Abstract
Inflammation has risen to the forefront of biomedical research into many chronic diseases prevalent in industrialized countries, including mental, metabolic, and postviral conditions. For sociologists, the rise of inflammation in explanatory models of chronic disease is an opportunity to grasp a historical shift in thinking about how society gets under the skin as new modes of conceptualization of the relationship between societies and bodies emerge in this domain. Highlighting two historical conjunctures between epidemiology and molecular biology concerning hormones and fat, this paper thereby contrasts an older cybernetic model of the social as a signal transduced via the brain and hormonal signaling system to become a biological accretion of stress or adversity with an explanatory trajectory centered on chronic inflammation. Rather than transducing the social environment, the inflammatory body emerging from the studies of adiposity and diabetes is produced by metabolizing material and psychosocial conditions. Inequalities in the social world are thereby reflected as inflammatory states that exist upstream of, not downstream to, the kinds of social signals previously deemed important to health and health disparities. Signals still matter, but they are not their own key determinant in terms of action or impact—that is a contextual matter within the chronicity of the processual metabolic life of a cellular and bodily milieu.
Zusammenfassung
Entzündungsprozesse sind in den Vordergrund der biomedizinischen Forschung zu vielen chronischen Krankheiten gerückt, die in den industrialisierten Ländern verbreitet sind, darunter psychische, metabolische und postvirale Erkrankungen. Eine Betrachtung dieser Entwicklung ermöglicht der Soziologie, während der Entstehung neuer Konzepte zum Verhältnis von Gesellschaften und Körpern einen historischen Wandel im Verständnis darüber zu erfassen, wie Gesellschaft „unter die Haut“ geht. Indem zwei historische Zusammenhänge zwischen der Epidemiologie und Molekularbiologie in Bezug auf Hormone und Fett hervorgehoben werden, kontrastiert dieser Beitrag ein älteres kybernetisches Modell des Sozialen als Signal, das über das Gehirn und hormonelle System transduziert wird und schließlich in einer biologischen Akkumulation von Stress oder Widrigkeiten mündet, mit einem auf chronische Entzündungsprozesse fokussierten Erklärungsansatz. Diesem neuen Konzept zufolge, das in der Forschung zu Adipositas und Diabetes zum Vorschein kommt, wandelt der entzündliche Körper nicht die soziale Umwelt um, sondern dieser entsteht durch das Metabolisieren materieller und psychosozialer Bedingungen. Ungleichheiten in der sozialen Welt spiegeln sich daher als entzündliche Zustände wider, die vor und nicht hinter den bisher für Gesundheit und Gesundheitsunterschiede als wichtig erachteten sozialen Signalen liegen. Signale sind nach wie vor wichtig, aber sie sind nicht die entscheidende Determinante für ihre Wirkung oder ihren Einfluss – das ist eine kontextuelle Angelegenheit innerhalb der Chronizität des prozessualen metabolischen Lebens eines zellulären und körperlichen Milieus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Inflammation was a key term of the COVID-19 pandemic. Infection with the SARS-CoV‑2 virus was fatal for many due to the body’s overwhelming immune inflammatory response to viral infection rather than to the direct effect of the virus. Colloquially, we tend to associate inflammation with things we can see and feel—the sensation of swelling and heat around a minor cut, or the fever brought on by a flu. In biomedical terms, however, inflammation refers to systemic molecular-level events. Sensing infection or injury, immune cells trigger physiological and cellular responses that can quell pathogens, clot blood, and repair tissues.
Some immune system cells are specialized to a sentinel role detecting bodily damage or the presence of pathogens. Such sentinels send off a suite of tiny biochemical signals to indicate trouble to faraway cells and tissues. These signals bring other immune cells to the site of infection or cause sensible physical changes. For example, they might trigger the extra permeability of blood vessels, allowing more fluids than usual into the affected tissues, a change felt as swelling. These processes normally ebb and flow, having an acute phase of response followed by a return to baseline once the problem is resolved. In some people infected by SARS-CoV‑2, what has been called a disproportionate or maladaptive inflammatory response occurs, with no abatement in the alarm signals ramping up response, causing tissue damage in the lungs and leading to acute respiratory distress syndrome (ARDS) and organ failure.
In other words, a bodily system that is supposed to sense, adapt to, and resolve a threat to bodily integrity loses the capacity to turn off. The response to danger becomes the danger. While there is some argument about whether the term “cytokine storm” is entirely accurate for these events in the case of SARS-CoV‑2 infection, it does capture the spirit of the problem by contrasting the idea of a “storm” to regular cellular “weather”: The pro-inflammatory cellular signals coming from the immune system (the cytokines) become an overwhelming phenomenon. The scale and severity of severe illness and death have thus made inflammation a key word for researchers and publics alike. As Carl Nathan starkly put it in a recent review, “since 2020, inflammatory responses to COVID-19 have driven the death toll from non-resolving inflammation to the highest level in the lifetime of anyone reading these words” (Nathan 2022, p. 592). Moreover, the unevenness with which an infection for one individual was mild or even nonsymptomatic while for another it was fatal, placed additional focus on chronic metabolic disorders, so-called underlying conditions, characterized by chronic inflammation, as the drivers of differential vulnerability to severe outcomes (Drucker 2021).
Certainly, such matters are of extreme concern to public health and disease researchers. But why should sociologists care about inflammation? In some ways this question has an obvious answer. The “underlying condition” is, for the sociologist, not background but foreground: The social striation of chronic metabolic disorders by class, race, income, education, immigration status, and other social determinants has been repeatedly demonstrated in studies of social disparities in health (Elovainio et al. 2011; Merkin et al. 2020). The triangulation between underlying metabolic health, social position, and COVID-19 mortality and morbidity only further positions inflammation as a concrete measurable outcome proving that “society gets under the skin” and manifests physically in ways that are consequential for socioeconomic and racial health disparities.
Indeed, measures of education and income are associated with molecules elevated in chronic inflammation such as C‑reactive protein (made in the liver in response to inflammation; Muscatell et al. 2020). Testing which social determinants have the most predictive power for biomarkers of inflammation thus provides insight into the causal pathways driving health disparities (Nazmi and Victora 2007; McDade et al. 2011). Inflammation in turn may shape social behavior, with inflammatory states associated with changes in social behavior in model organisms and human subjects (Moieni and Eisenberger 2018). In the wake of such studies, inflammatory biomarkers such as C‑reactive protein, interleukin‑6 (a “cytokine” or signal sent by sentinel immune cells such as macrophages to upregulate further immune response from other parts of the system), and the antiviral cytokine IFN‑γ have risen in favor in sociological, psychosocial, and public health study of the life course embodiment of early life adversity (McDade 2012; Lam et al. 2021).
At the same time, it is too facile to simply add inflammation to a folder of useful biomarkers, as though its molecules were interchangeable elements among others in the health disparities tool kit. This paper proposes instead that the growing social, epidemiological, and biomedical attention to inflammation is an important site of novel theorization of nature–human and body–society relations in increasingly industrialized life worlds. The specifics of inflammation and its study provide a useful focused case of a larger “metabolic turn” diagnosed below as a renegotiation of the idea that bodily insides and social outsides are primarily connected by incoming signals. Dominant twentieth-century models of how “society gets under the skin” have long framed social forces as signals that transduce information from one media (the environment) to another (the body) without loss.
By contrast, the study of inflammation derives from a historically distinct biochemical logic that is more compatible with contemporary ideas of the Anthropocene and “planetary health” in which the biophysical and psychosocial substance of human life is understood in terms of human-made, socially formatted changes to food, air, water, hygiene, temperature, light, sleep, toxicants, and noise (Prescott et al. 2022). These factors do not remain outside the body as context, nor is their main physical impact necessarily mediated through gene expression; they manifest through many entry points as the setting of processes rather than the deposition of residues: as “intracellular consequences of social determinants of health” such as the capacity for coping with free radicals or the ability of cells to repair DNA damage (Emeny et al. 2021).
Such conceptual work is of consequence for sociology beyond specialized subdisciplinary areas. Implications range from the possibility that a new chapter is opening in the history of concepts of the environment (Sprenger et al. 2023) to the generation of better models for understanding the embodiment of space and place in neighborhood and urban effects in mental and physical health (Rose und Fitzgerald 2022). Even from the beginnings of the discipline in the nineteenth century, interactions between ideas about social and bodily order such as the division of labor between specialized organs, or labor as the metabolism between Humankind and Nature, have been important resources for social theory (Durkheim 1947; Schmidt 2014). The separation of natural facts from social facts as different domains of knowledge likewise has been a core feature of distinguishing the discipline from other sciences of human life and has contributed to the study of humans as if their biology and physical environment were unaffected by human social behavior (Limoges 1994; Gunderson 2014). Such separation is increasingly untenable in our own times. The emergence of inflammation as a dominant theme in the biosciences in the 2010s is a distinctive historical formation whose contours provide an opportunity for sociologists to observe a shift in relations between social order and biological order (or disorder) in a period of anthropogenic planetary change, a shift that is simultaneously an empirical topic for study and a prompt to reexamine the models through which that topic is apprehended in the social sciences.
