Estimated reading time: 8 minutes
Measurements of coronary artery calcium score (CAC scoring) are commonly used to assess future heart disease risk.
When we age, calcium deposits can be found in many parts of our bodies. Calcification in the arterial walls is common in people aged 65 and older.
![]()
So, to some degree, calcification of arteries can be regarded as a normal part of aging.
Due to their metallic nature and density, calcium deposits are easily detected by X-ray images.
Today, a heart scan, also known as a coronary calcium scan, is used to assess the amount of calcium in the coronary arteries.
Coronary Artery Disease
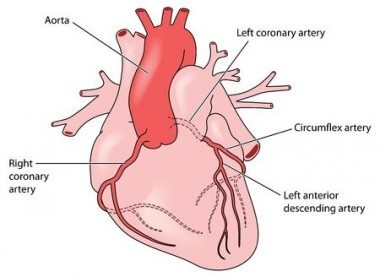
To be able to function normally, the heart needs a continuous supply of oxygen and other nutrients. The coronary arteries play an essential role in delivering these nutrients to the heart muscle.
Unfortunately, the coronary arteries are prone to a disease called atherosclerosis.
Atherosclerosis is a chronic inflammatory condition in which plaque builds up inside the arteries. A plaque is made up of inflammatory cells, cholesterol, calcium, and other substances.
Plaques in the coronary arteries may block blood flow to the heart muscle, leading to chest pain symptoms.
Furthermore, plaques may rupture, leading blood clotting at the plaque site. This may cause a sudden disruption of blood flow, leading to a heart attack.
In the early 1960s, several risk factors for coronary artery disease were defined. Since then, it has repeatedly been documented that smoking, high LDL-cholesterol, and high blood pressure are associated with increased risk.
Examples of other conditions that predispose to coronary artery disease are family history, insulin resistance, physical inactivity, mental stress, and depression.
Coronary heart disease remains the most common cause of death in the Western world. Hence, identifying individuals at risk is a significant step to reduce the burden of this disease.
Measuring the amount of calcium in the coronary arteries by CT scan may provide important information about the presence of coronary artery disease.
Coronary Artery Calcification
Most of us will ultimately get calcification in our arteries as we age. Hence, calcification of the coronary arteries can be regarded as an aging phenomenon.
However, if the amount of calcium is higher than expected by age, it may reflect an increased heart attack risk.
Coronary calcification can be seen in adolescents, although it usually starts later in life.
For many years, arterial calcification was thought to result from a degenerative process associated with aging. However, recent evidence suggests a more active process, likely arising from inflammation of the vessel wall.
Coronary Calcium Score
In the 1980s, US cardiologists lead by Dr. Arthur Agatston studied how to assess the amount of calcium in the coronary arteries.
Using an ultrafast CT scan technique, Agatston defined a method to calculate coronary artery calcium score (CAC score).
Initially, the CAC score was called the Agatston score,
CAC score is an important tool to predict heart attack risk and other vascular events (2).
Furthermore, it may help to detect the presence and extent of coronary artery disease.
Nonetheless, the CAC score does not reflect the presence or absence of blockages or impaired blood flow in the arteries.
Still, a patient with a high CAC score is more likely to block a coronary artery than a patient with a low CAC score.
An individual with a CAC score of zero is very unlikely to have a severe blockage of a coronary artery.
Coronary Calcium Score Interpretation
The following definitions are used to relate the CAC score to the extent of underlying coronary artery disease (3):
- Coronary calcium score 0: No identifiable coronary artery disease.
- Coronary calcium score 1-99: Mild coronary artery disease.
- Coronary calcium score 101-400: Moderate coronary artery disease.
- Coronary calcium score > 400: Extensive coronary artery disease.
When interpreting the CAC score, it is essential to consider age and gender. Women, in general, have lower calcium scores than men.
A calcium score calculator is available here that provides CAC score distribution based on age, gender, and ethnicity.
Using CAC Score to Assess Arterial Age
CAC score increases with age. Hence, at a certain age, we will be expected to have a specific CAC score that would be considered normal for that age. This score would then reflect the age of our arteries or the arterial age.
If everything is normal, we would expect our arterial age to be the same as our observed age.
However, if the CAC score is high, our arterial age may be higher than our observed age. Conversely, if our CAC score is low, the arterial age may be lower than our observed age.
The table below shows how arterial age can be predicted from the CAC score (4).
![]()
Let’s take an example.
A 60-year-old man has a CAC score of 500. According to the table above, his arterial age will be 84 years.
Hence, this 60-year-old man has arteries that are consistent with the arteries of an 84-year-old man.
Arterial age based on the CAC score can also be calculated here.
When Should CAC Scoring Be Performed?
Coronary calcium score guidelines don’t recommend routine use of CAC scoring in asymptomatic individuals (5).
However, the CAC score may be useful for individuals at increased risk based on the ASCVD score.
The ASCVD score is based on several parameters such as gender, race, cholesterol levels, blood pressure, smoking, and the presence of diabetes.
ASCVD score can be calculated here.
Hence, if ASCVD score is between 5-20 percent, CAC scoring may help to guide further therapy.
CAC scoring is not recommended in individuals with ASCVD risk below 5 percent.
How Is Coronary Calcium Assessment Performed?
Lately, ultrafast spiral CT has been used to assess coronary calcium. This technique, often called heart scan, makes the scanning time very short.
The patient usually needs no specific preparation. Fasting is not necessary.
As high heart rate may reduce imaging quality, patients are often asked to refrain from smoking and drinking coffee before the scan. Sometimes beta-blockers are administered to slow heart rate.
Many experts have expressed concerns about the radiation involved with the CT scan. It has been estimated that there may be an increase in cancer risk with repeated procedures (6).
What to Do About Extensive Coronary Calcification?
There is no specific treatment available that lowers coronary calcium.
Treatment of individuals with high calcium scores should aim at reducing risk. This involves treating lipid disorders, high blood pressure, and diabetes if present.
Due to the overwhelming evidence of benefit in individuals with coronary artery disease, treatment with aspirin and statins is often advised.
Refraining from smoking is essential, and regular, moderate exercise is advised.
Further evaluation may be needed if extensive calcification is present.
Coronary Calcium Score and Statins
Treatment with statins is often advised for patients with a high CAC score. This is based on their ability to reduce plaque size and improve clinical outcomes.
Interestingly, however, statins do not reduce calcifications in the coronary arteries. In fact, some studies suggest that statins may promote coronary calcification (7).
The fact that the CAC score is associated with increased risk does not prove that calcium itself is harmful. It is simply a marker of underlying coronary artery disease.
Patients with high CAC scores have simply had their coronary artery disease detected by the high amount of coronary calcium. The calcium itself is not the problem. Indeed, it has been suggested that the calcium may represent shrinkage and stabilization of plaques (8).
Statins are often recommended if the CAC score is above 100.
Conversely, statin therapy is not recommended in patients with a CAC score of zero.
The Role of Calcium and K2 Supplements
Inadequate calcium intake can lead to decreased bone density, thereby increasing the risk of osteoporosis and bone fractures.
Supplemental calcium can increase bone mineral density and bone strength. However, recent data suggests that high consumption of calcium supplements may increase calcification of the arteries (9).
Hence, it has been suggested that elevated consumption of calcium supplements may raise the risk of heart disease.
Vitamin K2 deficiency is associated with an increased risk of calcification of the blood vessels. Furthermore, researh indicates that the use of vitamin K2 supplements is associated with decreased arterial calcification (10).
Hence, increased intake of vitamin K2 might help to reduce the health risks associated with coronary calcium.
However, further studies are needed to establish the role of K2 supplements in people with high CAC score.
The article was initially published August 19, 2014.
It was revised, updated and republished on December 20th, 2020.
I had one of these done last year, 49 years old, score was 37, so I guess that’s pretty good. I had it done for my own personal interest.
Yes. 37 is great you fool. Stop eating sugar and processed foods.
Stop giving ridiculous advice.
Don’t knock a 37 at age 49. I sure wish I could have that.
A score of 37 indicates you will have a massive heart attack within 3 years so it looks like you have about one year left. Good luck!
Don’t listen to anything Jay Santos says… he is a troll.
58 and my score is 1178. I’m a dead man walking.
Not good. It should be no calcium present at 49. See dr
I got a 37 score at age 70. I asked my doctor if a zero score means a person doesn’t have to worry about plaque causing a stroke or heart attack. The answer was that calcium stabilizes plaque and you could still have soft plaque with a zero score and that is the type that could break loose and cause a stroke or heart attack. Also it is unlikely that any 70 year old male has no plaque in this country. My answer was that “now I don’t know what to wish for.” His answer: “Yes, we are all walking time bombs.” So I stopped thinking about CAC scores and just try to eat and live right.
I am 67 with a score of 0 !
I love this post PETER. There’s always something we could worry about isn’t there ? Health is a complicated thing.
I’ll trade you!!! I’m 74, asymptomatic, no blood pressure issues, slender, walk 5 miles most every day, never smoker, light drinker, but I have AFIB for which I take daily meds plus atorvastatin. No other health issues other than a family history of heary disease (father). My CAC score which I received online last week is a whopping 4253 with >90% blockage of my coronary arteries. Have an appointment with my cardiologist tomorrow to discuss results and options. Planning to review my will later this week. 🙂
I wish you all of the luck in the world. I’m 75 and the envy of my friends. I’m very mobile and also walk miles daily. My score was 926. I thought that it only went to 1,000. My ego balloon popped. I have been referred to a cardiologist and hope to hear from him soon. Good luck.
Good luck brother. I thought mine was bad. 11178 at 58. Stress test friday.
Your CAC score is high but it in no way indicates the DEGREE of blockage in your coronary arteries. Read through the literature. It might ease your mind.
I am curious as to your outcome, just saw your post today. My score 5 yrs ago 1540 and high LDL, high HDL, low Trigs. On Atorvastain 5 yrs and stopped recently. Am like you walk/run 5 miles plus a day, good eater/little processed stuff. What did your doctor say and what are you doing? Am on FB group with long discussions, quite interesting.
I’m 74 too. My CAC is “0.” Luck of the draw I guess?
CAC done at 70. I’m 74 now. My score was “0.” I think it’s the tequila, I donno.
So which is it – should we use statins to lower risk (with score under 400) or will it not have an effect on the calcification progression???
@ Edith Nir
There is no evidence thus far that statins will reduce the progression of coronary calcium.
The rationale for their use is based on the assumption that individuals with high calcium scores have extensive atherosclerosis, and the fact that statins have been shown to improve outcome in patients with established atherosclerotic cardiovascular disease.
I am being advised to commence “statin therapy”…strongly! using phrases like ‘The risk of death is greater than any other side-effects’, but I am far from convinced. I am 64; my CT Coronary Calcium Score was 3; my Carotid IMT Score was “1.1-1.3”; I am a non-smoker for the past ~30-40years; I am quite fit (swimming ~1km every day) to the point where the cardiologist was unable to stress my heart during a Stress Echocardiagram; and my diet is good, high in veg, fibres and fish with only token (perhaps once a week) red meat. Admittedly my Father died of a heart attack at 74, but I am a lot fitter than he was at my age. So…if there “is no evidence that statins will reduce coronary calcium”, why am I being so strongly pressed to take them, with all their recognized side-effects?!?
Thanks for the comment Don.
Although statins don’t appear to reduce coronary calcium, they may reduce the risk of future cardiovascular events. However, a coronary calcium score of 3 is fairly low and clearly below medium for your age. You can use the calculator here.
In order to see the whole picture it would be interesting to have some information on your lipid profile. Do you have high blood pressure?
Isn’t a score of 3 at age 64 VERY low? Top 25%?
Your health sounds fabulous. My doctor pushes a lot of tests and pills, too, and I keep telling him there is no heart disease in my family yet he acts like I might drop dead any moment. I am now taking statins which I resisted for years but I am diabetic and they think it has a correlation there to keep the blood sugar low.
What I am trying to do is find if there is a way to reduce these scores because mine was 61 and I am 72 but with low blood pressure and I exercise regularly.
Marilyn – you might want to remind your doctor that’s there’s no documented benefit for women to take statins and that people with higher cholesterol live longer on average than people with lower cholesterol after you reach the age of 50.
I’d send him this video and ask him why he’s never taken the time to understand the difference between relative risk ad absolute risk, why he’s never learned the difference between observational and randomized controlled trials.
https://www.youtube.com/watch?v=UCk_vTkS6bU
VERY INTERESTING!
I will tell him about this. Wish I could go back to my old heart doctor who gave me the stress test.
Thanks for taking the time to answer! I am very appreciative.
Any time. I get so frustrated by doctors whose first action is to reach for the prescription pad when the numbers don’t bear that course of action as prudent. The video is really good, not only does it explain the difference between relative risk and absolute risk but it tells you the true numbers on statins.
Long ago, when we went to a DO, we did not have that problem with the pills, but, gradually, they seem to have changed their thinking and are just as bad as an MD.
My 93 year old uncle was just put in the hospital for a very bad fall in a lot of pain but nothing broken. My 91 yo aunt kept telling them not to give him much in the way of pain pills because of his bad reactions to some of them. They wouldn’t listen and he was going absolutely insane with them. After about a week of them not listening to her, she called the family doctor who doesn’t use that hospital and asked him to intervene. Once he did and they stopped with all the meds, my uncle was his normal self again.
I did expect this video to touch on exercise and was disappointed it didn’t. I am off to discover the Mediterranean diet…thanks for that.
I actually almost didn’t post that video simply because of his endorsement of the Mediterranean diet – not because it’s much better than what a typical American eats but because there are many types of Mediterranean Diet (just look at all the countries in this area, all eating different foods) and it’s very confusing to try and pinpoint it. This doctor’s version is fine – meat, cheese, veggies and fruit – what he didn’t include in his description is whole grains, and I think that’s the key.
I am an unabashed advocate of a low carb diet. I believe the key to good health is to keep blood sugar at the levels that your body wants it maintained. In a normal person there is typically a teaspoon of glucose in the blood, roughly 3 to 5 grams. Every time you eat a meal full of carbs (and this includes whole grains), those carbs are meatabolized quickly and dumped into the bloodstream. A bagel is roughly 50 grams of carbs, that’s 10 times the amount of sugar that your body wants in the blood. Eating that bagel will spike blood sugar for several hours, eating a bagel or its equivalent at every meal will keep your blood sugar elevated all day long. Over time that causes a lot of damage, damage that occurs so slowly that people think it’s simply part of growing old. In the eyes of many, elevated blood sugar is the actual cause of heart disease (and cancer and Type II diabetes as well a host of other chronic conditions) – the way to beat heart disease is not to take a drug that lowers the very compound that’s trying to fix arterial damage (LDL) but to eat a diet that doesn’t spike blood sugar and causes the damage.
Here’s one more quick video that in anyone with an open mind should eradicate the notion that cholesterol is the culprit in heart disease. It blows my mind that health professionals still believe in this but they do. Fortunately with the internet we can do our own research nowadays and make up our own minds.
https://www.youtube.com/watch?v=TuxDuLKz39c&feature=player_embedded
Actually, the “Mediterranean Diet” uses little meat. Wikipedia has the standard definition:
“The Mediterranean diet is a modern nutritional recommendation originally inspired by the traditional dietary patterns of Greece, Southern Italy, and Spain.The principal aspects of this diet include proportionally high consumption of olive oil, legumes, unrefined cereals, fruits, and vegetables, moderate to high consumption of fish, moderate consumption of dairy products (mostly as cheese and yogurt), moderate wine consumption, and low consumption of non-fish meat and non-fish meat products.”
My family came from Southern Italy and that is what they eat and what I eat (and have all my life…except for when I was in college). Not all from the Mediterranean eat that way, but that is the standard definition.
This is the problem, Peter, few agree on what a Mediterranean Diet is. The French have one of the lowest heart attack rates in the world yet they eat a lot of saturated fat and nI’m pretty sure France is on the Mediterranean. Turks and Greeks don’t eat a lot of grains, mainland Italians eat a decent amount of pasta but also aren’t noted for a low rate of heart disease like the French. It’s confusing to say “Mediterranean Diet” as a catch-all phrase when it could mean a number of different things.
The doctor in the video I posted said “Mediterranean Diet” and then listed a number of good foods yet neglected to mention grains. Are you telling me that he should have said grains because that’s part of your understanding of a Mediterranean Diet or should we think that he only mentioned the specific foods he wanted to mention. I would say the latter.
Here’s the thing I think we can mainly agree on – pretty much any ancestral diet devoid of sugar is going to be better for heart health than the typical American diet. Now I would include with that foods that turn into sugar in your body because really, what’s the difference? If a carbohydrate metabolizes to the same substance (glucose), why would it matter if you ate in the form of cotton candy or a wheat tortilla? It’s all the same once it hits your gut. Pretty much any version of a Mediterranean Diet is going to be lower in sugar than the standard American diet but some are better than others due to the amount of carbohydrates you consume. You want to eat veggies and fruit, that’s fine. They’re carb content is generally low enough that you can’t eat so much that you’ll spike your blood sugar (although the fructose in fruit can be a problem). But you pasta or whole wheat bread and other stuff that easily converts to glucose in your body and you’re fooling yourself if you think it’s healthy. Better than a standard American diet full of sugar and processed foods but healthy, no way?
I eat few grains these days. A little pasta. Italians don’t gorge on pasta in Italy. I have found the most important thing to keep blood sugar stable and low is eating 5 small meals that include protein. Carbs without protein make blood sugar fluctuate wildly.
I believe our problem stems from our food that is filled with hormones, antibiotics that ruin the flora in our digestive system, GMO’s ,foods that are modified with roundup to resist pests along with msg that is in every packaged product , fillers, colorings, artificial sweeteners, corn syrup which our digestive system cannot metabolize and the list goes on and on.The difference in Europe is they don’t allow these toxins in their food supply. This is where our inflammation comes from. It is about time we demand that our food is free from these poisons and we will see our heart disease, diabetes celiac, all the digestive issues we have etc , will be lesser and our health would greatly improve.
Most of the elderly in France who don’t have as many heart attacks went through the war with very simple foods. They didn’t get cream, butter, etc. They didn’t get the rich pastries that the French eat today. You’ll need to see how he newer generations fare.
Actually the French consume the highest amounts of fats from a variety of sources of any nation. AND, they have the lowest rates of cardiovascular disease.
Therefore the “French Paradox”. The Swiss are right behind them with regard to both dietary fats and low risk of CV disease.
This is incorrect advice. There is a fair amount of data that women without coronary disease may benefit from taking statin therapy. The data is not as robust as it is with men but thousands of women have been enrolled in statin trials and there is significant evidence that women may benefit.
https://www.medscape.com/viewarticle/814526#vp_2
JUPITER was a terrible study – it weeded out everyone except for those with high C-reactive protein scores AND normal LDL-C scores. Just by this the results from JUPITER can only be applied to people who fit both those conditions, which is quite rare. I’ll repeat this because it’s pertinent – you cannot apply the JUPITER study results to people who didn’t have levated C-reactive protein and noral LDL-C.
And just look at the name, it stands for “Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin” – do you think with a name like that there was any way that Astro Zeneca wasn’t going to come up with a positive result for this? And then there’s the typical use of relative risk scores (a statistic only a propagandist would love) as opposed to using absolute risk. Using a relative risk score tells us nothing about how effective this treatment is. Relative risk was used because the differences in asbsolute risk were tiny. There’s actually more fishy stuff about JUPITER, you can (and should) read more about it here if you want.
https://proteinpower.com/drmike/2008/11/10/1853/
Your use of the phrase “fair amount of data” is troubling if you think that a single poorly done study is a “fair amount of data”.
Here is a good review for you about statins in women that contains multiple meta-analyses of the many trials with statins having women in the trial.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709236/
Their conclusion:
“For primary prevention, statin therapy reduces major CVD events in men and women, but we can debate whether it reduces all-cause death, especially in women.”
That is where the debate is, whether statins reduce all cause death in women, not whether statins work at ALL in women.
As far as the Jupiter study, it was a rigorous, randomized control trial. The data were clear, there was a mortality benefit for those with normal LDL and elevated CRP. Elevated CRP, a risk factor for heart disease, is common in the millions of Americans with metabolic syndrome, these people may benefit from a statin. To claim that those with high LDL and high CRP should not be treated because they were not included in the study is disingenuous and somewhat silly. It would be the equivalent of doing a trial that showed that treating blood pressure with hypertension meds in patients with blood pressures from 150-160 reduced strokes but then claiming that we shouldn’t treat those with blood pressures of 180 because they were not included in the trial.
I hate being dismissive and rude to people but your lack of critical thinking is pissing me off. You’re not even trying.
Let’s look at JUPITER again. This was a trial that only included people with normal LDL-C. Statins are supposed to be effective because they lower LDL-C, why would anyone take a statin when they have normal LDL-C? Why would this study even be done unless the group financing it knew that LDL-C wasn’t the problem? And you’re saying that elevated CRP is a risk factor for heart disease – that’s a new one on me. Doctors don’t even test C-reactive protein. Now I happen to agree that elevated CRP is a bad sign but the best way by far to lower CRP is to go on a well-formulated low carb diet. And you obviously didn’t read the link I posted about JUPITER otherwise you’d have serious doubts about how rigorous it was. I can’t make you read it but it’s boring to have you insist that it’s a well-designed trial when it’s clearly not.
And then indicating that all-cause mortality is irrelevant is just stupid. You seem to be saying that people lowering their risk of death from a heart attack by an infinitesimal amount is preferrential to dying from some other cause while also subjecting themselves to the side effects that statins cause. Your logic is not flawed, it’s simply non-existent.
And why not man up and post under your real name instead of posting anonymously. How do you expect to be taken seriously when you hide behind a pseudonym?
Here is some info on CRP and heart disease.
https://www.webmd.com/heart-disease/guide/heart-disease-c-reactive-protein-crp-testing
The Jupiter study was set up the way it was because many other previous trials had shown benefits of statins in patients with high LDL. If they had set up the trial in patients with high LDL and high CRP and shown a benefit it may have been just because the LDL was lowered. But the designers of the trial wanted to show that there could be a benefit of statins even in patients with normal LDL, which was an ambitious goal. And they achieved that goal. This expanded the group of patients that may benefit from a statin.
A healthy diet may lower CRP levels. But it is hard for most people to stick to a healthy diet. And while CRP is a risk factor for heart disease, it is still unclear if lowering CRP levels will reduce cardiac events, the CRP may just be a marker of increased risk. Correlation does not equal causation.
I never said all-cause mortality is irrelevant. I just said that the data were unclear if statins reduced all-cause mortality in women without established heart disease. This doesn’t mean that they don’t, the jury is still out. But while that question is being answered many women with increased risk of heart disease can reduce their risk of having a heart attack with statins.
Should I take statins for a hangnail too? I have a toothache, perhaps some Crestor will take care of it
This is pathetic. You’re making claims that statins are providing these great benefits (they’re not) and you completely discount the possible side effects.
This had me rolling – “But it is hard for most people to stick to a healthy diet”. You make it sound as if eating poorly can be counteracted by taking drugs. It doesn’t work that way. You get on those drugs and you never get off them because they don’t provide a cure, they simply lower what we’ve misidentified as a risk factor. How likely do you think it is that over our evolutionary period our bodies have evolved to create a substance (cholesterol) that will kill us? The chance of this happening is zero. Our bodies increase the production of cholesterol because our diets (high carbs) are causing chonic damage and inflammation and cholesterol is the building block for repair.
I’m getting bored with this conversation. If you think that statins are a great thing then by all means take them. Take lots of them, you have my blessing. It’s just that you’re doing yourself a great disservice by ignoring the difference between relative risk (meaningless) and absolute risk (meaningful), that trials like JUPITER are not well run and don’t show what you think they do or even that low carb diets are difficult to adhere to. I’ve been low carb for 5 years now, here are my lab results from a month ago.
Trigs – 56
HDL – 66
Fasting glucose – 86
Total Cholesterol – 217
LDL-C (calculated) – 140
Vitamin D – 65.8
Fasting Insulin – 6.9
I hesitated to include the LDL number because with a standard lipid profile it’s a calculated number using the Friedewald Equation which is notably inaccurate when triglycerides are under 100 (which mine are) or over 400. But I don’t actually believe LDL-C is relevant as a risk factor so I wouldn’t care if it was actually 140. To me the best marker determined by a standard lipid test is the TG to HDL ratio (which our host has written about before) with anything under 2 being good. Mine is well under even that.
So having lived a low carb lifestyle for many years now seeing the effects firsthand (no longer asthmatic) I hate the idea that people are taking drugs like statins because they believe there’s some benefit to them. It’s sad.
No, statins will not help with a hangnail. But they may help with a toothache. Periodontal disease can cause inflammation which may increase CRP levels — leading to an increased risk of heart disease.
Why are you on a low carb diet, are you trying to lose weight? Low carb Atkins or Atkins like diets can be good for weight loss but for reducing the risk of heart disease, -which was the point of this article on coronary artery calcium, they may not be great. Mediterranean diets or Ornish diets have more data showing benefits in preventing heart disease and in patients with established heart disease.
https://health.usnews.com/best-diet/mediterranean-diet
https://health.usnews.com/best-diet/atkins-diet
Here is an article from Harvard questioning the use of a low carb Atkins diet in people with heart disease and recommending a Mediterranean diet instead.
https://www.health.harvard.edu/staying-healthy/low-fat-low-carb-or-mediterranean-which-diet-is-right-for-you
Dude – you have no idea what you’re talking about, please stop (actually please continue, you amuse me with this stuff). I’m on a low carb diet because I want to be as healthy as possible and as you can see from my lab results that’s exactly what I am. And while I have no need to lose weight I did lose 35 pounds once I ditched the carbs. I suppose that was all water weight?
Your Harvard link is a joke – not only does Harvard put out some of the most questionable observational studies on nutrition out there but in this case instead of citing an actual study they’re quoting the American Heart Association, an organization that pimps itself out to the drug companies.
And US News? What, couldn’t you find any links to Yahoo or Huffington Post?
The more you write the more it’s apparent you’re only interested in a surface level examination of the data. That’s fine. Go ahead and eat your whole grains, watch that salt intake and follow it up with a big dose of statins. I simply don’t care. And if you’re going to reply again please do it with something better than US News and WebMD. Feel free to quote Harvard though, I love showing where those brainiacs like Frank Hu and his saturated fat witch hunting gang get it wrong.
You like being contrarian. And that is ok, even good every now and then. But if you are obstinately contrarian on every issue you will find that you are on the wrong side of the facts more often that not in life.
Your views on statins and diet are very fringe and radical. With the evidence known about heart disease up to this time, I would strongly recommend that anyone with heart disease not follow your ideas.
I am a contrarian when the available data indicates that the best course of action. I couldn’t care less how many and who believes it to be true if the data doesn’t agree. There are countless things where I agree with the conventional wisdom because that’s what our best information indicates. Nutrition and drug therapies for chronic disease are simply areas where the conventional wisdom aren’t backed up by the data and I’ve adjusted my beliefs accordingly. My own pesonal experience has shown me this to be correct.
Just look at your arguments on this thread – you started out citing the JUPITER study (which unbeknownst to you at the time doesn’t even touch on the lipid hypothesis – it’s actually a study about inflammation) and your arguments got weaker with each comment. In the end you were flailing with citations from WebMD and US News & World Report. If you can’t see the problem with that then perhaps you should ponder that for awhile.
The problem with people is that they (including myself) are all subject to basic human failings like confirmation bias and needing to avoid cognitive dissonance. We become so emotionally invested in our beliefs (“What, me wrong? No way!”) that evidence that goes against our beliefs is dismissed as propaganda or the person presenting it is said to be a lunatic. We will only believe evidence that supports our position and evidence to the contrary is dismissed. I know this because I’ve done it myself in the past and I work very hard to make sure I don’t do today. The great physicist Richard Feynman said “First, don’t fool yourself because you are the easiest person to fool”. This goes for everybody, you need to constantly examine your beliefs and ask yourself “Am I fooling myself? Do I have data to back up my beliefs? Is my interpretation of the data solid? What could I be missing”? Very few people have the ability to say “I was wrong and you were right” and that’s a huge problem. It’s why we get locked into bad science and bad policy for decades even when it’s obvious that the science is wrong and the policy isn’t working. That’s how we get into the situation where researchers say “Well obviously our cholesterol recommendations are low enough yet” or “More people need to be on statins” or “You need to cut your saturated fat even more” or in this particular case “Your views on statins and diet are very fringe and radical”. My views on diet and statins are fringe and radical only if your mind is solidly made up and you ignore evidence to the contrary.
I was like you at one point. I was sure I was fat because I ate too much and didn’t exercise enough and I spent years trying to eat less and move more and the end result was I was still getting fatter. I was frustrated and that was probably good because I was finally ready to hear an alternate viewpoint. And the rest is history. I realized that a lot of what I believed wasn’t based upon solid evidence or any evidence at all. Believe me, it’s hard as heck to admit that your belief system was awful and that everything I’d ever learned needed to be questioned and re-examined. I hated the idea that I’d been stupid for years but I got over it when I understood that everyone does it. I feel fortunate that even though it took me 40+ years to get it, I finally did get it. Most people don’t and they’ll sadly go to an early grave with diminished quality of life because of it.
“I am a contrarian when the available data indicates that the best course
of action. I couldn’t care less how many and who believes it to be true
if the data doesn’t agree.”
Any fool can cherry-pick studies from the millions available on PubMed, to prove their point. Gary Taubes is a classic example of this.
Doing science properly means looking at all of the evidence, not just the evidence that reinforces your confirmation bias.
Bob, you are a rock star. We LCHF people are certainly the current outcasts in this era of ADA and AHA guidelines and behind the scenes big pharma. Hey if you’re A1C/ LDL is too high here are expensive drugs to take/ inject- (never mind (good) diet). #bigpharmawantsyoufat
I’m with you brother.
Thanks Ted – Not only am I a big fan of LCHF to regain your health but I’m also beginning to think that a combo of LCHF and intermittent fasting is about as healthy an approach as you can get. We will see what kind of research comes out as time goes by.
“I’m on a low carb diet because I want to be as healthy as possible and
as you can see from my lab results that’s exactly what I am.”
You’re on a low-carb diet ‘cos you’re too stubborn or stupid to reverse your insulin resistance. Your surrogate markers are meaningless on a high-fat diet.
You ditched over-refined nutrient-poor, calorie-rich food products for nutrient-rich, calorie-poor produce. That’s what improved your health, not the carb reduction. You’ve fallen for the “cum hoc ergo propter hoc” fallacy.
So I am sure you also agree with Bob that statins suck…right?
Generally agree with your view that A. statins not terribly good therapy, and B. the studies re: statins are poor to terrible (not to mention the data is juggled and manipulated with by the Drug Company hacks).
Re: anonymity…proud tradition of several of our Founding Fathers.
