pernicious anemia
Also found in: Dictionary, Thesaurus, Acronyms, Encyclopedia, Wikipedia.
Related to pernicious anemia: iron deficiency anemia, aplastic anemia
Pernicious Anemia
Definition
Pernicious anemia is a disease in which the red blood cells are abnormally formed, due to an inability to absorb vitamin B12. True pernicious anemia refers specifically to a disorder of atrophied parietal cells leading to absent intrinsic factor, resulting in an inability to absorb B12.
Description
Vitamin B12, or cobalamin, plays an important role in the development of red blood cells. It is found in significant quantities in liver, meats, milk and milk products, and legumes. During the course of the digestion of foods containing B12, the B12 becomes attached to a substance called intrinsic factor. Intrinsic factor is produced by parietal cells that line the stomach. The B12-intrinsic factor complex then enters the intestine, where the vitamin is absorbed into the bloodstream. In fact, B12 can only be absorbed when it is attached to intrinsic factor.
In pernicious anemia, the parietal cells stop producing intrinsic factor. The intestine is then completely unable to absorb B12. So, the vitamin passes out of the body as waste. Although the body has significant amounts of stored B12, this will eventually be used up. At this point, the symptoms of pernicious anemia will develop.
Pernicious anemia is most common among people from northern Europe and among African Americans. It is far less frequently seen among people from southern Europe and Asia. Pernicious anemia occurs in equal numbers in both men and women. Most patients with pernicious anemia are older, usually over 60. Occasionally, a child will have an inherited condition that results in defective intrinsic factor. Pernicious anemia seems to run in families, so that anyone with a relative diagnosed with the disease has a greater likelihood of developing it as well.
Causes and symptoms
Intrinsic factor is produced by specialized cells within the stomach called parietal cells. When these parietal cells shrink in size (atrophy), they produce less and less intrinsic factor. Eventually, the parietal cells stop functioning altogether. Other important products of parietal cells are also lessened, including stomach acid, and an enzyme involved in the digestion of proteins.
People with pernicious anemia seem to have a greater chance of having certain other conditions. These conditions include autoimmune disorders, particularly those affecting the thyroid, parathyroid, and adrenals. It is thought that the immune system, already out of control in these diseases, incorrectly becomes directed against the parietal cells. Ultimately, the parietal cells seem to be destroyed by the actions of the immune system.
As noted, true pernicious anemia refers specifically to a disorder of atrophied parietal cells leading to absent intrinsic factor, resulting in an inability to absorb B12. However, there are other related conditions that result in decreased absorption of B12. These conditions cause the same types of symptoms as true pernicious anemia. Other conditions that interfere with either the production of intrinsic factor, or the body's use of B12, include conditions that require surgical removal of the stomach, or poisonings with corrosive substances which destroy the lining of the stomach. Certain structural defects of the intestinal system can result in an overgrowth of normal bacteria. These bacteria then absorb B12 themselves, for use in their own growth. Intestinal worms (especially one called fish tapeworm) may also use B12, resulting in anemia. Various conditions that affect the first part of the intestine (the ileum), from which B12 is absorbed, can also cause anemia due to B12 deficiency. These ilium-related disorders include tropical sprue, Whipple's disease, Crohn's disease, tuberculosis, and the Zollinger-Ellison syndrome.
Symptoms of pernicious anemia and decreased B12 affect three systems of the body: the system that is involved in the formation of blood cells (hematopoietic system); the gastrointestinal system; and the nervous system.
The hematopoietic system is harmed because B12 is required for the proper formation of red blood cells. Without B12, red blood cell production is greatly reduced. Those red blood cells that are produced are abnormally large and abnormal in shape. Because red blood cells are responsible for carrying oxygen around the body, decreased numbers (termed anemia) result in a number of symptoms, including fatigue, dizziness, ringing in the ears, pale or yellowish skin, fast heart rate, enlarged heart with an abnormal heart sound (murmur) evident on examination, and chest pain.