In short, what I detail below is a gestalt-like shift from figure to ground, signal to medium, best highlighted through historical comparison with what has come before. I show that the very idea that society can “get under the skin” was formulated via a framework of signal transduction borrowed from cybernetics and digital signal processing. In a historical conjuncture between social epidemiology of status and stress and the emerging molecular biology of mechanisms of hormone action, the social was reconceptualized as a signal. Factors such as stress and racism were understood as transduced via sense receptors and the brain, linked to hormonal signaling cascades, pouring from society into the body and becoming embedded there in physical form such as hardened arteries or, somewhat later, epigenetic “marks” that altered gene expression.
Historical comparison of this signal transduction model with more recent inflammatory theories of embodiment illuminates key distinguishing characteristics of both. The signal transduction model has by no means faded and is still a powerful framework for scholarly and popular understanding of how social forms are embodied and manifest as social and racial disparities in health. Nonetheless, a more recent metabolic turn in the biosciences, sharpened and made more urgent by the COVID-19 pandemic as described above, has underpinned the rise of inflammatory models of disease and disparity. The metabolic processual body evident in these models, a body that now includes the microbiome, lives in a socially formatted and differentially distributed milieu of food, toxicants, stress, work, exertion, sugar, sleep, deprivation, noise, temperature, and air, all of which are constantly metabolized (digested, detoxified, oxidized, phosphorylated, excreted, compartmentalized, resynthesized, or otherwise biochemically ordered).
To metabolize means to change a substance’s biochemical form within the enzymatic and spatial organization of metabolism. Metabolism, in turn, is generally defined as the chemical processes that occur within an organism to maintain life. Society—or at least the configuration of nutrition, status, behavior, stress, and pollution that we call society—is always already there being metabolized in the process of the maintenance of life. The resulting inflammatory ground state is an important determinant as to whether and how any of the millions of constantly incoming signals, whether a virus or a psychosocial stressor, is incorporated and responded to.
Empirically speaking, this analysis of a shift from a biosocial body of signals and cascades to a metabolic processual body manifesting an anthropogenic milieu as inflammation is based on archival work in the papers of scientists involved in the discovery of the mechanism of hormone action; interview data with researchers in immunology, microbiology and epigenetics; and participant observation fieldwork in scientific settings. It is a sociological reading of explanatory models, both in the past and the present. However, what follows is narrated in the style of a literature review for the purposes of foregrounding the main contours of a historical shift for readers of this special issue who may be interested in biosocial models of human life but do not have a great deal of familiarity with the biological side of the biosocial coin. By necessity, this article deals in materials that mostly come from outside the conventions and disciplinary confines of sociology proper, but it should be meaningful to sociologists nonetheless. In the account I give below, biosocial models of human life are forged at the conjuncture of epidemiology and molecular biology, in the sense that historian Hans-Jörg Rheinberger has given to the conjuncture: “crossing points of independent chains of events … forms in which the moment of the aleatoric plays out in scientific development, in which the unforeseen materializes” (Rheinberger 2022, p. 517).
Historicizing these conjunctures reveals joint conceptual formation that is as important for sociology, social epidemiology, and social psychology as it is for molecular biology, giving lie to a perhaps unrecognized assumption of a kind of service relationship in which social scientists problematize, asking questions such as why workplace hierarchies are linked to risk of heart attack, and molecular biology provides quantifiable biological correlates to prove causal chains of relations, such as those linking stress to arteries (Schulte and Perera 2012). What is shown below, in close study of the historical conjunctures around hormone mechanisms and fat, is that even the social scientist who never goes near a molecular explanation nor engages with natural sciences is nonetheless likely working within a heuristic explanatory frame for how social forces and institutions are linked to collective and socially striated bodily or health outcomes grounded in historical events in molecular biology. Molecular biologists in turn are working with ideas about social life such as the nature of shift work or adversity that remain unhistoricized and underspecified, more assumed than examined. Just as Durkheim drew on ideas of the hierarchy of biological organization as a resource for social theory, ideas that themselves were shaped by Darwin drawing on older social theories of the division of labor, what we have before us is a skein that does not begin in one discipline or another but may nevertheless be excavated archaeologically and historically as an analysis of joint and interlacing origins (Beer 2009; Foucault 1970).
2 Social Transduction at the Conjuncture of Social Gradients in Health and Mechanisms of Hormone Action
The idea that society “gets under the skin” crops up with some frequency today, both in popular literature and in research paper titles about stigma, unhealthy environments, adversity, and racial disparities in health, all of which are conceptualized in terms of causal pathways by which social factors or forces become expressed as physiology, often in ways that incur heightened risk of diseases of various kinds. The phrase verges on the banal—it is an unremarkable way to show that a research project or a theorist is talking about how the social world connects to the biological world. Despite this banality, its imagery remains vivid, depicting something outside the body that pierces the protective boundary of the skin and comes to inhabit the inside of the body. It implies breaching of the individual defenses by collective conditions, and a state transition from nonphysical to physical. The other colloquial use of this phrase points to its negative connotations—if I were to say that my neighbors were getting under my skin, I would mean that they were irritating me in a way that I am unable to avoid. Evoking splinters and the misery of burrowing parasites, there is rarely anything good about things that get under the skin. In terms of society, this phrase is generally meant to explain how differences in social life such as racial discrimination can translate into differences in health, with social disadvantage shortening both health-spans and lifespans (Green and Darity 2010).
It may surprise readers to know that society has been getting under the skin in this linguistic sense only since the late 1990s, when the phrase was introduced into its social scientific use by health psychologists reviewing evidence for environmental (community, work, family, peer group) drivers of chronic and acute health disorders via psychosocial mechanisms (Taylor et al. 1997). In this section of the paper, I show how this formulation marked not the beginning but the achievement of a merger of conceptual and technical resources from biology with explanations of longer-standing observations of socioeconomic gradients in health and mortality. While there are many models of how elements of social life can translate into biological form dating well back in time, a comprehensive survey is beyond the scope of this article and can be found elsewhere (Meloni et al. 2016; Krieger 2011).
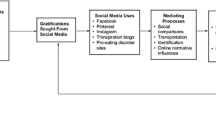
I shall concentrate more narrowly here on what are characterized as epidemiologically based “psychosocial” models for explaining how social difference becomes embodied that have drawn on the biology of stress for their mechanistic hypotheses about how one turns into the other. In this case, I show how these models were enabled by the idea of signal transduction and made possible by concepts from digital signal processing in the cross-fertilization of cybernetics and biology that occurred in the middle of the twentieth century. In particular, the idea of transduction between social or environmental conditions and physical outcomes was key to the idea that social forces would enter the body via the brain and sensory system and be translated by hormonal signals into bodily manifestations. This model, which I call the social signal transduction model, formed at the perhaps unexpected meeting place of the social epidemiology of class and cell signaling biology.
2.1 Social Class and Mortality
Before getting to the conjuncture itself, let us begin with a brief look at the origins of theories of social class differentials in chronic illness and mortality. Epidemiological studies such as the London Transport Workers Study initiated a focus on the customs and habits of the working class in relation to disease incidence and life expectancy in the mid-twentieth century (Mold et al. 2019). Language of human “behavior” followed only somewhat later as this kind of work became increasingly biologized and as an accelerating epidemiology of smoking singled out individual life choices as causes of lung cancer and heart disease. Large studies comprising thousands of subjects, such as Framingham (located in Massachusetts and launched in 1948), saw the development of statistical risk factor frameworks that “helped turn diseases into a matter of personal behavior and attitude” (Mold et al. 2019, p. 25).
In Britain, the Whitehall Study began on the model of Framingham in 1968. This ambitious cohort study enrolled thousands of male British civil service workers and followed their health and lifespans from 1967 to 1977. Unlike Framingham’s individualizing bent, the Whitehall Study produced what were at the time startling findings: a reverse social gradient showing that individuals employed at the lowest ranks of the civil service were at the highest risk of mortality. Men in the lower employment grades were shorter, were heavier for their height, had higher blood pressure, had higher plasma glucose, smoked more, and reported less leisure-time physical activity than men in the higher grades (Marmot et al. 1978). Contrary to dominant narratives of health behaviors, Whitehall researchers pinpointed class itself as a determinant of these markers of health and their disease outcomes (Clark 2021). Epidemiologist Michael Marmot argued that social hierarchy had material negative effects on health for those on the lower rungs of society in his widely read book, The Status Syndrome (Marmot 2004).
