Jaundice
Definition
Jaundice is a condition in which a person's skin and the whites of the eyes are discolored yellow due to an increased level of bile pigments in the blood resulting from
liver disease. Jaundice is sometimes called icterus, from a Greek word for the condition.
Description
In order to understand jaundice, it is useful to know about the role of the liver in producing bile. The most important function of the liver is the processing of chemical waste products like cholesterol and excreting them into the intestines as bile. The liver is the premier chemical factory in the body—most incoming and outgoing chemicals pass through it. It is the first stop for all nutrients, toxins, and drugs absorbed by the digestive tract. The liver also collects chemicals from the blood for processing. Many of these outward-bound chemicals are excreted into the bile. One particular substance, bilirubin, is yellow. Bilirubin is a product of the breakdown of hemoglobin, which is the protein inside red blood cells. If bilirubin cannot leave the body, it accumulates and discolors other tissues. The normal total level of bilirubin in blood serum is between 0.2 mg/dL and 1.2 mg/dL. When it rises to 3 mg/dL or higher, the person's skin and the whites of the eyes become noticeably yellow.
Bile is formed in the liver. It then passes into the network of hepatic bile ducts, which join to form a single tube. A branch of this tube carries bile to the gallbladder, where it is stored, concentrated, and released on a signal from the stomach. Food entering the stomach is the signal that stimulates the gallbladder to release the bile. The tube, which is called the common bile duct, continues to the intestines. Before the common bile duct reaches the intestines, it is joined by another duct from the pancreas. The bile and the pancreatic juice enter the intestine through a valve called the ampulla of Vater. After entering the intestine, the bile and pancreatic secretions together help in the process of digestion.
Causes and symptoms
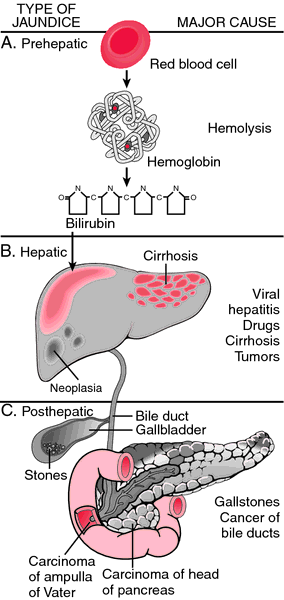
There are many different causes for jaundice, but they can be divided into three categories based on where they start-before, in, or after the liver (prehepatic, hepatic and post-hepatic). When bilirubin begins its life cycle, it cannot be dissolved in water. The liver changes it so that it is soluble in water. These two types of bilirubin are called unconjugated (insoluble) and conjugated (soluble). Blood tests can easily distinguish between these two types of bilirubin.
Hemoglobin and bilirubin formation
Bilirubin begins as hemoglobin in the blood-forming organs, primarily the bone marrow. If the production of red blood cells (RBCs) falls below normal, the extra hemoglobin finds its way into the bilirubin cycle and adds to the pool.
Once hemoglobin is in the red cells of the blood, it circulates for the life span of those cells. The hemoglobin that is released when the cells die is turned into bilirubin. If for any reason the RBCs die at a faster rate than usual, bilirubin can accumulate in the blood and cause jaundice.
Hemolytic disorders
Many disorders speed up the death of red blood cells. The process of red blood cell destruction is called hemolysis, and the diseases that cause it are called hemolytic disorders. If red blood cells are destroyed faster than they can be produced, the patient develops anemia. Hemolysis can occur in a number of diseases, disorders, conditions, and medical procedures:
- Malaria. The malaria parasite develops inside red blood cells. When it is mature it breaks the cell apart and swims off in the blood. This process happens to most of the parasites simultaneously, causing the intermittent symptoms of the disease. When enough cells burst at once, jaundice may result from the large amount of bilirubin formed from the hemoglobin in the dead cells. The pigment may reach the urine in sufficient quantities to cause "blackwater fever," an often lethal form of malaria.
- Side effects of certain drugs. Some common drugs can cause hemolysis as a rare but sudden side effect. These medications include some antibiotic and anti-tuberculosis medicines; drugs that regulate the heart-beat; and levodopa, a drug used to treat Parkinson's disease.