The link you provided is to be taken with a grain of salt. It’s a WEBMD site and they pretty much tow the line with big pharma. That’s who funds them.
Bravo.
@Marilyn Z: If you are diabetic you should try to keep your blood sugar in check, that is lower than 140mg/dl (120mg/dl) at 1 hour (2 hours) after meals.
I would read the two other most relevant links to Jenny Ruhl’s work too.
Misdiagnosis By Design – The Story Behind the ADA Diagnostic Criteria and How Blood Sugar Control Works–And How It Stops Working.
Under an unhealthy diet normal can be unhealthy. Everyone should check his/her postprandial blood glucose after most usual meals and act accordingly.
Finally, if you decide to stop statins (they cause diabetes) then do it slowly.
Thank you for that reminder. I remember reading that statins cause diabetes and had forgotten that. How do you stop slowly? Space the pills farther and farther apart?
I am new to this diabetes thing and my AVERAGE is 130 per wk. I have no idea what I am doing with it. I made some pretty bad tortillas to use as wraps and those got me thru until I found some wraps that are 7 gram net carbs and really love those.
I heard that COLD dishes with potatoes or pasta do not work as starch in the body, but merely as fiber, but I can’t find any studies to verify that. Has anyone else heard that?
120mg/dl after 2 hours is a bit low from checking my records so I will need to be more vigilant. I have found that fruit is a no no and I miss than more than anything.
The first article was a lot to digest and not encouraging,but helpful. I understand blood glucose a bit more and am even more determined to keep down.
I completely agree that keeping blood sugar in check is a very desirable goal, I differ from Andrés on the numbers though. I think the clinical blood sugar targets are high by quite a bit – I would avoid all foods that raised them over 100 mg/dl (fully understand that this is my own belief and not supported by most).
Something else to consider is that Type II diabetes is a disease brought about by the body producing too much insulin and not necessarily due to high blood sugar – groups like the ADA say to eat a carb-filled meal and then cover the blood sugar with injected insulin. They say that T2D is a chronic disease and will only get worse over time yet I know of many people who disregarded the ADA advice and now need no meds nor injected insulin.
The key to controlling/curing Type II diabetes is to (A) not eat foods that raise blood sugar and (B) not eat foods that stimulate insulin production. These two things are subtly different – carbohydrates are highly insulinogenic, protein is also to a lesser extent and even fat is a little bit. I’ve become increasingly swayed by the work of Dr. Jason Fung who is having success with his patients by putting them on a low carb diet along with a program of intermittent fasting (IF).
The key to intermittent fasting is that if you’re not eating at all, you’re not producing insulin that is worsening your T2D. Additionally IF produces a number of benefits like increasing your natural production of growth hormone and promoting cellular autophagy (the process where cells perform housekeeping and get rid of toxins that have accumulated). It’s sounds like magic but there have been many studies done showing this. I do a IF regimen where I only eat during an 8 hour window each day meaning I go at least 16 hours per day where I’m not eating and I’m not stimulating insulin production.
This is probably a lot to take in all at once – I’ll post a video by Dr. Fung that will do a better job explaining how the ADA gets T2D treatment wrong.
https://www.youtube.com/watch?v=oFJ5Sv5ifes&feature=youtu.be&a
I am 74 and had open heart surgery at 68. Fully recovered now. Diet is a personalized nutrition plan from Metabolic Balance (loricassidy.com) and all my lipid numbers are below the goal numbers my Lipid Doctor set for me when he said we were going to treat me aggressively. I am on Crestor 10mg, zetia, and berberine. My C-Reactive Protein is .02 which is very low (this measures inflammation). My ejection fraction is 59 up from 25 at the time of my surgery. I am living at my ideal weight and feeling better than ever and active in sports I love — golf, skiing, swimming, weight lifting, etc.
My understanding is that statins can contribute to diabetes occurring, not the opposite.
Don’t take their statins , Don. Run, don’t walk from that doctor. You are perfect not only at your age, but at ANY age!!!
Thanks Rita. Some further reading and (of course!) this forum lead to rejecting the statins and giving that doctor ‘the flick’, but it’s funny how that sort of experience leaves lingering doubts. We (or at least I!) tend to view the medical profession on a pedestal and it’s unsettling, in many ways. when evidence appears that pedestal can be very tarnished.
Because the pharm. companies make lots of money off of these drugs.
Because BigPharma like to profit off you. 50% of heart attack victims have “normal” cholesterol numbers. What a joke. Watch the ABC Australian documentary Heart of the Matter.
Last time I checked there weren’t any cardiologists roaming the internet answering health questions. In other words, quit typing and make an appt. with your doctor NOW.
This review may be useful to some readers of this article.
Vitamin K Dependent Proteins and the Role of Vitamin K2 in the Modulation of Vascular Calcification
I think it’s also worth considering the synergistic roles of magnesium and Vitamin d working together with the actions of Vitamin k. Vitamins D and K as pleiotropic nutrients
Thanks for the links Ted.
I really enjoyed reading the review on K2. Its promising role for preventing or modulating vascular calcification is of great interest.
The question whether the anti-inflammatory effects of vitamin K and vitamin D may be important when it comes to preventing vascular calcification is also of great interest. Both these nutrients appear relatively safe and they’re certainly not expensive.
For an easier read about the connection between vitamin K2 and calcium in the body, try “Vitamin K2 and the Calcium Paradox: How a Little-Known Vitamin Could Save Your Life” by Kate Rheume-Bleue. I found it very interesting and informative.
https://www.amazon.ca/Vitamin-K2-Calcium-Paradox-Little-Known/dp/1118065727
did it work
It’s not clear what CT measuring of arterial calcification really means. Is it the measurement of the length of arterial vessel affected by calcification? Or is the measurement of arterial narrowing from calcification?
If one has a score that puts them at the 50th percentile for their age/sex, then how frequent should CT technology be used to monitor the progression? Every year? Every 3 years? ???
@ Jkart
Coronary calcium score reflects the total amount of calcium within the walls of the coronary arteries, taken together to provide a single number. It’s based on density and area.
Coronary calcium score tells you nothing about arterial narrowing. One can have a high calcium score without any narrowing or blockages being present. However, a patient with high calcium score is more likely to have a significant narrowing affecting blood flow than a patient with low calcium score.
Regarding your last question the only thing I can tell you is that nobody really knows how to use coronary calcium score in clinical practice. Whether, or how often progression should be monitored is still a matter of debate.
Thanks for the clarifications. For whatever reason, it was in my mind that the calcium score was directly related to the level of vessel blockage.
Then why in the world has my doctor been after me to get one for the past three years? There is no heart disease in my family, at least within a generation or two. I think he means well, but I get so tired of being sent for tests when my blood work is great other than my cholesterol scores.
I had VERY high cholesterol numbers for many decades. As I am asymptomatic with no heart problems, dont smoke, no high BP and am athletic, I resisted taking Statins. BUT – after a calcium score test which revealed thta I had extensive calcification, I decided to take statins – to reduce my chol levels down to what the cardiologist wanted to see. I have no idea whether this is doing me any good , but I am still fit, asymptomatic and athletic at age 74.
I have since submitted to going to a heart specialist and really loved this guy. He put me through all the tests and I passed quite easily…the stress test was a breeze. Anyway, to what you were saying about high calcium scores, this doctor told me he has patients with scores as high as 5000 (yes 5 with FOUR zeroes) and their hearts and arteries are perfectly fine.
I am beginning to wonder if my doctor gets a kickback for sending me for unnecessary tests. As it is, I quit that doctor and found a young female osteopath, but the jury is still out on whether she will be better or not. My former doctor was in the same high school band as my kids so I think I stuck with him too long for that reason.
Thanks for the post Axel. In our reports Volume130 is also reported an it is suggested that it be used to measure progression from year to year rather than AJ scores.
There has been some debate regarding the essence of calcium scores and its ability to predict risk.
Glad you posted because I wanted to discuss with you. Comments?
Jeff
Thanks Jeff
I think there are several things to discuss and many unresolved issues when it come to coronary artery calcium score (CACS).
One thing worth mentioning is that CACS is probably not very useful as a diagnostic tool. By that I mean that if you have a patient with chest pain, breathlessness or other symptoms, you’ll have to use other methods such as exercise testing with or without nuclear or echocardiographic images and then, if positive,coronary angiography.
I don’t think CACS is a useful screening tool for large parts of the population. In that respect, it’s probably not cost-effective. Radiation is involved and there are cheaper methods available.
However, CACS may be helpful when assessing individuals at intermediate risk. There may be situations where you’re wondering whether to treat with statins or not. If there is extensive calcification, you might want to recommend statins while on the other hand, if there is no calcification, risk is low (even in the case of high LDL-cholesterol) and you might want to refrain from statin treatment.
What’s your experience in Denver and among general practitioners in the US? Is CACS being used to assess risk?
Axel,
In the US insurance is not paying for CACS, this usually means that insurance concludes that it does not provide useful information. However, many pay out of pocket for the screen and I agree as you stated above there may be some usefulness.
We do CIMT’s with limited doppler in our office as a competing technology. I am not sure itima thickness correlates with risk but I like to visualize plaque. I suppose that using these tools in the right context can be useful.
Jeff
Insurance companies care about your health? LMAO
I truly think mine does. They give me *rebates* for getting mammos, colonoscopies, annual checkups and a few others. This year I should get $70 from them plus they call and make sure I am refilling my prescriptions and getting my flu shots, etc. If I stay healthy, it is less outlay for them. Makes perfect sense to me.
They will not pay for the CACS though….stupid me, I paid for it myself.
I suspect a calcium score will turn out to have a practice value other than measuring it like the length of a fuse on a time bomb, and having no treatment to stop this progression. If a person has a high score and angina/significant block, then surgical treatment might be more indicated, as compared to same person except low calcium score. This person might respond better to medical treatment, ie statins, etc. bottom line, use it to help decide surgical versus medical treatment of coronary disease.
John.
That’s a hypothesis that is still to be tested.
I don’t now of any evidence so far suggesting that calcium score is useful when deciding whether to go for surgery or medical therapy. Usually these decision are based on the number of arteries with significant narrowing (stenosis) assessed by coronary angiography, the localization of the narrowings and the extent of myocardial ischemia.
I would appreciate any comments/advice from the experts on this blog. I am a 62y.o. male at 5’11’ and weigh 213 lbs after losing 20 lbs since Feb 2014 and have started exercising and cycling regularly since March of this year. I plan to lose another 20 lbs. I have mild asthma and take asmanex 220mcg
2 puffs daily. BP is well within normal limits. In Sept. 2000 I had aCAC of 11. LMA: 0, LAD: 9,CFX: 0, RCA: 2. IN 2007 I had an angiogram due to a thallium stress showing a possible problem but cardiologist thought was false positive. Results of angiogram was RCA – mild diffuse disease , left main – no disease, lad proximal <30%, Mid < 30%, D1 no obstruction, Lcx – no obstruction. No treatment rendered. After blood workup my cardiologist put me on 20mg of lipitor. I have been on 20 mg lipitor since early 2008.
Now for my concern, Sept 5th I had a stress echo. Negative findings except for showing pac on exercise. His concern was that the width of pvc ( recovery period ) was wider than usual. I am asymptomatic on 24 mile road bike trips and exercise. Sometimes on strenuous exercise take pulse and feel extra beats every 8 – 16 beats.
The kicker here is that I had a repeat CAC score November, 2013. Cardiologist told me via email that it was significantly higher, but nothing to worry about and didn't give me the number. Recommended stress/echo which I took my time about. At office visit I asked for test result, what a shock. Total CAC score 1693. LM- 0, LAD- 1141, D1 – 37, CX – 27, RCA – 488, PDA – 0. This shook me to my core. I questioned my cardiologist who is well respected in NYC and he assured me not to be worried. Told me about studies showing Lipitor helps soft plaque become more stable by hardening it and this causes deposition of calcium causing higher score. I have searched internet for this phenomena and found nothing but came upon your blog.
My cardiologist reiterated over and over not to worry but to be on safe side and not for elevated CAC score but for exercise induced pvc width referred me for a virtual angiogram ( cat of heart).
Needless to say, I am extremely concerned about the CAC score which is virtually off the charts.
Any recommendation/clarification you can give would be greatly appreciated
Don A.
Some studies have suggested that there is an association between statin use and coronary artery calcification. Furthermore, there is no evidence that statin treatment halts the progression of coronary calcification.
However, this does not mean that statins accelerate the progression of atherosclerosis. In fact, as your cardiologist suggested, calcification of plaques may indicate healing. In theory, a calcified plaque may be more stable and less likely to rupture than a non-calcified plaque.
It is possible that there are different mechanisms behind coronary calcification and coronary artery narrowing. In one meta-analysis, coronary calcification was not affected by statin therapy although there was a consistent moderation of progression of coronary artery narrowing with statins.
Thanks very much for your reply (22 Oct at 08:22) Axel. I am answering here because there was no “REPLY” link in your reply.
I should admit I am feeling way ‘out of my depth’ here. My understanding of all this feels incredibly superficial. My instincts tell me I am in good health and I should seek another opinion before I embrace statin drug therapies, but I live in a country area where specialists are few and far between. So your blog (and, even more so, your input re my circumstances) is hugely appreciated…and I will do my best to answer your questions…
My blood pressure is “120 over 80” and my Serum Lipid studies appear as follows:
Cholesterol 6.5 mmol/L
Triglyceride 0.8 mmol/L
HDL Cholesterol 1.5 mmol/l
Cholesterol/HDL-C Ratio 4.3
VLDL Cholesterol 0.4 mmol/L
LDL Cholesterol 4.6 mmol/L
My other details are in my earlier (22 Oct at 00:29) Comments.
Don.
Although your LDL-C is rather high there are positives. Triglycerides are low and so is TG/HDL-C ratio. This is an indirect sign of LDL-particles being large rather than small which is positive.
Generally speaking statins lower the risk of cardiovascular risk. When the risk is low, like it appears to be in your case (coronary calcium score of only 3, not smoking, no hypertension and regular exercise) the likelihood of benefit from statin treatment is probably very small.
Thanks Axel
Your comments are reassuring, not only because they appear to confirm my instincts, but also and especially because they give me another independent and very expert source that is looking at (at least some of!) my particulars.
My current cardiologist appears to be relying heavily on the Carotid IMT results. He suggests that those results effectively forecast a deterioration in my coronary calcium — His words were along the lines of ‘There is now a sludge, rather than hard calcium in my heart, but soon (as in the next couple years) the thickness in my carotid will be reflected by hard calcium in my heart’ — which made me a strong risk of heart attack or stroke within the next few years…all of which could be solved by “taking a little pill”. He also suggested I was now at a point where the process flagged in my carotid results could be reversed (by statin therapy) BUT once it moved on to the next phase in my heart, nothing could then be done.
My readings about Carotid IMT results are mixed. Not surprisingly, they confirm some of what my cardiologist is saying, but it also appears (to my VERY amateur understanding of the technical articles!) that there is confirmed thickening of the carotid with age anyway and the exact, age-adjusted risk range of results is not clear; that, plus there appears to be some uncertainty in the consistency of those results, leads me to pause at the suggestion that my results point without doubt toward statins for me. What is your ‘feel’ for Carotid IMT results? in general, but more importantly in my particular case with results of (in the cardiologist’s words as I did not actually see the results) “1.1 to 1.3”?
Then further, when I hesitated at the direction toward statins, the cardiologist went on to suggest an angiogram, with the prospect of the insertion of stents as a preventive measure. I believe I understand this process, but again it seems to me to be unwarranted by my current state of health?
Don
Unfortunately I have very limited experience with Carotid IMT.
I’m also reluctant to go into much detail regarding your health. That would be irresponsible of me. The only thing I can do is discuss these issues in general terms as I did in my previous comment.
Of course I think you should listen to your doctor. I have no doubt he wants what’s best for you. However, the question when to use statins is often difficult to answer and experts don’t always agree.
I am a 60 year old male. My cholesterol is and has been low for 30 years (with statin). I exercise regularly. My blood pressure is normal and I am in excellent physical condition-low body fat- no lipid issues Went for a Calcium score which was 426. Which falls under extensive cardiovascular disease. Any comment or suggestions
Rich.
A calcium score above 400 implies that your risk for having a cardiovascular event is elevated. However, it doesn’t imply that you have any significant narrowings/blockages in your coronary arteries. Sometimes other tests are performed to check for that.
I think you should focus on limiting your risk by not smoking, eating healthy and exercise regularly (which you already appear to be doing). In my opinion there’s no reason to stop the statin treatment. Although statins don’t appear to affect the calcifications per se they may help lowering your cardiovascular risk.
Discuss with your doctor whether he believes further testing is needed.
Thank You for your response. As a follow up to the calcium score I had a nuclear stress test and was told the result is “normal”.
I don’t know what that means. Since a score of 426 means “severe cardiac artery disease” (where I was)……does a “normal” nuclear stress test mean I don’t have “severe cardiac artery disease”. Just feel like I have no idea where that leaves me.
Rich
I presume the nuclear stress test shows that blood flow to the heart muscle is normal which indirectly suggests that there are no blockages/narrowing in the arteries affecting blood flow.
But, keep in mind, this is only my presumption based on the limited amount of inormation.
Your doctor should be able to explain it all to you.
I just received the results of my calcium scoring test. I am 44 years old, 100 pounds overweight. My cholesterol is “borderline”. My calcium score is zero. Does this mean that cholesterol isnt a problem for me, or just that it hasn’t effected my coronary arteries yet? Considering my weight, high blood pressure and eating habits, I was surprised to have such good results.
Andy
That’s good news. However, remember that you’re quite young. A calcium score of zero is fairly common at your age. I think you should do what you can to improve your lifestyle and try lo lose weight.
Hi,
Quick question….I just had a Calcium screening test done last week. Im 42 years old. All my vitals are good BP 110/60, cholesterol in normal range. My HDL has always been a little borderline low (42). Anyway, my Calcium score was 7. Id never even heard of Calcium scoring before this so im a little nervous and unsure what this all means. From what I know 7 is low, but perhaps not so low for my age. Im confused. Any light you can shed would be great. My Doctor and I are supposed to talk about beginning statins, but i feel uneducated on this whole thing. Am I code red? or am i over reacting?
Scott.
No I don’t believe your code red and as I see it you’re probably overreacting. I just wonder why you had a calcium score performed. In fact I think there’s limited data available for your age group. Anyway, a score of 7 is low. The sensible thing is to discuss the findings with your doctor.
Thanks Axel for the reply. That makes me feel better. To answer your question about why I had the test done…..Last weekend I had a very uncomfortable feeling in my chest, so after no relief for 12 hours I went to the Emergency Room where they did every test under the sun….EKG, Echocardiogram, x-rays, blood panel etc. It turns out that I have Pericarditis which im finishing up my treatment for with Colcrys. Feeling much better. So in running all those tests the calcium score was something they picked up in passing. I went to my primary care physician this week as a follow up and he strongly recomends I start a Statin. To me that sounds like a big deal so it got me a little worried which made me question how serious my score is or isnt.
7 is not a low score for someone your age. I’m 42 and mine is 14. At our age it should be 0. The key is to do anything you can re; diet , exercise, etc. to keep it from progressing. We are too young to have this score. So whatever we are doing needs to change. Inflammation, eating processed and fatty foods, lack of exercise, etc. will do this. So yes, a score of 7 may seem low but if you continue doing whatever you are doing then it will increase and will be very bad. Be careful and be well.
I guess my main worry wasn’t so much in the current score of 7. It was more because my understanding is that if you have a positive calcium score, even if its low at the moment, will continually increase to a significant # as time progresses. Thats what my confusion and sort of worry is.
I understand Scott. However, it’s very hard to tell how and if arterial calcifications will progress. You may still have a score of 7 after ten years although it’s likely to be higher just because you’ve aged.
Take this as a positive thing and tune your lifestyle so you may be able to reduce the likelihood of future disease.
Thanks Axel, thats comforting. Are there any lifestyle tips you can give me. I plan to up my cardio vascular exercise. I’ve mainly mostly done only weight training with a little cardio mixed in. As far as dietary are there things that are most desirable to eat aside from the obvious, staying away from bad fats and simple carbs.
Im also very confused about the statin thing. My Dr wants me to start it. But ive read so many conflicting things about the side effects and being only 42 years old, i feel that if I were to be on them now, that it would be a lot of years ahead of me for those side effects to happen as opposed to if i was 70 years old now. I kinda would like to know if lifestyle changes and habits at my age and score would be something to seriously consider as opposed to a life commitment to statins
Scott
Your reasoning is sensible and rational. When prescribing statins it’s important to be sure that the benefits outweigh the risks. Most people tolerate these drugs very well, even for long periods.
Of course you should focus on lifestyle issues. The question is whether statins will bring additional benefits. Your blood lipids, family history and other risk factors will have to be taken into account. Discuss the pros and cons of statins with your doctor. This is where shared decision making (between you and your doctor) is important.
I am 62 and my score just came back and is 912 and it was 800 three years ago. My cholesterol is 106 and labs are excellent, my stress test is wonderful I exercise 35 min on treadmill daily at 4.0 mph look and feel great for my age and am very active, I quit smoking 17 years ago do not drink anymore but eat sub sandwiches, bacon eggs butter and double cheeseburgers fries etc. I take Vytorin for cholesterol my doc says not to worry but the web says my chances for a heart attack are one in four within one year. Who should I go get a second opinion from and what are my options and risks for a heart attack?
Terry
The calcifications are not necessarily the problem by them selves although they may predict risk. Your target should be to lower your risk of cardiovascular events. Of course it’s mostly about lifestyle issues and like in your case, statins are frequently prescribed to lower risk. From your description it looks like you could do a bit better with your diet. Great you quit smoking because that’s a huge issue. I also believe regular exercise is often underrated as a preventive measure.
My 53 husband was originally given a calcium score of 960, which was then taken down to 640 following an angiogram. He is on statins, angina medicine, aspirin and carries a spray in case he has a heart attack. He has osteoporosis in his knee and I suspect in other places too. Thinking of putting him on Vit K2 as my other fear is a link between calcification and dementia if the plague starts to build up on the brain. This is one condition where there are multiple organs that you really need look at in treatment options, as treating the osteo could make the calcification worse and vice versa. Is there a time when you would not advocate the use of statins in someone with calcified arteries?
That’s a a difficult question Leigh. I suppose statin treatment may reduce his risk of cardiovascular events. However, more information is needed in order to have a say on that, for example his lipid numbers, information on smoking, blood pressure and family history.
Hello, I had a heart scan performed about three weeks ago.I am 48 about 15 lbs over weight but, I’m working on that . My calcium score came back at a 59. To be honest it has me shaking in my boots. The lower left descending artery has 58 and I have 1 in another.. Does this mean 58% of my artery is closed ? This has my children very upset.. Any and all advice would be appreciated…thanks and God bless you..Chris
Christian
No this doesn’t mean that there is 58% narrowing or blockage. Coronary calcium score only reflects the amount of calcium within the walls of the coronary arteries. If I understand it correctly, in your case the calcifications are mainly found in the left anterior descending artery which is quite common. Although calcium score is a marker of risk it doesn’t really tell you anything about the degree of blockage or narrowing.
Speak with your doctor about whether further work-up is indicated and if any treatment is necessary. Focus on reducing your risk by working on lifestyle issues.
Hello.
I have a calicum score of 450 at age 40. No significant blockages. normal weight and blood pressure.
Suffer from PVC s. Curious to know if that is a cause or effect of the high calicum number.
All I can get from my Doctor is this puts me at a high risk for a cardiac event and can’t predict if the plague will rupture. He said keep an eye on your risk factors. But no real advice on how to prevent a future event. I feel doomed. What can I do. Again not overweight. Excercise and blood pressure normal. Can the excercise cause the plague to rupture.
Correction to my previous Email. Typo. My age is 60 not 40.
I am looking forward to any advice you can give me based on the above information. Seems to me that with the knowledge that I am at a high risk. Something could be done. Removal of plaque etc. There must be a reason why it forms in the first place. Inflamation but what causes the inflamation. Etc. Thanks so much.
Joe
This is not something that can easily fixed. We don’t really know what causes arterial calcifications. Genetic factors play a role and probably inflammation as well. Why some people have low calcium score and some high is still not entirely known.
Having calcium in the arterial wall is not the same as having narrowing of the vessel or a blockage. Calcified plaques are not more prone to rupture than softer plaques.
However, studies show that high score is associated with higher risk of vascular events but it doesn’t mean you’re bound to have one.
Discuss with your doctor whether further testing is needed.
Do what you can to reduce your risk. Moderate exercise is usually not a problem. Don´t smoke. Eat healthy. Try not to get overweight. Have your blood pressure checked.
Good luck
Like many of the men in this blog, I was found to have a positive calcium score. The test was done as part of eval for atypical chest pain. I had no cardiac risk factors and was found to have a score of 330. I was started on aspirin and high dose lipitor. I had neg nuclear stress test. Not sure where to go from here as I run regularly, have normal baseline chol and BP and don’t smoke. Do I need to make a big change in diet ie The Dean Ornish low fat vegetarian diet? Are there false positive tests? Do they revert?
Thanks.
Oh boy! After reading about calcium scores in the single and double digits, and people are concerned, now I am really concerned. I have severe rheumatoid arthritis and fibromylagia, along with a few other issues that don’t really bother me. Sept 14, I passed out in the shower, cold. i woke up on the floor of the bathroom. I ended up seeing a neurologist and then a cardiologist. The neurologist said my brain was fine. The cardiologist I saw was not my regular cardiologist because mine was out on disability. The temp cardiologist ran a number of tests – echocardiogram, stress test, day heart monitor,etc. I also had a calcium scan that came back at at 248. My lab work was prefect with the exception of elevated liver enzymes and an increased SED rate – both normal considering the meds I am on for my RA. The temporary docs advice was to drink 10 glasses of water a day and avoid the heat – and oh “take an aspirin a day just in case one of these pieces of calcium should break free”!!! Water and aspirin was his answer. All other indicators that would lead to a high score did not apply, no diabetes, good cholesterol, low blood pressure, plenty of exercise, no drinking or smoking. I finally saw my regular cardiologist last week and he put me on a statin to lower my risk of a heart attack, even though I do not have a cholesterol problem. What other treatment is there? Am I doomed and will I be paranoid about having a heart attack at any moment? Is there anything I can do? According to my doc,I am already doing everything. I am afraid to get upset or get angry because that might raise by blood pressure and cause a heart attack? Can anything be done to remove the calcium? I just want it all taken out.
Denise.
Although high calcium score is associate with increased risk, removing or reducing the amount of calcium isn’t necessarily a good thing. For example it’s possible that calcium deposits may result from healing of inflammation within atherosclerotic plaques. High calcium scores should be approached by general risk modulation which includes healthy diet, regular exercise, not smoking, taking care of high blood pressure, avoiding obesity and treat lipid disorders.
Please correct me if I am wrong. The calcium could be a result of the inflammation? from my RA? I have had RA for about 12 years.I am just so physically and mentally tired from all of this.
High cholesterol runs in my family and I have had it all my life. I am 29 years old and it has finally hit me what great risk I have. I have been on statins for 10 years but cholesterol levels are still high. I am scheduled for a calcium score test tomorrow morning, hoping to find out I’m not too late to make life long life style changes. Would you think this is a good idea to get this procedure done?
Hi Axel,
I actually had a bit of an issue with this portion of the article.
Treatment of individuals with high calcium scores should aim at reducing risk. This involves treating lipid disorders, high blood pressure and diabetes if present. Refraining from smoking is essential. Regular, moderate exercise is advised. Due to the overwhelming evidence of benefit in individuals with atherocslerotic heart disease, treatment with aspirin and statins is generally advised.
Before getting started I should begin by saying I’m extremely skeptical of the lipid hypothesis and that saturated fat is bad for you and that taking statins is beneficial in terms of all-cause mortality for anyone except a very small portion of population – men under 45 who have already had a heart attack. It’s also my belief that insulin resistance and elevated blood sugar are the most likely causes of CAD/CHD (as well as a host of other chronic diseases).
With that in mind, I’m wondering what the evidence is that you think is so overwhelming that aspirin and statins are beneficial for treating heart disease. The NNT for statins to prevent a heart attack is tiny, one’s risk of contracting diabetes from a statin is actually higher. I know that NCEP has developed a standard of care for heart disease that is based upon a statin to lower LDL but I also know that 8 of the 9 members of NCEP have taken money from drug manufacturers. I know this post was about CACs but I think it’s important to point out that are many doctors/researchers now think statins are ineffective at best and detrimental at worst with the skeptical number growing all the time. (Forgive me advance if you’ve covered this in prior posts, I’m fairly new to this blog).
Thanks,
Bob Johnston
Hi Bob.
That’s a vey good question.
In fact you’re right that I have written a lot on statins on my blog and probably share some of your skepticism.
“Due to the overwhelming evidence of benefit in individuals with atherocslerotic heart disease, treatment with aspirin and statins is generally advised.”
Firstly, this is not about my personal opinion. This is the view of most cardiologists and experts on the issue.
In fact there is strong evidence for the efficacy of statins in secondary prevention. This is why clinical guidelines are very clear on the issue; statin treatment is recommended for individuals with established cardiovascular disease. The NNT for lives saved is approximately 83 for five years of treatment. For heart attacks it is approx. 39 and for strokes approx. 125. Here is my reference.
Patients with high coronary calcium scores are at elevated risk and they can be considered to have established cardiovascular disease. However, very few studies have directly addressed the efficacy of statins in individuals with high scores.
So, if high calcium score is regarded as established cardiovascular disease, it should be approached and treated as such. That means stepping on all available breaks in order to halt the progression of disease.
Personally I think lifestyle recommendation is immensely important. Of course, when it comes to medical therapy, it’s about shared decision making. The clinician has a duty to the patient about the pros and cons of statin therapy.
Furthermore, it’s not only about the LDL-cholesterol. Statins have other mechanisms of action which may be helpful.
Personally, if I was diagnosed with a coronary calcium score above 400 before the age of 60-65 I would choose to be treated with statins.
Bob: thank you for your cogent contribution to this thread. I’ve recently received a high calcium score and learned a lot from your posts. You’ve convinced me that finally I really do need to change my diet. Thanks again
Axel – thanks for the response and it certainly wasn’t my intention to draw attention away from coronary calcium scans, a test I think has strong benefits and is a much better indicator or coronary health than a treadmill stress test.
I think you make an important distiction between primary and secondary care which most people tend to gloss over. If a person has never had a heart attack the course of action for prevention should be very different than the course people who have had heart attacks should take. But the difference oftentimes seems to be blurred and people in both categories are lumped together with the resulting advice being to get on a statin. But this is a topic for another post and I apologize for taking this comment section off course.