It is in the explanatory model given to this correlational data that one begins to discern the conjuncture with hormone biology. Whitehall researchers turned to stress to explain how a collective condition such as social standing translated into variation in morbidity and mortality outcomes by civil service ranks. They focused on the stress of low-status jobs combining a high degree of demand with low levels of control over the working environment (Arminjon 2020). How could the workplace directly translate into a biological measure such as plasma glucose? The posited causal cascade had hormones at its core, drawing upon a Selyean model of stress. For Hans Selye, the hormones of the hypothalamic–pituitary–adrenal axis, in particular those of the adrenal glands, were the key protagonists in efforts to maintain homeostasis in the face of diverse disturbances (Viner 1999).
Importantly, in this framework “stress” described the physiology of the organism moving sequentially through the stages of alarm, resistance, and, finally, exhaustion and death. Stressors could be physical agents, tissue damage, or psychological states. Modern life was, in Selye’s view, a source of chronic challenge by “emotional irritants” (Selye 1954). While Selye formulated a distinction between acute and chronic stress based on experiments using rodents, the actual mechanism by which chronic hormonal activation led to death was, like the mechanism of hormone action itself, unknown (Harrington 2009). Nonetheless, the first models for workplace, status, and socioeconomic stress posited that the hormones of the hypothalamic–pituitary–adrenal axis were the physiological actors in a sequence of events by which the environment became manifest in biological form.
2.2 Hormones and Cybernetics
In 1969, just one year after Whitehall was launched, the language of signal transduction was imported from cybernetics into explanations of the mechanism of hormone action by Martin Rodbell at the National Institutes of Health (Landecker 2016). It is hard, today, to communicate this as a noninevitable turn of events, or even a moment of transformation, as it seems so self-evident to use the terminology of transduction to describe how something moves from one medium into another, i.e., from “the environment” to “the body” or from “the social” to “the biological,” but keeps its form, that is, its informational content.
To transduce means to alter the physical nature or medium of a signal, to convert variations in a medium into corresponding variations in another medium. In engineering, signal processing predated the use of the term in biology. The technology of digital signal processing then became a resource for the understanding of how a hormone could enact change inside a cell yet not enter it. Transduction allowed the construction of a model in which the hormone bound to a receptor, activated a signaling cascade, and then eventually triggered a change in gene expression, altering physiology. The hormone did not, as was previously thought, act directly on enzymes or cellular structures. Rather, its action was newly conceived in terms of its transduction via a set of molecular intermediaries that came to be understood as signal cascades. These cascades led in the end to a change in gene expression and a physiological response (the production of an enzyme or a shift in cellular activity).
This framework was initiated long before cybernetics, in the “chemical messenger” hormone concept of the early twentieth century (Starling 1907). However, the introduction of a transduction model by which a hormone meeting a G-protein linked receptor set off a cAMP “second messenger” cascade was a key moment, establishing cell signaling as a molecular infrastructure for understanding cell–cell communication of all kinds in the late twentieth century (Reynolds 2018; Landecker 2016). The study of oncogenes and the inappropriate amplification of cellular growth signals as potential targets in cancer therapy drove an enormous burst in activity in cell signaling; by the 1980s, immunology was likewise dominated by the search for the signals such as interleukins that cause immune cells to gather, proliferate, or morph (Fantuzzi 2016). Indeed, inter- and intracellular signaling has come to be accepted as a fundamental characteristic both of how cells live together in a body and how environmental conditions are sensed and adapted to in a coordinated way. While never theorized to the extent that the gene concept was, the signal concept is seen as a unifying framework across biology and biochemistry to understand how cells sense and respond to environments and each other (Hancock 2017).
Theories of the mechanism of hormone action and its subsequent connection to the larger rubric of cell signaling might seem far afield from the epidemiological work summarized above, in which studies such as Whitehall were distinguishing between “factors that determine which individuals within a population get a disease (individual fact) and the determinants of different incidence rates of disease among different populations (social fact)” (Hertzman 2012, p. 17160). Yet the centrality of hormones as mediators between social “factors” and bodies (especially brains) in the early years of the stress paradigm connected the epidemiology to the experimental life sciences through the signaling framework. It is important to underscore that this was not a one-way legitimation of floaty social science with more precise and therefore more believable mechanisms, or the grounding of correlation in causation, the usual caricatures ascribed to such exchanges.
Rather, gathered in the historical epidemiological–experimental conjuncture of the hormone mediator were several trajectories that had up until that point proceeded separately. Endocrinology was being pulled into the orbit of research on the control of gene transcription, away from its classical physiological form (Tomkins et al. 1970). The mid-1970s also saw a veritable explosion of research beyond these more classic steroid hormones, as smaller peptides such as endogenous opioid peptides and their corresponding receptors in the brain expanded the repertoire and complexity of signaling molecules moving between the brain and the viscera (Klavdieva 1996). And going beyond hormones themselves, the early 1970s was a time of transformation in ideas about how an ambient and generalized environmental condition, for example a change in temperature, might set off highly specific gene expression patterns in an organism, such as the expression of heat shock proteins (Tissiéres et al. 1974). At the same time, as noted above, things as nontangible and socially collective as status were being characterized as physiologically consequential external conditions, singled out as epidemiologically significant and carefully statistically disentangled from more straightforward narratives of individual behavioral risk such as cigarette smoking.
In short, different connections between physical and social environments all converged around hormones as embodiments of the idea that ambient, immersive and nonspecific kinds of exposures could act as triggers for signal cascades that were highly specific allosteric molecular cues, one molecule triggering another to change shape or move or react differently with another cellular component, eventually leading inward to the gene and then through gene transcription outward again to ensuing physiological changes. While these events in molecular biology are not generally discussed together with the development of sociobiological or sociopsychological models for how social conditions become embodied, they should be. The actors involved were assembling their studies and frameworks by drawing on conceptual and technical resources from across these domains.
At stake was a fundamental reorganization of the relationship of generality and specificity. Hans Selye had put emphasis on the nonspecific physiological impacts of stress: The lesions and symptoms elicited by restraint, cold, pain, or toxins were, after all, characterized as features of a general adaptation syndrome in his framework. By contrast, the unfolding work on a hormone mechanism of action as signal transduction was premised on the concept of allostery, itself grounded in the idea of the centrality of three-dimensional shape of receptors and ligands, a structural specificity that would allow one molecule to find and bind another in the blindingly complicated tumult of a cell surface or cytoplasm (Phillips 2020). In other words, while the trigger might be as general as a change in temperature, the outcome of the triggered signal-cascade mediation system had the exquisite specificity of molecular interaction. This quite literal channeling of the general into the specific provided a compelling and far more elaborated explanation for how something ambient could become a highly particular molecular outcome. Moreover, that specified outcome could be measured in finer units than the presence or absence of ulcers or the weight of an adrenal gland.
2.3 Enter Allostatic Load: The Hormone as Signal Needs the Body to Be an Information-Receiving Apparatus
The introduction of the framework of allostatic load in the early 1990s was strongly reinforcing for social epidemiologists beginning to understand hormones as transducers (Serviant-Fine et al. 2023). Allostatic load, arguably the most dominant model of causality by which social stressors drive chronic disease in the second half of the twentieth century, was defined by Bruce McEwen and Eliot Stellar as the “strain on the body produced by repeated ups and downs of physiological response, as well as the elevated activity of the physiological systems under challenge [causing] changes in metabolism … and wear and tear on a number of organs and tissues” (1993, S. 2094). They took the term allostasis from Peter Sterling and Joseph Eyer’s (1977) “Stress-Related Mortality and Social Organization,” a paper focused on how bodily baseline norms such as blood pressure were changing because of the alienating organization of work and family under industrial capitalism (Arminjon 2016). McEwen and Stellar very pointedly departed from collective social conditions as a focus by setting their theorizing under the title “Stress and the Individual.” For our purposes, what is of interest in the rise of the allostatic load model is that it shows the implications of the social as signal: the conceptualization of the body as receiver. Signals imply receivers, of course, and so the depiction of the body as a system organized by reception of incoming information is an important second arena in which the profound legacy of cybernetics may be traced in postwar biological and epidemiological thought.
