Abstract
Background
The formation of chronic wounds accounts for considerable costs in health care systems. Despite the several benefits of decellularized small intestinal submucosa (SIS) as an appropriate scaffold for different tissue regeneration, it has shortcomings such as lack of antibacterial features and inappropriate mechanical properties for skin tissue regeneration. We aimed to examine the efficacy and safety of decellularized SIS scaffold enhanced with cellulose acetate (CA) and silver (Ag) nanoparticles (NPs) for healing full-thickness wounds.
Methods and Results
The scaffolds were prepared by decellularizing bovine SIS and electrospinning CA/Ag nanoparticles and characterized using a transmission electron microscope (TEM), scanning electron microscope (SEM), tensile testing, and X-ray diffraction. In vivo evaluations were performed using full-thickness excisions covered with sterile gauze as the control group, SIS, SIS/CA, and SIS/CA/Ag scaffolds on the dorsum of twenty male Wistar rats divided into four groups randomly with 21-days follow-up. All in vivo specimens underwent Masson's trichrome (MT) staining for evaluation of collagen deposition, transforming growth factor-β (TGF-β) immunohistochemistry (IHC), and Haematoxylin Eosin (H&E) staining. The IHC and MT data were analyzed with the ImageJ tool by measuring the stained area. The TEM results revealed that Ag nanoparticles are successfully incorporated into CA nanofibers. Assessment of scaffolds hydrophilicity demonstrated that the contact angle of SIS/CA/Ag scaffold was the lowest. The in vivo results indicated that the SIS/CA/Ag scaffold had the most significant wound closure. H&E staining of the in vivo specimens showed the formation of epidermal layers in the SIS/CA/Ag group on day 21. The percentage of the stained area of MT and TGF-β IHC staining’s was highest in the SIS/CA/Ag group.
Conclusion
The decellularized SIS/CA/Ag scaffolds provided the most significant wound closure compared to other groups and caused the formation of epidermal layers and skin appendages. Additionally, the collagen deposition and expression of TGF-β increased significantly in SIS/CA/Ag group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The skin is the human body's biggest organ. It provides a barrier against viral and bacterial infection and is responsible for various activities, including protection from external assaults, fluid homeostasis, sensory detection, and self-healing [1, 2]. However, burns and chronic wounds cause extreme agony, rapid and hazardous water loss, and bacterial infection; Patients' quality of life is significantly lowered by chronic wounds and burns, connected with increased physical discomfort and socioeconomic difficulties [3]. As a result, cutaneous wounds, massive and full-thickness wounds, can have devastating consequences for humanity. In the world, full-thickness skin wounds represent a substantial clinical burden. Millions of people suffer from burn injuries worldwide [4]. Besides, Deep and persistent wounds, particularly in diabetic patients, have long been regarded as one of the most pressing medical concerns.
In recent years, skin tissue engineering has been considered an advanced therapeutic approach for wound healing applications through the design and fabrication of scaffolds and wound dressings [5, 6]. Developing wound dressings for deep wounds needs to address three main limitations; biocompatibility, mechanical strength, and antibacterial properties [7]. Implementing nanofabrication techniques with decellularization methods in the scaffold synthesis process can assist in reaching such aims [8, 9].
A variety of studies have implemented decellularized tissues such as amniotic membrane, small intestine submucosal (SIS), and chorionic membrane for wound healing application [10, 11]. Decellularized scaffolds have been used for tissue engineering, particularly wound healing, in several investigations [12]. Decellularized SIS can be used as a scaffold to help rebuild different tissues because of its good biocompatibility, rich extracellular matrix (ECM) proteins, and good mechanical properties [13, 14]. In addition, the low immunogenicity of decellularized SIS is considered a significant advantage that does not elicit immune-mediated inflammatory responses when transplanted [15]. Natural ECM in decellularized SIS offers substantial benefits such as high bioactivity, high histocompatibility, and low immunogenicity. SIS contains many growth factors well-known for their function in wound healing and tissue regeneration. In other words, decellularized SIS can behave as a wound dressing by providing a suitable surface for cell adhesion, differentiation, proliferation, and migration. Furthermore, by increasing angiogenesis and improving wound healing rate, SIS-based regeneration techniques can overcome the difficulties associated with skin damage repair, either alone or in combination with stem cells [16]. Wang et al. developed a one-step and straightforward decellularized SIS bilayer wound dressing technique. The top layer may prevent bacterial infection and offer a moist environment conducive to wound healing, while the cryogel layer may stimulate cell growth. They used crosslinking at a freezing temperature to create a novel SIS-based material with a two-layer structure. The proposed decellularized SIS bilayer material comprises a standard SIS membrane and a new SIS cryogel, which has excellent mechanical characteristics, exceptional biocompatibility, acceptable water vapor transmission rate, appropriate anti-infective behavior, cell adhesion, and proliferation. The SIS bilayer might be used to treat wounds [17]. Despite the unique properties of decellularized SIS mentioned above, these platforms lonely cannot fulfill all our desirable properties, including antibacterial capabilities and mechanical properties for healing deep wounds. Nanofabrication techniques such as electrospinning and incorporating antibacterial nanoparticles can assist in addressing these limitations.
Among the numerous biocompatible polymers that may be used to make electrospun nanofibers, cellulose acetate has several benefits, including its renewed capacity, affordability, and simplicity of mass manufacturing. It is also quite soluble in organic solvents, making it an excellent material for electrospinning. Biocompatible, biodegradable, nonirritating, and nontoxic cellulose acetate is good. This polymer has been widely investigated and utilized for wound dressings, dermal replacements, and synthetic skin tissues for effective wound healing due to its outstanding mechanical characteristics, strong affinity with other substances, and regenerative capabilities [18, 19]. Cellulose acetate is a naturally occurring polymer with superior biocompatibility, cellular mimicry, and hydrophilic characteristics than its proportional counterpart [20, 21]. A variety of studies used cellulose acetate-based biomaterials for healing applications. For instance, Sofi et al. developed a nanofibrous cellulose scaffold enriched with hydroxyapatite (HAp) and utilizing silver (Ag) nanoparticles (NPs) that enhanced proliferation and antibacterial characteristics for wound healing and bone tissue regeneration [20]. Esmaeili et al. developed porous antibacterial hybrid nanofibrous scaffolds by incorporating graphene oxide/Ag nanocomposites and curcumin into polyurethane and cellulose acetate using the electrospinning technique. Adding these materials to the structure of scaffolds reduced fiber diameter and increased antibacterial characteristics on direct contact with microbial cells (Pseudomonas and S. aureus) bacteria. The in vivo histopathology investigations revealed that the inclusion of these nanostructures can significantly improve wound healing and epidermal layer regeneration [22].