Bob
Again I was hoping that you could shed light on what type of diet is most beneficial for someone with a positive calcium score (330) at age 50 and no other CAD risk factors. I have read Dean Ornish’s books and would like an opinion regarding the need to severely restrict fat from the diet. Thanks
Hi gspappaPhil,
Here’s my $.02 on the topic of diet:
Before I start I should warn you that my ideas go against the mainstream but I believe I have an exceptional amount of evidence to back them up. I believe most doctors and nutritionists who promote a low fat, high carbohydrate diet don’t have a clue what they’re talking about. Most people are skeptical of what I tell them but if you have an open mind I think I can persuade you to go against the grain.
To me it seems quite apparent that heart disease is caused by chronic, low level inflammation, which in turn is caused by elevated blood sugar, insulin resistance and free radical damage. The key to heart health is to stop focusing on LDL cholesterol and simply stop eating foods that cause inflammation. The way to do this is to adopt a high fat, low carb diet. If you’re a believer in conventional wisdom then this way of eating sounds insane, if you look at the actual evidence it begins to make sense.
Carbohydrates are the drivers of elevated blood sugar, something your body normally maintains in a very narrow range. A meal full of carbohydrates will spike your blood which causes your pancreas to produce insulin, the hormone that is responsible for dealing with elevated blood sugar. It also has the role of fatty acid storage in the body – the more insulin the more fat is locked away in your ft cells and is unavailable to access for energy. A lifetime of eating carb-heavy meals causes insulin resistance, where it takes incresing amounts of insulin to knock down those blood sugar spikes. Eventually the insulin resistance becomes so marked that blood sugar levels become permanently elevated and this excess blood sugar does tremendous damage all throughout your body. Everydody’s seen what happens to a piece of meat that gets left in a can of Coke – this is the same thing that happens to your body’s cells shen blood sugar is high.
When blood sugar is elevated, inflammation occurs. In your arteries this inflammation results in damage to the endothelium, the single-layer of cells that form the inside. When a breach of the endothelium occurs LDL cholesterol and macrophages get trapped beneath the fibrous cap (essentially a scab) that forms over the breach. If the inflammation subsides then healing can fully occur but what generally happens is that blood sugar remains elevated, the breach never heals properly and the fibrous cap grows larger and larger over the trapped LDL and macrophages. After awhile the fibrous caps hardens and will either block the artery (CAD) or the fibrous cap breaks off and lodges downstream when the artery narrows. This is a heart attack. If that scab goes to the brain it’s a stroke (ischemic). People have the idea that LDL builds up on the inside of your arteries like minerals do inside a water pipe and that interpretation is totally incorrect.
So how do you prevent your blood sugar from becoming elevated? Stop eating carbohydrates. I’ve pretty much completely ditched them for over 3 years now, I’ve adopted what’s called a ketogenic diet. This means that my body is mainly fueled by fatty acids and ketones (a by-product of fatty acid metabolism). My diet is roughly 70% fat (saturated and mono-unsaturated), 25% protein and perhaps 5% carbohydrates. Wen testing my blood sugar after meals I’ve never seen it over 90 mg/dl. After a meal most people will routinely see values north of 140 mg/dl for several hours. Most people aren’t aware of this but when blood sugar is in normal range you have roughly 5 grams of glucose in your blood. This is roughly a large teaspoon. Eating a couple pieces of bread is about 70 grams of carbohydrate, or 14 times the amount of glucose your body wants to have. A typical person will eat 300-400 grams of carbohydrates per day, 7 days a week, 365 days a year. That’s a lot of sugar to metabolize, something we aren’t genetically eveolved to do. A small amount of glucose is needed to survive but your liver is more than capable of manufacturing this from protein, it’s totally unnecessary to consume carbohydrates.
Anyway, I realize I haven’t offered anything in the way of evidence yet and rather than make this comment into a novel I’ll direct you to the log of Dr. Peter Attia, who has done an excellent job showing research on low carb diets as well as documenting his own personal story about how he came to embrace a low carb diet (he is an endurance athlete who was getting fatter and fatter despite working out 3-4 hours a day). If you give it a read I’m sure you’ll find it fascinating.
https://eatingacademy.com/start-here
Most intelligent comment made
One more thing – I should have posted this last night but forgot.
I like this study by Stanford researcher Chris Gardner called the A to Z Diet Study. He put a group of participants on the various diets to see which is most effective for weight loss and improvement of the markers for heart health. What makes this study special is that Gardner is a vegetarian and was fully expecting to see his diet win out. It’s to his credit that he didn’t try to fudge the results when they didn’t turn out as expected.
Here’s a video recap of his results (the results being that the low-ish carb, high fat diet was by far the best for improving heart health.
https://www.youtube.com/watch?v=eREuZEdMAVo
Excellent video!
Back toy original question and please correct me if I am wrong. I am completely new to this. From what I have read and what my dr has told me, could my calcium be a result of my body trying to repair itself from inflammation caused by my RA, I have had high blood pressure in the past. I have had chest pains but no heart attack. All of my heart tests and lab work came back good. My dr put me on a statin to lower my risk dr a heart attack. I understand that that is what is done first. The second step is a stent. And the third is bypass. Can a stent work if it is calcium as opposed to fast? Should I be worried? Is calcium repairing my arteries a good thing? Could it have prevented something more serious? It seems like of it repaired itself that could be a good thing? Am I completely wrong? Is this very dangerous? My calcium score was 250 something if I remember correctly. I am trying not to be scared. All help is appreciated
I am a 40 year old male that spent my 20’s to mid 30’s around 210 pounds (I’m 5’11”). Ate the wrong foods, etc. In the past 2 years I have lost 60 pounds and have been feeling fine.
My dad just had a 4 way bypass 2 weeks ago and his calcium score was through the roof. They started to stent, but had to go the bypass route.
I took it upon myself to have my GP order a calcium score for me. The result was 25 in RCA and 9 in LDA, 23 overall.
With nothing more than family history, chest pains following meals, a “perfectly normal” EKG and now the calcium score my cardiologist is scheduling me for angioplasty! I feel we’re missing some other options and maybe pulling the trigger too fast on such an invasive procedure especially considering the risks and 10-year outcomes of the procedure.
I’ve started on Vitamin K-2, started on all the E,D, Omegas, and resveratrol.
Without health insurance I’m between a rock and a hard place as far as getting a 2nd opinion. Needless to say I feel like I may have a heart attack simply from the stress of this situation!
Is a 23 score in a 40/M worthy of angioplasty, or could this be shooting a mouse with a shot-gun?
Kyle H.
I assume your doctor has ordered coronary angiography. This procedure provides pictures of your coronary arteries in order to check there are any narrowings or blockages. If there are, angioplasty may be performed. Angioplasty is performed with a balloon and most often a stent is inserted in order to restore normal blood flow in the artery.
In fact, a coronary calcium score of 23 isn’t very high and does not by itself call for an angiography. However if there are symptoms such as chest pain or if exercise testing or other tests have suggested that blood flow is limited in soma parts of the coronary arteries, coronary angiography is usually performed.
I sincerely appreciate your response.
He’s basing this on an EKG and family history along with the calcium score. I’m apprehensive about anything this invasive (and expensive being self-pay). We have an imaging center that provides relatively affordable CTA scans (around $1,100).
**Could that be an alternative until there is more reason for concern? The cost of angiography might as well be $1M to me right now.
The chest pains I’ve described to him are more muscular, i.e. on top of the ribs than a deep pain.
Again, I feel he’s pulling the trigger too quickly.
Adding to my concern over the suggested procedure: my 45 year old cousin had the procedure done and they placed a stent on December 4th- same day as my dad’s bypass. They found him dead in his chair on 12/7 presumably from blockage.
I honestly feel that my CAD is just as much a death sentence as the procedures to investigate it. 🙁
Thank you again.
I am a 61 year old female. Post menopausal, not taking estrogen (a family history of uterine cancer prevents that) with a severe anxiety disorder and fibromyalgia. The last few years have been very stress filled – things i have no control over, unfortunately – and this has led (in addition to the constant stress) to my eating poorly, not moving enough, some weight gain, etc. I just had my calcium score taken, and it is 74, all in my left anterior descending artery. My dr. is VERY concerned that it is all in that area, and wants me to begin statins. Because I already have pain issues, I’m reluctant to do this. My feeling is that first I should make dietary and lifestyle changes – there is little I can do about much of the stress, but some of that situation is about to end, and I feel like that will help tremendously.
My dr. is making me feel as if I will have a heart attack any moment. My LDL is 125 – he wants me to get that down to 70 (!), and my triglycerides are also high. To be honest, he’s scaring me – something I admit is easy to do.
Should I be be more concerned that all the plaque is in that one spot?
Hi Deborah, I’m no Doctor so I’ll leave that aspect to Dr. Axel but you mentioned that you have a history of anxiety and feel you have no control over that. I’m also a pretty anxious individual and I think that deep breathing exercises and meditation, if done consistently, can help you lessen your anxiety. Just a thought.
Good luck
Thanks so much. I do both, and they do help, but the disorder is something I’ve had since a child, and sometimes leads to terrible panic attacks and as you know, just not fun. I’m one of those people who have to take meds daily. All that said, I appreciate your input – I have a feeling I’ll need to practice more meditation from here on out. It can only help. 🙂
Hi Deborah
A calcium score of 74 puts you at the 85th percentile. This means that 85 percent of women your age have lower calcium score and 15 percent have higher score. It is quite common to have most of the calcium in the left anterior descending artery. I don’t know of any studies suggesting that the localization of coronary calcium is an issue in terms of risk.
Of course lifestyle is important. Not smoking, healthy and regular exercise are key issues when it comes to lowering risk.
Your doctor obviously believes you may lower your risk further by taking statins. In fact, most people tolerate statin drugs very well although some experience muscle aching. Ask your doctor to explain the pros and cons of statin therapy.
Will do. Thanks so much for the information.
Hi. This is a query about whether I am ready for some surgical procedures, , angioplasty?
Last week, at the recommendation of the same physician I’ve been seeing, I had a coronary calcium scan. This past year, I have had a carotid scan (ultrasound) which showed moderate plaque in one artery but still good blood flow, and a stress echocardiogram which showed also showed good flow with some plaque buildup.
The latest Ca CT scan was pretty high,
Coronary Artery Calcium Score (i.e. Agatston Score with Threshold 130 HU)
Left Main = 0
Left Anterior Descending = 284
Left Circumflex = 50
Right Coronary = 109
Total = 443
IMPRESSION:
The coronary calcium score was 443.
The descending aorta is calcified.
I’ve been taking daily low doses of Lipitor/atorvastatin calcium (20mg) and Diovan (40mg) for over 10 years, but it seems to me that more should be done re the calcification. I’m 73.
For many years we always cook and eat the healthiest foods, and I do not often get seconds. Our diet and daily exercise have always been disciplined. Some years ago we both were very athletic, and while we are not at all athletes now, we still exercise regularly.
Hi L
I’m reluctant to give any personal advise, that would be irresponsible of me. But I’ll try to respond to you in general terms.
Angioplasty or surgery is not a treatment for calcifications or high calcium score per se. It is only performed if there is a significant narrowing (or blockage) in a coronary artery. A normal stress echocardiogram usually implies that there are no significant narrowings.
Hi Dr Axel,
I’m a 57 yr old woman, oopherectomy three years ago, (ER+ bc), strong FH heart disease, I had a calcium scan done 6 months ago at the urging of my endo ( hyperthyroid now under control). Score was 1100. Prompted a cardiology consult….stress echo normal, 48 hour holter showed occasional runs of svt, 24 hr BP monitor had some high #s but my normal is rather low. Started Lipitor 40 mg, aspirin 81 mg, and toprol XL 25 mg. I walk 2-4 miles per day, eat ( mostly) a healthy diet, and am 5’9″, 132lbs. Would you agree with this protocol? Should I be more proactive? I still feel like a ticking time bomb, especially since my mom had her first heart attack at age 52. Thank you for taking time to read my post!
Hi Sm
We’re all ticking time bombs and more so as we get older.
However, a negative experience may have positive consequences. Look at it positively and use this knowledge to motivate you to improve your lifestyle. There’s so much we can do ourselves; not smoking, regular exercise and healthy diet. it all counts. And of course, follow the protocol your doctor has suggested.
Hello, I had a chest CT Scan about four years ago and mild aorta calcification was found and I was told by my doctor that it was nothing to worry about, but I was only 42 at the time, now I’m 46. It has been bothering me for years that any calcification was found. I am thin , no family history of anything , parents are healthy and in their late 70s and I have 7 healthy siblings in their 50’s. My blood pressure is 106/64 . Just had lipid panel done
Total Cholesterol 144
Trig 47
HDL 48
LDL 87
VLDL 9
CRP <5
PROTIME 14.1 and INR 1.12
2 EKGs normal
All blood work normal including CBC and cardiac enzyme. My HDL used to be low at 25, then went to 38, and now 48.
Based on these , what are the chances of the calcification progressing and should I have test done?
Thank you
Pamela
Mild aortic calcification is a little bit different from coronary artery calcification. Your lipid profile looks good. So hopefully there’s nothing to worry about.
Hi Pamela – I’m curious about the dramatic change in your HDL levels. The 25 level is concerning but it seems to have improved dramatically since then. Your trigs are quite low (which is good), I’m wondering if you changed up your diet at some point.
I had the CT scan done in May of 2014 at the age of 38. I am a female, 145 pounds, 5’6″ and athletic, with a family history of heart disease and early death. My calcium score came back at 167. I was really scared, feeling like a ticking time bomb. My dad died at 51 from his fourth heart attack, his sister died in her early 40’s from the same thing. My cholesterol is consistently in the 300s, although I eat healthy. I was put on high dose statins but am scared of taking them because I hear it makes your score even higher. My theory is my dad was constantly on statins, three days before his death he called us to tell us he was excited for the first time ever, his cholesterol was perfect. Then he dies. I wonder if the statins contributed to his death? Now, the kicker here is my husband wanted to get his done. I thought he was being silly since his cholesterol is always under 200. He’s 43, 10 pounds overweight, but I would say decent condition. Would you believe his score is 704? We’re both panicking now, trying to really eat a strict diet but feel helpless. Is there truly a way to reverse the damage? We read about taking Vitamin K and are starting to take it. Any advice would be appreciated. Also, has anyone heard of anyone’s score reversing due to diet and exercise? Thanks for your input.
Hi Natasa
I don’t think we should regard coronary calcium as damage or anything that has to be reversed. It has not been proven that the calcium itself causes any harm. There’s no method available to reduce the calcium and reducing it is usually not regarded as a target in itself. However, high scores reflect increased risk. So focus on reducing risk by lifestyle measures. Discuss with your doctor whether he/she recommends statins.
My 70 yr old, healthy dad was just found to have a score of 1700. He has no symptoms and no risks of heart disease. We are in shock. Initially a concern was noted when images were taken for pneumonia that my dad had following a colonoscopy. He had stopped taking his prednisone that he is on daily for idiopathic hives. He has been on the prednisone for ten years It seems that somehow abruptly stopping his prednisone initiated an event that caused a rapid onset of pneumonia. Is it possible that the calcium measurement is reflective of inflammation from these events and not related to a heart issue? Thanks!
Kristin
There is quite much we still don’t know about arterial calcifications. It has been suggested, although still not proved that inflammatory diseases may affect coronary calcium. In fact there’s a thesis from UNTHSC 2010 that dealt with this question and found no clear relationship between inflammatory markers and coronary calcium in people with autoimmune disease. So, it’s difficult to tell whether inflammation plays a role in your father’s case or not.
I am 59 yrs old. I have had A-Fib since 2002. I have had 3 heart ablations and unfortunately, none have worked. Needless to say, I have regular visits to my EP and Cardilogist. Last year I had my Calcium test done and my score was 1858. naturally, this has me concerned because in looking at the ranges, they stop at 400 and that’s considered bad. If that’s the case, mine must be in a class all by itself. My Cardiologist has me on Lipitor and Zetia but I am really concerned about this. 2 Cardrilogists have mentioned that the score being that high is not a indicator that I will have a problem but I am wondering if aside from changing my diet, should I be doing anything else or should I be concerned?
Hi I had a calcium score of 14, I am 49 years old, I have high blood pressure and high colestrol, I have been but on statins and regurly excersise, I have a strong FH of hear disease, and suffer from anxiety, my doctor has said I have nothing to worry about but when a, reading post it says a, in 95th whatever for my age. I am now worked so much that I keep thinking am going to have a fatal heart attack any day. Shou.d I be worried
Hi Dr.
I am 39 years old, with family history of heart attacks, my cholestrol, blood pressure and daibities are normal.. I went through invasive angiography 2 month ago my calcium score was 7… Today I went through a calcium score CT my sore is 20… Is it logic that my score increase from 7 to 20 in 2 months time? Thank you.
Moussa
I would guess this is a methodological variation, meaning that the analysis isn’t performed in exactly the same way on both occaions. That would explain the difference. It is unlikely that the actual calcium amount has doubled in such a short time.
I am glad I found this site my cardiologist had me take the calcium test. Prior he did an EKG, ultra sound of my heart all normal. Blood pressure is normal.
Cholesterol 189
Triglycerides 72
HDL 65
LDL 110
However, my test came back at 172. I am 47 years old and in good health. What does this mean to me? He wanted to get me on Lipotor but I think its too early and I dont want to be on drugs. What are my options?
I am a 78 yr old woman with a CT Calcium score of 459. I have no CV symptoms and my last nuclear test was normal. On low carb healthy diet and exercise regularly. My LDLs have consistently been around 160, cholesterol 281, HDL 101, triglycerides 52
Unable to tolerate statins. Cardiologist now recommended Zetia which I am very concerned to take. (I meant nuclear stress test.). What are my risk factors if left untreated? Thank you for your help
Hi Axel, I am confused what to do for the best. I am 52 I eat a healthy diet, plenty of fresh fruit & veg, I exercise a few times a week, I am normal weight, I have normal blood pressure & I don’t smoke. I do however drink a little wine. My cholesterol is a worrying 8.3! & a CT scan revealed last year my coranary calcium score is 18. As my cholesterol level doesn’t seem to shift any lower than 7.3 my GP would like me to take statins but I am terrified of the side effects. I have read that cholesterol is high to protect against inflamation so does this mean I have inflamation in my body ? Should I perhaps wait to see if my calcium score goes up next time in 3 years before I consider statins. I am an anxious person & all this confusion just makes this worse ! Help !
I have FH Cholesterol and I am 33 years old, female, not overweight. I found out at the age of 24 that my total cholesterol was 385. I was put on a a statin and my total cholesterol has been a total of 180 ever since. I have always been very worried about what type of damage the 24 years that I did not know I had FH cholesterol caused. I went to have a calcium score done just to see what it would be. I had a score of 0. I am wondering what you think that means for me. Does this score of 0 mean that it is likely that I don’t have a build up of Atherosclerosis?
I feel the only way to know for sure the damage that was caused by all the years of untreated high cholesterol would be to have an angiogram. As you can imagine, at 33 years old, the risk and the lack of symptoms is enough that no doctor is going to perform one to “see” how much damage FH Cholesterol has done to me. My mother died at the age of 45 from this being untreated and I am just trying to prevent this from happening to me. Any feedback would be greatly appreciated!
Hi Casey
All I can say is that a calcium score of zero is good news. However, it’s unusual for women your age to have calcium in their coronary arteries. Hence, a calcium score of zero is to be expected.
When calcium score is zero in a young woman like you, it’s very likely that a coronary angiogram will turn out to be normal. So, if there are no symptoms, a coronary angiography will by most be considered unnecessary.
A carotid ultrasound might give some idea about whether there are any signs of atherosclerosis.
Good Day Doctor,
I am a 47 year old male w/family heart issues (grandfather and father had issues after 55/by pass etc)
I had a calcium test done 3 years ago at age 44 and my score came back at 51
I realized that over the past few years w/ a lot of stress and remaining probably 50 lbs or more overweight (5’11”-240+ pounds) and quite honestly a little paranoid (which I am probably now hence the comment) that I would have another test.
This time my test score came back at 198 at 47 years old.
I am guessing this is a very bad thing for the score to quadruple in 3 years???
I figured it might have a lot to do with my diet as I am a meat and potato guy…”No” and I mean no fruits and very little veggies???(which is why I have always had a terrible Cholesterol score)
My calcium scores:
LMA=0
LAD=40
LCX=140
RCA=18
PDA=0
I currently take fish oil, garlic, cinnamon, etc however not on a regular basis. (that will be changing along w/regular exercise)
I have not talked to my doctor about the results however I know there will be talk of using statins moving forward. I would rather not take them and get real about my diet and exercise.
Are there other vitamins I should consider as an alternative?
Should I be concerned that my score quadrupled in 3 years?
I thank you in advance and I look forward to your reply.
I am a 43 year old male with a calcium score of 28, cholesterol of 121, normal blood pressure ( I am on a blood pressure medication) 6 foot 280 lbs and my father had a heart attack. My doctor wants me to take Atorvastatin 10mg because of my calcium score. I am very concerned about taking it because I enjoy a few beers a few times a week. I am concerned about liver damage and the other side effects. I eat well non smoker and have been working on increasing my exercise and lowering my weight.
Hello. My name is Larry. I am new to docsopinion.com. I would like to present some info for evaluation.
Progression of Coronary Calcium and Incident of Coronary Heart Disease Events:
https://content.onlinejacc.org/article.aspx?articleid=1668131
Note Figure 2. Orange and Blue chart lines. It serves to control Calcium change to be less than 100 Agatstons per year.
Incidence of acute and chronic events by TCS categories. TCS – Total calcium score (AU).
Shemesh et al. Cardiovascular Diabetology 2013
https://www.cardiab.com/content/12/1/161
Control of Coronary Calcium. Confirmed by CT Scanning.
Please read the full text.
https://www.internationaljournalofcardiology.com/article/S0167-5273(11)00234-8/abstract
Hi Axel,
First of all, thank you for your insightful and responsible comments – I’ve read through almost all the Q’s and A’s.
I’m a 46 year old male in peak physical condition. I often compete in multi-day endurance MTB events. My total Cholesterol fluctuates between 300-400, BP 130/90. Before being able to enter an 8-day MTB race in March last year my doctor insisted on putting me on a statin which lowered my total Chols to 150. After completing the race, I stopped the statins and trusted my LCHF diet to do the work. On Tuesday this week, while training for this year’s race, I had a heart attack on the bike.
Cause of the MI: rupture of the plaque in coronary artery. Angiogram revealed a 90% blockage which was successfully treated by angioplasty only. FH is said to be the main cause of the artherosclerosis and resulting stenosis and my cardio insists statins is the only way forward.
Was there in your opinion any way I could have seen this one coming and avoided this very traumatic (for everyone around me) event? And do you know of scientific evidence that statins can reverse the plaque buildup?
Thanks for sharing your story Earle
I don’t think anyone would have been able to see this coming. Plaque ruptures are very difficult to predict. They can occur in very small, insignificant plaques. This is why heart attacks often occur out of the blue and sometimes shortly after a thorough work-up with all kinds of tests like, exercise testing, nuclear scans, CT scans etc.
There is strong evidence that statins reduce risk if given to people who have been diagnosed with coronary artery disease. They reduce the risk of further heart events and improve survival. There is some evidence as well that statins may reduce or reverse plaque build up (1,2,3, 4, 5)
Hi Axel,
Thanks so much for replying and for the literature. Looks like at best there is a very small effect by ruvastatin on the regression of the plaque and since I haven’t had any major side effects in the past (except for a hole in my wallet), I will most probably follow the conventional advice and stick to the meds.
I’m still sifting through all the research on LCHF at the moment and find it difficult to figure out my position in relation to the risks here. Can’t find anything on how good or bad LCHF is for recovering MI sufferers. Only for high risk CHD individuals… I suppose the I’ve gone from high risk to 100% statistic now?
Also: what would be the most sensible monitoring for me going forward? Do I get an MRI of the arteries or some derivative test (eg: Coronary Calcium Scan) on a regular basis?
As always, your input is highly appreciated.
At about age 62, Mayo Clinic reported my calcium score at 1200. I am female, exercise daily (mostly yoga, walking, and pilates), no meat other than fish, and my LDL is 60 with an HDL of 145. My CRP level is .04m, and my triglyceride level is very low. I am now 68 and the scores continue to ‘improve.’ The cardiologist even took my profile to a conference, but I have no idea what discussion followed. I do take crestor (mainly for protection and because my mother had alzheimer’s) and I do take ramipril for slightly elevated blood pressure (I have a very stressful high-profile position). It is frustrating that I cannot seem to find any information on ‘what to do.’ Are their any possible suggestions out there???
I am 66 years old and was just informed that my calcium score was 950. I now have appt. with cardiologist in 16 days. Is that too long to wait?
I am a female 65 years of age, just recently had a 150 score in my heart calcium testing and my cholesterol levels were 219, and my primary doctor put me on statin pills to lower my cholesterol, when I saw a cardiologist because I had my bp a bit high (I had never had high bp) he recommended I get the calcium testing and it came back at 150, he said I needed to take the statins…..I do not like taking pharmaceuticals, I do not trust them….but I took it anyway, my cholesterol levels went down to 175, but I started getting cramps in my muscles. I exercise regularly, routinely, I weight lift, been doing this for years, I am a vegetarian, but I do smoke occassionally (not a pack a day kind of thing) I am so torn on what to do, I have replaced the statin pill with omega three pills with flax, and I ingest garlic on a daily basis..my body produces this cholesterol, it is genetic…my mom who is 95 also has high cholesterol levels, also produced by her body. My blood pressure has leveled out, I personally think it was caused by emotional stress, but the cardiologist prescribed bp medicine three times a week which I still take. Am I hurting myself for discontinuing the statin pills? By the way my bp was no higher than 130/80.
My 70 yr old husband’s doctor suggested a heart score test for him. Our family dr was very concerned when his score was 1900….sent him to a specialist who did not seem concerned but started him on lipator. My husband has always been active, healthy, has smoked but has quit, on blood pressure medicine , 5’9, weighs 190. Since starting this medicine he complains of muscle discomfort and a little more tired than usual….help
I just had a calcium score test and it was 59. I’m a 46 year old white female with heart disease on both sides of the family. I’ve been having chest pain, right arm pain and pain between my shoulder blades;which is why I did the test. I’ve had this daily for a month and have been to doctors and no one is listening or testing. What should be the next step? Thank you!
Seeing a doctor is the only thing I can recommend. How about the one that ordered the calcium score test?
I am a 66 year old male. My cholesterol is 127 and my HDL and ratios are great. My calcium score is 17. My diet is excellent. All my heart tests and stress tests came back fine. I see that as you age it is expected that your calcium score will increase. So I’m thinking if I can lower my age to say 24… yeah, that would be great… it would extend my remaining years and certainly my quality of life. Do you have any ideas on how to lower my age from 66 to 24? 35 would be okay if it’s not possible. Thanks. -Pete
I can’t begin to tell you how much I agree with this treatment you are requesting. Revolutionary! I, too, would like to lower my age to 24 to enhance my quality of life going forward.
Follow up. 72 now. Cholesterol still below 130. The heart risk calculator won’t take anything below 130. HDL 52. BP 110-70. HR 60-72. No risks in the calculator. Still recommends statin. As an experiment I put 75 as my HDL and it still recommends statin. If you are male and 72, it will say to take a statin no matter what else you enter into the risk calculator. I guess I need age reduction surgery.
im a 53 year old female , my father died at 47 after his third open heart surgery, I had the calcium test done last week and my score was 800, what do you think should be done for me,
Hi Dr. Axel,
I am a 44 yr. old male with heart disease in my family. My father had a stent procedure when he was 53 and my mother has also had heart issues at 70. I work out 6 days a week, have normal blood pressure, normal cholesterol levels, I have recently had an EKG and a stress test, both coming back normal. However, my primary care physician mentioned getting a calcium scan. What do you think about this test? Are there other test you would recommend or do you think it is a good idea to go ahead with this scan?
Hi Shane
If your blood pressure and blood lipids are fine and stress testing normal, a calcium score won’t add much in my opinion. Of course it would be reassuring for you if it turns out to be zero. If it’s high your doctor may want to put you on a statin drug. In my opinion, the most important thing is to continue with your health lifestyle and abstain from smoking.
Hi – I am a 56 year old female, never smoked. Blood pressure and cholesterol normal. Due to history of CAD in family, I had an echocardiogram, which was normal and a Calcium Score test, which came up as 82. Cardiologist wants me to start lipitor but made no other recommendations. Does this sound right?
Hi Kathy
It’s difficult and often irresponsible to give individual advice in a comment forum like here.
What I can say is that I always believe that lifestyle modification comes first. Avoid smoking, eat healthy end exercise regularly. Statins like Lipitor may reduce risk in certain situations. Ask your doctor to explain to you the pros and cons of statin treatment.
I am a 57 yo PA, not in bad shape (exercise 3 days/week, no smoking, no drinking, no drugs), normal BMI. I discovered that I had high cholesterol and triglycerides during a random screening in college 40 years ago but nobody did anything about it then. There is some heart disease and high cholesterol in my family and I admit my diet sucks, generally. I started being treated for it when I was about 40, and it took a few adjustments to find a combo that worked (Crestor and TriCor). However, Crestor is very expensive, and I went off it. I didn’t take a different statin because either they didn’t work or they had intolerable side-effects. I had also tried niacin briefly but that was horrible for me.
I had asked about getting the CACS test done about 5 years ago, but at that time my doctor (whose husband is a cardiologist) said it was not “standard of care,” that insurance didn’t cover it, etc. However, Baptist Health was doing it for free this month (February being “heart month”), so I got it done yesterday. Not happy!! The score is broken down by each artery, but the total score is 160 (worst in LCx, 115, zero for the LAD). I do take calcium supplementation and get regular bone density testing. Was on aspirin until recent EGD showed ulcers (probably related to Mobic for shoulder) and told not to take either aspirin or Mobic, unless I also take Nexium…which I don’t want to do. Now doctor is telling me to go back on Crestor, not happy about that mainly because of expense ($180/month, doesn’t go generic until next year). Not sure if I should go back on it or not. Getting chest pain just thinking about all this!! Any opinions?
It’s difficult to give individual advice on the internet and often irresponsible.
However, I always believe that lifestyle issues come first, that is not smoking, healthy diet and regular exercise etc. Statins may reduce risk in certain situations but they sometimes have side effects as you mention, although most people tolerate them. It’s about shared decision making between you and your doctor. Have him/her explain to you the pros and cons of statin treatment.
As a PA, I’m fairly well aware of stated pros and cons, but so hard to know because I distrust Big Pharma and their claims etc. I don’t know enough to tell fact from hype. You know 30 years ago if your cholesterol was under 300, they didn’t treat it. Then all of a sudden if it was over 250 you had to treat it. Then it was 200. It makes me wonder who is making the rules…and if money, as usual, is the bottom line. My diet is not the best because I’m single and live alone and work 3 jobs from home, and I’m too lazy and tired to care what I eat, so I just sit at my desk and nibble all day. Again, I am not overweight and I do exercise, but the diet is the last frontier here. I am not making excuses but in the past, even changing to a super-healthy diet, my cholesterol was high. It is familial. I do need medication. I just question what it will do in terms of the CACS and what the score even means. My doctor said the Crestor would “reverse” the calcification in 5 years. Is that true?
