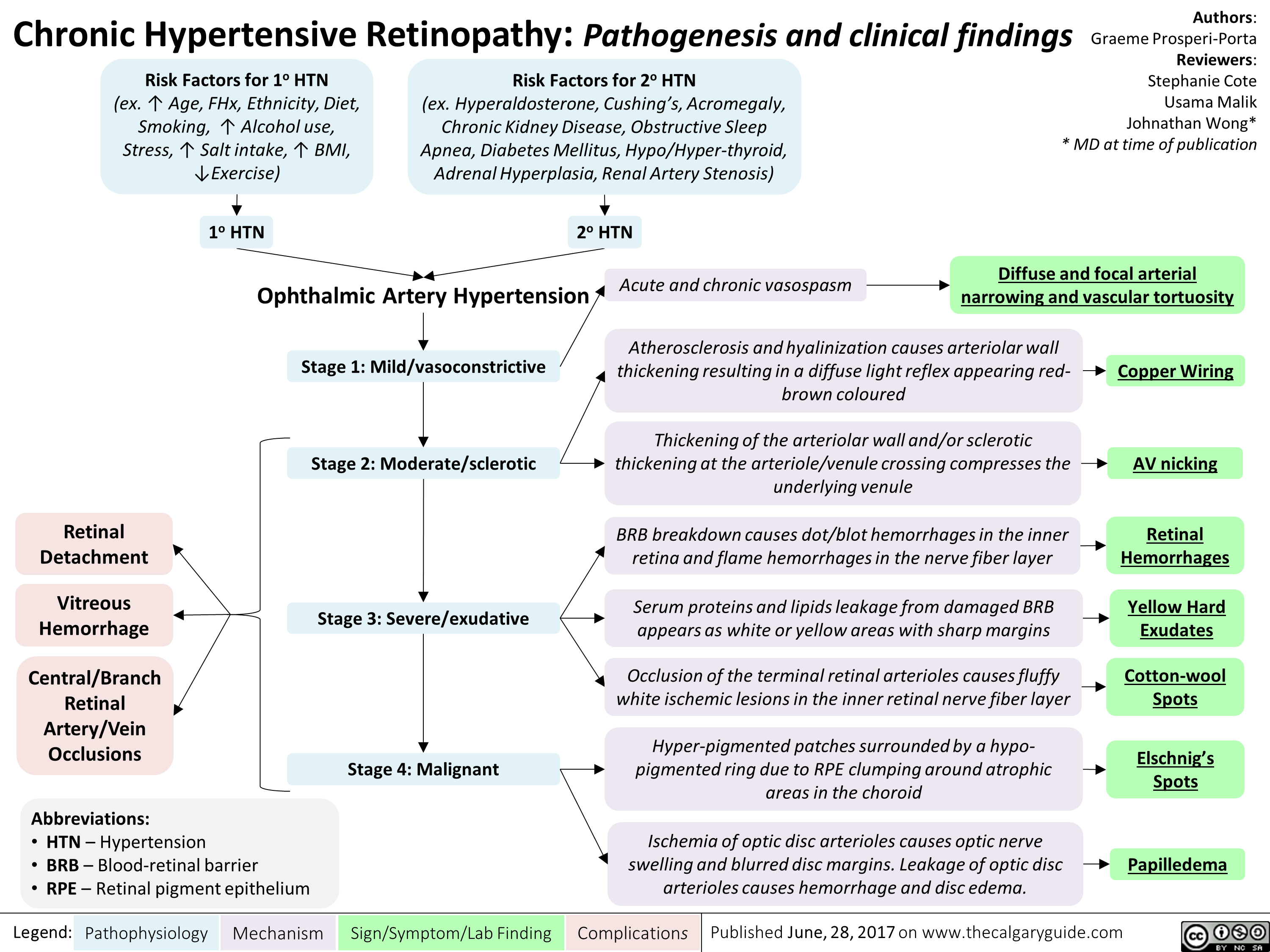
chronic-hypertensive-retinopathy-pathogenesis-and-clinical-findings
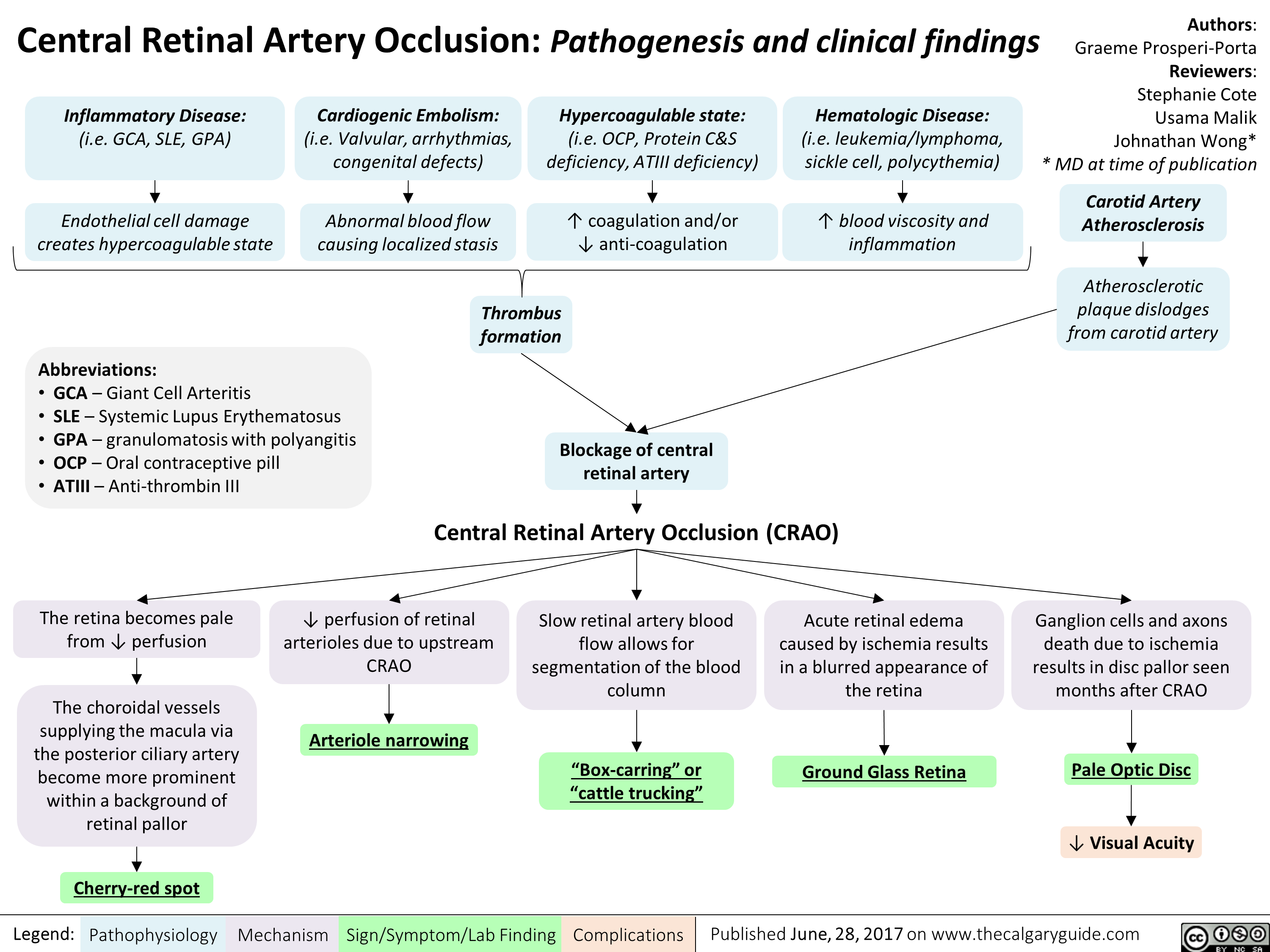
central-retinal-artery-occlusion-pathogenesis-and-clinical-findings
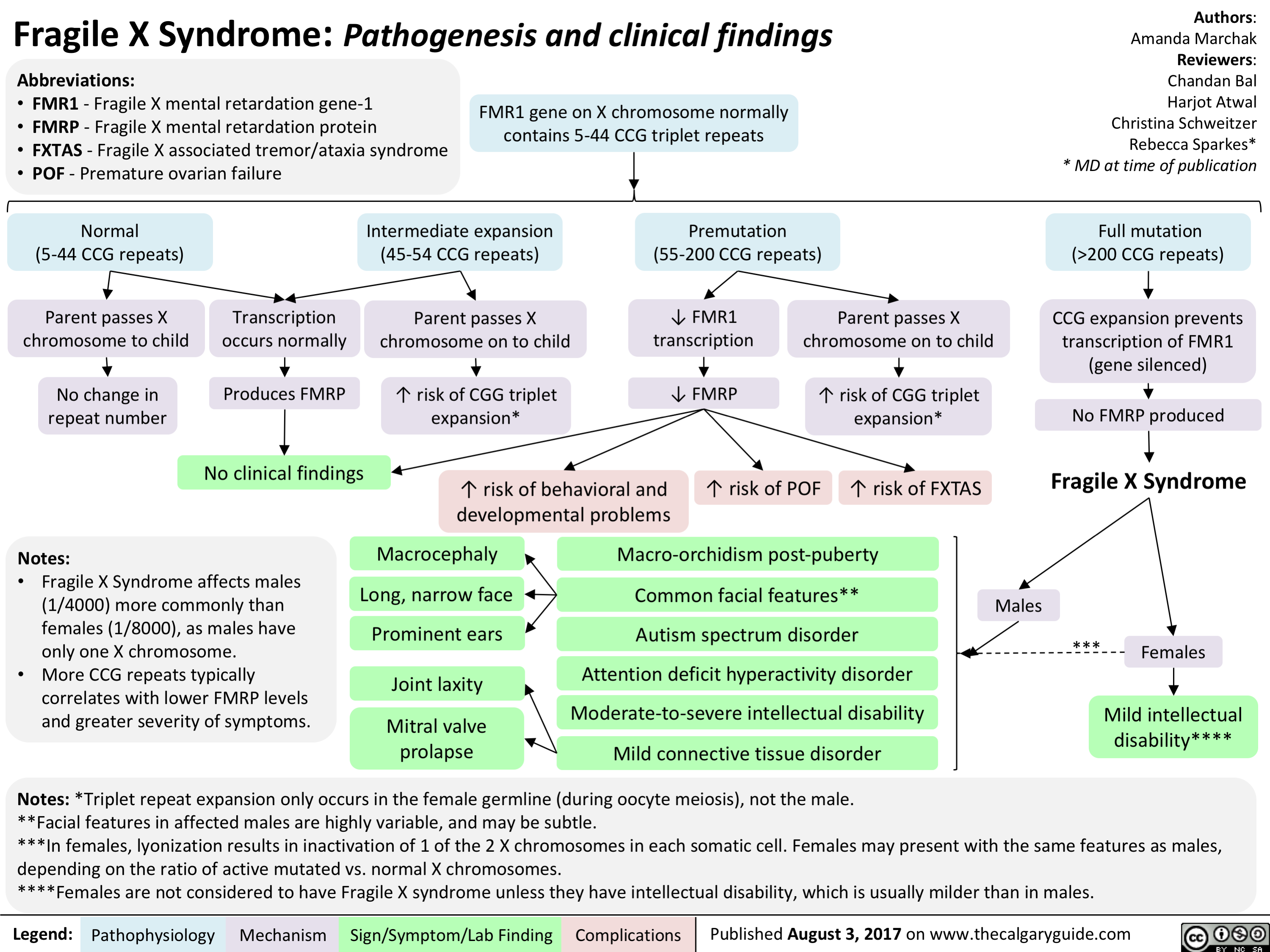
Fragile X Syndrome
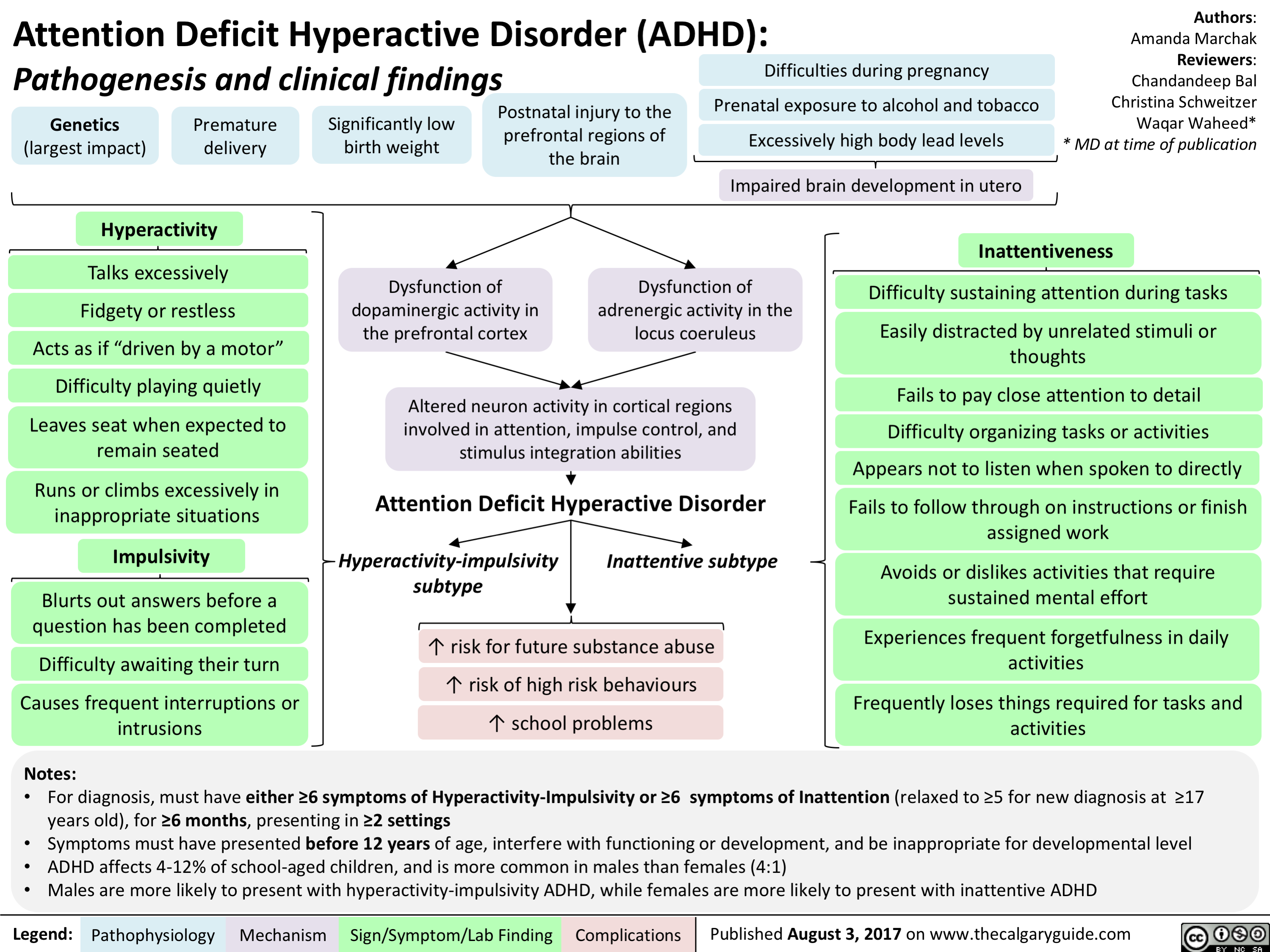
Attention Deficit Hyperactivity Disorder (ADHD)
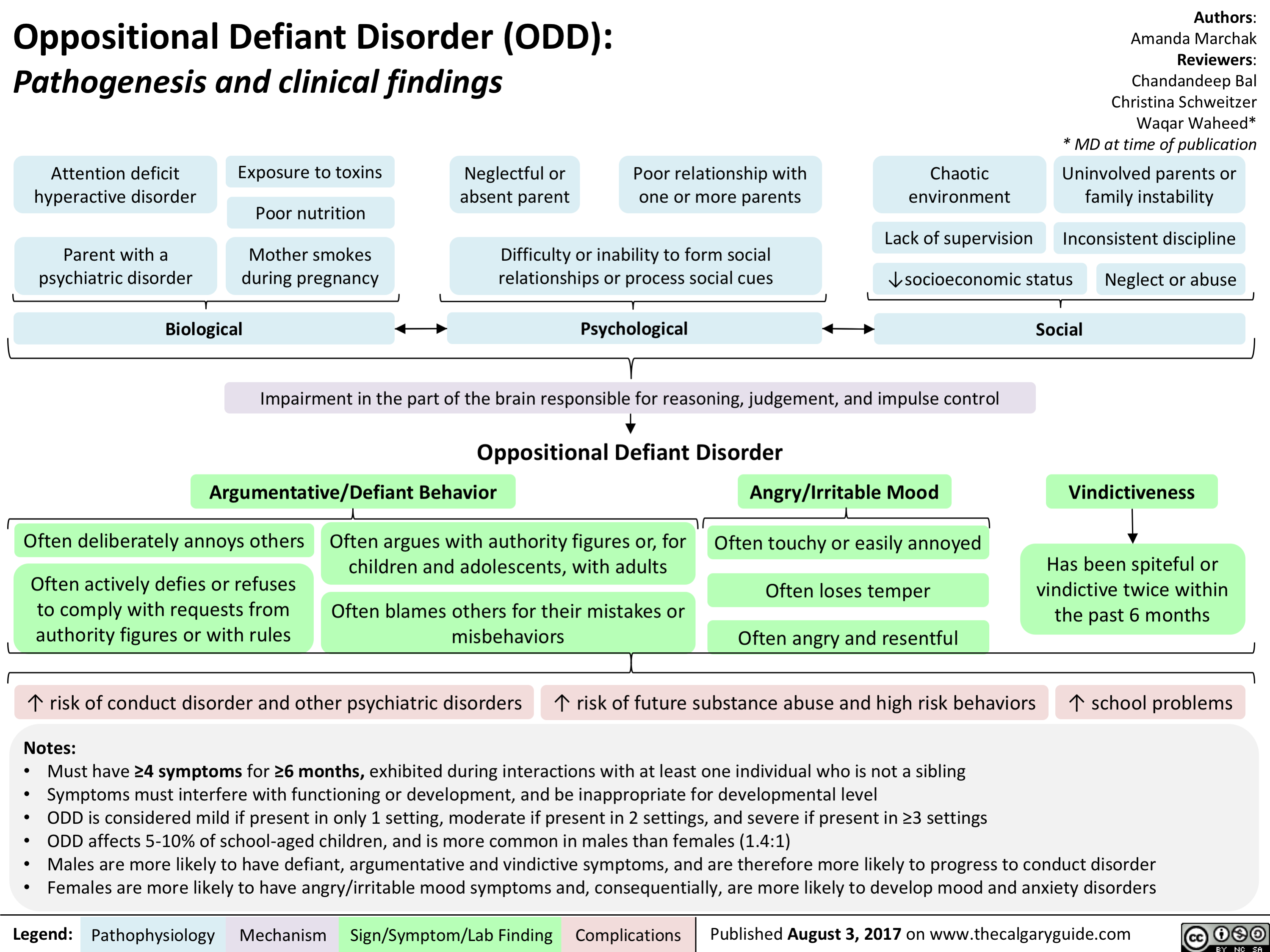
Oppositional Defiant Disorder (ODD)
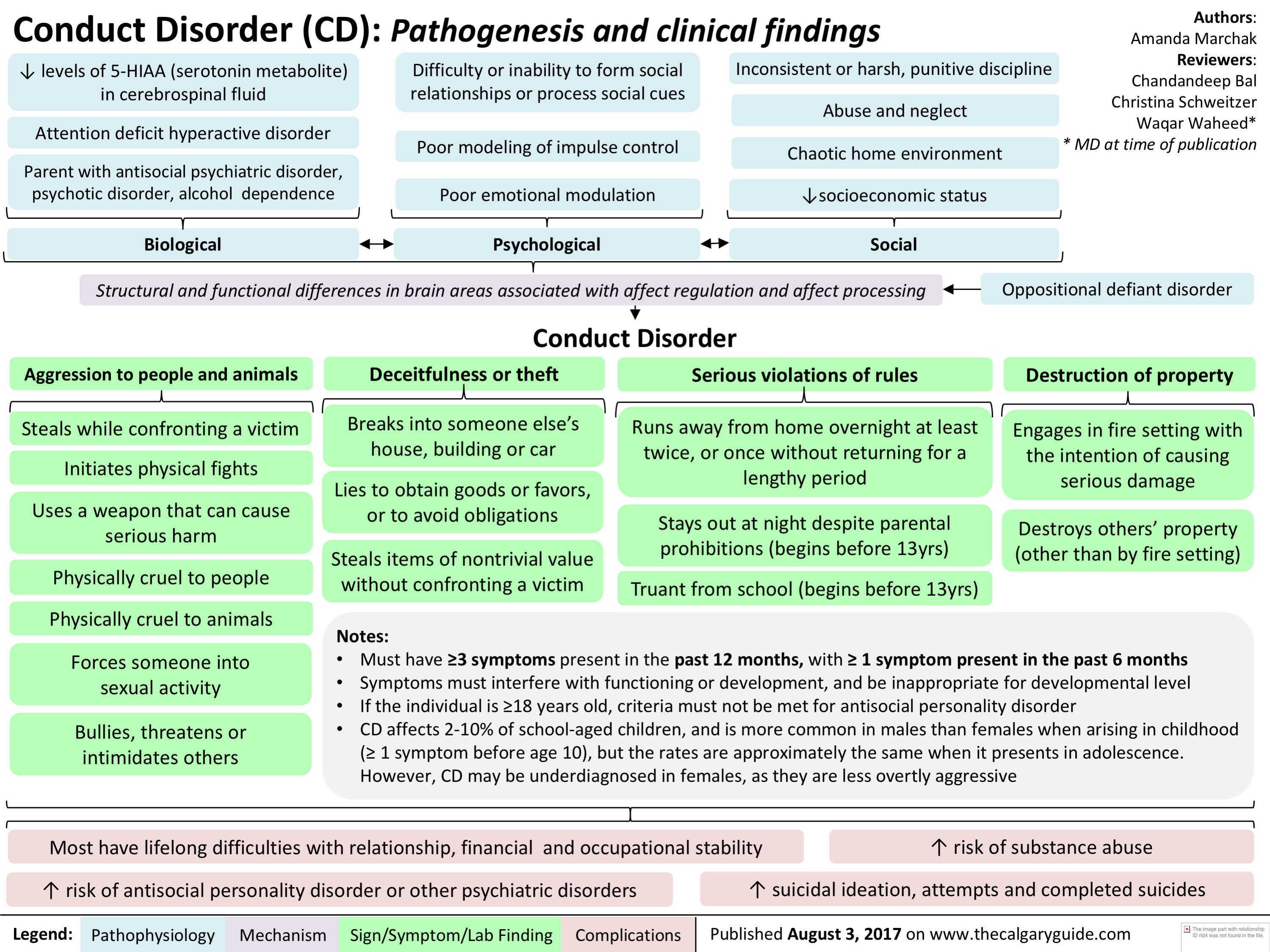
Conduct Disorder (CD)
Down Syndrome

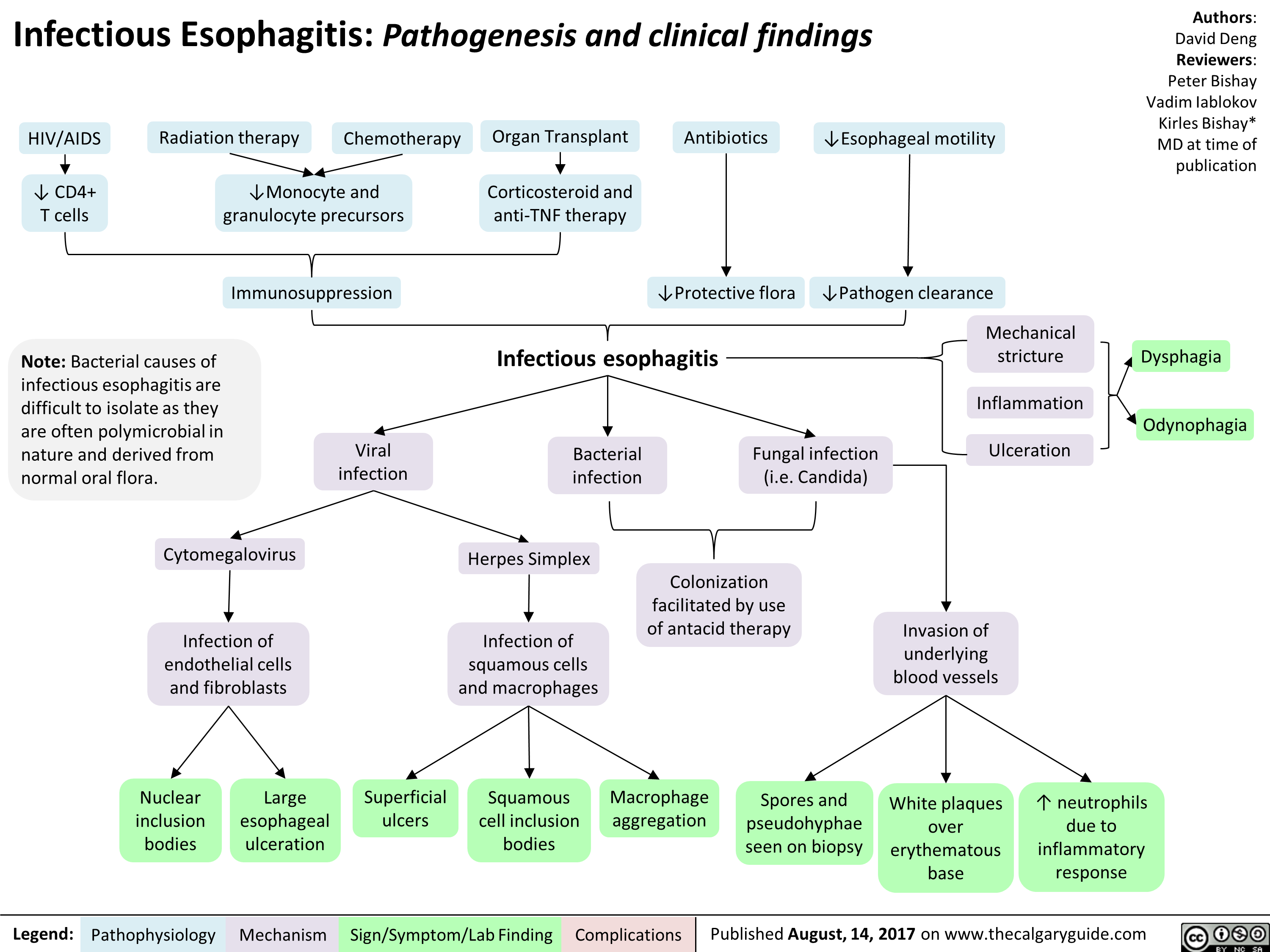
infectious-esophagitis-pathogenesis-and-clinical-findings
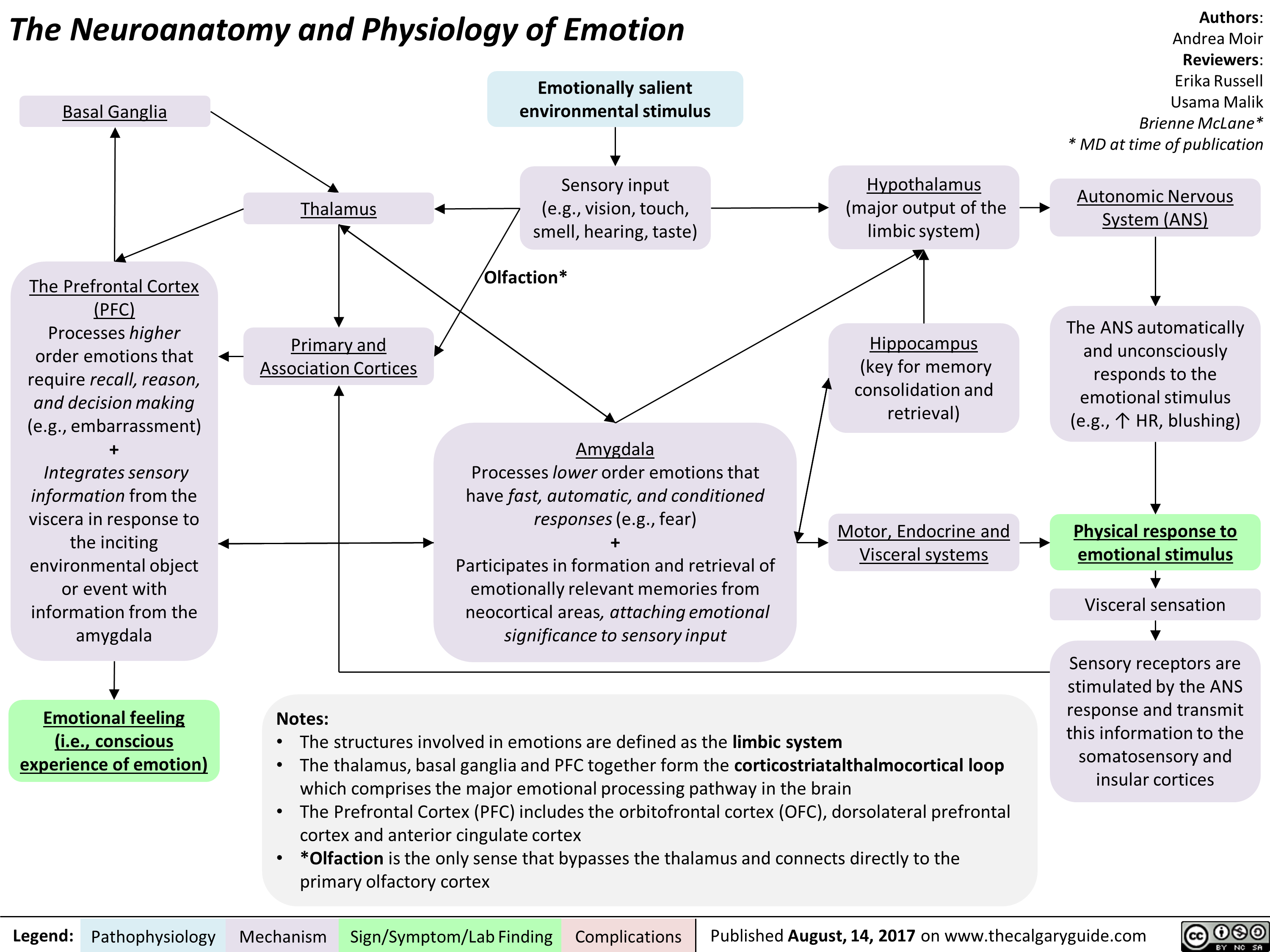
The Neuroanatomy and Physiology of Emotion
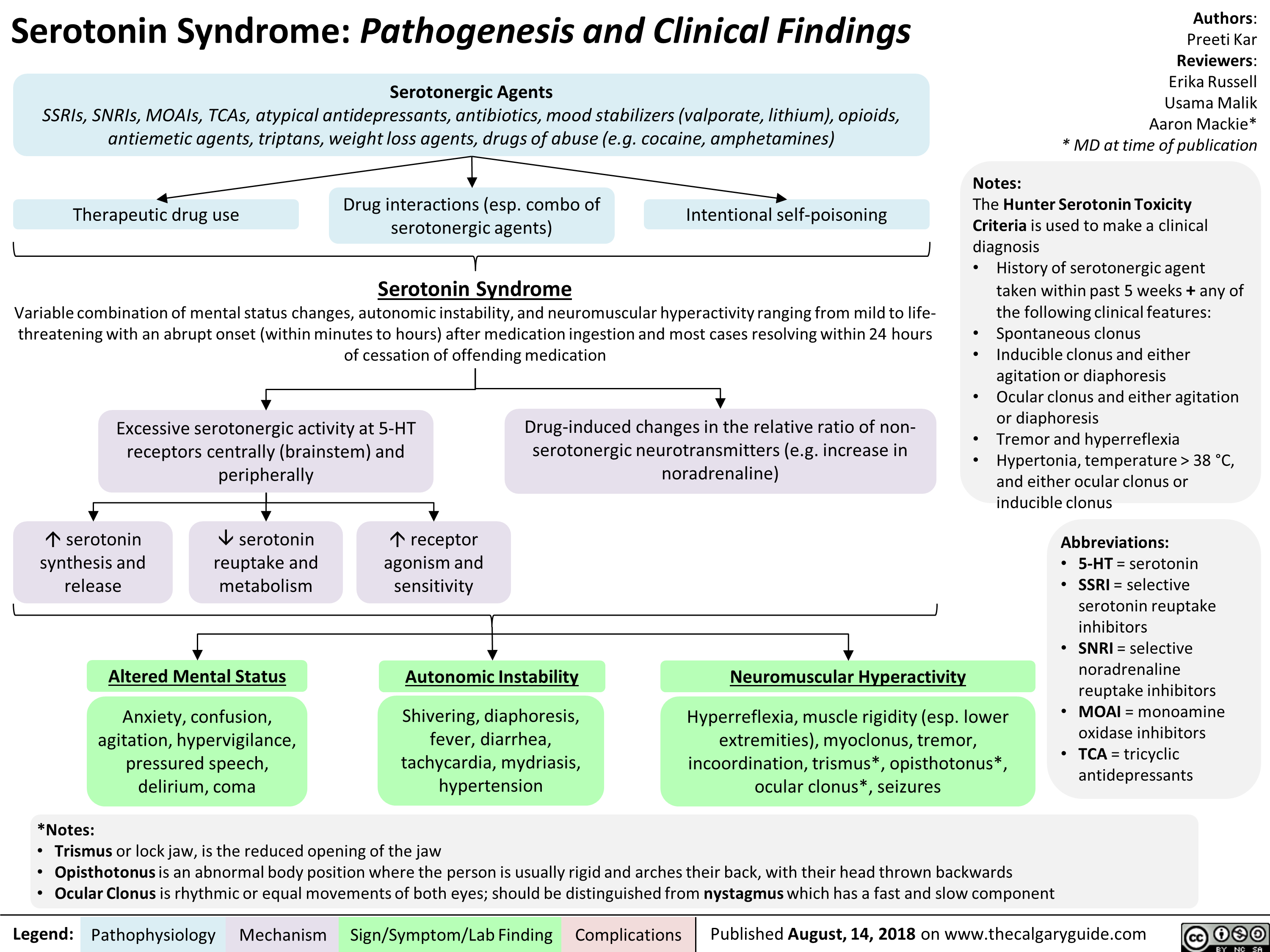
Serotonin Syndrome Pathogenesis and Clinical Findings
Side Effects of ACEi/ARBs During Pregnancy

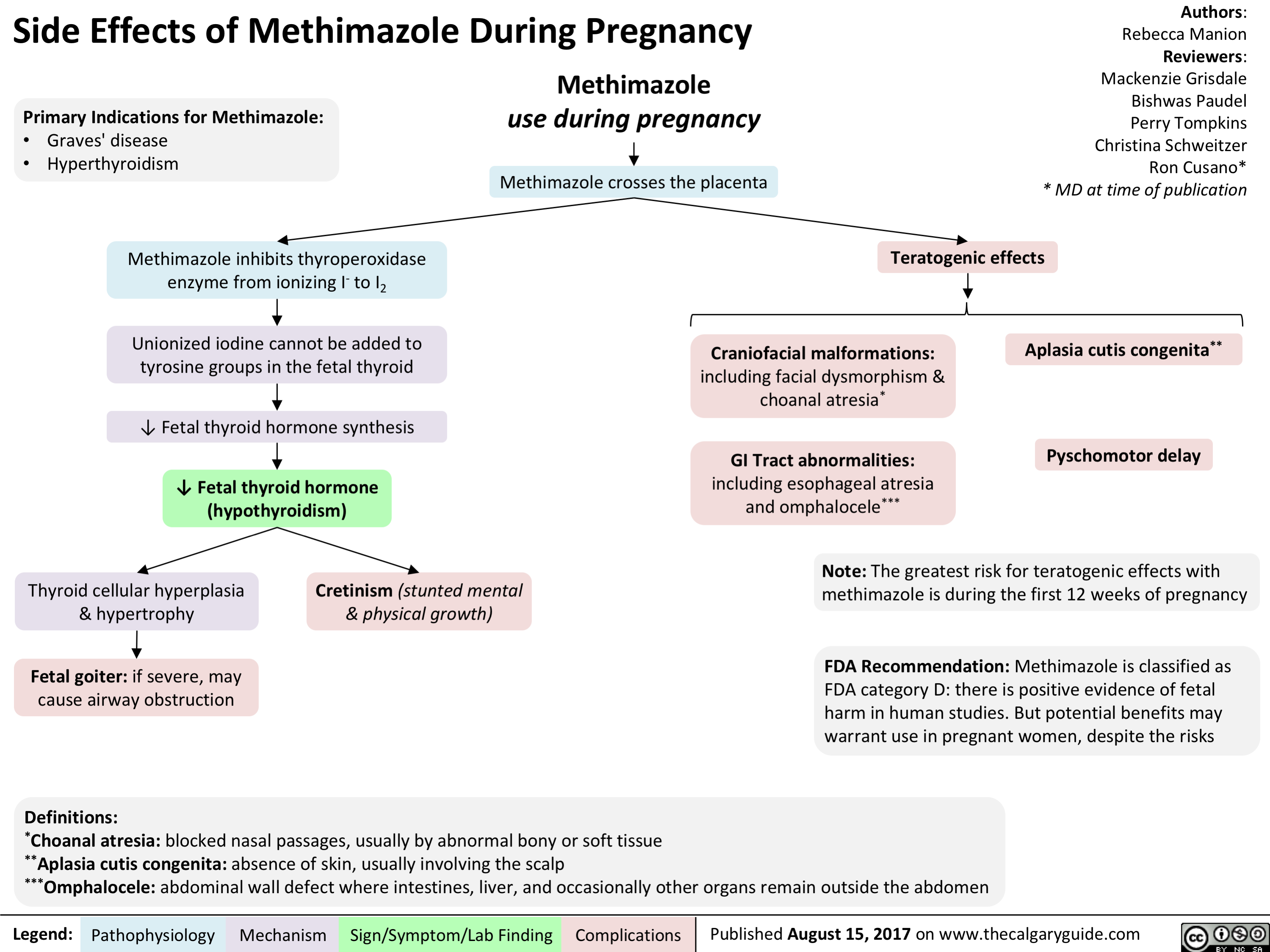
Side Effects of Methimazole During Pregnancy
Side Effects of NSAIDs During Pregnancy

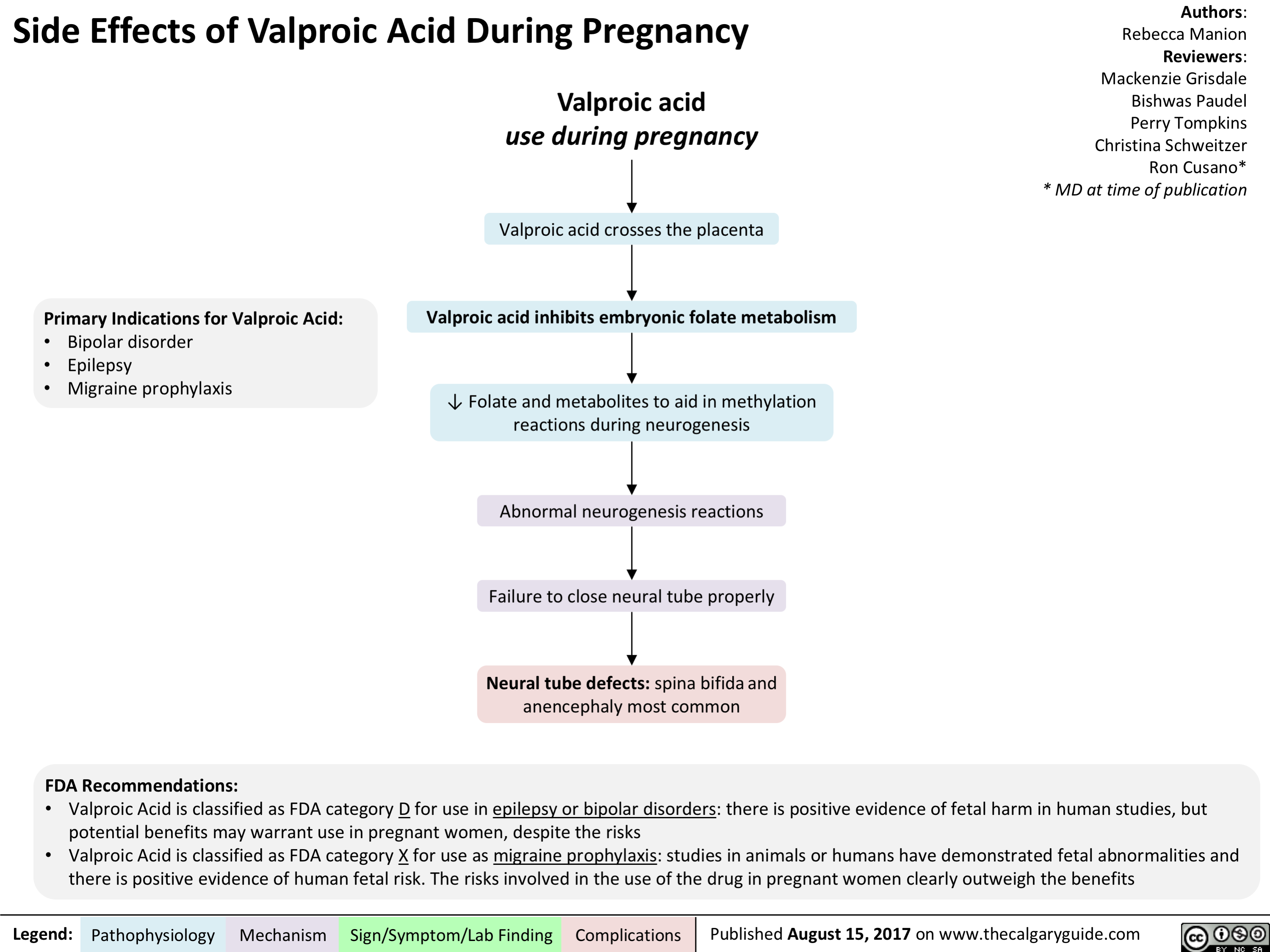
Side Effects of Valproic Acid During Pregnancy
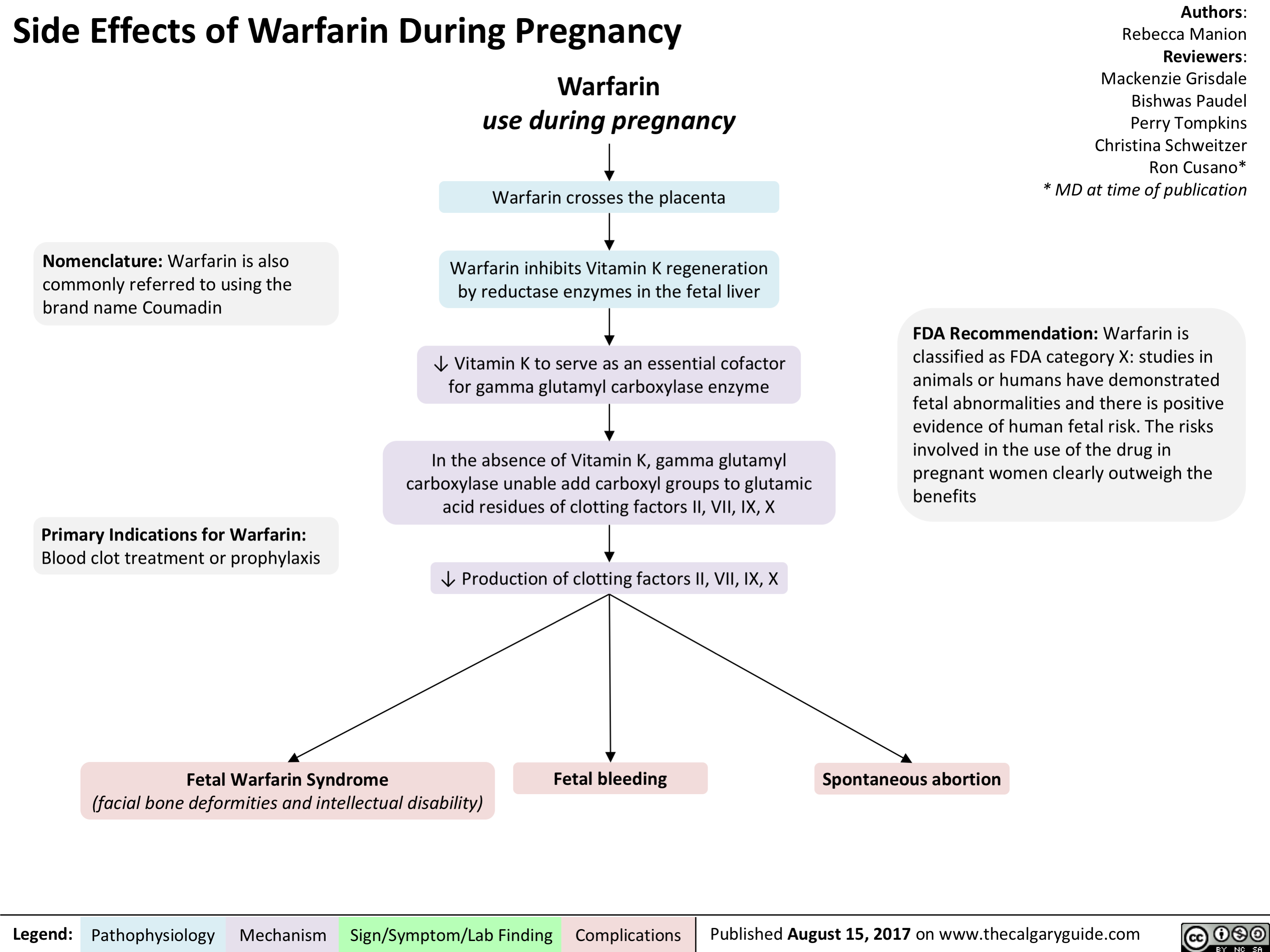
Side Effects of Warfarin During Pregnancy
Pediatric Parasomnias and Nightmares: Pathogenesis and clinical findings

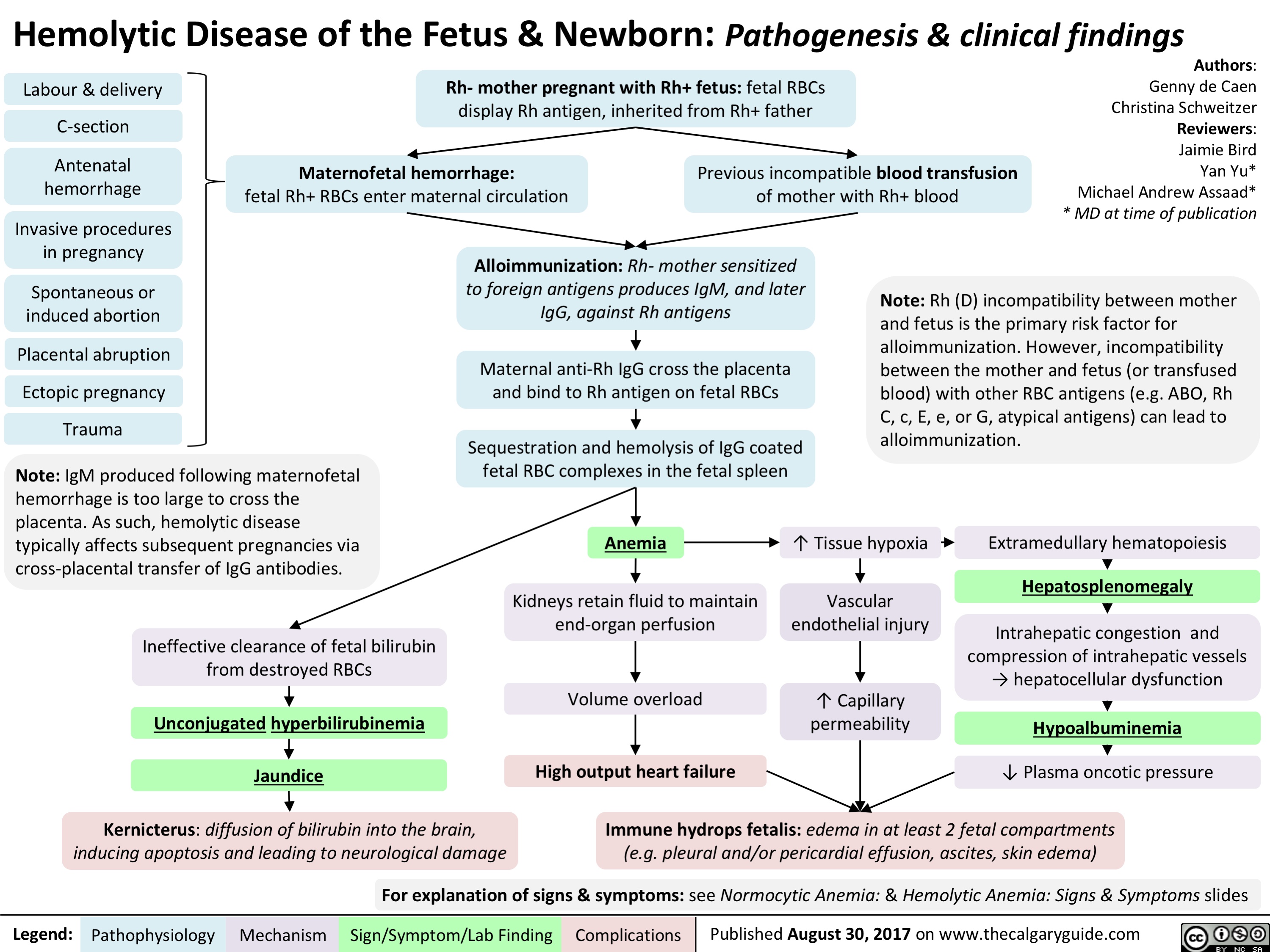
Hemolytic Disease of the Fetus and Newborn
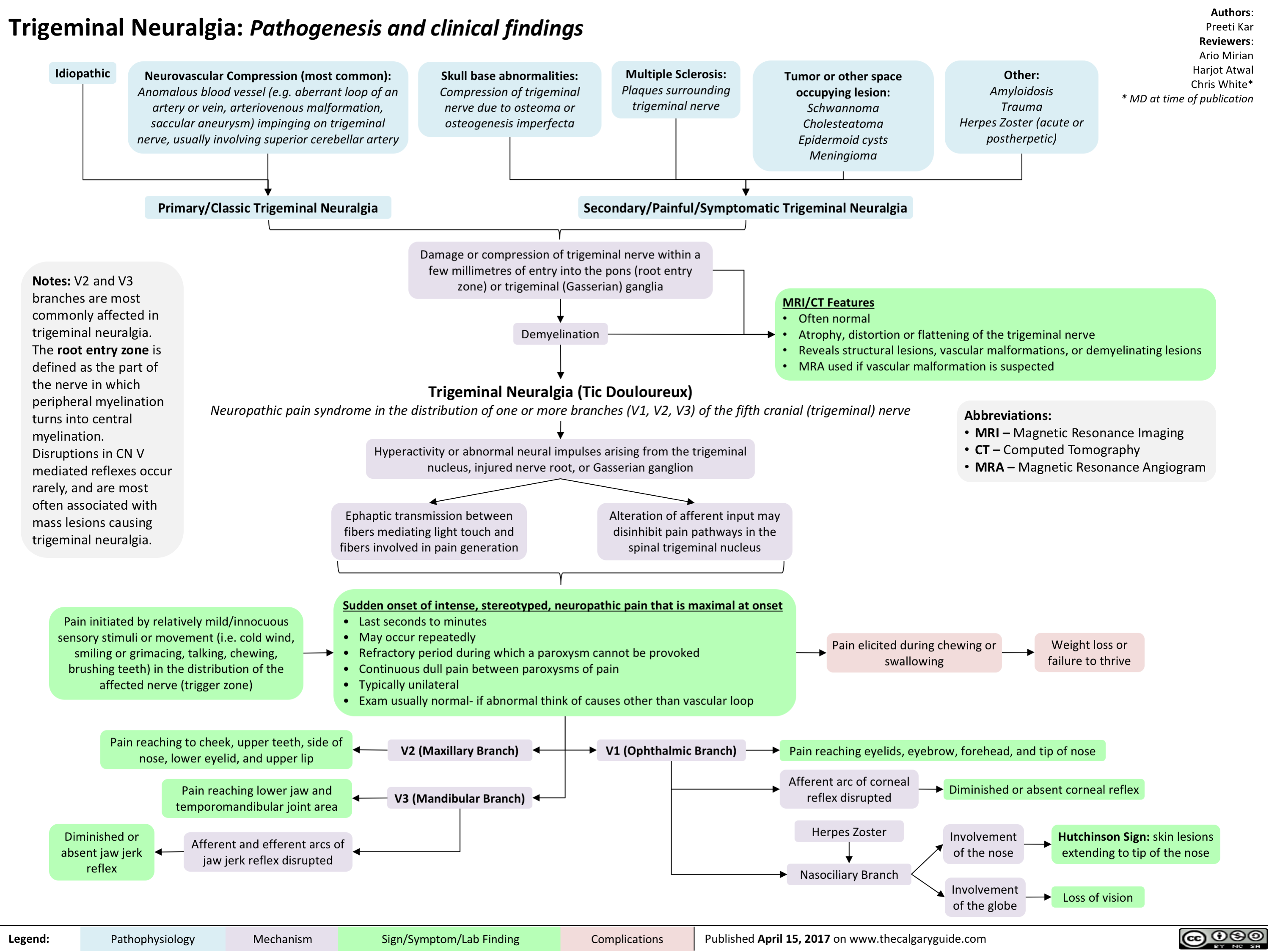
Trigeminal Neuralgia
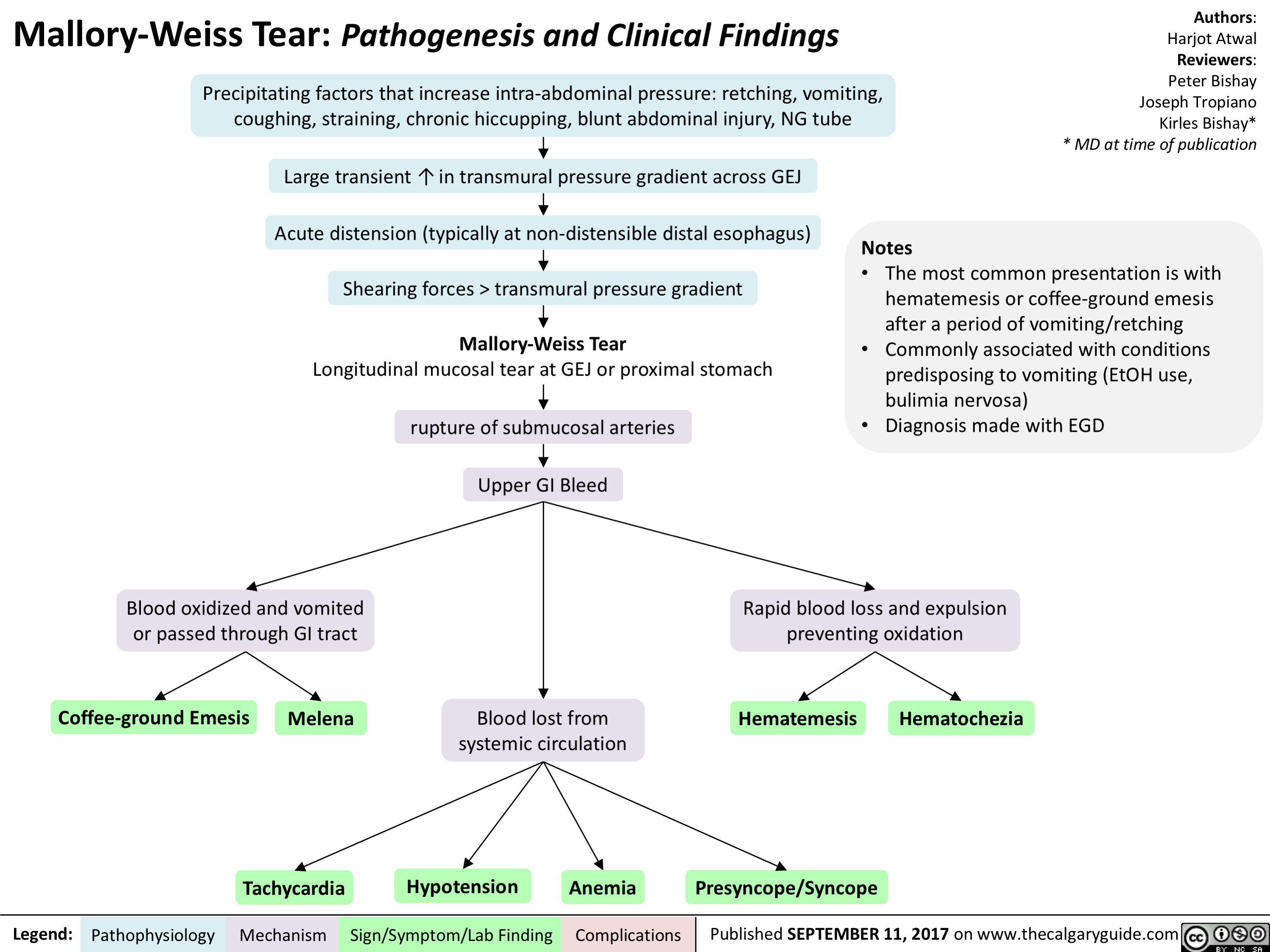
Mallory-Weiss Tear
Unconjugated Neonatal Hyperbilirubinemia - Complications