Antibacterial nanoparticles play a crucial role in controlling infection in wound dressings [23, 24]. Silver nanoparticles (Ag NPs) have attracted much attention because of their comprehensive inhibitory action against various bacteria, particularly antibiotic-resistant bacteria [25,26,27]. Ag NPs, in particular, appear to adhere to the membrane surface of microbial cells, altering the lipid bilayer and increasing membrane permeability; additionally, Ag + ions released by Ag oxidation appear to penetrate cells and precisely interact with respiratory chain enzymes, nucleic acids, and cytoplasmic components, modulating intracellular signal transduction pathways [28, 29].
In this study, we developed a bilayer decellularized SIS-based scaffold. First, the SIS was decellularized using the enzymatic method and was characterized. On the next step, cellulose acetate polymer and Ag NPs solution were electrospun on the surface of decellularized SIS. Then the mechanical and morphological properties of the hybrid scaffold and its biocompatibility were investigated. Finally, the scaffolds were transplanted to the wound area, after being cut to the desirable size. To assess the wound healing process, samples were collected during 21 days from the wound site, and immunohistochemistry and pathology tests were conducted on each sample.
Materials and methods
Scaffold preparation
Decellularization of SIS
SIS is immersed in a 50 mL ethanol 70% (Merck) and 50 mL chloroform (Merck, Germany) solution, and the mixture is stirred for 12 h. After that, it is washed with normal saline serum, and trypsin (0.05%, Thermo Fisher Scientific Corporation) is added to the solution and incubated for 12 h at 37 °C. After incubation, it is washed with normal saline three times with PBS, and then sodium dodecyl sulfate (SDS, 0.05%, Thermo Scientific™) is added to the solution, and the mixture is shaken for 6 h. In the end, it is washed with normal saline serum for 45 min, three times [30, 31].
Assessment of decellularization
After being fixed in 10% neutral buffered formalin, SIS samples were embedded in paraffin. To determine the existence of any remnant nuclei inside the SIS samples, sections were cut and stained with 40, 6-diamidino-2-phenylindole (DAPI). Each group had three samples. To quantify DNA, at 50 °C for 24 h, 100 mg of SIS powder was digested using proteinase K digestion buffer [100 mM NaCl, 10 mM Tris–HCl (pH 8), 25 mM EDTA (pH 8), 0.5 percent SDS, 0.1 mg/mL proteinase K]. Twice, 25:24:1 (v/v/v) phenol/chloroform/isoamyl alcohol. At -20 °C, DNA was precipitated from the aqueous phase by adding 2 volumes of ethanol and 0.1 volume of 3 M sodium acetate (pH 5.2). The precipitated DNA was then centrifuged at 10,000×g for 10 min before being resuspended in 1 mL of TE buffer (pH 8) and 1 mM EDTA [32].
Electrospinning CA/Ag nanoparticles on SIS
In a semi-industrial electrospinning setup, decellularized SIS and decellularized SIS/CA/Ag nanofibrous were electrospun. At a concentration of 10% w/v, SIS was dissolved in dimethylformamide (DMF, 25 percent v/v, Sigma Aldrich) and tetrahydrofuran (THF, 75 percent v/v, Sigma Aldrich). The mixture was stirred for 12 h until it was completely homogeneous. Following that, CA/Ag suspension was then loaded into a disposable syringe for electrospinning on the surface of decellularized SIS fixed on the drum’s surface. Due to the excellent solubility of NPS in THF/DMF, the corresponding solution remained stable during the electrospinning process, and there was no sedimentation of nanocomposites in the syringe. Electrospinning was performed for 8 h on a drum coated in aluminum foil, rotating at 350 rpm (applied voltage of 18 kV, flow rate of 0.3 mL/h, working distance of 17 cm). Additionally, SIS was dissolved in DMF/THF solvents for electrospinning under the same circumstances as the pristine SIS electrospun membrane.
Characterization of the scaffold
TEM
The integration of Ag Nps into integrated into nanofibers was examined using a transmission electron microscope (TEM). A TEM device (Philips CM‐30 TEM operating at a voltage of 250 kV) was utilized for this purpose. The TEM specimens were produced by electrospinning CA-Ag solution on carbon-coated copper grids linked to the drum for 3 min under the same electrospinning circumstances.
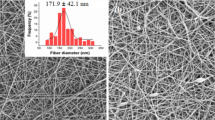
SEM
The morphology of electrospun scaffolds was characterized by SEM. After being coated with gold for 180 s with a sputter coater (SC7620, Quorum Technologies, England) at a 20-kV accelerating voltage, the fibers were analyzed with a scanning electron microscope (SEM, AIS2100, Seron Technology, South Korea). Using a computed image analyzer (ImageJ), the average diameter of the nanofibers was calculated statistically by measuring 20 different points at random. The diameters were given as an average with a standard deviation.
Mechanical properties
The SANTAM universal tensile testing device (Iran, SPM20) was used to evaluate the mechanical properties of fabricated scaffolds. At room temperature, single sheets of each scaffold were punched into three samples (10 mm 20 mm) and tested with a 1 mm/min loading velocity. Each scaffold's stress–strain curve was recorded, and stress, strain, and Young's modulus (E) were computed.
Water contact angle
The contact angle was measured on the SIS, SIS/CA, and SIS/CA/Ag sheet to evaluate the effect of incorporated CA–Ag nanocomposite into the SIS scaffold and investigate hydrophobicity. A G10 Kruss contact angle goniometer was used to measure the contact angle, which was written as follows: A syringe was used to deposit 10 µL of deionized water droplets on the surface of scaffolds, and the drop shape was recorded using a USB microscope. ImageJ's Drop Snake plugin was used to calculate the angle. Each substrate was subjected to three measurements.