- Certain drugs in combination with a hereditary enzyme deficiency known as glucose-6-phosphate dehydrogenase (G6PD). G6PD is a deficiency that affects more than 200 million people in the world. Some of the drugs listed above are more likely to cause hemolysis in people with G6PD. Other drugs cause hemolysis only in people with this disorder. Most important among these drugs are anti-malarial medications such as quinine, and vitamins C and K.
- Poisons. Snake and spider venom, certain bacterial toxins, copper, and some organic industrial chemicals directly attack the membranes of red blood cells.
- Artificial heart valves. The inflexible moving parts of heart valves damage RBCs as they flutter back and forth. This damage is one reason to recommend pig valves and valves made of other organic materials.
- Hereditary RBC disorders. There are a number of hereditary defects that affect the blood cells. There are many genetic mutations that affect the hemoglobin itself, the best-known of which is sickle cell disease. Such hereditary disorders as spherocytosis weaken the outer membrane of the red cell. There are also inherited defects that involve the internal chemistry of RBCs.
- Enlargement of the spleen. The spleen is an organ that is located near the upper end of the stomach and filters the blood. It is supposed to filter out and destroy only worn-out RBCs. If it has become enlarged, it filters out normal cells as well. Malaria, other infections, cancers and leukemias, some of the hereditary anemias mentioned above, obstruction of blood flow from the spleen—all these and many more diseases can enlarge the spleen to the point where it removes too many red blood cells.
- Diseases of the small blood vessels. Hemolysis that occurs in diseased small blood vessels is called micro-angiopathic hemolysis. It results from damage caused by rough surfaces on the inside of the capillaries. The RBCs squeeze through capillaries one at a time and can easily be damaged by scraping against the vessel walls.
- Immune reactions to RBCs. Several types of cancer and immune system diseases produce antibodies that react with RBCs and destroy them. In 75% of cases, this reaction occurs all by itself, with no underlying disease to account for it.
- Transfusions. If a patient is given an incompatible blood type, hemolysis results.
- Kidney failure and other serious diseases. Several diseases are characterized by defective blood coagulation that can destroy red blood cells.
- Erythroblastosis fetalis. Erythroblastosis fetalis is a disease of newborns marked by the presence of too many immature red blood cells (erythroblasts) in the baby's blood. When a baby's mother has a different blood type, antibodies from the mother may leak into the baby's circulation and destroy blood cells. This reaction can produce severe hemolysis and jaundice in the newborn. Rh factor incompatibility is the most common cause.
- High bilirubin levels in newborns. Even in the absence of blood type incompatibility, the newborn's bilirubin level may reach threatening levels.
Normal jaundice in newborns
Normal newborn jaundice is the result of two conditions occurring at the same time—a pre-hepatic and a hepatic source of excess bilirubin. First of all, the baby at birth immediately begins converting hemoglobin from a fetal type to an adult type. The fetal type of hemoglobin was able to extract oxygen from the lower levels of oxygen in the mother's blood. At birth the infant can extract oxygen directly from his or her own lungs and does not need the fetal hemoglobin any more. So fetal hemoglobin is removed from the system and replaced with adult hemoglobin. The resulting bilirubin loads the system and places demands on the liver to clear it. But the liver is not quite ready for the task, so there is a period of a week or so when the liver has to catch up. During that time the baby is jaundiced.
Hepatic jaundice
Liver diseases of all kinds threaten the organ's ability to keep up with bilirubin processing.
Starvation, circulating infections, certain medications, hepatitis, and
cirrhosis can all cause hepatic jaundice, as can certain hereditary defects of liver chemistry, including Gilbert's syndrome and Crigler-Najjar syndrome.
Post-hepatic jaundice
Post-hepatic forms of jaundice include the jaundices caused by failure of soluble bilirubin to reach the intestines after it has left the liver. These disorders are called obstructive jaundices. The most common cause of obstructive jaundice is the presence of
gallstones in the ducts of the biliary system. Other causes have to do with
birth defects and infections that damage the bile ducts; drugs; infections; cancers; and physical injury. Some drugs—and
pregnancy on rare occasions—simply cause the bile in the ducts to stop flowing.
