Liver disease toolkit
| Site: | Royal College of General Practitioners - Online Learning Environment |
| Course: | Clinical toolkits |
| Book: | Liver disease toolkit |
| Printed by: | Guest User |
| Date: | Wednesday, 24 April 2024, 12:24 PM |
Description
The aims of the BLT/RCGP Liver Priority Project are to raise awareness of liver disease as an increasingly important cause of morbidity and mortality in the UK and to provide resources to support its optimal management in primary care.
Table of contents
- Introduction
- Resources for practitioners (General)
- Resources for practitioners (National guidance)
- Resources for practitioners (Audit and reflection)
- Recommendations for commissioning bodies to improve the early detection of chronic liver disease in UK primary care
- 1) The rationale for change, the burden of chronic liver disease and finding out your local population needs
- 2) Review the data, assess your local population needs and scope what needs to be done in your area
- 3) Develop an agreed local pathway for assessing the risk of liver disease, finding patients at risk, testing, following up and referring to secondary care
- 4) Exemplar pathways to adapt for your local needs
- 5) Links to NICE and British Society of Gastroenterology guidelines and other resources
- Resources for practitioners (Links to training resources)
- Organisations to support you and your patients
- Liver disease information for patients and carers
- Innovation and best practice in primary care
- Resources for practices and practice nurses
- Resources for commissioners
Introduction
Liver disease is one of the five most common causes of premature death in the UK and is the only major cause of death that has a year by year increasing incidence. However, more than 90% of liver disease is preventable. The three major causes of liver disease in adults are alcohol-related liver disease, obesity and metabolic syndrome leading to non-alcohol-related liver disease, and viral hepatitis.
The aims of the British Liver Trust/RCGP Liver Clinical Priority Project are to raise awareness of liver disease as an increasingly important cause of morbidity and mortality in the UK and to provide resources to support its optimal management in primary care.
Upcoming Liver Disease Events : Improving the Detection and Management of Liver Disease in Primary Care
When you've used one of the resources, use the reflection template for your appraisal portfolio.
- Personal learning reflection template [75 KB, DOC]
Give your feedback and suggestions
This toolkit has been developed in partnership between the RCGP and the British Liver Trust.
Please send any feedback or suggestions to clinicalquality@rcgp.org.uk
Alcohol and Liver disease
On this page you will find useful links to guide consultations around alcohol use and risk of liver disease. This includes links to latest NICE and British Society of Gastroenterology (BSG) guidelines, tools to assess level of alcohol use and information sheets for your patients.
Cirrhosis develops progressively as a result of damage to the liver (which can be due to a number of causes), usually over a number of years.
- Summary on diagnosing and assessing problem alcohol use. Problem drinking is defined as regular consumption of alcohol above recommended levels.
- How to manage abnormal liver blood tests
- Alcohol use screening tests - GOV.UK. The alcohol use screening tests can be used by health professionals as a tool to assess a service users level of risk to alcohol harm.
A lot of people see alcohol as simply something to be enjoyed and as a normal part of life in the UK. Other than a few unwelcome side effects, such as a hangover or putting on a bit of weight, many of us are unaware about the unseen damage alcohol can do to the body.
NAFLD and liver disease
On this page you will find useful links to guide consultations with patients who are at risk of non-alcoholic fatty liver disease (NAFLD). This includes latest NICE and British Society of Gastroenterology (BSG) guidelines, tools to assess risk of liver fibrosis and information sheets for your patients.
- Summary on diagnosing and managing NAFLD. Covers the management of people with suspected or confirmed non-alcoholic fatty liver disease in primary care, and when to refer.
- How to manage abnormal liver blood tests. These guidelines on the management of abnormal liver blood tests have been commissioned by the Clinical Services and Standards Committee (CSSC) of the British Society of Gastroenterology (BSG) under the auspices of the liver section of the BSG.
- What is Non-Alcohol Related Fatty Liver Disease (NAFLD)? NHS.
- New NICE Guidelines on Cirrhosis and Non-Alcohol Related Fatty Liver Disease (NAFLD), British Liver Trust.
This is the name given to a condition in which you have too much fat in your liver. There should be little or no fat in a healthy liver and for most people, carrying a small amount of fat in the liver causes no major problems.
Hepatitis C and liver disease
On this page you will find useful links to guide consultations with patients who are at risk of Hepatitis C. This includes latest guidelines, information from Public Health England (PHE) around new treatments and elimination targets and information sheets for your patients.
Information for your patientsResources for practitioners (General)
This section contains articles and resources for primary care practitioners on liver disease, its impact, its risk factors and prevention, its early diagnosis and its management.