XRD
X-ray diffraction (XRD) was performed on the CA–Ag powder. Cu Kα radiation with a wavelength of 0.154 nm was used to generate the XRD patterns using a X'Pert PRO MPD instrument that is from the PANalytical company.
Swelling and degradation studies
In order to study the swelling of the scaffolds, the samples were weighed, and the dry weight of the samples were recorded. At room temperature and pH 7.4, the scaffolds were immersed in phosphate buffer saline in different time intervals. After removing the scaffolds from the solution, they were weighed immediately, and the wet weight of the samples were recorded. The experiment was carried out until no further weight changes could be absorbed. The degree of swelling was calculated using the following formula:
For degradation test, the scaffolds were weighed and sterilized, and they were soaked in PBS. The scaffolds were placed in incubator at 37 °C and at different time intervals, they were removed, lyophilized, and weighed. The weight loss was calculated using the following formula:
Antibacterial activity assessment
A refined AATCC-100 test method was used to determine the level of bacterial diminution. For this purpose the samples were cut into 1 cm2 mats and after adding 100 μL sterile nutritive solution with bacterial suspensions (E. coli ATCC25922 and S. aureus ATCC29212) that had 1.5 × 108 colony-forming units on the mat, another mat was placed on top of it. The mats and suspension were shaken after a 24-h period at 37 °C, and 0.1 mL of each specimen was seeded on Muller Hinton agar medium. After 24 h at 37 °C, colonies were quantified.
In vitro studies
MTT assay
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-2H-tetrazolium bromide (MTT) assay was used to assess the viability of L929 murine fibroblast cells seeded onto scaffolds at 1, 3, and 7 days following cell seeding. L929 fibroblast cells were cultivated in Dulbecco’s Modified Eagle Medium (DMEM). The medium consisted of 10% v/v Fetal Bovine Serum (FBS) and 1% v/v pen-strep (containing 100 U/mL Penicillin and 100 μg/ml Streptomycin). The culture medium was incubated at 37 °C in an environment with 5% CO2. Sterilized scaffolds were sectioned and placed in 48-well cell culture plates. Afterward, the cell solution with 10,000 per 1 cm2 fibroblasts was used to culture on each scaffolds. The scaffolds incubated in culture media and refreshed every 3 or 4 days. For 3.5 h at 37 °C, the samples were incubated in a serum-free medium and MTT reagent combination. After dissolving with dimethyl sulfoxide, the absorbance of the formed formazan crystals was measured at 570 nm (DMSO; Merck). MTT assays were used to assess the viability of cells seeded onto scaffolds at 1, 3, and 7 days following cell seeding. For 3.5 h at 37 °C, the samples were incubated in a serum-free medium and MTT reagent combination. After dissolving with dimethyl sulfoxide, the absorbance of the formed formazan crystals was measured at 570 nm (DMSO; Merck). The cell viability was measured using following formula:
In vivo studies
Sampling, animal wound models, surgery, and ethics
The wound-healing effect of scaffolds was examined using a male rat model. The Research Ethics Committees of Laboratory Animals at Tehran University of Medical Sciences (TUMS) approved the animal study (approval number: IR.TUMS.AEC.1401.083). Additionally, all steps comply with the "Guide for the Care and Use of Laboratory Animals” (NIH publication No. 85-23, revised 1996). Twenty healthy adult male Wistar rats (200 g) of 2 months of age were provided from Experimental Medicine Research Center, Tehran Heart Center and kept in polypropylene rat cages (435 × 290 × 150 mm) with the light cycle of 14-h light and 10-h darkness and accessibility to adequate lab chow and water. Rats were maintained at room temperature with suitable humidity. The animals were randomly divided into four groups, with five samples in each group. The rats were anesthetized by intraperitoneal injection of the mixture of ketamine hydrochloride (Gedeon Richter Ltd, Budapest, Hungary; 86 mg/kg) and xylazine (Bayer, Leverkusen, Germany; 13 mg/kg). The dorsum hair of the rats was shaved following the general anesthesia. Afterward, a full-thickness round shape 2.00 × 1.50 cm2 excision was covered by as-prepared scaffolds on the back skin of rats near the posterior side of the neck. Then, each group was treated with Small Intestinal Submucosal (SIS), SIS/Cellulose Acetate (CA), SIS/CA/Ag, and sterile gauze as the control intervention. The excisions were sampled at the day 21 post-surgery and were photographed at the 10 and 21 post-surgery by a digital camera (Canon Inc., Tokyo, Japan) to evaluate the efficacy of scaffolds. For histopathological evaluations, the specimens were fixed in a 10% formaldehyde solution and embedded in paraffin immediately after the sampling. Then, paraffin-blocked specimens were sliced into 5 µm thick samples with a Leica 2135 microtome (Deerfield, IL, USA) for Hematoxylin and Eosin (H&E) and immunohistochemistry (IHC) assays. To analyze the histological properties of the treatment, the skin, including the entire wound covered by scaffolds and normal adjacent sin, was excised and fixed in 5% paraformaldehyde in PBS. The wound closure was assessed by Wilson's formula as follows:
Scaffold transplantation
Scaffolds were cut into desirable sized and sterilized using O3 plasma (low temperature Hydrogen Peroxide Plasma Sterilizer, Standard Sterilization Time: 45 min, Sterilization temperature: 50 ± 5 °C, Sterilizing Agent:60% H2O2, MEDFUTURE China). The scaffolds were fixed at the wound sites using four simple sutures on 0, 3, 6, and 12 o’clock borders by 4–0 silk and 4–0 nylon sutures (Ethicon, Norderstedt, Germany).
Immunohistochemistry Assay
H&E staining technique was used for the histopathological assessment using the following protocol by a single, blinded pathologist. Samples were deparaffinized at 70 °C for 20 min, and then the pathologist performed xylene solution for 3 min. Afterward, specimens were rehydrated in two changes of absolute ethanol (5 min each). After that, samples were dipped into hematoxyline solution (15 min) and then were washed with tap water for 5 min to stain the nuclei. After that, slides were agitated in 0.2% ammonia water and rinsed with tap water for 5 min. Samples were counterstained with eosinophloxine for 1 min, and later, they were rinsed in 90%,96%, and 100% ethanol for 2 min. Subsequently, samples were embedded in xylene, and one or two drops of mounting medium were added to slides. Then, samples were covered with a coverslip and assessed with an optical microscope (resolution: 40 ×) to record skin tissue regeneration. To measure the blood vessels density, we counted the number of mature vessels containing red blood cells in 4 randomized areas (magnification 40 ×) and the mean of number of vessels was calculated.
