Abstract
Introduction
Tension-type headache (TTH) is common but challenging to manage due to limited effectiveness of conventional treatments. This study examines six complementary and alternative medicine (CAM) interventions through network meta-analysis to identify effective TTH management strategies.
Methods
We searched PubMed, Embase, Web of Science, Cochrane Library, OVID, CNKI, Wanfang, VIP, and CBM databases for randomized controlled trials on CAM for TTH treatment. Headache frequency and intensity were the primary outcomes. Methodological quality was evaluated on the basis of the Cochrane risk of bias tool. We used R software to conduct this Bayesian network meta-analysis. We used mean difference (MD) with 95% credible intervals (CI) to calculate the continuous outcomes and analyzed the percentages of the surface under the cumulative ranking (SUCRA) curve.
Results
In total, 32 randomized controlled trials (RCTs) with 2405 participants were analyzed. For reducing headache intensity, the network meta-analysis shows that acupuncture therapy combined with traditional Chinese medicine (AT_TCM), manual therapy (MT), psychological treatment (PT), and traditional Chinese medicine combined with acupuncture and manual therapy (TCM_AT_MT) are superior to Western medicine (WM). In the SUCRA curve, TCM_AT_MT is the best for reducing headache frequency (HF).
Conclusions
This review, assessed as low-quality evidence by GRADE, cautiously suggests potential benefits of PT over other CAM interventions for TTH and indicates TCM_AT_MT might better reduce HF. It proposes that combining CAM interventions could enhance outcomes. Due to the preliminary nature of these findings, further high-quality RCTs are essential to confirm these suggestions and provide clearer clinical guidance.
PROSPERO Registration Number
CRD42021252073.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The study was carried out to address the challenge of managing tension-type headache (TTH), which is common but difficult to treat effectively with conventional treatments. |
It aimed to examine six complementary and alternative medicine (CAM) interventions through network meta-analysis to identify effective TTH management strategies. |
What was learned from the study? |
From the study, we learned that PT may be more effective than other CAM interventions in reducing the intensity of headaches. Additionally, traditional Chinese medicine combined with acupuncture and manual therapy (TCM_AT_MT) appears to be particularly effective in reducing the frequency of headaches. |
These findings suggest that incorporating CAM interventions into treatment protocols for TTH could be beneficial. However, the results also highlight the need for further more rigorous studies to confirm these preliminary outcomes. |
Introduction
TTH is the most prevalent primary headache and ranks as the second most common chronic disease globally [1]. Data from the Global Burden of Disease (GBD) study estimate that in 2017, approximately 2.33 billion people globally suffered from TTH, and there were 882.4 million new cases of TTH worldwide in 2017 [2]. Significantly, TTH poses a greater social burden than migraines, incurring higher overall costs [3]. Despite this high prevalence, current management strategies for TTH are limited. The condition presents challenges not only to patients, but also to healthcare providers and society at large. In the field of headache disorders, despite the pathophysiology and etiology of migraines not being entirely clear, innovative and effective treatments have been developed and are widely used. The European Federation of Neurosciences (EFNS) guidelines currently recommend pharmacological management, primarily analgesics and nonsteroidal antiinflammatory drugs (NSAIDs), sometimes combined with caffeine-containing drugs [4]. However, the efficacy of these strategies decreases with prolonged headache duration, and drug therapy is not suitable for all patients due to various contraindications [4]. Additionally, up to 20% of patients with medication overuse headache (MOH) have TTH as the primary disorder [5,6,7]. Given these limitations, exploring a broader spectrum of management options, especially CAM, is essential. CAM, defined as practices that supplement mainstream medicine, enhances healthcare by addressing unmet needs and providing diverse, alternative solutions [8]. Examples of CAM interventions include chiropractics for headaches and low back pain [9,10,11,12,13] and acupuncture for various pain types [14,15,16,17,18,19]. The choice of CAM is invariably aimed at enhancing management outcomes.
This paper, therefore, conducts a literature search to compare and analyze six clinically recommended management approaches, aiming to identify the most effective CAM interventions for TTH. By bridging the gap between existing management options and the unmet needs in TTH management, this study contributes to a more comprehensive understanding and improved strategies for managing this prevalent condition.
Data and Methods
This study adheres to the Network Meta-Analysis extension of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA-NMA) guidelines [20]. It constitutes a systematic review, sourcing data exclusively from published literature, without involving trials or experiments. As such, this research did not require ethical approval since it is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. Registration of this study was completed with PROSPERO (CRD42021252073), and the original review protocol remains unaltered. The inclusion criteria are delineated below:
-
Study types: this review includes RCTs, without geographical restrictions but limited to studies published in Chinese and English.
-
Participant types: this analysis covers studies involving patients diagnosed with TTH. All included participants must meet the diagnostic criteria outlined in the current version of the International Classification of Headache Disorders (ICHD) or respective national standards derived from the ICHD. The study encompasses a diverse population without restrictions on gender, age, or nationality but excludes individuals with other types of primary or secondary headaches.
-
Intervention types: evaluated studies investigated the effectiveness of acupuncture therapy (AT), aerobic exercise (AE),manual therapy (MT), physical activity (PA), psychological treatment (PT), and traditional Chinese medicine (TCM) (see Table 1), including combinations of these methods in the observation group. The control group consisted of treatments with therapeutic effects, excluding routine nursing and blank controls.
-
Outcome measure types: included studies assessed headache frequency (HF, number of headache days per month) and intensity using a visual analogue scale (VAS, standardized 0–10 scale).
Search Strategy
A comprehensive search strategy was implemented across multiple databases, including PubMed, Embase, Web of Science, Cochrane Library, OVID, China National Knowledge Infrastructure (CNKI), Wanfang, VIP, and Chinese Biomedical Literature Database (CBM). An example of the Embase search is available in Supplementary Table 1. The final search was conducted on 1 June 2023.