My husband just received his CT Calcium score. LM 89. RCA 20. LAD 463. CX 61. He has a history of PAD, stents put in iliac arteries about 6 years ago, having pain again in leg and scheduled for doc to “go in” again next month. We were referred to a cardiology center due to calcium results and the appt won’t be till end of March. Should he be seen sooner than that? He is on avastatin for cholesterol
Hi,
I’m 48 and have a calcium score of 33. Because of some pain my doctor ordered a CT angio. It cam back showing one blockage at 50%. This freaked me out. He said that it’s not too bad and can be managed by lifestyle changes and medication – statins and asprin. Does this sound correct? I’m very stress about this and not sure what to do. I was shocked that I had 50% blockage with a calcium score of 33. Is this common? Any advice is appreciated.
Okay, so a few weeks ago I was having a little chest discomfort during a stressful time and decided to go to the ER ….just in case. Everything was fine but my cardiologist ordered a CT angio as an additional test to look for blockages. I just received the results and he said I had a 50% blockage of one artery. I was a little shocked and asked him if it was in a bad place. All he said was it’s not in a good place. I was a little dazed so I didn’t follow up with more questions. He said only at 70% would then he would recommend a stent but in my case he wants to put me on a low dose statin and a baby aspirin. He also recommended the the Mediterranean diet, no salt and exercise.
Honestly, I was so shocked about the results that I didn’t really ask as many questions as I should. He saw my distress and said that if I did a normal catheterization then the results would probably be lower than 50% and if he had one( he’s in his mid to high 30s) then he would probably have around 30% blockage. Not sure if he was just trying to calm me down or what but it didn’t work.
Anyway, it’s seemed bizarre that my Calcium score of 33 would also be a 50% blockage. Question, is 50% bad and should I take the statin? Everything I’ve read here says NO, but I’m a little freaked and am thinking about taking.
Any advice is appreciated and I would like to hear from anyone who has blockages and treating by just lifestyle changes.
Thanks,
John
Judging from what you’ve said, aspirin and statins sounds reasonable.
Not all plaques are calcified. Therefore it is possible to have a 50% blockage with a relatively low calcium score.
So now we have conflicting recommendations on fat and cholesterol in the diet, conflicting advice on whether cholesterol levels determine level of heart disease or some other factor like inflammation or genetics, new data that your HDL number alone is not predictive of protection… but rather the quality of the HDL that can’t be measured yet, stress tests including nuclear that are only effective for detecting blockages of about 70% or more, catheters that can only detect blockages in the area they are pushed through, calcium tests that may not be accurate because they cannot predict soft unstable plaque, no clear message about what level of exercise is healthy without being so excessive that it causes inflammation, conflicting advice on whether statins help someone who has never had a heart attack, conflicting advice on whether statins deplete COQ10 and therefore cause oxidation/inflammation, etc.
So what do we do? Exercise moderately, eat the right amount of calories consisting of a balanced diet of unprocessed foods, keep our weight down, discuss the pros and cons of statin therapy with our doctor, ignore whatever the tests find because the answer is always the same… exercise moderately, eat the right amount of calories consisting of unprocessed foods, keep our weight down, discuss the pros and cons of statin therapy with our doctor, ignore whatever the tests find because…
Thanks for the info. I’m wondering if I can take any supplements in place of the statin? My doc did mention that if he did the regular cardiac angiogram then the blockage would probably be less than the 50% shown on the CT angio. Does that mean the CT angio is not as accurate? Thanks again!
That’s right John.
CT angio isn’t accurate when it comes to predicting the degree of blockage. Most commonly, CT angio overestimates the degree of narrowing compared with coronary angiography performed by catheterisation.
No scientific study has shown that supplements have similar effects as statins so I would say the answer to that question is no.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2711245/
This website talks about 50-81% false positives. Second paragraph.
CT angiography is not the same as calcium scoring.
CT scanning is used for both. However, CT angiography uses contrast that is given intravenously. The 50-81% you’re talking about has do do with how good CT angiography is at measuring the degree of blockage compared with traditional coronary angiography (the gold standard).
Coronary calcium score is measured without the use of contrast and is by definition not an angiography.
Doc: I was just saying that John’s CT Angio (not calcium test) might have a false positive. His Coronary Calcium Score was only 33, so while it is possible his plaque is mostly soft, it is also possible the CT Angio was a false positive based on the article.
John said: “Everything was fine but my cardiologist ordered a CT angio as an additional test to look for blockages. I just received the results and he said I had a 50% blockage of one artery. I was a little shocked and asked him if it was in a bad place…Anyway, it’s seemed bizarre that my Calcium score of 33 would also be a 50% blockage.”
BTW, many articles say high dose statins may reverse plaque buildup:
https://www.webmd.com/heart-disease/news/20060313/statins-may-reverse-plaque-buildup
I’m sorry but this is too much. There have been more than a few articles recently talking about studies that show that abstaining from salt is a poor course of action. The fear of salt is nothing more than dogma and it needs to go away. What you should be afraid of is not getting enough salt because salt depletion also depletes your body’s store of potassium and magnesium.
Additionally, if you look at the NNT (number needed to treat) for a statin you’ll find that there is no benefit whatsoever in terms of all cause mortality to take these drugs and over 100 people need to take one for 5 years in order to prevent a single heart attack. However, 1 in 50 people will develop diabetes from statin use and 1 in 10 will develop muscle pain. These drugs are a sucker’s bet – are you going to be the 1 person in 100 who won’t have a heart attack? I’d bet you’re not.
And what exactly is “The Mediterranean Diet”? I bet if you asked 50 doctors you’d get 50 different answers.
@ Pete: FUNNY!!
As an aside, I just went to pick up my Crestor. I was flabbergasted that instead of $180 (standard price for 30 tabs), my insurance covered it for $30, and with the Crestor discount card it brought it down to $18. I am so grateful for that. I was really prepared to do without until it went generic next year. Who can afford $180 a month? Well OK probably there are people who can, but I’m not one of them.
Mediterranean diet: A diet traditionally followed in Greece, Crete, southern France, and parts of Italy that emphasizes fruits and vegetables, nuts, grains, olive oil (as opposed to butter) and grilled or steamed chicken and seafood (as opposed to red meat). Plus a glass or two of red wine.
To be exact, there is not merely one Mediterranean diet. What is eaten varies significantly from one Mediterranean country to another. There also are major differences in diet between some regions within a country, as in Italy. However, the shared features of what is usually spoken of as the Mediterranean-style diet are as follows:
High consumption of fruits, vegetables, bread and other cereals, beans, nuts and seeds;
Olive oil is the key monounsaturated fat source;
Dairy products, fish and poultry are consumed in low to moderate amounts;
Little red meat is eaten;
Eggs are eaten zero to four times a week; and
Wine is drunk in moderate (or low) amounts.
Now you know.
No, now I know what you say it is and I’m seeing exactly zero evidence this is correct and more importantly, that eating this is advantageous. I’d like to some some evidence and for once not have it be data from crummy observational studies and their correalations and also where the relative risk is given rather than the absolute risk.
Bob Johnston said in my post on Mediterranean diet: “No, now I know what you say it is and I’m seeing exactly zero evidence this is correct and more importantly, that eating this is advantageous. I’d like to some some evidence and for once not have it be data from crummy observational studies and their correalations and also where the relative risk is given rather than the absolute risk.”
My family came over to the US from Southern Italy. It was well into the 20th century. I grew up in NJ where there were many Italians, Southern Italians. The Italians ate the same things. We never had butter or margarine. It was always olive oil. There was always lots of fruit, nuts, seeds, spices, dark green salads, and vegetables. We seldom saw red meat. If we did, it was in meatballs only on Sundays. It was cut way down with bread crumbs and it consisted of beef, veal and pork. You would get 2. We had chicken, fish at least once a week, cheeses, decent bread, grains, beans, and meatless meals. The salads had tomatoes, sometimes spinach, radishes, onions, mushrooms, carrots sometimes, cucumbers, vinegar and olive oil. We always had peppers, olives, zucchini and summer (yellow) squash. We did eat omelettes. Usually with onions, peppers, spinach, maybe tomatoes, or mushrooms. Sometimes we had omelettes for dinner. Once in awhile we had potatoes. Once in a great while my mother would put a minimal amount of sweet sausage in the spaghetti sauce. Sometimes we had stuffed peppers with rice. If I ate over someone else’s house, I was always uncomfortable as I never knew what “different” food I was going to have to eat. I was surprised how different their diet was. It was the first time I ever saw white bread. Wonder bread. I asked if we could get it and my father just laughed. Seeing what other people ate was a big awakening. I thought everyone ate what we did.
So the diet is real. My parents were first generation and they ate like their parents did. We were introduced to some other types of food, but the Italian food was what we wanted as kids. I still eat the same things at home. Usually 4-5 small meals. My wife is Korean, so I eat some Korean food now. We just don’t have meat and potatoes or things like meatloaf. My weight is good and my cholesterol is 127. Is that good? I don’t know, but my coronary calcium score (17) is very low, particularly for my age, 66. I’m able to play sports, lift weights, do 5 miles a day… whatever. So Bob, there are people that are very sure what a Mediterranean diet is. And I don’t think it has hurt me. Hell, people think I’m in my 40s.
So what do you eat, Bob?
Pete – you’re misunderstanding my criticism. I’m quite certain that you eat what you say you eat – but how is that pertinent? I want to see controlled eating studies performed, not the typical Yahoo headline about some diet that’s labelled “The Mediterranean Diet” but doesn’t actually go into detail as to what that means and then only compares the health benefits versus people who eat crap like sugar, refined grains and more sugar. I see way too many times where the results of an observational study – which by definition cannot show cause and effect due to its uncontrolled nature – are used to implyy cause and effect (our host falls prey to this misconception all the time). This is the ultimate in crap science and the public in general has been hoodwinked by bad nutritional science for decades now. It needs to stop.
You want to know what I eat? It would be easier to say what I don’t eat – no sugar, no grains, no polyunsaturated vegetable oils and very little fruit. Everything else I eat to my heart’s content (and it is content).
And to be frank, while I don’t feel that cholesterol levels have much predictive value to health, I’d be scared to death of having a cholesterol level as low as yours. One thing an observational study can show is a lack of correlation – and everything I see shows that people with higher cholesterol levels live longer than people with lower levels. Cholesterol is a desrieable compound – your body uses it as a building block in a variety of things in your body. Without cholesterol you would die instantly. What isn’t desireable is to have cholesterol get trapped beneath the endothelium in your arteries and become oxidized. But that isn’t the fault of cholesterol – it’s the fault of inflammation caused by excessive blood sugar.
I’ll leave you with this graph from a study performed on the NHANES III data – you’ll see that from 136,000+ heart patients sampled, people with heart issues were more likely to have lower LDL-C than higher LDL-C and that when viewed against the general population heart issues are left-shifted. If the theory that high LDL is the cause of heart disease (and which the statins-as-prevention theory is predicated on), how can this be?
https://i81.photobucket.com/albums/j201/bobbyj0708/LDLvsPopulation_zps2727e15d.png
Bob: I agree it is as much what we don’t eat. getting rid of the processed stuff and sugars are a big part of it. However I can’t link the chart you have with NHANES iii, CDC, or AHA, only your photobucket and Ivor Cummins “Fat Emperor” website. I was able to find the NHANES iii website and there all kinds of demographic charts with cholesterol levels, but not the one you have. Can you link me to the actual NHANES iii, AHA, CDC or NIH websites that show that graph? I’d like to read the details. Cholesterol levels matter decades before the development of heart disease and not just after they modified their diet or took medicine after diagnosis. BTW, have you had any tests like a nuclear stress test, stress test, ECG, or coronary calcium test to know if you have heart disease? How long have you been on the high fat diet? Thanks.
Hi Pete – I initially saw the chart I posted in the 5th part of Peter Attia’s 10 part series on cholesterol (I heartily recommend it to anyone who’s interested in discovering just how much conventional wisdom is wrong when it comes to heart disease). Here’s a link to his blog post – there’s a link to the actual study in his post:
https://eatingacademy.com/nutrition/the-straight-dope-on-cholesterol-part-vi
Now as to your question regarding my own personal test results (which is quite fair), I have this to say – I don’t have any test results for the tests you asked about.
The reason I don’t is because I feel these tests, with the possible exception of the coronary calcium test, are worthless. I’ve lost track of how many times I’ve read about people who passed a stress test having a heart attack within a month. Their predictive value is poor at best.
In my eyes your risk factors for metabolic syndrome are a far better predictor of health than running on a treadmill. That’s because metabolic syndrome is highly associated with all the chronic disease that plagues our society – heart disease, cancer, diabetes, Alzheimer’s – you name it. So I gauge my health by looking at these 5 things:
1. Do I have a lot of visceral fat? (over 40″ waist in men, 35″ in women)
2. Do I have triglycerides over 150? (Personally I feel this number is too high, it should be under 100 with your TG/HDL ratio at 2 or less)
3. Do I have low HDL-C? (under 40 in men and under 50 in women)
4. Do I have high blood pressure?
5. Do I have elevated blood sugar? – I think this one misses the mark a bit as well as the std test is fasting blood sugar which may or may not indicate blood sugar issues. It would be more accurate to check your HbA1c which tests your level of blood sugar on average for the past 3 months.
Notice that LDL cholesterol and total cholesterol are not a risk factor for metabolic syndrome, that’s because these numbers are mainly irrelevant. And since I have no issues in regards to these 5 factors I have no reason to any further testing.
That’s why I feel bad for all the people in this comment section who are talking about their CC score and saying that the only advice their doctors are recommending is lowered salt intake and being put on a statin – both of which are ineffective at best, deadly at worst.
All 5 of the risk factors for metabolic syndrome have been shown to improve the best with a low carb, high fat diet for the vast majority of people tested. Here’s just one study – it’s Gardner’s A to Z study. I like this study because Gardner is a vegetarian and he was shocked to find out that low carb was the best diet (to his credit he didn’t try to hide this). I’m posting the youtube video about it because it’s easier to understand than reading the study but it’s easy to Google if you want to read it.
https://www.youtube.com/watch?v=IvWX33enZE0
I appreciate all the responses and opinions. One note, i tend to agree with Bob but the pressure from my family and Doctor to take meds is very strong. I understand their concern.
I have a lot to think about.
Hi John – the pressure from the family is the worst. Absolutely nobody in my family agrees with my ideas, they all believe that doctors are infallible. My dad is currently battling colon cancer and had a small heart attack. He’s also been overweight since his early 30’s, has gout and had cataract surgery – he’s been doing the low fat, healthy whole grains diet for years now. He also takes his statin and aspirin religiously (as well as 4 or 5 other drugs) and this is where it’s gotten him. I tell him – “why not try something else, what you’ve been doing obviously isn’t working” but it’s as if I’m speaking a foreign language. And then he tells me that I need to start following his diet advice…
So just so you know what my personal experience is – I was always heavy growing up (which sucked) even though I was active. I played a lot of organized sports in school and that continued until well after college. In my early 30’s (just like my dad) I began putting on more weight even though I was still playing basketball and mountain biking, it was frustrating. My diet was “good” – I was eating low fat with whole grains and low sugar yet I was gaining weight, I also had exercise induced asthma, shaky hands and suffered from fairly bad hayfever. A chance conversation in the early 2000’s with a couple who ate low carb made me try it, I lost about 40 pounds but I was really concerned about all that saturated fat and cholesterol so eventually I went back to my old ways with a ramped up exercise program. I was soon back at my old weight. Then the research starting coming out showing how it wasn’t fat and cholesterol that was causing obesity and chronic disease, it was more likely elevated blood sugar brought on by dietary carbohydrate. I abandoned wheat, starches and sugar, ditched diet sodas and artificial sweeteners, once gain lost that 40 pounds (while putting on muscle) and also lost the asthma, hand shakes and my hayfever isn’t nearly as pronounced. I will never, ever go back to a low fat, high carb diet and I will never, ever take medical advice without seeing the research that prompted it.
Your doctor works for you. I would ask him point blank why he thinks that medications will work for you. If he gets offended and blusters then get a new doctor. If he hides behind the statement that a statin is the treatment suggested by NCEP (The National Cholesterol Education Program) then get a new doctor. The only acceptable answer is for him to cite the appropriate studies, which if you then dig into you’ll find out that the benefit is vanishingly small if it’s there at all.
I wish you good luck and good health,
Bob
Bob: I agree with you that the tests (excluding the coronary calcium test) seem to have little value in diagnosing plaque buildup. I agree with your diet, though I eat fruit in lesser quantities and little red meat. Other than that, your diet is similar. Limited carbs. No sugar. Etc. Like you, I pass the metabolic syndrome test. I guess my diet is kind of a cross between yours and the low “bad” fat diet. What you “don’t eat” seems to be key. We just differ slightly.
I should add that, the calcium was never scored: that it was an incidental finding and that a bismuth breast shield should not have been used, which could have contributed to the findings. What do you think?
Thanks Bob! I’m still on the fence about the statin.
Hi Dr Axel
I’m a 63 yo white male. I recently scored 146 on my coronary calcium score.
My most recent lipid panel looks like this.
CHOL/HDL RATIO 3.5
CHOLESTEROL 260
HDL 74
LDL 172
TRIGLYCERIDE 86
I’m still an active runner (30+ mi/wk). Good BP. No other health issues. No family history of heart disease.
Cardiologist is prescribing statins. I’ve had high cholesterol as long as I can remember & have never wanted to take statins. After reading your blog I’m still resisting. Not sure how to resolve this impasse of the mind. Any wisdom?
Terry
We don’t really have studies directly addressing the question whether statins are beneficial for individuals with high calcium scores. However it has been assumed, based on other study findings, that statins lower risk if calcium score is high.
So, this has to be decided in each individual case, based on general risk assessment taking into account risk factors such as smoking, blood pressure, lipid panel etc.
To me your general risk appears relatively low apart from the slightly elevated calcium score. The lipid profile is not that bad really apart from the LDL-C. Whether to treat with a statin or not isn’t always obvious. It should be a shared decision making between you and your doctor.
Hi, just found this site after returning from having a test run. My score was 29. History: 52 years old. excellent shape. Been a avid runner since 1982. My numbers are good with exception of Good cholesterol was at 34. family history: both parents had heart attacks in their 70’s. Both longtime smokers. me, never had a cig in my life. younger brother( age 48) had stent put in 3 years ago in the LAD. that is where my calcium was found. Now I am a little heavy(5’10-200lbs) but exercise all the time(run, bike. weights. cross fit). I take supplements(fish oil, krill oil. multi-vitamin, magnesium, Coq10) how concerned should i be about this? I had the test ran 6 years ago and the score was 9.
I have to admit it was a eye-opener and had me REALLY stressed today. I even went through the kitchen last night and dumped all the sweets and poured out the soft drink.
On the average I do around 180-220 minutes of cardio a week, within a heart range of 130-170 BPM.
What else can I do ? Other supplements ? medications? Is this a bad number for someone with my history/age/lifestyle ?
Thanks for all the feedback. God bless
Hi Steve – I’m no doctor but I’m curious about your situation. Tossing the sweets and the soft drinks was great, just don’t buy any more now.
The rule of thumb I use for heart health is your triglycerides divided by your HDL. A ratio under 2 is good, anything over 2 and I’d be concerned. An HDL level of 34 isn’t good, that means you have one of the five risk factors for metabolic syndrome – the other 4 being triglycerides over 150, high blood pressure, abdominal fat and elevated fasting glucose. Fortunately all 5 of these risk factors are shown to improve by cutting carbohydrates, an easy fix.
I’m a big believer in the idea that pretty much all that ails a person is diet related – if you do Crossfit I’m sure you’re aware that a Paleo diet is a mainstay for a lot of folks in that community, for a reason. It works. My advice (and I am not a doctor) would be to forget the drugs and forget the supplements – just eat foods that won’t spike your blood sugar or cause inflammation.
Steve.
I don’t think a coronary calcium score of 29 is that scary really. Could be much worse. After age 50 only about 50% of people have lower score than this. You certainly have a family history of coronary artery disease which is why you should do what you can to minimise your risk.
Not smoking is certainly a blessing in this situation and will have lowered your risk dramatically for sure. I wouldn’t think too much about supplemements, maybe fish oil though.
I tend to agree with Bob about the dietary issue. Limiting sugar and carbs may help you lose weight, improve TG/HDL ratio and reduce insulin resistance.
Hello, I’m a 46 year old male with a calcium score of 25. My triglycerides are at 227h and HDL at 36 with VLDL cal at 45. All other blood work is fine other than Eos absolute at 0.5h. Taking a small does of Simastatin. Is there anything I need to do to better my heath here? Is 25 calcium score fine? Just looking after my health knowing my father had a triple bypass around 68. Thanks Alex
Interesting comments above. I’m a 48 yr old australian women 1.6 m tall 57kg . A family history of blocked arteries& heart attacks. I had a CT cardiac angiography 1 month ago & the results were:
Coronary calcium score: 139
Left anterior decending artery: calcified atheromatous disease involving the proximal and mid LAD causing 50% narrowing . No stenosis
A small left to right shunt passing from left chamber to junction of the SVC and right atrial chamber
Cholesterol 5.6
Triglycerides 0.9
Blood pressure average: 120/70 pulse 67
Small tiny pains in heart area for past 12 months – does not affect anything barely noticeable
Any thoughts of comments? Or advice regarding how to lower calcium score as I didn’t think one could?
Interesting to read Kim, this is for a doctor to provide. I have read that vitamin K2 works for the blood vessels, this would be a question for the doctor though!
I am a 49 year old female with history of anxiety. went to ER with chest tightness and jaw discomfort. all tests showed this was anxiety related. but my big fear was that the cat scan showed I had a calcium score of 80! at my age! I’m so worried about this. I am maybe 5 pounds overweight, bp 118/78, not diabetic and my LDL was 133 and HDL 53, total cholest 178. triglycerides in the 70’s. This upset me so much that I now have 3 months of worse chest tightness despite other tests, including EKG, and stress test. When I take valium I feel 75% better so it appears to be this massive gripping anxiety. the cardiologist put me on baby aspirin and pravastatin 10mg. I am questioning if I should be on the statin at all. I feel like I am a walking time bomb for a heart attack but the doctor said no, I should not worry now. How can someone my age have so much calcium? I do eat pretty healthy, 85% vegetarian, no red meat, but used to smoke( quit 15 years ago) and I exercise a bit a few days a week, do yoga , walk and eat lots of veggies. please help! Should I stay on statin? I hear they are not too safe? what about every other night? and I worry about taking aspirin too…at my age…. i started drinking pomegranate juice and want to do more catual therapies. does my score and my LDL number indicate that I have very bad problems? should I have more testing? thank you for your advice
I’m sorry but this is the problem I have with tests like coronary calcium scores. To me there’s nothing alarming about Lynn’s basic lipid profile and other markers – blood pressure is fine, TGs are great, HDL is really good although an advanced lipid profile that shows LDL particle count and LDL pattern would be very helpful. But now because of a score that simply may be an artifact from her smoking days some cardiologist has her on a drug that’s never been shown to be helpful in women and she’s taking a SSRI because of overwhelming anxiety. This is sound medical advice?
The only reason I would ever get a CC test is to see which way the score is trending over time. Perhaps when she was smoking it might have been the same or even higher – and over the intervening years her score might have flatlined or even improved, we have no way of knowing from a single test. But because of this single test her cardiologist now has a patient for life.
Hello Lynn, I’m not a doctor and I respect this website of Dr. Axel. I have seen so many people going to the cardio doctors for chest pain, jaw pain (TMJ) anxiety and so much more. What I have seen even for myself is people having mitral valve prolapse causing regurgitation of blood backflow. A lot of people have it even runners and they are healthy people. It’s just a condition people were born with, I’ve taken Toprol and Klonopin for years and that took all my symptoms away. Just thought I would share, but it worked for me to be stable!
Lynn: Coronary calcium does matter. Continue to do healthy things. I wouldn’t say the calcium is an “artifact” from smoking, maybe it is a “result” of smoking. Artifacts are things that aren’t real or “there” (or representing the condition of your body). On ECGs, artifacts can be electrical interference that alters the ECG tracing. The calcium is real. Pravastatin is believed to be beneficial to prevent more plaque buildup and reduce inflammation. They believe inflammation causes damage and calcium is formed when the body tries to heal. That’s probably an oversimplification. 10 mg is a small dose. It’s up to you to decide if you should take it, but it is most likely a good idea considering conventional medical thinking. Adverse effects are very uncommon on 10 mg of Pravastatin. If you can slow or stop the progression of calcification, you’ll find that others will catch up with your calcification levels in 10 years and your risk, given your older age, will go down. That is my two cents. Everyone doesn’t agree with my thinking. You decide. -Pete
Pete – I hate it when people try to put words in my mouth that I didn’t say. I didn’t say that coronary calcium doesn’t matter, I said we have no idea if Lynn’s CC score is worsening, staying the same or getting better because we have no baseline to measure against. Perhaps her CC score was even worse when she was a smoker, we have no clue. And despite your somewhat headscratching exception to using the word “artifact” rather than “result”, unless we know which way Lynn’s CC is trending it’s outrageous to put her on a prescription for drugs that are proven to cause a lot of side effects. And despite your assertion to the contrary, there is no evidence that statins are beneficial to women of any age or any CAD history. By prescribing statins for Lynn her cardiologist is subjecting her to all the side effect risks for no possible benefit. Who does that?
And if you object to my characterization of statins having no benefit for women, take a look at his Crestor ad targeted at women. If there had been any benefit whatsoever found in any clinical trials Astra Zeneca would have plastered the relative risk all over this ad – instead we see the words “Crestor has not been shown to prevent heart disease or heart attacks”. Obviously AZ doesn’t want to get sued by making untrue claims in their ads. And “conventional medical thinking” has been a collosal failure when it comes to the prevention of heart disease so I don’t believe it unwise to consider alternatives to trusting every word from a drug pusher in a white coat
https://i81.photobucket.com/albums/j201/bobbyj0708/Crestor_zps1bacen9l.jpg
Best information I have found to support the patient understanding the numbers. Thanks
I had a coronary artery calcium scan (EBT) in 2006 (age 58) with a score of 0. I had a second test (CT) recently (age 67.5) with a score of 21. I am female and caucasian. The radiologist interpreted the current result (characterizes it as in the 25-50 percentile, whereas your calculator says 58) but does not discuss whether the delta from 2006 suggests a progression of concern or typical. Doesn’t the ‘speed’ of progression over time have some bearing on risk and timeline for developing CAD? How can I determine what my results suggest in this regard? As with osteoporosis, I generally like to know what the progression suggests in terms of developing a serious problem, rather than just my status today (eg results relative to my history)
I am not a doctor. I do read though. It’s with that understanding, I am posting the below information.
I was reading this Life Extension website. They say statin drugs don’t prevent heart attack and stroke according to studies, but they do reduce the incidence of heart attack and stroke. It is not an “either/or” situation between reducing stroke risk versus “preventing” heart attack and stroke. So statin drugs lower total cholesterol and LDL cholesterol while modestly increasing HDLs. That is thought to reduce risk. Just because it doesn’t “prevent” heart attack and strokes, does not mean it doesn’t lessen them. Studies showed a 48% reduction in those events. Those studies, I understand, involved patients with very high cholesterol with high doses of statins. But it does work at some level, even reversing a small amount of plaque. It can’t un-do old damage to prevent bad events, only reduce them. They also believe statins reduce inflammation. Again, statins might possibly reduce plaque, but have no effect on coronary calcium, from what I have read from various sources besides Life Extension.
Life Extension is not pro-drug company, but they do point out that statins have a role in preventing heart disease progression. The problem, they say, is that statin drugs only attack 4 of the 17 contributing factors to heart disease (High LDLs, High Total Cholesterol, Low HDLs, and Excess C-Reactive Protein). Below are the 17 factors they propose. The website explains what you can do about them. It is an interesting proposition. And it’s complicated.
https://www.lef.org/Magazine/2009/5/Heart-Attack-Risk-Factors/Page-01
17 Independent Heart Attack Risk Factors
#1 and 2: Excess LDL and Total Cholesterol
#3: Low HDL
#4: Excess Glucose
#5: Excess Homocysteine
#6: Excess C-Reactive Protein
#7: Insufficient Vitamin D
#8: Insufficient Vitamin K
#9: Elevated Triglycerides
#10: Low Blood EPA/DHA
#11 and #12: Low Testosterone and Excess Estrogen (in Men)
#13: Excess Insulin
#14: Nitric Oxide Deficit
#15: Excess Fibrinogen
#16: Hypertension
#17: Oxidized LDL
So it would also seem that just focusing on just cholesterol levels, fat intake, and carbohydrate intake is not enough. But ultimately, a balanced “non fad” diet, moderate exercise, regular monitoring of blood and health by a doctor, and general healthy non-stressed living should address many of the above factors. Additionally, addressing the 17 factors should help prevent heart disease even more.
Well it appears that by simply pushing your support for the conventional wisdom you’re conceding my main point that we have no idea if Lynn’s CC score today has stayed the same, gotten worse or has gotten better and that a prescription for statins based upon her CC score from a single test isn’t a good idea. Small steps.
Let’s move on to your defense of conventional wisdom. Your beginning statement is nonsensical – how can a drug be shown to not prevent heart attack and stroke by actual clinical trials but still be thought to reduce the incidence of heart attack and stroke? It can’t, except in the magical world of dogma and conventional wisdom.
The problem is that people confuse risk factors with actual cause and effect. Suppose you believe that abnormal LDL-C (whatever that is) is a risk factor for heart disease (I do not). Because it’s a risk factor does that necessarily mean it’s a cause? Not on your life. It could easily be that whatever it is that causes heart disease also causes elevated LDL-C. Heart disease and LDL-C could both be the effect of some yet to be determined cause. And despite the fact that a risk factor like LDL-C is most likely an effect of something else, doctors prescribe drugs like statins to artificially reduce the level of LDL-C and then pat themselves on the back and say “Voila! I have cured you”. When the patient subsequently suffers a heart attack they most likely think that the patient stopped taking the drugs against their advice. The point is that reducing a risk factor should never be a target of therapy, a reduction on the actual disease should always be the target.
It’s very easy to mistake cause and effect from a correlation. As an example, suppose you do an observational study and you notice that having grey hair is highly correlated with CAD, diabetes, cancer and all-cause mortality. Now obviously the true cause is old age but don’t you see how people could see a result like that and jump to conclusions? Isn’t it likely that the hair dye companies and the hair styling industry would latch onto these results and issue ads saying “Get rid of that grey hair and reduce your risk of dying by 75%”. This is exactly the same thing that’s occurred with the Lipid Hypothesis – a weak risk factor was latched onto by the pharmaceutical companies and pushed as a cure for heart disease even though they’re actually just treating a risk factor and not the cause. The Pharmaceutical companies own research backs this up – none of their trials have ever shown a significant reduction in all-cause mortality. And yet these drugs are the most highly prescribed drugs in our history.