In this study, the expression of TGF—β was assessed using immunohistochemistry (IHC) techniques. For this purpose, specimens were collected and washed with PBS four times at 5 min intervals. For antigen retrieval, samples were put in 2 ordinary hydrochloric acid (HCL) solutions for 30 min. Afterward, Borate buffer was added to the samples to neutralize the acidic effect of HCL. Then, specimens were washed with PBS, and a 3% (v/v) Triton X-100 solution was used for 30 min to enhance cell membranes' permeability. Then, PBS was applied for washing samples. Subsequently, goat serum 10% (v/v) was added to samples and left for 30 min to block the secondary antibody reaction. Afterwards, a primary antibody diluted 1:100 in PBS was added to samples and then kept at 2–8 °C temperature for one day. After that, a secondary antibody diluted 1:150 was added to the samples, and the mixture was incubated for an hour and a half at 37 °C temperature. After that, 4′,6-diamidino-2-phenylindole (DAPI) were added in a dark room, and PBS was poured over the samples promptly. Afterward, samples were divided into five areas for cell calculation by an Olympus Fluorescent microscope (× 400), then images were captured from each section and analyzed using the ImageJ software (Fiji version). The percentage of positive immunolabeled cells to total cells ratio is provided as the result of these proceedings.
Statistical analysis
The IBM ® SPSS® 26 software program was used to conduct the statistical analysis. The results were analyzed using one-way ANOVA, followed by the Tukey’s post hoc test. The data are provided as means ± standard deviation(SD), and the statistical significance was determined as P-value < 0.05.
Results
TEM
TEM was used to examine the morphology of Ag NPs and their incorporation into CA nanofibers. As shown in Fig. 1d, spherical Ag NPs are successfully incorporated into CA nanofibers with an average size of 20 ± 2.67 nm. The figures indicate the nanofibrous structure of CA on the SIS sheet and incorporation of Ag NPs into CA nanofibers (Fig. 1d–f).
SEM
SEM was used to confirm the fibrous networks of two scaffold types after fabrication, including SIS/CA and SIS/CA/Ag. Figure 1 shows that the fiber diameters of SIS/CA and SIS/CA/Ag are 608 ± 13 nm and 499 ± 11 nm, respectively. The inclusion of Ag nanoparticles into SIS/CA resulted in a decrease in the diameter of nanofibers, as illustrated in Fig. 1a–c.
XRD spectroscopy
The XRD patterns of Ag nanoparticles synthesized in the 2 range from 30° to 90° are shown in Fig. 1. This result is compatible with the values for a face-centered cubic (FCC) crystal structure of Ag. The (111), (200), (220), (311), and (222) crystallographic planes of face-centered cubic Ag crystals may be ascribed to XRD peaks at 38.18°, 44.25°, 64.72°, 77.40°, and 81.6°, respectively. The acquired XRD spectrum revealed that the produced silver nanoparticles were in nanocrystal form and crystalline in nature when compared to the standard. Roy et al. [33] found the same thing, indicating that silver nanoparticles are face-centered, cubic, and crystalline in nature. In the XRD patterns, the primary crystalline phase was Ag, and no other phases were visible as impurities. As a result, the Debye–Scherrer equation may be used to calculate Ag-Nps average particle size:
where \(n\) is average crystallite size and \(\beta\) is line broadening in radians (full width at half maximum of the peak in radians). \(\lambda\) is the wavelength of X-ray, and \(k\) is Bragg's angle. \(k\) is constant (geometric factor = 0.94). The crystallite size of Ag nanoparticles determined by XRD analysis (using Scherrer's equation [34] and (111) as the most intense plane) was 7 nm, which was somewhat smaller than the SEM result but like the TEM result. For smaller nanoparticles, the crystallite size was very similar to the comparable TEM-derived particle size (15 nm). This confirmed our suspicions that the smallest nanoparticles were mostly monocrystalline. The rapid synthesis approach made it simple to make uniform Ag nanoparticles.
Tensile
A tensile analysis was used to measure the mechanical properties of the nanofibrous scaffolds as shown in Fig. 2. The mechanical strength of SIS, SIS/CA, and SIS/CA/Ag following Yield testing measured as 0.036 ± 0.008, 0.202 ± 0.007, and 0.2190 ± 0.046, respectively. Following the ultimate strength testing the strength of measured scaffolds were measured as 0.222 ± 0.053, 3.407 ± 0.072, and 3.856 ± 0.081 respectively. Furthermore, by Young’s modulus evaluation, the strength of mentioned scaffolds was measured as 0.517 ± 0.10, 0.714 ± 0.015, and 1.390 ± 0.337 respectively. The ANOVA analysis followed by Tukey’s posy-hoc demonstrated that the difference between all the groups in different assessment were statically significant (P-value ≤ 0.001).
Hydrophilicity
The contact angle measures the hydrophobicity of a scaffold's surface, which represents the substrate's wettability and plays a vital role in cell attachment and fate. By incorporating CA/Ag into SIS, the hydrophobicity of the scaffold was altered. The contact angle of SIS was initially estimated to be 103° ± 8° ° at zero time, but in the SIS/CA and SIS/CA/Ag samples, it was reduced to 100° ± 2° and 80° ± 4°, respectively. Furthermore, when the contact angles of SIS/CA and SIS/CA/Ag samples are compared to SIS, the contact angles of SIS/CA and SIS/CA/Ag samples are significantly reduced when the time is increased to 20 s, indicating enhanced hydrophilicity due to the addition of nanocomposite (Fig. 3).
DAPI staining and remnant DNA contents
The impact of tissue decellularization was detected using DAPI staining. In SIS samples, there were no apparent blue-dye intact nuclei. The concentration of residual DNA in the SIS samples was used to calculate the amount of cellular material that remained. SIS samples contained concentrations of DNA with 1.4 ± 0.11 ng dsDNA/mg dry weight (Fig. 4a, b).