Data Collection, Extraction, and Assessment
Study Selection and Data Extraction
Five researchers (Qin Lingli, Zhu Xueying, Cai Lizhen, Sun Weijia, Hu Guangdi) independently evaluated the retrieved articles on the basis of predefined inclusion and exclusion criteria, and systematically extracted relevant data. Discrepancies were resolved by consensus following discussion. Data extraction utilized a custom-made table, encompassing details such as authors, sample size, patient age, intervention measures, course of treatment, dropouts, adverse reactions, and follow-up.
Geometry of the Network
The treatment network will be evaluated using the available study data, which will be graphically represented. This evaluation will determine the adequacy of the comparisons within the network, considering the presence of closed loops that enable the assessment of consistency between direct and indirect comparisons. Additionally, the feasibility of conducting a network meta-analysis will be examined. In the network diagram, each dot symbolizes a treatment modality, with its size reflecting the number of participants receiving that treatment. The thickness of the lines indicates the quantity of studies involved; directly connected dots signify a direct comparison between two treatments, while unconnected dots are compared indirectly through the network meta-analysis.
Assessment of Risk of Bias
We employed the risk-of-bias assessment tool recommended by the Cochrane Institute [27]. Two researchers assessed the risk of bias in the included articles and resolved discrepancies through discussion. The evaluation criteria encompassed various aspects, including the randomization method, blinding of participants and researchers, blinding of evaluators, allocation concealment, completeness of outcomes, selective reporting of results, and other potential sources of bias. Each RCT included in the analysis received an assessment of either low risk, high risk, or unclear risk. An RCT was categorized as high quality if both the randomization method and allocation concealment were rated as low risk of bias, along with all other aspects receiving low-risk or unclear risk evaluations. Conversely, if either the randomization method or allocation concealment was deemed high risk of bias, the study was considered low quality, irrespective of the risk assessment of other aspects. When both randomization method and allocation concealment were assessed as low risk of bias, and at least one of the remaining five aspects was determined as high risk of bias, the RCT was classified as moderate quality.
GRADE Evaluation
The quality of evidence for each of the direct, indirect, and network impact assessments was determined on the basis of the primary outcomes [28, 29]. The assessment of evidence quality was conducted by considering five key factors: research limitations, indirectness, inconsistency, inaccuracy, and publication bias [28]. Publication bias was evaluated by examining funnel plot asymmetry. The assessment of indirect evidence quality involved estimating indirect comparisons from network diagrams, qualitatively assessing non-transitivity, and quantitatively evaluating inconsistencies through inconsistency testing [29].
Summary Measures
The VAS score and HF were reported as the MD with 95% CI, and the treatment effect was assessed using the SUCRA curve.
Data Analysis
Pairwise meta-analysis was conducted through direct comparisons using a random-effects model, followed by a Bayesian random-effects model employing the Markov-chain Monte Carlo method (MCMC) [30, 31]. Network meta-analysis involving all interventions was carried out assuming transitivity. Transitivity was defined as the assumption that the studies exhibited sufficient similarity in their distribution of effect modifiers, enabling the use of indirect comparisons as a valid method to compare two treatment regimens [32, 33]. Transitivity was assessed through a subjective comparative study of age characteristics, interventions, and methodological aspects. The entire network was first globally assessed, followed by a local evaluation of each treatment comparison using the node-splitting model [34,35,36]. The SUCRA was employed to evaluate the efficacy of each intervention. On the basis of the SUCRA values, line charts were generated to efficiently identify the most and least effective interventions for each outcome [37]. Bayesian hierarchical models with noninformative priors assigned to all model parameters were used for both the meta-analysis and network meta-analysis. I2 statistics were employed to assess trial heterogeneity in each meta-analysis [38]. In the network meta-analysis, it was assumed that no heterogeneity existed within the network due to the similarity in treatment approaches. A series of 50,000 simulations were conducted to ensure convergence. After applying a thinning factor of 1 and discarding the initial 20,000 simulations, the outputs were generated. Model convergence was assessed using the Gelman and Rubin diagnostic tests [39]. The MD and its 95% CI were estimated from the median and the 2.5th and 97.5th percentiles of the posterior distributions in the simulations. All analyses were performed using Review Manager 5.3 and R 3.6.3.
Assessment of Inconsistency
We employed both a consistency model and an inconsistency model, assessing the goodness of fit for each model on the basis of the deviance information criterion (DIC) values. A DIC difference of approximately five points was deemed significant, indicating consistency between the two models. In cases where the difference exceeded five points, we selected the model with the lower DIC value [40]. We employed node analysis to examine consistency and identify potential inconsistencies. A significance level of P < 0.05 was used to detect local inconsistency [41].
Risk of Bias across Studies
We assessed the potential presence of small sample utility or publication bias using an funnel plot. In this analysis, studies with large sample sizes and high event incidence rates had small standard errors, leading to a concentrated distribution in the upper part of the coordinate system. Conversely, studies with small sample sizes and low event incidence rates exhibited larger standard errors, resulting in a scattered distribution in the lower part of the coordinate system. We visually examined each included study for symmetry around the axis. Lack of symmetry would suggest the potential presence of publication bias, small sample size effects, or other contributing factors [42, 43].
Regression Analysis
Initially, we investigated potential sources of heterogeneity, including variables such as age, year of publication, sample size, duration of the disease course, and follow-up period. In cases where a minimum of ten studies were available, we conducted meta-regression analysis to examine the influence of these covariates on the study outcomes.
