Abstract
Purpose of Review
This is to highlight the relationship between the morphologically identical pathogenic and nonpathogenic amoebae commonly recovered from human feces. Microscopy does not differentiate pathogenic from nonpathogenic strains. The problem of treat or do not treat infection depends on whether it is pathogenic or not, and whether reported in endemic or non-endemic country.
Recent Findings
Prevalence of amoebiasis differs greatly in different areas of the world reaching up to 50%. Easy diagnosis of amoebiasis now depends on the use of immunochromatography and/or PCR. Multiplex PCR can differentiate the pathogenic amoebae. The phylogenetic analysis of the nonpathogenic E. dispar showed a variety of genotypes. A pathogenic E. dispar genotype was isolated from an amebic liver abscess.
Summary
E. histolytica is now easily identified in laboratories, saving time and effort in diagnosis and management of infection. Phylogenetic analysis of E. histolytica and E. dispar and studying the detected genotypes can explain the big variation in pathogenicity in humans.
Similar content being viewed by others
Introduction
Entamoeba histolytica is a unicellular, protozoon parasite of humans. It moves by a jelly-like tongue-like protrusion of the cytoplasm “pseudopodium.” Infection with E. histolytica may be the cause of a variety of symptoms, beginning from no symptoms to severe fulminating intestinal and/or life-threatening extraintestinal disease. There are at least six species of the genus Entamoeba that can be identified in human stools. These are E. histolytica, E. dispar, E. mshkoveskii, E. hartmanii, E. polecki, and E. coli. E. histolytica is the only species associated with disease [1•, 2]. E. histolytica, E. dispar, and E. moshkovskii are morphologically identical and cannot be differentiated by microscopic examination. The problem with this finding is that E. histolytica was overestimated in epidemiological surveys, a fact that made the reports of infection reached more than 50% in some endemic areas [3, 4]. After the development of DNA analysis of organisms, pathologic amoebae were properly identified in pathological samples and the prevalence of E. histolytica is expected to be less than before. Entamoeba dispar and Entamoeba moshkovskii were detected as causes of asymptomatic carriers [2].
E. histolytica is considered an important cause of prolonged traveller’s diarrhea. The majority of infections occur in Central and South America, Africa, and the Indian subcontinent. The risk to travellers is paralleled to the local endemicity of the organism [5, 6]. Homosexual males showed significant higher rate of infection than normal individuals highlighting the possibility of sexual transmission of the parasite [7].
Historical Background
Ronald Elsdon Dew made a full comprehensive description of the history of amoebae in a review article published in 1969 [8]. He mentioned that Lösch was the first to report the amoebic trophozoites in the stools of a Russian patient in St. Petersburg suffering from severe dysentery in 1875.
Definite association of amoeba with disease was established by Kock and Gaffky in 1887 and Kartulis in 1889, as they described the amoebae in the intestinal ulcers of dysenteric patients.
Councilman and Luffleur identified amoebae from hepatic abscesses in 1889. They mentioned the presence of red blood cells (RBCs) inside the trophozoites and called them E. dysenteriae.
However, Fritz Schaudinn gave the Latin name “Entamoeba histolytica,” in the year 1903 [9]. He suggested “histo lytic with the meaning of tissue destruction” describing its pathogenic effect on tissue. This name “E. histolytica” was given to the haematophagous form and E. tetragena to the quadrinucleate cysts. Schaudinn imagined a fantastic life cycle of those amoebae suggesting that they multiply by some kind of schizogony or bud formation of trophozoites.
Elmassian (1909) called the trophozoites associated with the quadrinucleate cysts E. minuta [10]. Later, Walker reported that names the tetragena and minuta were applied to phases of E. histolytica and that the species has similar development as E. coli [11]. Walker and Sellards mentioned the difference in pathogenicity between the two species. They also described the commensal phase of E. histolytica and the transformation to pathogenic organism on lowering the host’s natural resistance [12]. Wenyon and O’connor and Dobell described the carrier state of the host suggesting that amoebae feed, grow and multiply on the expense of living tissue of the colon of man. They considered the ideal condition to be a state of equilibrium in which man regenerates sufficient tissue each day to compensate for the ravages of the parasite. They called man in this condition a carrier [13, 14]. Emile Brumpt had some experimental studies on E. histolytica in 1928 and could distinguish two different species, E. dysentriae that cause symptoms and E. dispar that was identified in asymptomatic carriers [15, 16]. This hypothesis was supported later by more studies done by Diamond and Clark [17].
E. moshkovskii is one of the species of the genus Entamoeba which is morphologically similar to E. histolytica/dispar. It was isolated in Moscow from sewage in 1941 [18]. This amoeba was later recovered from a human case. It was also detected from polluted water, called “Laredo strain” and was known to be nonpathogenic.
Morphology and Biology
Entamoeba histolytica occurs in the following forms, the trophozoites, precyst, cyst, metacyst, and metacystic trophozoite. The trophozoite is about 10–60 μm in size with a clear finely granular cytoplasm and a spherical nucleus that shows aggregation of chromatin beads at the nuclear membrane and a centrally located karyosome. The trophozoite is the active stage that moves, feeds, and divides. Amoebae are anaerobic and have no mitochondria [19].
The pathogenic amoeba may be haematophagous, with ingested RBCs in its cytoplasm. The nonpathogenic ameba feeds on bacterial microbiota and intestinal contents. In fresh-stool examined under the microscope, the trophozoite moves actively by a finger-like protrusion of the ectoplasm “pseudopodium,” into which the cytoplasm is pulled moving the whole body of the organism in its direction. In order to encyst, the trophozoites rounds up, discharges the undigested food, and becomes a precyst. The precyst contains collections of cigar-shaped ribosomes, called chromatoid bodies, as well as a glycogen food vacuole. All are extruded as the cell shrinks to become a mature cyst. In the process of becoming tetranucleated, the nucleus of the cyst undergoes two mitotic divisions. Chromatoid bodies and glycogen vacuoles cannot be seen at this stage and the mature cyst has an average size of around 12–13 μm [20,21,22] (Fig. 1). Encystation never occurs outside the body or in the tissue. Cysts pass in human feces and can remain viable in damp soil for up to 8 days, and in water for 9 to 90 days according to temperature [23]. Mature cyst is the infective stage and infection occurs by ingestion of these cysts in contaminated water or food.