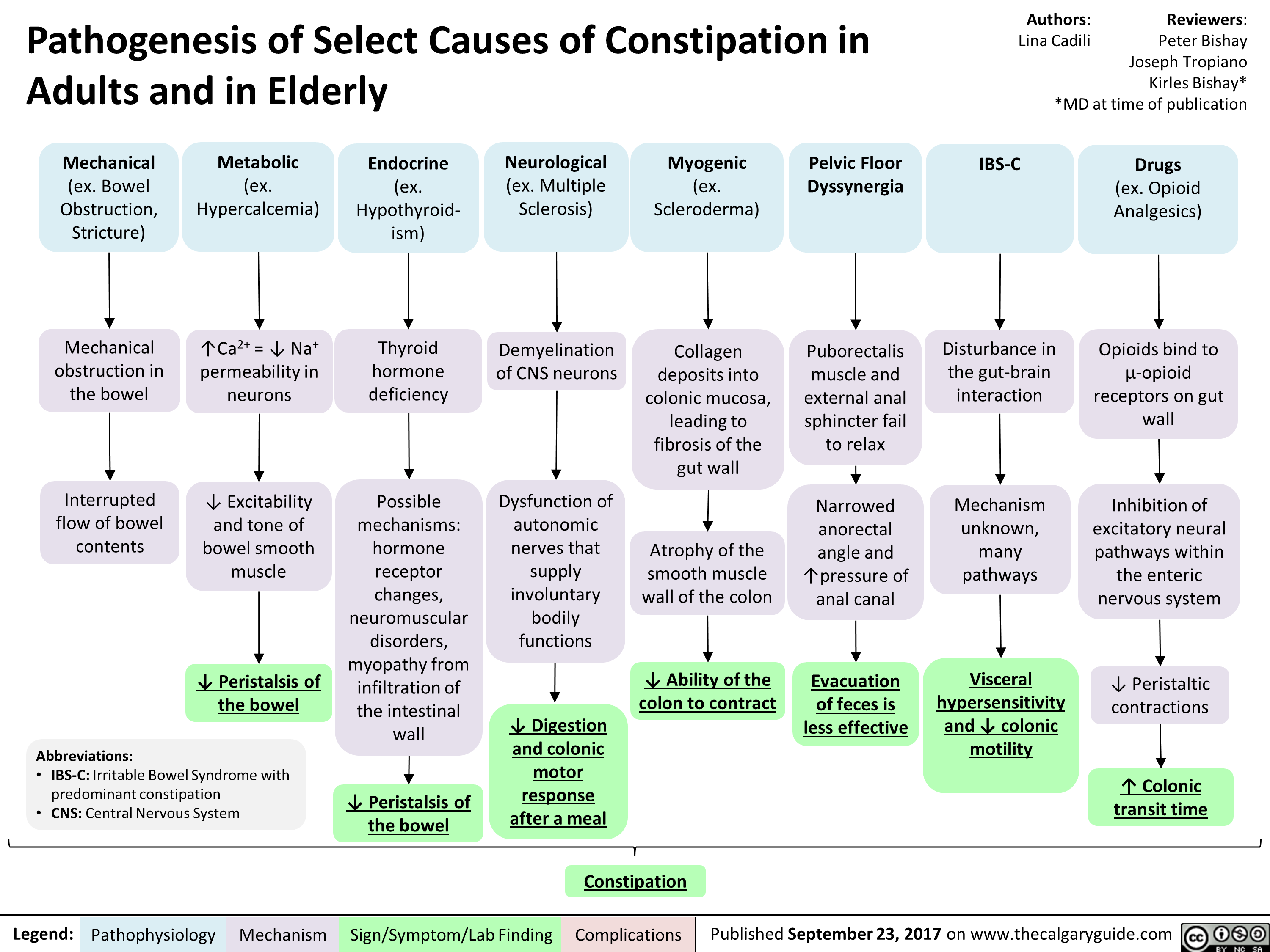
pathogenesis-of-select-causes-of-constipation-in-adults-and-in-elderly
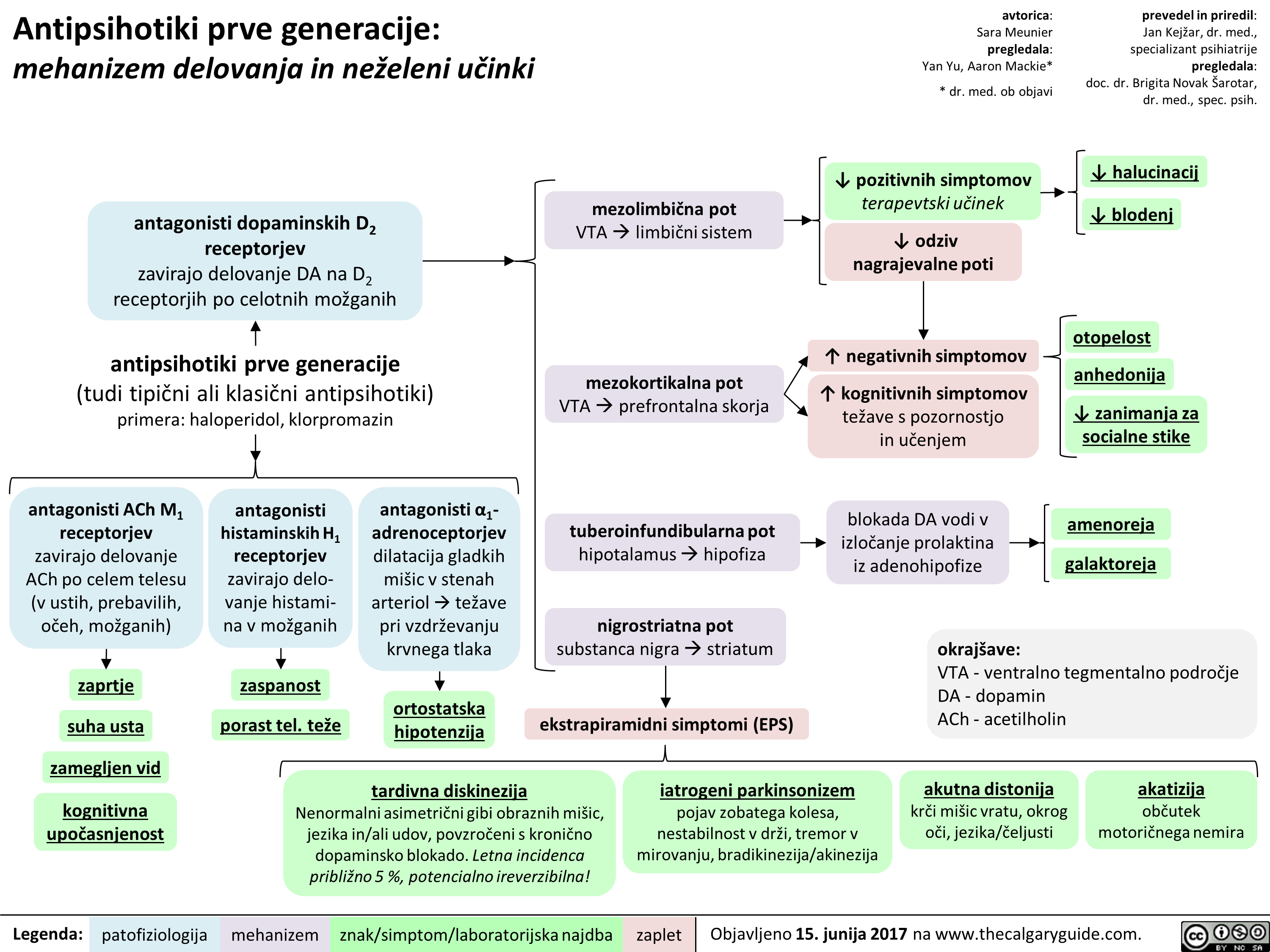
1st gen antipsychotics (Slovenian translation) - FINAL VERSION
2nd gen antipsychotics (Slovenian translation) - FINAL VERSION
3rd gen antipsychotics (Slovenian translation) - FINAL VERSION
Alcohol Use Disorder (Slovenian translation) - FINAL VERSION
BMR (Slovenian translation) - FINAL VERSION
Bupropion (Slovenian translation) - FINAL VERSION
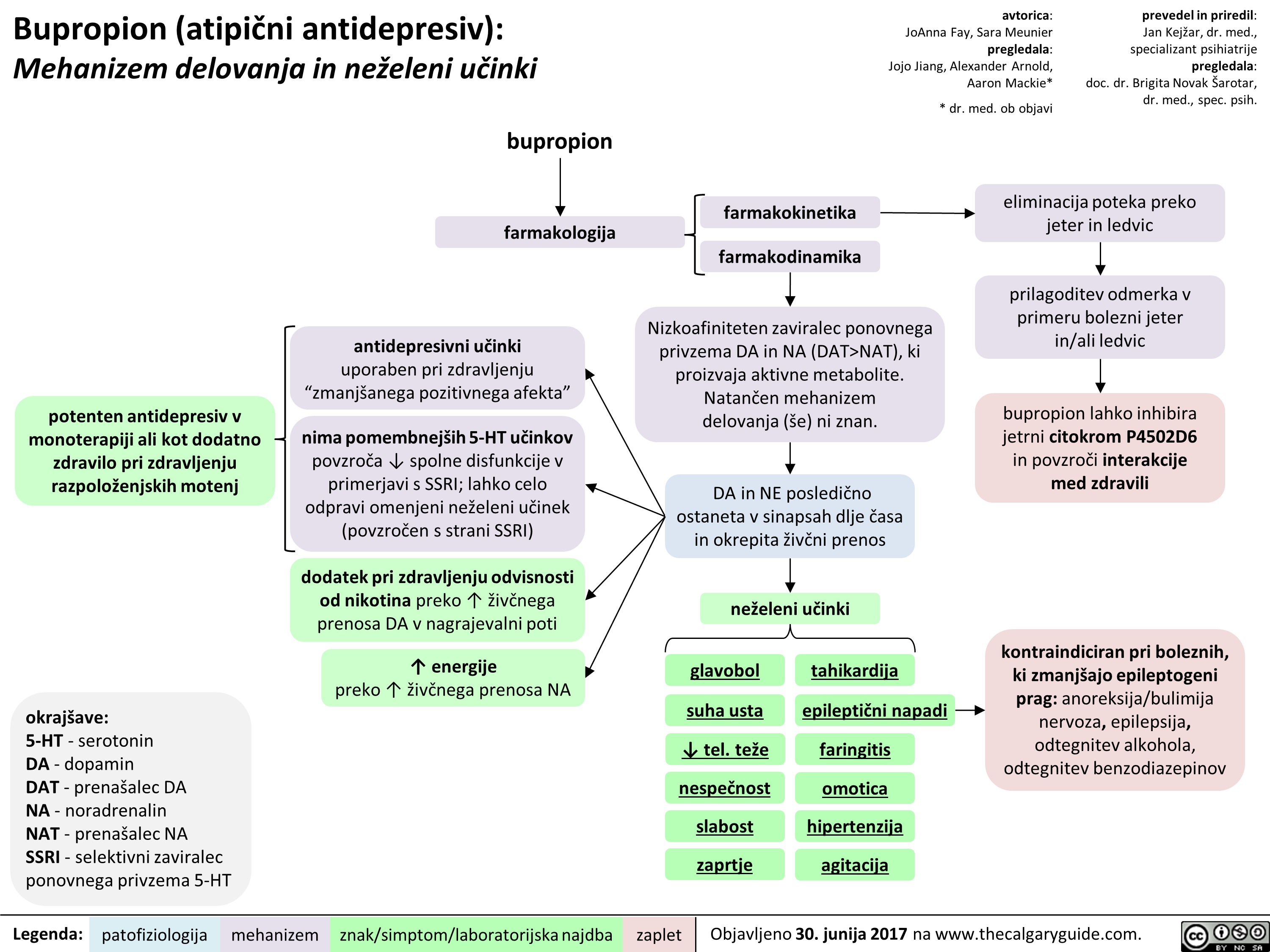 NAT), ki proizvaja aktivne metabolite. Natan'6en mehanizem delovanja (se) ni znan.
znak/simptom/laboratorijska najdba
DA in NE posledi6no ostaneta v sinapsah dlje Casa in okrepita 2iv6ni prenos
neieleni udnki
glavobol
suha usta
4, tel. tee nespeEnost slabost zaprtie
tahikardija
epileptiEni napadi
faringitis
omotica hipertenziia agitacija
prevedel in priredil: Jan Kejiar, dr. med., specializant psihiatrije pregledala: doc. dr. Brigita Novak Sarotar, dr. med., spec. psih.
eliminacija poteka preko jeter in ledvic
prilagoditev odmerka v primeru bolezni jeter in/ali ledvic
bupropion lahko inhibira jetrni citokrom P4502D6 in povzrod interakcije med zdravili
kontraindiciran pri boleznih, ki zmanIgajo epileptogeni prag: anoreksija/bulimija nervoza, epilepsija, odtegnitev alkohola, odtegnitev benzodiazepinov
zaplet Objavljeno 30. junija 2017 na www.thecalgaryguide.com.
" title="Bupropion (atipiEni antidepresiv): Mehanizem delovanja in neieleni utinki
potenten antidepresiv v monoterapiji all kot dodatno zdravilo pri zdravljenju razpoloienjskih motenj
okrajgave: 5-HT - serotonin DA - dopamin DAT - prenagalec DA NA - noradrenalin NAT - prenagalec NA SSRI - selektivni zaviralec ponovnega privzema 5-HT
Legenda:
bupropion
farmakologija
antidepresivni udnki uporaben pri zdravljenju "zmaniganega pozitivnega afekta"
nima pomembnelgih 5-HT udnkov povzraa spolne disfunkcije v primerjavi s SSRI; lahko celo odpravi omenjeni neieleni udnek (povzraen s strani SSRI)
dodatek pri zdravljenju odvisnosti od nikotina preko T iive'nega prenosa DA v nagrajevalni poti
energije preko T 2ivbega prenosa NA
patofiziologija mehanizem
farmakokinetika
farmakodinamika
avtorica: JoAnna Fay, Sara Meunier pregledala: Jojo Jiang, Alexander Arnold, Aaron Mackie*
* dr. med. ob objavi
Nizkoafiniteten zaviralec ponovnega privzema DA in NA (DAT>NAT), ki proizvaja aktivne metabolite. Natan'6en mehanizem delovanja (se) ni znan.
znak/simptom/laboratorijska najdba
DA in NE posledi6no ostaneta v sinapsah dlje Casa in okrepita 2iv6ni prenos
neieleni udnki
glavobol
suha usta
4, tel. tee nespeEnost slabost zaprtie
tahikardija
epileptiEni napadi
faringitis
omotica hipertenziia agitacija
prevedel in priredil: Jan Kejiar, dr. med., specializant psihiatrije pregledala: doc. dr. Brigita Novak Sarotar, dr. med., spec. psih.
eliminacija poteka preko jeter in ledvic
prilagoditev odmerka v primeru bolezni jeter in/ali ledvic
bupropion lahko inhibira jetrni citokrom P4502D6 in povzrod interakcije med zdravili
kontraindiciran pri boleznih, ki zmanIgajo epileptogeni prag: anoreksija/bulimija nervoza, epilepsija, odtegnitev alkohola, odtegnitev benzodiazepinov
zaplet Objavljeno 30. junija 2017 na www.thecalgaryguide.com.
" />
NAT), ki proizvaja aktivne metabolite. Natan'6en mehanizem delovanja (se) ni znan.
znak/simptom/laboratorijska najdba
DA in NE posledi6no ostaneta v sinapsah dlje Casa in okrepita 2iv6ni prenos
neieleni udnki
glavobol
suha usta
4, tel. tee nespeEnost slabost zaprtie
tahikardija
epileptiEni napadi
faringitis
omotica hipertenziia agitacija
prevedel in priredil: Jan Kejiar, dr. med., specializant psihiatrije pregledala: doc. dr. Brigita Novak Sarotar, dr. med., spec. psih.
eliminacija poteka preko jeter in ledvic
prilagoditev odmerka v primeru bolezni jeter in/ali ledvic
bupropion lahko inhibira jetrni citokrom P4502D6 in povzrod interakcije med zdravili
kontraindiciran pri boleznih, ki zmanIgajo epileptogeni prag: anoreksija/bulimija nervoza, epilepsija, odtegnitev alkohola, odtegnitev benzodiazepinov
zaplet Objavljeno 30. junija 2017 na www.thecalgaryguide.com.
" title="Bupropion (atipiEni antidepresiv): Mehanizem delovanja in neieleni utinki
potenten antidepresiv v monoterapiji all kot dodatno zdravilo pri zdravljenju razpoloienjskih motenj
okrajgave: 5-HT - serotonin DA - dopamin DAT - prenagalec DA NA - noradrenalin NAT - prenagalec NA SSRI - selektivni zaviralec ponovnega privzema 5-HT
Legenda:
bupropion
farmakologija
antidepresivni udnki uporaben pri zdravljenju "zmaniganega pozitivnega afekta"
nima pomembnelgih 5-HT udnkov povzraa spolne disfunkcije v primerjavi s SSRI; lahko celo odpravi omenjeni neieleni udnek (povzraen s strani SSRI)
dodatek pri zdravljenju odvisnosti od nikotina preko T iive'nega prenosa DA v nagrajevalni poti
energije preko T 2ivbega prenosa NA
patofiziologija mehanizem
farmakokinetika
farmakodinamika
avtorica: JoAnna Fay, Sara Meunier pregledala: Jojo Jiang, Alexander Arnold, Aaron Mackie*
* dr. med. ob objavi
Nizkoafiniteten zaviralec ponovnega privzema DA in NA (DAT>NAT), ki proizvaja aktivne metabolite. Natan'6en mehanizem delovanja (se) ni znan.
znak/simptom/laboratorijska najdba
DA in NE posledi6no ostaneta v sinapsah dlje Casa in okrepita 2iv6ni prenos
neieleni udnki
glavobol
suha usta
4, tel. tee nespeEnost slabost zaprtie
tahikardija
epileptiEni napadi
faringitis
omotica hipertenziia agitacija
prevedel in priredil: Jan Kejiar, dr. med., specializant psihiatrije pregledala: doc. dr. Brigita Novak Sarotar, dr. med., spec. psih.
eliminacija poteka preko jeter in ledvic
prilagoditev odmerka v primeru bolezni jeter in/ali ledvic
bupropion lahko inhibira jetrni citokrom P4502D6 in povzrod interakcije med zdravili
kontraindiciran pri boleznih, ki zmanIgajo epileptogeni prag: anoreksija/bulimija nervoza, epilepsija, odtegnitev alkohola, odtegnitev benzodiazepinov
zaplet Objavljeno 30. junija 2017 na www.thecalgaryguide.com.
" />
PTSD (Slovenian translation) - FINAL VERSION
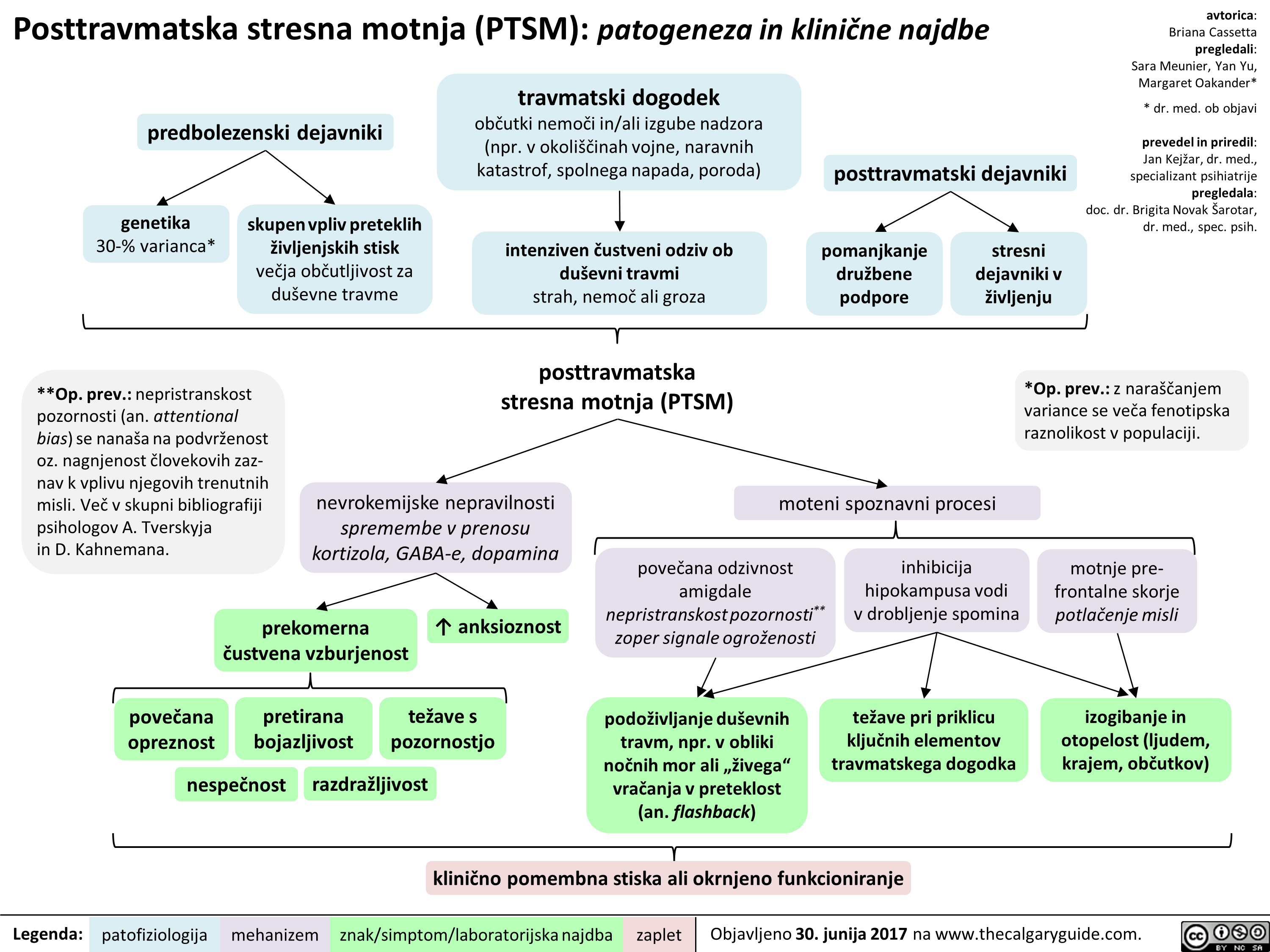
Lipid Physiology Slide
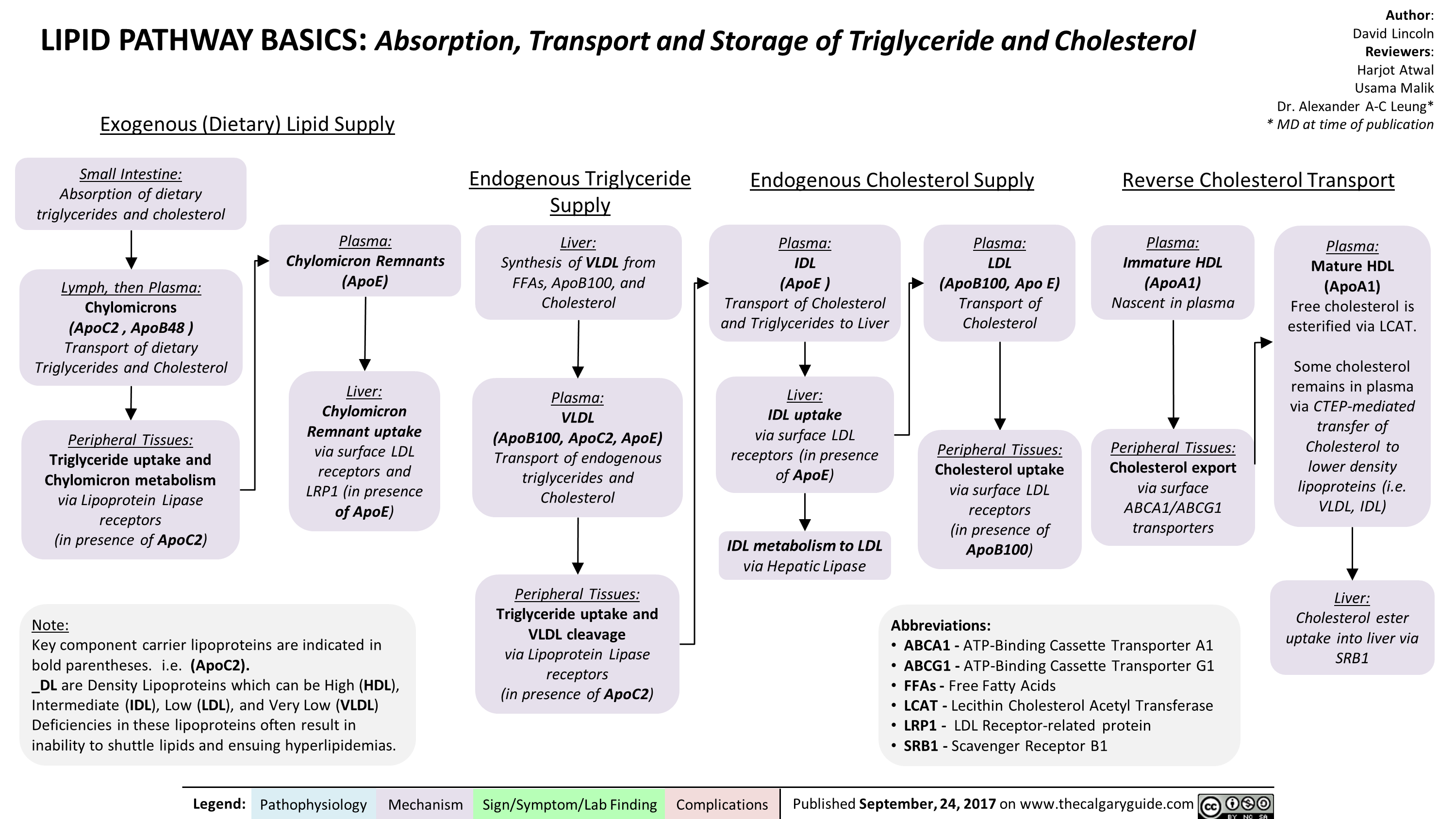
Subtrochanteric Femur Fracture
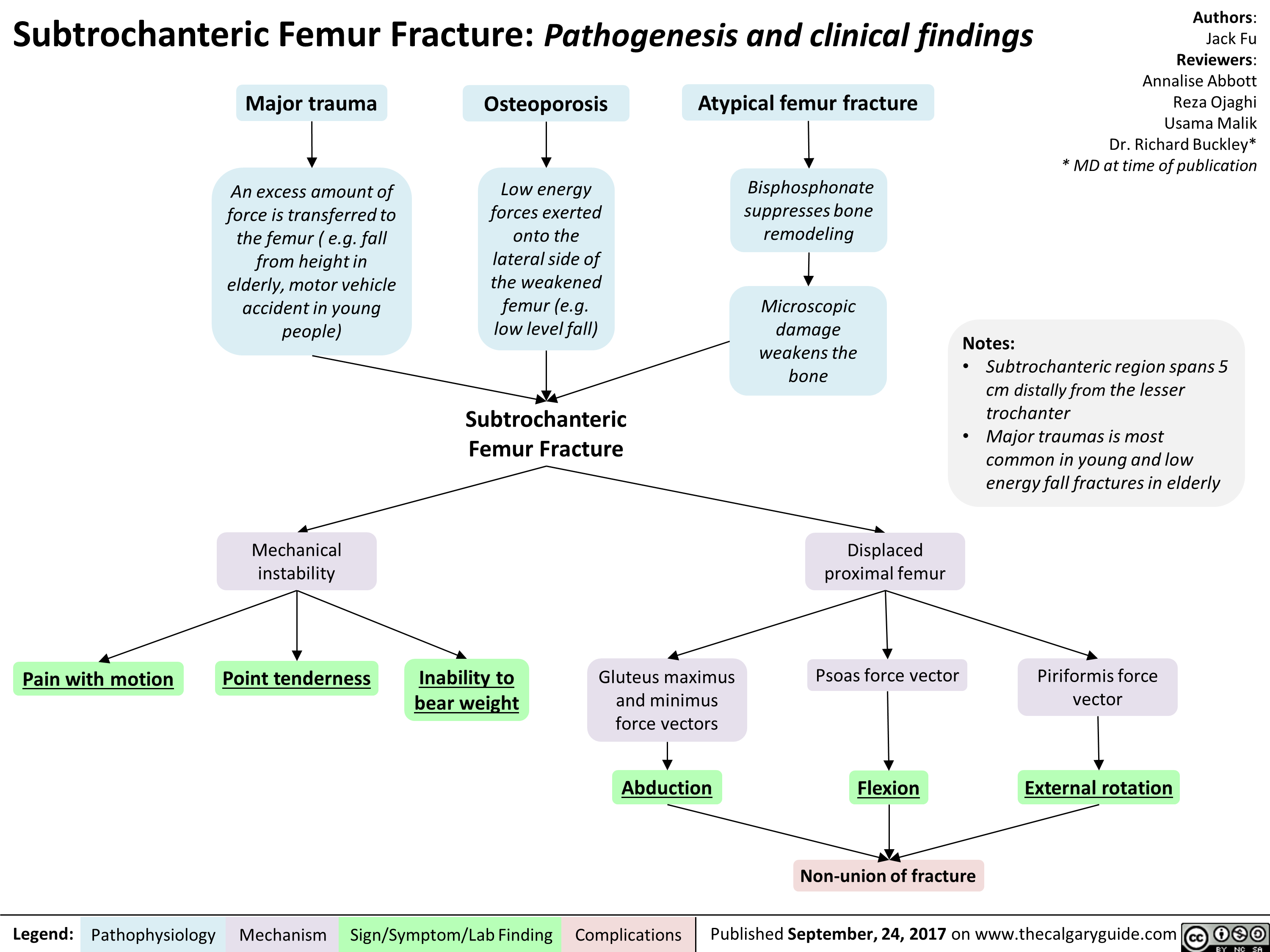
Ovarian Torsion
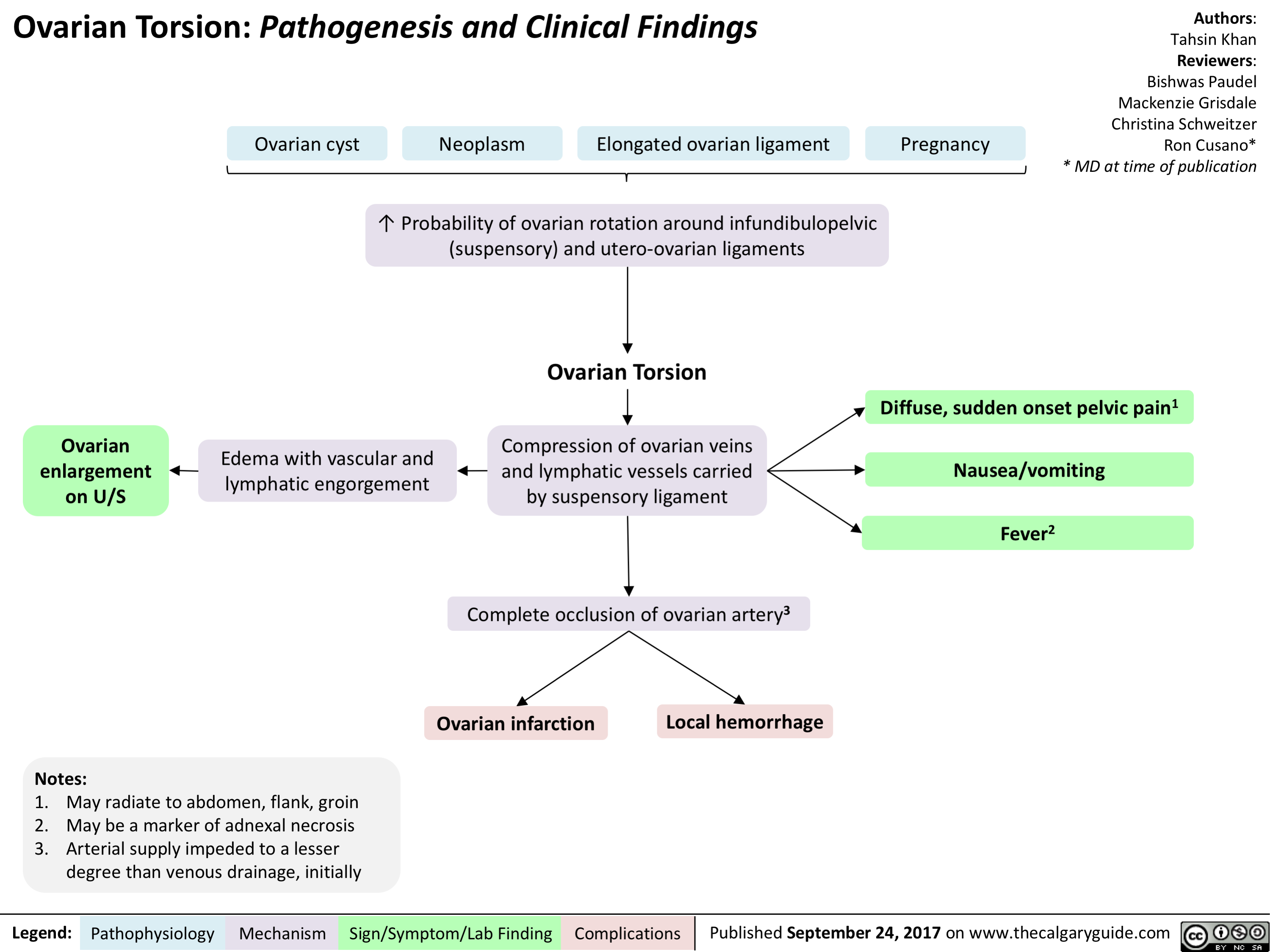
Non-Hodgkin Lymphoma
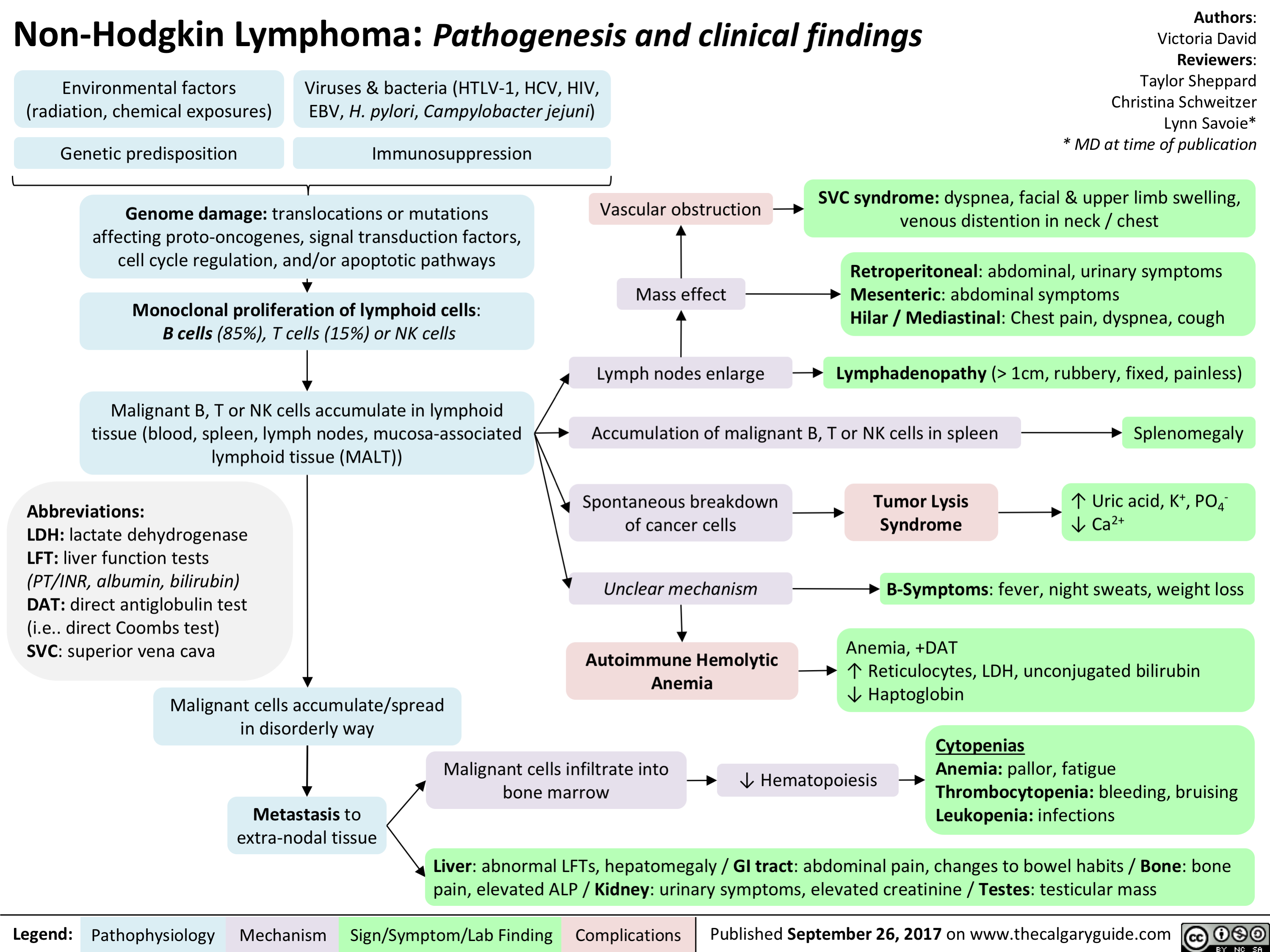
Pelvic Inflammatory Disease
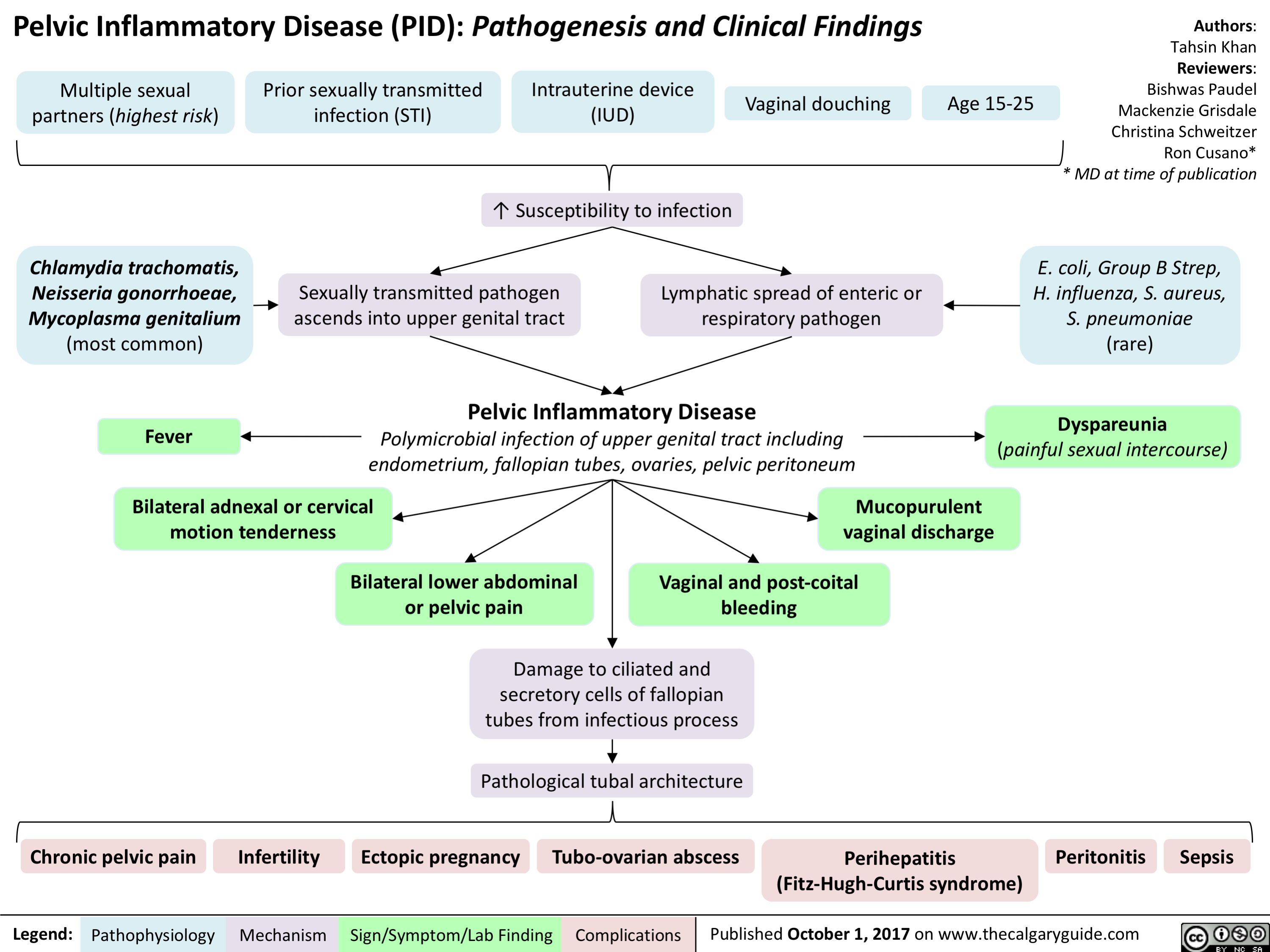
Pituitary Mass Effects
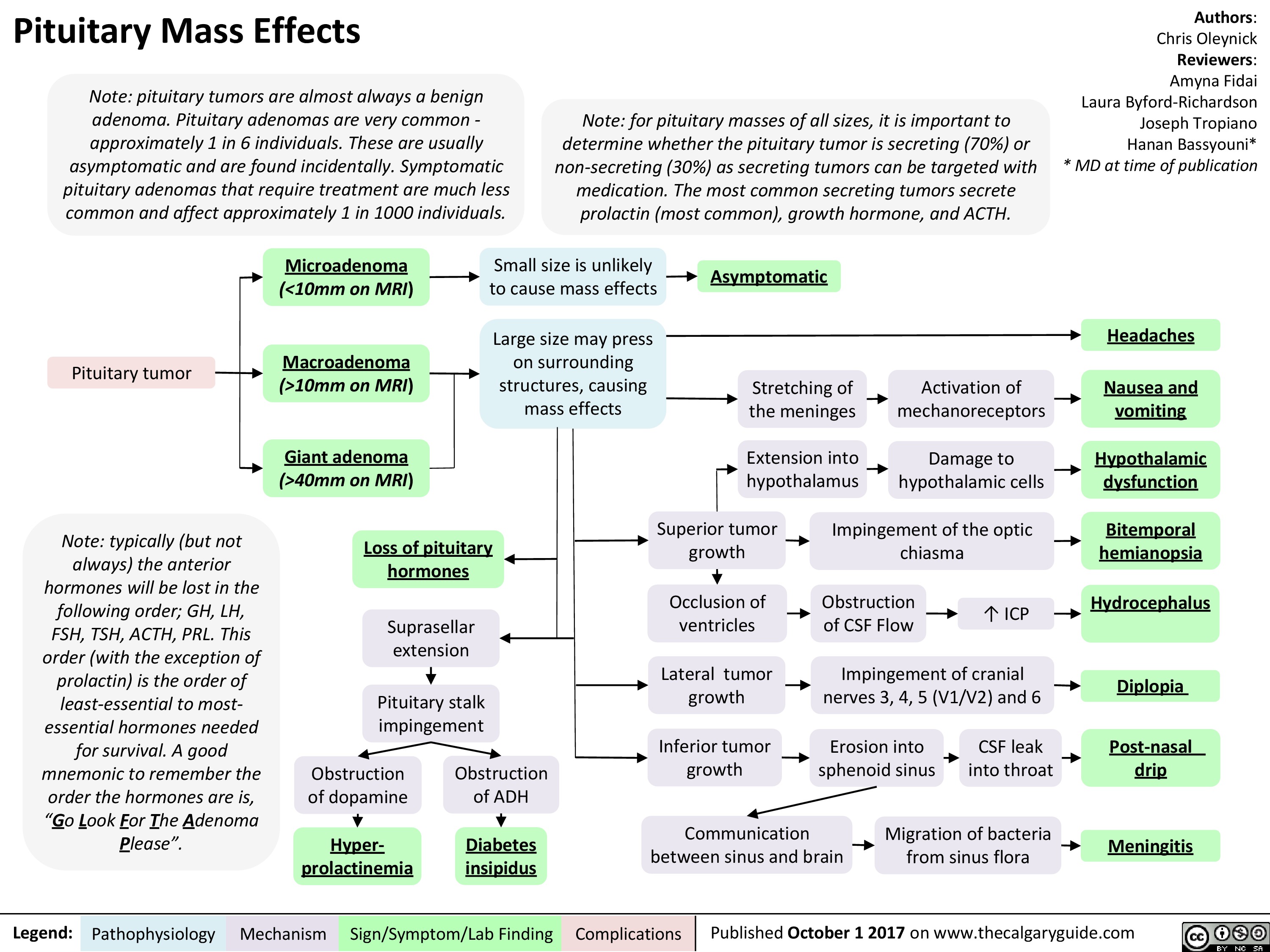 10mm on MRI) vomiting Giant adenoma Extension into hypothalamus —1■• Damage to hypothalamic cells Hypothalamic (>40mm on MRI) dysfunction Obstruction of dopamine Superior tumor growth Impingement of the optic chiasma Bitemporal Loss of pituitary hemianopsia hormones ICP Suprasellar extension Occlusion of ventricles Obstruction of CSF Flow Hydrocephalus Lateral tumor growth Impingement of cranial nerves 3, 4, 5 (V1/V2) and 6 4 Pituitary stalk impingement Diplopia Inferior tumor growth Erosion into sphenoid sinus CSF leak into throat Post-nasal Obstruction of ADH drip Communication between sinus and brain Migration of bacteria from sinus flora Hyper-Diabetes Meningitis prolactinemia insipidus
Pathophysiology Mechanism
Sign/Symptom/Lab Finding
Complications
Published October 1 2017 on www.thecalgaryguide.com
" title="Pituitary Mass Effects
Note: pituitary tumors are almost always a benign adenoma. Pituitary adenomas are very common -approximately 1 in 6 individuals. These are usually asymptomatic and are found incidentally. Symptomatic pituitary adenomas that require treatment are much less common and affect approximately 1 in 1000 individuals.
Pituitary tumor
Note: typically (but not always) the anterior hormones will be lost in the following order; GH, LH, FSH, TSH, ACTH, PRL. This order (with the exception of prolactin) is the order of least-essential to most-essential hormones needed for survival. A good mnemonic to remember the order the hormones are is, "Go Look For The Adenoma Please".
Legend:
Note: for pituitary masses of all sizes, it is important to determine whether the pituitary tumor is secreting (70%) or non-secreting (30%) as secreting tumors can be targeted with medication. The most common secreting tumors secrete prolactin (most common), growth hormone, and ACTH.
Authors: Chris Oleynick Reviewers: Amyna Fidai Laura Byford-Richardson Joseph Tropiano Hanan Bassyouni* * MD at time of publication
Microadenoma Small size is unlikely to cause mass effects (<10mm on MRI) Asymptomatic Macroadenoma Large size may press on surrounding structures, causing mass effects Headaches Stretching of the meninges Activation of mechanoreceptors Nausea and (>10mm on MRI) vomiting Giant adenoma Extension into hypothalamus —1■• Damage to hypothalamic cells Hypothalamic (>40mm on MRI) dysfunction Obstruction of dopamine Superior tumor growth Impingement of the optic chiasma Bitemporal Loss of pituitary hemianopsia hormones ICP Suprasellar extension Occlusion of ventricles Obstruction of CSF Flow Hydrocephalus Lateral tumor growth Impingement of cranial nerves 3, 4, 5 (V1/V2) and 6 4 Pituitary stalk impingement Diplopia Inferior tumor growth Erosion into sphenoid sinus CSF leak into throat Post-nasal Obstruction of ADH drip Communication between sinus and brain Migration of bacteria from sinus flora Hyper-Diabetes Meningitis prolactinemia insipidus
Pathophysiology Mechanism
Sign/Symptom/Lab Finding
Complications
Published October 1 2017 on www.thecalgaryguide.com
" />
10mm on MRI) vomiting Giant adenoma Extension into hypothalamus —1■• Damage to hypothalamic cells Hypothalamic (>40mm on MRI) dysfunction Obstruction of dopamine Superior tumor growth Impingement of the optic chiasma Bitemporal Loss of pituitary hemianopsia hormones ICP Suprasellar extension Occlusion of ventricles Obstruction of CSF Flow Hydrocephalus Lateral tumor growth Impingement of cranial nerves 3, 4, 5 (V1/V2) and 6 4 Pituitary stalk impingement Diplopia Inferior tumor growth Erosion into sphenoid sinus CSF leak into throat Post-nasal Obstruction of ADH drip Communication between sinus and brain Migration of bacteria from sinus flora Hyper-Diabetes Meningitis prolactinemia insipidus
Pathophysiology Mechanism
Sign/Symptom/Lab Finding
Complications
Published October 1 2017 on www.thecalgaryguide.com
" title="Pituitary Mass Effects
Note: pituitary tumors are almost always a benign adenoma. Pituitary adenomas are very common -approximately 1 in 6 individuals. These are usually asymptomatic and are found incidentally. Symptomatic pituitary adenomas that require treatment are much less common and affect approximately 1 in 1000 individuals.
Pituitary tumor
Note: typically (but not always) the anterior hormones will be lost in the following order; GH, LH, FSH, TSH, ACTH, PRL. This order (with the exception of prolactin) is the order of least-essential to most-essential hormones needed for survival. A good mnemonic to remember the order the hormones are is, "Go Look For The Adenoma Please".
Legend:
Note: for pituitary masses of all sizes, it is important to determine whether the pituitary tumor is secreting (70%) or non-secreting (30%) as secreting tumors can be targeted with medication. The most common secreting tumors secrete prolactin (most common), growth hormone, and ACTH.
Authors: Chris Oleynick Reviewers: Amyna Fidai Laura Byford-Richardson Joseph Tropiano Hanan Bassyouni* * MD at time of publication
Microadenoma Small size is unlikely to cause mass effects (<10mm on MRI) Asymptomatic Macroadenoma Large size may press on surrounding structures, causing mass effects Headaches Stretching of the meninges Activation of mechanoreceptors Nausea and (>10mm on MRI) vomiting Giant adenoma Extension into hypothalamus —1■• Damage to hypothalamic cells Hypothalamic (>40mm on MRI) dysfunction Obstruction of dopamine Superior tumor growth Impingement of the optic chiasma Bitemporal Loss of pituitary hemianopsia hormones ICP Suprasellar extension Occlusion of ventricles Obstruction of CSF Flow Hydrocephalus Lateral tumor growth Impingement of cranial nerves 3, 4, 5 (V1/V2) and 6 4 Pituitary stalk impingement Diplopia Inferior tumor growth Erosion into sphenoid sinus CSF leak into throat Post-nasal Obstruction of ADH drip Communication between sinus and brain Migration of bacteria from sinus flora Hyper-Diabetes Meningitis prolactinemia insipidus
Pathophysiology Mechanism
Sign/Symptom/Lab Finding
Complications
Published October 1 2017 on www.thecalgaryguide.com
" />
Acute Chest Syndrome (Sickle Cell Disease)
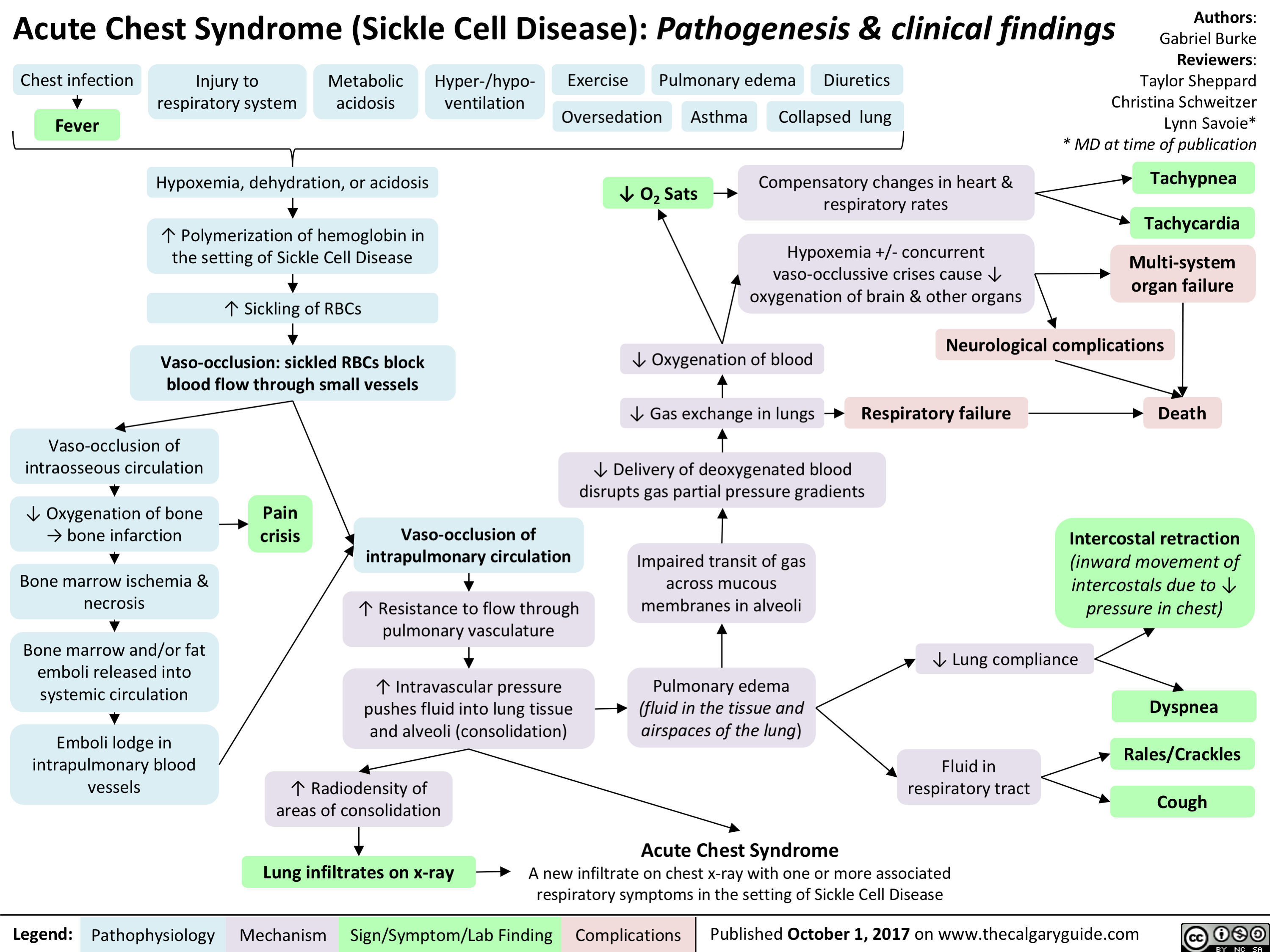
tetanus
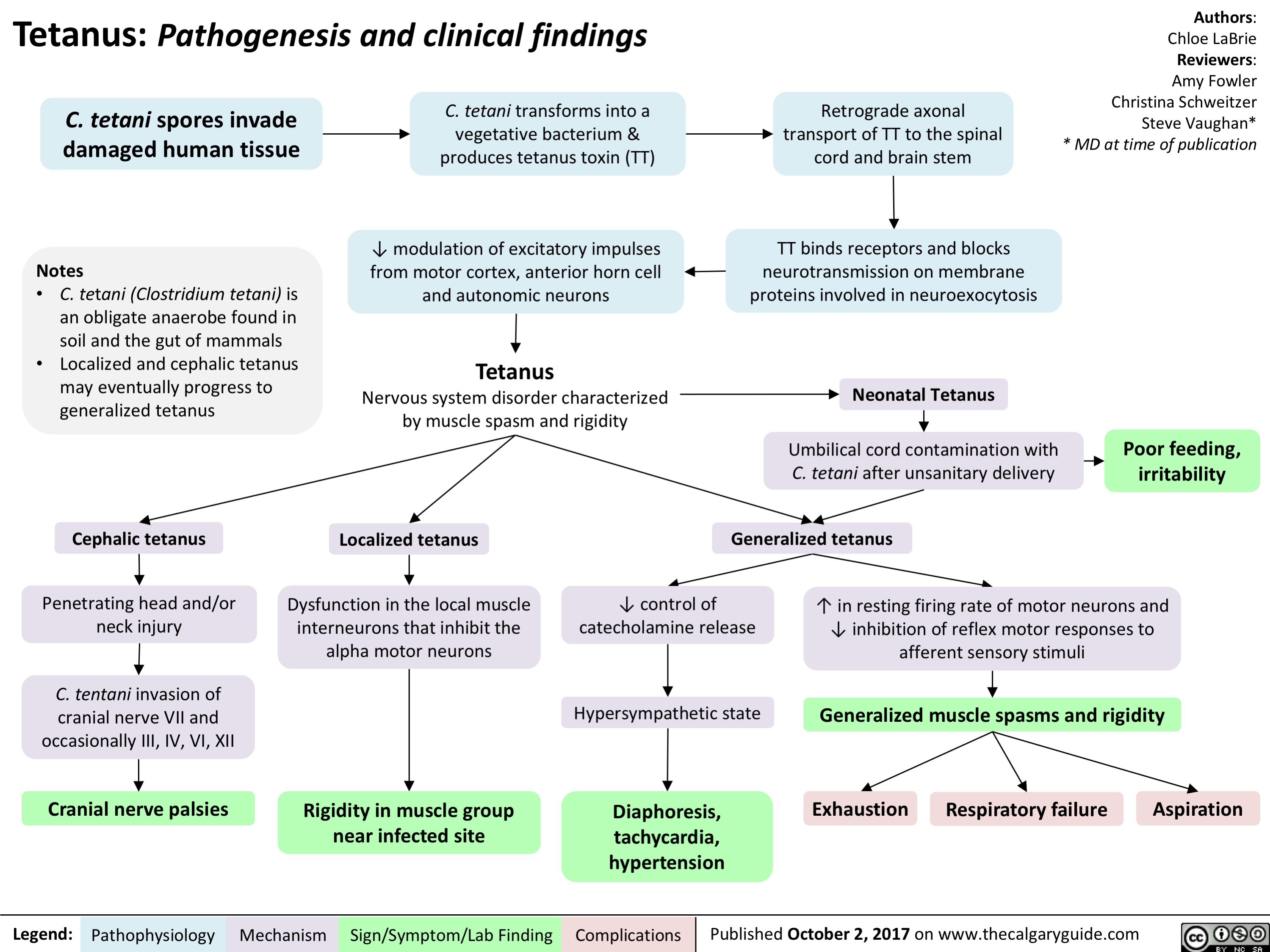
Anaphylaxis - Pathogenesis
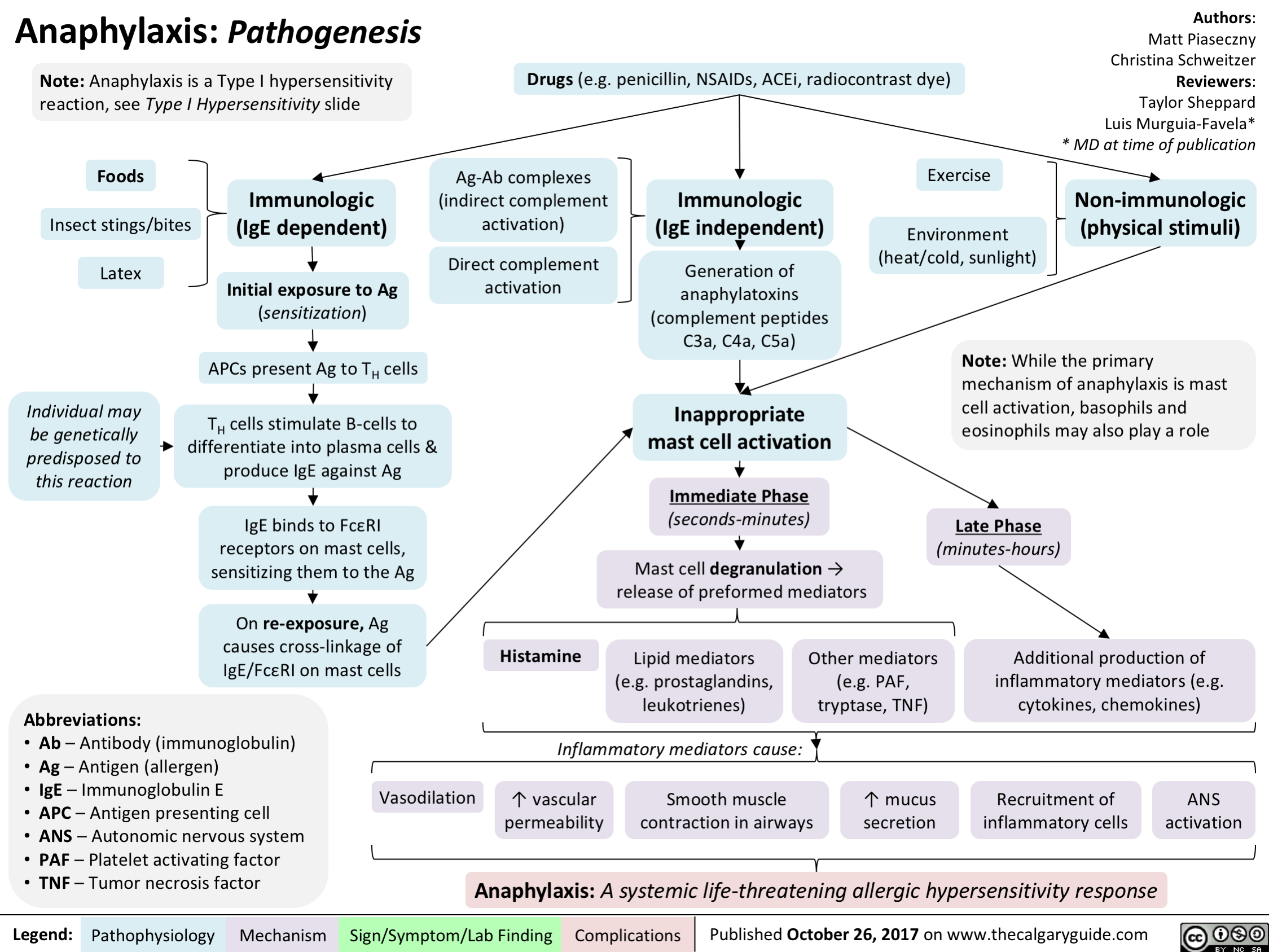
Ischemia: Pathogenesis of Cellular Injury and Death
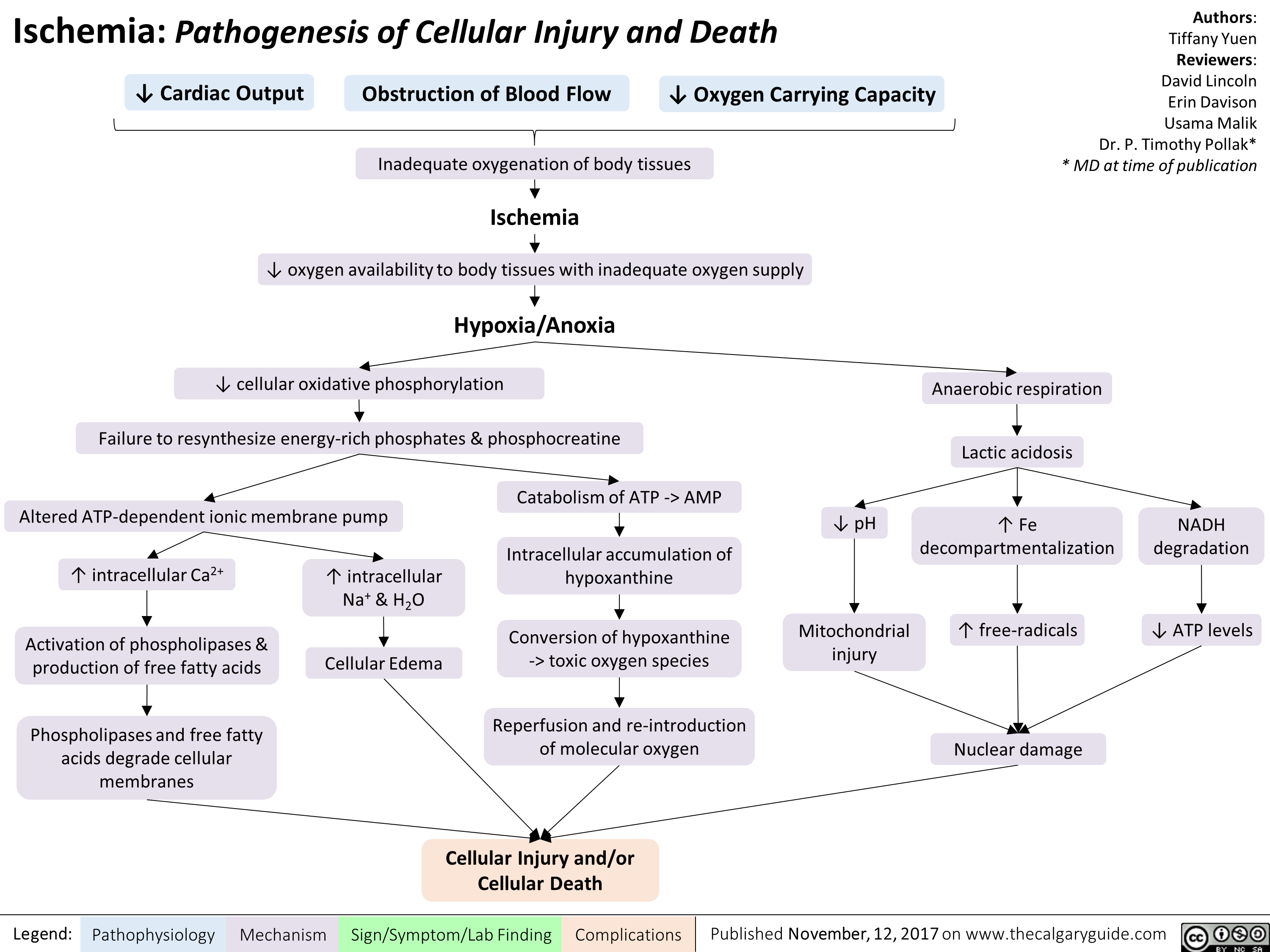
Hepatitis C (HCV) Infections: Explaining Serology Patterns
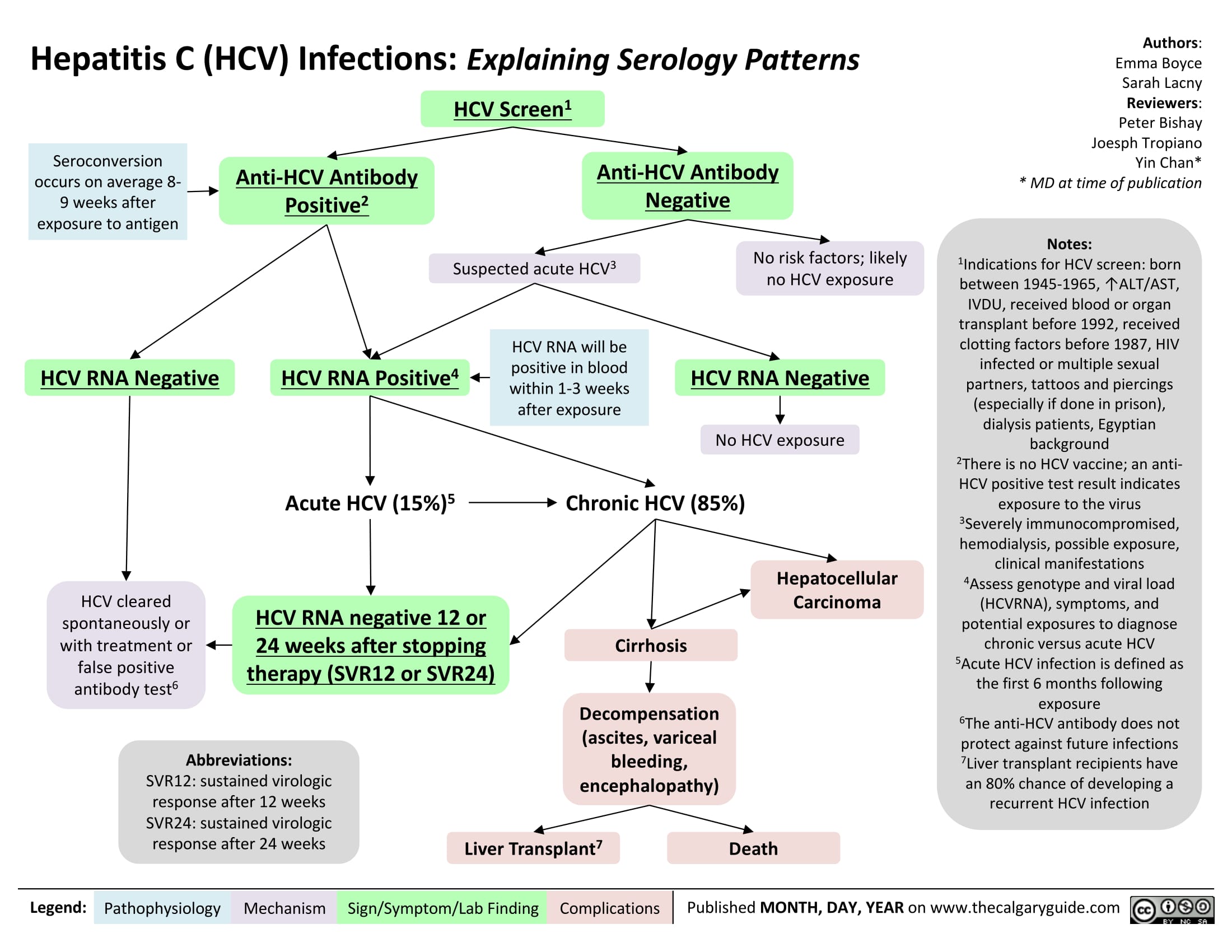
Hepatitis C (HCV) Infection: Explaining Serology Patterns
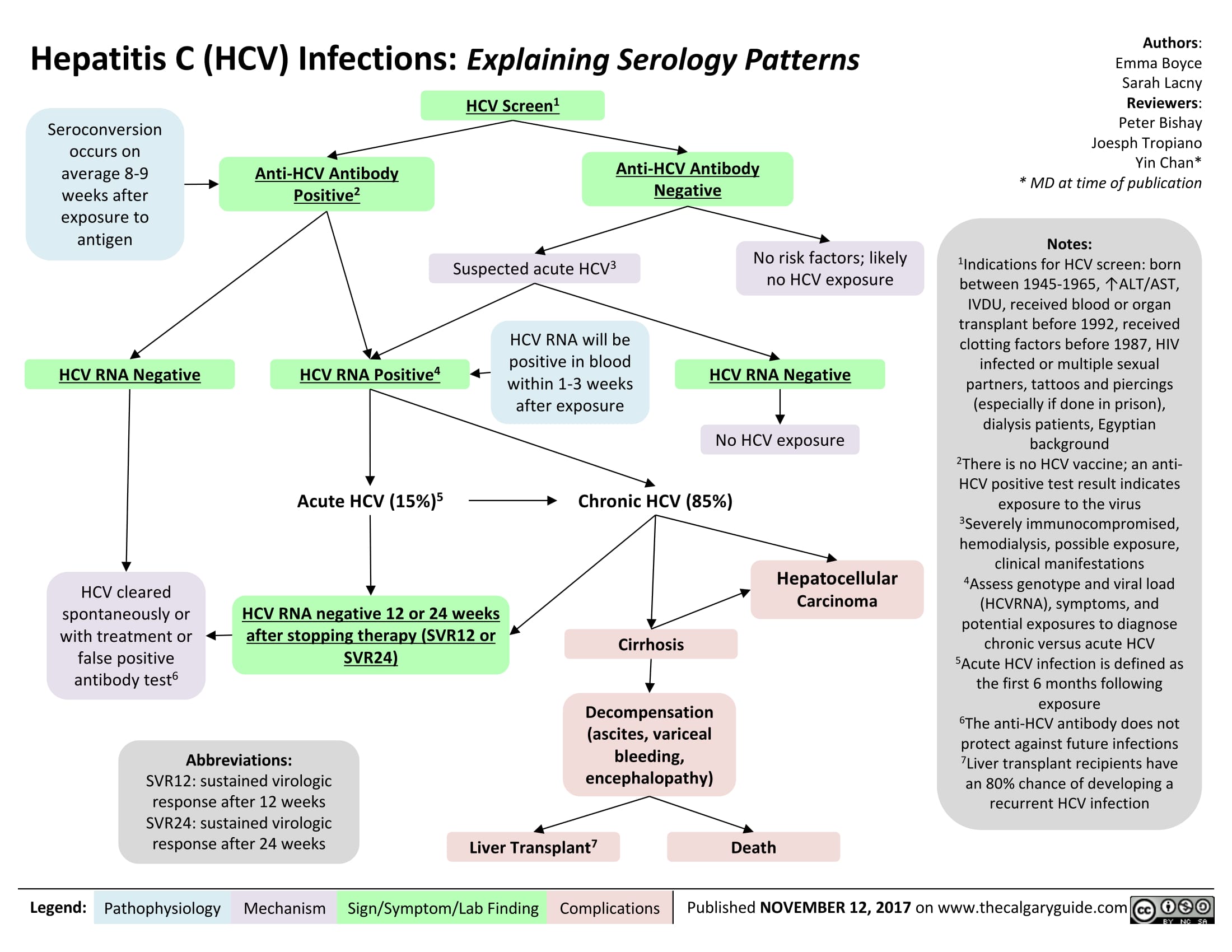
Medical Conditions Causing Mania or Mania-Like Episodes: Pathogenesis
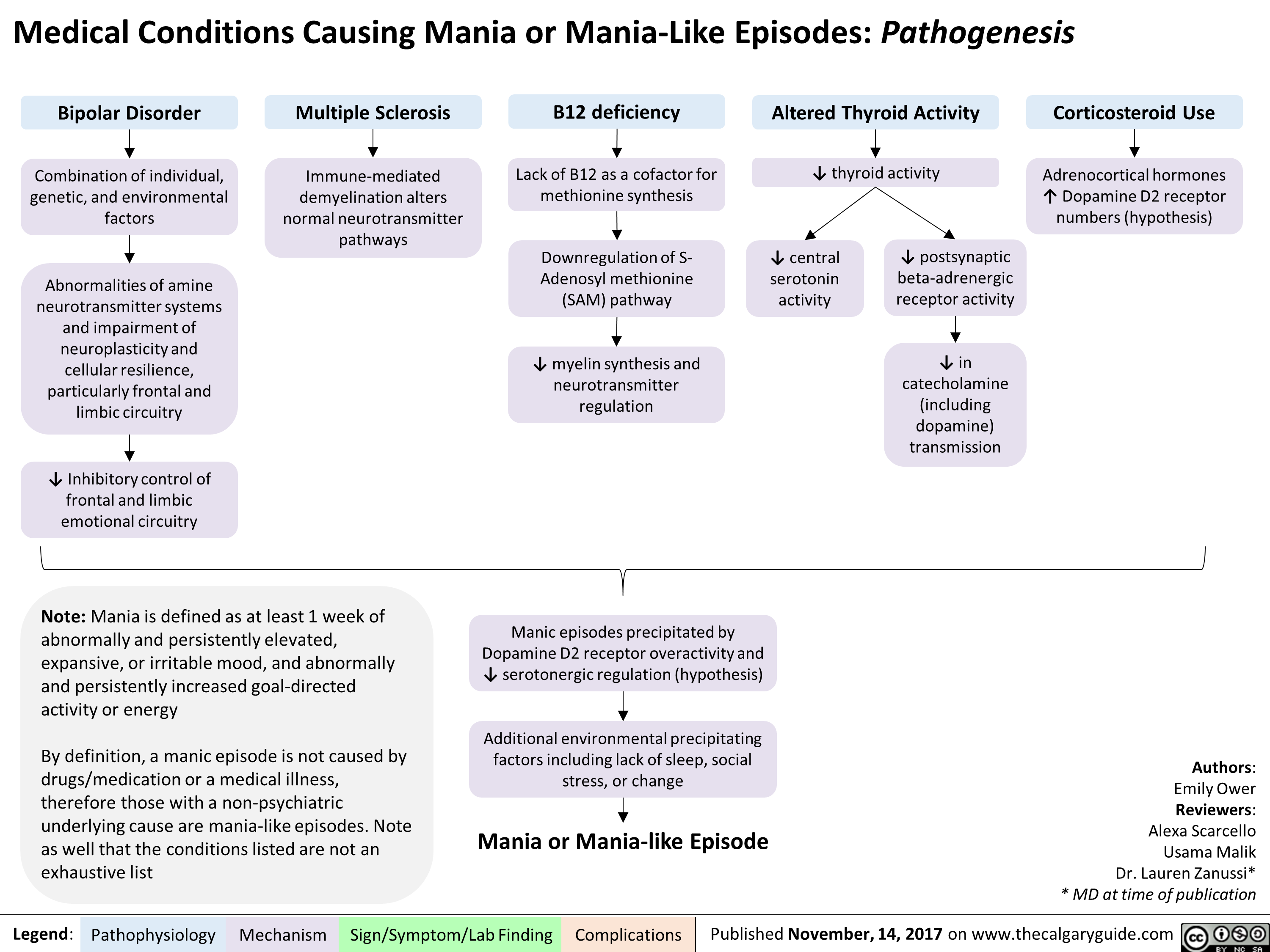
Left Heart Failure: Pathophysiology (Neurohormonal Activation)
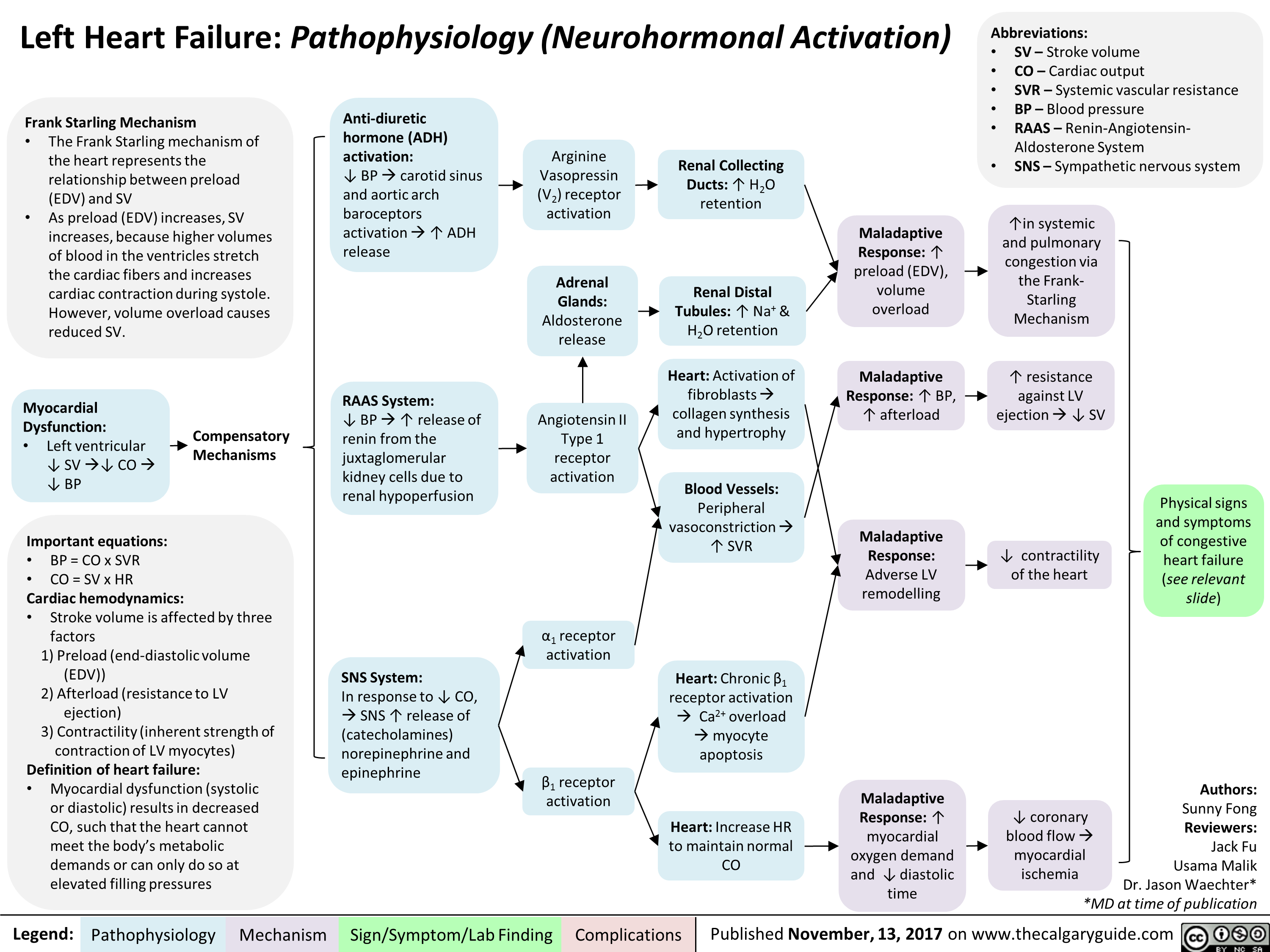
Primary Spontaneous Pneumothorax: Pathogenesis and clinical findings
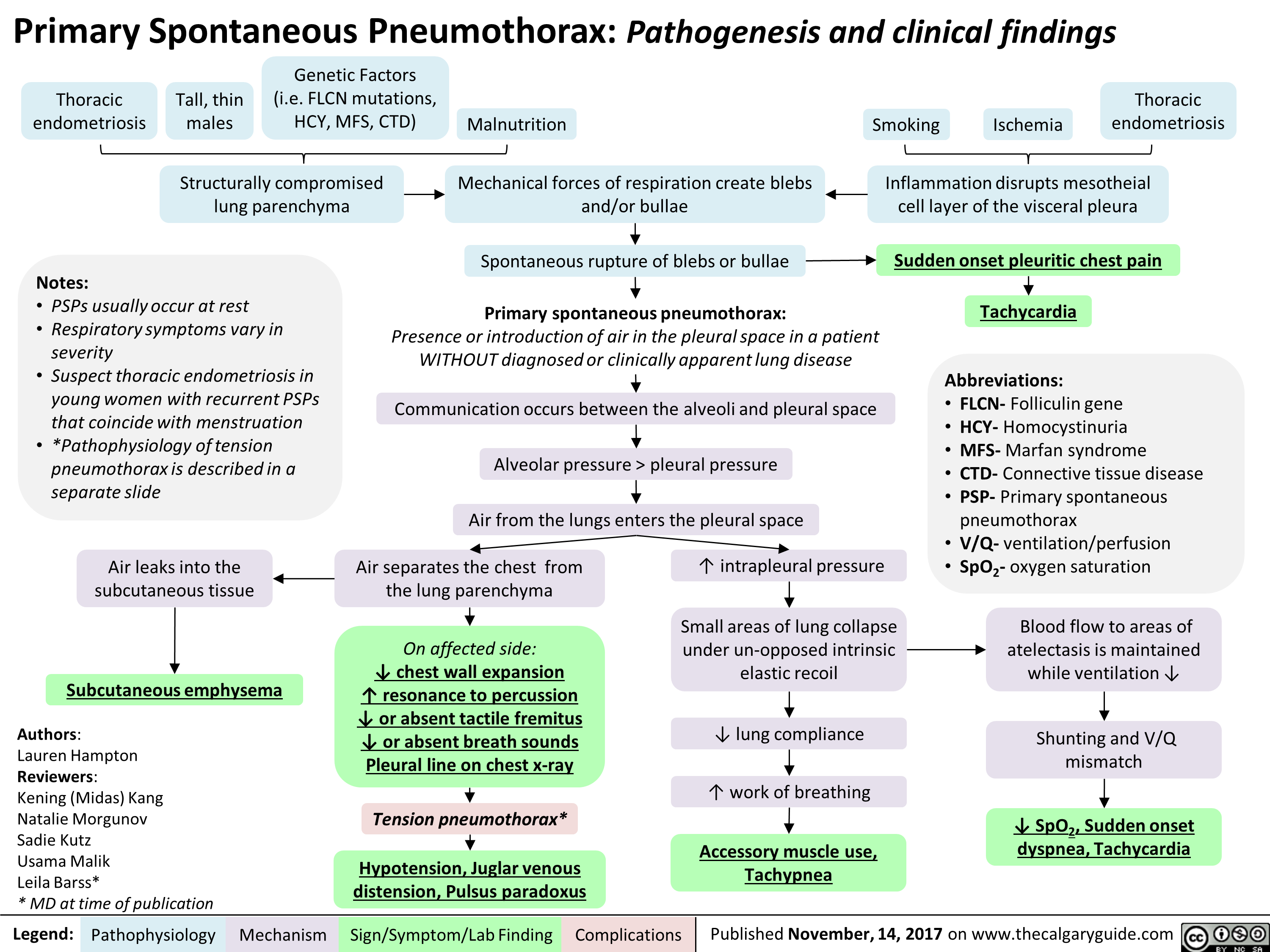
Anksiozne motnje: patogeneza tesnobe
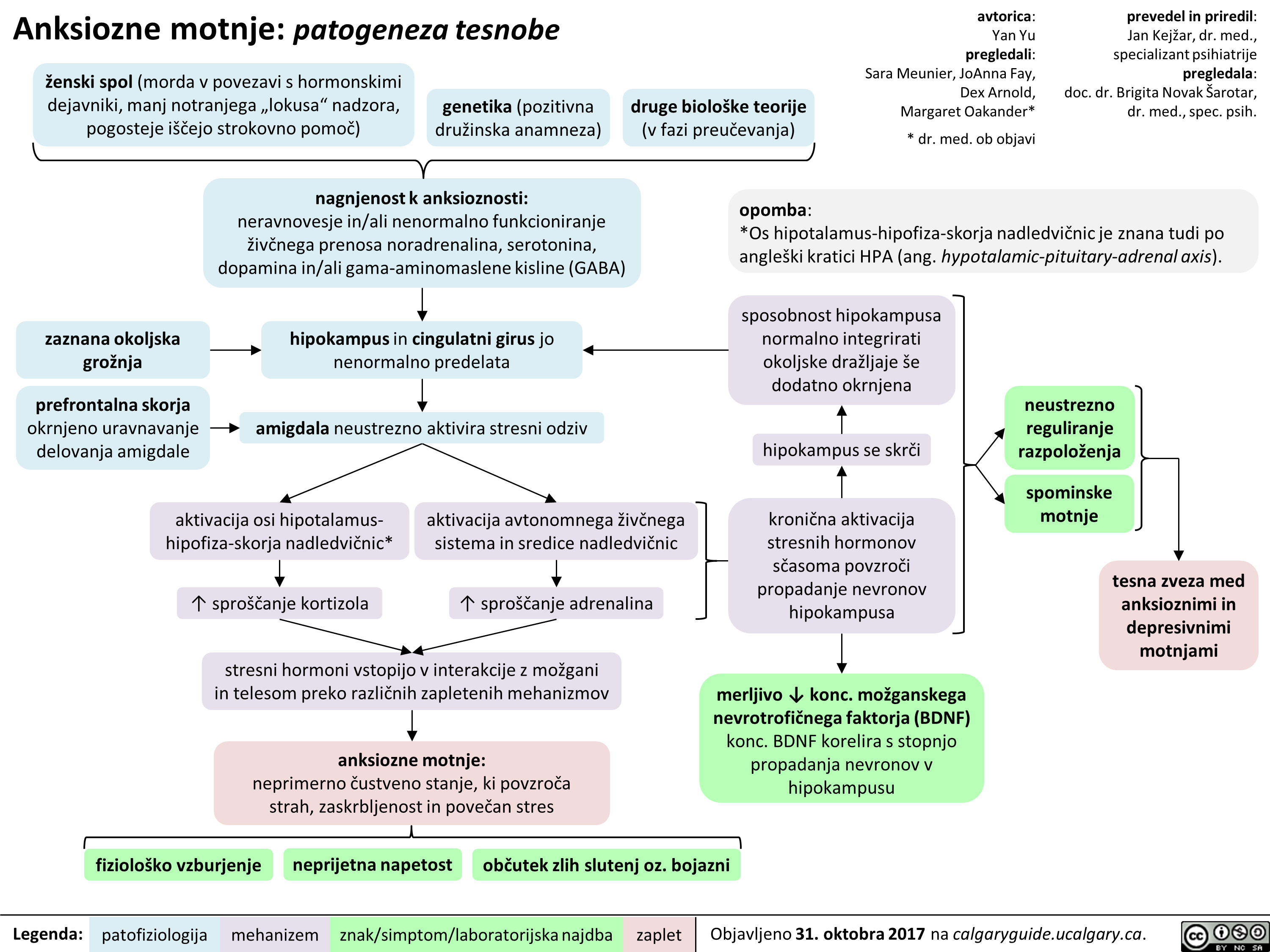
Depresivna epizoda/motnja: patogeneza in klinične najdbe
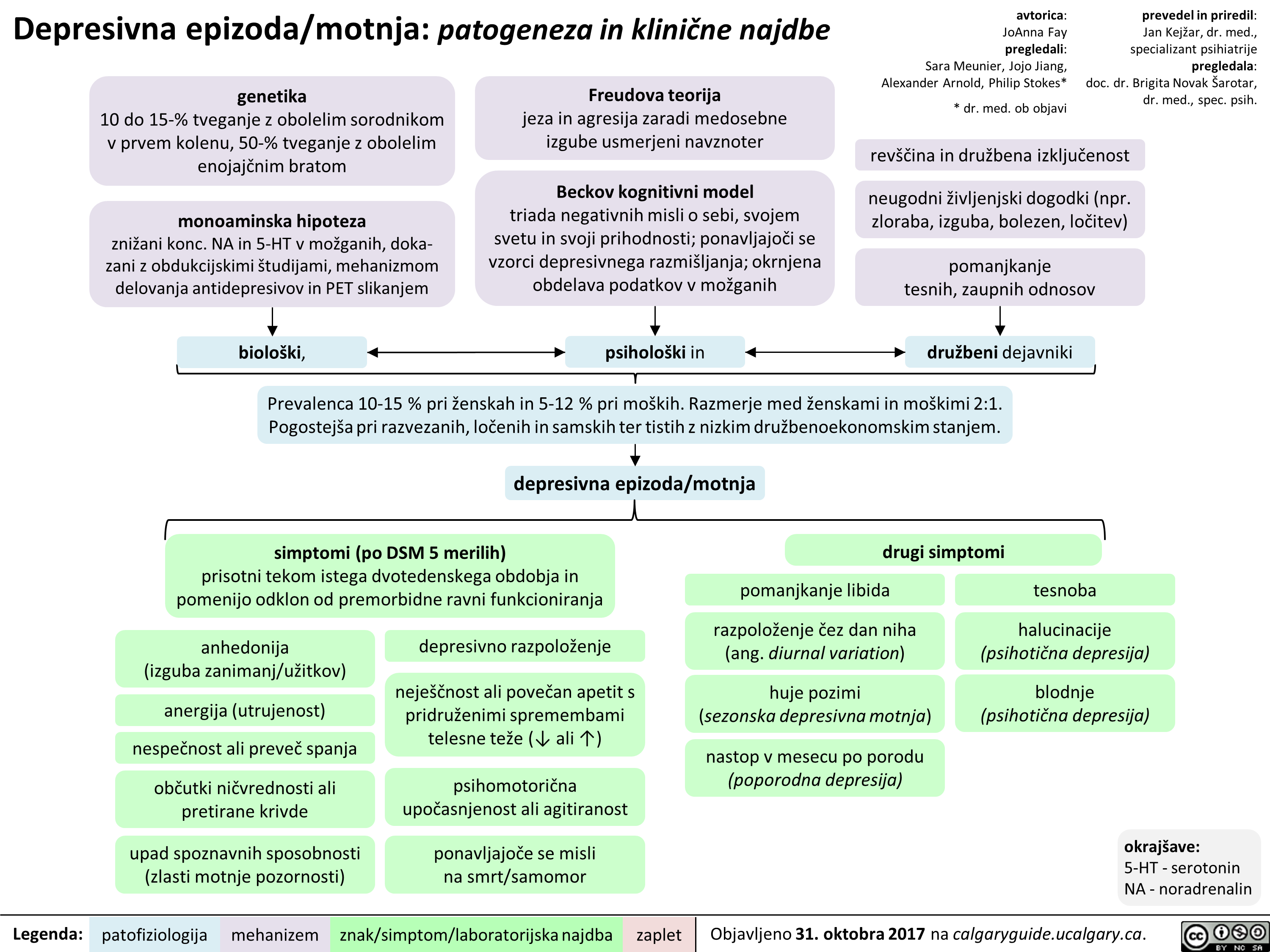
Obsesivno-kompulzivna motnja: patogeneza in klinične najdbe
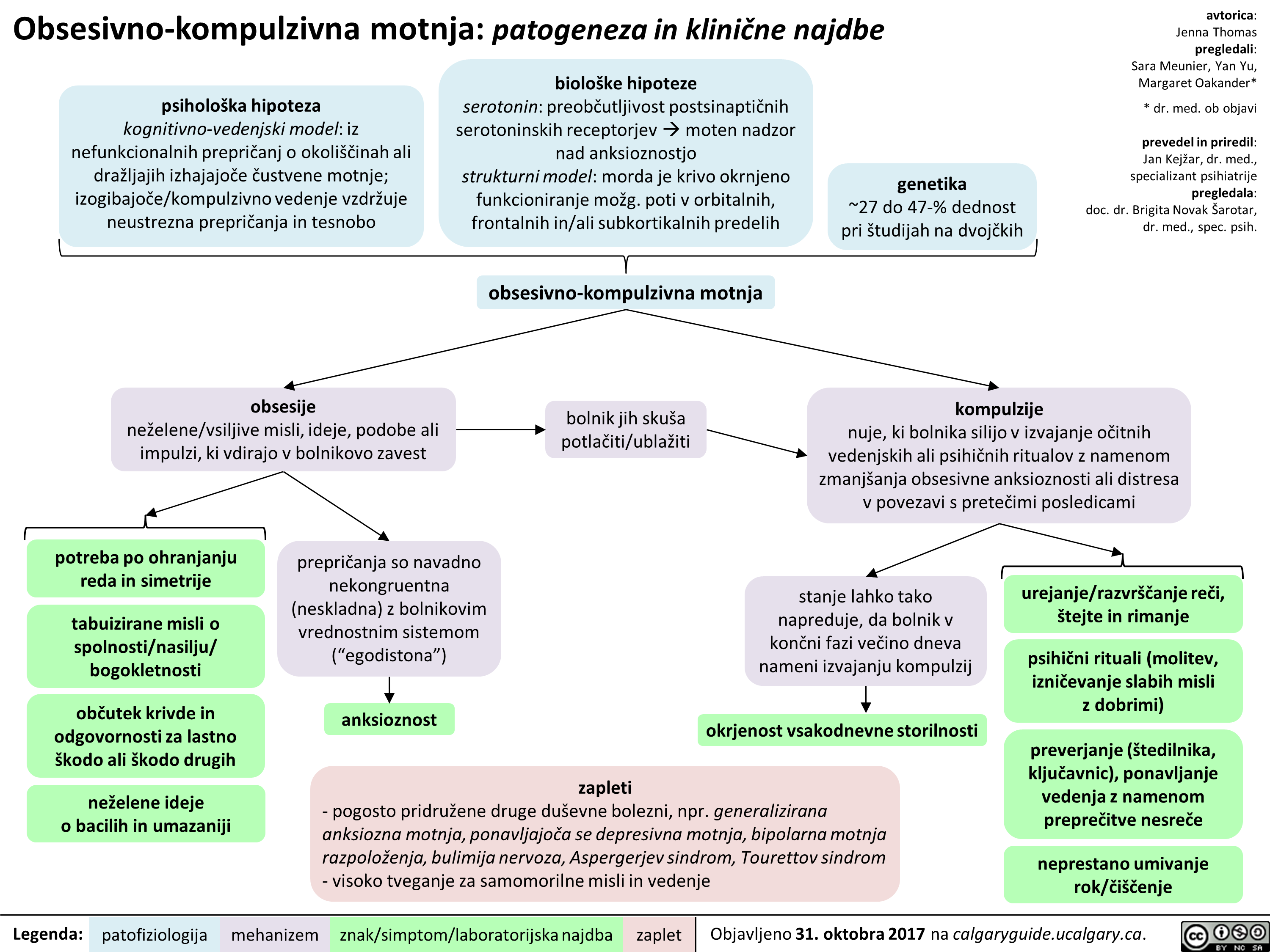
Panična motnja: patogeneza in klinične najdbe
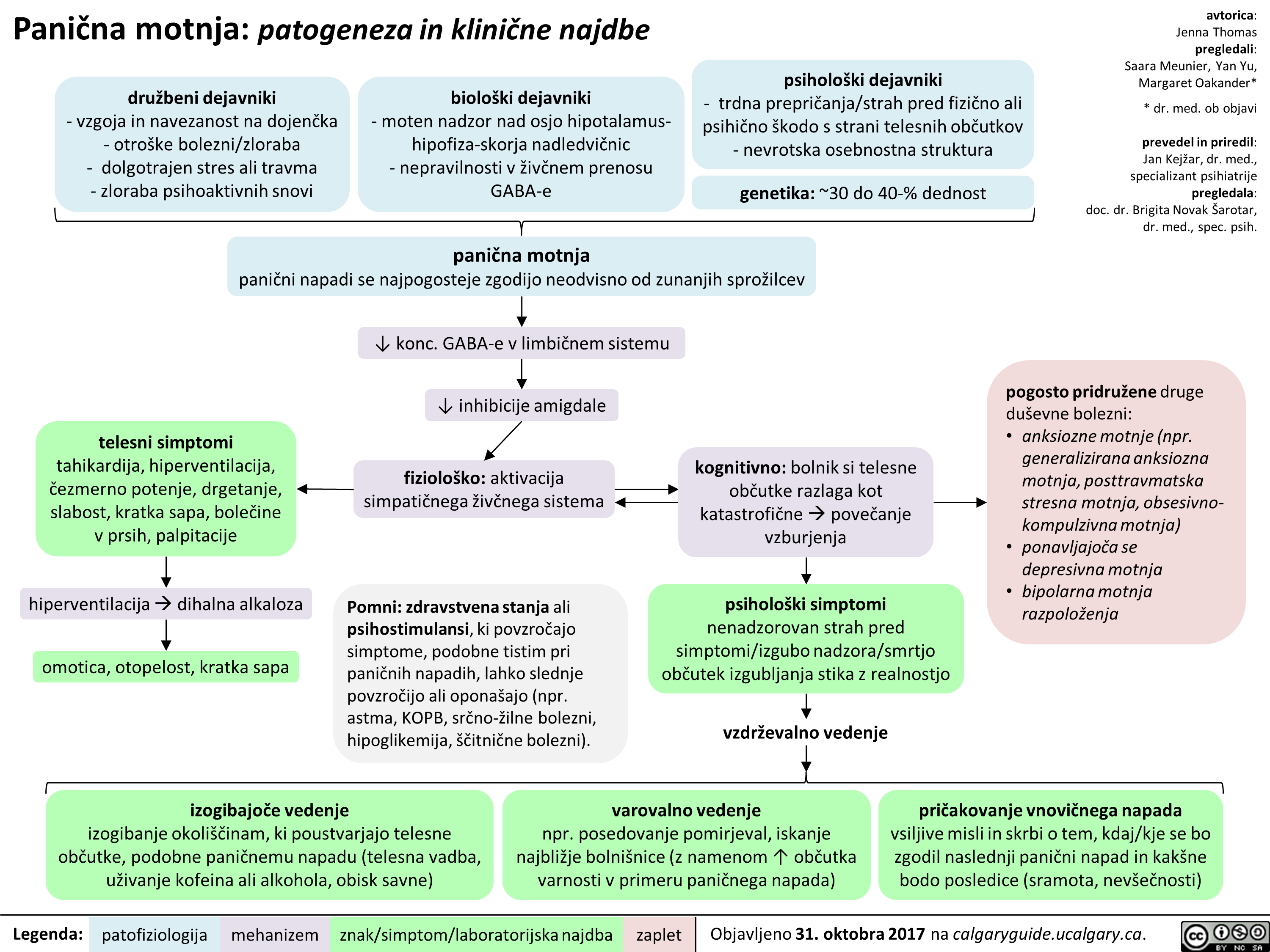
Sezonska depresivna motnja: patogeneza in klinične najdbe
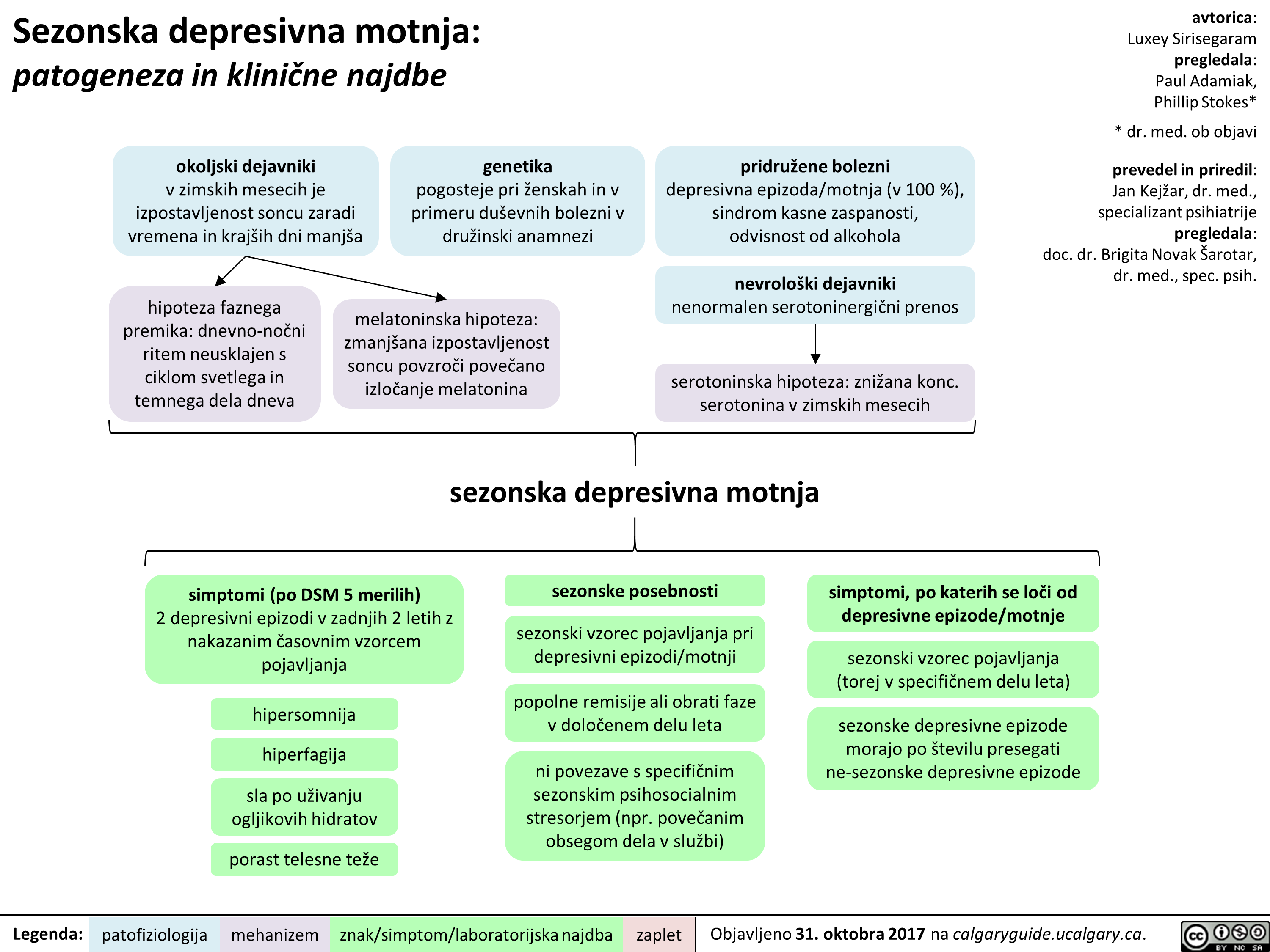
Shizofrenija: patogeneza in klinične najdbe
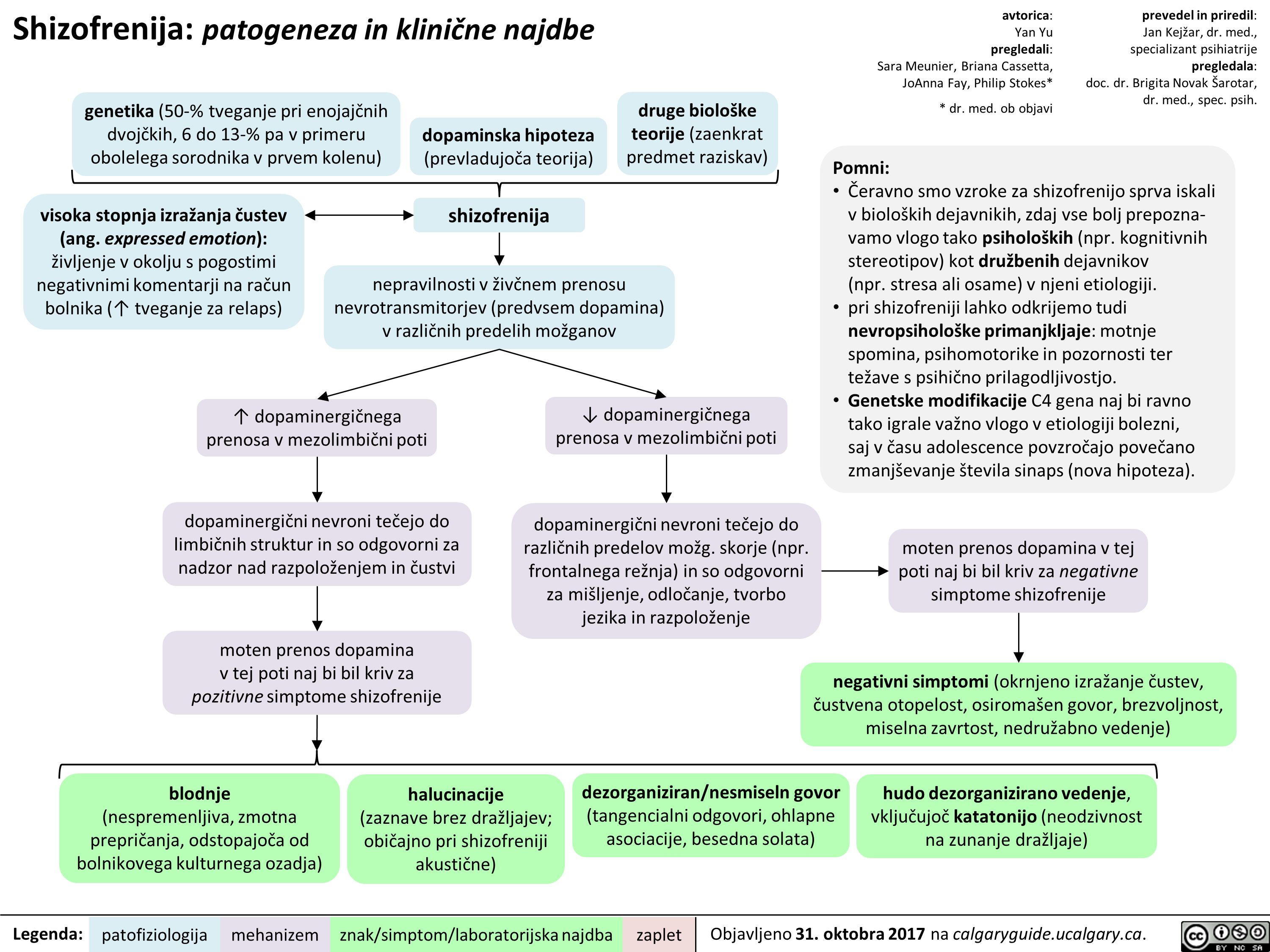
Serotoninski sindrom: patogeneza in klinične najdbe
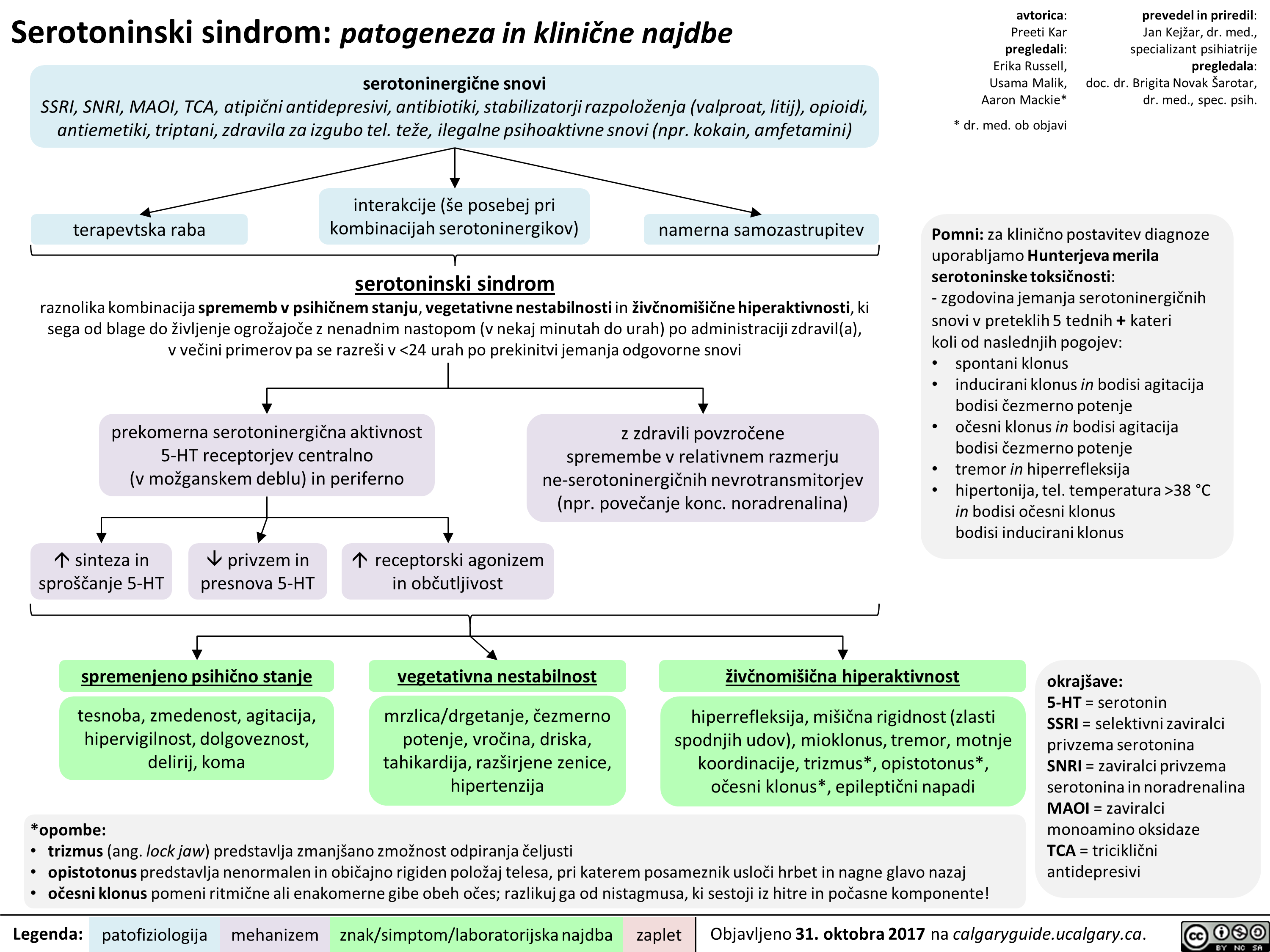
Zaviralci privzema serotonina in noradrenalina (SNRI): mehanizem delovanja in neželeni učinki
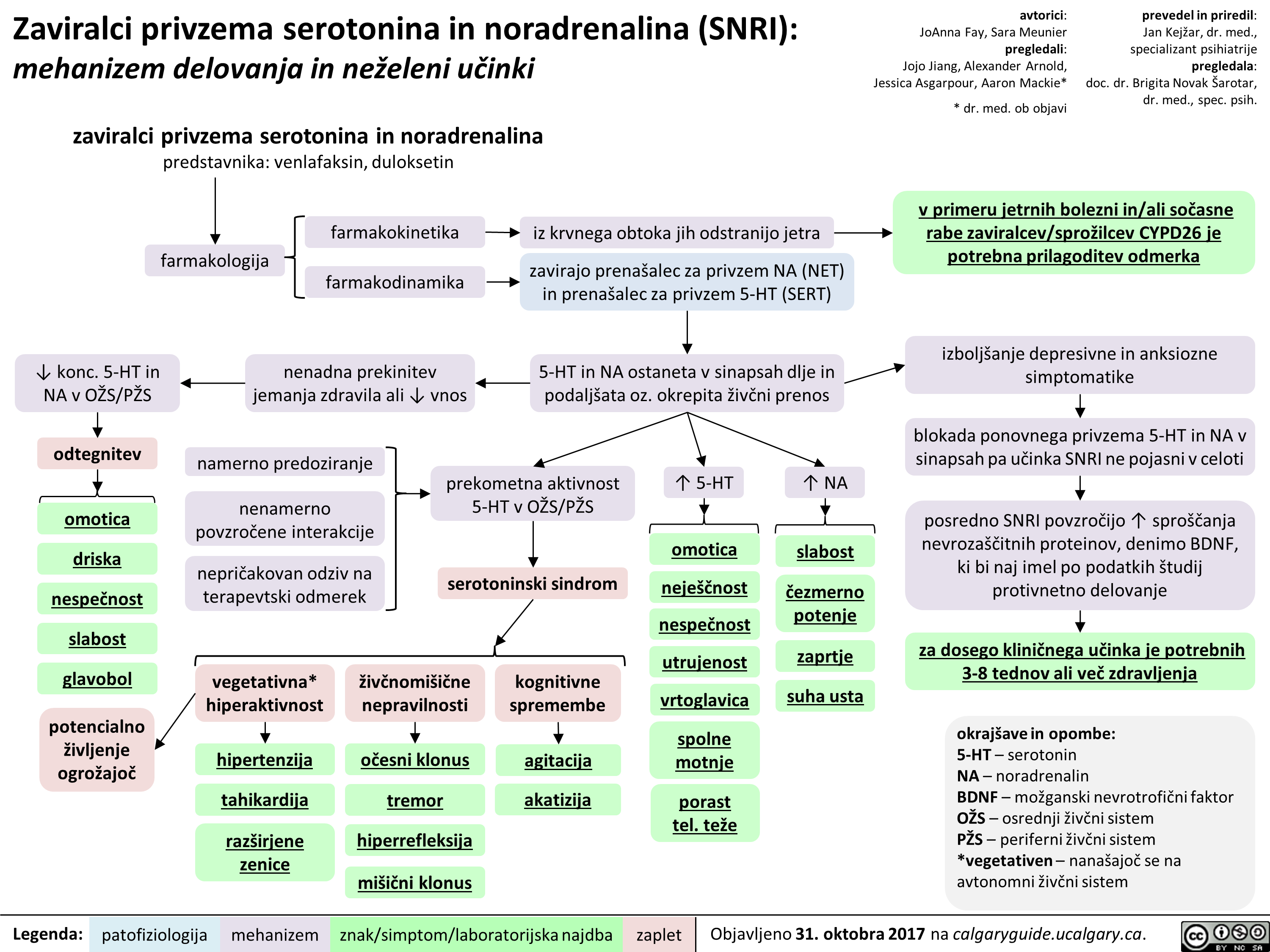
Socialna anksiozna motnja: patogeneza in klinične najdbe
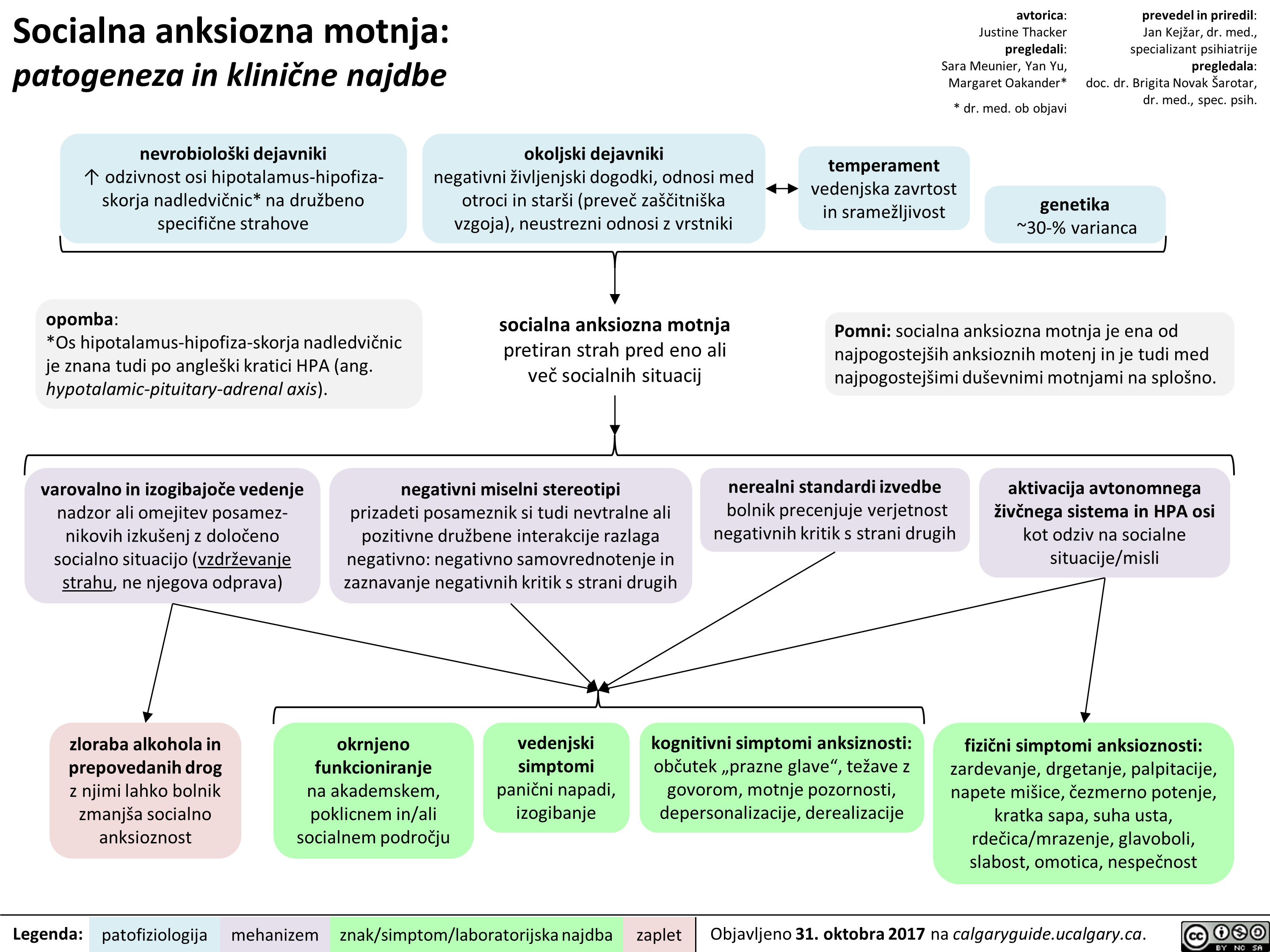
Selektivni zaviralci privzema serotonina (SSRI): mehanizem delovanja in neželeni učinki
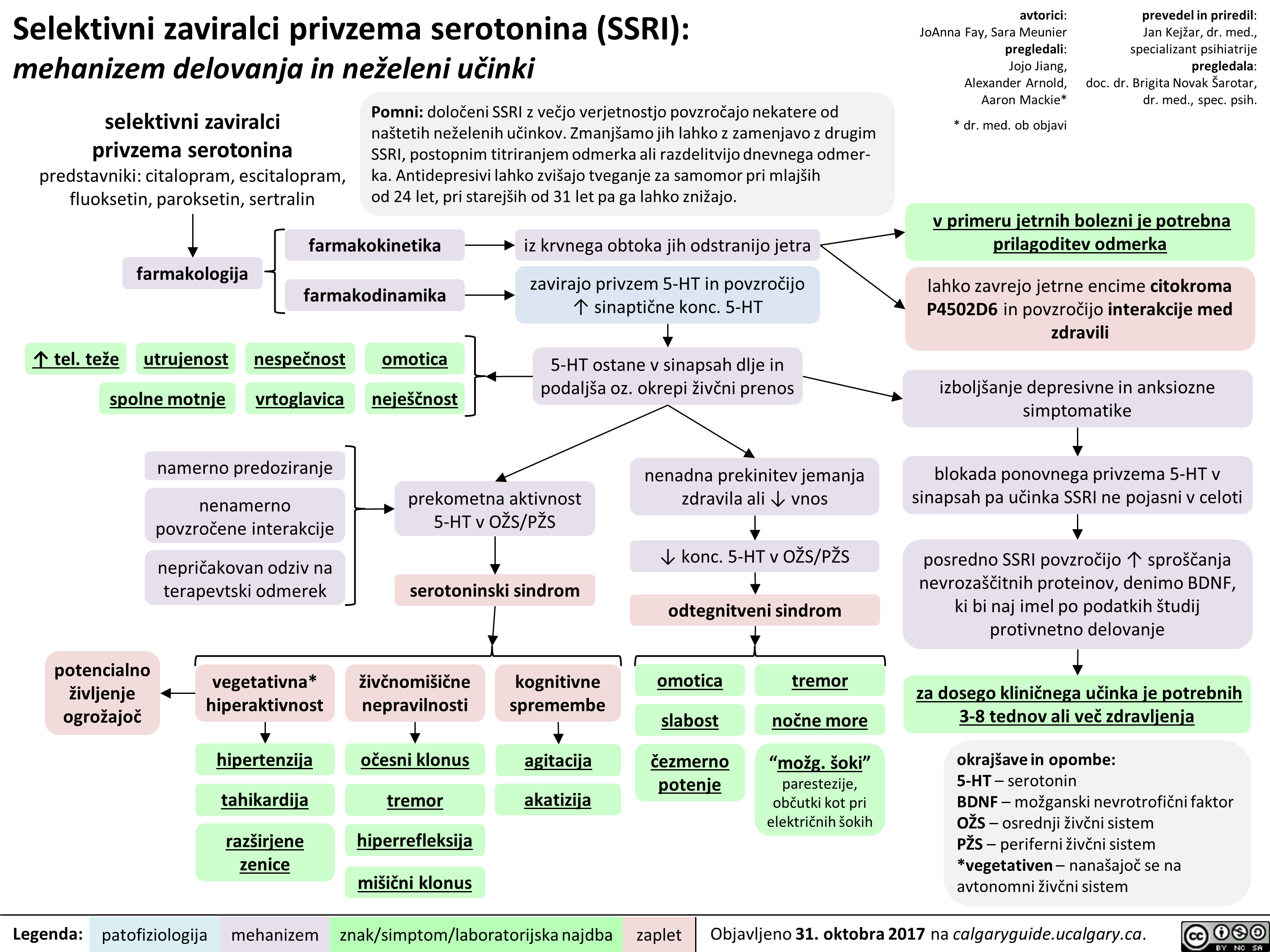
Nevroanatomija in fiziologija čustev
![Nevroanatomija in fiziologija tustev
bazalni gangliji
prefrontalna skorja obdeluje 6ustva vgje-ga reda, ki zahtevajo priklic, razum(sko) presojo in sposobnost odloCanja (npr. sramota) senzorne informacije iz notranjih organov kot odziv na spralne okoljske objekte ali dogodke integrira z informacijami iz amigdale
Zustveni obEutki (npr. zavestne izkugnje Zustev)
1—
talamus
Zustveno izstopaja okoljski drailjaj
zaznave (npr. vid, sluh, tip, oku'ganje, vonjanje)
avtorica: Andrea Moir pregledali: Erika Russell, Usama Malik, Brienne McLane*
* dr. med. ob objavi
hipotalamus (glavna izhodna [ang. output] struktura limbibega sistema)
voh*
prim. in asociacijski predeli mo2g. skorje •
amigdala obdeluje 6ustva niijega reda, torej tista s hitrimi, samodejnimi in pogojevanimi odzivi (npr. strah) sodeluje pri tvorbi in priklicu C'ustveno pomembnih spominov iz neokortikalnih podrodj, torej zaznavi pripi§e neko Custveno vrednost
hipokampus (kljaen za utrditev in priklic spominov)
motorl6ni, endokrini in visceralni sistemi
prevedel in priredil: Jan Kejiar, dr. med., specializant psihiatrije pregledala: doc. dr. Brigita Novak Sarotar, dr. med., spec. psih.
avtonomni zivcni sistem (A2S) A2S se samodejno in podzavestno odziva na okoljske dra2ljaje (npr. s '(` frekvence sr6nega utripa ali zardevanjem)
telesni odziv na Zustveni drailja(
Pomni: • Strukture, ki sodelujejo pri C'ustvovanju, se imenujejo limbiEni sistem. • Talamus, bazalni gangliji in prefrontalna skoraj skupaj tvorijo kortiko-striato-talamo-kortikalno zanko, ki predstavlja glavno pot za obdelavo C'ustev v moiganih. • Prefrontalna skorja vkljue'uje orbitofrontalno skorjo, dorzolateralno prefrontalno skorjo in sprednjo cingulatno skorjo. • *Voh je edini cut, cigar vlakna zaobidejo talamus in se stekajo neposredno v primarno olfaktorno skorjo. Nevroanatomija in fiziologija tustev
bazalni gangliji
prefrontalna skorja obdeluje 6ustva vgje-ga reda, ki zahtevajo priklic, razum(sko) presojo in sposobnost odloCanja (npr. sramota) senzorne informacije iz notranjih organov kot odziv na spralne okoljske objekte ali dogodke integrira z informacijami iz amigdale
Zustveni obEutki (npr. zavestne izkugnje Zustev)
1—
talamus
Zustveno izstopaja okoljski drailjaj
zaznave (npr. vid, sluh, tip, oku'ganje, vonjanje)
avtorica: Andrea Moir pregledali: Erika Russell, Usama Malik, Brienne McLane*
* dr. med. ob objavi
hipotalamus (glavna izhodna [ang. output] struktura limbibega sistema)
voh*
prim. in asociacijski predeli mo2g. skorje •
amigdala obdeluje 6ustva niijega reda, torej tista s hitrimi, samodejnimi in pogojevanimi odzivi (npr. strah) sodeluje pri tvorbi in priklicu C'ustveno pomembnih spominov iz neokortikalnih podrodj, torej zaznavi pripi§e neko Custveno vrednost
hipokampus (kljaen za utrditev in priklic spominov)
motorl6ni, endokrini in visceralni sistemi
prevedel in priredil: Jan Kejiar, dr. med., specializant psihiatrije pregledala: doc. dr. Brigita Novak Sarotar, dr. med., spec. psih.
avtonomni zivcni sistem (A2S) A2S se samodejno in podzavestno odziva na okoljske dra2ljaje (npr. s '(` frekvence sr6nega utripa ali zardevanjem)
telesni odziv na Zustveni drailja(
Pomni: • Strukture, ki sodelujejo pri C'ustvovanju, se imenujejo limbiEni sistem. • Talamus, bazalni gangliji in prefrontalna skoraj skupaj tvorijo kortiko-striato-talamo-kortikalno zanko, ki predstavlja glavno pot za obdelavo C'ustev v moiganih. • Prefrontalna skorja vkljue'uje orbitofrontalno skorjo, dorzolateralno prefrontalno skorjo in sprednjo cingulatno skorjo. • *Voh je edini cut, cigar vlakna zaobidejo talamus in se stekajo neposredno v primarno olfaktorno skorjo.](http://calgaryguide.ucalgary.ca/wp-content/uploads/2017/11/The-Neuroanatomy-and-Physiology-of-Emotion-Slovenian-translation-FINAL-VERSION.png)
Diabetic Foot: Pathogenesis and clinical findings
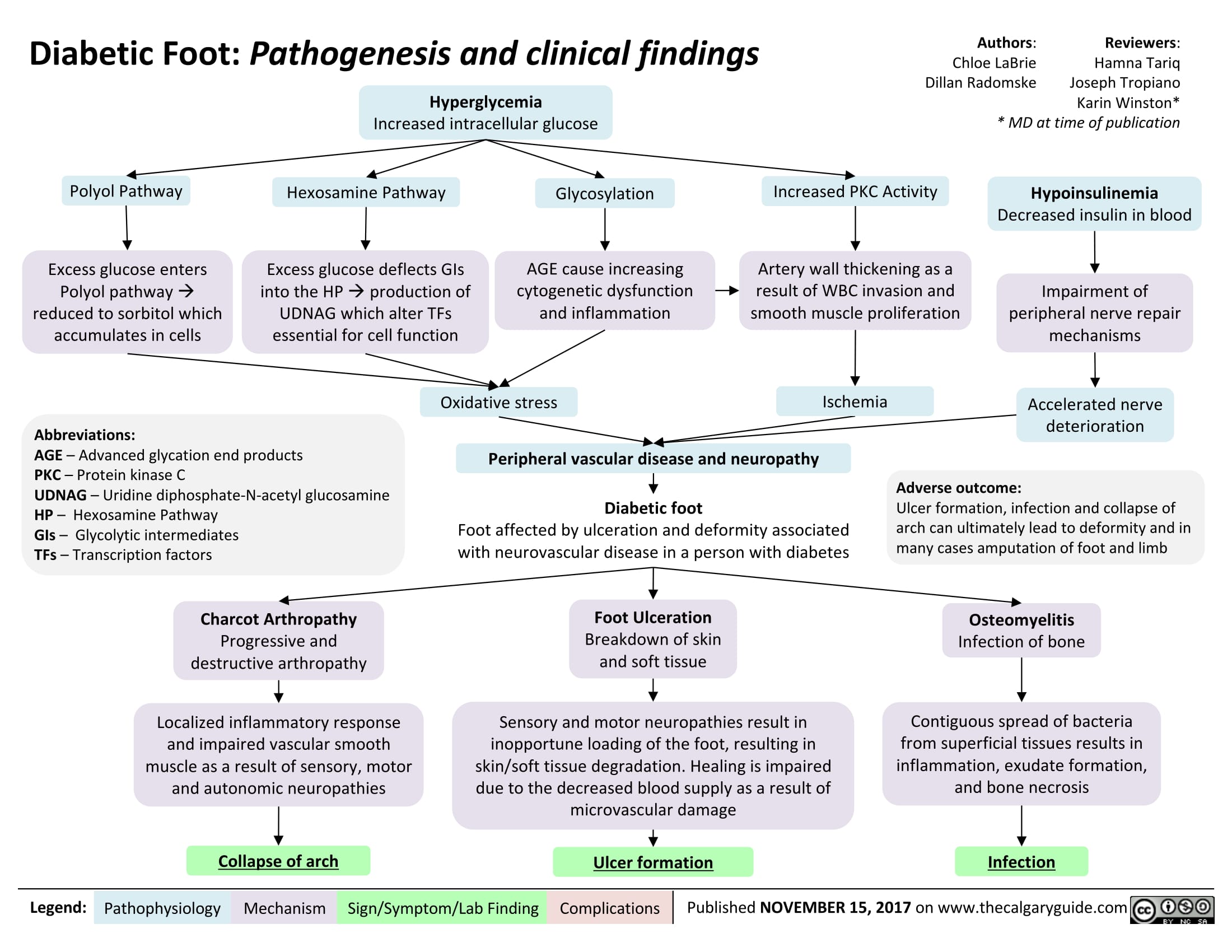
Classification of Pelvic Ring Fractures: Mechanisms, Clinical Features and Complications
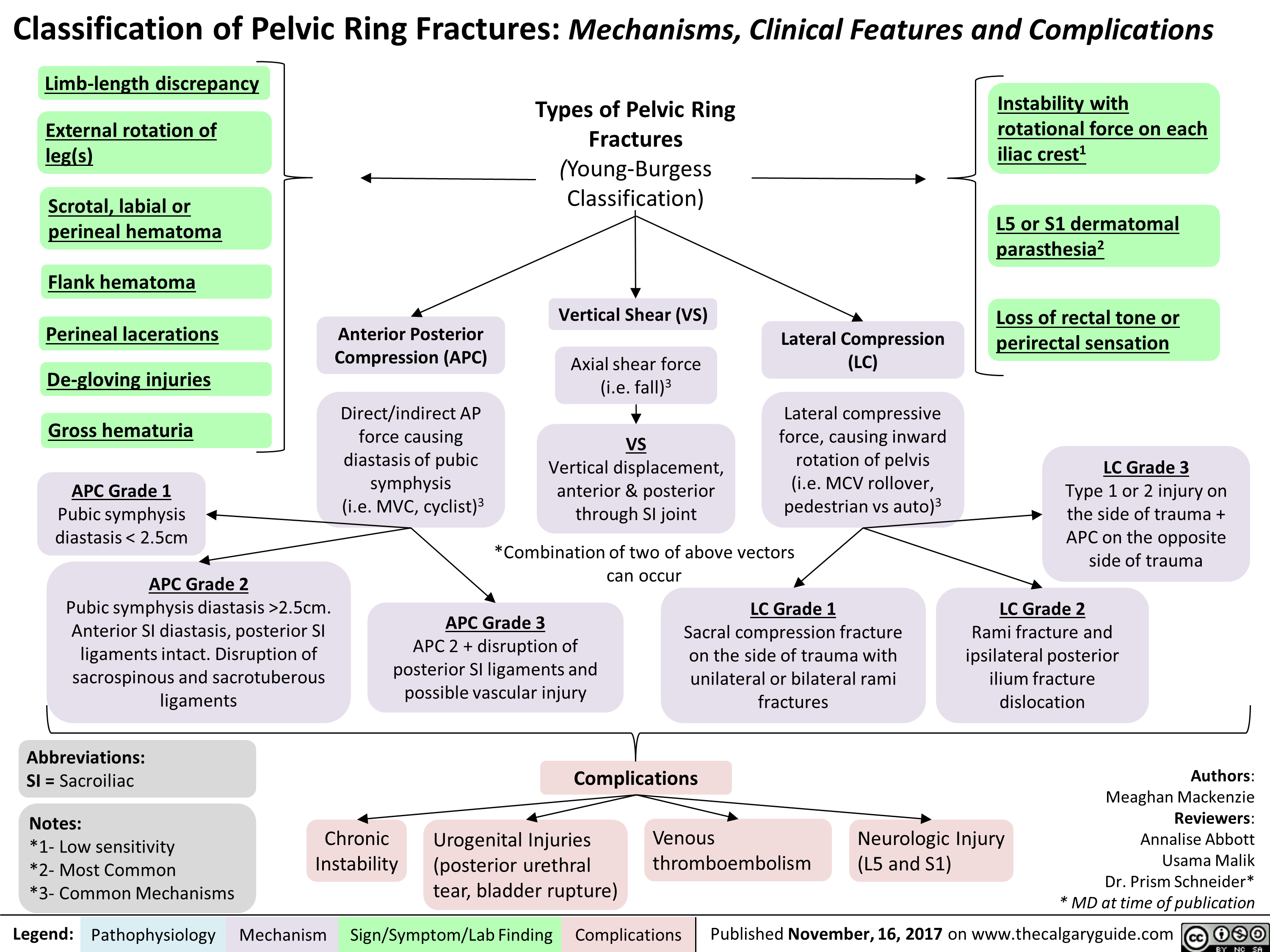
Open Fractures: Mechanisms, Clinical Features and Complications
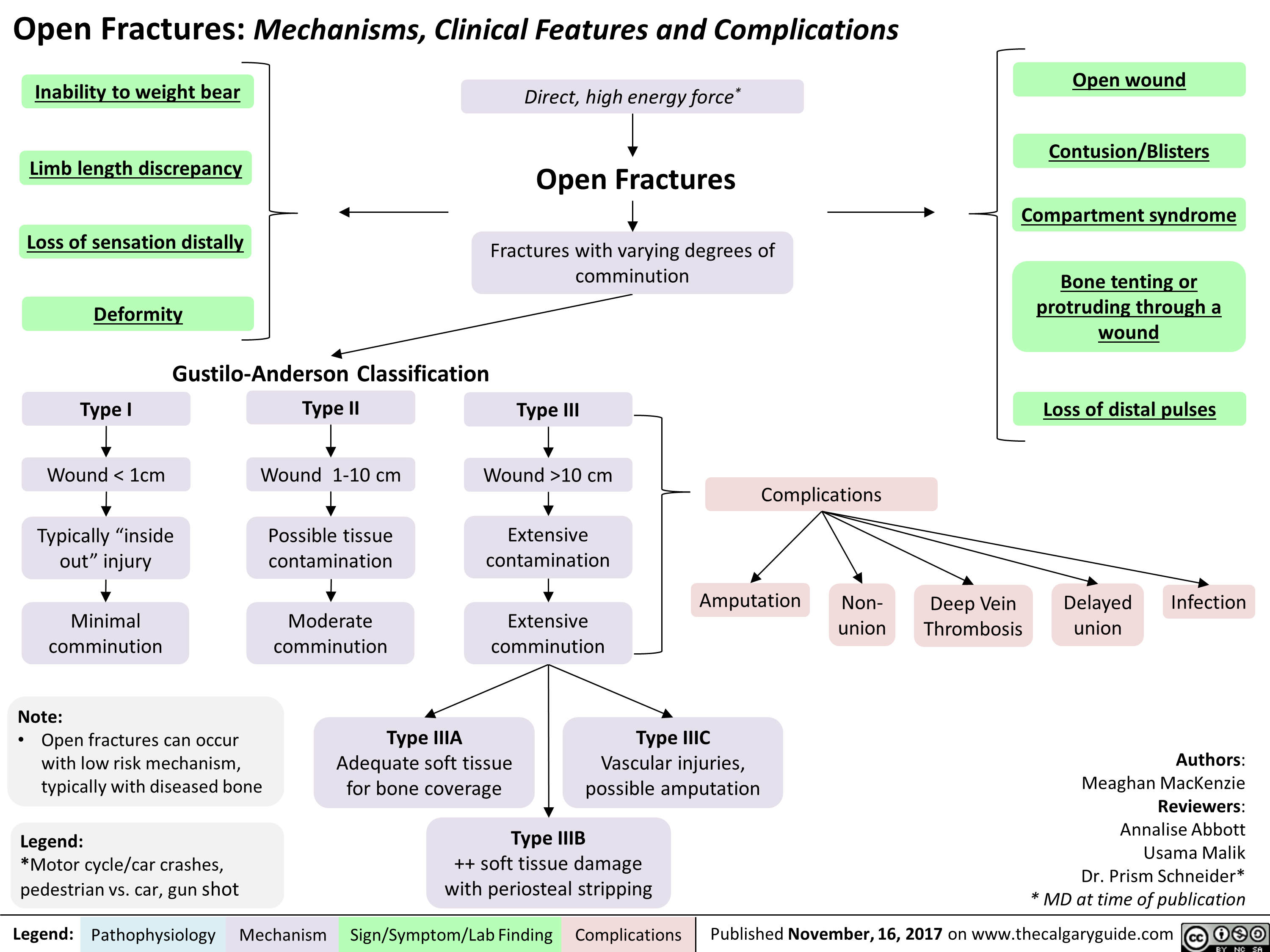 10 cm
4,
Extensive
contamination
Extensive
comminution
Type IIIA
Adequate soft tissue
for bone coverage
Legend: Pathophysiology Mechanism
Complications
Open wound
Contusion/Blisters
Compartment syndrome
Bone tenting or
protruding through a
wound
Loss of distal pulses
Amputation
Type IIIC
Vascular injuries,
possible amputation
•
Type IIIB
++ soft tissue damage
with periosteal stripping
Sign/Symptom/Lab Finding
Non-
union
Deep Vein
Thrombosis
Delayed
union
Infection
Authors:
Meaghan MacKenzie
Reviewers:
Annalise Abbott
Usama Malik
Dr. Prism Schneider*
* MD at time of publication " title="Open Fractures: Mechanisms, Clinical Features and Complications
Inability to weight bear
Limb length discrepancy
•
Loss of sensation distally
Deformity
Gustilo-Anderson Classification
Type I
Wound < 1cm
Typically "inside
out" injury
Yir
Minimal
comminution
Type II
Wound 1-10 cm
4,
Possible tissue
contamination
Moderate
comminution
Note:
• Open fractures can occur
with low risk mechanism,
typically with diseased bone
Legend:
*Motor cycle/car crashes,
pedestrian vs. car, gun shot
Direct, high energy force*
Open Fractures
Fractures with varying degrees of
comminution
Type Ill
Yir
Wound >10 cm
4,
Extensive
contamination
Extensive
comminution
Type IIIA
Adequate soft tissue
for bone coverage
Legend: Pathophysiology Mechanism
Complications
Open wound
Contusion/Blisters
Compartment syndrome
Bone tenting or
protruding through a
wound
Loss of distal pulses
Amputation
Type IIIC
Vascular injuries,
possible amputation
•
Type IIIB
++ soft tissue damage
with periosteal stripping
Sign/Symptom/Lab Finding
Non-
union
Deep Vein
Thrombosis
Delayed
union
Infection
Authors:
Meaghan MacKenzie
Reviewers:
Annalise Abbott
Usama Malik
Dr. Prism Schneider*
* MD at time of publication " />
10 cm
4,
Extensive
contamination
Extensive
comminution
Type IIIA
Adequate soft tissue
for bone coverage
Legend: Pathophysiology Mechanism
Complications
Open wound
Contusion/Blisters
Compartment syndrome
Bone tenting or
protruding through a
wound
Loss of distal pulses
Amputation
Type IIIC
Vascular injuries,
possible amputation
•
Type IIIB
++ soft tissue damage
with periosteal stripping
Sign/Symptom/Lab Finding
Non-
union
Deep Vein
Thrombosis
Delayed
union
Infection
Authors:
Meaghan MacKenzie
Reviewers:
Annalise Abbott
Usama Malik
Dr. Prism Schneider*
* MD at time of publication " title="Open Fractures: Mechanisms, Clinical Features and Complications
Inability to weight bear
Limb length discrepancy
•
Loss of sensation distally
Deformity
Gustilo-Anderson Classification
Type I
Wound < 1cm
Typically "inside
out" injury
Yir
Minimal
comminution
Type II
Wound 1-10 cm
4,
Possible tissue
contamination
Moderate
comminution
Note:
• Open fractures can occur
with low risk mechanism,
typically with diseased bone
Legend:
*Motor cycle/car crashes,
pedestrian vs. car, gun shot
Direct, high energy force*
Open Fractures
Fractures with varying degrees of
comminution
Type Ill
Yir
Wound >10 cm
4,
Extensive
contamination
Extensive
comminution
Type IIIA
Adequate soft tissue
for bone coverage
Legend: Pathophysiology Mechanism
Complications
Open wound
Contusion/Blisters
Compartment syndrome
Bone tenting or
protruding through a
wound
Loss of distal pulses
Amputation
Type IIIC
Vascular injuries,
possible amputation
•
Type IIIB
++ soft tissue damage
with periosteal stripping
Sign/Symptom/Lab Finding
Non-
union
Deep Vein
Thrombosis
Delayed
union
Infection
Authors:
Meaghan MacKenzie
Reviewers:
Annalise Abbott
Usama Malik
Dr. Prism Schneider*
* MD at time of publication " />
Bronchogenic Carcinoma - Pancoast Tumors Pathogenesis and clinical findings
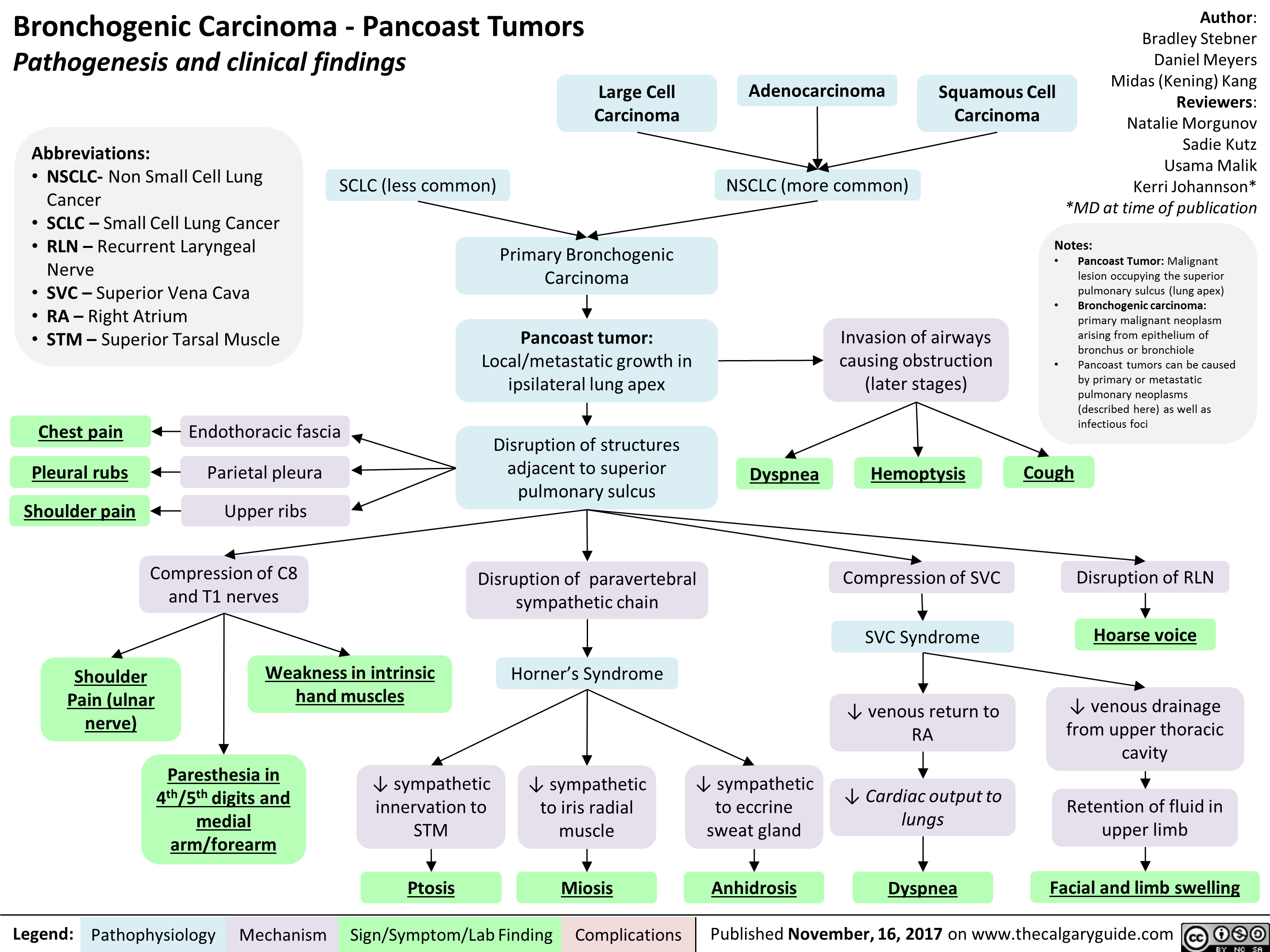
Polycystic Ovarian Syndrome