Results
Search Results
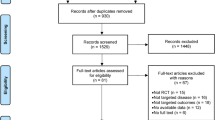
Through a preliminary search, we identified 1427 articles: 344 from CNKI, 231 from Wangfang, 98 from VIP, 126 from CBM, 124 from PubMed, 19 from Web of Science, 90 from Ovid, 98 from EMBASE, and 297 from Cochrane Library. We utilized Endnote X9 to eliminate duplicate articles, subsequently screening the remaining 545 articles in a systematic manner, which led to the inclusion of 32 articles in our study [75,76,77]. The flow chart of literature retrieval is shown in Fig. 1.
Summary of Network Geometry
The network diagram is presented in Fig. 2. In the VAS network diagram, 28 RCTs were included, along with 12 nodes, each representing a different intervention. Notably, the nodes for AT and WM are larger, signifying a higher number of patients receiving these treatments. The thickest line, between AT and WM, indicates that direct comparisons between these two treatments are most frequent. The presence of ten closed loops suggests good consistency. However, potential heterogeneity is indicated by indirect connections among three pairs of interventions: AE and AT_TCM, AT_TCM and sham acupuncture (SA), and WM and traditional Chinese medicine combined with psychological treatment (TCM_PT).
In the HF network diagram, 16 RCTs are included. This diagram features 13 nodes representing various intervention measures, with WM and AT having larger nodes. Lines of equal thickness between AT and SA, AT and WM, AT_TCM and WM, and MT and WM imply an equal number of direct comparison experiments. Six closed loops in this diagram also suggest good consistency. The potential for heterogeneity is again indicated, this time by indirect connections in four intervention pairs: SA and sham acupuncture combined with Western medicine (SA_WM), SA and MT, acupuncture therapy combined with physical activity (AT_PA) and PT, and MT and acupuncture therapy combined with manual therapy (AT_MT).
Characteristics of the Included Studies
The 32 studies included in our analysis encompassed 16 types of intervention measures: AE, AT, AT_MT, AT_TCM, AT_PA, MT, manual therapy combined with psychological treatment (MT_PT), PT, TCM, TCM_AT_MT, TCM_PT, PA, physical activity combined with manual therapy (PA_MT), SA, SA_WM, and WM. Analysis of the basic information, including age, sample size, treatment duration, and follow-up period, revealed no statistically significant differences among the studies. The total treatment duration ranged from 2 weeks to 12 weeks. A total of 20 studies mentioned dropouts and adverse reactions [45, 49, 51, 53, 56, 61,62,63,64,65,66,67,68,69,70,71,72,73,74,75], and 12 studies reported on follow-up outcomes [45, 49, 50, 62, 65, 67, 69, 71,72,73,74,75]. Four of these studies were three-arm trials, among which three arms in three studies [48, 51, 54] all met the inclusion criteria, whereas one of the interventions in one study [70] did not meet the inclusion and exclusion criteria of this article; hence, this intervention was excluded. In a four-arm study [65], one of the interventions did not meet the inclusion and exclusion criteria of this article; hence, this intervention was excluded. Table 2 summarizes the basic features of the included studies.
Risk of Bias in the Included Studies
We assessed the quality assessment by the Cochrane Handbook for Systematic Reviews of Interventions. A total of 4 articles [66,67,68,69] were evaluated as having low risk, 7 articles [62, 65, 70, 72,73,74,75] were evaluated as having uncertain risk of bias, and 21 articles [44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61, 63, 64, 71] were evaluated as having high risk of bias. The risk-of-bias map of the included articles is shown in Fig. 3.
The GRADE methodology provides a structured and transparent framework for evaluation of the evidence quality of systematic reviews and clinical practice guidelines. In this study, the quality of each outcome index was evaluated according to the GRADE methodology. The quality of all comparisons was graded, and the reasons for reduction were indicated (see Supplementary Table 2).
Results of Individual Studies
In terms of VAS score reduction, this study assessed 19 types of pairwise treatments. Meta-analysis showed that TCM_AT_MT [−3.2 (−4.4, −2.0)], TCM [−1.9 (−2.5, −1.3)] and AT [−2.6 (−3.8, −1.4)] were superior to AT_MT. AT_TCM [−1.8 (−3.1, −0.45)], MT [−2.1 (−4.0, −0.24)], PT [−3.9 (−6.7, −1.1)], and TCM [−0.74 (−1.4, −0.12)] were superior to WM. Furthermore, TCM_AT_MT [−1.3 (−1.8, −0.76)] and TCM_PT [−0.84 (−1.7, −0.03)] were superior to TCM. AT_TCM [−2.0 (−2.8, −1.2)] was superior to AT.
In terms of reducing the frequency of headache, we assessed 16 direct comparisons. Meta-analysis results showed that AT [−7.6 (−12.0, −3.0)] was superior to SA_WM. AT_MT [−6.5 (−7.3, −5.7)], PT [−4.7 (−5.6, −3.9)], and TCM [−7.0 (−9.6, −4.4)] were superior to WM. TCM_AT_MT [−3.3 (−5.6, −1.0)] and AT_TCM [−3.2 (−5.2, −1.2)] were superior to TCM. TCM_AT_MT [−4.3 (−6.9, −1.7)] was superior to AT_MT. Additionally, PA_MT [−1.4 (−2.7, −0.09)] was superior to PA. See Table 3 for details.
Synthesis of Results
VAS
In reducing the VAS score, PT was superior to AT [−2.38 (−0.14, −4.65)]; AT_TCM [−2.20 (−0.57, −3.85)], MT [−2.60 (−0.49, −4.79)], and PT [−3.34 (−0.90, −5.85)], TCM_AT_MT [−2.79 (−0.45, −5.15)] were superior to AT_MT; AT_TCM [2.77 (4.75, 0.71)], MT [3.18 (5.59, 0.71)], MT_PT [3.42 (6.63, 0.12)], and PT [3.92 (6.62, 1.16)], TCM_AT_MT [3.38 (0.36, 6.28)] were superior to SA; AT_TCM [2.03 (3.11, 0.95)], MT [2.43 (4.12, 0.80)], and PT [3.17 (5.25, 1.14)], TCM_AT_MT [2.63 (5.09, 0.17)] were superior to WM. See Table 4 for details.