This is not science. Relying upon conventional wisdom will be the death of us all.
Hi,
Do most people by the time they reach 50 have some calcification in there arteries?
I had a ct scan done for abdominal pain and everything was normal except for minimal aorta atheroclerosis calcification. My doctor said he sees this all the time.
with incidental findings. I have normal blood pressure total cholesterol is 187 ldl72
hdl73 trigs 70 crp below 0. I am concerned because I have read that you can have a stroke from the Aorta.
Can you please let me know what you think.
Mary
Mary
I would tend to agree with your doctor about “minimal aortic calcification” at age of fifty when he says “he sees this all the time”. It’s unlikely to be of any signinificant importance.
Hi Dr. Axel
I am a healthy 54 year-old male. 2 years ago I had a scan done where my score was 405. I had no real prior risk factors. I have exercised all my life and pretty much ate fairly clean …my only vice was cheese. After my CT scan came back I also had a stress test which I passed with flying colors.. I am in the gym lifting 4 days .. Cardio 3-4 days. my cardiologist put me on 10 mg of avorstatin I am now taking every other day and baby aspirin. I have cut cheese out of my diet. Despite my cardiologist telling me I won’t drop from a heart attack in the next 10 years I am still freaked out everytime I get a pain in my chest or arm. I have a nutritionist who has me on a bunch of supplements including coq10 and tocatrianols
who has told me to avoid all saturated fats. I have replaced my turkey sandwiches w almond butter.
My LDL is 62 HDL 51 TRI 60. My doc says I am doing everything I can and not to worry… I worry everyday. My parents were holocaust survivors who lived into there 80’s. They did not have heart disease. Everyday there is a different report or study that comes out on heart disease. I don’t know what to eat, drink or supplement to take any more.
Lew
I understand your frustration.
The calcium score puts you at a somewhat increased risk. On the other hand your family history, lipid profile and lifestyle suggests your risk for cardiovascular events like stroke or heart attack is very low.
So stop worrying. You’re doing everything you can. Enjoy life 🙂
Thank you for your response Dr Axel. It is frustrating and scary. As Pete said in an earlier
post the info on heart disease.. It’s causes and
treatments seem to change every week. Yesterday a report came out on the benefits of coffee! How do I know if all I am doing is slowing,
reversing or stopping the plaque build up. My cardiologist says my Cholesterol numbers are a
good indicator and that repeating the scan after only 3 years will not give me any answers and subject me to more radiation.
Hi Dr. Axel, I’m a 46 year old male with a calcium score of 25. My triglycerides are at 227h and HDL at 36 with VLDL cal at 45. All other blood work is fine other than Eos absolute at 0.5h. Taking a small does of Simvastatin. Is there anything I need to do to better my health here? Is 25 calcium score fine? Just looking after my health knowing my father had a triple bypass around 68. Thanks Axel
Setting the Record Straight on Fats from Cleveland Clinic
Cleveland Clinic has an excellent summary of the new guidelines on fat.
https://health.clevelandclinic.org/2015/02/you-can-eat-fat-if-you-choose-wisely/?utm_campaign=hvi+enews&utm_medium=email&utm_source=hv1503&utm_content=fats+moderation
Excerpts:
Saturated fat: OK in moderation
Animal products such as meat, whole milk, ice cream and butter.
Unsaturated fat: May benefit your heart when eaten in moderation
Unsaturated fat falls into two types — polyunsaturated and monounsaturated:
• Polyunsaturated fats (neutral in terms of heart health) Examples are salmon and canola oil.. Oils rich in polyunsaturated fats also provide essential fats that your body needs but can’t produce itself — such as omega-6 and omega-3 fatty acids.
• Monounsaturated fats provide the most health benefit and are an important component of the heart-healthy Mediterranean diet, Examples are olive oil, sesame oil, and in raw nuts such as almonds or walnuts.
Trans fat: Still dangerous
Trans fats are artificial, man-made substances created by bubbling hydrogen gas through healthy oils. They’re primarily found in processed foods and typically are listed on food packages as “trans fat” or “partially hydrogenated oil.”
Trans fats raise your bad (LDL) cholesterol levels and lower your good (HDL) cholesterol levels. Eating trans fats increases your risk of developing heart disease and stroke. It’s also associated with a higher risk of developing type 2 diabetes.
Thanks Pete
Appears reasonable.
Doc: I think we are looking for some “middle ground”… a strategy that won’t be too far off when the next study comes out that rewrites the rules again. I thought by 2015 Dr. McCoy and the rest of the medical community would have had all this stuff figured out. I know: “I’m not a magician, Spock, just an old country doctor.”
I am 59 years old and had a Calcium score of 6 two years ago. I just had another done and it was 30! From what I have quickly learned from this blog and other googled articles is that “progression” is the problem. Well it seems I have that and now I am nervous. I am a woman with a chronic cholesterol problem (220 – 240)! My cardiologist didn’t want me to go on Statins before the second test, but now because of the “progression” he is advising it. I can tell he is still hesitant but is advising just as a precaution. Is it your opinion that a progression from 6 to 30 in 2+ years is problematic? Thank you for all the helpful information.
Hi Jill,
It staggers the imagination to think that your doctor would put you on a statin “as a precaution”. Statins have never been shown to be helpful for women (if anyone has a study showing this incorrect then I’d love to see it), people with higher cholesterol actually live longer than people with lower cholesterol and statins can have horrific side effects. This study just popped up on my twitter feed – statins are known to cause diabetes; this study says that the number of cases was undereported.
https://www.medscape.com/viewarticle/840884?src=rss&utm_source=dlvr.it&utm_medium=twitter
If it were me (and I know it’s not), I would ask my doctor which specific studies he finds so persuasive that he would want you to go on a statin. And no, saying that it’s the recommendation of NCEP isn’t enough.
Jill: I’m not a doctor, but I would like to add to the discussion and get varying opinions. Here’s what I have from a reliable source-
The Journal of the American College of Cardiology (JACC) has an interesting 2010 article on the subject of statins and CAC scores.
https://content.onlinejacc.org/article.aspx?articleid=1143872
“There remains a need for studies to correlate statin treatment with both CAC progression and cardiac events. The St. Francis Heart Study is the only such trial to date. .. Despite significant reductions in LDL over a treatment course of 4.3 years, there was no effect on CAC progression. There was a non-statistically significant 30% reduction in cardiac events in the overall cohort. However, there was a significant 42% reduction in events in treated patients who had CAC >400 at baseline (8.7% vs. 15.0%), suggesting that these patients might be suitable candidates for future primary prevention statin-CAC trials…”
“So, why have statins been unsuccessful in reducing CAC progression? The AHA model of atherosclerosis, where plaque evolves from a non-calcified lesion to a calcified one, is useful in conceptualizing the issue. It is possible to induce regression of the non-calcified portion of plaque with statin therapy. Whether this is possible with the calcified portion of plaque is unknown. Animal models suggest that a reduction in LDL-C does not decrease the amount of plaque calcification… Pathologically, statins have been shown to promote micro-calcification, which might lead to CAC score increases even when total atherosclerosis is reduced on statin therapy. This argument is bolstered by Burgstahler et al. who used MDCT to assess CAC progression in men treated with 20 mg/day of atorvastatin. They found no effect on CAC progression but did note a significant reduction in non-calcified plaque burden. Also, when statins reduce the soft lipid core of a calcified plaque, the density of the plaque and its Agatston calcium score might increase, whereas its volume might decrease.”
“This might explain why some of the early risk factor studies found an increased CAC progression rate with statin therapy (although a major confounder is that those receiving statins have a history of dyslipidemia). It seems doubtful that the small increase in the incidence of diabetes (a risk factor associated with increased CAC progression) associated with statin use is playing a role.”
Based on what it says above and the fact that you have had a progression of your CAC (even though your baseline score is low), I would guess that your doctor’s thinking is taking into account the following:
1) If your CAC is progressing at a higher than desired amount, it infers that your soft plaque may be increasing. Remember, CAC is not a perfect measure of overall plaque, just an indicator. You could have a zero CAC score and still have plaque that isn’t calcified. CAC progression matters most as a diagnostic test.
2) Statins have been shown to significantly reduce LDLs and plaque. They don’t reduce calcified plaque. They may increase it a little. They think this might be because when the statins reduce the soft portion of calcified plaque, the density increases (which raises your score) even though volume of decreases. Or maybe it just because of statin-induced micro-calcification. Remember it isn’t the calcium that you worry about, it is the total plaque, particularly soft, unstable plaque statins reduce. If your calcium went up a little because of the above, they don’t see it as bad. If it went up because of overall untreated plaque accumulation, that is bad.
3) The doctor may believe your risk of statin-induced diabetes is less than the need to slow, stop, or reduce your soft plaque burden.
I would do everything to reduce your soft plaque progression naturally using diet and exercise strategies. I’m not sure they will measure your soft or overall plaque because it would involve invasive tests. I guess they would see if your plaque progression slowed down after 5 years… maybe. In any case, no test “cures” you. Changes in habits and medicine do. The question as to how you do that is what the debate is about. They are saying statins DO slow plaque progression, (possibly more significantly for those with high CAC scores). I’d like to hear the doctor weigh in on this.
Bob and Pete. Thank you very much for your responses! I have been studying everything I can about this issue and I must admit the information is conflicting and terrifying! As I calculate it, my progression is 400% in a little more than 2 years! I obviously hope and pray some diet and lifestyle changes can help stop this trajectory. I have been tall and thin all my life. But I think this is part of my problem. I haven’t really needed to excerize or diet to loose weight. But I now think I am carrying about 10 extra pounds right in my waist – yes the dreaded abdominal fat AND now I have progressively high calcium scoresI So I know what I must do on the excersize front, but what about diet!! Low fat? Low carbs? Poly or mono? Omega 3 or 6? It’s all so confusing! I have lived a lifetime of eating sugars in all forms and am now learning I have probably ruined my insulin regulatory system. Any suggestion on what a good healthy diet consists of and what foods should never pass my lips. And more importantly is bad diet like smoking- in that I needed to give up sugar a long long time ago because the cumulative damage to my sugar-washed inflamed organs is irreversible!!!! I am now sufficiently scared enough to eat right- if only I knew what that meant!! Any suggestions would be greatly appreciated! And please tell me that I didn’t wait too long to shape up.
Jill
Don’t worry too much about the calcification per se or how to get rid of the calcium or preventing it from increasing further. Calcification will increase as you age. It may be a sign of repair, possibly following some inflammatory process. For example, calcifications are often seen in scar tissue.
So focus on the risk factors and how you can improve your lifestyle ((as you seem to be doing) in order to improve your health and reduce the risk of disease.
Hi Jill,
As you can probably tell I’m not a big fan of taking pharmaceuticals, I feel that for the most part they are prescribed to target risk factors and symptoms which should never be confused with actually curing or preventing a disease. As an example, taking insulin when you’re diabetic does control blood sugar but it doesn nothing in terms of curing the diabetes.
With that said I’m a huge believer in the notion that elevated blood sugar and the resultant chronic low level inflammation is the source of nearly all the chronic disease that plagues our society. And the fix is tremendously easy and effective – stop eating foods that raise blood sugar. Sugar and wheat are at the top of the list.
I know it sounds strange but allow me to explain. Your body attempts to keep blood sugar in a very narrow range – the amount of actual glucose in a person who is regulating blood sugar well is about a teaspoon (roughly 5 grams), that’s a very small amount. Popular dietary advice today is for people to eat smaller meals more frequently with carbs being 50% – 60% of the calories eaten. If your meal is 400 calories and 50% of that is carbohydrate that works out to abut 50 grams of glucose, or 10 times the amount of glucose your body wants to be in the blood. If people are doing that at every meal and it takes several hours for your body to metabolize that glucose by either storing it in your muscles or turning it into fatty acids for storage in adipocytes, your blood sugar will be elevated and bathing your cells in an inflammatory environment for 16-18 hours per day.
The problem is your body can deal with this low level inflammation for a long, long time before actual disease develops but it does eventually develop. But the fortunate thing is that I’ve seen many, many people turn things around from very dire circunstances quite quickly simply by not eating foods that raise blood sugar. Believe it or not but wheat is the worst, even whole grains – it elevates blood sugar higher and longer than even table sugar and I haven’t even mentioned the proteins it contains that we are not genetically adapted to process and probably have a lot to do with autoimmune disease.
So my advice would be to pick up a book on low carb eating and try it to see how it affects your risk factors. If you’re looking at a basic lipid profile I’d be most concerned about the Triglyceride to HDL ratio (anything under 2) and I’d want to have Triglycerides under 100 and HDL over 50. LDL-C and TC don’t seem to actually be good markers for predicting future disease. And that’s it. Your diet has by far the most effect on your health. I feel that a low carb approach typicaly shows the most benefit for most people – if you try it and don’t have success then I’d explore other dietary approaches before going on pharmaceuticals. And again, let me stress that I am not a medical professional, I’m simply a guy who stumbled across the low carb approach, had amazing success with it and gained a large interest in diet and health because of that.
Bob
I meet with my cardiologist this Monday. I will bring with me this blog and some of the links provided herein, Especially interesting was the JACC article that Pete referenced. I plan on saying no to the statins and asking my doctor for his reasoning if he insists! Also. Thanks for the diet suggestions, Bob! I made my first batch of no wheat low carb bread today and it was good! I just hope that oatmeal is still part of a heart healthy diet!
Question,
With so much informative regarding calcium score and the benefits of knowing, why isn’t anyone shedding light on why the values and prognosis the same for anyone starting from 400 to 2000. And if the your score will increase no matter what you do, take,or for that matter talk too,
Continuation,
how can you not think about it.
I am 33 years old; recently i did my yearly lab health screening. And the Lab report says i have high LDL Cholesterol Calc which is 109. Is it too high? Should i see doctor or do anything about it. Recently i have high heart beat rate at night when i go bed. You advise is really appreciated. Thanks
Sorry but I couldn’t not comment on this.
First off, with a standard lipid test your LDL-C is not measured, it’s calculated using a rule of thumb called the Friedewald Equation. This rule of thumb has been shown to inaccurate, particularly if you have triglycerides under 100 or over 400. You score of 109 is barely high and certainly within the possible realm of being normal (whatever that may be).
Second, LDL-C is a terrible marker for your heart disease risk. I know many people think it’s so but LDL-C is often discordant with heart disease risk. I’ve posted a study earlier showing a study from the NHANES III data that shows you are just as likely to have heart issues with LDL-C under 100 than over 100.
Third – A “normal” LDL-C has been steadily lowered over the years by NCEP despite there being no data to indicate this is correct. What lowering the normal range does though is put more people on statins, drugs that show no benefit for overall mortality and increase your risk of getting diabetes, Parkinson’s (this study just came out), liver problems and muscle issues.
Fourth – if you only have a basic lipid profile done and don’t know either your LDL-P (total number of particles) or your LDL pattern, the best rule of thumb is to look at your triglyceride to HDL ratio. Anything under 2 is good. Example – TG of 100 and HDL of 50. Also I would be concerned if my TGs were over 100 or my HDL was under 35.
Hi Doctor,
There have been a lot of contradicting information concerning calcified and non calcified plaque rupture, is calcified plaque considered more stable? While non calcified more prone to rupture? I have been going through some recent research saying that this isn’t true.
Secondly, the percentile ranking is so contradicting and variable from one source to another, I am 40 and my score is 7, what is my percentile rank?
Moussa: Send us a link to your contradictory info relative to stable and unstable plaque. I guess you know the percentile is different for males then females. MESA scoring starts at age 45: https://www.mesa-nhlbi.org/Calcium/input.aspx
I have some questions about the calcium score. My friend is 42 and he just got a score back that was 917! Yes, 9-1-7!!! He only had the test done because his mother, who just had her score done, was over 950 and heart disease runs in the family. His uncle had heart surgery at age 45 so his mother was rightly concerned.
He is scheduled for tests in a couple of weeks. Shouldn’t tests be done sooner? He is against medications but won’t medications be required to extend his life? How serious is this as I am worried because he has an 11 year old son. Can diet make a difference – his doctor said no, none of this can be reversed? What does the future hold for such a young man and did his past (alcohol, recreational drugs, bad food for a couple years) contribute to this or is it that plus the genetic hand of cards he was dealt?
I have so many questions. Thank you for this website! I’m sure you overwhelmed with the comments. You are serving so many people and your website has a nice look, reads well, and is informative. Thank you very much!
PS- I read the August 2014 article you posted about calcium score.
Thanks again,
Rebekah
Rebekah
If I understand you correctly your friend is asymptomatic. Therefore I believe two weeks are okay. Nothing suggests this is an emergency.
Of course your he needs to be evaluated by a specialist and he may need some additional tests. Of course there’s a lot he can do in terms of diet and lifestyle and sometimes medications can help to reduce risk.
I’m following a many relatively young people with coronary calcium score in this range and higher and most of them are doing fine.
Thanks for the kind words about my website.
Thank you. His follow-up is some 5 hour stress test and I’m sure there are other tests as you suggest.
One thing I thought I asked but possibly didn’t: He had an issue once with drugs at one time. It was at least 10-15 years ago. I’m not saying this caused it but what is the likelihood that it contributed to it? should he be blaming his past, even if it was a long time ago?
Thanks again!
Rebekah
White female with sign family CAD: early ONSET MI both father & brother both under 50. Mother/sister/myself have HTN me/mother hypothyroid under 50. In 2011 had incidental finding on CT Lungs of significant coronary calcification. Had CT calcium score scan & at that time in 2011 I was 43 with score >2600!!! (Radiologist recommended MIBI at that time) significant calcium in LAD & RCA, saw cardiology did Echo/treadmill stress test & holter. All tests inconclusive & at that time was already on HTN/Thyroid meds he suggested statin be added tried both Crestor & Lipitor & both caused excruciating leg cramps and not continued. Cardiologist didn’t have worries on my calcium score (HUGE RISK!!!!!!). Was told if something happens in the future we have a base of tests to fall on, not what I wanted to hear:( Developed severe angina on vacation Dec 2014 in different country, was given angio & told I have coronary aneurysyms in both my left & right CA’s!!!! Very rare, the cardiologist in my country involved his team of 15 to view my films from vacation. His decision was to have MIBI & IVUS to look closer to an aneurysyms that appeared shaded & his concern was thrombus/dissection/occlusion. I was started on Coumadin following the ACS and my doc changed to Xarelto. The MIBI showed no ischemia and/or infarct, great!!!! The report notes a tiny narrowing at apical other than that no other comments noted about calcification and if any narrowing? I spoke with cardiologist & was told to continue meds and he had cancelled the IVUS??? Told me I just had funny aneurysmal arteries…..I did not find thus at all to be funny. He will do no further cardiac diagnostics & will see me in a year or sooner if concerns. I did not get any further rationales as to why the angio was discontinued? I am very high risk for family/personal factors. Can MIBI show actual percentages of narrowing in all the coronary arteries? I am missing something huge here …….. Just having to be on anticoagulant therapy long term is causing great stress as I am also anemic thereby increasing my risks further with potential to bleed. Any information about coronary aneurysyms & treatment options? Greatly appreciate feedbad
For those asking about diet/alternative impact on calcium score.
I am not an MD just a high cholesterol (a year ago: CT 369mg/dl, HDL 105mg/dl, TG 81mg/dl) dude but without family history of early death due to heart disease (only a heavy-smoker uncle) so I am not getting any calcium score done. At the RCT level I am not aware of any study so Dr. Sigurdsson’s advice. This being said I have chosen to follow almost all pieces of advice derived from the Track Your Plaque experiment tank, those using annual Agatston scores in order to refine the methods to decrease the calcified plaque considering it the best available proxy to track cardiac risk. Their somewhat internally challenged strategy is outlined in this blog post from Dr. Dach. You may take a look at Dr. Davis’ video and comments on Ivor Cummins’ post. Dr. Davis published some results back in 2009. Also it is not so important to reverse the score because slowing its increase may be enough as I have commented before (relative risk of 17.9 —95% confidence interval of 4.3 to 74.2— of those with an annual increase greater than 15% with respect to those with an increase lower than 15%). Dr. Davis seems not to see heart attacks in his diet-complying patients anymore. At the one hand without RCTs of course it is fairly speculative. At the other hand it empowers you through being able to track your personal results of the biomarker (CAC-score annual variation) with highest correlation with coronary events.
My first Cholesterol test was done when I was 28, and it was 250. I have always been concerned about that number. I am now 71 years old and my cholesterol readings has remained at 250, except when my doctor started me of Lipitor. I had a terrible reaction to it and after extensive testing it was determined that I was allergic to Lipitor. I am a research scientist and have gone through the literature extensively. Essentially all the “published” adverse effect rates are way under the actual number, since doctors, in general, don’t report the adverse reactions, which they are required to do. Too much paperwork. Several studies suggest that the real rate is about 30%. There is a real risk that anyone will have an adverse reaction. Now at 71, I had a calcium score performed and the result is 0. Yes zero! I have all the scans and have analyzed them myself, since I ma a physicist and understand x-ray physics. Then my cardiologist suggested a Lipoprotein-a test, now believed to be a “sticky” type of lipoprotein, and the result is that I am less that 10. Below 50 is desirable. And your lipoprotein-a level is genetic and cannot be modified by statins, exercise, diet, etc. It is like having blue eyes, that’s it, the color is not going to change. So for a person like myself, medical research and physicians do not have a way to relate cholesterol to calcium score or echocardio results or radio stress tests. Had them all performed. Good and negative results. Summary, there is no predictive causative relationships that have been developed and proven to work in all cases. So, eat healthy, drink in moderation, and if you experience any signs of angina (chest, shoulder, neck, jaw pain) or overall weakness or any other symptom that you are concerned with, see your doctor immediately. They can fix many problems, but don’t dwell of numbers that are not definitely proven to be future predictors of heart disease, which there are many types of. My sister, at 78, now has afib, and has just had a pacemaker implanted. Her arteries are fine, but the nerve signals in her heart are not functioning correctly.
Chest CT came back with new findings. This is just 6 months after previous CT. Is this cause for concern or something that has been there and noted by Radiology. Extensive coronary arterial calcification and mild athermatous. Calcified right hilar lymph node likely reflecting prior granulomatous. Diagnosed 2012 with Lupus. Hypertension was difficult to control during major flare in 2012. Cant take statins (metabolic myopathy).
Hello. I just stumbled across this page & discussion. I just got my coronary calcium arterial score back today of 394. I’m on 20mg lipitor–been on it since about 2005. I’m only 44 yrs old. I have an appt Monday with a Cardiologist. Father just had a quadruple bypass on Feb 17. Am I doomed? What’s your advice? Thanks Michael
I just had a calcium score done because my father had congestive Heart Failure. My score was 28. I am 43 with low Cholesterol 129, My blood pressure is 123 over 83 (I am on a BP Med) and about 80 lbs over weight. I do try to walk often and I eat a very solid heart healthy diet. My weight is down about 18 pounds and dropping andI have increased the the exercise a removed sugar and most breads. My concern is that my DR has put me on 10mg lovastatin. I am concerned about the side effects of the med and is it really necessary. After ready the blog, i am going to start taking k2. Any advice would be helpful.
MF
Most people tolerate statins very well and 10 mg Lovastatin is a relatively low dose (side effects are less likely with smaller doses).
You seem to have adopted a healthy lifestyle which in my opinion is a key issue.
How much lovastatin will add in terms of risk reduction is difficult to tell and one will need to see the whole picture, lipid numbers, family history, smoking etc.
I assume your doctor has come to the conclusion that statin therapy is likely to be of benefit in your case.
To say that most people tolerate statins very well seems misleading to me. Side effects are vastly underreported and if a patient does complain the doctor will more likely than not chock it up to the person getting older and not the statin. I think it would be very prudent to see how MF’s change to reducing carbohydrates affects his lipid profile and it wouldn’t hurt to have a C-reactive protein test done to check on inflammation. I have little doubt the reduction in carbohydrates will benefit his blood pressure as well. Lifestyle changes should always be given time to work before pharmaceuticals are prescribed.
Just because his doctor advised him to take a statin doesn’t mean it’s a great idea. Doctors prescribe a lot of things that may cause more harm then good for a variety of reasons. If his total cholesterol is already very low then how does it make any sense to take a medication that will drive it any lower? If would havebeen nice to see what MF’s HDL and triglycerides are, w/o that basic knowledge I don’t see how there would be enough evidence to know whether a drug should even be considered.
Bob, I disagree.
I’ve been prescribing statins for more than 20 years. I’ve followed patients for years who have been taking them regularly. So, I think my experience as well as scientific data will allow my to say that most people tolerate statins very well.
By that Im not saying that everybody should take them and that the risk of side effect is zero.
There is a responsibility involved in advising people through a blog page. My relationship with people who comment on my blog is not a doctor-patient relationship. Advising someone not to trust his own doctor without knowing the whole history and all the details is in my mind highly irresponsible.
I’m in no way trying to be rude but I think it would go against human nature to affect a behavior for 20 years in hopes of doing good for others and then be able to admit that it might not have been a great idea. That’s simple human nature and we’re all affected by it.
I don’t understand how a man with a total cholesterol of 129 could be prescribed a statin when the miserably small benefit of statins has always thought to be due to its cholesterol lowering properties. Adminstering a statin for the purpose of lowering cholesterol to a man with already low cholesterol in effect opens him up to all the risks associated with statins and none of the benefits. How is this reasonable, let alone ethical, when MF has shown the desire to work hard on lifestyle changes?
Statins don’t only exert their benefits through lowering of cholesterol.
But I agree with you Bob, I would not treat someone with a total cholesterol of 129 with a statin drug, at least not in primary prevention. But are you sure this is his total cholesterol? If so, is it before or after he was put on statins?
As always, you will need exact information in order to be able to give advice.
Thanks for all the feedback. I am concerned because of the risk of Diabetes and the other list of side effects. As part of a healthy lifestyle, I only have a few beers once or twice a week, but I worry about the effects on the liver. I don’t smoke . I do have a cigar once a month give or take. My HDL is low at 32. Will the statin reduce the build up of plaque? I started to take k2 vitamin. Is that proven to be helpful? Thanks again
MF. K2 has not been proven to be helpful. To my knowledge, the hypothesis hasn’t been tested in a clinical trial.
Can I ask you what your total cholesterol, LDL-C, HDL-C and triglyceride levels were before you started taking the statin.
My triglycerides were 79 LDL 94 HDL 32. My cholesterol has always been in that range. I don’t have my most recent numbers. My cholesterol was the same and my triglycerides were lower (I believe in the 50’s)
So. I guess Bob’s right. Would be very hard to recommend someone with such a low risk lipid profile to take statins despite the slight coronary calcium.
I just got done reading an article at https://www.medscape.com/viewarticle/842499 that says that statins seem to promote calcification, no matter what dose you are on (low or high). But they are saying it may be a good thing because atheroma volume goes down in these same patients… so maybe the existing plaque is stabilizing. Whew! Didn’t think they would come up with that one. I guess they measured the atheroma levels by doing an ultrasound of the carotid arteries. That’s not a perfect test either. They go on to say that the action of statins is not well understood: “We know the drugs have complex biological effects, and some of those effects have not been worked out scientifically.” So anyway, progression of calcification after statin treatment is not a good measurement of heart disease. They are saying that statin treated patients need only the baseline test and a second test is well… maybe useless.
So now I’m thinking that CAC scores that are non-zero only tell us that the person has some plaque. Maybe a lot of soft plaque. Maybe none. Maybe it is all stable. And maybe the person with a zero score has no plaque, or lots of soft plaque. And the person with a score of 20 at age 70 may have less soft plaque than the zero score person, (because all their plaque is stable). But the person with the CAC of 20 may have a significant amount of soft plaque and a small amount of stable plaque. Hmmm. So they look at your carotid arteries with an ultrasound to determine intima-media thickness. That’s used to estimate atherosclerosis elsewhere, as well as regression or progression. Oh no! They also say the thickness can be influenced by other factors besides atherosclerosis.
So I’m 66. Started with BP of 110/70, no history in my family of heart problems, asymptomatic, active, eat well, CAC of 17, great stress test and nuclear stress test results, starting cholesterol of 146, HDL of between 70-80… I’m put on statins (10 mg Pravastatin 3 times a week). Cholesterol falls to 127 in a few months. HDLs stayed the same. So now I don’t know what to wish for… higher or lower CAC. If I die of heart disease or they do an autopsy after I die of any cause, they will get an exact measurement of plaque. It will be too late to come up with a better treatment plan at that point. I think I read too much. Maybe I should get a dog. They say people who have dogs are happier and live longer. Do you think Crestor is a good name for a dog? “Come here Crestor. Down boy. You’re a good boy, Crestor. Daddy’s on the floor. Sit down on Daddy’s tummy.” Yeah! Get down with Crestor!
Thanks for the comment Pete and for mentioning the recent publication addressing plaque volume regression, coronary calcium and low vs. high dose statin therapy.
,
Below is a link to the paper. It’s not open access but there is a good audio commentary from Valentin Fuster, the JACC editor, summarising the results of the paper as well as an accompanying editorial https://content.onlinejacc.org/article.aspx?articleID=2211958
my score, is 400plus. dense, calcium. in arteries, am 81 old white, male had,a AAArepair. 25 years ago
I am a 68 yo mail with a CAC of 9,400, more than a 100% increase since Oct., 2011, when the first test was performed. The first test was conducted incidental to a cardiac cath and I was unaware of the test, or the results until obtaining and studying medical records during a more recent incident.. BP is generally good. I exercise five times a week on average using the treadmill and can do 200 pushups in three sets, take plenty of vitamins and supplements and have reasonably good died – never fried food, or foods with high fat. LDL and HDL cholesterol are nearly even in the 70s and triglycerides are below 100. At 68, I thought I was in decent shape until learning of this tests and repeating it to find a tremendous increase. Cardiologist says it is irreversible. Available literature on internet give a grim prognosis for this type of score. Any suggestions on reversing the calcium level would be most appreciated.
I don’t understand the scores. Mine was given as a percent of blockage.
Wulf
Percent blockage describes the degree of narrowing in an artery, it doesn’t tell you anything about the amount of calcium. Coronary calcium score reflects the amount of calcium within the walls of the coronary arteries. It doesn’t say anything about the degree of blockage.
However, persons with high calcium score are more likely to have severe blockages than those with low calcium scores.