MTT assay
The MTT colorimetric test was utilized to assess the proliferation and viability of cells on electrospun SIS, SIS/CA, and SIS/CA/Ag scaffolds. Results showed a rising trend in optical density, indicating increased cell viability due to increased metabolism and proliferation of cells on the scaffolds. The findings further show that SIS, SIS/CA, and SIS/CA/Ag scaffolds had no cytotoxic impact on cells after 1, 3, and 7 days of in vitro growth (Fig. 4c).
Degradation and swelling results
The degradation results of SIS are presented in Fig. 5a which show that in the first 7 days there was only 2 ± 0.41% weight loss and the SIS started to degrade slowly in the PBS. After 35 days, SIS lost 23 ± 0.98% of its weight and the rate of weight loss slightly increased after 35 days and in the end of the 70 days period the SIS had 76 ± 4.27% weight loss. The swelling results of SIS which are presented in Fig. 5b indicate that after the first 50 h, the swelling degree reach 240 ± 7.51% and in the next 150 h, it didn’t have a significant change. After 150 h, the swelling degree reached 285 ± 6.52% and it reached a swelling equilibrium which shows the SIS sample didn’t swell more. Based on the swelling results and the water contact angle results, it is observed that the SIS sample had low hydrophilicity and CA was added to improve the hydrophilicity of the sample and quickly absorb the exudates of the wound site. There were three replicates for both degradation and swelling test.
Antibacterial activity assessment
As demonstrated in Fig. 6, following antibacterial assessments, the decellularized SIS and the decellularized SIS/CA do not exhibit any inhibition zone against S. aureus and E. coli. The decellularized SIS/CA/Ag samples exhibited the inhibition zone against S. aureus and E. coli and the dimeters of inhibition zone were measured as 2.9 cm and 2.6 cm respectively.
In vivo results
Macroscopic images
Figure 7 demonstrates the healing effect of Decellularized SIS, SIS/CA, and SIS/CA/Ag as the wound dressings and the control group. Based on the results, SIS/CA/Ag accelerated wound closure during 21 days of follow-up. On day 10 post surgery, the wound closure of control, SIS, SIS/CA, and SIS/CA/Ag groups were 34.80% ± 1.79%, 42.55% ± 2.31%, 51.14% ± 3.45%, and 58.99% ± 2.65%, respectively. On day 21, complete wound closure was seen in all animals in SIS/CA/Ag group. The wound closure of control, SIS, and SIS/CA groups were 57.20% ± 5.07%, 71.40% ± 3.85%, and 89.60% ± 2.92, respectively. The ANOVA followed by Tukey post hoc tests demonstrated statistical significance between all the groups on day 10 and 21 post-surgery (P-value ≤ 0.001 for all comparisons).
a macroscopic appearances of intervention and control groups wounds at day 0, 10, and 21 day post-surgery. b Histogram on days 10 and 21 post-surgery. SIS/CA/Ag scaffolds accelerated healing and caused complete wound closure within 21 days. Values represent mean ± SD. SD standard deviation. * P-value ≤ 0.001. SIS small intestine submucosa, CA cellulose acetate
Microscopic pathologic images (Trichrome (TC), hematoxylin and eosin (H&E), immunohistochemistry(IHC))
Histopathological evaluation of the control group revealed a considerable difference between the thickness of granulation tissue compared to other groups on day 21. In detail, the granulation tissue can be found clearly in the histopathological specimen of the control and SIS group. The thickness of granulation tissue in the control and SIS groups were 93.66 µm ± 22.24 µm and 39.90 µm ± 10.70 µm respectively (P-value ≤ 0.001), and initiation of epidermal formation is evident in the SIS group. In the other groups, consisting of SIS/CA and SIS/CA/Ag groups, epidermal layer formation has been shown. In the SIS/CA and SIS/CA/Ag group, the specimen revealed the complete formation of epidermal tissue; however, skin appendages were absent in histological evaluations. The density of blood vessels in control, SIS, SIS/CA, and SIS/CA/Ag groups were 1.70 ± 0.51, 3.80 ± 0.64, 5.35 ± 0.37, and 6.90 ± 0.51 respectively. Following one-way ANOVA analysis, it was revealed that the difference between the groups were significant statistically (P-value ≤ 0.001) and Tukey’s post-hoc revealed that the difference between all the groups are significant statistically (P-value ≤ 0.001 for all the groups compared to each other). Despite the significance difference between intervention groups regarding blood vessels density, epidermal layer formation, and granulation tissue thickness, there is not any significant difference between intervention group regarding inflammatory cells infiltration (Figs. 8 and 9).
H&E, Masson’s Trichrome, and TGF-β IHC stained microscopic sections of healed incisions at day 21 post-surgery(X40). The H&E staining at day 21 the granulation tissue can be seen in the control and SIS group. The thickness of granulation tissue in the SIS group is lesser than the control group and initiation of epidermal formation is evident in this group. In the SIS/CA and SIS/CA/Ag groups, the specimens revealed the complete formation of epidermal tissue. Masson’s trihrome stained microscopic samples of healed wounds demonstrated higher rate of collagen deposition in SIS/CA/Ag group, TGF-β IHC stained microscopic samples of healed wounds represented expression of TGF-β in SIS/CA/Ag group more than the others groups. The percentage of stained area among the different groups was calculated using the ImageJ softwareScale bar:100 µm and 0.1 mm. SIS small intestine submucosa, CA cellulose acetate, H&E hematoxylin and eosin, TC trichrome, IHC immunohistochemistry, TGF-β tumor growth factor β
One-way ANOVA analysis of MT staining revealed statistical significance between the intervention and control groups (P-value = 0.002). Following the Tukey' post hoc test, it was demonstrated that, however; collagen deposition in the SIS, SIS/CA, and SIS/CA/Ag was higher than control groups (P-value = 0.037, P-value = 0.016, and P-value = 0.002 respectively), there was no statistical significance between the scaffold groups.