HF
There were no statistically significant differences among treatments in reducing HF. See Table 5 for details.
SUCRA Curve
In terms of reducing VAS scores, the order of efficacy, as determined by SUCRA scores from highest to lowest, is as follows: PT at 84.7%, TCM_AT_MT at 73.7%, MT_PT at 72.6%, MT at 70.1%, AE at 69.9%, AT_TCM at 63.1%, TCM_PT at 56.7%, TCM at 38.0%, AT at 35.2%, WM at 15.7%, AT_MT at 13.4%, and SA at 6.6%. When it comes to reducing HF, the hierarchy of efficacy based on SUCRA scores from highest to lowest is as follows: TCM_AT_MT at 80.8%, AT_TCM at 72.4%, TCM at 63.5%, AT_MT at 62.8%, MT at 60.3%, PT at 56.6%, PA_MT at 54.6%, AT_PA at 54.7%, PA at 47.1%, AT at 40.2%, WM at 27.0%, SA at 18.2%, and SA_WM at 12.3%. Further details can be found in Fig. 4.
Exploration for Inconsistency
-
(1)
VAS score: The convergence degree of the model for the VAS score can be judged by the trajectory map, density map, and Brooks–Gelman–Rubin diagnostic map. After 20,000 adapts and 50,000 iterations, the median value and 97.5% value of the reduction factor approximated 1 and stabilized, indicating that the model had a good convergence degree and could effectively predict data. After calling JAGS to run with the gemtc package in R, an inconsistency model and a consistency model were obtained. In the consistency model, DIC = 108.22283 and I2 = 2%, whereas in the inconsistency model, DIC = 109.91461 and I2 = 2%. The DIC difference was < 5, indicating that the models fitted consistently. The node-splitting test showed that P > 0.05, reflecting the absence of significant inconsistency between the results of direct comparison and indirect comparison.
-
(2)
HF: The convergence degree of the model for headache frequency can be judged by the trajectory map, density map, and Brooks–Gelman–Rubin diagnostic map. After 20,000 adapts and 50,000 iterations, the median value and 97.5% value of the reduction factor approximated 1 and reached stability, indicating that the model had a good convergence degree and could effectively predict data. An inconsistency model and a consistency model were obtained as for the VAS score. For the consistency model, DIC = 69.12057 and I2 = 7%, while for the inconsistency model, DIC = 67.92035, I2 = 3%. The DIC difference was < 5, indicating that the models fitted consistently. The node-splitting test showed that P > 0.05, reflecting that there was no significant inconsistency between the results of direct comparison and indirect comparison.
Risk of Bias across Studies
According to the funnel plot (Fig. 5), the VAS points were concentrated in the upper part of the funnel plot and were largely symmetrical along the central axis, but several studies fell outside the funnel plot. This indicates that the presence of a small sample size effect is less likely, but heterogeneity may exist. However, the HF points fall mostly along the central axis, indicating that small sample size effect and heterogeneity are less likely to exist.
Regression Analysis
Through regression analysis of publication year and sample size, the CI of beta coefficients contained 0, indicating that the covariates were meaningless. The publication year and sample size had no statistically significant influence on the research results.
Discussion
Summary of Evidence
We undertook a thorough and systematic review and meta-analysis, incorporating criteria encompassing six distinct intervention measures. These interventions could be combined to create novel treatment strategies. Regarding control groups, beyond standard nursing and placebo controls, alternative therapeutic measures were also considered as control interventions. Through rigorous literature screening, we ultimately selected 32 studies, covering 16 diverse intervention measures. We employed the Cochrane Handbook for Systematic Reviews of Interventions to assess the risk of bias in the studies, which comprised 4 low-risk articles, 7 articles of uncertain risk, and 21 high-risk articles. From this, it is not difficult to observe that the overall risk of the included literature is relatively high, which can affect the quality of the literature and consequently influence the outcome analysis. Consequently, we utilized the GRADE methodology to assess the quality of evidence and implement downgrading strategies in our study, thus improving the transparency of our reported research findings. According to GRADE methodology, the highest level of recommendation strength was deemed moderate for comparing PT with WM in VAS-related interventions. Pairwise analysis revealed that PT was significantly more effective than WM [−3.9 (−6.7, −1.1)], while results from the synthesis analysis further confirmed the superiority of PT over WM [3.17 (5.25, 1.14)]. In the comparison of interventions for HF, the highest level of recommendation was moderate, encompassing comparisons such as AT versus SA_WM, AT_MT versus WM, PT versus WM, PA_MT versus PA, AT_PA versus AT, PA versus AT, and PA versus AT_PA. Pairwise analysis revealed that AT [−7.6 (−12.0, −3.0)] was significantly more effective than SA_WM, AT_MT [−6.5 (−7.3, −5.7)], and PT [−4.7 (−5.6, −3.9)] outperformed WM, while PA_MT [−1.4 (−2.7, −0.09)] demonstrated superiority over PA. However, the overall assessment of interventions comparing VAS and HF was rated as low, leading us to approach the interpretation of final results with increased caution.
-
1.