Symptoms that affect the gastrointestinal system include a sore and brightly red tongue, loss of appetite, weight loss, diarrhea, and abdominal cramping.
The nervous system is severely affected when pernicious anemia goes untreated. Symptoms include numbness, tingling, or burning in the arms, legs, hands, and feet; muscle weakness; difficulty and loss of balance while walking; changes in reflexes; irritability, confusion, and depression.
Diagnosis
Diagnosis of pernicious anemia is suggested when a blood test reveals abnormally large red blood cells. Many of these will also be abnormally shaped. The earliest, least mature forms of red blood cells (reticulocytes) will also be low in number. White blood cells and platelets may also be decreased in number. Measurements of the quantity of B12 circulating in the bloodstream will be low.
Once these determinations are made, it will be important to diagnose the cause of the anemia. True pernicious anemia means that the parietal cells of the stomach are atrophied, resulting in decreased production of intrinsic factor. This diagnosis is made by the Schilling test. In this test, a patient is given radioactive B12 under two different sets of conditions: once alone, and once attached to intrinsic factor. Normally, large amounts of B12 are absorbed through the intestine, then circulate through the blood, and enter the kidneys, where a certain amount of B12 is then passed out in the urine. When a patient has pernicious anemia, the dose of B12 given by itself will not be absorbed by the intestine, so it will not pass into the urine. Therefore, levels of B12 in the urine will be low. When the B12 is given along with intrinsic factor, the intestine is able to absorb the vitamin. Urine levels of B12 will therefore be higher.
Treatment
Treatment of pernicious anemia requires the administration of lifelong injections of B12. Vitamin B12 given by injection enters the bloodstream directly, and does not require intrinsic factor. At first, injections may need to be given several times a week, in order to build up adequate stores of the vitamin. After this, the injections can be given on a monthly basis. Other substances required for blood cell production may also need to be given, iron and vitamin C.
Prognosis
Prognosis is generally good for patients with pernicious anemia. Many of the symptoms improve within just a few days of beginning treatment, although some of the nervous system symptoms may take up to 18 months to improve. Occasionally, when diagnosis and treatment have been delayed for a long time, some of the nervous system symptoms may be permanent.
Because an increased risk of stomach cancer has been noted in patients with pernicious anemia, careful monitoring is necessary, even when all the symptoms of the original disorder have improved.
Resources
Books
Babior, Bernard M., and H. Franklin Bunn. "Megaloblastic Anemias." In Harrison's Principles of Internal Medicine, edited by Anthony S. Fauci, et al. New York: McGraw-Hill, 1997.
Periodicals
Toh, Ban-Hock, et al. "Pernicious Anemia." The New England Journal of Medicine 337, no. 20 (November 13, 1997): 52+.
Key terms
Anemia — A condition in which those elements of the blood responsible for oxygen delivery throughout the body (red blood cells, hemoglobin) are decreased in quantity or defective in some way.
Atrophy — Refers to the shrinking in size of an organ or cell.
Autoimmune disorder — A disorder in which the immune system, (responsible for fighting off such foreign invaders as bacteria and viruses), begins to attack and damage a part of the body as if it were foreign.
Hematopoietic system — The system in the body which is responsible for the production of blood cells.
Intrinsic factor — A substance produced by the parietal cells of the stomach. In order to be absorbed by the intestine, vitamin B12 must form a complex with intrinsic factor.
Parietal cells — Specific cells which line the inside of the stomach. These cells are responsible for producing intrinsic factor and hydrochloric acid.
Reticulocyte — An early, immature form of a red blood cell. Over time, the reticulocyte develops to become a mature, oxygen-carrying red blood cell.