Nitrous Oxide
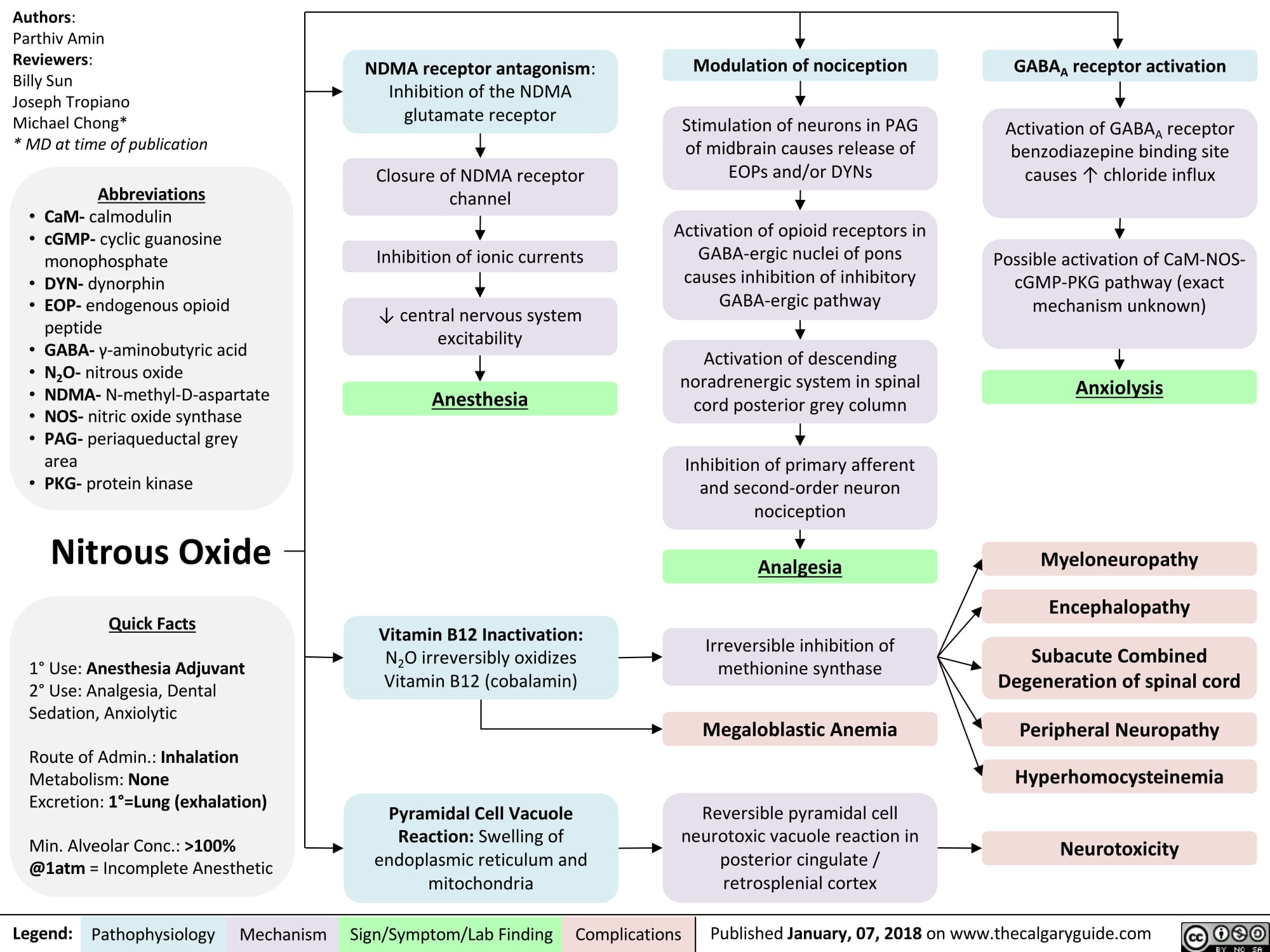
Hyperthyroidism
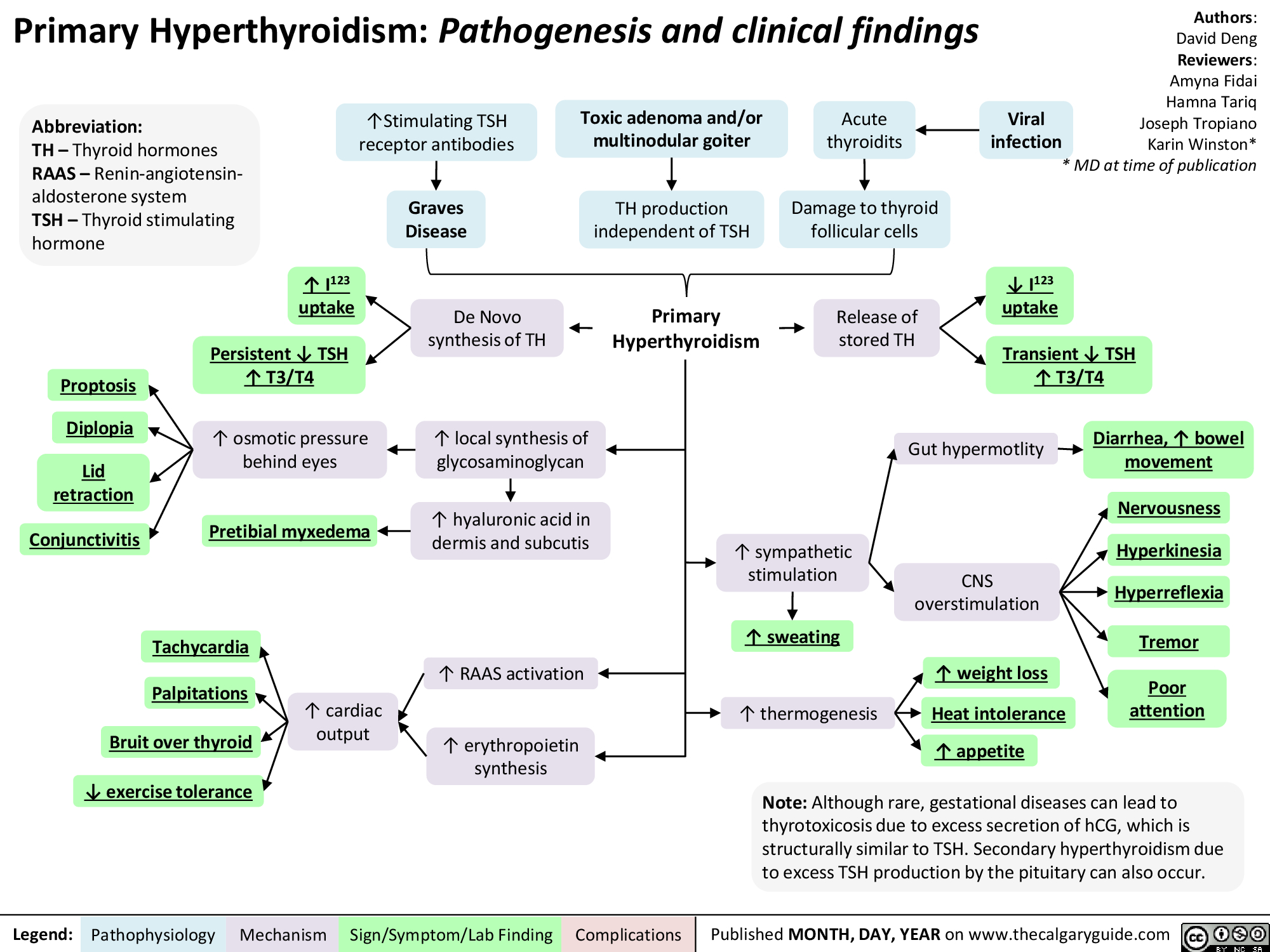
Hyperthyroidism
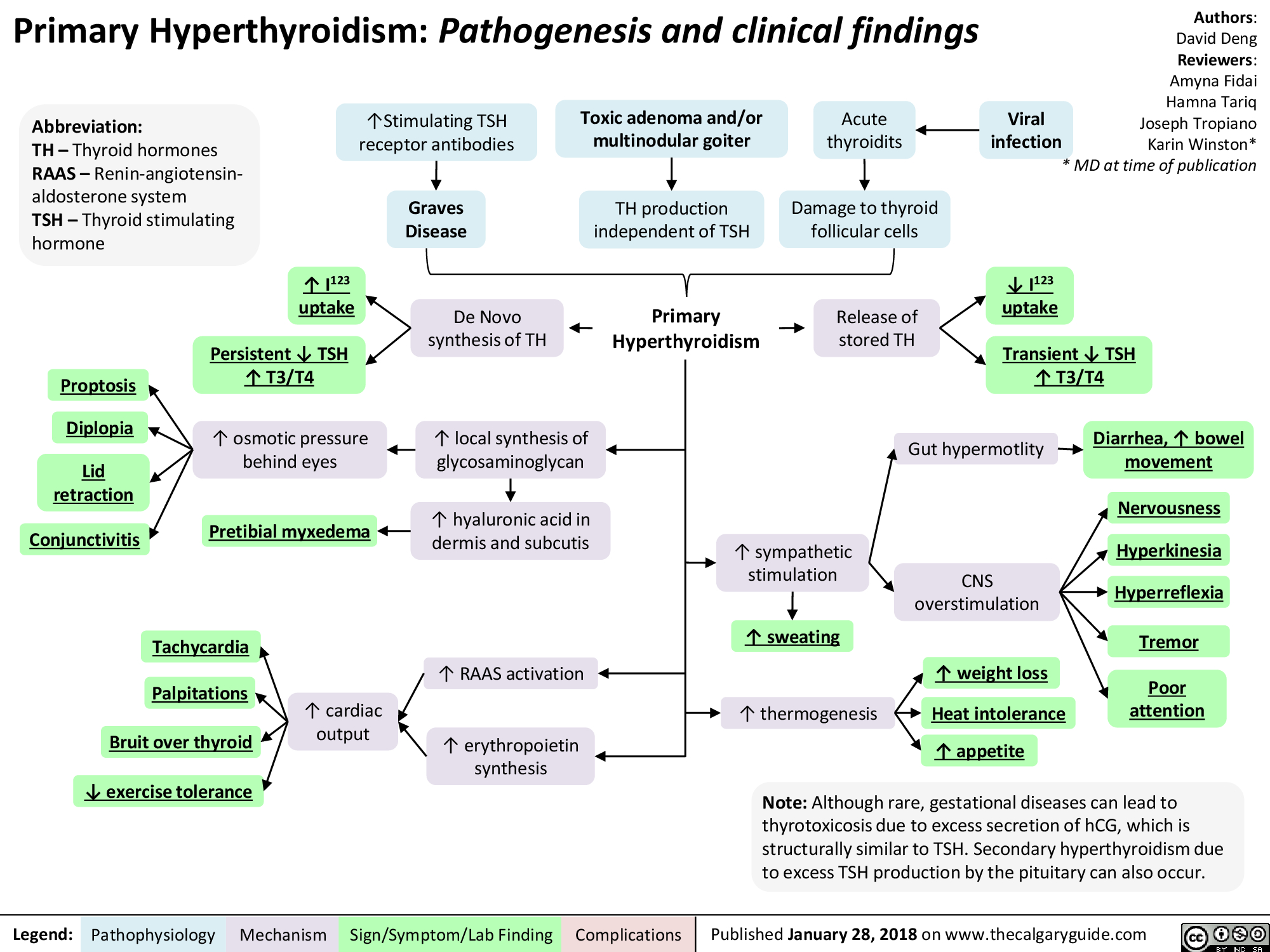
Growth Hormone Excess
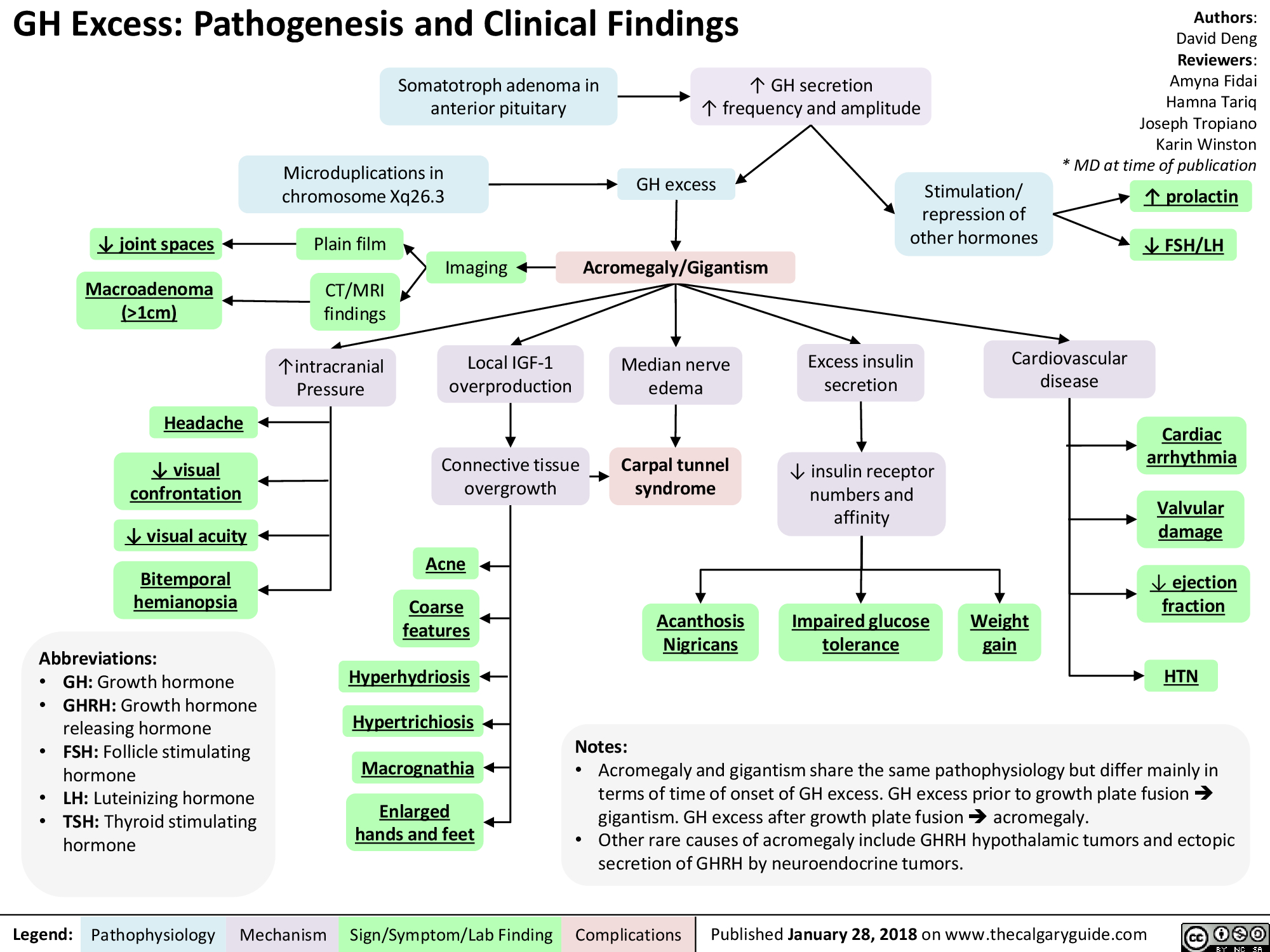
Asthma Acute Exacerbation: Pathogenesis and Treatment
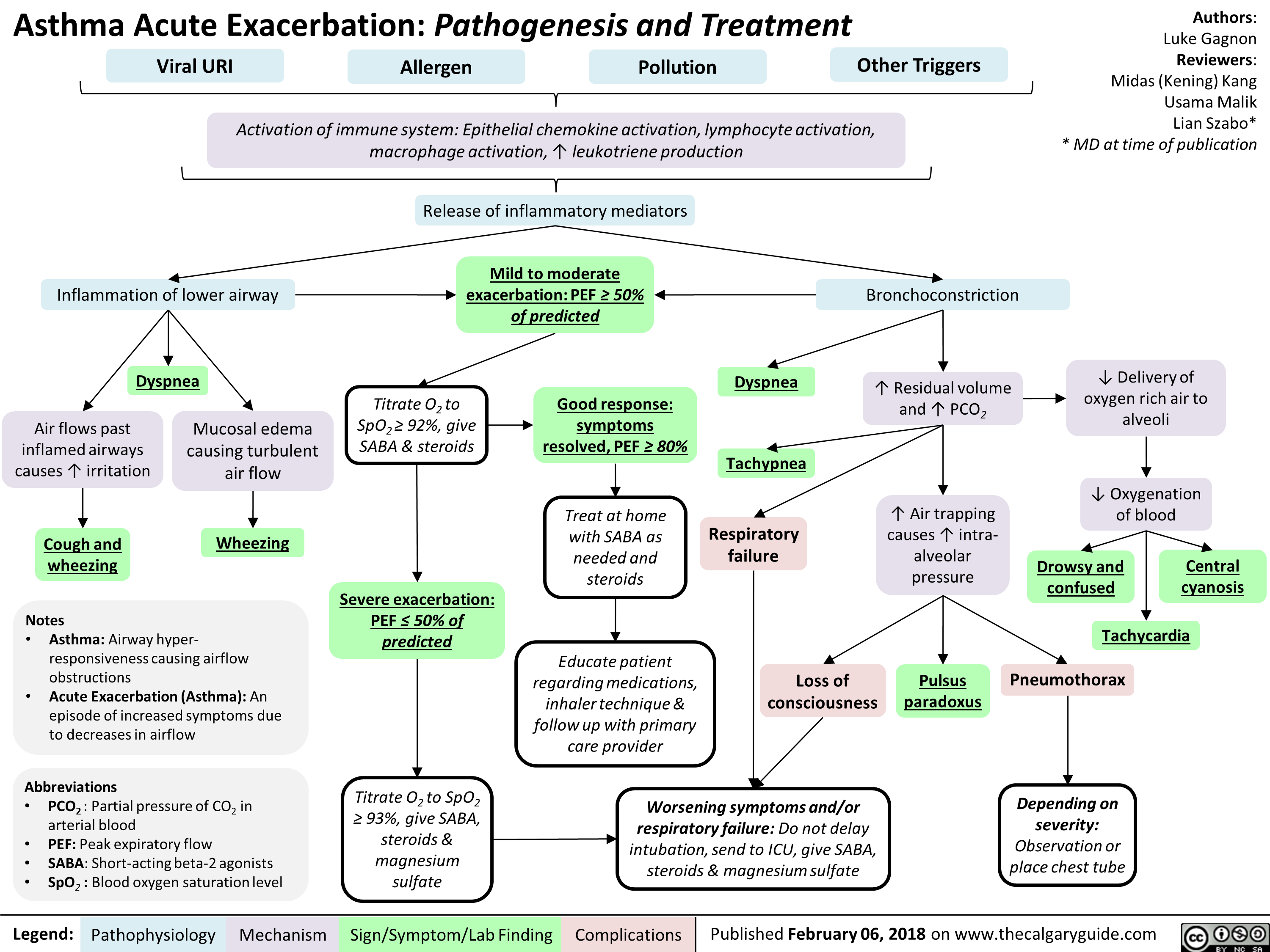
Bronchiectasis Pathogenesis and clinical findings
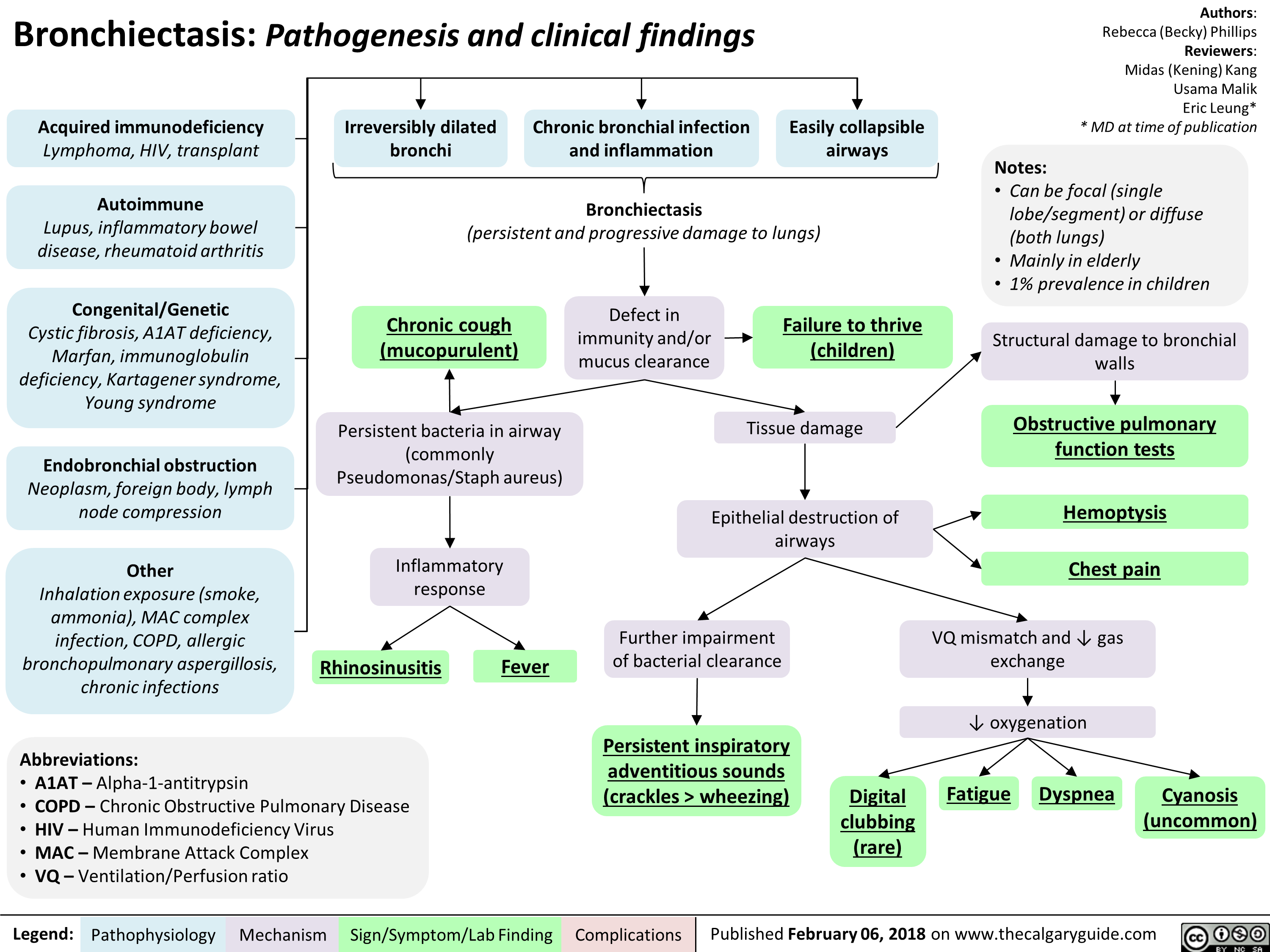
Chronic Thromboembolic Pulmonary Hypertension (CTEPH) Pathogenesis
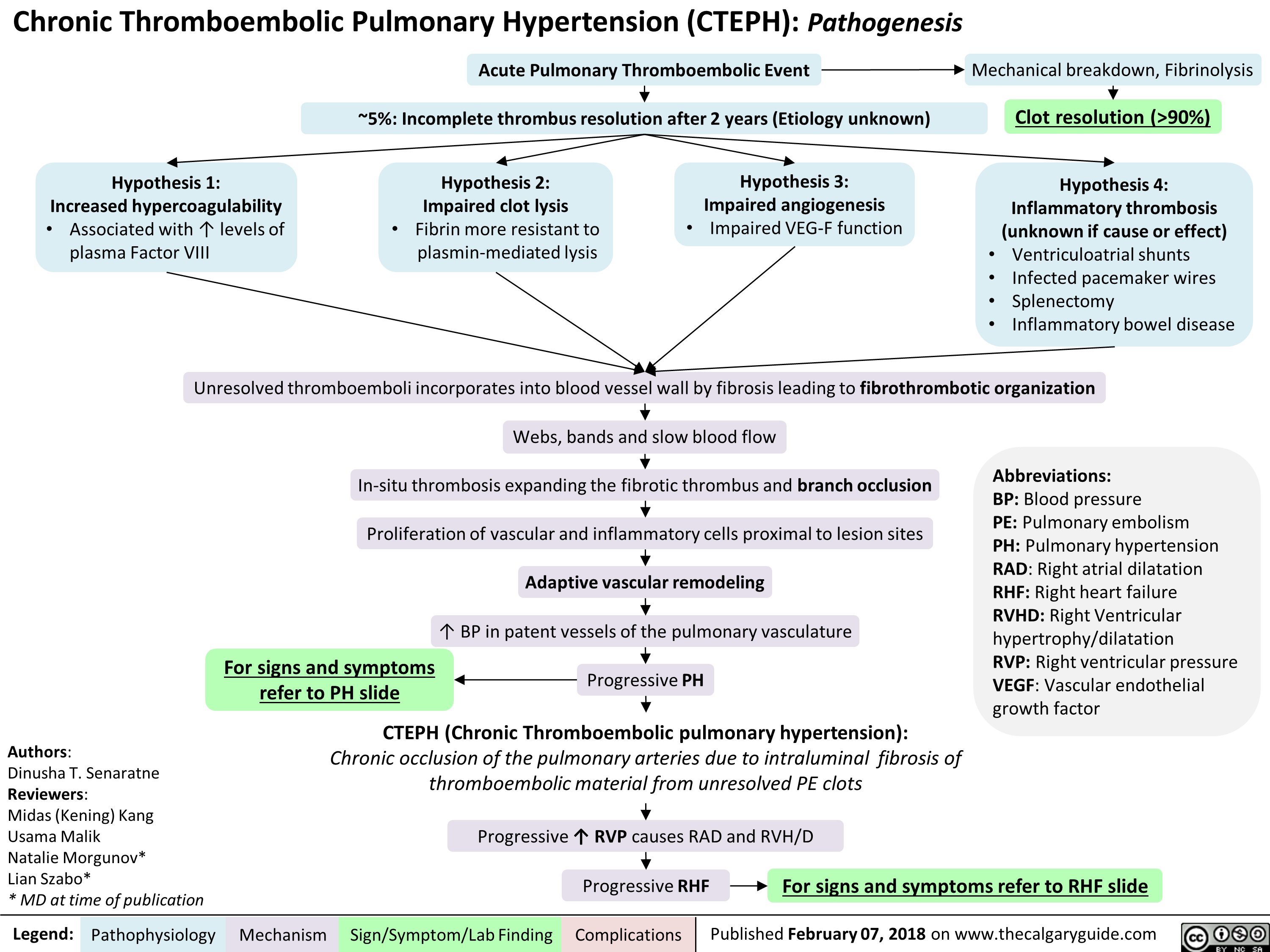
Lung cancer clinical findings and paraneoplastic syndromes
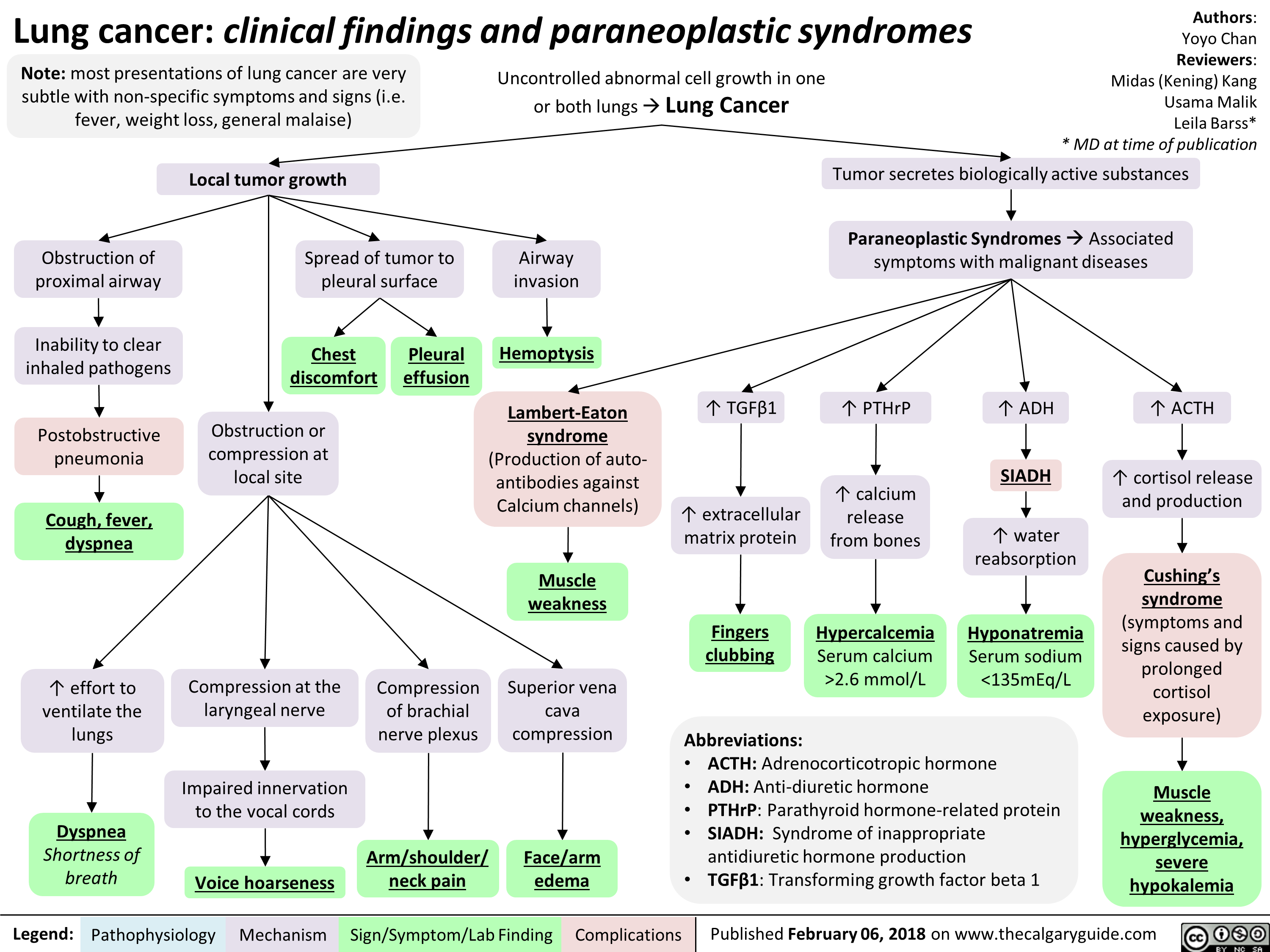
Impetigo Pathogenesis and clinical findings
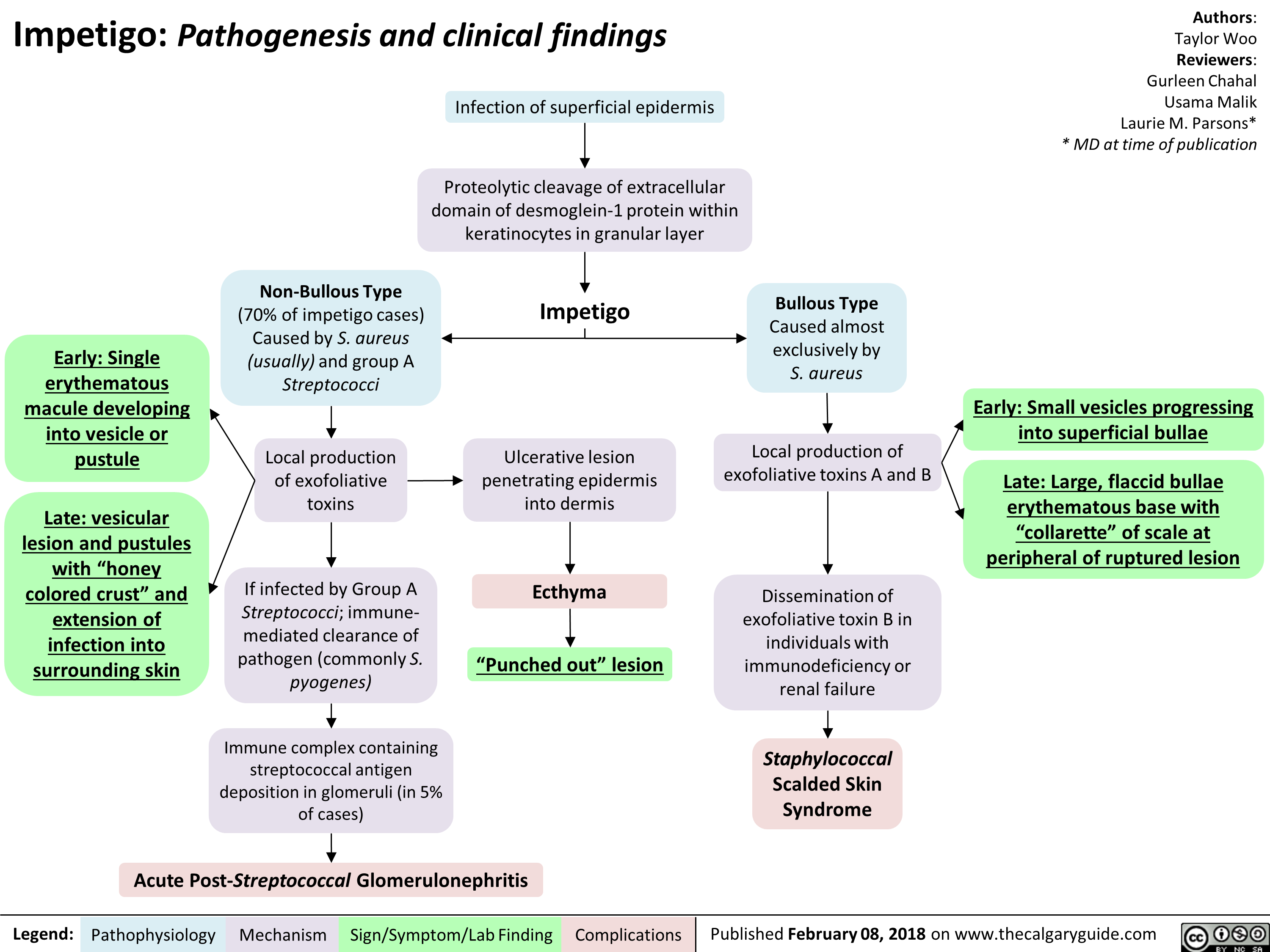
Pressure Ulcers Pathogenesis and clinical findings
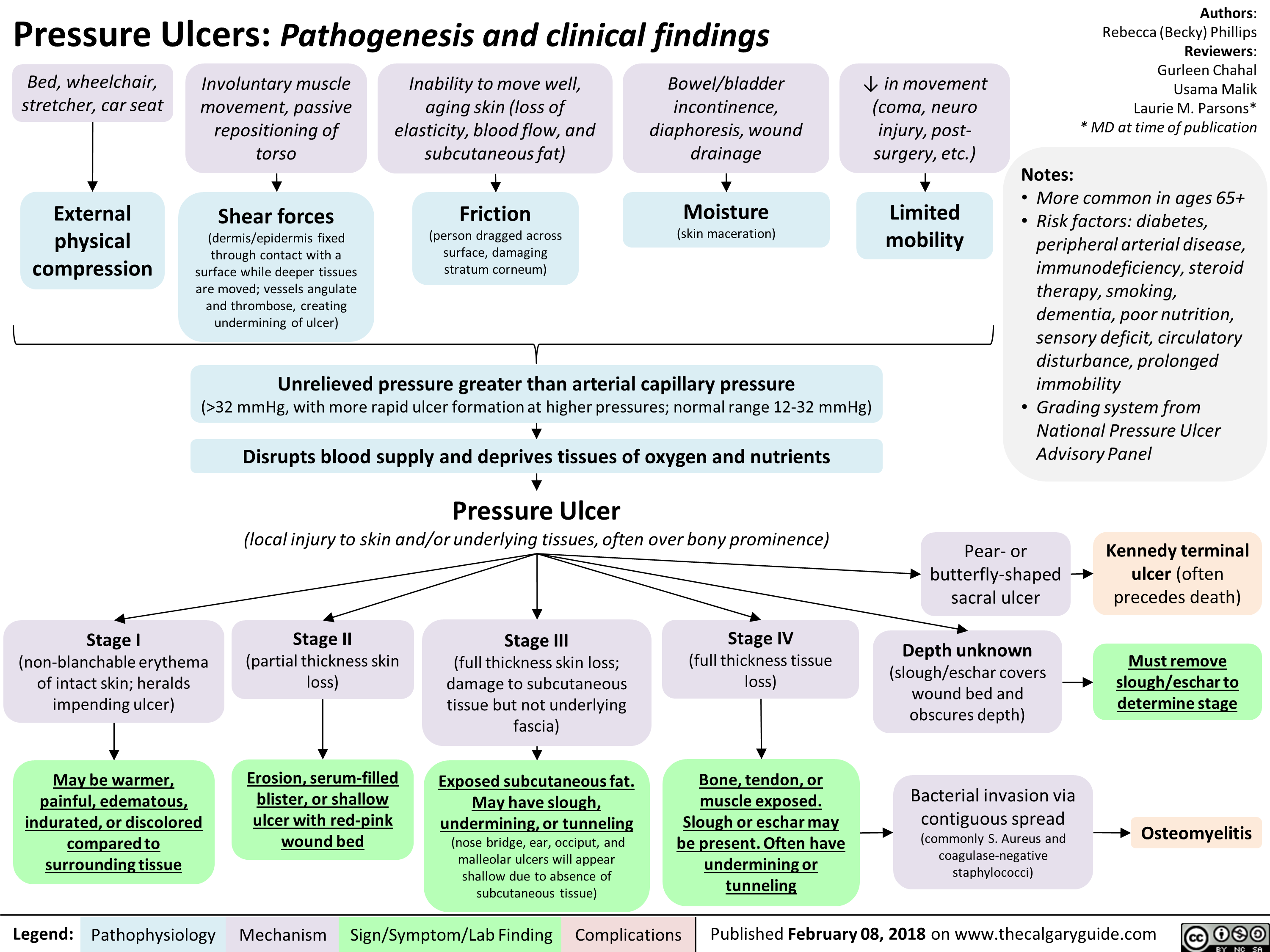
Benign Prostatic Hyperplasia: Pathogenesis and medications
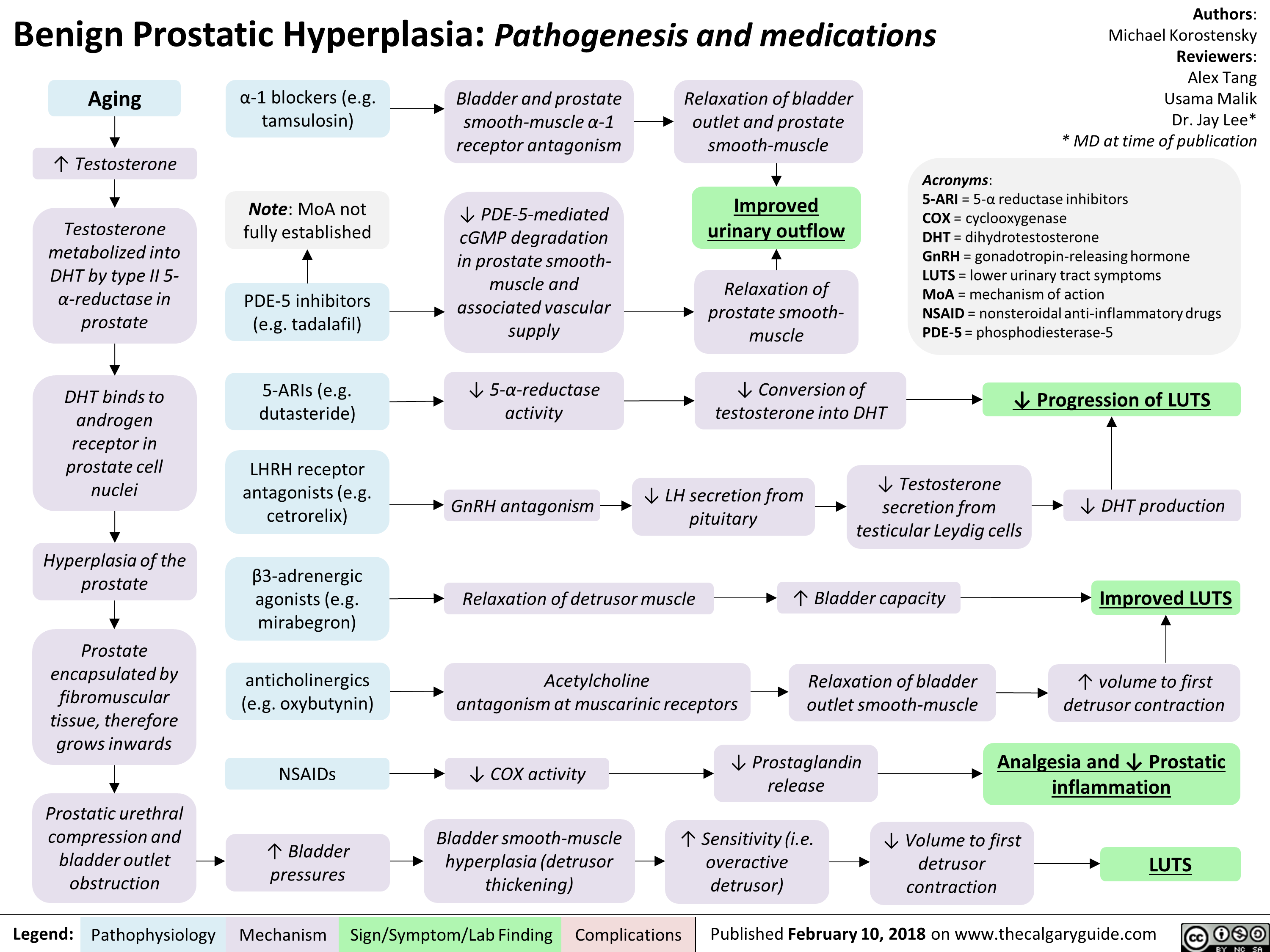
Erectile Dysfunction: Pathogenesis
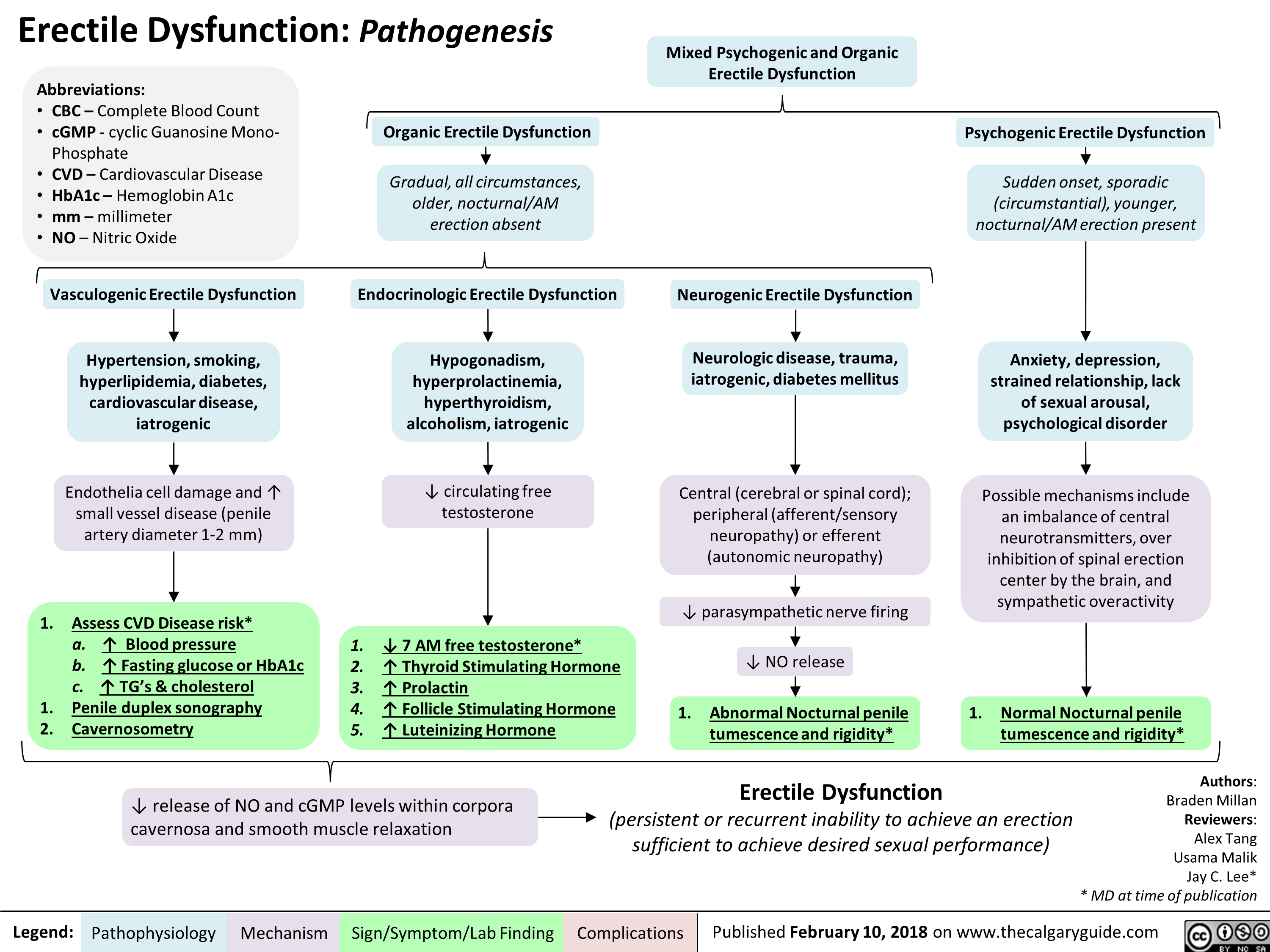
Mixed Urinary Incontinence Pathogenesis and clinical findings
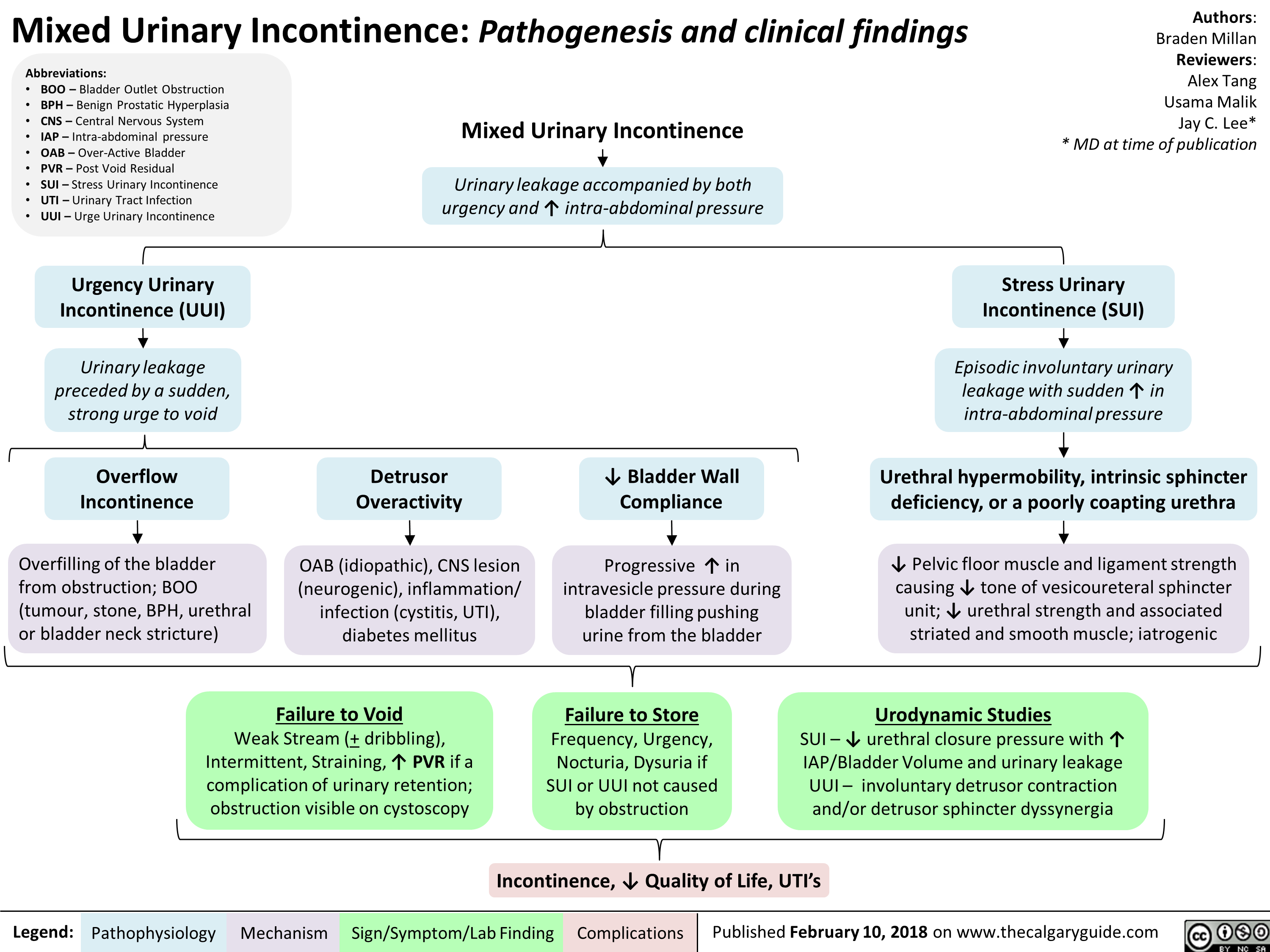
Penyembuhan Luka Akut: Patogenesis dan Temuan Klinis
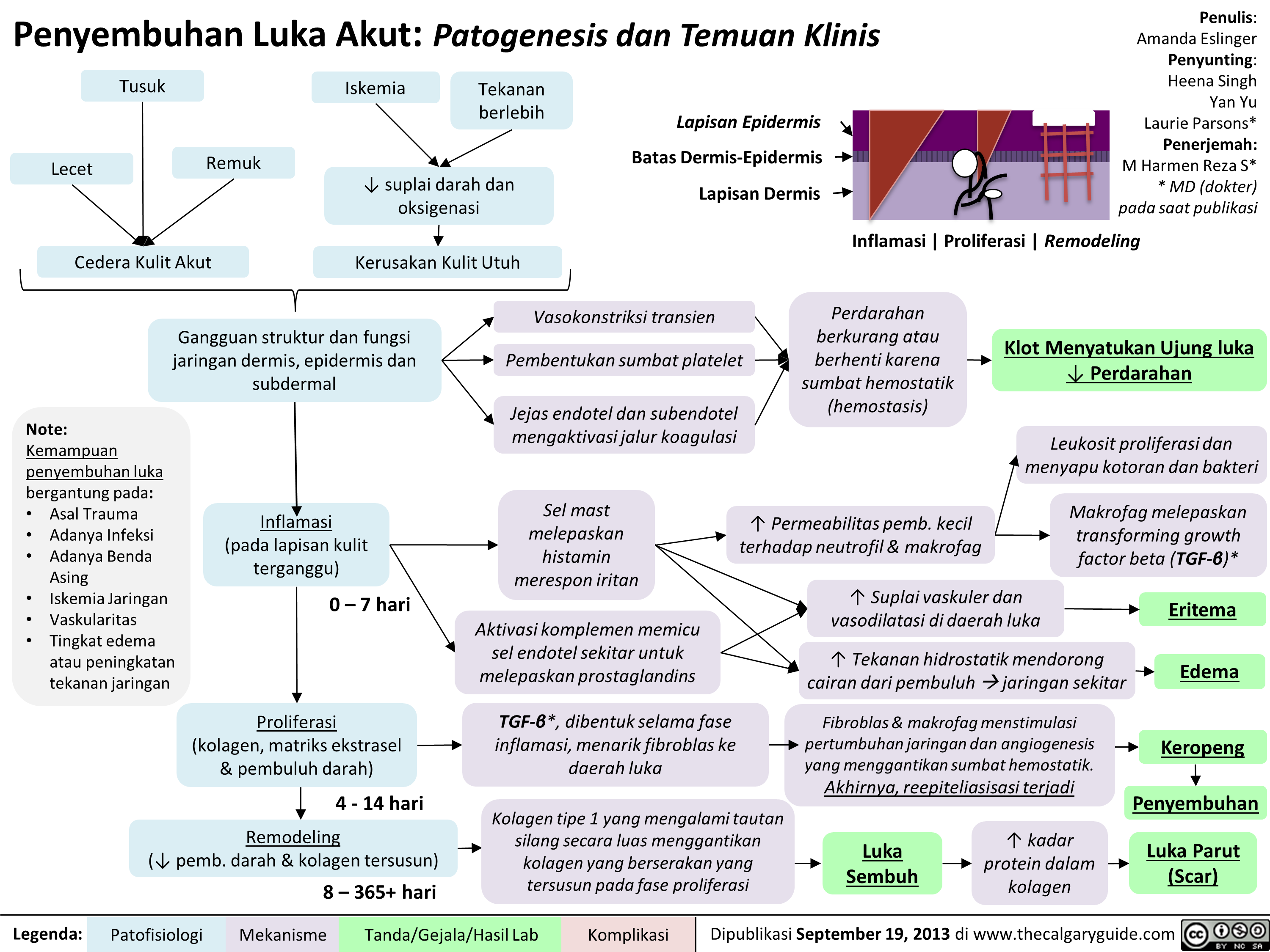
Penyembuhan Fraktur: Tahapan dan Faktor Pengganggu
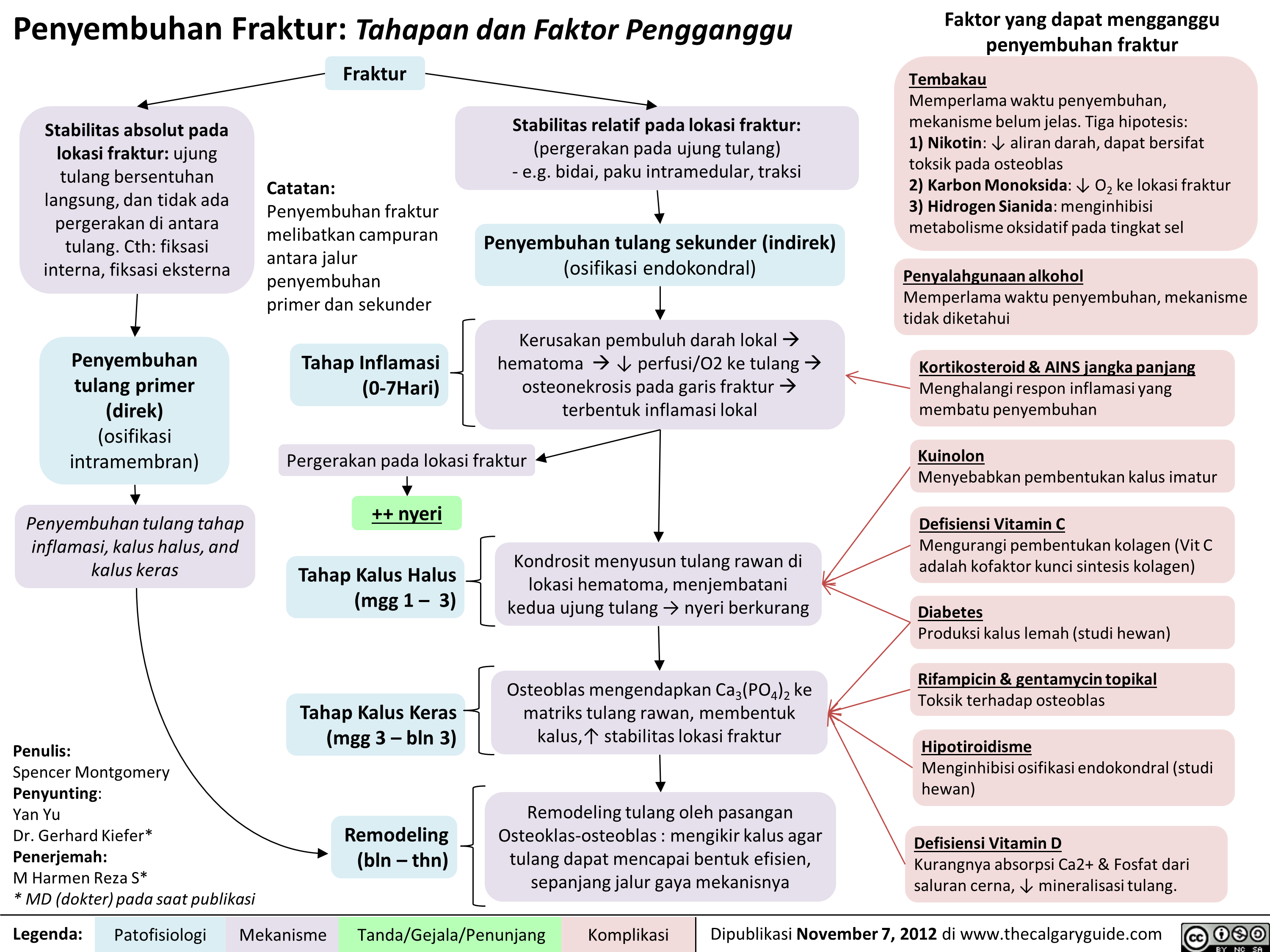
RICE: Mekanisme Aksi
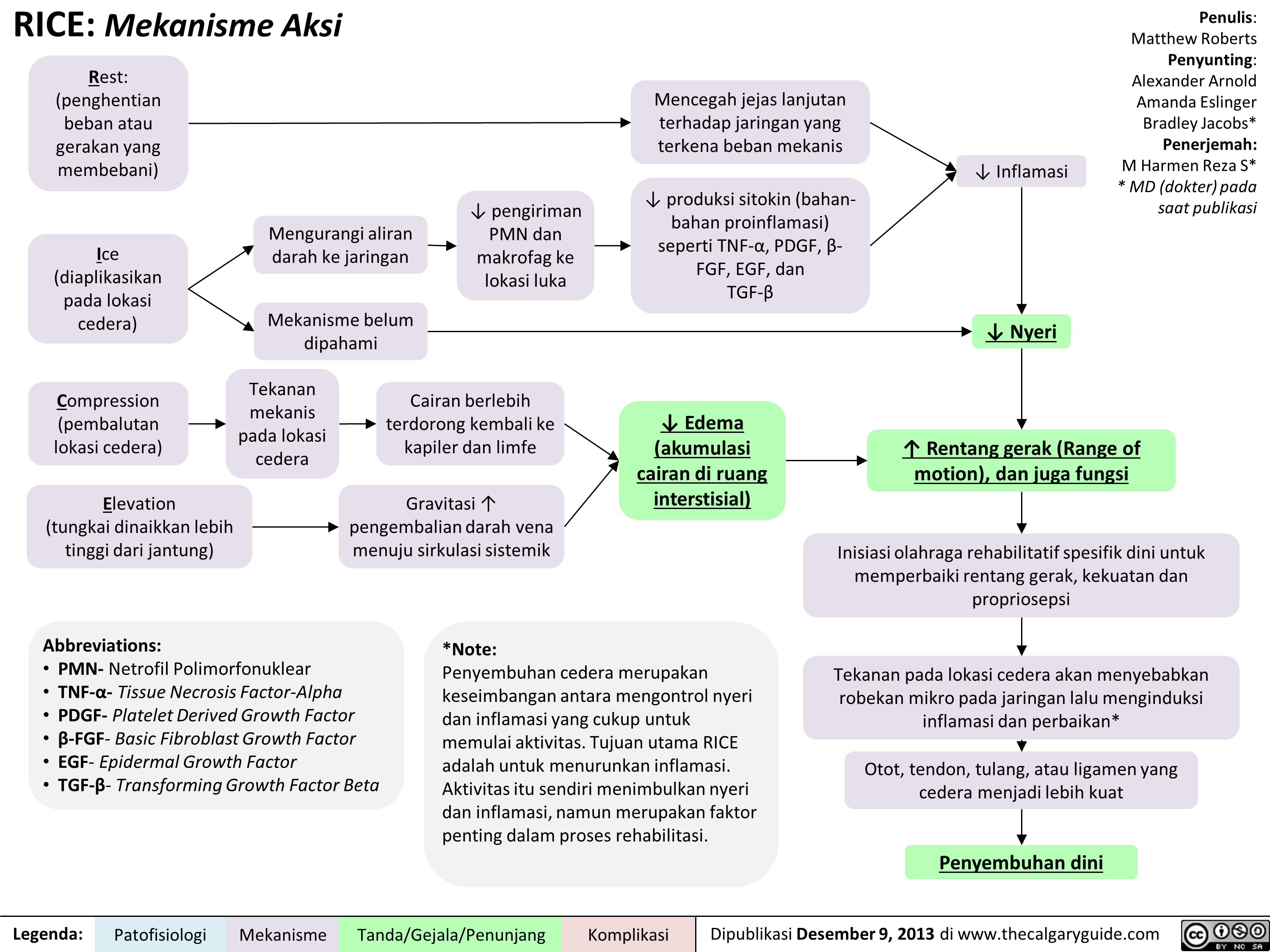
Hemostasis Sekunder: Kaskade Koagulasi
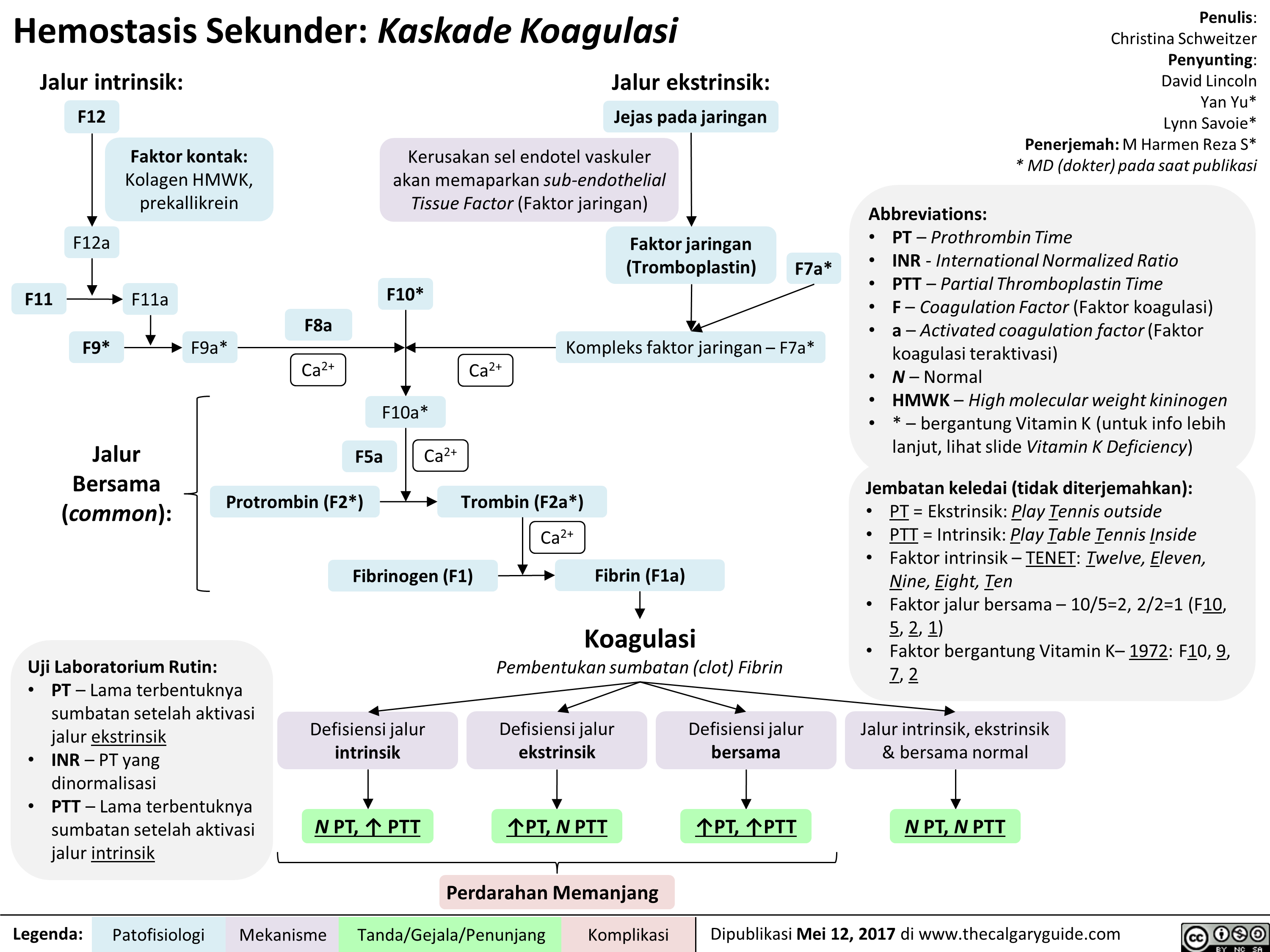
Fisiologi sistem Renin-Angiotensin-Aldosteron (RAAS)
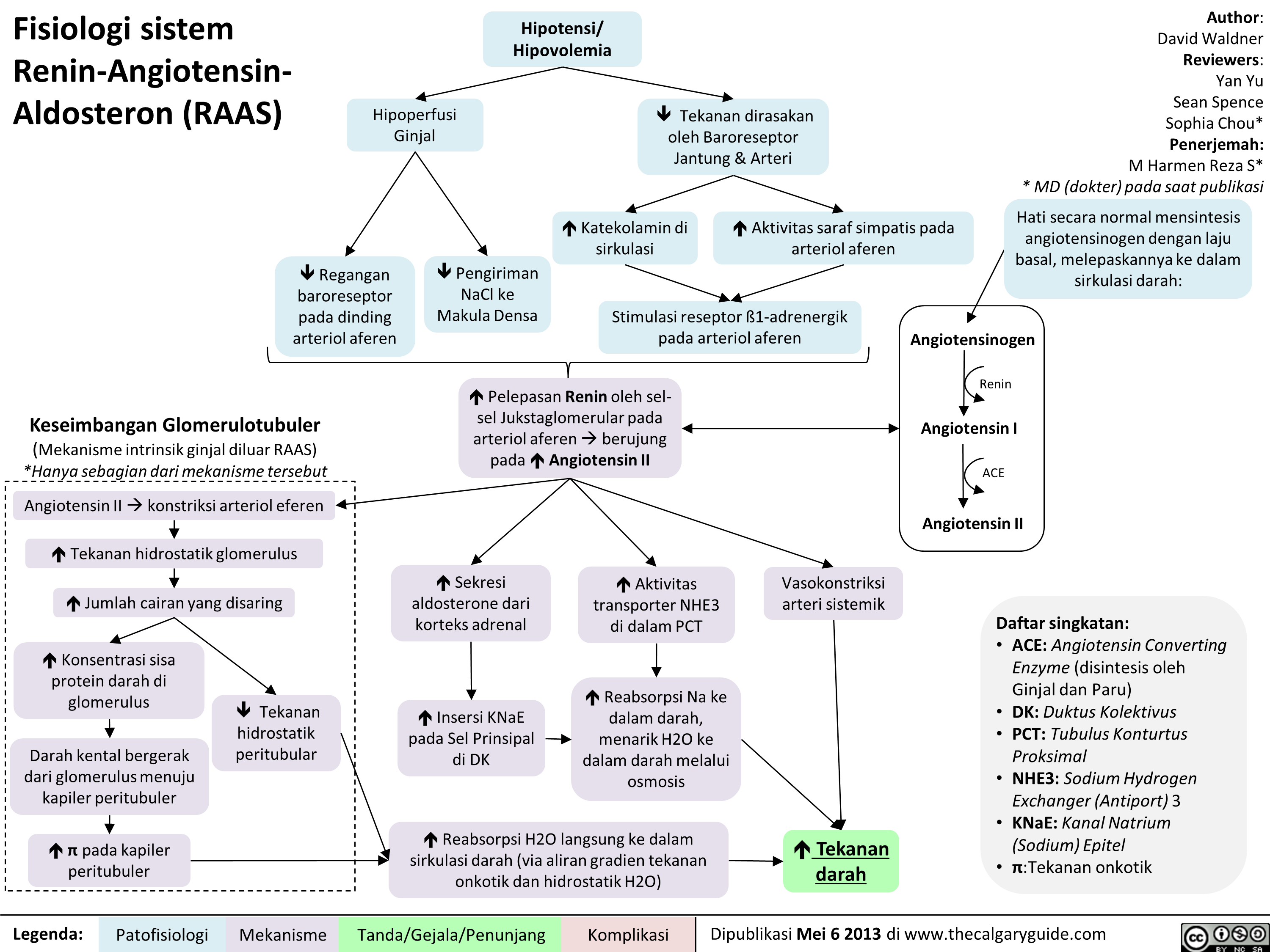
Gradien pO2 Alveolus-arteri: Mengapa ada, dan mengapa penting
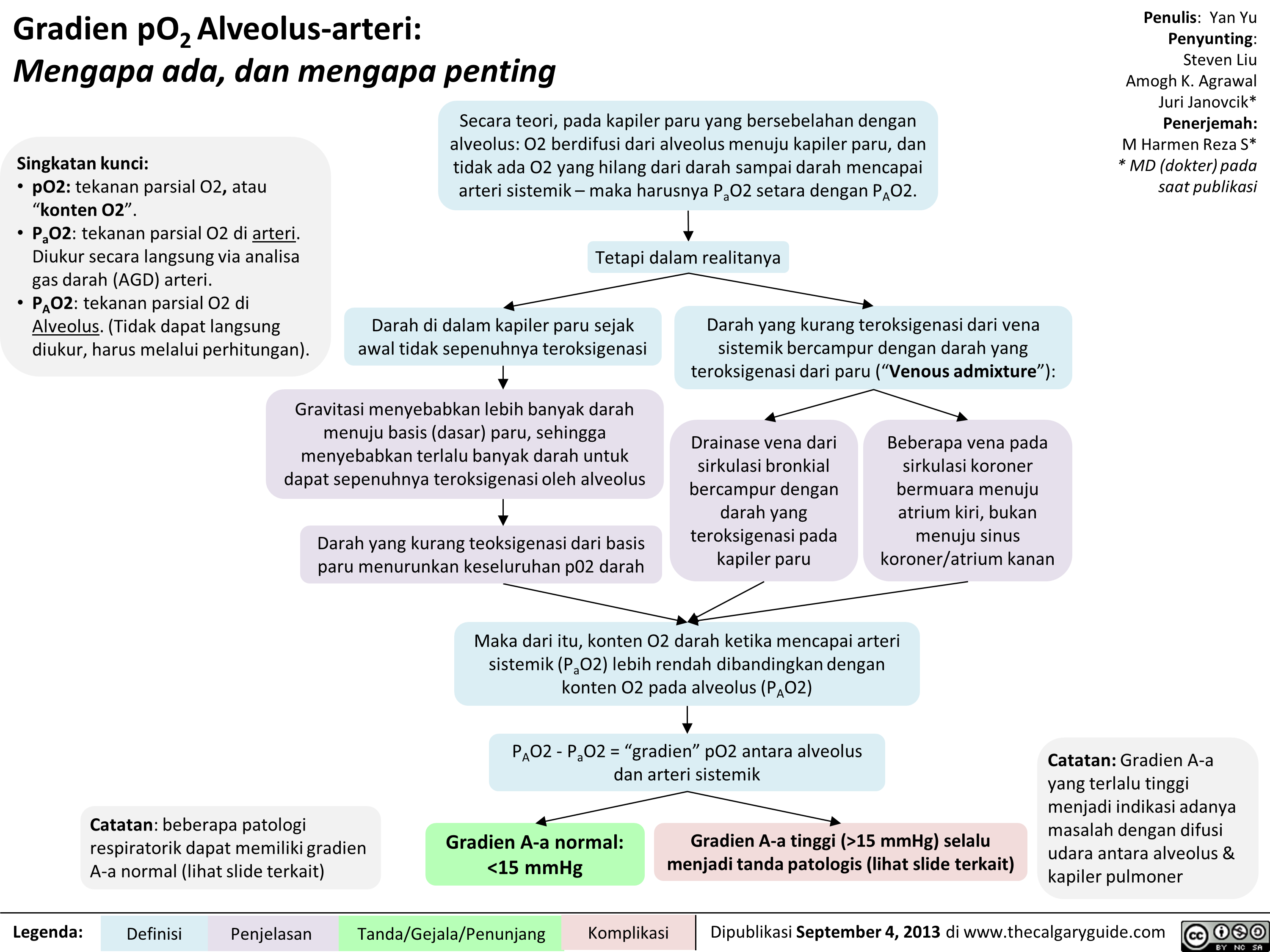 15 mmHg) selalu menjadi tanda patologis (lihat slide terkait)
Penulis: Yan Yu Penyunting: Steven Liu Amogh K. Agrawal Juri Janovcik* Penerjemah: M Harmen Reza S* * MD (dokter) pada saat publikasi
Catatan: Gradien A-a yang terlalu tinggi menjadi indikasi adanya masalah dengan difusi udara antara alveolus & kapiler pulmoner " title="Gradien pO2Alveolus-arteri: Mengapa ada, dan mengapa penting
Singkatan kunci: • p02: tekanan parsial 02, atau "konten 02". • Pa02: tekanan parsial 02 di arteri. Diukur secara langsung via analisa gas darah (AGD) arteri. • PA02: tekanan parsial 02 di Alveolus. (Tidak dapat langsung diukur, harus melalui perhitungan).
Secara teori, pada kapiler paru yang bersebelahan dengan alveolus: 02 berdifusi dari alveolus menuju kapiler paru, dan tidak ada 02 yang hilang dari darah sampai darah mencapai arteri sistemik— maka harusnya Pa02 setara dengan PA02.
1
Tetapi dalam realitanya
Darah di dalam kapiler paru sejak awal tidak sepenuhnya teroksigenasi
Gravitasi menyebabkan lebih banyak darah menuju basis (dasar) paru, sehingga menyebabkan terlalu banyak darah untuk dapat sepenuhnya teroksigenasi oleh alveolus
Darah yang kurang teoksigenasi dari basis paru menurunkan keseluruhan p02 darah
Catatan: beberapa patologi respiratorik dapat memiliki gradien A-a normal (lihat slide terkait)
Legenda: Definisi
Penjelasan
Darah yang kurang teroksigenasi dari vena sistemik bercampur dengan darah yang teroksigenasi dari paru ("Venous admixture"):
Drainase vena dari sirkulasi bronkial bercampur dengan darah yang teroksigenasi pada kapiler paru
Beberapa vena pada sirkulasi koroner bermuara menuju atrium kiri, bukan menuju sinus koroner/atrium kanan
.111••••■•
Maka dari itu, konten 02 darah ketika mencapai arteri sistemik (Pa02) lebih rendah dibandingkan dengan konten 02 pada alveolus (PA02)
PA02 - Pa02 = "gradien" p02 antara alveolus dan arteri sistemik
Gradien A-a normal: <15 mmHg
Tanda/Gejala/Penunjang
Gradien A-a tinggi (>15 mmHg) selalu menjadi tanda patologis (lihat slide terkait)
Penulis: Yan Yu Penyunting: Steven Liu Amogh K. Agrawal Juri Janovcik* Penerjemah: M Harmen Reza S* * MD (dokter) pada saat publikasi
Catatan: Gradien A-a yang terlalu tinggi menjadi indikasi adanya masalah dengan difusi udara antara alveolus & kapiler pulmoner " />
15 mmHg) selalu menjadi tanda patologis (lihat slide terkait)
Penulis: Yan Yu Penyunting: Steven Liu Amogh K. Agrawal Juri Janovcik* Penerjemah: M Harmen Reza S* * MD (dokter) pada saat publikasi
Catatan: Gradien A-a yang terlalu tinggi menjadi indikasi adanya masalah dengan difusi udara antara alveolus & kapiler pulmoner " title="Gradien pO2Alveolus-arteri: Mengapa ada, dan mengapa penting
Singkatan kunci: • p02: tekanan parsial 02, atau "konten 02". • Pa02: tekanan parsial 02 di arteri. Diukur secara langsung via analisa gas darah (AGD) arteri. • PA02: tekanan parsial 02 di Alveolus. (Tidak dapat langsung diukur, harus melalui perhitungan).
Secara teori, pada kapiler paru yang bersebelahan dengan alveolus: 02 berdifusi dari alveolus menuju kapiler paru, dan tidak ada 02 yang hilang dari darah sampai darah mencapai arteri sistemik— maka harusnya Pa02 setara dengan PA02.
1
Tetapi dalam realitanya
Darah di dalam kapiler paru sejak awal tidak sepenuhnya teroksigenasi
Gravitasi menyebabkan lebih banyak darah menuju basis (dasar) paru, sehingga menyebabkan terlalu banyak darah untuk dapat sepenuhnya teroksigenasi oleh alveolus
Darah yang kurang teoksigenasi dari basis paru menurunkan keseluruhan p02 darah
Catatan: beberapa patologi respiratorik dapat memiliki gradien A-a normal (lihat slide terkait)
Legenda: Definisi
Penjelasan
Darah yang kurang teroksigenasi dari vena sistemik bercampur dengan darah yang teroksigenasi dari paru ("Venous admixture"):
Drainase vena dari sirkulasi bronkial bercampur dengan darah yang teroksigenasi pada kapiler paru
Beberapa vena pada sirkulasi koroner bermuara menuju atrium kiri, bukan menuju sinus koroner/atrium kanan
.111••••■•
Maka dari itu, konten 02 darah ketika mencapai arteri sistemik (Pa02) lebih rendah dibandingkan dengan konten 02 pada alveolus (PA02)
PA02 - Pa02 = "gradien" p02 antara alveolus dan arteri sistemik
Gradien A-a normal: <15 mmHg
Tanda/Gejala/Penunjang
Gradien A-a tinggi (>15 mmHg) selalu menjadi tanda patologis (lihat slide terkait)
Penulis: Yan Yu Penyunting: Steven Liu Amogh K. Agrawal Juri Janovcik* Penerjemah: M Harmen Reza S* * MD (dokter) pada saat publikasi
Catatan: Gradien A-a yang terlalu tinggi menjadi indikasi adanya masalah dengan difusi udara antara alveolus & kapiler pulmoner " />
Gradien pO2 Alveolus-arteri: Penjelasan rumus (Penjelasan ringkas)
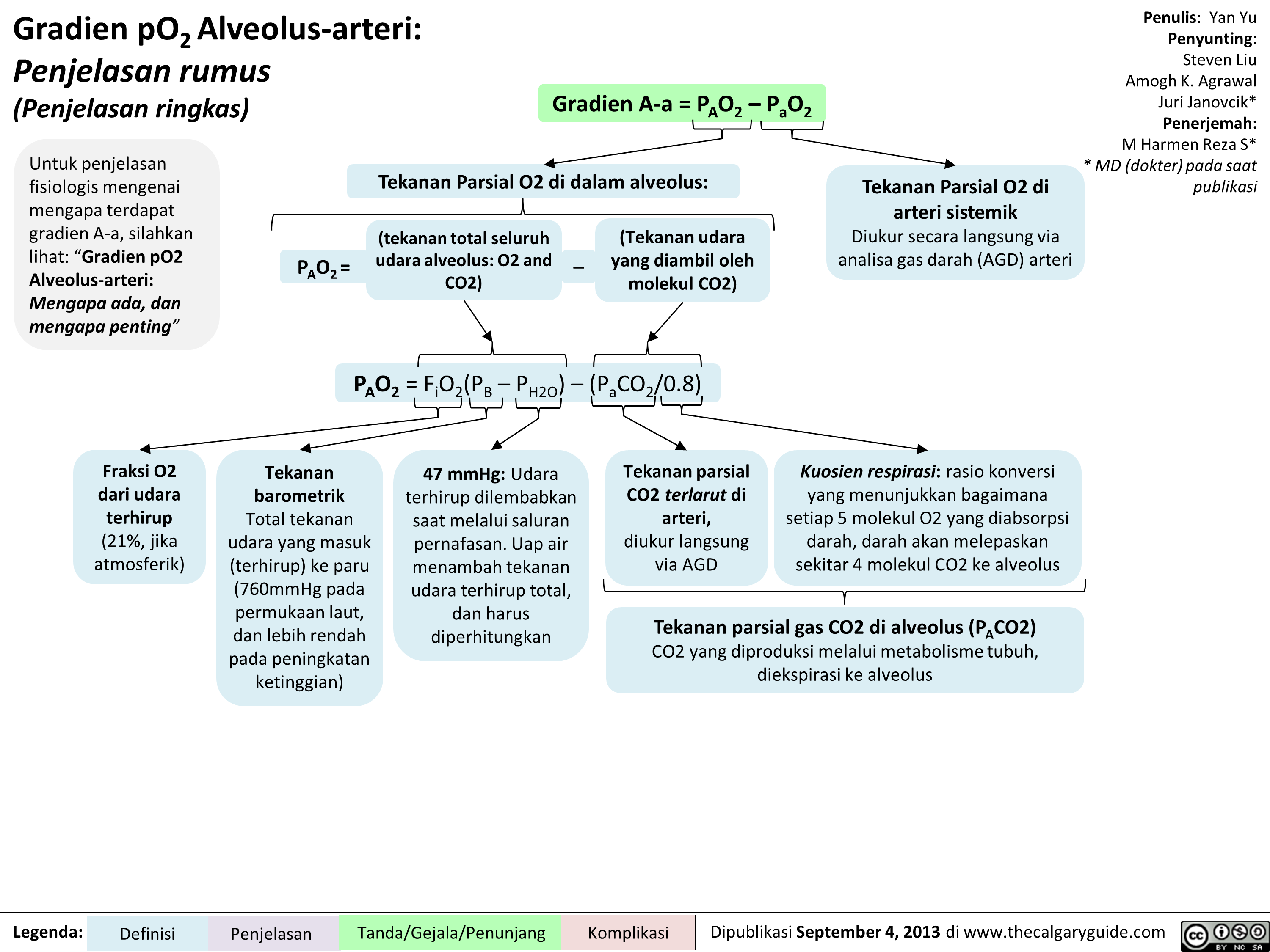
Gradien pO2 Alveolus-arteri: Penjelasan rumus (Penjelasan secara ilmiah)
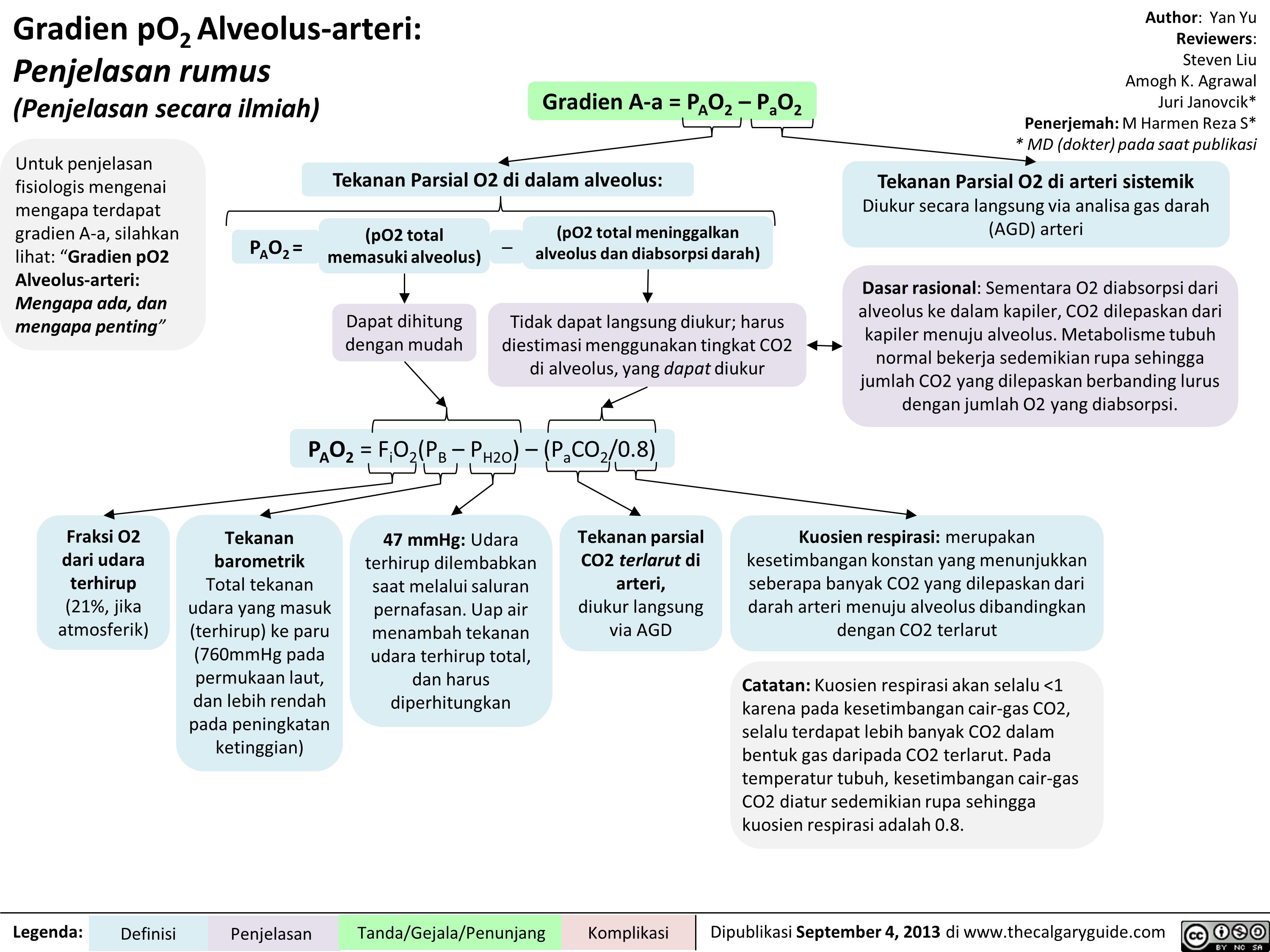
Acetylcholinesterase Inhibitors
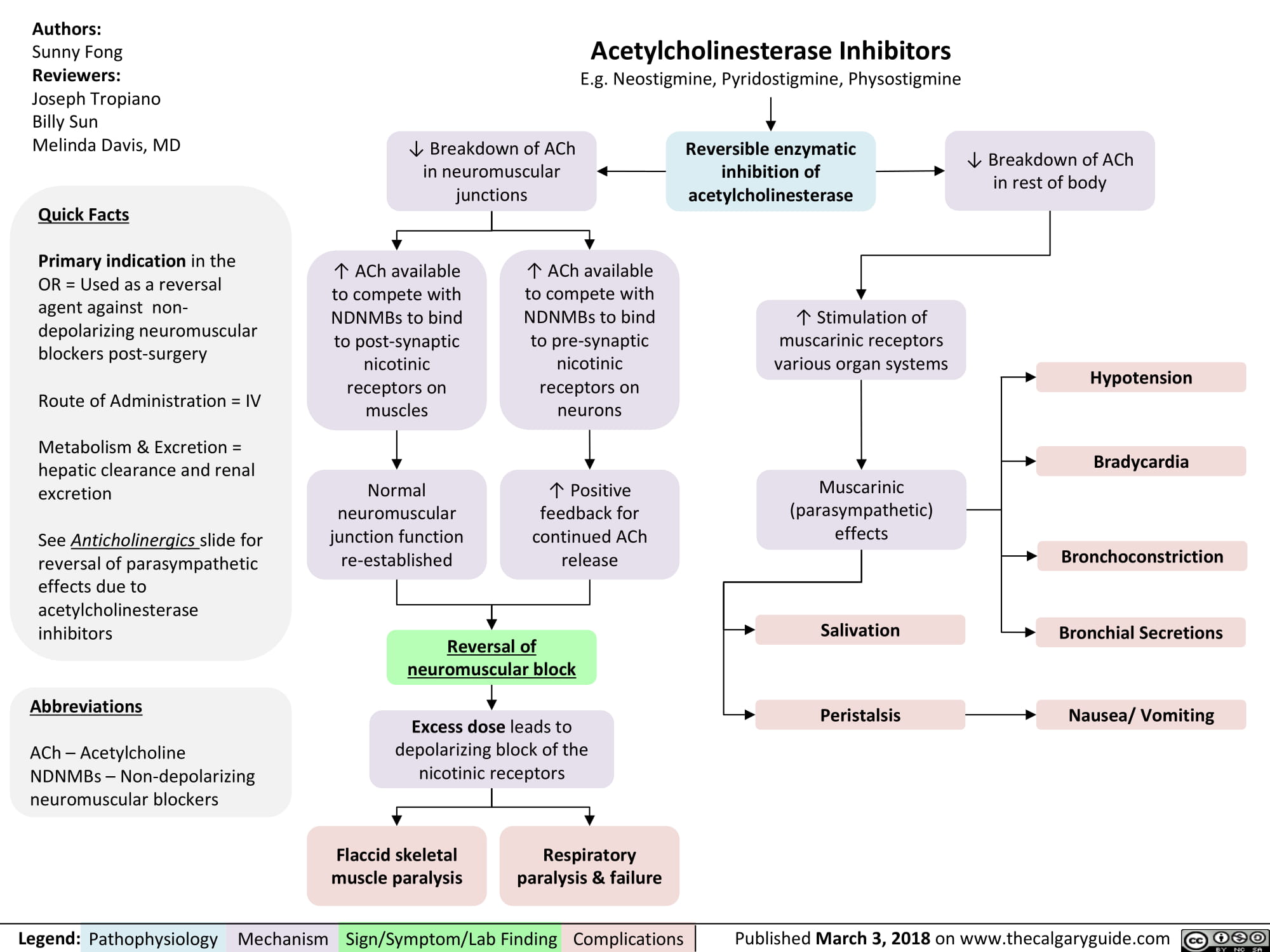
Anticholinergics
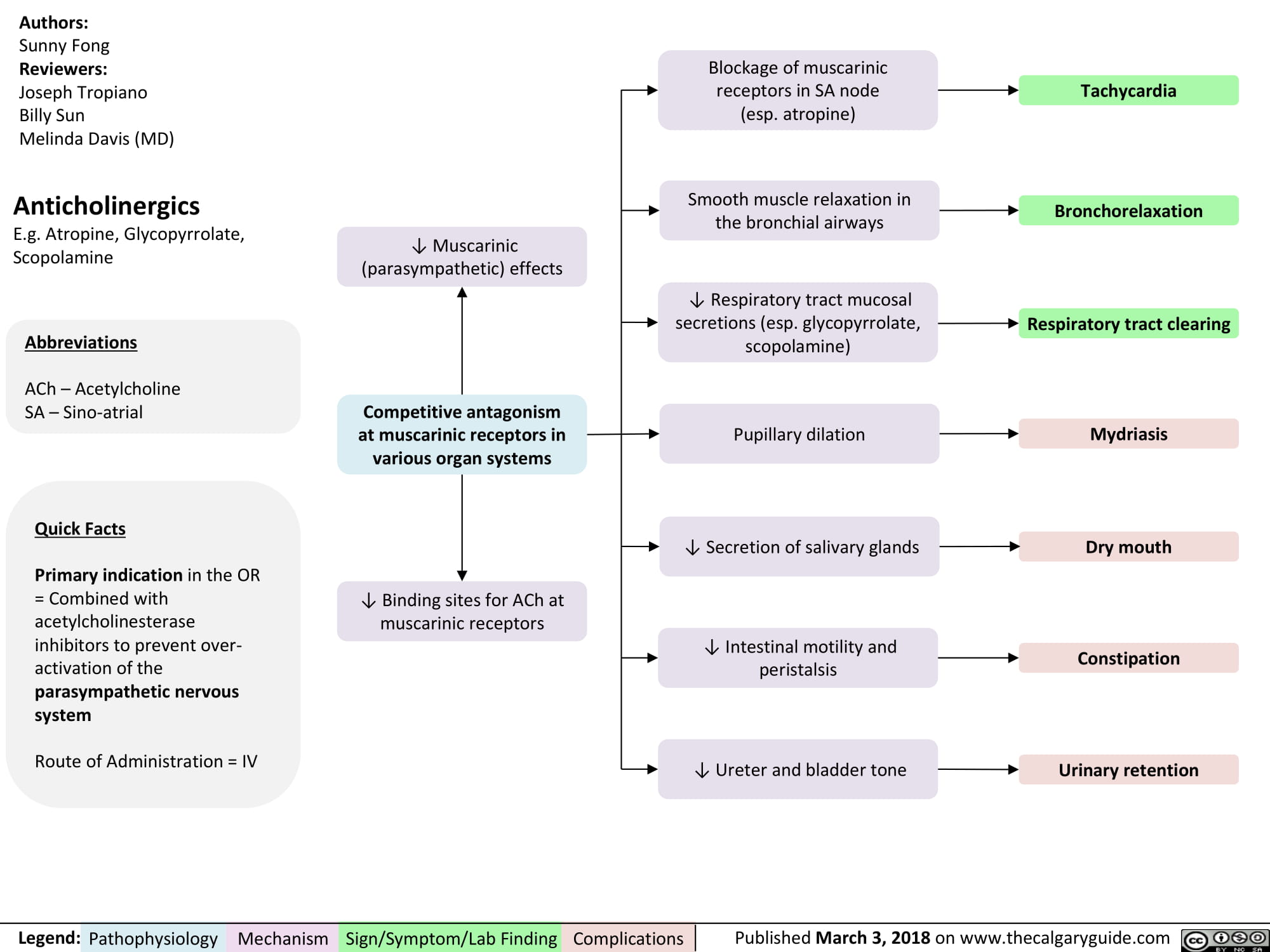
non-depolarizing-neuromuscular-blocks-ndnmbs
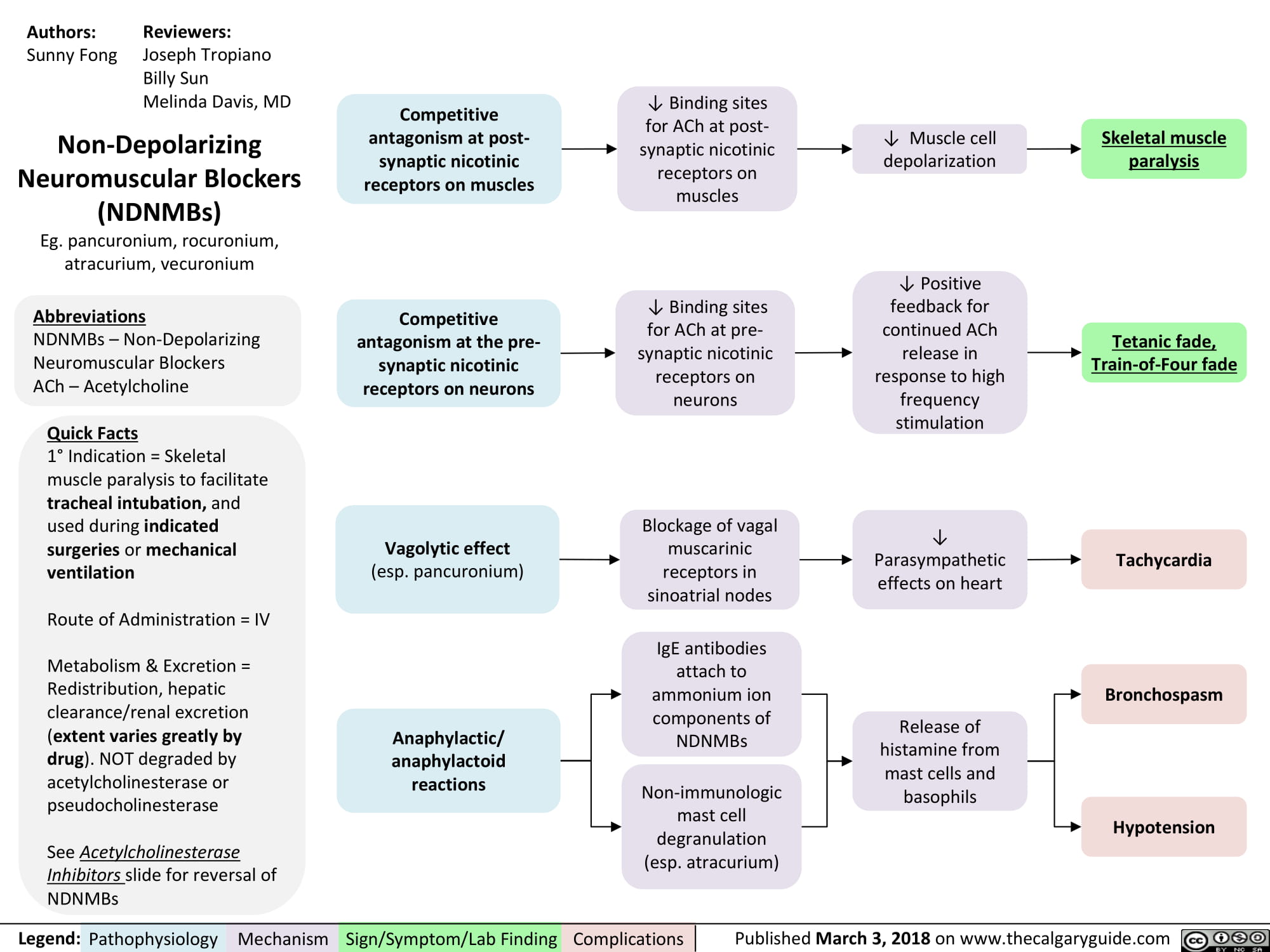
Propofol
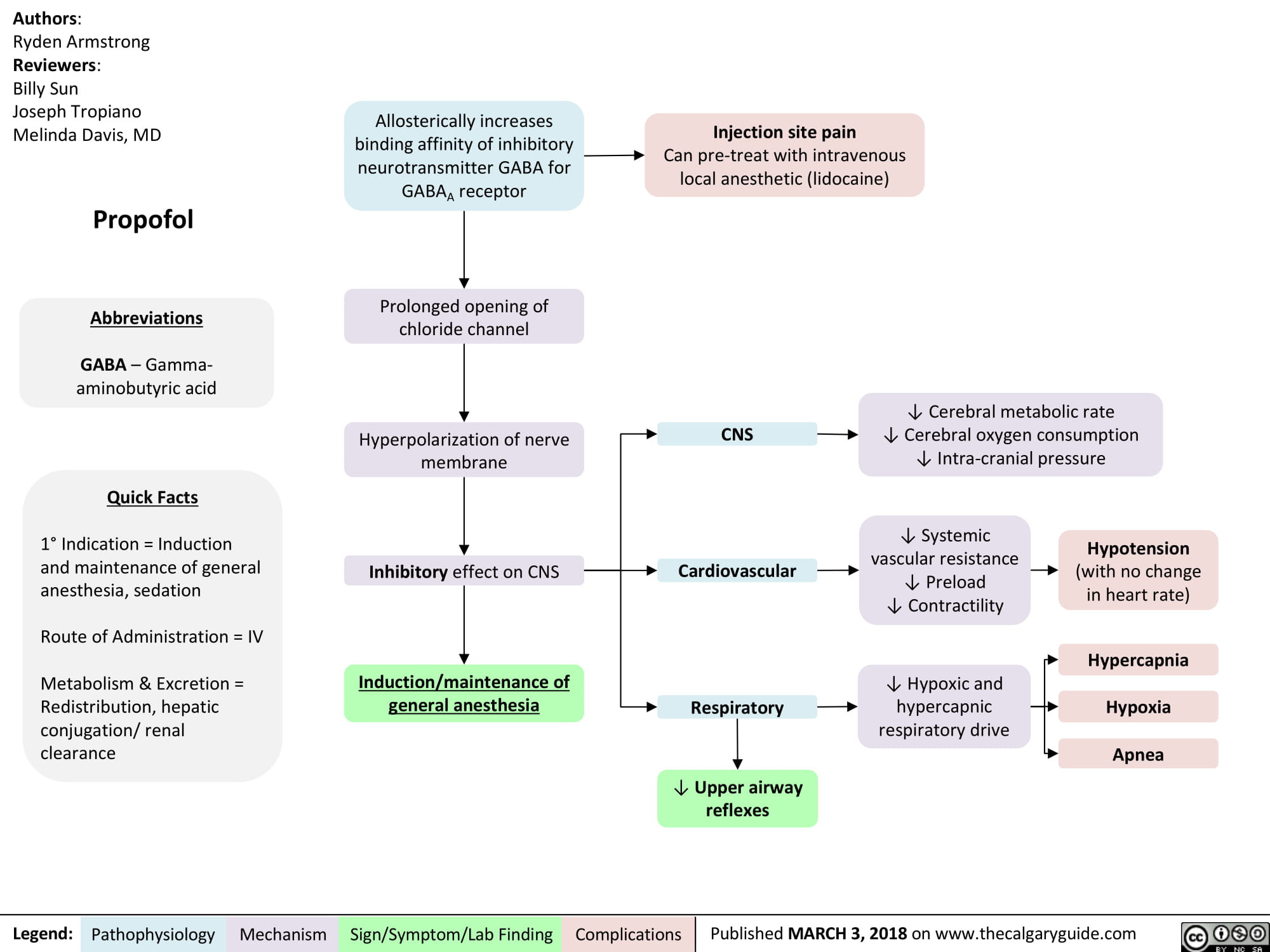
Succinylcholine
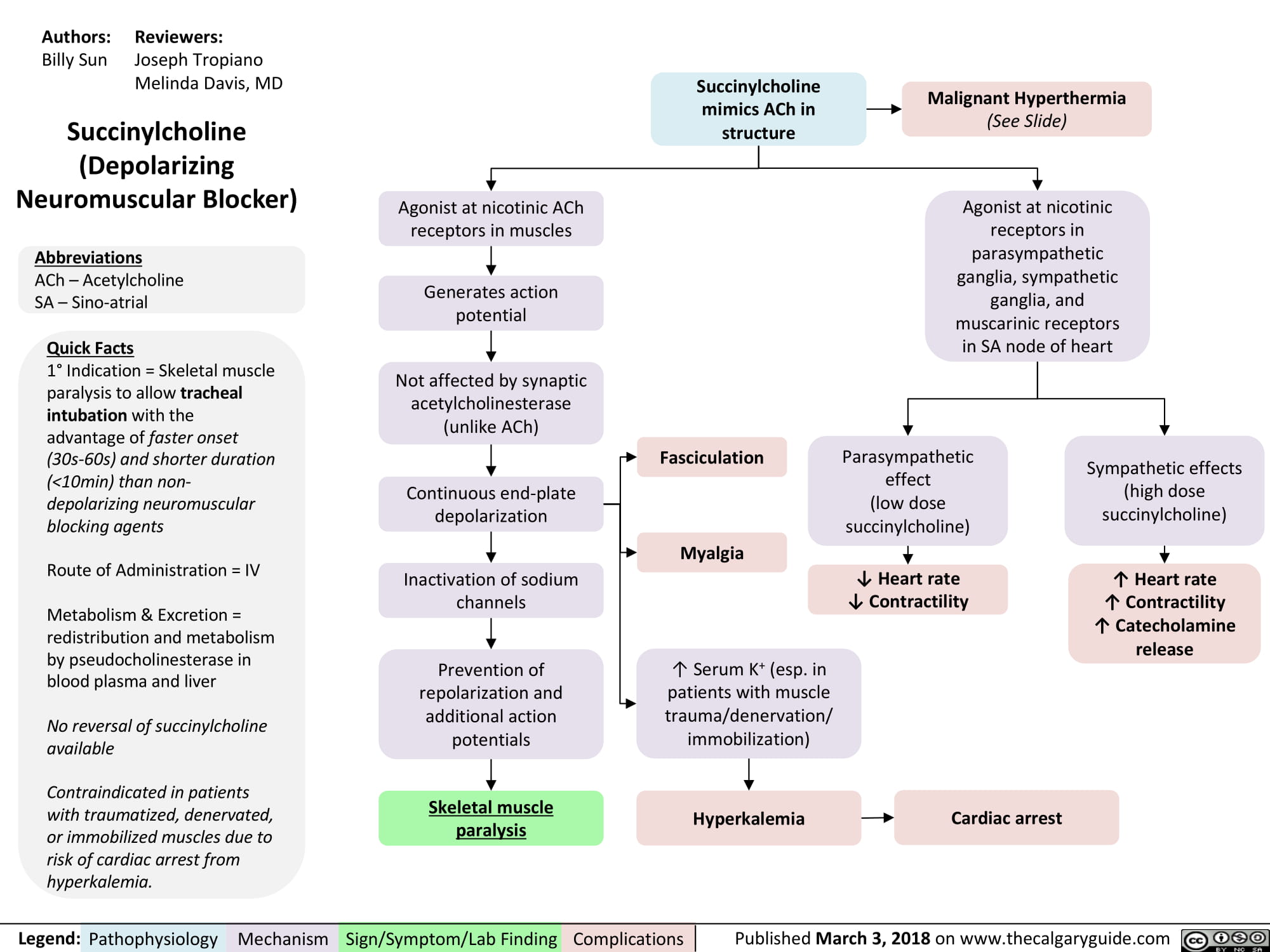
Volatile Gases
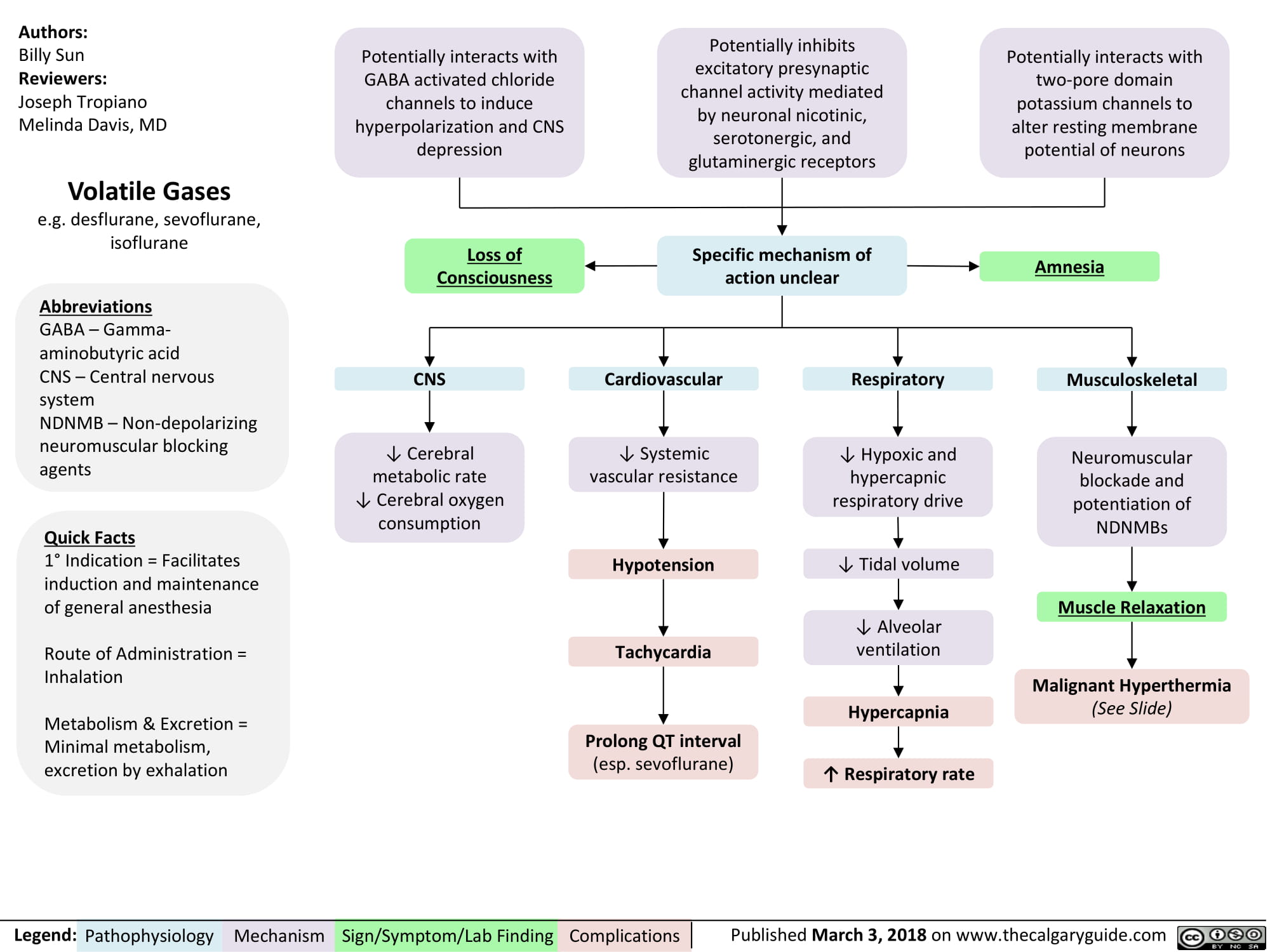
non-depolarizing-neuromuscular-blocks-ndnmbs
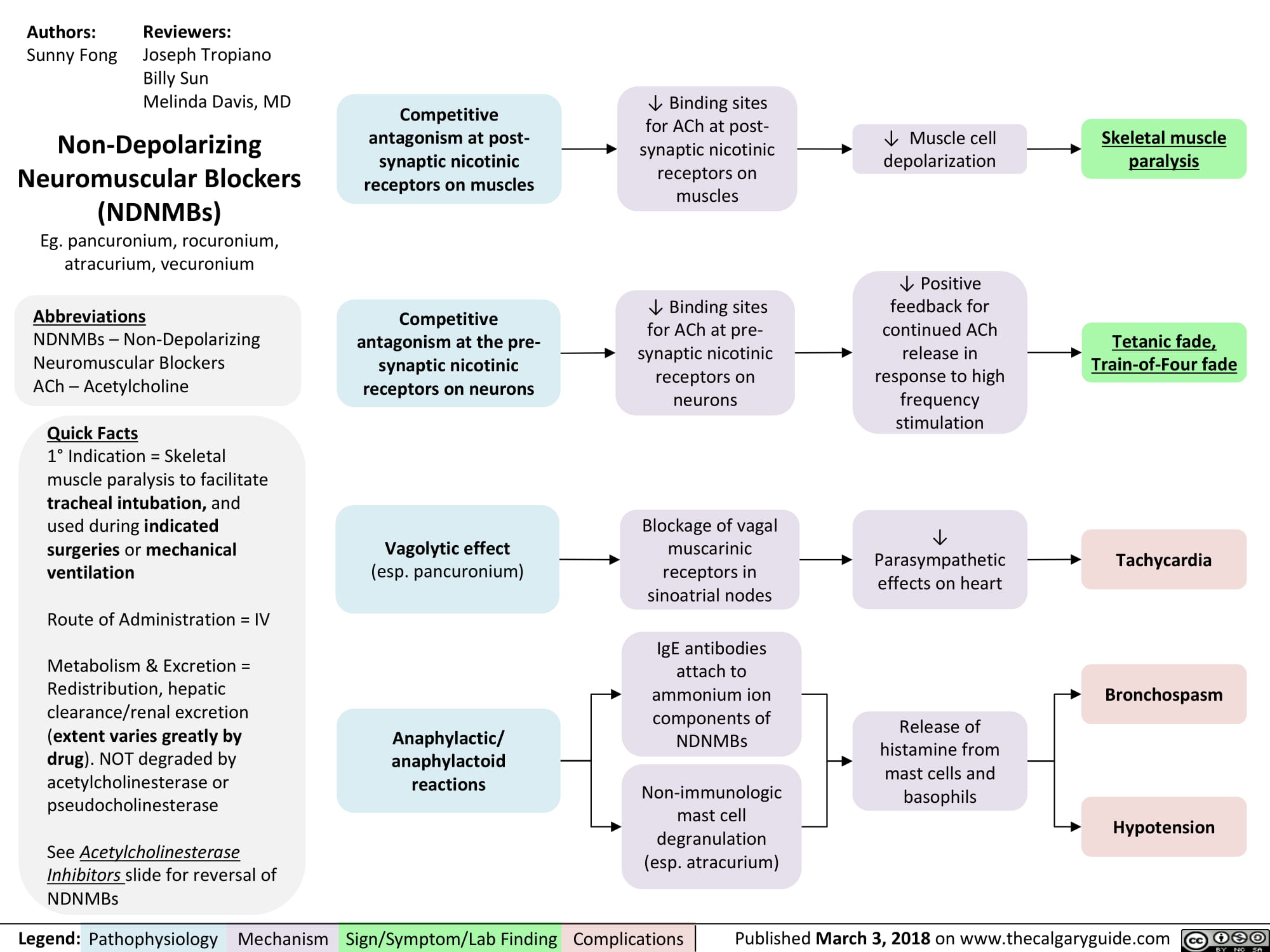
Succinylcholine
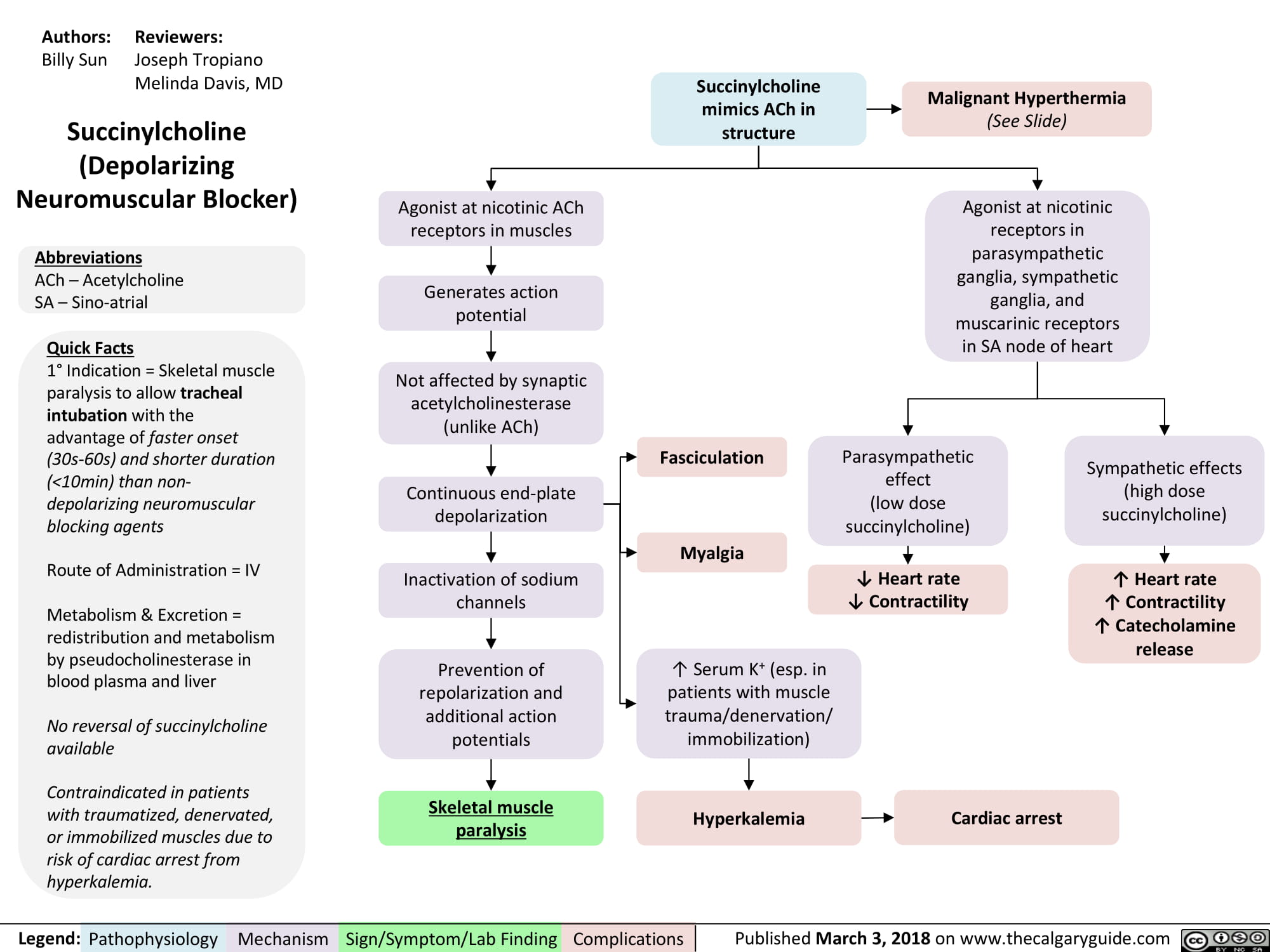
Clavicular Fracture: Pathogenesis and clinical findings
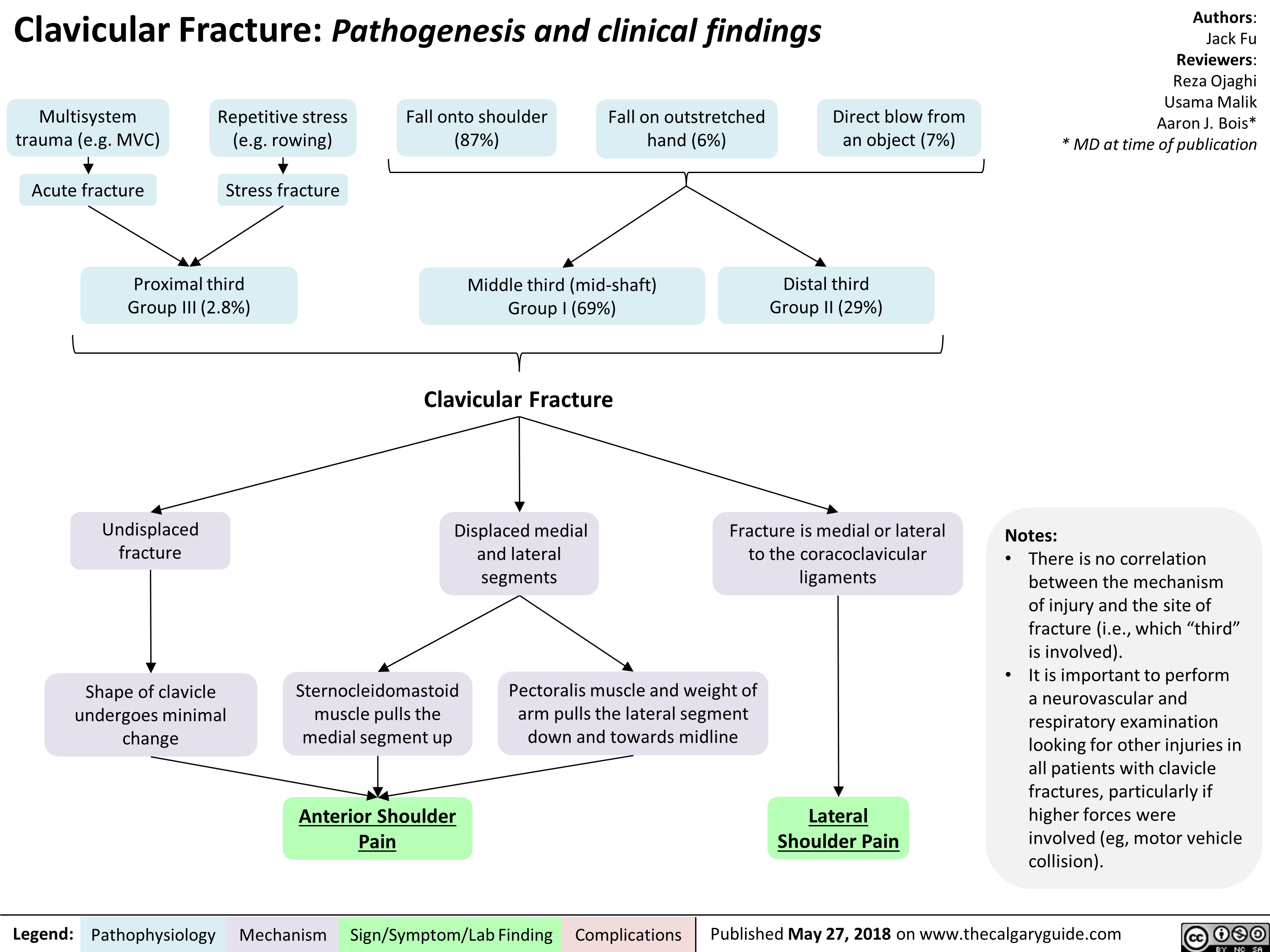
Pediatric Pneumonia: Pathogenesis and clinical findings