- Liver disease in the UK, an overview [237 KB, PDF]
- Cirrhosis and its management in primary care [157 KB, PDF]
- Non-alcohol-related fatty liver disease and its management [136 KB, PDF]
- Alcohol-related liver disease and its management [283 KB, PDF]
- Hepatitis B infection [269 KB, PDF]
- Hepatitis C infection [172 KB, PDF]
- Eliminating Hepatitis C as a major public health threat - the challenges ahead
- NHS England strikes world leading deal to help eliminate hepatitis C, 30 April 2019, NHS
- Hepatitis C: patient re-engagement exercise, NHS England and Public Health England, 13 November 2020
- Prolonged neonatal jaundice and its management, October 2016 [124 KB, PDF]
- LFT blood testing and investigations in liver disease (summarising the British Society of Gastroenterology guidelines 2021) [522 KB, PDF]
Resources for practitioners (National guidance)
This section provides links to national guidance and resources focusing on the management of liver disease
- NICE NG49 non-alcoholic fatty liver disease guidance (2016)
- NICE NG50 cirrhosis in over 16s guidance (2016)
- Guidelines on the management of abnormal liver blood tests, British Society of Gastroenterology
- NICE PH43 hepatitis B and C testing guidance (2013)
- NICE CG165 hepatitis B (chronic): diagnosis and management (2017)
- Management of hepatitis C, Healthcare Improvement Scotland, Scottish Intercollegiate Guidelines Network (SIGN).
- Management of obesity, Healthcare Improvement Scotland, Scottish Intercollegiate Guidelines Network (SIGN).
- NICE CG189: obesity guidance (2014)
- NICE CG115: Alcohol-use disorders: diagnosis, assessment and management of harmful drinking and alcohol dependence (2011)
- The Liver Disease Delivery Plan for Wales (2015-2020).
- Lancet Commission: Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis (2014)
- Lancet Commission: Implementation of the Lancet Standing Commission on Liver Disease in the UK (2015)
- Lancet Commission: New metrics for the Lancet Standing Commission on Liver Disease in the UK (2018)
- Caring for people with liver disease: a competency framework for nursing, Royal College of Nursing
- WHO Hepatitis C fact sheet
- WHO Hepatitis B fact sheet
- Shooting Up: Infections among people who inject drugs in the UK
- Public Health England guidance and resources for GPs and patients: towards Hepatitis C elimination - patient re-engagement exercise
Resources for practitioners (Audit and reflection)
Review your practice - Ideas for audit and reflection?
These links contain ideas and suggestions to help you reflect on your clinical practice relating to liver disease. Are you equipped to identify patients with risk factors for liver disease and to help them reduce their risk? Are you equipped to identify and manage early liver disease?
- Practice checklist are all the right things in place for you to prevent and manage liver disease [84 KB, DOC]
- Clinical audit ideas: identification and management of NAFLD [75 KB, DOC]
- Clinical audit ideas: identifying and managing cirrhosis in primary care [75 KB, DOC]
- Clinical audit ideas: reducing the risk of liver disease in those with high alcohol consumption [76 KB, DOC]
- Clinical audit ideas: managing hepatitis C in primary care [78 KB, DOC]
- Clinical audit ideas: managing hepatitis B in primary care [80 KB, DOC]
- Personal reflections: managing neonatal jaundice [78 KB, DOC]
Recommendations for commissioning bodies to improve the early detection of chronic liver disease in UK primary care
Mortality from liver disease is increasing in the UK. It is a leading cause of death in working age, yet 90% is preventable. Three quarters of people are currently diagnosed at a late stage when it is often too late for effective interventions or treatment. The same level of attention that has previously been given to the prevention of cardiovascular disease and cancer now needs to be directed at the other major causes of years of life lost (YLLs), such as liver disease.
The Royal College of General Practitioners and British Liver Trust have worked with stakeholders to create recommendations and a set of resources to support primary care commissioning bodies in the UK to plan and commission effective liver services for adults, adapted to local needs and circumstances. These recommendations have been developed from the latest NICE and British Society of Gastroenterology guidelines.
The resources are divided into the following sections:
1. The rationale for change, the burden of chronic liver disease and finding out your local population needs
2. Review the data, assess your local population needs and scope what needs to be done in your area
3. Develop an agreed local pathway for assessing the risk of liver disease, finding patients at risk, testing, following up and referring to secondary care
4. Exemplar pathways to adapt for your local needs
5. Links to NICE and British Society of Gastroenterology guidelines and other resources
These recommendations were developed by a stakeholder group led by the Royal College of General Practitioners and the British Liver Trust liver disease priority programme. Stakeholders invited included GPs, commissioners, public health professionals, hepatologists, third sector representatives and representatives from the devolved nations. These recommendations have been reviewed and endorsed by the Lancet Liver commission, British Association for the Study of the Liver (BASL) and the British Society of Gastroenterology (BSG).
1) The rationale for change, the burden of chronic liver disease and finding out your local population needs
These recommendations will improve early detection and better initial management of chronic liver disease in primary care. This will lead to:
- More appropriate referrals to secondary/tertiary care
- Fewer admissions with decompensated liver cirrhosis
- Less repeat blood testing without decision making
- Long term improvement in morbidity and mortality for people with chronic liver disease
- Significant cost savings for the NHS
Three quarters of patients currently present too late. With education of GPs and access to easier testing we can change this trend.