Symptoms and complications associated with jaundice
Certain chemicals in bile may cause
itching when too much of them end up in the skin. In newborns, insoluble bilirubin may get into the brain and do permanent damage. Long-standing jaundice may upset the balance of chemicals in the bile and cause stones to form. Apart from these potential complications and the discoloration of skin and eyes, jaundice by itself is inoffensive. Other symptoms are determined by the disease producing the jaundice.
Diagnosis
Physical examination
In many cases the diagnosis of jaundice is suggested by the appearance of the patient's eyes and complexion. The doctor will ask the patient to lie flat on the examining table in order to feel (palpate) the liver and spleen for enlargement and to evaluate any abdominal
pain. The location and severity of abdominal pain and the presence or absence of
fever help the doctor to distinguish between hepatic and obstructive jaundice.
Laboratory tests
Disorders of blood formation can be diagnosed by more thorough examination of the blood or the bone marrow, where blood is made. Occasionally a bone marrow biopsy is required, but usually the blood itself will reveal the diagnosis. The spleen can be evaluated by an ultrasound examination or a nuclear scan if the
physical examination has not yielded enough information.
Liver disease is usually assessed from blood studies alone, but again a biopsy may be necessary to clarify less obvious conditions. A
liver biopsy is performed at the bedside. The doctor uses a thin needle to take a tiny core of tissue from the liver. The tissue sample is sent to the laboratory for examination under a microscope.
Assessment of jaundice in newborns
Newborns are more likely to have problems with jaundice if:
- They are premature.
- They are Asian or Native Americans.
- They have been bruised during the birth process.
- They have lost too much weight during the first few days.
- They are born at high altitude.
- The mother has diabetes.
- Labor had to be induced.
In 2003, research was continuing to find noninvasive methods to determine bilirubin levels in newborns so that physicians did not have to rely on visual examination alone to determine which infants should receive blood tests. Once these measurements of skin pigment can be shown effective and cost-effective in clinical practice, they may become more available. Another study used this measurement method incorporated into home health visits to monitor babies within 24 hours of discharge from the hospital following birth.
Imaging studies
Disease in the biliary system can be identified by imaging techniques, of which there are many. X rays are taken a day after swallowing a contrast agent that is secreted into the bile. This study gives functional as well as anatomical information. There are several ways of injecting contrast dye directly into the bile ducts. It can be done through a thin needle pushed straight into the liver or through a scope passed through the stomach that can inject dye into the Ampulla of Vater. CT and MRI scans are very useful for imaging certain conditions like cancers in and around the liver or gallstones in the common bile duct.
Treatment
Jaundice in newborns
Newborns are the only major category of patients in whom the jaundice itself requires attention. Because the insoluble bilirubin can get into the brain, the amount in the blood must not go over certain levels. If there is reason to suspect increased hemolysis in the newborn, the bilirubin level must be measured repeatedly during the first few days of life. If the level of bilirubin shortly after birth threatens to go too high, treatment must begin immediately. Exchanging most of the baby's blood was the only way to reduce the amount of bilirubin until a few decades ago. Then it was discovered that bright blue light rendered the bilirubin harmless. Now jaundiced babies are fitted with eye protection and placed under bright fluorescent lights. The light chemically alters the bilirubin in the blood as it passes through the baby's skin. In 2003, researchers were testing a new drug called Stanate that showed promise in blocking bilirubin production. However, debate concerning the use of the drug for treatment of only those infants with jaundice or as a preventive measure was delaying its FDA approval and widespread use.
Hemolytic disorders
Hemolytic diseases are treated, if at all, with medications and blood transfusions, except in the case of a large spleen. Surgical removal of the spleen (
splenectomy) can sometimes cure
hemolytic anemia. Drugs that cause hemolysis or arrest the flow of bile must be stopped immediately.
Hepatic jaundice
Most liver diseases have no specific cure, but the liver is so robust that it can heal from severe damage and regenerate itself from a small remnant of its original tissue.
Key terms
Ampulla of Vater — The widened portion of the duct through which the bile and pancreatic juices enter the intestine. Ampulla is a Latin word for a bottle with a narrow neck that opens into a wide body.
Anemia — A condition in which the blood does not contain enough hemoglobin.
Bilirubin — A reddish pigment excreted by the liver into the bile as a breakdown product of hemoglobin.
Erythroblastosis fetalis — A disorder of newborn infants marked by a high level of immature red blood cells (erythroblasts) in the infant's blood.