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
anemia
[ah-ne´me-ah]a condition in which there is reduced delivery of oxygen to the tissues; it is not actually a disease but rather a symptom of any of numerous different disorders and other conditions. The World Health Organization has defined anemia as a hemoglobin concentration below 7.5 mmol/L (12 g/dL) in women and below 8.1 mmol/L (13 g/dL) in men.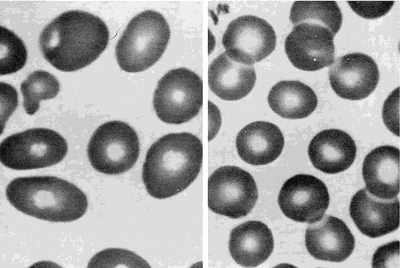
Some types of anemia are named for the factors causing them: poor diet (nutritional anemia), excessive blood loss (hemorrhagic anemia), congenital defects of hemoglobin (hypochromic anemia), exposure to industrial poisons, diseases of the bone marrow (aplastic anemia and hypoplastic anemia), or any other disorder that upsets the balance between blood loss through bleeding or destruction of blood cells and production of blood cells. Anemias can also be classified according to the morphologic characteristics of the erythrocytes, such as size (microcytic, macrocytic, and normocytic anemias) and color or hemoglobin concentration (hypochromic anemia). A type called hypochromic microcytic anemia is characterized by very small erythrocytes that have low hemoglobin concentration and hence poor coloration. Data used to identify anemia types include the erythrocyte indices: (1) mean corpuscular volume (MCV), the average erythrocyte volume; (2) mean corpuscular hemoglobin (MCH), the average amount of hemoglobin per erythrocyte; and (3) mean corpuscular hemoglobin concentration (MCHC), the average concentration of hemoglobin in erythrocytes. adj., adj ane´mic.
Activity intolerance is a common problem for patients with anemia. Physical activity increases demand for oxygen, but if there are not enough circulating erythrocytes to provide sufficient oxygen, patients become physically weak and unable to engage in normal physical activity without experiencing profound fatigue. This can result in some degree of self-care deficit as the fatigue interferes with the patient's ability to carry on regular or enjoyable activities.
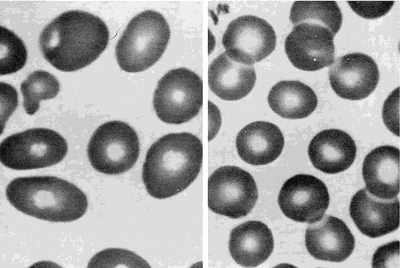
Peripheral blood smears from a patient with megaloblastic anemia (left) and from a normal subject (right), both at the same magnification. The smear from the patient shows variation in the size and shape of erythrocytes and the presence of macro-ovalocytes. From Goldman and Bennett, 2000.
Some types of anemia are named for the factors causing them: poor diet (nutritional anemia), excessive blood loss (hemorrhagic anemia), congenital defects of hemoglobin (hypochromic anemia), exposure to industrial poisons, diseases of the bone marrow (aplastic anemia and hypoplastic anemia), or any other disorder that upsets the balance between blood loss through bleeding or destruction of blood cells and production of blood cells. Anemias can also be classified according to the morphologic characteristics of the erythrocytes, such as size (microcytic, macrocytic, and normocytic anemias) and color or hemoglobin concentration (hypochromic anemia). A type called hypochromic microcytic anemia is characterized by very small erythrocytes that have low hemoglobin concentration and hence poor coloration. Data used to identify anemia types include the erythrocyte indices: (1) mean corpuscular volume (MCV), the average erythrocyte volume; (2) mean corpuscular hemoglobin (MCH), the average amount of hemoglobin per erythrocyte; and (3) mean corpuscular hemoglobin concentration (MCHC), the average concentration of hemoglobin in erythrocytes. adj., adj ane´mic.
Symptoms. Mild degrees of anemia often cause only slight and vague symptoms, perhaps nothing more than easy fatigue or a lack of energy. As the condition progresses, more severe symptoms may be experienced, such as shortness of breath, pounding of the heart, and a rapid pulse; these are caused by the inability of anemic blood to supply the body tissues with enough oxygen. Pallor, particularly in the palms of the hands, the fingernails, and the conjunctiva (the lining of the eyelids), may also indicate anemia. In very advanced cases, swelling of the ankles and other evidence of heart failure may appear.