2) Review the data, assess your local population needs and scope what needs to be done in your area
Public Health England’s Atlas of Variation in risk factors and healthcare for liver disease demonstrates geographical variation in healthcare provision, access and outcomes which cannot be explained by the underlying prevalence of risk factors or liver disease. The data can be used by commissioning groups to identify the need for action.
In addition, liver disease profiles for all regions of England are available here.
There is public health information for Scotland relating to: Chronic liver disease; Liver disease mortality; Chronic liver disease morbidity.
Public Health Wales have information on the prevalence of a range of liver diseases in Wales.
The data in these resources will enable commissioners to understand the local population and its associated needs in relation to liver disease and compare themselves with the national picture. This is the starting point for commissioning appropriate services and reducing the burden of liver disease.
3) Develop an agreed local pathway for assessing the risk of liver disease, finding patients at risk, testing, following up and referring to secondary care
Look at whether there is an existing pathway that GPs are aware of and using in your area. Assess whether this meets the steps below. in different regions of the country, it is important that any pathway is agreed with secondary care, particularly around agreed methods of fibrosis testing and referral criteria. Examples of pathways working in parts of the UK are given below. They can be adapted according to your local needs and resources and all groups are happy to be contacted to discuss their pathways in more detail.
It is very important that the agreed pathway does not rely solely on liver blood tests or LFTs(liver enzymes) but adequately assesses liver fibrosis. The exemplar pathways showcase potential approaches for doing this.
The locally agreed pathway should include the following:
(i) Assessing the risk of liver disease for individuals – how to find patients at risk
The main drivers of chronic liver disease in the UK are alcohol and the combined effects of obesity and type 2 diabetes. We recommend that services are commissioned so that liver disease is considered regularly in people with these risk factors as well as those with risk factors for viral hepatitis.
Alcohol related liver disease:
Recommendation 1: Assess and code alcohol risk (both dependence and non-dependent excessive drinking) using NICE/BSG guidelines and recognised tools
- At new patient registration
- During annual hypertension reviews
- As part of any NHS/other routine ‘health check’
- Opportunistically during consultations
- Aim for all registered adults to have their alcohol risk assessed at least every 5 years
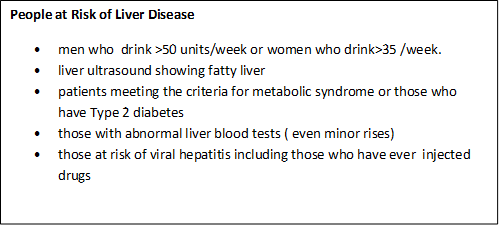
Those at risk of alcohol related liver disease are defined by NICE as men who regularly drink over 50 units of alcohol or women who drink over 35 units of alcohol weekly.
Rationale for recommendation: Information on drinking behaviour is unlikely to be volunteered or coded unless people are routinely and regularly asked about their alcohol consumption. Alcohol-related liver disease contributes the biggest morbidity and mortality burden of all liver disease.
Non-alcohol related fatty liver disease:
Recommendation 2: Assess metabolic risk (obesity, Type 2 diabetes, other metabolic risk factors) leading to non-alcohol related fatty liver disease (NAFLD)
- Keep a register of all patients coded as having NAFLD
- Assess for NAFLD every 3-5 years in all registered patients with Type 2 diabetes (set up recall as for other chronic disease management)
- Code people with a liver ultrasound showing fatty liver
- Consider keeping a register of all patients meeting criteria for the metabolic syndrome and assessing for NAFLD in these patients as for people with Type 2 diabetes
Rationale for recommendation: Most patients at risk of NAFLD are likely to be under review for other reasons due to common metabolic and cardiovascular risk profiles. Only minor systems changes are needed to ensure liver disease is also routinely considered and coded in these patients.
Recommendation 3: Investigate incidental abnormal liver enzyme blood tests (LFTs)
These individuals are at risk of liver disease and should be investigated regardless of level of abnormality (use BSG guidelines to triage these patients and identify those at risk of common chronic liver disease as well as ruling out and referring on for rarer causes)
Rationale for recommendation: Patients with even minor abnormalities in their liver enzymes can have significant liver disease and a diagnosis should be sought /ruled out in all cases rather than re-testing/not acting on results. This is a cost effective approach and nationally recommended.
Viral Hepatitis:
Recommendation 4: Offer tests to those who inject drugs or have other risk factors for viral hepatitis
- People who inject drugs (PWID) should be offered testing for Hepatitis C routinely. 90% of HCV is acquired through injecting drugs
- Follow NICE guidelines to ensure testing for Hepatitis B and C is being carried out in high risk patients
- All patients testing positive for Hepatitis B and C should be offered referral to consider treatment options
Rationale for recommendation: Untreated hepatitis C infection causes cirrhosis and liver cancer. Very effective, well tolerated oral therapies are now available on the NHS. There are national and international targets to eliminate Hepatitis C within the next 15 years. There are also effective treatments to control Hepatitis B.