Hemoglobin — The red chemical in blood cells that carries oxygen.
Hemolysis — The destruction or breakdown of red blood cells.
Icterus — Another name for jaundice.
Pancreas — The organ beneath the stomach that produces digestive juices, insulin, and other hormones.
Sickle cell disease — A hereditary defect in hemoglobin synthesis that changes the shape of red cells and makes them more fragile.
Post-hepatic jaundice
Obstructive jaundice frequently requires a surgical cure. If the original passageways cannot be restored, surgeons have several ways to create alternate routes. A popular technique is to sew an open piece of intestine over a bare patch of liver. Tiny bile ducts in that part of the liver will begin to discharge their bile into the intestine, and pressure from the obstructed ducts elsewhere will find release in that direction. As the flow increases, the ducts grow to accommodate it. Soon all the bile is redirected through the open pathways.
Prevention
Erythroblastosis fetalis can be prevented by giving an Rh negative mother a gamma globulin solution called RhoGAM whenever there is a possibility that she is developing antibodies to her baby's blood. G6PD hemolysis can be prevented by testing patients before giving them drugs that can cause it. Medication side effects can be minimized by early detection and immediate cessation of the drug. Malaria can often be prevented by certain precautions when traveling in tropical or subtropical countries. These precautions include staying in after dark; using prophylactic drugs such as mefloquine; and protecting sleeping quarters with mosquito nets treated with insecticides and mosquito repellents. In 2003, new studies showed promise for a possible vaccine against malaria. Early trials showed that
vaccination combination might stimulate T-cell activity against malaria, the best type of protection that researchers can hope to find. However, further studies will have to be done.
Resources
Periodicals
Grimm, David. "Baby Pigment Peril." U.S. News & World Report July 28, 2003: 39.
Lawrence, David. "Combination Malaria Vaccine Shows Early Promise in Human Trials." The Lancet May 31, 2003: 1875.
Morantz, Carrie, and Brian Torrey. "AHRQ Report on Neonatal Jaundice." American Family Physician June 1, 2003: 2417.
Richmond, Glenn, Melissa Brown, and Patricia Wagstaff. "Using a Home Care Model to Monitor Bilirubin Levels in Early Discharged Infants." Topics in Health Information Management January-March 2003: 39-43.
Organizations
American Liver Foundation. 1425 Pompton Ave., Cedar Grove, NJ 07009. (800) 223-0179. http://www.liverfoundation.org.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
jaundice
[jawn´dis] yellowness of skin, sclerae, mucous membranes, and excretions due to hyperbilirubinemia and deposition of
bile pigments. It is usually first noticeable in the eyes, although it may come on so gradually that it is not immediately noticed by those in daily contact with the jaundiced person. Called also
icterus.
Jaundice is not a disease; it is a symptom of a number of different diseases and disorders of the
liver and
gallbladder and of hemolytic blood disorders. One such disorder is the presence of a gallstone in the common bile duct, which carries bile from the liver to the intestine. This may obstruct the flow of bile, causing it to accumulate and enter the bloodstream. The obstruction of bile flow may cause bile to enter the urine, making it dark in color, and also decrease the bile in the stool, making it light and clay-colored. This condition requires surgery to remove the gallstone before it causes serious liver injury.
The pigment causing jaundice is called
bilirubin. It is derived from hemoglobin that is released when erythrocytes are hemolyzed and therefore is constantly being formed and introduced into the blood as worn-out or defective erythrocytes are destroyed by the body. Normally the liver cells absorb the bilirubin and secrete it along with other bile constituents. If the liver is diseased, or if the flow of bile is obstructed, or if destruction of erythrocytes is excessive, the bilirubin accumulates in the blood and eventually will produce jaundice. Determination of the level of bilirubin in the blood is of value in detecting elevated bilirubin levels at the earliest stages before jaundice appears, when liver disease or hemolytic anemia is suspected.
Patient Care. Assessment of the patient with jaundice includes observations of the degree and location of yellowing, noting the color of urine and stools, and the presence of itching. Since jaundice can be accompanied by severe itching, frequent skin care is important to preserve skin integrity. Tepid sponge baths can help reduce discomfort and promote rest.
