What are splinter hemorrhages
Splinter hemorrhages are small areas of bleeding (hemorrhage) under the fingernails or toenails. Splinter hemorrhages in nails are formed by the hemorrhage of blood from the longitudinally oriented vessels of the nail bed. Splinter hemorrhages look like thin, red to reddish-brown lines of blood under the nails. They run in the direction of nail growth.
They are named splinter hemorrhages because they look like a splinter under the fingernail. The hemorrhages may be caused by tiny clots that damage the small capillaries under the nails.
Splinter hemorrhages occur commonly in psoriasis but may be seen with infection of the heart valves (infective endocarditis), rheumatic heart disease, valvular replacement, SLE (systemic lupus erythematosus), antiphospholipid syndrome, IV drug abusers, and congenital heart diseases 1. Splinter hemorrhages may be caused by vessel damage from swelling of the blood vessels (vasculitis) or tiny clots that damage the small capillaries (microemboli). A simultaneous occurrence in multiple nails is indicative of a systemic cause 2.
Other common systemic causes of splinter hemorrhages include dermatoses (e.g., psoriasis and lichen planus), connective tissue diseases, vasculitis, drugs, particularly kinase inhibitors, infectious diseases, such as acute endocarditis and meningococcemia and renal failure 3 and congenital heart diseases 1. In addition, splinter hemorrhages may be idiopathic, as seen in elderly, or they can be caused by various types of trauma, such as playing percussion instruments, housework, sports, and habits/tics.
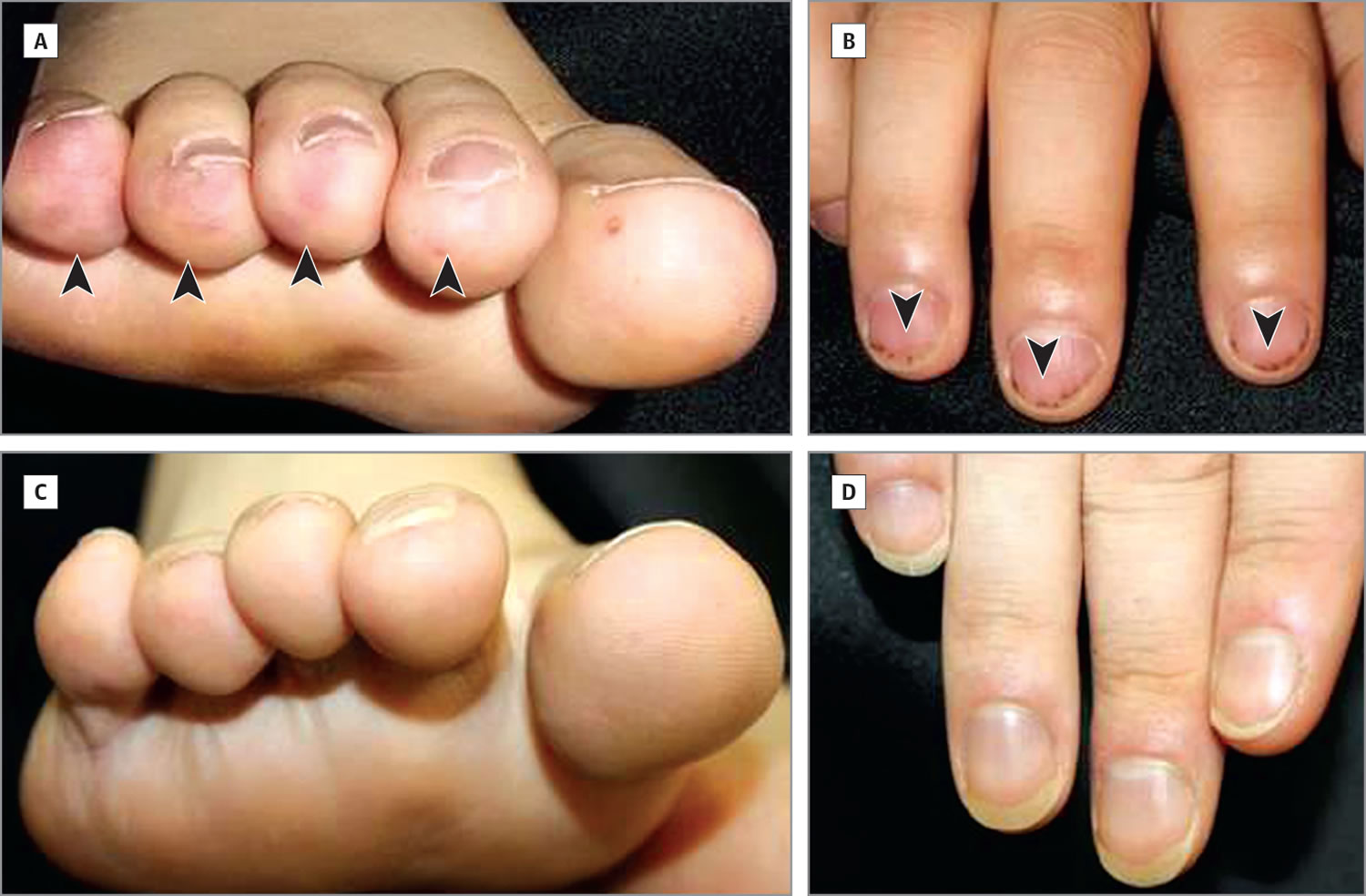
Figure 1. Splinter hemorrhages
Figure 2. Splinter hemorrhage with bacterial endocarditis
Contact your provider if you notice splinter hemorrhages and you haven’t had any recent injury to the nail.
Splinter hemorrhages most often appear late in endocarditis. In most cases, other symptoms will cause you to visit your provider before splinter hemorrhages appear.
Splinter hemorrhages causes