Recommendation 5: Diagnostic testing in patients at risk of chronic liver disease (Alcohol related and NAFLD) should focus on diagnosing/ruling out liver fibrosis
- Assessing fibrosis can be done using blood-based algorithms, serum fibrosis markers, transient elastography (fibroscan) or these methods in combination. The choice of tests depends on local availability.
- Do not use a set of normal routine liver enzymes (LFTs or liver blood tests) to rule out fibrosis in those identified as individuals at risk (including those with alcohol risk, NAFLD risk or viral hepatitis risk)
- Fibrosis assessment should run in parallel with brief interventions/lifestyle advice
- All patients where an initial liver screen, based on risk factors, has identified a cause other than alcohol or NAFLD should be referred to gastroenterology/hepatology
Rationale for recommendation: Liver fibrosis is the best predictor of progression to cirrhosis and poor clinical outcomes in patients with chronic liver disease. There are now several methods of assessing for fibrosis in the community. There is a lack of consensus around which is the best initial test of fibrosis to use, but it is important that ONE of the assessment methods is employed consistently according to local resources. All patients with liver disease aetiology other than alcohol or NAFLD require further investigation and management, which is not currently available in the community for most.
- Direct to fibroscan if available
- If not available then direct to ELF testing
- If neither available then referral to gastroenterology/hepatology
- Direct to ELF test if available (see NICE guidance)
- Or serum based algorithm test (Fib 4, NAFLD fibrosis score, AST:ALT ratio) followed by fibroscan if available
- If neither ELF or direct access fibroscan are available to request from primary care then referral on the basis of an indeterminate Fib 4, NAFLD fibrosis score or high AST:ALT ratio to gastroenterology/hepatology
Rationale for recommendation: There is a lack of consensus around which is the best initial test of fibrosis to use, but it is important that ONE of the assessment methods is employed consistently according to local resources. See example pathways later in this document.
Recommendation 7: Develop robust systems for follow up
- Individuals identified as being at low risk of liver fibrosis should be coded and re-assessed for fibrosis in the community using routine recall facilities every 3-5 years
- It is essential that follow up should include targeted brief interventions and lifestyle advice which should be coded and repeated if risk factors remain
- Alcohol support services and weight loss services should be used as available and considered to be commissioned or expanded to meet demand
- High risk individuals* should be referred for specialist follow up. Local referral pathways should be determined by local resource availability and capacity, in discussion with primary care, secondary care and commissioners.
Rationale for recommendation: If risk factors remain, patients at low risk of fibrosis may become high risk over time and it is crucial that these people are coded and followed up. To reduce this risk, brief interventions (both alcohol and weight loss) have been shown to be clinically and cost effective
*Note : There is some dispute around which ELF values and fibroscan scores should warrant referral/ cirrhosis assessment - commissioners should review the evidence and make locally agreed decisions in conjunction with the clinicians who will be receiving referrals
Recommendation 8: Audit any new pathway introduced to drive quality improvement making use of RCGP QI resources
Quality Improvement (QI) is an evidence-based approach that helps primary care free up time to deliver and evaluate initiatives, and embed new approaches more effectively and efficiently into practice. QI helps us to make the most of our systems, organisations, talents and expertise to deliver better outcomes for patients. Read more.
QI Ready is a free resource for all practices and has been developed to support GPs and practice teams with QI activities in practices. It is the starting place for all QI tools, guidance and case studies. Read more about the this RCGP programme here.
4) Exemplar pathways to adapt for your local needs
The Scarred Liver Project, Greater Nottingham
The Scarred Liver Project is risk factor focussed and uses Fibroscan to stratify patients at risk of liver disease. Developed out of pilot project in 2014 a fully integrated CCG commissioned pathway is now in place across Greater Nottingham.
The scarred liver project has implemented an integrated pathway within the community to identify patients with risk factors for liver disease. GPs opportunistically identifying patients with risk factors for alcohol related liver disease, NAFLD or with unexplained abnormal liver enzymes are able to refer directly to liver fibrosis assessment using Fibroscan. All patients who attend for a Fibroscan® receive brief lifestyle intervention about their liver health. Patients stratified to have significant liver disease or cirrhosis are referred to a hepatologist for further review.
The pathway has been demonstrated to be cost effective (ICER per QALY £2138 for NAFLD and £6537 for ALD) and has seen over 3000 patients in its first 18months since full implementation in September 2016
Full details of the pathway, its evaluation, associated publications and contact details for the clinicians involved are available on the website.