Patients with severe jaundice are at risk for encephalopathic changes that produce confusion, impaired mentation, and altered levels of consciousness. The potential for injury is increased and demands vigilance and safety measures to protect the patient.
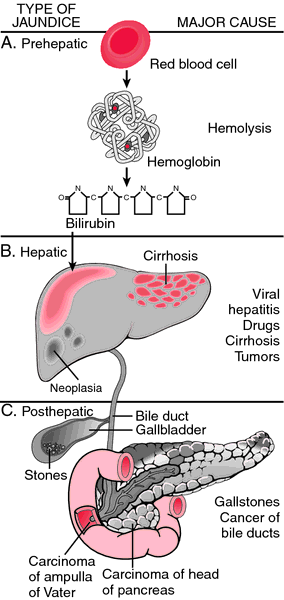
Jaundice may be attributable to prehepatic (A), hepatic (B), or posthepatic (C) causes. From Damjanov, 2000.
acholuric jaundice jaundice without bilirubinemia, associated with elevated unconjugated bilirubin that is not excreted by the kidney.
Familial acholuric jaundice is another name for the hereditary form of
hemolytic jaundice.
breast milk jaundice elevated unconjugated bilirubin in some breast-fed infants due to the presence of an abnormal
pregnane that inhibits glucuronyl transferase conjugating activity.
cholestatic jaundice that resulting from abnormality of bile flow in the liver.
hepatocellular jaundice jaundice caused by injury to or disease of the liver cells.
nonhemolytic jaundice that due to an abnor-mality in bilirubin metabolism.
obstructive jaundice that due to blockage of the flow of bile.
physiologic jaundice mild icterus neonatorum during the first few days after birth.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
jaundice
(jon'dis) [Fr. jaunisse, fr. jaune, yellow] 

JAUNDICE: Skin of the abdomen
Yellow staining of body tissues and fluids, due to excessive levels of bilirubin in the bloodstream. Jaundice is not usually visible until the total bilirubin level rises above 3 mg/dl. It is a symptom of many illnesses, including those marked by any of the following: obstruction of the biliary tract by gallstones, inflammatory masses, or tumors (such as cholecystitis, pancreatic carcinoma); slowing of the release of bile from hepatic portals (such as cholestasis); alteration of bile metabolism at the cellular level (such as in genetic diseases such as Gilbert's disease); release of bilirubin because of liver cell injury by toxins or viruses (such as acetaminophen overdose; hepatitis B virus infection); release of bile pigments as a result of the destruction or ineffective manufacturing of red blood cells (such as hemolysis; hereditary spherocytosis); or resorption of bile from hematomas within the body, esp. after trauma. See:
illustrationjaundiced (jon'dist),
adjective Synonym:
icterusSymptoms
Deposits of bilirubin in the skin often cause itching. Other symptoms of jaundice depend on whether the bilirubin is direct (conjugated [i.e., soluble in body fluids]) or indirect (unconjugated). Obstructive jaundice causes conjugated hyperbilirubinemia; in this disease, bile pigments dissolve in the urine, which turns bright green, and the stool appears gray or white owing to the deprivation of bile.
Diagnosis
Tests to determine the cause of jaundice include a carefully performed history and physical exam, urinalysis (positive for bilirubin only in conjugated hyperbilirubinemia), liver function tests, blood tests for hepatitis, and abdominal ultrasonography. Invasive diagnostic testing with cholangiography, endoscopic retrograde cholangiopancreatography, or percutaneous trans-hepatic cholangiography is performed when occult biliary obstruction is suspected.
Treatment
The precise cause of jaundice must be determined in each patient to provide suitable therapies. For example, patients with gallstones obstructing the cystic duct need surgical treatment, and newborns with severe jaundice may require treatment with ultraviolet light to prevent kernicterus, but jaundiced patients with acute hepatitis A usually heal with symptomatic rather than specific remedies.
acholuric jaundice
Jaundice without bile pigment in the urine. Most of the excess bilirubin is unconjugated.
breast milk jaundice
, breast-feeding jaundiceHyperbilirubinemia resulting from pregnanediol or free fatty acids that inhibit bilirubin conjugation. Serum bilirubin level usually peaks above 20 ml/dl by 14 to 21 days of age. Some pediatricians recommend stopping breast-feeding for 24 to 36 hr if the level exceeds 20 ml/dl. If the infant's bilirubin level drops rapidly, the mother may resume nursing. It typically lasts for the first week of life or until the mother produces adequate milk.