I have been very active since Jan 2015, working out every day for an hour or so and have lost 15 lbs. I feel great and can fit in my 36 waist jeans now with out the muffin top. I have a gym available for my use where I work and that makes it very easy to get my exercise. I noticed that before working out, my BP was 155/90. So I paid a visit to my family physician and they were surprised at my bp level. I was put on 25 mg of Losartan and now my PB is around 110/65, big difference. I was told to get a CT calcium score scan. I get a call from my family physician and all they said was that I should make an appointment with a cardiologist sooner rather than later. Ok. I have a score of 430. I don’t know what that means but I make an appointment with a Cardiologist. I get to the cardiologist appointment and get an EKG, that checks out ok. I get a sonogram and that checks out ok. He says that I have a strong heart muscle. Then When he’s about to release me, I mention the calcium score data, and he does a double take and says, “That’s kind of high for someone at your age of 46” So, He puts me on a daily 81 mg baby aspirin regiment for life, and prescribes 5 mg Crestor and orders a Nuclear Stress Test. I guess I’ll wait until after the stress to get really worried. It sounds pretty scary. I’m just worry about the side effects of Crestor. Or is the risk of heart attack greater than the risk of Liver failure?
Hi I had one of these tests done and my score was 5. I have to say this has got me worried as i’m only 44 years old. My cholesterol and blood pressure has always been fine and i exercise 3 times a week. I have a family history of heart disease, my father had his first heart attack aged 46 and my mum was 57 when she had one. If the doctor said to me this was normal for someone my age i don’t think i would be too worried, it’s just that she wants me to go on statins and aspirin. I’m worried also what long term effect this may have.
Some advice please…I am a 52 year old male, 6 ft tall 170 pounds with low body fat, exercise 4 – 5 times per week (including running, weights and teaching two aerobics classes), cholesterol and blood pressure normal, don’t smoke, parents lived to their 80’s…and received a cardiac calcium score today of 300. How can this happen? This is quite a shock to say the least. The radiologist said I should “reduce my risk factors”. By doing what exactly? Any advice?
I just received my CT Cal score- 400 plus- and would like to know if taking Calcium 1800 mg per day would affect my score? The reason I take the Calcium is due to having sleeve surgery about two years ago. I have lost 100 pounds. When I had my annual physical last week I brought up the CT Calcium score test to my Dr. and he agreed it would be a good idea to have the test. All of my blood test were good. I don’t take 81 mg aspirin anymore due to the sleeve surgery. My primary Dr. called and he is setting me up with a cardiologist for a stress test. Does this sound about the normal protocol for this..??? Thanks Monty…
Yes Monty. In my opinion a stress test sounds reasonable.
Hi Dr. Sigurdsson,
Thanks for the insights and excellent information. It’s comforting to find someone like you out there to help make sense of it all.
I’ll start out with the bad news. My total calcium score is 1689. I found this out two months ago after my cardiologist recommended a coronary artery calcium scan. I’m 67 years old and have been on statins for 25 years. I’ve been a vegetarian since my 40s and have been diligent about maintaining a healthy diet, i.e. egg whites, whole wheat breads, minimal dairy, moderate exercise, the whole nine yards. I have a positive outlook on life, am active in my work (film production), play music, look young for my age and feel fit and healthy.
Both my parents died of heart disease but I have to say this news floored me. After the scan, my cardiologist suggested I add 10mg of Zetia to my daily dosage of 40mg of Crestor. Within five days, my cholesterol dropped 40 points to 144. He then suggested an echocardiogram. That revealed some aortic sclerosis but otherwise good. Then he recommended a stress test which also went well. After those results, he added a daily intake of 25 mg of Metoprolol.
I see him again in two months and, at that time, he said he would probably increase the Metoprolol to 50mg a day. I get it – he doesn’t want me to have a heart attack or stroke. Neither do I. And he’s being cautious by pursuing non-invasive therapies. That being said, g
iven your thoughts on arterial narrowing and whether or not they are present in someone with elevated calcium scores, would you suggest an angiogram? And what’s your view on plaque regression? Would an accelerated exercise regimen (more than 150 minutes a week) help reduce the amount of plaque in my arteries?
Thanks in advance. Jim
Hi Jim,
Forgive me for sticking my nose in here, I know you were asking for Dr. Sigurdson’s advice but it’s just that I see all the comments on this thread and it’s a bit frustrating to not say anything.
Reading your comment it’s very apparent that you’ve gone above and beyond what your doctor and conventional wisdom would require for good health. A boring diet, drugs, endless exercise – and yet you still have a poor coronary calcium score. Is there any point where it might be appropriate to sit back and ask “Am I going about this the correct way”? If your approach of 20+ years has left you unhealthy, is it a good idea to think that adding another medication or going another 20 minutes on the treadmill is going to be the magical breakthrough? Results ultimately are all that matters and your results have been pretty poor. At what point does a person begin to suspect that conventional wisdom and pharmaceuticals might actually be the cause rather than the cure? At what point does someone say “Doc, in the 20 years I’ve been seeing you I’ve gotten worse and worse, you’re fired”.
I’m a huge fan of a low carb diet, not just because it personally works for me but because there is an overwhelming amount of data showing it’s great for heart health. It’s scary going against conventional wisdom and possibly doctor’s advice but I’ve seen way too many people do just that and have tremendous success. Anyhow, sorry to butt in and I wish you all good health in the world.
Bob
Hi Bob,
Thanks for your comments. I don’t look at my life that way. Yes, I have an elevated calcium score but by all other measures, I’m very healthy. It’s interesting how you characterize the way I live: “boring diet, drugs, endless exercise”. First, I don’t consider my diet boring. I’m fortunate enough to be able to live near and afford to buy fresh fish and vegetables from a farmers’ market. I eat delicious food every day. Second, I don’t exercise endlessly. I try to get in 30 minutes a day five days a week on an elliptical. It helps me stay in shape, keeps my weight down and, maybe most importantly, keeps me in a good mental state. It’s meditative for me. As far as the drugs go, maybe the statins have contributed to my arterial calcification. Maybe they’ve kept me alive this far too. Both my parents died of heart disease and I had four uncles and a cousin who died of heart attacks in their 50s. So, at 67, I consider myself ahead of the game.
Jim
There’s so much we don’t know yet about coronary calcium. The fact that it is associated with risk doesn’t necessarily imply that calcium itself is bad. In fact, calcium may reflect a healed or repaired plaque.
The association between coronary calcium and statin therapy is also a bit controversial. A recent study suggested that statins may increase arterial calcification at the same time they seem to reduce plaque volume/size.
It’s not really for me to tell whether you should have an angiogram, that’s for your doctor to decide. A raised calcium score in itself is usually not a reason to perform coronary angiography. That decision is more often based on symptoms and other tests such as exercise testing etc.
Dr. Sigurdsson,
Thanks for your reply. I appreciate the information.
Jim
I had a calcium test done 7 years ago my score was 750 . I have been on a 40 mg of simvastatin, for 12 years, I went to a heart doctor who claims I should be on a stronger dose. I tried Lipitor which made me feel awful. I then switched to Crestor which also made me feel awful. I’m questioning the entire statin regime. I had a great stress test. What is your opinion?
bob what would suggest?
Hi Howard,
I’m a huge proponent of a low carb diet, it’s great for lowering inflammation brought on by elevated blood sugar (your blood sugar will drop like a stone, HbA1c will improve quickly) and alleviating metabolic syndrome and insulin resistance. I believe that heart disease is caused by continuously elevated blood sugar on the endothelium of our arteries and that if blood sugar is reduced to normal levels (around 80 mg/dl) the endothelium will have a chance to heal properly. And if you’ve been reading Axel’s blog you know that metabolic syndrome/blood sugar abnormalities are highly associated with all chronic disease that currently plagues our society. Axel recently did a post on low carb that discusses the new information on the topic and is recommended reading.
https://www.docsopinion.com/2014/07/29/fat-carbs-metabolic-syndrome/
If Axel will forgive me for promoting another doctor’s blog on his own, I would suggest visiting the “Track Your Plaque” blog run by Dr. William Davis, the author of Wheat Belly. There’s a lot of information there and he discusses coronary calcium scores quite a bit if you go back through his blog posts. It certainly can’t hurt to sample different opinions from that of your doctor.
As an avid follower of many paleo and low carb doctors and blogs, I know a tremendous number of people have success curing their crippling chronic disease just by changing their diet. I’d urge you to look into it before upping your medications. The goal of medicine should be to eliminate medications, I struggle to understand why people are comfortable following advice that tells them what they need is ever-increasing amounts of drugs.
Bob
Thank you for the advise. I’ll be in touch and let you know my progress. Howard
I am a 47-year old male who just received a calcium score of 348, with borderline high cholesterol, but otherwise healthy, a non-smoker who exercises some but probably not enough. I am taking 20 mg of simvastatin daily. Any thoughts? I know I should exercise more and be a bit more careful with my diet. Should I increase the simvastatin dosage to 40 mg? Thanks, Brent
I wouldn’t.
https://www.ncbi.nlm.nih.gov/pubmed/?term=Statins+stimulate+atherosclerosis+and+heart+failure%3A+pharmacological+mechanisms
I am 69. I had a coronary angiography CTA done 6-10-2015. My calcium score came back at 1694. I am a Type 2 diabetic with no chest pains. I run 30 minutes a day, which I started doing 3rd week in March this year. I had 21 lesions on my LADCA and 347 lesions on my RCA. Yet, Matthew Budoff MD of Harbor UCLA noted in Impression: “CT pulmonary angiogram without embolism. Normal Aorta. Diffuse atherosclerosis, no severe disease.” This conclusion seemed strange to me. Isn’t 1694 high on a calcium score. Stenosis in all arteries was less than 50 per cent, with a 50 to 70 per cent on the first diagonal vessel off the left anterior descending CA. I was not told what to do next except keep exercising and watch my diet. If I am going to have a heart attack any day I would like to know. Should I get further testing? Thanks for any info.
I am a family medical practitioner. Common sense unfortunately isn’t common. I think tests should be done for good reasons, not for the worried well. Symptoms and risk factors are the important criteria.
Calcium in the arteries simply reflects arteriosclerosis, a process that will be more common and widespread as we get older, It does not measure whether there is significant narrowing inside your artery.
Let us look and do a score of risk factors and ask about symptoms and do whatever is neccessary to reduce risk and evaluate symptoms(not a calcium score on your heart arteries)
My suspicion is that calcium scores on arteries being done is a radiology / radiologist driven investigation. If people have symptoms that warrant it , do tests reflect blood flow through arteries to detect significant narrowing for possible stenting. If people have a high risk profile and no symptoms – stop smoking , lower blood pressure , control diabetes, improve cholesterol profile and exercise and eat healthily.
Harald: But people with low cholesterol and no known risk factors find out they have a problem after they’ve had a heart attack and I have read that half of those that have heart attacks had what was considered healthy levels of cholesterol. As I have read, arteriosclerosis can set the wheels of atherosclerosis ,in motion. The site owner says: “The presence and extent of coronary calcium are first and foremost markers of the extent of atherosclerosis within the coronary arteries.”
If you are a middle age male, it would seem cholesterol testing, inflammation testing, nuclear stress testing, sonograms of the carotids, ecg, heart rate, blood pressure, and coronary calcium tests would, together, give a person a good idea of where they stand and a way of measuring the affect of health measures adopted. Of course, tests don’t cure anything and people should adopt healthy habits anyway, but it seems coronary calcium tests still would have a place in assessing heart health.-Pete
https://www.health.govt.nz/system/files/documents/publications/cardiovascular-disease-risk-assessment-updated-2013-dec13.pdf
Hi Pete.
You are right about cholesterol not being the only or even the most important indicator.of cardiovascular risk.
The link above has a lot of evidence based information. I’d like to refer you especially to the table re males page 6. This is a good summary with a 5 year predicted risk calculator that is increasingly being adopted world wide. Men and woman tables are different. It doesn’t seem fair but all other things being equal our risk as men is higher. The problem with oronory calcium scores is that they don’t relate to arterial obstruction and some people with marked calcium deposits especially older people have no significant arterial narrowing ( a bit like the person with normal cholesterol but still high cardiovascular risk). Calcium scores go up with age and heart attacks and strokes go up with age – so this test in my opinion tells us very little. One in 4 deaths in the developed countries is due to cardiovascular risk (heart attacks and strokes) – more than all cancers combined (20%). I guess unfortunately as you get older something will get you in the end.but it is about reducing risk based on factors that we know are important in asymptomatic patients and about investigating those with established disease to see whether medical or surgical treatment is needed.
Regards
Harald
You are right about cholesterol not being the only or even the most important indicator of cardiovascular risk.
Or more likely not of any importance whatsoever. 🙂
But I agree with the idea that it’s unlikely a single CC scan can give you meaningful information to act upon. I’ve lost count of how many people in this comment section have said “Here’s my score, is this good, bad or what? What do I do with this?”
I think it’s a somewhat useful test if a baseline is established and you have it done every couple years to see how your score is trending. Other than that though, it’s hard to see the usefulness.
My calcification reading is 896 found that out on Thursday and I am having an angiogram tomorrow.
Really haven’t had any symptoms, just a check before I had a shoulder replacement
Am very confused about the predictive value of calcified and non calcified plaque.. I read few articals mentioning that it’s the non calcified plaque is the one that ruptures and cause MI, i also went through some studies saying that calcified is as dangerous and non calcified, as calcification increase the sheer stress on plaque etc… Where is the truth? I am 39 male my score is 7, I have only calcified plaque as shown in my CT angio.. Normal cholestol, normal BP and not diabetic… I use to smoke 2 packs per day for 15 years.. Am I at elevated risk?
I had a calcium score of 150, age 65 and ardent weight lifter and vegetarian for many years, my doctor put me on statins because my cholesterol levels were 209, I took them for about a month, the cholesterol level did drop, but the amount of cramps and charlie horses I experienced were too muh to bear, I took myself off them and continued my lifestyle…pharmaceutical companies and doctors don’t want you to get well, they want customers that will continue taking their often fatal pills…have no trust in doctors in general or the pharmaceutical companies, so I opt to go the natural way, herbs and plants, and wholesome foods……
Soooo should I be overly concerned??? My age is 56, female, Non smoking, normal Cholesterol, Lipids, and Blood Pressure. Don’t eat red meat, some exercise, no diabetes or obesity (although it wouldn’t hurt to lose a few pounds), long family history of CAD, sister, father, grandmother… Strokes, Stents, in their 50’s. Elevated CRP 17.2(even after Methotrexate and Naproxen), Elevated Homocysteine, Positive RA Factor but negative ANA, CAC Score of 116…… Cardiologist just added Lipitor to my list of meds..
I’d be curious to know what your triglyceride and HDL levels are. Saying lipids are “normal” isn’t enough info. Axel did a post on the triglyceride/HDL ratio – it’s a much better marker for heart disease than LDL-C or total cholesterol.
https://www.docsopinion.com/2014/07/17/triglyceride-hdl-ratio/
Axel recently did a post on the the efficicacy of statins in women w/o known heart disease – the upshot in my estimation would be to skip the Lipitor and perhaps look for a new doctor. Anyone who suggests a treatment that will provide no statistical benefit and possibly expose you to side effects isn’t worth your time.
https://www.docsopinion.com/2015/04/14/statins-for-women/
To me the most important marker for health is whether or not you have metabolic syndrome. This marker is predictive of just about every chronic disease. It’s a measure of 5 different things – having 3 of them means you have metabolic syndrome (I would be concerned if I had any of the 5). They are:
Triglycerides over 150 (way too high in my estimation, I’d shoot for under 100)
Low HDL (under 40 for mean and under 50 for women)
Abdominal obesity – do you have belly fat
High blood pressure
High fasting blood sugar over 1000 (my personal thoughts on this is that fasting blood sugar is a poor marker, I would test the HbA1c score or fasting insulin levels instead).
If you have metabolic syndrome the best way to fix this is with diet (medications that attack markers don’t actually fix the underlying problem, they simply make a marker look better which is pretty dumb). I would recommend a low carb diet, others would recommend a Mediterranean diet which I believe is too high in carbohydrate content. The best thing to do would be to adapt your diet to one of these and see how your metabolic syndrome markers change. If they improve but still aren’t great, keep lowering the carbohydrate content until your numbers are pristine.
LDL – 101, Tryg – 125, HDL – 56, glucose – 95, no belly fat, no high blood pressure, pretty sure I have not had a HbA1C in a while but I do remember that it was normal the last time I had it done.
Personally I would consider the trigs to be high-ish, the HDL is fine (but over 60 would be better) and the fasting glucose to be concerning. As I mentioned before I believe fasting glucose to be a poor test because there are plenty of people who after a night of fasting can show normal glucose but require abnormally high amounts of insulin to get it there, which the pancreas is still capable of creating. Fasting glucose measures the best case scenario which is why the HbA1c (the measurement of your blood glucose for the past 3 months) or fasting insulin (how much insulin you’re producing to get to your best case blood glucose) would be much better measures of how your body is managing glucose. At 95 I think that’s high and I would be concerned. I would change my diet (meat and saturated fat are fine, btw) and consider some intermittent fasting to work on getting your glucose in better shape.
Just for a reference, I eat a very low carb diet and my numbers are:
Trigs – 55
HDL – 66
Fasting glucose – 86
Fasting insulin – 6.9
CRP – 2.56
I actually think I should do better on the insulin and CRP so I’m switching up my plan a bit to include more intermittent fasting – basically just skipping breakfast a couple days a week.
Obviously I’m not a doctor, I’m just a very interested layperson who thinks that the conventional wisdom for health and chronic disease is flawed.
“Obviously I’m not a doctor, I’m just a very interested layperson who thinks that
the conventional wisdom for health and chronic disease is flawed.”
Obviously! You’re just a nosy-parker who wants to criticise someone, based on your latest crack-pot hypothesis.
I am 44 and a kidney transplant patient 2x. I am seemingly very healthy and eat well and exercise regularly. Play basketball twice a week as well for about 2-3 hours at a time. LDL – 93 HDL – 52 Triglycerides – 63 Glucose 90 . But I got a CT scan for a lung infection and my Calcium score for my heart came back at 800! They put me on Statins but my body does not handle them well. So I can only tolerate(if thats what you want to call it because it still makes me feel miserable) 5 mg Crestor. I have had 3 stress tests in the last 18 months and all came back normal. I kind of wish I didn’t know the score because I don’t think the stress of knowing you are a ticking time bomb helps! Is there anyway to reverse this or am I just stuck with it? How do they come up with these %’s? 25% chance I will have a major cardiac event in the next year?
Also, I have begun taking Niacin, L-Arginine, C, D3, B12, Fish Oil, Flaxseed Oil, Magnesium, Co-Q10 in the last several months. Is there any benefit to these supplements?
I had a bout with diverticulitis late last year and had a CT Scan. One of the observations was “prominent coronary artery calcification. I had a follow up CT scan specifically to determine coronary artery calcification and received the following scores: left anterior descending: 509, circumflex 170 and right coronary artery 35. Has anyone been diagnosed in these ranges? My primary care doctor prescribed a statin – I’m skeptical that this will help. I have been evolving into a plant based diet because I have heard it can “reverse” the coronary heart disease. Dr. Esselstyn of the famous “Forks over Knives” is an advocate of this “therapy”. Anyone else pursuing this? Thank you.
The funny thing about the vegetarian diets promoted by the low fat, no meat advocates is that these diets don’t just eliminate meat (and perhaps dairy), they eliminate a lot of foods that you won’t find in a good, low carb diet either. In the case of Esselstyn he eliminates vegetable oils, refined grains, white
flour, and products made from enriched flour such as bread, pasta,
bagels and baked goods. None of these are eaten by people following a low carb or Paleo diet either. So is the benefit you see from Esselstyn’s diet due to not eating meat or is from not eating crappy carbs? I would say it’s the latter and the diet would be even healthier if you included meat, dairy and both saturated and monounsaturated fats.
I would say to choose a diet that eliminates cruddy, refined carbs and rancid vegetable oils and is one you can stick with. I think you get much better nutrition in a diet that includes meat and dairy but if that’s not your thing then follow Esselstyn’s – just stop eating foods that raise insulin resistance and inflammation.
Excellent analysis and observations. To be honest – total elimination of animal protein is somewhat extreme. It seems that salmon and other Omega 3 rich fish provide good nutrition. I concur that inflammation causing foods are probably the primary cause of CAD (that and genetics). A new study was published in January in the Proceedings of the National Academy of Sciences that directly linked a sugar found in red meat (Neu5Gc) to inflammation of blood vessels. Looks like they finally found the smoking gun. I guess our knowledge evolves. Thanks for your response – it is appreciated.
I hadn’t heard of that study before but after looking into it but w/o doing a thorough reading of it I have a couple of comments right off the bat. The first is that it’s a mouse study and applying the results of mouse studies to humans is problematic. The second is that every low carb study I’ve seen that studies inflammation shows a lowering of inflammation levels, which would indicate that eating meat does not have a significant effect on inflammation.
This blog post by Dr. Peter Attia talks a bit about this in a study done on humans.
https://eatingacademy.com/books-and-articles/good-science-bad-interpretation
A 53 year old doctor and 15 year low carb diet enthusiast just announced his CAC score – Zero.
Just how long is it before the supposedly bad effects of a low carb, high fat diet are supposed to take effect?
https://denversdietdoctor.com/lchf-15-years-coronary-artery-calcium-score-zero/
Well Bob, I’m a 53 y.o. doctor with good lipid profile, normal BP, exercise regularly, non smoker, BMI 18.5 and have been on low car diet for 15 years and just did my Calcium score for a check and which is 46 and is 75th percentile. So go figure as they say……Due to have CT angio to determine presence/extent of any stenosis.
It’s a bummer we don’t know what your CC score was 15 years ago. Earlier in the comments I said I wasn’t a fan of an individual CC score, I think they’re most helpful as a tool to see which way things are trending but not particularly useful when it’s an isolated test.
Out of curiosity – what is a “good” lipid score? And a BMI of 18.5 is underweight, why are you so skinny?
Trigs 85
HDL 58
LDL 125
All other clinical indicators including ESR/CRP/Lipoprotein A are all normal.
The BMI I quoted was through a manual/digital assesment which always comes out lower than those online ones that only use your height and weight(those ones measure me as 24.8 but they are rubbish really)
The fact is Bob the etiology of CHD is not cut and dry and is not down to one or another factor solely. I have been preaching low carb diets for over 15 years and have practiced this religiously and I have to say I feel good on it. I am certain that the various low carb diets are the way forward, sugar/processed is the enemy and we all have to eliminate it from our diet.. However there are other things we clearly do not understand still and it seems the hereditary ones are the ones we cannot get a grip on. My father needed a CABG at the age of 64 and lived to 78 in reasonable help. His lipid profile was reasonable, and he was also a non smoker/trim and exercised and ate sensibly avoiding trashy food. As he was born and raised in Med, his diet reflected most of the things we say are good. I’m not saying anyone is perfect but i don’t think we can be absolute in our knowledge about anything and we really are still learning all the time……
Well said Alexk
There are multiple factors at play. Hereditary factors are certainly important and although I believe that diet does play a role, very few people get coronary artery disease because of wrong dietary choices only.
very few people get coronary artery disease because of wrong dietary choices only.
And you know that how?
Bob
Clinical experience. Been practicing cardiology for almost 25 years now, in three countries, mostly treating patients with coronary artery disease. Does that count?
Coronary artery disease is a multifactorial disease. Most of us will be affected if we live long enough. However, the clinical picture varies a lot. Some patients are asymptomatic, some are hit by acute heart attack and in some cases the disease results in sudden death, Primary prevention aims at delaying the onset of disease and it certainly involves diet as well as a number of other factors.
I’m really not trying to be a jerk but I have to ask – So you’re saying that you’ve treated people for heart disease who have been on a well-formulated low carb, high fat, moderate protein diet who don’t eat grains and sugar, don’t eat HFCS, don’t eat natural or artificial sweeteners, don’t eat manmade polyunsaturated vegetable oils, don’t eat trans fats and eat a limited amount of fruit?
Certainly. Vegetarians, high carb paleo’s, low carb, ketotic… They can all have heart attacks. But, a healthy diet can surely reduce risk. However, if other factors are present (genetic factors, smoking, diabetes, hypertension, lipid abnormalities etc) it may not be enough. I’ve had patients with coronary heart disease who have done everything “right” in terms of lifestyle but still haven’t manage to avoid the disease, mostly due to genetic factors.
I’ve had patients with coronary heart disease who have done everything “right”
in terms of lifestyle but still haven’t manage to avoid the disease, mostly due
to genetic factors.
It seems to me that the definition of “right” is still up for much debate. I’ve been following this blog for a couple years now and most of the posts seem to be about what we think we know to be true may not actually be so. I have no doubt you treat a lot of vegetarians and high carb paleo (a name that seems to be a contradiction to me – paleo is generally low carb although higher carb than low carb – if that makes sense) but I’ll be honest, I’m a bit surprised to read that you get true low carbers and ketogenic folks with heart disease. But I’ll take your word for it.
Sorry Bob for not being clear on this. What I meant to write was low carb, paleo (low carb and paleo). I agree that paleo is usually low carb.
“It seems to me that the definition of “right” is still up for much debate. I’ve been following this blog for a couple years now and most of the posts seem to be about what we think we know to be true may not actually be so.”
Good point Bob. That’s probably why you shouldn’t take my word for granted.
One more thing – In the vein of not taking things for granted, when you say you’ve had patients who eat low carb with coronary heart disease, what is meant by that? Have these verified, long term low carbers actually had heart attacks? Or do they simply present with an unusual profile? And if they have had heart attacks how many people are we talking here?
I value the input of clinicians who actually deal with patients a lot – the problem I’m having here is that the doctors who I’ve spoken with who put their patients on well-formulated low carb diets almost always report their patients getting better – meaningful markers like Triglycerides, HDL and fasting insulin improve. That doesn’t mean they can’t have heart attacks in the future but it certainly would indicate that any current arterial damage was due to their prior diets.
Bob
I’ve learned that you are persistent and I respect and admire your interest in the importance of dietary choices for health and disease.
I don’t think I can really address your question directly as we seldom analyze in detail the diet of our patients.
I agree that a well-formulated low-carb diet may improve many metabolic markers, not least for those who already struggle with overweight or insulin resistance.
The most important thing to understand is that everyone can have a heart attack but we can certainly decrease our risk by healthy dietary choices, not smoking, regular exercise etc.
Another thing I think is important to understand is that we are all different. Although both you and I seem to understand the benefits of low carb/high fat diets, some people simply feel bad on such diets and have trouble adapting to this type of lifestyle. In my experience, this is more common among women. They sometimes feel better on a plant based high carb/low fat diet. In fact, such a diet also improves most metabolic makers and can be considered heart healthy.
So, my role as a doctor is to educate my patients about different alternatives and to help them make choices and try out different options in order to find out what suits them best.
Sorry Axel, I know I’m persistent and it gets annoying (even to me), it’s just that I’ve learned over the years that getting people to consider new information is not a matter of simply having solid evidence, I’m actually fighting human nature in the form of cognitive dissonance and confirmation bias. Once someone adopts a firm opinion on a matter it’s nearly impossible to persuade a person by using evidence as it will simply be ignored and the person written off as ignorant, compromised or crazy. This is the role I accepted when I adopted a minority opinion on how diet affects health and wanted to share my views. I accept that.
As a case in point, let’s look at our earlier discussion. You made the statement that it’s possible for a person on any diet to have a heart attack because that’s been your experience from 25 years of practicing… while I tend to believe that’s not true although factors like smoking perhaps can override a good diet I’m not dogmatic on that because I have little evidence to refute it. But when I questioned you on why you felt so strongly about that you indicated that you don’t actually have any real data on what your patients have been eating which would mean that we’re back to it simply being a strongly held opinion that I imagine you’ll still believe as soon as you’re done reading this sentence.
Avoiding cognitive dissonance is the single largest impediment to changes of thought in science. It’s what led Max Planck to state “Science advances one funeral at a time” – meaning that new ideas aren’t allowed to take hold until the old guard die off – new ideas are quashed and requests for funding are denied if you don’t fall in line with the status quo. It’s why we can’t get past the notion that LDL-C is a cause of heart disease and that a “food” like wheat is good for you; doctors are trained to believe these things early on and spend their entire careers reinforcing that prescribing statins and a low fat, high carb diet. If someone has been doing the wrong thing their entire careers it seems pretty likely that admitting it to themselves would be something that’s pretty difficult to do. It’s not evil or malicious, it’s simply human nature.
Cognitive dissonance is why we spend $30 billion a year on drugs that even the most favorable drug company-funded studies show they prevents 1 person in a 100 from having a heart attack and no effect on all cause mortality but does expose all these people to the more probable side effects. As an outsider looking in I say “what the heck are they thinking” but as someone who understands that our cognitive biases are incredibly strong I can understand how very few people can ever change their minds once they’ve been made up.
So yes, I’m persistent because persistence is the only way I can make a dent on changing ideas. The hardest part is because I know what I do about cognitive biases I am always questioning myself whether I actually know what I know or am I fooling myself. Questioning yourself all the time isn’t fun. Most people think that cognitive biases are what the other person suffers from, I realize I’m just as capable of suffering from them as the next person. That makes it easier to admit when I’m wrong because it gives me an opportunity to be right, which should be the ultimate goal.
Not to be argumentative but trigs at 85 isn’t that low. It’s better than most but not as low as some (my trigs are 55, HDL is 66). I realize it’s lower than “normal” but I don’t view normal as necessarily being good because normal is generally derived from assessing the numbers of people who aren’t on a low carb diet. I’d be curious to find out why your TGs are higher than most low carbers I know.
The fact is Bob the etiology of CHD is not cut and dry and is not down to one or another factor solely.
I agree that the cause of heart disease hasn’t been pinned down yet but the fact remains that you believe strongly enough in the health benefits of a low carb diet that you’ve been on one for 15 years – I’m not sure why you saw fit to be critical of my earlier comment about the other doctor. But my main beef with medical conventional wisdom is that it’s pretty apparent that LDL-C has nothing to do with causing CAD yet doctors still prescribe statins simply because they are quite good at lowering LDL-C (yet have an insignificant to almost imperceptible effect on CAD, depending upon which drug company funded study you’re looking at).
Fasting TG’s are meaningless when you’re on a HF diet, as exogenous TG intake suppresses endogenous hepatic TG synthesis. What’s far more meaningful is 2 to 4 hour postprandial TG’s, which are higher on HF diets (even after “adaptation”) than on LF diets.
Postprandial lipaemia is atherogenic. There are dozens of studies supporting this, many showing causation. Guess where you can find them? 😀
CAC scans can’t detect non-calcified plaques. You need to have a CIMT ultrasound to measure those. See https://www.modernmedicine.com/modern-medicine/news/modernmedicine/modern-medicine-news/stenosis-can-still-exist-absence-coronary-c
The good news is that non-calcified plaques don’t tend to suddenly rupture & kill you with a massive MI.
Dr Gerber is slim. He’ll be fine.
Jimmy Moore – not so much.
