Acute Respiratory Failure
Medically reviewed by Drugs.com. Last updated on May 6, 2024.
What is acute respiratory failure (ARF)?
ARF is a condition that happens when your lungs cannot get enough oxygen into your blood. ARF can also happen when your lungs cannot get the carbon dioxide out of your blood. A buildup of carbon dioxide in your blood can cause damage to your organs. The decrease in oxygen and the buildup of carbon dioxide can happen at the same time. Acute respiratory failure may develop in minutes, hours, or days.
 |
What increases my risk for ARF?
- Pneumonia, fluid buildup in the lungs from heart failure, COVID-19, or acute respiratory distress syndrome (ARDS)
- A condition such as Guillain-Barré syndrome or myasthenia gravis that affects nerves or muscles used for breathing
- A blood clot in your lungs (pulmonary embolism, or PE) or brain (stroke)
- An exacerbation of COPD or asthma
- A lung condition such as cystic fibrosis or bronchiolitis
- A heart attack
- Medicines or drugs that slow your breathing, such as opioids or alcohol
- A head trauma or a collapsed lung
What are the symptoms of ARF?
Symptoms depend on the kind of ARF you have, and if it is mild, moderate, or severe:
- Rapid or noisy breathing
- Flushed skin
- Heart rate that is faster or slower than usual
- Shortness of breath, dizziness, or headaches
- Muscle twitches, trouble walking, or tingling in your hands or feet
- Feeling drowsy or sleepy during the day, confusion, or mood changes
- Swelling of your hands and feet
- A bluish color on your skin, fingernails, and lips, or pale skin
- Vision problems, seizures, or loss of consciousness
How is ARF diagnosed?
Your healthcare provider will ask about your symptoms and when they began. Tests do not always diagnose ARF. Your provider will also look for signs of medical conditions that may mean you have ARF. Examples include cor pulmonale and pulmonary hypertension. You may need any of the following:
- An arterial blood gas (ABG) test measures the amount of oxygen and carbon dioxide in your blood. An ABG test also measures the pH of your blood.
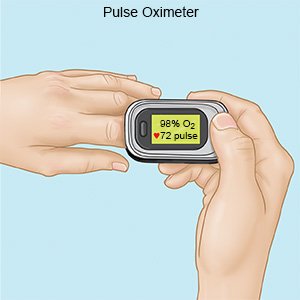
- Pulse oximetry will show the level of oxygen in your blood.
How is ARF treated?
Treatment depends on the cause and how severe your symptoms are. You may need any of the following:
- Medicines may be given to open your airways or relieve fluid buildup in your arms or legs. You may also need medicines to treat the cause of your ARF.
- Extra oxygen may be given if your blood oxygen levels are low.
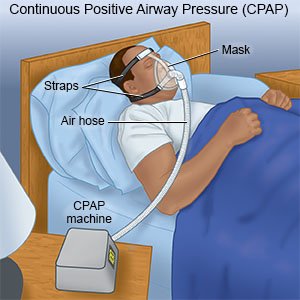
- Ventilation helps get oxygen into your lungs and carbon dioxide out. Ventilation also makes the work of breathing easier. Some systems, such as a CPAP or BiPAP, may only be needed while you sleep. A mechanical ventilator may be needed some or all of the time. It is attached to a mask or breathing tube.
- A procedure may be used to drain fluid if you have a pleural effusion (fluid between the lining of the lungs and the chest). Air may be drained from around your lung if you have a collapsed lung.
What can I do to manage or prevent shortness of breath?
- Check your oxygen level, if directed. Your healthcare provider may recommend you use a pulse oximeter (pulse ox). A pulse ox is a device that measures the amount of oxygen in your blood. You may be given an oxygen level goal for when you are at rest and another goal for activity.
- Use your oxygen as directed. You may need extra oxygen if your blood oxygen level is lower than it should be.
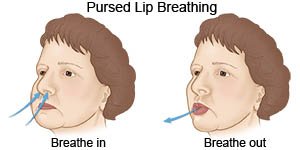
- Use pursed-lip breathing any time you feel short of breath. Take a deep breath in through your nose. Slowly breathe out through your mouth with your lips pursed for twice as long as you inhaled. You can also practice this breathing pattern while you bend, lift, climb stairs, or exercise. It slows down your breathing and helps move more air in and out of your lungs.
What can I do to manage ARF?
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung damage and make your symptoms worse. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products. Secondhand smoke can also make your symptoms worse. Avoid others who are smoking.
- Prevent the spread of germs. Wash your hands often with soap and water. Use gel hand cleanser when soap and water are not available. Do not touch your eyes, nose, or mouth unless you have washed your hands first. Cover your mouth when you cough. Cough into a tissue or your shirtsleeve so you do not spread germs from your hands. If you are sick, stay away from others as much as possible.

- Limit alcohol. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Ask about vaccines you may need. Vaccines can help prevent some lung infections. Examples include pneumonia, COVID-19, pertussis (whooping cough), tuberculosis (TB), and diphtheria. Get a flu vaccine every year as soon as it is recommended, usually in September or October.
- Prepare for emergencies. Keep phone numbers for your healthcare provider, hospital, and someone close to you with you at all times.
Call your local emergency number (911 in the US) or have someone call if:
- You have more trouble catching your breath.
- You have stopped breathing.
When should I call my doctor?
- You have new symptoms.
- Your symptoms get worse.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