According to the results from SUCRA rankings and comprehensive analysis results, PT demonstrates a significant advantage in reducing headache intensity. Pairwise analysis indicated that PT [−3.9 (−6.7, −1.1)] was superior to WM. Synthesis analysis further revealed the superiority of PT over AT (−2.38 (−0.14, −4.65)], AT_MT [−3.34 (−0.90, −5.85)], SA [3.92 (6.62, 1.16)], and WM [3.17 (5.25, 1.14)]. Although the evidence quality, as per GRADE analysis, is considered low, existing literature suggests a direct link between TTH and symptoms such as fatigue, stress, and inadequate sleep, with psychological therapies providing relief [76]. Psychological interventions, including electromyography biofeedback, relaxation training, and cognitive behavioral therapy, have been noted to alleviate these symptoms [77]. Increasing evidence supports mindfulness-based therapies, encompassing mindfulness meditation and cognitive techniques, relaxation, and stress management, as well as acceptance and commitment therapy, a form of behavioral therapy [78].
-
2.
According to the SUCRA rankings, TCM_AT_MT exhibited a significant advantage in reducing the frequency of headache occurrence, even though the results from the integrated analysis were not statistically significant. Pairwise analysis indicated that TCM_AT_MT was superior to TCM [3.3 (−5.6, − 1.0)] and AT_MT [−4.3 (−6.9, −1.7)]. Literature review suggests that combined interventions are more effective when single adjunctive treatment approaches fail [79,80,81,82]. PT, AE, and MT in particular may be beneficial in the management of TTH [83,84,85,86]. The efficacy of AT in the treatment of TTH is demonstrated in a systematic review [87], and the safety of AT in the treatment of TTH has significant advantages compared with amitriptyline. TCM is a characteristic treatment in China, where it is a highly accepted therapy. There are systematic studies showing the potential advantages of Chinese herbal medicine in the treatment of TTH [88]. Each of the included interventions has been reported to have good efficacy and potential advantages, and a combination of complementary and alternative therapies is a good choice based on accurate physician judgment and patient acceptance.
-
3.
In the heterogeneity test, the P-values were all greater than 0.05, indicating that there is less possibility of heterogeneity among the studies, and the studies are homogeneous (see Supplementary Table 3).
Limitations
Among the included articles, 4 were assessed as low risk, 7 had an uncertain risk of bias, and 21 were deemed high risk. This highlights a common limitation in many CAM interventions, characterized by a lack of high-quality scientific research supporting their efficacy and safety. Furthermore, these studies often suffer from small sample sizes, lax designs, or biases. We employed the GRADE analysis method to evaluate the quality of evidence, ensuring transparency and fairness.
Minimal differences in SUCRA data can result in unstable rankings of intervention measures. This is due to regional variations in CAM, where different practitioners may offer diverse treatments such as acupuncture, massage, herbal remedies, etc. This diversity in CAM, coupled with low standardization in treatment, makes it challenging to find similar studies for synthesis analysis among numerous literature, resulting in limited original studies meeting inclusion criteria, thus leading to unstable rankings of intervention measures. Within this study, there was little disparity among AE, MT, MT_PT, and TCM_AT_MT in the recommended order of intervention measures to reduce the VAS score. Similarly, there was minimal variation among AT_MT, PT, PA_MT, and TCM in the recommended order of intervention measures to reduce HF. This inconsistency in rankings arises from the scarcity of similar studies. Additionally, the long-term efficacy and duration of CAM remain unclear, underscoring the need for more standardized, long-term studies in subsequent clinical research for evaluation.
We limited our literature inclusion to English and Chinese languages, potentially overlooking relevant studies in other languages. Variations in CAM across different countries underscore the importance of considering a broader linguistic scope. While our study focused on English and Chinese literature, future researchers are encouraged to supplement our work by incorporating studies from diverse linguistic backgrounds.
Regrettably, our study was confined to RCTs to uphold the integrity of our research. However, this stringent criterion meant that numerous valuable single-arm studies could not be included. These non-RCT studies might offer significant evidence supporting the effectiveness of CAM for TTH, despite potential biases inherent in such literature.
In many instances, particularly with novel or less common treatment modalities, there might be insufficient research or data to definitively establish their efficacy. In such scenarios, employing non-informative priors in Bayesian network meta-analysis ensures that the analysis remains uninfluenced by irrelevant or uncertain information, while allowing new data to impartially influence the conclusions. In our Bayesian network meta-analysis, non-informative priors are typically utilized to minimize the impact of prior information on the final results. This approach aims to enhance objectivity in the analysis outcomes, ensuring they more accurately reflect the actual data collected, rather than being swayed by prior biases.
Conclusions
According to the GRADE methodology, the evidence supporting the conclusions of this review is considered of low quality. Therefore, while the conclusions may suggest potential trends, they should be interpreted with caution and regarded primarily as a clinical reference. The review tentatively suggests that PT could offer some benefits over other CAM interventions in reducing VAS scores for individuals with TTH, advocating for the potential value of incorporating physical and emotional relaxation strategies. Additionally, the review tentatively identifies TCM_AT_MT as a potentially more effective option for reducing HF, though these findings are preliminary. It is also suggested that a combined approach, integrating multiple CAM interventions, may be more beneficial than using single treatments in isolation. However, due to the low quality of the existing evidence, these conclusions should be viewed as hypotheses rather than definitive outcomes. Consequently, conducting further high-quality RCTs is crucial to validate these findings and provide more definitive guidance for clinical practice.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Repository SS. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;386(9995):743–800.
Deuschl G, Beghi E, Fazekas F, Varga T, Christoforidi KA, Sipido E, Bassetti CL, Vos T, Feigin VL. The burden of neurological diseases in e¡Europe: an analysis for the global burden of disease study 2017. Lancet Public Health. 2020;5(10):551–67.
Stovner L, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, Steiner T, Zwart J. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210.
Bendtsen L, Evers S, Linde M, Mitsikostas D, Sandrini G, Schoenen J. Efns guideline on the treatment of tension-type headache–report of an Efns task force. Eur J Neurol. 2010;17(11):1318–25.