Epidemiology
Amebiasis is responsible for around 100,000 deaths/year, mainly in Central and South America, Africa, and India, as well as for a significant rate of morbidity manifested as invasive intestinal or extraintestinal disease [24].
Infection with E. histolytica has been estimated to be as high as 50% in some developing countries as South and Central America, Africa and Asia [3]. Factors as illiteracy, poverty, low socio-economic standards including bad sanitation, improper water supply, and overcrowding contribute positively to the increased rates of transmission of the parasite and disease [25]. Infection is commonly detected in tropical and subtropical countries; however, in developed countries, infection is seen among travellers, immigrants, homosexual males, and cases in institutions. The infection usually prevails in two extremes of age: the children and the old individuals. One of the youngest reported cases is a 4-month-old baby boy in Iran [26].
USA is considered a non-endemic country. Amebic colitis is uncommon in short-term travellers returning to USA. The rate of acute amebiasis in travellers returning from Southeast Asia was 1.5%, and from Central America was 3.6% [27].
Amebiasis caused 134 deaths between 1990 and 2007 in residents of California and Texas [28]. The sero-prevalence studies of E. histolytica in Mexico revealed that more than 8% of the populations were positive for antibodies of E. histolytica [29].
Amebiasis in the Mediterranean Countries
The Mediterranean countries cover parts of the three old continents Africa, Asia, and Europe with an area of 2,085,292 km2 “(https://en.wikipedia.org/wiki/Mediterranean_Basin).” Its climate is generally moderate; however, it differs according to many factors as topography, plant cover, and rain fall. These differences plus political and financial situations may have some impact on the socioeconomic standards and health services provided to communities. Epidemiological studies of E. histolytica/dispar in the Mediterranean countries show a great variability in its prevalence among population of different countries.
Italy is a favorable country for refugees from North Africa. Studies have been done to measure the impact of infected refugees on the prevalence of parasitic infections reported that Italians had less parasitic infections than the non-Italian immigrants (10 and 31%, respectively) [30]. Some other scientists reported similar results. They reported the prevalence of parasitic infections between Italians and non-Italians to be 8.9 and 26.8%, respectively [31]. An analysis was carried out involving 1766 patients (natives and immigrants) observed during the period 2009–2010 and 771 native patients observed during the period 1996–1997, a time at which immigration in the area was minimal. The result showed that parasitic infection was much higher among immigrants (18.3–44.7%) than natives (9.6%). E. histolytica/dispar was identified in 8% of immigrants and 3% of the natives examined [32].
In Bosnia, a significant association between E. histolytica/dispar infection and ulcerative colitis was detected in 14.3 and in 20% among cases with Crohn’s disease with significant difference from the control group [33].
In Turkey, the prevalence of intestinal parasites was studied in Istanbul and different geographic regions of Turkey between January 1999 and December 2009, examining a total of 27.664 stool samples. The prevalence of E. histolytica/dispar in Mediterranean (3%), Black Sea (2%), Eastern Anatolia (2%), and Southeast Anatolia (4%) was higher than Marmara (0.1%) and Aegean regions (0.3%) [34]. In another study, 1449 stool samples were examined microscopically after staining. The result showed that 22% of samples were positive for one or more parasite species. Additionally, 1.5% of stool samples were positive for E. histolytica/dispar cysts; however, they were negative for specific E. histolytica antigen by ELISA [35]. Another study was carried out in Bursa Province to determine the prevalence of intestinal parasites in relation to personal and environmental risk factors using direct microscopic and ELISA to detect coproantigen of E. histolytica/dispar from randomly collected people from regions of the Bursa City Centre, where crowded families of low socio-economic levels reside. The overall result showed 2.27% E. histolytica/E. dispar [36].
In Lebanon, a study was carried out on children (from birth to 15 years) with acute gastroenteritis in hospitals, collecting clinical and laboratory findings during the period from January 2008 through December 2012. The result showed that almost 50% of cases had amebiasis. They attributed this result to low socioeconomic and poor hygienic conditions in the country [37]. A more recent study of stool samples collected in January 2013 from 249 children in two schools in Tripoli, Lebanon showed 5.6% rate of infection with Entamoeba histolytica/dispar by direct microscopy [38].
In Jordan, the food handlers in the area of the Dead Sea were examined for the presence of parasitic infections. E. histolytica/dispar was detected in 0.11% of persons examined. This low infection rate was attributed to the need for a health certificate that necessitates annual health examination for working as food handlers [39]. Some previous studies showed 8% in diarrheic cases in the Jordan Badia Region and 27.81% in Amman were positive to E. histolytica/dispar [40, 41]. An interesting study to detect the degree of contamination of vegetables used for salad was done in Amman and Baqa’a – Jordan showed that 10% of lettuce examined, were contaminated with cysts of E. histolytica/dispar [42].
In five Governorates of Ghaza Strip, the prevalence of infection with E. histolytica/dispar was reported to be ranging from 12.3 to 16.63% among school children by stool analysis [43]. The authors detected a significant difference in prevalence according to seasons. The rate of infection was higher in spring and summer and reached 16.4 and 17.4% in spring and summer respectively in comparison to 14.7 and 15.9% in autumn and winter, respectively [43]. In another more recent study on preschool children in Gaza City with gastroenteritis, the prevalence of pathogens causing gastroenteritis among symptomatic cases was significantly higher than the prevalence in asymptomatic carriers (88.5 and11.1%, respectively). The most prevalent isolated enteric pathogens were Entamoeba histolytica (28.0%) and Giardia lamblia (26.7%) [44].
In Egypt, Stanley reported that up to 38% of cases presenting with diarrhea were infected with E. hystolytica and were diagnosed as amoebic colitis [45]. Banisch et al. in 2015 reported 12.5% infection with E. histolytica/dispar among cases with gastroenteritis in Greater Cairo [46] and Ibrahim et al. reported that E. histolytica was in 3.6% of cases examined by PCR and this was 14 times less in prevalence than the nonpathogenic amebae in Beni-Suef, Egypt [47]. In Damietta City of the North Delta of Egypt, a Multiplex Allele Specific Chain Reaction (MAS-PCR) assay was used to detect four parasitic pathogens, E.histolytica, G. intestinalis, Cryptosporidium and D. fragilis in stool samples of cases with gastroenteritis during the period from June to September 2013. In this test, E. histolytica was detected in 1.2% of studied cases, while E. dispar was in 6.9% [48]. A study to determine the association between risk factors and the occurrence of intestinal parasitic infections (potentially pathogenic) among municipal waste collectors in Alexandria, Egypt, detected E. histolytica/dispar was in 3.2% of examined samples [49].