The colloquial framing of wear and tear in the definition of allostatic load, above, belies a thoroughly cybernetic framework derived directly from American psychobiology. Explicitly drawing on the work of University of California Los Angeles psychiatrist Herbert Weiner and his 1992 monograph, Perturbing the Organism: The Biology of Stressful Experience, McEwen and Stellar depicted external stimuli as received (and thereby modulated) by the “information processor” (the central nervous system) and then transduced by the neuroendocrine system of “mediators” (hormones and signaling peptides), which in turn cued “effectors,” components of the metabolic and immune response (1993, p. 2095). The “principles of function” laid out by Weiner were “signaling, regulation, modulation, and redundancy [that] apply at every level of organization” (Weiner 1992, p. 257). “Though complex,” he wrote, “organisms can be described by their interacting functions and systems arranged in feedback loops, or paced by oscillators, and organized in multiple parallel pathways” (Weiner 1992, p. 18).
The system could be reorganized by stress, as seen in the psychology of individuals experiencing civil disaster, or could wear out, just as modern machines were prone to do (Rioch 1971). Within this schema, individuals are depicted as receptacles; society poured down a “neuroendocrine cascade” into these receptacles (Sapolsky et al. 1986). Each brain is an individual entry point through which collective conditions become individual outcomes. Individual outcomes, in turn, add up to population health. Allostatic load was a summation of the “cascading relationships, beginning early in life, between environmental conditions and genetic predispositions that lead in large individual differences in susceptibility to stress … and disease” (McEwen and Stellar 1993, p. 2093). The same biology led to different individual outcomes because individuals experienced different loads over time.
Importantly, one could measure not just the mediators and effectors of social or physical stressors but also the resulting degree of wear and tear in each individual’s “system.” Social differences in embodied health outcomes were thus cast as the result of multiple impacts on these diverse mediators. Epinephrine, for example, triggers cellular responses that result in briefly elevated blood glucose. Although transient, frequent and repetitive stress means, over time, higher average blood glucose levels than would occur in other less-stressed individuals. In turn, elevated blood glucose can react with blood proteins, such as hemoglobin, resulting in a stable and measurable modification of the protein with a sugar moiety. Thus, glycated hemoglobin levels, which are easily quantifiable from blood samples via an automated and standardized laboratory procedure, could then be interpreted as an accumulation of many events that had occurred over the 2–3-month lifespan of the red blood cell (Kelly et al. 1997). The obdurate physicality of the endpoint of the cascade involving social or job stress driving elevated blood sugar lent a concrete sense to the idea of “biological embedding”—physical traces accreting in physiologically consequential places such as arterial walls (Hertzman 2012). Such notions of a cascade triggered by events leading to an implacable physiological change are still visible in the language of childhood poverty leaving a “biological residue” that endures over the lifespan (Miller and Chen 2013).
This is how we arrive, historically, at the very possibility of saying that society can get under the skin, in the late 1990s. The physical medium of embedding has shifted since, coming to include epigenetic marks and telomere length, with the idea of chromatin configuration as a biophysical “receiver” and registrant of incoming signals (Badeaux and Shi 2013). Yet the basic conceptual structure held steady even as the use of epigenetic biomarkers surged in the literature as another way to gauge the physical manifestation of social inequality (Martin et al. 2022). For example, the idea that social experience would leave “epigenetic marks” in the biophysical medium of chromatin was supported by empirical demonstrations of how extreme restraint stress in animal models of post-traumatic stress disorder changed post-translational methylation and acetylation modifications of DNA or histone proteins in neurons (Hunter et al. 2009). The rise of a body of signals and cascades provided a model to epigenetics for how a general environmental condition could become specified in a set of receptor-mediated interactions that ended in physiologically consequential changes in gene transcription. These changes in gene transcription or epigenetic marks on gene promoters could then be detected quantitatively as biomarkers. While ceding environmental determinants more entry to the genetic domain than previously, the epigenetics of the early 2000s nonetheless flowed into the conceptual cast set by the status/hormone conjuncture in which social and environmental conditions were seen as signals transduced into the hormonal and therefore the cellular economy of the body.
Psychosocial epidemiological theories of disease distribution have been masterfully critiqued by epidemiologist Nancy Krieger, who compares them to sociopolitical models as according “less attention, theoretically and empirically, to who and what generated psychosocial insults and buffers, and also how the social, spatial and temporal distribution of these exposures—along with that of ubiquitous or non-ubiquitous pathogenic physical, chemical or biological agents—is shaped by extant and changing social, political, and economic priorities and policies” (Krieger 2011, p. 198). Others have similarly decried the loss of a sense of the social in what is ostensibly a biosocial model: Focus on molecular mechanisms in these social transduction models “keeps cause small” and mistakes the mechanism for the cause, obscuring its location and workings in society (Geronimus 2013; Roberts 2021; Chiapperino and Paneni 2022). Fundamental cause theory likewise insists that it is social organization, particularly that which differentially impacts access to resources, that drives inequalities in health as the set of “inputs” that drive health-related “outputs” (Clouston and Link 2021).
Despite their acuity, what is still missing from these critiques is, I think, a deeper appreciation of the historical specificity of the enduring cybernetic legacy of the mid- to late twentieth century. The very terms of debate are structured by this legacy—contesting which “input” into the “system” is most fundamental and arguing that one should study the pretransduced “social” versus the onward biological form. Moreover, the critique seems moot to its intended recipients. Signal transduction licensed researchers to build a quantitative framework for following society across the skin and into the body, and then to assume that what they were measuring was still society, just a version transduced into the biological medium. This assumption of fidelity is key. It is intrinsic to the definition of transduction that there is no loss of information even as a signal moves from one medium to another. A historical appreciation helps us understand exactly how causal reasoning became entrained to assumptions that more or less cryptically carried forward cybernetic forms of valuation focused on reception, transmission, and fidelity even as a signal was constituted by different media: an emphasis on “communication—not substance” (Fantuzzi 2016).
3 The Metabolic Turn and the Inflammatory Milieu
The particularity and cultural specificity of the ascendence of the signal across the life and epidemiological sciences in the twentieth century is made more legible by the emergence of alternative molecular-level causal frameworks that explicitly question assumptions around signaling. In this second part of the paper, I give a brief historical overview of the emergence of inflammation in explanations of cancer and metabolic disorder and discuss some examples of what I call a “metabolic turn” in reasoning whereby social environments are metabolized or give rise to metabolic conditions. While an understanding of hormones and other cell signaling molecules remains highly relevant in these explanatory models, the determining status of the signal is reduced, becoming much more context dependent. Those metabolic states form the dynamic ground condition of any cell, tissue, or body and help determine how any incoming signals will be received and responded to. In other words, society is always already there, conditioning what any given signal will mean. A few examples drawn from cancer biology and studies of air pollution will assist in making these somewhat abstract comparisons more tangible.
3.1 Inflammation at the Conjuncture of Epidemiology and Molecular Biology
Inflammation was conceptualized from ancient medicine forward as a phenomenon characterized by the classic signs first denominated in the first century AD as rubor (redness), calor (heat), tumor (swelling), and dolore (pain) and further elaborated by Rudolph Virchow in the nineteenth century as accompanied by functio laesa, or disturbance of function (Medzhitov 2010). An innovative theorist of inflammation in his own right, immunobiologist Ruslan Medzhitov observes that Virchow’s classification of inflammation as a pathological state meant that for much of the twentieth century, inflammation was the domain of pathologists rather than physiologists. This masked its continuity with normal physiological homeostatic responses.
The place of inflammation in the normal–pathological spectrum began to shift within the cell signaling era described above. The study of cell signaling from the 1970s forward into the molecular era was dominated on the one hand by oncology research seeking to understand how mutations in key signaling pathways caused cancer and on the other hand by the elaboration of the signals that elicited and magnified immune responses. Immunologists understood that immune cells produced and responded to signals, classifying these signals by the cell type that made them: lymphokines from lymphocytes, monokines from monocytes, macrophage inhibitory factor from macrophages. The term “cytokine” was proposed in 1974 when it was realized that these small peptide signals could be produced by virus-infected nonimmune cells as well (Cohen et al. 1974).
Paradoxically, the molecular characterization of cytokines in injury and infection in the 1970s and 1980s led to the realization that inflammatory responses can readily occur in the absence of either injury or infection. Inflammation is a spectrum, with pathogen invasion or tissue injury only the extreme end of perturbations that cause enough pain or swelling to be readily perceptible. This realization did not, however, simply come from the molecular tools by which to perceive inflammatory cytokines in tissues and study subjects; it arose from a conjuncture between this kind of basic cell biology and the epidemiology of obesity, type 2 diabetes, and chronic metabolic conditions, particularly the increasing connections being newly drawn between obesity and cancer in industrialized societies with aging populations.