The Gwent AST project
All blood tests sent from primary care where ALT is raised have a ‘reflex’ AST measured in the laboratory. If the AST:ALT ratio is >1 and no other diagnosed reason, advice to refer directly for transient elastography (fibroscan).All fibroscan >15 Kpa (likely cirrhosis) referred to hepatologist
Results so far (19 months of pathway in action):
- 13 % of abnormal ALT results revealed an AST:ALT ratio over 1 (1826 from 13929 ALTs requested in Gwent area)
- 648 were referred for fibroscan (some had other clear cause requiring alternative action, others not referred ?reason)
- 271 have had a fibroscan to date. 120 Fibroscan <8kPa = 44% (low risk of significant liver fibrosis; 73 Fibroscan 8-15 kPa = 27% (possible fibrosis/early cirrhosis); 76 Fibroscan >15 kPa = 28% (probably cirrhosis or advanced fibrosis)
Take home message: up to 30% of patients investigated along this pathway had likely cirrhosis of the liver. Simple pathway requiring minimal additional tests/GP time which picks up significant numbers of previously undiagnosed cirrhosis of the liver
For more information about this project please contact Dr. Andrew Yeoman, clinical lead for Welsh Liver Plan: andrew.yeoman@wales.nhs.uk
A Scottish Government supported, research funded, development of an automated investigation algorithm which maximises diagnosis and management.
1. GP requests LFTs via electronic system, entering data about patients’ alcohol consumption, BMI and features of metabolic syndrome.
2. In the laboratory, the finding of abnormal LFT results triggers an automated cascade of additional tests on the same sample to find an cause (viral serology, liver immunology, iron studies, alpha 1 anti-trypsin, and caeruloplasmin) and stage fibrosis (Fib 4 and NAFLD fibrosis score) This information automatically populates diagnostic algorithms and management plans.
3. The report is made available to the GP in real time for them to action. Access to the management plans is delivered electronically as web hyperlinks.
Results: In a trial of iLFT, the diagnosis rate was increased by 43% and it was cost-effective, with a saving to the NHS of £3,216 over a patient lifetime. It is now being rolled out in other sites across Scotland.
For more information about this project please contact Professor John Dillon, lead clinician on iLFT project at j.f.dillon@Dundee.ac.uk
Southampton
St Marys (a large, inner city practice) worked in partnership with secondary care to develop a pathway for the management of patients at risk of liver disease/ with abnormal LFTS. This was integrated in to the clinical system and liver health was promoted to patients through work with the British Liver trust (2016). The pathway was shared city wide in December 2017 and led to the commissioning of direct access fibroscan in October 2018.
Outcomes:
Within St Marys surgery population steep rise in coded / diagnosed liver disease:
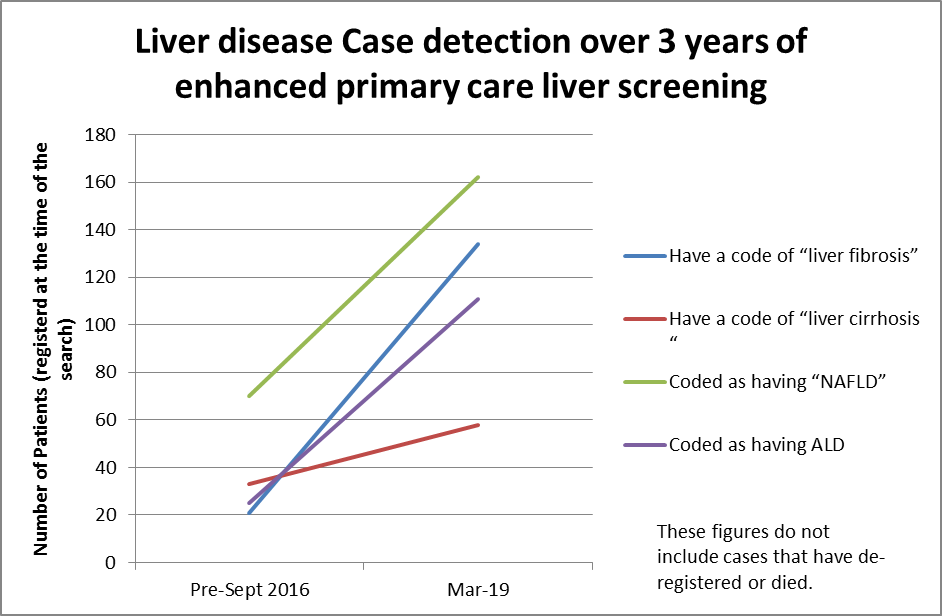
City wide data will be available shortly.
For more information about this project please contact Dr Mead Mathews, lead clinician and RCGP/British Liver Trust Liver Disease Clinical Priority Clinical Fellow, on meadmathews@nhs.net
5) Links to NICE and British Society of Gastroenterology guidelines and other resources
British Society of Gastroenterology guidelines on the management of abnormal liver blood tests. These guidelines deal specifically with the management of abnormal liver blood tests in children and adults in both primary and secondary care and cover what constitutes an abnormal liver blood test; what constitutes a standard liver blood test panel; Further investigation and response.
NICE Quality standard for the management of liver disease. This quality standard covers identifying, assessing and managing chronic liver disease in children, young people and adults, and cirrhosis in young people and adults. It describes high-quality care in priority areas for improvement.