In Libya, studies “between 2000 and 2015” showed prevalence rates of 0.8–36.6% (mean 19.9%) for E. histolytica/dispar. The mean prevalence rate of E. histolytica/dispar was significantly higher among individuals with gastroenteritis (mean 19.9%). The authors used second generation of enzyme immunoassays (EIAs), which was able to detect 0.8% of E. histolytica in fecal samples [50]. Scrutiny of stools of 1250 Libyan and 1133 other African residents of Al-Khoms, Libya, were examined during the period “from June 2012 to May 2013” for intestinal protozoan parasites. Infection with E. histolytica/dispar was in 9.8% among Libyans and 14.7% in other Africans [51].
In Tunisia, the first intestinal infections with Entamoeba moshkovskii were reported in two healthy adults. Specific nested polymerase chain reaction and sequencing was used to distinguish Entamoeba moshkovskii from those of the morphologically identical parasites Entamoeba histolytica and Entamoeba dispar [52].
In Morocco, a study was conducted from January 2007 to December 2013 to outline the prevalence of intestinal parasites. Entamoeba histolytica/dispar was in 28.9% of studied samples. However, most of the cases were asymptomatic. Polyparasitism was common among studied cases [53].
In Spain, a study was done during the years 2008–2011 on all immigrant cases attending the Tropical Medicine Unit of Hospital Universitario Central de Asturias, in the North of Spain. Stool analysis and nested PCR targeting 18S-like ribosomal RNA were done to all stool samples. E.histolytica/dispar was detected in 11% of total cases. E. histolytica was more predominant (in 78%) among cases with amoebiasis, while E. dispar was in 12%. E. histolytica infection was reported to be a prevalent parasitosis in immigrant population specially in patients from Sub-Saharan Africa, particularly from Senegal [54].
In France, there are no general data for the population parasitic infection, but only for occupations at risk, or for patients treated in hospitals. Sewer workers were examined for presence of parasitic infections and E. histolytica/dispar was demonstrated in 11% of the examined asymptomatic individuals, whereas these frequencies were much lower in the general population (about 2% of stools examined in hospital outpatients) [55]. In a previous study in France, E. histolytica/dispar was rarely differentiated and positive cases have to be treated systematically. E. histolytica/dispar showed a prevalence rate of 1.87% among 7301 patients attending the Pitié-Salpêtrière teaching hospital between 2002 and 2006 by microscopy, followed by PCR test which could identify E. histolytica in a rate of 0.12%. This finding confirmed the fact that E. dispar is more prevalent than E. histolytica in France [56].
Pathophysiology
Amoebiasis is thought to be one of the most commonly known parasitic diseases affecting millions of people worldwide [57, 58]. Many of the cases have been discovered accidentally during a routine stool analysis and unfortunately many of them were given unneeded treatment for ameba. Those cases infected with the organism without symptoms were called carriers. It is believed that the nonpathogenic E. dispar prevails 10 times more than pathogenic E. histolytica in countries as Egypt and Brazil, while in Western countries, where male homosexuality is more common, both E. histolytica and dispar can be equally detected [1•, 45].
The combination of intestinal symptoms with the microscopic finding of haematophagous forms of amebae in feces is an indication of an attack of the intestinal epithelium by pathogenic amebae. This usually occurs as a result of unknown stimuli that trigger a process of adhesion of amebae to the epithelial cells. The amebae use their lectins to adhere to the cell surface sugars “galactose and N-acetylgalactosamine” and a 260-kd surface protein that contains 170 and 35 kD subunits [45, 59, 60]. Immunoglobulin A (IgA) against amebic lectin may result in recurrence of attacks [61]. IgA response is considered an indication of invasiveness. However, there is no evidence that IgA deficiency may aggravate severity of the disease [62••].
Amebae begin to secrete their lytic enzymes including pore-forming proteins, lipases and the cysteine proteases, which initiate a process of cell necrosis and apoptosis in the affected colonic epithelial cells. Immune cells become attracted to the damaged colonic cells and become destroyed by the lytic enzymes secreted by the active trophozoites. The destroyed host immune cells release more lytic enzymes into the surrounding tissue, initiating an ulcer in the affected area. Amebic ulcer in the colonic epithelium is typically flask-shaped. In case trophozoites reach a blood vessel during tissue destruction, blood will appear in stool causing the typical amebic dysentery. Some trophozoites can pass into the portal vessels to reach the liver, evading the complement-mediated lysis in blood, where they can produce similar pathological effect in the liver cells ending in a typical abscess.
The amebic abscess in the liver is composed of dead liver cells in the center of the abscess surrounded by amoebic trophozoites and inflammatory cells and unaffected cells of the liver at the outer margin of the abscess [45]. Trophozoites could also be carried by the blood stream to other organs of the body, or reach the nearby organs directly after rupture from the amebic abscess [62••].
Limitation and prevention of recurrence of infection is due to cell-mediated immunity. Lymphokines, particularly the interferon delta, are produced in response to an antigen specific reaction leading to active killing of the trophozoites of E. histolytica by macrophages. This mechanism depends on contact, nitric oxide (NO) as well as oxidative and non-oxidative pathways. Amebicidal activity of neutrophils is activated by lymphokines as TNF-α [62••].
Blood route or direct spread by rupture may carry E. histolytica trophozoites to other organs in the body other than the liver as the lungs causing pleuropulmonary disease, peritoneum causing peritonitis, pericardium leading to pericarditis, to the brain causing a brain abscess and/or may spread to the genital and urinary system causing genitourinary infection [62••].
Many scientists declared the association of amebiasis with AIDS [63,64,65,66,67,68]. Hung et al. suggested that amebic liver abscess is an emerging infection in cases infected with HIV in endemic and non-endemic areas [69].
HIV was incidentally detected among 40% cases infected with E. histolytica in Taiwan among males that practice oral, anal, or oral–anal sex behavior, raising the possibility of sexual transmission of E. histolytica [7].