TGF-β is the prototypic driver of myofibroblasts infiltration, excessive ECM synthesis, and an ECM degradation inhibitor, leading to fibrosis formation (1). Based on the crucial role of TGFβ in scar formation and wound healing, we performed immunohistochemistry staining on the tissues to evaluate the TGF-β levels in different treatment groups. The ANOVA analysis of the TGF-β stained area demonstrated that there was statistical significance between the groups (P-value = 0.025). The Tukey’s post hoc test revealed that only SIS/CA/Ag had statistical significance compared to the control group(P-value = 0.045), and there was no statistical significance between other groups.
Discussion
Skin repair requires several interactions between different cells and physiological sequences. The wound healing process consists of three distinct phases: inflammation, proliferation, and remodelling [35]. The first physiological reaction to a wound is local vasoconstriction and the formation of fibrin clots by platelets activation [36]. The fibrin clots lead to stasis of bleeding and make a scaffold for incoming inflammatory cells. During the inflammatory phase, different inflammatory cells, including neutrophils, monocytes, and adaptive immune cells, recruit to the injury site, respectively [37]. After three days, the inflammatory phase ends, and angiogenesis occurs. During the proliferation phase, local cells and circulating progenitor cells from bone marrow form new blood vessels [38]. While the proliferation of endothelial cells and activation of pericytes as a scaffold for endothelial cells emerge new blood vessels, the formation of contractile granulation tissue occurs by the invasion of resident fibroblasts to the clot. At this time, fibroblasts differentiate to myofibroblast to provide wound intension. Other fibroblasts synthesize ECM and alter the microenvironment from the inflammatory to proliferative state [39]. Following the proliferation phase, re-epithelialization and skins regeneration occur by proliferation and differentiation of epidermal stem cells [40]. Failure of the normal wound healing process in an orderly and timely sequence leads to the formation of chronic wounds with an estimated health care cost of $28.1 to $96.8 billion annually in the United States [41]. The failure of the healing process occurs due to numerous determinants, including diabetes, vascular diseases, overweight and obesity, and infections [42].
As demonstrated in this study, similar to previous studies, the application of decellularized SIS enhances the healing process compared with control group. Based on the "seed" and "soil" theories, mentioned barriers change the microenvironment or the "soil" addition to the local and circulating cells or "seed" [35]. Based on the microenvironment roles in this theory, it can be concluded that decellularized SIS enhances healing process by providing the appropriate microenvironment for skin regeneration. SIS contains a variety of collagens such as I, III, V and VI type, and also contains various cytokines, such as basic fibroblast growth factor (bFGF), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), and transforming growth factor b (TGF-b). These signals can promote cell growth, vascularization, and differentiation [17]. Moreover, these growth factors play an essential role in the wound healing process and improve angiogenesis as a critical component of wound healing [16]. Other features of decellularized SIS including mechanical characteristics and exceptional biocompatibility play significant role for skin regeneration, too [17]. Even though SIS has a good ability in suturing, its strength is low and by adding CA, the strength of the scaffold improves dramatically.
The scaffolds should be hydrophilic in order to absorb the secretions from the wound. Moreover, hydrophilic surfaces can facilitate the diffusion of oxygen and improve biocompatibility. CA is a very hydrophilic substance that has excellent liquid transport and water absorption properties [43]. SIS is hydrophobic and adding cellulose acetate to the SIS sheet, increases the hydrophilicity of the scaffold. These abilities make CA a very good candidate for wound dressing, since it can deeply absorb the wound drainage and also let oxygen reach the wound site. The increase in hydrophilicity of scaffolds will also lead to an increase in cell adhesion and migration.
Local infections are considered as another critical tackle for wound healing. Microorganisms such as bacteria rapidly colonize in skin wounds after skin injuries such as surgical incisions [44,45,46]. It is estimated that Surgical Site Infections (SSIs) are account for a cost of $3.3 billion annually in the United States [41]. As the possibility of triggering bacterial resistance, the application of chemotherapeutics/antibiotics is not recommended for preventing wound infections [47]. For generations, Ag has been utilized as an anti-bacterial material. Additionally, the anti-bacterial properties of Ag NPs are effective against antibiotic-resistant microorganisms [48]. The action mechanism of Ag NPs is not known correctly but it seems that anti-bacterial effects of Ag NPs are based on adhering to the membrane surface of bacteria and increasing membrane permeability. Moreover, Ag+ ions interfere with respiratory chain enzymes and modulate intracellular signalling pathways. Additionally, Ag produces reactive oxygen species(ROS) as harmful oxidative radicals for bacteria[49].
The antibacterial assessments revealed that the silver nanoparticles have a wide range of activity against Gram-positive and Gram-negative bacteria. Ag nanoparticles have effective antibacterial capabilities, due to their enormous surface area, when compared to other silver compounds. Microorganisms have a better chance of interacting with the silver due to its wide surface morphology [50]. Moreover, the MTT test reveals that adding Ag nanoparticles to the scaffold didn’t cause any toxicity. Adding Ag nanoparticles significantly increased the young modulus of the scaffold and also the scaffold faced its most hydrophilicity while Ag nanoparticles were added and the water contact angle of the SIS/CA/Ag was almost a sixth of the SIS scaffold after 20 s. The macroscopic images of the rats show that the wound site treated with the Ag nanoparticles scaffold had no infection and contraction.
As demonstrated in this study, enhancement of decellularized SIS silver promotes the efficacy of decellularized scaffold for healing full thickness wounds. In previous study, it was demonstrated that SIS ECM contains anti-inflammatory cytokines as crucial mediators for healing process[16]. The wound site infection leads to the expression of inflammatory cytokines and inhibiting the effects of anti-inflammatory cytokines including reinforcement of healing process [51]. As silver nano-particles prevent the bacterial infections, it can be hypothesized that enhancing decellularized SIS with silver nanoparticles can promotes the effects of SIS ECM by prevention of site infections.