Diener H-C, Dodick D, Evers S, Holle D, Jensen RH, Lipton RB, Porreca F, Silberstein S, Schwedt T. Pathophysiology, prevention, and treatment of medication overuse headache. Lancet Neurol. 2019;18(9):891–902.
Bottiroli S, Allena M, Sances G, De Icco R, Avenali M, Fadic R, Katsarava Z, Lainez MJ, Goicochea MT, Bendtsen L, et al. Psychological, clinical, and therapeutic predictors of the outcome of detoxification in a large clinical population of medication-overuse headache: a six-month follow-up of the comoestas project. Cephalalgia. 2019;39(1):135–47.
Monteith TS, Oshinsky ML. Tension-type headache with medication overuse: pathophysiology and clinical implications. Curr Pain Headache Rep. 2009;13(6):463–9.
Ernst E. The usage of complementary therapies by dermatological patients: a systematic review. Br J Dermatol. 2000;142(5):857–61.
Chaibi A, Tuchin PJ, Russell MB. Manual therapies for migraine: a systematic review. J Headache Pain. 2011;12(2):127–33.
Walker BF, French SD, Grant W, Green S. A Cochrane review of combined chiropractic interventions for low-back pain. Spine. 2011;36(3):230–42.
Bronfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopat. 2010;18(1):1–33.
Bronfort G, Assendelft WJ, Evans R, Haas M, Bouter L. Efficacy of spinal manipulation for chronic headache: a systematic review. J Manipulative Physiol Ther. 2001;24(7):457–66.
Cherkin DC, Mootz RD. Chiropractic in the United States: training, practice, and research. AHCPR publication No; 1997. p. 98–002
Liu L, Skinner M, McDonough S, Mabire L, Baxter GD. Acupuncture for low back pain: an overview of systematic reviews. Evid-Based Complement Altern Med. 2015. https://doi.org/10.1155/2015/328196.
Manyanga T, Froese M, Zarychanski R, Abou-Setta A, Friesen C, Tennenhouse M, Shay BL. Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC Complement Altern Med. 2014;14(1):1–9.
Vickers AJ, Cronin AM, Maschino AC, Lewith G, MacPherson H, Foster NE, Sherman KJ, Witt CM, Linde K, Acupuncture Trialists’ Collaboration f.t, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172(19):1444–53.
Cherkin DC, Sherman KJ, Avins AL, Erro JH, Ichikawa L, Barlow WE, Delaney K, Hawkes R, Hamilton L, Pressman A, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169(9):858–66.
Yuan J, Purepong N, Kerr DP, Park J, Bradbury I, McDonough S. Effectiveness of acupuncture for low back pain: a systematic review. Spine. 2008;33(23):887–900.
Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture for patients with chronic neck pain. Pain. 2006;125(1–2):98–106.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Britannica, The Editors of Encyclopaedia. Acupuncture. 2024. https://www.britannica.com/science/acupuncture. Accessed 3 Mar 2024.
Sagiv MS. Oxygen uptake and anaerobic performances. In: Sagiv MS, editor. Basic exercise physiology. Cham: Springer; 2020. p. 3–17. https://doi.org/10.1007/978-3-030-48806-2.
Bizzarri P, Foglia A. Manual therapy: art or science? In: Physical Therapy Effectiveness, pp. 1–26. IntechOpen, London 2020. https://www.intechopen.com/chapters/70681. Accessed 29 Feb 2024.
Physical Activity. https://www.who.int/news-room/fact-sheets/detail/physical-activity. Accessed 3 Mar 2024.
Claiborn CD, Psychotherapy. 2024. https://www.britannica.com/science/psychotherapy. Accessed 3 Mar 2024.
Britannica, The Editors of Encyclopaedia. Traditional Chinese Medicine. 2024. https://www.britannica.com/science/traditional-Chinese-medicine. Accessed 3 Mar 2024.
Higgins JP, Altman DG, Gøtzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011. https://doi.org/10.1136/bmj.d5928.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Puhan M, Schunemann H, Murad M, Li T, Brignardello-Petersen R, Singh J, Kessels A, Guyatt G, et al. A GRADE working group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:5630.
Lu G, Ades A. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23(20):3105–24.
Mills EJ, Ioannidis JP, Thorlund K, Schunemann HJ, Puhan MA, Guyatt GH. How to use an article reporting a multiple treatment comparison meta-analysis. JAMA. 2012;308(12):1246–53.
Baker SG, Kramer BS. The transitive fallacy for randomized trials: if a bests b and b bests c in separate trials, is a better than c. BMC Med Res Methodol. 2002;2(1):1–5.
Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med. 2013;159(2):130–7.
White IR, Barrett JK, Jackson D, Higgins JP. Consistency and inconsistency in network meta- analysis: model estimation using multivariate meta-regression. Res Synt Methods. 2012;3(2):111–25.
Veroniki AA, Vasiliadis HS, Higgins JP, Salanti G. Evaluation of inconsistency in networks of interventions. Int J Epidemiol. 2013;42(1):332–45.
Dias S, Welton NJ, Caldwell D, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7–8):932–44.
Salanti G, Ades A, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions. Hoboken, NJ: John Wiley & Sons; 2019.
Gelman A, Rubin DB. Inference from iterative simulation using multiple sequences. Stat Sci. 1992. https://doi.org/10.1214/ss/1177011136.
Spiegelhalter DJ, Best NG, Carlin BP, Van Der Linde A. Bayesian measures of model complexity and fit. J R Stat Soc: Ser B (Stat Methodol). 2002;64(4):583–639.
Valkenhoef G, Dias S, Ades A, Welton NJ. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res Synth Methods. 2016;7(1):80–93.
Richard J, Pillemer DB, Light RJ. Summing up: the science of reviewing research. Cambridge, MA: Harvard University Press; 2009.