Radiological findings of child abuse
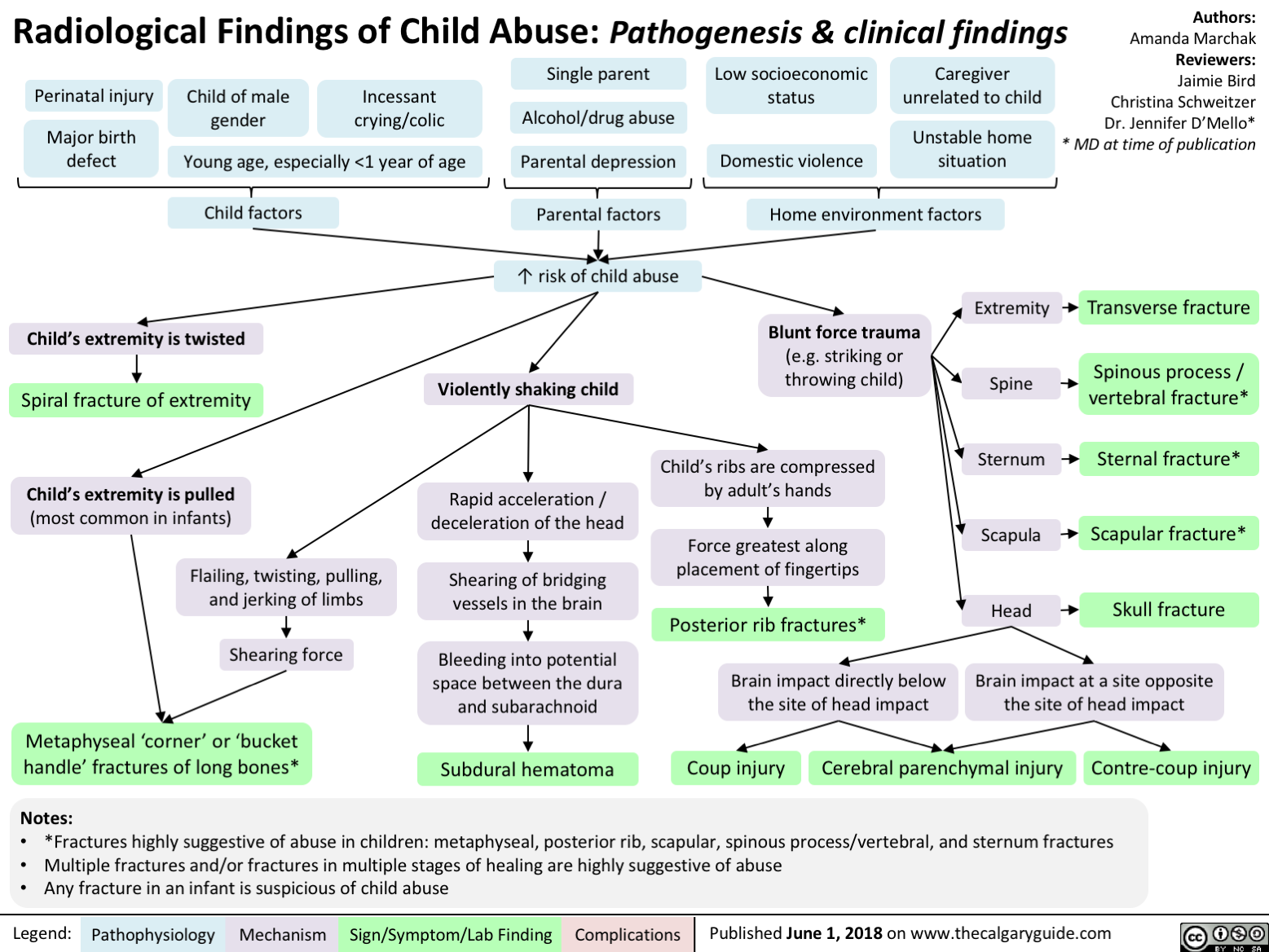
Non-Accidental Head Trauma
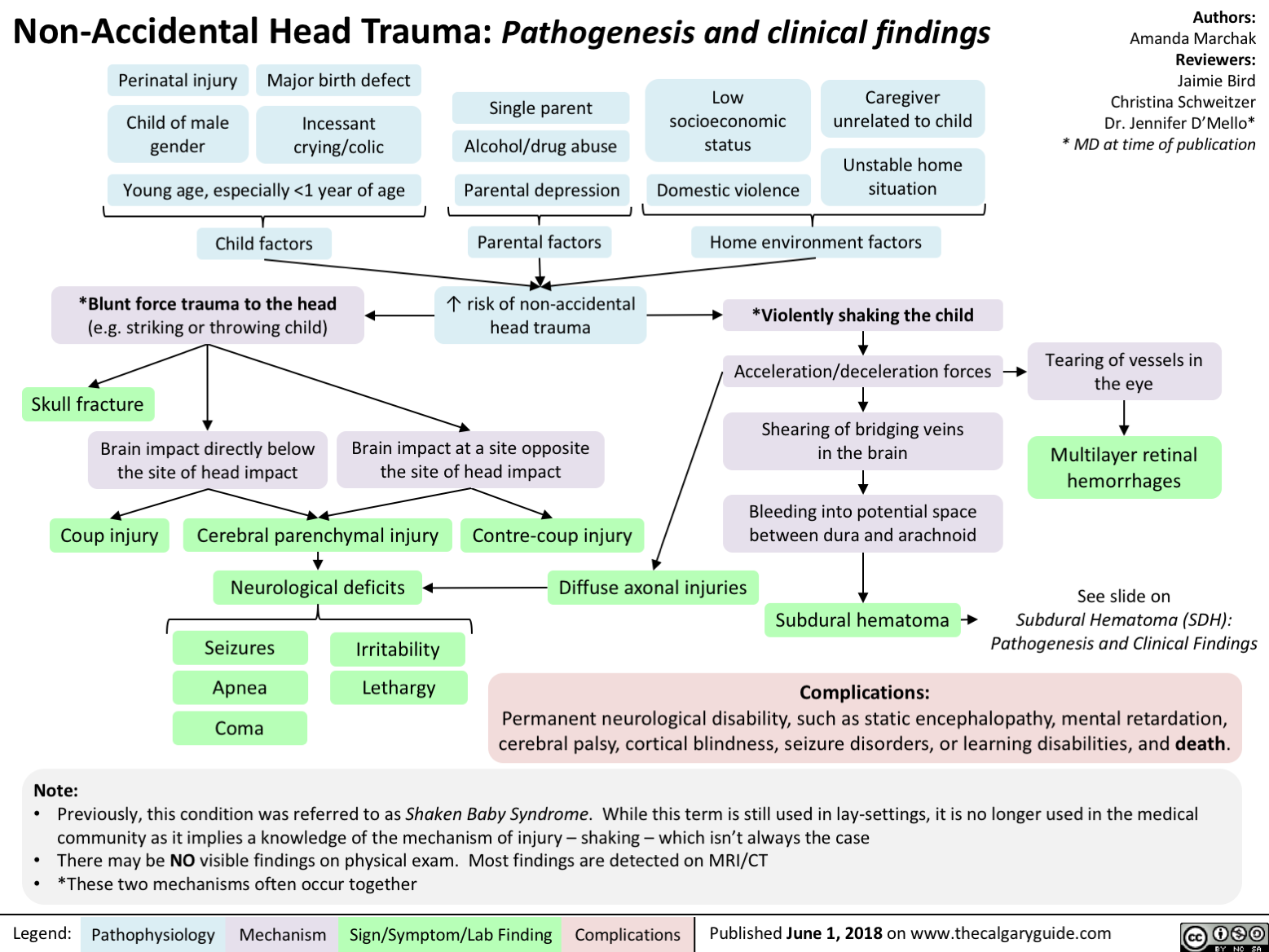
Duchenne Muscular Dystrophy
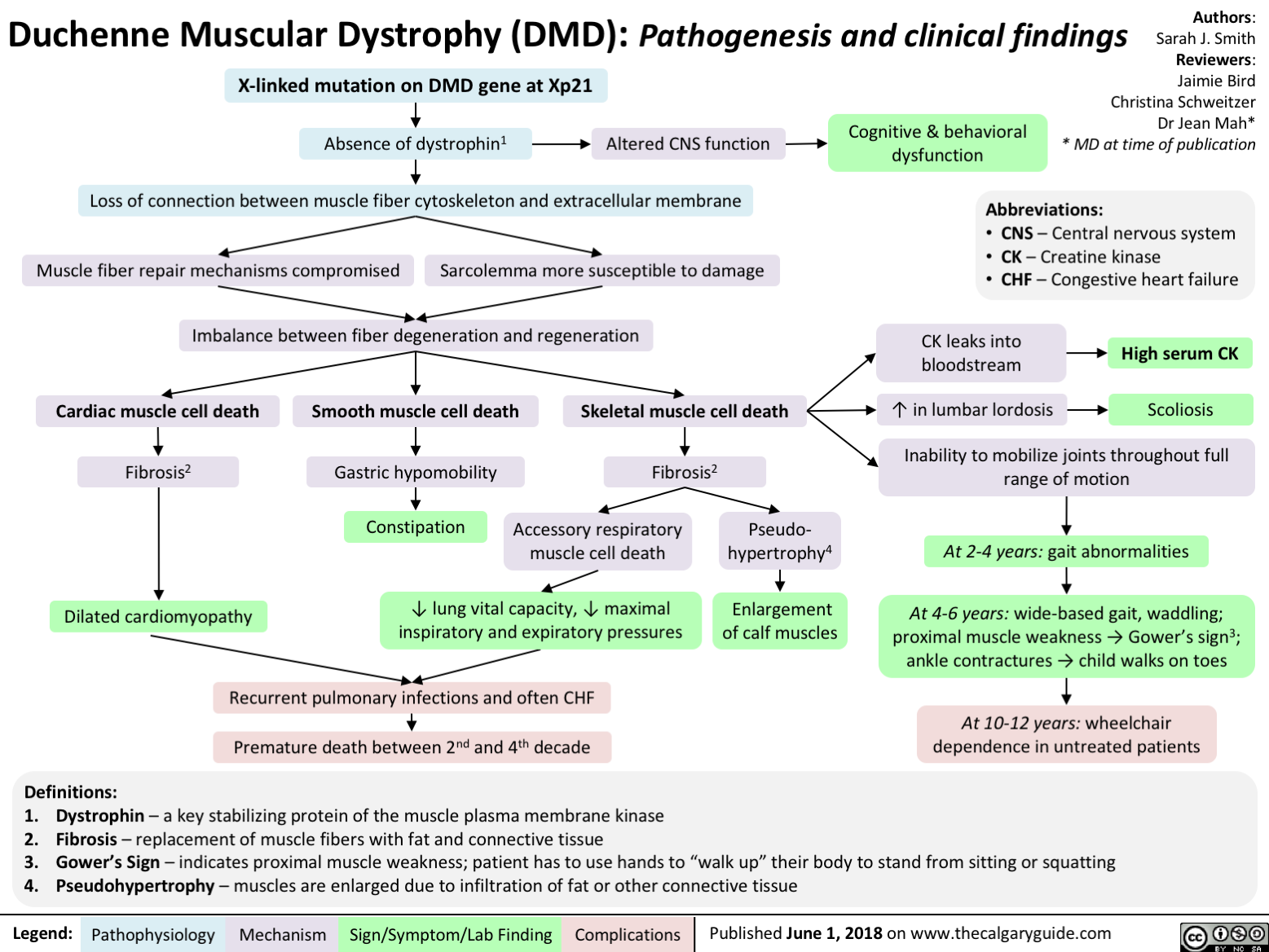
Acquired Inguinal Hernias: Indirect + Direct
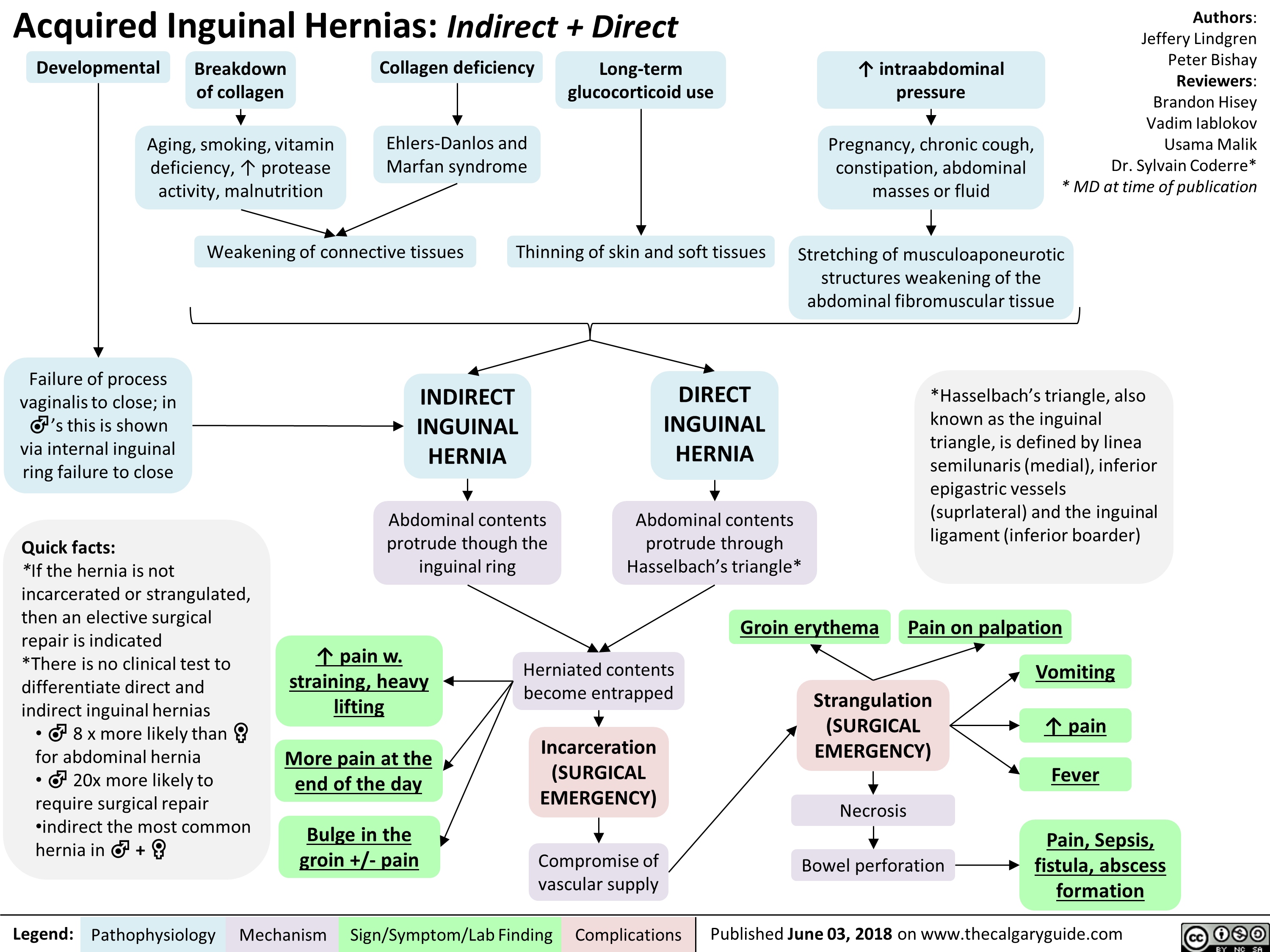
Celiac Disease: Pathogenesis and clinical findings
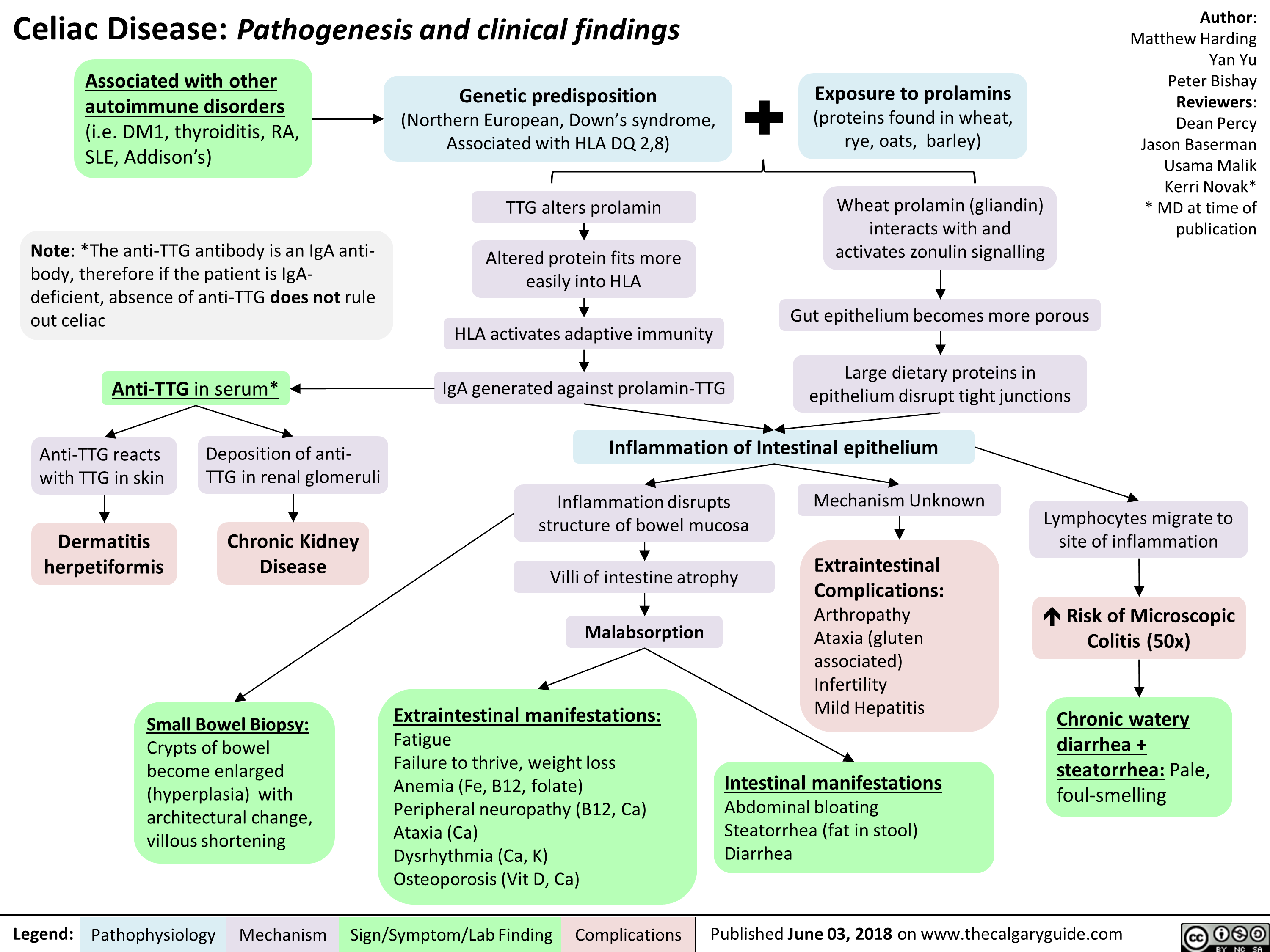
Celiac Disease: Complications
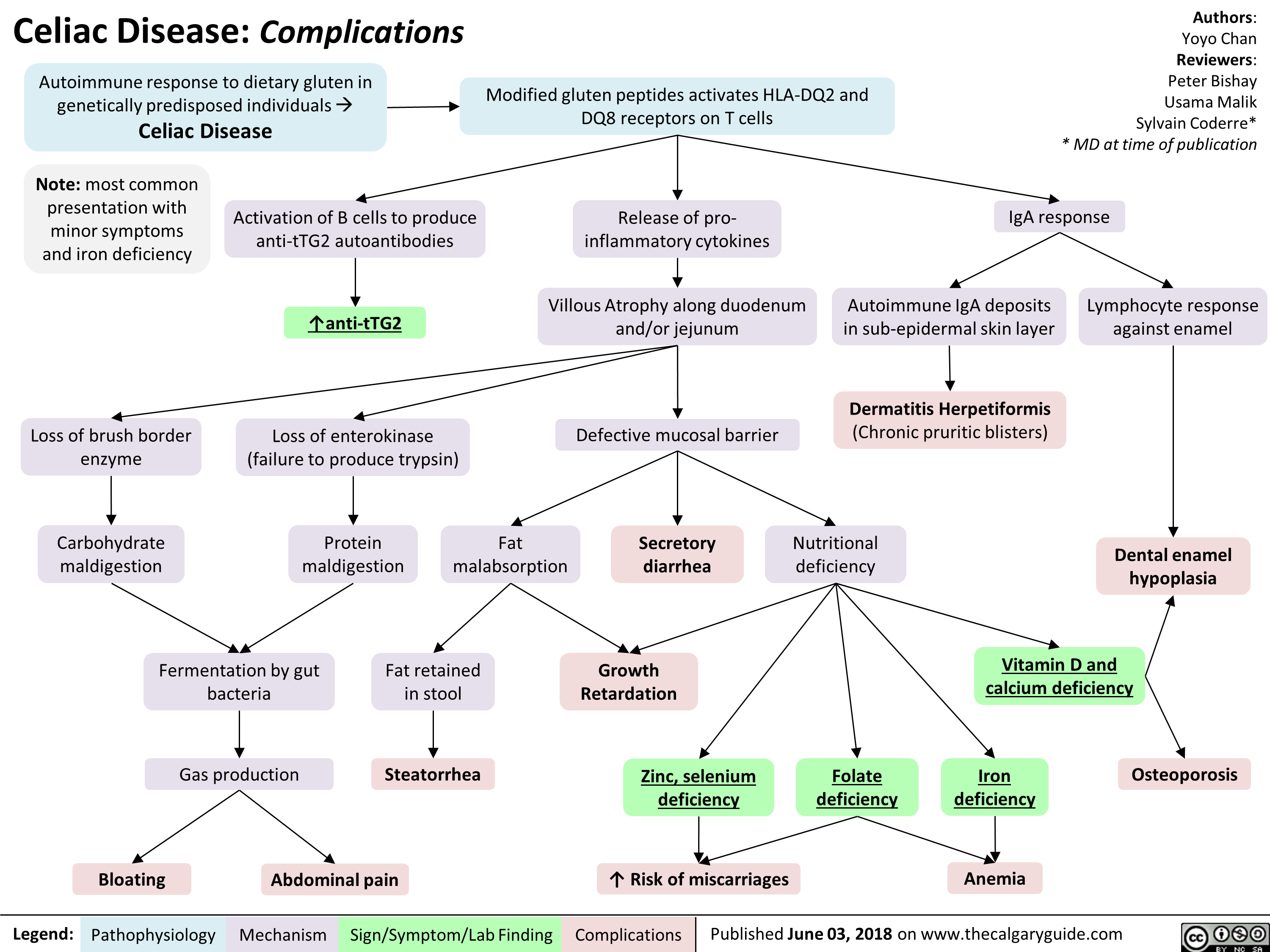
Orofacial Clefts cleft lip cleft palate
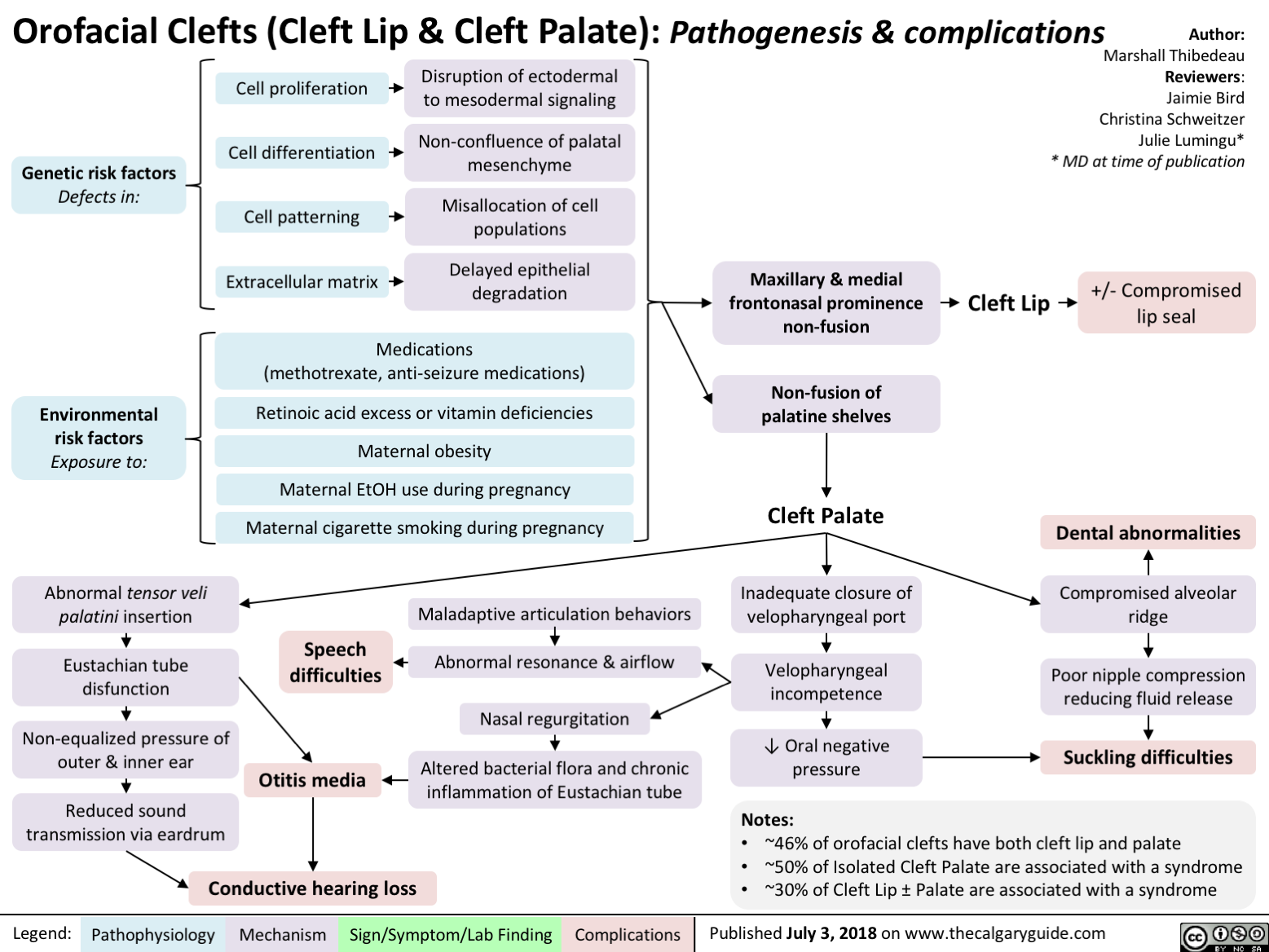
Cerebral Palsy clinical findings
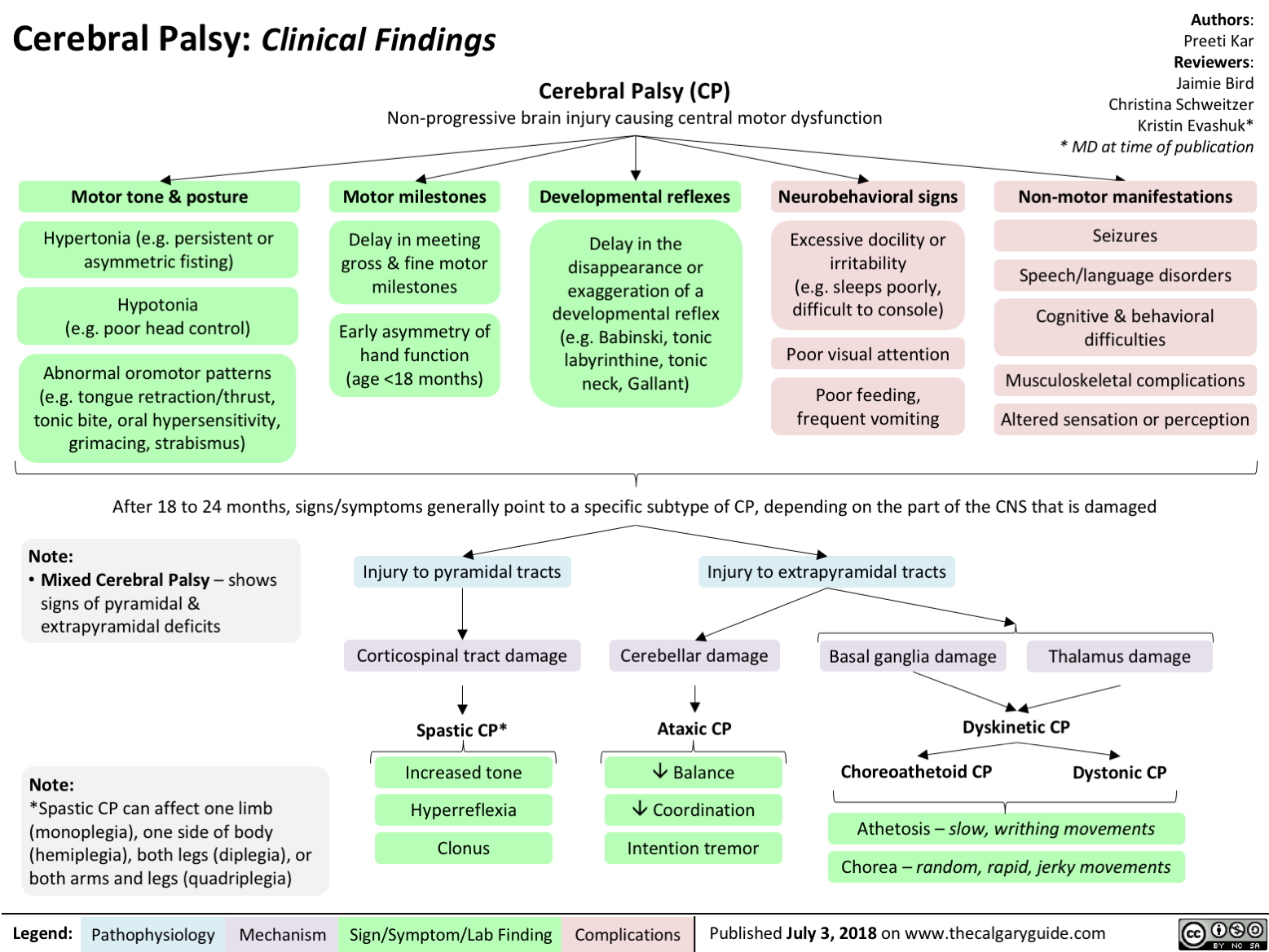
Developmental Coordination Disorder
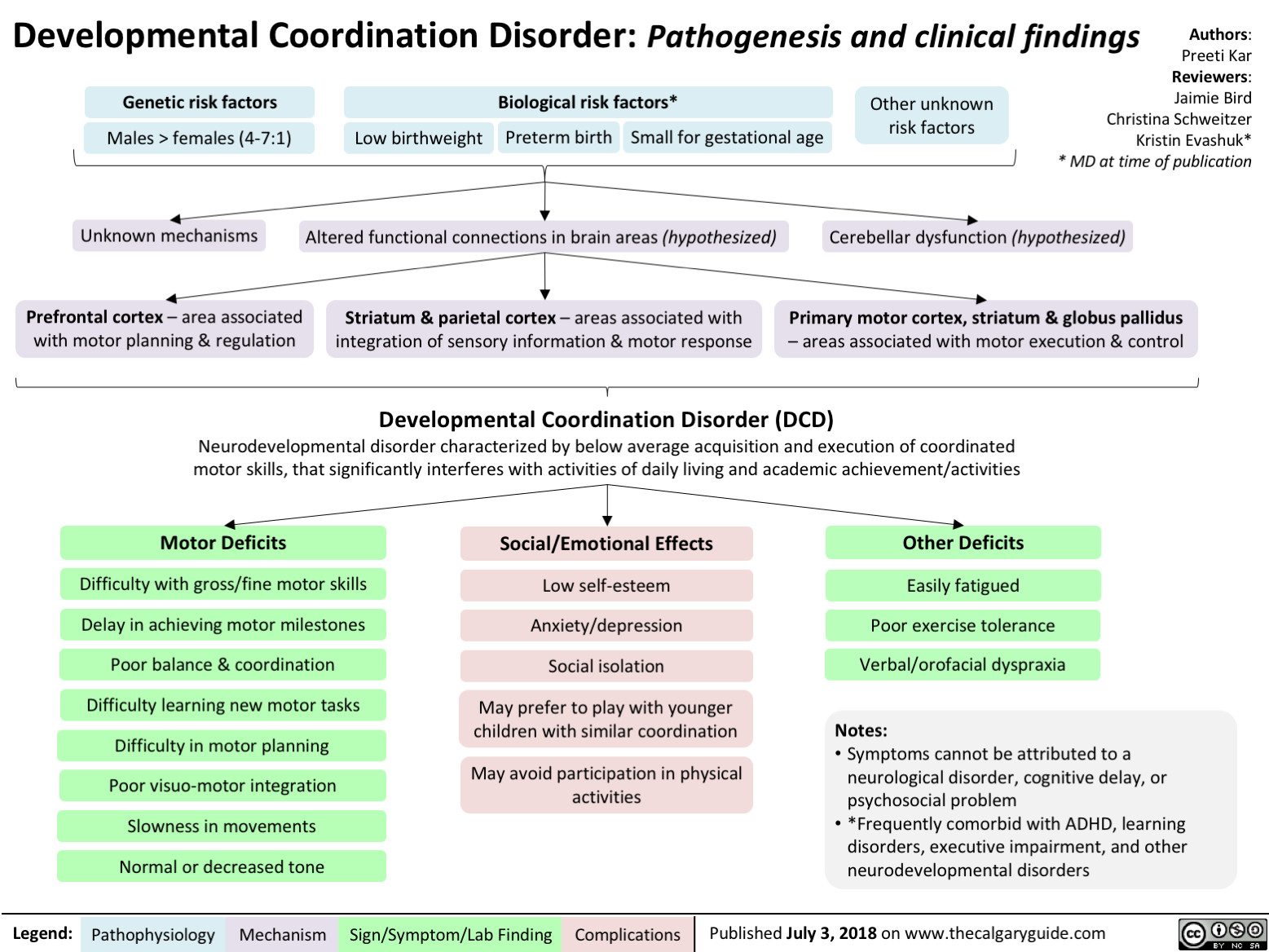
Sudden Infant Death Syndrome SIDS Triple Risk Model

Aplastic Anemia: Pathogenesis and Clinical Findings
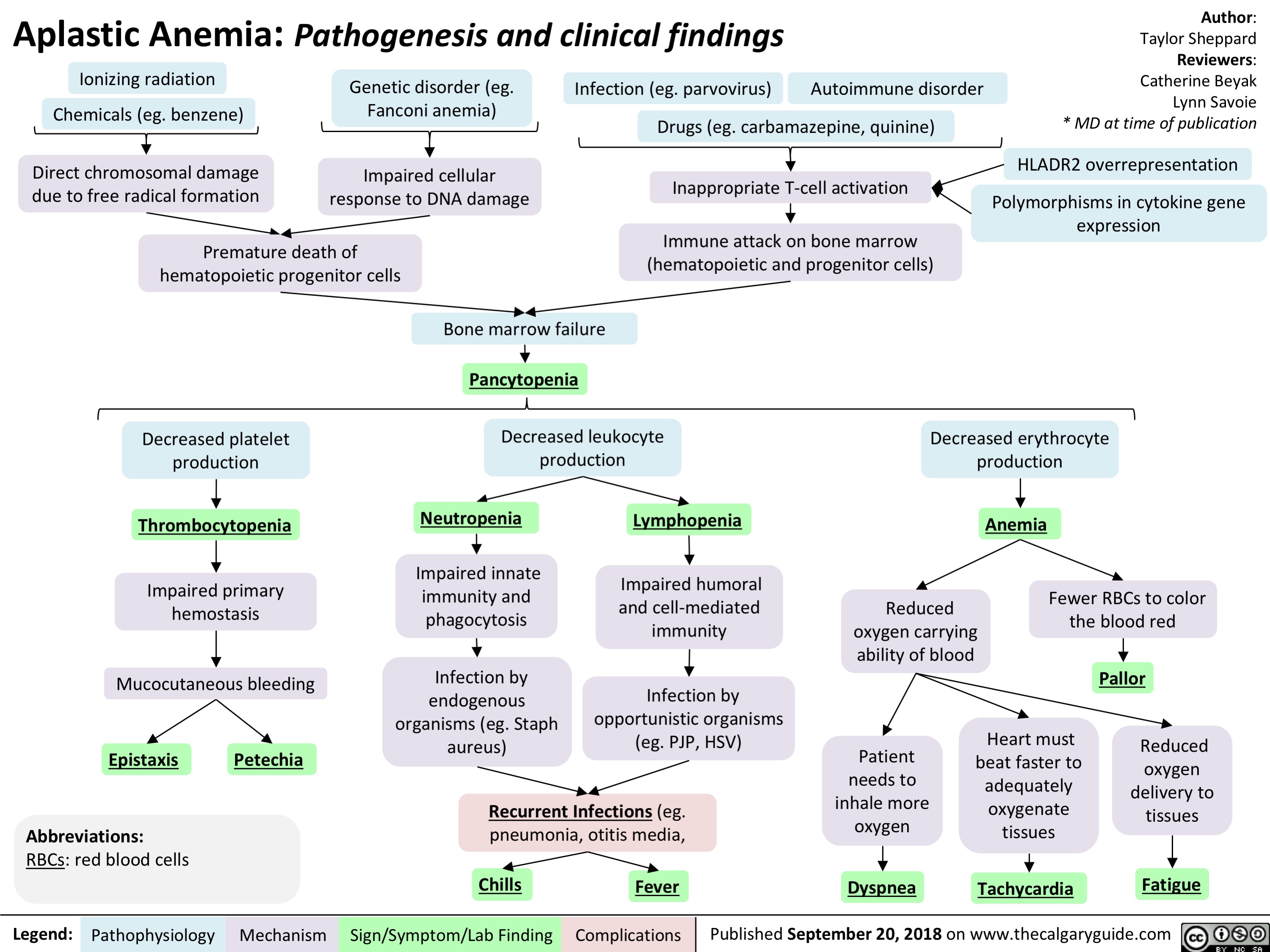
Feedback Loops Growth Hormone
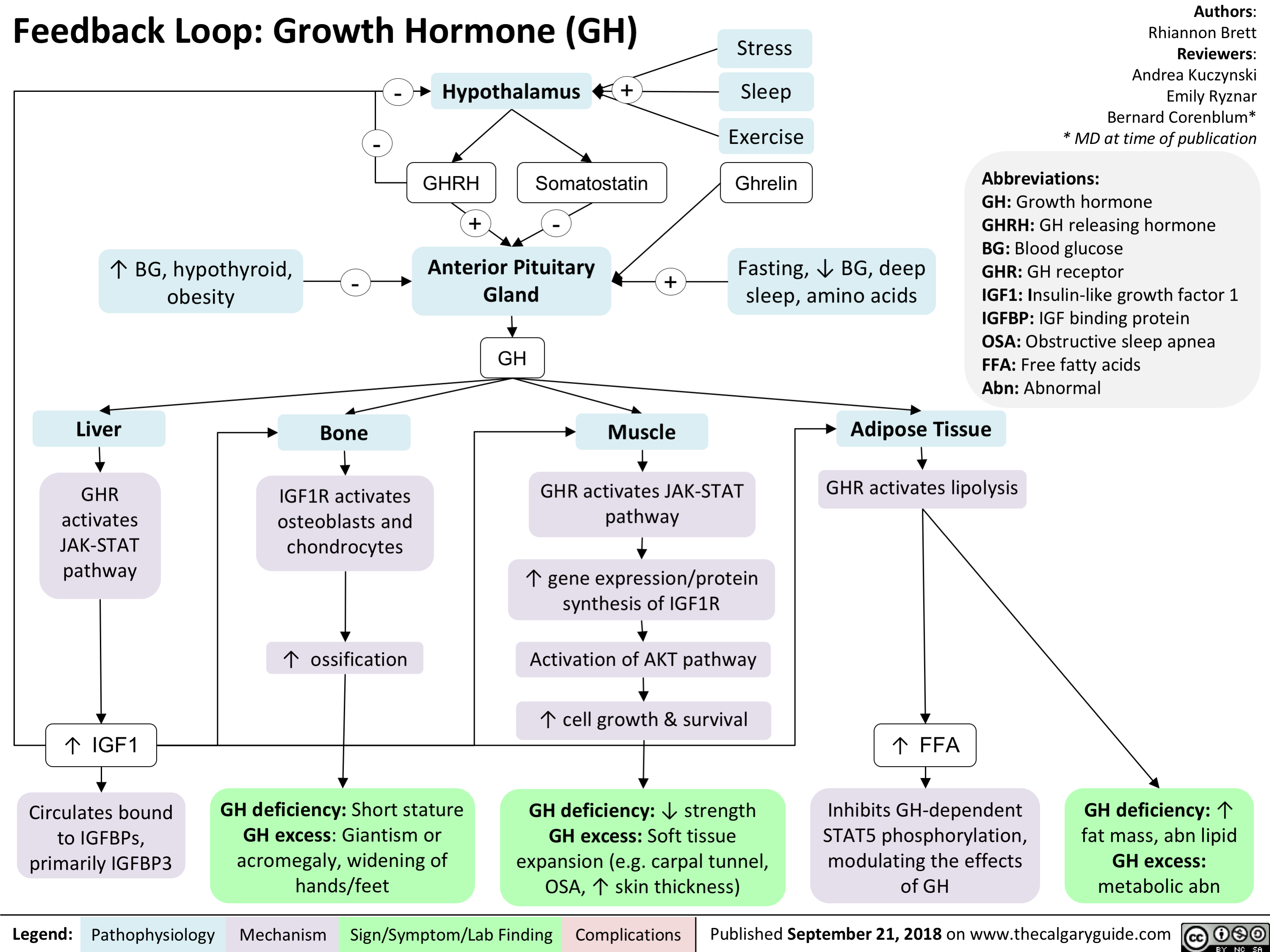
Kallmann Syndrome and Normosmotic Idiopathic Hypogonadotropism: Pathogenesis and Clinical Findings
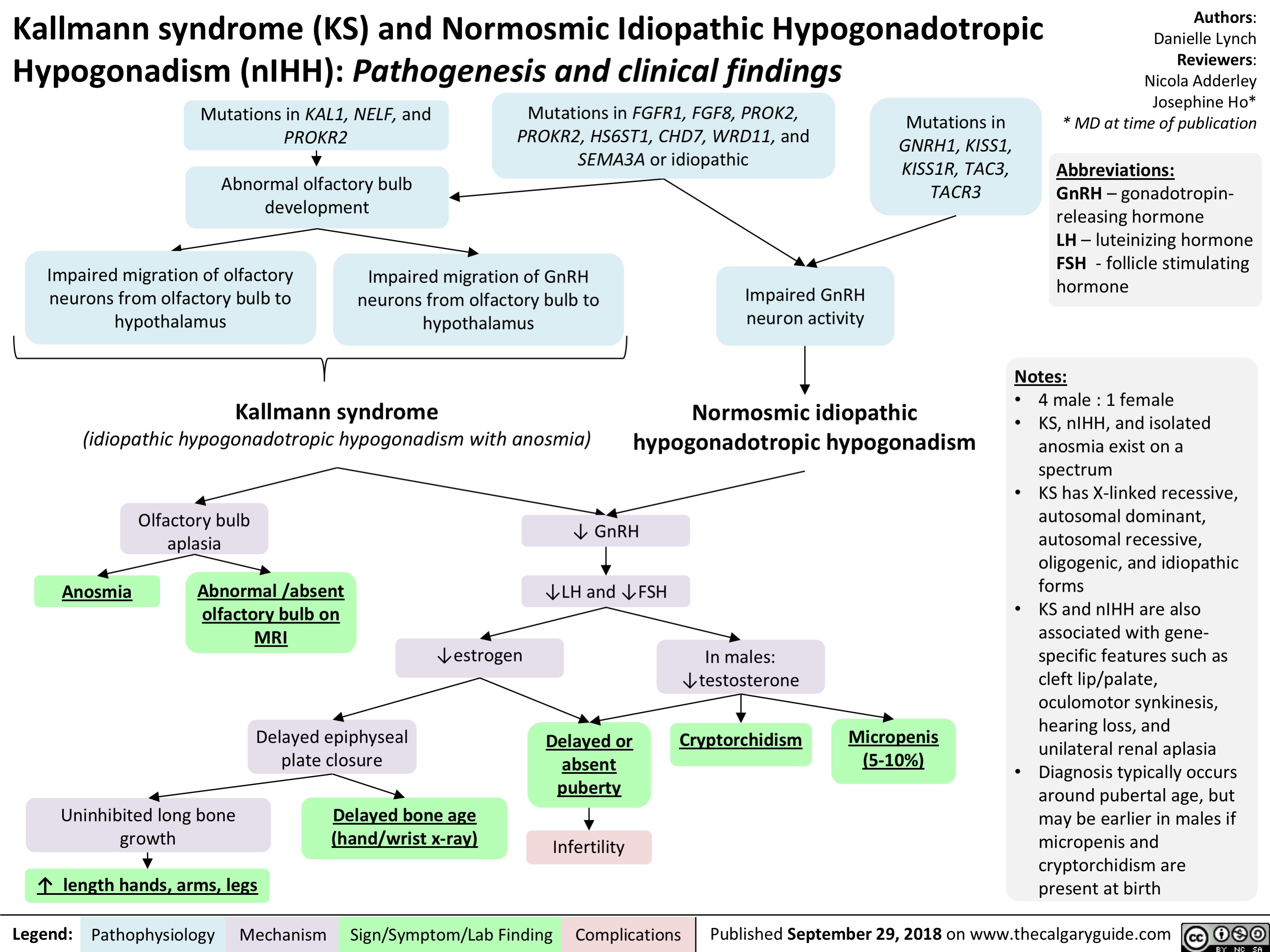
Posterior Cruciate Ligament (PCL) Injury Pathogenesis and Clinical Findings
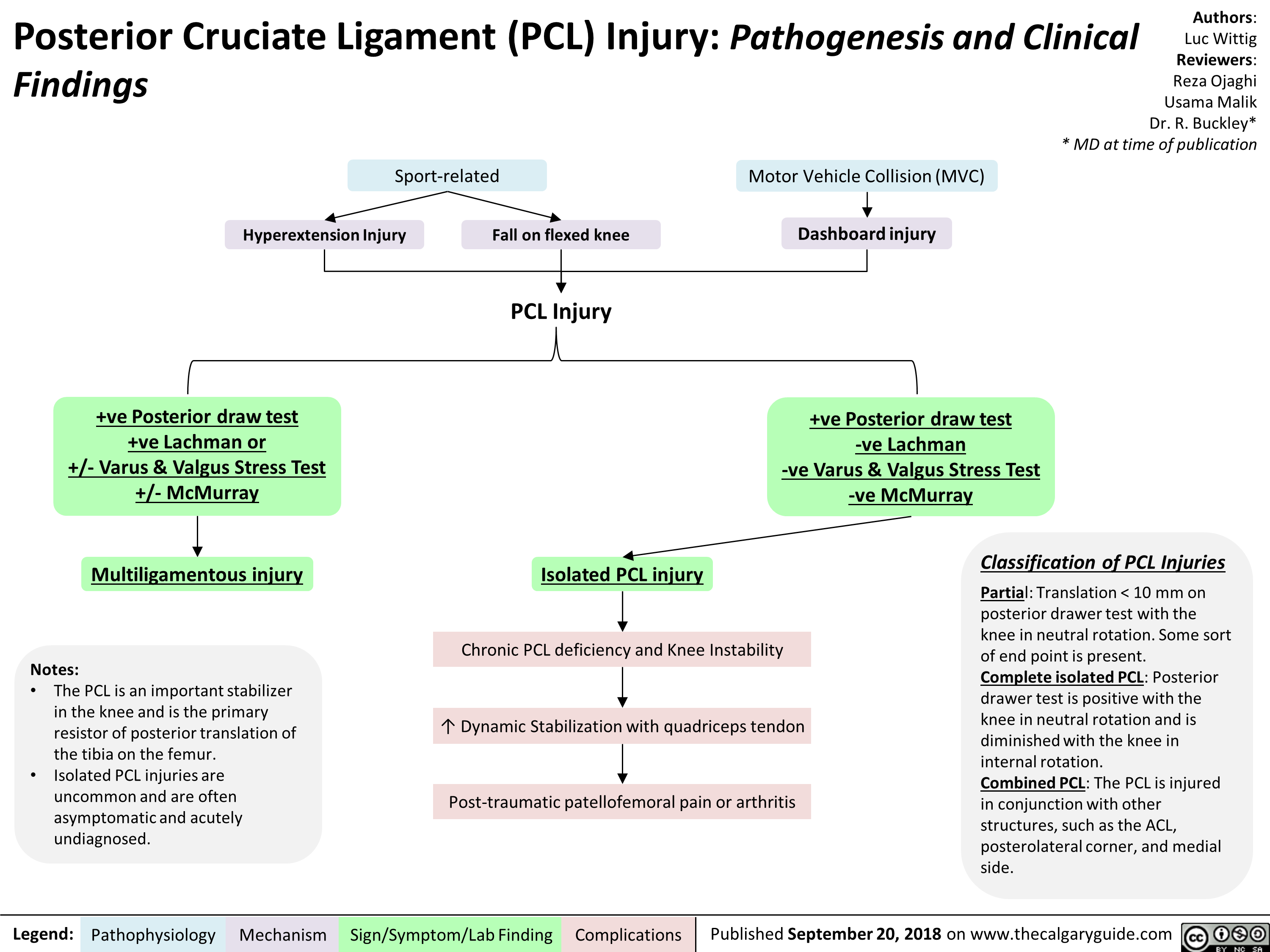
Feedback Loop: Adrenocorticotropic Hormone (ACTH)
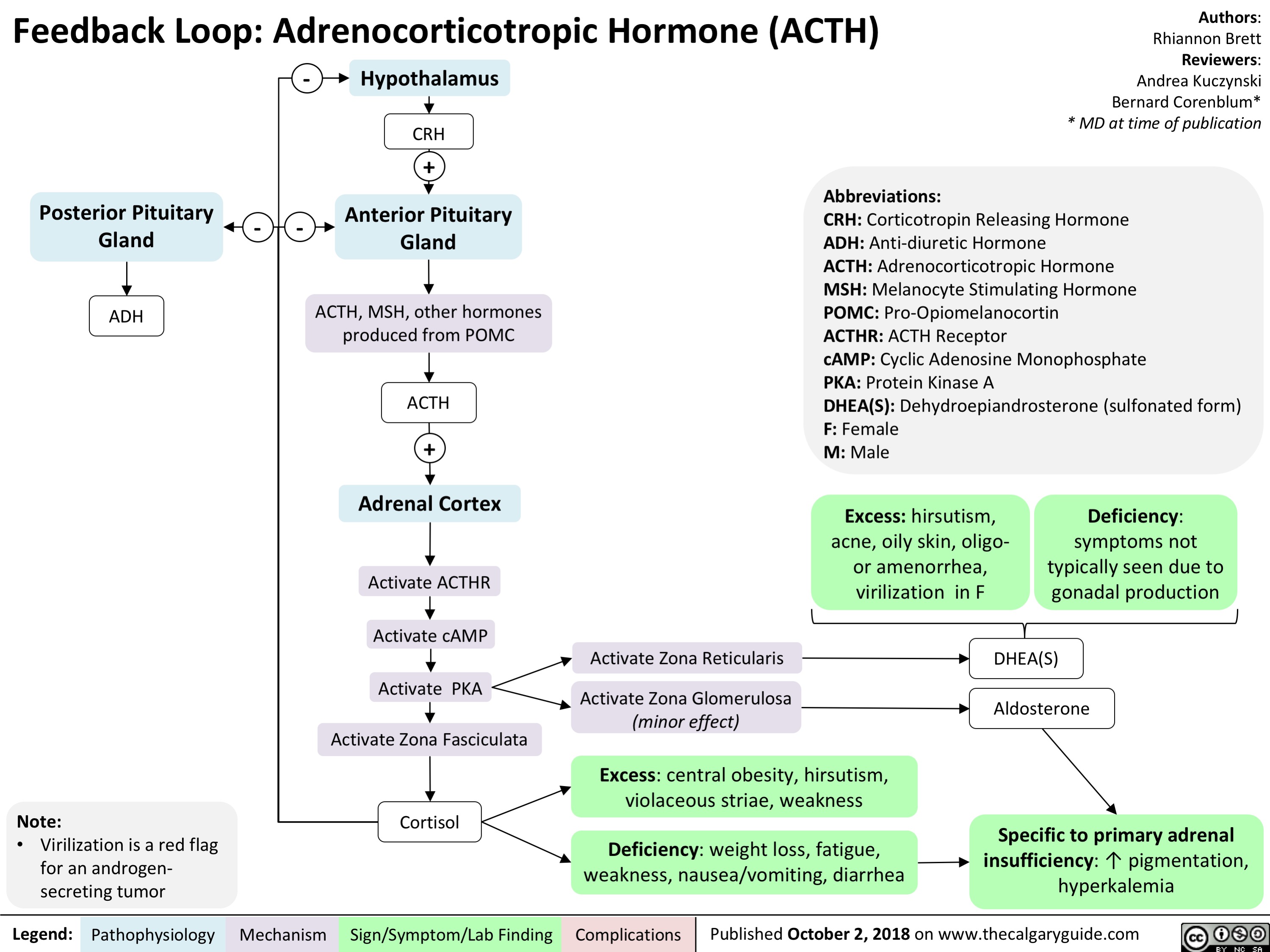
Feedback Loop- Thyroid Stimulating Hormone (TSH)
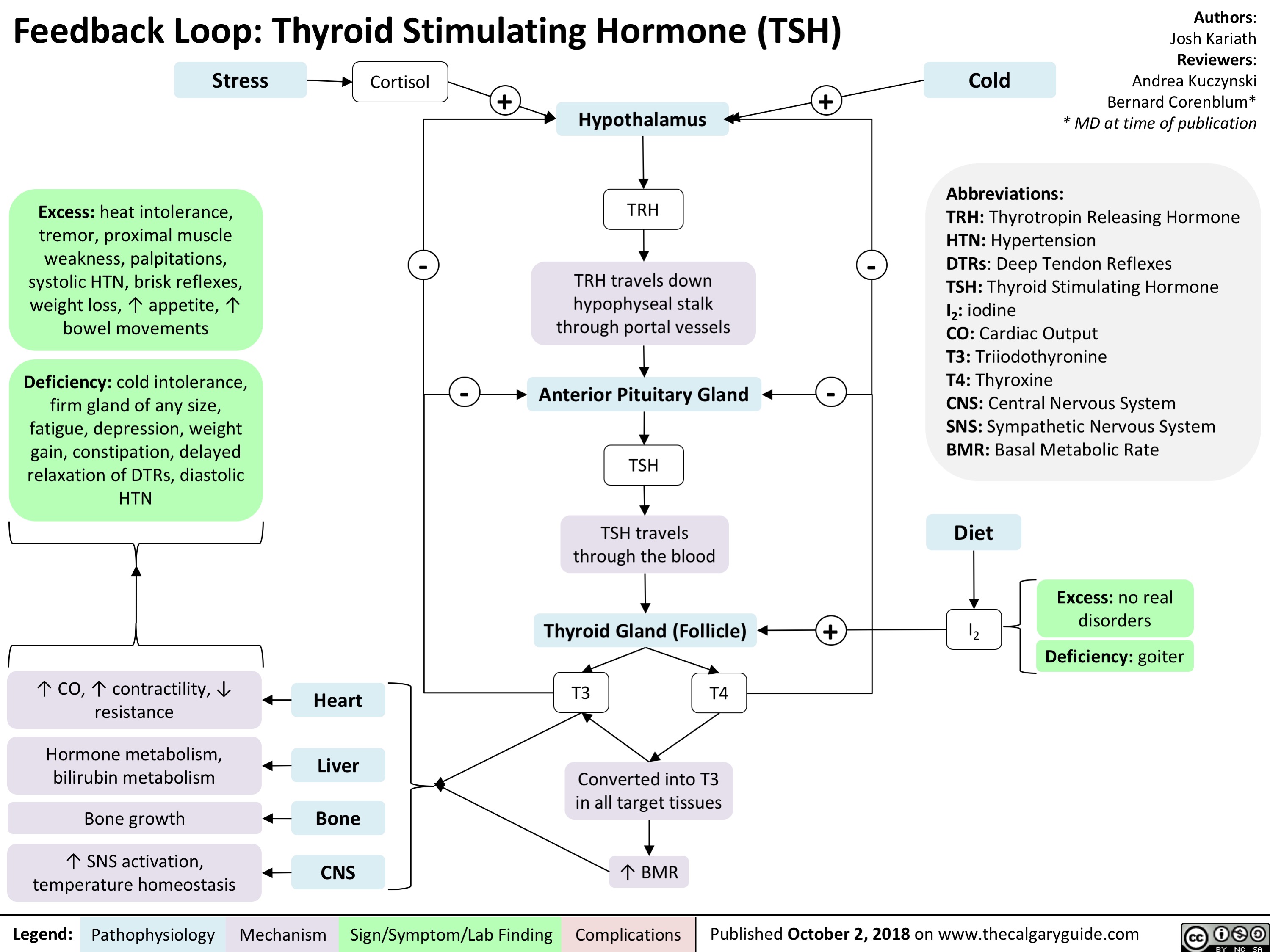
Anaphylaxis: Signs and Symptoms

Giant Cell Arteritis: Pathogenesis and Clinical Findings
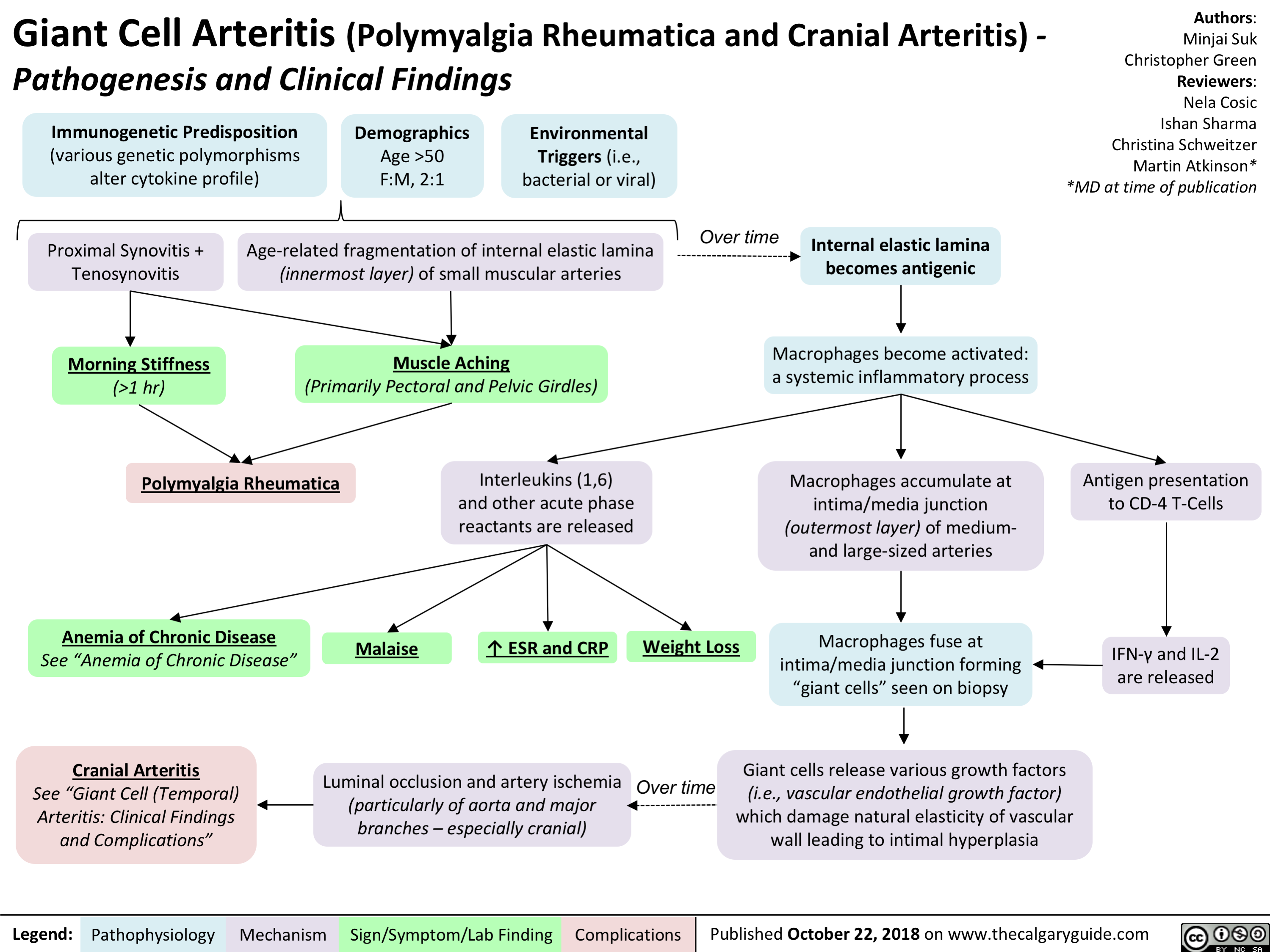
Acute Hemolytic Transfusion Reaction: Signs and Symptoms
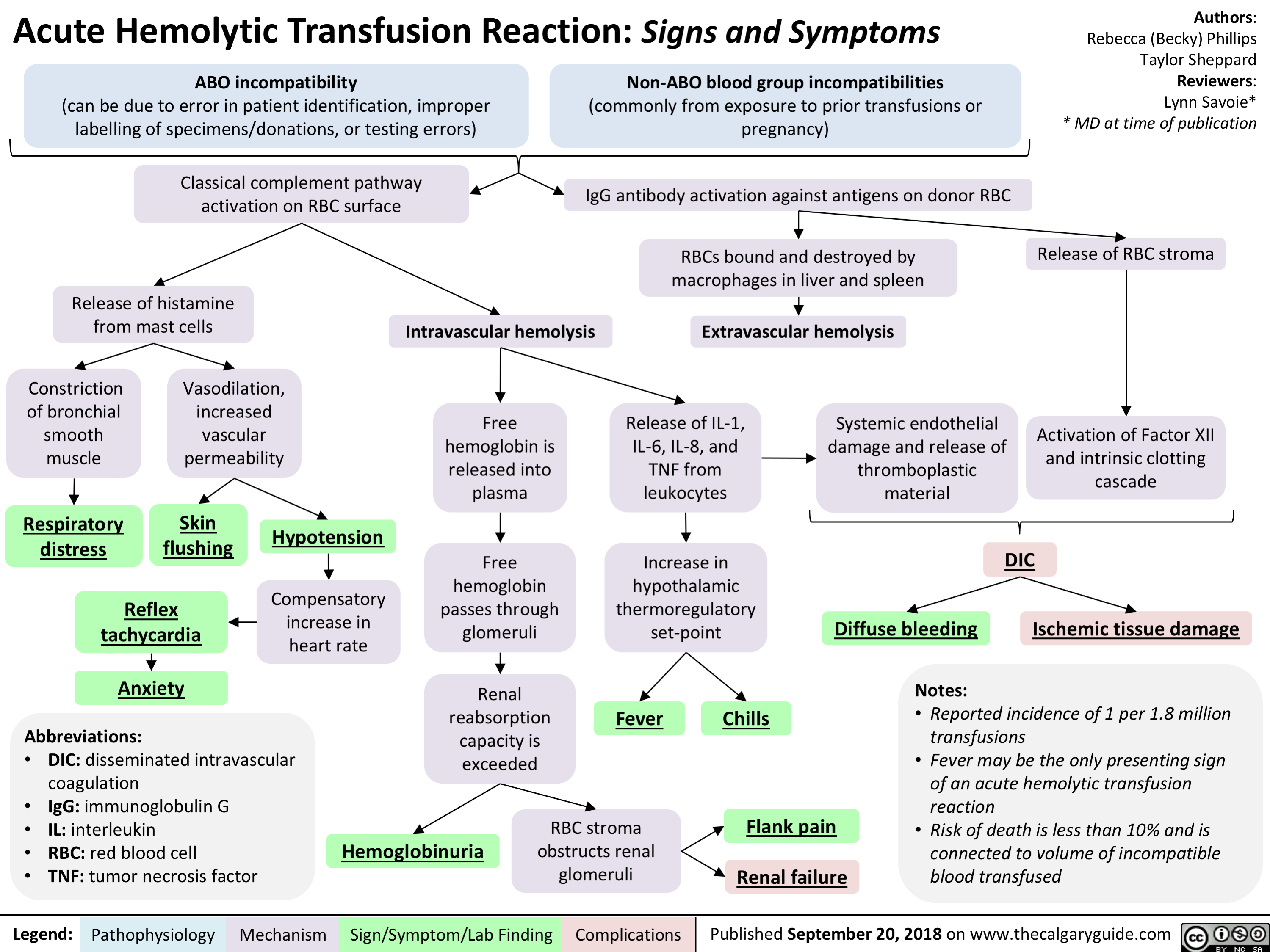
Anaphylaxis: Treatments
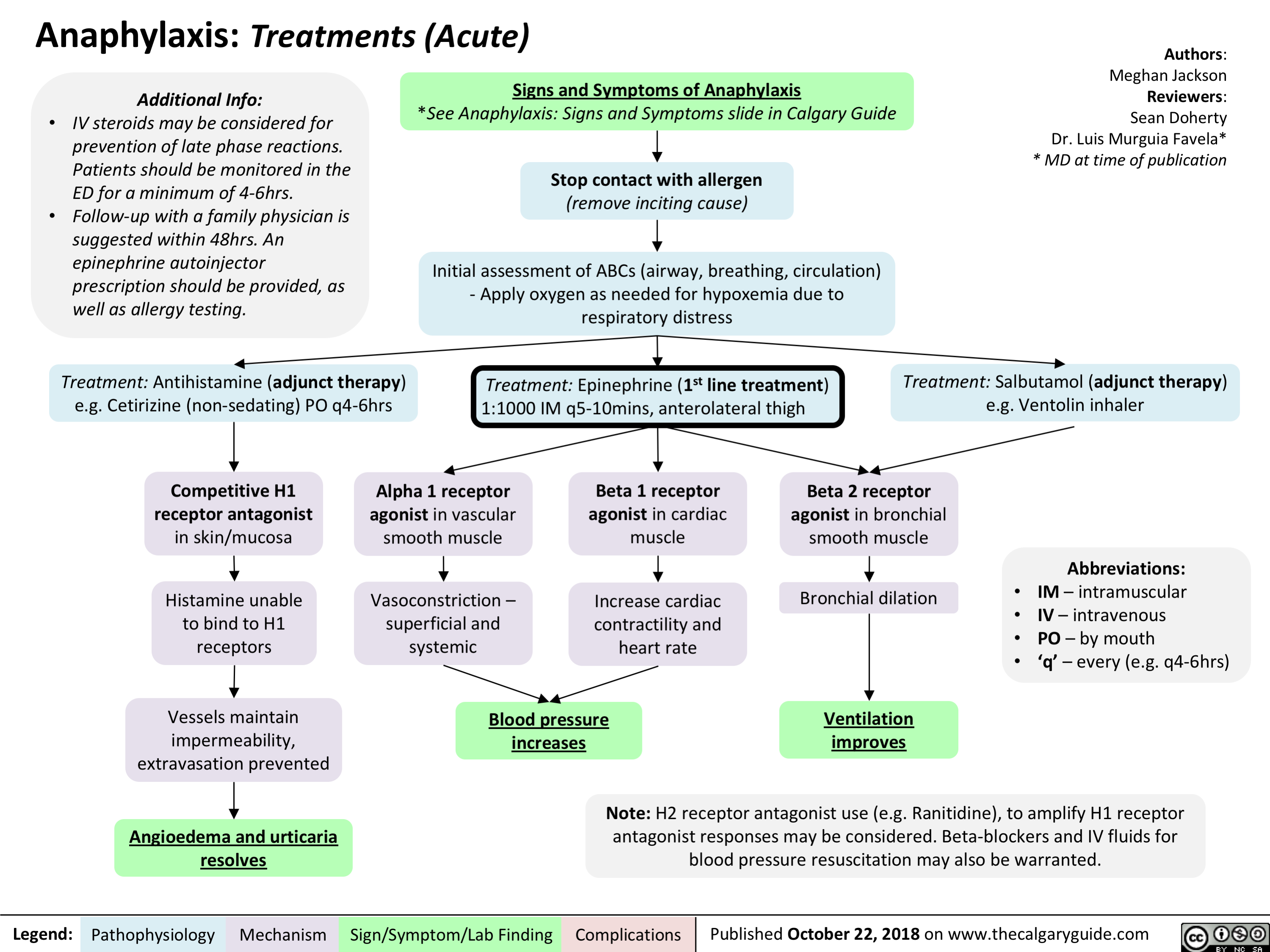
Glucocorticoid Induced Osteoporosis: Pathogenesis and Clinical Findings

intrauterine-growth-restriction-iugr-pathogenesis
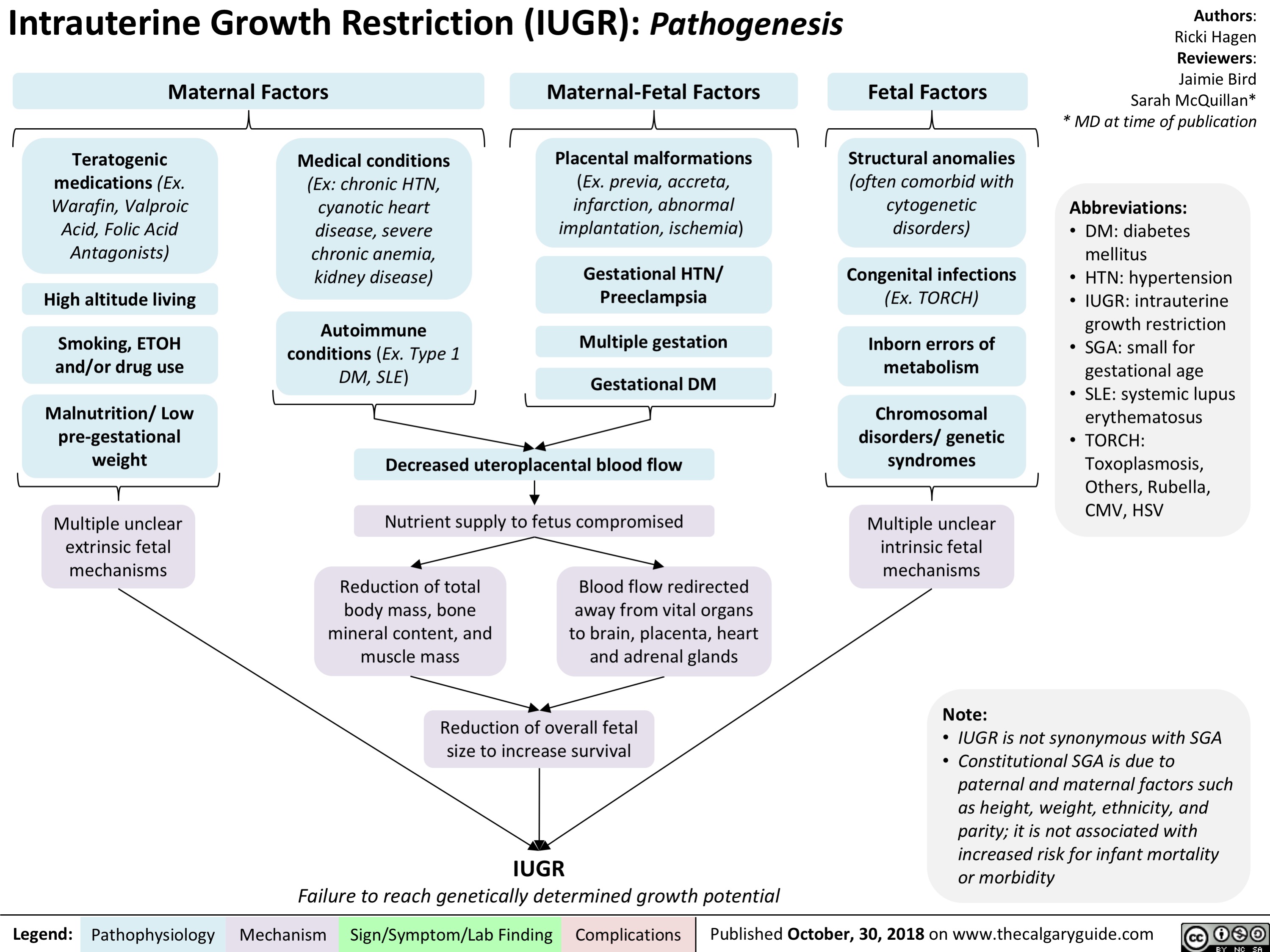
fetal-alcohol-spectrum-disorder-pathogenesis-and-clinical-findings
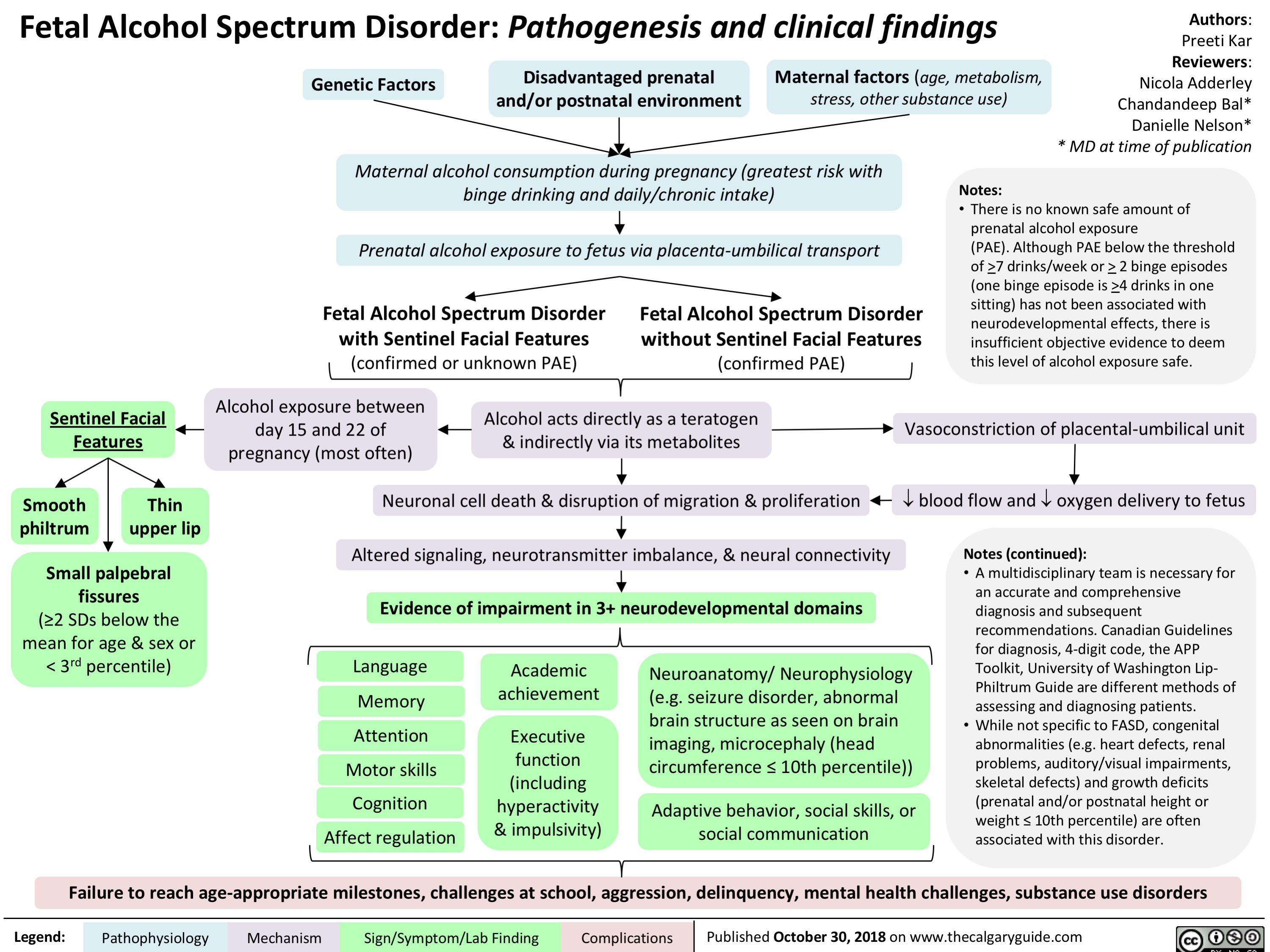
Hydrocephalus: Clinical Findings
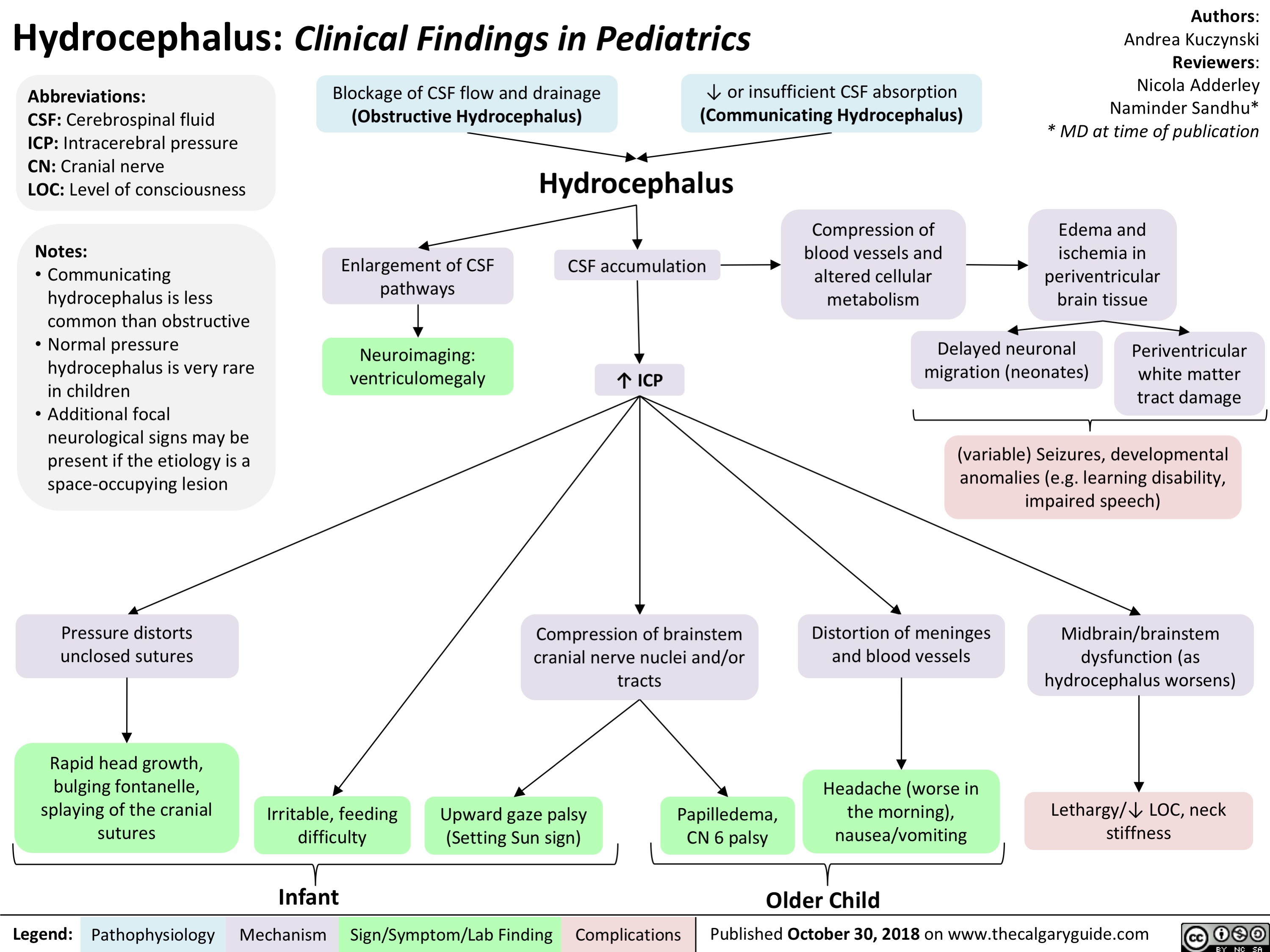
Orbital Cellulitis: Pathogenesis and clinical findings
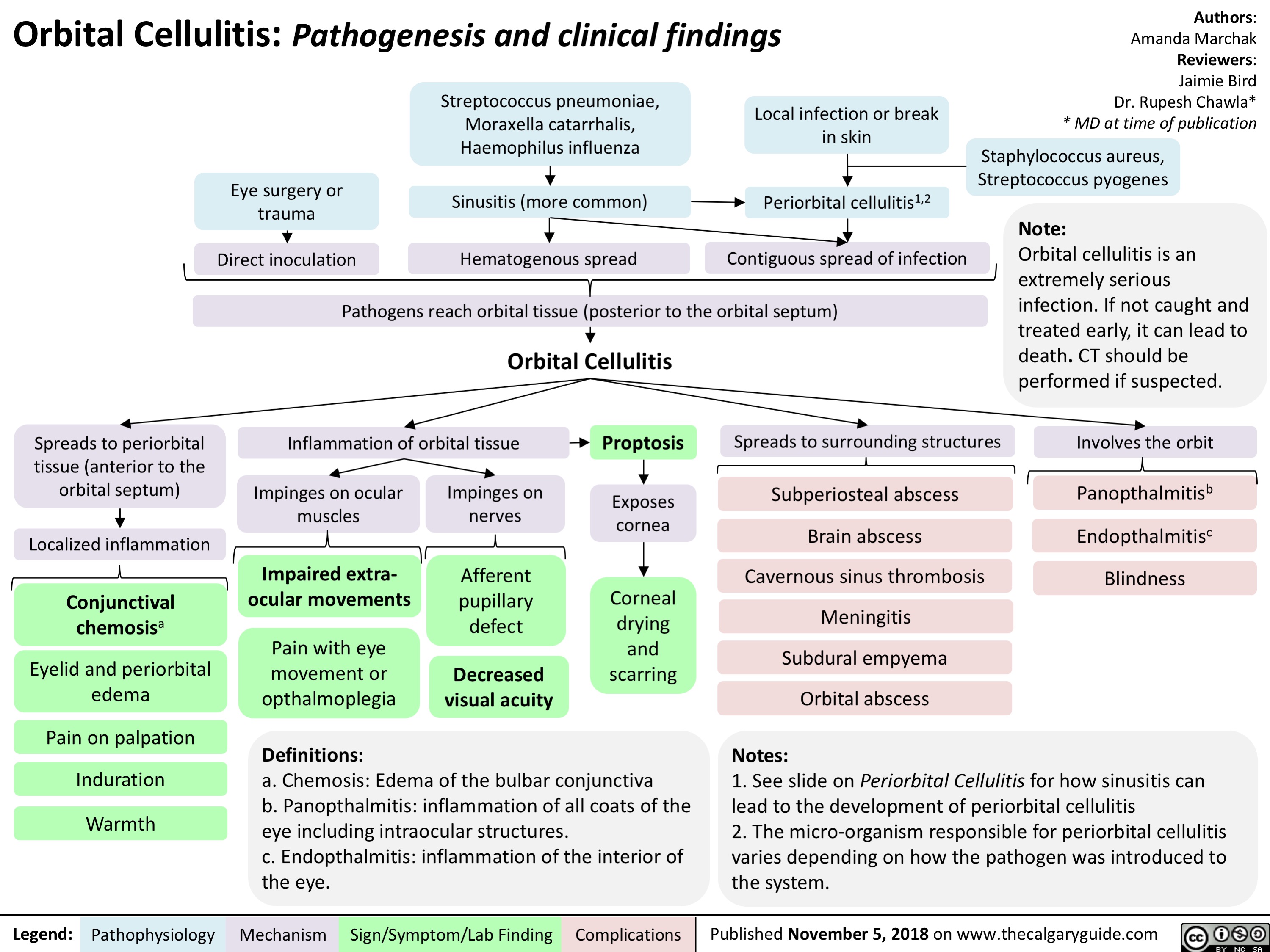
Periorbital Cellulitis: Pathogenesis and Clinical Findings
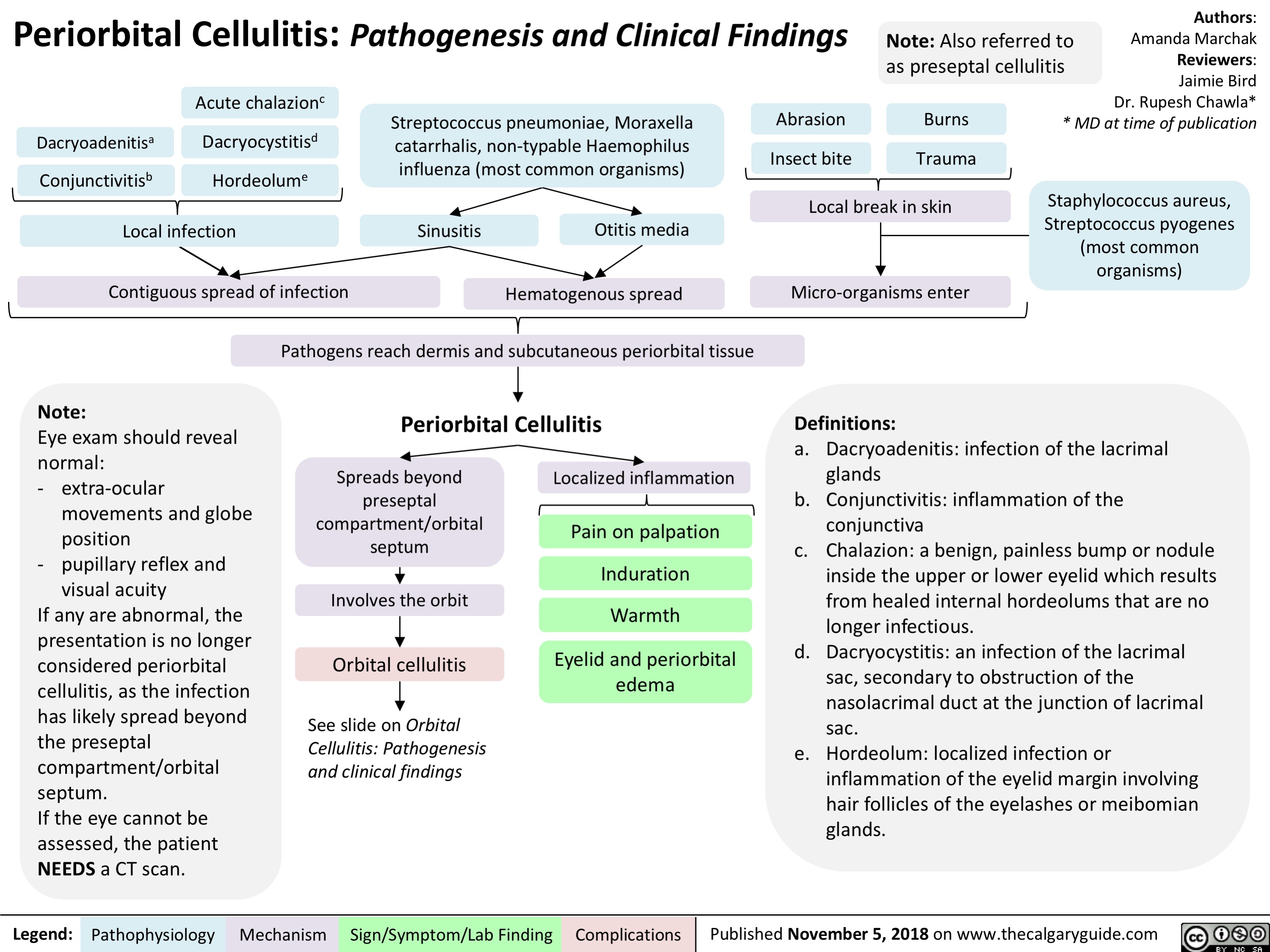
Child Abuse: Risk Factors and Possible Indicators
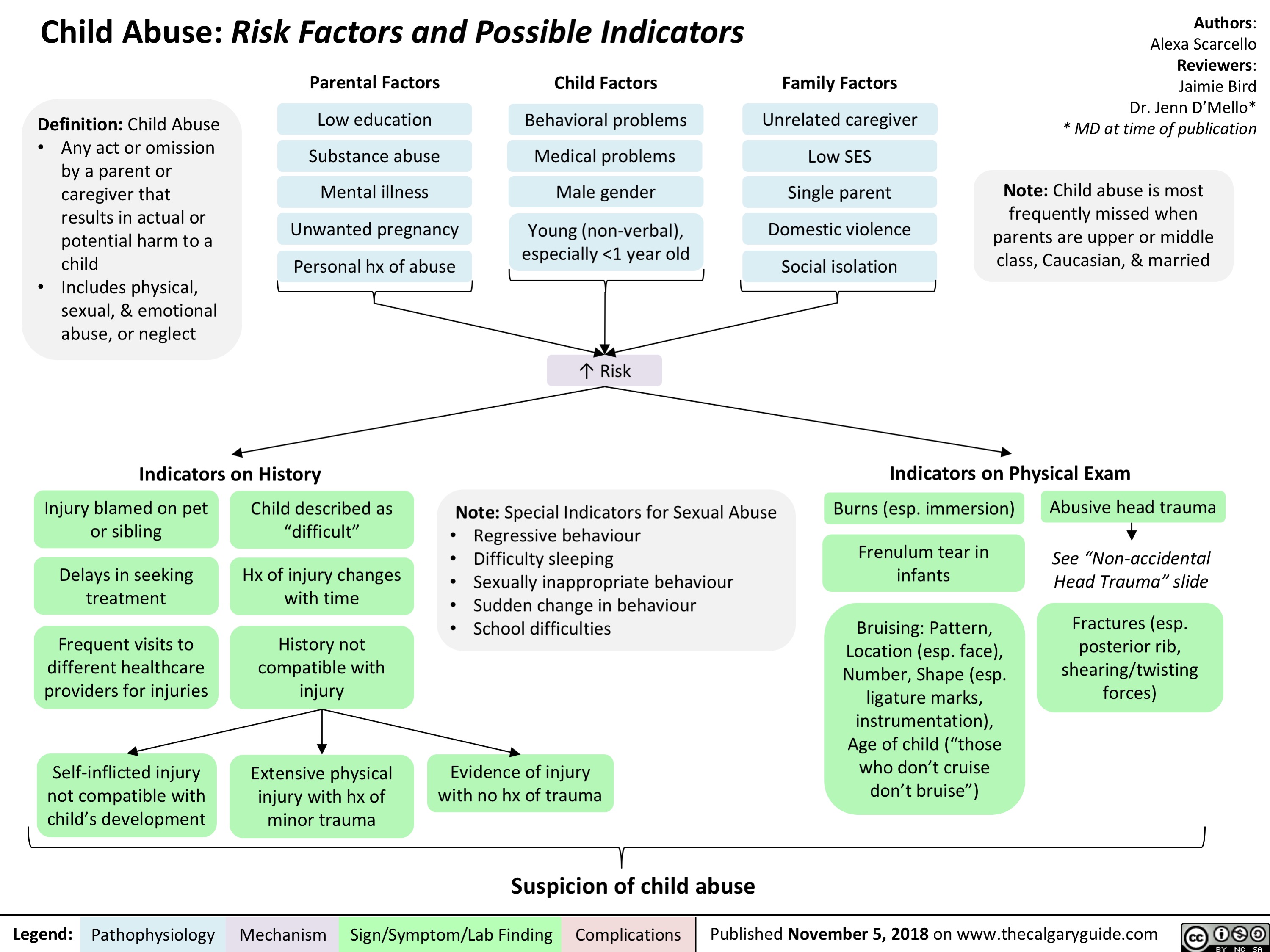
Circle of Willis: Anatomy and Physiology

Mastoiditis: Pathogenesis and clinical findings
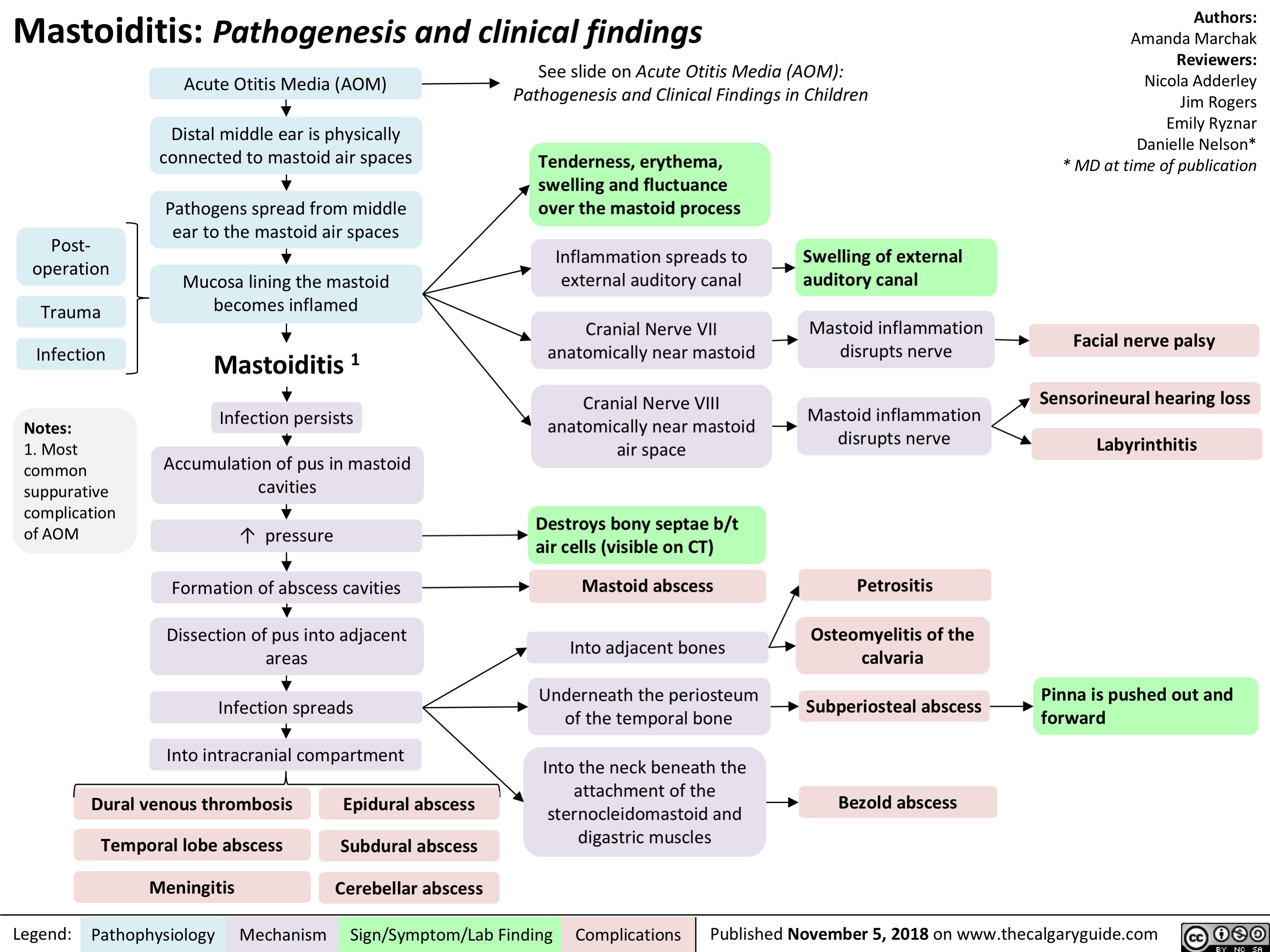
Scarlet Fever: Pathogenesis and clinical findings
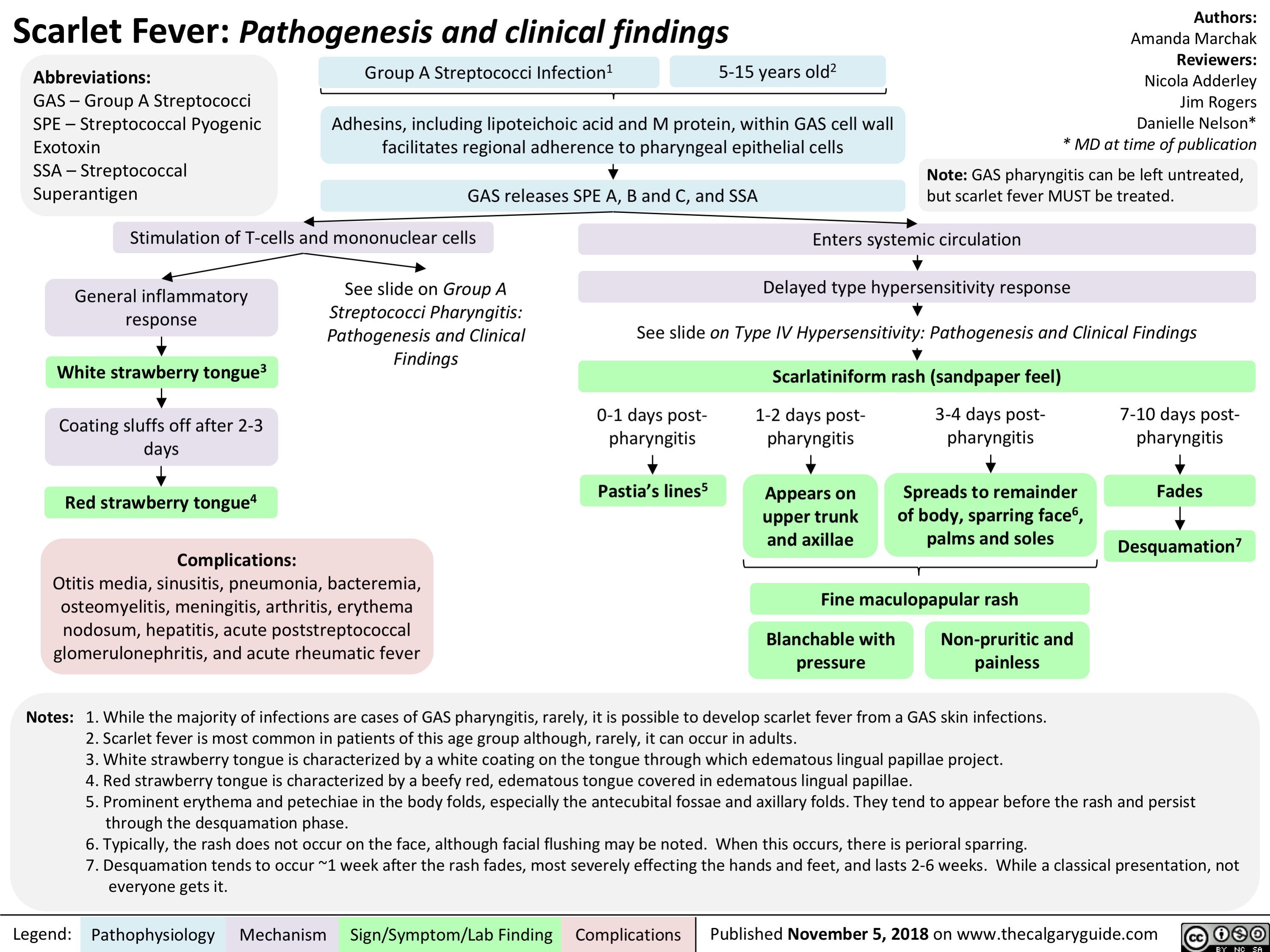
Sinusitis: Pathogenesis and clinical findings
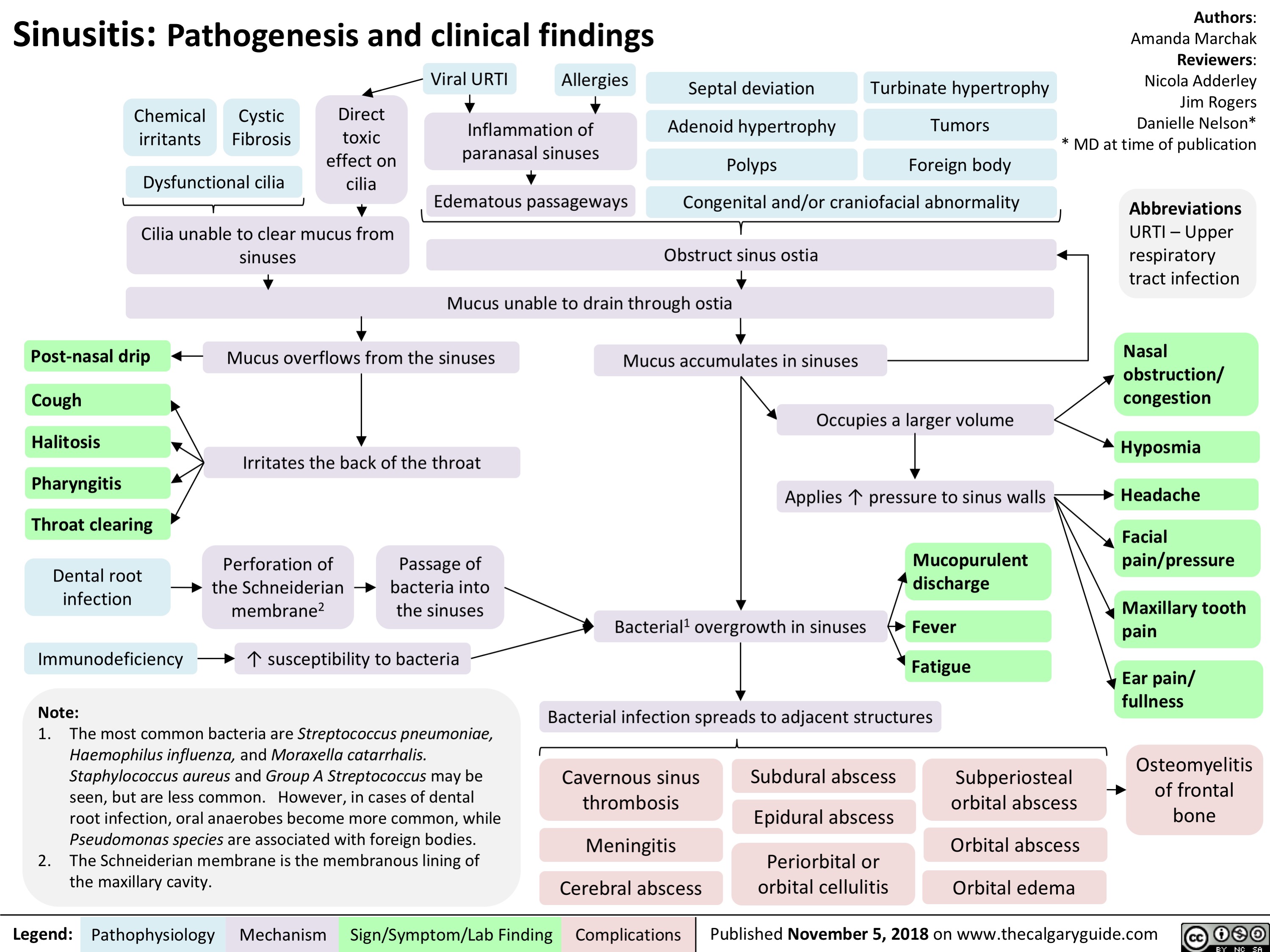
Tonsillitis: Pathogenesis and clinical findings
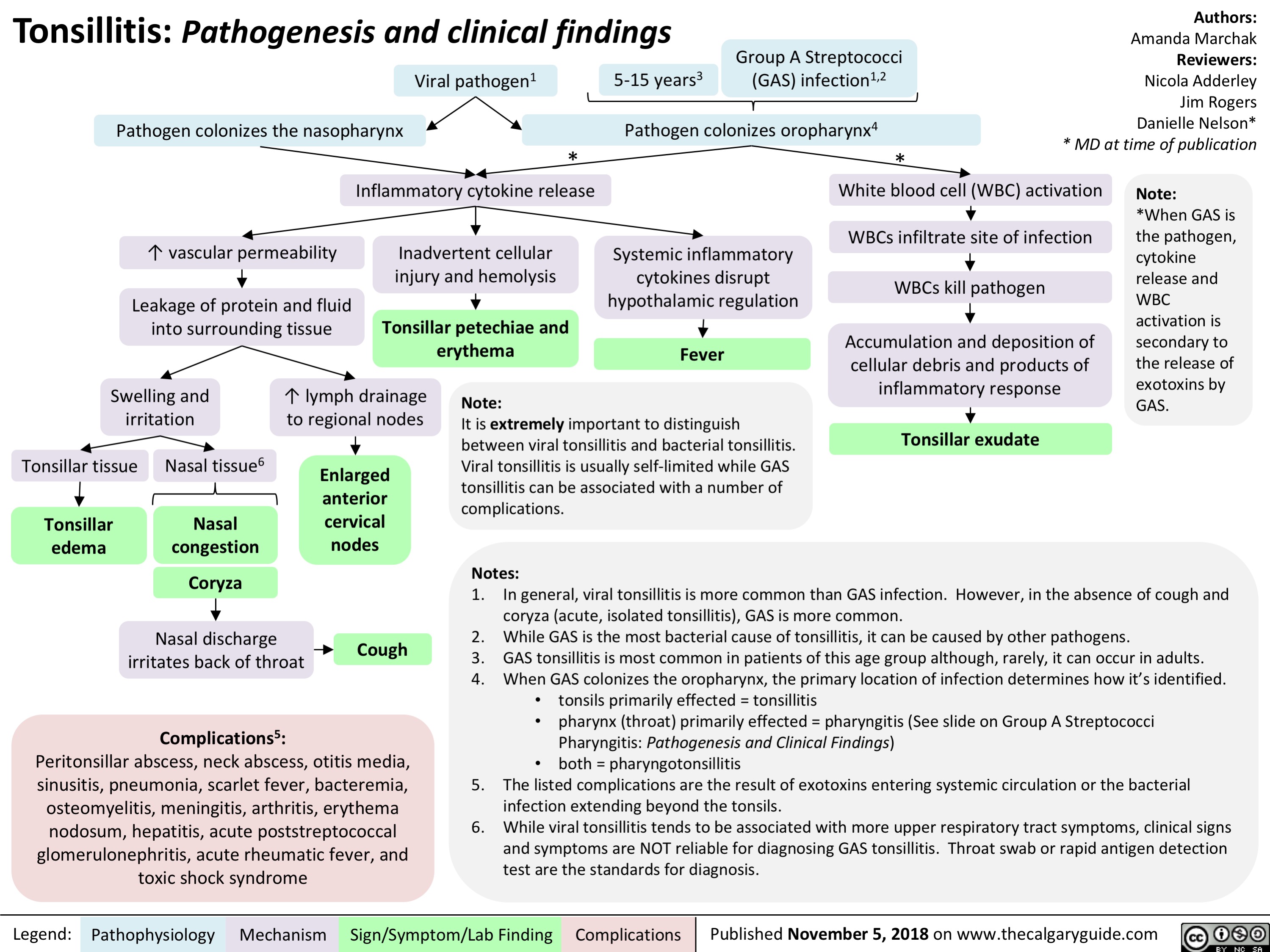
Stomach Acid Reducing Medications - Mechanisms of Action
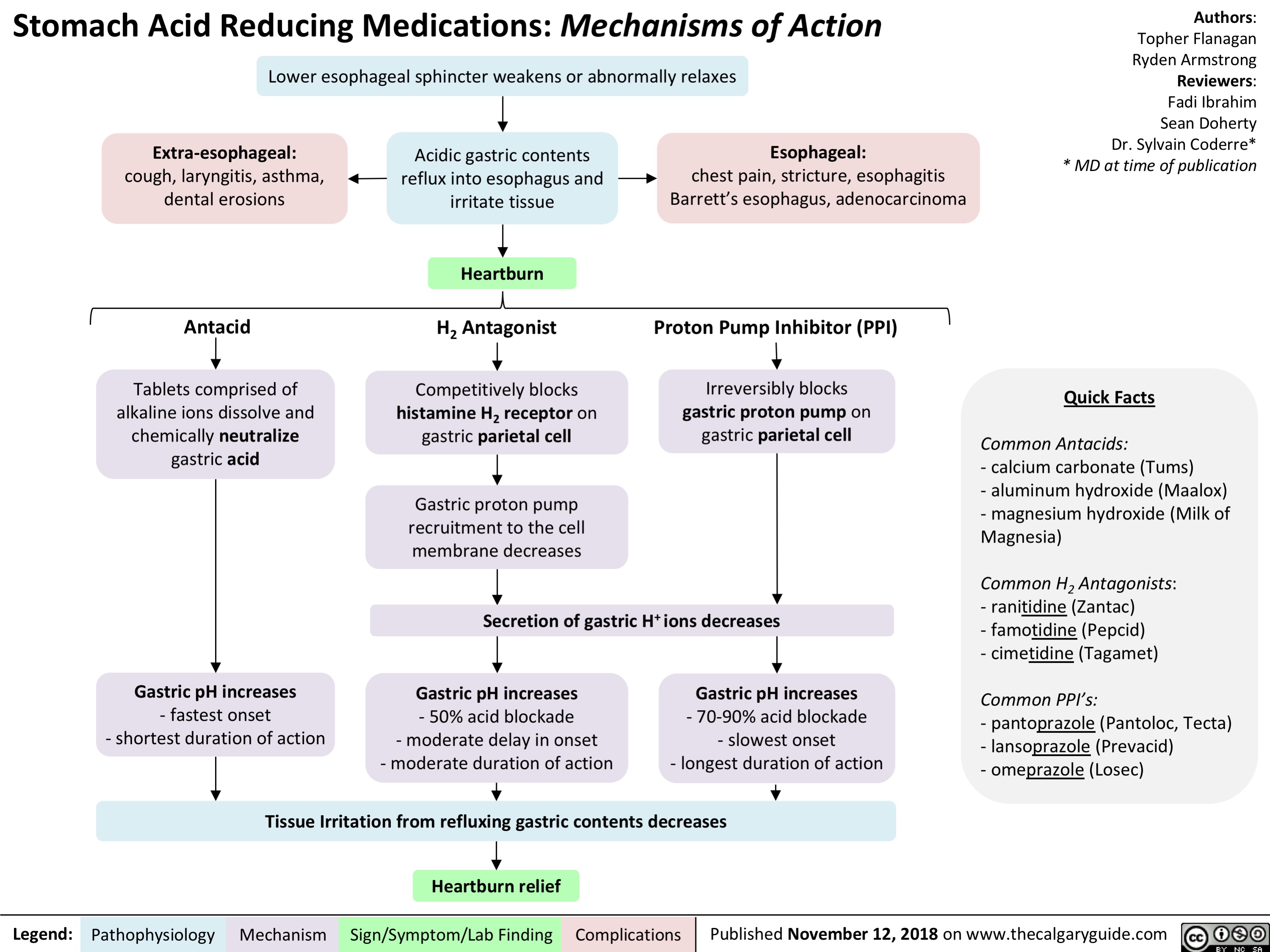
Dependent Personality Disorder Slide - Pathogenesis and clinical findings
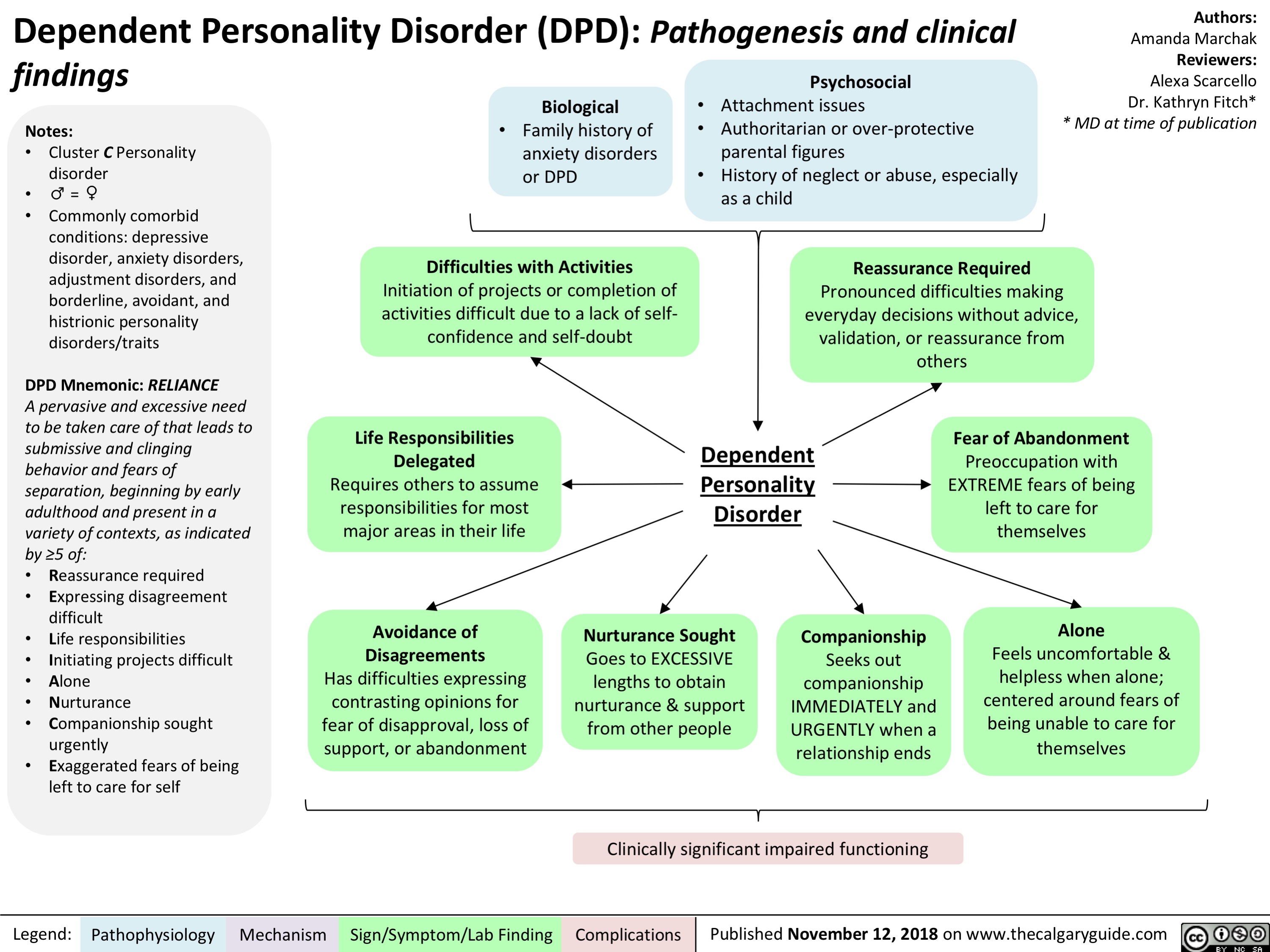
Obsessive-Compulsive Personality Disorder Slide - Pathogenesis and clinical findings