Despite the findings of this study regarding the efficacy of decellularized SIS enhancement with silver and CA, this study has certain limitations. The first one is related to the follow-duration of the in vivo evaluations. The healing process of full thickness wounds contains different stages and lasts for a few months [35]. In this study we followed up the study only for two weeks and the effect of the scaffolds on the other stages of healing process was not assessed properly. Another limitation is related to the model of creating full-thickness wounds for in vivo assessment. there are several causes for creation of full thickness wounds including burning and lack of enough vasculature at the site of injury [52]. Our wound model was not appropriate to assess the efficacy of scaffolds for this special type of chronic wound. The data used for the in vivo studies are from rat models and there are a number of differences in the process of wound healing between rats and humans, accordingly, using a splinted wound model helps to move a step closer to recapitulating certain aspects of human wound healing by stabilizing the wound area, minimizing wound contraction, and enabling more precise monitoring and assessment of wound closure and tissue regeneration. According to these limitations, further studies with longer follow-up duration and different wound models and clinical evaluations are needed to evaluate the effect of our method for healing full-thickness wounds.
In this study, it has been demonstrated that SIS enhancement with CA and silver nanoparticles can promote the biomechanical properties and the efficacy of decellularized SIS for healing full-thickness wounds and can be considered as novel solution for chronic wounds potentially.
Conclusion
In conclusion, electro spun CA–Ag nanocomposites were incorporated into SIS with the notion that they can improve the mechanical properties, hydrophilicity, collagen deposition, skin regeneration, and wound closure. After including CA/Ag nanocomposites, the tensile strength and wettability of SIS scaffolds were dramatically enhanced. Furthermore, these biocompatible scaffolds were recruited for in vitro tests, which demonstrated that they had no toxicity.
References
Tottoli EM, Dorati R, Genta I, Chiesa E, Pisani S, Conti B (2020) Skin wound healing process and new emerging technologies for skin wound care and regeneration. Pharmaceutics 12(8):735
Zhong S, Zhang Y, Lim C (2010) Tissue scaffolds for skin wound healing and dermal reconstruction. Wiley Interdiscip Rev 2(5):510–525
Oliveira A, Simões S, Ascenso A, Reis CP (2020) Therapeutic advances in wound healing. J Dermatol Treat 20:1–21
Jorgensen AM, Varkey M, Gorkun A, Clouse C, Xu L, Chou Z et al (2020) Bioprinted skin recapitulates normal collagen remodeling in full-thickness wounds. Tissue Eng Part A 26(9–10):512–526
Dai C, Shih S, Khachemoune A (2020) Skin substitutes for acute and chronic wound healing: an updated review. J Dermatol Treat 31(6):639–648
Dong R, Guo B (2021) Smart wound dressings for wound healing. Nano Today 41:101290
Moeini A, Pedram P, Makvandi P, Malinconico M, d’Ayala GG (2020) Wound healing and antimicrobial effect of active secondary metabolites in chitosan-based wound dressings: a review. Carbohyd Polym 233:115839
Nazari H, Azadi S, Hatamie S, Zomorrod MS, Ashtari K, Soleimani M et al (2019) Fabrication of graphene-silver/polyurethane nanofibrous scaffolds for cardiac tissue engineering. Polym Adv Technol 30(8):2086–2099
Xu Q, Sigen A, Gao Y, Guo L, Creagh-Flynn J, Zhou D et al (2018) A hybrid injectable hydrogel from hyperbranched PEG macromer as a stem cell delivery and retention platform for diabetic wound healing. Acta Biomater 75:63–74
Shi L, Ronfard V (2013) Biochemical and biomechanical characterization of porcine small intestinal submucosa (SIS): a mini review. Int J Burns Trauma 3(4):173
Cao G, Huang Y, Li K, Fan Y, Xie H, Li X (2019) Small intestinal submucosa: superiority, limitations and solutions, and its potential to address bottlenecks in tissue repair. J Mater Chem B 7(33):5038–5055
Dussoyer M, Michopoulou A, Rousselle P (2020) Decellularized scaffolds for skin repair and regeneration. Appl Sci 10(10):3435
Parmaksiz M, Elçin AE, Elçin YM (2019) Decellularized bovine small intestinal submucosa-PCL/hydroxyapatite-based multilayer composite scaffold for hard tissue repair. Mater Sci Eng C 94:788–797
Andrée B, Bär A, Haverich A, Hilfiker A (2013) Small intestinal submucosa segments as matrix for tissue engineering. Tissue Eng Part B 19(4):279–291
Simman R (2023) Role of small intestinal submucosa extracellular matrix in advanced regenerative wound therapy. J Wound Care 32(Sup1a):S3–S10
Magden GK, Vural C, Bayrak BY, Ozdogan CY, Kenar H (2021) Composite sponges from sheep decellularized small intestinal submucosa for treatment of diabetic wounds. J Biomater Appl 36(1):113–127
Wang L, Wang W, Liao J, Wang F, Jiang J, Cao C et al (2018) Novel bilayer wound dressing composed of SIS membrane with SIS cryogel enhanced wound healing process. Mater Sci Eng C 85:162–169
Dos Santos AEA, Dos Santos FV, Freitas KM, Pimenta LPS, de Oliveira AL, Marinho TA et al (2021) Cellulose acetate nanofibers loaded with crude annatto extract: preparation, characterization, and in vivo evaluation for potential wound healing applications. Mater Sci Eng C 118:111322
Akturk A (2023) Enrichment of cellulose acetate nanofibrous scaffolds with retinyl palmitate and clove essential oil for wound healing applications. ACS Omega 8(6):5553–5560
Sofi HS, Akram T, Shabir N, Vasita R, Jadhav AH, Sheikh FA (2021) Regenerated cellulose nanofibers from cellulose acetate: Incorporating hydroxyapatite (HAp) and silver (Ag) nanoparticles (NPs), as a scaffold for tissue engineering applications. Mater Sci Eng C 118:111547
Fischer S, Thümmler K, Volkert B, Hettrich K, Schmidt I, Fischer K (2008) (eds) Properties and applications of cellulose acetate. Macromolecular symposia; Wiley Online Library.