Clinical Picture
Infection may be asymptomatic in most of the cases; however, severe fulminating disease may occur after an incubation period of 7–28 days from exposure to infection. Mild symptoms may be in the form of abdominal cramps, diarrhea with passage of 3–8 soft stools/day, or passage of stool with mucus and occasional blood. There may be fatigue, excessive gasses, rectal pain “tenesmus,” and weight loss. In heavy infection, the patient may show, fever, abdominal tenderness, vomiting and bloody diarrhea of about 10–20 motions/day [70].
Cases with amebic liver abscess usually show sub-acute onset with fever and pain in the right upper quadrant of the abdomen. Diarrhea may be an associated symptom in 30% and Jaundice in about 10% of cases. There may be previous history of dysentery few months before [71, 72]. Diagnosis needs the combination of clinical, radiological and immunological methods. The liver abscess is usually solitary and mostly in the right lobe of the liver with high titer of antibodies against E. histolytica, detected in more than 99% of cases.
Aspiration is very important for diagnosis and healing. The aspirated pus is thick, brownish, and typically called “anchovy sauce” [71, 72].
Other site for extraintestinal spread of E. histolytica includes the pulmonary amoebiasis. Infection may reach the pleural cavity and lungs by the haematogenous route or after perforation of a hepatic abscess through the diaphragm. Brain abscess may also develop via the heamatogenous route, while the cutaneous infection can occur at site of aspiration of a liver abscess [73].
The nonpathogenic E. dispar was detected as a causative agent of amebic liver abscess. Molecular phylogenetic analysis done in this case showed that E. dispar has genetic diversity with existence of several different genotypes that can be associated with tissue damage as in the case of E. histolytica [74]. This finding is of extreme importance as it simply shows that E. dispar could unexpectedly behave in a crazy way.
Ameboma
It is one of the rare complications of colonic infection with pathogenic E. histolytica. It occurs as a result of deep invasion of the wall of the colon by invasive E. histolytica trophozoites with extensive formation of granulation tissue and the development of tumor-like mass. The most common sites of ameboma are the cecum and ascending colon. It is manifested by intestinal obstruction and bleeding. Radiological examination shows local thickening of the wall of the cecum. This should be differentiated from malignant growths, TB and fungal infections [75,76,77]. Colonoscopy shows ulcerated mass in the wall of the cecum. Histological examination reveals multiple crypt abscesses with ulcerations and trophozoites with phagocyted RBCs in the exudative tissue. Immunological tests may be of importance to confirm the diagnosis. The cause of this unusual reaction was suggested to be due to superimposed bacterial infection [78].
Laboratory Diagnosis
Amebiasis is diagnosed in the laboratory by detecting the parasite in specimens or by an immunologic or a molecular technique [79,80,81,82,83].
In case of invasive intestinal amebiasis, the blood picture in 80% of cases may show leukocytosis without eosinophilia, elevation of erythrocytic sedimentation rate (ESR), elevation of serum alkaline phosphatase and transaminase levels, mild elevation in bilirubin level, reduction in albumin levels and mild anemia [62••].
Not only microscopic detection of E. histolytica but also other specific methods should be included in the diagnosis of amebiasis, e.g., immunologic techniques and/or PCR assay.
Microscopy
Identification of haematophagous trophozoites in fresh stool smears is the primary step for the identification of intestinal amebiasis and is an indication of infection [1•]. Because of irregular output of the parasite stages in stool, a single stool analysis is not usually positive. To further improve the sensitivity of the microscopic examination, it is indicated to examine two or three stool specimens on different days, or to do microscopic examination of the second motion after a saline purge. However, microscopy cannot distinguish the pathogenic from the non-pathogenic strains of amebae.
Microscopy is also used to examine aspirates from liver or lung abscess and the parasite can only be visualized in about 20% of cases [62••].
Culture
Culture is a method of diagnosis, however it is not easy to perform and less sensitive than microscopic examination with a success rate of 50–70% [1•].
Xenic cultivation, first introduced in 1925, is defined as the growth of the parasite in the presence of an undefined flora. This technique is still in use today utilizing the modified Locke egg or the modified Boek and Drbohlav’s media particularly in research studies [84].
Axenic cultivation, first achieved by Diamond in 1961, involves growing the parasite in the absence of any other metabolizing cells. The technique is considered very sophisticated and is used mainly for research studies [84, 85]. Only a few strains of E. dispar have been reported to be viable in axenic cultures [62••].
Antigen Detection
Detection of coproantigen of E. histolytica by ELISA is a sensitive and specific test that depends on the use of monoclonal antibodies kits [1•]. It is considered more sensitive than light microscopy for detection of infection with E. histolytica [86,87,88].
Some very important tests are the immunochromatographic assays. They are practical and easy to perform and could be applied in the laboratories with limited facilities or in the field. A test can detect E. histolytica separately or may combine three intestinal pathogens (E. histolytica, Giardia and Cryptosporidia) in one step to be detected in fecal samples. This test utilizes monoclonal antibodies of Entamoeba species. It has the disadvantage of inability to differentiate between pathogenic and non-pathogenic strains. It was evaluated in Zaragoza, Spain, in comparison with microscopy and PCR, and revealed acceptable sensitivities and specificities for G. duodenalis and cryptosporidia and slightly inferior results for E. histolytica/dispar and also showed similar results when evaluated in Egypt [46, 89].
Antibody Detection
Cases with pathogenic intestinal amoebiasis, showing symptoms, usually possess antibodies against E. histolytica in their sera [1•]. These antibodies appear in blood after 1 week and stay for years after acute infection that is why detection of antibodies does not differentiate between new and past infection. Antibodies are detected in 99% of cases with amoebic liver abscess [62••]. ELISA, the most commonly used worldwide, is a sensitive and specific test that can differentiate E. histolytica from E. dispar. False negative results can occur within the first 7–10 days after infection.
Other Methods of Detection of Antibodies
Other methods of detection of antibodies are immunofluorescent assay (IFA), indirect haemagglutination assay (IHA), immunoelectrophoresis, counterimmunoelectrophoresis (CIE), immunodiffusion (ID), and complement fixation (CF).
Molecular Techniques
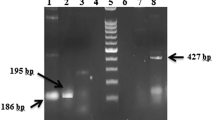
The identification of E.histolytica/E. dispar/E. moshkovskii is now using a wide variety of PCR-based assays. Different genes are targeted in these assays, e.g., ssrRNA gene (18S rDNA) and many other genes.