Epidemiological correlations between obesity and reproductive system cancers in women opened out the study of adipose tissue as a “source of hormones,” a search that would eventually transform perception of adipose tissue from that of a passive storage organ to a highly active endocrine organ (Siiteri 1987). Studies of rodent models of obesity characterized a series of what came to be called “adipokines”—signaling molecules secreted by adipose cells such as adipsin and leptin (Flier et al. 1987; Ahima and Flier 2000). The similarity of adipokines to inflammatory cytokines and their pleiotropic effects on immune function was one element in the dawning realization of obesity as a state of chronic low-level inflammation, driven by the endocrine activity of adipose tissue (Fantuzzi and Faggioni 2000). A similarly profound ontological reconfiguration came with the discovery that adipose tissue was a source of tumor necrosis factor (Hotamisligil et al. 1993). Why would a peptide studied previously only in the context of cancer be produced by what was at the time regarded as merely a storage organ for lipids? It came as a surprise to find that similar signaling peptides were produced by adipose cells, because “the potential for an immunological nature of metabolic disease and its relation to obesity was largely disregarded for decades” (Hotamisligil 2017, p. 406).
Interestingly, from the beginning, the epidemiology of obesity has been attentive to social difference, initially driven by the concerns of the life insurance industry (Fletcher 2014). A psychiatric theory of obesity motivated the study of the relationship between mental health and body weight, but an “incidental” finding came from the introduction of parental social class as a controlling variable (Moore et al. 1962). The controlling variable turned out to be more predictive of overweight than the psychological measures putatively under study (Goldblatt et al. 1965). These findings in turn set off a flurry of studies looking at the socioeconomic correlates of obesity (Rimm and Rimm 1974). Again, as in the example above, this history of epidemiology of social status is never discussed in the same breath as the conceptual unfolding of molecular immunology—indeed, they are assumed to be worlds apart—but they co-occur in a conjuncture around fat and together give rise to another trajectory through which to think about social and biological relations, detailed below. Chronic low-level inflammation as a hallmark of both social adversity and chronic disease comes to us from the concurrent study of fat and fatness in society, the bloodstream, cancer, and immunology.
3.2 Inflammation in the Metabolic Processual Body: An Alternative to the Signal Transduction Model?
Inflammation continues to surge today as a focus for research in part because of its cross-cutting presence in a wide range of diseases, in particular the chronic illnesses characterizing industrialized societies (Furman et al. 2019). For many theorists and empirical workers researching health disparities, inflammation simply constitutes another downstream manifestation of “biological embedding” because long-term exposure to stressful experiences such as financial deprivation is seen to lead to overstimulation of the sympathetic nervous system, with concurrent repression and wearing out of anti-inflammatory bodily responses such as cortisol secretion (Kokosi et al. 2021). The signal transduction framework has remained robust, in terms of the history just recounted, for a good 50-year run at least. The primacy of neuroendocrinological pathways as primary mediators between social conditions and psychobiological states continues to be asserted in practice and theory, for example in the relatively recent articulation of the “social signal transduction theory” of depression that includes inflammation as a downstream effect of hormonal transduction of psychological states (Slavich and Irwin 2014; Slavich and Sacher 2019).
At the same time, a distinctly different set of logics has begun to emerge around inflammation, oxidative stress, and metabolism, particularly in biosocial thinking. At its most abstract, one can perceive a shift in emphasis from “outside-in” information models to what might be called “metabolized-world” substance models (this is my term for it). The question of how an ambient condition was channeled into a highly specific signal cascade—mostly mediated by the brain—was at the heart of the previous model. Things downstream from the brain’s directions to the body were the outcomes of whatever came in via the brain or the senses more generally. By contrast, the metabolic framework tends to view the outside environment as constitutive of an inside environment through the many channels and ports of entry that embed a body in a sociomaterial world of practices and unequal distribution of resources and pollutants (Shove and Spurling 2013).
This shift from outside-in to metabolized-world thinking is visible in the increasing agency granted to a range of entities that were previously assumed only to hold the role of downstream effectors of upstream signals. Mitochondria, for example, traditionally cast as the powerhouse of the cell concerned only with energy transformation, have recently been appearing in explanatory models of stress as key mediators (Picard et al. 2018). The so-called stress hormones are, after all, produced in the first place inside mitochondria, and mitochondria are deeply attuned to substance exactly because of their central role in energetics (Picard und McEwen 2018). These organelles are sensitive to oxygen levels, nutrient balance, and oxidative stress in the cells and tissues that surround them, and dynamically sense and react to the demands and threats of exercise, sleep, nutrition, pollution, and stress. Elsewhere, the microbiome produces metabolites that move systemically through the body shaping cellular epigenomes, including those in the brain (Louwies et al. 2020). Some of those metabolites are crucial to health, and some are not; microbial digestion of carnitine (abundant in red meat) in the gut is “both a biomarker for and a driver of vascular inflammation, leading to both atherosclerosis and stroke” (Nathan 2022, p. 597). The inflammatory tone set by pollutants or dietary patterns working through multiple agencies within cells and tissues thus sets the milieu within which behavior, decisions, and hormone production are initiated.
In short, the ambient outside becomes an ambient inside, taking the form of the flow and chronicity of substrates, oxidants, antioxidants, fatty acids, toxicants, and bacterial metabolites via the constant mediation of cellular and systemic metabolism. That inside environment then functions as the context into which any incoming signal arrives. The signal does not determine what is done with it, but the cellular milieu—itself a reflection (but not a microcosm) of an environmental milieu—determines what occurs. This shift will be easier to perceive in the form of specific examples: metabolic environments as upstream of cancer causation, and air pollution patterned by environmental racism or socioeconomic status.
As noted above, researchers have long struggled to understand the epidemiological links between chronic metabolic conditions and certain forms of cancer (Calle et al. 2003). A few studies have now begun to unravel a sequence of events by which metabolic conditions are actually upstream of the genetic mutations long thought to be the initiating cause of cancer. For example, in pancreatic cancer, researchers have shown that high blood glucose conditions can initiate a sequence of events that lead to genome instability in pancreatic cells, making a mutation in a cancer-driving gene, KRAS, more likely (Hu et al. 2019). Subsequent studies have suggested that KRAS mutation-bearing pancreatic cells (whose presence is made more likely by high blood glucose) will remain normal until an inflammatory event pushes them into a state of increased epigenetic plasticity, only then progressing toward cancerous phenotypes by altering the way these cells respond to and emit cell-signaling molecules (Burdziak et al. 2023). It is worth noting that these are not gene–environment interactions, but protein–environment interactions. High blood glucose induces environmentally mediated changes in the post-translational modification of DNA synthesis enzymes, inducing genome instability; then inflammation changes the post-translational configuration of histone proteins, which only then affects gene expression.
This may seem a very technical example that is only to do with biology: blood glucose upstream of mutation instead of mutations upstream of signaling. Yet one only needs to open the aperture slightly to see that blood glucose control is profoundly socially patterned (Lutfey and Freese 2005). Beyond dietary content, access to diabetes control technologies, air pollution, exposure to heavy metals, shift work, and the periodicity of eating are all socially mediated environmental factors that can distort blood glucose regulation (Weiss et al. 2020; Yang et al. 2020; Wu et al. 2021). Populations chronically exposed to shift work are going to experience metabolic shifts patterned by their work schedule, and precarious or off-hours scheduling is in turn patterned in human populations by education, class, gender, and ethnicity (Kalsbeek et al. 2014; Lieberman et al. 2020). The metabolized-world thus sets the conditions for the “meaning” of mutations and signals; disease becomes a failure in the ongoing-ness of maintenance (of genome stability, of cell differentiation) rather than the accretion of societal residue.
Air pollution, just mentioned as a factor in deranging homeostatic blood glucose control also serves as an excellent example of what it means to think via a metabolic processual model of the outside environment as constitutive of an inside environment. Let us take this passage from a recent review discussing “inflammatory inequity” as a starting point for understanding the delineation of the explanatory logic. Observing that the social world is stratified in terms of proximity to sources of air pollution by race and economic status, which also structure diet, social, and built environments, the author writes:
People can develop non-resolving inflammation in response to their physical, economic, and psychosocial environments, including through the air they breathe, the temperatures they experience, the diet they access, and the stresses they endure from poverty, discrimination, or dysfunctional relationships … for example, inhaling fine particulates causes inflammation that contributes to cardiovascular disease and insulin resistance. Metals and organic compounds borne on the particles may generate reactive oxygen species (Nathan 2022, p. 598).
It is not that the brain, gene expression, or hormonal signaling are lost from sight, but that the setting in which these organs or processes function is always already conditioned by the metabolized environments in which the body lives and has lived over time. The psychosocial and the physical environment are not operating on separate systems, one a question of psychology and one a question of toxicology.