Sutton AJ, Duval SJ, Tweedie R, Abrams KR, Jones DR. Empirical assessment of effect of publication bias on meta-analyses. BMJ. 2000;320(7249):1574–7.
Zheng K, Lu R, Wei Y. Observation of clinical efficacy of balanced acupuncture in the treatment of primary tension-type headache. Chin Manip Rehabil Med. 2020;14:17–9.
Nie W, Zhang L, Li S. Clinical observation on tension-type headache treated with oblique needling through tendons. Chin J Integr Tradit West Med. 2019;18:156–7.
Zhang Y. Acupuncture and massage combined with danzhen headache capsules in the treatment of tension-type headache effect observation. Diet Health. 2019;6:99–100.
Wang Y, Zhao Z, Chen D. Observation on the effect of “lao shi zhen” in the treatment of chronic tension-type headache. Shanghai J Acupunct Moxibustion. 2018;09:1003–6.
Ma Y, Mai D, An N. Naprapathy combined with psychotherapy in the treatment of tension headache in 40 cases of clinical observation. China J Tradit Chin Med Pharm. 2017;12:5699–701.
Cai X, Yang Z, Li Y. Clinical observation of electroacupuncture combined with naprapathy in the treatment of chronic tension headache. J Acupunct Tuina Sci. 2017;15:120–5.
Huang L, Yin Y, Wu S. 40 cases of tension headache treated with acupuncture and reasonable tendon manipulation. J Extern Ther Tradit Chin Med. 2017;04:32–3.
Wu Y, Lin L, Xiao Y. Analysis of the efficacy of danzhen headache capsules combined with acupunc- ture and massage in the treatment of tension-type headache. China Pract Med. 2016;28:197–8.
Guo S. Acupuncture combined with chai ge jie ji decoction in the treatment of 40 cases of tension headache. Chin Med Modern Distance Educ China. 2015;03:79–80.
Zhao B, Li C, Wang Y. Clinical observation on treatment of tension-type headache with cold coagulation and blood stasis syndrome with modified gegen decoction and acupuncture. Beijing J Tradit Chin Med. 2014;03:288–9.
Li L. Treatment of 40 cases of tension-type headache with toutongning capsules combined with acupuncture. Med People. 2014;08:160–160.
Fu M. Clinical observation of acupuncture in the treatment of tension-type headache. J Basic Chin Med. 2013;07:810–1.
Yan W, Liu Q, Yan Y. Acupuncture rehabilitation combined with Chinese medicine treatment of tension headache analysis. China Modern Doctor. 2012;50:80–1.
Sun Y, Guo Y. Clinical observation on the treatment of tension-type headache with plum-blossom needle percussopuncture. J Changchun Univ Chin Med. 2012;28:671–2.
Fan C, Qian LF. Soothing the liver, relieving the depression, and nourishing the blood and emolliating the liver for the treatment of tension headache. Modern J Integr Tradit Chin West Med. 2011;20(24):3035–6.
Zhang X, Peng C. Acupuncture treatment for tension-type headache based on root and branch theory: a study of 30 cases. J Tradit Chin Med. 2011;52(06):521–2.
Yan B. Clinical observation on the treatment of tension headache with the combination of traditional Chinese medicine and psychotherapy. J Basic Chin Med. 2010;16:227–8.
Wei S. Comprehensive treatment of tension headache. China Modern Med. 2009;16(3):30–1.
Zhang L, Zhang Y, Hui-lin L. Randomized controlled trial of acupuncture treatment for chronic tension- type headache. J Cap Med Univ. 2009;30:441–4.
Chen X, Huang J, Huang D. Clinical observation of tension-type headache treated by internal administration of Chinese medicine combined with acupoint injection. J Liaoning Univ Tradit Chin Med. 2006;8:73–4.
Liu J, Liu X. Observation on the effect of shuji zhitong decoction in the treatment of tension headache. Lishizhen Med Materia Medica Res. 2005;16:563–4.
Schiller J, Karst M, Kellner T, Zheng W, Niederer D, Vogt L, Eckhardt I, Beissner F, Korallus C, Sturm C, et al. Combination of acupuncture and medical training therapy on tension type headache: results of a randomised controlled pilot study. Cephalalgia. 2021;41(8):879–93.
Mohamadi M, Rojhani-Shirazi Z, Assadsangabi R, Rahimi-Jaberi A. Can the positional release technique affect central sensitization in patients with chronic tension-type headache? A randomized clinical trial. Arch Phys Med Rehabil. 2020;101(10):1696–703.
Gildir S, Tuzun EH, Eroglu G, Eker L. A randomized trial of trigger point dry needling versus sham needling for chronic tension-type headache. Medicine. 2019;98(8):e14520.
Deodato M, Guolo F, Monticco A, Fornari M, Manganotti P, Granato A. Osteopathic manip- ulative therapy in patients with chronic tension-type headache: a pilot study. J Am Osteopath Assoc. 2019;119(10):682–7.
Alvarez-Melcon A, Valero-Alcaide R, Atin-Arratibel M, Melcon-Alvarez A, Beneit-Montesinos J. Effects of physical therapy and relaxation techniques on the parameters of pain in university students with tension-type headache: a randomised controlled clinical trial. Neurologia (English Edition). 2018;33(4):233–43.
Sertel M, Bakar Y, Simsek TT. The effect of body awareness therapy and aerobic exercises on pain and quality of life in the patients with tension type headache. Afr J Tradit Complement Altern Med. 2017;14(2):288–310.
Damapong P, Kanchanakhan N, Eungpinichpong W, Putthapitak P, Damapong P. A randomized controlled trial on the effectiveness of court-type traditional Thai massage versus amitriptyline inpatients with chronic tension-type headache. Evid-Based Complement Altern Med. 2015. https://doi.org/10.1155/2015/930175.