Esmaeili E, Eslami-Arshaghi T, Hosseinzadeh S, Elahirad E, Jamalpoor Z, Hatamie S et al (2020) The biomedical potential of cellulose acetate/polyurethane nanofibrous mats containing reduced graphene oxide/silver nanocomposites and curcumin: antimicrobial performance and cutaneous wound healing. Int J Biol Macromol 152:418–427
Ezhilarasu H, Vishalli D, Dheen ST, Bay B-H, Srinivasan DK (2020) Nanoparticle-based therapeutic approach for diabetic wound healing. Nanomaterials 10(6):1234
Rajendran NK, Kumar SSD, Houreld NN, Abrahamse H (2018) A review on nanoparticle based treatment for wound healing. J Drug Deliv Sci Technol 44:421–430
Le Ouay B, Stellacci F (2015) Antibacterial activity of silver nanoparticles: a surface science insight. Nano Today 10(3):339–354
Marambio-Jones C, Hoek E (2010) A review of the antibacterial effects of silver nanomaterials and potential implications for human health and the environment. J Nanopart Res 12(5):1531–1551
Wilkinson L, White R, Chipman J (2011) Silver and nanoparticles of silver in wound dressings: a review of efficacy and safety. J Wound Care 20(11):543–549
Sandri G, Miele D, Faccendini A, Bonferoni MC, Rossi S, Grisoli P et al (2019) Chitosan/glycosaminoglycan scaffolds: the role of silver nanoparticles to control microbial infections in wound healing. Polymers 11(7):1207
Sharma D, Srivastava S, Kumar S, Sharma PK, Hassani R, Dailah HG et al (2023) Biodegradable electrospun scaffolds as an emerging tool for skin wound regeneration: a comprehensive review. Pharmaceuticals 16(2):325
Luo J-C, Chen W, Chen X-H, Qin T-W, Huang Y-C, Xie H-Q et al (2011) A multi-step method for preparation of porcine small intestinal submucosa (SIS). Biomaterials 32(3):706–713
Brown B, Lindberg K, Reing J, Stolz DB, Badylak SF (2006) The basement membrane component of biologic scaffolds derived from extracellular matrix. Tissue Eng 12(3):519–526
Keane TJ, Londono R, Turner NJ, Badylak SF (2012) Consequences of ineffective decellularization of biologic scaffolds on the host response. Biomaterials 33(6):1771–1781
Roy K, Sarkar C, Ghosh C (2015) Plant-mediated synthesis of silver nanoparticles using parsley (Petroselinum crispum) leaf extract: spectral analysis of the particles and antibacterial study. Appl Nanosci 5(8):945–951
Scherrer P (1918) Estimation of the size and internal structure of colloidal particles by means of röntgen. Nachr Ges Wiss Göttingen 2:96–100
Liang Y, He J, Guo B (2021) Functional hydrogels as wound dressing to enhance wound healing. ACS Nano 15(8):12687–12722
Clark R (2003) Fibrin is a many splendored thing. J Invest Dermatol 121:21–22
Wilgus TA, Roy S, McDaniel JC (2013) Neutrophils and wound repair: positive actions and negative reactions. Adv Wound Care 2(7):379–388
Kosaraju R, Rennert RC, Maan ZN, Duscher D, Barrera J, Whittam AJ et al (2016) Adipose-derived stem cell-seeded hydrogels increase endogenous progenitor cell recruitment and neovascularization in wounds. Tissue Eng Part A 22(3–4):295–305
Werner S, Krieg T, Smola H (2007) Keratinocyte-fibroblast interactions in wound healing. J Invest Dermatol 127(5):998–1008
Donati G, Rognoni E, Hiratsuka T, Liakath-Ali K, Hoste E, Kar G et al (2017) Wounding induces dedifferentiation of epidermal Gata6(+) cells and acquisition of stem cell properties. Nat Cell Biol 19(6):603–613
Sen CK (2021) Human wound and its burden: updated 2020 compendium of estimates. Adv Wound Care (New Rochelle) 10(5):281–292
FrykbergRobert G (2015) Challenges in the treatment of chronic wounds. Advances in Wound Care.
Liu X, Lin T, Gao Y, Xu Z, Huang C, Yao G et al (2012) Antimicrobial electrospun nanofibers of cellulose acetate and polyester urethane composite for wound dressing. J Biomed Mater Res B 100(6):1556–1565
Fields AC, Pradarelli JC, Itani KM (2020) Preventing surgical site infections: looking beyond the current guidelines. JAMA 323(11):1087–1088
Abbas M, Holmes A, Price J (2020) Surgical site infections following elective surgery. Lancet Infect Dis 20(8):898–899
Zabaglo M, Sharman T (2021) Postoperative wound infection. StatPearls
Simões D, Miguel SP, Ribeiro MP, Coutinho P, Mendonça AG, Correia IJ (2018) Recent advances on antimicrobial wound dressing: a review. Eur J Pharm Biopharm 127:130–141
Zewde B, Ambaye A, Stubbs Iii J, Raghavan D (2016) A review of stabilized silver nanoparticles–synthesis, biological properties, characterization, and potential areas of applications. Nanomed 4(1043):1–14
Lee SH, Jun B-H (2019) Silver nanoparticles: synthesis and application for nanomedicine. Int J Mol Sci 20(4):865
Konop M, Damps T, Misicka A, Rudnicka L (2016) Certain aspects of silver and silver nanoparticles in wound care: a minireview. J Nanomater 6:47
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M (2008) Growth factors and cytokines in wound healing. Wound Repair Regen 16(5):585–601
Morton LM, Phillips TJ (2016) Wound healing and treating wounds: Differential diagnosis and evaluation of chronic wounds. J Am Acad Dermatol 74(4):589–605 (quiz-6)
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Zahra Khorasani Zavareh, Reza Akbari Asbagh, Kiana Hajikhani, Asieh Heirani Tabasi, Hojjatollah Nazari, and Maryam Abbasi. The first draft of the manuscript was written by Zahra Khorasani Zavareh, Reza Akbari Asbagh, and Kiana Hajikhani and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Approval was granted by the Research Ethics Committees of Laboratory Animals of Tehran University of Medical Sciences (TUMS) approved the animal study (Number: IR.TUMS.AEC.1401.083/Date:10/04/2022).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zavareh, Z.K., Asbagh, R.A., Hajikhani, K. et al. Reinforcing decellularized small intestine submucosa with cellulose acetate nanofibrous and silver nanoparticles as a scaffold for wound healing applications. Mol Biol Rep 51, 658 (2024). https://doi.org/10.1007/s11033-024-09465-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09465-x