According to this view, the liver matters to the brain as much as the brain matters to the liver because they are each other’s metabolic interlocutors. The physical environment that causes a higher inflammatory tone in the brain can influence disinhibition in behavior (Shi et al. 2022). Cells are not only at the receiving end of hormonal signals mediated by the brain but are coping with a high level of reactive oxygen species, known as a state of oxidative stress, which will change how they respond to signals. This is the reasoning behind studies, for example, of children who live in low-income neighborhoods with high exposures to traffic-related air pollution, that show increases in high-density lipoprotein cholesterol and elevated markers of oxidative stress (8-isoprostane; Zhang et al. 2022). We can remark, therefore, both on the findings themselves (about nondietary drivers of metabolic disease risk factors) and on the form: The ambient condition of high concentrations of particulate matter is not a signal that is transduced but a material condition that is metabolized, “shaping inflammatory phenotypes” characteristic of Western industrialized urban populations within the life course (McDade 2023, p. 1).
In other areas of investigation of the role of inflammation in chronic disease and health disparities, intense focus has come to rest on economically and culturally contoured features of industrialized societies such as ultraprocessed foods and detergents, whose effects on the microbiome mediate inflammatory states in the body (Akdis 2022). And studies of lipid metabolism, particularly around nonalcoholic fatty liver disease, point to the inflammatory role of free fatty acids spilling over from overfull adipose stores, a phenomenon referred to as “lipotoxicity” (Unger and Scherer 2010). Lipotoxicity is contingent on the larger metabolic milieu of the body, which is shaped by food, oxygen, and toxicant intake, as well as the microbiome (Ly et al. 2020). Food, toxicants, and microbiomes are in turn shaped by the social and built environment, including stressors, green space, parental leave policies, attitudes to hygiene, agricultural subsidies, and a whole raft of other forces (Robinson et al. 2022). Society, then, might have always been there, waiting for the signals to arrive.
4 Conclusion
In this historical analysis, I have offered up a contrast between a well-established model of society “getting under the skin” via a signal transduction model of hormone-mediated information transfer and its emerging and still rather amorphous counterpoint: an inflammatory biosocial body in which the psychological and material environment is metabolized rather than transduced. The first sees ambient conditions from adversity to pollution entering via the sensory system through a series of receptors, cascades, and gene transcription outcomes, and then becoming embedded or encoded in arterial walls, chromatin configurations, and the reactivity of response systems. Generality becomes specificity. Understanding the historical particularity of this model allows us to better see its assumptions and draw out the comparison with models that descend from, but then depart from, this body of signals and cascades.
The body of modifications emerging from a metabolic turn in the biomedical sciences has more capacity for substance. It has more channels of entry—breathing, eating, feeling—through portals that include a wide diversity of epithelial surfaces, from leaky guts to lungs, and distributes the capacity to signal across a wider range of entities, including adipose tissue, mitochondria, microbiota, and the vast complexity of immune cells. The logics of biochemical modification see the body as perpetual organized simultaneous deconstruction and reconstruction of the body–environment relation, where that relation is at any moment being sensed, represented, and acted upon in cellular contexts. It is not that signals disappear from the metabolic body; rather, they multiply. Everything signals—the cell and the brain and the body are in a vast sea of signals; the conditions under which signals are compartmentalized, prioritized, heeded, or sensed becomes the question. Inflammation is not pathology, it is process (McDade 2023).
However, just because these inflammatory conceptual configurations have the potential to change our ideas about the relations between society and biology does not mean that they necessary will; that remains to play out. This exercise of tracing the career of older signal-based models and contrasting them to in-formation metabolic–inflammatory models should allow for critical circumspection not just of past models but also a better realization of the assumptions structuring current ones. It is not new to argue between soil- and seed-style arguments about causation, or to emphasize constitution over pathogen. Yet the rise of inflammatory states as explanatory keys in both infectious and chronic illness indicates the onset of a new period in a long set of oscillations in the conceptual history of medicine identified by Georges Canguilhem between external incursions and internal conditions (Timmermann 2001; Canguilhem 1978). Nor do I wish to imply that a fashion for inflammatory markers or anti-inflammatory drugs will necessarily help with criticisms that a focus on molecular mechanisms misses the fundamental social causes of health disparities and directs intervention at the wrong causal points.
Indeed, these models at certain points overlap, and the metabolic turn is partial and ongoing, whereas the signal transduction model has been established for decades. Nevertheless, it is my hope that the work of exploring the epidemiological–molecular conjunctions of hormones and fat has allowed for the elaboration of assumptions in these different models that might otherwise remain obscure. All investigators, quantitative or qualitative, biologically or socially oriented, should have access to resources for historical insight concerning where their empirical endeavors lie in the field of practice and in the shape of thought, where their terminologies come from, and how to think carefully about the breaks and continuities presented by emerging frameworks employing new measurement techniques and ideas about outsides and insides.
References
Ahima, Rexford S., and Jeffery S. Flier. 2000. Adipose Tissue as an Endocrine Organ. Trends in Endocrinology & Metabolism 11:327–332.
Akdis, Cezmi A. 2022. The epithelial barrier hypothesis proposes a comprehensive understanding of the origins of allergic and other chronic noncommunicable diseases. Journal of Allergy and Clinical Immunology 149:41–44.
Arminjon, Mathieu. 2016. Birth of the Allostatic Model: From Cannon’s Biocracy to Critical Physiology. Journal of the History of Biology 49:397–423.
Arminjon, Mathieu. 2020. The American Roots of Social Epidemiology and its Transnational Circulation. From the African-American Hypertension Enigma to the WHO’s Recommendations. Gesnerus 77:35–63.
Badeaux, Aimee I., and Yang Shi. 2013. Emerging roles for chromatin as a signal integration and storage platform. Nature Reviews Molecular Cell Biology 14:211–224.
Beer, Gillian. 2009. Darwin’s Plots: Evolutionary Narrative in Darwin, George Eliot and Nineteenth-Century Fiction. Cambridge, UK: Cambridge University Press.
Burdziak, Cassandra, Direna Alonso-Curbelo, Thomas Walle, José Reyes, Francisco M. Barriga, Doron Haviv, Yubin Xie, Zhen Zhao, Chujun Julia Zhao, Hsuan-An Chen, Ojasvi Chaudhary, Ignas Masilionis, Zi-Ning Choo, Vianne Gao, Wei Luan, Alexandra Wuest, Yu-Jui Ho, Yuhong Wei, Daniela F. Quail, Richard Koche, Linas Mazutis, Ronan Chaligné, Tal Nawy, Scott W. Lowe and Dana Pe’er. 2023. Epigenetic plasticity cooperates with cell-cell interactions to direct pancreatic tumorigenesis. Science 380:eadd5327.
Calle, Eugenia E., Carmen Rodriguez, Kimberly Walker-Thurmond and Michael J. Thun. 2003. Overweight, Obesity, and Mortality from Cancer in a Prospectively Studied Cohort of U.S. Adults. New England Journal of Medicine 348:1625–1638.
Canguilhem, Georges. 1978. On the Normal and the Pathological. Dordrecht: D. Reidel.
Chiapperino, Luca, and Francesco Paneni. 2022. Why epigenetics is (not) a biosocial science and why that matters. Clinical Epigenetics 14:144.
Clark, Peder. 2021. ‘What else can you expect from class-ridden Britain?’: the Whitehall studies and health inequalities, 1968 to c.2010. Contemporary British History 35:235–257.
Clouston, Sean A.P., and Bruce G. Link. 2021. A Retrospective on Fundamental Cause Theory: State of the Literature and Goals for the Future. Annual Review of Sociology 47:131–156.
Cohen, Stanley, Pierluigi E. Bigazzi and Takeshi Yoshida. 1974. Similarities of T cell function in cell-mediated immunity and antibody production. Cellular Immunology 12:150–159.
Drucker, Daniel J. 2021. Diabetes, obesity, metabolism, and SARS-CoV‑2 infection: the end of the beginning. Cell Metabolism 33:479–498.
Durkheim, Émile. 1947. The Division of Labor in Society. Glencoe, IL: Free Press.
Elovainio, Marko, Jane E. Ferrie, Archana Singh-Manoux, Martin Shipley, G. David Batty, Jenny Head, Mark Hamer, Markus Jokela, Marianna Virtanen, Eric Brunner, Michael G. Marmot and Mika Kivimaki. 2011. Socioeconomic Differences in Cardiometabolic Factors: Social Causation or Health-related Selection? Evidence From the Whitehall II Cohort Study, 1991–2004. American Journal of Epidemiology 174:779–789.
Emeny, Rebecca T., David O. Carpenter and David A. Lawrence. 2021. Health disparities: Intracellular consequences of social determinants of health. Toxicology and Applied Pharmacology 416:115444.
Eyer, Joseph, and Peter Sterling. 1977. Stress-Related Mortality and Social Organization. Review of Radical Political Economics 9:1–44.
Fantuzzi, Giamila. 2016. Body Messages: The Quest for the Proteins of Cellular Communication. Cambridge, MA: Harvard University Press.
