Sepsis is a potentially fatal disease. For the best chance of treating it successfully, clinicians need to recognize it early and treat it quickly; however it can be difficult to diagnose, especially early in the course of the disease.
Sepsis coexists with an infection, and often with other comorbidities, all of which produce their own signs and symptoms. The challenge is to pick out the signs of sepsis from among the other abnormalities plaguing the patient. To make sepsis easier to identify, there has been an effort to standardize its definition despite its wide range of presentations. Following are the current clinical definitions of sepsis and its related terms. Earlier terms for the syndrome included “blood poisoning”, “bacteremia,” and “septicemia”, but in 1991 the American College of Chest Physicians standardized terminology to include, from mild to severe: infection, SIRS, sepsis, severe sepsis, septic shock, and multiple organ dysfunction syndrome (MODS).
Source: Hadroncastle, Wikimedia Commons.
Infection is the presence of microorganisms causing an inflammatory response and triggering the natural immune system to fight the infection.
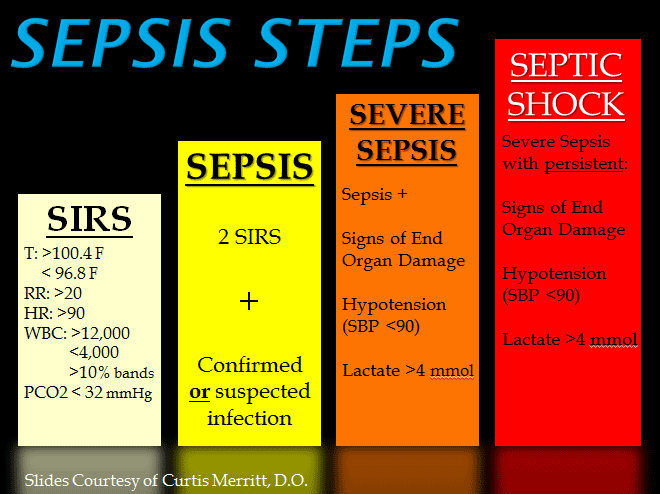
Systemic inflammatory response syndrome (SIRS) is an inflammatory reaction that produces at least two of the following four signs:
- Abnormal body temperature: hypothermia, <96.8°F/36°C; or fever, >100.4°F/38.3°C
- Tachycardia (>90 beats/min)
- Tachypnea (>20 breaths/min) or a rate sufficient to produce PaCO2 <32 mm Hg)
- Abnormal white blood cell count (>12,000/mm3, <4000/mm3, or >10% immature WBCs)
SIRS is generally triggered by an infection that produces abnormal white blood cell counts, but it can also arise from noninfectious sources such as trauma, hemorrhage, burns, surgery, adrenal insufficiency, pulmonary embolism, dissecting or ruptured aortic aneurysm, myocardial infarction, occult hemorrhage, cardiac tamponade, post cardiopulmonary bypass syndrome, autoimmune disorders, pancreatitis, vasculitis, anaphylaxis, or drug overdose (Neviere, 2013a,b). Untreated or unresolved SIRS can progress to sepsis, severe sepsis, septic shock, or MODS.
Sepsis is an uncontrolled complete-body response to an infection, regardless of whether the infection is local, extensive, or bloodborne. This over-reactive response produces two or more of the signs of SIRS. The septic reaction threatens to damage organs and to destabilize the circulatory system. Sepsis can lead to organ failure, shock, and death (Surviving Sepsis Campaign, 2011).
Severe sepsis, or sepsis syndrome, is present when the patient has progressed to a stage in which one or more organs or organ systems begin to fail. The Surviving Sepsis Campaign no longer uses the term severe sepsis but simply sepsis.
Severe sepsis is sepsis plus one of the following clinical problems:
- Cardiovascular system dysfunction
- Acute respiratory distress syndrome (ARDS)
- Dysfunction of two or more other organs or systems
Septic Shock occurs when blood pressure cannot be maintained above 90 mmHg systolic despite adequate fluid resuscitation. The sepsis creates massive vasodilation and without adequate circulatory support and pressure, organs become hypoxic and can eventually die. Septic shock is acute circulatory failure with refractory (difficult to reverse) hypotension that is unexplainable by other causes. The term shock describes a condition in which many tissues throughout the body become hypoxic due to poor perfusion. In shock, normal homeostatic mechanisms are either not functioning or not adequate to deliver enough oxygen to tissues. If it is not reversed, shock leads to organ failure and death. Septic shock is a form of distributive shock. In septic shock, there is hypotension and vasodilation that cannot be reversed by giving adequate fluids. When the hypotension of septic shock does not respond to vasopressors, the condition is called refractory septic shock (Munford & Suffredini, 2009).
Shock is categorized as:
- Hypovolemic, in which the patient has suffered a large loss of fluid, such as by hemorrhage.
- Cardiogenic, in which the heart cannot pump sufficient blood volume, such as after a major myocardial infarction or congestive heart failure.
- Distributive, in which sufficient fluid cannot be kept inside the vasculature, as in anaphylaxis, sepsis or neurogenic causes (Gaieski, 2013).
- Multiple Organ Dysfunction Syndrome (MODS) is the failure of a number of organs or organ systems caused by an illness. To be considered “in failure,” an organ must persist in its severe dysfunction for at least 24 hours. As the number of failing organs increases, so does the risk of mortality.
Other terms related to sepsis include:
- Microbial infection—growth of nonnative microbes or overgrowth of native microbes in the body
- Bacteremia—viable bacteria in the bloodstream
- Hypotension—systolic blood pressure <90 mm Hg or mean arterial pressure <60 mm Hg, or drop in systolic blood pressure of >40 mm Hg from the patient’s baseline (Dellinger et al., 2013)
- Mean arterial pressure (MAP)—An indicator of general tissue perfusion-pressure, the arterial blood pressure is the driving force to push oxygen and nutrients from the vascular system into tissues and cells of the body. If cardiac output is constant, blood flow to tissues does not change until blood pressure falls below a critical value. Any additional decrease will compromise blood flow and oxygen to the organ. The Surviving Sepsis Campaign (discussed later) recommends a MAP of >65 during the initial resuscitation period (Corrêa et al, 2013). Normal MAP is 70–110 mm Hg.
Test Your Knowledge
Severe sepsis, or sepsis syndrome, is:
- The stage in which organs begin to fail.
- Identified by the failure of three organs.
- Sepsis that has progressed to suppurating wounds.
- Seen when the patient is unconscious from admission to the ED.
Septic shock is:
- Acute cardiac failure reversible with medication.
- Preventable by adequate infection controls such as hand washing.
- Acute circulatory failure with refractory hypotension.
- Associated with pulmonary collapse.
Apply Your Knowledge
Q: In our case scenario, what kind of sepsis did Nancy Murphy have? Why?
A: She initially presented with a pneumonia that could be treated with antibiotics. Due to the delay in IV therapy, the inflammatory response moved in severity from an infection to SIRS and later to full sepsis.
Answers: A,C