Common Causes of Anemia. Loss of Blood (Hemorrhagic Anemia): If there is massive bleeding from a wound or other lesion, the body may lose enough blood to cause severe and acute anemia, which is often accompanied by shock. Immediate transfusions are generally required to replace the lost blood. Chronic blood loss, such as excessive menstrual flow, or slow loss of blood from an ulcer or cancer of the gastrointestinal tract, may also lead to anemia. These anemias disappear when the cause has been found and corrected. To help the blood replenish itself, the health care provider may prescribe medicines containing iron, which is necessary to build hemoglobin, and foods with high iron content, such as kidney and navy beans, liver, spinach, and whole wheat bread.
Dietary Deficiencies and Abnormalities of Red Blood Cell Production (Nutritional Anemia, Aplastic Anemia, and Hypoplastic Anemia): Anemia may develop if the diet does not provide enough iron, protein, vitamin B12, and other vitamins and minerals needed in the production of hemoglobin and the formation of erythrocytes. The combination of poor diet and chronic loss of blood makes for particular susceptibility to severe anemia. Anemias associated with folic acid deficiency are very common.
Excessive Destruction of Red Blood Cells (hemolytic anemia): Anemia may also develop related to hemolysis due to trauma, chemical agents or medications (toxic hemolytic anemia), infectious disease, isoimmune hemolytic reactions, autoimmune disorders, and the paroxysmal hemoglobinurias.
Dietary Deficiencies and Abnormalities of Red Blood Cell Production (Nutritional Anemia, Aplastic Anemia, and Hypoplastic Anemia): Anemia may develop if the diet does not provide enough iron, protein, vitamin B12, and other vitamins and minerals needed in the production of hemoglobin and the formation of erythrocytes. The combination of poor diet and chronic loss of blood makes for particular susceptibility to severe anemia. Anemias associated with folic acid deficiency are very common.
Excessive Destruction of Red Blood Cells (hemolytic anemia): Anemia may also develop related to hemolysis due to trauma, chemical agents or medications (toxic hemolytic anemia), infectious disease, isoimmune hemolytic reactions, autoimmune disorders, and the paroxysmal hemoglobinurias.
Patient Care. Assessment of patients with some form of anemia will depend to some extent on the specific type of blood dyscrasia presented. In general, these patients do share some common problems requiring special assessment skills and interventions. Anemia can affect many different body systems
(see table). Although pallor of the skin is a sign of anemia, it is not the most reliable sign; many other factors can affect complexion and skin color. Jaundice of the skin and sclera can occur as a result of hemolysis and the release of bilirubin into the blood stream, where it eventually finds its way into the skin and mucous membranes. (See also jaundice.) Bleeding under the skin and bruises in response to the slightest trauma often are present in anemic and leukemic patients. A bluish tint to the skin (cyanosis) can indicate hypoxia due to inadequate numbers of oxygen-bearing erythrocytes.Activity intolerance is a common problem for patients with anemia. Physical activity increases demand for oxygen, but if there are not enough circulating erythrocytes to provide sufficient oxygen, patients become physically weak and unable to engage in normal physical activity without experiencing profound fatigue. This can result in some degree of self-care deficit as the fatigue interferes with the patient's ability to carry on regular or enjoyable activities.
acute posthemorrhagic anemia hemorrhagic anemia.
aplastic anemia see aplastic anemia.
autoimmune hemolytic anemia (AIHA) an acquired disorder characterized by hemolysis due to the production of autoantibodies against one's own red blood cell antigens.