cholestatic jaundice
Jaundice produced by failure of bile to flow to the duodenum. It may be caused by intrahepatic bile duct obstruction (as in certain drug reactions), liver cell damage (as in viral hepatitis), or extrahepatic obstruction to the flow of bile (as in cholecystitis).
congenital jaundice
Jaundice occurring at or shortly after birth.
familial nonhemolytic jaundice
Gilbert syndrome.hematogenous jaundice
Hemolytic jaundice.hemolytic jaundice
Jaundice caused by the fragmentation of red blood cells and the release of unconjugated bilirubin in the bloodstream. This finding is associated with hemolytic anemia (HA). Because the bilirubin is not conjugated by the liver, it is not soluble in water and does not discolor the urine. Many conditions may be responsible, including congenital HA; sickle cell anemia; autoimmune HA (as in infectious mononucleosis or Mycoplasma pneumoniae infections); microangiopathic HA (as in hemolytic uremic syndrome); or transfusion-associated HA.
Synonym: hematogenous jaundice; hemolytic icterus; nonobstructive icterushemorrhagic jaundice
Leptospiral jaundice.hepatocellular jaundice
Jaundice resulting from disease of liver cells, e.g., in acute hepatitis. Synonym: parenchymatous jaundice
infectious jaundice
Infectious hepatitis.leptospiral jaundice
Jaundice caused by leptospirosis. Synonym: hemorrhagic jaundice
neonatal jaundice
Nonpathological jaundice affecting newborns, usually resulting from the destruction of red blood cells by the immature liver at birth. The destruction of red blood cells causes unconjugated bilirubin to accumulate in the blood and skin. Benign neonatal jaundice manifests 48 to 72 hr after birth, lasts only a few days, and typically does not require therapy.
Patient care
Levels of bilirubin less than 2 in the first week of life are common, occurring in about 80% of premature babies and half of all full-term babies. They are typically not hazardous to the developing infant. When jaundice develops in the first 24 hr of life, however, or when bilirubin levels exceed published guidelines, kernicterus (neurotoxicity caused by bilirubin) may develop. Infants with potentially damaging levels of bilirubin in the blood are treated with phototherapy (bili lights). Synonym: icterus neonatorum; jaundice of newborn; physiologic jaundicehemolytic disease of the newborn; isoimmunization; kernicterus; phototherapy;
jaundice of newborn
Neonatal jaundice.nonhemolytic jaundice
Jaundice due to abnormal metabolism of bilirubin or to biliary tract obstruction, and not to excessive destruction of red blood cells.
obstructive jaundice
Jaundice caused by a mechanical impediment to the flow of bile from the liver to the duodenum. Gallstones are the most common cause. Cholangitis, obstructing cancers, cysts, parasites in the bile ducts, or hepatic abscesses are responsible less frequently. Synonym:
obstructive icterus;
postobstructive jaundice;
regurgitation jaundiceSymptoms
The condition is marked by yellow staining of the skin, mucous membranes, sclera, and secretions. The patient may complain of pruritus caused by bile pigments in the skin. The urine is yellow or green, but the stools turn light or clay-colored because of absence of bile pigment in the intestinal tract. Acute obstruction to the flow of bile causes right upper quadrant pain and may be associated with biliary colic due to entrapment of gallstones.
Treatment
Cholecystectomy with common bile duct exploration (choledochostomy) is used to resolve obstructive jaundice caused by gallstones. Radical surgeries (as the Whipple procedure) or stenting of the biliary tract with or without external damage may temporarily relieve obstructive jaundice caused by cancer.
parenchymatous jaundice
Hepatocellular jaundice.pathological jaundice of newborn
Hemolytic disease of the newborn.physiologic jaundice
Neonatal jaundice.postobstructive jaundice
Obstructive jaundice.regurgitation jaundice
Obstructive jaundice.retention jaundice
Jaundice resulting from the inability of liver cells to remove bile pigment from circulation.
spirochetal jaundice
Leptospirosis.toxic jaundice
Jaundice resulting from chemical injury to the liver or sepsis.
Medical Dictionary, © 2009 Farlex and Partners