Fantuzzi, Giamila, and Raffaella Faggioni. 2000. Leptin in the regulation of immunity, inflammation, and hematopoiesis. Journal of Leukocyte Biology 68:437–446.
Fletcher, Isabel. 2014. Defining an epidemic: the body mass index in British and US obesity research 1960–2000. Sociology of Health & Illness 36:338–353.
Flier, Jeffrey S., Kathleen Sue Cook, Patricia Usher and Bruce M. Spiegelman. 1987. Severely Impaired Adipsin Expression in Genetic and Acquired Obesity. Science 237:405–408.
Foucault, Michel. 1970. The Order of Things: An Archaeology of the Human Sciences. New York: Pantheon Books.
Furman, David, Judith Campisi, Eric Verdin, Pedro Carrera-Bastos, Sasha Targ, Claudio Franceschi, Luigi Ferrucci, Derek W. Gilroy, Alessio Fasano, Gary W. Miller, Andrew H. Miller, Alberto Mantovani, Cornelia M. Weyand, Nir Barzilai, Jorg J. Goronzy, Thomas A. Rando, Rita B. Effros, Alejandro Lucia, Nicole Kleinstreuer and George M. Slavich. 2019. Chronic inflammation in the etiology of disease across the life span. Nature Medicine 25:1822–1832.
Geronimus, Arline T. 2013. Deep Integration: Letting the Epigenome Out of the Bottle Without Losing Sight of the Structural Origins of Population Health. American Journal of Public Health 103:S56–S63.
Goldblatt, Phillip B., Mary E. Moore and Albert J. Stunkard. 1965. Social Factors in Obesity. JAMA 192:1039–1044.
Green, Tiffany L., and William A. Darity. 2010. Under the Skin: Using Theories From Biology and the Social Sciences to Explore the Mechanisms Behind the Black–White Health Gap. American Journal of Public Health 100:S36–S40.
Gunderson, Ryan. 2014. Erich Fromm’s Ecological Messianism: The First Biophilia Hypothesis as Humanistic Social Theory. Humanity & Society 38:182–204.
Hancock, John T. 2017. Cell Signalling. Oxford: Oxford University Press.
Harrington, Anne. 2009. The Cure Within: A History of Mind-Body Medicine. New York: W. W. Norton & Company.
Hertzman, Clyde. 2012. Putting the concept of biological embedding in historical perspective. Proceedings of the National Academy of Sciences 109:17160–17167.
Hotamisligil, Gökhan S. 2017. Foundations of Immunometabolism and Implications for Metabolic Health and Disease. Immunity 47:406–420.
Hotamisligil, Gökhan S., Narinder S. Shargill and Bruce M. Spiegelman. 1993. Adipose Expression of Tumor Necrosis Factor-α: Direct Role in Obesity-Linked Insulin Resistance. Science 259:87–91.
Hu, Chun-Mei, Sui-Chih Tien, Ping-Kun Hsieh, Yung-Ming Jeng, Ming-Chu Chang, Yu-Ting Chang, Yi-Ju Chen, Yu-Ju Chen, Eva Y.-H.P. Lee and Wen-Hwa Lee. 2019. High Glucose Triggers Nucleotide Imbalance through O‑GlcNAcylation of Key Enzymes and Induces KRAS Mutation in Pancreatic Cells. Cell Metabolism 29:1334–1349.e10.
Hunter, Richard G., Katharine J. McCarthy, Thomas A. Milne, Donald W. Pfaff and Bruce S. McEwen. 2009. Regulation of hippocampal H3 histone methylation by acute and chronic stress. Proceedings of the National Academy of Sciences 106:20912–20917.
Kalsbeek, Andries, Susanne la Fleur und Eric Fliers. 2014. Circadian control of glucose metabolism. Molecular Metabolism 3:372–383.
Kelly, Shona, Clyde Hertzman and Mark Daniels. 1997. Searching for the biological pathways between stress and health. Annual Review of Public Health 18:437–462.
Klavdieva, Maria M. 1996. The History of Neuropeptides IV. Frontiers in Neuroendocrinology 17:247–280.
Kokosi, Theodora, Eirini Flouri and Emily Midouhas. 2021. The role of inflammation in the association between poverty and working memory in childhood. Psychoneuroendocrinology 123:105040.
Krieger, Nancy. 2011. Epidemiology and the People’s Health: Theory and Context. Oxford: Oxford University Press.
Lam, Phoebe H., Jessica J. Chiang, Edith Chen and Gregory E. Miller. 2021. Race, socioeconomic status, and low-grade inflammatory biomarkers across the lifecourse: A pooled analysis of seven studies. Psychoneuroendocrinology 123:104917.
Landecker, Hannah. 2016. The Social as Signal in the Body of Chromatin. Sociological Review Monographs 64:79–99.
Lieberman, Harris R., Sanjiv Agarwal, John A. Caldwell and Victor L. Fulgoni III. 2020. Demographics, sleep, and daily patterns of caffeine intake of shift workers in a nationally representative sample of the US adult population. Sleep 43:zsz240.
Limoges, Camille. 1994. Milne-Edwards, Darwin, Durkheim and the Division of Labour: A Case Study in Reciprocal Conceptual Exchanges between the Social and the Natural Sciences. In The Natural Sciences and the Social Sciences: Some Critical and Historical Perspectives, Boston Studies in the Philosophy of Science, ed. I. Bernard Cohen, 317–343. Dordrecht: Springer Netherlands.
Louwies, Tijs, Anthony C. Johnson, Albert Orock, Tian Yuan and Beverley Greenwood-Van Meerveld. 2020. The microbiota-gut-brain axis: An emerging role for the epigenome. Experimental Biology and Medicine 245:138–145.
Lutfey, Karen, and Jeremy Freese. 2005. Toward Some Fundamentals of Fundamental Causality: Socioeconomic Status and Health in the Routine Clinic Visit for Diabetes. American Journal of Sociology 110:1326–1372.
Ly, C. Hai, Gordon S. Lynch and James G. Ryall. 2020. A Metabolic Roadmap for Somatic Stem Cell Fate. Cell Metabolism 31:1052–1067.
Marmot, Michael. 2004. The Status Syndrome: How Social Standing Affects Our Health and Longevity. New York: Holt.
Marmot, Michael G., Geoffrey Rose, M. Shipley and P. J. S. Hamilton. 1978. Employment grade and coronary heart disease in British civil servants. Journal of Epidemiology and Community Health 32:244–249.
Martin, Chantel L., Lea Ghastine, Evans K. Lodge, Radhika Dhingra and Cavin K. Ward-Caviness. 2022. Understanding Health Inequalities Through the Lens of Social Epigenetics. Annual Review of Public Health 43:235–254.
McDade, Thomas W. 2012. Early environments and the ecology of inflammation. Proceedings of the National Academy of Sciences 109:17281–17288.
McDade, Thomas W. 2023. Three common assumptions about inflammation, aging, and health that are probably wrong. Proceedings of the National Academy of Sciences 120:e2317232120.
McDade, Thomas W., Stacy Tessler Lindau and Kristen Wroblewski. 2011. Predictors of C‑Reactive Protein in the National Social Life, Health, and Aging Project. The Journals of Gerontology: Series B 66B:129–136.
McEwen, Bruce S., and Eliot Stellar. 1993. Stress and the Individual: Mechanisms Leading to Disease. Archives of Internal Medicine 153:2093–2101.
Medzhitov, Ruslan. 2010. Inflammation 2010: New Adventures of an Old Flame. Cell 140:771–776.
Meloni, Maurizio, Simon J. Williams and Paul Martin. 2016. Biosocial Matters: Rethinking the Sociology-Biology Relations in the Twenty-First Century. 1 edition. Chichester, West Sussex, UK; Malden, MA: Wiley-Blackwell.
Merkin, Sharon Stein, Arun Karlamangla, Ana Diez Roux, Sandi Shrager, Karol Watson and Teresa Seeman. 2020. Race/ethnicity, neighborhood socioeconomic status and cardio-metabolic risk. SSM—Population Health 11:100634.
Miller, Gregory E., and Edith Chen. 2013. The Biological Residue of Childhood Poverty. Child Development Perspectives 7:67–73.
Moieni, Mona, and Naomi I. Eisenberger. 2018. Effects of inflammation on social processes and implications for health. Annals of the New York Academy of Sciences 1428:5–13.
Mold, Alex, Peder Clark, Gareth Millward and Daisy Payling. 2019. The Public and Public Health. In Placing the Public in Public Health in Post-War Britain, 1948–2012, Medicine and Biomedical Sciences in Modern History, eds. Alex Mold, Peder Clark, Gareth Millward and Daisy Payling, 7–32. Cham: Springer International Publishing.