Blackfan-Diamond anemia congenital hypoplastic anemia (def. 1).
congenital hypoplastic anemia
idiopathic progressive anemia occurring in the first year of life, without leukopenia and thrombocytopenia; it is due to an isolated defect in erythropoiesis and is unresponsive to hematinics, requiring multiple blood transfusions to sustain life. For those responding to steroid therapy the prognosis is good. Called also Blackfan-Diamond anemia or syndrome, Diamond-Blackfan anemia or syndrome, and erythrogenesis imperfecta.
Fanconi's syndrome (def. 1).
Cooley's anemia tthalassemia major.
deficiency anemia nutritional anemia.
Diamond-Blackfan anemia congenital hypoplastic anemia (def. 1).
drug-induced hemolytic anemia (drug-induced immune hemolytic anemia) a form of immune hemolytic anemia induced by the taking of drugs, involving one of four different mechanisms:
Immune complex problems: Ingestion of any of a large number of drugs is followed by immunization and the formation of a soluble drug–anti-drug complex that adsorbs nonspecifically to the erythrocyte surface.
Drug absorption: Drugs bind firmly to erythrocyte membrane proteins, inducing the formation of specific antibodies; the drug most commonly associated with this mechanism is penicillin.
Membrane modification: A nonimmunologic mechanism whereby the drug involved is able to modify erythrocytes so that plasma proteins can bind to the membrane.
Autoantibody formation: Methyldopa (Aldomet) induces the production of autoantibodies that recognize erythrocyte antigens and are serologically indistinguishable from those seen in patients with warm autoimmune hemolytic anemia.
Immune complex problems: Ingestion of any of a large number of drugs is followed by immunization and the formation of a soluble drug–anti-drug complex that adsorbs nonspecifically to the erythrocyte surface.
Drug absorption: Drugs bind firmly to erythrocyte membrane proteins, inducing the formation of specific antibodies; the drug most commonly associated with this mechanism is penicillin.
Membrane modification: A nonimmunologic mechanism whereby the drug involved is able to modify erythrocytes so that plasma proteins can bind to the membrane.
Autoantibody formation: Methyldopa (Aldomet) induces the production of autoantibodies that recognize erythrocyte antigens and are serologically indistinguishable from those seen in patients with warm autoimmune hemolytic anemia.
Fanconi's anemia (Fanconi's hypoplastic anemia) Fanconi's syndrome (def. 1).
hemolytic anemia see hemolytic anemia.
hemorrhagic anemia anemia caused by the sudden and acute loss of blood; called also acute posthemorrhagic anemia.
hypochromic anemia anemia in which the decrease in hemoglobin is proportionately much greater than the decrease in number of erythrocytes.
hypochromic microcytic anemia any anemia with microcytes that are hypochromic (reduced in size and in hemoglobin content); the most common type is iron deficiency anemia.
hypoplastic anemia anemia due to incapacity of blood-forming organs.
immune hemolytic anemia an acquired hemolytic anemia in which a hemolytic response is caused by isoantibodies or autoantibodies produced on exposure to drugs, toxins, or other antigens. See also autoimmune hemolytic anemia, drug-induced immune hemolytic anemia, and erythroblastosis fetalis.
iron deficiency anemia a type of hypochromic microcytic anemia that results from the presence of greater demands on stored iron than can be met, usually because of chronic blood loss, dietary deficiency, or defective absorption; it is characterized by low or absent iron stores, low serum iron concentration, low transferrin saturation, elevated transferrin (total iron-binding capacity), and low hemoglobin concentration or hematocrit. Iron deficiency anemia is the most common nutritional disorder in the United States.
macrocytic anemia anemia characterized by macrocytes (erythrocytes much larger than normal).