Brain Death: Pathogenesis assessment and clinical findings
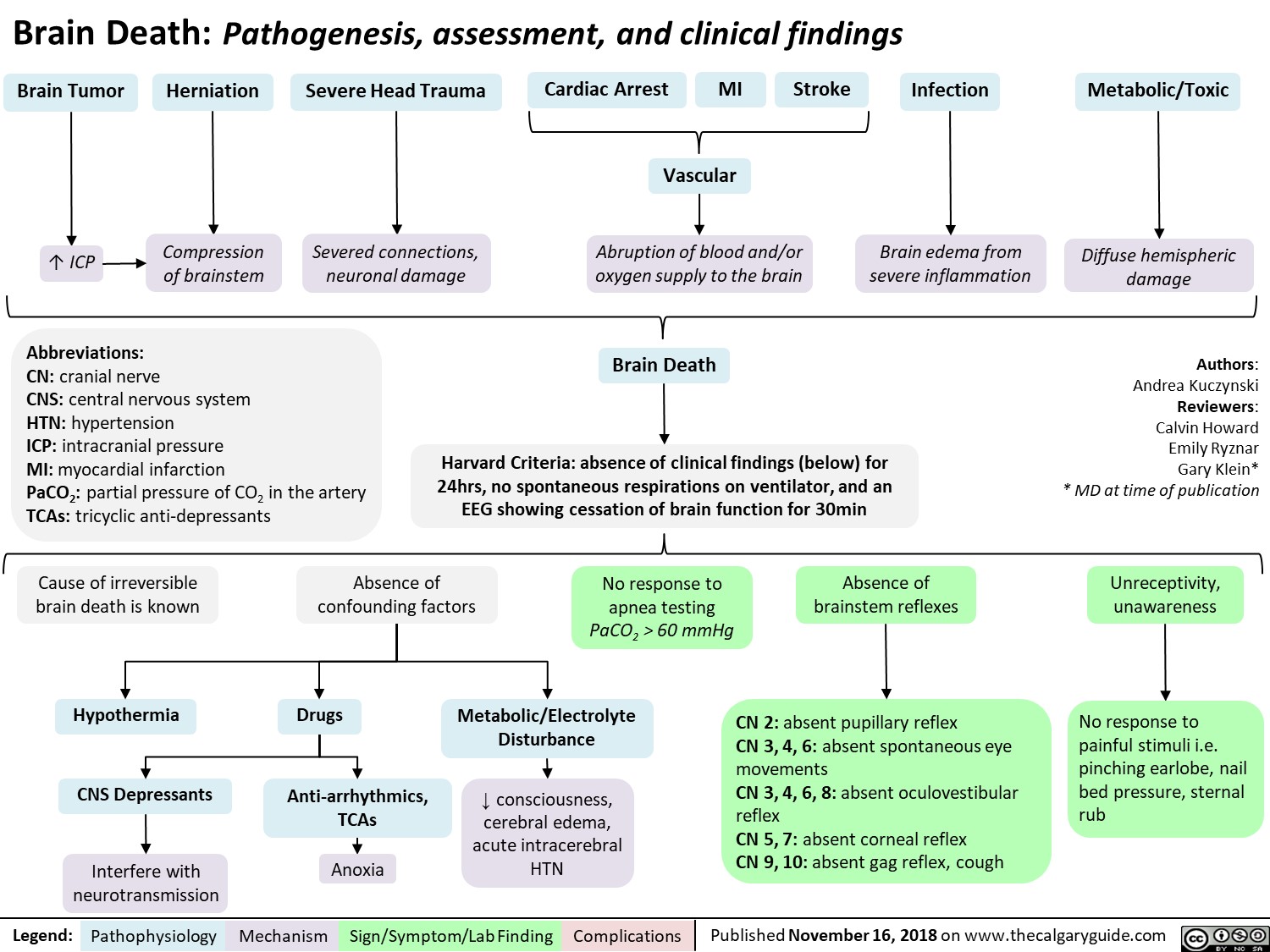
Benefits of Breast Milk: Mechanism of Action