Splinter hemorrhages occur when blood leaks or swells from small blood vessels that run up and down the nail bed. Tiny blood clots known as microemboli in the capillaries can also cause splinter hemorrhages. Splinter hemorrhages can be caused by environmental factors, skin disorders, systemic diseases, and medication use. However, nail trauma (e.g., from sports, housework, personal habits) is the most common cause, accounting for 20 percent of cases 4.
Splinter hemorrhages are more commonly associated with nail psoriasis, but can also occur with eczema, vasculitis, or onychomycosis 4. Dermal vascular dilatation and tortuosity from psoriasis can lead to splinter hemorrhages. Splinter hemorrhages of the psoriatic nail are thought to be similar to the cutaneous Auspitz sign 5.
Systemic disease may be the cause if the splinter hemorrhages appear in several nails, are located in the proximal portion of the nail plate, or are painful 6. Petechiae and splinter hemorrhages are classic lesions of subacute endocarditis, especially when accompanied by fever, Roth spots, Osler nodes, Janeway lesions, or a murmur. Splinter hemorrhages can occur with systemic lupus erythematosus, along with other nail changes such as periungual telangiectasias, hyperkeratotic ragged cuticles, onycholysis, and red lunula 7.
Splinter hemorrhages can be an adverse effect of medications that impair blood vessels in the nail bed, although this is uncommon 8. These reactions are usually dose-related, involve several or all nails, and resolve after the medication is discontinued 9. Medications that may lead to this reaction include antithrombotics and anticoagulants, such as aspirin and warfarin (Coumadin) 10; cancer chemotherapeutic agents, such as taxanes 11; tetracycline; and ganciclovir (Cytovene) 12.
Splinter hemorrhages symptoms
Splinter hemorrhages cause small blood vessels to rupture along the natural lines that run up and down the nails. The underlying blood will attach to the nail plate and seems to move up as the nail grows.
