The difference between Chest Posterior Anterior (PA) and Anterior Posterior (AP) radiographs.
| Site: | ISRRT e-Learning |
| Course: | International Covid-19 support for Radiographers and Radiological Technologists |
| Book: | The difference between Chest Posterior Anterior (PA) and Anterior Posterior (AP) radiographs. |
| Printed by: | Guest user |
| Date: | Friday, 24 May 2024, 3:11 AM |
Table of contents
- 1. The difference between Chest Posterior Anterior (PA) and Anterior Posterior (AP) radiographs
- 2. Figure 1 Radiographs and line diagrams demonstrating the difference between a PA and AP projections
- 3. Why do we do Chest projection imaging PA Erect
- 4. Why do we do Chest projection imaging AP
- 5. The chest radiograph assessement
1. The difference between Chest Posterior Anterior (PA) and Anterior Posterior (AP) radiographs
Erect PA projections are considered the ‘gold standard’ for chest projection imaging (CXR). In some instances, it will not be possible to acquire an erect PA or even an erect AP image and the radiographer / Radiological Technologist will need to opt for a semi-erect or supine image. Research has shown you may also be asked to undertake mobile chest radiography with the patient in the prone position. Projection Chest radiographs are often abbreviated to CXR or chest film (It’s not a film but clinicians still call it a film). It is essential that the correct anatomical and positional markers are included on the image. Any modifications from the standard projection should be noted on the image (See figure 1).
2. Figure 1 Radiographs and line diagrams demonstrating the difference between a PA and AP projections
Figure 1 demonstrates what the appearance of an AP & PA radiograph with annotation and corresponding line diagrams. They appear different because of the positioning and magnification of structures like the heart and mediastinum
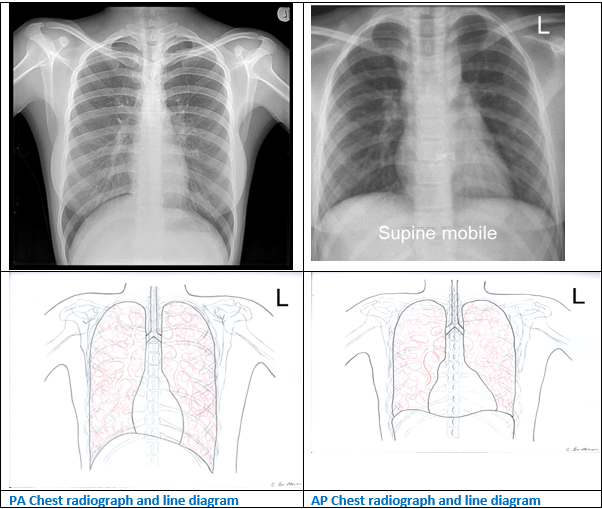
Figure 1 Radiographs and line diagrams demonstrating the difference between a PA and AP projections For all projections the patient needs to be positioned parallel to the detector so that the median sagittal plane is at right-angles to, and in the midline of, the image receptor. For both projections the scapula should be rotated so they do not obscure the lungfields. The lungs, mediastinum and bony thorax (ribs, spine and clavicles) need to be demonstrated. Some spine detail is visualised through the heart and mediastinum. Symmetry is checked by having the medial ends of the clavicle equidistant from the spinous process.
3. Why do we do Chest projection imaging PA Erect
- The patient is positioned easily, its comfortable and they keep still because they can lean on the detector
- It is easier to move the scapula out of the lung fields
- We get an image of the heart with reduced magnification if we use long FRD (180cms)
- The heart is distorted by its position in the mediastinum but you can assess the size of the heart on a PA you cannot on an AP
- There is reduced radiation dose to the anterior radiosensitive organs
- Respiration is more effective when standing
- The anterior ribs are better defined to enable you to check the level of inspiration
- Fluid levels are defined more easily with the use of a horizontal central beam
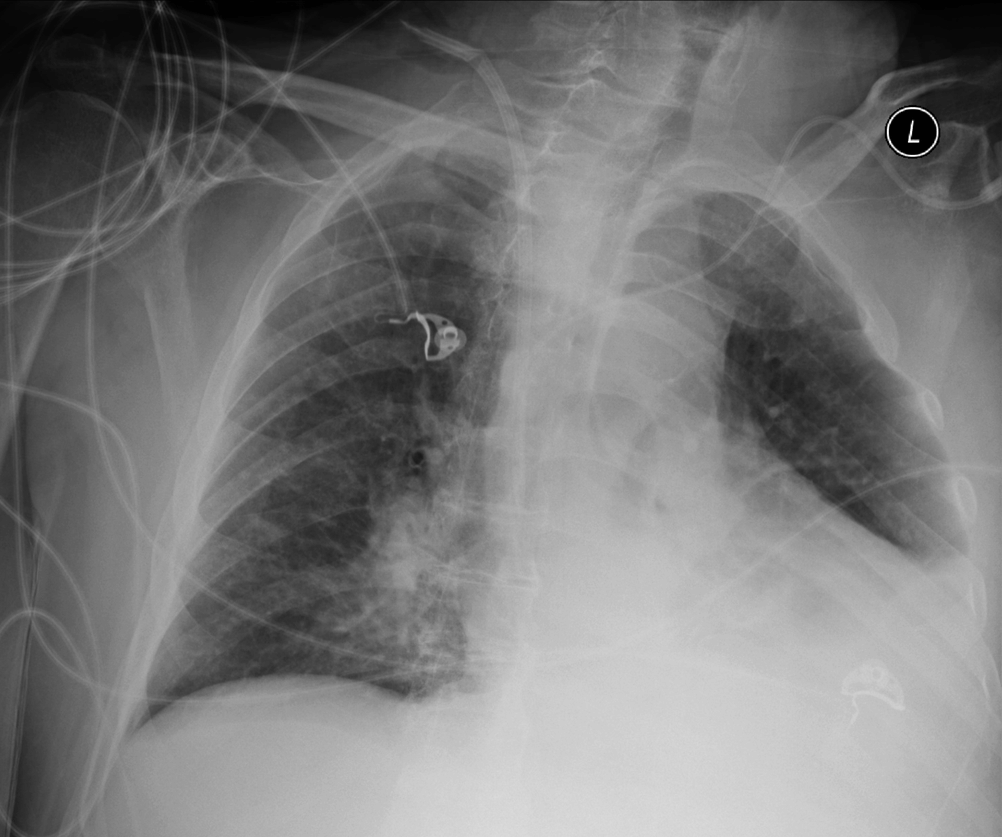
4. Why do we do Chest projection imaging AP
- The patient is not well enough to get into the correct position
- They may be:
- unconscious on the Intensive Treatment Unit (ITU)
- Catheters and tubes for life support and monitoring
- Generally unwell or have learning or physical disabilities
- They may be:
- The patient is being barrier nursed eg COVID-19 patients
5. The chest radiograph assessement
The chest radiograph is assessed to determine if it is a visually sharp reproduction of the anatomy with limited / no distortion of:
- Lungs
- Lateral margins, apex and diaphragm
- Trachea and proximal bronchi
- Vascular pattern in the whole lung particularly the peripheral vessels
- Costophrenic angles
- Retrocardiac lung
- Heart, mediastinum and aorta
- Borders of the heart, mediastinum and aorta
- Bone margins and cortex/trabecular patterns
The X-ray beam is projected onto the detector with the patient in the beam to produce a radiograph
Three things improve the quality of the image in CXR’s
- The patient needs to be straight (not twisted or leaning)
- The patient needs to be as close to the detector as possible
- The X-ray tube needs to be a long way from the patient and detector (it is usually 180 to 200 cms for a CXR
Figures 2 and 3 demonstrates a PA erect projection and diagrams to show a normal projection and how the image may be distorted

