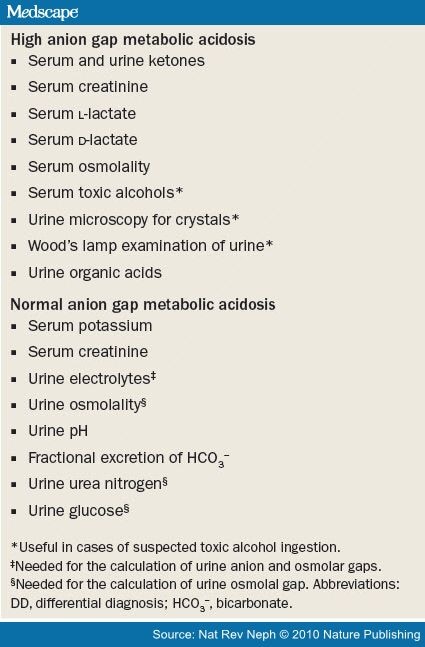
Box 1.
Tests useful in the DD of metabolic acidosis
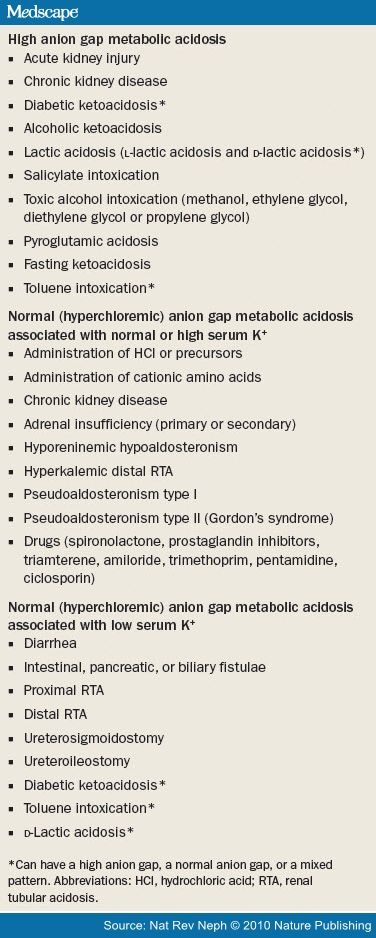
Box 2.
Causes of metabolic acidosis
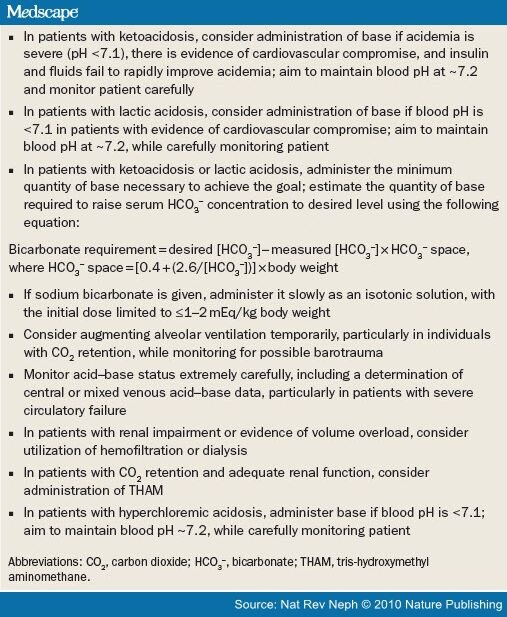
Box 3.
Recommendations for the treatment of acute metabolic acidosis
CME
Metabolic Acidosis: Pathophysiology, Diagnosis and Management
- Authors: Jeffrey A. Kraut, MD; Nicolaos E. Madias, MD
- CME Released: 3/23/2010
- THIS ACTIVITY HAS EXPIRED FOR CREDIT
- Valid for credit through: 3/23/2011, 11:59 PM EST
Target Audience and Goal Statement
This activity is intended for primary care physicians, intensive medicine specialists, nephrologists, and other physicians who care for patients with metabolic acidosis.
The goal of this activity is to describe the diagnosis and treatment of metabolic acidosis.
Upon completion of this activity, participants will be able to:
- Describe the pathophysiology of metabolic acidosis
- Diagnose the cause of metabolic acidosis effectively
- Distinguish the causes of metabolic acidosis associated with an elevated anion gap
- Treat metabolic acidosis effectively
Disclosures
As an organization accredited by the ACCME, Medscape, LLC, requires everyone who is in a position to control the content of
an education activity to disclose all relevant financial relationships with any commercial interest. The ACCME defines "relevant
financial relationships" as financial relationships in any amount, occurring within the past 12 months, including financial
relationships of a spouse or life partner, that could create a conflict of interest.