Mediterranean anemia thalassemia major.
megaloblastic anemia any of various anemias characterized by the presence of megaloblasts in the bone marrow or blood; the most common type is pernicious anemia.
microangiopathic hemolytic anemia thrombotic thrombocytopenic purpura.
microcytic anemia anemia characterized by microcytes (erythrocytes smaller than normal); see also hypochromic microcytic anemia and microcythemia.
myelopathic anemia (myelophthisic anemia) leukoerythroblastosis.
normochromic anemia that in which the hemoglobin content of the red blood cells is in the normal range.
normocytic anemia anemia characterized by proportionate decrease in hemoglobin, packed red cell volume, and number of erythrocytes per cubic millimeter of blood.
nutritional anemia anemia due to a deficiency of an essential substance in the diet, which may be caused by poor dietary intake or by malabsorption; called also deficiency anemia.
pernicious anemia see pernicious anemia.
sickle cell anemia see sickle cell anemia.
sideroachrestic anemia (sideroblastic anemia) any of a heterogenous group of acquired and hereditary anemias with diverse clinical manifestations, commonly characterized by large numbers of sideroblasts in the bone marrow, ineffective erythropoiesis, variable proportions of hypochromic erythrocytes in the peripheral blood, and usually increased levels of tissue iron.
spur cell anemia anemia in which the erythrocytes are acanthocytes (spur cells) and are destroyed prematurely, primarily in the spleen; it is an acquired form occurring in severe liver disease in which there is increased serum cholesterol and increased uptake of cholesterol into the erythrocyte membrane, causing the abnormal shape.
pernicious
[per-nish´us]tending to a fatal outcome.
pernicious anemia a type of megaloblastic anemia seen most often in older adults, caused by lack of intrinsic factor, which normally is produced by the stomach mucosa. The deficiency results in inadequate and abnormal formation of erythrocytes, leukocytes, and platelets, with failure to absorb vitamin B12. Some patients show only mild symptoms and are not particularly aware of the illness; in others it becomes very serious and if untreated can lead to permanent neurologic impairment and even death. It may be caused by deficient vitamin B12 intake, impaired absorption due to intrinsic factor deficiency or intrinsic intestinal disease or increased requirements and impaired utilization.
Symptoms. A pale, colorless, or lemon-yellow complexion is typical. jaundice also occurs, with soreness and reddening of the tongue, difficulty in swallowing, and digestive disturbances such as diarrhea. Other symptoms may include fatigability, heart palpitation, and dyspnea. Changes in the nerves and spinal cord may produce numbness and tingling in the fingers and toes, and the gait may become unsteady; involvement of the nerves can be avoided if the condition is detected and treated in the early stages. Laboratory tests reveal abnormalities in the erythrocytes in the blood and in the bone marrow. Gastric analysis shows an absence of hydrochloric acid and perhaps even an absence of gastric juice.
Treatment. Pernicious anemia is successfully treated by regular injections of vitamin B12, given several times a week at first and monthly after the condition has been brought under control. This treatment must be lifelong to prevent relapse. The injections do not cure the disease but arrest it by providing the body directly with the necessary vitamin that it fails to absorb from the digestive tract. Special diets, liver extract, and other medications taken by mouth usually are not required since the basic defect is not dietary deficiency but improper use of food ingested. The etiology of pernicious anemia is unknown although there appears to be an autoimmune component, as anti–intrinsic factor antibodies are often found. For patient care, see also anemia.
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
per·ni·cious a·ne·mi·a
[MIM*170900]a chronic progressive anemia of older adults (occurring more frequently during the fifth and later decades, rarely before 30 years of age), due to failure of absorption of vitamin B12, usually resulting from a defect of the stomach accompanied by mucosal atrophy and associated with lack of secretion of "intrinsic" factor; characterized by numbness and tingling, weakness, and a sore smooth tongue, as well as dyspnea after slight exertion, faintness, pallor of the skin and mucous membranes, anorexia, diarrhea, loss of weight, and fever; laboratory studies usually reveal greatly decreased red blood cell counts, low levels of hemoglobin, numerous characteristically oval macrocytic erythrocytes (Colour Index greater than normal, but not truly hyperchromic), and hypochlorhydria or achlorhydria, in association with a predominant number of megaloblasts and relatively few normoblasts in the bone marrow; the leukocyte count in peripheral blood may be less than normal, with relative lymphocytosis and hypersegmented neutrophils; a low level of vitamin B12 is found in peripheral red blood cells; administration of vitamin B12 results in a characteristic reticulocyte response, relief from symptoms, and an increase in erythrocytes, provided that pernicious anemia is not complicated by another disease; the condition is not actually "pernicious," as it was before availability of therapy with vitamin B12. At least two autosomal recessive forms are known. In one there is a defect of intrinsic factor [MIM*26100] and in the other a defective absorption of vitamin B12 from the intestine [MIM*261100].