Some PCR techniques can successfully and simultaneously differentiate all the Entamoeba spp. from fecal samples in one test. An example of these tests is the Luminex PCR assay and Multiplex PCR [90,91,92,93].
Multiplex PCR can also be utilized to detect pathogenic E. histolytica with other pathogenic protozoa in one step, which is very important in epidemiological surveys in endemic areas [88,95,, 94–96].
This method of diagnosis is sensitive, specific, easy, and simple and can help in the epidemiological studies concerned with multiple infections in endemic areas.
Treatment
Metronidazole is recommended by the WHO as the drug of choice for treatment of cases with amebiasis. Metronidazole is a 5-nitroimidazole derivative, which has an antimicrobial effect against the anaerobic bacteria and protozoa as E. histolytica, G. lamblia and T. vaginalis. This drug is absorbed after oral intake and is excreted in urine with half-life about 8 h [97].
In case of invasive amebiasis, it is recommended to take a dose of metronidazole: 35–50 mg/kg/day in three divided doses after meals for 8–10 days, or I.V. in three divided injections/day, if the patient is unable to take the oral medicine. Generally, It is important to eliminate any viable amebae in the colon with luminal amebicide, e.g., paromomycin, idoquinol or diloxanide furoate, after a course of tissue amebicide, as each drug may enhance the effect of the other [98].
In the endemic areas, asymptomatic carriers should not be given treatment; however, in non-endemic areas, they must be treated with one of the known luminal drugs [98,99,100]. This assumption is based on the fact that invasive disease may occur and E. dispar is considered an indication of fecal contamination, which necessitates some control measures [45].
Tinidazole has been approved by the US Food and Drug Administration (FDA), for treatment of both intestinal and extraintestinal amebiasis. It is more effective in comparison with metronidazole with less dosage, less duration of intake and less adverse effects. In addition, the use of a broad-spectrum antibiotic to the regimen of treatment gives the best result in cases with fulminant amebic colitis [98].
Control
Avoid the poor personal hygienic practices, such as neglecting washing hands before eating, especially after working with the soil. It is also of great importance to wash raw vegetables before using in salad. Food handlers should be inspected regularly and those infected should be prevented from food handling until proved non-infective. Treatment of the infected family members and health education for proper sanitary conditions are of prompt importance. Genotyping of E. histolytica/dispar/moshkovskii from humans and animals are highly recommended to identify the dynamics of transmission of these protozoa.
Conclusion
Amebiasis continues to be one of the most important health problems in tropical and subtropical countries. It occurs as a result of infection with the pathogenic strain of E. histolytica. Infection may be asymptomatic or may be fulminating with intestinal and extraintestinal tissue invasion. The prevalence of amebiasis all over the world has dropped significantly after improvement of the diagnostic methods that could differentiate E. histolytica from the other nonpathogenic strains. The role of E. dispar is still very vague, although it is considered as nonpathogenic since decades. Phylogenetic analysis of E. dispar, detected a variety of genotypes, some of them may act differently under unusual circumstances. Cases could be treated successfully with metronidazole or tinidazole plus tissue amebicides. Travellers are at risk of catching infection in exotic countries due to lack of proper health facilities.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Fotedar R, Stark D, Beebe N, Marriott D, Ellis J, Harkness J. Laboratory diagnostic techniques for Entamoeba species. ClinMicrobiolRev. 2007;20(3):511–32. A descriptive review for diagnosis of amebiasis.
Romano N, Fakhrurrazi A, Yvonne A, Jamaiah I, Rohela M. Differentiating Entamoeba histolytica, Entamoeba dispar and Entamoeba moshkovskii using nested polymerase chain reaction (PCR) in rural communities in Malaysia. Parasites and Vectors. 2010;5:187.
Tengku SA, Norhayati M. Public health and clinical importance of amoebiasis in Malaysia: a review. Trop Biomed. 2011;28(2):194–222.
Ouattara M, N’Guéssan NA, Yapi A, N’Goran EK. Prevalence and spatial distribution of Entamoeba histolytica/dispar and Giardia lamblia among school children in Agboville area (Côte d’Ivoire). PLoS Negl Trop Dis. 2010;4(2):10.1371.
World Health Organization. Amebiasis. Weekly Epidermiol Rec. 1997;72:97–100.
Slack A. Parasitic cases of prolonged diarrhea in travellers. Diagnosis and management. Reprod Health. 2012;41(10):782–6.
Lo YC, Ji DD, Hung CC. Prevalent and incident HIV diagnosis among Entamoeba histolytica-infected adult males: a changing epidemiology associated with sexual transmission-Taiwan, 2006-2013. PLoS Negl Trop Dis. 2014;8(10), e3222.
Elsdon-Dew R. Amoebiasis: its meaning and diagnosis. Review article. S.A. Medical Journal. 1969;19:483–6.
Schaudinn F. Arb Gesundh-Amte (Berl). 1903;19:547.
Elmassian, M. Zbl. Bakl. 1. Abt. Orig. 1909: 52, 335.
Walker EL. The parasitic Amebae of the intestinal tract of man and other animals. J Med Res. 1908;17(4):379–460.
Walker EL, Sellards AW. Experimental entamebic dysenrery. Philip J Sci. 1913;8:253–331.
Wenyon, C. M. and O’Connor, F. W. (1917): J. Roy. Army Med. Cps., 28, I, 151, 346, 461, 557 and 686.
Dobell C. The amebas living in man. A zoological monograph. London: Bale, Sons and Danielsson, Ltd; 1919. p. 155.
Brumpt E. Differentiation of human intestinal amoebae with four-nucleated cysts. Trans R Soc Trop Med Hyg. 1928;22:101–14. Discussion pp. 115-124.
Pinella AE, Lopez MC, Viasus DF. History of Entamoeba histolytica Protozoan. Rev Med Chil. 2008;136(1):118–24.
Diamond LS, Clark CG. A redescription of Entamoeba histolytica Schaudinn, 1903 (emended Walker, 1911) separating it from Entamoeba dispar Brumpt. J Eukaryot Microbiol. 1993;1925(40):340–4.
Tshalaia LE. On a species of Entamoeba detected in a sewage effluents. (in Russian). Med Parazit (Moscow). 1941;10:244–52.
Sodeman WA. Intestinal protozoa, Amebas. Chapter 79. In: Baron S, editor. Medical microbiology. 4th ed. Galveston: University of Texas Medical Branch of Galviston; 1996.