Major Depressive Disorder: Complications

Avoidant Personality Disorder - Pathogenesis and clinical findings

Measures of Population Health
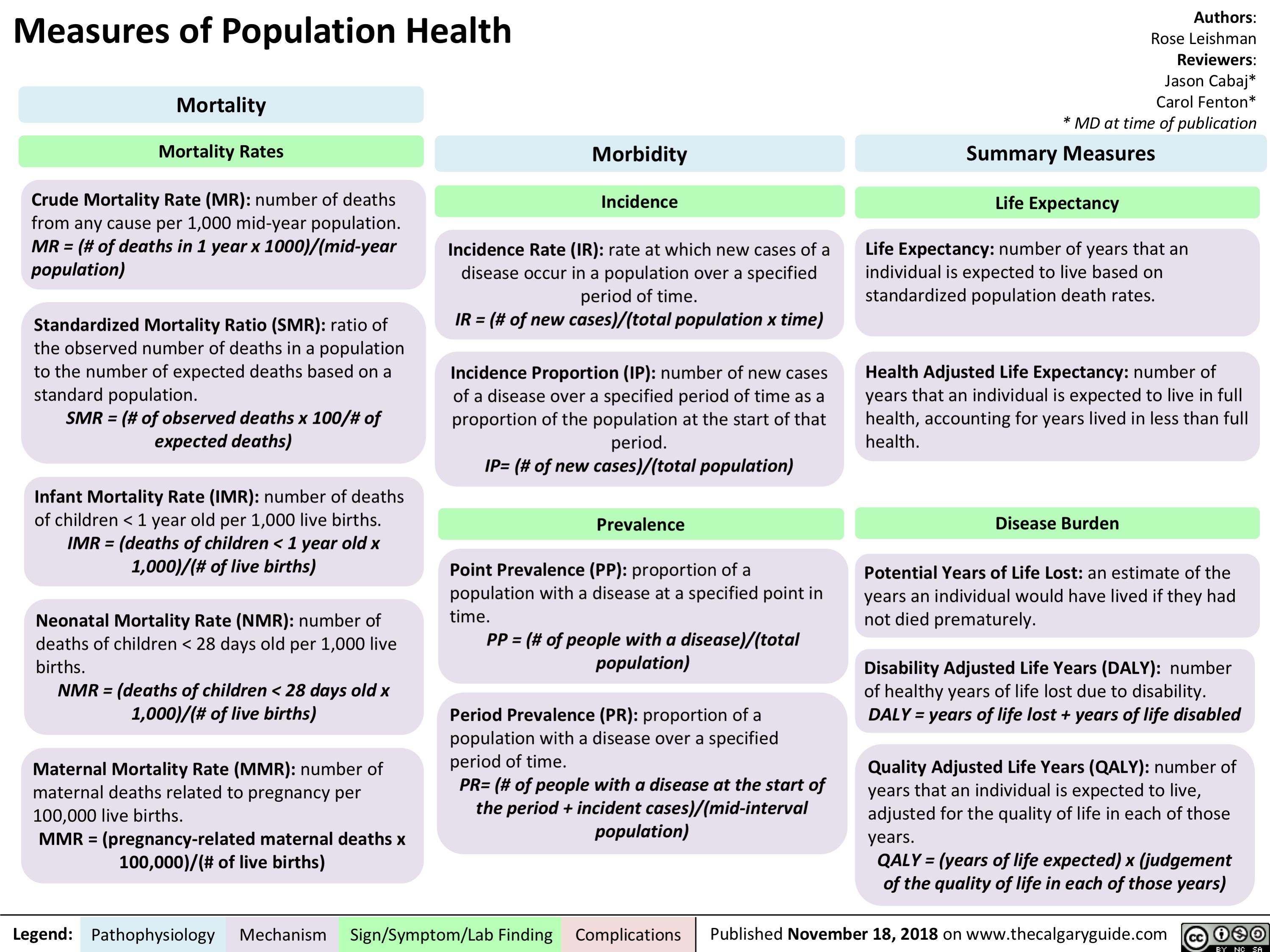
Employment as a Determinant of Health
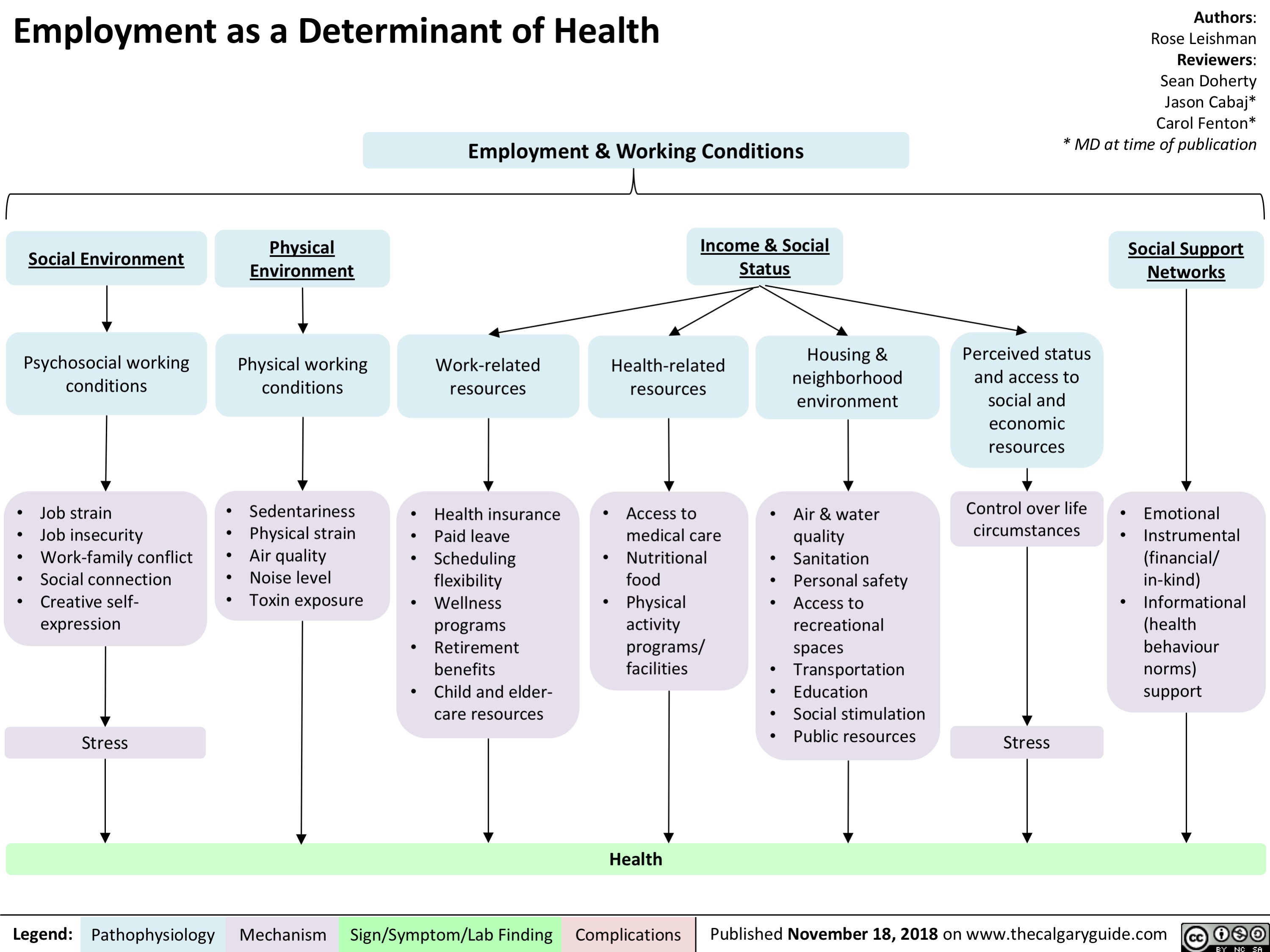
Menopause contraindications to hormone replacement therapy
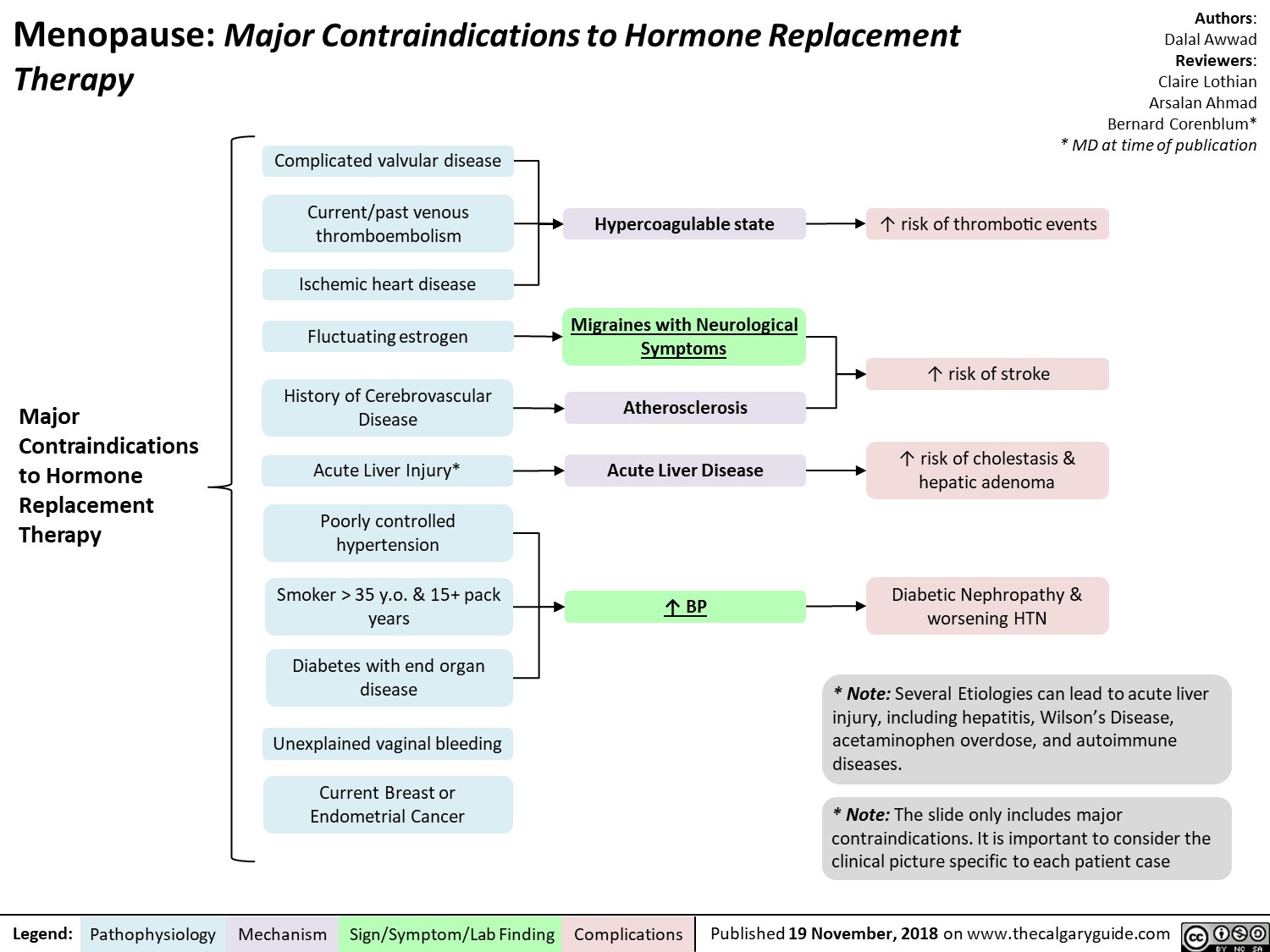
Phenylketonuria (PKU): Pathogenesis and clinical findings
![Phenylketonuria (PKU): Pathogenesis and clinical findings
Authors: Hamna Tariq Reviewers: Chandan Kaur Bal Nicola Adderley Rebecca Sparkes* * MD at time of publication
Abbreviations:
PAH – phenylalanine hydroxylase BH4 – tetrahydrobiopterin
Phe – phenylalanine
Tyr - tyrosine
LAT-1 - L-amino acid transporter 1 LNAA – large neutral amino acids NT – neurotransmitter
Biallelic mutations in PAH gene on chromosome 12q23.2
Loss of activity/deficiency of PAH
Inability to convert Phe to Tyr
Buildup of Phe and its metabolites
↑ transport of Phe via LAT-1 at the blood brain barrier
Phe outcompetes LNAA for binding sites on LAT-1
↓ LNAA transport
↓ cerebral protein synthesis and ↓ NT synthesis
White matter lesions, oxidative damage, hypomelination & demyelination
Sources of Phe
Dietary protein
Breakdown into amino acids
↓ Tyr and derivatives
↓ melanin
Fair skin and hair
Notes:
Endogenous recycling of amino acid stores
Phe oxidized to phenylacetate
Musty odor to urine, sweat and breath
• Autosomal recessive inborn error of metabolism; clinical severity depends on residual PKU activity
• This slide denotes clinical features of classical PKU in untreated patients. Symptoms develop within a few months of birth only if untreated.
• PAH, using a BH4 cofactor, converts Phe to tyrosine, which is necessary to produce epinephrine, norepinephrine, dopamine and melanin. (Rare inherited disorders of BH4 synthesis/recycling cause elevated Phe and neurologic symptoms.)
• PKU is screened for at birth in most developed nations.
• In early-diagnosed, continuously treated patients, ID,
microcephaly and neurologic features are not expected, but there is still an increased incidence of behavioral, emotional and social problems
↑ brain [Phe]
Behavioral, emotional & social problems (ADHD, mood disorders, aggression, ↓ self-esteem, ↓ social competency, ↓ autonomy)
Intellectual disability
(↓ language, memory & learning skills, executive function, IQ, school performance)
Neurological findings (tremor, shaking, seizures, poor coordination)
Microcephaly
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 19, 2018 on www.thecalgaryguide.com
Phenylketonuria (PKU): Pathogenesis and clinical findings
Authors: Hamna Tariq Reviewers: Chandan Kaur Bal Nicola Adderley Rebecca Sparkes* * MD at time of publication
Abbreviations:
PAH – phenylalanine hydroxylase BH4 – tetrahydrobiopterin
Phe – phenylalanine
Tyr - tyrosine
LAT-1 - L-amino acid transporter 1 LNAA – large neutral amino acids NT – neurotransmitter
Biallelic mutations in PAH gene on chromosome 12q23.2
Loss of activity/deficiency of PAH
Inability to convert Phe to Tyr
Buildup of Phe and its metabolites
↑ transport of Phe via LAT-1 at the blood brain barrier
Phe outcompetes LNAA for binding sites on LAT-1
↓ LNAA transport
↓ cerebral protein synthesis and ↓ NT synthesis
White matter lesions, oxidative damage, hypomelination & demyelination
Sources of Phe
Dietary protein
Breakdown into amino acids
↓ Tyr and derivatives
↓ melanin
Fair skin and hair
Notes:
Endogenous recycling of amino acid stores
Phe oxidized to phenylacetate
Musty odor to urine, sweat and breath
• Autosomal recessive inborn error of metabolism; clinical severity depends on residual PKU activity
• This slide denotes clinical features of classical PKU in untreated patients. Symptoms develop within a few months of birth only if untreated.
• PAH, using a BH4 cofactor, converts Phe to tyrosine, which is necessary to produce epinephrine, norepinephrine, dopamine and melanin. (Rare inherited disorders of BH4 synthesis/recycling cause elevated Phe and neurologic symptoms.)
• PKU is screened for at birth in most developed nations.
• In early-diagnosed, continuously treated patients, ID,
microcephaly and neurologic features are not expected, but there is still an increased incidence of behavioral, emotional and social problems
↑ brain [Phe]
Behavioral, emotional & social problems (ADHD, mood disorders, aggression, ↓ self-esteem, ↓ social competency, ↓ autonomy)
Intellectual disability
(↓ language, memory & learning skills, executive function, IQ, school performance)
Neurological findings (tremor, shaking, seizures, poor coordination)
Microcephaly
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 19, 2018 on www.thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2018/11/Phenylketonuria_Final.jpg)
Feedback Loop: Prolactin (PRL)
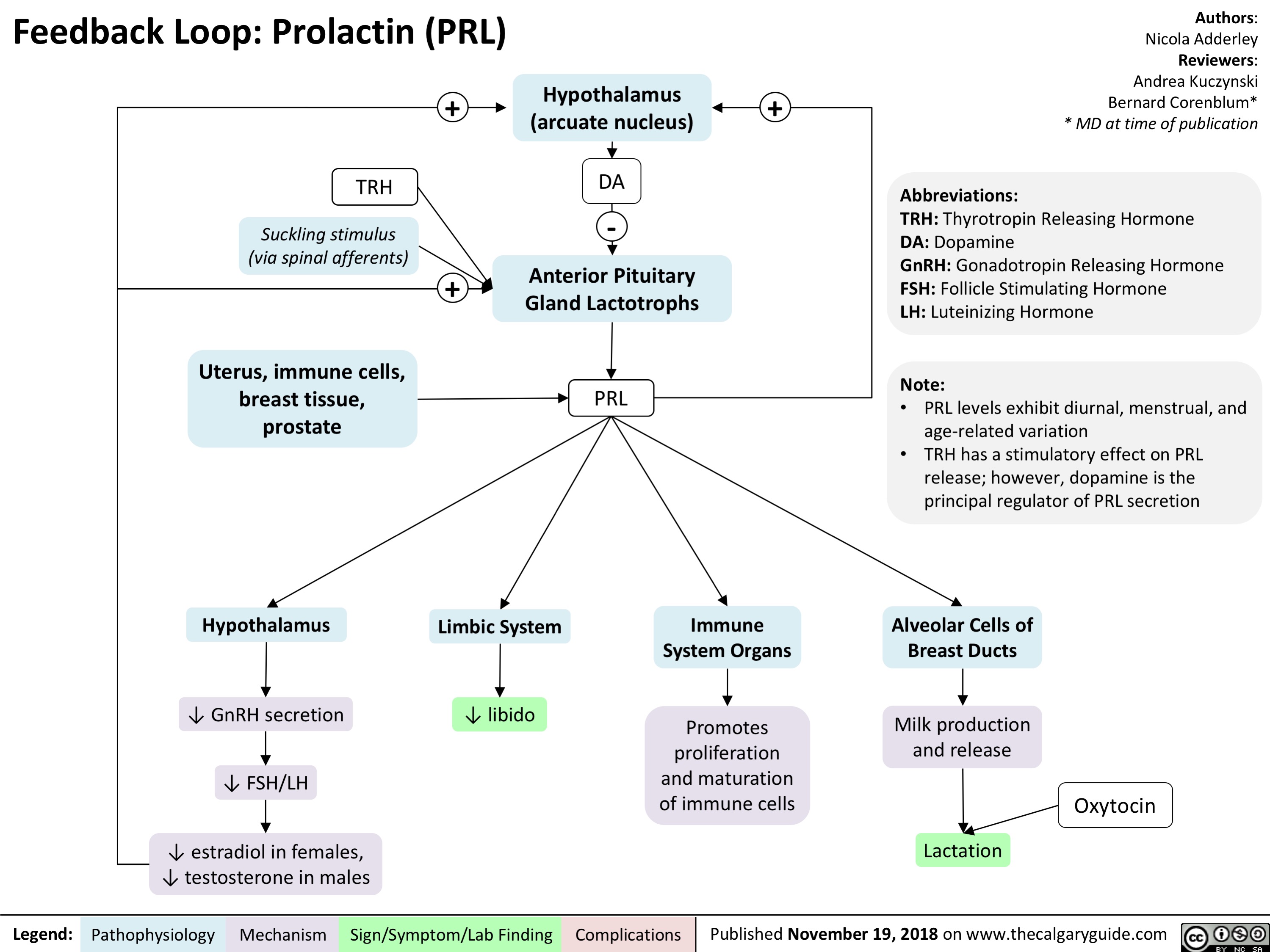
Vesicoureteric reflux (VUR): Pathogenesis and clinical findings
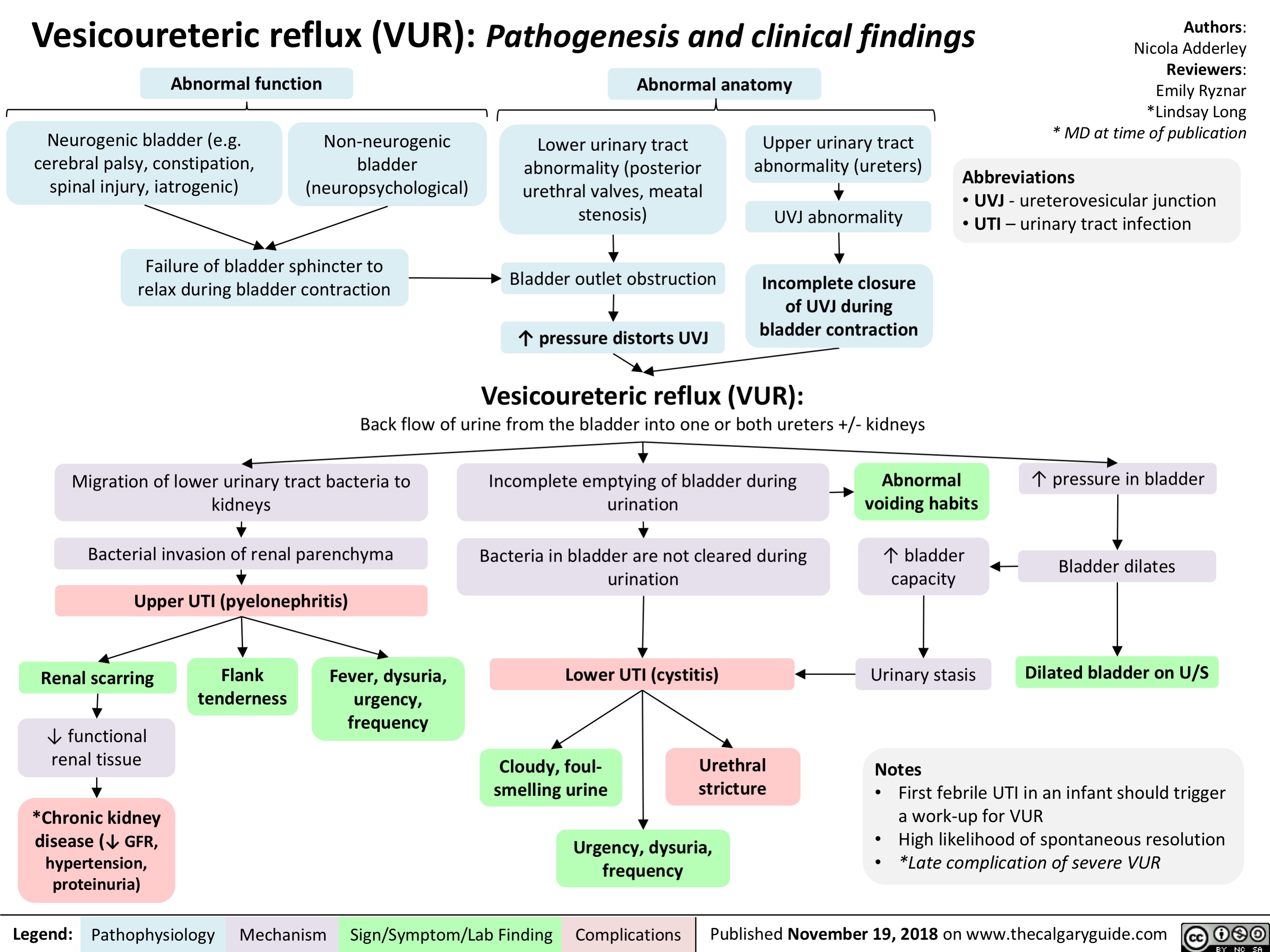
IVH Intraventricular Hemorrhage in Preterm Infants - Pathogenesis
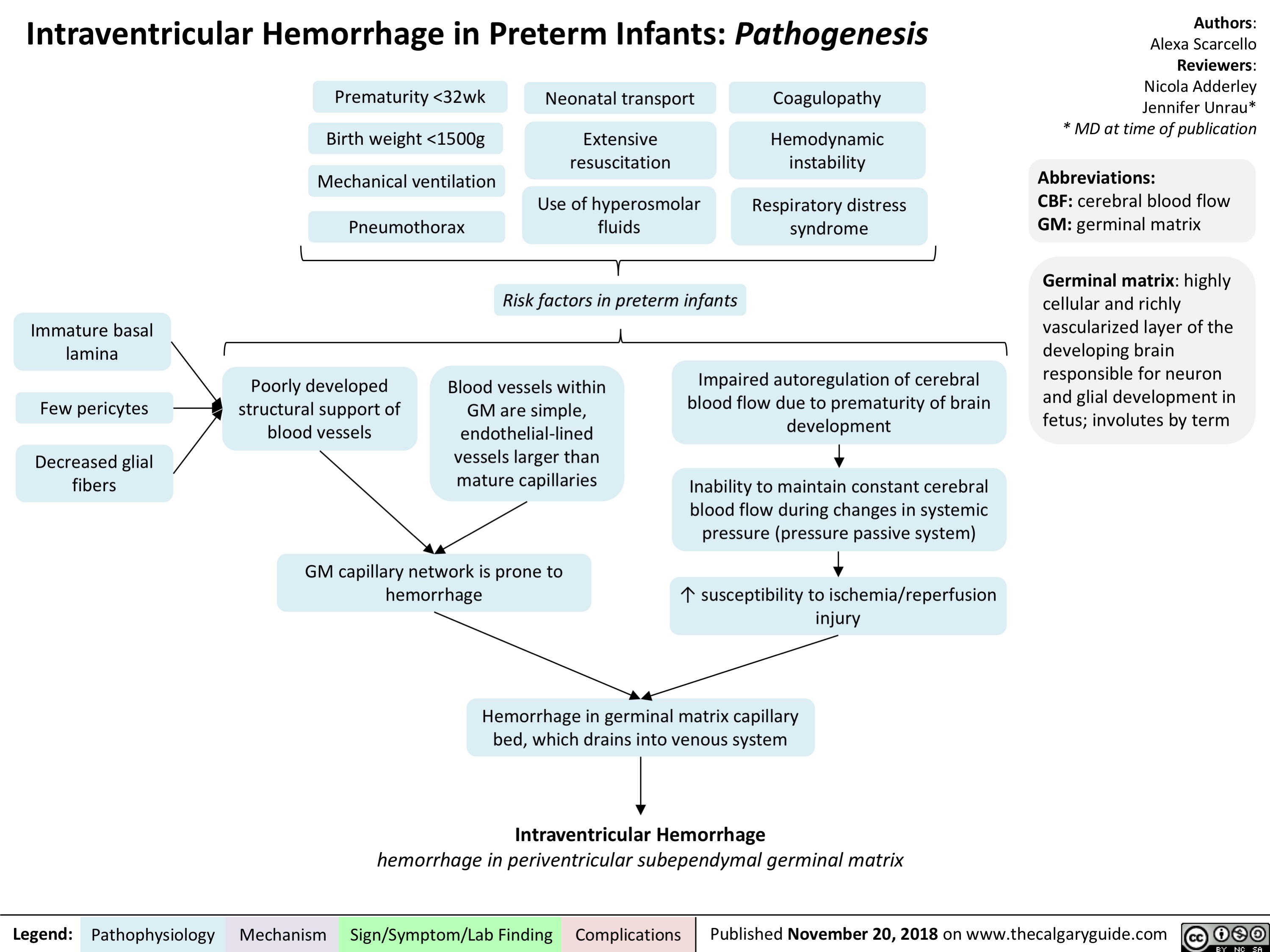
Prader Willi syndrome: pathogenesis and clinical findings
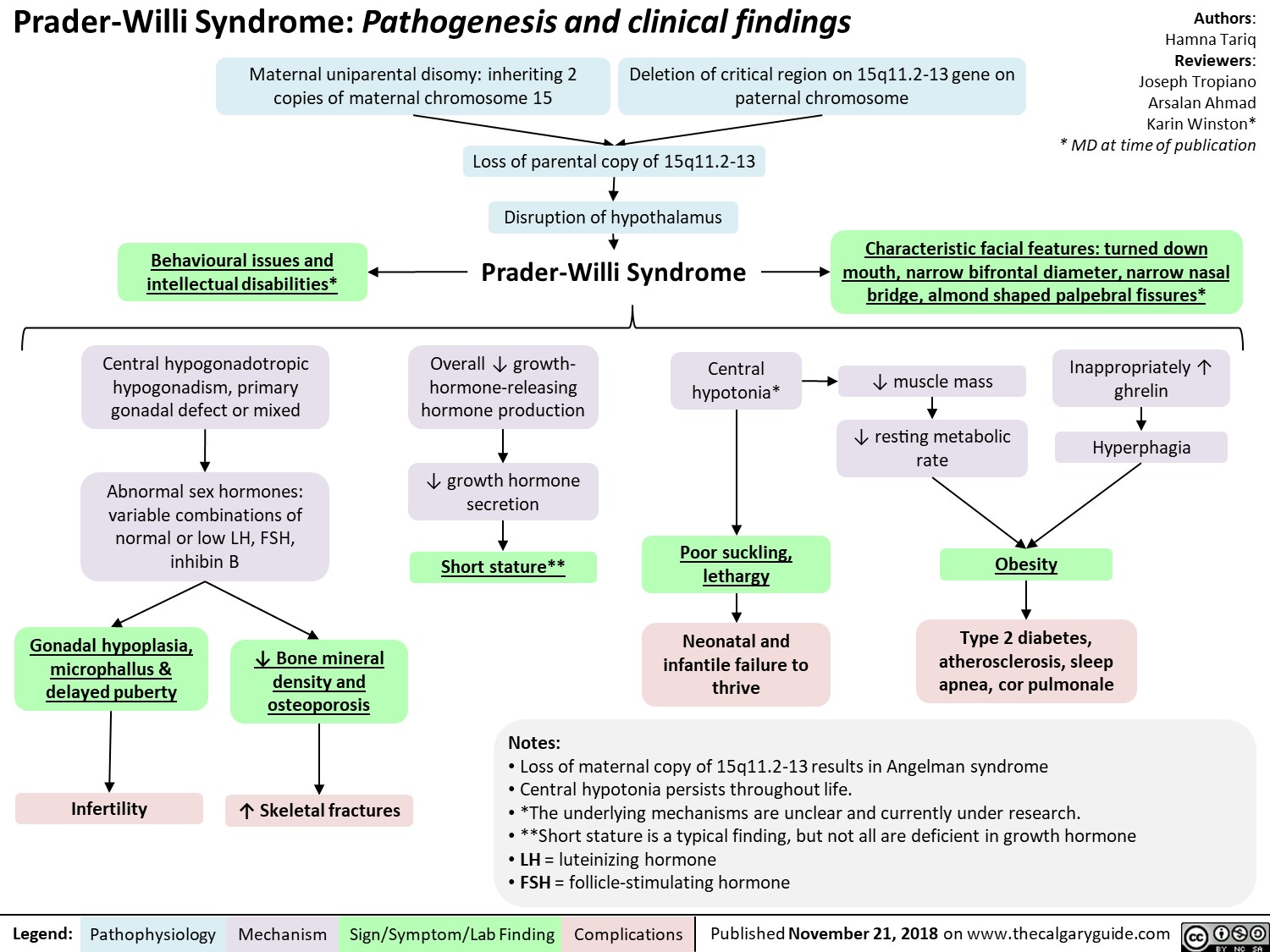
Anticonvulsants as Mood Stabilizers: Mechanism and Side-effect
Benzodiazepine (BZD) withdrawal: clinical findings and complications
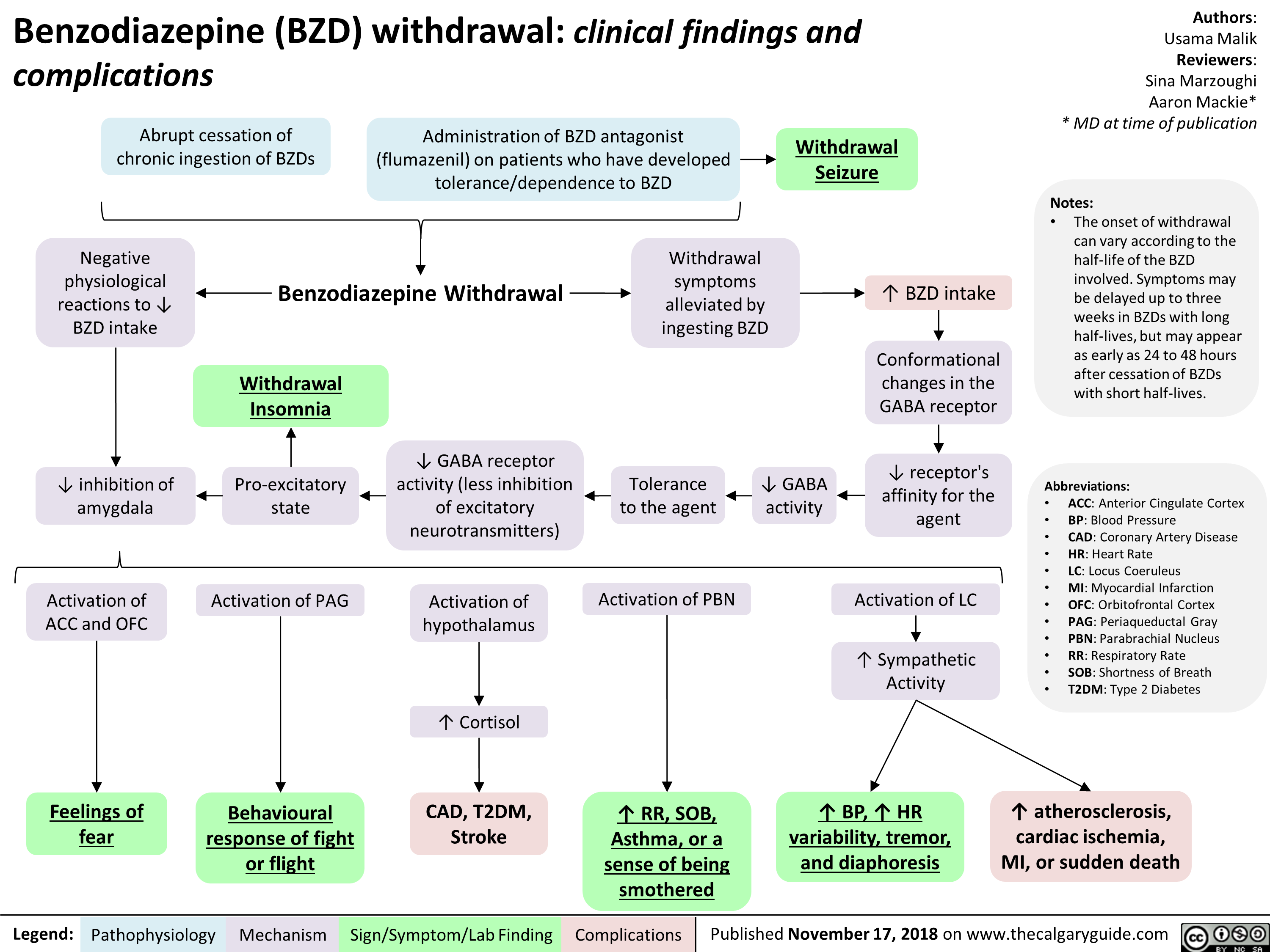
Benzodiazepines: Mechanism of Action and Side Effects
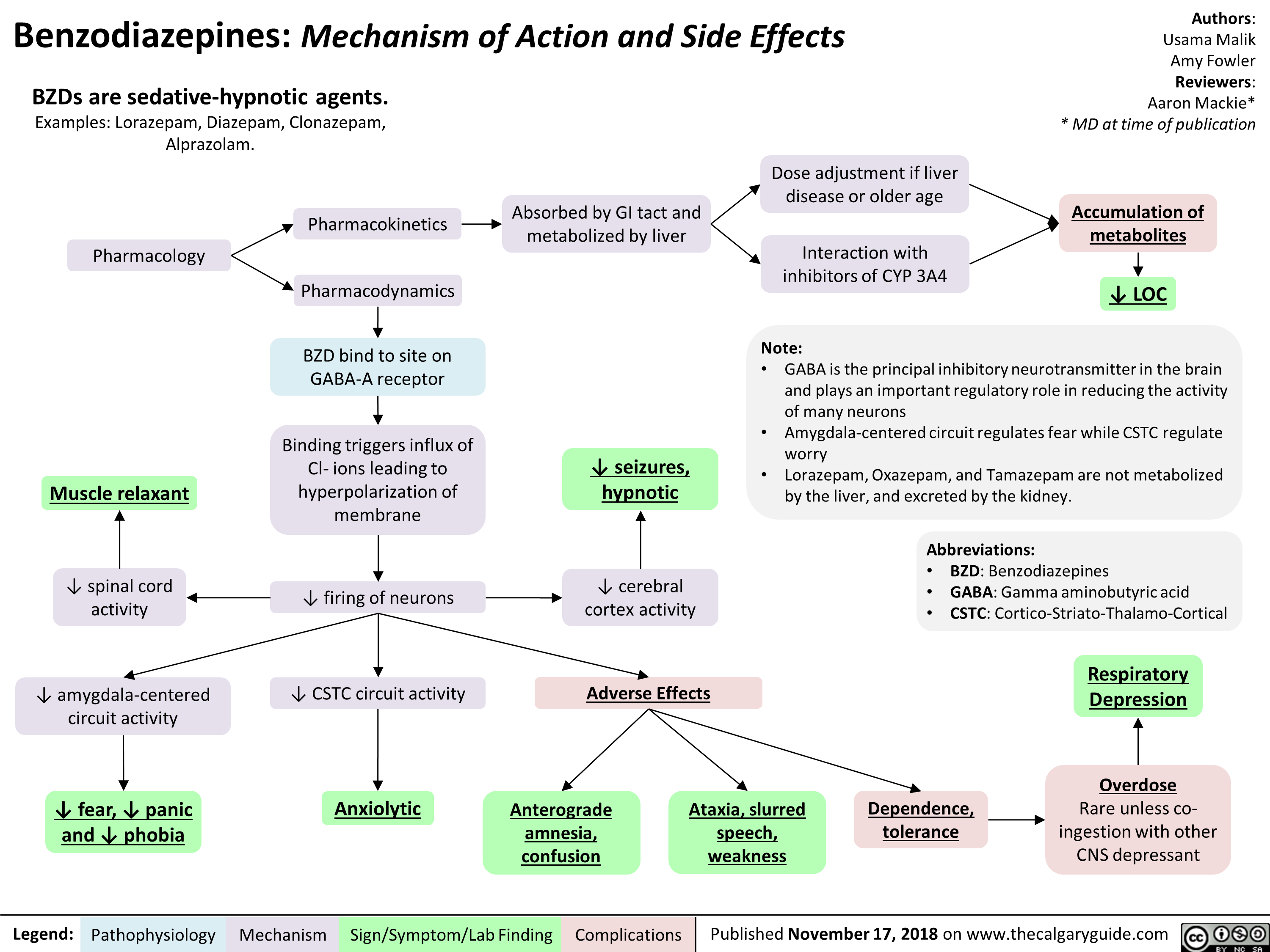
Schizotypal Personality Disorder (SPD): Pathogenesis and clinical findings
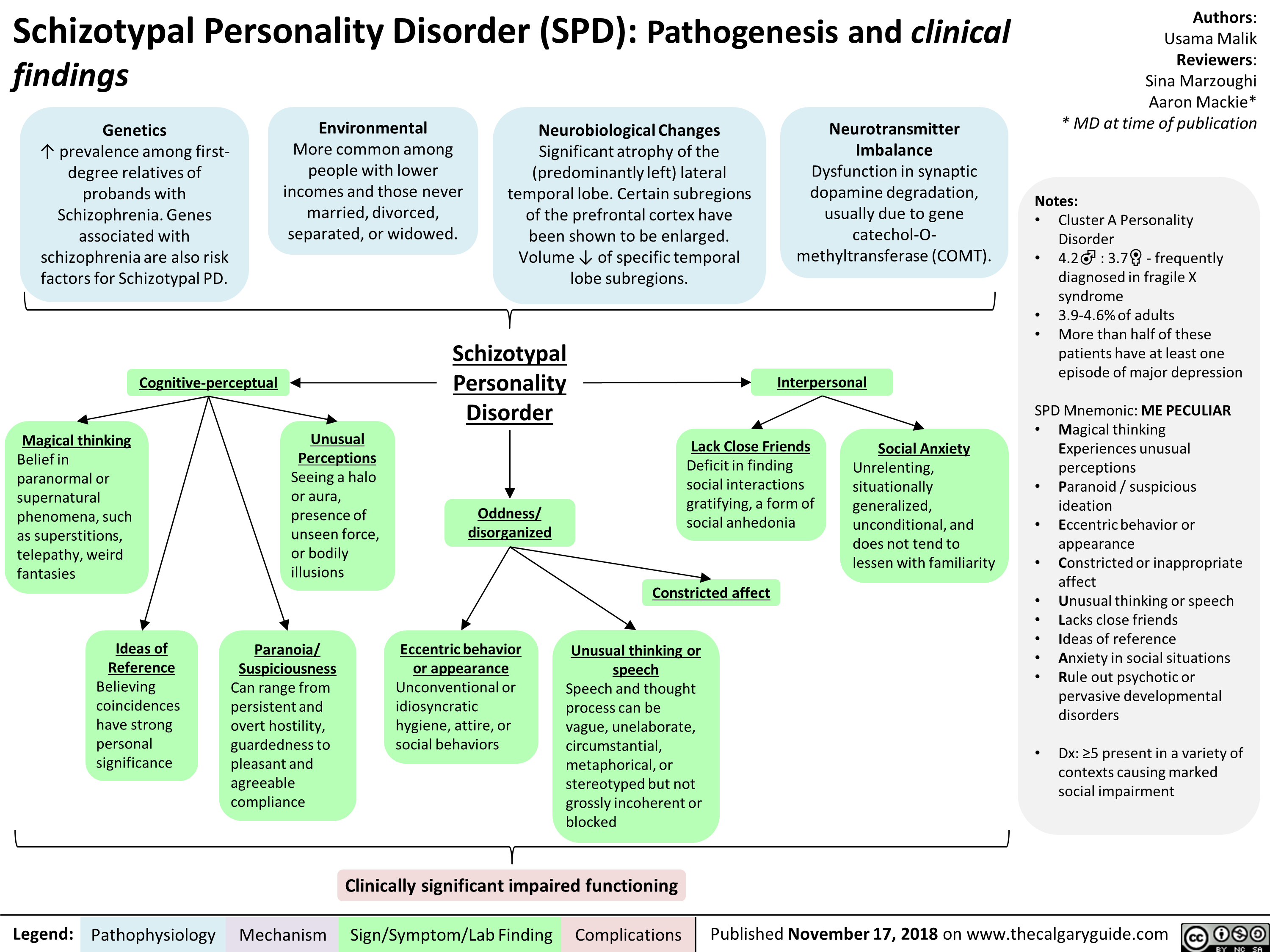
Boutonniere Deformity: Pathogenesis and Complications
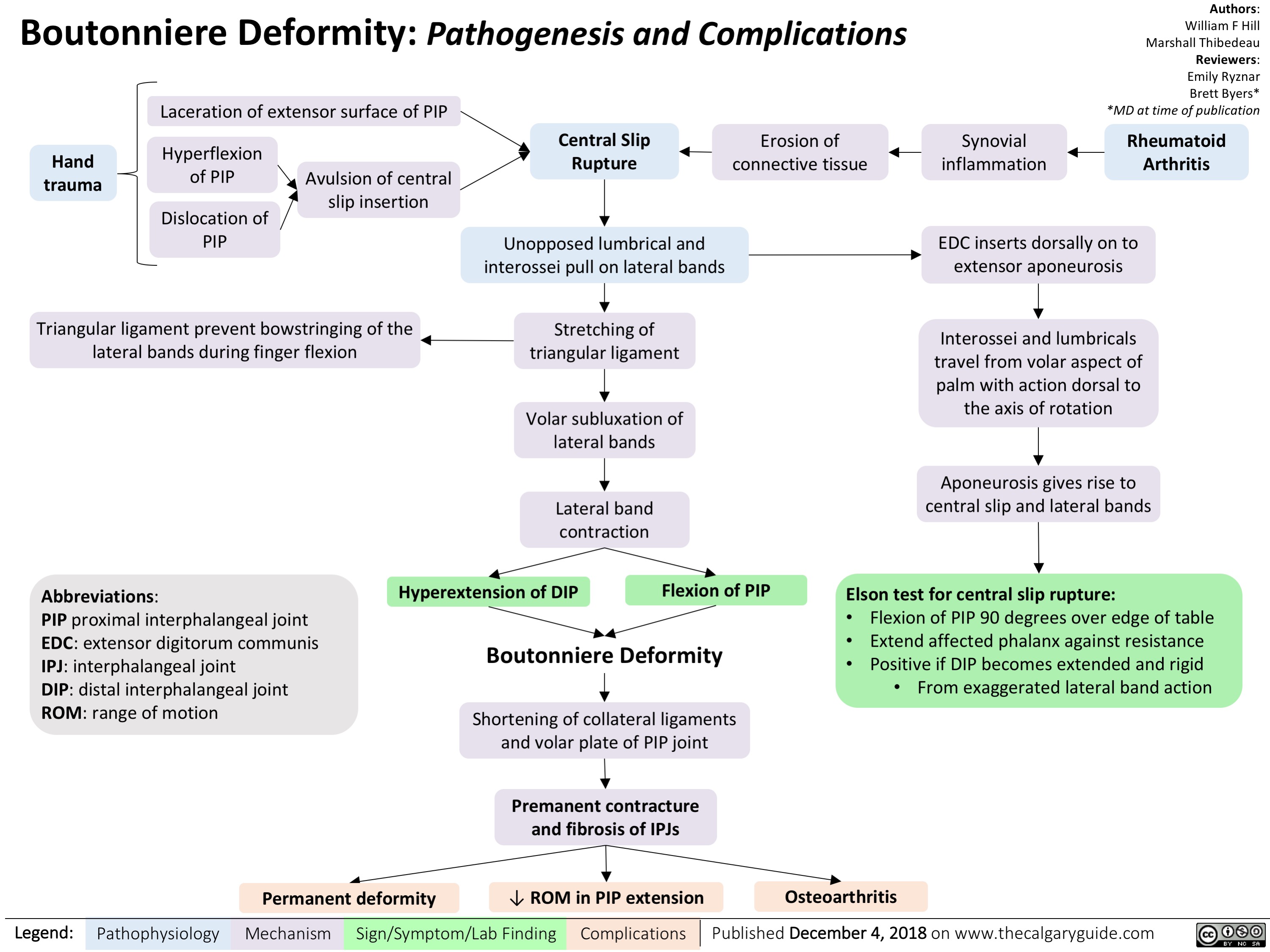
menstrual-cycle-physiology-ovarian-cycle-brief-overview
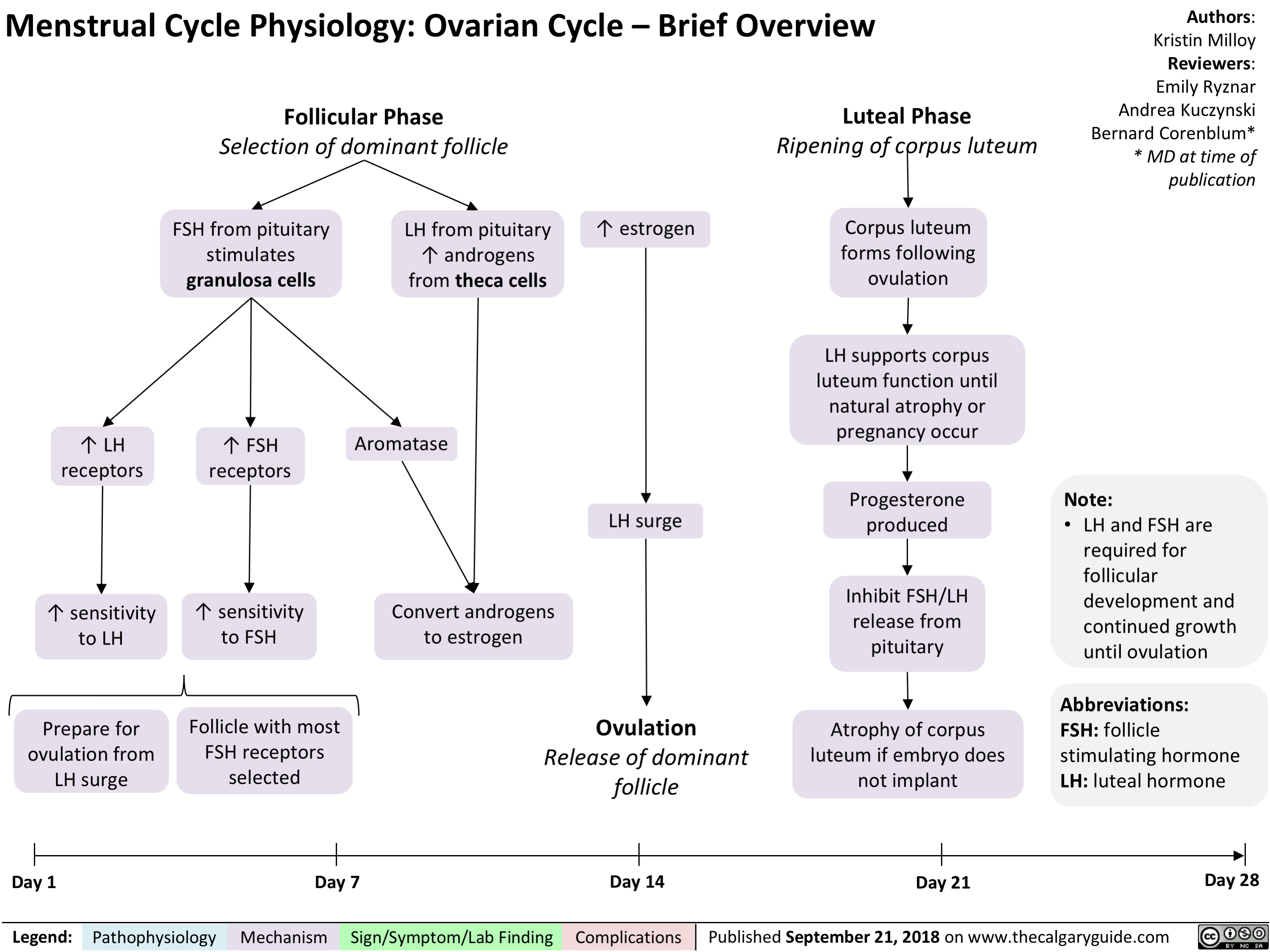
Complex Regional Pain Syndrome: Pathogenesis and clinical findings
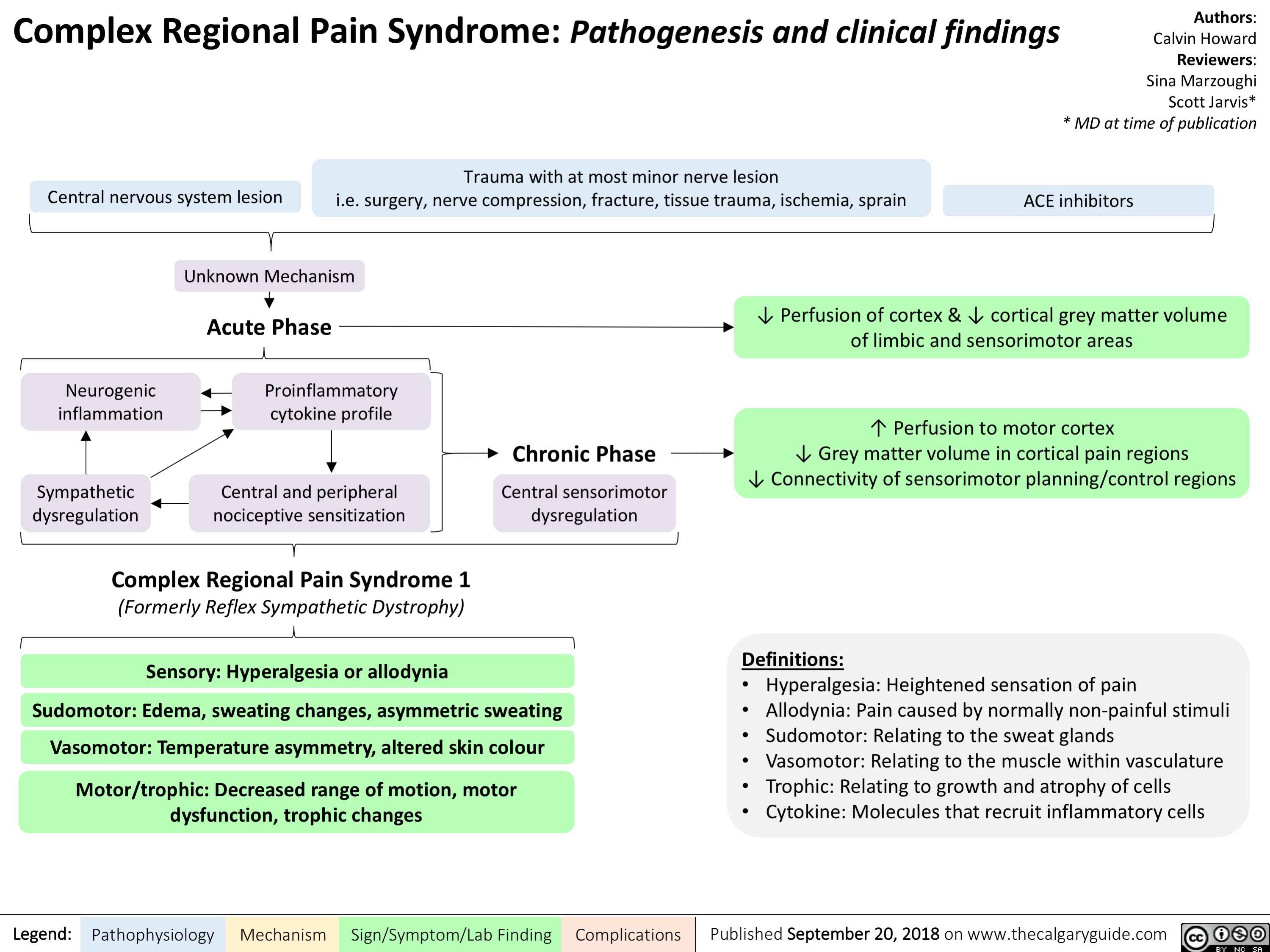
Microangiopathic Hemolytic Anemia: Pathogenesis and clinical findings
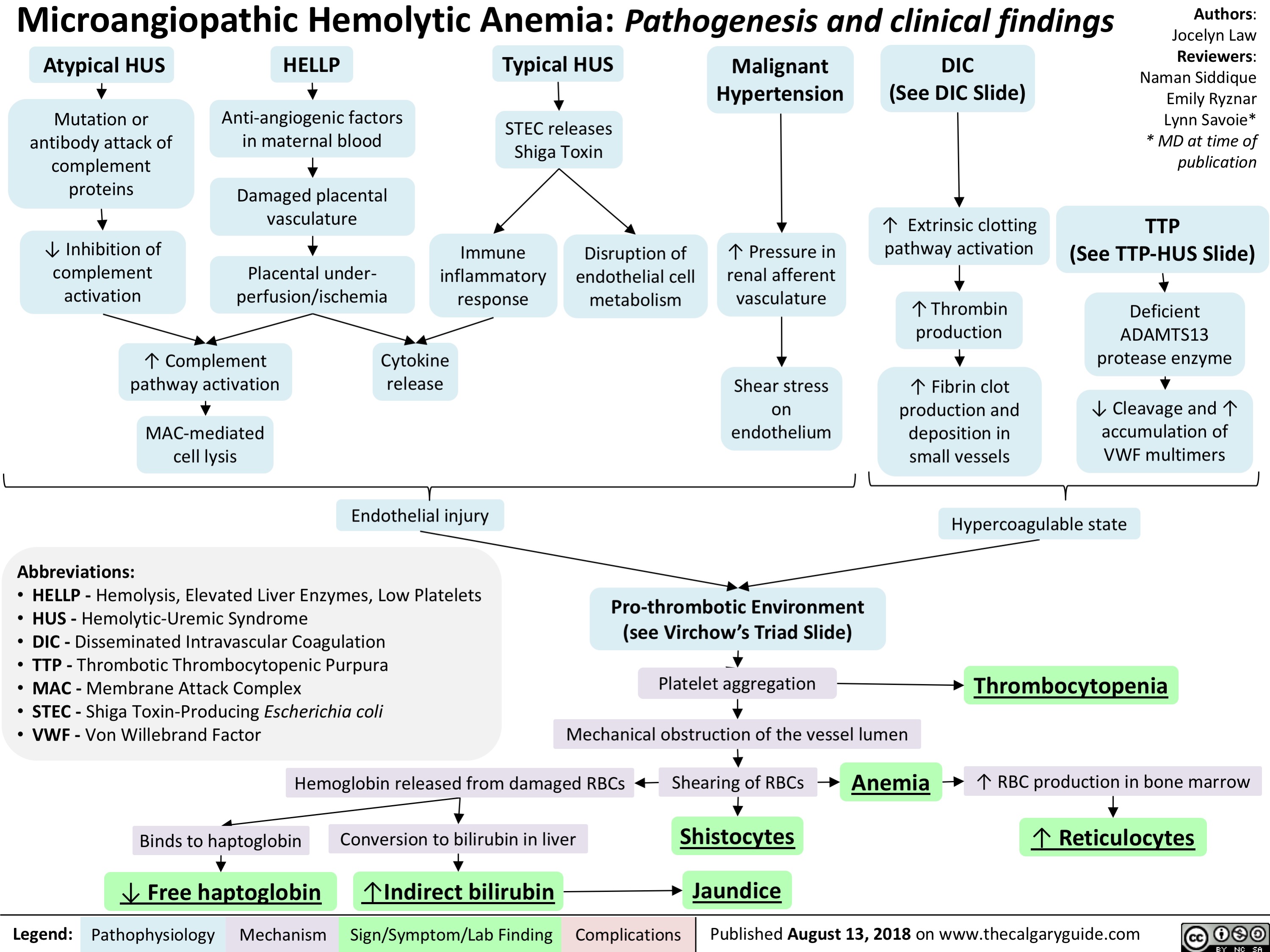
Neurogenic Claudication: Pathogenesis and Clinical Findings
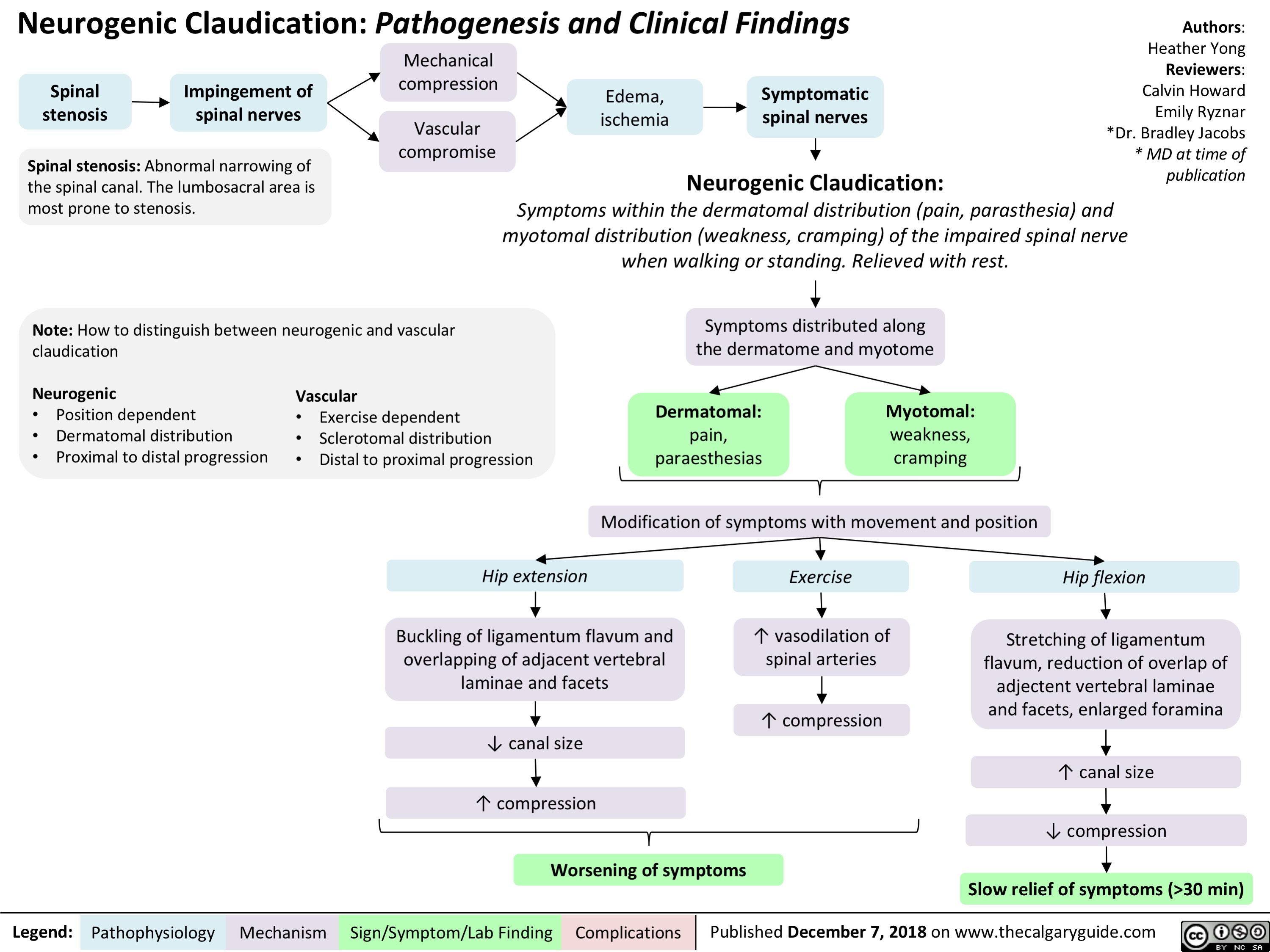
Atopic Dermatitis: Pathogenesis and Clinical Findings
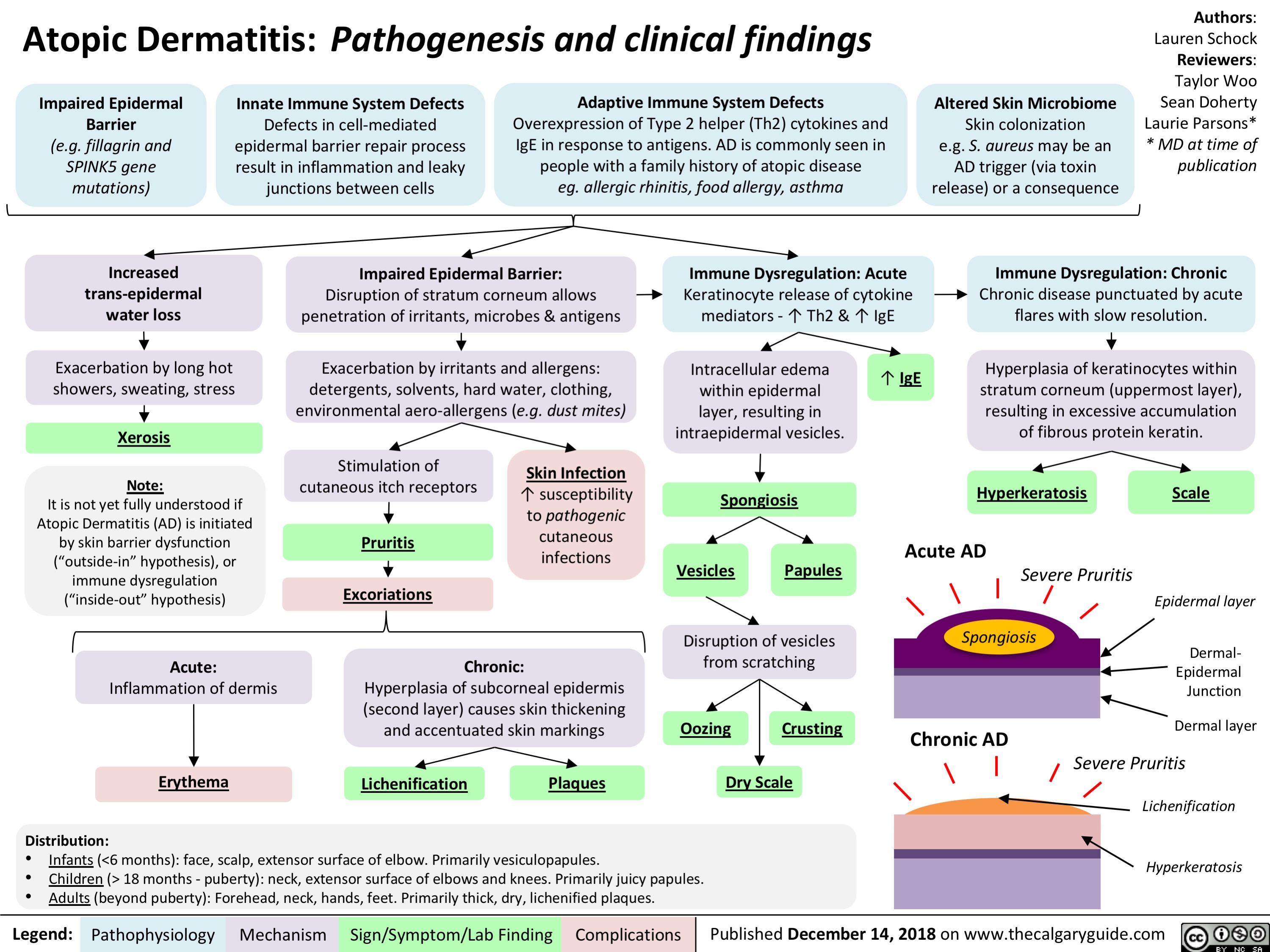
Rosacea: Pathogenesis and Clinical Findings
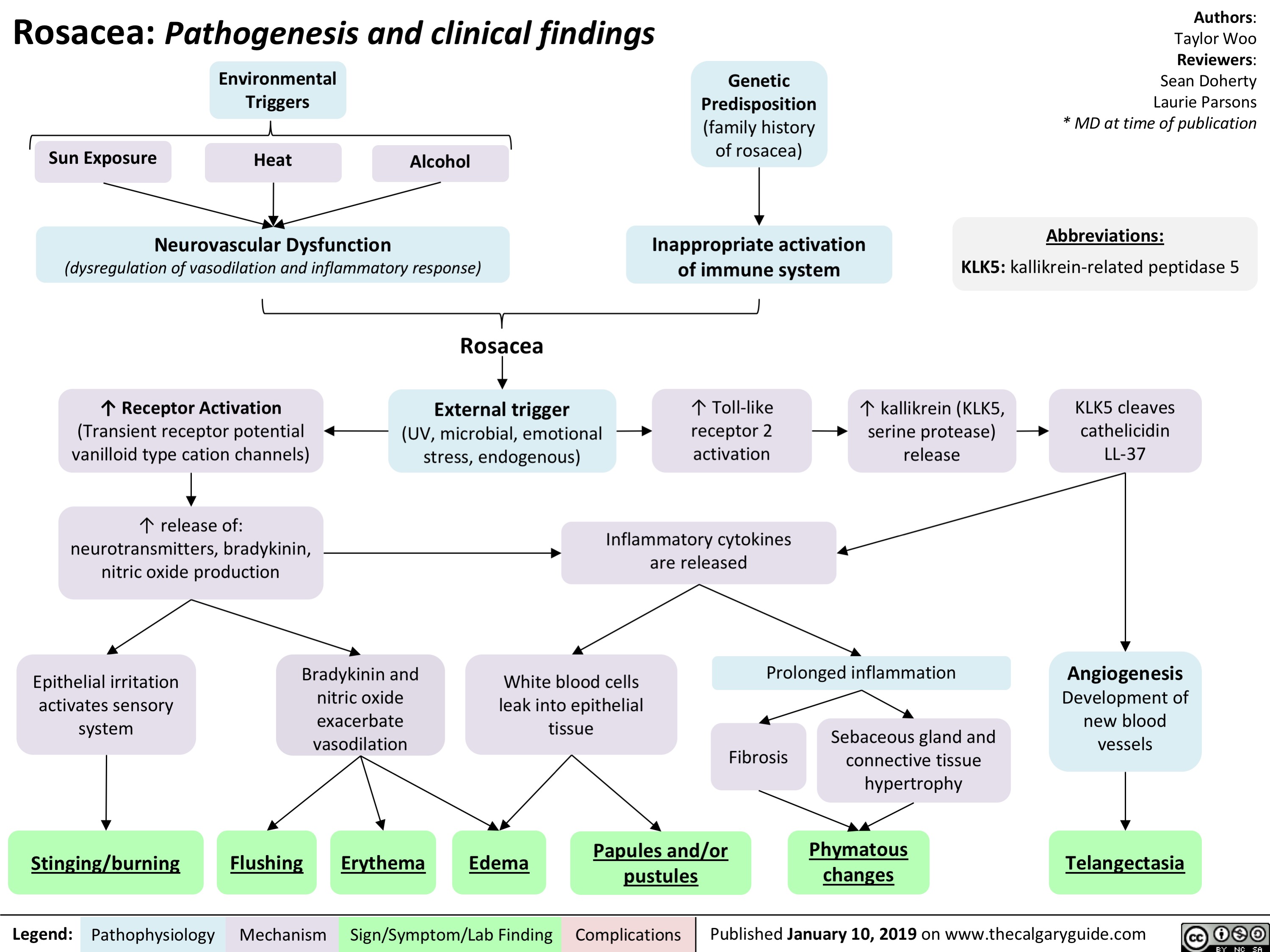
Hepatic Encephalopathy: Pathogenesis and Clinical Findings
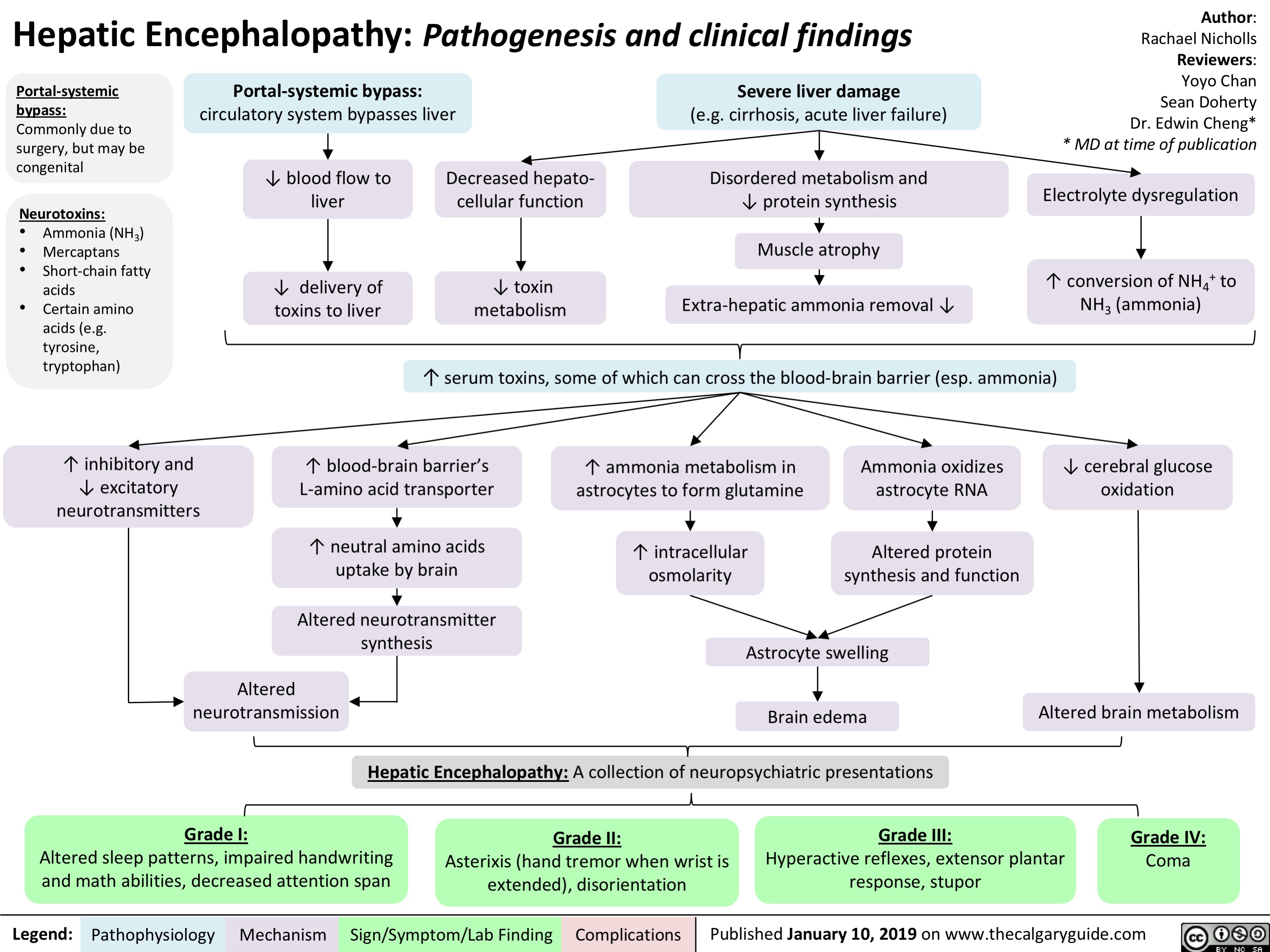
Hypernatremia Physiology
![Hypernatremia: Physiology Unreplaced H2O loss
Hypodipsia
H2O shift into cells
Severe exercise, electroshock induced seizures
Transient ↑ cell osmolality
Na+ overload
Inappropriate IV hypertonic solution, salt poisoning
Abbreviations:
H2O: Water
GI: Gastrointestinal
DM: Diabetes Mellitus
DI: Diabetes Insipidus
Na+: Sodium ion
IV: Intravenous
ADH: Antidiuretic Hormone LOC: Level of Consciousness
Skin
Sweat, burns
GI
Vomiting, bleeding, osmotic diarrhea
Fluid [Na+] < serum [Na+]
↑ H2O loss compared to Na+ loss
Renal
DM, Mannitol, Diuretics
Absent thirst mechanism
Hypothalamic lesion impairs normal drive for H2O intake
Nephrogenic
↑ renal resistance to ADH
H2O Deprivation Test + no AVP response
↓ access to H2O
DI
Central
↓ ADH secretion
H2O Deprivation Test + AVP response
↑ [Na+] 10- 15 mEq/L within a few minutes
Weakness, irritability, seizures, coma
↑ thirst, ↓ urinary frequency and volume
Note:
Hypernatremia
Serum [Na+] > 145 mmol/L
Intracranial hemorrhage
Headache, vomiting, ↓ LOC
• Plasma [Na+] is regulated by water intake/excretion, not by changes in [Na+].
• Effects on plasma [Na+] of IV fluids or loss of bodily fluids is determined by the tonicity of the fluid, not the osmolality.
Authors: Mannat Dhillon Reviewers: Andrea Kuczynski Kevin McLaughlin* * MD at time of publication
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published January 11, 2019 on www.thecalgaryguide.com
Hypernatremia: Physiology Unreplaced H2O loss
Hypodipsia
H2O shift into cells
Severe exercise, electroshock induced seizures
Transient ↑ cell osmolality
Na+ overload
Inappropriate IV hypertonic solution, salt poisoning
Abbreviations:
H2O: Water
GI: Gastrointestinal
DM: Diabetes Mellitus
DI: Diabetes Insipidus
Na+: Sodium ion
IV: Intravenous
ADH: Antidiuretic Hormone LOC: Level of Consciousness
Skin
Sweat, burns
GI
Vomiting, bleeding, osmotic diarrhea
Fluid [Na+] < serum [Na+]
↑ H2O loss compared to Na+ loss
Renal
DM, Mannitol, Diuretics
Absent thirst mechanism
Hypothalamic lesion impairs normal drive for H2O intake
Nephrogenic
↑ renal resistance to ADH
H2O Deprivation Test + no AVP response
↓ access to H2O
DI
Central
↓ ADH secretion
H2O Deprivation Test + AVP response
↑ [Na+] 10- 15 mEq/L within a few minutes
Weakness, irritability, seizures, coma
↑ thirst, ↓ urinary frequency and volume
Note:
Hypernatremia
Serum [Na+] > 145 mmol/L
Intracranial hemorrhage
Headache, vomiting, ↓ LOC
• Plasma [Na+] is regulated by water intake/excretion, not by changes in [Na+].
• Effects on plasma [Na+] of IV fluids or loss of bodily fluids is determined by the tonicity of the fluid, not the osmolality.
Authors: Mannat Dhillon Reviewers: Andrea Kuczynski Kevin McLaughlin* * MD at time of publication
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published January 11, 2019 on www.thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2019/01/Hypernatremia-Physiology-.jpg)
Hyponatremia- Physiology
![Hyponatremia: Physiology
Authors: Mannat Dhillon Reviewers: Andrea Kuczynski Kevin McLaughlin* * MD at time of publication
Abnormal Renal H2O Handling (hypo-osmolar serum)
AKI/CKD Heart failure
↓ renal blood flow
↓ glomerular filtration
GFR < 25 mL/min, ↓ urine dilution ↑ H2O retention
Note:
• Plasma [Na+] is regulated by water intake/excretion, not by changes in [Na+].
• Artifactual hyponatremia can be differentiated by a normal or hyperosmolar serum.
Appropriate ADH secretion
↓ EABV
Hypovolemia: losses via GI, renal, skin, 3rd spacing, bleeding
Hypervolemia: heart failure, cirrhosis
↑ Na+/H2O absorption at PCT
↓ EABV, ↑ H2O retention
Urine [Na+] < 20 mmol/L
Hereditary: tubular disorders
(Bartter, Gitlemann syndromes).
Thiazide diuretics
Inappropriate: SIADH, hypothyroidism, AI
Normal EABV
Anti-diuresis
Primary polydipsia, eating disorder
↑ H2O or ↓ solute intake
↓ Osmoles
Impaired desalination
Block NCC
↑ H2O retention ↑ Na+/K+ excretion
Hyponatremia
Serum [Na+] < 135 mmol/L
Urine osmolality > 100 mmol/L
Urine osmolality < 100 mmol/L
Cerebral edema, ↑ intracranial pressure, vasoconstriction
If hypovolemic: ↓ JVP, ↓ blood pressure
Lethargy, altered mental status
Abbreviations:
AKI: Acute Kidney Injury
CKD: Chronic Kidney Disease
GFR: Glomerular Filtration Rate
H2O: Water
PCT: Proximal Convoluted Tubule
EABV: Effective Arterial Blood Volume
NCC: Na+/Cl- Co-Transporter
SIADH: Syndrome of Inappropriate ADH Secretion AI: Adrenal Insufficiency
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published January 11, 2019 on www.thecalgaryguide.com
Hyponatremia: Physiology
Authors: Mannat Dhillon Reviewers: Andrea Kuczynski Kevin McLaughlin* * MD at time of publication
Abnormal Renal H2O Handling (hypo-osmolar serum)
AKI/CKD Heart failure
↓ renal blood flow
↓ glomerular filtration
GFR < 25 mL/min, ↓ urine dilution ↑ H2O retention
Note:
• Plasma [Na+] is regulated by water intake/excretion, not by changes in [Na+].
• Artifactual hyponatremia can be differentiated by a normal or hyperosmolar serum.
Appropriate ADH secretion
↓ EABV
Hypovolemia: losses via GI, renal, skin, 3rd spacing, bleeding
Hypervolemia: heart failure, cirrhosis
↑ Na+/H2O absorption at PCT
↓ EABV, ↑ H2O retention
Urine [Na+] < 20 mmol/L
Hereditary: tubular disorders
(Bartter, Gitlemann syndromes).
Thiazide diuretics
Inappropriate: SIADH, hypothyroidism, AI
Normal EABV
Anti-diuresis
Primary polydipsia, eating disorder
↑ H2O or ↓ solute intake
↓ Osmoles
Impaired desalination
Block NCC
↑ H2O retention ↑ Na+/K+ excretion
Hyponatremia
Serum [Na+] < 135 mmol/L
Urine osmolality > 100 mmol/L
Urine osmolality < 100 mmol/L
Cerebral edema, ↑ intracranial pressure, vasoconstriction
If hypovolemic: ↓ JVP, ↓ blood pressure
Lethargy, altered mental status
Abbreviations:
AKI: Acute Kidney Injury
CKD: Chronic Kidney Disease
GFR: Glomerular Filtration Rate
H2O: Water
PCT: Proximal Convoluted Tubule
EABV: Effective Arterial Blood Volume
NCC: Na+/Cl- Co-Transporter
SIADH: Syndrome of Inappropriate ADH Secretion AI: Adrenal Insufficiency
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published January 11, 2019 on www.thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2019/01/Hyponatremia-Physiology-.jpg)
Coronary anatomy on ECG- Localizing Ischemia
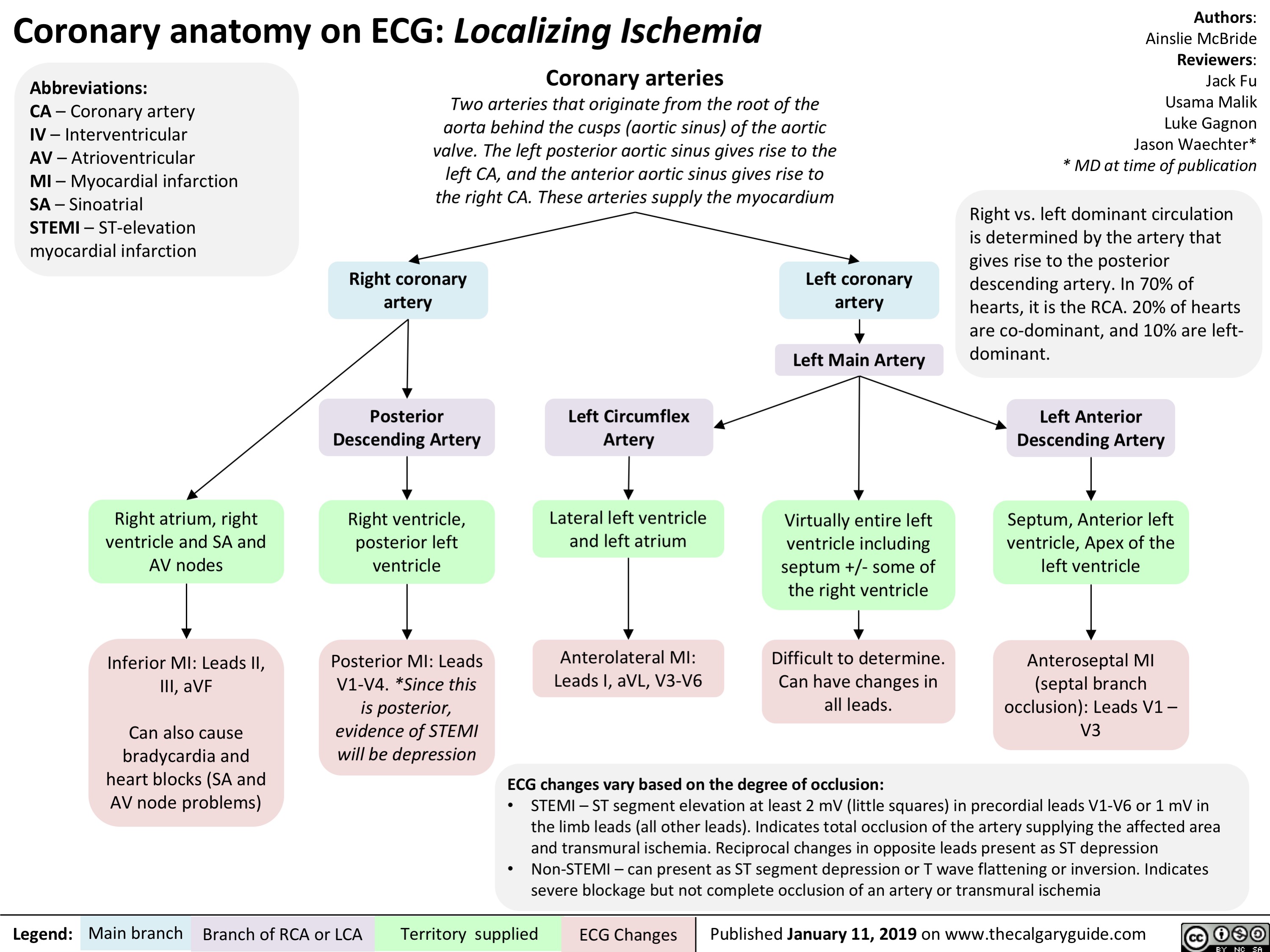
Patent Ductus Arteriosus (PDA)- Pathogenesis and Clinical Findings
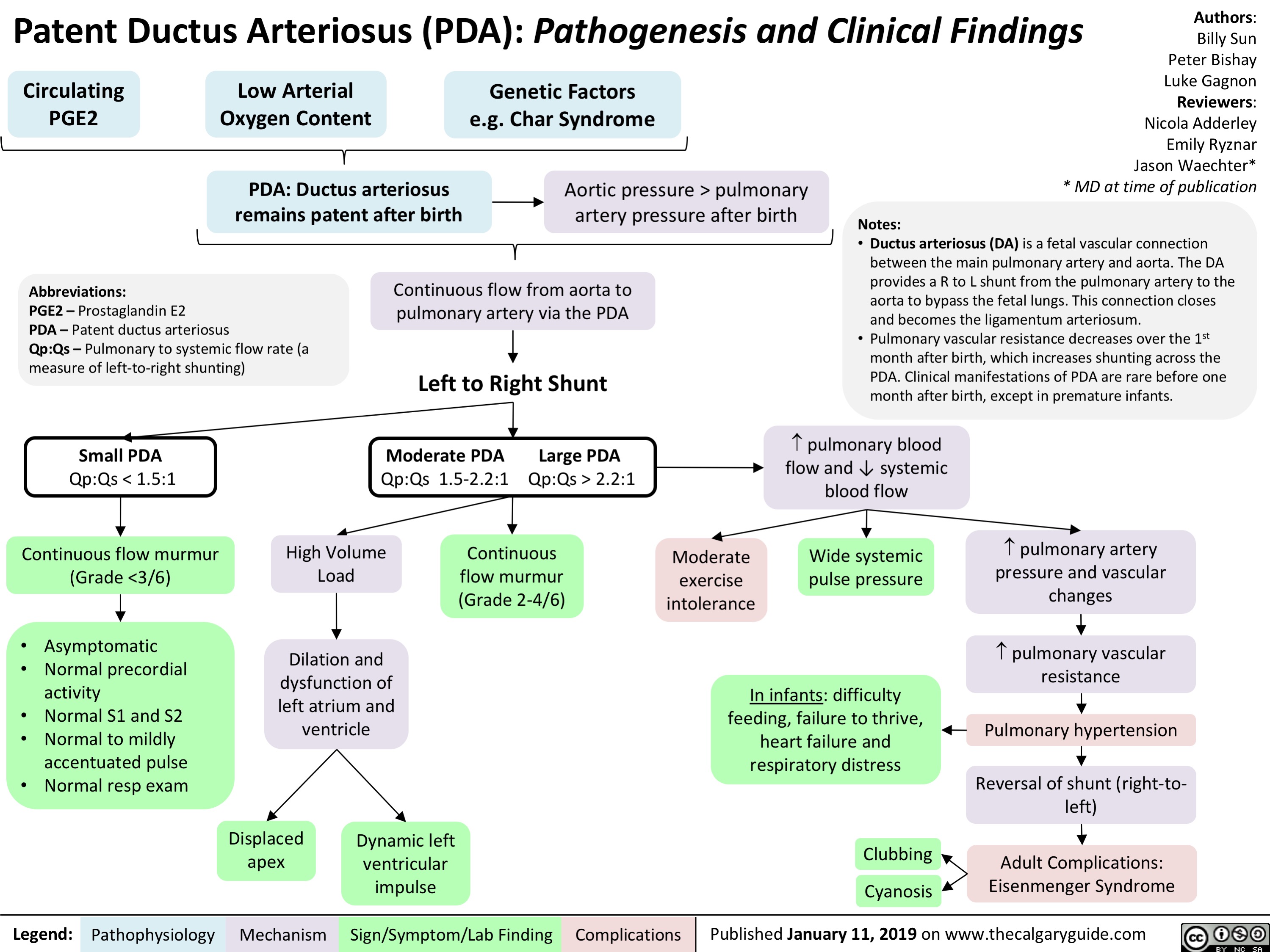
Arterial Insufficiency- Signs and symptoms
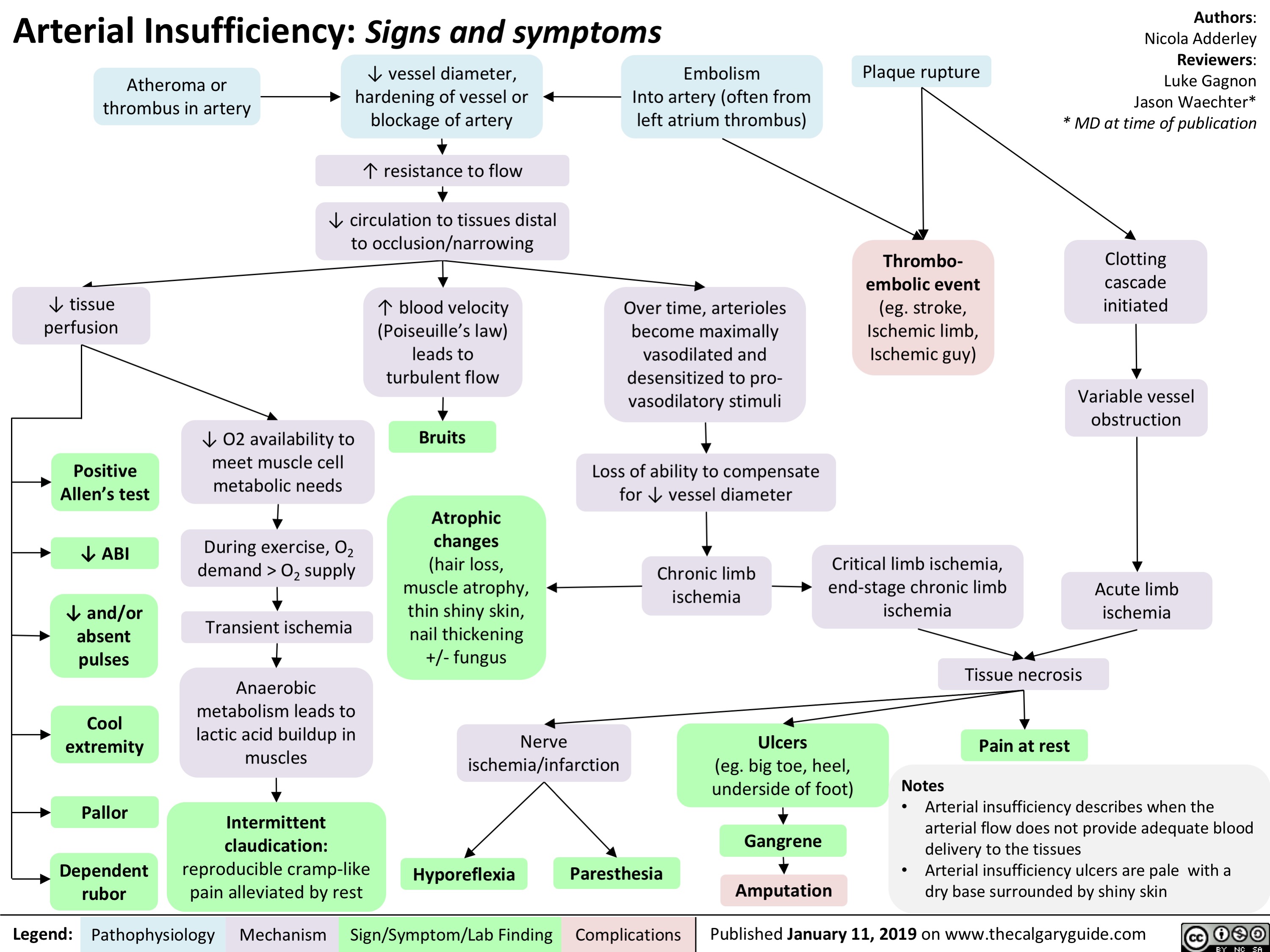
Venous insufficiency- Signs and symptoms
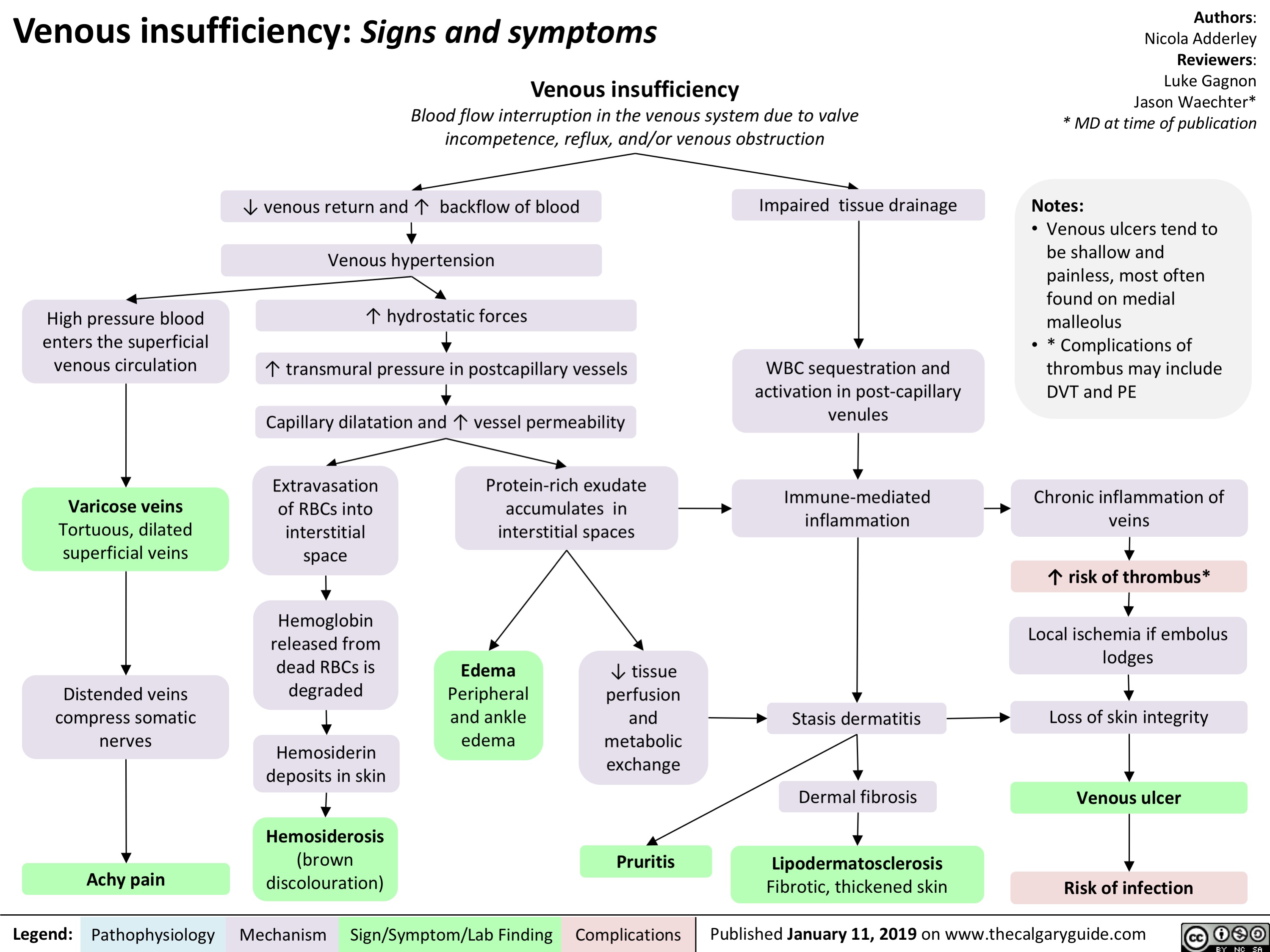
Takotsubo Cardiomyopathy- Pathogenesis and clinical findings
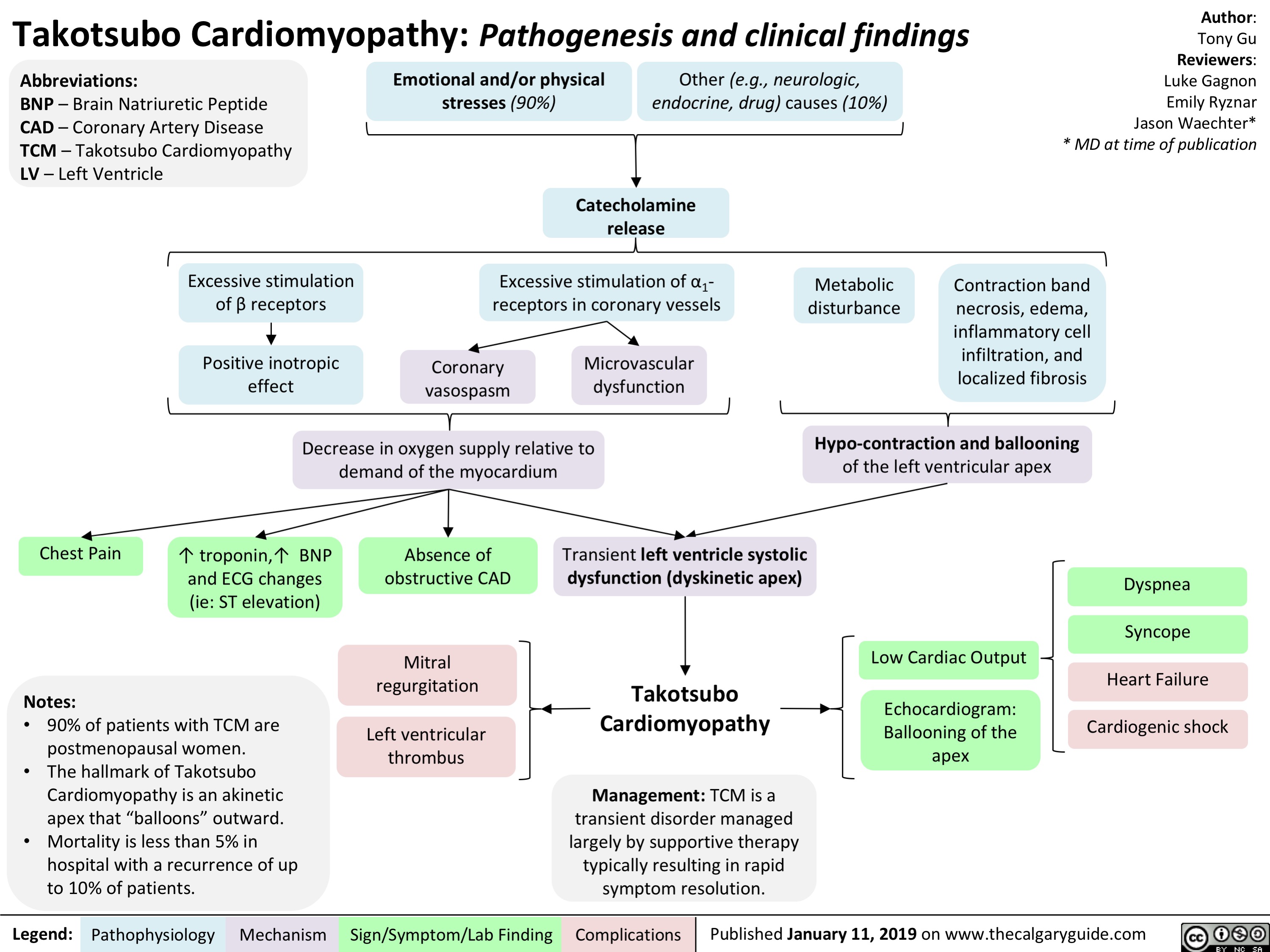
Meralgia paresthetica- Pathogenesis and Clinical Findings
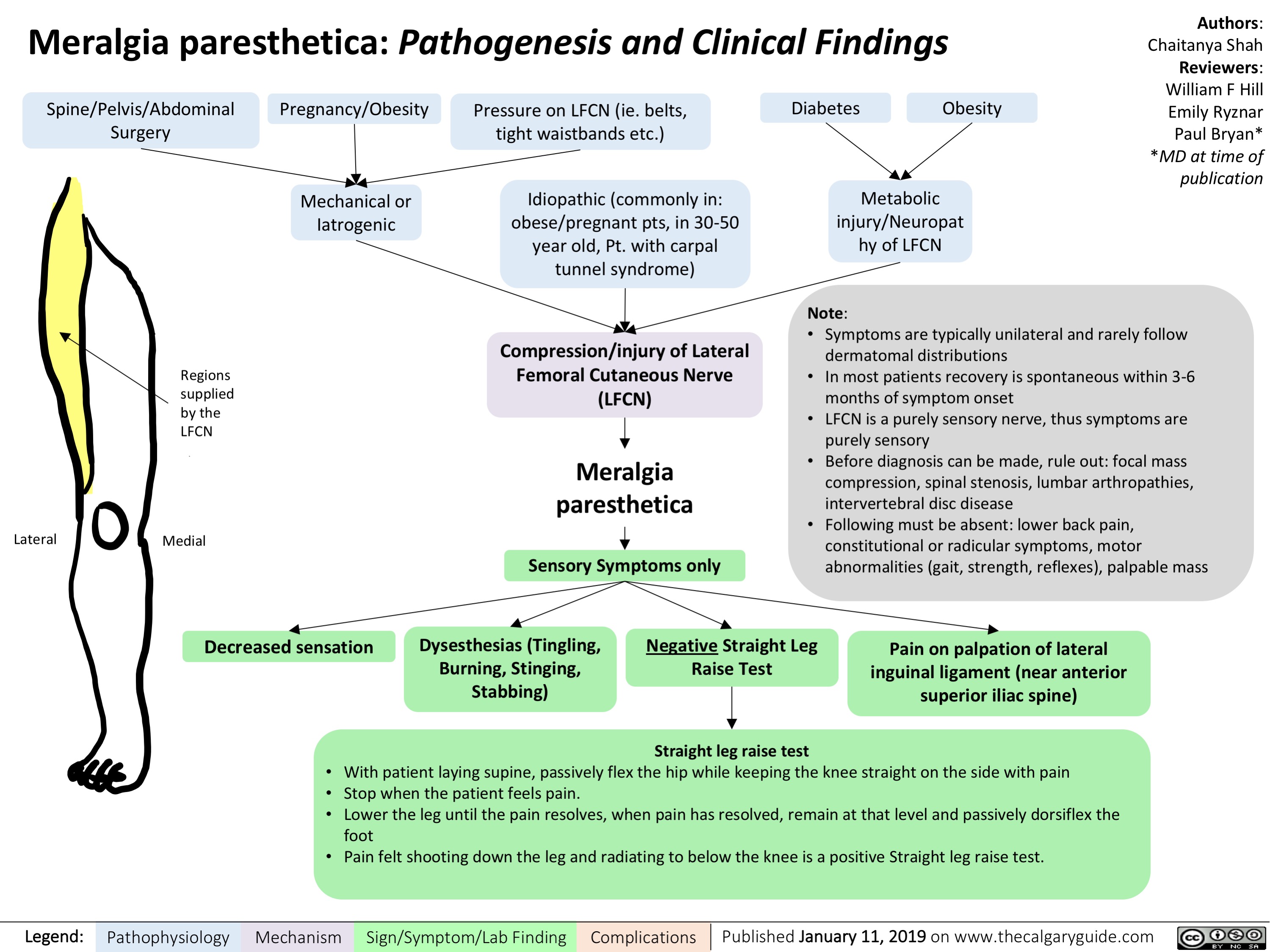
Simple Febrile Seizure- Pathogenesis and clinical findings
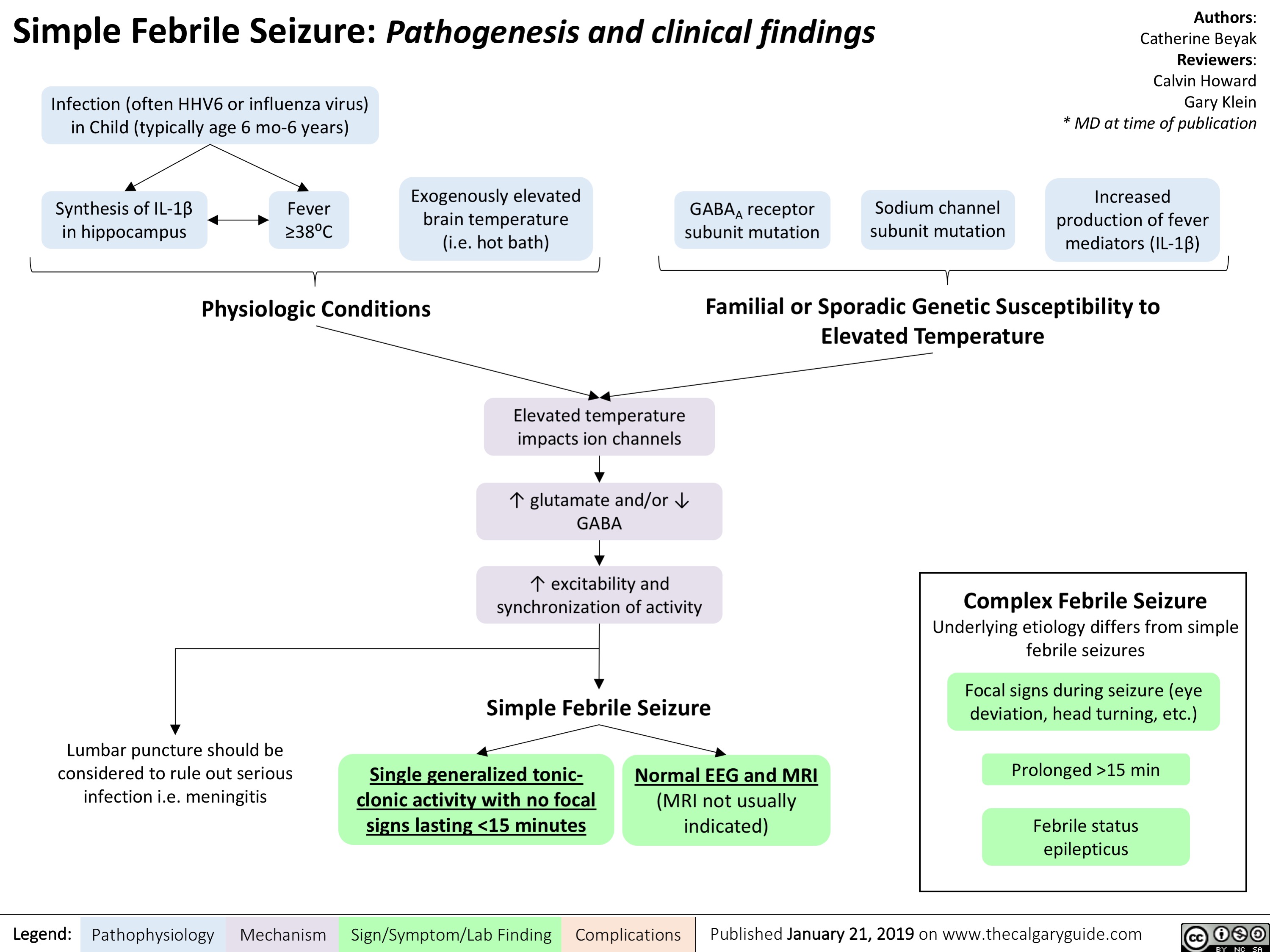
Reactive Neutrophilia- Pathogenesis and Clinical Findings
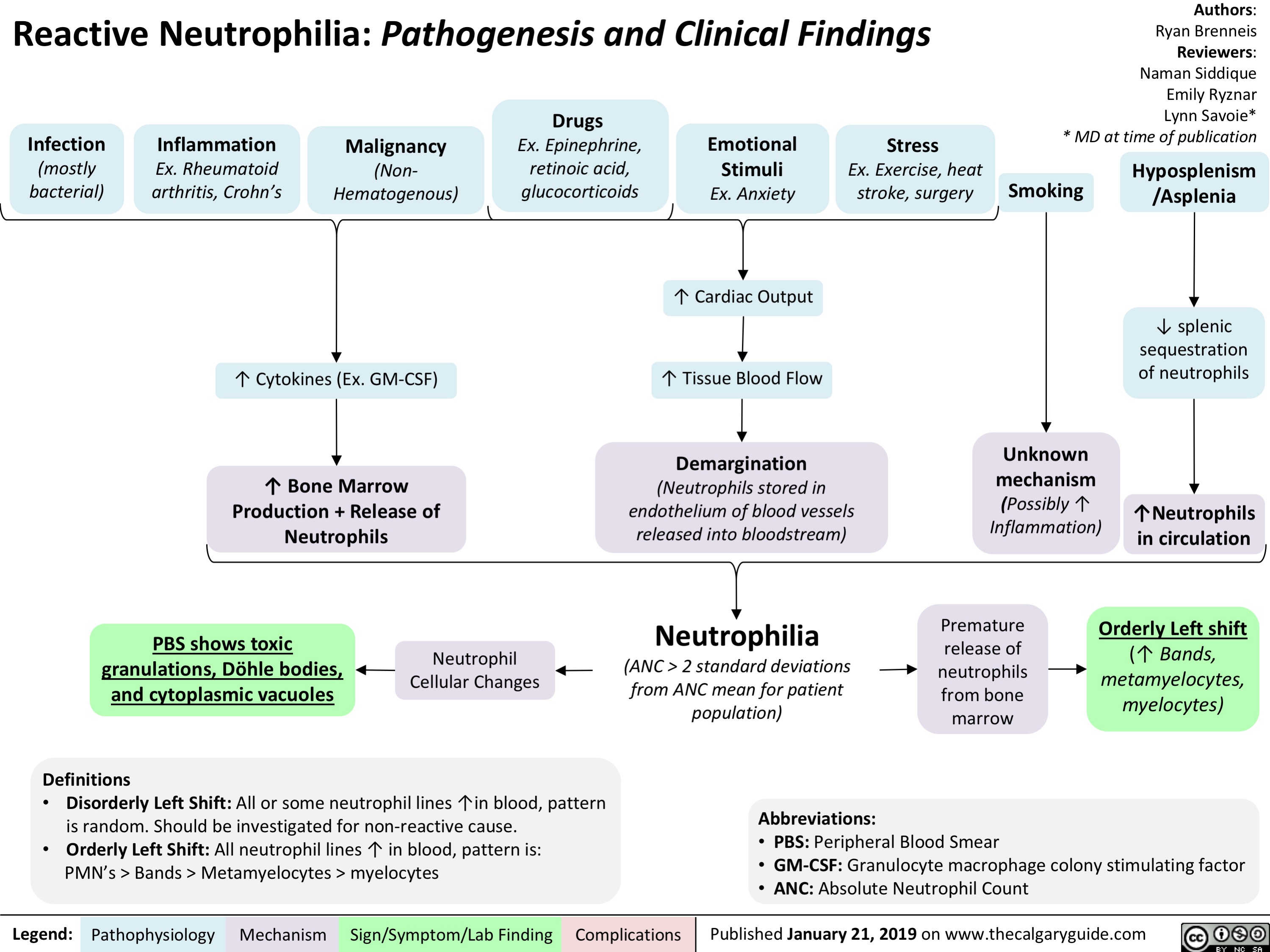
Hypoxemia- Pathogenesis and clinical findings
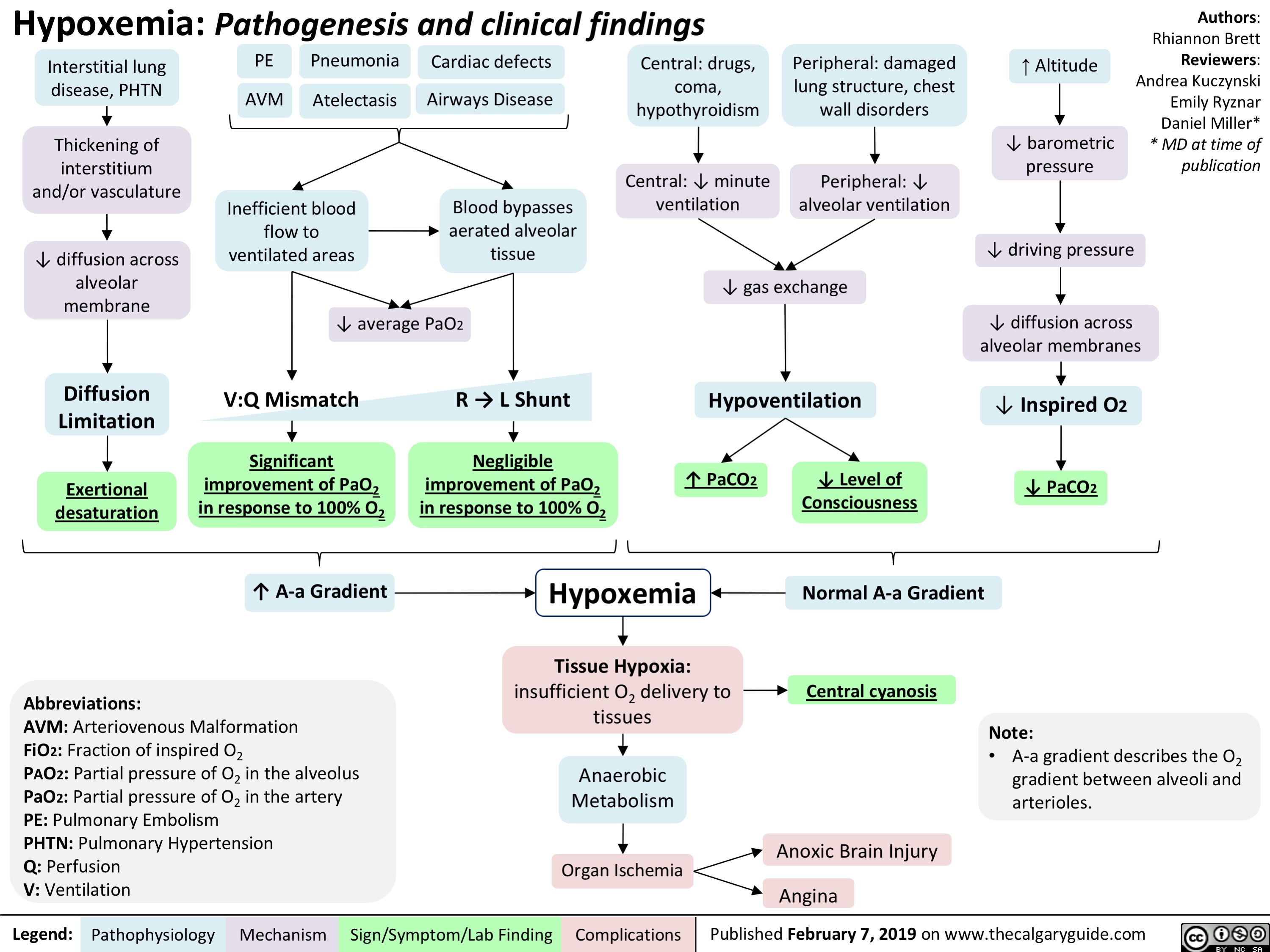
Bronchopulmonary Dysplasia (BPD)- Pathogenesis and clinical findings
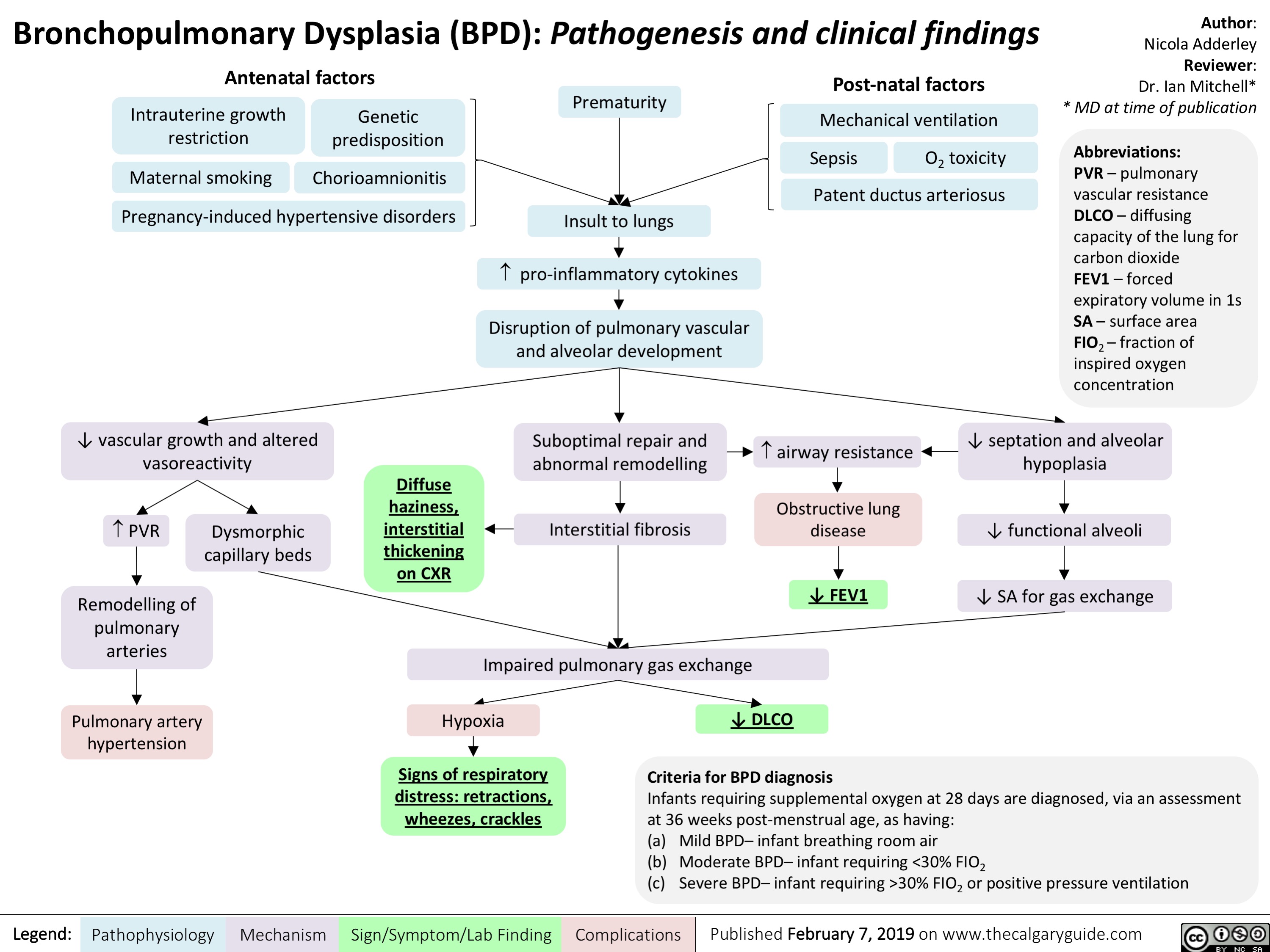
Neuromuscular Junction (NMJ)- Physiology and pharmacology
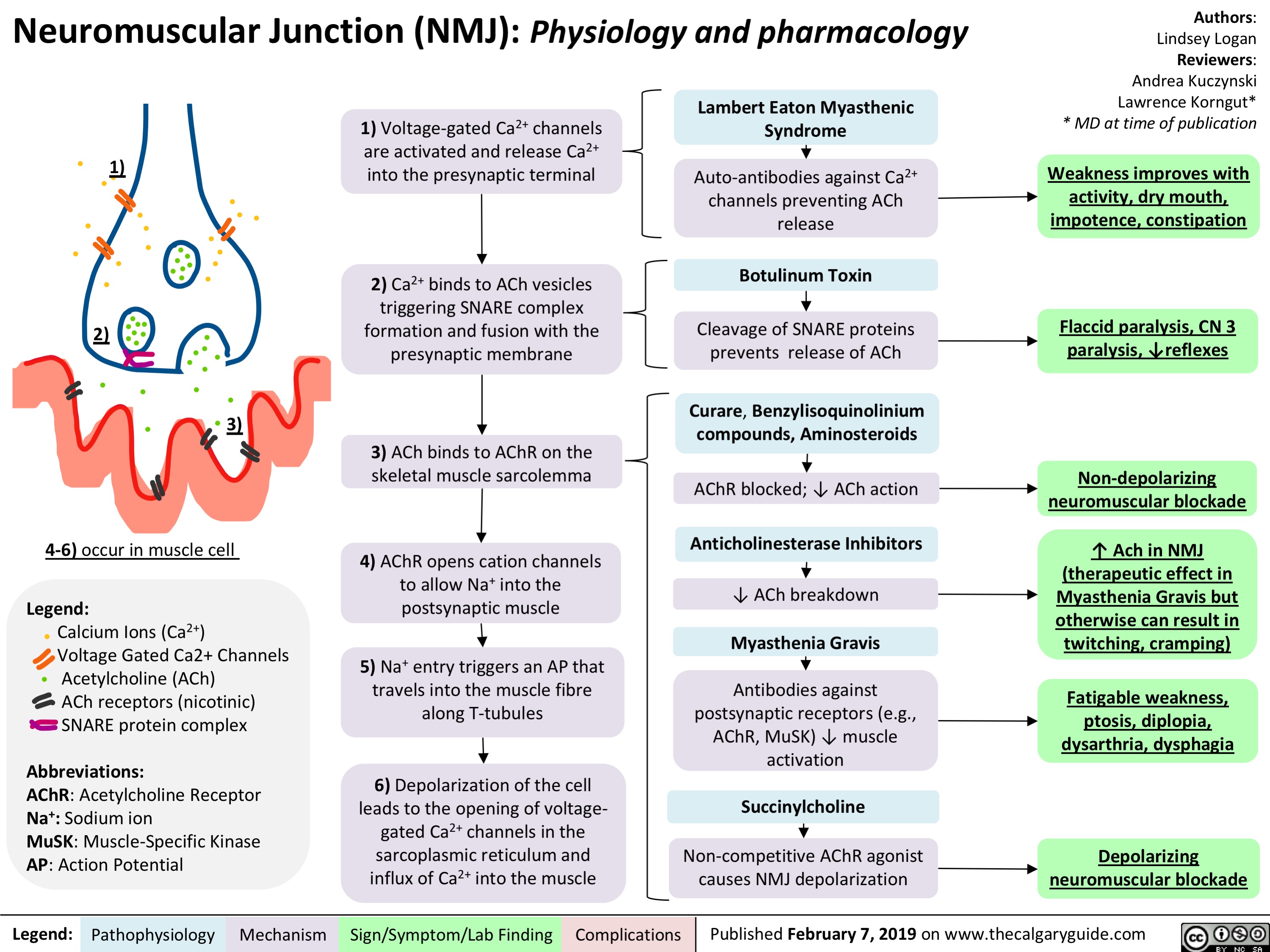
Biliary Atresia (BA)- Pathogenesis and clinical findings
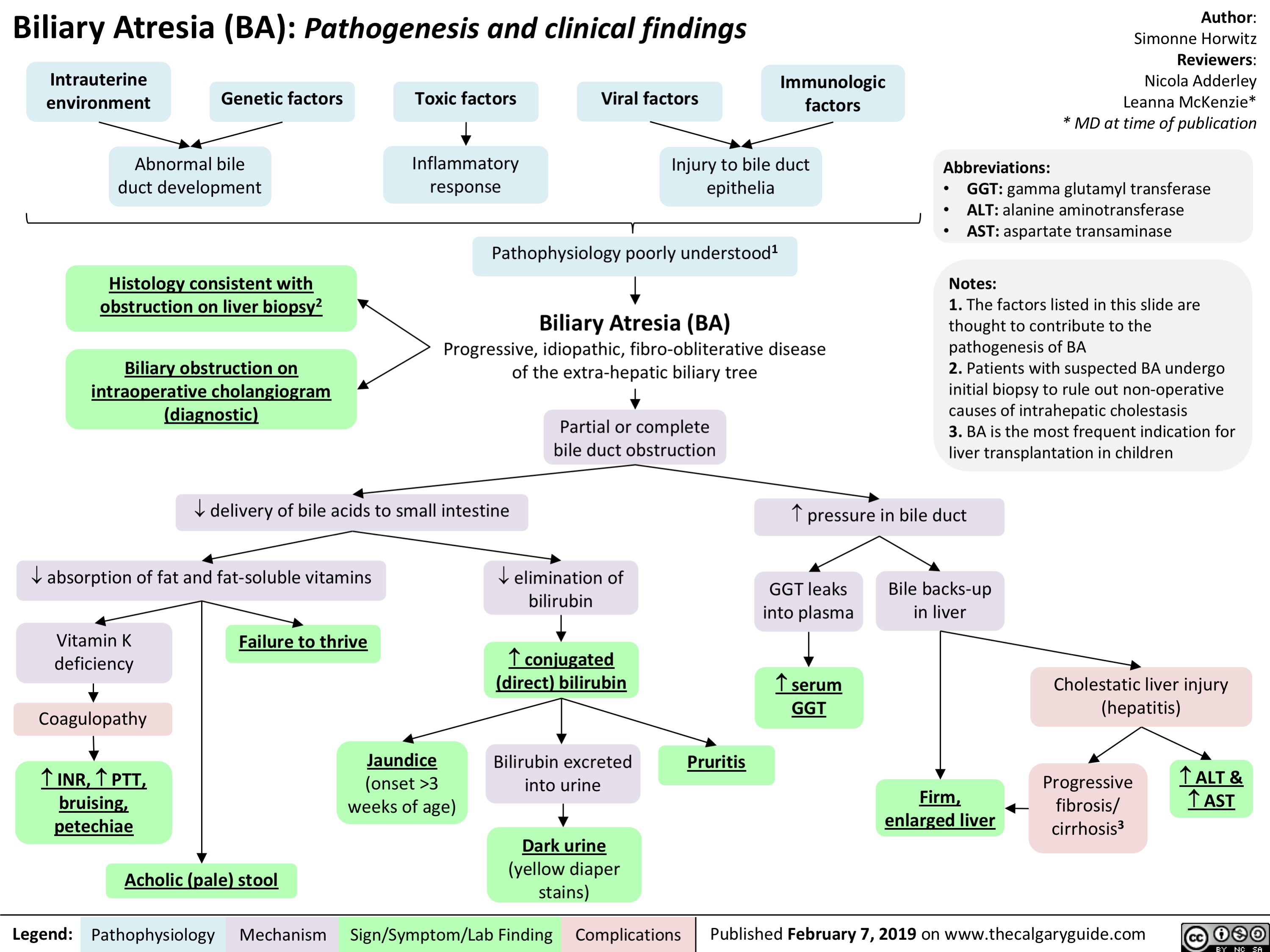
Inflammatory-Cascade-Pathogenesis-and-Clinical-Findings
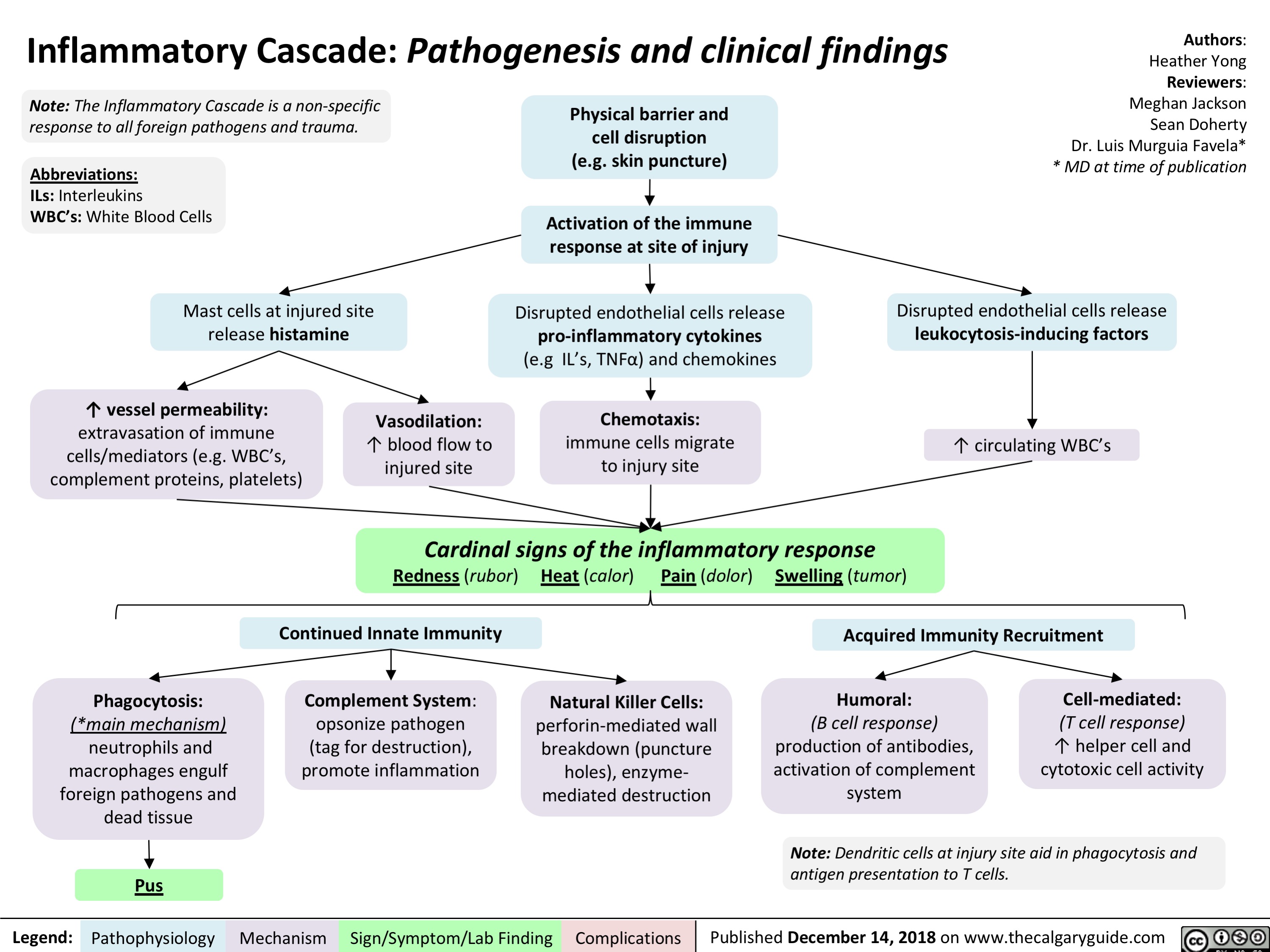
Sepsis, and Septic Shock- Pathogenesis and Clinical Findings
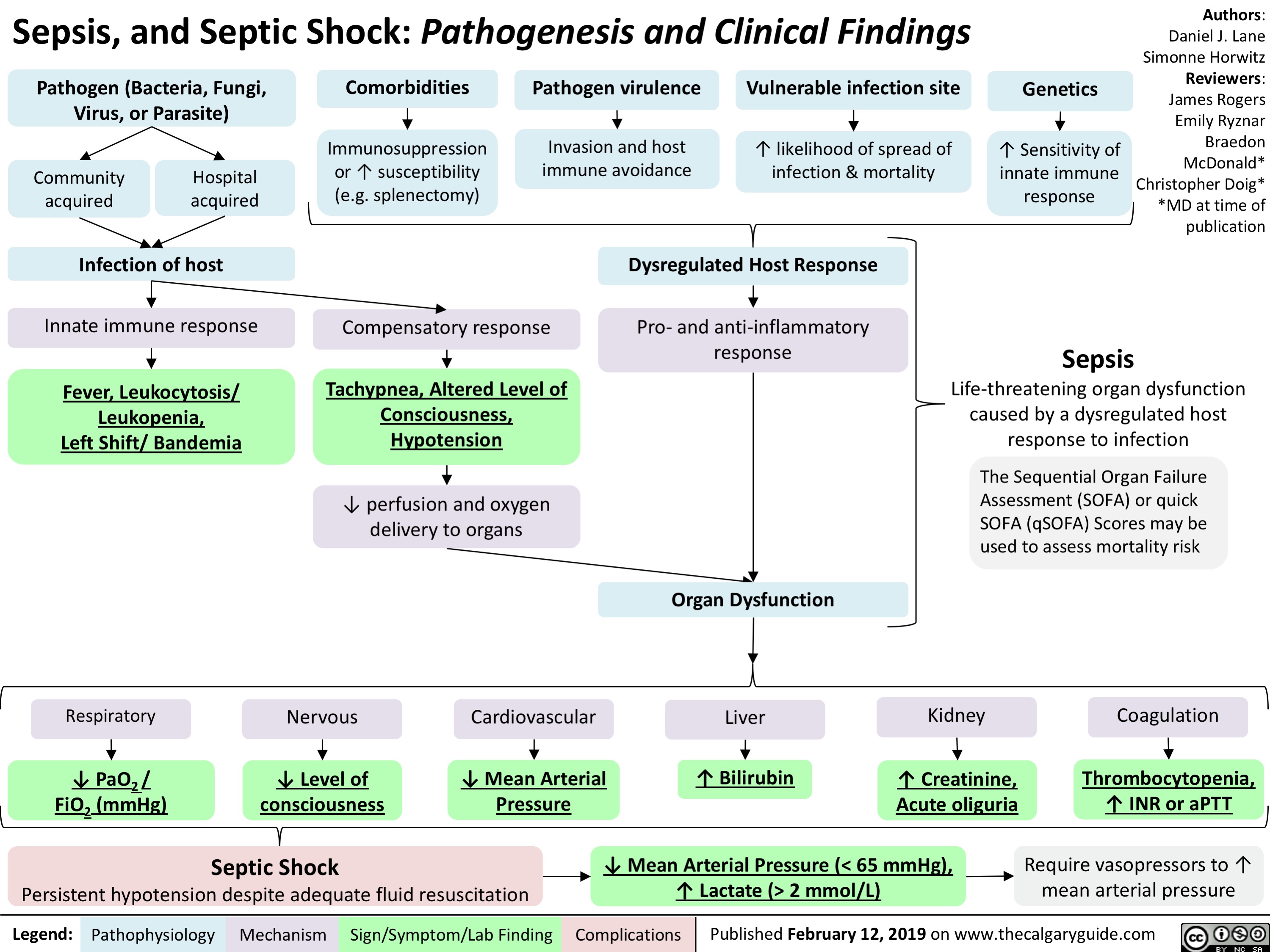
adrenergic-agonists-for-treating-hypotensionlow-blood-pressure
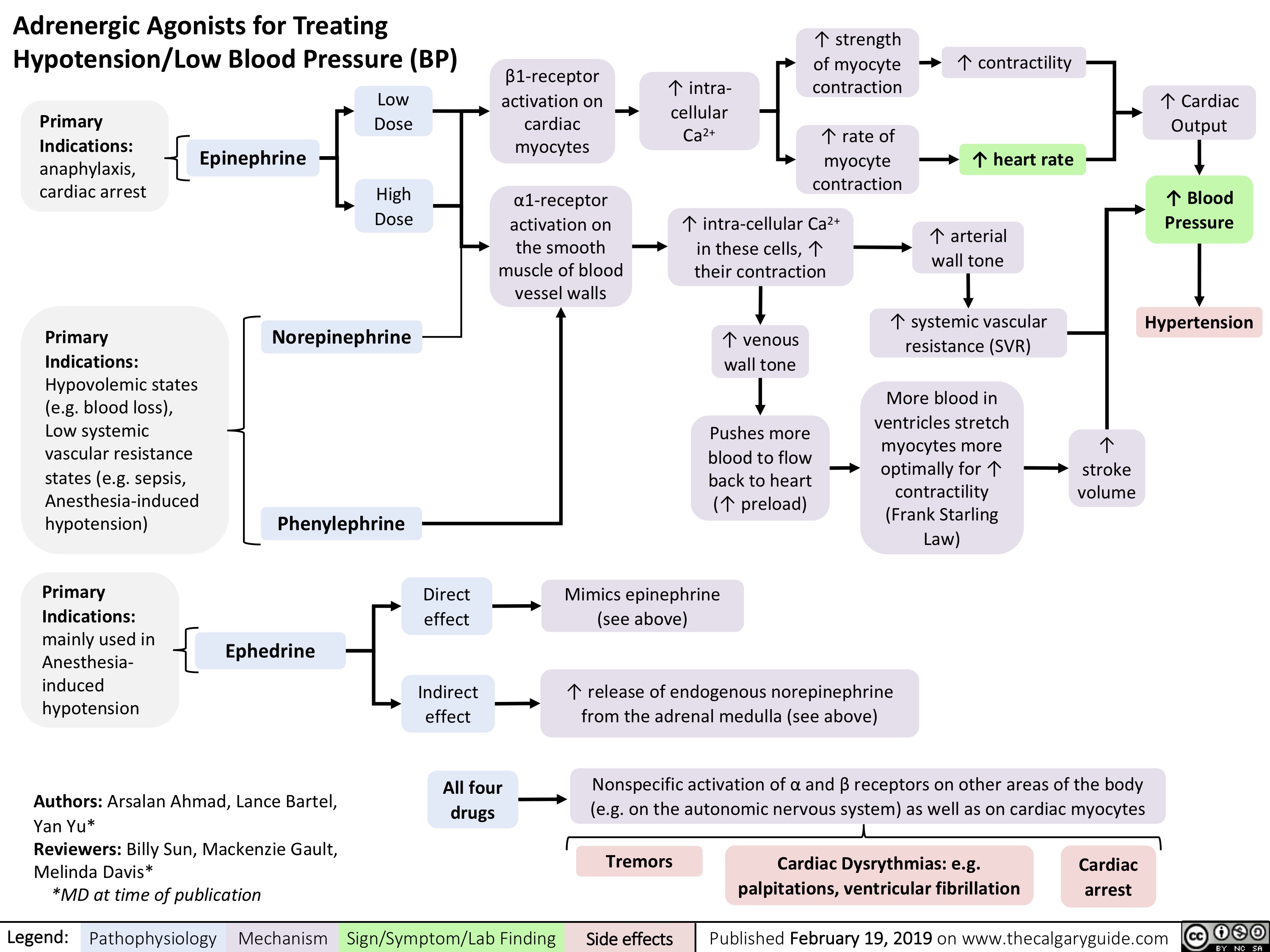
Hyperkalemia- Physiology
![Hyperkalemia: Physiology ↓ Renal Excretion
↑ Intake
↓ Intracellular Shift
Acute and chronic kidney disease; CHF
Principal Cell Dysfunction (TTKG < 7)
ACEi/ARB; AI; heparin
Hypovolemia (TTKG > 7)
↓ EABV
↓ distal flow of Na+ and H2O
Urine [Na+] < 20 mmol/L
Cell lysis
↑ osmolarity H2O efflux
Solvent drag
β2 inhibition α1 stimulation
Digoxin ↓ A
NAGMA ↓ insulin
↓ NHE1 activity
Diabetic nephropathy; NSAIDs
↓ A: ↓ R
K+ sparing diuretics; voltage- dependent RTA
↓ Na+/K+ ATPase activity
↓ GFR
↓ A: ↑ R ↑ A: ↑ R
↓ CCD K+ secretion
↑ K+ availability
↑ K+ release
↓ intracellular K+ influx
Chronic: Desensitize voltage- gated Na+ channels and ↓ membrane excitability
ECG: Peaked T-waves, ↑ PR interval, flat/absent P-wave, ↑ QRS, QRST “sine wave”
Hyperkalemia
Serum [K+] > 5.1 mmol/L
Acute: ↑ extracellular [K+] makes the RMP less (-)
Abbreviations:
A: Aldosterone
AI: Adrenal Insufficiency
CCD: Cortical Collecting Duct
CHF: Congestive Heart Failure
EABV: Effective Arterial Blood Volume H+: Hydrogen ion
K+: Potassium ion
Na+: Sodium ion
NAGMA: Normal Anion Gap Metabolic Acidosis
NSAIDs: Non-steroidal anti-inflammatory drugs Note:
Muscle weakness or paralysis, ↓ urinary acid excretion
R: Renin
RTA: Renal Tubular Acidosis
RMP: Resting Membrane Potential TTKG: Transtubular Potassium Gradient
• Pseudohyperkalemia should always be excluded; can be caused by thrombocytosis, leukocytosis or improper blood withdrawal technique.
Authors: Mannat Dhillon Joshua Low Reviewers: Andrea Kuczynski Kevin McLaughlin* * MD at time of publication
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published March 6, 2019 on www.thecalgaryguide.com
Hyperkalemia: Physiology ↓ Renal Excretion
↑ Intake
↓ Intracellular Shift
Acute and chronic kidney disease; CHF
Principal Cell Dysfunction (TTKG < 7)
ACEi/ARB; AI; heparin
Hypovolemia (TTKG > 7)
↓ EABV
↓ distal flow of Na+ and H2O
Urine [Na+] < 20 mmol/L
Cell lysis
↑ osmolarity H2O efflux
Solvent drag
β2 inhibition α1 stimulation
Digoxin ↓ A
NAGMA ↓ insulin
↓ NHE1 activity
Diabetic nephropathy; NSAIDs
↓ A: ↓ R
K+ sparing diuretics; voltage- dependent RTA
↓ Na+/K+ ATPase activity
↓ GFR
↓ A: ↑ R ↑ A: ↑ R
↓ CCD K+ secretion
↑ K+ availability
↑ K+ release
↓ intracellular K+ influx
Chronic: Desensitize voltage- gated Na+ channels and ↓ membrane excitability
ECG: Peaked T-waves, ↑ PR interval, flat/absent P-wave, ↑ QRS, QRST “sine wave”
Hyperkalemia
Serum [K+] > 5.1 mmol/L
Acute: ↑ extracellular [K+] makes the RMP less (-)
Abbreviations:
A: Aldosterone
AI: Adrenal Insufficiency
CCD: Cortical Collecting Duct
CHF: Congestive Heart Failure
EABV: Effective Arterial Blood Volume H+: Hydrogen ion
K+: Potassium ion
Na+: Sodium ion
NAGMA: Normal Anion Gap Metabolic Acidosis
NSAIDs: Non-steroidal anti-inflammatory drugs Note:
Muscle weakness or paralysis, ↓ urinary acid excretion
R: Renin
RTA: Renal Tubular Acidosis
RMP: Resting Membrane Potential TTKG: Transtubular Potassium Gradient
• Pseudohyperkalemia should always be excluded; can be caused by thrombocytosis, leukocytosis or improper blood withdrawal technique.
Authors: Mannat Dhillon Joshua Low Reviewers: Andrea Kuczynski Kevin McLaughlin* * MD at time of publication
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published March 6, 2019 on www.thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2019/03/Hyperkalemia-Physiology-.jpg)
Torsades de Pointes (TdP)- Pathogenesis and Clinical Findings
![Torsades de Pointes (TdP): Pathogenesis and Clinical Findings
Drugs (e.g. Class 1A [quinidine], Class III [sotalol,
amiodarone], TCAs, erythromycin, quinolones, anti-histamines)
Sinus bradycardia, AV block
Metabolic abnormality (hypo K+/Ca2+/Mg2+)
Primary heart disease: ischemic, congestive heart failure, cardiomyopathy
Acquired long QT syndrome
Congenital long QT syndrome
↓ repolarizing current/ depolarizing current in cardiomyocytes
Mutated cardiac ion channels
Author: Nicola Adderley Reviewers: Luke Gagnon Emily Ryznar *Saman Rezazadeh *George Veenhuyzen MD at time of publication*
↓ repolarizing current in cardiomyocytes
QTc interval
Prolonged ventricular action potential duration
Early after depolarization (EAD) triggering PVC
Torsades de Pointes
Illustrated changes to action potential:
Normal cardiac action potential
EAD
Abbreviations: TCAs: tricyclic antidepressants AV: atrioventricular QTc: QT interval, corrected for heart rate
PVC: premature ventricular contraction
VF: ventricular fibrillation
SR: sinus rhythm
Polymorphic ventricular tachycardia initiated by PVC in the setting of QT interval prolongation and maintained by functional re-entry
Non-sustained TdP
Asymptomatic, palpitations, syncope (length-dependent)
Illustrated changes to ECG Strip:
OR
Sinus rhythm restored
Degeneration to VF
Sudden cardiac death
Prolonged repolarization
Triggered beat (PVC)
A
BCDE
A. Prolonged QT interval B. PVC
C. PVC triggers TdP
D. Non-sustained TdP
E. Return to SR
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published March 10, 2019 on www.thecalgaryguide.com
Torsades de Pointes (TdP): Pathogenesis and Clinical Findings
Drugs (e.g. Class 1A [quinidine], Class III [sotalol,
amiodarone], TCAs, erythromycin, quinolones, anti-histamines)
Sinus bradycardia, AV block
Metabolic abnormality (hypo K+/Ca2+/Mg2+)
Primary heart disease: ischemic, congestive heart failure, cardiomyopathy
Acquired long QT syndrome
Congenital long QT syndrome
↓ repolarizing current/ depolarizing current in cardiomyocytes
Mutated cardiac ion channels
Author: Nicola Adderley Reviewers: Luke Gagnon Emily Ryznar *Saman Rezazadeh *George Veenhuyzen MD at time of publication*
↓ repolarizing current in cardiomyocytes
QTc interval
Prolonged ventricular action potential duration
Early after depolarization (EAD) triggering PVC
Torsades de Pointes
Illustrated changes to action potential:
Normal cardiac action potential
EAD
Abbreviations: TCAs: tricyclic antidepressants AV: atrioventricular QTc: QT interval, corrected for heart rate
PVC: premature ventricular contraction
VF: ventricular fibrillation
SR: sinus rhythm
Polymorphic ventricular tachycardia initiated by PVC in the setting of QT interval prolongation and maintained by functional re-entry
Non-sustained TdP
Asymptomatic, palpitations, syncope (length-dependent)
Illustrated changes to ECG Strip:
OR
Sinus rhythm restored
Degeneration to VF
Sudden cardiac death
Prolonged repolarization
Triggered beat (PVC)
A
BCDE
A. Prolonged QT interval B. PVC
C. PVC triggers TdP
D. Non-sustained TdP
E. Return to SR
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published March 10, 2019 on www.thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2019/03/Torsades-de-Pointes-TdP-Pathogenesis-and-Clinical-Findings-.jpg)
Shoulder Dystocia: Complications
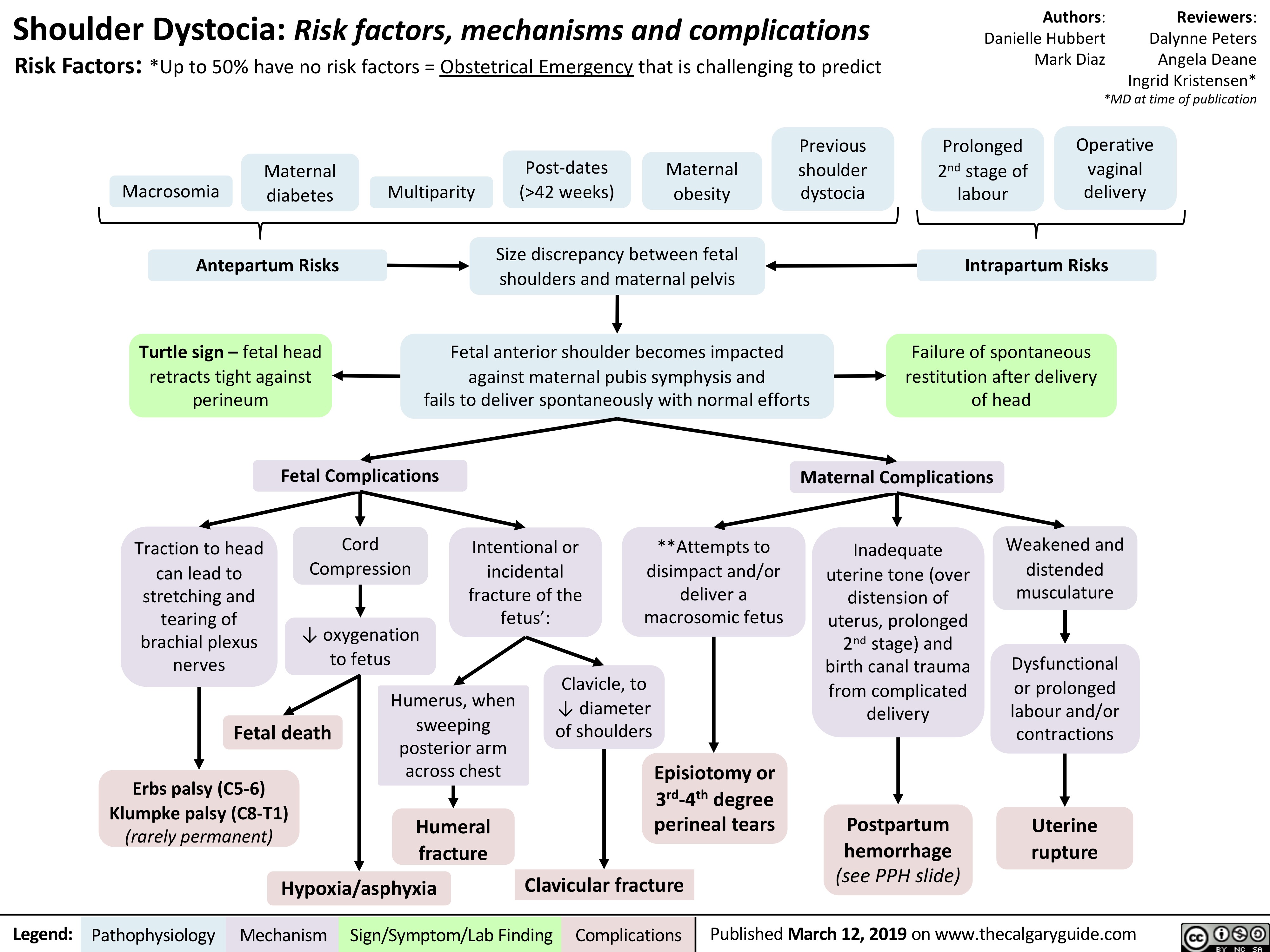
Primary Myelofibrosis pathogenesis and clinical findings
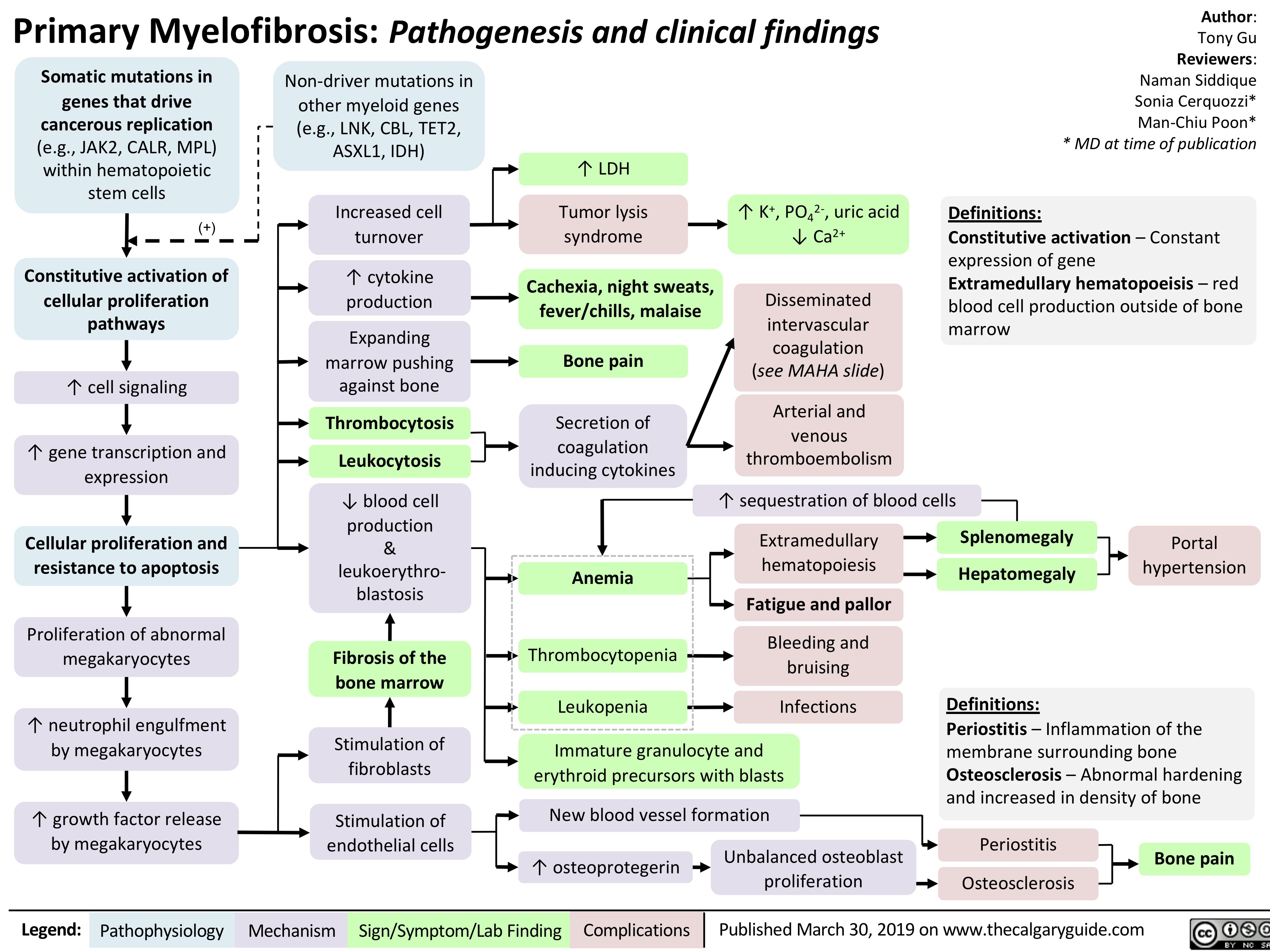
Hemorrhoids - Pathogenesis and Clinical Findings
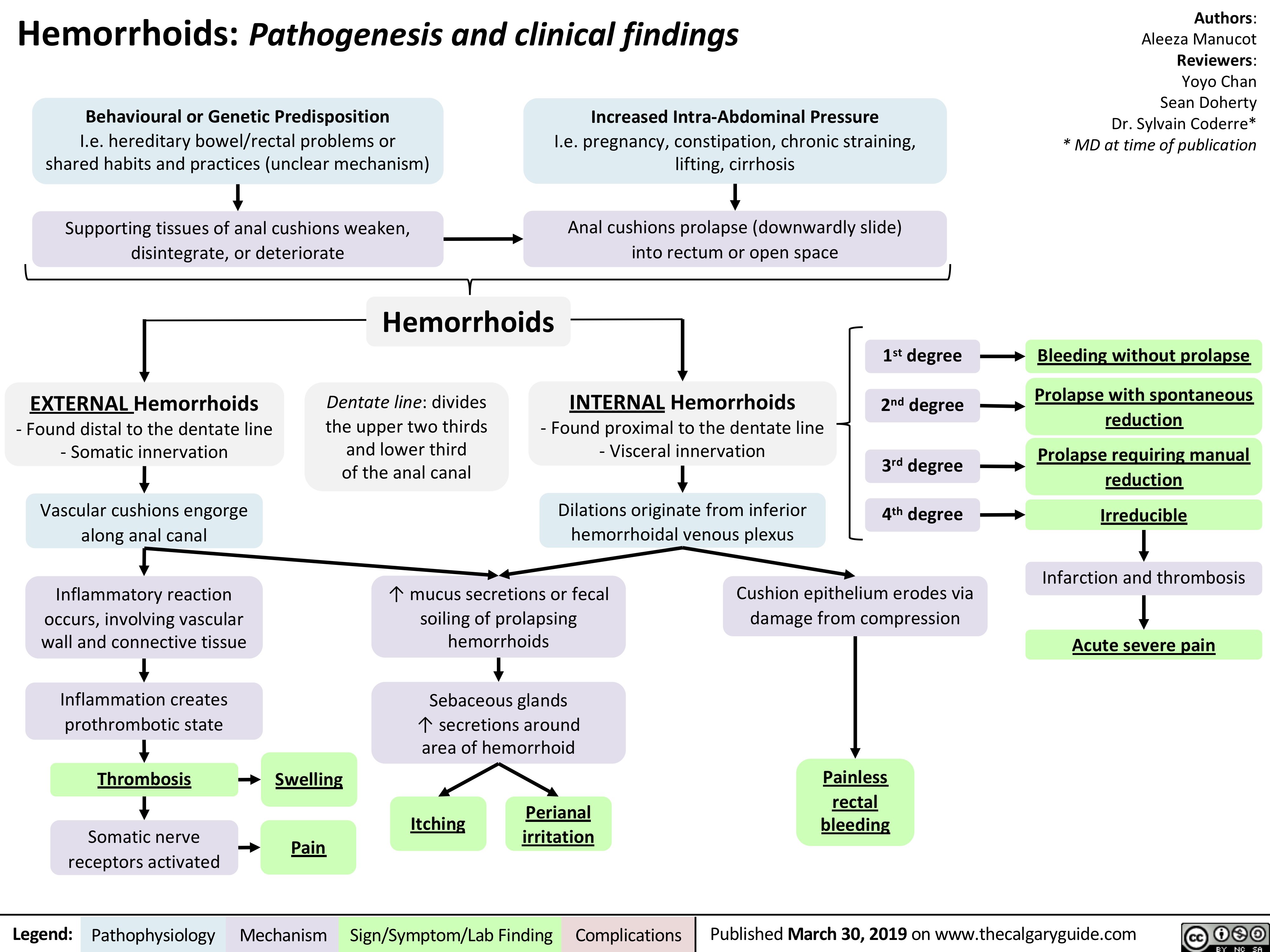
gastroesophageal-reflux-disease-gerd-complications
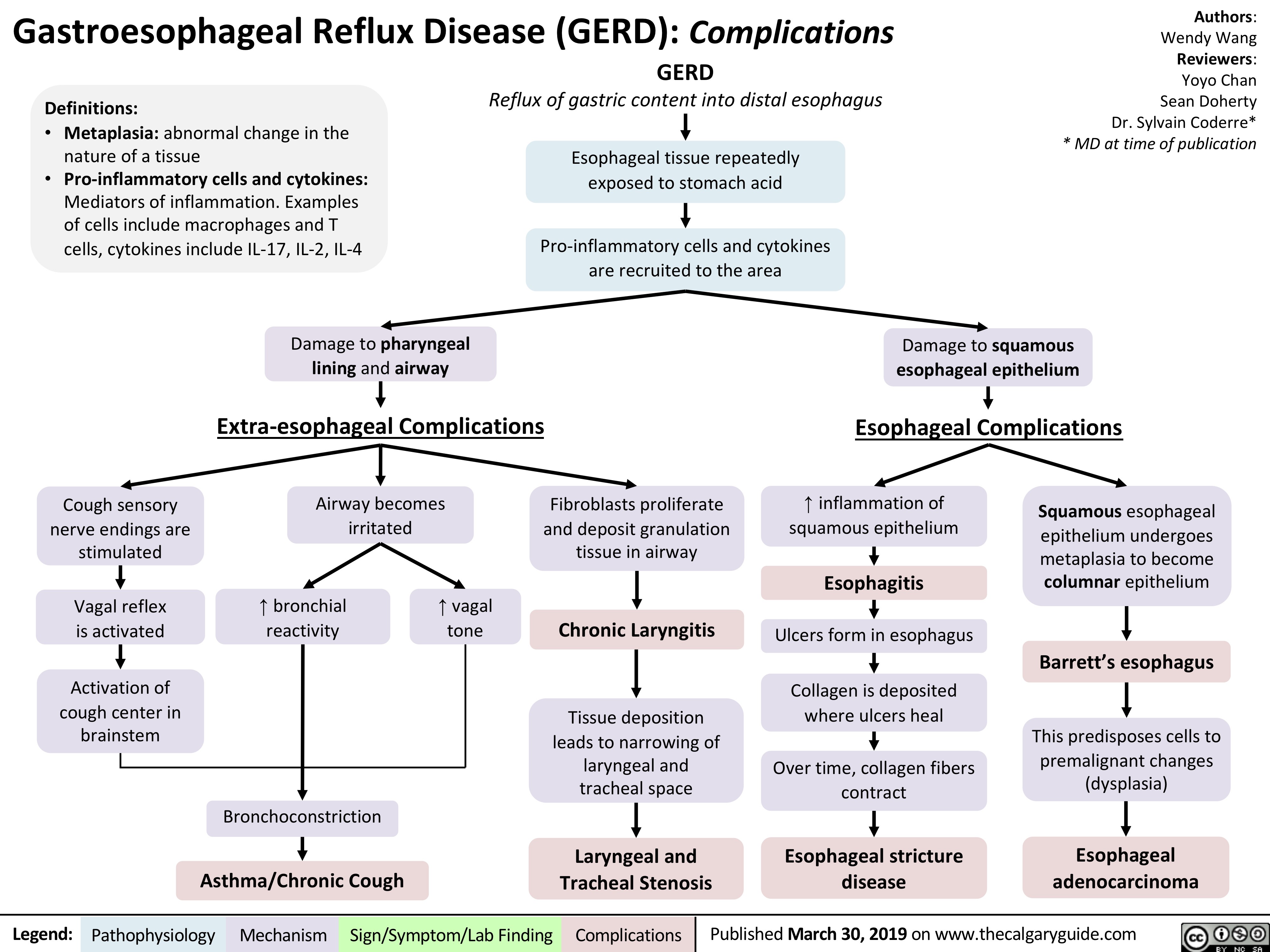
autosomal-dominant-polycystic-kidney-disease-adpkd
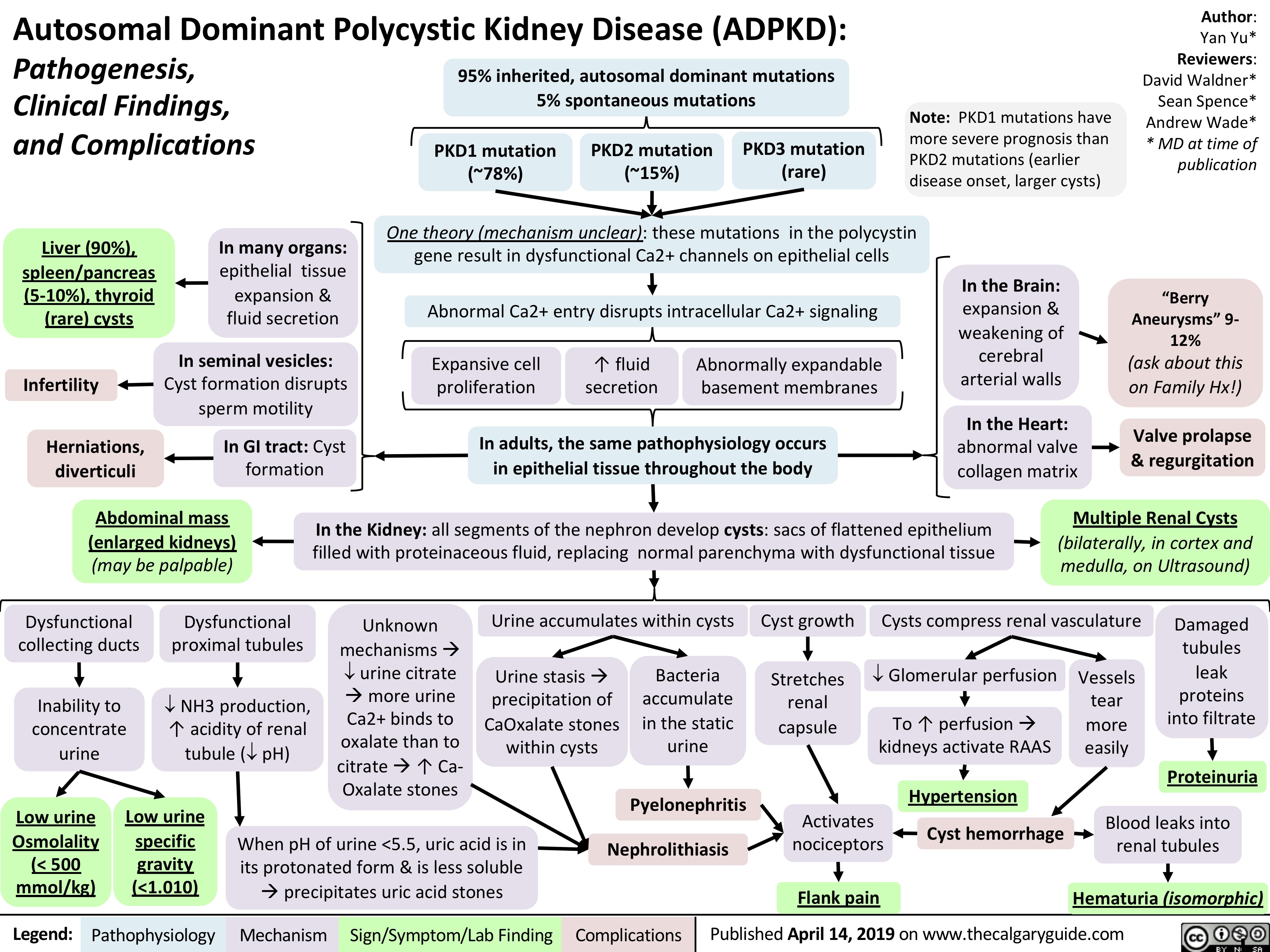
Rickets and Osteomalacia: Pathogenesis and Clinical Findings
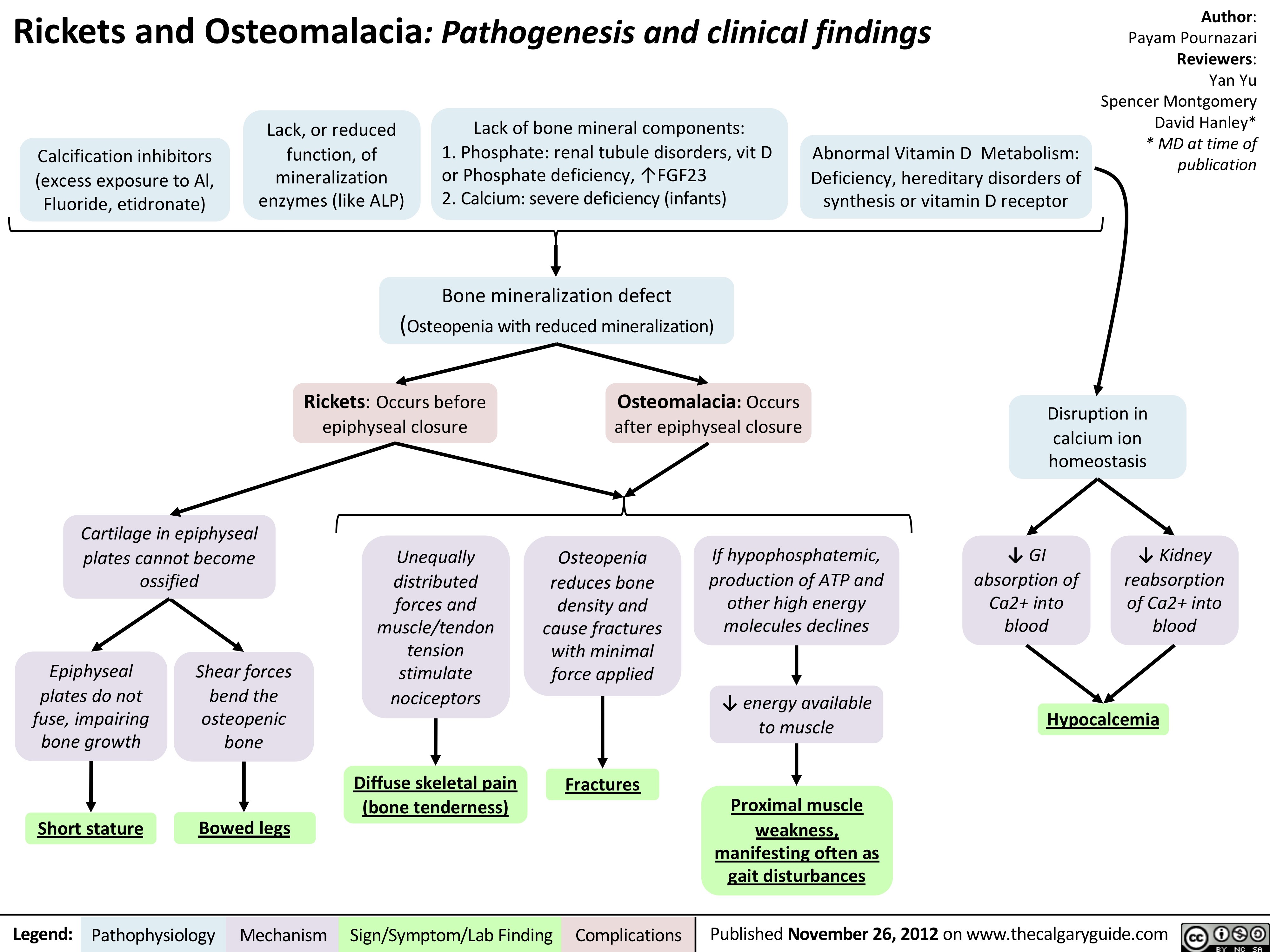
Polyarteritis Nodosa (PAN): Pathogenesis and Clinical Findings
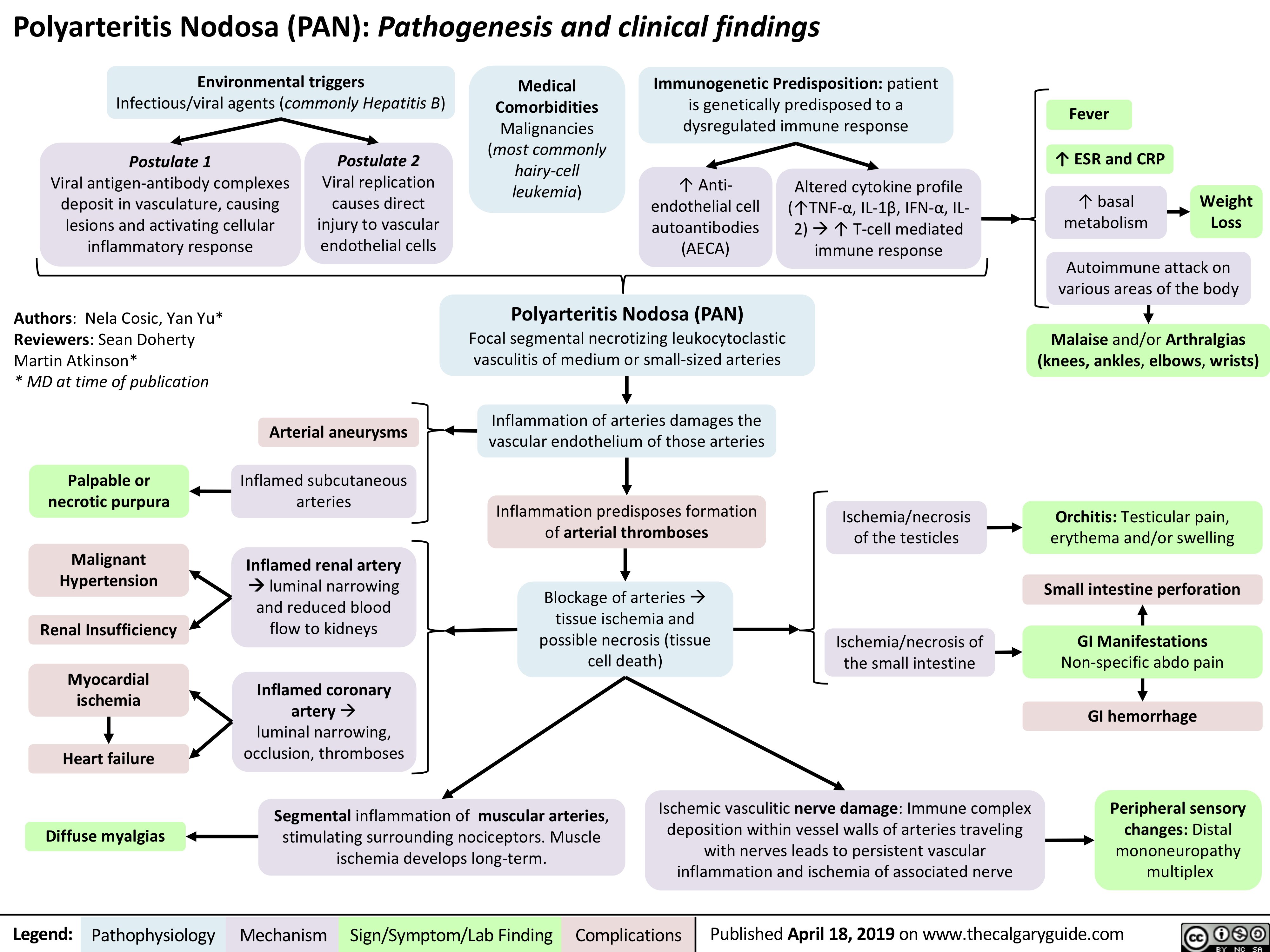
dermatomyositis-dm-and-polymyositis-pm-pathogenesis-and-clinical-findings
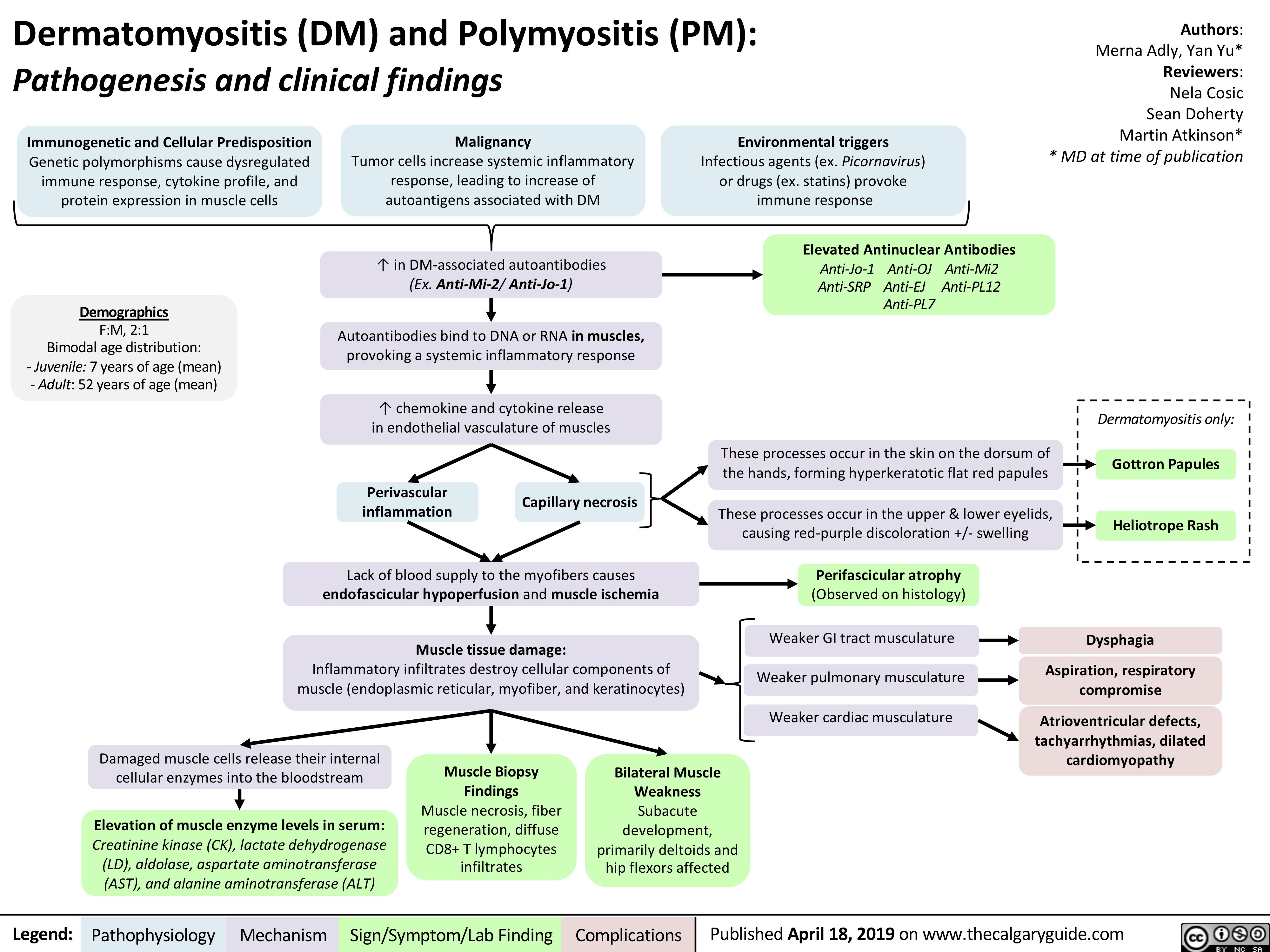
DiGeorge Syndrome: Pathogenesis and Clinical Findings
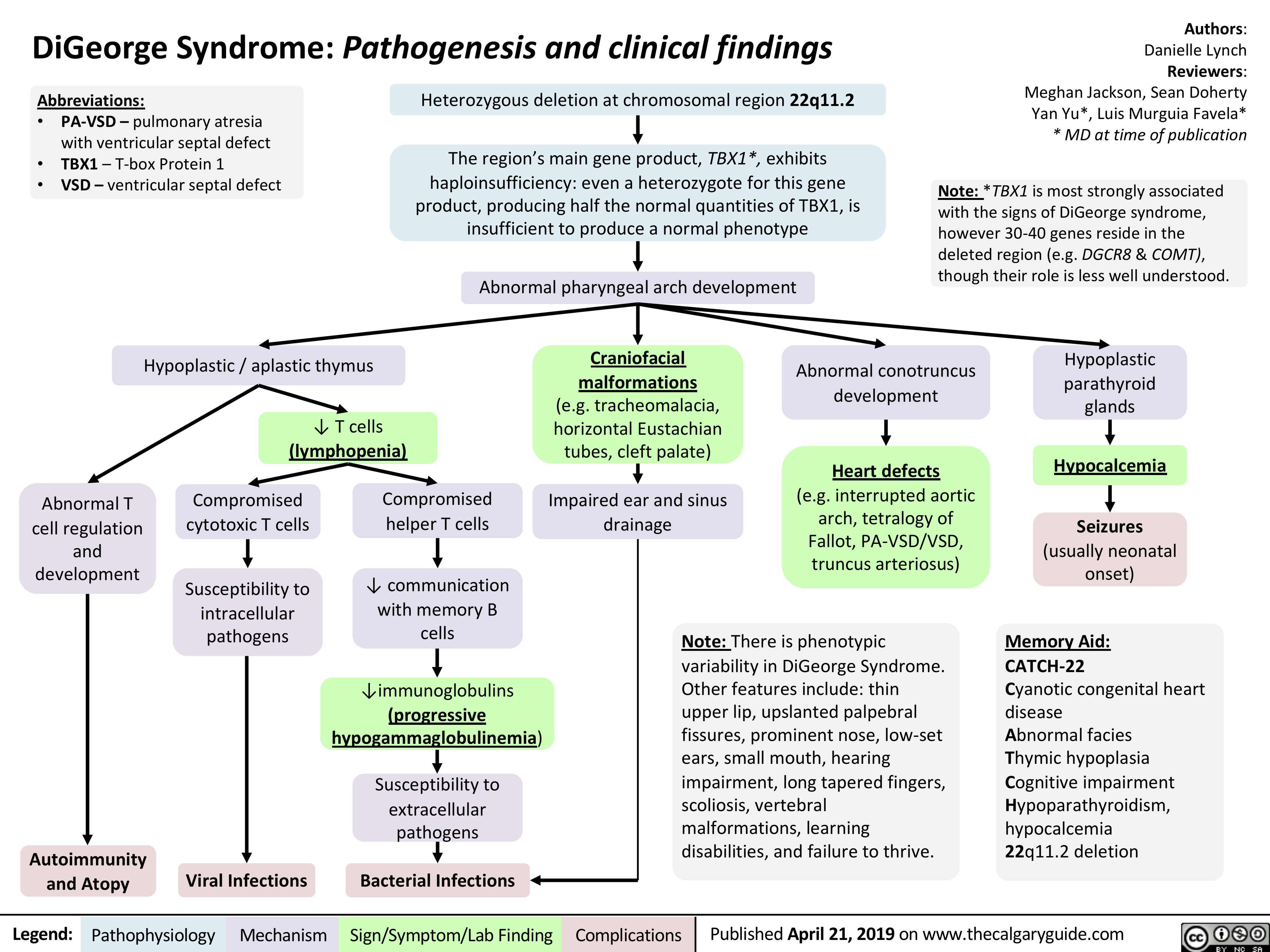
Molluscum Contagiosum: Pathogenesis and Clinical Findings
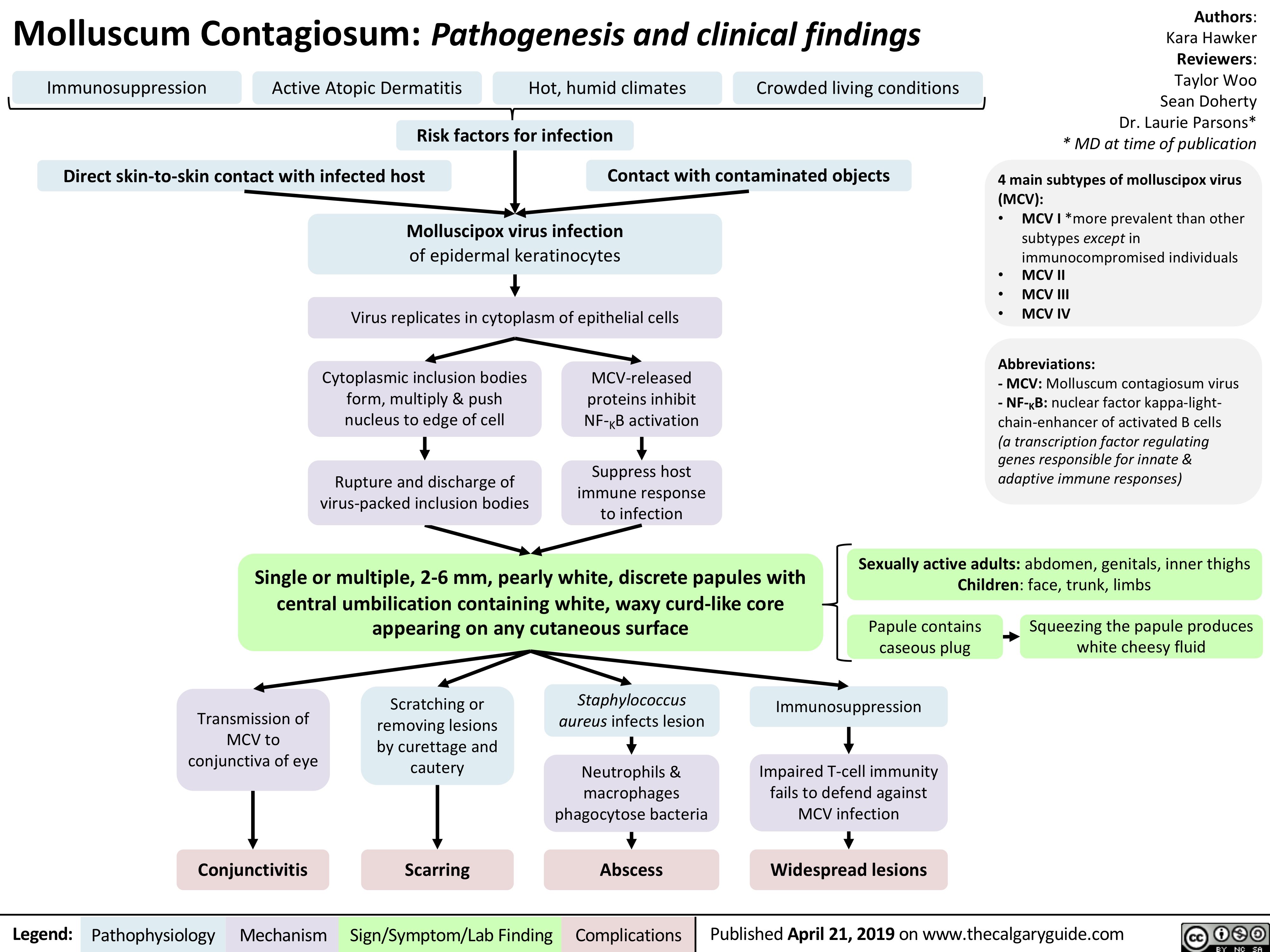
acute-somatic-pain
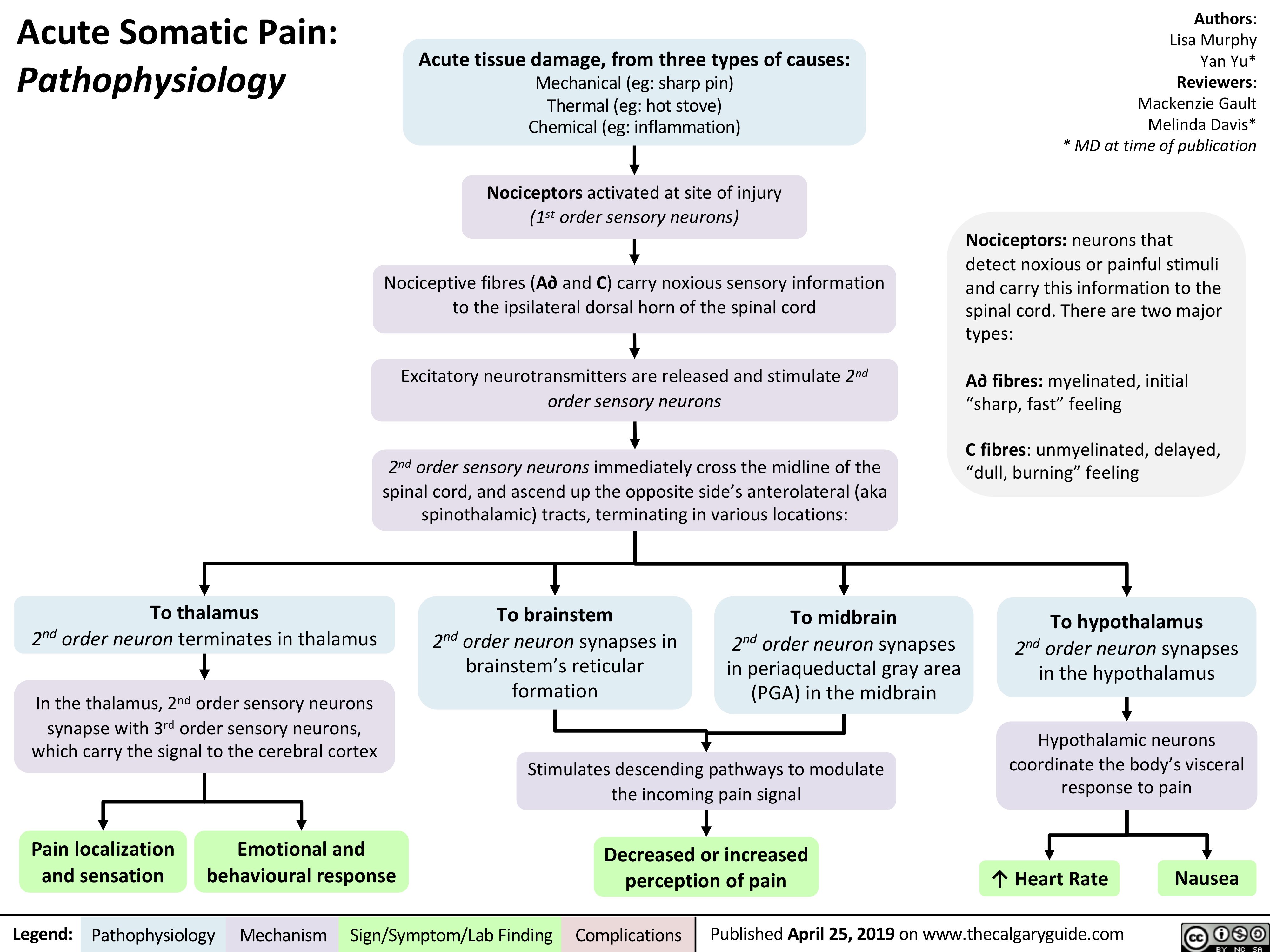
Small Bowel Infarction
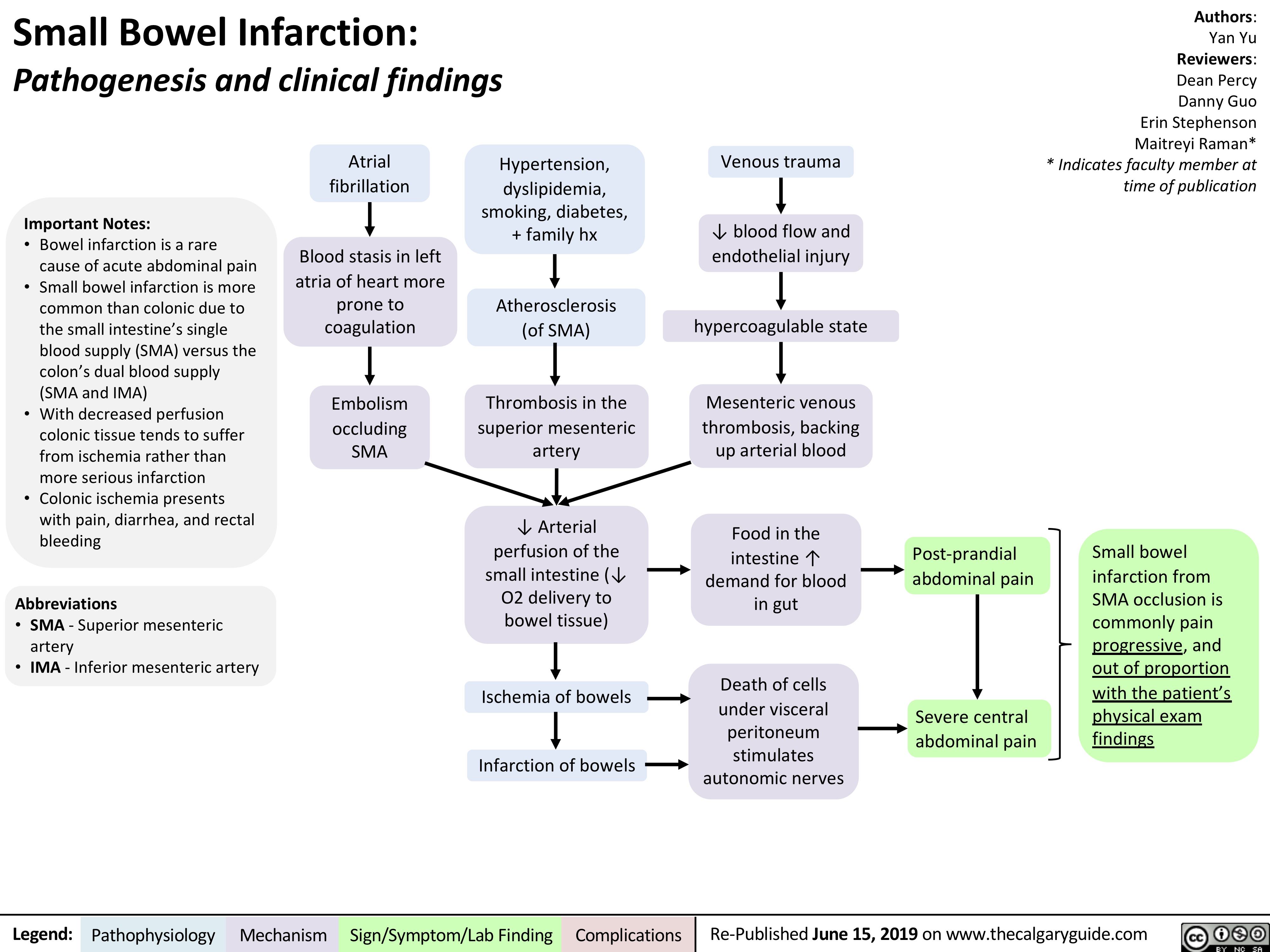
Crohn's Disease
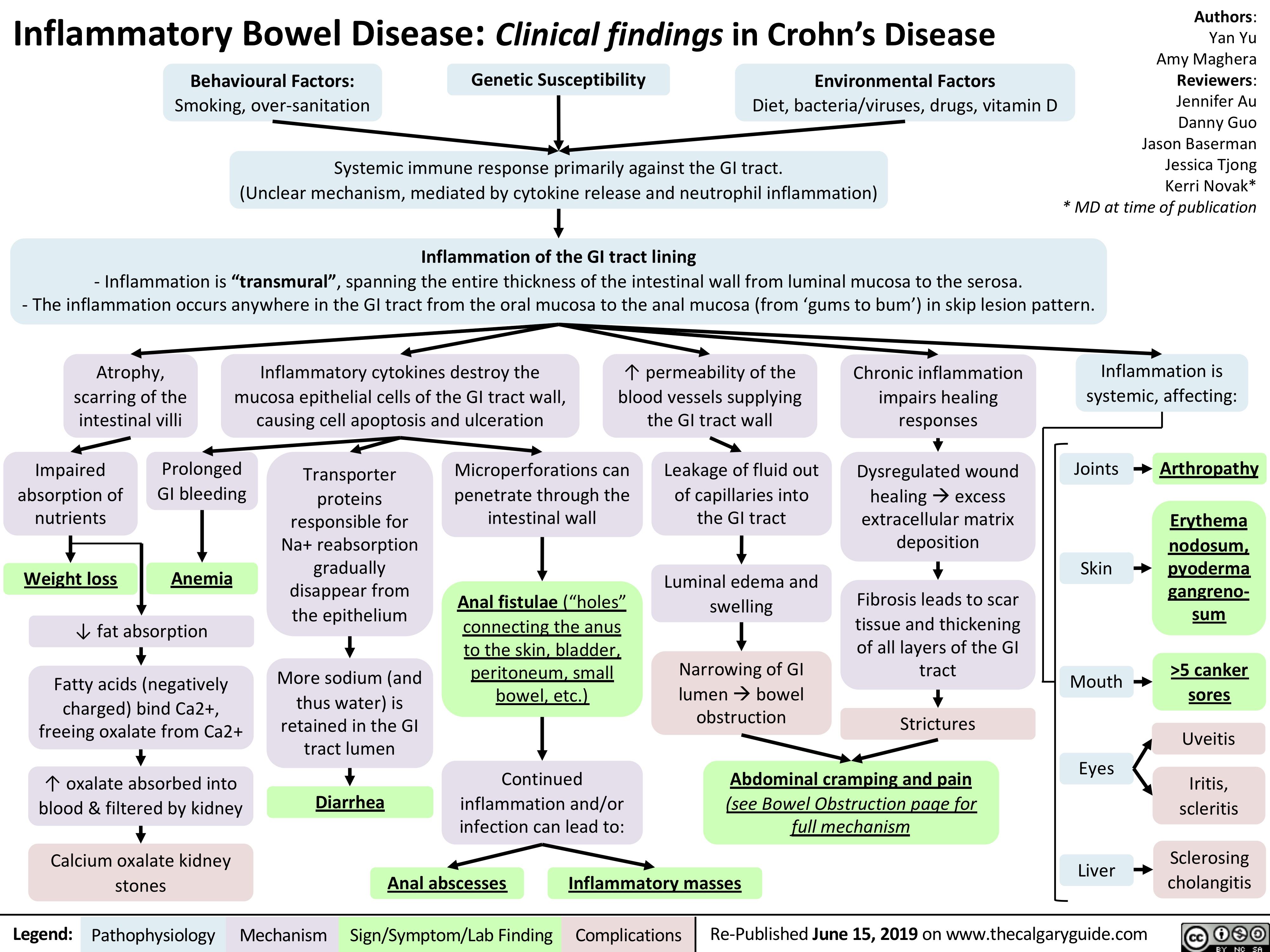
Hemophilia
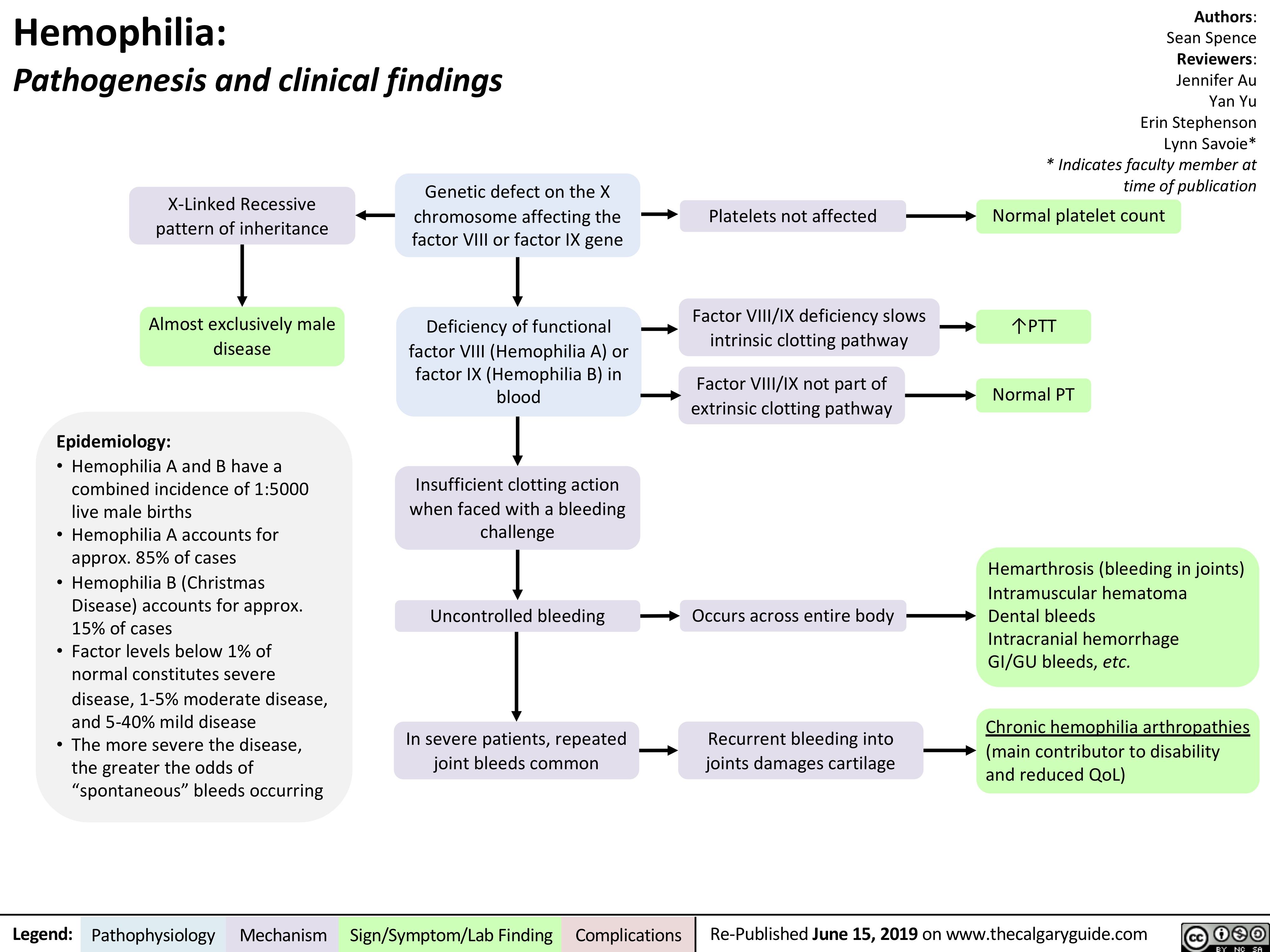
Signs and Symptoms of Pulmonary Embolism
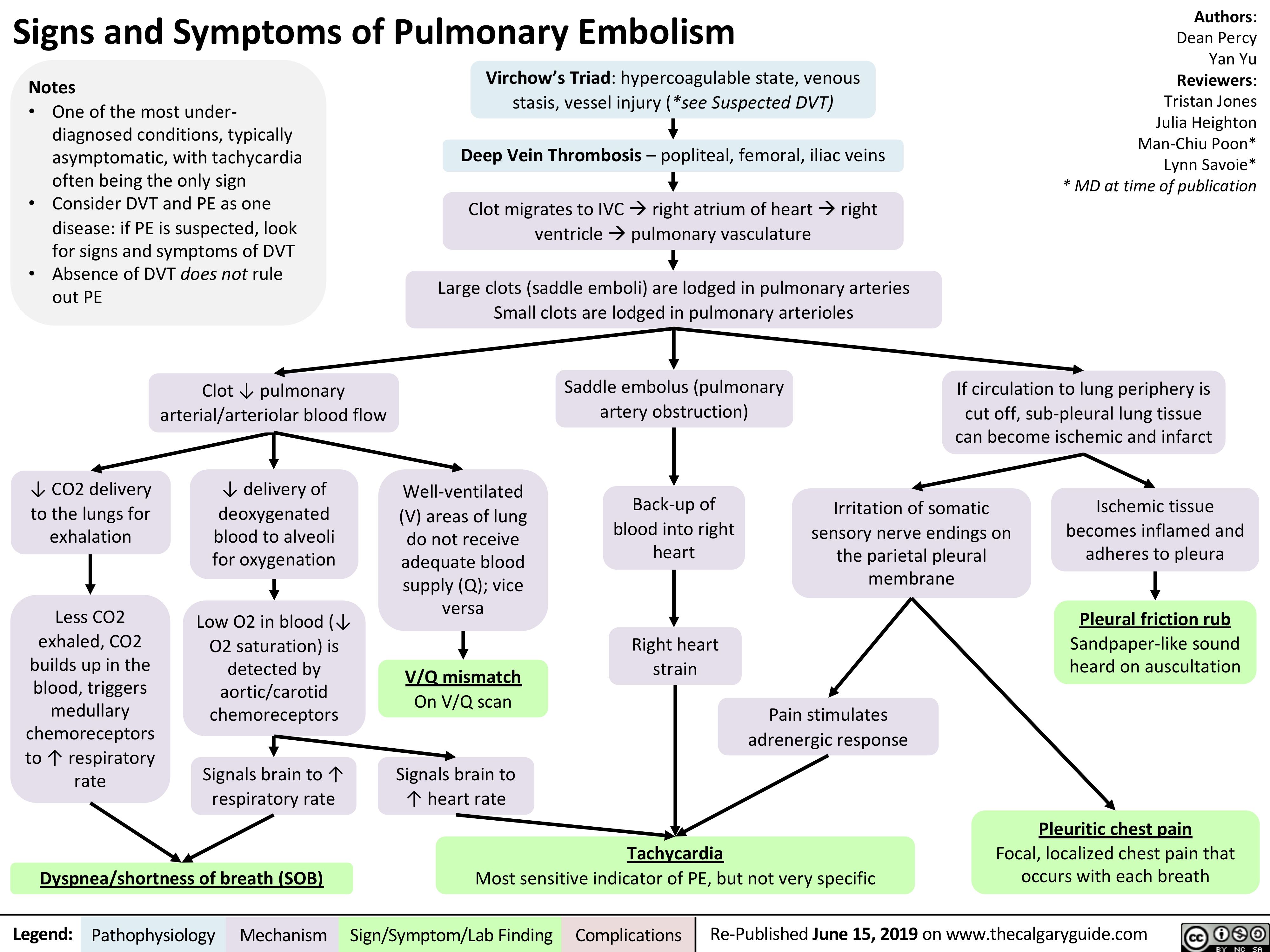
Hemolytic Anemia - Pathophysiology
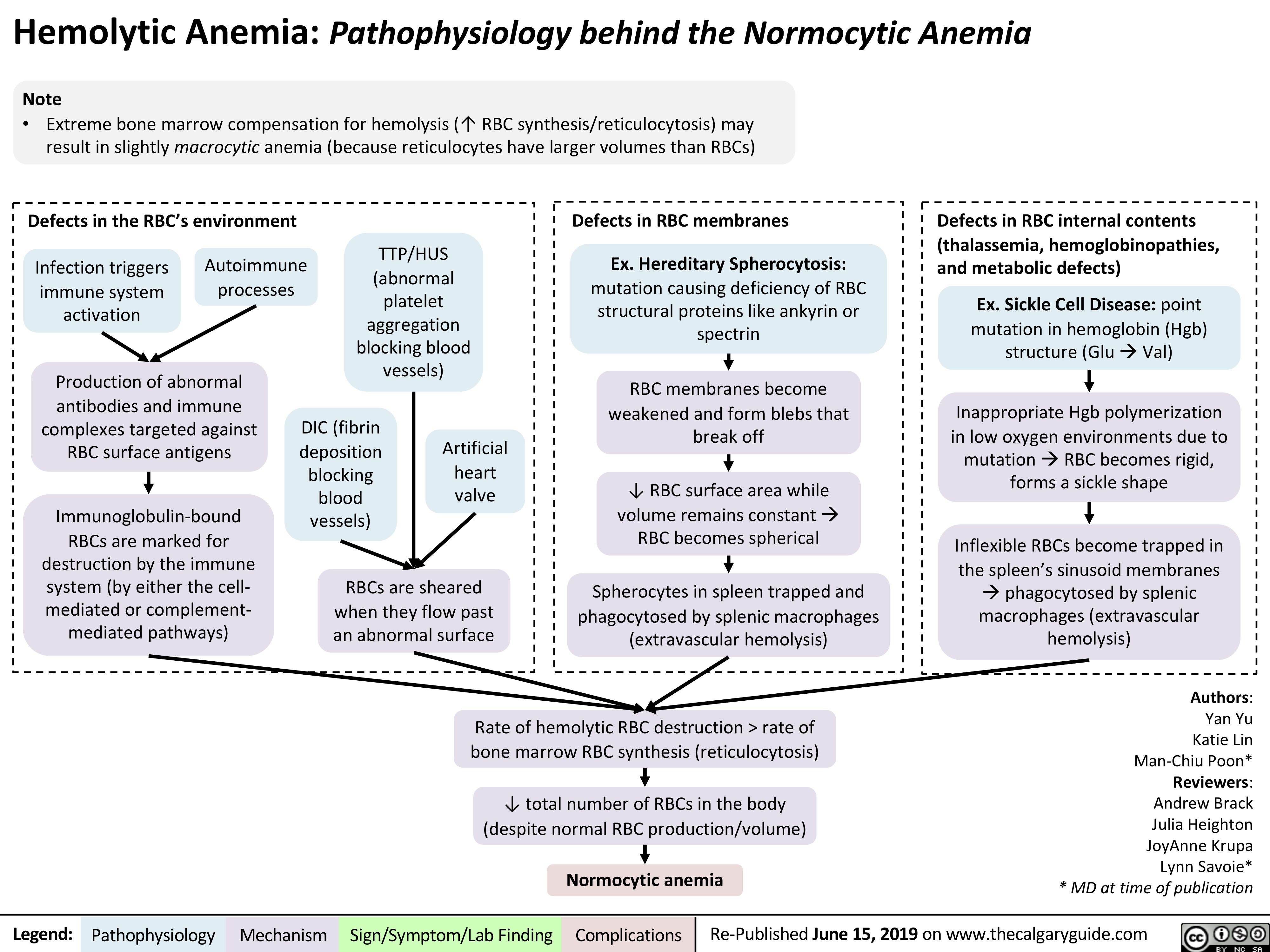
Wilson's Disease
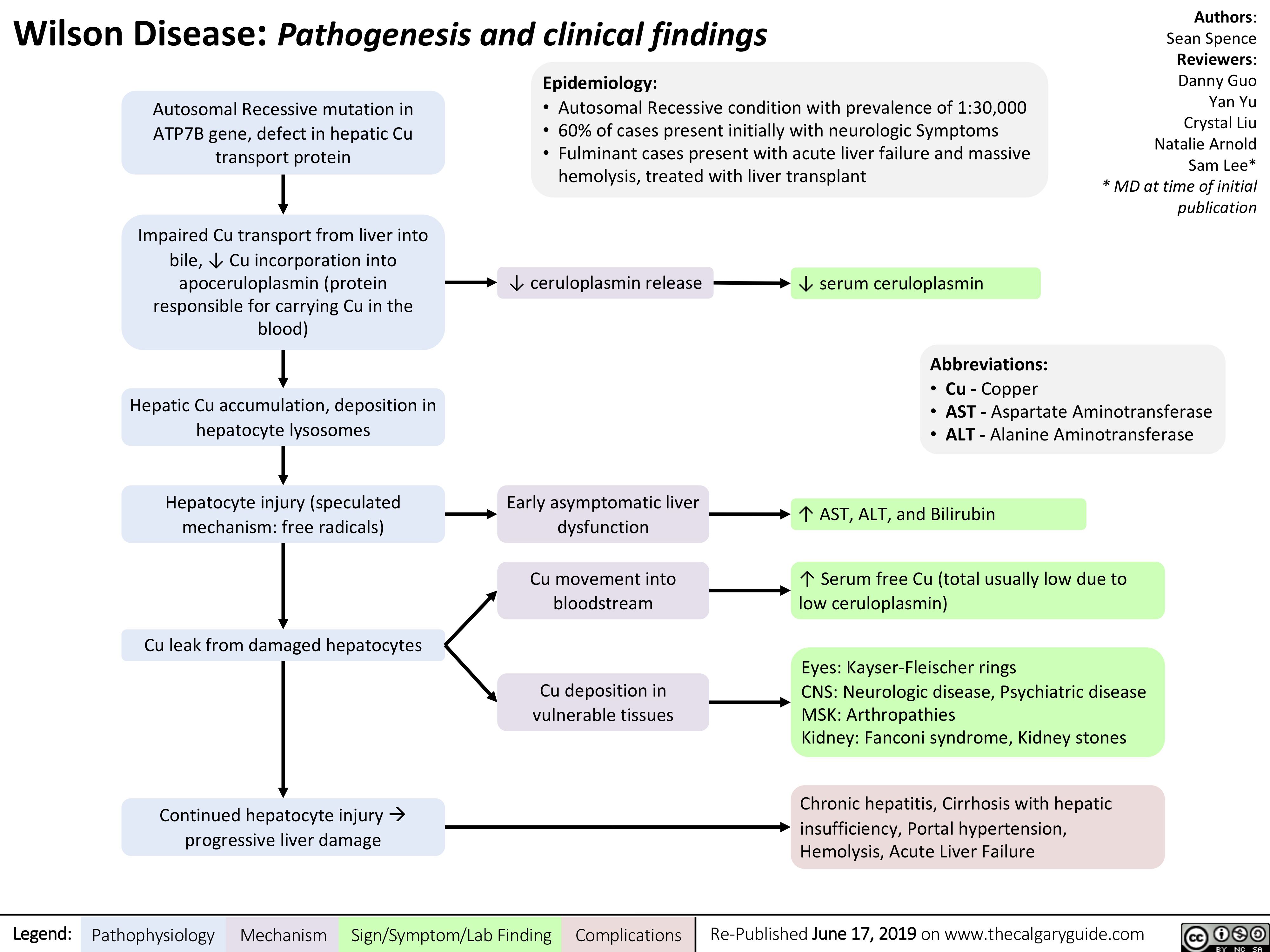
chronic-myeloid-leukemia
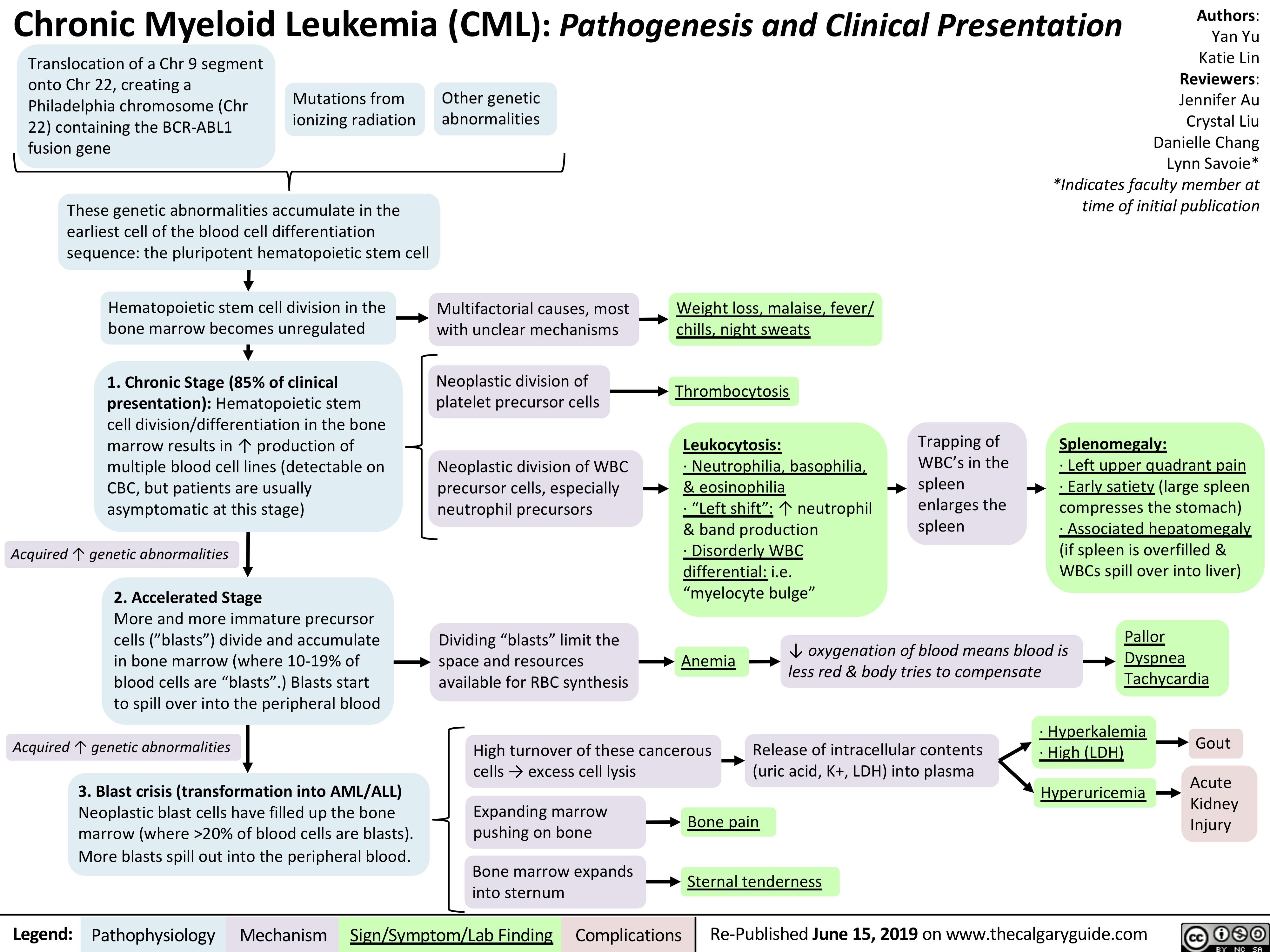
Secondary Polycythemia
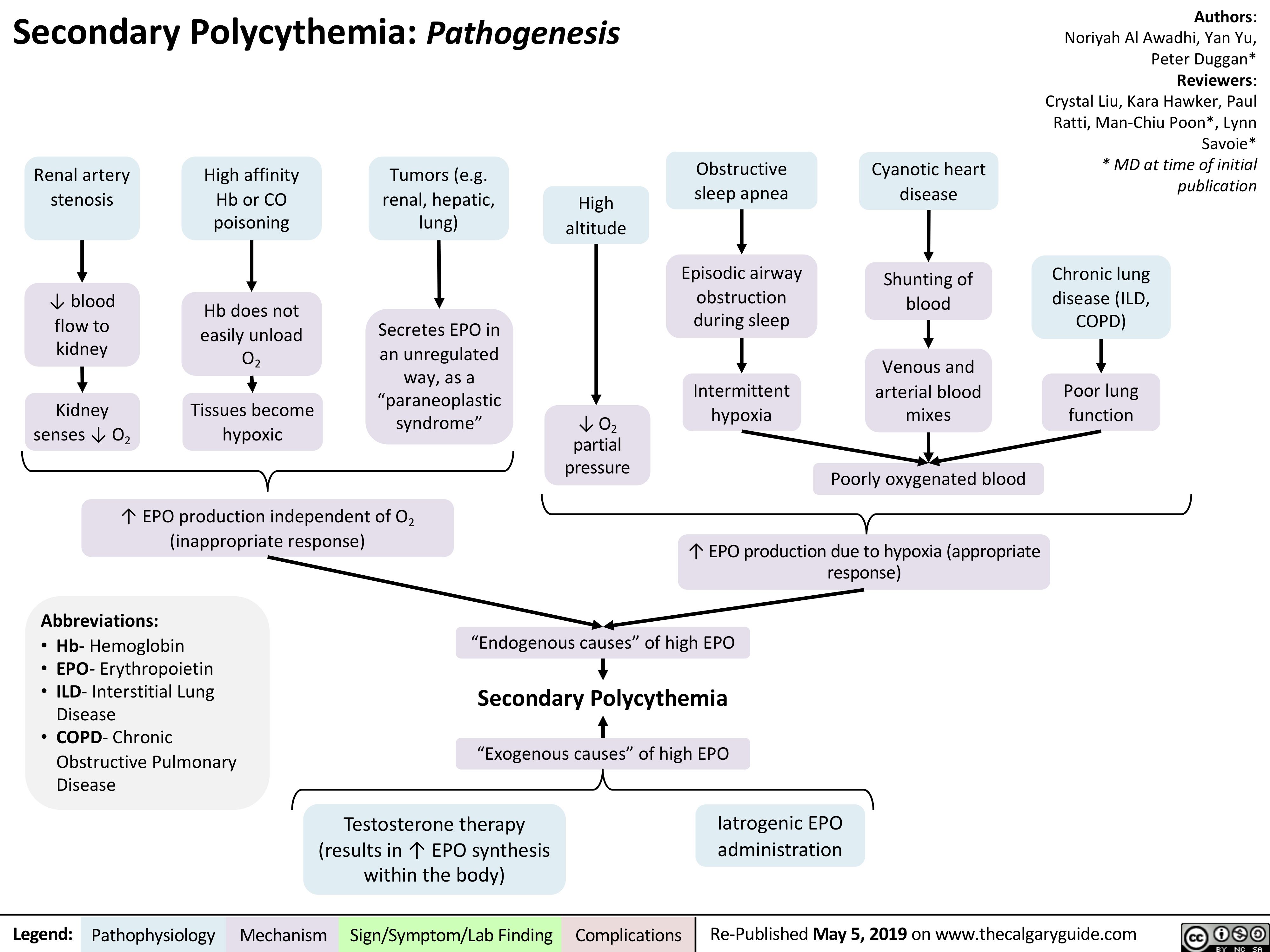
Acute Lymphoblastic Leukemia
![Acute Lymphoblastic Leukemia (ALL): Pathogenesis and Clinical Presentation
Authors: Yan Yu, Katie Lin Reviewers: Crystal Liu, Kara Hawker, Jennifer Au, Lynn Savoie* * MD at time of initial publication
Note: ALL is much rarer than AML and is usually seen in children
Accumulation of genetic abnormalities in immature lymphoid precursor cells (B/T cell precursors)
Neoplastic lymphoid precursor cells (“blasts”) divide and accumulate in bone marrow
Abundance of blasts displaces other blood precursors from marrow, inhibiting their development/differentiati on
After neoplastic blasts fill up bone marrow, they spill out into blood
High turnover of these cancerous cells
Multifactorial causes, most with unclear mechanisms
Expanding marrow pushing on bone
Pancytopenia on CBC
20% of marrow is blasts (on bone marrow aspirate and/or biopsy)
Neoplastic blasts continue to divide and accumulate in lymph
nodes and spleen (can occur, but not that common)
Blasts detected as white blood cells on CBC
High rate of cell lysis
Weight loss, malaise, fever/chills, night sweats
Bone pain (worse than that felt in AML, especially in children)
↓ in neutrophils
↓ in RBCs
↓ in platelets, reduced blood clotting ability
Lymphadenopathy Splenomegaly
May cause leukocytosis, despite pancytopenia
Release of intracellular contents (uric acid, K+, LDH) into plasma
Greater chances of infection
Anemia
Fatigue, shortness of breath, pallor
Easy bruising and petechiae on skin
Hyperuricemia Hyperkalemia High [LDH]
Tumor lysis syndrome
Acute kidney injury
Gout
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published May 5, 2019 on www.thecalgaryguide.com
Acute Lymphoblastic Leukemia (ALL): Pathogenesis and Clinical Presentation
Authors: Yan Yu, Katie Lin Reviewers: Crystal Liu, Kara Hawker, Jennifer Au, Lynn Savoie* * MD at time of initial publication
Note: ALL is much rarer than AML and is usually seen in children
Accumulation of genetic abnormalities in immature lymphoid precursor cells (B/T cell precursors)
Neoplastic lymphoid precursor cells (“blasts”) divide and accumulate in bone marrow
Abundance of blasts displaces other blood precursors from marrow, inhibiting their development/differentiati on
After neoplastic blasts fill up bone marrow, they spill out into blood
High turnover of these cancerous cells
Multifactorial causes, most with unclear mechanisms
Expanding marrow pushing on bone
Pancytopenia on CBC
20% of marrow is blasts (on bone marrow aspirate and/or biopsy)
Neoplastic blasts continue to divide and accumulate in lymph
nodes and spleen (can occur, but not that common)
Blasts detected as white blood cells on CBC
High rate of cell lysis
Weight loss, malaise, fever/chills, night sweats
Bone pain (worse than that felt in AML, especially in children)
↓ in neutrophils
↓ in RBCs
↓ in platelets, reduced blood clotting ability
Lymphadenopathy Splenomegaly
May cause leukocytosis, despite pancytopenia
Release of intracellular contents (uric acid, K+, LDH) into plasma
Greater chances of infection
Anemia
Fatigue, shortness of breath, pallor
Easy bruising and petechiae on skin
Hyperuricemia Hyperkalemia High [LDH]
Tumor lysis syndrome
Acute kidney injury
Gout
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published May 5, 2019 on www.thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2015/05/Acute-Lymphoblastic-Leukemia.jpg)
Ulcerative Colitis
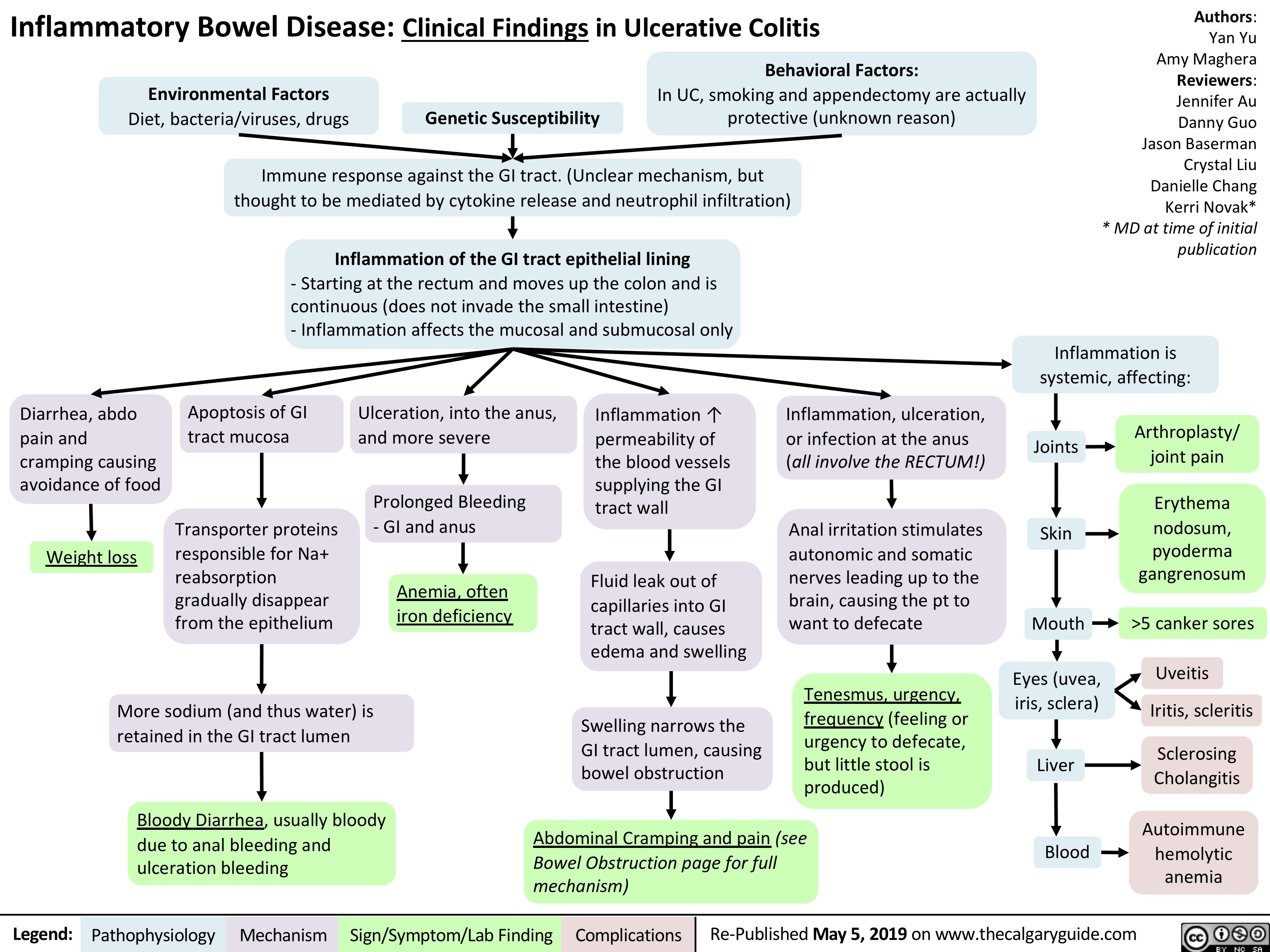
HBV Serology
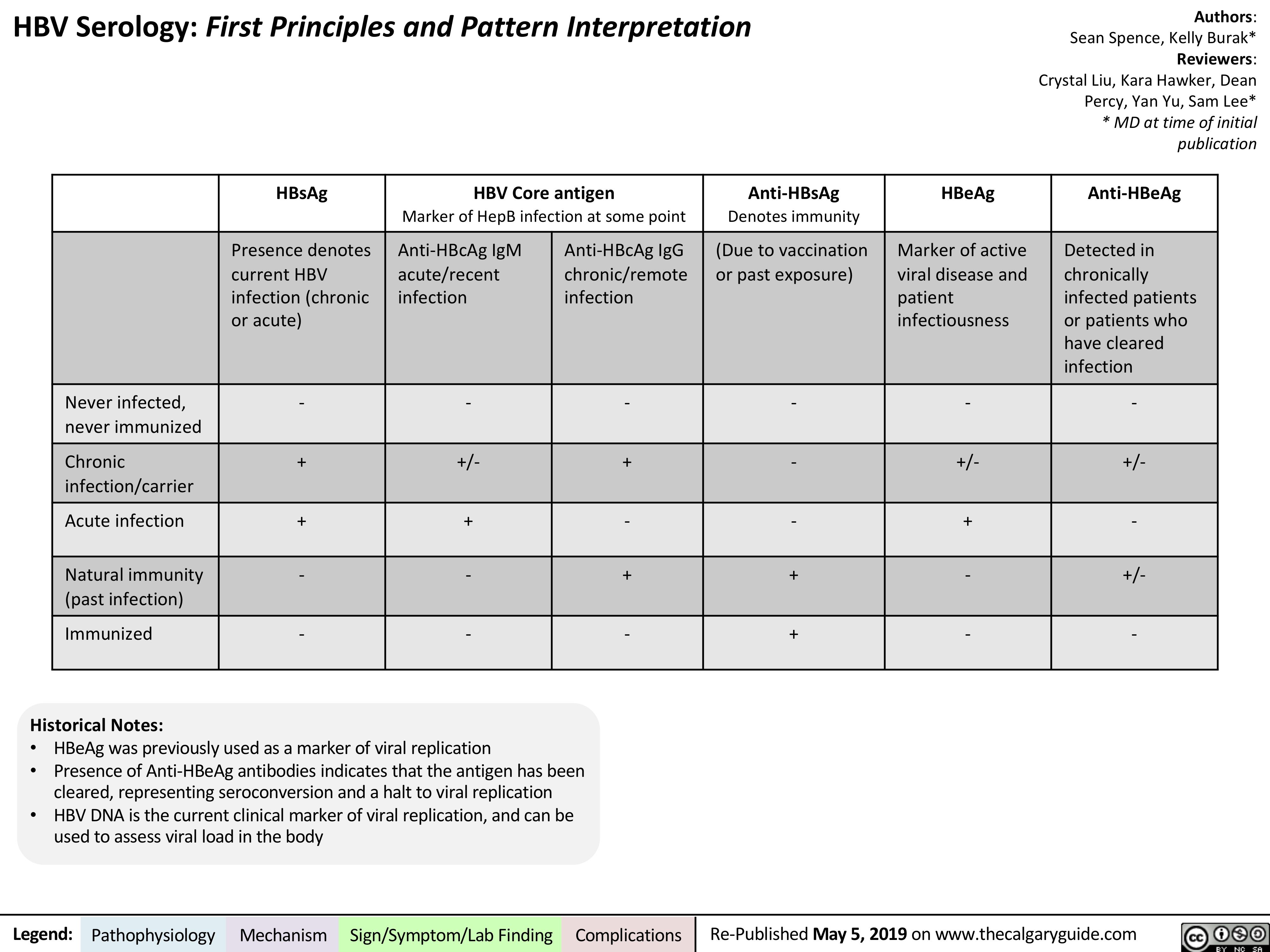
Chronic Lymphocytic Leukemia
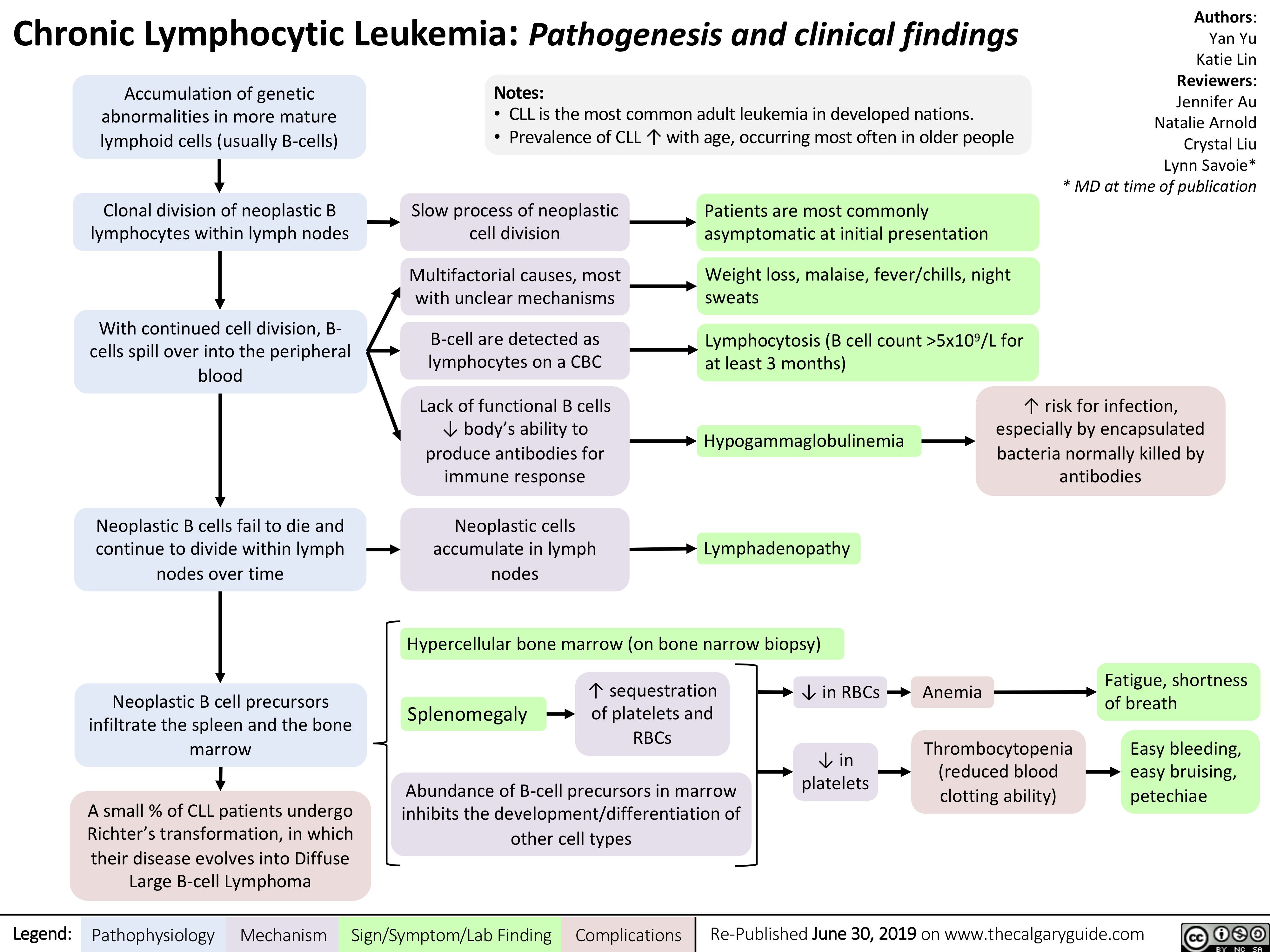
perforated-viscous
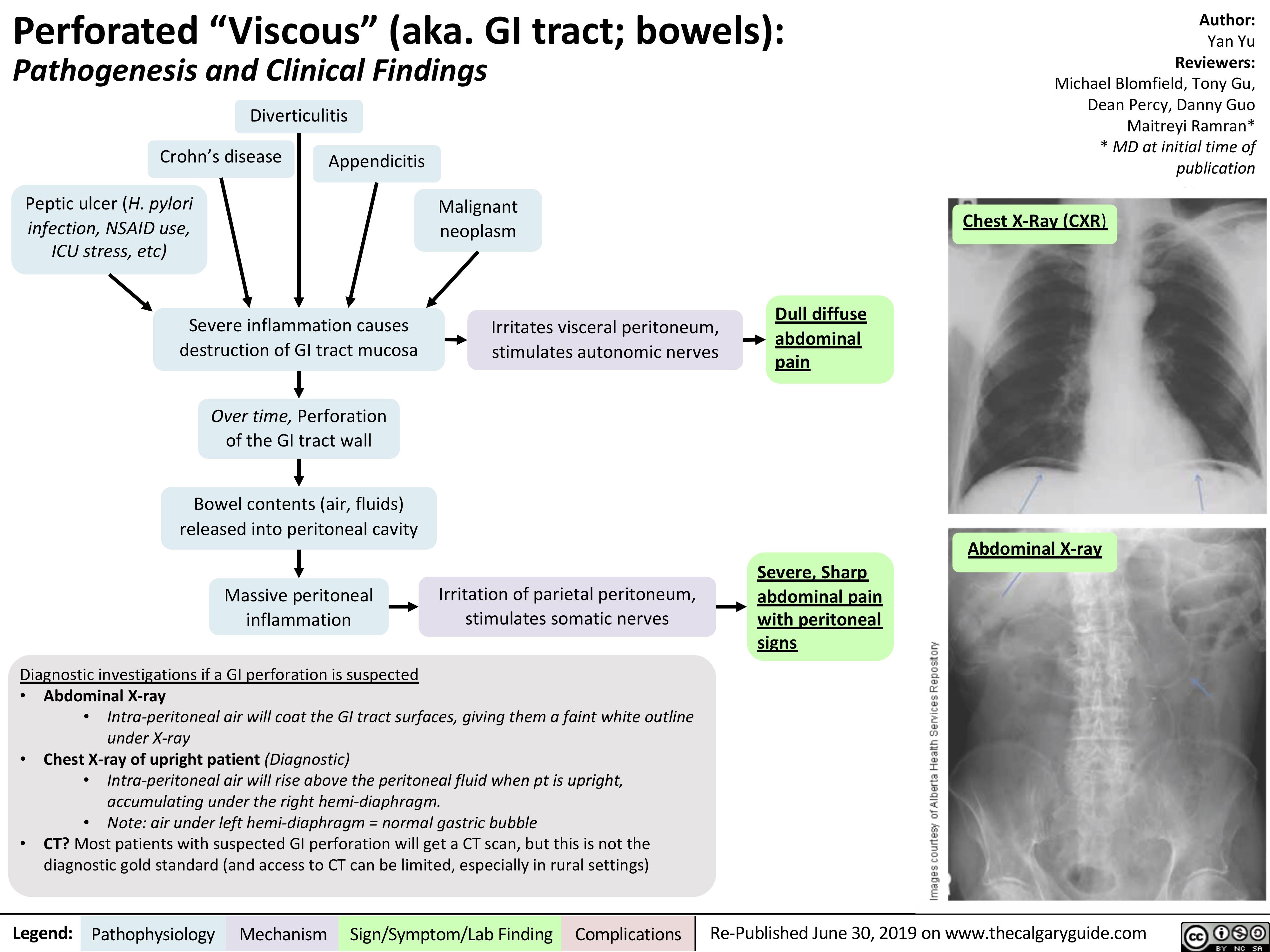
acanthosis-nigricans-pathogenesis-and-clinical-findings
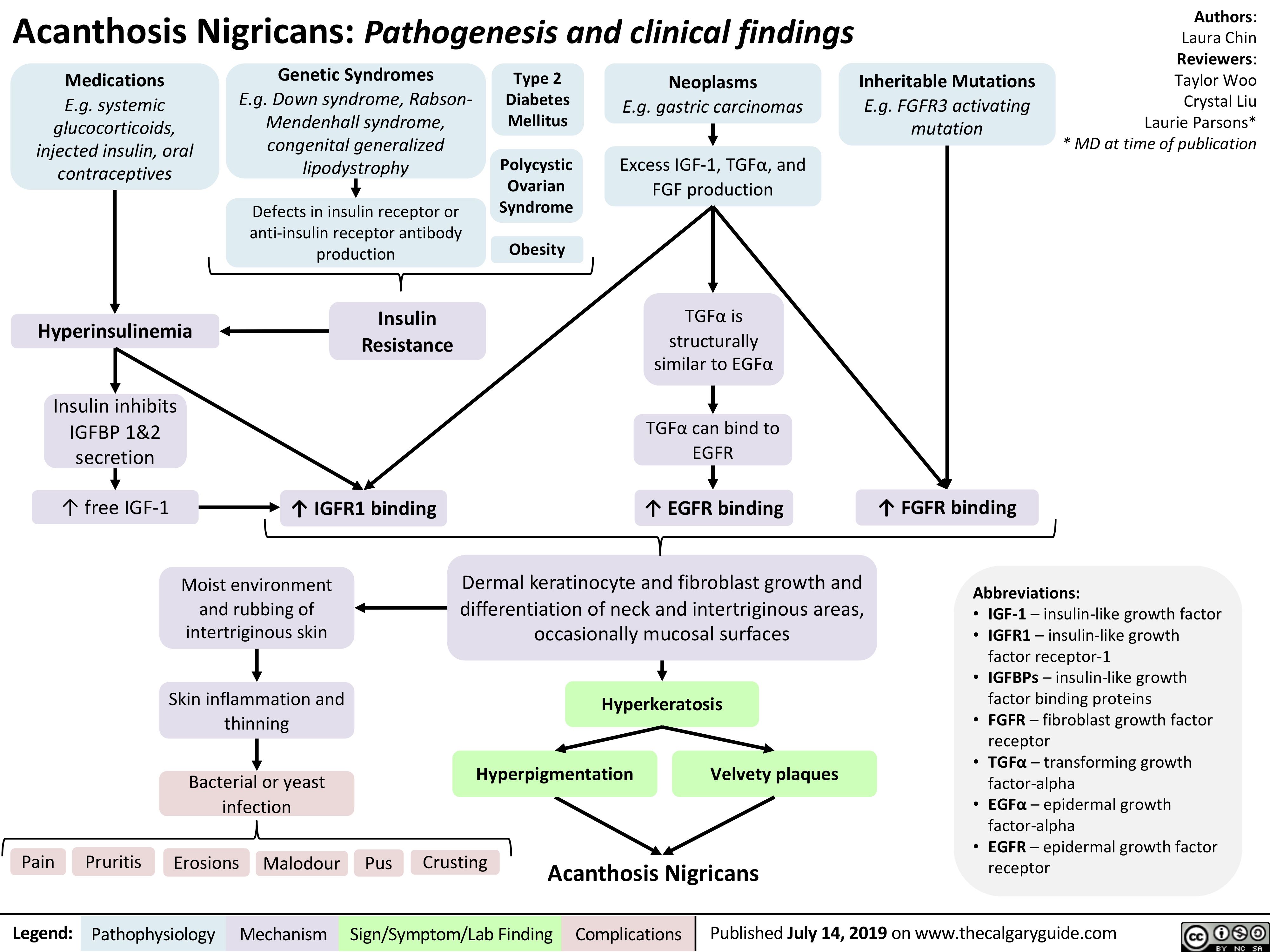
HELLP syndrome pathogenesis and clinical findings
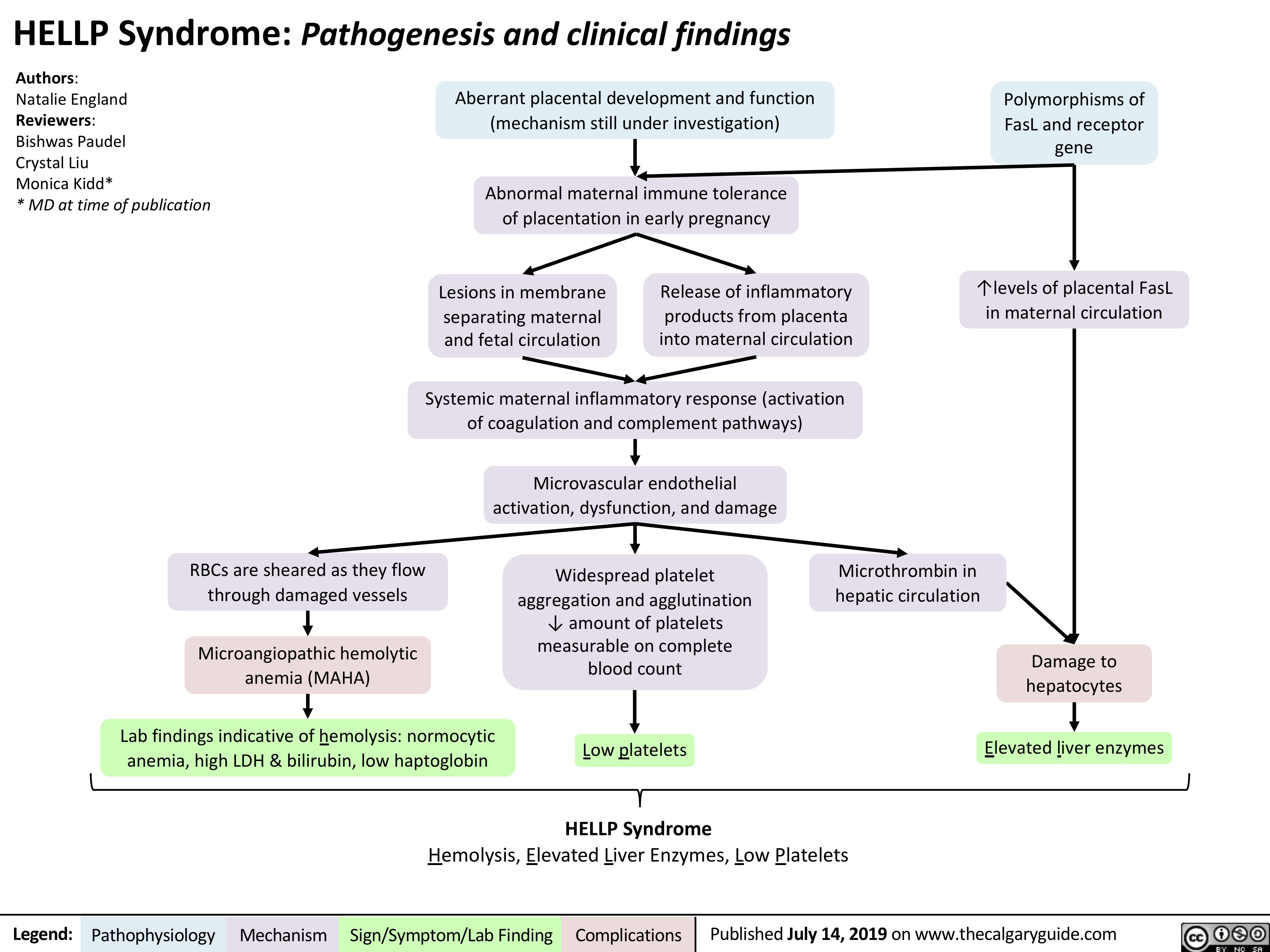
Lyme Disease Pathogenesis and Clinical Findings
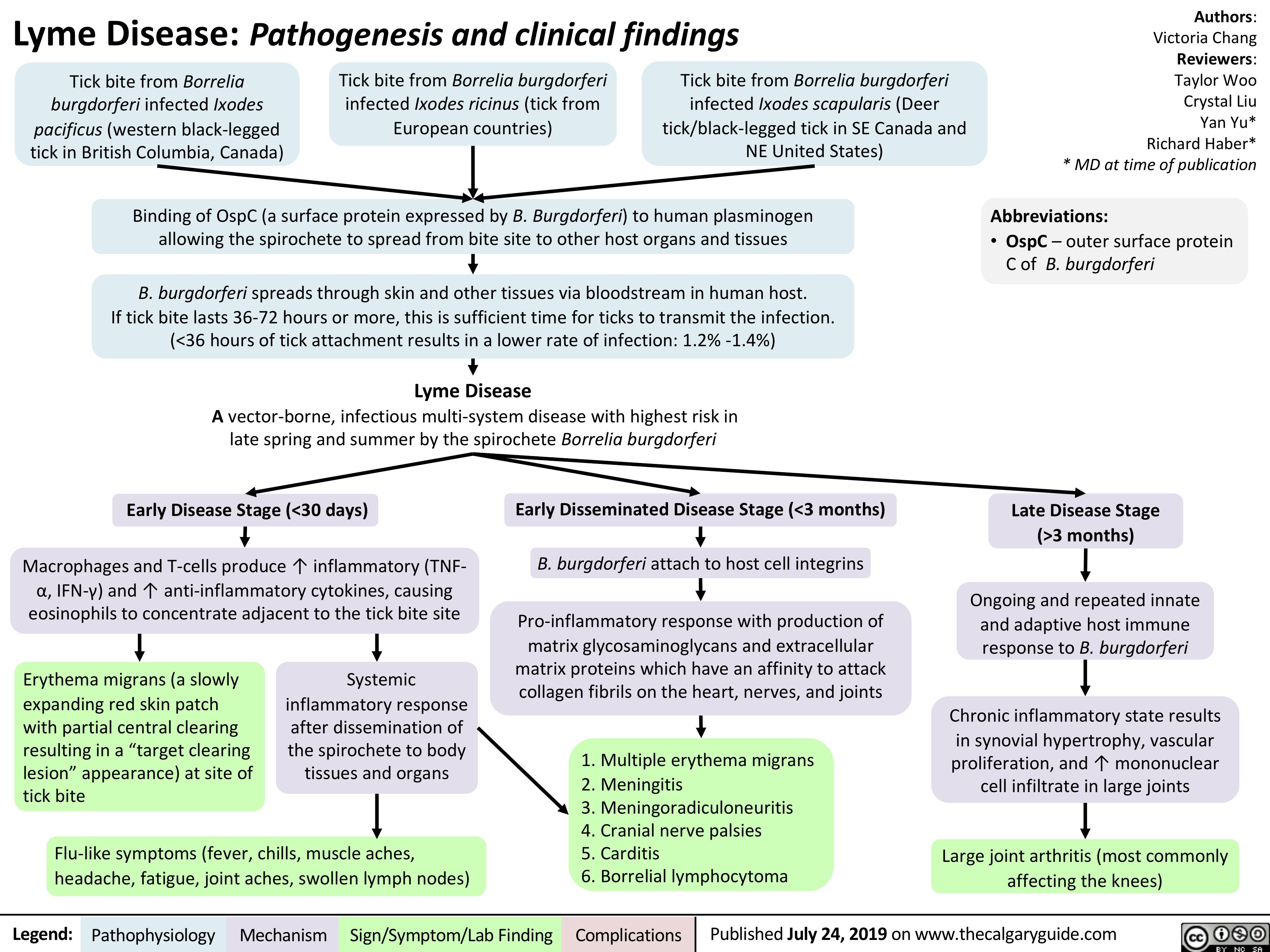
intraventricular-hemorrhage-in-preterm-infants-clinical-findings-and-complications
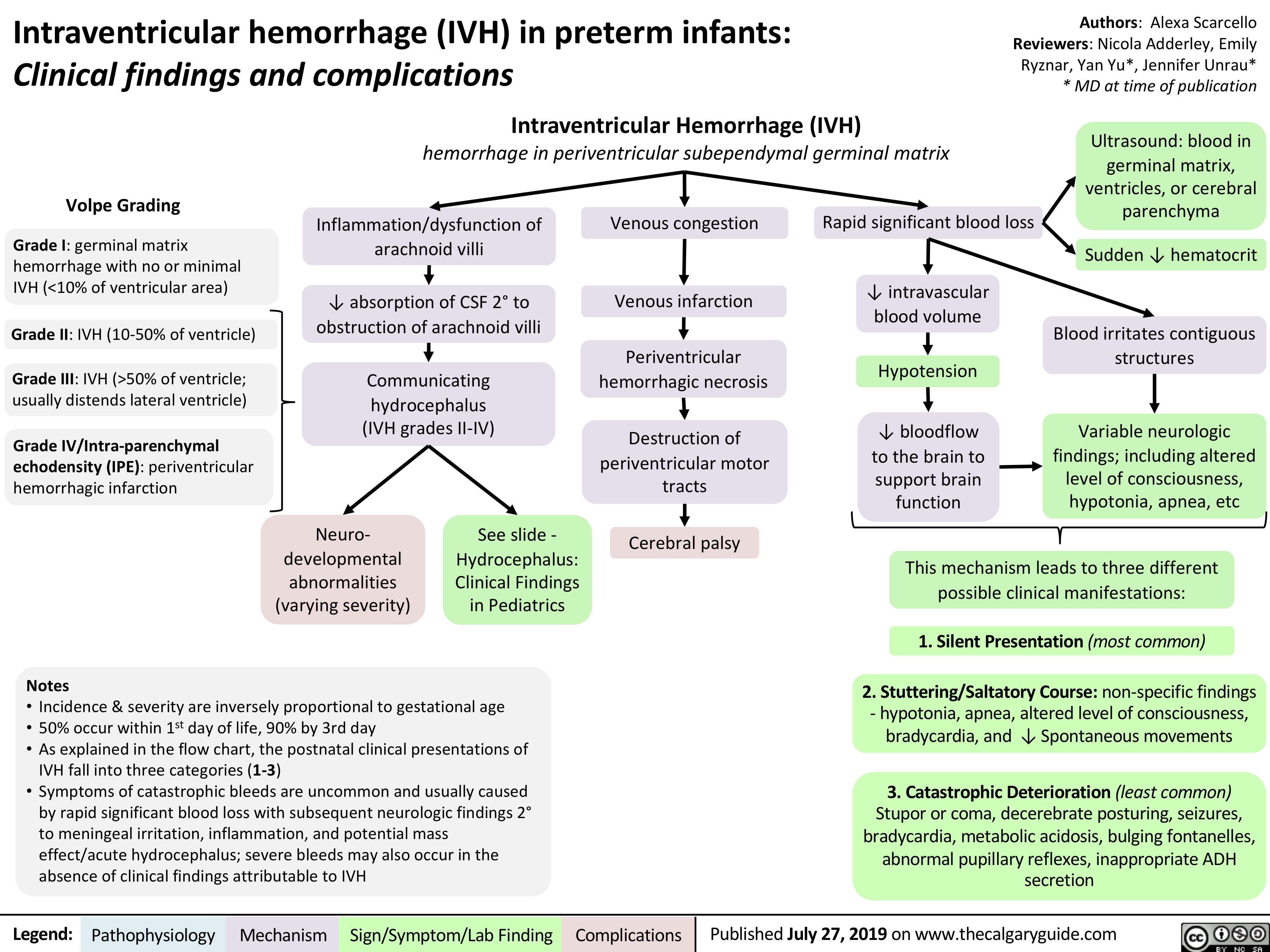
Vitamin K Deficiency