Bougea AM, Spandideas N, Alexopoulos EC, Thomaides T, Chrousos GP, Darviri C. Effect of the emotional freedom technique on perceived stress, quality of life, and cortisol salivary levels in tension-type headache sufferers: a randomized controlled trial. Explore. 2013;9(2):91–9.
Wang K, Svensson P, Arendt-Nielsen L. Effect of acupuncture-like electrical stimulation on chronic tension-type headache: a randomized, double-blinded, placebo-controlled trial. Clin J Pain. 2007;23(4):316–22.
Karst M, Reinhard M, Thum P, Wiese B, Rollnik J, Fink M. Needle acupuncture in tension-type headache: a randomized, placebo-controlled study. Cephalalgia. 2001;21(6):637–42.
Karst M, Rollnik JD, Fink M, Reinhard M, Piepenbrock S. Pressure pain threshold and needle acupuncture in chronic tension-type headache–a double-blind placebo-controlled study. Pain. 2000;88(2):199–203.
Lyngberg A, Rasmussen B, Jørgensen T, Jensen R. Incidence of primary headache: a danish epidemiologic follow-up study. Am J Epidemiol. 2005;161(11):1066–73.
Sun-Edelstein C, Mauskop A. Complementary and alternative approaches to the treatment of tension- type headache. Curr Pain Headache Rep. 2012;16(6):539–44.
Gu Q, Hou J-C, Fang X-M. Mindfulness meditation for primary headache pain: a meta-analysis. Chin Med J. 2018;131(07):829–38.
Falsiroli Maistrello L, Geri T, Gianola S, Zaninetti M, Testa M. Effectiveness of trigger point manual treatment on the frequency, intensity, and duration of attacks in primary headaches: a systematic review and meta-analysis of randomized controlled trials. Front Neurol. 2018;9:254.
Falsiroli Maistrello L, Rafanelli M, Turolla A. Manual therapy and quality of life in people with headache: systematic review and meta-analysis of randomized controlled trials. Curr Pain Headache Rep. 2019;23(10):1–14.
Bot MN, Wijer A, Pool J, Bronkhorst EM, Kalaykova SS, Creugers NH, Putte EM. Physical treatments reduce pain in children with tension-type headache: a systematic review and meta-analysis. J Oral Facial Pain Headache. 2020;34:240–54.
Kamonseki DH, Lopes EP, Meer HA, Calixtre LB. Effectiveness of manual therapy in patients with tension-type headache. A systematic review and meta-analysis. Disabil Rehabil. 2022;44(10):1780–9.
Tornøe B, Andersen LL, Skotte JH, Jensen R, Jensen C, Madsen BK, Gard G, Skov L, Hallstrom I. Specific strength training compared with interdisciplinary counseling for girls with tension- type headache: a randomized controlled trial. J Pain Res. 2016;9:257.
Andersen CH, Jensen RH, Dalager T, Zebis MK, Sjøgaard G, Andersen LL. Effect of resistance training on headache symptoms in adults: secondary analysis of a RCT. Musculoskelet Sci Pract. 2017;32:38–43.
Krøll LS, Hammarlund CS, Linde M, Gard G, Jensen RH. The effects of aerobic exercise for persons with migraine and co-existing tension-type headache and neck pain. A randomized, controlled, clinical trial. Cephalalgia. 2018;38(12):1805–16.
Espi-Lopez GV, Zurriaga-Llorens R, Monzani L, Falla D. The effect of manipulation plus massage therapy versus massage therapy alone in people with tension-type headache. A randomized controlled clinical trial. Eur J Phys Rehabil Med. 2016;52(5):606–17.
Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Shin B-C, Vickers A, White AR. Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev. 2016. https://doi.org/10.1002/14651858.CD001218.pub3.
Fu G, Shen W, Zhang L, Guo C, Lu Y, Liu S, Liang X, Wei J, Liu H, Zhang Y. Systematic evaluation of the efficacy and safety of Chinese medicine in the treatment of tension-type headache. Chin J Integr Med Cardio-Cerebrovasc Dis. 2022;01:37–45.
Acknowledgements
We greatly appreciate the support from, the NATCM TCM Inheritance and Innovation “Hundred-Thousand-Ten Thousand” Talents Project (QiHuang Scholar), National TCM Leading Personnel Support Program NATCM Personnel and Education Department [2018] No. 12., and the Science and Technology Innovation Project of the China Academy of Traditional Chinese Medicine (no.: CI2021B012). We thank the participants of the study.
Funding
This research was supported by the NATCM TCM Inheritance and Innovation “Hundred-Thousand-Ten Thousand” Talents Project (QiHuang Scholar), National TCM Leading Personnel Support Program NATCM Personnel and Education Department [2018] No. 12., and the Chinese Academy of Traditional Chinese Medicine Science and Technology Innovation Project under grant (no.: CI2021B012). Contributions to the study, such as the research itself and the Rapid Service Fee were financed by these three sources.
Author information
Authors and Affiliations
Contributions
Qin Lingli and Song Ping conceived and participated in the design of the study and established the initial protocol. Qin Lingli and Li Xian drafted the manuscript. Qin Lingli, Song Ping, Li Xian, Xu Feng, Zhang Lu, Yang Longhui, and Zhang Yunling participated in the revision of the manuscript. Qin Lingli, Zhu Xueying, Cai Lizhen, Hu Guangdi, and Sun Weijia participated in data extraction. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Qin, L., Song, P., Li, X. et al. Tension-Type Headache Management: A Systematic Review and Network Meta-analysis of Complementary and Alternative Medicine. Pain Ther (2024). https://doi.org/10.1007/s40122-024-00600-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40122-024-00600-x