Clark CG, Espinosa-Cantellano M, Bhattacharya A. Entamoeba histolytica: an overview of the biology of the organism. In: Ravdin JI, editor. Amebiasis. London, United Kingdom: Imperial College Press; 2000. p. p. 145.
Garcia LS, Bruckner DA. Diagnostic medical parasitology. 3rd ed. Washington, D.C: ASM Press; 1997.
Katz M, Despammier DD, Gwadz RW. Parasitic diseases. New York, N.Y.: Springer Verlag; 1989.
Beaver PC, Jung RC, Cupp EW. Amebae inhabiting the Alimentary Canal. In Clinical Parasitology, 9th edition, Lea & Febiger, Philadelphia. 1984; 101-148.
Houpt E, Hung C, Petri W. Entamoeba histolytica (amebiasis). Infectious Disease and Antimicrobial Agents. 2016: http://www.antimicrobe.org/new/b137.
WHO. Health conditions in the occupied Palestinian territory, including east Jerusalem, and in the occupied Syrian Golan. Sixty-second World Health Assembly, provisional agenda item14. May 2009.
Zibaei M, Firooz F, Azargoon A. Infantile Amoebiasis: A Case Report. Case Reports in Infectious Diseases. Volume 2012 (2012), Article ID 614398, 3 pages doi:10.1155/2012/614398
Freedman DO, Weld LH, Kozarsky PE, Fisk T, Robins R, von Sonnenburg F, et al. Spectrum of disease and relation to place of exposure among all returned travellers. N Engl J Med. 2006;354(2):119–30.
Gunther J, Shafir S, Bristow B, Sorvillo F. Amoebiasis-related mortality among United States residents, 1990-2007. Am J Trop Med Hyg. 2011;85(6):1038–40.
Caballero-Salcedo A, Viveros-Rogel M, Salvatierra B, Tapia-Conyer R, Sepulveda-Amor J, Gutierrez G, et al. Seroepidemiology of amebiasis in Mexico. Am J Trop Med Hyg. 1994;50(4):412–9.
Peruzzi S, Gorrini C, Piccolo G, Calderaro A, Dettori G, Chezzi C. Prevalence of intestinal parasites in the area of Parma during the year 2005. Acta Biomed. 2006;77:147–15.
Masucci L, Graffeo R, Bani S, Bugali F, Boccia S, Nicolotti N. Intestinal parasites isolated in a large teaching hospital, Italy, 1 May 2006 to 31 December 2008. Euro Surveill. 2011;16:19–25.
Belli A, Coppolab MG, Petrullob LP, Lettieric G, Palumboc C, Dell’Isolac C, et al. The current spectrum and prevalence of intestinal parasitosis in Campania region of southern Italy and their relationship with migration from endemic countries. Int J Infect Dis. 2014;29:42–7.
Babic E, Bevanda M, Mimica M, Karin M, Volaric M, Boqut A, et al. Prevalence of amebiasis in inflammatory bowel disease in University Clinical Hospital Mostar. Springer plus. 2016;5(1):1586.
Koksal F, Baslanti I, Samasti M. A retrospective evaluation of the prevalence of intestinal parasites in Istanbul, Turkey. Türk Parazitol Derg. 2010;34(3):166–71.
Malatyali E, Ozcelik S, Celiksoz A. The investigation of Entamoeba histolytica prevalence in some villages of Sivas by ELISA method. Turkiye Parazitol Derg. 2011;35:6–9.
Alver O, Heper Y, Erkan I, Akalin H, Tore O. Prevalence and assessment of enzyme-linked immunosorbent assays (ELIsA) and three microscopic methods in the diagnosis of Entamoeba histolytica/dispar. Afr J Microbiol Res. 2011;5(12):1443–9.
Naous A, Naja Z, Zaatari N, Kamel R, Rajab M. Intestinal amebiasis, a concerning cause of acute gastroenteritis among hospitalized children. N Am J Med Sci. 2013;5(12):689–98.
Osman M, El Safadi D, Cian A, Benamrouz S, Nourrisson C, Poirier P, et al. Prevalence and risk factors for intestinal protozoan infections with Cryptosporidium, Giardia, Blastocystis and Dientamoeba among schoolchildren in Tripoli, Lebanon. PLoS Negl Trop Dis. 2016;10(3), e0004496. doi:10.1371/journal.pntd.0004496.
Abdel-Dayem M., Al Zou’bi R., Bani Hani R., Amer ZS. Microbiological and Parasitological investigation among food handlers in hotels in the Dead Sea area, Jordan. Journal of Microbiology, Immunology and Infection (29 June 2013); doi:10.1016/jmii.2013.06.001
Nimri LF. Cyclospora cayetanensis and other intestinal parasites associated with diarrhea in a rural area of Jordan. Int Microbiol. 2003;6:131. doi:10.1007/s10123-003-0121-4.
Chazal AM, Adi HK. The prevalence of intestinal parasites in Amman, Jordan. Bull Pharm Sci, Assuit Univ. 2007;30:335–40.
Ismail Y. Prevalence of parasitic contamination in salad vegetables collected from supermarkets and street vendors in Amman and Baqa’a – Jordan. Pol J Microbiol. 2016;65(2):1204480.
Alhindi AI, Al-Louh M. Trends of intestinal parasites prevalence in the Gaza Strip, 1998-2007: the use of government health records. TurkJMed Sci. 2013;43:65–595.
Al LN, Elyazji M, Al-Haddad R, Ridwan F. Prevalence of enteric pathogen-associated community gastroenteritis among kindergarten children in Gaza. J Biomed Res. 2015;29(1):61–8.
Stanley Jr SL. Amoebiasis. Lancet. 2003;361(9362):1025–34.
Banisch DM, El-Badry A, Klinnert JV, Ignatius R, El-Dib N. Simultaneous detection of Entamoeba histolytica/dispar, Giardia duodenalis and cryptosporidia by immunochromatographic assay in stool samples from patients living in greater Cairo Region, Egypt. World J. of Microbiol, and. Biotechnol. 2015;31(8):1251–8.
Ibrahim SS, El-Matarawy OM, Ghieth MA, Abu Sarea EY, El-Badry AA. Copro prevalence and estimated risk of Entamoeba histolytica in diarrheic patients at BeniSuef, Egypt. World J Microbiol Biotechnol. 2015;3(2):385–90.