Jimmy Moore’s coronary calcium score is also zero. Oops…
https://livinlavidalowcarb.com/blog/jimmy-moores-cholesterol-test-results-2008-2013/18256
Do you have dementia, Bob?
You appear to have the memory of a goldfish, as you’ve already forgotten https://www.modernmedicine.com/modern-medicine/news/modernmedicine/modern-medicine-news/stenosis-can-still-exist-absence-coronary-c
Chronically-high cortisol caused by an over-reliance on gluconeogenesis adversely affects the hippocampus, the part of the brain that stores short-term memories.
Oh, dear! Poor, poor Bob. :-/
Is gluconeogenis activated only when glucose is depleted? What about those who eat their carbs in the evening? Are they stimulating gluconeogensis during the morning/afternoon?
I think the short answer is “It depends”.
For a non-insulin resistant person I think it would be reasonable to assume that the hormones stimulating glucose production in the liver would only occur at the appropriate times. This would be when glucose is low due to being fasted or some athletic endeavor. There is also the “Dawn Effect”, where your liver is prompted to produce glucose through the proddings of various hormone levels affected by cirrcadian rhythms.
Things get interesting when you’re insulin resistant though. Glucagon is one of the hormones that stimulate glucose production and being insulin resistant has profound effects on the effectiveness of glucagon. This article does a good job of describing it and it explains a lot why diabetics have a tough time controlling blood sugar with insulin. I couldn’t hope to explain the situation well in a single comment – read the article if you’re interested.
https://www.tuitnutrition.com/2015/10/its-the-insulin-3.html
It depends on your blood glucose level and your liver glycogen stores. GNG usually only kicks-in in the morning, when liver glycogen is most likely to run out.
If you’re fasting or on a low-carb diet, liver glycogen will be depleted a lot of the time, so blood glucose will be produced by GNG a lot of the time. This tends to chronically-raise cortisol, so I’m not over-keen on the long-term use of low-carb diets,
Does https://www.medbio.info/Horn/Time%203-4/homeostasis1.htm help at all?
Yes, that is interesting, but that article suggests blood sugar has to fall to a miniscule 3.2 for cortisol to be released. My blood sugars are never that low and I eat a low carb diet. In fact, my problem with low carb is that it has been raising my blood sugars. I assumed that was because of cortisol. But why would cortisol be released if by blood sugars are not getting anywhere near the lower threshold for cortisol release?
The BG at which cortisol is released isn’t precise. The cortisol+adrenaline/insulin NFB loop is there to stop our brains from dying due to a lack of blood glucose, when there’s no food available.
The normal NFB loop for blood glucose control uses glucagon & insulin to maintain a fairly precise 5mmol/L (90mg/dL). As glucagon acts on the liver to convert liver glycogen into glucose, this loop stops working when liver glycogen runs out.
Yes, but does it stop working because it is “broken” or does it stop working because the body has evolved to use another fuel source (ketones) when glucose runs out? after all, did the bodies of our ancestors really “stop working” during the frequent periods when carbs were not plentiful? Did every winter in the northern hemisphere result in cortisol levels so high that they damaged the HPA axis? This doesn’t seem evolutionarily likely to me. (these are all genuine, not rhetorical or insinuating, questions)
Normally, the back-up loop & ketogenesis are only used when there’s no food available. This minimises LBM loss by reducing glucose utilisation to a minimum. Death by starvation can be postponed for quite a long time, depending upon fat mass & lean body mass at the start. If a bit of (temporary & reversible) minor damage occurs, it’s a small price to pay for not dying! In the Northern hemisphere, edible roots could sustain people during the winter if animals were not available.
Nowadays, LCHF diets put the body into a similar state, but as there are AA’s, EFA’s, vitamins & minerals available, this state can be maintained indefinitely. Now, damage due to sustained hypercortisolaemia can occur.
A lucid explanation – many thanks.
If what you are saying is true then does that not mean that the recommendation of ketogenic diets for people with adrenal fatigue is downright dangerous. If so, how can people like Nora Gedgaudas and Jack Kruse – both well educated and clinically experienced practitioners – overlook such obvious biochemistry? Maybe there is more at play here? I think I might have heard Kruse say that the brain is capable of switching completely to ketones for fueld which would lessen the glucose requirements of the body significantly, I guess.
As “Adrenal Fatigue” isn’t a lack of cortisol secretion from the adrenal glands, but is cortisol resistance in target tissues due to the gradual down-regulation of transporters/receptors, then yes. Diets that rely on the cortisol+adrenaline/insulin loop make things worse.
Stating facts like this makes me as popular as a fart in a space-suit in LCHF circles – I got kicked off a LCHF group today. I hadn’t even asked to join the damned group in the first place – someone added me. I had to block members who were orthorectic, carbophobic, believed everything that came from “experts” like Ron Rosedale, Jeff Volek etc. I was treated like a heretic and got regularly “stoned”. It was a relief to get kicked off.
As for Jack Kruse, well. His stuff on EMF is garbage. I’ve heard of Nora Gedgaudas, but I’ve never crossed literary swords with her.
If Kruse said that the brain can switch completely to ketones, he’s . . . . . . words fail me! 😀
Long, dendritic neurons like astrocytes don’t have room for mitochondria and can only use glucose for fuel. After ketone-adaptation, the brain can reduce its glucose consumption from ~140g/day to ~70g/day, not zero.
If adrenal fatigue is not a lack of secretion from the adrenal glands, but a resistance in target tissues, why do people with “Adrenal Fatigue” present with depressed salivary cortisol levels?
Yep, the LCHF crew are pretty dogmatic. I got blacklisted for mentioning that, in a book I was reading called ‘The Old Way’, by Elizabeth Marshal (fantastic anthropologist), the bushmen survived on roots and berries for the large majority of the time, gorging on meat only infrequently when the hunt was lucky. Of course it is debatable whether 20th Century Africa mimics Palaeolithic Africa and whether northern hemispheres had the same diet. But even so, there was surely topic for discussion.
As for EMF, I am not so sure I agree with you. Jack might exaggerate a bit but a number of national health organisations warn against EMF e.g. Swedish gov suggest to avoid anything over 3milligaus…
Nora seems switched on. Peter Attia certainly seems like a “real scientist”. I have my suspicions about Kruse, but have yet to see anyone actually dissect his work in a way that let’s him respond appropriately. E.g. Heavylyn Insane’s critiques are just crass
“If adrenal fatigue is not a lack of secretion from the adrenal glands, but a resistance in target tissues, why do people with “Adrenal Fatigue” present with depressed salivary cortisol levels?”
I don’t know.
“Yep, the LCHF crew are pretty dogmatic.”
‘Nuff said!
“Swedish gov suggest to avoid anything over 3milligaus…”
The milligauss is a unit of magnetic flux density, not Electro-Magnetic Field. As the flux density in a MRI scanner is ~1.5T, which is ~15,000,000 milligauss, I think that the Swedish government are being way too cautious. The human body naturally contains no magnetic parts.
“Nora seems switched on. Peter Attia certainly seems like a “real
scientist”. I have my suspicions about Kruse, but have yet to see anyone actually dissect his work in a way that let’s him respond
appropriately. E.g. Heavylyn Insane’s critiques are just crass.”
Where low-carb & keto dieting is concerned, there can be only one!
He wrote the book “The Ketogenic Diet”. See https://bit.ly/1Mnmijx
Disqus seems to tolerate shortened links better than full ones.
I don’t know Nora or Peter Attia’s work. Kruse is a known liar (he was suspended for lying in court about the length of pedicle screws) & fantasist (he was caught-out using a stock photo in his Facebook profile picture when he claimed to have gained a lot of muscle), so I don’t believe a word he says.
Refuting evidence on the grounds that you don’t like the person who’s quoting it is an ad hominem argument (i.e. invalid).
Ah, this makes sense actually. My blood cortisol levels are always borderline high. My salivary (intracellular?) are always low. My cells are just not up-taking cortisol.
Hi Nigel, I’ve left two comments now and both have disappeared. I’ll try one more time.
Your suggestions regarding adrenal fatigue being caused, not by a lack of cortisol output, but by cortisol resistance or reduction in cellular uptake, is very interesting to me and explains a lot. My salivary stress profiles (measuring cellular cortisol?) always came back low whilst my serum cortisol always comes back borderline high. I suffer from high blood pressure and insulin resistance/high blood sugar so could not work out how my circulating cortisol output could be low, as suggested by my ASI profiles.
This theory raises many interesting questions:
– If cortisol resistance during low carb diet caused by prolonged elevated serum cortisol, will raising carbs actually make symptoms much worst by decreasing amount of available cortisol in an already cortisol resistant physiology. Could this in itself lead to a stress response!?
– How does the body perceive cortisol levels i.e. does the brain think “well I have enough cortisol in the blood so no need to pump out any more” or, during cortisol resistance, does the brain think, “fuck, these cells aren’t getting bugger all cortisol, better send some ACTH pronto!”? If the latter is the case then lowering serum cortisol levels in an attempt to reverse cortisol resistance would be pretty difficult.
Nora seems fairly switched on, although I distrust anyone with blinkers (ketogenic blinkers in her case). Kruse does exaggerate somewhat, but there are quite a few national bodies who are warning against EMFs e.g. I believe Swedish gov say it’s best to avoid anything above 3 milligaus. Finally Peter Attia seems like a “proper scientist” who is all for ketosis.
The link about victorian diet and health is fascinating. But it’s hard to say whether they would have been more or less healthy substituting the whole grains for more oily fish/natural fat.
“This theory raises many interesting questions:
– If cortisol resistance during low carb diet caused by prolonged elevated serum cortisol, will raising carbs actually make symptoms much worst by decreasing amount of available cortisol in an already cortisol resistant physiology. Could this in itself lead to a stress response!?”
As I said in my reply to you on my blog, you need to reintroduce carbs very slowly. Use “safe” i.e. slow release carbs, as per https://bit.ly/1MnoXtB
“- How does the body perceive cortisol levels i.e. does the brain think “well I have enough cortisol in the blood so no need to pump out any more” or, during cortisol resistance, does the brain think, “fuck, these cells aren’t getting bugger all cortisol, better send some ACTH pronto!”? If the latter is the case then lowering serum cortisol levels in an attempt to reverse cortisol resistance would be pretty difficult.”
AFAIK, the hypothalamus monitors serum cortisol level & stimulates the pituitary gland via the hypophyseal duct. The pituitary gland secretes ACTH (adrenocorticotropic hormone), which stimulates the adrenal cortex to secrete cortisone which is hydroxylated to hydrocortisone a.k.a. cortisol.
The hypothalamus monitors other parameters e.g. blood glucose level, adrenaline level etc.
As emotional stress & anxiety also chronically-raise raise serum cortisol level, I’d recommend that you supplement with 4g/day Epsom Salts (spread over 24 hours) , to chill you out.
Thanks for the reply. I have attempted to reintroduce carbs but have suffered each time.
I am in no way sticking up for Kruse, but I think it’s only fair to copy and paste an explanation he gave on another blog I follow :
“I turned a fellow surgeon in to PEER review who I felt was doing some nefarious things to patients in my community over a decade. As a result that surgeon lost his privileges at all hospitals at that time. As retaliation he said that I lied about the size of a screw used to harm one of these patients. This was sent in to a professional society we both happen to belong to that police our specialty within our confines. Mind you, the screw size had zero to do with what he did. In neurosurgery there is unwritten rule that you do not testify against another surgeon. This is why this profession conduct committee exists. It has nothing to do with medical licensure. It is a good old boys club for NS to police themselves. They did not like the fact that I protected patients over a fellow surgeon, so I took their punishment. I knew what their modus operundi was but I felt it was the right thing to do. The community hospitals did too because they acted to remove him from their medical staff way before his retaliation case against me was even complete. The AANS knew I was right about the merits, because they saw the actions of the hospitals unfold, yet they decided to slap my wrist for turning on a fellow AANS member. That is taboo in NS. I lost a battle but I won the war because that surgeon is no longer able to hurt patients in my community. I also realized I did not need to be part of specialty society that puts its members above patients.”
He wasn’t banned from practicing at all. In fact, all of the reviews of people that have been treated by him are nothing but glowing. Again, I do not agree with everything he says.
I already started taking magnesium L threonate yesterday, which is supposed to cross the blood brain barrier. Hopefully that will do the trick. Any reason for epsom salts in particular?
“Thanks for the reply. I have attempted to reintroduce carbs but have suffered each time.”
What carbs did you try?
Kruse definitely lied about his profile picture on Facebook and he’s said many extremely odd things (including smearing MRSA all over himself before surgery on him, in a video) on blog comment sections. Then there was that incident when he was escorted off a low-carb cruise and he made all sorts of odd accusations. Sorry, but Kruse has zero credibility where I’m concerned, other than as a neurosurgeon.
As Mg crosses the BBB, why take the L threonate variety? Magnesium sulphate heptahydrate is very well-absorbed (but don’t take 4g in one go!), and sulphate is good for maintaining tight junctions, as per https://bit.ly/1TXKHlB
Magnesium seldom crosses the blood brain barrier to an extent that affords significant cognitive benefits
McKee JA, Brewer RP, Macy GE, Phillips-Bute B, Campbell KA, Borel CO, Reynolds JD, Warner DS. Analysis of the brain bioavailability of peripherally administered magnesium sulfate: A study in humans with acute brain injury undergoing prolonged induced hypermagnesemia. Crit Care Med. 2005 Mar;33(3):661-6.
L-threonate has been shown to cross BBB
“Thirty patients with acute brain injury secondary to subarachnoid hemorrhage, traumatic brain injury, primary intracerebral hemorrhage, subdural hematoma, brain tumor, central nervous system infection, or ischemic stroke were studied.”
As IV Magnesium Sulphate Heptahydrate solution is the gold standard treatment for stopping seizures in women with pre-eclampsia, I can only conclude that Mg has trouble crossing the BBB in people with acute brain injury.
Everyone that’s tried Epsom Salts has told me that it reduced their anxiety, so I know that Mg is getting into their brains.
You guys sound so complicated about your diets and supplements. I guess the most important question is “Do you eat the turkey franks or the ball park franks?”
My husband just had this test and his score was 0 he said. But he is on a crazy amount of medication to keep his lipids low. If his score is 0 does he need all those pills… he does run a high cholesterol without them. Thanks!
Bob: As an outsider from your debate with Dr. S, I don’t see that your data is any better than his. Newer studies aren’t always better studies. The same diet or medicine that are good for one person, may not be good for another. The pendulum of fact and truth is constantly swinging. I tend to embrace when the pendulum is in the middle. Moderation and common sense. People do so many things wrong regarding their health, probably there are many good ways to make a significant difference. I’m still going to stay away from “bad” sources of fat (fatty greasy meat) and “bad” sources of carbohydrates (sugar/processed foods/grains) and stick with balanced proportions of the good sources (beans/nuts/vegetables/chicken/turkey/salmon/apples/pears/berries/tomatoes/potatoes/quinoa/barley/oats/etc.). Combine that with moderate to “more than moderate” exercise, proper caloric intake, medicine when absolutely necessary (my personal call based on educating myself), and staying out of debates like this as much as possible.
Not to be offensive, but the irritating thing about your posts isn’t your persistence, it’s that you think you have the only answer, and if someone has a different idea, you can’t leave it alone and you attack. This has to cause you stress. Stress can’t be cured with diet or medicine, it starts with the person and how they think. I used to think like you, but as I got older, it got to be exhausting, and I often found out my “ultimate truth” was not so accurate as new information came to light. I hope you have a great weekend. I’m going to watch a comedy this weekend. I don’t think I’ll die laughing. 🙂
Peter – I appreciate the comment, it’s always good to get feedback on what people are thinking.
I don’t think I have the only answer though, if people aren’t having problems with their current methods then why would I say they have to follow what I think, Here’s the problem, how many of the people who have posted on this thread are having problems, despite having already heard and followed all the advice about a low fat, high carb diet full of whole grains and moderation and swallowing statins? Probably a lot.
I was one of those people, I don’t know if I ever had “abnormal” cholesterol issues because I never had it checked until well after I started a low carb diet but I was fat and I was an asthmatic and that’s not the case anymore. And if you’re a believer that the TG/HDL ratio is more telling about your heart health than your LDL-C score (I am and I believe Axel is swinging that way), then my current measure of TGs at 55 and HDL at 66 is probably about as good as you’re going to see. (I don’t actually know what my LDL-C is currently because my last test was a basic lipid profile and those tests use the Freidewald equation to estimate LDL and that equation is very inaccurate when trigs are 400). I had an NMR performed 3 years ago that accurately measured my LDL-C at 107, which I didn’t find noteworthy in any way.
What I’m trying to do is present an option and along the way show that what we think we know about diet and health probably isn’t as solid as we were led to believe. If you think that saturated fat is bad for you then there’s little I can say that will dissuade you but there may be people reading this who may be interested enough to start their own investigation. That’s what happened with me – I was getting lousy results from the conventional wisdom and I realized I didn’t actually know anything about why I was doing the things I was doing. And fortunately I realized that before I dropped my dietary fat even lower and spent even more time in the gym it might be a good idea to see just how solid the science is. So I looked, and what I found made me believe that our dietary recommendations are very suspect. Other people may do this same investigation and come to a different conclusion but the important thing is that shifting my approach made dramatic improvements in my health. Body fat dropped off, lean tissue increased and I am no longer an asthmatic. Believe it or not but this does not cause me any stress whatsoever – nor does it stress me out when people disagree with me. Disagreeing with me is fine, it gives me an opportunity to express myself again in a way that might persuade someone following along to look at things in a different perspective. That’s a positive, isn’t it?
So anyway, I do appreciate the comment and I do realize that the way I espouse may not be right for everyone else. But if it’s right for just a single person and I’ve managed to get them to consider that then I think it’s been time well spent.
Peter – here’s an example of why I contribute to blogs in the manner I do. If I can help just one person it’s worth it to me. Fortunately I’ve managed to help a lot and it’s tremendously rewarding. Here’s a facebook post from a person who saw my advice on an economics/stock trading blog (of all places). Donna didn’t know me from Adam back then although we later became internet friends. This is why I’m persistent and why I present alternatives.
https://i81.photobucket.com/albums/j201/bobbyj0708/Donna_zpsztutuj6q.png
So, getting people to adopt a restricted diet for the rest of their lives when it’s completely unnecessary (because insulin resistance is almost always reversible) is “helping” them?
You’re using a definition of the word “helping” that I’m not familiar with.
Try https://bit.ly/1Zbohkj
I really don’t understand why you’re going after me, Nigel. You make the claim that I suggest people adopt a “restrictive” diet for the rest of their lives and then I find out you “mum” is improving after adopting a ketogenic diet, which is a much more restrictive diet than the one I’ve adopted. I think it’s time for you to pause and consider what you write before hitting “Post”
From your link…
“I nearly forgot! Today, when I arrived at mum’s nursing home, I found her reading a book. She hasn’t done that for over a year. She even knew that it was
Wednesday. Ketogenic diet for the win. Mum now has a dual-fuel brain.
I’m deliberately replying to a lot of your comments because you’re an arrogant know-it-all, who actually knows sweet-F/A.
Mum’s mental faculties temporarily improved, due to the provision of a second fuel supply for her brain. Unfortunately, ketosis didn’t stop the progression of her Lewy Body Dementia (plaques & tangles in alpha-synuclein) and she died in April 2013, roughly when predicted (6 years after symptoms started).
She had a better quality of life thanks to my interventions (it wasn’t just a ketogenic diet that I tried), even if she didn’t have a better quantity of life.
I managed to post a link to my blog post about insulin resistance by shortening it with bit.ly. I hope you found it useful.
Sorry to hear about your mom,.
Thank you. Are we going to stop arguing, now?
Would really appreciate if you did guys. I love to have you around but you’ve been leaving some dirty foodprints all over the place. It’s fine to disagree but I prefer a respectful discussion in this forum.
Hi,
Sorry about that. Due to an (officially diagnosed) Autism Spectrum
DisorderDifference, I have little tolerance for bullshit regarding low-carb diets. Having had success with the Atkins diet in 1997, I was like Bob from 1997 to 2002!Then I started mixing with bodybuilders & health professionals and learned how to use PubMed properly. In 2005, I discovered Lyle McDonald’s site and learned how to do science properly i.e. examine all of the evidence. You do this, which is good.
I’m not anti-low-carb diets. I’m just anti-bullshit. See https://bit.ly/1Yn8WLb
Cheers, Nige
Here’s the thing, Nigel. I initially read everything you posted and I still don’t understand what you disagree with me about. You’ve done a poor job articulating that, particularly when each comment is also ended with calling me an ass. I pointed this out several times, asked you to stop and now I’m in Axel’s doghouse because of your antics. I’m all for civil discussion and I’m quite willing to have one with you but it’s damn tough when your comments are an attack meant to denigrate rather than to stimulate discussion.
With that, sermon over.
Bob,
I read a lot of your comments on your Disqus profile and got the distinct impression that you’re a denialist, as you employ many of the tactics used by them. Your comments in reply to Mie were particularly bad in this respect. This pissed me off, so I did what I often do to people who piss me off – I gave you an internet “spanking”.
I called you an Ass because you kept Assuming things. Geddit? Haven’t you heard the saying “Assume makes an Ass out of u and me”?
Anyway, I’m done with “spanking” you, as you were kind enough to offer your condolences for my mum’s death. I don’t hold grudges, so I’ll leave you alone from now on.
My one request to you is for you to show a little humility. You’re too sure of yourself that you’re right and that anyone who disagrees with you is wrong. Diet & Nutrition is a humongously complicated subject. The more I learn, the more complication I find, which shows me that there’s even more stuff I don’t know.
Anyway, that pretty much wraps it up. Peace.
Nige
If you think you need to give a spanking to everyone who you disagree with on the internet you’re probably wasting your time. Most people with a firm opinion can’t change their minds (cognitive dissonance is a real bitch), you can only change the mind of people who aren’t convinced of their unassailability. Calling me names isn’t changing my mind in any way and it turns off the people who might be following along and have an open mind.
Now I know I’ve been wrong on a vast number of things in the past because I made assumptions that the experts knew what they were talking about. I eventually understood how dumb this was and now any firm opinion I hold is simply due to as much study to a discipline I can dedicate. I have an open mind, I am capable of changing my mind when presented with solid evidence that I’m wrong. What doesn’t convince me is name-calling and the directive to read the contents of someone’s blog and cross verify the info there so I can see where I’m not correct. If you have something specific you want to bring to my attention, do so in a direct manner and then I’ll take it in and either thank you for bringing it to my attention or explain why I don’t agree with it. I can’t do any more than that.
As for Mie, when someone is assuming the mantel of being knowledgeable in a topic yet remains anonymous I become suspicious. When their comments are full of studies with dubious outcomes (small trials, outcomes reported as relative risk only, obfuscation with confidence intervals) then I really begin to wonder about the motive behind them posting. I’m not anonymous. I don’t make a damn dime posting the reasons people should adopt a wheat-free, low carb diet or a fasting protocol; I simply want people to have a high quality of life free from the clutches of those who profit from their chronic illness. I’m open to changing my views, the last 10 years of my life have been devoted to that.
I appreciate that you have strong views yourself and I’m quite interested in hearing them. Just understand that administering a spanking is simply going to make people dig their heels in and ignore you. With written comments it’s difficult to convey tone, understand that I try hard to keep any sarcasm out of a response unless I’m simply over it (see comments to Mie). You probably have some information I’d love to see, I hope that we are able to actually talk about our difference in opinion at an objective level.
I administer “spankings” partly to take people down a peg or two and partly for shits & giggles.
As I pointed out, I was using a play on words to call you an Ass.
As everything that I know is brain-dumped into my blog, I don’t fancy writing stuff out especially if it means posting more than one link. Disqus seems to use a pseudo-random number generator to decide if a link is SPAM, or how many links I’m allowed to post per comment. That’s why I post links to my blog.
I run an evidence-based blog, so my Engineering qualifications are generally irrelevant, unless I’m discussing negative feed-back (NFB) control loops, as everything in the body is regulated using biochemical NFB loops.
RE Mie: Playing the “shill” card is a cheap shot and a tactic used by denialists. It’s been used on me several times. I’m a retired Electronic Engineer and my main source of income is a company pension scheme. You don’t know who Mie is and neither do I, so you shouldn’t make assumptions.
As you’ve noticed, I have fairly strong views on things, backed-up by evidence. My ASD gives me focus, so I can spend many happy hours making my blog a good source of information which looks half-decent and is easy to navigate & find stuff. Comments are welcomed, but please read my moderation policy before commenting (link in Info section).
Now that we understand each other better (as you say, tone is a real bugger to convey!), we should be able to discuss things in a cordial manner from now on.
Cheers, Nige
Bob: You and Nigel sound like Jane Curtin and Dan Akroyd: https://www.hulu.com/watch/2306
Give a listen. 🙂
Juat so long as I’m not the “ignorant slut”, I’m fine with that comparison. 🙂
Bob: Nice post. I try to do the same on other blogs for people with atrial fibrillation. I was wondering what you do for enjoyment besides heart stuff. I was going to watch a comedy, but instead revisited a Robert DeNiro Movie called “Everybody’s Fine”, a drama. There is a whole plot, but what I noticed is the main character cooks a steak on the grill for a family gathering(no-one shows up, so I guess he eats the whole thing), later has a heart attack on a plane about 3/4s into the movie, and then cooks a turkey at the end. There’s more to the movie, but that’s what I got out of it. 🙂 hahaha
Gotta love Hollywood… 🙂
For fun I’m remodeling my house (landscaping the backyard right now) and play with my dogs at the beach (I live in So Cal). Between that, my girlfriend and following the health debate I’m plenty busy.
Oh and everyone shows up for the turkey. Not sure if it was stuffed with bread.
Probably the most important read for those with high CAC scores!!!! This is new. If your CAC is mostly high density… you are not as bad off as you thought. High density calcium is protective. Cuts risk up to half for any given calcium volume, according to this read. This is the missing link people have been waiting for… there was a disconnect before… they would say calcium stabilizes plaque (good), but calcium is an indicator of plaque (bad). No-one knew what to wish for. Note that no calcium (zero score) doesn’t mean you have no plaque, it just means your risk is way down that you would have a major blockage. Major blockage? Whoa! They’re not sticking their necks out with that statement!
Now all you have to do is see if your cardiologists have or will look at whether or not you have high density calcium. As a person with a very low score in the low 30s at age 66, I still would like to know if I have mostly high density calcium. I wonder if the CAC test reveals this information already, but was ignored. I’m going to try to find out. I think knowing your density will tell you where your are going as you age.
https://www.ecardiologynews.com/specialty-focus/cad-atherosclerosis/single-article-page/esc-coronary-artery-calcium-score-gets-an-upgrade/1c82f28b7219e95fe7f573f72c9aca4d.html?utm_source=News_CARD_enl_101215&utm_medium=email&utm_content=Watchman%3A+Insurance%2C+labeling+problems+hinder+LAA+closure+in+AF+patients
From the annual congress of the European
Society of Cardiology…
“We no longer believe in the Agatson score. We took a look
at it and found out that at any given level of plaque calcium volume, a higher
density score is protective. So when we look at our scans now, we no longer use
the Agatson. We take the volume, then measure density separately, and we
calculate a score that’s based on both.”
“The new concept is that as your density score gets higher your risk goes way down. In the fourth quartile of density, you have only half the risk of developing a coronary event at any given calcium volume.”
“Asked if any biomarkers are related to CAC density, Dr. Criqui replied, “Preliminary data show that most of the risk factors we know are bad for us, like diabetes and smoking, are associated with lower CAC density. And the things that are good for us, like exercise and statins, are associated with higher density.”
“He and his coworkers are now looking at plaque calcium density versus volume in the abdominal and thoracic aorta to learn if the same relationships seen in the coronary arteries hold true.”
Hi Peter.
Thanks for highlighting these study results. I think they may have important implications in the future. I’ve been following patients with very high calcium scores (Agatston) for years and some of them seem to do very well. They’re asymptomatic and clinical events are rare.
So, it doesn’t surprise me that there may be a subgroup of patients with high calcium scores that may do well and have a good prognosis. It would be great if assessing calcium density could help us identify those patients.
And let me emphasize that they are saying statins are contributory to your calcium being more dense!
I had the scan for coronary calcification done 3 years ago at age 55 and my score was 116. The more I read about this the more concerned I get. My cholesterol has never been very high, but they put me on atorvastatin any way because of the score. Both my parents had strokes and heart attacks. What other treatment should I have? I’m concerned even more because the calcification is in my left main artery which is a very serious place to have a heart attack.
I had the test done and my score was 29. All my blood work came back good but my LDL could be better. I exercise a lot( over 200 minutes of cardio per week at HR above 130, Im 53 Years old) , never smoked, take supplements, BP is always 120/80 or better and have always worked out since age 17.
As for supplements I take Cq10, Niacin, Multi vitamin, magnesium, krill oil and Vitamin D. My diet is ok but am trying to do better. Family history of Heart attacks both both parents smoked but lived long lives(79/86). Should I be overly concerned about this score? And what else can I do to slow this down ?
Perhaps my story will help alleviate some concerns. I am a 69 year old white male.
I was perhaps one of the first to have one of these heart scans. Heard a radio spot actually advertising them in 1996. Went to UIC (Chicago) and had the test — unbeknownst to my cardiologist in Milwaukee.
Cost, out of my own pocket, around $400.
Test result came back as a score of 449 — with most of that in the left anterior descending, the so-called “widowmaker” coronary artery.
My wife and I were terrified.
Went to my cardio in Milwaukee and sheepishly admitted what I had done. His look suggested: “What the hell did you do that for? I’m your doctor!”
Long story short, it is now 16 years later. I have had no cardiac “events” — despite a calcium score in 1999 that suggested I was at highest risk relative to the rest of my gender and age group. I see a cardiologist annually for my long history of idiopathic atrial fib. I have been cardioverted successfully 7 times in 30 years, and now believe my-afib was induced by excessive caffeine. (Cardio doesn’t believe that, but I know my body. I am not in a-fib and take no meds for it. I no longer consume excessive caffeine.)
Moral of story: this particular test — the coronary artery scan — can scare the hell out of people. I may be very living proof that these scores are at best guesses. I no longer worry about a heart attack tomorrow. I am 50 pounds overweight but otherwise without bad health habits. (I know. 50 pounds extra is the baddest of health habits, but I am working on it.)
Good luck to all and avoid the calcium score nightmare if you can.
P.S. Another rather nationally renowned cardio once told me these tests are designed more to up a testing center’s bottom line. “Heart scams”, she said, is the better term.
Owen May, New Berlin WI
P.S. Forgot to mention. My cardiologist provides excellent care — and calls my every-other-year alternating echo or nuclear stress test the “gold standard” in cases like mine. He is not worried…and neither am I.
P.P.S. A typo. I believe these tests first came available in 1999, not 1996. That was the year I had mine…1999.