Medscape, LLC, encourages Authors to identify investigational products or off-label uses of products regulated by the US Food
and Drug Administration, at first mention and where appropriate in the content.
Accreditation Statements

-
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and Nature Publishing Group. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this educational activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™ . Physicians should only claim credit commensurate with the extent of their participation in the activity.
Medscape, LLC staff have disclosed that they have no relevant financial relationships.
For Physicians
For questions regarding the content of this activity, contact the accredited provider for this CME/CE activity noted above. For technical assistance, contact [email protected]
Instructions for Participation and Credit
There are no fees for participating in or receiving credit for this online educational activity. For information on applicability
and acceptance of continuing education credit for this activity, please consult your professional licensing board.
This activity is designed to be completed within the time designated on the title page; physicians should claim only those
credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the
activity online during the valid credit period that is noted on the title page.
Follow these steps to earn CME/CE credit*:
- Read the target audience, learning objectives, and author disclosures.
- Study the educational content online or printed out.
- Online, choose the best answer to each test question. To receive a certificate, you must receive a passing score as designated at the top of the test. MedscapeCME encourages you to complete the Activity Evaluation to provide feedback for future programming.
You may now view or print the certificate from your CME/CE Tracker. You may print the certificate but you cannot alter it.
Credits will be tallied in your CME/CE Tracker and archived for 6 years; at any point within this time period you can print
out the tally as well as the certificates by accessing "Edit Your Profile" at the top of your Medscape homepage.
*The credit that you receive is based on your user profile.
Metabolic Acidosis: Pathophysiology, Diagnosis and Management
CME Released: 3/23/2010
Valid for credit through: 3/23/2011, 11:59 PM EST
processing....
Abstract and Introduction
Abstract
Metabolic acidosis is characterized by a primary reduction in serum bicarbonate (HCO3 -) concentration, a secondary decrease in the arterial partial pressure of carbon dioxide (PaCO2) of ~1 mmHg for every 1 mmol/l fall in serum HCO3 - concentration, and a reduction in blood pH. Acute forms (lasting minutes to several days) and chronic forms (lasting weeks to years) of the disorder can occur, for which the underlying cause/s and resulting adverse effects may differ. Acute forms of metabolic acidosis most frequently result from the overproduction of organic acids such as ketoacids or lactic acid; by contrast, chronic metabolic acidosis often reflects bicarbonate wasting and/or impaired renal acidification. The calculation of the serum anion gap, calculated as [Na+] - ([HCO3 -] + [Cl-]), aids diagnosis by classifying the disorders into categories of normal (hyperchloremic) anion gap or elevated anion gap. These categories can overlap, however. Adverse effects of acute metabolic acidosis primarily include decreased cardiac output, arterial dilatation with hypotension, altered oxygen delivery, decreased ATP production, predisposition to arrhythmias, and impairment of the immune response. The main adverse effects of chronic metabolic acidosis are increased muscle degradation and abnormal bone metabolism. Using base to treat acute metabolic acidosis is controversial because of a lack of definitive benefit and because of potential complications. By contrast, the administration of base for the treatment of chronic metabolic acidosis is associated with improved cellular function and few complications.
Introduction
Metabolic acidosis is characterized by a primary reduction in the serum concentration of bicarbonate (HCO3-), a secondary decrease in the arterial partial pressure of carbon dioxide (PaCO2), and a reduction in blood pH. Metabolic acidosis frequently occurs as a part of mixed acid-base disorders, especially among the critically ill. Metabolic acidosis can be acute (lasting minutes to several days) or chronic (lasting weeks to years) in duration. Acute metabolic acidosis is relatively common among seriously ill patients, with one study showing that the disorder affected approximately 64% of patients in a large intensive care unit in the US.[1] Chronic metabolic acidosis is less common; only 1.9% of more than 15,000 individuals surveyed in the NHANES III study[2] had a serum HCO3 -concentration below 22 mmol/l, although this value rose to 19% in patients with an estimated glomerular filtration rate (eGFR) within the range 15-29 ml/min/1.73 m2. Therefore, the frequency of chronic metabolic acidosis might increase with the anticipated rise in chronic kidney disease (CKD) in our aging population. Metabolic acidosis—acute or chronic—can have considerable adverse effects on cellular function and can contribute to increased morbidity and mortality.[1,3-5]
In this Review, we summarize current views on the pathogenesis, diagnosis, adverse effects, and management of metabolic acidosis. Owing to space constraints, we address the causes of this acid-base disorder only briefly.