Mohammad KA. Detection of human intestinal protozoa by using multiplex allele specific polymerase chain reaction (MAS-PCR) in New Damietta City. ZUMJ. 2013;19(6):556–68.
Eassa SM, Abd El-Wahab EW, Lotfi SE, El Masry SA, Shatat HZ, Kotkat AM. Risk factors associated with parasitic infection among municipality solid-waste workers in an Egyptian community. J Parasitol. 2016;102(2):214–21.
Ghenghesh KS., Ghanghish K., BenDarif ET., Shembesh K, and Franka E. Prevalence of Entamoeba histolytica, Giardia Lamblia and Cryptosporidium Spp. In Libya: 2000-2015. Libyan J Med 2016, 11: 32088 - doi:10.3402/ljm.v11.32088
El Ammari NE, Nair GA. Critical evaluation of the intestinal protozoan parasites among Libyan and other African residents of Al-Khoms, Libya. Journal of Entomology and Zoology Studies. 2015;3(2):42–6.
Ben AS, Aoun K, Maamouri N, Ben AR, Bourtabine A. Short report: first molecular identification of Entamoeba moshkovskii in human stool samples in Tunisia. Am J Trop Med Hyg. 2008;79(5):706–70.
El Mezouari E, Belhamri N, Lamrani HA, Kaddouri M, Zyani M, Qacif H, et al. Intestinal parasitic infections in adults in Marrakech: review of 7 years intestinal parasitic in adult at Marrakech: review of 7 years. Journal of Applied Science And Research. 2014;2(4):18–24.
Rojo S, Fernandez E, Balado C, Dominguez J, Morilla A, Perez F, et al. Geographic distribution of Entamoeba histolytica and Entamoeba dispar in immigrant population in Spain. Barcelona, Spain: European Congress of Clinical Microbiology and Infectious Diseases; 2014. p. 10–3.
French agency for food, environmental and occupational health and safety. Data sheet on foodborne biological hazards/Entamoeba histolytica, E. histolytica/E. dispar. January 2011. https://www.anses.fr/…/french-agency-food-environmental-and-occupational health and safety
Thellier M., Bart-Delabesse E., Poupon MC., Faussart A. Human intestinal amoebiasis revisited: pathogenic Entamoeba histolytica is less common than non pathogenic Entamoeba dispar. La Lettre de l’Infectiologue –Septembre-Octobre 2007; Tome XXII - n° 5
Leishout L, Verweij JJ. Newer diagnostic approaches to intestinal protozoa. Curr Opin Infect Dis. 2010;23:488–93.
Stensvold RC, Nielsen HV. Comparison of microscopy and PCR for detection of intestinal parasites in Danish patients supports an intensive for molecular screening platforms. JClin Microbiol. 2012;25(2):450–1.
Ravdin JI, Jackson TF, Petri Jr WA, Murphy CF, Ungar BL, Gathiram V, et al. Association of serum antibodies to adherence lectin with invasive amebiasis and asymptomatic infection with pathogenic Entamoeba histolytica. J Infect Dis. 1990;162:768–72.
Ximénez C, Cerritos R, Rojas L, Dolabella S, Morán P, Shibayama M, et al. Human amebiasis: breaking the paradigm? Int J Environ Res Public Health. 2010;7(3):1105–20.
Haque R, Mondal D, Duggal P, Kabir M, Roy S, Farr B, et al. Entamoeba histolytica infection in children and protection from subsequent amebiasis. Infect Immun. 2006;74(2):904–9.
•• Dhawan V. Amebiasis: Background, Pathophysiology, Etiology. http://emedicine.medscape.com/article/212029-overview. March 24 2016. A comprehensive review on amebiasis.
Bowley DM, Loveland J, Omar T, Pitcher GJ. Human immunodeficiency virus infection and amebiasis. Pediatr Infect Dis J. 2006;25(12):1192–3.
Brindicci G, Picciarelli C, Fumarola L, Carbonara S, Stano F, Ciracì E, et al. Amoebic hepatic abscesses in an HIV positive patient. AIDS Patient Care STDs. 2006;20(9):606–11.
Chen Y, Zhang Y, Yang B, Qi T, Lu H, Cheng X, et al. Seroprevalence of Entamoeba histolytica infection in HIV infected patients in China. Am J Trop Med Hyg. 2007;77(5):825–8.
Hsu MS, Hsieh SM, Chen MY, Hung CC, Chang SC. Association between amebic liver abscess and human immunodeficiency virus infection in Taiwanese subjects. BMC Infect Dis. 2008;8:48.
Park WB, Choe PG, Jo JH, Kim SH, Bang JH, Kim HB, et al. Amebic liver abscess in HIV infected patients, Republic of Korea. Emerg Infect Dis. 2007;13(3):516–7.
Karp CL, Auwaerter PG. Coinfection with HIV and tropical infectious diseases. I. Protozoal pathogens. Clin Infect Dis. 2007;45(9):1208–13.
Hung CC, Ji DD, Sun HY, Lee YT, Hsu SY, Chang SY, et al. Increased risk for Entamoeba histolytica infection and invasive amebiasis in HIV seropositive men who have sex with men in Taiwan. PLoS Negl Trop Dis. 2008;2(2):175.
Petri Jr WA, Haque R. Entamoeba species, including amebic colitis and liver abscess. In: Bennett JE, Dolin R, Mandell GL, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 8th ed. Philadelphia: Elsevier Saunders; 2014. p. 274.
Maltz G, Knauer CM. Amebic liver abscess: a 15-year experience. Am J Gastroenterol. 1991;86:704–10.
Anesi JA, Gluckman S. Amebic liver abscess, review. Clinical liver disease. A Multimeria Review Journal. 2015;6(2):41–3.
Hesse AAJ, Nouri AN, Hassan HS, Hashish AA. Parasitic infestations requiring surgical intervensions. Semin Pediatr Surg. 2012;21(2):142–50.
Dolabella SS, Serrano-Luna J, Navarro-Garcia F, Cerritos R, Ximenez C, Galvan-Moroyoqui JM, et al. Amoebic liver abscess production by Entamoeba dispar. Ann Hepatol. 2012;11(1):107–17.