However, in people with systemic diseases, splinter hemorrhages will often reappear, sometimes in different locations. The hemorrhages are usually 1 to 3 millimeters in length, and the streaks are typically red or reddish-brown.
Men experience splinter hemorrhages more often than women. People with a darker complexion may also have a greater risk of splinter hemorrhages.
In most instances, a splinter hemorrhage is not painful. However, if the hemorrhages are painful, they are more likely to be the result of a systemic disease. Also, hemorrhages close to the nail plate and on several fingers can indicate an underlying systemic disease.
Splinter hemorrhages diagnosis
Your doctor will examine you to look for the cause of splinter hemorrhages. You may be asked questions such as:
- When did you first notice this?
- Have you had an injury to the nails recently?
- Do you have endocarditis, or has your provider suspected that you have endocarditis?
- What other symptoms do you have, such as shortness of breath, fever, general ill feeling, or muscle aches?
The physical exam may include special attention to the heart and blood circulation systems.
Laboratory studies may include:
- Blood cultures
- Complete blood count (CBC)
- Erythrocyte sedimentation rate (ESR)
In addition, your doctor may order:
- Chest x-ray
- ECG
- Echocardiogram
After seeing your doctor, you may want to add a diagnosis of splinter hemorrhages to your personal medical record.
Splinter hemorrhages treatment
There is no specific care for splinter hemorrhages. Follow your health care provider’s instructions for treating endocarditis.
When splinter hemorrhages result from trauma, they do not usually need treatment. As the nails continue to grow, the splinter hemorrhages should disappear over time. This process usually takes 3 to 4 months.
A person can take steps to make their nails stronger, which may help prevent splinter hemorrhages, resulting from trauma or injury. Drinking plenty of water and eating a diet that is high in vitamin B and zinc can support the growth of stronger fingernails.
However, splinter hemorrhages that are a symptom of an underlying condition could indicate the need for treatment. If a person’s splinter hemorrhages are related to taking certain medications, they should consult their doctor about whether or not to stop taking the medication.
References- Singal A, Arora R. Nail as a window of systemic diseases. Indian Dermatol Online J. 2015;6(2):67-74. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
- Lawry M, Daniel CR., 3rd . Nails in systemic disease. In: Scher RK, Daniel CR, editors. Nails: Diagnosis, Therapy, Surgery. 3rd ed. Philadelphia: Elsevier Science Limited; 2005. pp. 147–69.
- Haber R., Khoury R., Kechichian E., Tomb R. Splinter hemorrhages of the nails: a systematic review of clinical features and associated conditions. International Journal of Dermatology. 2016;55(12):1304–1310. doi: 10.1111/ijd.13347
- Saladi RN, et al. Idiopathic splinter hemorrhages. J Am Acad Dermatol. 2004;50(2):289–292
- Mayeaux EJ Jr. Nail disorders. Prim Care. 2000;27(2):333–351.
- Tosti A, et al. The nail in systemic diseases. Dermatol Clin. 2006;24(3):341–347.
- McDonnell JK. Cardiac disease and the skin. Dermatol Clin. 2002;20(3):503–511.
- Asymptomatic Linear Hemorrhages. Am Fam Physician. 2010 Jun 1;81(11):1375-1376. https://www.aafp.org/afp/2010/0601/p1375.html
- Piraccini BM, et al. Drug reactions affecting the nail unit. Dermatol Clin. 2007;25(2):215–221.
- Varotti C, et al. Subungual haematomas in a patient treated with an oral anticoagulant (warfarin sodium). Eur J Dermatol. 1997;7(5):395–396.
- Ghetti E, et al. Onycholysis and subungual hemorrhages secondary to systemic chemotherapy (paclitaxel). J Eur Acad Dermatol Venereol. 2003;17(4):459–460.
- Lorenzi S, et al. Skin rash and splinter hemorrhages from ganciclovir. J Dermatolog Treat. 2003;14(3):177–178.