Gunshot Wound to the Chest
Medically reviewed by Drugs.com. Last updated on May 6, 2024.
What do I need to know about a gunshot wound (GSW) to the chest?
A GSW to the chest may cause damage to your heart, lungs, esophagus, ribs, or major blood vessels.
How are injuries from a GSW diagnosed?
Your healthcare provider will examine your body to check for injury. Your provider will look to see if there is an entrance and exit wound from the bullet. You may need any of the following tests to diagnose the damage caused by your GSW:
- An x-ray, ultrasound, CT, or MRI may show damage to your heart, lungs, ribs, or blood vessels. It may also show where the bullet is. You may be given contrast liquid to help your organs or blood vessels show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- Blood and urine tests will show infection, kidney function, and give healthcare providers information about your overall condition.
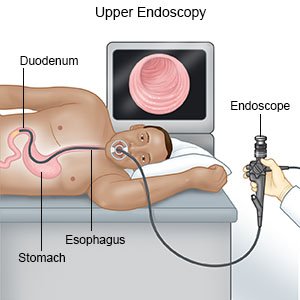
- An endoscopy may show damage to your esophagus or stomach. Small damages to your esophagus may be repaired during an endoscopy.
- A bronchoscopy may show damage to your airways or lungs. Small damages to your airways may be repaired during a bronchoscopy.
- Surgery may be needed to check damage to your organs and blood vessels. It may also help your healthcare provider find out where you are bleeding from.
How is a minor GSW treated?
A minor GSW is diagnosed after an x-ray, ultrasound, CT, or MRI, and a physical exam by your healthcare provider. A GSW may be minor if it does not go deep into your skin or damage any of your organs. Your provider may or may not remove the bullet. Your provider may clean your wound and close it with stitches or staples. Medicine may be prescribed to decrease your pain or prevent infection.
How is a severe GSW treated?
You may need any of the following treatments after a GSW to the chest:
- Medicines may be given to treat pain and prevent infection. You may be given a tetanus shot. Tetanus is a severe infection caused by bacteria.
- A blood transfusion may be given if you have lost blood from your GSW.
- IV fluids may be given to prevent dehydration and increase blood flow to major organs.
- A nasogastric tube may be inserted to remove air, fluid, or blood from your stomach. A nasogastric (NG) tube is a long, thin, flexible tube inserted through your nose and down into your stomach or small intestine.
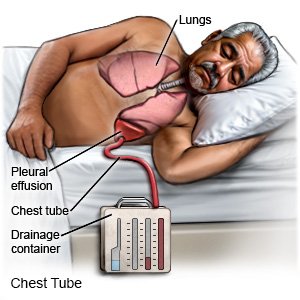
- A chest tube may be inserted. A chest tube is also known as chest drain or chest drainage tube. It is a plastic tube that is put through the side of your chest. It uses a suction device to remove air, blood, or fluid from around your lungs or heart. A chest tube will help you breathe more easily. It may also relieve pressure on your heart and help your circulation.
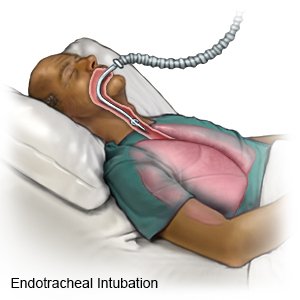
- An endotracheal tube may be inserted to help protect your airway and help you breathe. An endotracheal (ET) tube is a hollow plastic tube that is placed in your trachea through your mouth. The trachea is also called the windpipe or airway. The ET tube is attached to a machine called a respirator. A respirator gives you oxygen and breathes for you when you cannot breathe on your own.
- Surgery may be needed to repair damage to organs or blood vessels. It may also be needed to clean your GSW or remove the bullet. Your healthcare provider can close your GSW with stitches or staples, or leave it open. Your GSW may need to be left open to allow swelling to decrease and tissues to heal.
How can I care for myself after a GSW to the chest?
- Do breathing exercises as directed. Take a deep breath and hold the breath as long as you can. Then push the air out of your lungs with a deep, strong cough. Put any sputum that you have coughed up into a tissue and throw it away. Take 10 deep breaths in a row every hour that you are awake, even during the night. Remember to follow each deep breath with a cough.
- Take short walks. Walk 2 to 3 times per day. This may help prevent blood clots and help you heal faster.
- Do not lift anything heavy. Heavy lifting may place too much stress on your GSW. Ask your healthcare provider how much weight you can lift.
- Sleep in a comfortable position. Do not lie on your injured side. Sleep with your head propped up on pillows. This may make breathing more comfortable.
- Perform wound care as directed. Remove your dressing before showering unless your healthcare provider tells you not to. Do not soak your GSW. Let your wound air dry. Apply a clean bandage as directed. Change your bandage if it becomes dirty or wet. Monitor your wound for signs of infection such as redness, swelling, or pus.
- Get support. It is normal to have difficult and unexpected feelings after a GSW. You may have feelings such as anger, depression, fear, or anxiety. You may have nightmares or continue to think about what has happened. Talk to your healthcare provider if you have any of these feelings. There are treatments available to help you.
When should I call 911?
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
- You have trouble breathing.
When should I seek immediate care?
- Blood soaks through your bandage.
- Your wound comes apart.
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You are vomiting blood or what looks like coffee grounds.
- You feel weak, dizzy, or faint.
When should I contact my healthcare provider?
- You have a fever.
- Your wound is red, swollen, or draining pus.
- You have nausea or are vomiting.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Gunshot Wound to the Chest
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