NICE NAFLD guideline. This guideline covers how to identify the adults, young people and children with non-alcoholic fatty liver disease (NAFLD) who have advanced liver fibrosis and are most at risk of further complications. It outlines the lifestyle changes and pharmacological treatments that can manage NAFLD and advanced liver fibrosis.
NICE cirrhosis guideline. This guideline covers assessing and managing suspected or confirmed cirrhosis in people who are 16 years or older.
Hep C elimination material for GPs. The World Health Organisation aims to eliminate hepatits C by 2030. Public Health England has produced information for GPs about the NHS England and Public Health England initiative to support finding undiagnosed patients and ensuring they are treated.
Resources for practitioners (Links to training resources)
- RCGP Hepatitis B and C eLearning course. This course helps understand the epidemiology of hepatitis B and C and how to assess the risk of both conditions for a patient. It informs treatment options for hepatitis C, and their success rates. After completing the course the learner will be ale to confidently refer or re-referred patients with hepatitis B and C, to secondary care in view of changes in treatment options.
- British Association for the Study of the Liver. Access information regarding BASL organised events, BASL endorsed events and other educational events related to hepatology.
- Primary Care Society for gastroenterology courses and conferences. The PCGS holds major educational events throughout the year, giving those involved in Primary Care a chance to hear from leading experts in gastroenterology and associated fields.
- RCGP Courses and conferences. The RCGP runs extensive resources of conferences, courses, events and e-learning modules, many of which are relevant to the management of liver disease.
- RCGP Very Brief Advice training. This e-learning module is aimed at healthcare professionals who would like to promote behaviour change in their patients to reduce their cancer risk, though is applicable to patients with risks in other areas. The module highlights the links between cancer and smoking, obesity and alcohol and supports leaning in delivery of very brief advice to promote behaviour change.
The British Liver Trust website has a section for healthcare professionals and researchers. There is information about:
- The Love Your Liver campaign briefing
- Liver-related clinical research
- A comprehensive range of published leaflets and factsheets on liver diseases to download and read or order.
All British Liver Trust information is written by, or rigorously assessed and reviewed by, medical specialists or other health care professionals and will be of value both to patients and practitioners. Many of these information documents are available in languages other than English.
The website has a range of other valuable information including how patients can access the British Liver Trust support line and information on patient support groups.
Organisations to support you and your patients
This section provides links to a range of organisations that work to prevent liver disease, to support those with liver disease, or provide resources and guidance to practitioners working with patients with liver disease.
British Liver Trust. The British Liver Trust is the leading UK liver disease charity, providing information and support for professionals, patients and carers; promoting prevention and early diagnosis of liver disease; funding and championing research; and campaigning for better services. In addition the Trust has an anonymous love your liver health screener that assesses the risks posed by alcohol, obesity and viral hepatitis and provides a print out of what you need to do and if need be what to discuss with your GP.
Children's Liver Disease Foundation. The CLDF is a UK-wide charity that provides support, information research funds and a voice for all those affected by childhood liver disease.
Yellow Alert. Yellow alert is CLDF's prolonged jaundice in newborn babies awareness campaign. Yellow Alert promotes the early diagnosis and appropriate referral for liver disease in newly born infants.
Drinkline. Drinkline provides a national helpline to offer help and signposting for callers worried about their drinking, support for the family and friends of people who are drinking and links to information and self-help materials.
Alcohol Health Alliance. The Alcohol Health Alliance brings together more than 40 organisations that have a shared interest in reducing the damage caused to health by alcohol. Members include medical royal colleges, charities, patient representatives and alcohol health campaigners. Its aims are to highlight the rising levels of alcohol-related harm; propose evidence-based solutions to address the harms; and encourage decision makers to take positive action.
Obesity Health Alliance. The Obesity Health Alliance is a coalition of over 30 organisations who have joined together to fight obesity. Members include medical royal colleges, charities, campaigners and professional associations. The alliance works together to influence Government policy on overweight and obesity.
Hepatitis C Trust. The Hepatitis C Trust is a national UK charity supporting those with hepatitis C infection. It is a patient-led and patient-run organisation and most of its board, staff, and volunteers either have hepatitis C or have had it and have cleared it after treatment.
Hepatitis B positive. This organisation provides information for the public on hepatitis B infection.
Hepatitis Scotland. Hepatitis Scotland provides training for non-statutory organisations, information and support for patient involvement for those with hepatitis B or C infection in Scotland, and resources for health professionals.
British Association for the Study of the Liver. BASL is a multidisciplinary association with 850 members from medical, nursing and research backgrounds. It aims to advance knowledge about liver biology and pathology; disseminate research findings and promote clinical care of liver disease.
British Society of Gastroenterology. The British Society of Gastroenterology promotes the practice and study of gastroenterology within the United Kingdom. It has over three thousand members including physicians, surgeons, pathologists, radiologists, scientists, nurses, dietitians, and others interested in the field. Internationally it is represented at World and European level.