Moore, Mary E., Albert Stunkard and Leo Srole. 1962. Obesity, Social Class, and Mental Illness. JAMA 181:962–966.
Muscatell, Keely A., Samantha N. Brosso and Kathryn L. Humphreys. 2020. Socioeconomic status and inflammation: a meta-analysis. Molecular Psychiatry 25:2189–2199.
Nathan, Carl. 2022. Nonresolving inflammation redux. Immunity 55:592–605.
Nazmi, Aydin, and Cesar G. Victora. 2007. Socioeconomic and racial/ethnic differentials of C‑reactive protein levels: a systematic review of population-based studies. BMC Public Health 7:212.
Phillips, Rob. 2020. The Molecular Switch: Signaling and Allostery. Princeton: Princeton University Press.
Picard, Martin, und Bruce S. McEwen. 2018. Psychological Stress and Mitochondria: A Conceptual Framework. Psychosomatic Medicine 80:126–140.
Picard, Martin, Bruce S. McEwen, Elissa S. Epel and Carmen Sandi. 2018. An energetic view of stress: Focus on mitochondria. Frontiers in Neuroendocrinology 49:72–85.
Prescott, Susan L., Alan C. Logan, Jamie Bristow, Ricardo Rozzi, Rob Moodie, Nicole Redvers, Tari Haahtela, Sara Warber, Blake Poland, Trevor Hancock and Brian Berman. 2022. Exiting the Anthropocene: Achieving personal and planetary health in the 21st century. Allergy 77:3498–3512.
Reynolds, Andrew S. 2018. The Third Lens: Metaphor and the Creation of Modern Cell Biology. Chicago: The University of Chicago Press.
Rheinberger, Hans-Jörg. 2022. Postscriptum. Berichte Zur Wissenschaftsgeschichte 45:517–523.
Rimm, Ilonna J., and Alfred A. Rimm. 1974. Association between socioeconomic status and obesity in 59,556 women. Preventive Medicine 3:543–572.
Rioch, David. 1971. Transition states as stress. Society, stress, and disease 1:85–90.
Roberts, Elizabeth F. S. 2021. Commentary: Causal Enclosures—Over and Over. Medical Anthropology Quarterly 35:547–552.
Robinson, Jake M., Nicole Redvers, Araceli Camargo, Christina A. Bosch, Martin F. Breed, Lisa A. Brenner, Megan A. Carney, Ashvini Chauhan, Mauna Dasari, Leslie G. Dietz, Michael Friedman, Laura Grieneisen, Andrew J. Hoisington, Patrick F. Horve, Ally Hunter, Sierra Jech, Anna Jorgensen, Christopher A. Lowry, Ioana Man, Gwynne Mhuireach, Edauri Navarro-Pérez, Euan G. Ritchie, Justin D. Stewart, Harry Watkins, Philip Weinstein and Suzanne L. Ishaq. 2022. Twenty Important Research Questions in Microbial Exposure and Social Equity. mSystems 7:e01240-21.
Rose, Nikolas, and Des Fitzgerald. 2022. The Urban Brain: Mental Health in the Vital City. Princeton: Princeton University Press.
Sapolsky, Robert M., Lewis C. Krey and Bruce S. McEwen. 1986. The neuroendocrinology of stress and aging: the glucocorticoid cascade hypothesis. Endocrine Reviews 7:284–301.
Schmidt, Alfred. 2014. The Concept of Nature in Marx. London: Verso Books.
Schulte, Paul A., and Frederica P. Perera. 2012. Molecular Epidemiology: Principles and Practices. London, Oxford, Boston, New York and San Diego: Academic Press.
Selye, Hans. 1954. The Physiology and Pathology of Exposure to Stress; a Treatise Based on the Concepts of the General-adaptation-syndrome and the Diseases of Adaptation: Annual report on stress. Montreal: Acta.
Serviant-Fine, Thibaut, Mathieu Arminjon, Yohan Fayet and Élodie Giroux. 2023. Allostatic load: historical origins, promises and costs of a recent biosocial approach. BioSocieties 1–25.
Shi, Huiqing, Lizanne J. S. Schweren, Rob ter Horst, Mirjam Bloemendaal, Daan van Rooij, Alejandro Arias Vasquez, Catharina A. Hartman and Jan K. Buitelaarl. 2022. Low-grade inflammation as mediator between diet and behavioral disinhibition: A UK Biobank study. Brain, Behavior, and Immunity 106:100–110.
Shove, Elizabeth, and Nicola Spurling. 2013. Sustainable Practices: Social Theory and Climate Change. New York: Routledge.
Siiteri, Pentti K. 1987. Adipose tissue as a source of hormones. The American Journal of Clinical Nutrition 45:277–282.
Slavich, George M., and Michael R. Irwin. 2014. From Stress to Inflammation and Major Depressive Disorder: A Social Signal Transduction Theory of Depression. Psychological bulletin 140:774–815.
Slavich, George M., and Julia Sacher. 2019. Stress, sex hormones, inflammation, and major depressive disorder: Extending Social Signal Transduction Theory of Depression to account for sex differences in mood disorders. Psychopharmacology 236:3063–3079.
Sprenger, Florian, Erik Born and Matthew Stoltz. 2023. Surrounding and Surrounded: Toward a Conceptual History of Environment. Critical Inquiry 49:406–427.
Starling, Ernest Henry. 1907. The chemical control of the body. Harvey Lectures 1908:115–131.
Taylor, Shelley E., Rena L. Repetti and Teresa Seeman. 1997. HEALTH PSYCHOLOGY: What is an Unhealthy Environment and How Does It Get Under the Skin? Annual Review of Psychology 48:411–447.
Timmermann, Carsten. 2001. Constitutional Medicine, Neoromanticism, and the Politics of Antimechanism in Interwar Germany. Bulletin of the History of Medicine 75:717–739.
Tissiéres, Alfred, Herschel K. Mitchell and Ursula M. Tracy. 1974. Protein synthesis in salivary glands of Drosophila melanogaster: Relation to chromosome puffs. Journal of Molecular Biology 84:389–398.
Tomkins, Gordon M., David W. Martin, Jr., Robert H. Stellwagen, John D. Baxter, Pierre Mamont and Barbara B. Levinson. 1970. Regulation of Specific Protein Synthesis in Eucaryotic Cells. Cold Spring Harbor Symposia on Quantitative Biology 35:635–640.
Unger, Roger H., and Philipp E. Scherer. 2010. Gluttony, sloth and the metabolic syndrome: a roadmap to lipotoxicity. Trends in Endocrinology & Metabolism 21:345–352.
Viner, Russell. 1999. Putting Stress in Life: Hans Selye and the Making of Stress Theory. Social Studies of Science 29:391–410.
Weiner, Herbert. 1992. Perturbing the Organism: The Biology of Stressful Experience. Chicago: The University of Chicago Press.
Weiss, Daniel, Erik R. Sund, Jeremy Freese and Steinar Krokstad. 2020. The diffusion of innovative diabetes technologies as a fundamental cause of social inequalities in health. The Nord-Trøndelag Health Study, Norway. Sociology of Health & Illness 42:1548–1565.
Wu, Fen, Yu Chen, Ana Navas-Acien, Michela L. Garabedian, Jane Coates and Jonathan D. Newman. 2021. Arsenic Exposure, Arsenic Metabolism, and Glycemia: Results from a Clinical Population in New York City. International Journal of Environmental Research and Public Health 18:3749.
Yang, Bo-Yi, Shujun Fan, Elisabeth Thiering, Jochen Seissler, Dennis Nowak, Guang-Hui Dong and Joachim Heinrich. 2020. Ambient air pollution and diabetes: A systematic review and meta-analysis. Environmental Research 180:108817.
Zhang, Amy L., John R. Balmes, Liza Lutzker, Jennifer K. Mann, Helene G. Margolis, Tim Tyner, Nina Holland, Elizabeth M. Noth, Fred Lurmann, S. Katharine Hammond and Stephanie M. Holm. 2022. Traffic-related air pollution, biomarkers of metabolic dysfunction, oxidative stress, and CC16 in children. Journal of Exposure Science & Environmental Epidemiology 32:530–537.
Acknowledgements
Thanks to Aaron Panofsky, Stefan Timmermans, Robbin Jeffries Hein, and Lieba Faier for their generous reading of earlier iterations of the manuscript. The author gratefully acknowledges the support and intellectual community of the Canadian Institute for Advanced Research Future of Flourishing Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Landecker has no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Landecker, H. How the Social Gets Under the Skin: From the Social as Signal to Society as a Metabolic Milieu. Köln Z Soziol (2024). https://doi.org/10.1007/s11577-024-00951-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11577-024-00951-5