I’m a 54-year old woman and my calcium score is 63. I do not want to take statin drugs but my cardiologist is insistent. I exercise and very fit and my weight is perfect. Should I be over
concerned about my score?
okay I just got my score of 73, I am a female, smoker, and have been on a statin for about a year, although I did not want too. but, I also am diabetic and had high cholesterol.
WFPB
I’m 57 with a score of 55 which comes to 89% says the calculator. Doctor wants me to take Statins. My cholesterol levels are low, tri’s low too, any suggestion … Don’t want to take statins. I also am a pretty healthy eater.
My cholesterol was high 235 but HDL and Triglycerides were great. NP wanted me to go on statins and I balked so she recommended CT Cardiac Calcium score first. My score is 2005 which places me in the 96/98 percentile for heart attach or stroke. I am now on statins and CoQ. To cardiologists, MD and NP all seem to think the 2005 score is unimportant as my weight, diet, exercise are all very good.
Makes no sense to me that a score five times higher than the 400 (critical) is fine
Hello Everyone! I’m in need of some healthy advice. My husband just received news that his calcium score is 3000 & we don’t have insurance & don’t know what we should do? Please help! Thank you!
My Calcium score was 1806, which is off the charts. I am a type 1 Diabetic for 30 years and recently had 2 stints done. I have a very stressful job and have requested from my doctor to be placed on disability. I am 57 years old.
BWS
Are there any doctors out there who can give me their opinion on my situation. I accept that this is not a diagnosis and I accept that they are not legally liable for anything they say, as I will take my own independent medical advice. However…
I am female, only 54, with high (not OTT, but just over the recommended guidelines) LDL cholesterol, high levels of HDLs, just about zero triglycerides – and a calcium score of 34, which puts me on the 90th percentile. My blood pressure is also moderately raised so I am on Ramipril, which controls it reasonably well much of the time (although the minute I am subjected to any form of stress – sometimes even just typing an email, for example – my BP goes over the range.)
I am told that my family has a history of high cholesterol. Maternal grandma died of a pulmonary embolism at 58; my mother is almost completely blocked in her carotid artery, has been on statins for years and now has rapidly worsening dementia, although she smoked for many years. Dad is fit as a fiddle at 84, still teaching in school.
I look young (regularly told I look late 30s/40), am very slim, with long, healthy, thick, dark hair that’s not even gone grey – 103 lbs, 5 ft 3 ins – and fit. I exercise reasonably regularly but not excessively and passed the exercise stress test with flying colours, about 30% fitter than your average woman my age. I am pretty well vegetarian, just sometimes having fish and very occasionally a little chicken or beef. Mainly I live on nuts, vegetables, seeds, pulses, avocados and other healthy fats and oily fish.
I was put on Lipitor (atorvastatin) – only the very smallest dose (10) and soon started to ache to such an extent that I could not lift weights or exercise properly. This, for someone with my issues, seemed counter-productive – surely exercising is what will help me to stay alive??? Blood tests after just 8 weeks on statin showed elevated CK/muscle damage and also an abnormal liver function test. No wonder I felt lousy. The cardiologist, after the results of my CT angiogram (which showed at least calcification in my LAD artery, and there could’ve been more elsewhere but the images were not clear enough), had wanted my dose quadrupled, Since then, though,I’ve seen four different GPs who have done everything from respect my choice to take zero statins, to suggesting doses of 10 and 20. One prescribed ezetimibe, but after just a couple of days of that, I experienced some aches and numbness/tingling in my left foot – and suddenly felt incredibly depressed. The GPs deny that any of the effects I experienced had anything to do with the vile drugs I was prescribed. One of them is now adamant that I should take the ezetimibe (even though it hasn’t been proven to be safe and all it does is lower cholesterol, which I am not sure is the problem here; inflammation is.)
Now, I live in constant fear that my calcification will progress. Yes, I have been under constant severe stress in my life in recent years, so am taking steps to change that. I also am continuing with my nuts, oily fish etc but have reined right back on the wheat based, hi fibre carbs I used to eat, in favour of fats like avocado. And trying to keep up moderate but REGULAR exercise. And increase my sleep. Am I taking a real risk by not taking the statins etc? I went to an iridologist who told me that my main problem, from looking in my eyes, is not cholesterol right now but insulin resistance. I did get mild gestational diabetes during my first pregnancy, but have not developed diabetes in the 20 years since then – possibly because I have never been overweight or eaten a poor diet. But, with this brief experience of diabetes, it’s just another reason why I am so scared to take statins. Any ideas from you doctors out there, or folks with similar problems to mine? Thank you.
I had my CAC score done last year at the age of 42, and it was 156. So I’m doing GREAT, right?
Seriously, I’m in the worst 1% for guys my age. That’s not just a bad score — it’s a “the doctor spit coffee all over the office when he looked at your test results, and will see you as soon as he picks his eyeballs up off of the floor and puts them back in his sockets” score.
And what did the doc do? Put me on a statin, and some aspirin. And that’s it.
That’s all they CAN do, it seems.
So for me, the coronary CT scan was really just a test that told me I’m doomed.
Hi. I really am in a dilemma on the statins issue. I don’t know what to do. I am only 55 but have a calcium score of 34 as well as mild/minimal plaque in my abdominal artery and those in my legs. I have very poor bloodflow to my feet, with tests showing borderline zero bloodflow to all ten of my toes in cold conditions such as on winter days. I wouldn’t mind, but I am very slim (5ft 3 ins and 103 lbs), scored excellent/athletic on the treadmill test and am fit and active. I also have eaten what we were all told was the best diet, ie fruit, veg, lowfat this and that, not much meat (don’t like it anyway), zero cream – no chips, French fries etc and wholegrains. For years. Not much fat. Despite all that and despite having just about zero triglycerides, I have struggled with high LDLs, even though my HDLs are also high and technically my risk score should be very low because of the high HDLs. My blood profile is otherwise fine, not diabetic (although I did get mild gestational diabetes with my first child – twenty years ago.) Well, the doctors put me on statins – atorvastatin 10. And after just eight weeks’ use, I had no energy, could not do my usual exercise, my arms ached and I couldn’t even lift the club properly at a staff fun golf day. I was horrified. Tests showed that, after just 8 weeks, I had muscle problems/damage and an abnormal liver function test, yet GPs were encouraging me to continue statins and even increase to 20. I later tried ezetimibe, but besides feeling very depressed within 48 hours, I started experiencing tingling in my left foot; I have since developed a problem with my left pinkie intermittently swelling up and throbbing, before spontaneously resolving. My family, it turns out, all have high LDL and the females have had trouble with taking statins, although my 80 year old aunt, now on rosuvastatin, says she’s been better on that. My mum has blocked arteries and is battling vascular dementia – but she is 82. My mum’s mother, in contrast, died of a pulmonary embolism at age 58. I have been through significant stress owing to domestic abuse, which I tolerated for years, going from lowish (90/55 to 100/60) to high BP (now controlled by ACE inhibitors and I’ve ended the marriage recently) and am wondering now if resuming statins is the way forward or not. As a naturopath did iridology on me and said he saw very little cholesterol issues in my eyes but could identify substantial insulin resistance developing, I have started to consume fewer grains and instead increased my already high vegetable intake to even higher amounts and live on fish (mainly oily fish), seafood, raw nuts, fruit, veg, legumes, a little natural yogurt and small quantities of wholegrains – plus just about no processed foods – and I have massively increased my intake of good HDL in the form of avocado, olive oil, nuts and oily fish. I am trying to stay away from statins and just exercise more, sleep more, curb stress (I’ve found a very loving new man). However, in taking this approach and ignoring statins, I wonder if I am taking a very serious risk with my health as I do have cardiovascular disease, however mild. Any views? I am also blood group A, which apparently is associated with more cardiovascular health issues, and have never been much of a meat/saturated fat eater. Just don’t like it.
I’m sorry Katie but I’m going to be blunt. If know you get debilitating side effects from statins why would you take them? And considering that even when examining mostly drug company funded study results the absolute risk reduction for cardiovascular events and overall mortality for women on statins essentially was within a rounding error (meaning no documentable benefits) I can’t believe your doctors are wanting you to take them.
https://www.docsopinion.com/2015/04/14/statins-for-women/
There’s more to the cause of heart disease than just diet. I can’t begin to imagine how the stress from your past relationship was affecting your health. Cortisol and adrenalin are powerful hormones that are produced at times of stress and too much can affect your health negatively. If it were me I’d continue doing what you’re doing without any drug intervention and see how future CC scans progress. What you have right now is just a snapshot, you don’t know which way the trend is headed now that a major stressor has been removed without letting time pass and getting another CC scan performed. Stay off the drugs because you already know they’re doing damage and see how your body responds to your new situation.
Have you ever heard of a calcium score above 2500. (Yes 2500) I’m 61 5’11″and weigh 225 lbs I passed my last stress test. (Doc said very good) Heart cath showed 30% blockage on left side. Quit smoking 8/2008. Have another appt with heart Dr next month. The only Meds that I am taking is Lipitor and fish oils. (cq10) My blood pressure is good now that I retired 4/1/2016. Are there some questions that I need to ask my Dr? Any other advise. Thanks
Please advise…..Im 45 years old. Good Health. Cholesterol #’s are good. Total Cholesterol:170…..LDL:102…..HDL: 42….Triglycerides 120. …..My Calcium score is 22. My doctor said although that’s a low #, but he wants to start me on statins. Is that normal course of action for my #’s ?? His initial reaction was that a 22 calcium score was a good # and not alarming… But a minute later, he decided I should be on a statin. Not sure what to do or believe, with all the +/- info out there.
I had a mild arterial plaque spot in one artery (less than 30%)….All other arteries were all clear….Any advice or help or questions I should be asking would be greatly appreciated. Not sure what I should do. Or where I stand compared to average person. Doctor said the statin will slow down any progression. I thought that its normal as you age to have a little arterial plaque, as long as its not anything significant.
Hi Joe,
First off I must say that I’m a cholesterol/statin skeptic, meaning that I don’t believe the evidence shows that cholesterol levels or the effects of statins on cholesterol contribute to a statin’s incredibly tiny benefit on heart disease (but not overall mortality). In my eyes the only dangerous cholesterol level is a level that’s too low. With that said, here goes.
Basically what you’ve said is that your cholesterol is within “normal” levels but your doctor wants to put you on a cholesterol lowering drug anyway. Frankly I would say “Doc, what’s your reasoning behind this? Either my cholesterol is fine or it’s not, putting me on a drug when I have normal cholesterol seems outrageous, particularly when drugs like statins have known, detrimental side effects.”
Your doctor is asking you to take a dangerous drug when it cannot by definition produce a benefit. Personally I would run, not walk, to find another doctor who has your best interests at heart rather than just trying to cover his/her butt.
Hi Bob, Thank you for your reply and insight. Its pretty much what I was thinking. My cholesterol levels are in a very good range. And I eat very healthy, mostly plant based diet, along with fish. Get a lot of exercise….From your knowledge is my calcium score anything to be concerned with? (Its 22 at age 45). Im not as familiar with what that means for me and where I stand in the grand scheme of things on that. Since that’s not a test most people have done.
my doctor rationalized his recommendation by saying that even thou my current risk is low, he said the statin would slow any progression down the road so that I wouldn’t run into a problem 10+ years from now. But I just don’t know if that is legit advice. As I mentioned my cholesterol and Blood Pressure and all are great. His advice was based on me being 45 and my having a 22 calcium score and some mild plague
I am a 58 year old female who recently requested a coronary calcium scan – as my sister had by pass surgery this year and another sister died. My scores came back very high at 1780. I am confused as to next steps. My cardiologist put me on a statin and recommended diet and exercise. I currently exercise 4 times a week but am overweight at 190 pounds. I am doing whatever is recommended but cannot shake the thought that I may need more invasive treatment beyond statins, exercise and weight loss. Please let me know your thoughts. Would a cardiac catheterization be a more prudent course as I’m in the 90% or great risk pool?
I’m a 72 yr. old male. (5’7″ – 155 lbs – 17% body fat.) My brother had heart attack at 50, but was overweight and out of shape. My mother had one at 63, but smoked. I’ve always been active. My job was very physical. I exercised 5 days per week for 1 hour ea. Half aerobic and half anaerobic. I have absolutely no symptoms. I had a nuclear stress test at 61 which showed normal. I found out about the ct scan. Out of curiosity, I checked it out and was completely shocked. My calcium score was 2936. What now? Angiogram? Stents? Maybe quadruple bypass? My doctor increased my lipitor from 20 to 40 mg. I have an appointment with Abbott Northwestern to discuss it. I talked to a doctor at St. Johns and he suggested an Angiogram. This seems rather a risky procedure for a person with no symptoms. I’m completely stumped. I need info on other people in this situation. What to do?
Hi Charles. I would be pleased you got the angiogram. I’m sure you’ll be fine with it – most people are. It will give you a much clearer idea as to what the extent of your plaques is and could be a lifesaver. Very many people have extremely furred up arteries yet remain asymptomatic, never realising that they are at risk of what could be a fatal heart attack. As this is a year ago and I’ve not been on here for a long while, I hope your procedure went well and that you are on the road to good health.
What does it mean if 3 or the arteries were all very low scores (<30) and one was 238? Could this be an incorrect reading?
That is indeed very common. The amount of calcium in each artery may be different. Calcifications are most common in the left anterior descending (LAD) coronary artery.
Is there a case for a 57 year old female, with a calcium test score 2.5 years ago of 34, with confirmed plaques of <50% narrowing in the LAD, to be referred for lipidology studies and further specialist screening, if her mom had severe blockages and the entire maternal side of the family has high cholesterol? I was diagnosed in Australia with FH, high BP (now treated) and Raynaud's Syndrome and referred to a cardiologist and lipidologist, but unfortunately had abnormal liver function and creatine kinase results in blood tests after just 8 weeks on atorvastatin 10mg, and could barely lift a kids' crazy golf club or do my exercises, the muscle aches were so bad. Although my total cholesterol is now fairly OK – about 6.7 mmol – and my LDL score is 3.0 with almost zero tryglycerides, this is only because I am now on ezetimibe, am very slim and fit, exercise regularly and am naturally inclined towards a pescatarian/Mediterranean diet. The problem is that, now that I am staying in the UK, I am considered within normal range for LDL cholesterol by British referral criteria, so am not statistically considered 'at risk' for CVD, hence they are reluctant to send me for a repeat calcium score test/CT angiogram or refer me for lipids testing or cardiologist support – yet I know that I have existing plaques that put me at higher risk than most women my age. Perhaps if I ate more of the wrong foods, put on masses of weight and went into the surgery with a Coke and a cig in one hand and a burger and a box of fries in the other, they would take me more seriously? I am worried because I believe my target LDL should be even lower with preexisting known plaques than it is for the general population; don't know how fast my disease is spreading as I so far have been unable to take statins; and wonder if a lipidologist (and possible further calcium test) could shed light on what sort of non-HDL cholesterols/their particle size etc I am producing so that we can possibly know how recent the calcification is, how stable the plaques are, how quickly the disease is progressing or if it is contained, and then have some idea of what my longer term prognosis will be? My specialists in Australia have offered to work with the UK doctors, but just getting the referral is the problem and going privately is not a viable option for me because, however sub-clinical the disease, it is pre-existing and I do not have health insurance in the UK. Does anyone else have this outwardly slim and healthy/known plaques/can't get GPs to take it seriously problem, or any helpful insights? Many thanks.
Should a female with last tests +/- 2.5 years ago showing Ca test score of 34 at only 54 yrs old and CT angio <50% LAD narrowing, combined with belatedly detected FH and hypertension, be referred for follow-up tests or lipids testing? I moved last year from Australia, where I had just been referred for lipids studies and was under a cardiologist, to the UK, where I am now struggling to get specialist referrals on the state health system, despite being British and having paid into it for 35 years, and being unable to purchase reasonably priced health insurance owing to preexisting conditions. What concerns me is not knowing the rate at which my atherosclorosis has progressed since then after two very stressful years or whether it has stayed in check; whether the plaques are stable; what sort of non-HDL cholesterols I am producing; and what my longer term prognosis is. My other family members are on statins for high LDLs and my aunt has no plaque, even at age 81 – seems it's just me who's got this, but I've suffered a lot of mental stress and a long, very unhappy marriage I've recently left. The cardiologist wanted me on Lipitor 40mg, but I had severe muscle aches, abnormal liver function tests and abnormal CK levels after just 8 weeks on Lipitor 10mg, so am now on Ezetimibe. I've always been very slim, very fit, regular exerciser, naturally inclined to a pescatarian-Mediterranean type of diet – and I feel my appearance is counting against me in getting a referral. My total cholesterol is around 6.6, mostly HDL – triglycerides are usually 0.5-0.6 – LDLs 3.0 and my hypertension is upper end of normal/only mildly raised owing to Ramipril 5mg. My problem is that I look healthy and because I am not over 3.0 mmol LDL now (even though it's artificially achieved with strict diet, exercise and Ezetimibe), I am considered within targets and therefore not "at risk". But aren't people with known plaques meant to aim for much lower LDL targets, ie under 2.0? And if I have calcification and mild plaques already, so relatively young in life, despite lifestyle changes, aren't I also "at risk"? My Australian lipidologist has said he will try to expedite things for me in the UK if he can help, but I am seriously wondering whether what I really need to do is to put on heaps of weight and turn up with a cig and can of Coke in one hand and bacon double cheeseburger and chips in the other to get taken seriously. Meanwhile, several of my professional girlfriends, who also appear fit, have had heart attacks recently. Any views on what I should do? And any thoughts on what may have caused my plaques/what they could be made of and whether stable or not? Should I be worried? Thanks.
Females with heart disease are not taken seriously.
You are so right, alas. Since my post, I finally succeeded in getting a lipidologist referral in the UK – and it turns out that I have not got FH but high Lp(a) – over 121 – which in some ways is WORSE news, as Lp(a) is much harder to reduce than just LDL. All of a sudden I have become a subject of academic interest for lipidologists, and one apheresis unit staff member told me that they have patients with Lp(a) much lower than mine who are really ill. Nonetheless, nothing really is being done and I am no wiser, almost another year further on, as to what the progress of my plaques is because the UK NHS will not do an angiogram. They did an MRI perfusion scan and said that, because my blood flow to the heart was good and I remained asymptomatic and looked well, they assumed that my atherosclerosis could not have progressed mcuh as it hadn’t caused damage to my heart or blood flow. So, they won’t treat me unless I become sick or have an MI (if I don’t die.) Wonder if they’d think the same if I were an overweight male smoker of similar age? I asked for a second opinion and again, the cardiologist would not take me seriously; the conversation was patronising in the extreme – explained to me my own condition in simplistic terms likening my arteries to furred up water pipes (pretty insulting to a postgrad researcher with an Oxford degree) – and then wrote a sexist, BS letter to my GP talking about what a “delightful 57 year old lady” I am. All that has happened is that I have had 5mg of rosuvastatin added to my ezetimibe (no PCSK9 inhibitors, no niacin, no angiogram) and have been told by the lipidologist simply to come back in a year, just in case new drugs for Lp(a) are on the market by then (in reality, more likely 2-5 years until the ASO drugs come out.) So I have now increased my fish oils still further, become more strict about a dairy- and wheat-free, high good fats/low carb diet, increased my exercise and sleep and bought over the counter niacin plus l-lysine, alpha lipoic acid, acetyl l-carnitine, resveratrol, curcumin, magnesium, ubiquinol and, of course, my usual D3/K2. Oh, and aspirin at night, too. I just hope I don’t drop dead in a year’s time, at 58, like my grandmother did of a clot. Nice.
Thank you, it is indeed the LAD with the high reading
My score at 53 was 689
What advice have you been given? I am also 53 years old with a high score. Wish I had known about the calcium score CT years ago. I am now exercising every day; avoiding saturated fats, sugar, and white carbs; and on 20mg or pravastatin. 81mg of aspirin, and 1gm of fish oil per day.
I am 52 and have severe rheumatoid arthritis and fibromyalgia. I had an incident about 3 years ago and needed to see a cardiologist, who was not my regular doctor. According to my dr he did the tests out of order. My calcium score was 243. Then I passed the stress test and an echocardiogram along with every other test possible. My cholesterol was low and my blood pressure was normal. The incident I had was passing out at work and then at home two days later in the shower. The RA and fibromyalgia were my only health issues at the time. (And no. I was not pregnant). The dr told me that I had a 75% chance of having a heart attack, stroke, or sudden death in three years. Those three years have passed and I am still here. I have since moved 85 miles away and have had to find new doctors. My regular cardiologist said, when I moved a year ago, that my heart issues were minor. My question is this: Are my heart issues minor with a calcium score of 243? I do my best to eat healthy, and exercise when my RA isn’t causing too much pain. I don’t drink or smoke I take blood pressure and cholesterol meds as a preventive measure. Any guidance is greatly appreciated. Thank you
Dr. Sigurdsson,
I am a 53 year old woman who, otherwise relatively healthy, has just received a 53.8 calcium score (50.1 of which is in my Left Main coronary artery), which puts me in the 91st percentile for my gender/age. I have a very strong family history of heart disease: my Dad had his 1st heart attack at age 52 and both parents died from cardiac events.
Below are some numbers. The changes are based on changes in diet from my unhealthiest point in January 2017:
– I am thin, at 5’2.5″ and 104 lbs (down from 115 in 1/2017)
– LDL=96 (down from 127 in 1/2017)
– HDL=127 (up from 75 in 1/2017)
– H1AC=5.1 (down from 5.5 in 1/2017 and 5.7 in 7/2014)
– My EKG, stress test, and abdominal aorta ultrasound (all done in the past few months) were all normal.
– I eat a low fat and lean protein diet, with the following daily supplements:
o women’s 1-a-day multivitamin (since 1/2014)
o B-complex (since 5/2017)
o Ester C, 500 mg (since 2013)
o D3, 2000 mg (since 2014)
o K2, 500 mcg MK-4 + 100 mcg MK-7 (since 1/2017)
o Magnesium, 300 mg (since 1/2017)
o Probiotic (since 11/2015)
o Psyllium fiber, 6 grams (since 3/2013)
– I was diagnosed with Osteopenia in 9/2007, and took a generic form of Boniva for about 8 years
– I took low dose BCPs from 1981 – 2016ish.
– I have been on PremPro (.625mg estrogens/2.5mg progesterone) and Estrace cream since 1/2018, as I am post-menopausal.
– My cardiologist just put me on 20mg/night of pravastatin and 81mg/day of aspirin.
When I told my cardiologist that I think I eat well, but could exercise much more, he was unimpressed. He said that he doesn’t think my coronary calcium is linked to being sedentary and that he does not expect exercise would help. Even when I said I wanted to exercise regularly and repeat the CT Calcium Scoring Heart Scan in a couple of years, he said it was not advisable to repeat the test and that although I should exercise for other health benefits, it won’t help and could present its own risks for my situation with coronary calcium.
I am requesting your advice on how to reduce my coronary calcium. I am motivated to make changes. Should I adjust my supplements? Diet? Medications? I have already started 10k steps/day, which is a big improvement in my physical activity.
Please let me know what I can do to reverse, or at a minimum, stop the progression of my calcium buildup. Your advice will be highly appreciated!
Also, I would appreciate a recommendation for how to find a good local cardiologist (I live in McLean VA) who specializes in treating/reversing early onset coronary calcification in females. Thank you!!
You might look into Aged Garlic Extract (there have been some studies done with 2 Grams per day) . Also the Linus Pauling Protocol. I am doing the Aged Garlic, but not yet the Pauling Protocol. Not sure what Doc would have to say about this. Other than that and keeping inflammation down by low carving, I’m not sure what can be done.
Mark
My Agatston score is 457 and hoping to get a catherization as quickly as I can in these crazy Covid-19 days. Anyone else out there with thoughts?
I am 72 with a calcium score of 33. Not too bad I guess?
My ex husband just told me his score is 1200. Can this be true?
Hi Julie
Yes, a score of 1200 is a number you can expect to see quite often.
Axel
I used the calculator by inputting the information requested. I was unable to enter my correct HDL level because it would not accept anything over 100. I’m a vegetarian and my recent HDL level is reported at 180. How can I get a more accurate assessment?
Axel–
Thanks for this blog and forum!
I am a 66 male. No history. Tall and lean. I workout 5 days a week. My last lipid panel was a bit higher than usual. Total Chol 205, LDL 136, HDL 60 and the tri’s were 79 and the VLDL 14.I will easily get the LDL down with some fine tuning of diet and exercise.My Dad passed from an MI at age 68.
I just got my Calc. scan back—
Agatston 78
LMCA 0
LAD 34.56 Agat.
CX 0
RCA 44.1 Agat.
The recomendations on the report are–
rescan in 5 years
aspirin every day (which I have done for decades)
target chol LDL near or below 130
target tri’s near or above 50
target tri’s below 100
cal score target <100 and <50th percent.
Seems to me like my numbers are pretty close to this anyway?
I’ll try to get to my Doc or his nurse this week re the report. Do you think he will advise me to take statins????
My LM CAC went from 43.3 to 0 in one year. Guess wha tI’m doing is working
Hi Charles!
That is great! Can you tell us what you are doing that reduced your score?
I heard you can’t reverse the numbers. So what is it?
I’m 69, smoked a pack a day for 43 years, quit 8 years ago and have a calcium score of zero. Also a resting BPM of 52 and BP of 115/70.
I do have some mild emphysema & breathing issues but just yesterday I did a hike/jog covering 11 miles while climbing 2300 ft in 3:05:10. I typically do 80-100 miles monthly of hiking/jogging.
I take no drugs of any kind other tan an occasional ibuprofen, don’t drink, don’t smoke, don’t use caffeine. Seems I have good genes!
Turned 30 in March, had a CT scan out of curiosity. Play lots of tennis, never any chest pain. The score was 425! Yikes. Sent for a nuclear stress test. Passed easily. Now on Mediterranean diet as I have put on 20lbs in the past 3 years……., lost 15 lbs as of today, a low dose statin, low dose aspirin, vitamin K2/MK7, magnesium, fish oil, garlic, COQ10. Watching tons of YouTube’s on this. Ivor Cummins, Berg, and others. Hopefully modifying my risk factors as I am doing will improve my chances of survival. Fingers crossed.
Dr Sigurdsson,
I’m curious as to your opinion on the consumption of 2 grams of Aged Garlic extract daily to reduce arterial calcifications? Also your opinion on the Linus Pauling Protocol for doing the same? I’m 70 with diabetes and RA. Normal blood pressure (110/60) , HBA1c of 6.1, cholesterol 157, HDL 39, LDL 103, trigs 76. Walk 4 miles per day. Have had a few pcv’s but nothing alarming. Recently fell and had chest CT done which per the findings revealed “ Heart/vessels: The heart is normal in size with trace pericardial fluid. Heavy burden of coronary artery calcifications. Calcifications of the thoracic aorta without aneurysmal dilatation.”. I have not had a CAC. Cardiologist recommended Crestor 10 mg but I’m not delighted with potential side effects and other things I read , thus the reason for my questions concerning the alternative therapies. I have had an echocardiogram in Feb of 2021. Seemed normal. Left ventricular
ejection fraction was 55
Thanks!
Mark
Hello Dr. Axel, thanks for the wonderful explanation. Do you think that multivitamins pills need to be examined for its ingredients? and check whether it have any item that can mess with the CC score?
My doctor said the same, about inadequate calcium intake.
Nice information.
Nice article.
I’ve been advised to not worry about calcium. Elevated coronary artery calcium score
My question is do you recommend a stress test? Vitimin K?
@Julie A Peterson That is not too bad!! Mine is 4624.62. I work in the garden shifting tons of earth, walk 6 to 8 kilometers a day and don’t have any chest pain, shortness of breath or any other symptoms.
@Dr Sigurdsson: In your opinion is it possible to make any reduction in calcification by way of diet and lifestyle changes?
Hi David
There is no method available that can reduce the amount of coronary calcium.
Furthermore, there is no evidence for the hypothesis that reducing coronary calcium will be beneficial.
It is not known to what extent diet and lifestyle changes may affect calcium deposits in the coronary arteries.
However, lifestyle issues will certainly affect the risk of developing cardiovascular events such as heart attack and stroke.
What I am trying to say is that, although CCS is a marker of risk, we should not look at the calcium itself as a a target. Many individuals with high CCS never develop cardiovascular events.
I’m a female who just turned 46 and had a CT angiogram done last week. 9 lesions found and total calcium score is 671. Have only received the images from scan and report won’t be available for another 9 days. I don’t think my cardiologist has seen the images yet as he is only in the office 1 day a week. He works as ER cardiologist on other days. From the images, I seem to have about a 95% blockage in my LAD. I have lesions in 3 of my arteries. The CT scan was performed after 2 failed stress tests. I have a lot of chest pain, shortness of breath, and leg swelling. I’m really worried as I feel I will have a heart attack at any moment. I am so young and I am sure I need bypass surgery asap. My cholesterol levels are good, no diabetes, have hypertension. My father passed away from massive heart attack at 56. How can I make sure my cardiologist sees my results asap?
I hope you are well, Stephanie!
Hope you got everything strengthened out.
I am a 76 YO female. Taking meds for hypertension. I have a very strong history of heart disease on my paternal side. I have never smoked. In the past couple of years, my cholesterol has increased. I have treated it on my own without drugs. I have also virtually stopped eating meat, very little cheese, no eggs. I am physically active – hike, cross-country ski, bicycle, kayak.
I just had a CAC test and the score was 0.
Hi, I just got the report of the CT Angiogram today and found that the CAC score is 158. I am 60 years age. I don’t know what kind of treatment I need to pursue.
I hear you BK. I just go mine back and I’m 58 and the score is 120. That is moderate but given my family history, I expected higher. We both have the blockage of around a 72 year old. I wish I had not gone to my patient portal to look at the results before my doctor went over them with me. Now I’m playing Dr google.
I hear you BK. I just go mine back and I’m 58 and the score is 120. That is moderate but given my family history, I expected higher. We both have the blockage of around a 72 year old. I wish I had not gone to my patient portal to look at the results before my doctor went over them with me. Now I’m playing Dr google.Total Agatston coronary calcium score:
Calcium Score
LM: 0
LAD: 103.5
Circumflex: 0.6
RCA: 16.1
Total Score 120.2
Excellent Article!
Hello all. Just stumbled across this site and find it very interesting.
I recently had a CT angiogram and have an overall CAC of 283 but it is 272 in just my LAD. I have a <50% blockage in my LAD due to vulnerable plaque. My LDL is 133. I am unable to take statins because of high CK. My dr put in a prescription for Praluent but it was rejected by my insurance provider. Any suggestions for what I should do?
My husband just had a ct done and his number is 5100. He has an appointment with a cardiologist on the 27th, but I’d prefer he just go to the ER. He did have an EKG after getting the results and the EKG was ok. Do you all think it’s ok for him to wait? It’s 13 days.