PSC Support is the leading UK-based organisation for anyone affected by Primary Sclerosing Cholangitis (PSC). They offer advice for patients, family members, healthcare providers and researchers. The Primary Sclerosing Cholangitis Online Support Group is a group consisting of people with PSG and provides mutual support
Primary Care Society for Gastroenterology. The PCSG supports the practice of gastroenterology within primary care through providing guidelines, supporting research and educational events. Membership is free.
The RCGP is the professional membership body for family doctors in the UK and overseas. It is committed to improving patient care, clinical standards and GP training and offers resources for GPs in practice including CPD targeted towards liver disease.
Liver disease information for patients and carers
If you have a liver problem yourself, or you are a health professional and one of your patients is worried about developing liver disease, has had an abnormal liver function test, has been diagnosed or is caring for a loved one with a liver condition or has questions about liver cancer, you will need access to jargon-free, patient-friendly, reliable information that has been checked by experts.
This section of the toolkit provides signposts to these resources. Much of the information is detailed and will useful for health care professionals as well as patients.
Fact sheets for patients
Alcohol-related liver disease [134 KB, PDF]
Non-alcohol related fatty liver disease [139 KB, PDF]
General Information
The British Liver Trust has a free patient helpline run by nurses with liver disease expertise.
Helpline: 0800 652 7330 (10am to 3pm Monday to Friday)
Liver Cancer Information
- British Liver Trust on liver cancer
- Liver Cancer leaflet free download
- Cancer Research UK Liver cancer
- Macmillan Cancer Support Liver cancer
Hepatitis C Trust
The Hepatitis C Trust produces a range of materials and run a helpline on 0845 223 4424 or 020 7089 6221 (10.30am to 4.30pm Monday to Friday). Alternatively, you can email helpline@hepctrust.org.uk
Patient leaflets on different liver conditions
The British Liver Trust has a full range of leaflets on the whole range of liver diseases that can be downloaded for free. The full range of leaflets can be downloaded from the BLT website or your patient can order a free hard copy by calling 01425 481320. The most popular leaflets include:
- Hepatitis C: guidance, data and analysis, Public Health England
- Living with Liver disease
- Diet and Liver disease
- Alcohol and liver disease
- Non-alcohol related liver disease
- Different types of liver disease
Liver disease often has no symptoms in the early stages. The British Liver Trust has developed a range of materials covering the risk factors for liver disease and the signs and symptoms of liver disease. They are free to order and include posters and leaflets for display in GP surgeries.
Children's Liver diseases
The Children's Liver Disease Foundation has a range of support information and offers support on the different types of liver disease affecting children.
There are also local support groups and support groups for rarer types of liver disease.
Innovation and best practice in primary care
Many local teams have led innovative and exciting developments in the prevention and management of liver disease in their areas across the UK, some of these are listed below.
If you've been involved in innovative or best practice in the management of liver disease and you would like to share details of your project, please complete the pro forma and email it to clinicalquality@rcgp.org.uk
- GP-based best practice pro forma [409 KB, DOC]
- Non-GP best practice pro forma [412 KB, DOC]
The Bolton Alcohol Project
Teams in Bolton have developed integrated and collaborative changes that led to:
- the creation of a consultant-led hospital based alcohol care team that has improved the care and reduced admissions for alcohol-related conditions
- a primary care project that has been highly successful in identifying alcohol problems through screening with the AUDIT-C test and signposting patients to early interventions
Liver health screening in Middlesbrough
Middlesbrough has developed a 'Live Well Centre'. The centre is a one-stop shop to support people in changing their lives for the better across a full spectrum of life issues. The project is specifically building in the identification of risk factors for liver disease together with signposting to further interventions as part of an opportunistic screening programme.
End of life care for patients with advanced liver disease
St Luke's Hospice, Basildon, has worked collaboratively with local secondary care hepatology services to create a Shared Care Liver Project designed to meet the unmet needs of patients with advanced liver disease and to improve end of life care.
The Scarred Liver Project Nottingham
The Scarred Liver Project has developed an effective community-based diagnostic pathway for identifying liver disease which stratifies patients using validated non-invasive tests. GPs can refer patients with a defined risk factor for chronic liver disease directly for transient elastography (FibroScan) before considering referral to secondary care. The aims of the project include improving the early detection of liver disease and providing brief lifestyle interventions for those attending for screening.
The St Mary's Surgery Liver Project Southampton
The St Mary's Surgery Southampton recognised that the patients in their large inner city practice were likely to have a high prevalence of liver disease. Having been part of the ‘Locate’ project the practice worked with local liver specialists to improve their identification and management of liver disease through the development of local clinical pathways and through direct GP access to transient elastography (TE).
The West Midlands Liver Health Work
Recognising higher than average liver disease mortality in the region, together with high levels of health inequality, local PHE leads have brought together services and organisations to address the human and financial costs arising from this. Through local workshops and the creation of a local network, the region has put in place strategies to improve the early detection of liver disease and improve the patient experience.