Normocytic Anemia
![Normocytic Anemia: Causes, Signs, and Symptoms
Authors: Katie Lin Yan Yu Reviewers: Andrew Brack Jessica Tjong Man-Chiu Poon* Lynn Savoie* * MD at time of publication
Aplastic anemia: hypo-proliferation of bone marrow RBC precursors
Anemia of Chronic Disease
Splenomegaly
↑ RBC sequestration within enlarged spleen
Acute bleeding
Hemolysis (infection, autoimmune, RBC structural defects)
↓ RBC production
↑ RBC destruction/elimination
Normocytic Anemia:
[Hgb] <120g/L in females, <140g/L in males, with the RBC mean corpuscular volume (MCV) still within the normal range: 80-100 fL
RBCs that ultimately end up in the blood are still qualitatively normal/functional; there is a quantitative shortage of these RBCs in the blood relative to body needs
Spurious/False normocytic anemia:
Any fluid overload state (pregnancy, heart failure, kidney disease, etc.) can ↑ plasma volume which can dilute RBCs and cause apparent anemia, but the mean volume of each RBC is still normal
Normocytic Anemia
Heart needs to work faster to pump
sufficient oxygenated blood to tissues
↑ Heart rate
Reduced oxygen- carrying ability of blood
Patient feels oxygen- deprived, needs to inhale more oxygen as compensation
Dyspnea (shortness of breath) ↑ Respiratory rate (RR)
Not enough oxygen being delivered to body tissues, including brain
Fatigue
Reduced absolute number of RBCs means less RBCs to color the blood red
Pallor (especially conjunctival and palmar)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published July 27, 2019 on www.thecalgaryguide.com
Normocytic Anemia: Causes, Signs, and Symptoms
Authors: Katie Lin Yan Yu Reviewers: Andrew Brack Jessica Tjong Man-Chiu Poon* Lynn Savoie* * MD at time of publication
Aplastic anemia: hypo-proliferation of bone marrow RBC precursors
Anemia of Chronic Disease
Splenomegaly
↑ RBC sequestration within enlarged spleen
Acute bleeding
Hemolysis (infection, autoimmune, RBC structural defects)
↓ RBC production
↑ RBC destruction/elimination
Normocytic Anemia:
[Hgb] <120g/L in females, <140g/L in males, with the RBC mean corpuscular volume (MCV) still within the normal range: 80-100 fL
RBCs that ultimately end up in the blood are still qualitatively normal/functional; there is a quantitative shortage of these RBCs in the blood relative to body needs
Spurious/False normocytic anemia:
Any fluid overload state (pregnancy, heart failure, kidney disease, etc.) can ↑ plasma volume which can dilute RBCs and cause apparent anemia, but the mean volume of each RBC is still normal
Normocytic Anemia
Heart needs to work faster to pump
sufficient oxygenated blood to tissues
↑ Heart rate
Reduced oxygen- carrying ability of blood
Patient feels oxygen- deprived, needs to inhale more oxygen as compensation
Dyspnea (shortness of breath) ↑ Respiratory rate (RR)
Not enough oxygen being delivered to body tissues, including brain
Fatigue
Reduced absolute number of RBCs means less RBCs to color the blood red
Pallor (especially conjunctival and palmar)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published July 27, 2019 on www.thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2015/05/Normocytic-Anemia-1.jpg)
Appendicitis
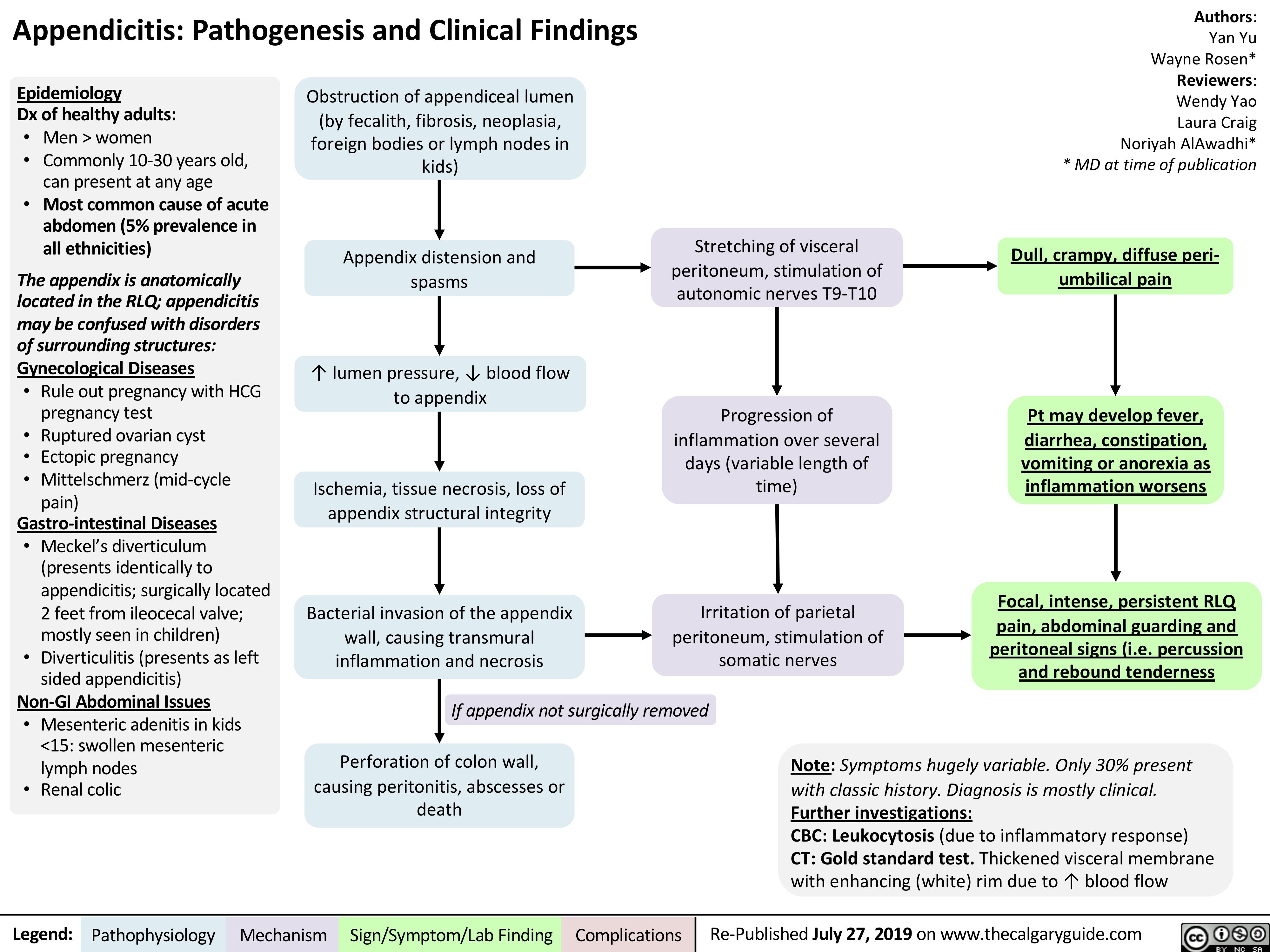
Acute GI Related Abdominal Pain

