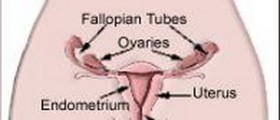
When there is an infected labia minora that is located on one side, the first thing that a gynecologist will think is some type of infection with the Bartholin glands that are located around the wall of the labia minora. Under normal circumstances, the Bartholin glands play a critical role in secreting fluids to help lubricate the walls of the vagina and are never seen because of their small size. Because of their close proximity to the wall of the vagina, however, they are also prone to infections and can quickly turn into a Bartholin gland cyst.
Women between 20 and 30 years old are at the greatest risk for developing a Bartholin gland cyst but even women after menopause are able to develop this condition. Women from minority backgrounds are more likely to get Bartholin gland cysts whereas women from white heritage are more likely to develop a Bartholin gland abscess. Women who have had multiple pregnancies are less likely to get this disease. [1]

The best way to tell if you suffering from a Bartholin gland cyst or abscess is the presence of pain. Cysts will be painless and only appear as enlarged glands. Unless you visit the gynecologist or self-check your vagina frequently, you may not be aware of having a cyst until the infection ensues. At this point, you have a Bartholin gland abscess and it becomes a more complicated medical management. When you have an abscess, you can expect to have pain during urination, unilateral swelling of the labia minora, and constant pain while walking or sitting. If the pain suddenly disappears, you can suspect that the abscess has ruptured.
These cysts and abscesses are generally caused by bacterial infections. As decades have passed, so to have the principle agents that can cause this type of infection. In the 1970s, most infections were caused by Neisseria gonorrhoeae and Chlamydia trachomatia, while more recently, this can be caused by Streptococcus and Staph infections. The most frequent culprit in modern society, however, would be simple E. coli infections. In single infections, E. coli is responsible 43. 7 percent of the time whereas in recurrent episodes, E. coli can be found in 57 percent of cases.
Now that we know what can be causing your pain, the treatment options are the next most important step. Depending on the severity of the symptoms and if it is still a cyst or has progressed to an abscess, your gynecologist can give you several different recommendations to proceed with your treatment. For simple cysts without any sign of infection, the standard of care is the Sitz bath. Women are encouraged to sit in a bathtub filled with a few inches of warm water multiple times a day for up to 4 days to see if the cyst will rupture on its own (the most desirable outcome).
In the event the cyst has already progressed to an abscess, surgical drainage may be the only viable solution. Patients will require an outpatient surgery where the doctor applies anesthesia to the surrounding tissue and makes an incision to drain the fluid. The fluid is then fully drained by curettage and antibiotics like Clindamycin are applied to the area. Studies show that this technique is more effective than the marsupialization techniques that were traditionally used. Patients will recover on average 5 days quicker and will have a reduced chance of recurrence of future abscesses. [2]
What you can do to limit your risk of developing this infection in the future would be to do ensure proper hygiene when using the bathroom. E. coli can be found anywhere along your urinary or colon canal and ensuring adequate cleaning of your vagina afterward is essential to reduce your chance of future infections. When wiping, moving from the front to back is an easy way to prevent cross-contamination.
- Photo courtesy of SteadyHealth