The Liver Matters Project
The 'Liver Matters' project has worked across the Birmingham South Central CCG to enhance the quality of life for people with alcohol related liver disease and their carer(s) and families, providing information and advice, liaising with treatment services, expanding social networks, and supporting end of life care.
The Glasgow Liver Support Service
The Glasgow Ambulatory Liver Support Service was set up with the aim of reducing re-admissions in patients admitted with decompensated cirrhosis by 20%. Focusing on three novel interventions: pre-discharge patient education; post-discharge review; and re-admission prevention strategies; it has been successful in achieving its goals.
Tayside iLFTs
Testing LFTs should be an opportunity to allow early diagnosis, but abnormal LFTs are often incompletely investigated. The Tayside iLFTs project developed an automated investigation algorithm, which maximises diagnosis of liver diseases.
Resources for practices and practice nurses
Patient leaflets on different liver conditions
The British Liver Trust has a full range of leaflets on the whole range of liver diseases that can be downloaded for free. The full range of leaflets can be downloaded from the BLT website, or your patient can order a free hard copy by calling 01425 481320.The most popular leaflets include:
- Living with Liver disease
- Diet and Liver disease
- Alcohol and liver disease
- Non - alcohol related liver disease
- Different types of liver disease
Liver disease often has no symptoms in the early stages. The British Liver Trust has developed a range of materials covering the risk factors for liver disease and the signs and symptoms of liver disease. They are free to order and include posters and leaflets for display in GP surgeries.

- British Liver Trust At risk patient materials
- British Liver Trust online test to see if you are at risk
- NHS Choices symptoms of liver disease in the later stages
Updates and snapshots of interest to nurses:
1. RCN: Caring for people with liver disease: a competence framework for nursing
This framework was developed especially to support all HCPs in identifying patients with known liver disease, identifying those at risk of developing liver disease, promoting health livers and positive lifestyle choices, and to help increase practitioners’ skills and knowledge around managing liver disease. The framework gives examples of what evidence is needed to achieve each area of competence.
For practice nurses, competence 2 gives advice on signposting and supporting patients (and families) to deepen their understanding of their condition through patient education and health promotion.
Community nurses and matrons managing patients with long-term liver conditions may find it useful to use competence 6, working alongside and with the patient (and families), to address the psychological and social impact of their condition. This competence supports appropriate referral to drug and alcohol services, diabetes community teams and coordination of the patient’s care.
Of value to any community practitioner, competence 7.3 looks at managing the pharmacological treatments that may be used in treating patients with liver disease.
2. In order to help understand the needs of community and practice nurses there is an RCN ‘Caring in Practice’ project currently underway (run by Michelle Clayton and Lynda Greenslade).
This project aims to assess the educational needs of community and practice nurses in order to improve their management of patients with liver disease or who are at risk of developing liver disease.
Information will be gathered via a confidential questionnaire which will be available soon on this website. We encourage all practice and community nurses to complete the questionnaire.
Evaluation of responses to the questionnaire will lead onto a study day to address the training needs identified and applying them to the competence framework.
The project will also:
- use social media to deliver bit size chunks of liver learning, relating it to the competence framework
- support nurses in developing skills through practice education sheets
- improve the secondary and primary care pathways for patients with liver disease.
3. The launch of a new liver nursing group called British Liver Nurses Association (BLNA) linked to British Association for the Study of the Liver (BASL) in Sept 2017.
The aims of the BLNA are to:
- one voice for all nurses in primary and secondary care looking after those at risk of or who have liver disease
- work across all four countries in the UK to promote and raise awareness of liver nursing
- work at national and international level to improve the care of patients at risk of or with liver disease
- give a voice to our patients and their families at local and national level to promote equitable access to liver care.
4. Future Plans for developing nursing for those at risk of or with liver disease
- Respond to community and practice nurses’ needs for liver education and support the development of skills needed
- Develop the right educational and support materials and tools for all.
- Use links to the RCN forums to find out what additional support is needed and use those forums to network and share learning and education
- Develop patient-specific care plans for patients as they leave hospital that are available for community services
Resources for commissioners
This section provides links to resources specifically aimed at commissioners.
A financial case for action on liver disease has been developed by the Foundation for Liver Research and this report has been endorsed by the lancet commission on liver disease.
Scotland
There is public health information for Scotland relating to:
Wales
England
In England NICE has produced a quality standard for the management of liver disease. This quality standard covers identifying, assessing and managing chronic liver disease in children, young people and adults, and cirrhosis in young people and adults. It describes high-quality care in priority areas for improvement.
NHS England has published a policy statement on the management of chronic Hepatitis C in patients with cirrhosis.
The Foundation for Liver Research has compiled customised liver disease profiles for each of the 533 parliamentary constituencies in England:
- Profiles for constituencies with names beginning a-s
- Profiles for constituencies with names beginning t-z
Public Health England has developed an atlas that shows variation in healthcare for people with liver disease England. [14,885 KB, PDF]