Synonym(s): Addison anemia, Addison-Biermer disease, addisonian anemia, Biermer anemia, Biermer disease
Farlex Partner Medical Dictionary © Farlex 2012
pernicious anemia
n.
A severe anemia most often affecting older adults, caused by failure of the stomach to absorb vitamin B12 and marked by a decrease in number and an increase in the size of red blood cells, by gastrointestinal disturbances, and by lesions of the spinal cord.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
pernicious anemia
Addison's anemia, megaloblastic anemia Hematology Anemia caused by ↓ vitamin B12, due to a lack of intrinsic factor which facilitates vitamin B12 absorption Clinical Glossitis, neurologic signs, achlorhydria, gastric atrophy Lab Antibodies against intrinsic factor, parietal cells. See Anemia.McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
per·ni·cious a·ne·mi·a
(pĕr-nish'ŭs ă-nē'mē-ă)A chronic progressive anemia of older adults due to failure of absorption of vitamin B12, usually resulting from a defect of the stomach accompanied by mucosal atrophy and associated with lack of secretion of "intrinsic" factor; characterized by numbness and tingling, weakness, and a sore, smooth tongue, as well as dyspnea after slight exertion, faintness, pallor of the skin and mucous membranes, anorexia, diarrhea, loss of weight, and fever; laboratory studies usually reveal greatly decreased red blood cell counts, low levels of hemoglobin, numerous characteristically oval macrocytic erythrocytes, and hypochlorhydria or achlorhydria, in association with a predominant number of megaloblasts and relatively few normoblasts in the bone marrow; the leukocyte count in peripheral blood may be less than normal, with relative lymphocytosis and hypersegmented neutrophils; a low level of vitamin B12 is found in peripheral erythrocytes; administration of vitamin B12 results in a characteristic reticulocyte response, relief from symptoms, and an increase in erythrocytes, provided that pernicious anemia is not complicated by another disease.
See also: diphyllobothriasis
Synonym(s): Addison anemia, malignant anemia.
See also: diphyllobothriasis
Synonym(s): Addison anemia, malignant anemia.
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
Addison,
Thomas, English physician, 1793-1860.Addison anemia - a chronic, progressive anemia of older adults due to failure of absorption of vitamin B12. Synonym(s): Addison-Biermer disease; addisonian anemia; Biermer anemia; Biermer disease; pernicious anemia
Addison-Biermer disease - Synonym(s): Addison anemia
Addison disease - Synonym(s): chronic adrenocortical insufficiency
addisonian anemia - Synonym(s): Addison anemia
addisonian crisis - Synonym(s): acute adrenocortical insufficiency
Addison-Schilder disease - Synonym(s): Schilder disease
Medical Eponyms © Farlex 2012
per·ni·cious a·ne·mi·a
(pĕr-nish'ŭs ă-nē'mē-ă) [MIM*170900]Chronic progressive anemia of older adults (occurring more frequently during the fifth and later decades, rarely before 30 years of age), due to failure of absorption of vitamin B12, usually resulting from a defect of the stomach accompanied by mucosal atrophy and associated with lack of secretion of "intrinsic" factor.
Synonym(s): Addison anemia, Addison-Biermer dis ease, addisonian anemia.
Synonym(s): Addison anemia, Addison-Biermer dis ease, addisonian anemia.
Medical Dictionary for the Dental Professions © Farlex 2012