Fernandes H, D’Souza CR, Swethadri GK, Naik CN. Ameboma of the colon with amebic liver abscess mimicking metastatic colon cancer. Indian J Pathol Microbiol. 2009;52(2):228–30.
Zapata L, Flores R, Jurado JJ, Hernández N, Altamirano J. Success of medical therapy in a rare case of cecal ameboma. El éxito del tratamiento médico en un raro caso de ameboma cecal. Rev Gastroenterol Mex. 2011;76:55–9.
Lin C, Kao K. Ameboma: a colon carcinoma-like lesion in a coloscopy finding. Case Rep Gastroenterol. 2013;7(3):438–41.
Majeed SK, Ghazanfar A, Ashraf J. Caecal amoeboma simulating malignant neoplasia, ileocaecal tuberculosis and Crohn’s disease. J Coll Physicians Surg Pak. 2003;13:116–7.
AbdAlla MD, ElHawey AM, Ravdin JI. Use of an enzyme linked-immunosorbent assay to detect anti-adherence protein antibodies in sera of patients with invasive amebiasis in Cairo, Egypt. Am J Trop Med Hyg. 1992;47:800–4.
Haque R, Mollah NU, Ali IK, Alam K, Eubanks A, Lyerly D, et al. Diagnosis of amebic liver abscess and intestinal infection with the Tech Lab Entamoeba histolytica II antigen detection and antibody tests. J Clin Microbiol. 2000;38(9):323–59.
Tanyuksel M, Petri Jr WA. Laboratory diagnosis of amebiasis. Clin Microbiol Rev. 2003;16(4):713–29.
Helmy MM, Rashed LA, Abdel-Fattah HS. Detection and differentiation of Entamoeba histolytica and Entamoeba dispar isolates in clinical samples by PCR. J Egypt Soc Parasitol. 2007;37(1):25774.
Singh A, Houpt E, Petri WA. Rapid diagnosis of intestinal parasitic protozoa, with a focus on Entamoeba histolytica. Interdiscip Perspect Infect Dis. 2009;5:47–90.
El-Deeb, NA. In virto comparative study on Entamoeba histolytica isolates from asymptomatic and symptomatic cases. PhD thesis, Faculty of Medicine, Cairo University 1983.
Diamond LS. Axenic cultivation of Entamoeba histolytica. Science. 1961;134:336.
Den Hartoq J, Rosenbaum L, Wood Z, Burt Jr D, Petri WA. Diagnosis of multiple enteric protozoan infections by enzymelinked immunosorbent assay in the Guatemalan highlands. Am J Trop Med Hyg. 2013;88:167–71.
Selim S, Nassef N, Sharaf S, Badra G, Abdel AD. Coproantigen detection versus direct methods for the diagnosis of Giardia lamblia in patients from the National Liver Institute. J Egypt Soc Parasitol. 2009;39:575–83.
Stark D, Al-Qassab SE, Barratt JLN, Stanley K, Roberts T, Mariott D, Harkness J, Ellis JT. Evaluation of Multiplex Tandem Real-Time PCR for Detection of Cryptosporidium spp., Dientamoeba fragilis, Entamoeba histolytica, and Giardia intestinalis in Clinical Stool Samples. J Clin Microbiol. 2011 Jan. 49(1): 257-262
Goni P, Martin B, Villacampa M, Garcia A, Seral C, Castillo FJ, Clavel A. Evaluation of an immunochromatographic dip strip test for simultaneous detection of Cryptosporidium spp., Giardia duodenalis, and Entamoeba histolytica antigens in human faecal samples. Eur J Clin Microbiol Infect Dis. 2012: 31:2077–2082
Santos HL, Bandyopadhyay K, Bandea R, Peralta RH, Peralta JM, Da Silva AJ. LUMINEX: a new technology for the simultaneous identification of five Entamoeba spp. commonly found in human stools. Parasit Vectors. 2013;6:69.
Zebardat N, Haghighi A, Yeganeh F, Tabaei SJS, Gharavi MJ, Fallahi S, et al. Application of multiplex PCR for detection and differentiation of Entamoeba histolytica, Entamoeba dispar and Entamoeba moshkovskii. Iran J Parasitol. 2014;9(4):466–73.
Fallah E, Shabhazi A, Yazdanjoii M, Esboei BR. Differential detection of Entamoeba histolytica from Entamoeba dispar by parasitological and nested multiplex polymerase chain reaction methods. J Anal Res Clin Med. 2014;2(1):25–9.
Gachuhi S, Obonyo M, Odhiambo R, Swierczeweski B, Mwakubambanya R. Differentiation of Entamoeba histolytica and Entamoeba dispar complex by multiplex polymerase chain reaction. Sch Acad J Biosci. 2014;2(11):762–7.
Verweij VJ, Blange RA, Templton K, Schinkel J, Brienen EA, van Rooyen MAA, et al. Simultaneous detection of Entamoeba histolytica, Giardia lamblia and Cryptosporidium parvum in fecal samples using multiplex real-time PCR. J Clin Microbiol. 2004;42(3):1220–3.
Verweij J, van Lieshout L. Intestinal parasitic infections in an industrialized country; a new focus on children with better DNA-based diagnosis. Symposia of the British Society of Parasitology. 2011;47:1492–8.
Shin J, Lee S, Kim TS, Ma D, Chin J, Shin E. Multiplex–touch down pcr to simultaneously detect Cryptosporidium parvum, Giardia lamblia and Cyclospora cyetenensis, the major causes of Traveller’s diarrhea. Korean J Parasitol. 2016;54(5):631–6.
WHO Model Prescribing Information. Drugs used in parasitic diseases. Secondth ed. 1995. p. 152.
Gonzales MLM, Dans LF, Martinez EG. Antiamoebic drugs for treating amoebic colitis. Cochrane Database of Systematic Reviews 2009, Issue 2
Petri Jr WA, Singh U. Diagnosis and management of amebiasis. Clin Inf Dis. 1999;29(5):117–25.
Roy SL. Amebiasis. In: Infectious Diseases Related to Travel. Chapter 3. 2016: CDC website: www.cdc.gov/parasites/amebiasis
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nadia A. El-Dib declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Tropical Medicine in the Mediterranean Region
Rights and permissions
About this article
Cite this article
El-Dib, N.A. Entamoeba histolytica: an Overview. Curr Trop Med Rep 4, 11–20 (2017). https://doi.org/10.1007/s40475-017-0100-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-017-0100-z