Figure 2 The position for a PA radiograph and a diagram showing limited distortion and magnification if the patient is parallel to the detector and X-ray beam is at right angles
We get distortion when the patient is not parallel to the detector or the beam is angled

Figure 3 Distortion of the image with angulation of the patient or X-ray beam
It is easy to get confused by left and right because we view all the images as if the patient is standing facing us as if in the anatomical position. Figure 4

Figure 4 The anatomical position
Figure 5 Radiographs which demonstrates the anatomy which can be recognised on a PA projection

Figure 5 Anatomy labelled on a PA erect Radiographs
We evaluate the image using the 10 point plan (see section in e-learning)
Note. The image should not be blurred
- No blurring because the patient has breathed or moved during the exposure
- Use the fine focus (an option on the X-ray equipment to reduce Unsharpness)
The image should not be distorted
- The PA is distorted because the patient is learning forward 10 degrees and the heart is not parallel to the detector
- But it is what we are used to looking at so we see this as normal
Patient positioning
- Patient should not be rotated / angled in relation to the detector
- Rotated around any plane
- Angled to the detector
- Patient as close to the detector as possible and X-ray tube a far away as possible / reasonable
Common positioning problems with AP erect mobile CXR’s

Patient leaning backwards or the tube angled incorrectly (also no anatomical marker)
Patient rotated