Operative vaginal delivery Complications of Vacuum
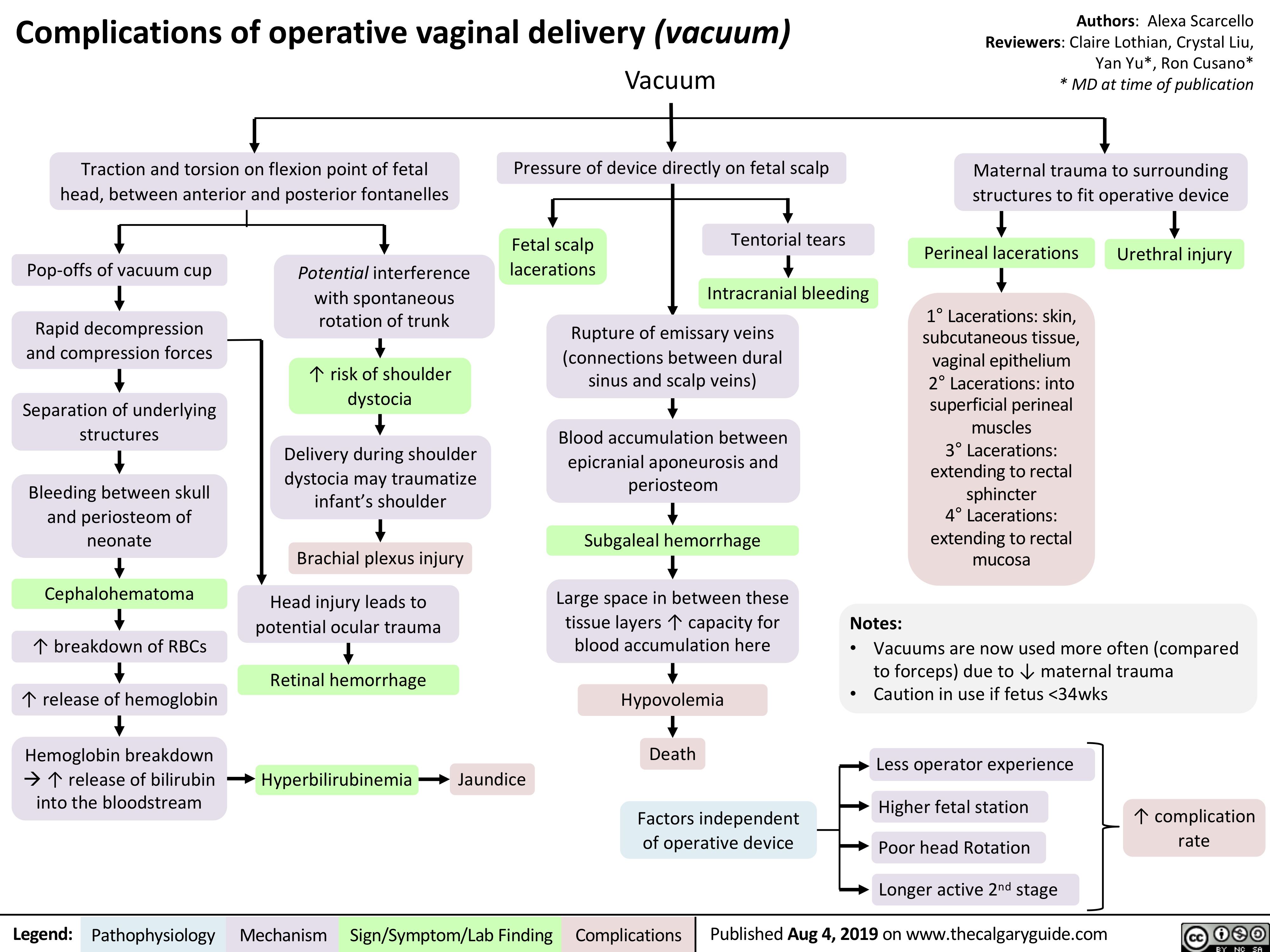
Ataxia Telangiectasia Pathogenesis and Clinical Findings
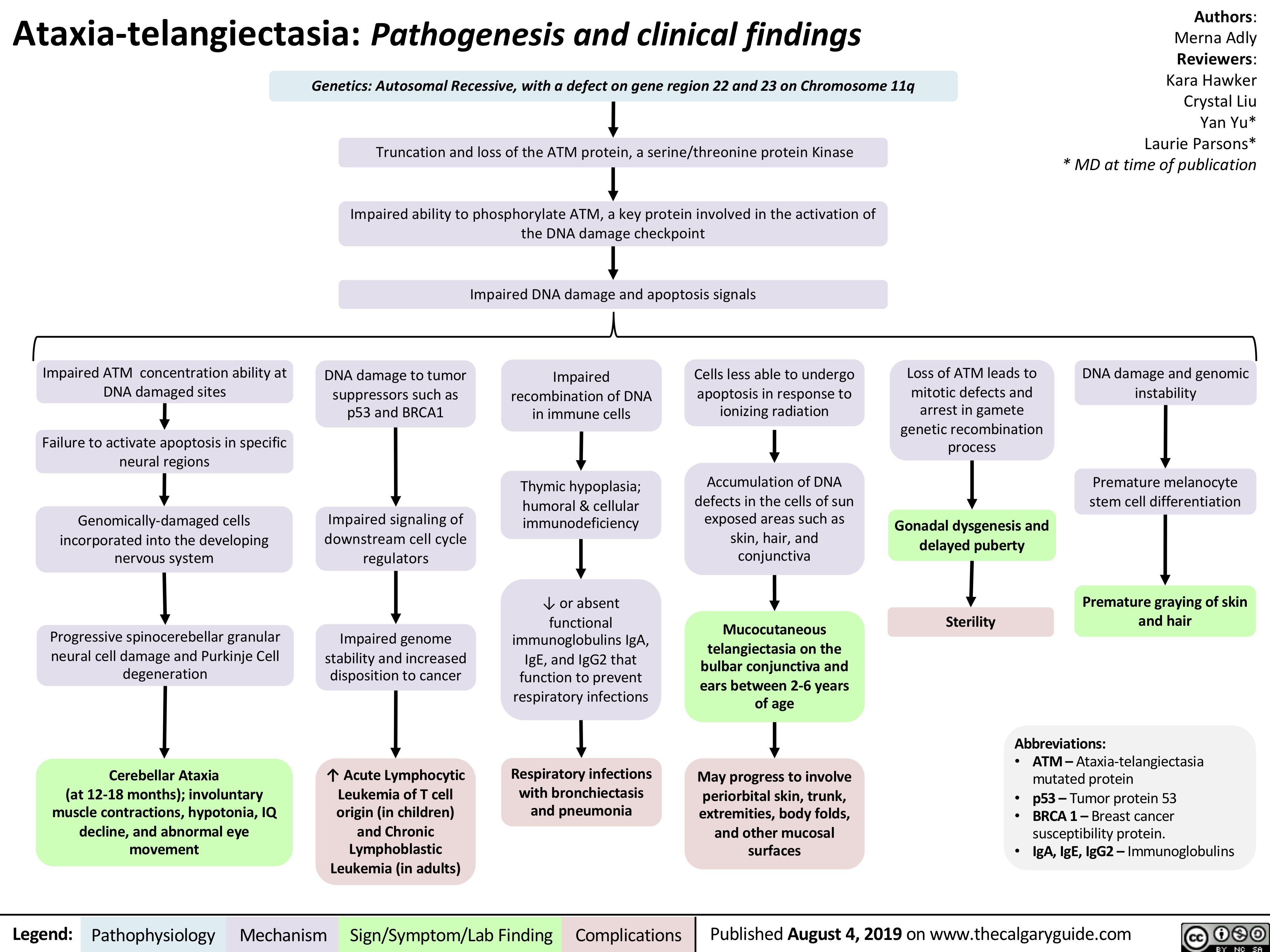
Diverticulosis and Angiodysplasia
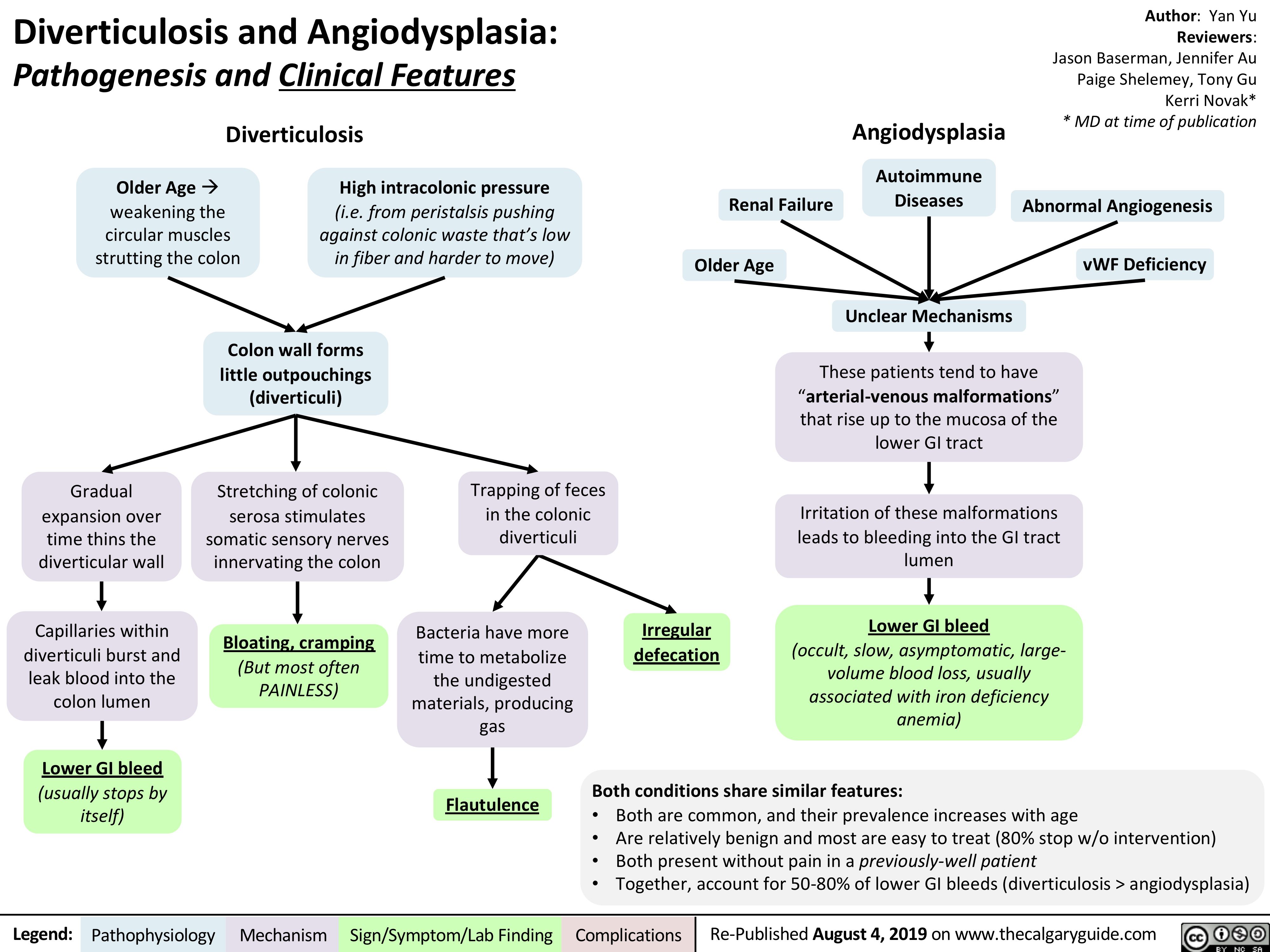
Erythema Nodosum pathogenesis and clinical findings
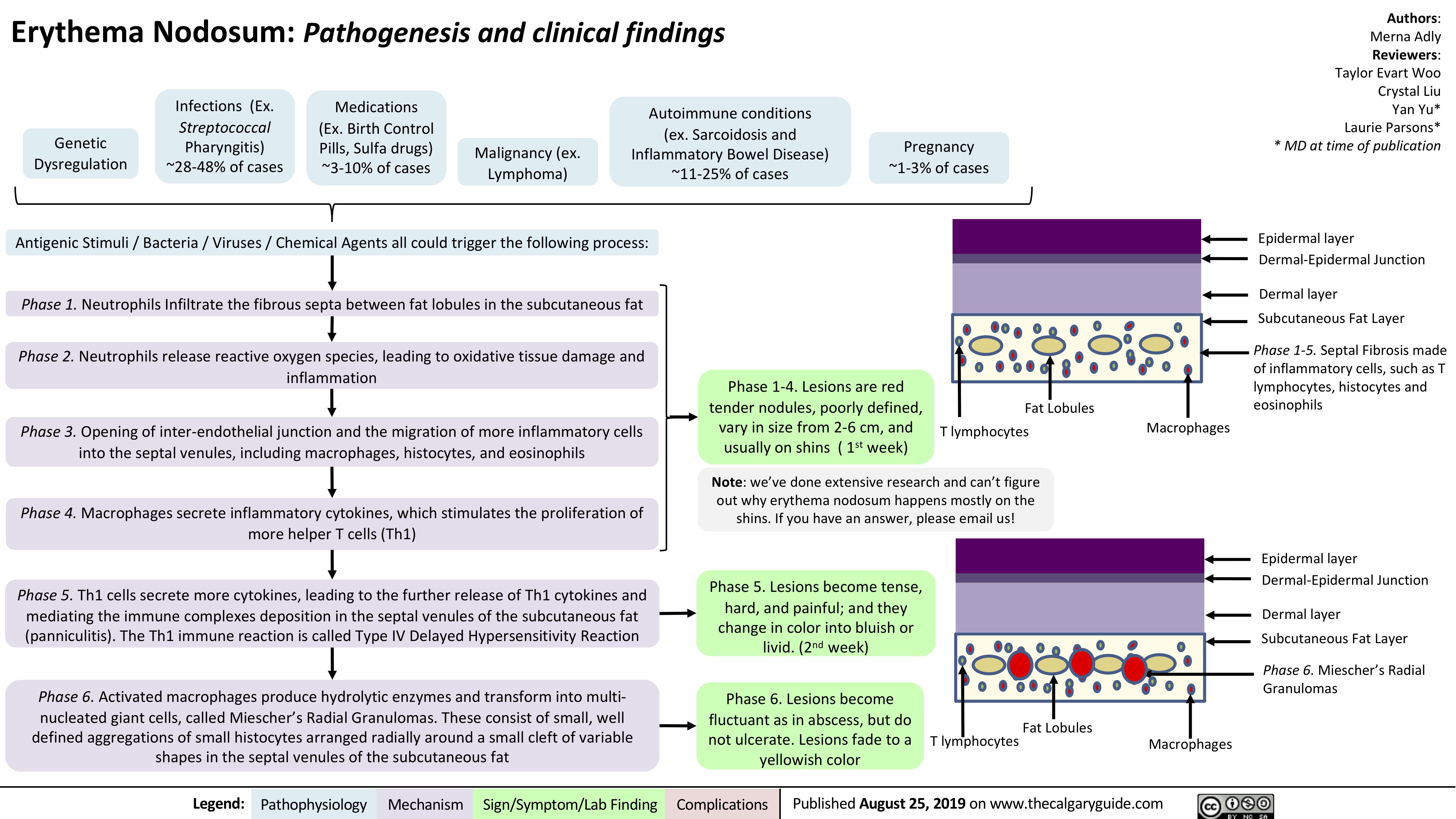
Colorectal Carcinoma pathogenesis and clinical findings
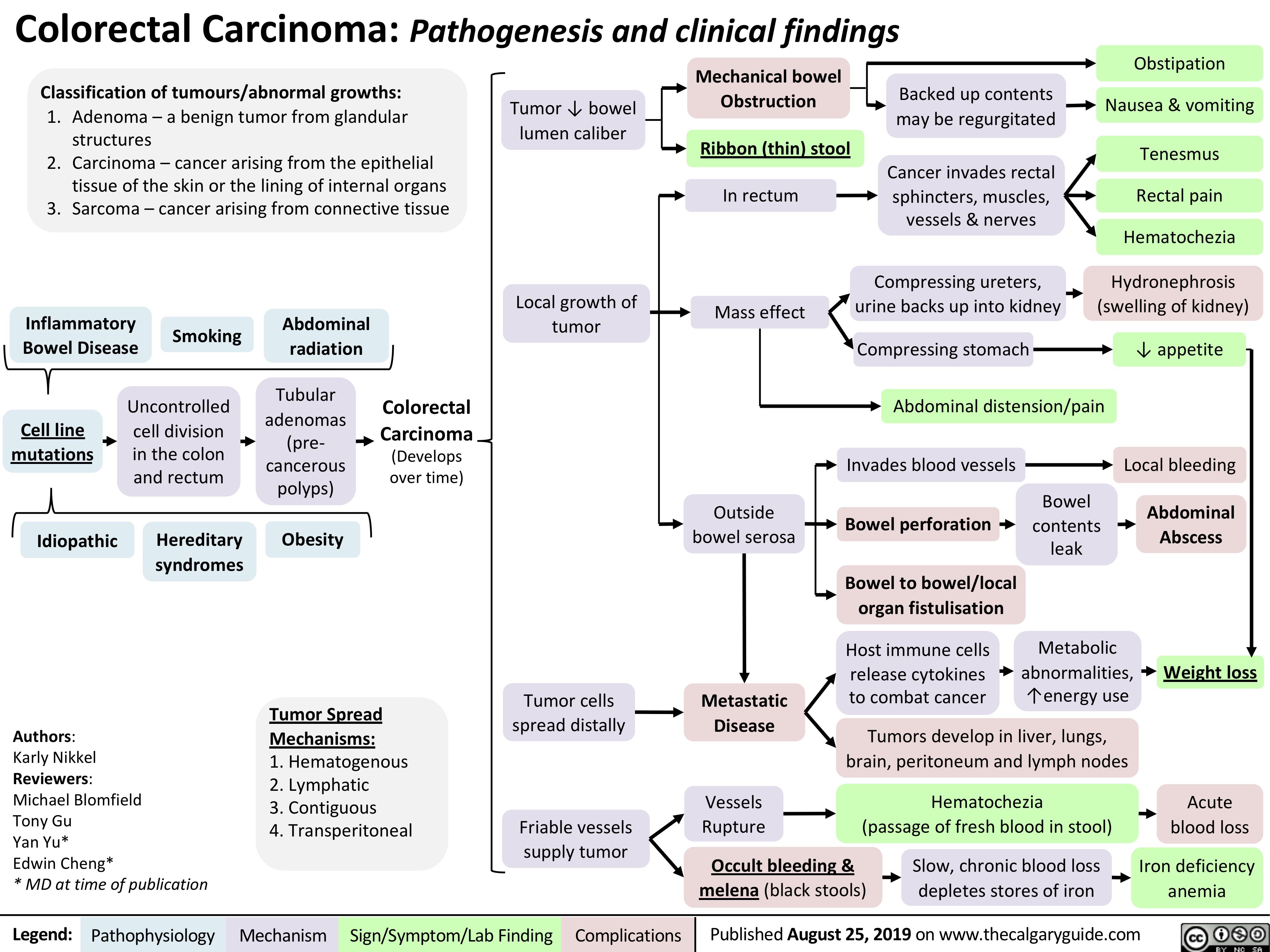
iga-vasculitis-henoch-scholein-purpura-pathogenesis-and-clinical-findings
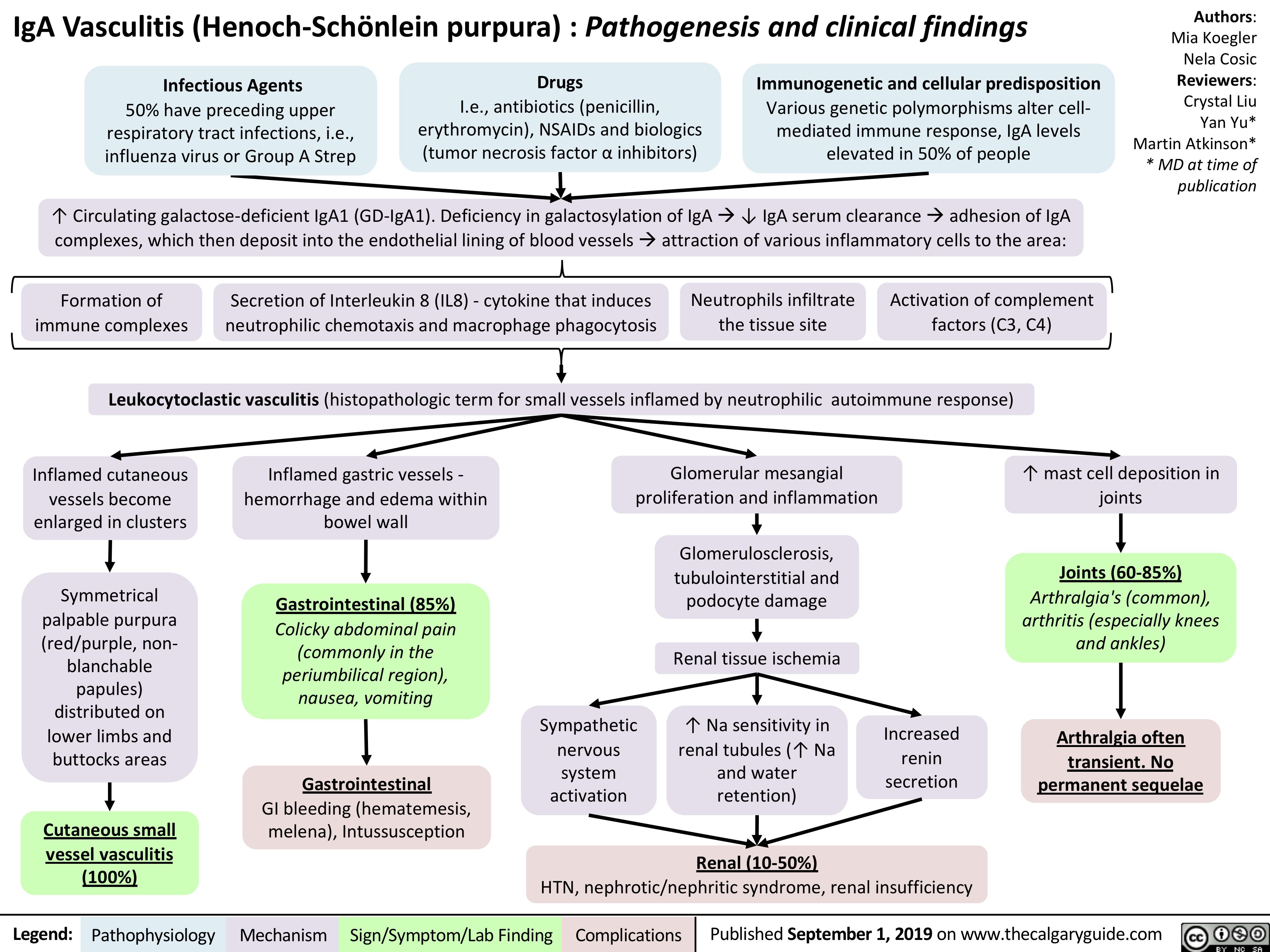
Negative-Pressure-Pulmonary-Edema
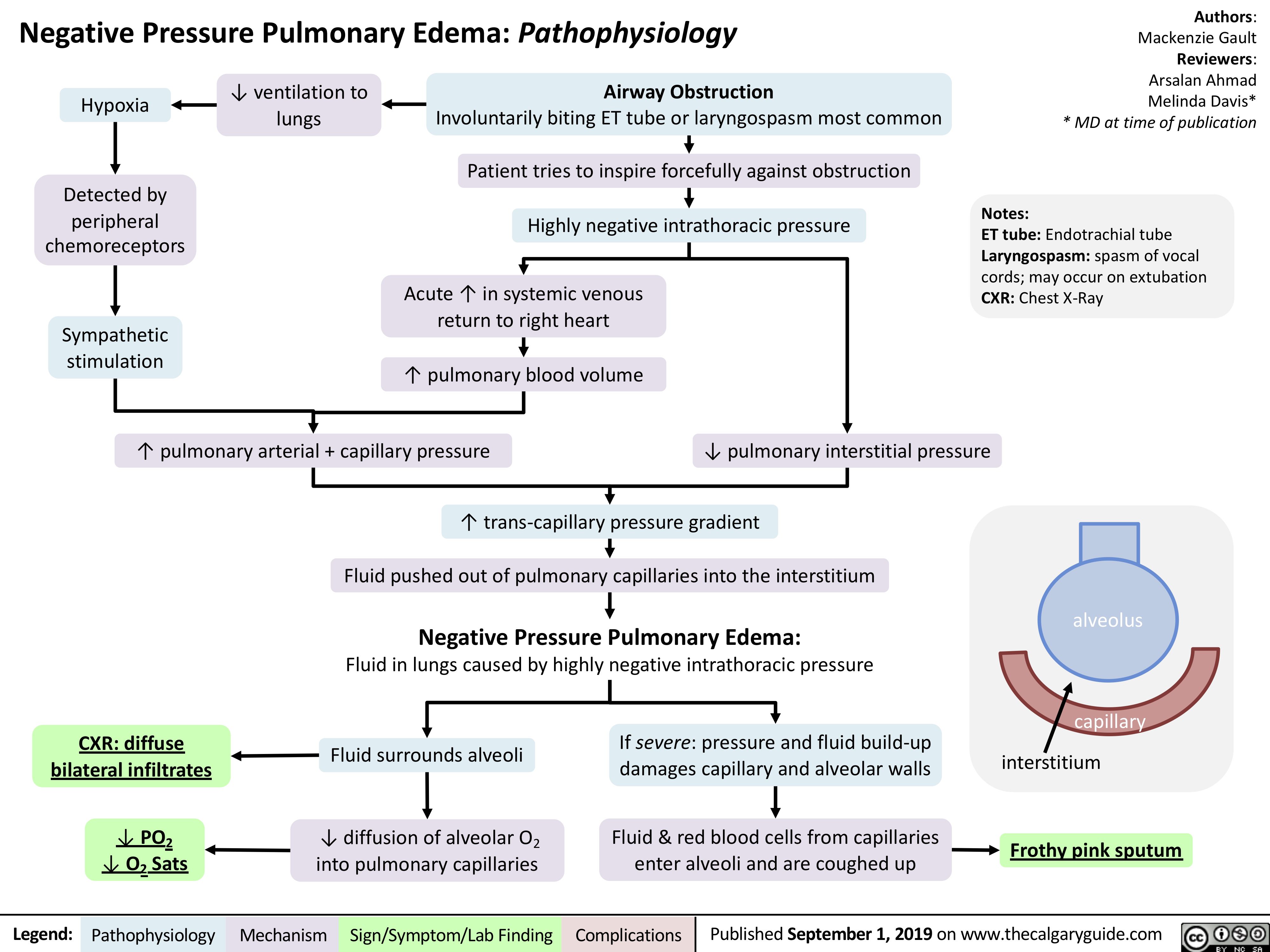
Thrombotic Thrombocytopenic Purpura-Hemolytic Uremic Syndrome (TTP-HUS): Pathogenesis and clinical findings
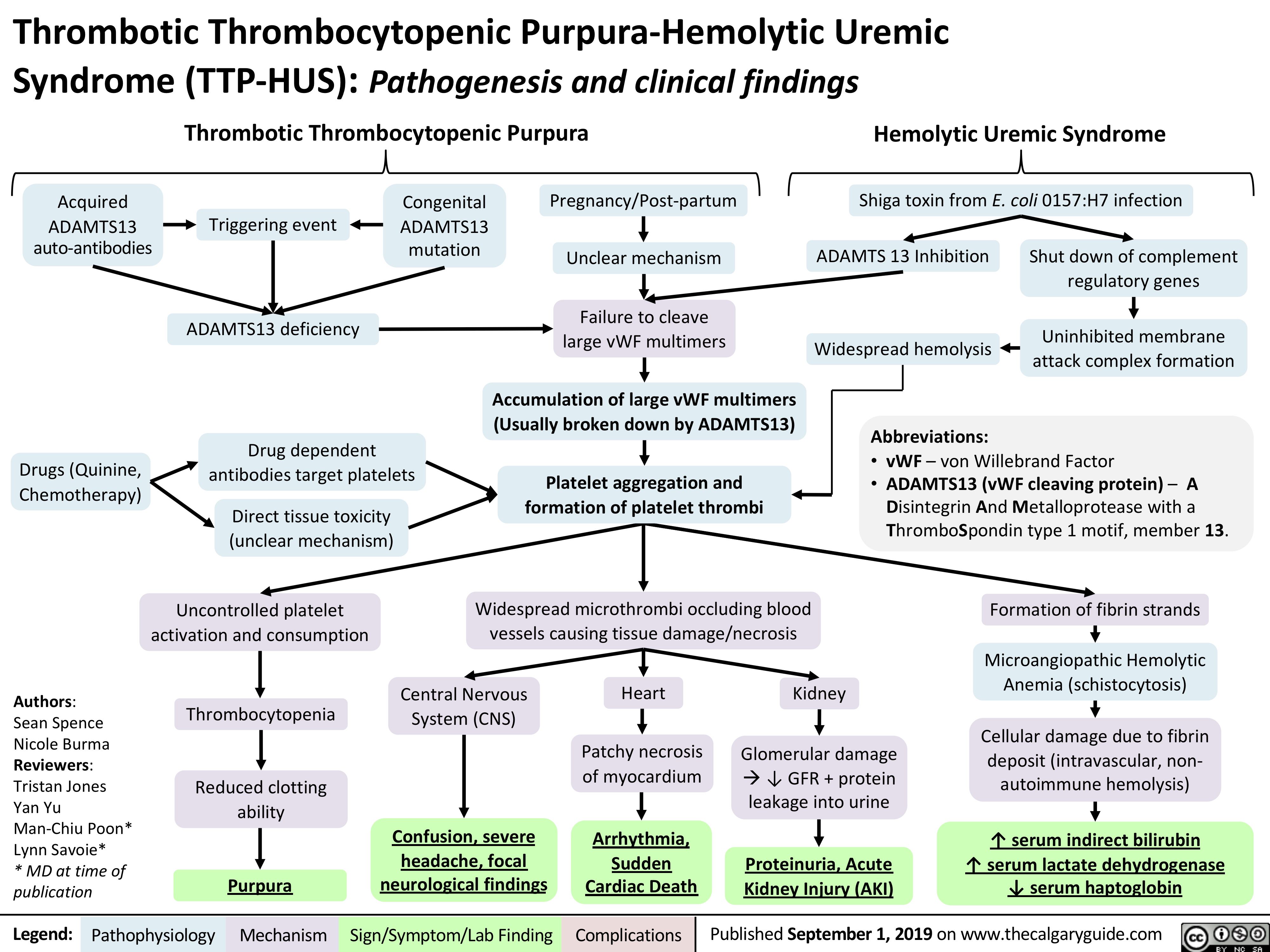
Acute-diverticulitis
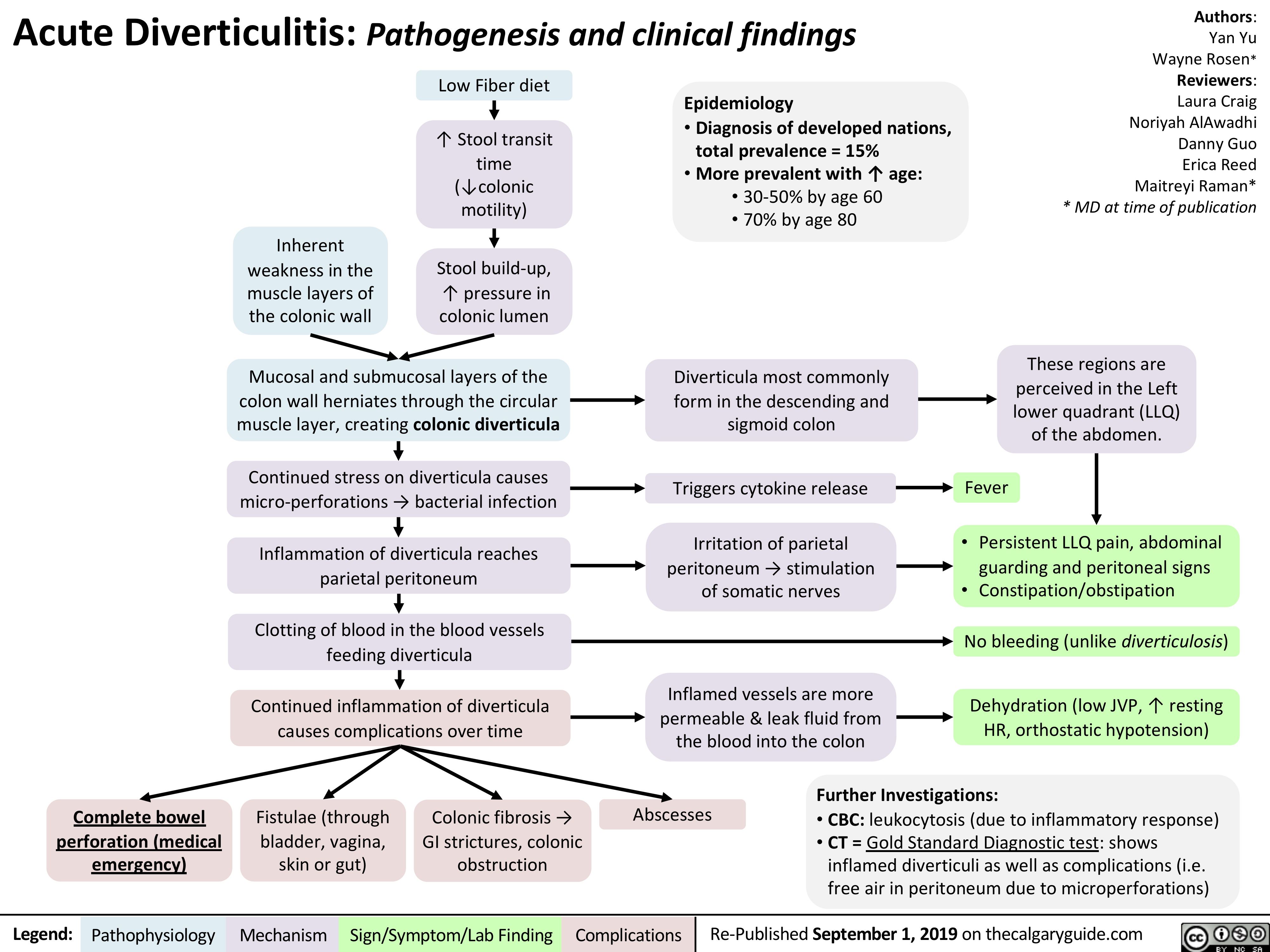
virchows-triad-and-deep-vein-thrombosis-dvt
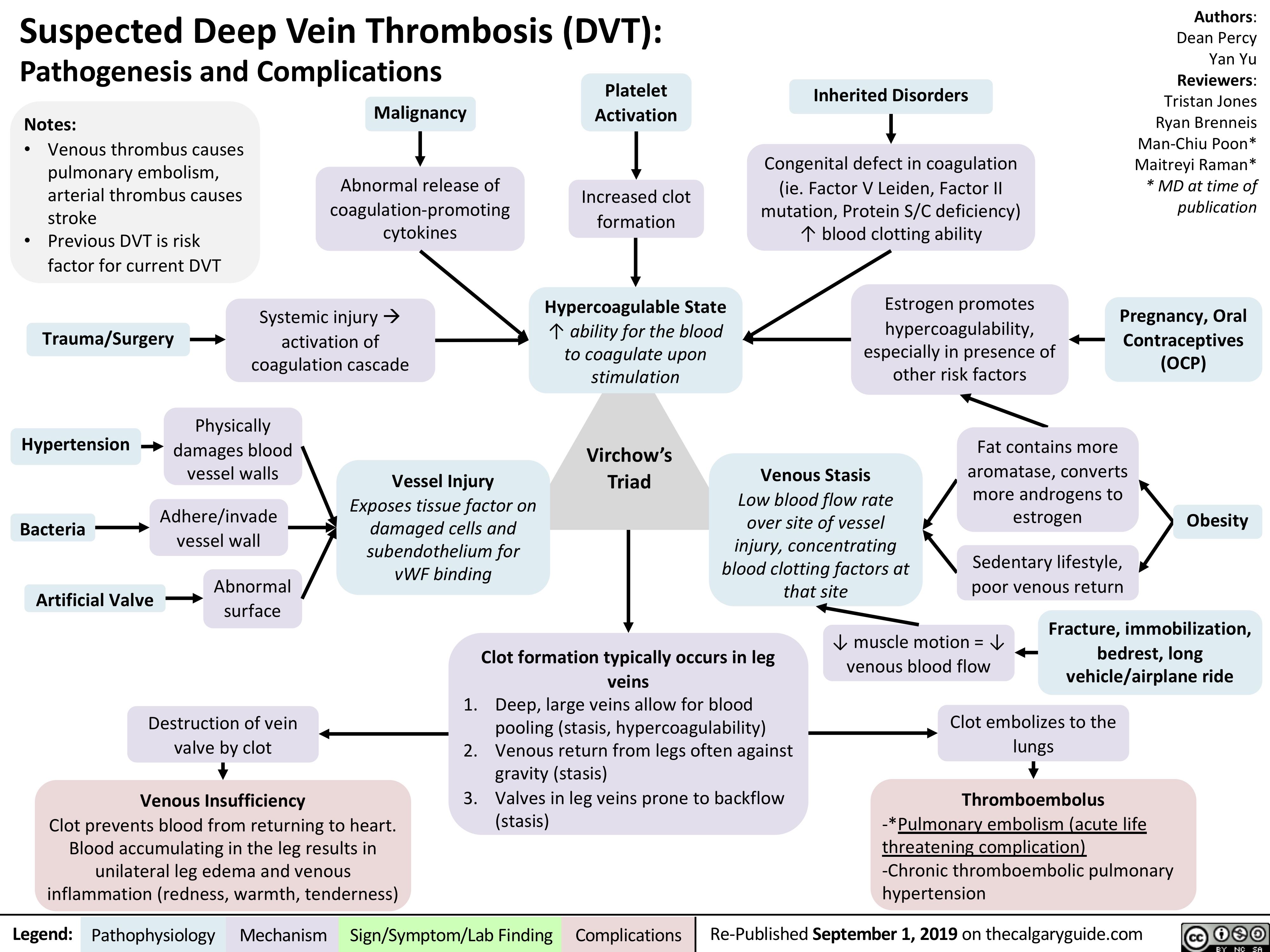
Acute-Pancreatitis
![Acute Pancreatitis: Pathogenesis and Clinical Findings
Authors: Yan Yu Reviewers: Laura Craig Noriyah AlAwadhi Ryan Brenneis Maitreyi Raman* * MD at time of publication
Associated signs due to intra- abdominal hemorrhage from an unknown mechanism (classically associated with pancreatitis, but happens in <1% of cases):
Note:
It is not enough to just diagnose “acute pancreatitis”. Full management requires determining underlying etiology with further work-up.
Alcohol
↑ Toxic metabolites within pancreas and Spincter of Oddi Spasms
Gallstones
Migration to common bile duct blocks Sphincter of Oddi
Hypertriglyceridemia
Unknown
mechanism (rare)
Idiopathic
Further investigations:
CBC: Cell counts elevated, due to sever hypovolemia
Serum [Lipase]: Gold Standard Diagnostic Test; rupture of pancreatic cells releases lipase into circulation
Pancreatic secretions back up, ↑ pressure within pancreas
Hypercalcemia (Rare; Ca2+ depositions in bile ducts block outflow of pancreatic secretions)
Since pancreas is retroperitoneal, somatic
nerves in the parietal peritoneum are directly stimulated
Inflammation triggers cytokine release
Inflamed pancreas irritates adjacent intestines, causing ileus
Inflamed, more permeable blood vessels leak fluid into pancreas
• •
Cullen’s sign (bruising in peri-umbilical region) Grey-Turner’s sign (bruises along both flanks)
Sudden, severe epigastric pain (with peritoneal signs), radiates to the center of the back
Fever, nausea/vomiting
(general signs of inflammation)
Diminished bowel sounds Profound dehydration
(flat JVP, hypotension, tachycardia, oliguria) – may happen, not always
1. Pressure compresses pancreatic blood vessels, causing tissue ischemia.
2. Activation of inactive proteases (zymogens) digesting pancreatic tissue
Necrosis (death) of pancreatic cells
Inflammation self- perpetuates
Massive systemic inflammatory response
2 main complications, usually detected on CT;
may happen, but not always
1. Pancreatic pseudocyst (enlargement of the
pancreas due to fluid accumulation)
2. Pancreatic necrosis/abscesses (death of a part of the pancreas)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-published September 1, 2019 on thecalgaryguide.com
Acute Pancreatitis: Pathogenesis and Clinical Findings
Authors: Yan Yu Reviewers: Laura Craig Noriyah AlAwadhi Ryan Brenneis Maitreyi Raman* * MD at time of publication
Associated signs due to intra- abdominal hemorrhage from an unknown mechanism (classically associated with pancreatitis, but happens in <1% of cases):
Note:
It is not enough to just diagnose “acute pancreatitis”. Full management requires determining underlying etiology with further work-up.
Alcohol
↑ Toxic metabolites within pancreas and Spincter of Oddi Spasms
Gallstones
Migration to common bile duct blocks Sphincter of Oddi
Hypertriglyceridemia
Unknown
mechanism (rare)
Idiopathic
Further investigations:
CBC: Cell counts elevated, due to sever hypovolemia
Serum [Lipase]: Gold Standard Diagnostic Test; rupture of pancreatic cells releases lipase into circulation
Pancreatic secretions back up, ↑ pressure within pancreas
Hypercalcemia (Rare; Ca2+ depositions in bile ducts block outflow of pancreatic secretions)
Since pancreas is retroperitoneal, somatic
nerves in the parietal peritoneum are directly stimulated
Inflammation triggers cytokine release
Inflamed pancreas irritates adjacent intestines, causing ileus
Inflamed, more permeable blood vessels leak fluid into pancreas
• •
Cullen’s sign (bruising in peri-umbilical region) Grey-Turner’s sign (bruises along both flanks)
Sudden, severe epigastric pain (with peritoneal signs), radiates to the center of the back
Fever, nausea/vomiting
(general signs of inflammation)
Diminished bowel sounds Profound dehydration
(flat JVP, hypotension, tachycardia, oliguria) – may happen, not always
1. Pressure compresses pancreatic blood vessels, causing tissue ischemia.
2. Activation of inactive proteases (zymogens) digesting pancreatic tissue
Necrosis (death) of pancreatic cells
Inflammation self- perpetuates
Massive systemic inflammatory response
2 main complications, usually detected on CT;
may happen, but not always
1. Pancreatic pseudocyst (enlargement of the
pancreas due to fluid accumulation)
2. Pancreatic necrosis/abscesses (death of a part of the pancreas)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-published September 1, 2019 on thecalgaryguide.com](http://calgaryguide.ucalgary.ca/wp-content/uploads/2019/09/Acute-Pancreatitis.jpg)
Peptic Ulcer Disease
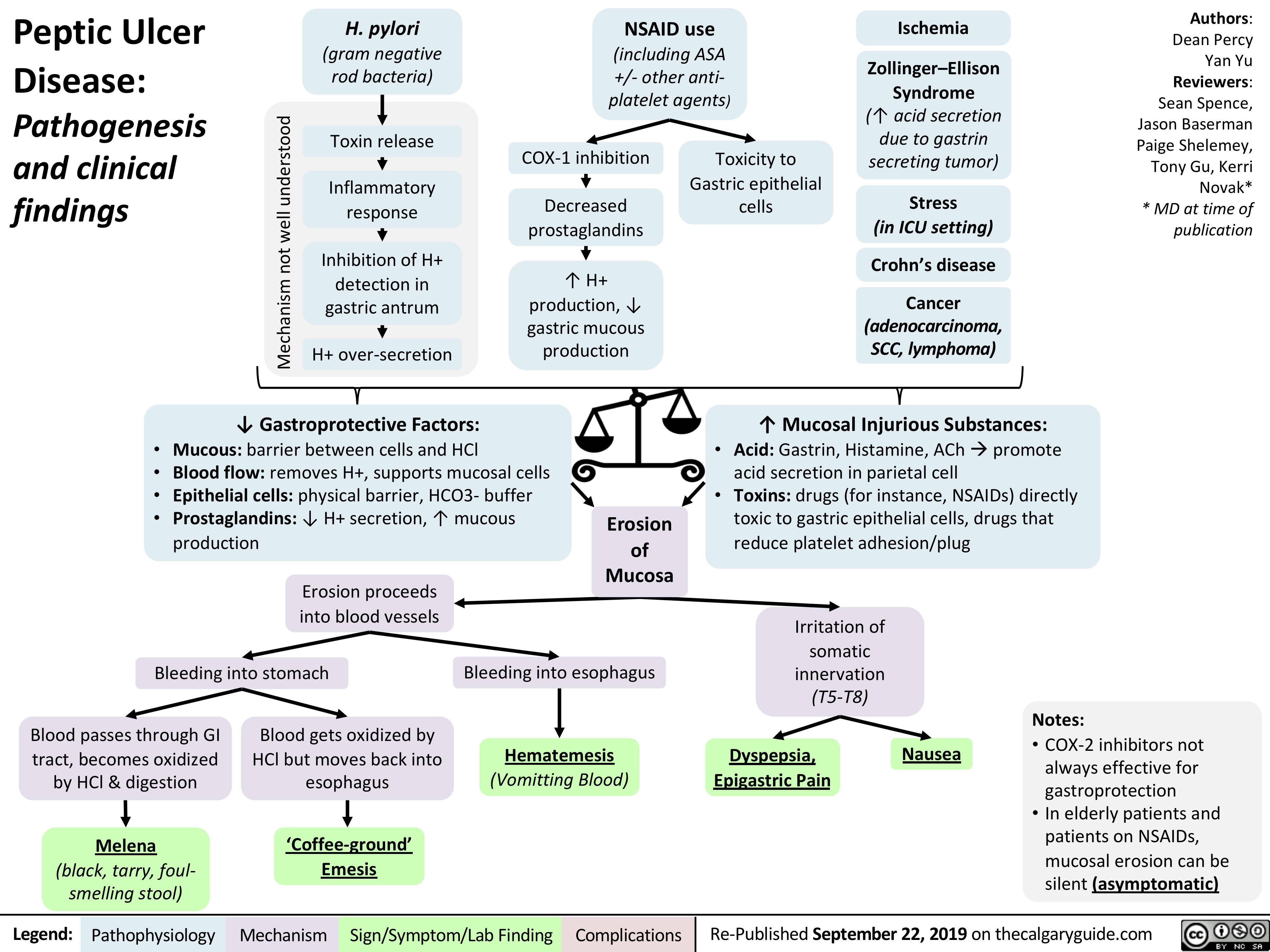
Rapid Sequence Induction and Intubation (RSII): Clinical Approach
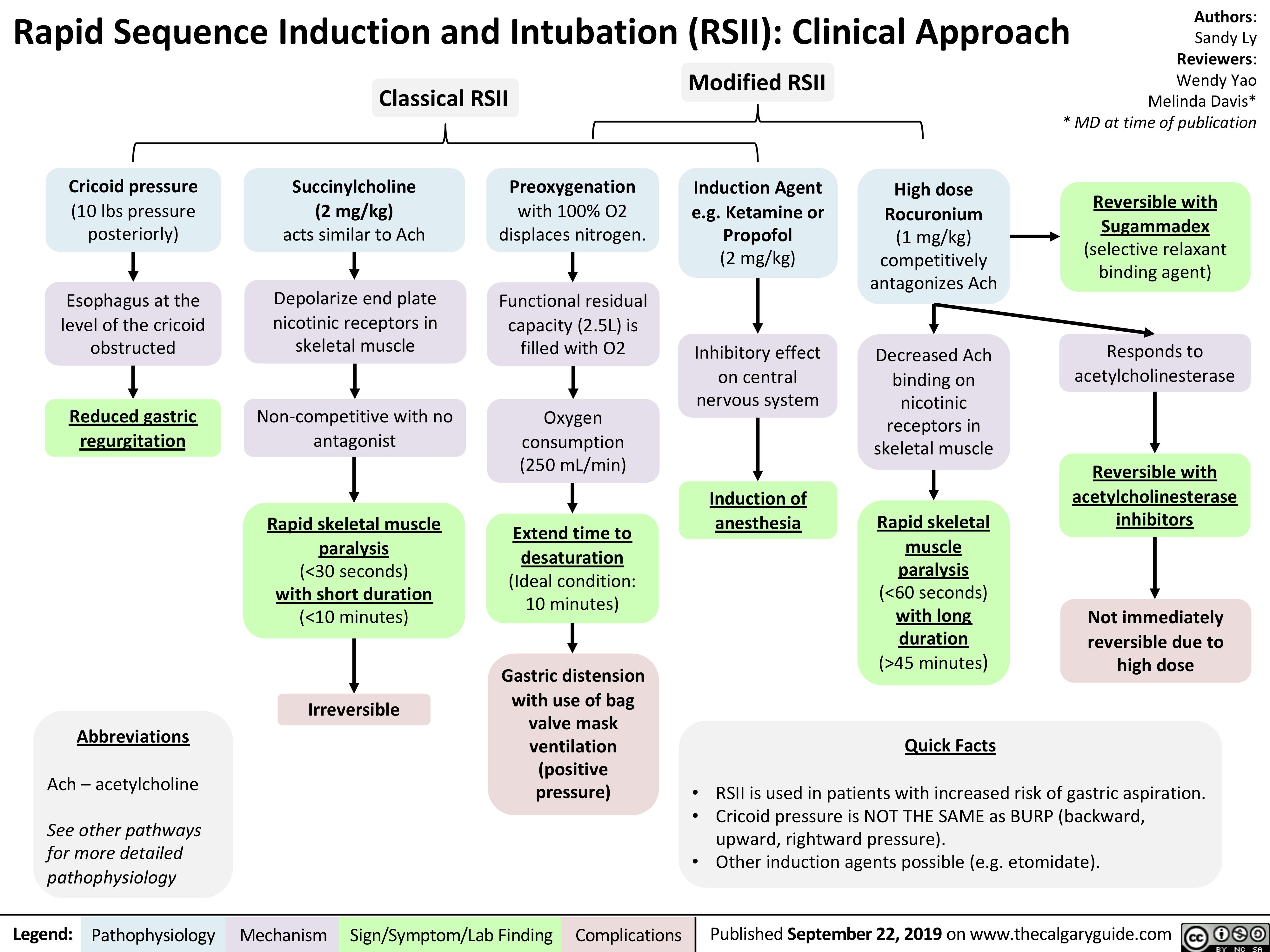
Priapism
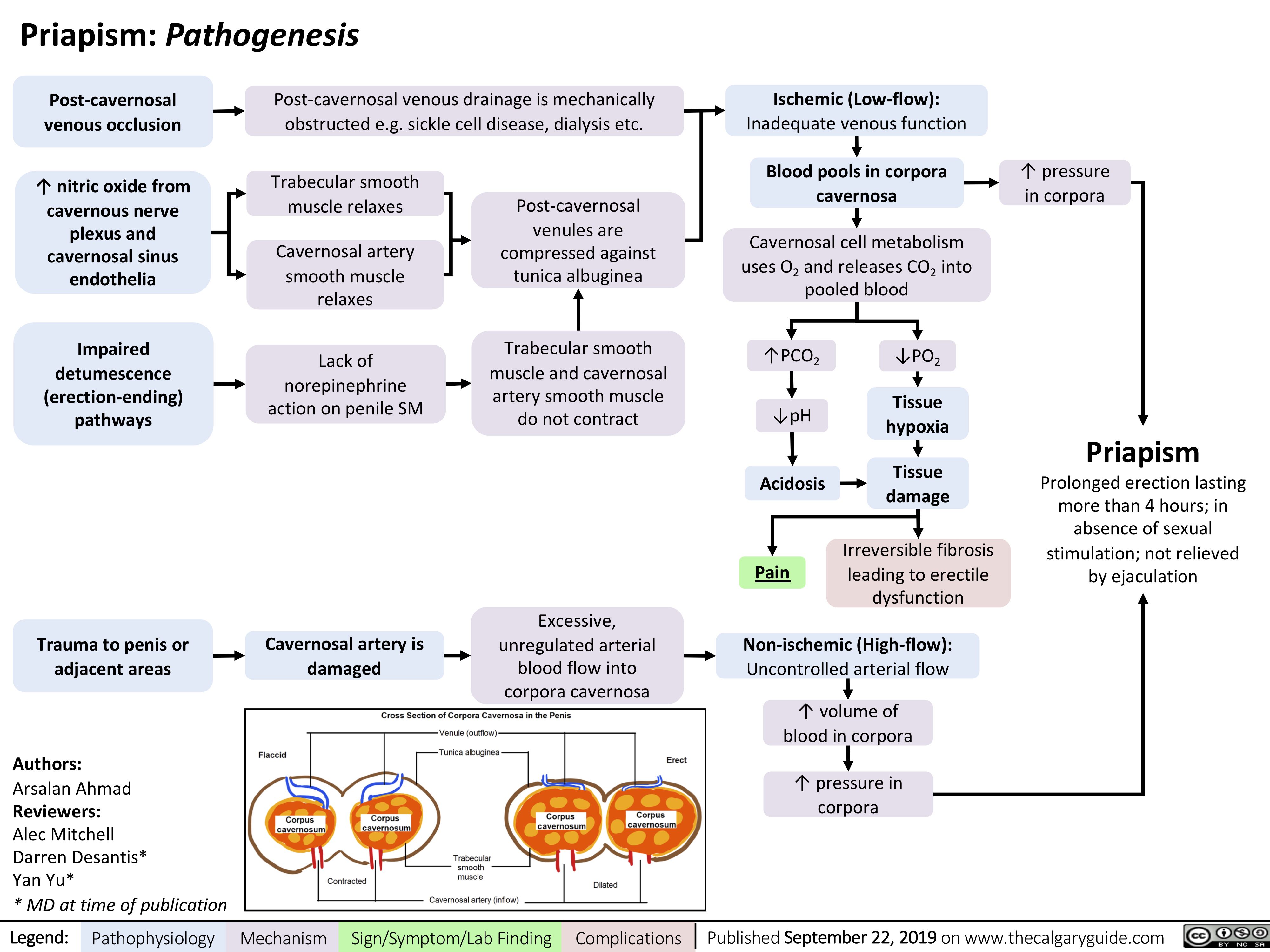
Infantile Colic
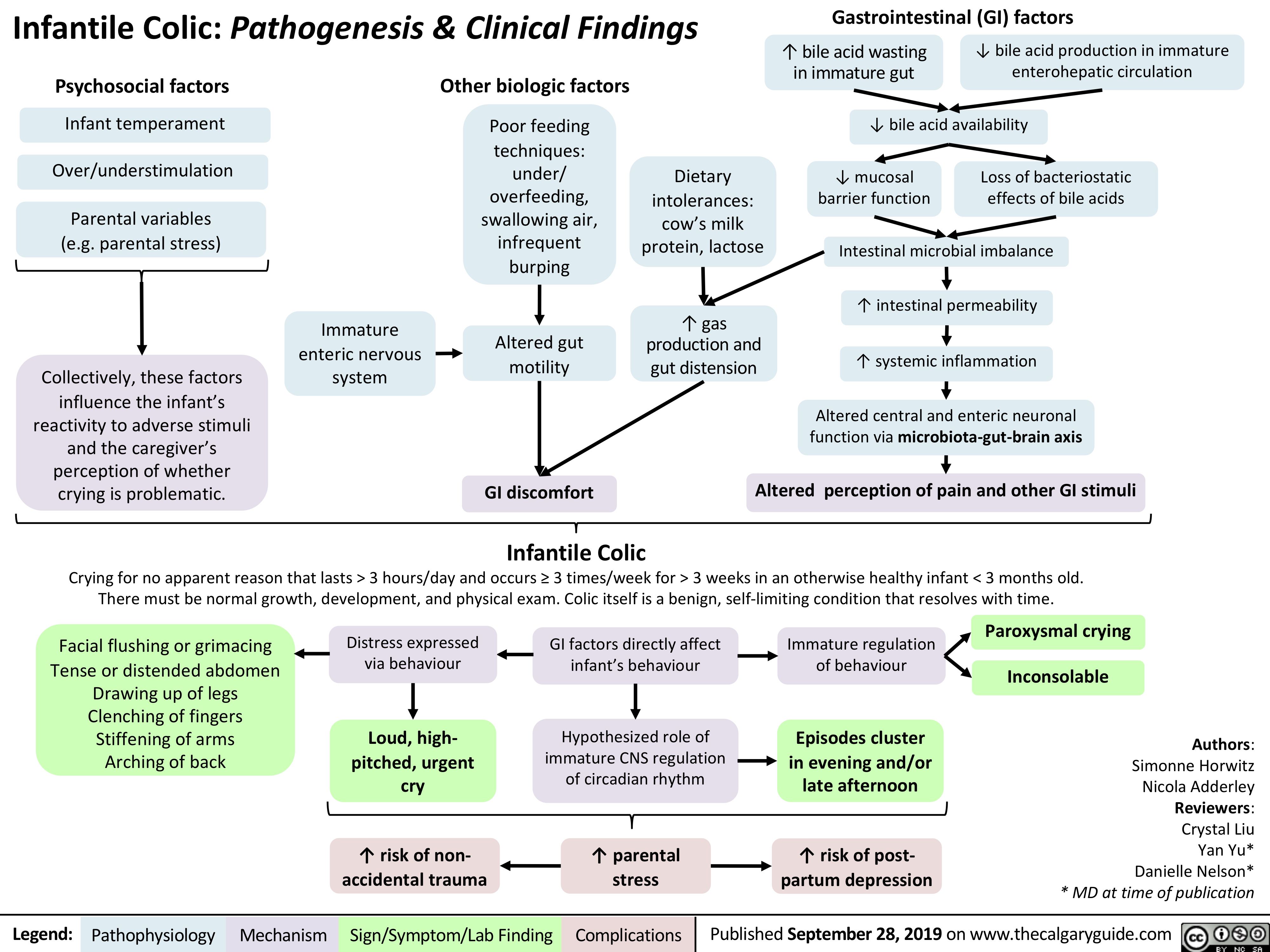
Macrosomia-Fetal-Complications
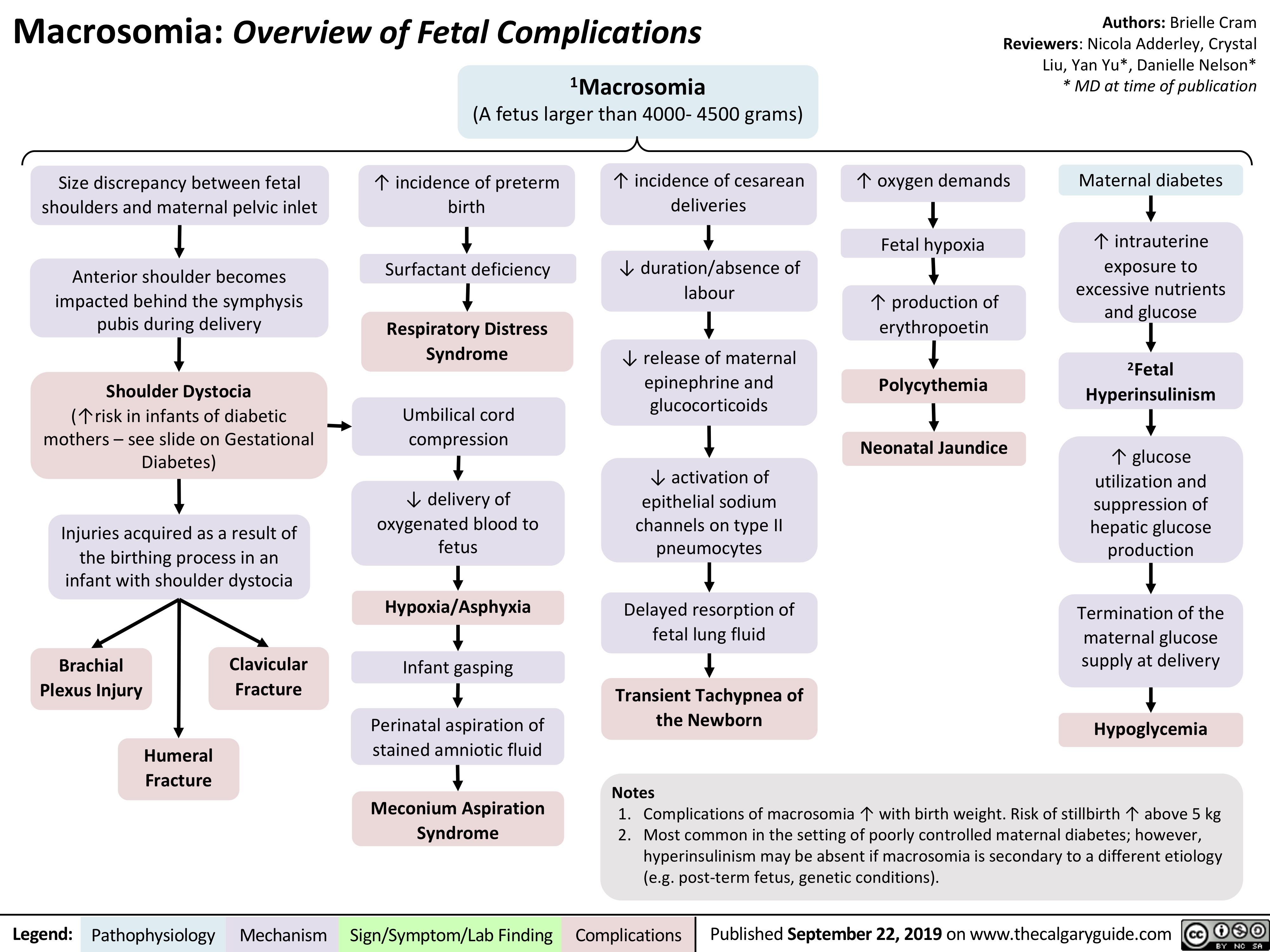
intrauterine-devices-iuds-mechanism-of-action
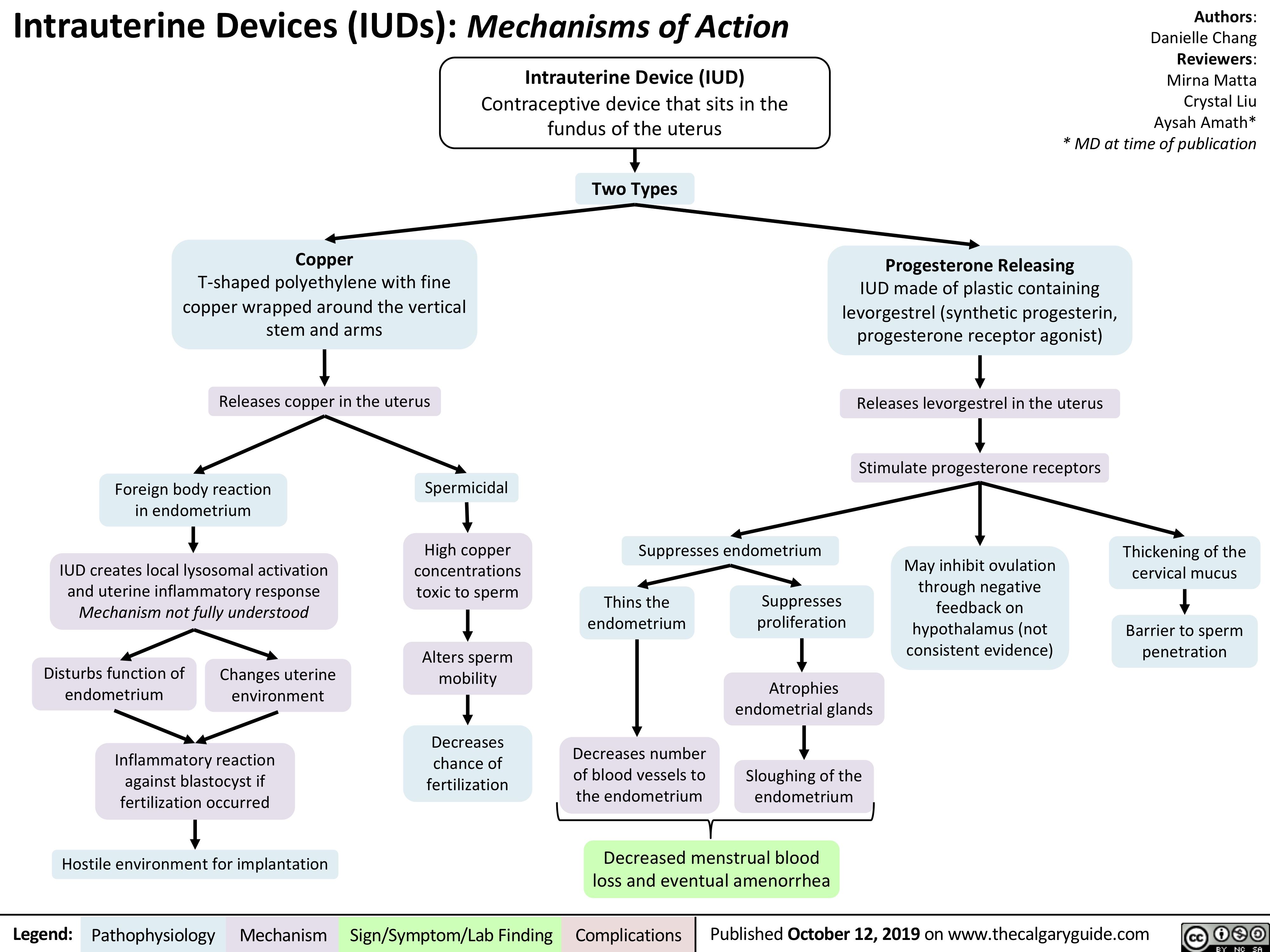
X-linked Severe Combined Immunodeficiency (SCID)
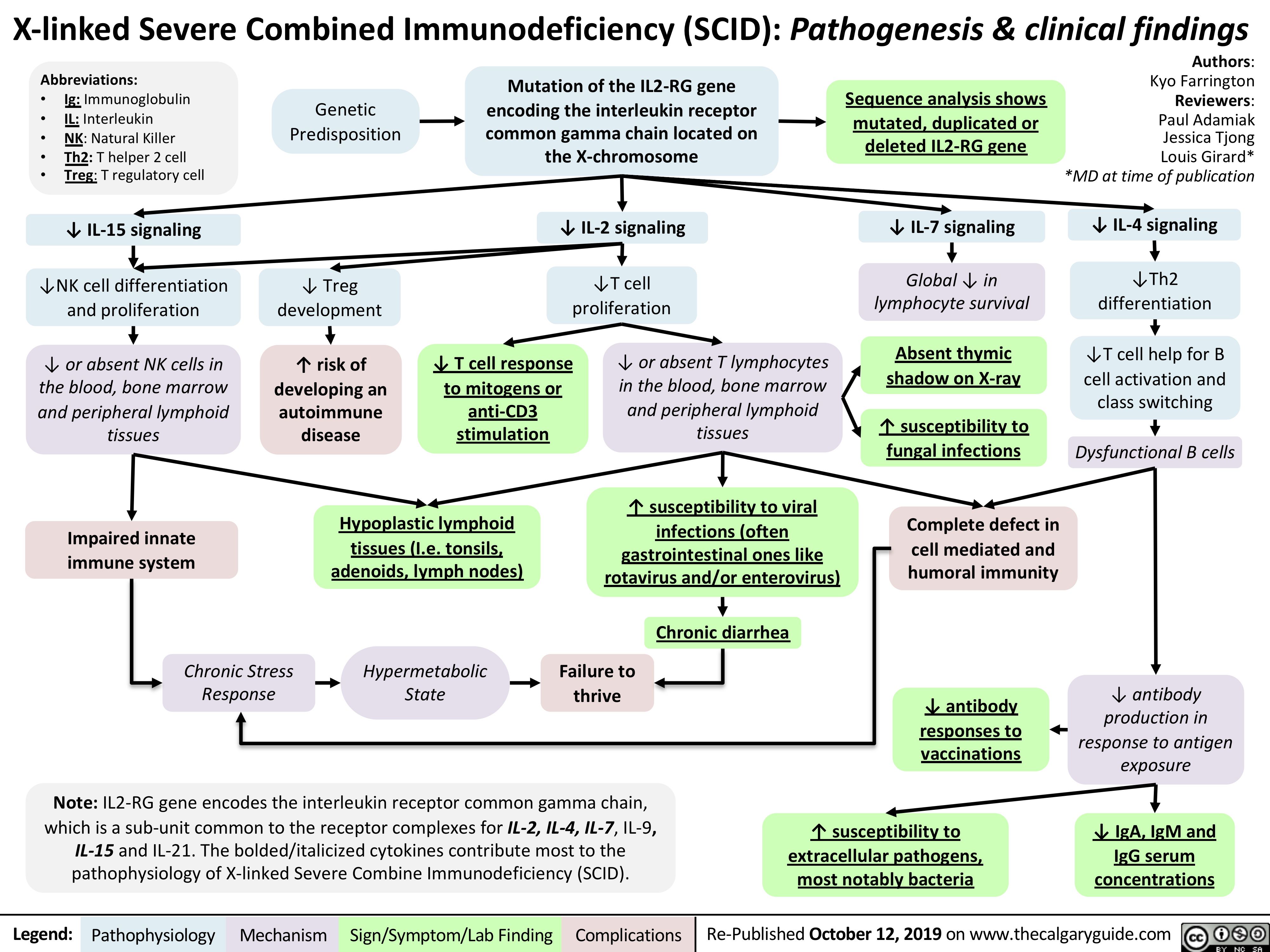
Ischemic Colitis
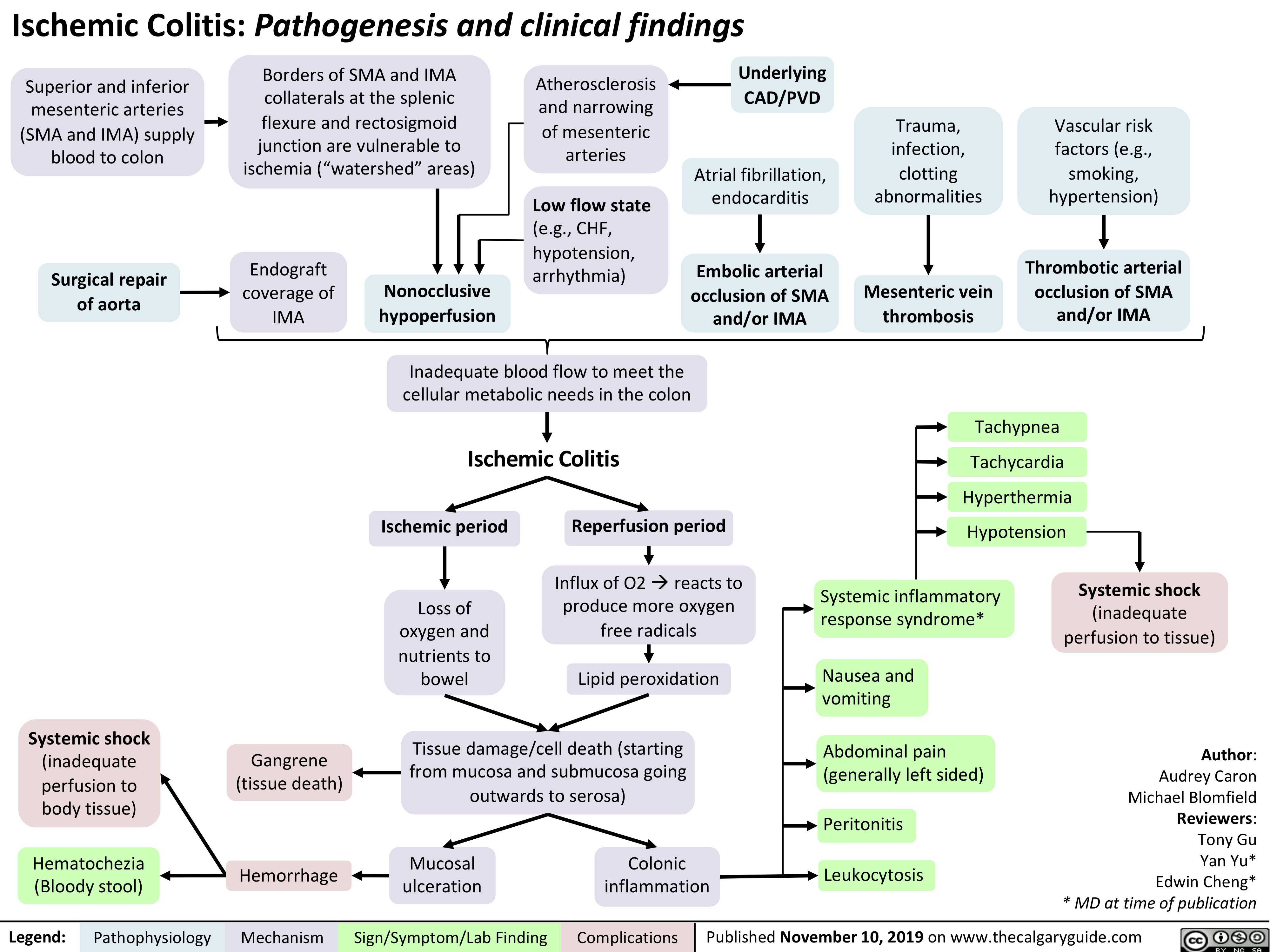
Incisional-Hernia
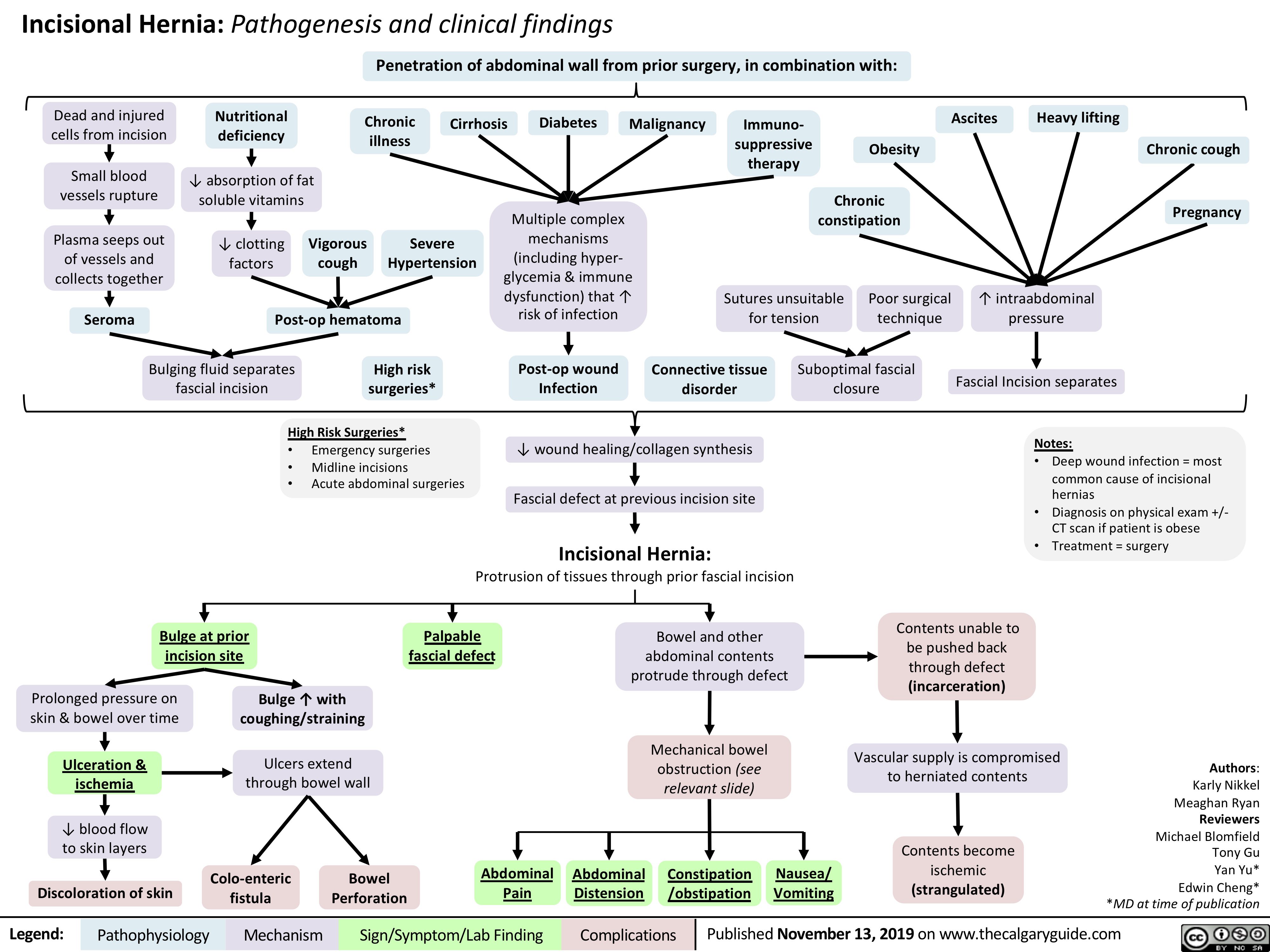
Endometritis
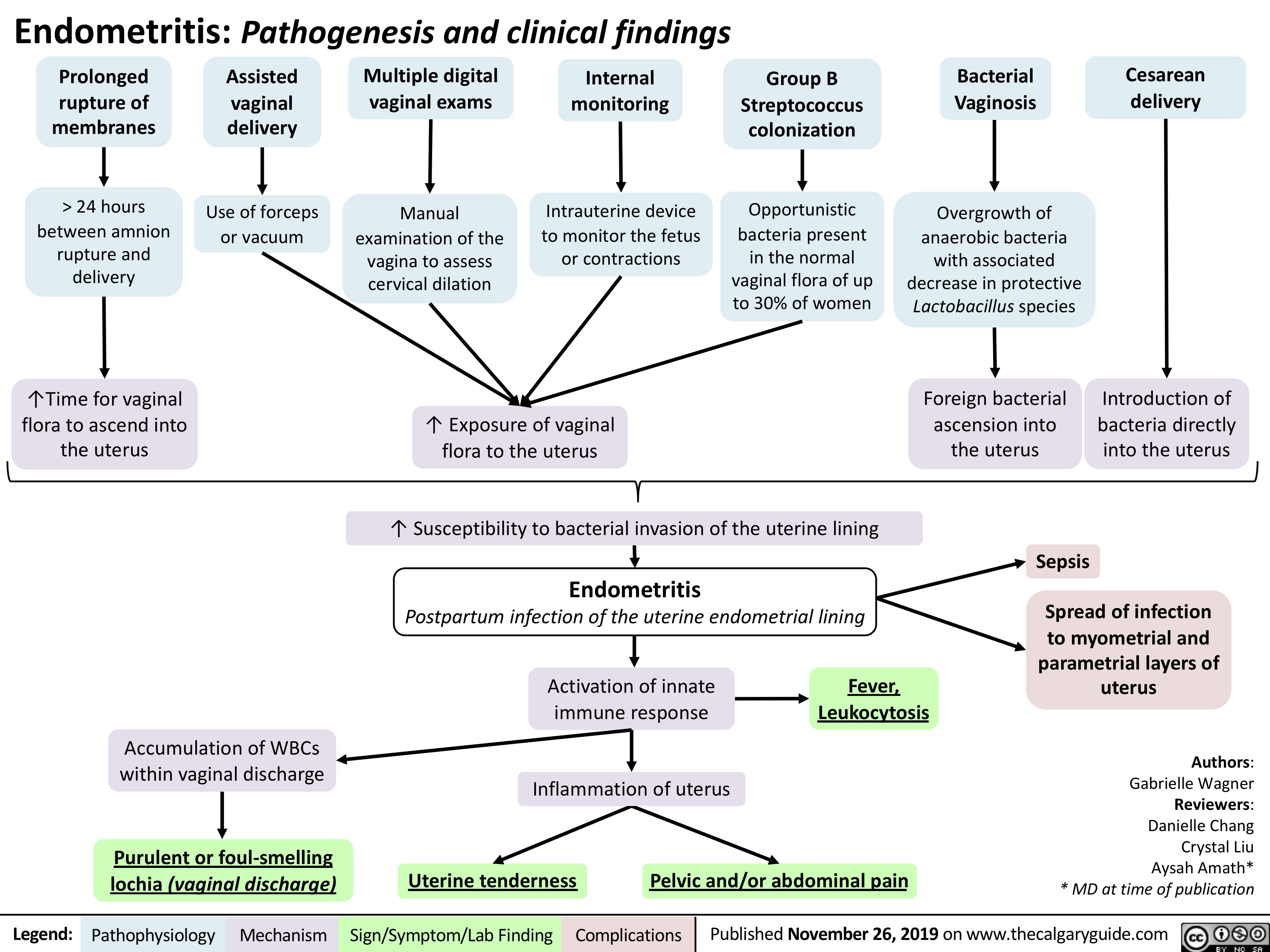
Hydrocele
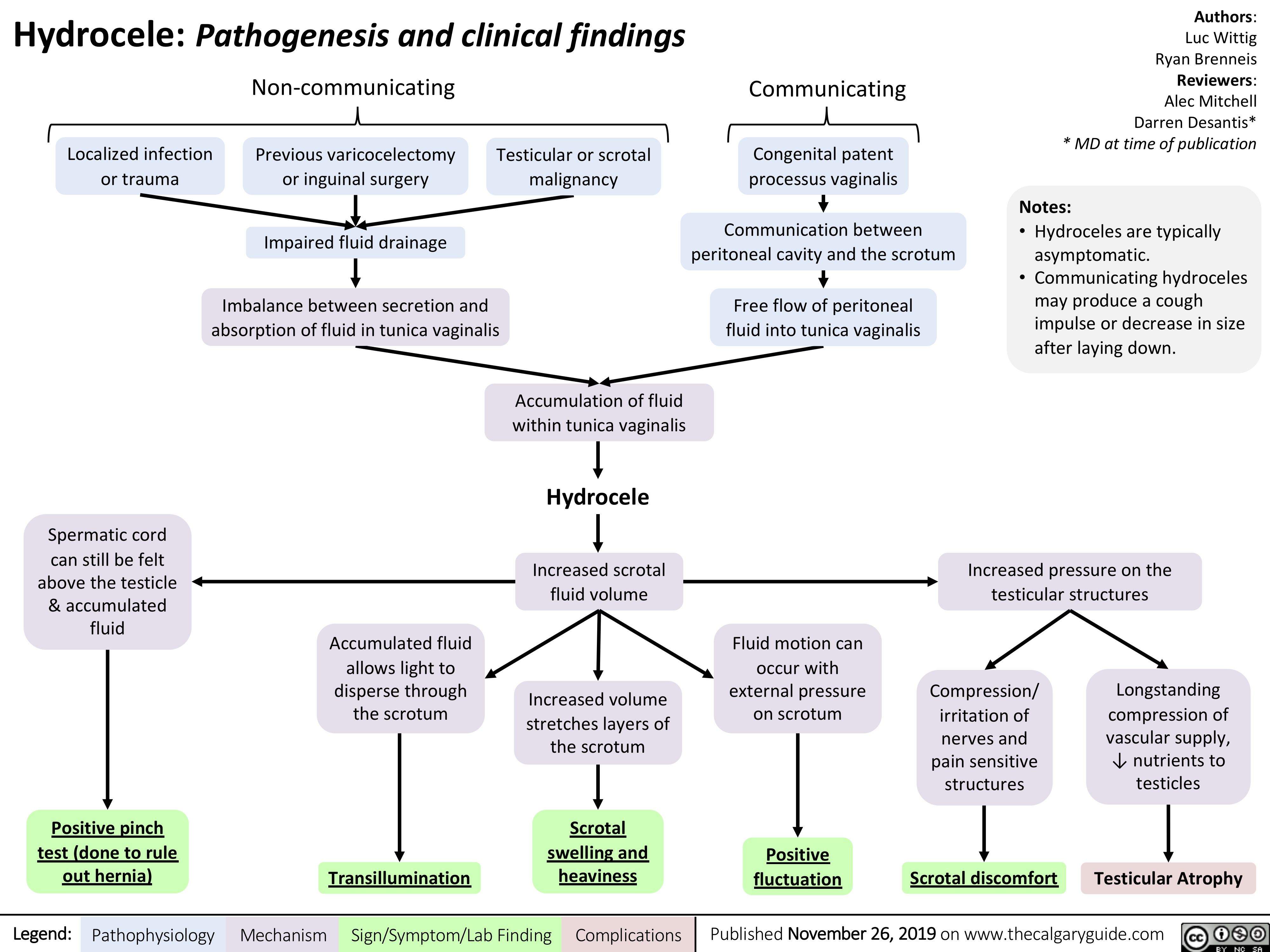
Varicocele
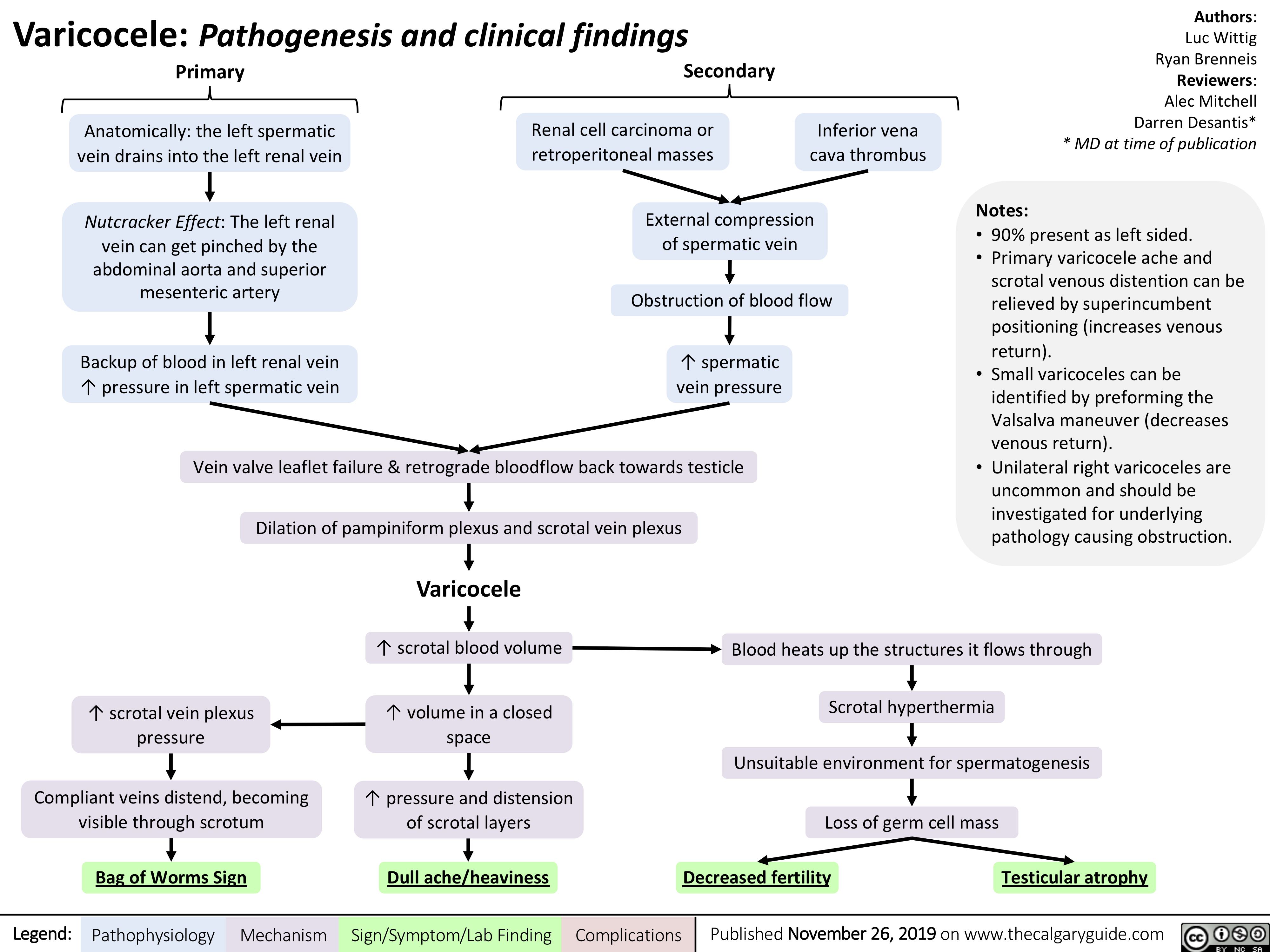
Aphasia
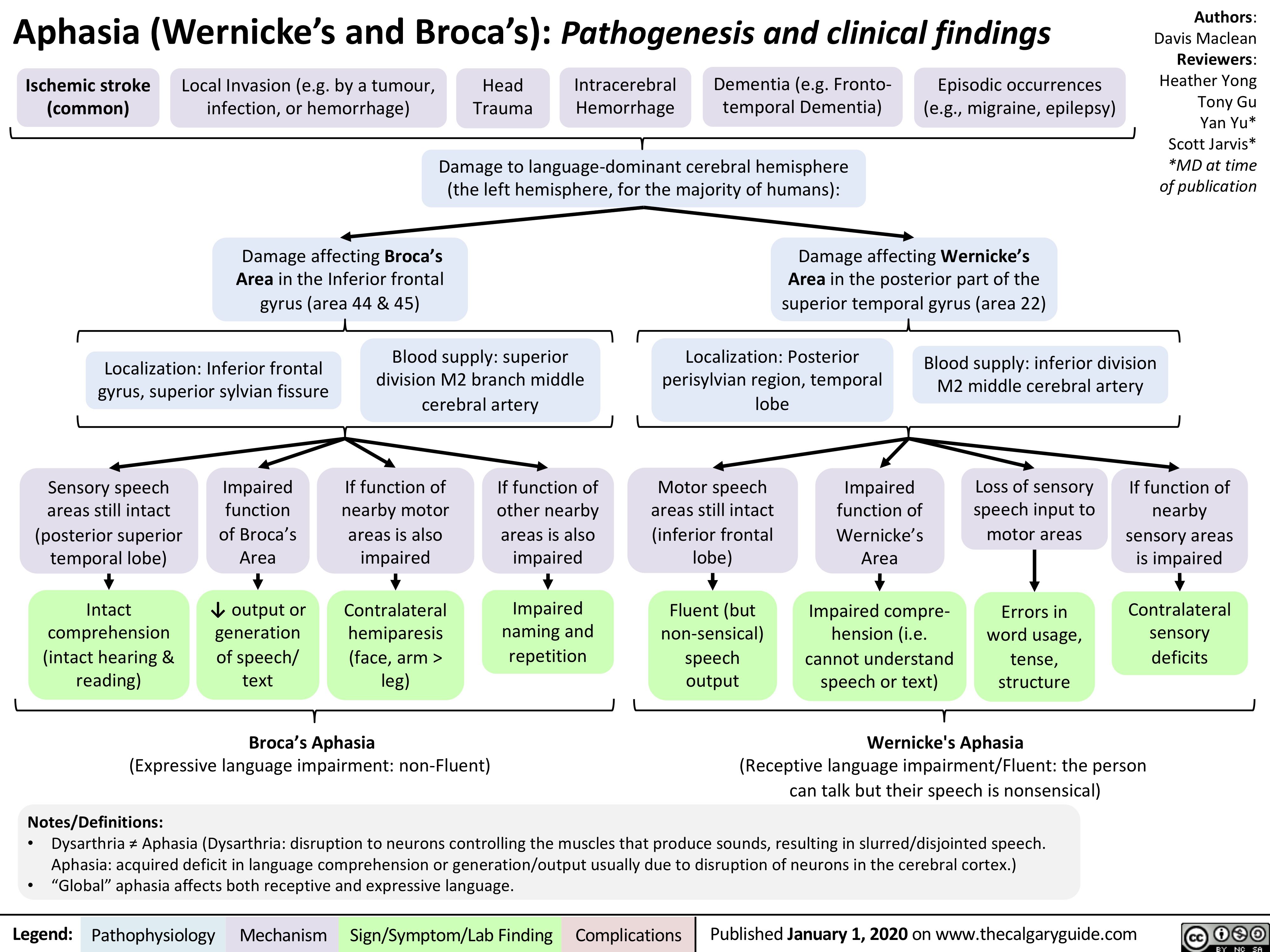
Slide-authoring-process-FINAL-2
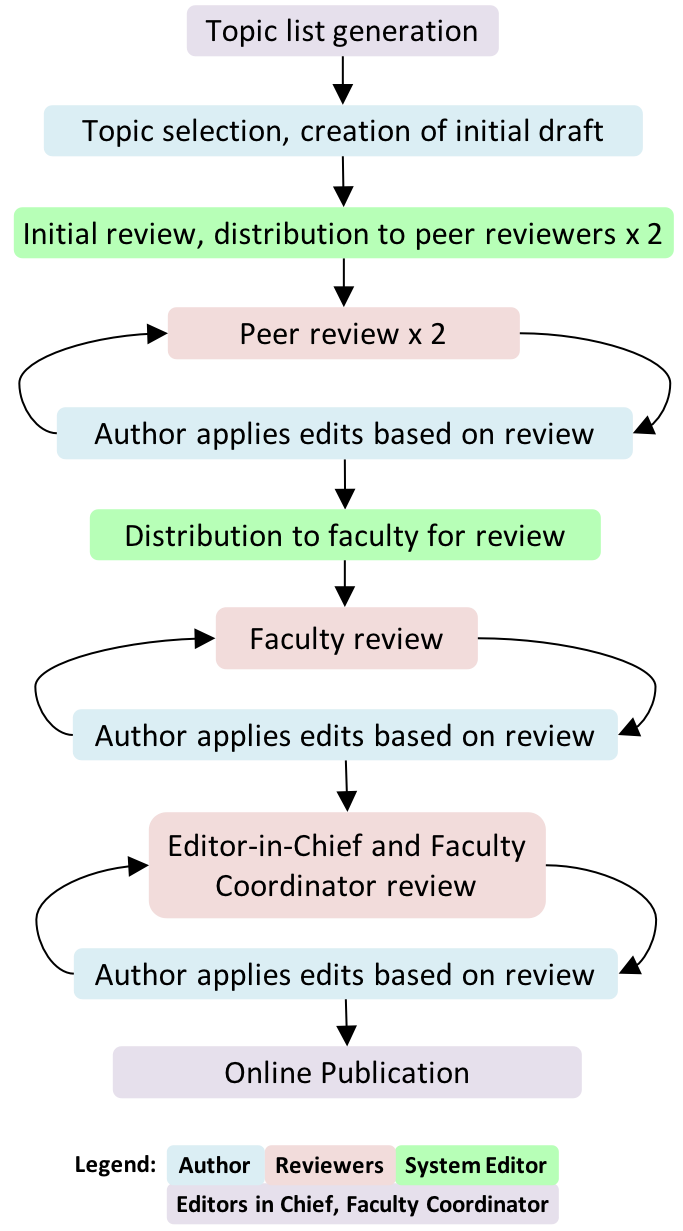
A1AT-Deficiency
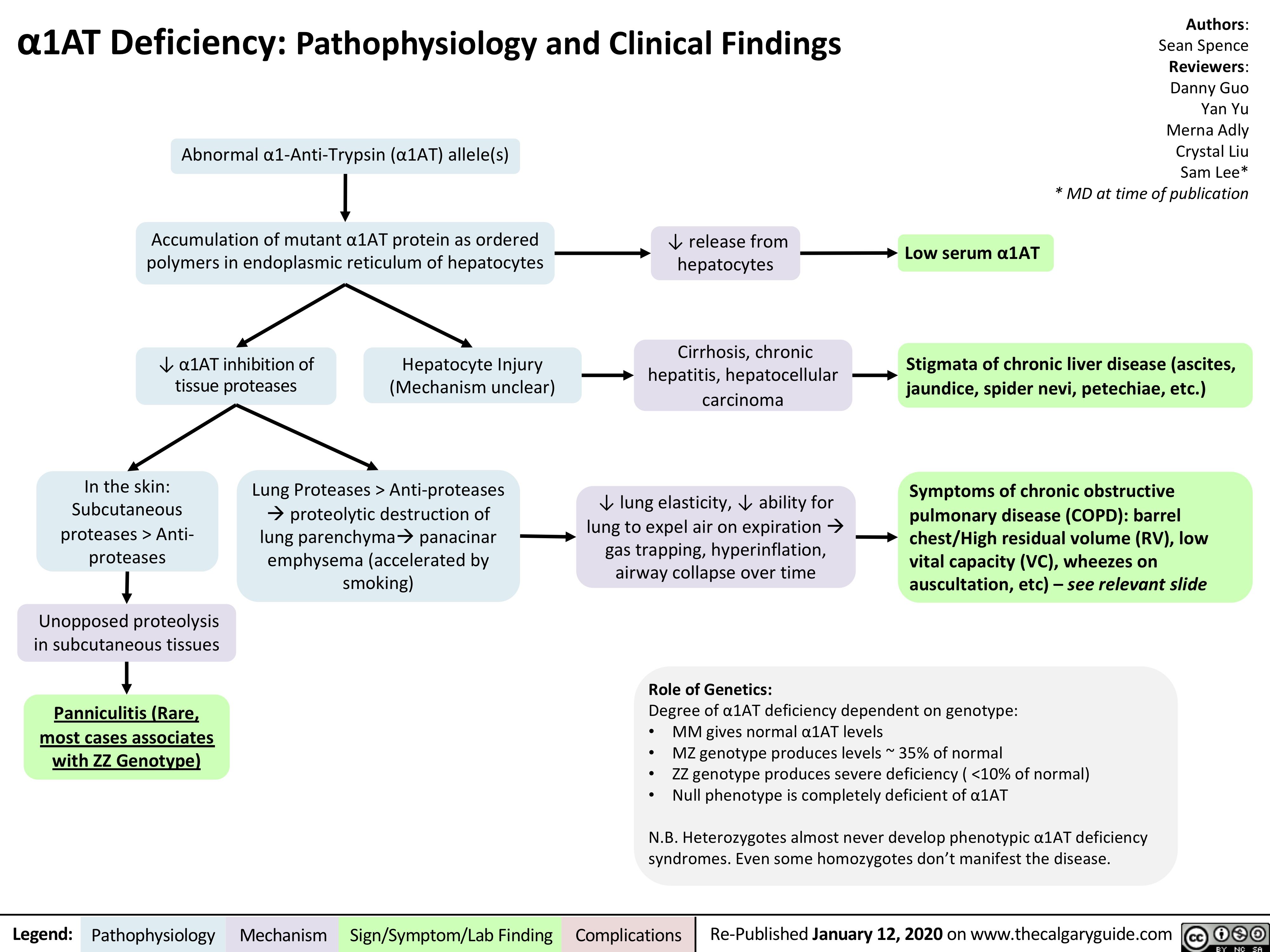
Viral-Hepatitis
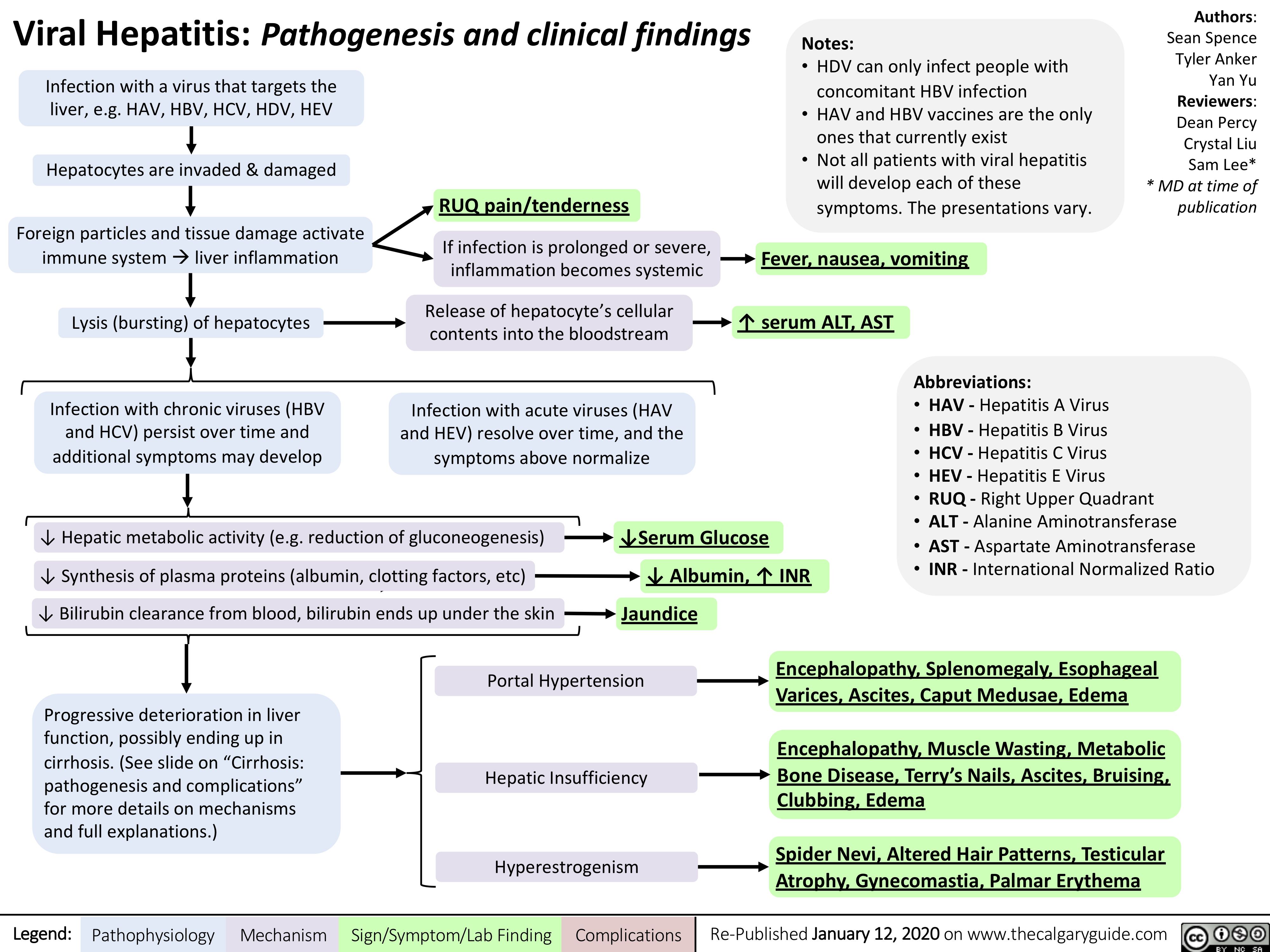
Multiple-Myeloma
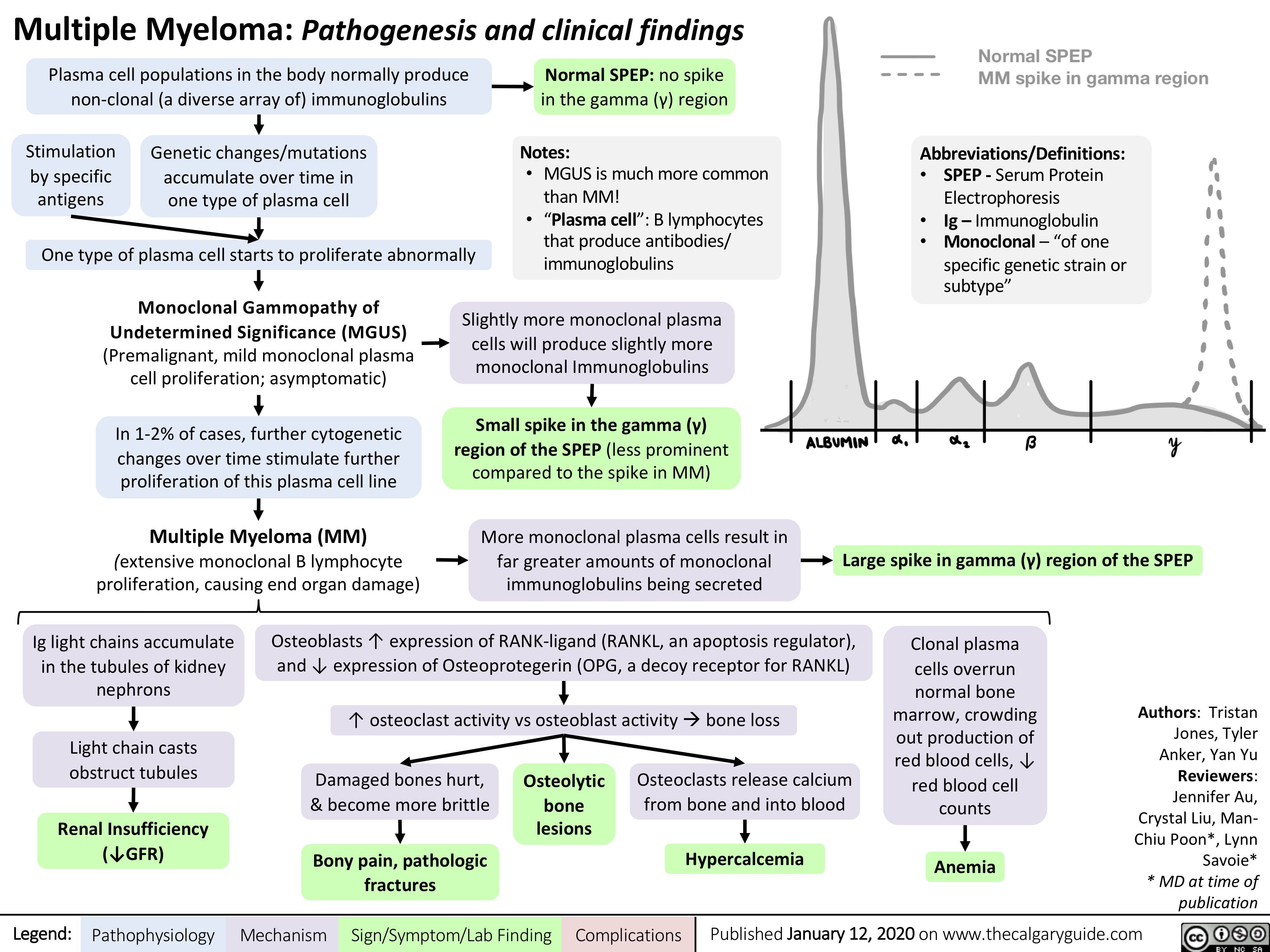
Pathophysiology-Behind-the-Leukemias
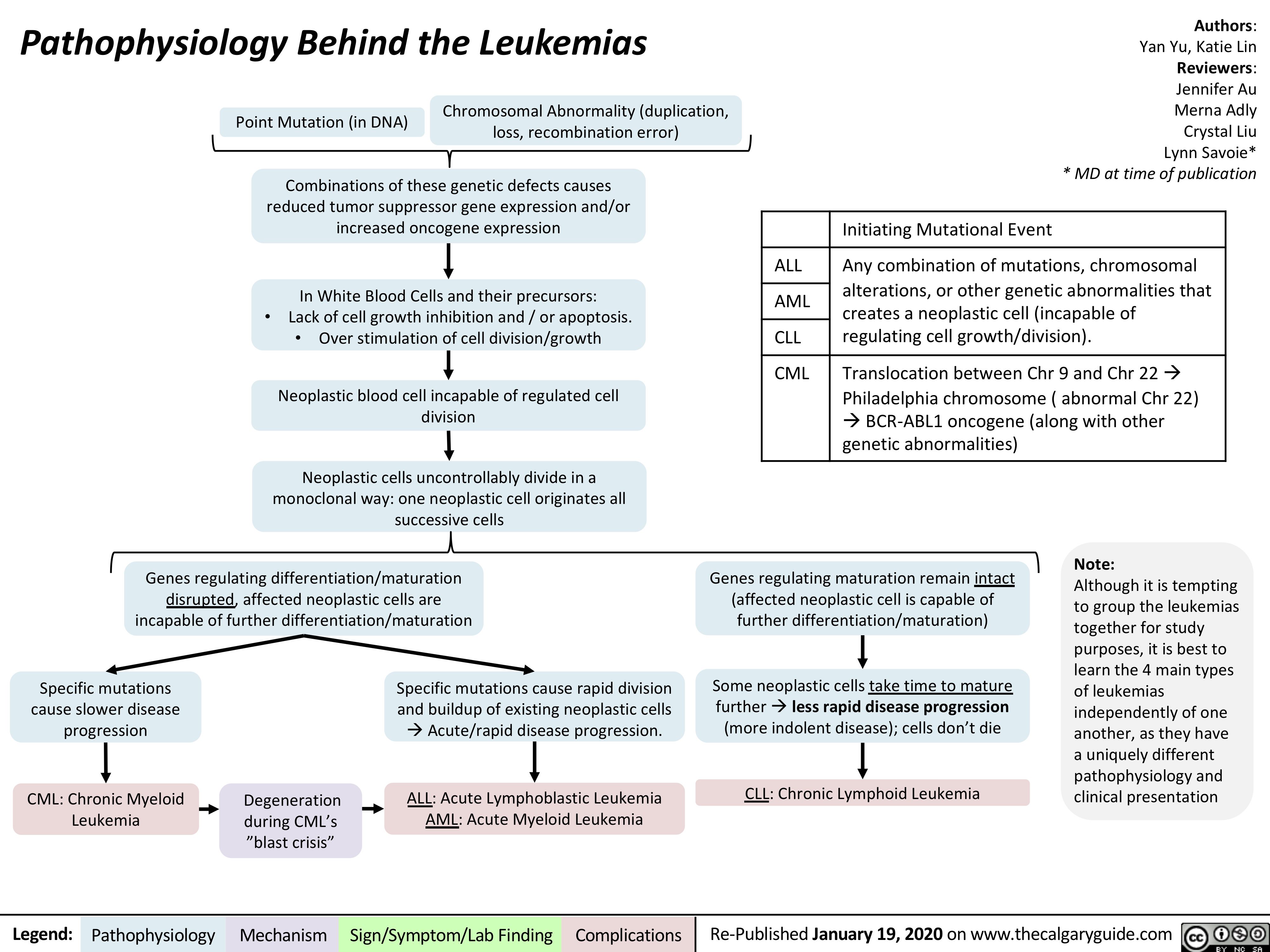
Aqueous-Humor-Production-and-Drainage
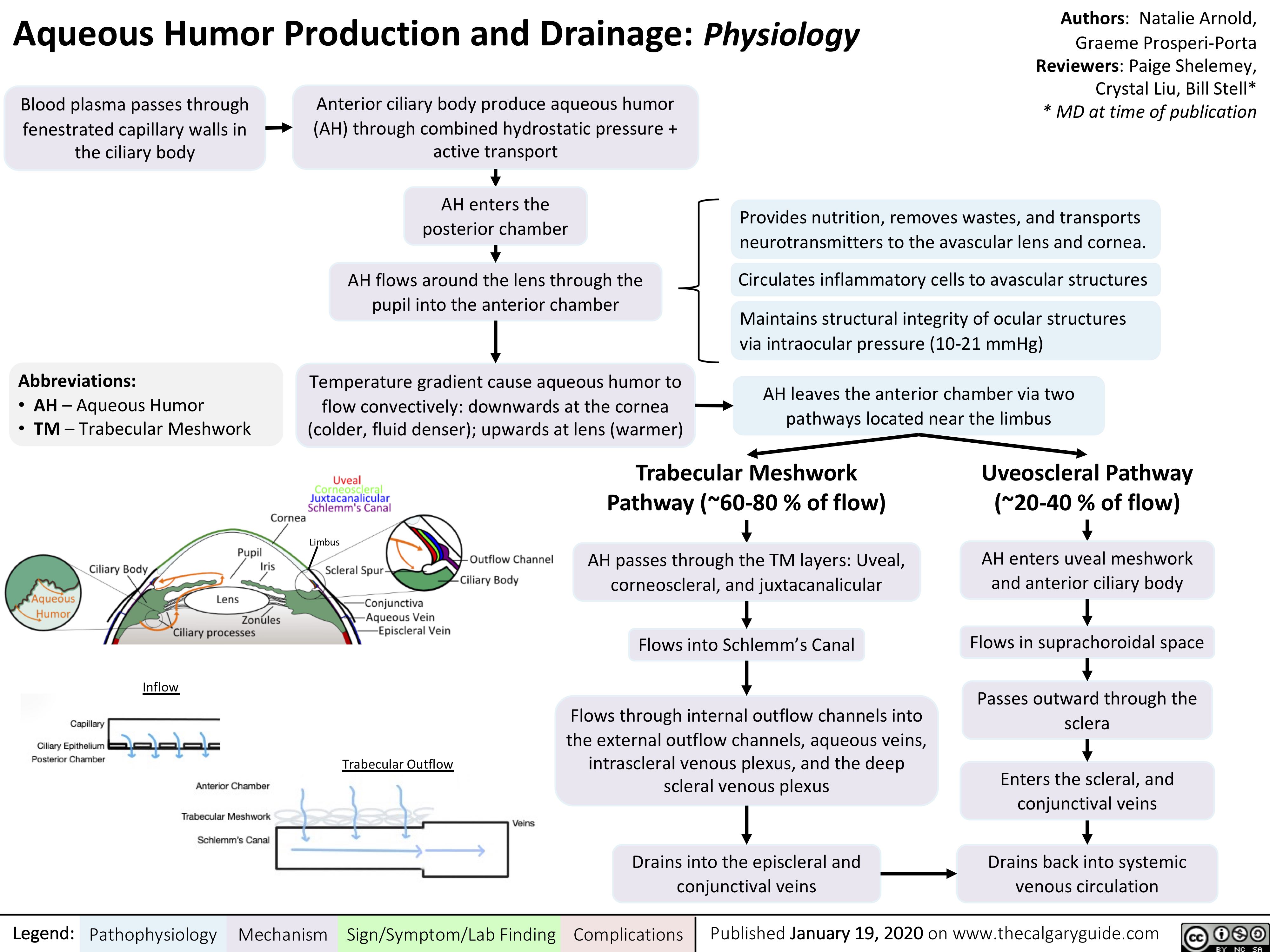
Innate-Immune-Response
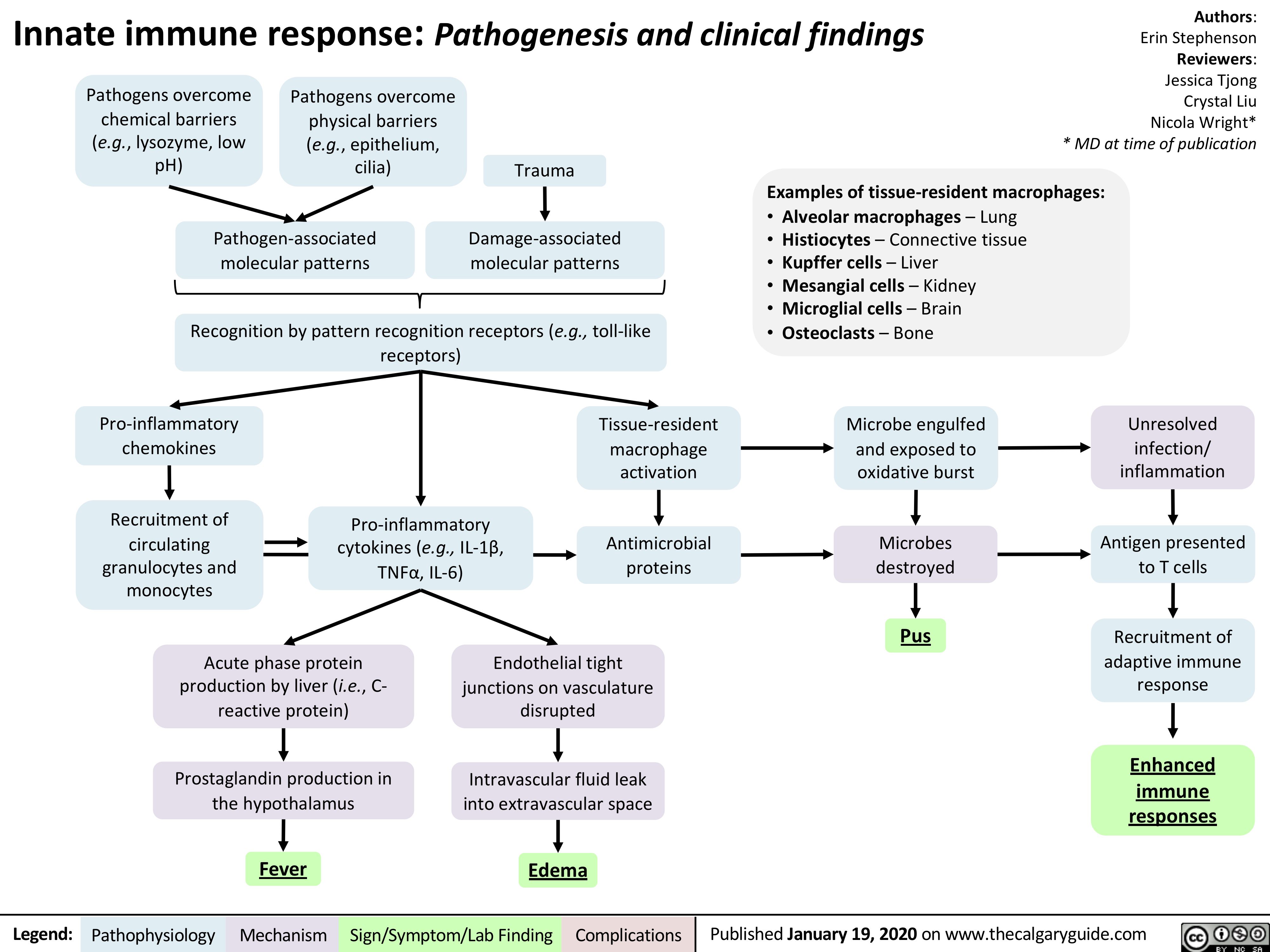
vomiting-pathogenesis
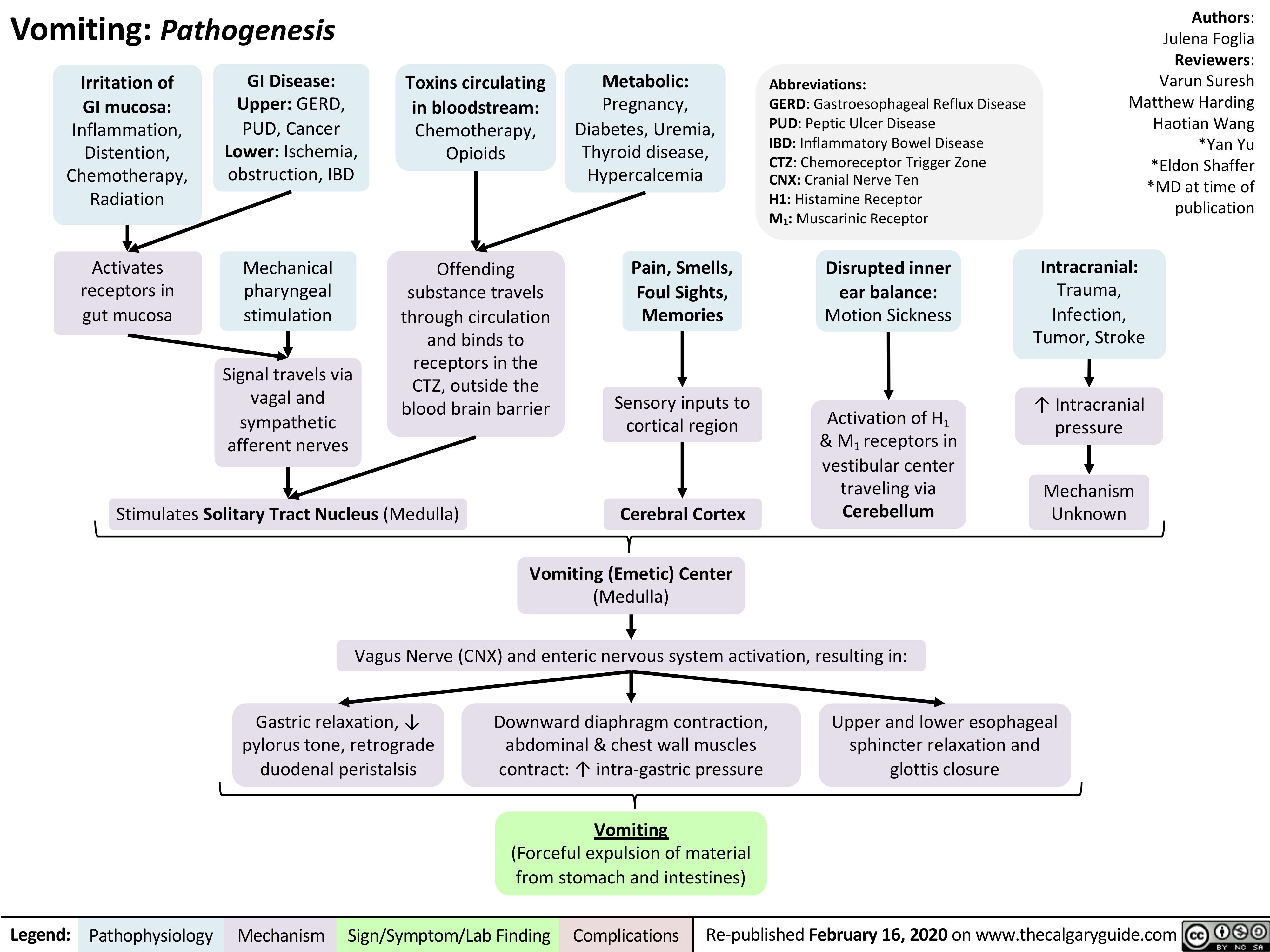
Pseudogout
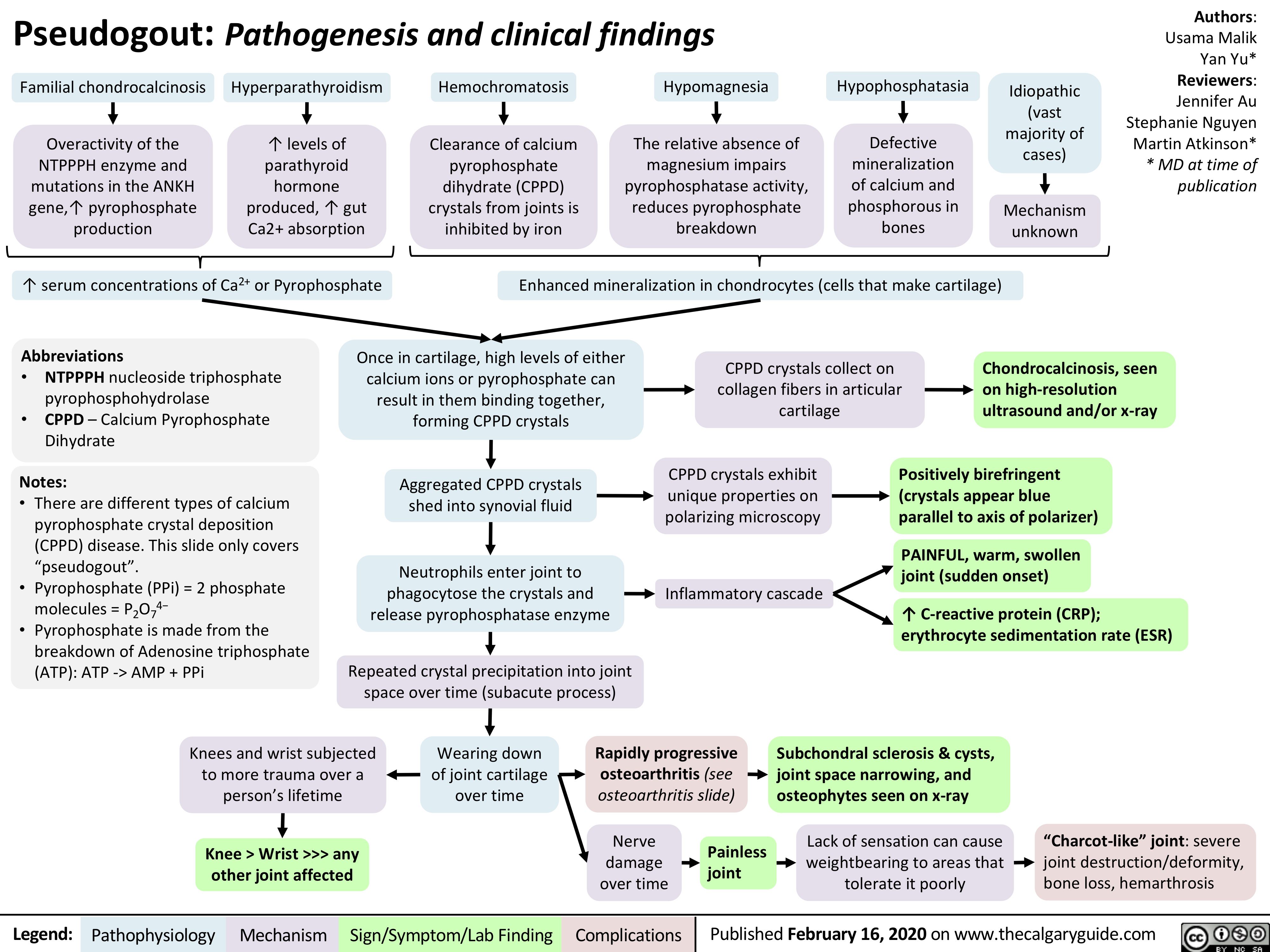
C5-C9-deficiency
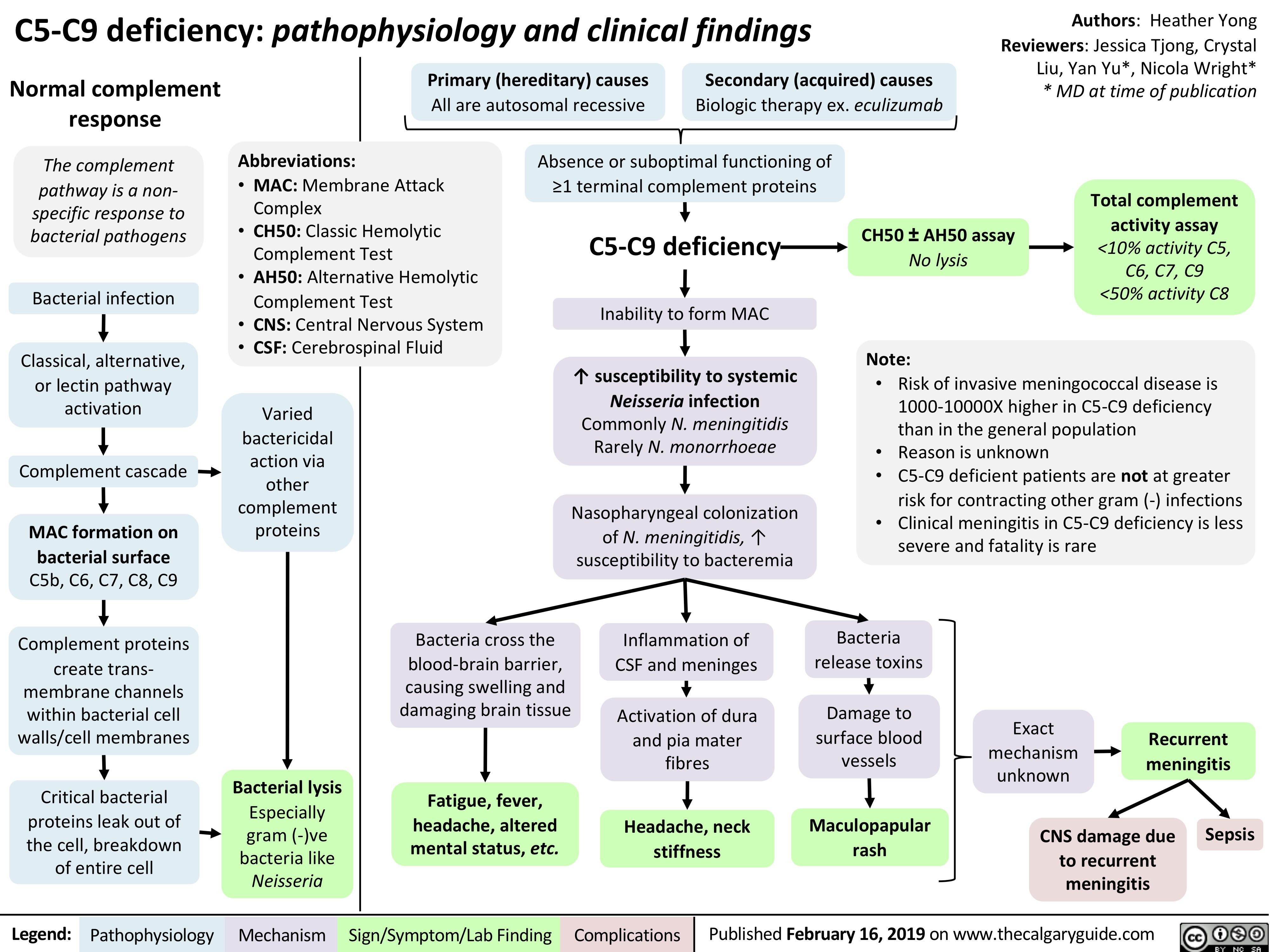
tinea-capitis-tinea-corpora-and-tinea-pedis
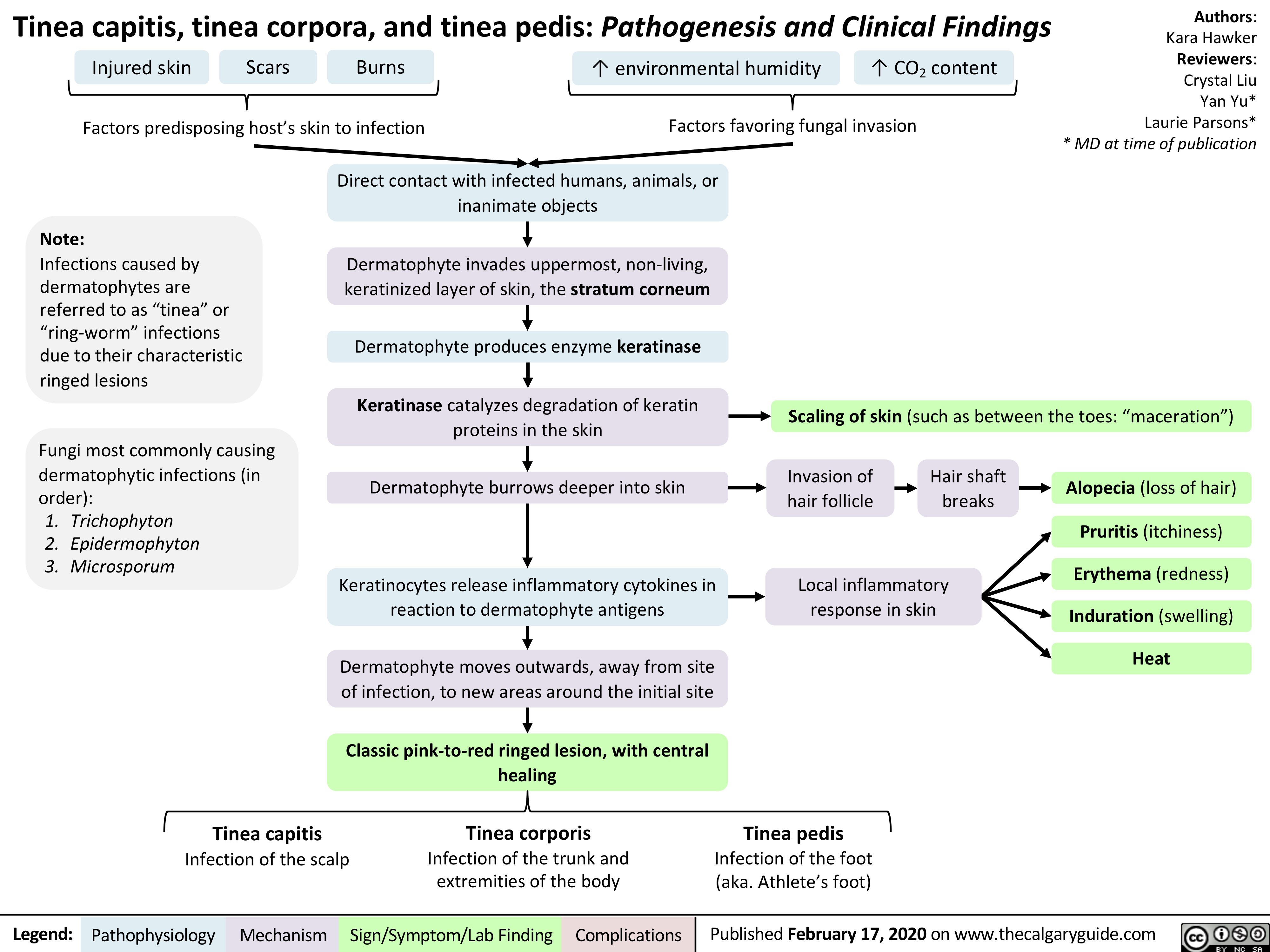
Brain-Neoplasms
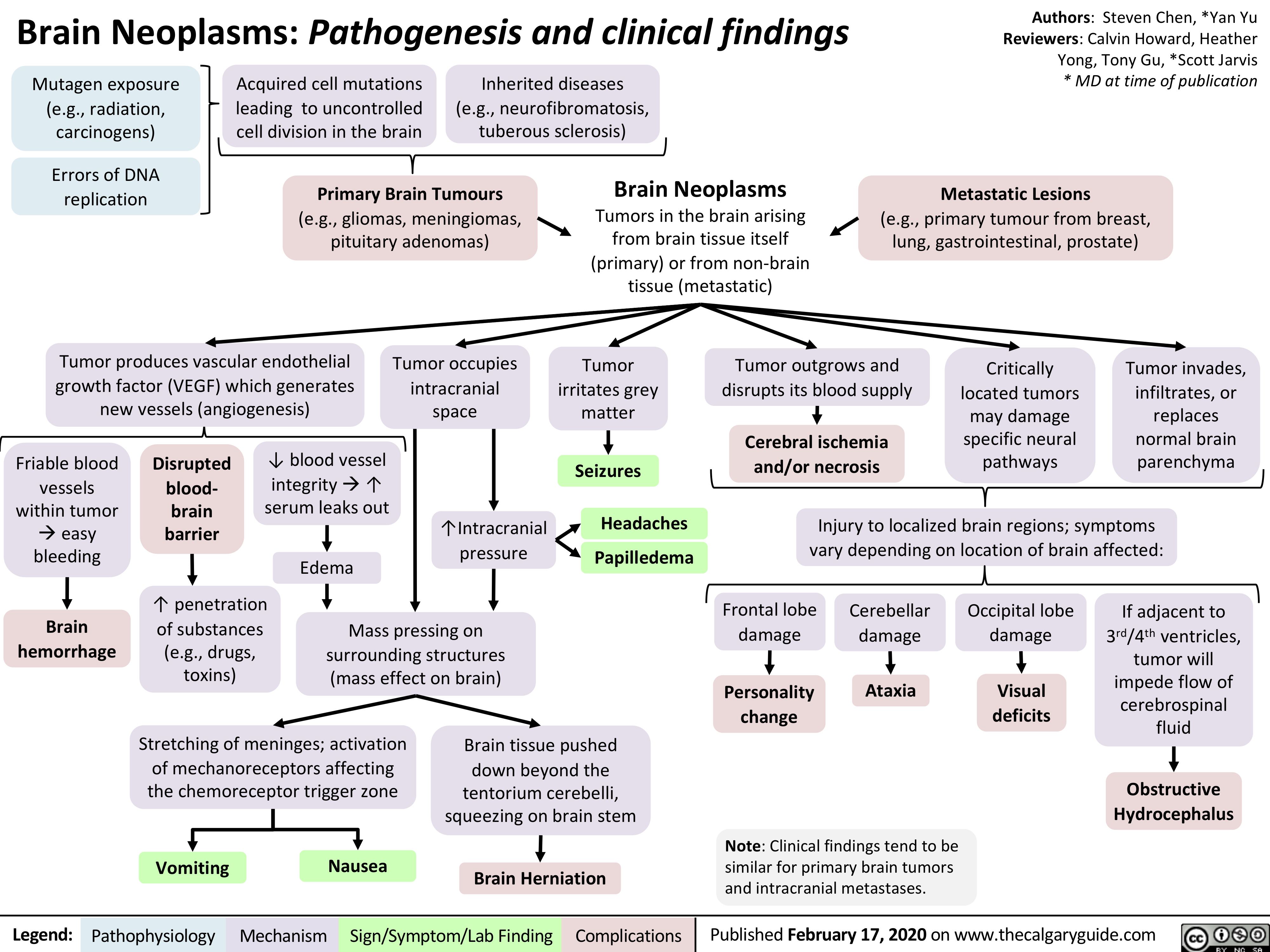
Umbilical-Cord-Prolapse
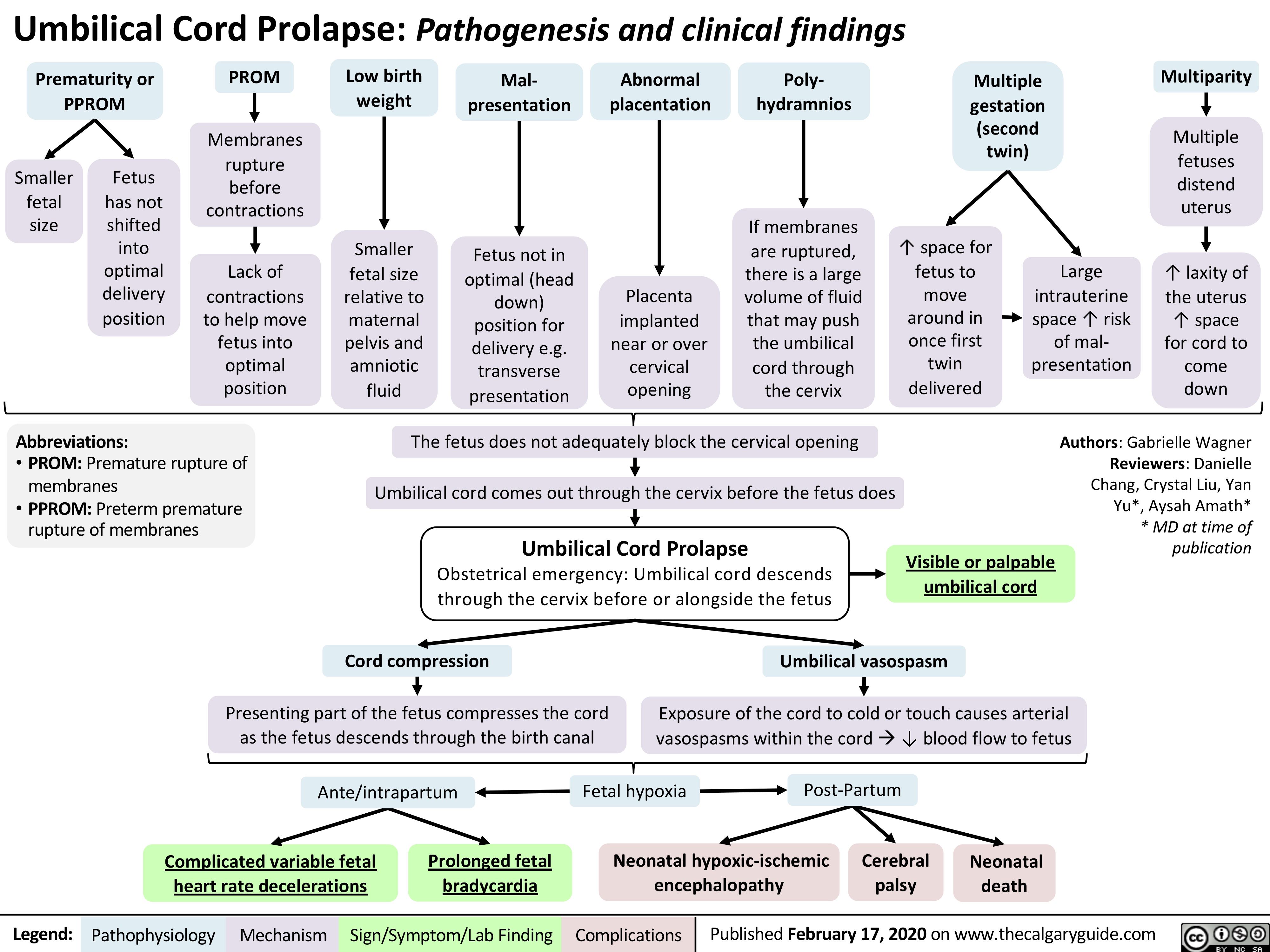
mechanisms-of-opioid-analgesia-in-the-peripheral-nervous-system
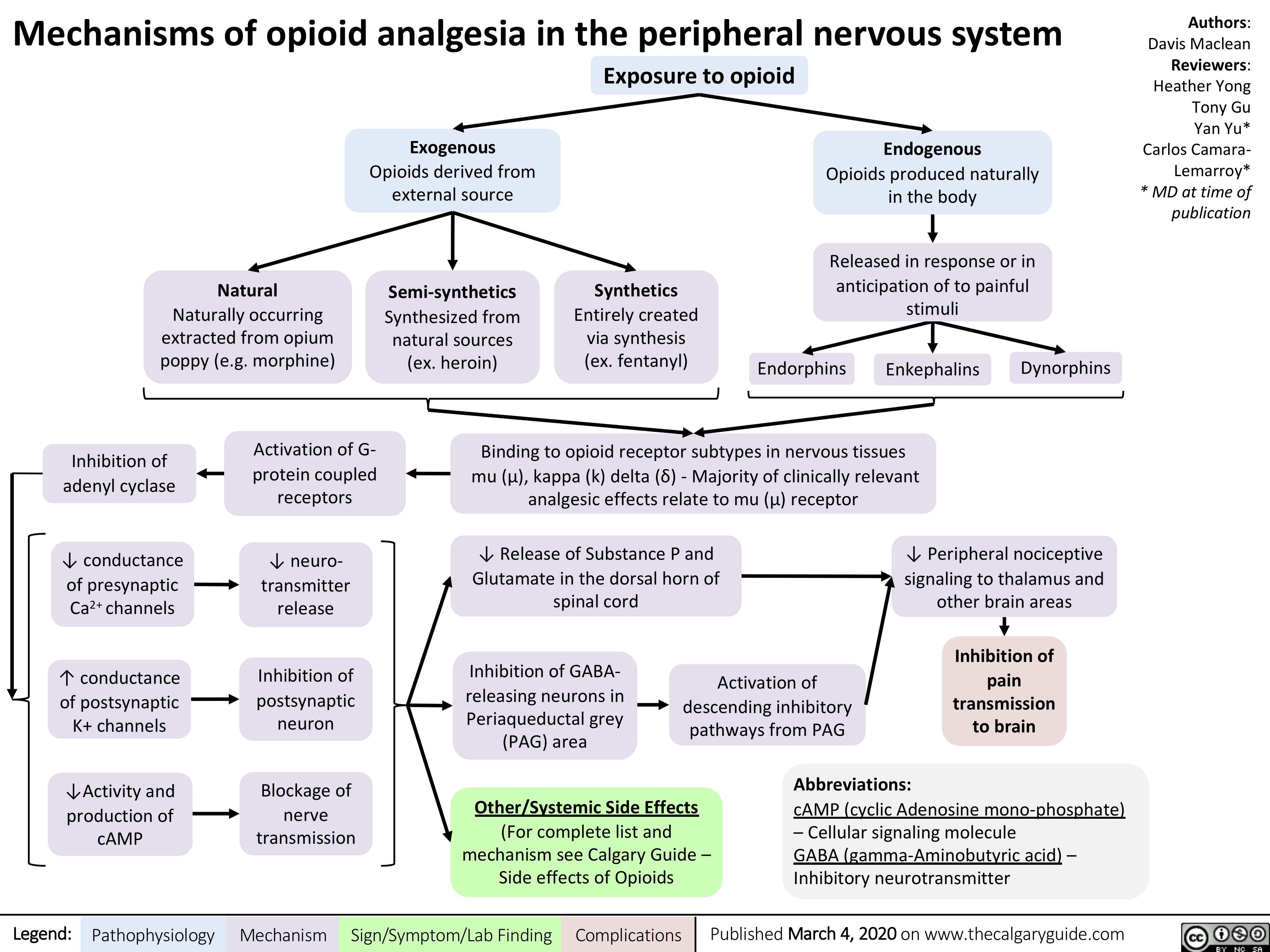
pharmaceuticals-under-investigation-by-who-for-treating-covid-19-proposed-mechanisms
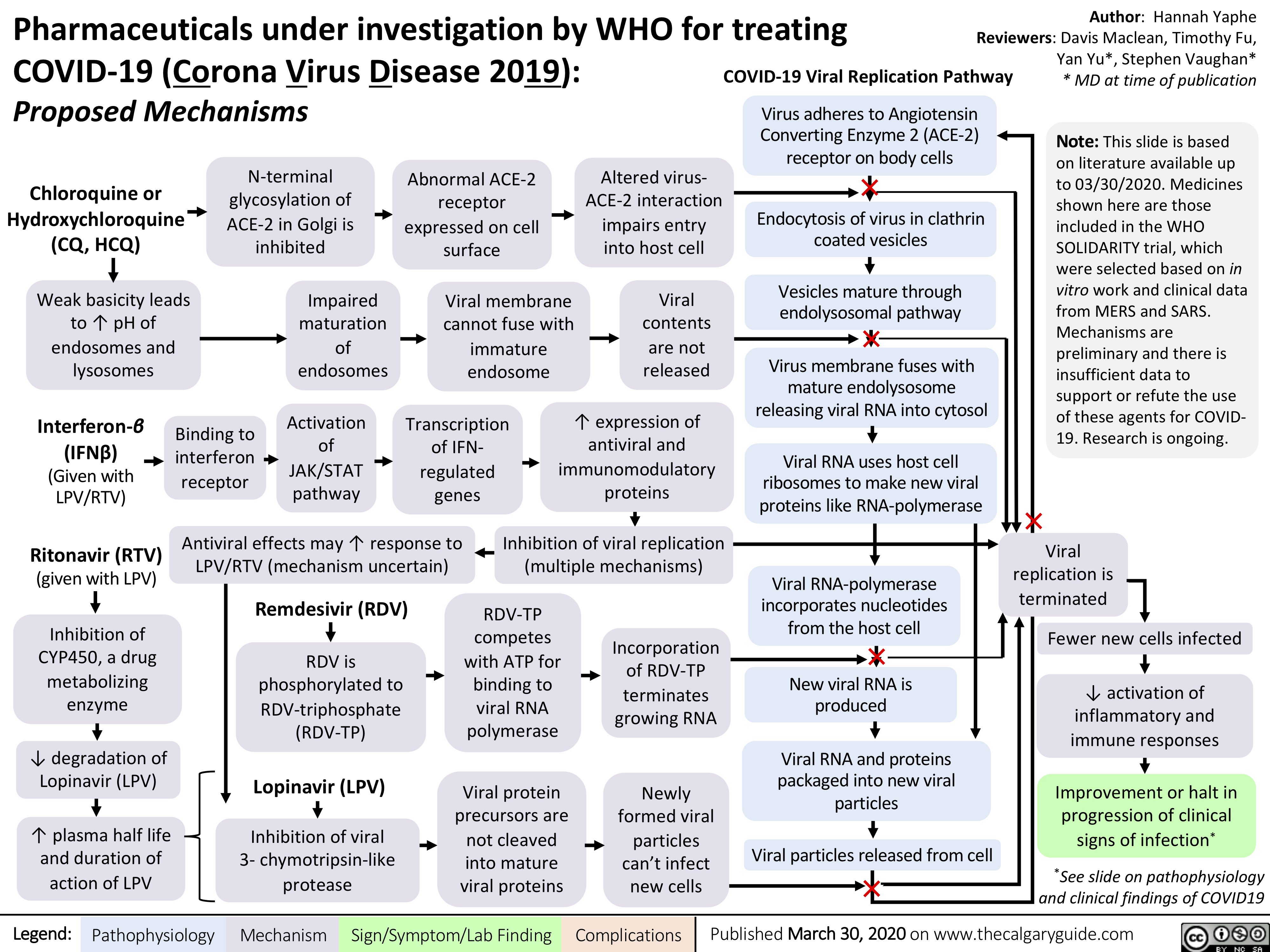
GI-changes-during-pregnancy
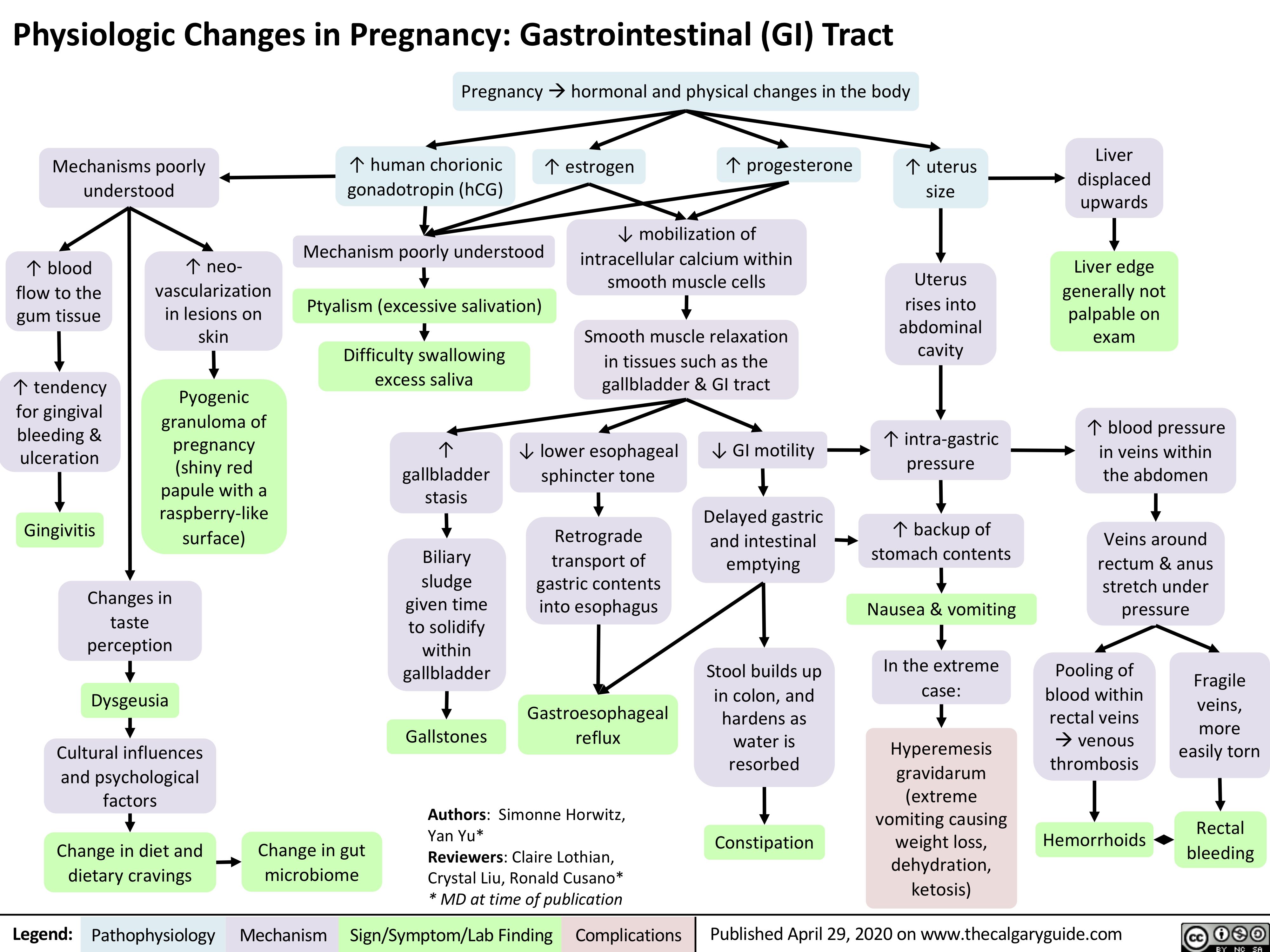
Fecal-Incontinence
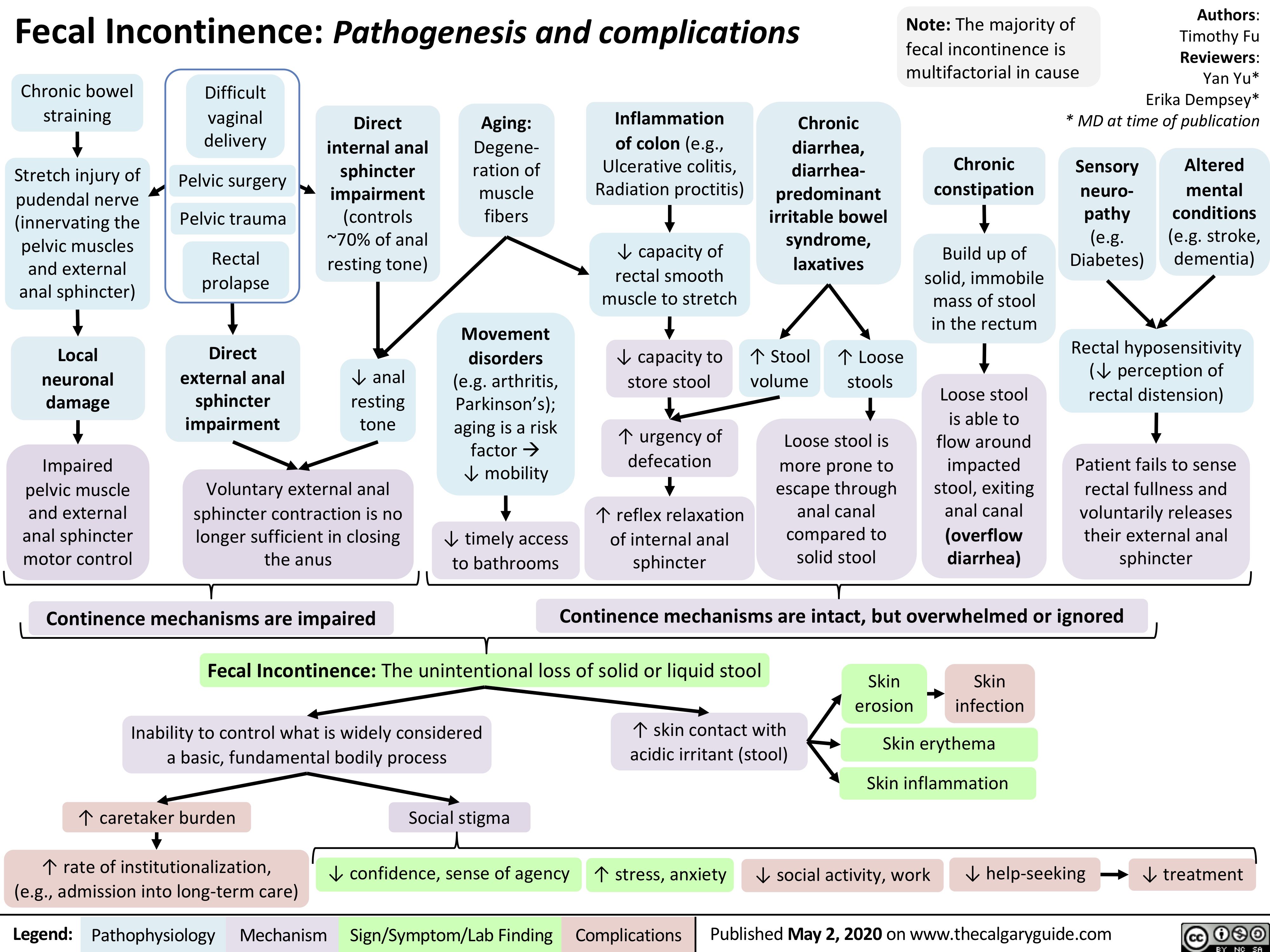
Placenta-Previa
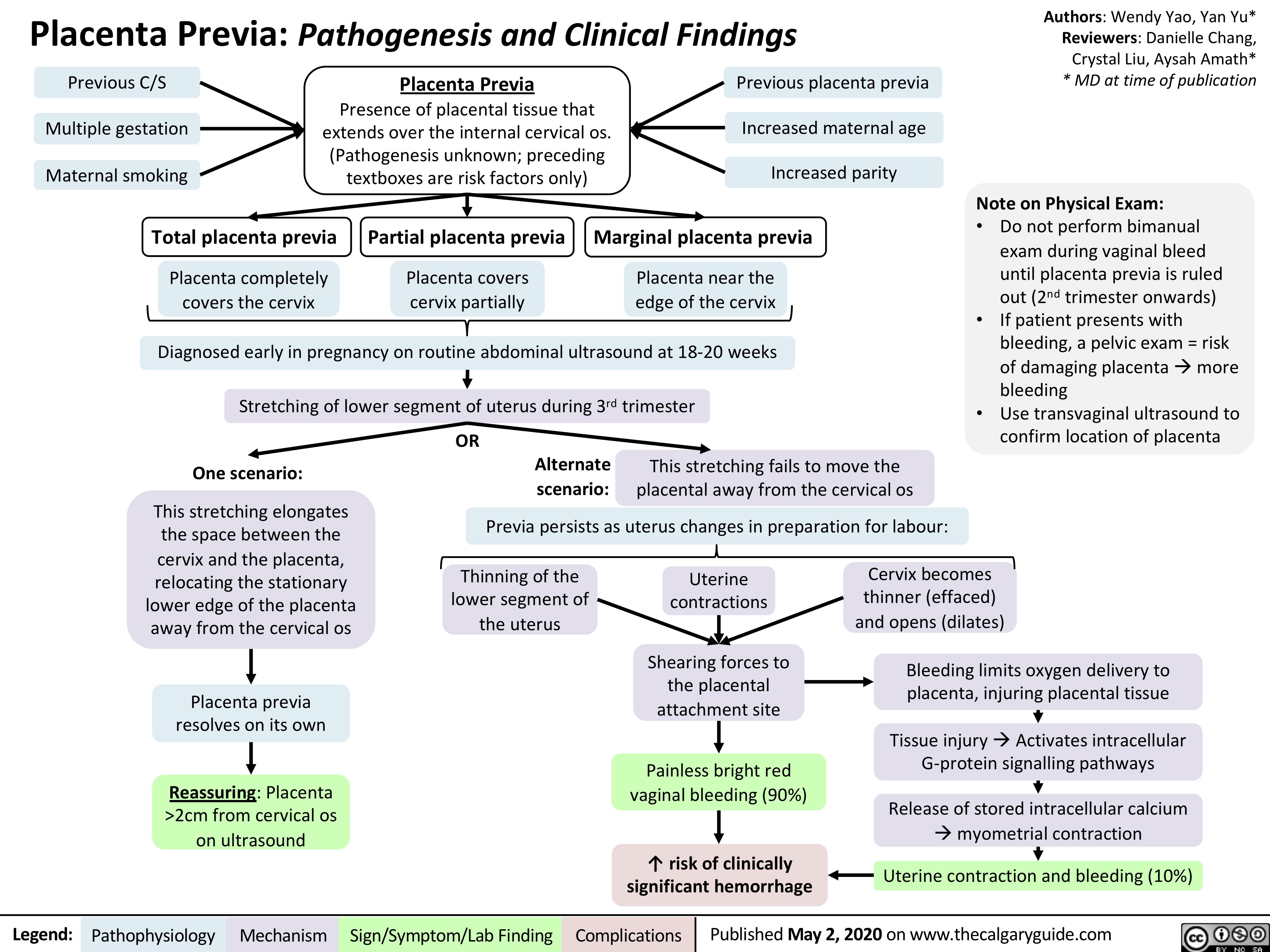
Humoral-Immunity
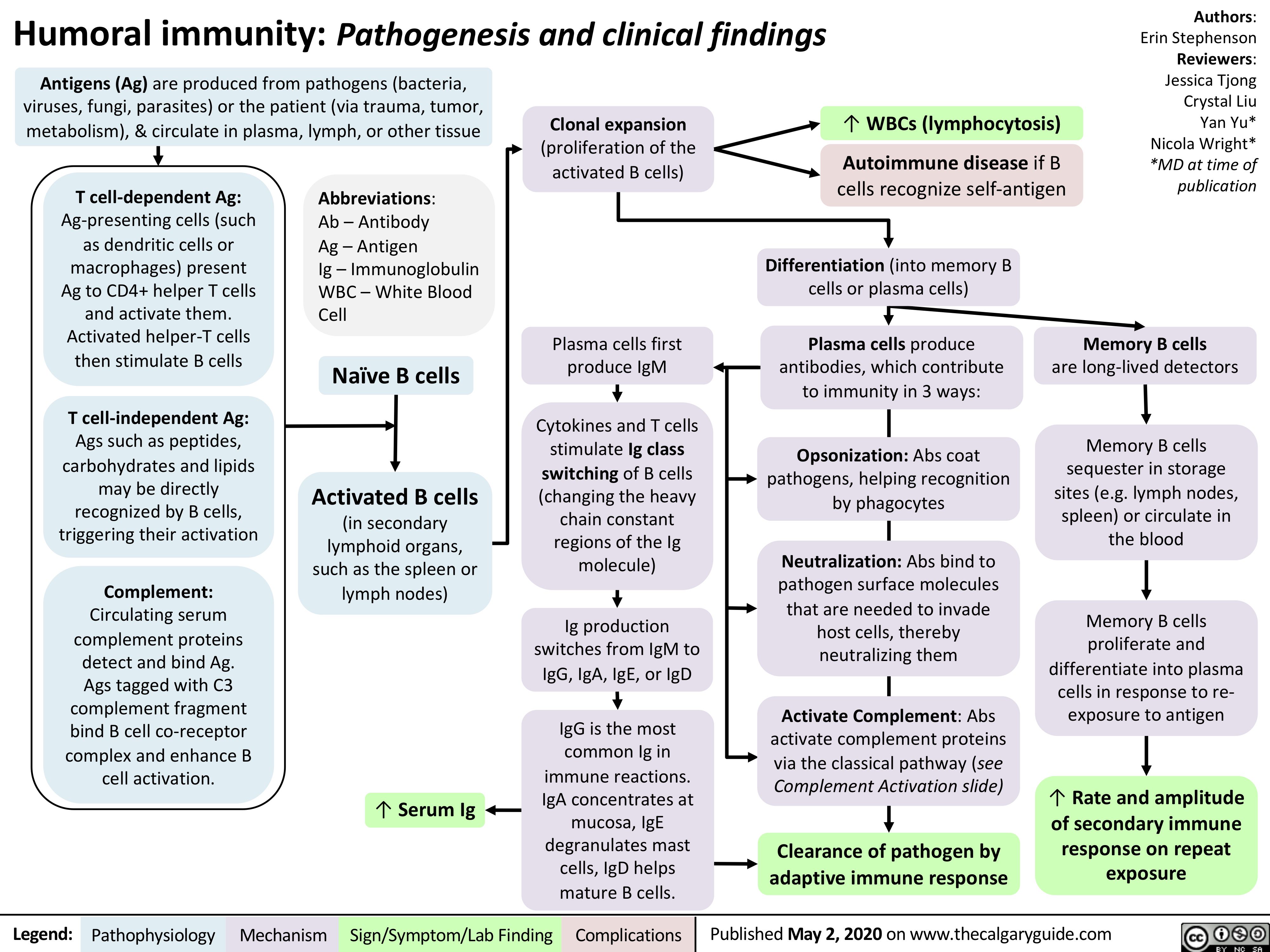
Diabetic-Nephropathy
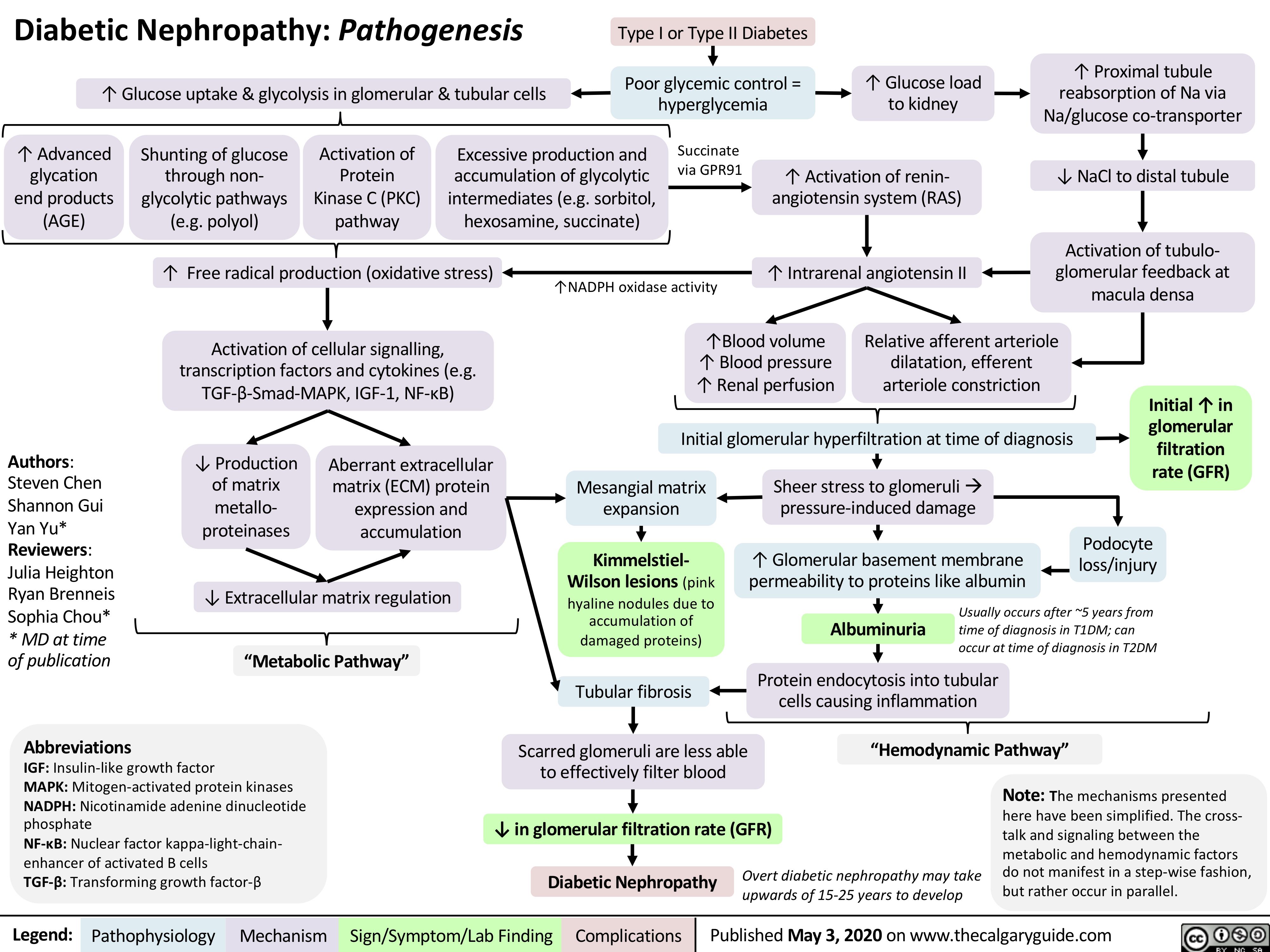
Infarctus du myocarde: Antécédents médicaux
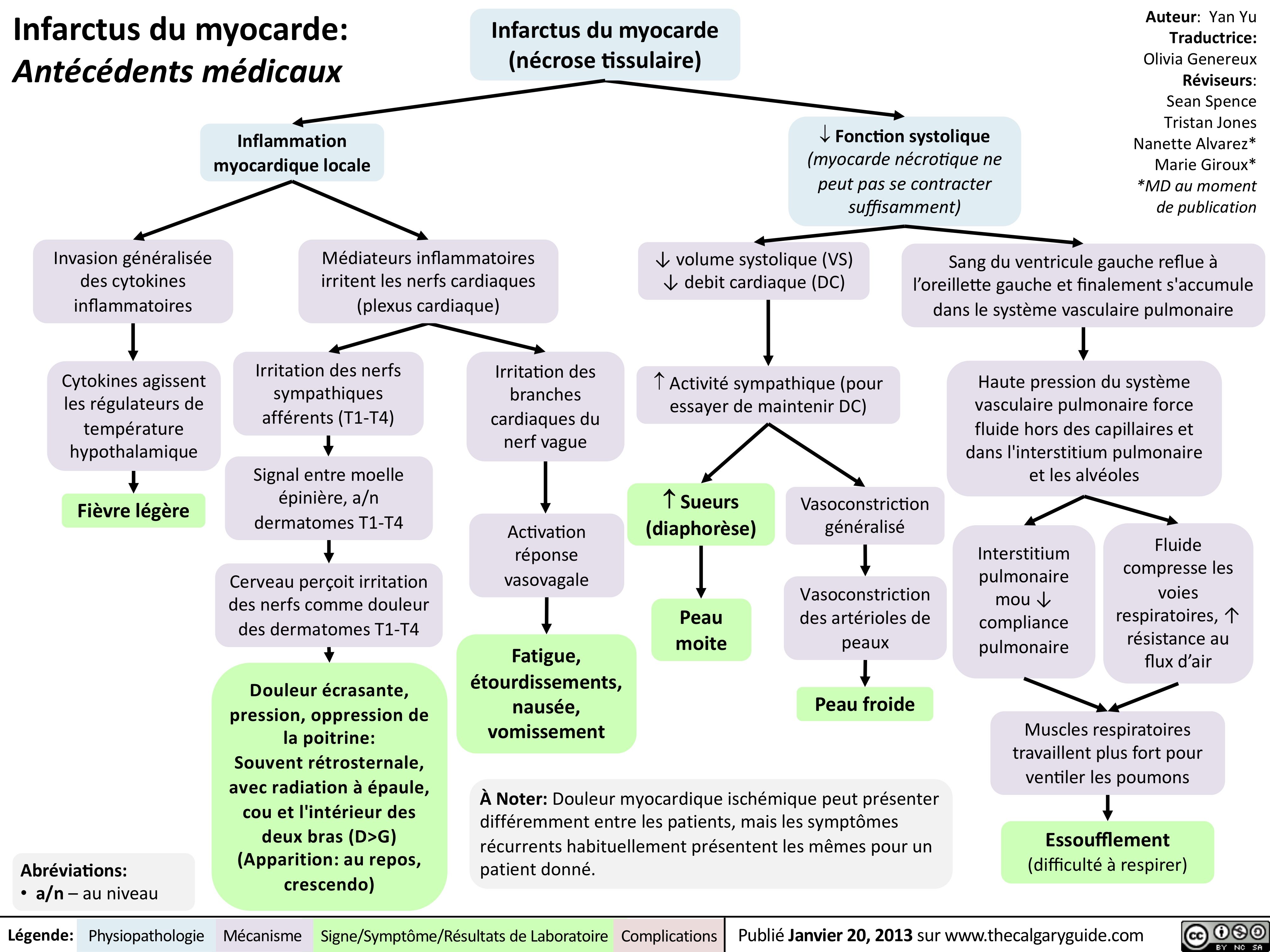
Marfan-Syndrome
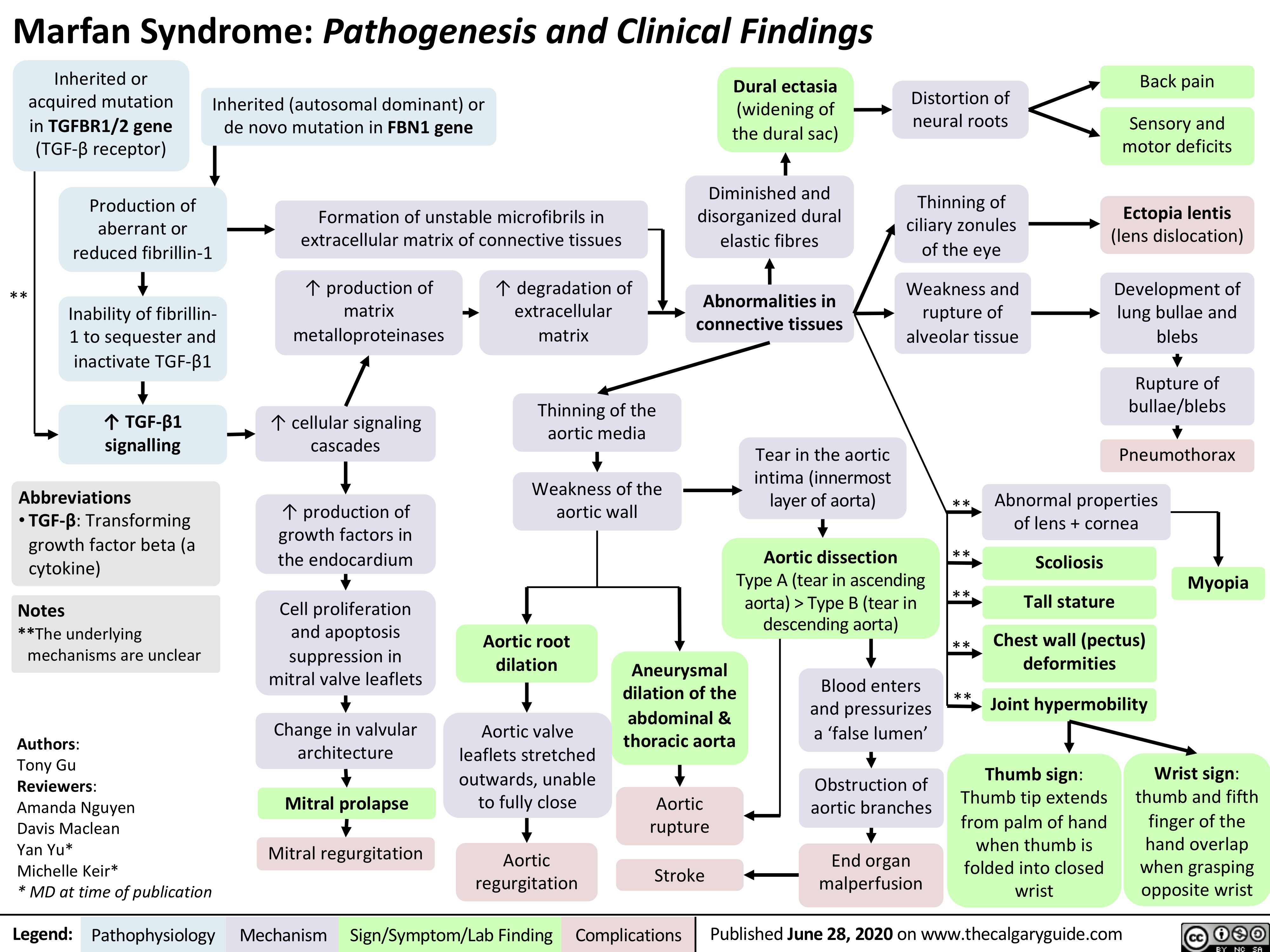
GU-changes-in-pregnancy
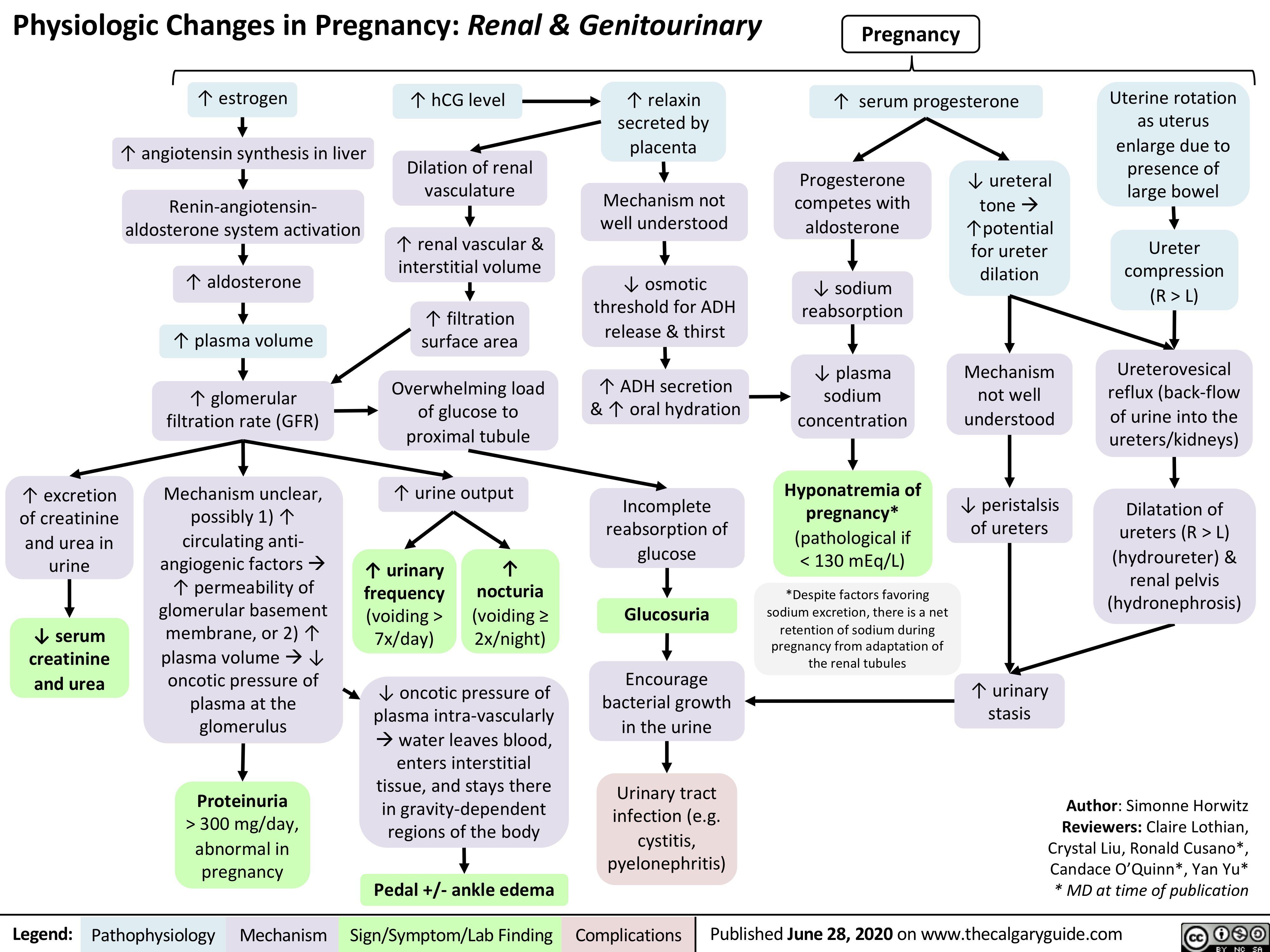
Retinal-Detachment-Pathogenesis